Summary
The Asia-Pacific region is home to more than half of the global population and accounted for 62·6% of global deaths due to liver diseases in 2015. 54·3% of global deaths due to cirrhosis, 72·7% of global deaths due to hepatocellular carcinoma, and more than two-thirds of the global burden of acute viral hepatitis occurred in this region in 2015. Chronic hepatitis B virus (HBV) infection caused more than half of the deaths due to cirrhosis in the region, followed by alcohol consumption (20·8%), non-alcoholic fatty liver disease (NAFLD; 12·1%), and chronic infection with hepatitis C virus (HCV; 15·7%). In 2015, HBV accounted for about half the cases of hepatocellular carcinoma in the region. Preventive strategies for viral hepatitis-related liver disease include increasing access to clean drinking water and sanitation. HBV vaccination programmes for neonates have been implemented by all countries, although birth-dose coverage is extremely suboptimal in some. Availability of screening tests for blood and tissue, donor recall policies, and harm reduction strategies are in their initial stages in most countries. Many governments have put HBV and HCV drugs on their essential medicines lists and the availability of generic versions of these drugs has reduced costs. Efforts to eliminate viral hepatitis as a public health threat, together with the rapid increase in per-capita alcohol consumption in countries and the epidemic of obesity, are expected to change the spectrum of liver diseases in the Asia-Pacific region in the near future. The increasing burden of alcohol-related liver diseases can be contained through government policies to limit consumption and promote less harmful patterns of alcohol use, which are in place in some countries but need to be enforced more strictly. Steps are needed to control obesity and NAFLD, including policies to promote healthy lifestyles and regulate the food industry. Inadequate infrastructure and insufficient health-care personnel trained in liver diseases are issues that also need to be addressed in the Asia-Pacific region. The policy response of most governments to liver diseases has thus far been inadequate and poorly funded. There must be a renewed focus on prevention, early detection, timely referral, and research into the best means to introduce and improve health interventions to reduce the burden of liver diseases in the Asia-Pacific region.
Introduction
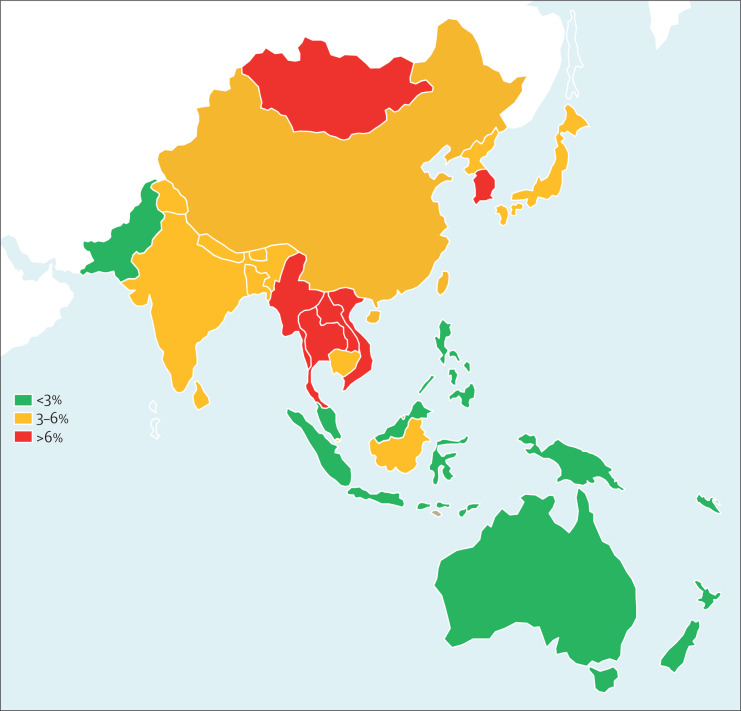
According to the third round of WHO's 2015 Global Health Estimates (GHE),1 liver diseases caused 1 312 480 (4·6%) of 28 444 814 deaths in the Asia-Pacific region in 2015, compared with 72 437 (2·7%) of 2 649 742 in the USA and 197 179 (2·1%) of 9 278 557 in Europe. The Asia-Pacific region accounts for 62·6% of 2 095 207 deaths due to liver diseases globally for that year. In Asian countries, the median proportion of deaths attributable to liver disease was 3·9% (range 1·86–13·9). By contrast, liver diseases caused 2·05% of all deaths in Australia and 1·33% of those in New Zealand in 2015 (figure 1 ), with underlying aetiologies varying between countries (figure 2 ).1
Figure 1.
Liver-related deaths as proportion of overall deaths in the Asia-Pacific region1
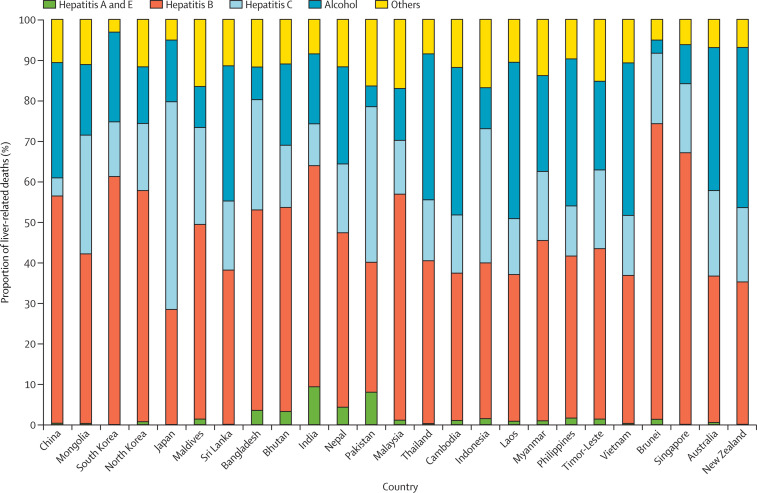
Figure 2.
Causes of liver-related deaths by country in the Asia-Pacific region1
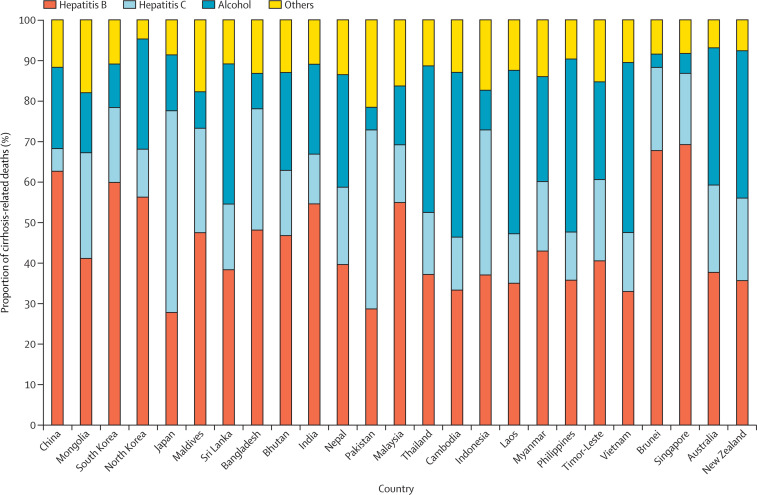
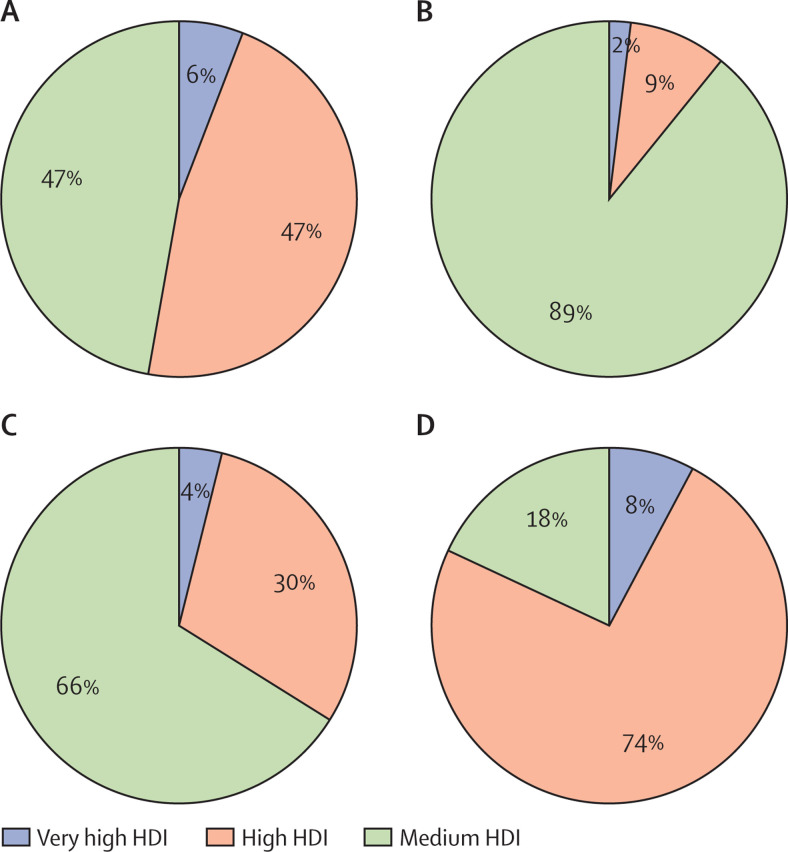
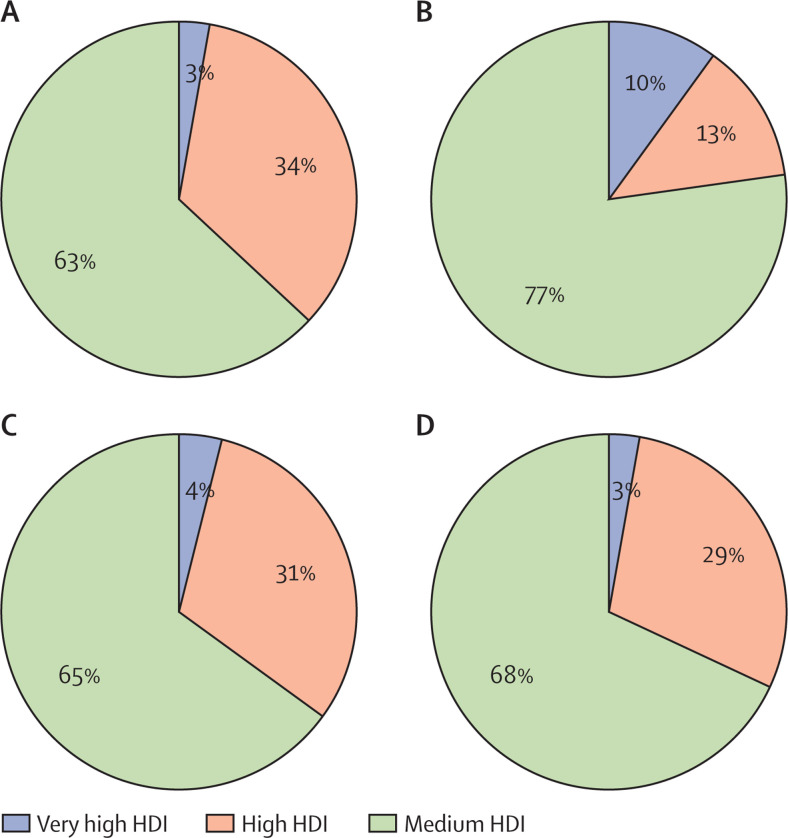
Cirrhosis is the leading cause of liver-related deaths in the Asia-Pacific region, accounting for 630 843 (48·2%) of such deaths in 2015, compared with 46 941 (64·8%) of those in the USA and 115 075 (58·4%) of those in Europe. Deaths due to cirrhosis in the Asia-Pacific region in 2015 represented 54·3% of 1 161 914 cirrhosis-related deaths globally; the region accounted for almost 70% of global cirrhosis-related deaths due to HBV, almost 40% of those due to HCV, just under half of those related to alcohol consumption, and just over a half of those due to NAFLD or other causes (eg, autoimmune, cholestatic, metabolic, or drug-induced liver diseases). In the region, 51·3% of deaths due to cirrhosis were caused by HBV, compared with 18·4% in the USA and 24·3% in Europe; HCV caused 15·7% of deaths due to cirrhosis (vs 37·5% in the USA and 32·6% in Europe), alcohol consumption caused 20·8% (31·2% in the USA and 30·9% in Europe), and NAFLD and other diseases caused 12·1% (12·8% in the USA and 12·1% in Europe; figure 3 ).1
Figure 3.
Causes of cirrhosis-related deaths by country in the Asia-Pacific region1
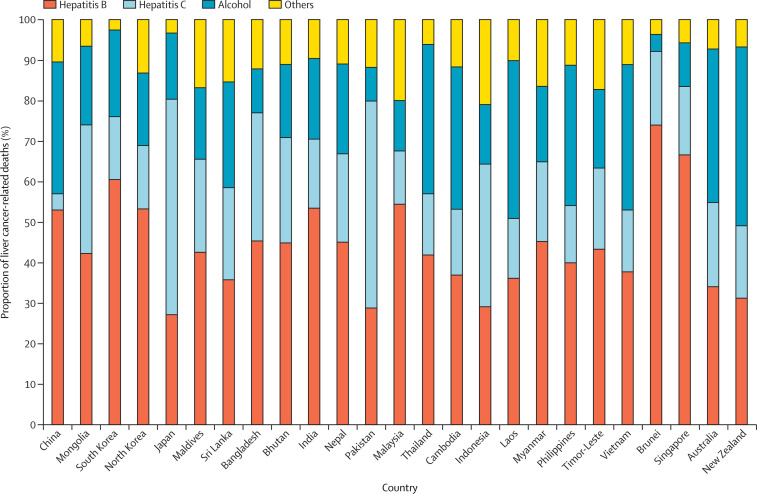
The second largest cause of liver-related deaths in the Asia-Pacific region is liver cancer, which accounted for 573 361 (43·6%) of all 2015 liver-related deaths in the region, compared with 24 565 (33·9%) of those in the USA and 78 072 (39·4%) of those in Europe. These deaths represent almost three-quarters of the estimated global number of deaths due to liver cancer for that year; the region accounted for more than 80% of the global total of HBV-related liver cancer deaths, just under half of those due to HCV, more than 70% of those that were alcohol-related, and more than three-quarters of those due to other causes including NAFLD. In 2015, HBV infection caused 49·1% of all deaths due to liver cancer in the Asia-Pacific region (vs 12·7% in the USA and 20·4% in Europe), HCV infection caused 10·8% (37·1% in the USA and 37·2% in Europe), 29·8% were due to alcohol consumption (38·1% in the USA and 37·1% in Europe), and NAFLD and other diseases caused 10·1% (12·1% in the USA and 5·3% in Europe; figure 4 ).1
Figure 4.
Causes of liver cancer-related deaths by country in the Asia-Pacific region1
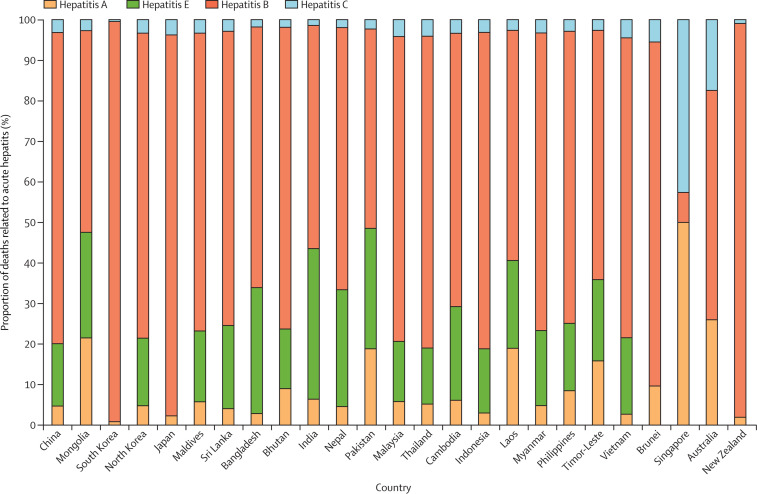
The remaining major contributor to liver-related deaths in the Asia-Pacific region is acute viral hepatitis, which accounted for 108 276 (8·2%) of the total liver-related deaths in the region in 2015, compared with 929 (1·2%) of 72 437 in the USA and 4032 (0·3%) of 197 179 in Europe. Deaths in the Asia-Pacific region represented three-quarters of the global total number of deaths due to acute viral hepatitis. In 2015, the region accounted for three-quarters of the global total number of deaths related to acute HBV, almost two-thirds of those due to acute hepatitis A infection, and almost 80% of those due to acute hepatitis E infection. Of all deaths due to acute viral hepatitis in the region for that year, most were caused by acute hepatitis B infection (59·6%) and acute hepatitis E infection (32·1%), whereas only 6·3% were due to acute hepatitis A. By comparison, in 2015, of all deaths related to acute viral hepatitis, hepatitis B infection caused 81·7% in the USA and 70·0% in Europe, hepatitis E caused no deaths in the USA and 8·3% in Europe, and hepatitis A caused 13·4% in the USA and 18·0% in Europe (figure 5 ).1
Figure 5.
Causes of acute hepatitis-related deaths by country in the Asia-Pacific region1
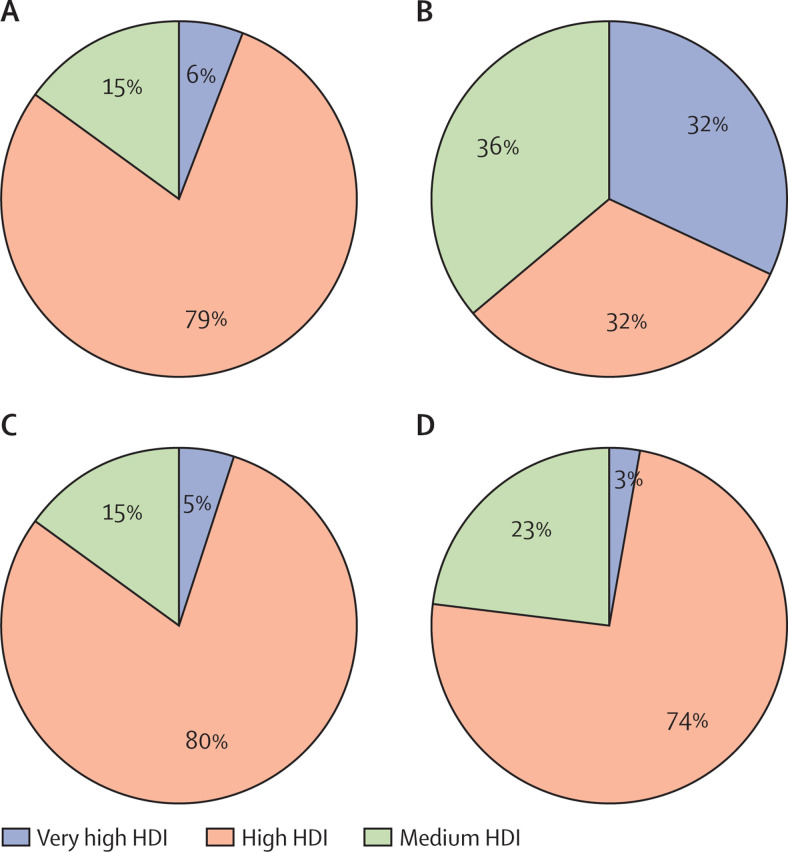
Given the large contribution of the Asia-Pacific region to the global burden of liver diseases, the epidemiology and aetiology of the region's burden need to be reviewed. In this Commission, we document the burden of liver diseases in the region and formulate recommendations to tackle it. It was not feasible to cover every country in the Asia-Pacific region in this Commission. Thus, to maximise our scope by including territories at various stages of development, we divided countries according to their Human Development Index (HDI), selecting the top five most populous countries in the medium-to-high HDI category (China, India, Indonesia, Pakistan, and Bangladesh) and the top five in the very high HDI category (Japan, South Korea, Australia, Singapore, and New Zealand; table 1 shows demographics and health and socioeconomic indicators).2 Given its achievements in controlling HBV, we also included Taiwan when discussing HBV-related liver disease. Commissioners were invited from each of the selected countries and were provided with an outline for data collation and literature review. After this information was synthesised, a draft manuscript was circulated to all collaborators for suggestions, comments, and consensus-building. A final manuscript was then circulated for approval.
Table 1.
Demographic characteristics and health and social indicators of selected countries in the Asia-Pacific region in specific years
| India | Pakistan | Bangladesh | Indonesia | China | South Korea | Taiwan | Japan | Singapore | Australia | New Zealand | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Population characteristics | |||||||||||
| Total population, million | 1324·2 (2016) | 193·2 (2016) | 162·9 (2016) | 258·7 (2016) | 1400·0 (2015) | 51·0 (2015) | 23·5 (2016) | 127·0 (2016) | 5·6 (2016) | 24·7 (2018) | 4·7 (2016) |
| Crude birth rate, per 1000 people | 19·7 (2015) | 29·8 (2016) | 18·9 (2016) | 19·0 (2016) | 13·3 (2015) | 8·6 (2015) | 8·3 (2017) | 7·8 (2016) | 8·9 (2016) | 12·7 (2015) | 13·3 (2015) |
| Crude death rate, per 1000 people | 7·3 (2015) | 7·5 (2016) | 5·3 (2017) | 7·1 (2016) | 7·2 (2015) | 5·4 (2015) | 7·3 (2018) | 10·1 (2015) | 5·0 (2016) | 6·7 (2017) | 6·9 (2017) |
| Annual population growth rate, % | 1·1% (2016) | 2·0% (2016) | 1·1% (2016) | 1·1% (2016) | 4·9% (2015) | 0·5% (2015) | 0·0% (2017) | −0·1% (2016) | 1·3% (2016) | 1·3% (2018) | 2·1% (2016) |
| Average life expectancy | |||||||||||
| At birth, years | 69·0 (2016) | 66·5 (2016) | 72·0 (2015) | 69·0 (2015) | 76·1 (2015) | 82·2 (2015) | 80·0 (2016) | 84·0 (2016) | 82·9 (2016) | 82·8 (2015) | 81·6 (2015) |
| At age 60 years, years | 17·9 (2015) | 17·0 (2013) | 18·0 (2015) | 18·0 (2016) | 19·7 (2015) | 24·0 (2015) | 23·8 (2016) | 26·0 (2016) | 20·8*(2016) | 25·1 (2015) | 25·0 (2015) |
| Average healthy life expectancy, years | 59·3 (2016) | 57·7 (2016) | 63·3 (2016) | 61·7 (2016) | 68·5 (2016) | 73·2 (2015) | 71·2 (2016) | 74·8 (2016) | 73·7 (2016) | 73·0 (2016) | 72·8 (2016) |
| Health indicators | |||||||||||
| Infant mortality rate, per 1000 livebirths | 37·9 (2015) | 65·7 (2015) | 28·2 (2016) | 22·2 (2015) | 9·2 (2015) | 2·7 (2015) | 6·3 (2016) | 2·0 (2016) | 2·2 (2016) | 3·2 (2015) | 4·1 (2015) |
| Mortality rate of children younger than 5 years, per 1000 livebirths | 43·0 (2016) | 79·0 (2016) | 35·0 (2016) | 26·3 (2015) | 10·7 (2015) | 3·4 (2015) | 4·8 (2016) | 2·9 (2015) | 2·7 (2016) | 4·2 (2015) | 5·1 (2015) |
| Maternal mortality rate, per 100 000 livebirths | 174·0 (2015) | 178·0 (2015) | 176·0 (2017) | 5·0 (2015) | 27·0 (2015) | 8·7 (2015) | 11·6 (2016) | 5·0 (2015) | 4·8 (2016) | 6·8 (2012) | 11·0 (2015) |
| Pregnant women receiving prenatal care, % | 75·2% (2015) | 73·1% (2013) | 63·9% (2016) | 95·4% (2014) | 96·2% (2015) | 98·1% (2015) | 94·8% (2016) | .. | .. | 58·0% (2015) | .. |
| Birth attended by skilled staff, % | 81·0% (2016) | 55·0% (2016) | 44·0% (2016) | 92·6% (2016) | 99·7% (2015) | 99·2% (2015) | 99·8% (2016) | 99·8% (2014) | 100% (2016) | 98·8% (2015) | .. |
| Children younger than 5 years with stunted growth, % | 38·0% (2015–16) | 45·0 % (2016) | 36·1% (2017) | 36·4% (2013) | 9·4% (2010) | 2·5% (2008–11) | .. | 7·1% (2010) | 11% (2015) | 1·8% (2007) | .. |
| Children younger than 5 years who are underweight, % | 35·7% (2016) | 31·6% (2012) | 36·1% (2017) | 13·5% (2013) | 2·3% (2010) | 0·9% (2010) | .. | 3·4% (2010) | 9·0% (2015) | 0·2% (2007) | .. |
| Children aged 12–23 months who have received three doses of hepatitis B vaccine, % | 63·0% (2015–16) | .. | 97·0% (2016) | 63·7% (2017) | 99·0% (2016) | 96·3% (2015) | 97·9% (2017) | .. | 96·1% (2016) | 100% (2000) | 100% (1988) |
| Socioeconomic indicators | |||||||||||
| World Bank income classification | Lower-middle (2016) | Lower-middle (2015) | Lower-middle (2017) | Lower-middle (2016) | Upper-middle (2015) | High (2015) | High (2017) | High (2016) | High (2016) | High (2018) | High (2018) |
| GNI per capita, US$ | 1680 (2016) | 1500 (2016) | 1330 (2016) | 3400 (2016) | 8250 (2016) | 27 250 (2015) | 24 936 (2017) | 38 000 (2016) | 51 880 (2016) | 54 230 (2016) | 38 740 (2016) |
| PPP per capita, US$ | 6500 (2016) | 5560 (2016) | 3790 (2016) | 11 220 (2016) | 15 470 (2016) | 34 520 (2015) | 45 582 (2015) | 43 630 (2016) | 85 050 (2016) | 45 210 (2016) | 37 190 (2016) |
| GDP growth rate, % per year | 7·1% (2016) | 2·0% (2016) | 7·1% (2016) | 5·0% (2016) | 6·7% (2016) | 2·6% (2015) | 2·9% (2016) | 0·9% (2016) | 2·4% (2018) | 2·8% (2016) | 3·1% (2016) |
| Poverty headcount ratio at national poverty line, % population | 21·9% (2010) | 29·5% (2016) | 24·3% (2016) | 10·7% (2017) | 3·1% (2016) | .. | 6·6% (2016) | .. | .. | .. | .. |
| Poverty headcount ratio at US$1·90 a day by 2011 PPP, % population | 21·2% (2010) | 6·1% (2016) | 14·8% (2016) | 10·6% (2016) | 1·9% (2013) | 0·3% (2012) | .. | 0·3% (2010) | .. | 0·3% (2010) | .. |
| Income share held by the lowest 20% of the population, % | 8·3% (2010) | 9·2% (2016) | 8·6% (2016) | 7·2% (2013) | 5·2% (2012) | 7·3% (2012) | 6·8% (2007) | 7·0% (2010) | .. | 7·7% (2015–16) | 6·4% (1979) |
| Households with a clean drinking water source, % | 89·9% (2015–16) | 36·0% (2015) | 98·0% (2017) | 86·0% (2015) | 95·5% (2015) | 97·6% (2012) | 93·5% (2015) | 100% (2015) | 100% (2016) | 100% (2016) | 100% (2016) |
| Households using a hygienic sanitation facility, % | 48·4% (2015–16) | .. | 75·0% (2017) | 67·0% (2015) | 76·5% (2015) | 100% (2015) | 100% (2015) | 100% (2015) | 100% (2016) | 100% (2016) | .. |
GNI=gross national income. PPP=purchasing power parity. GDP=gross domestic product.
At 65 years of age.
Viral hepatitis
Hepatitis B, D, and C
According to the GHE 2015 dataset, in mainland China, hepatitis B infection accounted for 63% of all deaths due to cirrhosis and other chronic liver diseases and for 53% of all deaths due to liver cancer, whereas hepatitis C accounted for 6% and 4% of such deaths, respectively (table 2 ).1 Acute hepatitis B infection caused 76·7% of acute hepatitis-related deaths in China in 2015; by comparison, hepatitis C caused 3·1%.1 China has the most people infected with HBV and HCV worldwide. In Asia-Pacific, China accounts for a large proportion of the regional burden of viral hepatitis, particularly HBV, with prevalence in 2018 of more than 80 million estimated chronic infections.4 Nevertheless, the country is moving towards elimination of viral hepatitis4 via a universal HBV vaccination programme in infants and mandatory screening of blood products for HBV and HCV,5 and has exceeded WHO's Western Pacific regional target for HBV vaccination and reduction of HBsAg prevalence in children younger than 5 years.4 According to a 2015 systematic review,6 the estimated HBsAg endemicity in mainland China decreased from 14·0% in 1957–89 to 5·4% in 1990–2013. More recently, a modelling study7 estimated HBsAg prevalence in China to be 6·1%. In national surveys, the prevalence of HBsAg in the general population decreased from 9·8% in 1992 to 7·2% in 2006.8 In people aged 1–29 years, the prevalence of HBsAg decreased from 10·1% in 1992 to 5·5% in 2006 and to 2·6% in 2014.9 Nonetheless, there are still an estimated 77–97 million people with chronic HBV infection in China, including more than 20–30 million with active liver disease,7 of whom 7 million need urgent treatment because of advanced fibrosis or high risk of developing hepatocellular carcinoma.8 The average annual cost per case of HBV-related liver disease in China was estimated at US$4454·0 (direct), $924·3 (indirect), and $6611·10 (intangible).10
Table 2.
Estimated deaths due to liver diseases in selected countries in the Asia-Pacific region for 20151
| India | Pakistan | Bangladesh | Indonesia | China | South Korea | Taiwan | Japan | Singapore | Australia | New Zealand | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| All-cause deaths | 10 287 691 (9 947 812–10 636 408) | 1 370 825 (1 298 521–1 444 605) | 867 299 (809 733–926 040) | 1 842 465 (1 758 635–1 926 294) | 9 911 318 (9 408 313–10 430 339) | 279 100 (246 417–311 720) | 163 574 (124 321–211 234) | 1 310 237 (1 239 659–1 382 256) | 27 233 (17 029–37 436) | 85 372 (84 256–86 486) | 16 192 (15 684–16 709) |
| All acute hepatitis | 46 483 (42 761–50 112) | 4527 (357–8782) | 2918 (429–6335) | 6285 (1371–11 198) | 8877 (6223–12 310) | 1064 (938–3085) | 3 (1–9) | 784 (134–2555) | 0 | 113 (91–142) | 1 (1–1) |
| Acute hepatitis A | 6001 (4089–8084) | 852 (95–2699) | 82 (27–656) | 187 (61–1034) | 415 (203–784) | 9 (6–194) | 0 | 17 (7–284) | 0 | 10 (3–22) | 0 (0–0) |
| Acute hepatitis B | 24 429 (20 045–28 891) | 2226 (199–5210) | 1876 (234–4615) | 4906 (564–9247) | 6813 (3619–12 334) | 1050 (924–3058) | 1 | 737 (124–2454) | 0 | 95 (72–122) | 1 (1–1) |
| Acute hepatitis C | 602 (123–1427) | 103 (18–748) | 52 (15–511) | 197 (56–1068) | 282 (137–537) | 5 (2–140) | 2 (1–7) | 29 (13–374) | 0 | 7 (1–17) | 0 (0–0) |
| Acute hepatitis E | 15 450 (11 031–20 439) | 1344 (59–3663) | 907 (124–2812) | 995 (343–2949) | 1367 (695–1367) | .. | 0 | 0 | 0* | 0 (0–0) | 0 (0–0) |
| All liver cancer | 34 855 (32 035–39 960) | 4457 (3195–8680) | 2926 (435–6347) | 18357 (9959–26 754) | 396 791 (316 550–484 601) | 12 373 (5479–19 266) | 8528 (3245–13 214) | 32 389 (21 236–43 770) | 797 (498–2548) | 1301 (1145–1445) | 149 (129–171) |
| Liver cancer due to hepatitis B | 14 622 (13 052–16 962) | 1283 (802–3549) | 1326 (234–3630) | 5341 (811–9870) | 210 225 (166 477–258 811) | 7487 (2124–12 850) | .. | 8783 (2975–14 711) | 531 (330–1959) | 113 (95–134) | 14 (11–16) |
| Liver cancer due to hepatitis C | 6849 (6106–7917) | 2278 (1543–5296) | 926 (198–2850) | 6467 (1482–11 450) | 15 964 (12 234–20 359) | 1922 (851–4644) | .. | 17 237 (9100–25 540) | 134 (83–854) | 523 (446–607) | 43 (35–51) |
| Liver cancer due to alcohol use | 7204 (6346–8515) | 370 (251–1587) | 317 (73–1443) | 2701 (467–5922) | 129 117 (101 877–159 586) | 2645 (1171–5834) | .. | 5294 (784–9896) | 86 (52–661) | 492 (425–554) | 80 (68–92) |
| Liver cancer due to other causes | 6179 (5621–7151) | 525 (345–1975) | 356 (87–1550) | 3848 (767–7693) | 41 485 (32 182–52 219) | 317 (140–1421) | .. | 1072 (159–3144) | 45 (27–464) | 172 (142–203) | 11 (9–14) |
| Cirrhosis and other chronic liver diseases | 239 376 (220 246–299 528) | 18 451 (10 032–27 041) | 223 455 (13 081–31 799) | 55 860 (41 212–70 506) | 161 376 (117 035–215 518) | 6 499 (1503–11 496) | 4688 (1206–7864) | 17 561 (9348–25 941) | 188 (116–1 040) | 1857 (1703–2015) | 146 (112–167) |
| Cirrhosis and other chronic liver diseases due to hepatitis B | 79 472 (71 558–99 749) | 5283 (778–9880) | 107 446 (4321–17 302) | 20 690 (11 775–29 605) | 101 070 (72 926–135 746) | 3656 (845–7403) | .. | 4880 (550–9298) | 130 (81–838) | 254 (217–296) | 23 (17–28) |
| Cirrhosis and other chronic liver diseases due to hepatitis C | 51 549 (46 226–64 838) | 8157 (2559–13 869) | 6691 (1621–11 864) | 19 989 (11 226–28 751) | 9038 (6336–12 532) | 767 (177–2483) | .. | 8740 (2945–14 625) | 33 (20–390) | 801 (721–888) | 58 (43–67) |
| Cirrhosis and other chronic liver diseases due to alcohol use | 63 238 (56 655–78 650) | 1030 (304–3061) | 1950 (786–4743) | 5472 (886–10 056) | 32 338 (23 031–44 064) | 1770 (409–4378) | .. | 2422 (340–5535) | 9 (3–197) | 561 (493–634) | 51 (39–60) |
| Cirrhosis and other chronic liver diseases due to other causes | 45 115 (40 127–58 050) | 3980 (908–7969) | 2957 (1021–6396) | 9709 (3601–15 815) | 18 932 (13 392–25 991) | 306 (70–1390) | .. | 1518 (289–3982) | 15 (5–261) | 239 (204–277) | 13 (9–16) |
Data are mean estimated deaths (95% CI) and include all ages and sexes.
Based on the Ministry of Health's communicable disease surveillance report 2000–16.3
Overall, the nationwide prevalence of anti-HCV antibodies has drastically declined from 3·2% in 1992 to 0·43% in 2006, and is higher in northern than in southern China.8 Conversely, the reported incidence of HCV infection increased between 1997 and 2012, from 0·7 to 15·0 cases per 100 000 people, with the largest disease burden concentrated in individuals older than 35 years and rural residents.11 This change in incidence does not reflect an actual increase in incidence but improved reporting after reinforcement of the reporting system following the 2003 outbreak of severe acute respiratory syndrome coronavirus.12
The predominant routes of HCV infection in mainland China include transfusion of contaminated blood products, invasive medical procedures, and use of injectable drugs. Since the implementation of mandatory HCV screening for blood products, infection via transfusion has decreased significantly (eg, in Beijing, the proportion of new infections caused by blood transfusion was 84·2% before 1992 and 14·3% after 2004).13 With the adoption of mandatory nucleic acid testing for HBV and HCV in donated blood since 2013, transfusion-related HCV infections will decrease further. Infection via non-transfusion medical procedures procedures was infrequent in Beijing in the period before implementation of mandatory HCV screening for blood products (accounting for 7·0% of HCV infections before 1992), but this proportion has increased over time (accounting for 33·3% of HCV infections after 2004).13 Similar data showing continuously decreasing HCV transmission via blood transfusion and a concomitant increase in HCV transmission via intravenous drug use, unsafe sexual behaviour, and invasive procedures outside health-care settings (eg, piercings, tattoos, acupuncture, barbershop shaving, etc) have been reported in Beijing, as well as in other parts of mainland China.14, 15 Between 2010 and 2012, disease sentinel surveillance identified that the incidence of HCV seropositivity was highest in people who inject drugs and who require haemodialysis, and was far lower, but not negligible, in the sexually active general population.11
As is the case in China, the greatest contributing factor to the burden of liver disease in India is viral hepatitis, particularly HBV. According to estimates from the 2015 Global Burden of Disease (GBD) Study,1, 16 hepatitis B infection accounted for 33% of all deaths due to cirrhosis and other chronic liver diseases and for 42% or all deaths due to liver cancer, whereas hepatitis C accounted for 22% and 20% of deaths, respectively. Acute hepatitis B and C infections accounted for 55% and 1·4% of all deaths due to acute hepatitis in India in 2015 (table 2).1 Community data on the burden of disease caused by chronic liver diseases due to hepatitis B and C are scarce. On the basis of a systematic review of published literature, the proportion of liver diseases attributable to HBV was 67%, 17–19% for HCV, and 71–72% for either virus (some patients had HBV-HCV co-infection).17 Further, the annual number of deaths from liver cancer attributable to these viruses was estimated to be approximately 17 000 for HBV, 4500 for HCV, and 18 500 for either or both viruses.17
Data on HBV seroprevalence in India are available from blood-bank screening and a few community-based studies, with marked variation across studies.18 On the basis of data from 19 studies from the mid-1990s,19 the prevalence of HBV infection was estimated at 4·7%. Subsequent literature reviews and meta-analyses have provided estimates of 2·4% and 3·7%.20, 21 A 2015 global systematic review of HBV prevalence included 129 studies from India; of these, 24 reported (with 46 463 participants) data up to 1989 and 106 (3·7 million people) thereafter.6 Pooled prevalence was estimated at 2·6% before 1989 and 1·4% after.6 A 2018 modelling study found that the prevalence of HBsAg in India in 2016 was 2·5% (95% CI 2·2–2·7).7 Some tribal groups have a higher prevalence of HBV infection than the general population;18 however, these subpopulations are small and their disease burden was deemed unlikely to influence the overall estimates.
Direct evidence on routes of transmission of HBV is insufficient. Early data suggested that a horizontal (close interpersonal contact between children) route was predominant;22 however, newer data suggest that perinatal transmission is also important.23 Hepatitis D virus (HDV) infection was once thought to be common in India, but a 2015 study found that none of the 318 participants with HBV infection had detectable anti-HDV IgG or HDV RNA.24 The national immunisation schedule includes three doses of hepatitis B vaccine (along with diphtheria-pertussis-tetanus), one of which is a birth dose (within 12 h of birth) where possible (eg, with institutional deliveries).
Positivity for anti-HCV in people donating blood to blood banks has been reported to be 0–2%, with clustering around 1% of blood donors.25 Community-based seroprevalence studies have mostly reported similar results,26, 27 but in some areas such as Punjab state, higher prevalence of 3·2–5·2% has been reported.28, 29 In a survey of 14 481 people who inject drugs, the weighted anti-HCV prevalence was 37·2% (including 13·2% with HCV-HIV co-infection), varying from 4·9% to 64·9% across 15 Indian cities.30 Indirect evidence suggests that most cases of HCV infection are related either to unsafe injection practices or transfusion of contaminated blood or blood products before the introduction of mandatory testing of donated blood.25
HBV and HCV are major contributors to the liver disease burden in Indonesia, similar to China and India. According to the GHE 2015 dataset, hepatitis B infection in Indonesia accounted for 37·0% of all deaths due to cirrhosis and other chronic liver diseases and for 29·1% of all deaths due to liver cancer, whereas these proportions were 35·8% and 35·2% for hepatitis C (table 2).1 Acute hepatitis B and C infection accounted for 78·1% and 3·1% of all deaths due to acute hepatitis in Indonesia in 2015.1 Information about the prevalence of HBV and HCV in the general Indonesian population is unavailable because of inadequate disease surveillance and probable under-reporting, geographical barriers for collecting data on 250 million people living on more than 17 000 islands, and few testing facilities. The prevalence of HBsAg ranged from 4% to 20·3% in 1990–97,31 making Indonesia a country with intermediate-to-high endemicity of hepatitis B. HBsAg prevalence during that period ranged between 37% and 76% in patients with liver cirrhosis and was 37–68% in patients with hepatocellular carcinoma.31 Efforts to collect national-level data were made in 2007 through Indonesia's Basic Health Research survey (known as RISKESDAS) in 21 of 33 provinces. The prevalence of HBsAg in 2007 was 9·4%, that of anti-HBc was 32·8%, and of anti-HBs was 30·6%.32, 33 A nationwide study in 2015 covering 33 provinces showed that the prevalence of HBsAg was 7·1%, that of anti-HBc was 31·9%, and of anti-HBs was 35·6%.34 These data showed a decline in the prevalence of HBsAg (9·4% in 2007 to 7·1% in 2013), suggesting that Indonesia has moved from high endemicity to moderate endemicity of hepatitis B (appendix p 1).
Despite substantial progress in reducing HBV infection by a universal immunisation programme for infants, new cases in Indonesia still occur in early childhood, and the prevalence of HBsAg in children younger than 5 years can be as high as 4·2%.35 This high prevalence could be due to uneven coverage of birth-dose vaccination, which is low (<50%) in areas that are difficult to access in the eastern part of Indonesia, and to the high HBsAg prevalence in pregnant women, which facilitates vertical or mother-to-child transmission.36 In parallel, HBV transmission also occurs horizontally, as shown by the increasing trend of the prevalence of anti-HBc antibodies by age.31 A 2016 study in 12 provinces observed a HBsAg prevalence of 2·76% in pregnant women. With 5 000 000 pregnancies per year in Indonesia, approximately 150 000 pregnant mothers could potentially transmit HBV to their babies annually, of whom 95% will develop chronic hepatitis B and be infectious for their entire lives. This transmission incidence is of serious concern, considering that coverage of HBV birth-dose vaccination is low, screening tests for HBV in pregnant women are not routinely done, and antiviral treatment for women infected with HBV has not been adopted as a preventive strategy for mother-to-child transmission.31
A 2018 study37 showed that hepatitis B is an important occupational hazard for health-care workers in Indonesia. The study reported that the acquisition of HBV infection (indicated by anti-HBc prevalence) and the evidence of repeated natural boosting (indicated by anti-HBs prevalence together with either or both HBsAg and anti-HBc) increased significantly with the length of service period and the type of work (administrative, non-intervention, and intervention). Needle injury was confirmed to be the greatest risk factor for acquiring HBV among health-care workers.37
Information on hepatitis C prevalence in Indonesia are also scarce. Data from blood donors in 1998–2000 showed that anti-HCV prevalence was 1·5% in Java and 1·0% outside Java.32 Data from the RISKESDAS surveys in 2007 and 2013 reported anti-HCV prevalence of 0·8% and 1·0%, with high prevalence in children (1–14 years of age; 0·5% in 2007 and 0·6% in 2013).38, 39 The Indonesian Red Cross notified between 8400 and 12 100 individuals annually that they had HCV infection acquired through receiving blood transfusion in 2010–14.37 It was estimated that there were 1 284 000 viraemic individuals in 2014, projected to increase to 1 303 000 by 2023.37 A survey in 2012 showed that 2·5% of the population infected with HCV were active injecting drug users. Of an estimated 70 000 (95% CI 61 901–88 320) people who inject drugs, 77·3% (95% CI 40–80) had HCV infection. Assuming spontaneous clearance in 20% of cases, the number of viraemic people who inject drugs was estimated to be 22 400–43 680.37
In Pakistan, HCV has replaced HBV as the most common cause of cirrhosis and hepatocellular carcinoma.40, 41 Up to 86% of cases of cirrhosis and 58% of cases of hepatocellular carcinoma in Pakistan have been attributed to HCV.40, 41, 42 According to the GHE 2015 dataset, hepatitis B accounted for 28·6% of all deaths due to cirrhosis and other chronic liver diseases and for 28·8% of all deaths due to liver cancer in Pakistan, whereas hepatitis C accounted for 44·2% and 51·1% of such deaths, respectively (table 2).1 Acute hepatitis B infection caused 49·2%, and acute hepatitis C infection caused 2·3%, of all deaths due to acute hepatitis in Pakistan in 2015.1 An increased prevalence of either HBV or HCV has been reported in prisoners.43, 44 HDV has been reported in 16·6–44% of patients with hepatitis B.42
The first Pakistani national survey45 done in 2008 reported that the overall prevalence of HCV was 4·8% and of HBV was 2·5% for that year, with an estimated 13 million people having co-infections. Reusing syringes for therapeutic injections, receipt of contaminated blood or blood products, reuse of razors by barbers, and medical exposure to contaminated sharps were the major risk factors (appendix p 2).45, 46 The prevalence of HCV in Pakistan is projected to increase by approximately 60% over the next 15 years, which is equivalent to 1 million new cases annually, representing 10% of the global HCV burden by 2030.42 It has been estimated that 510 000 HCV cases treated annually, mass screening, effective awareness campaigns, and availability of sterile equipment would significantly reduce burden of HCV and avert 220 000 liver-related deaths and 116 000 new cases of liver cancer cases in Pakistan in the next 15 years.42
As with other Asian countries, HBV and HCV cause the most cases of chronic liver disease in Japan. HCV is the most prevalent cause of such deaths: in 2015, 27·8% of all deaths due to cirrhosis and other chronic liver diseases, and 27·1% of those due to liver cancer, were caused by hepatitis B, whereas 49·8% and 53·2% of them were caused by hepatitis C (table 2).1 For that year, hepatitis B accounted for 93·9%, and hepatitis C for 3·6%, of all deaths due to acute hepatitis infection.1 The chronic carrier prevalence of HCV in Japan in 2005 was reported to be 0·8% in people aged 60–64 years, which has gradually decreased, and was reported as 0·07% in people aged 20–24 years for the same year.47 174–236 cases of acute hepatitis B cases per year were reported for the period of 2006–15 to the Governmental Registry of Japan.48 70% of these new acute HBV infections were sexually transmitted.49 The number of cases of acute hepatitis C is currently not known, but about 27 to 52 cases of acute hepatitis C were reported to the Registry per year for 2006–15.48
Since records began in 1958, until 1970, there were no drastic changes in mortality due to viral hepatitis-related hepatocellular carcinoma in Japan(appendix p 4).50, 51 However, an exponential increase in the incidence of, and deaths from, primary liver cancer began in the early 1970s and peaked in the early 2000s (appendix p 4).50 This marked increase is most likely explained by an increase of HCV infection in the era after WW2 in the so-called baby-boomer generation.50 After plateauing in 2002–04, the number of deaths due to hepatocellular carcinoma has started to decline and was 28 889 in 2015.51 The Japanese Government introduced a universal health insurance coverage system in the 1960s, which covered almost 90% of total overall medical costs.52 Consequently, expensive surgeries requiring blood transfusion (eg, total gastrectomy for peptic ulcer) were widely done.53 Contaminated syringes were frequently used in medical settings for intravenous infusion of vitamins, to supposedly counteract the common cold or to improve spirits.53 This practice continued until a few years after the discovery of HCV in 1989. Subsequently, introduction of nucleic-acid amplification testing for HCV, HBV, and HIV in blood products by the Japanese Red Cross in 1999, and screening of pregnant women for HBV infection, lead to a decline in hepatocellular carcinoma cases due to viruses transmitted by transfusion.51 The incidence of transfusion-transmitted viral hepatitis in people who had a transfusion in 2007 was reported to be 0·0007%.54
In Japan, mother-to-child transmission is the major route of establishing chronicity of HBV, but it is less common than in other Asian countries. From June, 1985, all pregnant women were screened for the presence of serum HBsAg, and from January, 1986, the Government started financing programmes for prevention of vertical transmission of HBV infection.55 A retrospective, nationwide, multicentre study in 430 patients born between 1976 and 2010 who were younger than 20 years when diagnosed with chronic HBV infection showed that the number of cases according to birth year increased within this timeframe. After the introduction of perinatal immunoprophylaxis of HBV vaccination plus hepatitis B immunoglobulin (IgG) in 1986, the proportion of chronic HBV infections caused by mother-to-child transmission decreased from 73% between 1981 and 1985 to 47% between 1986 and 1990. However, mother-to-child transmission then persistently increased from 62% between 1991 and 1995, to 64% between 1996 and 2000, 74% between 2001 and 2005, and finally to 86% (67 of 78 cases of HBV) between 2006 and 2010.
To identify the causes of the increase in mother-to-child transmission despite perinatal immunoprophylaxis, the association between the implementation of immunoprophylaxis and chronic HBV infection was evaluated. The prevalence of confirmed lack of immunoprophylaxis decreased continuously from 38% between 1986 and 1990 to 9% between 2006 and 2010. Similarly, the proportion of patients with no medical record of immunoprophylaxis also decreased from 38% between 1986 and 1990 to 3% between 2006 and 2010. The prevalence of incomplete prophylaxis ranged from 30% to 50% across the 1986–2010 period. By contrast, the prevalence of complete prophylaxis increased continuously from 0% between 1986 and 1990 to 55% between 2006 and 2010. These findings indicate that the increase in chronic HBV infection due to mother-to-child transmission was probably caused by poor efficacy of the prophylaxis regimens or the antibodies used.
By contrast with trends in Pakistan and Japan, HBV is the most common cause of liver diseases in Bangladesh. According to the GHE 2015 dataset, hepatitis B caused 48·1% of all deaths due to cirrhosis and other chronic liver diseases and 45·3% of all deaths due to liver cancer in Bangladesh (table 2).1 Conversely, hepatitis C, the second leading cause of chronic liver diseases in Bangladesh, accounted for 29·9% and 31·6% of these deaths. Hepatitis B also accounted for 64·3%, and hepatitis C for 1·7%, of all deaths due to acute hepatitis.1 Hospital-based data indicate that 60% of cirrhosis cases56 and 65% of hepatocellular carcinoma cases57 in Bangladesh are thought to be direct consequences of HBV infection, while HCV accounts for 30% of cirrhosis cases and 17% of cases of hepatocellular carcinoma.56, 57
In the absence of a nationwide seroprevalence study of HBV, high variability in the prevalence of HBsAg in Bangladesh has been shown. Several studies from the 2000s show variation from 0·7% to 5·5% in the general population.58, 59 However, these proportions are lower than those reported by Islam and colleagues in 1984.60 Risk factors for HBV transmission in Bangladesh include treatment by non-qualified medical practitioners, shaving and hair-cutting with shared razors in barber shops, body piercing, dental procedures, and intravenous infusion, together with mass vaccination against smallpox and cholera.58, 59 Chronic hepatitis B infection that is negative for HBeAg and positive for anti-HBe is common in Bangladeshi patients.61 Data from Bangladesh on HCV prevalence is sparse, but is reported to be low (0·84%).62 Prevalence is as high as 40% in people who inject drugs with unknown HIV status and 60·7% in those with HIV co-infection; therefore, the burden of HCV is highest in people who inject drugs.63 Most people who do not inject drugs but are infected with HCV have a history of any injection (treatment by non-qualified village doctors), sharing blades in barber shop, or of circumcision by traditional practitioners.63
In South Korea, similar to Bangladesh, HBV is the most prevalent cause of chronic and acute liver disease. According to the GHE 2015 dataset, hepatitis B accounted for 56·3% of all deaths due to cirrhosis and other chronic liver diseases, and for 60·5% of those due to liver cancer (table 2).1 Hepatitis C infections caused 11·8% and 15·5% of such deaths, respectively.1 Acute hepatitis B and C accounted for 98·7% and 0·4%, respectively, of all deaths due to acute hepatitis in South Korea in 2015.1 Although the prevalence of HBV in the general population was around 8% until the 1980s, the introduction of a HBV vaccine in South Korea in 1983, and the national vaccination programme in 1995, have lowered the prevalence of HBV to about 3% in adults and to less than 1% in children.64 The overall prevalence of HBV continues to decline; nonetheless, around 2 million people still carry the virus. In South Korea, HBV-HDV co-infection is very rare.
Hepatitis B is most commonly spread from mother to child in South Korea. During the 1980s, about 11% of neonates in South Korea were infected with HBV via vertical transmission. Particularly, many (ie, 65–93%) unvaccinated infants born to mothers positive for HBeAg and HBsAg became infected.65 Therefore, the Ministry of Health and Welfare and Korea Centers for Disease Control and Prevention implemented a prevention programme for HBV vertical transmission in July, 2002, which provides complete financial support for HBV vaccination and tests for neonates with mothers positive for HBsAg, irrespective of HBeAg status. Through these endeavours, 180 690 (96·0%) of 188 224 neonates born to carrier mothers participated in the prevention programme between 2002 and 2014. Overall, 98 293 (54·2%) of 180 690 neonates completed the 3-dose vaccination regimen. Of those who completed the regimen, 84 201 (85·7%) acquired immunity (ie, were negative for HBsAg and positive for anti-HB). Completion has increased from 92·9% in 2008 to 99·4% in 2013, and the prevalence of HBV infection in children decreased from 2·6% in 1994 to 0·2% in 2006.66
HCV infection is the second leading cause of liver disease in South Korea.67 An HCV screening test for blood donors was introduced in 1991 and transmission via transfusion has not been a major route of infection after 1992. One nationwide epidemiological study68 reported that the prevalence of anti-HCV positivity adjusted for age, sex, and area was 0·78%, using estimated population data from 2009 from 29 health check-up centres in South Korea. In this study, 56·1% of patients positive for anti-HCV had detectable HCV RNA. Another study of 207 patients with chronic HCV infection69 showed that risk factors for HCV infection include older age, needle-stick injury, dental procedures, multiple sex partners (≥4), receiving a blood transfusion before 1991, and surgery. A comparative study of 1173 patients with HCV and 534 healthy control participants in five university hospitals between 2007 and 2011 in South Korea reported several independent risk factors for infection, including use of illicit drugs, needle-stick injury, receiving blood transfusion before 1995, having a tattoo, and age.70
HBV is also a major cause of liver disease in Australia. According to GHE estimates in 2015, 37·7% deaths due to cirrhosis and other chronic liver diseases, and 34·0% of those due to liver cancer, resulted from hepatitis B infection (table 2).1 21·6% and 20·8% of these deaths were due to hepatitis C.1 Acute hepatitis B and C infection accounted for 56·6% and 17·5% of all deaths due to acute hepatitis in Australia in 2015.1
In Australia, hepatocellular carcinoma is the fastest growing incident cancer; it is now in the top 10 causes of total cancer death and the seventh cause of cancer deaths in men.71 Between 2011 and 2020, the annual incidence of liver cancer in Australia is projected to increase from 1520 to 2465 cases.72 Liver cancer incidence for 1989–90 was also 5–10 times greater in Indigenous than in non-Indigenous Australians, with 12 times higher expected mortality for Indigenous than non-Indigenous people.73 These prevalence estimates seem to have substantially improved on the basis of 2017 data,72 in which Indigenous Australians had 2·8 times higher age-standardised incidence and 2·5 times higher mortality than non-Indigenous Australians. Notably, although survival for many cancers has improved over the past two decades in Australia and globally, there has been no improvement in liver cancer prognosis, and hepatocellular carcinoma remains the fastest-growing cause of cancer death in Australia. 5-year survival is just 15% (18% if the cancer is localised and 2% if metastasis occurs).72 According to the most recent 2017 estimation,72 between 1982 and 2017 the greatest estimated proportional increase in mortality was from liver cancer (from 2·3% to 6·8% per 100 000 individuals).72 Currently, more than 1400 Australians die from liver cancer each year and a third of those diagnosed do so within a month of diagnosis.72 HBV or HCV is linked to 30% of hepatocellular carcinoma cases in Australia.
A study of a patient database in New South Wales74 found that the population-level burden of new cases of hepatocellular carcinoma per year has stabilised in people with HBV infection (52 in 2001 and 44 in 2013) but increased markedly in those with HCV infection (49 in 2001 and 151 in 2013). The age-standardised incidence of hepatocellular carcinoma per 1000 person-years decreased 2·3% (95% CI 1·4–3·1) in 2001 to 0·9 (0·6–1·2) in 2012 in patients with HBV and remained stable between 2001 (1·4, 0·8–1·9) and 2012 (1·5, 1·2–1·7) in those with HCV.74 Thus, individual-level risk of HBV-related hepatocellular carcinoma had decreased, suggesting that antiviral therapy introduced in the mid-2000s has been effective. By contrast, HCV treatment based on interferons had no effect on individual-level, HCV-related risk of hepatocellular carcinoma and has contributed to the increasing population burden of this cancer type.
Australia has required notification of all cases of viral hepatitis B and C since the early 1990s. This mandatory notification system has helped to monitor the epidemiology of viral hepatitis and, more importantly, has enabled a coordinated public health response. 218 000 (1%) of the Australian population (plausible range 192 000–284 000) are estimated to be living with chronic hepatitis B infection.75 Overall notification of newly acquired hepatitis B (ie, infection acquired within the preceding 24 months) has decreased from 1·2 per 100 000 individuals in 2009 to 0·7 per 100 000 in 2013.76 Notification of newly acquired HBV infection has been consistently low across this period in children younger than 15 years and has declined substantially in people aged 15–29 years. Adolescent catch-up immunisation programmes could have contributed to this decrease in young adults. However, there was an increase in complications related to chronic HBV such as cirrhosis and hepatocellular carcinoma from 450 cases in 2008 to 1550 in 2017.77 The seroprevalence of HBsAg in Indigenous Australian adults was estimated to be 17% in a meta-analysis of studies done before 2000.78 Since then, HBsAg seroprevalence in Indigenous Australians is estimated to have declined to 3·7% of the 548 366 total population in 2011. This seroprevalence is still more than 10 times that in non-Indigenous Australians born in Australia (0·3% of 13 836 559, excluding people who inject drugs and men who have sex with men).79
The prevalence of detectable HCV RNA in the general population in 2014 was approximately 0·9% (range 0·7–1·0%), of Australia representing 227 000 people (range 167 620–249 710).75 However, the number of new HCV infections in Australia has declined since 2000, with modelling studies suggesting that incidence peaked at 14 000 infections in 1999 and then fell to 8500–9000 in 2013 in young adults (aged 20–39 years).80, 81 This decline is attributed to the improvement in harm reduction measures and a reduction in the prevalence of the use of injectable drugs.82 8% of newly diagnosed cases of HCV in 2014 were in Aboriginal people.83 The notification of newly diagnosed HCV cases in Aboriginal people increased by 38%, from 119 per 100 000 people in 2010 to 164 per 100 000 in 2014.83 By contrast in non-Aboriginal people, notification of new cases decreased by 15%, from 41 per 100 000 people in 2010 to 35 per 100 000 in 2014.83
Similar to Australia, HBV is a major cause of liver disease in New Zealand. In New Zealand, hepatitis B accounted for 35·6% of all deaths due to cirrhosis and other chronic liver diseases, and 31·2% of all deaths due to liver cancer in 2015, according to GHE data (table 2).1 20·4% and 17·9% of these deaths were due to hepatitis C.1 Acute hepatitis B and C accounted for 97·1% and 0·009% of all deaths due to acute hepatitis in New Zealand in 2015.1 The quality of epidemiological data for viral hepatitis from New Zealand is poor compared with that in Australia, probably because viral hepatitis is not a disease for which notification is compulsory in New Zealand. However, in 2012, there were an estimated 50 000 (1·5%) people aged 15 years and older with HCV, and approximately 1000 new cases are identified each year.84 It was estimated that only half of the people in this age group are currently diagnosed and only a quarter are aware that they have the disease.84 Approximately 90 000 individuals are living with chronic HBV infection.85 In New Zealand, there was an increase in the incidence of liver cancer, from 145 in 1999 to 253 new registrations in 2009 and high fatality (from 127 to 208 people) in the same period.86 There are four main ethnic groups in New Zealand (European, Māori, Pacific Islander, and Asian), with smaller proportions identifying with other ethnic groups. Liver cancer is the fourth most common in incidence and mortality in Māori men. In this group, hepatocellular carcinoma registration and mortality were almost 3·5 times those of non-Māori men in 2010–12,87 which has perhaps declined since a study done in 1983–94 that suggested that Māori people had a 7 times higher risk than non-Māori people,88 and a further study in 1981–2004 that indicated that risk was 4·79 times higher.89
HBV is also the main contributor to the liver disease burden in Singapore. In Singapore, according to the GHE 2015 dataset, hepatitis B accounted for 69·2% of all deaths due to cirrhosis and other chronic liver diseases, and for 66·6% of all deaths due to liver cancer (table 2).1 These proportions were 17·6% and 16·9% for hepatitis C.1 Acute hepatitis B and C accounted for 7·4% and 42·6% of all deaths due to acute hepatitis in Singapore in 2015.1 In the Singapore Burden of Disease Survey,90 liver cirrhosis contributed 0·9% of the 182 752 years of life lost (YLL) in 2010. Additionally, in a study of patients with liver cirrhosis from a hospital-based population, the main aetiologies were chronic HBV infection (63·3%) and chronic HCV infection (6·9%).91
Liver cancer in Singapore is ranked as the fourth most common cancer in men by the Singapore Cancer Registry for 2010–14,92 and the fifth most common cancer in men for 2011–15 by the Singaporean Ministry of Health, with an age-adjusted prevalence of 17·6 cases per 100 000 people.93 In the Singapore Burden of Disease Survey 2010, liver cancer contributed 5886 disability-adjusted life years (DALYs), equivalent to 1·5% of total DALYs, and 5783 YLL (3·2% of the total).90 The aetiology of hepatocellular carcinoma is not clearly documented, but in a large patient cohort who had surgical resection, 55·6% of cases were due to chronic HBV infection and 6·2% to chronic HCV infection.94 Between 1973 and 2012, the incidence of liver cancer declined steadily. The incidence in men decreased from 27·4 cases in 100 000 people in 1973–77 to 17·2 in 100 000 in 2008–12, whereas the incidence in women decreased from 6·9 in 100 000 in 1973–77 to 4·8 in 100 000 in 2008–12. This decrease is possibly due to the introduction of voluntary HBV vaccination in 1985 as an integral part of the national childhood immunisation programme and improved screening.
A community study in 2010 reported that age-standardised HBsAg seroprevalence in Singapore was 3·6% (95% CI 2·9–4·3) in adults aged 18–69 years.95 Among the three main ethnic groups in Singapore, age-standardised HBsAg seroprevalence in Chinese people (4·2%, 3·4–5·0) was significantly higher than in Malay people (2·2%, 0·7–3·6) and Indian people (0·6%, 0·0–1·4). Regular surveys for chronic HBV show a steady decreasing trend in its seroprevalence. More than 90% of children aged up to 12 years have been immunised against hepatitis B. In 2001, a school immunisation programme against hepatitis B was initiated to screen and immunise all children who were not covered under the national programme. Both programmes have been very successful, as there have been no reports of acute childhood hepatitis B infections since 1997.
There has been no well done community study of HCV prevalence, but estimates from the Ministry of Health for 2016 approximate that it is 0·1%.96 A study found that HCV seroprevalence was 0·06% in 161 658 blood donors between 2011 and 2014, and in 1575 patients receiving haemodialysis, the prevalence was 2·2%.97 There are no data on risk factors associated with HCV, but a study from a single institution of 266 patients with HCV found that 36% had a history of blood transfusion, 16·6% had a history of intravenous drug use, 12·3% had blood disorders, and 8·8% were receiving haemodialysis.98 Nucleic acid amplification testing is effectively used to screen blood products in Singapore. The country has does not have formal harm reduction strategies because its official stance on drug use is zero tolerance.
The epidemiology of viral hepatitis in Taiwan changed drastically after the implementation of a Viral Hepatitis Control Program in 1981,99 and Taiwan has been largely successful in controlling HBV infection. The programme focused on research and development and public education and hepatitis B immunisation. In 2002, treatment of chronic viral hepatitides was added to its aims. As part of the programme, a mass vaccination campaign was launched in 1984, with neonates being a top priority. The campaign also included infants born to mothers carrying hepatitis B. As of 1986, it was extended to all neonates and subsequently to adolescents and adults.
A nationwide study100 that assessed mortality caused by infantile fulminant hepatitis, cirrhosis, and hepatocellular carcinoma (the National Death Certificates Database 1977–2011 was used to calculate mortality) in cohorts of children born before and after the launch of the HBV vaccination campaign in Taiwan in 1984 found that mortality from infant fulminant hepatitis declined significantly for infants born between 1977 and 1980 (5·76 per 100 000 person-years) to 2009–2011 (0·19 per 100 000 person-years). Also, mortality due to cirrhosis and hepatocellular carcinoma in people aged 5–29 years decreased significantly for those born in 1977–80 (0·65 deaths per 100 000 person-years for cirrhosis and 0·81 per 100 000 for carcinoma) to 0·02 deaths per 100 000 person-years for cirrhosis and 0·05 per 100 000 for carcinoma in 2001–04.100 The incidence of HBV infection has decreased markedly, mainly due to the 1984 immunisation campaign.101, 102 The most recent data (from 2016) show that HBsAg positivity in people aged up to 30 years has decreased from more than 11% in 1984 to 0·5% in 2014 (appendix p 5).103 For those older than 30 years, HBsAg positivity was still about 7% in 2016.103 Despite active control programmes, the decline of the hepatitis B burden was slow, as shown in a population-based survey with longitudinal follow-up.104 An outreach community-based screening in 164 302 adults in Taiwan from 1996 to 2005 estimated that the total number of HBsAg carriers was about 3 million, indicating the carrier loads of hepatitis B had remained substantial.105 Since the 1984 immunisation campaign, the incidences of hepatocellular carcinoma,100, 106 cirrhosis,100 acute hepatitis B,107 and childhood fulminant hepatitis108 have decreased.
HCV infection is second to HBV in causing hepatocellular carcinoma and cirrhosis in Taiwan.109 The overall anti-HCV prevalence was 5·5% in 1991–92, and HCV RNA was detectable in 68% of people with anti-HCV.110 Unsafe injections and blood transfusions were the commonest routes of transmission110, 111 before programmes on safe blood transfusions (after 1992) and harm reduction (after 2005) were introduced to reduce the incidence of HCV.111, 112
In summary, hepatitis B and C still contribute to considerable morbidity and mortality due to liver diseases in almost all countries in the Asia-Pacific region, and some countries such as Taiwan and Singapore have addressed the problem better than others. The routes of transmission of HBV are predominantly perinatal, horizontal transmission during childhood, unsafe injection practices, and transfusion of blood products in countries with medium and high HDIs. Conversely, with the successful implementation of HBV vaccination and safety policies on blood transfusion and injection, intravenous drug use remains the predominant route of HBV transmission in countries with very high HDI.
Hepatitis A and E
Acute hepatitis A virus (HAV) and hepatitis E virus (HEV) accounted for 4·7% and 15·4% of all deaths due to acute hepatitis in mainland China in 2015 (table 2).1 As in other low-income and middle-income countries, a relatively high seroprevalence of anti-HAV antibodies compared with high-income countries is reported in China.113 The seroprevalence of anti-HAV has been reported as 51·6% in blood donors with increased alanine aminotransferase concentrations, 41·4% in blood donors without such an increase,113 and 52·9% in a population aged up to 30 years in Shanghai.114 With anti-HAV IgM prevalence of 0·08% in donors of source plasma,115 transmission of HAV by blood transfusion occurs very rarely. Insufficient food and water hygiene as well as hand washing could be responsible for local outbreaks.116
The prevalence of IgG HEV was 23·5% in the general Chinese population according to the 2005–06 Third National Viral Hepatitis Prevalence Survey.117 Farmers, people aged 15–60 years, and those living in the midwest or mideast provinces and northwest region, including Xinjiang, had the highest seroprevalence estimates; within any region, the seroprevalence of HEV generally increased with age.117 In pregnant women, the reported prevalence of anti-HEV IgG positivity was 10·2–16·2% and that of anti-HEV IgM was 0·6–2·6%.118, 119 Acute HEV infection in pregnant women can have serious consequences, although few fatal infections have been reported.
HEV outbreaks were reported before 1988, with one epidemic of HEV genotype 1 in Xinjiang in 1986–88 infecting more than 120 000 people.120 Subsequently, sporadic infections and small-scale outbreaks have replaced epidemics of HEV.121 Presently, zoonotic transmission with sporadic infections is the major mode of transmission, succeeding transmission through contaminated water or food, which was previously the main route of transmission. Large community-based epidemiology surveillance found that HEV genotype 4 was the dominant type, indicative of zoonotic transmission.122 China has made progress in preventing HAV and HEV transmission through improving food and water hygiene, as well as vaccination against HAV.123 A vaccine against HEV has been approved in mainland China, with short-term and long-term efficacy being reported.124
Similar to China, HAV and HEV are common causes of acute hepatitis-related mortality in India. In India, according to the GHE 2015 dataset,1 hepatitis A and E accounted for 6·3% and 37·2% of all deaths due to acute hepatitis in 2015.1 HAV is highly prevalent in the Indian population. A systematic review of studies during 1980–2008 showed that seroprevalence exceeded 90% in adolescents and adults,125 although some pockets of epidemiological transition with lower seroprevalence are emerging in urban high-income groups,126 leading to outbreaks.127, 128
HEV infection is hyperendemic in India and its neighbouring countries. The transmission is primarily through faecal contamination of water supplies. Outbreaks of acute hepatitis E are common; the largest recorded outbreak in the country, in 1990, had about 79 000 cases.128 Additionally, HEV infection accounts for 30–50% of cases of sporadic acute hepatitis. Only genotype 1 HEV has been isolated from human cases in India; genotype 4 has been isolated from pigs, but not from humans, suggesting that zoonotic transmission is rare. Chronic hepatitis E infection is infrequent. Transfusion-related and mother-to-child transmission appear to account for only a few cases. HEV mainly affects young adults, in whom spontaneous recovery is high. A few individuals (0·1–1·0%) develop acute liver failure with 30–70% mortality. HEV infection during pregnancy is particularly severe, and case-fatality rates in pregnant women can be as high as 25%.129
HEV infection in patients with pre-existing chronic liver disease is a common cause of acute-on-chronic liver failure. Although HEV infection is frequent, anti-HEV antibodies are detected in only 20–30% of the healthy population,130 possibly because antibodies disappear over time. The HEV vaccine that has been marketed in China is not licensed in India.
HAV and HEV are common causes of acute hepatitis-related mortality also in Indonesia. In Indonesia, acute hepatitis A and E infection accounted for 2·9% and 15·8% of all deaths due to acute hepatitis in 2015, according to the GHE 2015 dataset (table 2).1
The prevalence of HAV infection varies among islands in Indonesia. It is endemic in some areas with sporadic cases every year, but it also occurs as spontaneous outbreaks in other parts of the country. In the 1990s, nearly all children aged 10–14 years in Jayapura (Papua New Guinea), Mataram (Lombok), and Sumbawa Besar (Sumbawa) were infected with HAV, but only about 45–60% children in the same age group in Jakarta (Java), Bandung (Java), and Makassar (Sulawesi) had had this infection.131 With improved socioeconomic status, hygiene, and sanitation, the prevalence of anti-HAV in these areas declined since 2000.131 In 2006, the prevalence of anti-HAV was 60% in young adults aged 18–20 years in Jayapura and Biak (Biak). However, the prevalence was still high (up to 90%) in isolated areas of Biak island, with predominantly indigenous populations.132 The decrease of anti-HAV prevalence was also observed in Lombok, where anti-HAV prevalence in students aged 12–14 years decreased from 64·8% to 13·6% over 30 years, from 1986 to 2016.132
Hepatitis A outbreaks, which occurred in several areas in Java (1998–2007) and in Sumatra and Borneo (2014), have been reported more frequently in areas with low prevalence of anti-HAV. Health education, as well as hygiene and sanitation promotion programmes, have been implemented in areas with hepatitis A endemicity. However, HAV vaccination is still not widespread and is not included in the national immunisation schedule, so it is only available to people in wealthy urban areas.
There are few reports about hepatitis E in Indonesia. Only three outbreaks of HEV infection that occurred in 1987, 1991, and 1998 have been documented in restricted areas (west Kalimantan [Borneo] and east Java) and were presumably caused by faecal contamination.133, 134, 135 It has also been reported that HEV is transmitted to humans through the consumption of uncooked or undercooked pork and viscera.136 In addition to outbreaks, HEV infection accounts for a considerable proportion of sporadic hepatitis infections with varying prevalence of anti-HEV in apparently healthy individuals in some areas.137 The risk of infection has been found to increase in association with occupational contact with swine and swine excrement.136, 137 Infection in humans is mostly due to genotype 1, whereas genotypes 3 and 4 are zoonotic.136 However, it was reported that genotype 4 has also been isolated from people with acute hepatitis E infection.138
In Pakistan, mortality related to acute hepatitis is also commonly caused by HAV and HEV. According to the GHE 2015 dataset, acute hepatitis A and E accounted for 18·8% and 29·7% of all deaths due to acute hepatitis in the country (table 2).1
Lack of clean water, poor sanitation practices, poor access to health facilities across the country, social and political upheavals, and many refugees are the main factors responsible for the high number of sporadic cases of HAV and HEV in Pakistan. The Viral Hepatitis Surveillance System in Pakistan reported 3825 cases of acute hepatitis from June, 2010, to October, 2014, of which 679 were due to acute HAV and 468 to acute HEV.139 Most children in Pakistan contract hepatitis A at an early age, leading to an almost 100% exposure by the age of 14 years, but HAV was reported in only 6% of adults.42, 140 Despite a subclinical, asymptomatic course in most children, acute liver failure was reported in 30 of 232 children with HAV seen at Aga Khan University Hospital (Karachi), with 36·7% mortality from 1991 to 1998.141
Approximately 80% of acute hepatitis in adults is attributed to HEV. In Pakistan, epidemics of acute viral hepatitis were reported as early as the 1950s and 1960s. Many outbreaks of hepatitis E had been wrongly assumed to be caused by HAV.42, 142 HEV has been found to be the main cause of acute-on-chronic liver failure in patients with underlying liver disease143, 144 and acute liver failure in pregnant women, with maternal mortality ranges from 36–71%. The frequency of acute liver failure is higher (10–22%) in pregnant women with HEV infection than in men and non-pregnant women (1–2%).145 HEV genotype 1 is prevalent in Pakistan, mainly transmitted via the faecal–oral route,146, 147 consistent with the observation that 44·7% of samples from sewage water samples and fresh vegetables are contaminated with HEV.148 The disease's subclinical course, the patient's expected self-recovery, and the high cost or unavailability of diagnostic tests for HAV and HEV mean that most cases are undiagnosed, leading to underestimated disease burden.42
Similar to Pakistan, HAV and HEV are common causes of mortality due to acute hepatitis in Bangladesh. Hepatitis A and E accounted for 2·8% and 31·1% of all deaths due to acute hepatitis in Bangladesh in 2015 (table 2).1 Historically, hepatitis A infection was thought to be hyperendemic in Bangladesh; a study from 2000 showed that 100% of children up to 6 years of age had been exposed and were immune to HAV.149 A 2009 seroepidemiological study showed a clear trend in anti-HAV seroconversion with age, where seropositivity progressively increased from 40·4% in children aged 1–5 years to more than 98·0% in adults older than 30 years, and very low anti-HAV seroprevalence of about 30% in children younger than 10 years in high-income settings.150 The prevalence of anti-HAV in people aged 20–40 years in Bangladesh has declined rapidly during the past three decades because of a general increase in socioeconomic status and hygiene standards.151 As a result, this age group has a high risk for HAV infection, and clinically overt hepatitis A is increasing in adolescents and adults.152 Although the endemicity of HAV seems to be decreasing, adolescents and adults with high socioeconomic status remain at particularly high risk of symptomatic and severe illness, because individuals of high socioeconomic status have a low chance of HAV infection as children.152 The clinical manifestations of hepatitis A depend on the age of the host: less than 30% of infected young children showed symptomatic hepatitis, whereas about 80% of infected adults had symptoms of severe acute hepatitis.151
HEV infection is also still common in Bangladesh and occurs sporadically throughout the year.153 In a longitudinal cohort study in rural Bangladesh, the incidence of hepatitis E infection was common (64 cases per 1000 person-years), even without epidemics of clinically obvious disease.154 HEV is the leading cause of acute hepatitis155 and has resulted in fatal outcomes in pregnancy, especially in the third trimester, and in patients with acute-on-chronic liver failure.156
By contrast with many other countries in the Asia-Pacific region, HAV and HEV rarely cause acute hepatitis-related mortality in Japan. Hepatitis A accounted for 2·3% of all deaths due to acute hepatitis in 2015, whereas there were no deaths due to acute hepatitis E, according to the GHE 2015 dataset (table 2).1 The number of cases with acute hepatitis caused by HAV that were reported to the Governmental Registry of Japan ranged from 128 to 433 cases per year in Japan and there has been no change in this incidence in the past 10 years.48 However, the incidence of acute hepatitis E has gradually increased from 2005 to 2013.48 There were 44 to 60 cases of acute HEV infection per year from 2006 to 2011, but this prevalence increased to more than 200 cases in 2015. This increase might be related to eating raw pork liver and boar and deer meat.48
Similar to Japan, HAV and HEV are rare causes of acute hepatitis-related mortality in South Korea: according to the GHE 2015 dataset, acute hepatitis A accounted for 0·8% of all deaths due to acute hepatitis in 2015, whereas there were no deaths due to acute hepatitis E (table 2).1 Improvements in sanitation and living standards have contributed to a change in the epidemiology of acute viral hepatitis in South Korea. The decrease in HAV infection in young children has resulted in a reduction in the seroprevalence of anti-HAV IgG, with a corresponding increase observed in the adult population.157 As a result, since 2000, hepatitis A has overtaken hepatitis B as the leading cause of acute viral hepatitis in adults in South Korea.158 In 2009, the incidence of hepatitis A was at its highest since 2000, and 15 231 cases were reported to the Korea Centers for Disease Control and Prevention, but in 2010 the number decreased to 7655.159 HAV infection was designated a national notifiable disease in 2001, and a surveillance system based on sentinel hospitals was established. The incidence has continuously decreased since 2011, the year when the surveillance system was expanded to every hospital. 7585 cases of HAV infection were reported through this National Infectious Diseases Surveillance system between 2011 and 2013, steadily declining in each of those years.160 Of these cases, 58 were caused by infection outside the country, and 7527 patients represented autochthonous HAV infection cases.160 HAV comprises up to 80% of all acute hepatitis infections in South Korea.67
HEV is not endemic in South Korea and is responsible for only 2% of acute viral hepatitis cases.161 Surprisingly, the seroprevalence for anti-HEV antibody was about 17–34% in South Koreans, according to surveys of the general population and blood donors done between 2003 and 2009, suggesting that there are many undetected, subclinical HEV infection cases.161, 162
Unlike South Korea, HAV is a common cause of deaths related to acute hepatitis in Australia, whereas HEV is a rare cause and only a few cases have ever been reported. Hepatitis A accounted for 25·9% of all deaths due to acute hepatitis in 2015 in Australia, whereas there were no deaths due to acute hepatitis E (table 2).1 In Australia, the number of hepatitis A cases reported per year has been declining nationally since the late 1990s from approximately 300–500 cases to 144 in 2011.163 Infection is usually related to high-risk groups such as infants in childcare facilities, users of injected drugs, men who have sex with men, and travellers to countries where infection is common. Occasional outbreaks due to consumption of contaminated shellfish have been reported. Hepatitis A vaccination is therefore recommended for high-risk groups.
Deaths related to acute HAV and HEV infections rarely occur in New Zealand. According to the GHE 2015 dataset, hepatitis A accounted for 1·9% of all deaths due to acute hepatitis in 2015, whereas there were no deaths due to acute hepatitis E (table 2).1 In New Zealand, the number of notified cases of hepatitis A has decreased from 347 in 1997 to 74 in 2014, or 1·6 per 100 000 individuals, with no deaths reported.164 Similar to Australia, only a few cases have of hepatitis E have ever been reported in New Zealand.
By contrast with New Zealand, HAV is prevalent as a cause of acute hepatitis-related deaths in Singapore, but HEV is rare. In Singapore, the GHE 2015 dataset documented that hepatitis A accounted for 50·1% of all deaths due to acute hepatitis in 2015, whereas there were no deaths due to acute hepatitis E (table 2).1 However, deaths from liver disease caused by acute hepatitis A and E are rare in Singapore (0·11% of all liver-related deaths). In 2012–16, 323 cases of acute hepatitis A and 345 cases of acute hepatitis E were reported.3 Most of these cases were local residents who contracted the disease overseas or foreigners who were working in Singapore. However, the overall number of cases has been declining and no deaths from acute hepatitis A and E have been reported between 2012 and 2016. For the entire 1997–2016 period, 1899 cases of hepatitis A and 961 cases of hepatitis E were reported.96
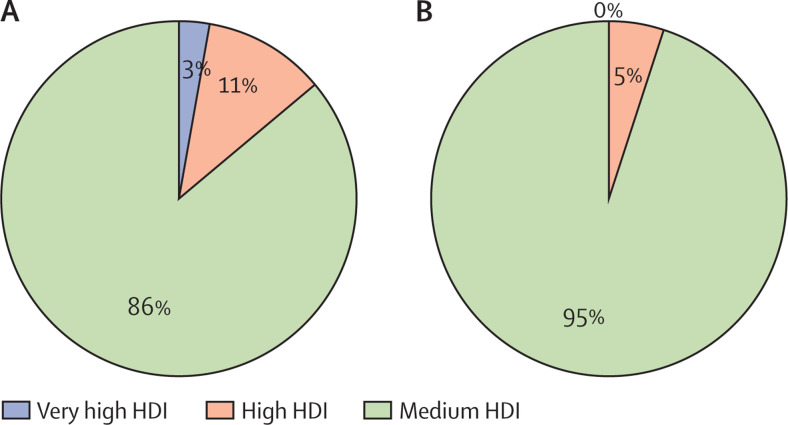
In summary, viral hepatitis A and E are a major cause of acute hepatitis-related morbidity and mortality in countries with medium and high HDIs in the Asia-Pacific region, the population of which has low access to clean drinking water and appropriate sanitation facilities. In these areas, acute HEV infection causes high mortality, especially in pregnant women and in patients with underlying chronic liver diseases. Acute HAV is increasingly leading to severe hepatitis in adults as the quality of sanitation is improving in certain localised areas of these regions, reducing earlier exposure and immunity to infection. In countries with very high HDIs, acute HAV, although rare, is seen predominantly in travellers to endemic areas, men who have sex with men, and people who inject drugs. Conversely, acute HEV infection is predominantly zoonotic and is acquired by eating infected meat or handling pigs.
Alcohol-related liver disease
According to the GHE 2015 dataset, alcohol consumption accounted for 20·0% of all deaths due to cirrhosis and other chronic liver diseases and for 35·5% of all deaths due to liver cancer in mainland China (table 2).1 According to WHO estimates from 2016, age-standardised mortality from cirrhosis in adult Chinese men was 14·6 per 100 000 individuals per year and in women was 8·3 per 100 000 per year, with 62·6% (in men) and 41·6% (in women) of these being attributable to alcohol.165
Data on nationwide, large-scale epidemiological surveys of alcohol-related liver disease are unavailable in China. The prevalence of alcohol-related liver disease in some Chinese studies ranges from 2·3% to 6·1% for the 2003–11 period, with a median prevalence of 4·5% in heavy drinkers with a drinking history of more than 5 years.166, 167, 168, 169 Incidence was at least 50% for alcohol-related steatosis, at least 10% for alcohol-related hepatitis, and at least 10% for alcohol-related cirrhosis, in heavy drinkers with a 5-year drinking history.170 In eastern China (Shandong province), the population-based prevalence of alcohol-related liver disease was 8·55% in 2011.171 Data from a big hospital specialising in infectious and liver diseases showed that alcohol-related liver disease accounted for 3·93% of all liver diseases, with the proportion increasing from 1·68% in 2002 to 4·59% in 2013 in hospitalised patients with liver diseases.172 Similarly, the proportion of patients with alcohol-related cirrhosis increased from 3·34% in 2002 to 8·40% in 2013, making it the third commonest cause of liver cirrhosis.173
In 2016, WHO's estimates of total annual alcohol consumption per capita for that year in people aged 15 years and older in China was 7·2 L of pure alcohol (11·7 L in men and 2·5 L in women), and total alcohol consumption per capita considering only people who drink (aged ≥15 years) was 26 L of pure alcohol (30·5 L in men and 11·3 L in women).165 Overall, 42·1% of people aged at least 15 years (29·1% of men and 55·6% of women) in mainland China abstain from alcohol throughout their lives.165 The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 40·7% (52·9% in men and 20·1% in women).165 Between 2006 and 2010, admissions to hospital for cirrhosis caused by viral hepatitis decreased by 10%, but admissions for alcohol-related cirrhosis increased by 33% in 31 hospitals in Beijing.174
In India, alcohol consumption is also a common cause of liver disease-related mortality. Alcohol consumption accounted for 22·2% of all deaths due to cirrhosis and other chronic liver diseases and for 19·9% of all deaths due to liver cancer in India, as reported by the GHE 2015 dataset (table 2).1 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Indian men and women were 45·8 per 100 000 individuals per year and 14·7 per 100 000 individuals per year, respectively, with 60·0% (in men) and 33·3% (in women) of these attributed to alcohol consumption.165 This prevalence might be underestimated because of poor reporting, low social acceptance of drinking, and no insurance cover for alcohol-related diseases. Of all deaths due to alcohol-related cirrhosis worldwide in 2015, 19·8% were estimated to occur in India; this is a high proportion, given that the Indian population comprises 17·8% of the global population, has a smaller proportion (72·3%) of people aged at least 15 years than the global average, and has a very high proportion of lifetime alcohol abstainers (53·5% of individuals aged ≥15 years in 2016) compared with other countries.165 WHO estimates indicate that the numbers of deaths due to alcohol-related cirrhosis in India increased by 22·7% (from 47 000 to 57 700) between 2000 and 2015.1
Rising incomes have led to an increase in per-capita annual alcohol consumption in Indian adults (those 15 years and older), from 1·8 L of pure alcohol in 2000 to 4·3 L in 2010 and 5·6 L in 2016.165 In 2016, nearly 53·5% (39·1% of men and 68·8% of women) of this age group were lifetime abstainers. The annual per-capita consumption of pure alcohol in current drinkers (aged ≥15 years) was 14·6 L (18·3 L in men and 6·6 L in women). The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 44·4% (55·1% in men vs 21·4% in women).
By contrast with India, alcohol consumption is an uncommon cause of mortality from liver disease in Indonesia, although data about alcohol-related liver disease are scarce. According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Indonesian men and women (aged ≥15 years) were 51·1 per 100 000 per year and 27·1 per 100 000 individuals per year, with 16·5% (in men) and 15·2% (in women) of these being attributable to alcohol.165 Alcohol consumption reported in the GHE 2015 dataset accounted for 9·8% of all deaths due to cirrhosis and other chronic liver diseases and for 14·7% of all deaths due to liver cancer in Indonesia (table 2).1 Alcohol consumption in Indonesia is one of the lowest in southeast Asia.165 In 2016, WHO's estimates of total alcohol consumption per capita in people aged at least 15 years in Indonesia was 0·8 L of pure alcohol (1·4 L in men and 0·2 L in women) and total alcohol per capita in this age group, only for people who drink, was 3·4 L of pure alcohol (4·2 L in men and 1·5 L in women). Overall 57·2% of people aged 15 years and older (42·6% of men and 71·8% of women) in Indonesia are lifetime abstainers. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 28·6% (35·9% in men and 10·8% in women).165 Alcohol in Indonesia is expensive and difficult to obtain, so people in some areas drink five times more unrecorded (ie, unaccounted for in official statistics, taxation, or sales because it is produced, distributed, and sold outside channels under government control) than legally purchased alcohol.175 In 2016, WHO's estimates of total alcohol consumption per capita in people aged at least 15 years in Indonesia was 0·8 L of pure alcohol, of which 0·3 L was recorded and 0·5 L was unrecorded.
Similar to Indonesia, alcohol is an uncommon cause of liver disease-related mortality in Pakistan. According to the GHE 2015 dataset, alcohol consumption accounted for 5·6% of all deaths due to cirrhosis and other chronic liver diseases and for 8·3% of all deaths due to liver cancer (table 2).1 According to WHO's 2016 estimates, age-standardised mortality from cirrhosis in adult Pakistani men was 28·7 cases per 100 000 people for that year, with 12·8% of these being attributable to alcohol. For women, these proportions were 30·1 cases per 100 000 people and 3·2%. In 2016, the projected estimates of total alcohol consumption per capita (people aged ≥15 years) in Pakistan was 0·3 L of pure alcohol (0·5 L in men and 0·1 L in women) and total alcohol per capita considering drinkers only was 26 L of pure alcohol (30·5 L in men and 11·3 L in women). Overall, 96·5% of Pakistani people aged at least 15 years (94·7% of men and 98·4% of women) are lifetime abstainers. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 5·3% (6·5% in men vs 1·5% in women). Alcohol use disorder has been reported in 0·3% of men and in 0·1% of women. The unrecorded per-capita annual total alcohol consumption in 2016 in people aged at least 15 years was 0·3 L of pure alcohol, almost all of which was unrecorded.165 However, it has been presumed that alcohol use is underreported in Pakistan because of religious and cultural issues and lack of social acceptance.
Liver disease-related mortality is uncommon in Bangladesh as well. Data from the GHE 2015 dataset estimate that alcohol consumption accounted for 8·7% of all deaths due to cirrhosis and other chronic liver diseases and for 10·8% of all deaths due to liver cancer (table 2).1 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Bangladeshi men were 35·8 per 100 000 individuals per year and in women they were 15·2 per 100 000 per year, with 10·0% (in men) and 8·4% (in women) of these attributable to alcohol.165 There are no systematic data about prevalence of alcohol-related liver diseases in Bangladesh. In a survey involving 59 227 patients from all regions of Bangladesh and encompassing most medical institutions in the country, alcohol-related liver diseases occurred in less than 0·8% of patients with liver diseases.176
Because of religious beliefs and social taboos, alcohol use is uncommon in Bangladesh, although home-made alcohol is consumed by different tribes. The annual per capita consumption of pure alcohol in adults aged at least 15 years is very low in Bangladesh (0·2 L in 2010 and 0·0 L in 2016) compared with 4·5 L in the WHO-defined southeast Asia region in 2016.165 Overall, 92·5% of people in this age group (88·9% of men and 96·1% of women) are lifetime abstainers. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 36·8% (43·1% in men vs 14·4% in women). In 2010, WHO's estimates of total alcohol consumption per capita in people aged at least 15 years in Bangladesh was 0·2 L of pure alcohol, almost all of which was unrecorded and is likely to be underestimated, similar to Pakistan.
Unlike Bangladesh, alcohol is a not a rare cause of liver disease-related mortality in Japan. According to the GHE 2015 dataset, alcohol consumption accounted for 13·8% of all deaths due to cirrhosis and other chronic liver diseases and for 16·4% of all deaths due to liver cancer (table 2).1 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Japanese men and women were 10·9 per 100 000 individuals per year and 4·3 per 100 000 individuals per year, respectively, and 67·8% (in men) and 48·6% (in women) of these were attributed to alcohol consumption. In Japan, the consumption of alcohol per year per adult decreased by about 80% during the past 20 years. In 2016, WHO's estimates of total alcohol consumption per capita in Japanese adults aged at least 15 years was 8·0 L of pure alcohol (13·5 L in men and 2·9 L in women) and total alcohol consumption per capita in this age group for drinkers only was 14·1 L (19·0 L in men and 6·6 L in women). Overall, 9·1% of Japanese people aged at least 15 years (4·3% of men and 13·7% of women) are lifetime abstainers. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 40·0% (53·0% in men and 20·3% in women).165 Alcohol-related hepatocellular carcinoma accounts for 6·3–7·2% of all hepatocellular carcinoma cases in Japan.177
Alcohol is also a common cause of liver disease-related mortality in South Korea. Alcohol consumption accounted for 27·7% of all deaths due to cirrhosis and other chronic liver diseases and for 21·4% of all deaths due to liver cancer, according to the GHE 2015 dataset (table 2).1 In 2016, WHO's estimates of total alcohol consumption per capita in South Korean adults aged at least 15 years was 10·2 L of pure alcohol (16·7 L in men and 3·9 L in women) and total alcohol consumption per capita for drinkers in this age group only was 16 L of pure alcohol (21·7 L in men and 7·6 L in women). Overall, 7·1% of adults aged at least 15 years (3·3% of men and 10·8% of women) do not drink alcohol throughout their lives. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 47·7% (62·2% in men and 26·6% in women).165 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult South Korean men and women were 18·5 per 100 000 per year and 4·5 per 100 000 individuals per year, respectively, with 74·5% (in men) and 56·3% (in women) of these due to alcohol consumption. The Korea National Health and Nutrition Examination Survey (KNHANES) is a nationwide, population-based, cross-sectional health examination and survey done regularly by the Division of Chronic Disease Surveillance of the Korea Centers for Disease Control and Prevention in the Ministry of Health and Welfare. KNHANES 2012 reported a significant proportion of individuals with high-risk alcohol consumption: 21·8% of men had more than seven glasses of alcohol more than twice a week, and 6·0% of women had five glasses.178 In this study, one glass is equivalent to about 8 g of pure alcohol, which can be found in 220 mL of beer with 4·5% alcohol and 50 mL of distilled spirits with 19% alcohol.
Alcohol-related liver disease is prevalent and is a common cause of hospital admission and mortality of patients with advanced liver disease in Australia. According to the GHE 2015 dataset, alcohol consumption accounted for 33·4% of all deaths due to cirrhosis and other chronic liver diseases and for 37·9% of all deaths due to liver cancer in Australia (table 2).1 In 2012, there were 6203 individuals with alcohol-related liver disease and this proportion was projected to increase by nearly 12% by 2030 to 7824.81 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Australians were 9·6 per 100 000 per year in men and 3·7 per 100 000 per year in women, with 74·1% (in men) and 62·5% (in women) of these related to alcohol consumption. In 2016, WHO's estimates of total alcohol consumption per capita in Australian adults aged at least 15 years was 10·6 L of pure alcohol (16·6 L in men and 4·7 L in women) and total alcohol consumption per capita for drinkers in this group was 13·4 L of pure alcohol (18·8 L in men and 6·6 L in women). Overall, 8·5% of Australian adults aged at least 15 years (4·1% of men and 12·9% of women) are lifetime abstainers from alcohol. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 45·3% (60·7% in men and 26·4% in women).165
The prevalence of harmful alcohol use in Indigenous Australians is about twice as high as that of non-Indigenous Australians.179 Indigenous Australians also have a higher prevalence of alcohol-related liver disease.179 In people aged 35–54 years, liver diseases are the second largest contributor in men (12%) and the largest in women (16%) to the mortality gap between Aboriginal and Torres-Strait Islander people and other Australians.179 Most of the difference in years of life lost is attributed to alcohol-related liver disease (9% in men and 10% in women).
Similar to Australia, alcohol consumption is a common cause of liver disease-related mortality in New Zealand. 36·4% of all deaths from cirrhosis and other chronic liver diseases, and 44·2% of all deaths due to liver cancer, were due to alcohol consumption as per GHE 2015 data (table 2).1 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult men and women in New Zealand were 4·9 and 2·0 per 100 000 individuals per year, respectively, and 74·5% (in men) and 61·2% (in women) of these were attributable to alcohol consumption. In 2016, WHO's estimates of total alcohol consumption per capita in adults aged at least 15 years for New Zealand was 10·7 L of pure alcohol (17·2 L in men and 4·6 L in women) and total alcohol consumption per capita in drinkers from this age group was 14·3 L of pure alcohol (20·2 L in men and 7·1 L in women). Overall 10·6% of adults aged at least 15 years (5·1% of men and 15·8% of women) in New Zealand are life-time abstainers. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 42·9% (58·0% in men and 24·4% in women).165
Alcohol is responsible for a small but important proportion of deaths due to liver disease in Singapore. According to the GHE 2015 dataset, alcohol consumption accounted for 4·9% of all deaths due to cirrhosis and other chronic liver diseases, and for 10·8% of all deaths due to liver cancer (table 2).1 According to 2016 WHO estimates, age-standardised deaths from cirrhosis in adult Singaporean men and women were 4·4 and 2·4 per 100 000 individuals per year, respectively, and 30·3% (in men) and 34·9% (in women) of these were attributable to alcohol cosnumption.165 The 2010 Singapore Burden of Disease survey reported that, in patients admitted for hospital treatment with liver cirrhosis in 1991–2010, 27·6% of cases were alcohol-related and 68·5% were non-alcohol-related.90 A study of 564 patients with liver cirrhosis treated in a major public hospital in Singapore showed that 11·2% of these patients were admitted because of alcohol-related liver disease.180 Consequently, alcohol-related liver disease can be considered a small but important cause of liver cirrhosis. In 2016, WHO's estimates of total alcohol consumption per capita in Singaporean adults aged at least 15 years was 2·0 L of pure alcohol (3·3 L in men and 0·8 L in women) and total alcohol consumption per capita in this age group for drinkers only was 2·9 L of pure alcohol (4·0 L in men and 1·4 L in women). Overall, 6·7% of Singaporean adults aged at least 15 years (3·1% of men and 10·2% of women) never consume alcohol throughout their lives. The prevalence of heavy episodic drinking in 2016 for drinkers only (≥15 years) was 42·9% (57·4% in men and 23·5% in women).165
In summary, commensurate with an increase in mean incomes, per-capita alcohol consumption has increased in the Asia-Pacific region, especially China and India, but not in Muslim-dominated countries.181 A systematic analysis of comparative risk of 84 behavioural, environmental, occupational, and metabolic risk factors or clusters of risk factors (based on the GBD Study) reported that, globally, alcohol is estimated to be the seventh-leading risk factor for DALYs in 2016 and that alcohol-attributable DALYs have increased by more than 25% between 1990 and 2016, driven primarily by increased consumption in south Asia, southeast Asia, and central Asia, in both men and women. The largest increases in exposure have been in countries in the low-to-middle quintile of the GBD sociodemographic index (SDI).182 These changes are likely to increase alcohol use and the burden of alcohol-related liver disease in the future.
NAFLD and other causes of liver disease
Systematically collected data regarding the contribution of other liver diseases—including autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, and IgG4-related liver disease—to liver disease-related morbidity and mortality in the Asia-Pacific region are insufficient; these conditions are categorised in the GHE 2015 dataset together with NAFLD as “other causes”.1 Autoimmune liver diseases are rare across Asia-Pacific. By contrast, drug-induced liver injury is relatively common in some areas—eg, China (where acute drug-induced liver injury accounts for approximately 20% of hospital admissions due to acute liver injury)183 and India (where anti-tuberculosis drugs, complementary medicines, and herbal drugs and supplements are common causes). Although often under-recognised and under-reported, drug-induced liver injury seems to be increasing in some areas of the Asia-Pacific region. The following section, however, focuses on NAFLD, given the relatively small contribution made by other causes of liver disease to the overall burden.
GHE 2015 data show that NAFLD and other causes accounted for 11·7% of all deaths due to cirrhosis and other chronic liver diseases, and for 10·5% of all deaths due to liver cancer in mainland China (table 2).1 Changing lifestyles and dietary habits have resulted in an increased prevalence of NAFLD in mainland China. Population-based epidemiological studies have indicated that the prevalence of NAFLD in China is 6·3–27·0% in adults, with prevalence being higher in urban areas than rural areas, in men than women, and in the eastern coast than further inland.170 As shown by a systematic review of articles published between 1997 and 2013, the overall prevalence of NAFLD was about 20% in mainland China.184 The prevalence of NAFLD was reported to be 15·35% in 2005 in Shanghai185 and has approximately doubled in the past decade.186 An estimated 1·3–2·1% of schoolchildren have NAFLD.187 Incident NAFLD is not uncommon in lean people; a cross-sectional study of 6905 people without obesity188 estimated that 7·3% of them had NAFLD at baseline. By the end of the study's 5-year follow-up, 494 (8·9%) of 5562 people who completed the study had developed NAFLD. Total case estimates of prevalent NAFLD in 2016 in China were 243·67 million, with 32·61 million cases of non-alcoholic steatohepatitis (NASH), 1·09 million cases of cirrhosis, and 7000 cases of hepatocellular carcinoma due to NAFLD.189
With economic growth in mainland China averaging 10% over the past 30 years, a westernised diet and a sedentary lifestyle have drastically reshaped the pattern of Chinese daily life. The gradually growing prevalence of obesity, type 2 diabetes, dyslipidaemia, and metabolic syndrome has put the Chinese population at risk of developing NAFLD.190
Similar to China, NAFLD is an important cause of liver disease-related mortality in India. The GHE 2015 dataset documented that NAFLD and other causes accounted for 10·9% of all deaths due to cirrhosis and other chronic liver diseases, and for 9·6% of all deaths due to liver cancer (table 2).1 Risk of developing NAFLD is influenced by several environmental and metabolic factors, including obesity, type 2 diabetes, and physical inactivity, which are common in the Indian population.191 In the general population, according to community-based studies, the prevalence of NAFLD on ultrasonography in urban areas was 18·9% in 2007 and 32·0% in 2009,192, 193 and in rural areas was 8·7% in 2010 and 30·7% in 2016.194, 195 In urban, hospital-based studies, this prevalence was 25·3% in 2012 and 32·2% in 2009.196, 197 The prevalence is higher in high-risk groups, such as people with type 2 diabetes (10·5–88%)198, 199 or obese people (50–80%).192, 200 11–32% of patients with NAFLD had a normal body-mass index (BMI).201
The number of overweight and obese adults in India had nearly doubled to 18·6% in 2015–16 from 9·3% in 2005–06 in men, and to 20·7% from 12·6% in women.202 Additionally, there are currently 69·2 million adults with type 2 diabetes aged 20–79 years, and this population is likely to increase to 123·5 million by 2040,203 which would probably lead to an increase in the burden of NAFLD.
In hospital-based studies, liver biopsies in nearly half of patients with NAFLD with increased aminotransferase concentrations had histologically confirmed NASH, although most (80–98%) had only stage 1 or stage 2 changes.204, 205 Patients with NASH who have a normal or low BMI are common in India, as was seen in a large series of histologically proven cases.201 Longitudinal studies on the natural history of NAFLD and NASH in Indian patients are scarce. In hospital-based studies between 2003 and 2011, cryptogenic cirrhosis, believed to be largely due to NAFLD progression, accounted for 15·8–48·8% of patients with cirrhosis.206 Additionally, 4·6–19% of patients with liver cancer did not have hepatitis B or C or did not drink alcohol.207, 208
In Indonesia, NAFLD is also becoming an important cause of liver disease-related mortality. According to the GHE 2015 dataset, NAFLD and other causes accounted for 17·4% of all deaths due to cirrhosis and other chronic liver diseases, and for 20·9% of those due to liver cancer (table 2).1 Data on the prevalence of NAFLD have been scarce in Indonesia.209 However, risk factors for NAFLD (ie, type 2 diabetes, increased triglycerides, low HDL-cholesterol, and metabolic syndrome exemplified by obesity, type 2 diabetes, hypertension, and increased waist circumference), are prevalent and increasing in Indonesia.210
Age-standardised estimates for Indonesian adults aged 20 years and older analysed by the NCD Risk Factor Collaboration (NCD-RisC) showed increasing prevalence of type 2 diabetes from 3·2% for men and 4·1% for women in 1975 to 7·4% for men and 8·0% for women in 2014 (appendix p 6).210 They also showed an increase in the prevalence of obesity from 0·2% for men and 0·7% for women in 1975 to 5·0% for men and 9·3% for women in 2016. Moreover, age-standardised obesity for children and adolescents aged 5–19 years has drastically increased from 0·10% in 1975 to 7·1% in 2016.211 These children and adolescents are at a high risk of progressive liver disease in the future because weight gain during school years carries a higher risk of NAFLD than weight gain in late adulthood.212
NAFLD is also becoming an important cause of liver disease-related mortality in Pakistan. NAFLD and other causes accounted for 21·6% of all deaths due to cirrhosis and other chronic liver diseases, and for 11·8% of all deaths due to liver cancer, according to GHE 2015 data (table 2).1 Increasing incidence of obesity and metabolic syndrome could lead to high burden of NASH that causes cirrhosis and hepatocellular carcinoma. Data on NAFLD from Pakistan are scarce. The prevalence of NAFLD has been reported as 9–27% in rural areas and as 21–42% in urban areas, reflecting the impact of industrialisation and urbanisation on lifestyle and disease status.213 Presence of metabolic syndrome or its individual components were found to be major contributing factors associated with increased prevalence of NAFLD in communities, with most cases being found in women.214, 215, 216 In a hospital-based study,217 the prevalence of NAFLD and the multiplicative effect of combinations of predictive factors associated with NAFLD were studied in patients with newly diagnosed type 2 diabetes; NAFLD was found in 71·9% of cases. Additionally, an increasing trend in the odds ratio of having NAFLD was observed as the number or risk factors increased. A combination of physical inactivity, hypertension, dyslipidaemia, large waist circumference, high BMI, high HbA1c, high triglycerides, low HDL, high LDL, and high alanine aminotransferase predicted the highest odds of 10·8 for NAFLD (95% CI 4·9–24; p=0·001).217 In a large community-based study of 1225 individuals, NAFLD was found in 741 (60·5%); this proportion was higher in those with impaired glucose tolerance and type 2 diabetes.217 Considering the increasing burden of type 2 diabetes and other non-communicable diseases, NAFLD is emerging as a major threat for the health-care system in Pakistan.
Similar to Pakistan, NAFLD is causing high liver disease-related mortality in Bangladesh. In the GHE 2015 dataset, NAFLD and other causes accounted for 13·2% of all deaths due to cirrhosis and other chronic liver diseases, and for 12·2% of those due to liver cancer (table 2).1 NAFLD is increasing in Bangladesh because of changing dietary patterns and sedentary lifestyles. In a large cross-sectional study done in urban and rural areas of Bangladesh, the prevalence of NAFLD determined by ultrasound was 36·9% (95% CI 33·0–40·3) in rural and 33·0% (31·0–39·9) in urban areas. The prevalence was 71·2% (64·1–77·4) in people with diabetes and 63·6% (59·4–67·5) in obese individuals (BMI ≥27·50 kg/m2).218 By comparison, a rural study in Bangladesh showed that the overall prevalence of NAFLD was 18·4% (12·4–25·6).219
The prevalence of overweight, obesity, and diabetes in Bangladesh has increased in the past three decades, thus increasing the NAFLD-related liver disease burden. Data from the 2011 Bangladesh Demography and Health Survey reported an overall prevalence of 18·9% (95% CI 17·9–19·9) of overweight and 4·6% (4·0–5·2) of obesity; people living in urban areas were more likely to be overweight or obese than those living in rural areas (odds ratio [OR] 1·27, 95% CI 1·05–1·55; p=0·02).220 There has been a substantial increase in overweight and obesity from the early 1990s when their prevalence was reported to be 4%.220, 221 The prevalence of type 2 diabetes has increased 2·5 times in Bangladesh, from 4% in 1990 to 10% in 2011.222 Additionally, a study done in a tertiary care liver clinic estimated the prevalence of biopsy-proven NASH in people with NAFLD to be 42·4%.223
Liver diseases caused by lifestyle factors have gained importance in Japan as the proportion due to viral hepatitis has decreased. According to the GHE 2015 dataset, NAFLD and other causes accounted for 8·6% of all deaths due to cirrhosis and other chronic liver diseases, and for 3·3% of all deaths due to liver cancer (table 2).1 Case estimates of the total prevalence of NAFLD in 2016 were 22·7 million, with 3·79 million cases of NASH, 0·19 million cases of cirrhosis, and 2200 cases of hepatocellular carcinoma due to NAFLD.189
In 1992, the prevalence of new cases of non-B, non-C hepatocellular carcinoma was only 6·5%, but in 2010 it increased to 24·1% (appendix p 7).224 The number of patients who died with non-B, non-C hepatocellular carcinoma increased 5·4 times in 24 years, from 1741 in 1992 to 9389 in 2015. The relative increase of non-B, non-C hepatocellular carcinoma is due to the decrease in the number of cases caused by HCV.
The prevalence of obesity (BMI≥25) in men (aged 20–69 years) increased from 25% to 30% between 1995 and 2005 (appendix p 8) but plateaued and began to decline over the subsequent 8 years, according to e-Stat, Japan's official statistics portal. Conversely, the prevalence of obesity in women has gradually decreased throughout this period.
NAFLD is also gaining greater importance as a cause of liver disease-related mortality in South Korea. The prevalence of NAFLD in South Korea is estimated to range from 16·1–42·9%.225, 226 4·7% of all deaths due to cirrhosis and other chronic liver diseases, and 2·6% of those due to liver cancer, were due to NAFLD and other causes according to GHE 2015 data (table 2).1 NAFLD has gained clinical attention because of its increasing prevalence, owing to a westernised diet and sedentary lifestyle and thus to an increasingly obese population.227 Indeed, over the past two decades, the prevalence of NAFLD has nearly doubled in South Korea, with a study reporting that it was 1178 (42·9%) of 3033 of recruited participants for 2013–14.228 A 1997 study in people who had undergone health screenings found that the prevalence of NAFLD was 19·7%.229
As with South Korea, NAFLD is becoming an important cause of liver disease-related mortality in Australia. GHE 2015 data suggest that NAFLD and other causes accounted for 6·9% of all deaths due to cirrhosis and other chronic liver diseases, and for 7·3% of all deaths due to liver cancer (table 2).1 NAFLD is by far the most prevalent form of chronic liver disease in Australia, estimated to affect 5·5 million people, including 40% of all adults aged 50 years and older, and representing about 90% of the liver disease burden.81 In 2014–15, 63·4% of Australians aged 18 years and older were overweight or obese (11·2 million people), comprising 35·5% who were overweight (6·3 million people) and 27·9% who were obese (4·9 million people).75 Furthermore, NAFLD currently affects 15% of school children, which will probably affect its future burden.81 The estimated annual total cost of obesity in Australia (which has doubled since 2005) was $58·2 billion in 2008.230 Globally and in Australia, given the population prevalence of NAFLD, it is becoming an increasing risk factor for the development of hepatocellular carcinoma, even in people without liver cirrhosis.
Indigenous Australians have a higher prevalence of type 2 diabetes than non-Indigenous Australians: Aboriginal and Torres Strait Islander adults are 3·5 times more likely than non-Indigenous adults to have diabetes.179, 231 69% of Aboriginal and Torres Strait Islander people older than 18 years were considered to be overweight (29%) or obese (40%) in 2012–13, and this likelihood was 1·2 times more than in non-Indigenous adults.232
In New Zealand, NAFLD is also gaining prominence as a cause of liver mortality. According to the GHE 2015 dataset, NAFLD and other causes accounted for 7·6% of all deaths due to cirrhosis and other chronic liver diseases, and for 6·8% of all deaths due to liver cancer (table 2).1 The prevalence of obesity in New Zealand has also drastically increased since 1990 (10% in men and 13% in women for that year).233 The New Zealand Health Survey Results for 2015–16 indicate that almost one in three adults (aged 15 years and older) were obese (32%) and a further 35% of adults were overweight.234 Health-care costs attributable to obesity were estimated to be NZ$686 million (4·5% of New Zealand's total health-care expenditure in 2006), or $911 million when lost productivity was included. Data on liver enzymes as indirect indices of NAFLD from a nutritional survey of more than 4721 New Zealanders aged 15 years and older indicated that the prevalence of increased concentrations of alanine aminotransferase and γ-glutamyltransferase was approximately 13% for 2008–09.235
As with New Zealand, NAFLD is gaining prominence as a cause of liver mortality in Singapore. NAFLD and other causes accounted for 8·3% of all deaths due to cirrhosis and other chronic liver diseases in the GHE 2015 dataset, and for 5·7% of all deaths due to liver cancer (table 2).1 There are no formal studies of prevalence of fatty liver disease in Singapore but at a 2012 public health forum, 40% of 227 attendees were diagnosed with a fatty liver.236 In a study of fatty liver disease in patients undergoing cholecystectomy, the prevalence increased over time in a 10-year period, from 40% to 56·6%.237 In the Singapore Chinese Health Study,238 a large prospective cohort study, 63 257 patients were followed up since 1993–98 for an average of 14 years; of them, 499 developed hepatocellular carcinoma. People with diabetes in this study had a hazard ratio of 2·14 (95% CI 1·69–2·71) of developing hepatocellular carcinoma. This effect was independent of markers for viral hepatitis. In the study, a history of diabetes was present in 8·9% of the population at baseline.238 Data from the Singapore Ministry of Health showed that 11·3% of Singaporeans had diabetes in 2010, representing an increase from 8·2% in 2004.239 Since diabetes is a major risk factor for fatty liver disease and NASH other than obesity, this increase provides some insight into the potential increase in burden of NAFLD. The Ministry of Health also found that there was an increasing trend of obesity from 6·9% in 2004 to 10·8% in 2010 and 8·6% in 2013.93 The general lifestyle of Singaporeans involves low physical activity and high-calorie diets, both of which increase the risk of obesity and diabetes, and thus the risk of NAFLD.
In summary, data on NALFD epidemiology in the Asia-Pacific region indicate a rapid increase in the disease's burden over the past three decades, which is supported by a systematic review and meta-analysis that assessed the prevalence, incidence, and outcomes of NAFLD in Asia.240 The analysis estimated that the overall prevalence of NAFLD was 29·62% (95% CI 28·13–31·15), with prevalence increasing significantly over time.240 Obesity and NAFLD are being increasingly recognised and are an emerging epidemic in the region, irrespective of country or regional income. South Asia and the Indian subcontinent are currently undergoing rapid economic and social change. The whole Asia-Pacific region is shifting towards increased consumption of energy-dense food and reduced physical activity, leading to increasing prevalence of NAFLD risk factors, such as diabetes and obesity.
Economy, health-care infrastructure, and policies related to liver diseases
According to World Bank data,241 the Chinese economy is the second largest in the world in nominal terms, might be the largest by purchasing power parity (PPP) as of 2013, and was the sixth fastest-growing major economy in the world, with a growth rate of 6·7% in 2016.242 The per-capita gross national income (GNI) in 2012 was US$ 10 890 in PPP terms.243 The country's health-care expenditure (about 5·55% of gross domestic product [GDP] in 2014) compares well with other similarly-placed countries.244 In 2009, the Government launched an ambitious health-care reform initiative and by 2015, 95% of the population had health insurance.245
Antiviral drugs for HBV, including conventional and pegylated interferons, entecavir, tenofovir, lamivudine, adefovir, and telbivudine, have been on the national reimbursement list since early 2017 (see table 3 for the status of policies and interventions against viral hepatitis in China). Direct-acting antiviral drugs against HCV, such as simeprevir, asunaprevir, daclatasvir, sofosbuvir, velpatasvir, ombitasvir/paritaprevir/ritonavir plus dasabuvir, elbasvir, and grazoprevir have been approved and are already on the reimbursement lists in some provinces.
Table 3.
Status of various policies and interventions to contain viral hepatitis in the Asia-Pacific region
| India | Pakistan | Bangladesh | China | Japan | South Korea | Indonesia | Taiwan | Singapore | Australia and New Zealand | |
|---|---|---|---|---|---|---|---|---|---|---|
| National plan | Yes | Yes | In drafting stage | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Reliable national epidemiological data | No | Yes (national) | No | Yes | Yes | Yes | No | Yes | No | Yes |
| Reliable economic burden data | No | No | No | Yes | Yes | Yes | No | Yes | No | Yes |
| Mandatory screening for HBV and HCV of donated blood | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mandatory nucleic-acid testing for screened blood | No | No | No | Yes | Yes | Yes | Yes (12 tertiary care centres for blood screening in surrounding areas) | Yes | Yes | Yes |
| Safe injections policy implementation | Yes (not well applied) | No | Yes (not well applied) | Yes | Yes | Yes | Yes | Yes | Yes (institution level since 2015 after hepatitis C outbreak) | Yes |
| Needle exchange and opioid substitution programmes for intravenous drug users | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No (zero-tolerance policy on drugs) | Yes |
| Children with 3 doses of hepatitis B vaccine (%, year) | 63·0%, 2015–16 | 54·0% (by the age of 12–23 months), 2015 | 97·0%, 2016 | 99·0%, 2016 | 99·0%, 2016 | 99·0%, 2016 | 93·3%, 2016 | 97·9%, 2017 | 96·1%, 2016 | 100% (children born after May 1, 2000), 2016 |
| Birth dose HBV vaccine coverage (%) | 45·0%, 2015 | No (pentavalent vaccine given at 6, 10, and 14 weeks of age) | No | 90·0%, 2016 | 99·0%, 2016 | 99·0%, 2016 | 32·4%, 2016 | 98·7%, 2016 | 100% (assumed, no data available) | >95 ·0% (children born to mothers with hepatitis B receive vaccine and hyperimmune globulin within first 24 h after delivery and complete doses thereafter), 2016 |
| HBV vaccination for health-care workers | Yes | Yes (80% coverage) | Piloting stage | Partially | Yes | Yes | No | Yes | Yes | Yes |
| Publicly funded HBV and HCV screening programmes | In a few states | Yes | No | Yes | Yes | Yes for HBV; for HCV only (abnormal ALT >60 IU/mL) | Started in a few areas, will be expanded to the whole country | Yes for narrow age ranges (≥18 years vs ≤years) | Yes (National Childhood Immunisation Programme) | Yes |
| HBV screening for pregnant women | No | No | No | Yes | Yes | Yes | To be implemented | Yes | Yes | Yes |
| HBV medicines on national essential medicines list or subsidised by the Government | Yes | Yes | No | Partially | No | 70% subsidised by national insurance reimbursement policy | Provided via Government-owned insurance | Yes | Yes (entecavir and tenofovir) | Yes |
| HCV medicines on national essential medicines list or subsidised by the Government | Yes | Yes | Free direct-acting antiviral drugs in piloting stage | Partially | No | 70% subsidised by national insurance reimbursement policy | In application to Indonesian FDA | Yes | Yes (pegylated interferon and ribavirin) | Yes |
| Households with an improved drinking water source (%, year) | 89·9%, 2015–16 | 93·0%, 2012–13 | 98·0%, 2017 | 95·5%, 2015 | 97·0%, 2016 | >90·0% (water purification controlled by Waterworks Bureau except rural areas), 2015 | 45·5%, 2007 | 93·4%, 2015 | 100%, 2016 | 100%, 2016 |
| Households using improved sanitation facility (%, year) | 48·4%, 2015–16 | 59·5%, 2012–2013 (unshared facility); 9·6% (shared facility) | 75·0% (2017) | 76·5%, 2015 | 99·7%, 2016 | >90·0%, 2015 | .. | 100%, 2015 | 100%, 2016 | 100%, 2016 |
| National sanitation and cleanliness programme | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Status of HAV vaccination | Not in a national programme (currently not needed) | Not in a national programme | Not in a national programme | Yes | Not in a national programme | Yes | Not in a national programme | Yes (for all neonates, 70·9% born in 2012–16 received 2 doses) | Not in a national programme | Recommended for particular high-risk groups |
ALT=alanine aminotransferase.
The public health system of mainland China consists of national and local Centers for Disease Control and Prevention and has functioned well in the prevention of viral hepatitis, with current coverage and timely free universal vaccination of infants against HBV exceeding 90%. China has released national action plans for control of viral hepatitis that set clear targets on prevention. However, a specific, large-scale, test-and-treat financed programme for patients with chronic hepatitis B or C is still to be established. Guidelines for prevention and control of hepatitis B and hepatitis C have been published and are regularly updated, with most recommendations in line with the major international guidelines.246, 247 To facilitate clinical research and evidence-based decision making for clinical practice and public health, a nationwide hospital-based registry for patients with chronic hepatitis B was initiated in 2012, which might prove to be essential to investigate disease burden and long-term outcomes in patients with chronic hepatitis B in a real-world setting.248
Many aspects of alcohol policy are weaker in China than in its neighbouring countries (table 4 ). For example, China has no enforceable legal drinking age and does not regulate when or where alcoholic products are sold. An advertising regulation on alcoholic beverages was issued in 1995, but its enforcement has also been weak. Moreover, taxation in China has not been used to improve public health. Few treatment programmes are available in China for people with alcohol use disorders. Although some psychiatric hospitals in China have special addiction units for the treatment of patients with alcohol-related mental disorders, most of these units, which were established in the 1990s, are in major cities.181
Table 4.
Status of various policies and interventions to reduce harmful alcohol use in the Asia-Pacific region
| India | Pakistan | Bangladesh | China | Japan | South Korea | Indonesia | Singapore | Taiwan | Australia | New Zealand | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Written policy on alcohol | |||||||||||
| National policy | Subnational | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| National action plan | No | No | No | No | Yes | No | No | No | Yes | Yes | No |
| Excise tax | |||||||||||
| Beer | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Wine | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Spirits | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| National legal minimum age for on-premise and off-premise sales of alcoholic beverages | |||||||||||
| Beer | State-specific | Total ban | No | No | 20 years | 19 years | 21 years | 18 years | 18 years | 18 years | 18 years |
| Wine | State-specific | Total ban | No | No | 20 years | 19 years | 21 years | 18 years | 18 years | 18 years | 18 years |
| Spirits | State-specific | Total ban | No | No | 20 years | 19 years | 21 years | 18 years | 18 years | 18 years | 18 years |
| Restrictions for on-premise and off-premise sales of alcoholic beverages | |||||||||||
| Working hours | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No | Yes |
| Weekdays | Yes | Yes | Yes | No | No | No | No | Yes | No | No | Yes |
| Types of premises | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No | No |
| Density of alcohol outlets per area | No | Yes | No | No | No | No | .. | Yes | No | No | No |
| Specific events | Yes | Yes | Yes | No | No | No | No | Yes | No | No | Yes |
| Intoxicated people | No | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes |
| Petrol stations | No | Yes | Yes | No | No | No | No | Yes | No | No | Yes |
| National maximum legal blood-alcohol concentrations when driving (%) | |||||||||||
| General population | 0·03% | Total ban | Total ban | 0·02% | 0·03% | 0·05% | No | 0·08% | 0·03% | 0·05% | 0·05% |
| Young people (<21 years) | 0·03% | Total ban | Total ban | 0·02% | 0·03% | 0·05% | No | 0·08% | 0·03% | 0·0% | 0·0% |
| Professional drivers | 0·03% | Total ban | Total ban | 0·02% | 0·03% | 0·05% | No | 0·08% | 0·03% | 0·02% | 0·05% |
| Legally binding regulations on alcohol sales | |||||||||||
| Alcohol advertising | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No |
| Product placement | No | Yes | Yes | No | No | No | Yes | No | Yes | Yes | No |
| Sponsorship | Yes | Yes | Yes | No | No | No | Yes | No | Yes | No | No |
| Sales promotion | No | Yes | Yes | No | No | No | Yes | No | Yes | No | Yes |
| Warning labels on advertisements | Yes | No | No | No | Yes | No | No | No | Yes | No | No |
| Warning labels on containers | Yes | No | No | No | Yes | Yes | No | No | Yes | No | No |
| National support and monitoring | |||||||||||
| Government support for community action | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| National monitoring systems | Yes | No | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes |
In an effort to tackle obesity and NAFLD from an early age, the Chinese Government has launched several public health campaigns, including Happy 10 Minutes, which encourages schoolchildren to have daily 10-min breaks for exercise (table 5 ). However, these strategies have paid seemingly little, if any, attention to diet. The Chinese Government's attempts to tackle obesity are being supported by several large multinational food companies, including the Coca-Cola Company, PepsiCo, and Nestlé.249 These companies fund a non-profit research organisation, the International Life Sciences Institute (ILSI), originally established in the USA in 1978 by a Coca-Cola executive. For several decades, ILSI–China has led public health initiatives emphasising the importance of exercise and physical activity—rather than nutrition—as key to solving the obesity problem. By focusing more on physical activity than on a healthy diet, attention has been diverted away from highly processed food and calorie-dense snacks and drinks. Dietary policies advocated by the WHO, such as taxing sugary drinks and restricting food advertising to children, are missing.249
Table 5.
Status of various policies and interventions to reduce NAFLD in the Asia-Pacific region
| India | Pakistan | Bangladesh | China | Japan | South Korea | Indonesia | Singapore | Taiwan | Australia | New Zealand | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| National food and nutrition policy and action plan | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Taxes on sugar-sweetened beverages | Yes | No | Yes | No | No | No | No | No | No | Yes | No |
| Food labelling for ingredients and nutritional value | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Marketing restrictions on unhealthy food | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| School-based environmental and cultural interventions supporting children to eat healthy foods | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| National guidelines on physical activity for health | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Urban planning or reengineering for active transport and walkable cities | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| School-based programmes to support physical activity | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Incentives for workplace healthy lifestyle programmes | No | No | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Mass-media campaigns to promote healthy eating and lifestyle | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Economic interventions to promote physical activity* | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Example interventions are taxes on motorised transport or subsidies on bicycles and sports equipment.
The Indian economy was the fastest-growing major economy in the world in 2016, with a growth rate of 7·1%.2 Its per-capita GNI in 2016 was $1680 ($6500 in PPP terms). The country's health-care expenditure (about 4% of GDP) compares well with other similarly placed countries. More than 70% of the population uses private health-care facilities250 that have high costs,251 often out of necessity rather than by choice.
India launched a National Viral Hepatitis Control Program in 2018,252 which aims to provide testing and treatment with antivirals to patients infected with hepatitis B and C and their sequelae of chronic liver diseases. With large-scale procurement, the current cost of a 12-week HCV treatment regimen of sofosbuvir and daclatasvir is $70 and is expected to decrease (Sarin S K, Institute of Liver and Biliary Sciences, New Delhi, India, personal communication). This is one of the most comprehensive hepatitis control programmes globally, on the basis that it incorporates the sequelae of hepatitis infection together with hepatitis infection itself, and intends to reach out to primary health centres in a phased manner. It also features surveillance for acute hepatitis, including hepatitis A and E. Some ongoing related programmes are hepatitis B immunisation for infants, safe blood transfusion, policies on injection safety, safe disposal of biomedical waste, food safety, and, most recently, treatment of hepatitis C. India does not currently have a national alcohol policy, but it has several policies and interventions aimed at reducing the harmful effects of alcohol (table 4). The Ministry of Social Justice and Empowerment also has reduction and prevention policies on alcohol and drugs. Alcohol is a subject in the State List under the Seventh Schedule of the Constitution of India, which defines the exclusive legislative powers of state governments. Therefore, the laws governing alcohol, such as the legal drinking age in India and the laws that regulate its sale and consumption, vary from state to state. In India, consumption of alcohol is prohibited in the states of Bihar Gujarat, and Nagaland, as well as the union territory of Lakshadweep. There is a partial ban on alcohol in some districts of Manipur. All other Indian states permit alcohol consumption but have various legal drinking ages. In some states, the legal drinking age can be different for different types of alcoholic beverages.
Current policies in India largely do not focus directly on overweight, obesity, and NAFLD (table 5). However, in the context of ameliorating the burden of non-communicable diseases, certain government initiatives have been undertaken. The GBD statistics253 and the projected prevalence of death and disability due to non-communicable diseases (obesity being the major risk factor) led the Indian Ministry of Health and Family Welfare to reduce the overweight diagnostic threshold for BMI to 23 kg/m2 (from 25), and the standard waist circumference indicative of abdominal obesity to 90 cm in men and 80 cm in women (internationally accepted waist circumference thresholds for abdominal obesity are 102 cm in men and 88 cm in women). These standards have been published in the ministry's Consensus Guidelines for the Prevention and Management of Obesity and Metabolic Syndrome, which were released jointly with the Diabetes Foundation of India, the All-India Institute of Medical Science, the Indian Council of Medical Research, the National Institute of Nutrition, and 20 other health organisations.254 Considering the increasing burden of non-communicable diseases and the risk factors common among the major non-communicable chronic conditions, the Government of India initiated the integrated National Programme for Prevention and Control of Diabetes, Cardiovascular Disease, and Stroke.255 The programme focuses on health promotion and prevention, strengthening infrastructure and human resources, early diagnosis and management, and integration with the primary health-care system through non-communicable-disease cells at different levels for optimal operational synergies.255 Consumption of junk food has also increased rampantly in India over the past two decades, and the industry primarily targets children. Although the Indian Government has not yet established a policy to ban junk food in schools and their close perimeters, the state governments of Delhi and Uttar Pradesh have instructed schools not to allow the sale of junk food in their canteens. In India, no specific laws or guidelines regulate the advertising or marketing of junk foods, but provisions under laws in other policy areas and some guidelines issued by the self-governing Advertising Standards Council of India could be used to regulate their advertising. The Food Safety and Standards Authority of India (FSSAI) has also produced the Guidelines–Code of Self-Regulation in Food Advertisement to control the objectivity and accuracy of food advertisements.256 However, all of these measures are recommendations rather than mandatory.257 Amendments regarding packaging and labelling of food under part VII of the Prevention of Food Adulteration Rules of 1955 mandate the disclosure of health claims alongside nutritional labeling.258 However, stricter policies are required to prevent misleading information. For example, most packaged junk food in India does not mention trans fat because that is not required by the law. In 2010, the FSSAI expert group formulated guidelines that recommend less than 10% trans fats in food products.259
Indonesia has the largest economy in southeast Asia and is one of the emerging market economies of the world, according to 2016 World Bank estimates. Its GDP per capita, however, ranks below the world average, making Indonesia a lower-middle-income country with a GNI per capita of $3440 and PPP per capita of $10 680 in 2015.260
In 2015, Indonesia spent 3·6% of its GDP on health-care, which is less than its neighbouring countries such as Singapore (5·8%), Malaysia (4·3%), and Thailand (4·2%).260 This expenditure covered 40% of the country's total health-care costs, whereas the remaining 60% were covered by private firms or out-of-pocket expenses, but by 2020 it is expected that public and private expenditure will contribute equally.244
A serious effort to address hepatitis infection began in 1991 with a WHO-sponsored neonatal hepatitis B vaccination project in Lombok. In 1992, the Indonesian Red Cross started programmes for safe blood. These efforts—and more recent active harm reduction measures from 2010—were considered to support the decreasing incidence of HBV and HCV.261 In 1997, hepatitis B immunisation for infants was launched as a national programme and upscaled in 1999 by the introduction of birth-dose vaccination.262 A Hepatitis Control Program within the Ministry of Health was launched in 2012.263 The Indonesian Government issued a decree on the National Control of Viral Hepatitis in 2015, supported by a national budget,263 followed by a decree in 2017 for the Triple Elimination of Mother-to-Child Transmission of HIV, Syphilis, and Hepatitis B by integrating HIV, syphilis, and hepatitis B antenatal screening, prevention, and treatment interventions into Mother-and-Child Health Care services.264 A government assistance programme began in 2017 that provides free testing and direct-acting antiviral drugs for 6000 patients with chronic hepatitis C infection who cannot afford diagnosis and treatment.36 Meanwhile, efforts are made to include these drugs in the Essential Medical List to be used through the public health-care insurance system. Sofosbuvir, simeprevir, daclastavir, and one fixed-combination (elbasvir–grazoprevir) drug are the currently registered direct-acting antivirals in Indonesia.
Currently, there are no alcohol bans being enforced in Indonesia, with the exception of Aceh province (Sumatra; table 4). In 2015, the Government began to restrict the availability of alcohol by banning sales from mini-marts and groceries.
In a bid to prevent the prevalence of overweight and obesity, the Health Ministry has set the improvement of public health and nutrition as a top priority in the National Long-Term Development Plan (table 5).265 In November, 2016, the Indonesian Government launched a programme to improve public health called Healthy Living Community Movement (GERMAS).266 One of the key elements included in the programme was the Isi Piringku (My Plate) campaign,267 which describes the proportion of carbohydrates, protein, vegetables, and fruit each meal should contain. The scheme aims to drive change using a cost-effective model targeting individuals and the community by harnessing their motivations (eg, improved appearance, social acceptance, overall wellbeing) to improve health. School settings are recognised as an ideal and crucial starting point, to help children to acquire basic knowledge in the areas of nutrition and health, which would persist through adulthood, and to actively improve their diets through the provision of fruits and vegetables in their school meals.
According to the World Bank's income classification, Pakistan is a lower-middle-income country, with GNI per capita of $5560 in PPP terms in 2016. Pakistan is developing and is one of the 11 countries identified as having high potential of becoming one of the world's largest economies in the 21st century.268
The current policies and national action plan that track liver diseases, such as food, nutrition, alcohol, and HBV policies, have largely not been acted on or adequately popularised. These policies need to be updated with result-oriented strategies that aim to improve accountability and effectiveness by clearly defining expected outcomes, facilitating monitoring and evaluation, and reflecting improvements resulting from performance assessment processes. For example, in 1997, Pakistan introduced a National Health Policy targeting non-communicable diseases, and in 2003, it introduced an integrated national plan for action on four major non-communicable diseases and their risk factors, injuries, and mental health. Both the Policy and plan could not be implemented properly because of a change in government.269
In Pakistan, vaccination against HBV was incorporated into WHO's Expanded Programme on Immunisation in 2002, providing the first vaccine dose at the age of 6 weeks; however, coverage for all three doses has reached 75% according to WHO-UNICEF estimates in 2018.270 National guidelines on treatment and surveillance, provision of screening kits, injection safety equipment, training for preventive measures, and campaigns to increase mass awareness and financial support for treatment have also been developed.271
The National Programme for Hepatitis Prevention and Control was launched in 2005, after which provincial implementation units were also set up.272 The Programme focused on screening and treatment for HCV infection and did not establish laboratory-based viral hepatitis surveillance. At the time, hepatitis surveillance in Pakistan was syndromic, not providing laboratory confirmation of infection or information on the type of virus, and not collecting information on risk factors. In 2009, to monitor the effectiveness of the Programme's activities and guide the implementation of evidence-based preventative interventions, the Pakistan Field Epidemiology and Laboratory Training Programme (under the akistani Centres for Disease Control and Prevention and the Ministry of Health) launched a hepatitis sentinel-site surveillance system (appendix p 3). The sites were located in five public tertiary care hospitals in four provincial headquarters (Lahore, Peshawar, Karachi, and Quetta) and in Islamabad. To engage Sindh province to implement strategies, the United States Agency for International Development further supported the Pakistani Centres for Disease Control and Prevention toward expansion of the surveillance sites.273, 274 A National Hepatitis Strategic Framework for viral hepatitis (2017–21)274, 275 has been launched to eliminate viral hepatitis C by 2030, reduce hepatitis B and C by 10% reduction by 2021, and reduce new cases of hepatitis B, C, and D by 30% by 2021. So far, the measures implemented by the Government of Pakistan include HBV vaccination for children and adults and providing antiviral therapy for patients with HBV and HCV through various programmes and public awareness campaigns. The national essential medicines list, subsidised by the government, includes antiviral therapy for HBV (interferon alpha, pegylated interferon, entecavir, tenofovir, and lamuvidine) and HCV (interferon alpha, pegylated interferon, ribavirin, sofosbuvir, daclatasvir, and velpatsavir).
After its independence in 1947, Pakistani law was fairly liberal regarding alcohol (table 4). Major cities had a culture of drinking, and alcohol was readily available until the mid-1970s when the Government introduced prohibition. As a result of the prohibition, the consumption of alcohol in the country has been very low, but mostly unrecorded.
Many nutritional programmes (eg, School Health Programme, Micronutrient Initiative, National Programme for Family Planning and Primary Health Care, and Tawana Pakistan Project) have been initiated by governmental and nongovernmental organisations (table 5).276 Some of these programmes focus on raising awareness in the general public, and others focus on directly supplying food or fortified nutrition to communities. A national action plan for prevention and control of non-communicable diseases and health promotion277 has been devised but has not been implemented. The Ministry of Planning and Development and Reform, in collaboration with the UN Food and Agriculture Organization, launched the Pakistan dietary guidelines for better nutrition in December, 2018.278
Bangladesh is a lower-middle-income economy which grew by 7·1% in 2016–17.2 The per-capita GNI in 2016 was $1330 ($3790 in PPP terms). According to the latest Bangladesh national health accounts, the country spends $2·3 billion on health or $16·20 per person per year, of which 64% comes through out-of-pocket payments.279 Health insurance initiatives cover a very small proportion of the total population.
Hepatitis B vaccination was introduced in Bangladesh in phases during 2003–05 under the Expanded Program on Immunization280 and since 2007, more than 95% of infants younger than 1 year have been vaccinated against HBV.281 The coverage in 2016 was reported to be as high as 97% by WHO and UNICEF. HBV prevalence appears to have declined in Bangladesh, from 5·5% in 2008 and from 6·4% in 1997 to 0·7% in 2010.58, 59
Local generics are available for tenofovir, entecavir, adefovir, lamivudine, and pegylated interferon at reduced costs. However, eliminating HBV remains a challenge because of factors such as an increase in HBeAg-negative infections, lack of adequate numbers of hepatologists, insufficient availability of laboratory facilities for viral load estimation, social taboos, lack of public awareness about hepatitis B and its preventability, and misconceptions about the mode of transmission and consequences of HBV infection. Regarding HCV, local generic direct-acting antiviral drugs such as sofosbuvir, ledipasvir, daclatasvir, and velpatasvir are available at low cost, offering HCV treatment of good quality. However, the challenges in the management of transmission resemble those for HBV.
Harm reduction interventions, particularly a needle syringe programme for people who inject drugs, have been implemented in Bangladesh since 1998. Opioid substitution therapy commenced in 2010 but only covers 2·9% of the total estimated people who inject drugs in the country.63
The Government is allocating funds and staff for the national Nohep programme for viral hepatitis. This strategy for elimination of HBV, HCV, and HEV has been drafted and is now in the final stage of approval. Advocacy programmes on viral hepatitis and validated training modules for training health-care personnel have been developed. More than 3000 physicians serving the Health Cadre of the Bangladesh Civil Service have already received training about hepatitis and its management strategies.
The status of various policies and interventions to reduce the harmful use of alcohol in Bangladesh is shown in table 4. In 1990, the Ministry of Home Affairs in Bangladesh published the Narcotic Control Act,282 which outlines national policies on alcohol tax rates, selling and serving of alcohol, alcohol advertisements, legal blood alcohol concentration when driving, and alcohol licensures. Although the Act restricts alcohol use, enforcement of its policies is minimal, so alcohol is still widely used in Bangladesh. Non-Muslim residents and foreign visitors are not affected by such restrictions, as long as they consume alcohol in private.
The Bangladesh National Plan for Action on Nutrition was started in 1997,283 with a focus on targeting undernutrition (table 5). Dietary guidelines for Bangladesh were introduced in 2013 that describe population goals for intake of various nutrients, including saturated fats, trans fats, and sugars, which represent the average nutrient intake needed to maintain a healthy population. Bangladesh also endorsed a second National Plan of Action for Nutrition for 2016–25 in March, 2017.284 Its goal is to improve the nutritional status of all citizens and reduce all forms of malnutrition, with a focus on children, adolescent girls, and pregnant and lactating women. The only strategies that discuss overnutrition in depth as a development challenge are the National Urban Health Strategy 2011285 and the Strategic Plan for Surveillance and Prevention of Non-Communicable Diseases in Bangladesh 2011–15.286 The Health, Nutrition, and Population Sector Program,287 which began in 2011, also recognises overnutrition and obesity as development challenges. The programme is particularly focused at early intervention to address obesity and its risk factors, but trains front-line fieldworkers on prevention of all risk factors related to non-communicable diseases.288
According to the World Bank's income classification, Japan is a high-income country with GNI per capita of $43 630 in PPP terms in 2016. Japan's health-care system is largely successful because of its wide availability, effectiveness, and efficiency.289 The Japanese population has the longest life expectancy of all members of the Organisation for Economic Co-operation and Development (OECD),290 and its health-care expenditure as a share of GDP is lower than most of the developed OECD countries. In 2013, health expenditure in Japan was 10·3% of GDP, compared with an OECD average of 8·9%.291 Health insurance is mandatory in principle, but there is no penalty for the 10% of individuals who evade the compulsory insurance premium contribution, making it optional in practice.292 Health insurance can be either national or provided by the employer. In 1958, a new citizens' health insurance law formally committed Japan to universal health coverage by making enrolment in governmental insurance systems mandatory for people not covered by employee-based plans, and by 1961 all municipalities had established insurance programmes with near-complete coverage.52
The Japanese Government has been providing free hepatitis testing since 2002 for all citizens aged 40–70 years as part of routine health examinations. In 2007, patient management was strengthened by the establishment of a community hepatitis care network that links primary care physicians with specialised regional centres to co-manage patients with liver disease. Treatment for hepatitis was expensive, so the Government introduced a subsidy programme in 2008 to reduce the burden of out-of-pocket expenses.293 The cost of subsidies is borne by the national and local governments. People living with hepatitis currently pay ¥10 000–20 000 (approximately $100–200) per month on the basis of their income to cover the cost of drugs, medical appointments, and laboratory tests.
In 1985, Japan implemented public programmes for mandatory HBsAg tests for pregnant women to prevent mother-to-child HBV transmission. Infants who were born to HBsAg-positive mothers began receiving HBV vaccination plus IgG therapy in 1986. Further, the Japanese Red Cross implemented nucleic acid screening programmes for HBV and HCV in 1999. These national efforts markedly reduced the prevalence of childhood HBV infections. Nevertheless, about 200 new, primarily adult infections of acute HBV are reported annually.48 The distribution of HBV genotypes also appears to have changed on the basis of an observed increase of chronic infections but without obvious household transmission, which makes controlling infection challenging.294 The Japanese Ministry of Health, Labour and Welfare implemented routine immunisation of children for HBV in 2016 to prevent horizontal HBV transmission and to eradicate infection incidence, in line with WHO's target of eliminating the public health threat of viral hepatitis by 2030.294
Because of the universal health insurance system and the subsidy programme, the economic barrier to HCV eradication is very low in Japan, with all patients with HCV having access to direct-acting antiviral drugs (sofosbufir, sofosbufir–ledipasvir, ombitasvir, paritaprevir–ritonavir, daclatasvir, elbasvir–grazoprevir, and sofosbufir–velpatasvir). In a 5-year retrospective cohort study between 2008 and 2013 that estimated HCV in blood donors from their medical records, the incidence of HCV infection was 0·40 per 100 000 person-years (95% CI 0·27–0·57) on the basis of viral RNA seroconversion.295 Incidence was as low as that reported between 1994 and 2004 (1·9 per 100 000 person-years, 95% CI 1·1–3·0).296 Additionally, the incidence of HCV infection is very low, and HCV is nearly eradicated. As discussed, deaths due to hepatocellular carcinoma plateaued in 2002–04 and have declined since. Access to medical examinations is easy, so patients with high risk of hepatocellular carcinoma can be regularly monitored and many cases are treatable because they are detected at an early stage. The production and off-premise sale of all alcoholic beverages based on the Liquor Tax Law requires a Government licence (table 4). This licensing system has been strictly imposed over time and almost no home-brewed alcohol has been available on the market for the past 30 years. However, there is virtually no restriction on off-premise sales in Japan and there are no restrictions on the advertising alcoholic beverages.
Encouraging weight loss is a central aim of Healthy Japan 21, a series of 10-year public-health goals devised at the start of the millennium (table 5).297 This reduction of overweight is to be achieved through public education campaigns on healthy eating and increased physical activity.298 Japan's school lunches programme has helped to slow the rise of child obesity in Japan. Lunches tend to be planned by a nutritionist, include locally grown and fresh ingredients, and tend to be dominated by rice, vegetables, soups, and fish. Childhood obesity has increased in Japan since the 1970s, but that increase has happened more slowly than in other economically developed countries. The Government has established healthy waistline thresholds for adults aged 40–74 years with the metabo law, which came into effect in 2008, and these are measured at annual checkups.298 The threshold for men is 33·5 inches or less and women, it is 35·4 inches. People who exceed those norms are required to attend counselling and support sessions. Companies are required to measure the waistlines of at least 80% of their employees along with their families, and of retired employees. Furthermore, at the time of introduction, companies were required to help 10% of those who were above the thresholds to lose weight by 2012, and 25% by 2015. Companies and local governments that failed to meet specific targets were liable for financial penalties, potentially as high as $19 million.298 The targets have not been updated, but companies are now required to increase their contributions to their welfare fund by 10% if they do not perform well. Men and women who exceed the waistline measurement threshold during their annual medical examinations are enrolled in diet programmes, fitness classes, or are asked to see a doctor. The long-term effectiveness of this controversial stringent approach are yet to be clarified.299
South Korea is a high-income country with nominal GNI per capita of $28 380 and annual GDP growth of 3·1%.2 By contrast with most OECD countries, health spending in South Korea has been growing continuously since the 1970s at a rate above the OECD average. Total health expenditure as a proportion of GDP was 7·1% in 2014.300 Although the public sector is the main source of health funding in nearly all OECD countries, the private sector has a much more important role in South Korea and only 56% of health spending was funded by public sources in 2013, well below the average of 73% in OECD countries.300 Out-of-pocket spending is also an important component of overall health expenditure in South Korea. At 37% of health spending, its share is almost twice the overall OECD average (19·5%).300
South Korea achieved universal health coverage in 1989. The national health insurance covers about 97% of the population, and the remaining 3% are covered by the Medical Aid Program, a tax-funded programme for health-care access of citizens with low incomes. By contrast with public health financing, health-care delivery relies heavily on the private sector, although some public health facilities provide medical services at the central, regional, and municipal levels. As of 2012, almost all clinics and about 94% of hospitals were privately owned.301
For hepatitis B in South Korea, the use of oral antiviral drugs is done according to the reimbursement guidelines of the national health insurance programme. Pegylated interferon can also be used. For HCV, the use of pegylated interferon and ribavirin has been covered by the national health insurance programme. Coverage is not complete for direct-acting antiviral drugs but is improving and the following drugs have been approved by the South Korean Ministry of Food and Drug Safety for the treatment of HCV: sofosbuvir–ledipasvir, sofosbuvir, daclatasvir, asunaprevir, ombitasvir/paritaprevir/ritonavir plus dasabuvir, elbasvir–grazoprevir, and glecaprevir–pibrentasvir.
South Korea has implemented a minimum age for purchasing alcohol, but other legally binding policies (eg, regulating promotion of the sales of alcoholic beverages or sale restriction in petrol stations and to intoxicated individuals) do not exist (table 4).
South Korean ministries, especially the Ministry of Health and Welfare and the Ministry of Education, have introduced many interventions to improve diets and increase physical activity (table 5). For example, the Ministry of Health and Welfare provides budget support to local governments' obesity programmes, develops educational materials and publicises them, and provides vouchers for management services of physical activity and diets for obese children. The National School Lunch Act, introduced in 1981, has provisions on school dietitians, nutritional requirements, and dietary consultation. In July, 2018, the South Korean Government set a goal to keep the population's obesity prevalence lower than 35% by implementing measures on nutrition, exercise, obesity treatment, and improved awareness. Surgical procedures to treat obesity are covered by public health insurance. Starting in 2020, medical consultations and dietary training will also be eligible for partial coverage under the national insurance plan. Additionally, the Government will finance outdoor activities for students so that children will have access to activities outside their school gyms such as swimming, skating, bowling, climbing, and baseball. The Government plans to create a monitoring system for television programmes and advertisements that promote overeating; however, because of widespread critique, these plans have not yet been implemented.302
The economy of Australia is a large mixed-market economy, with a GDP of $1·43 trillion as of 2017. In 2018, Australia became the country with the largest median wealth per adult.303 According to the World Bank's income classification, it is classified as a high-income country, with GNI per capita of $45 210 in PPP terms in 2016.
Health care in Australia is delivered as a mixed system via universal health care (public), which predominates, and private providers (insurance), who make a small contribution. Australia's universal health care is primarily funded by Medicare, a financing system that covers most costs of health services, including those in public hospitals. Medicare is funded partly by a 2% Medicare income levy (with exceptions for people with low incomes), with any shortfall being met by the Government from its general revenue.304 The proportion of Australia's health expenditure of GDP (9·5%) for 2011–12 was slightly above average compared with other OECD countries.305
In Australia, a universal hepatitis B vaccination programme for all infants was introduced in 2000.306 It was preceded by various programmes implemented in the late 1980s that targeted individuals at increased risk of HBV infection. Catch-up vaccination programmes against hepatitis B for adolescents have been implemented at different times, settings, and jurisdictions since 1997.71 However, health inequity between Indigenous and non-Indigenous Australians regarding HBV infection is still substantial. Vaccination coverage of Indigenous Australian adults needs to be increased through a state-funded vaccination catch-up programme. In 2017, an estimated 149 746 people living with chronic hepatitis B in Australia had been diagnosed, representing 68% of the total estimated population living with chronic hepatitis B and a modest increase from the 63% estimate in 2011.307 The first National Hepatitis B Strategy 2010–13308 sought to reduce disease transmission and the morbidity and mortality associated with hepatitis B. Furthermore, the introduction of highly effective HBV antiviral therapy in Australia with entecavir in 2005 and tenofovir in 2007 was accompanied by considerable increases in treatment uptake. During 2017, 19 358 people were administered drugs for hepatitis B, representing 8·7% of those estimated to be living with chronic hepatitis B. Modeled trends between 2011 and 2017 show an ongoing modest increase (average 0·93% per year) in this proportion.307 At the population-level, only a few people with chronic HBV infections (possibly 10–15%) would be recommended for treatment on the basis of national and international consensus guidelines.309, 310 These vaccination efforts are collectively reflected in the fact that Australia was recognised by WHO as meeting the regional control target of hepatitis B, which is a prevalence of less than 1% in children younger than 5 years.311 Australia implemented its Third National Hepatitis B Strategy for 2018–22 to achieve and maintain 95% vaccination coverage against hepatitis B in infants, increase the proportion of diagnosed people with chronic hepatitis B infection to 80%, increase the proportion of those receiving care to 50% and those receiving antiviral treatment to 20%, and reduce mortality related to chronic hepatitis B by 30%.312
Estimates from modelling studies indicate that 75–85% of Australians with HCV are diagnosed, one of the highest proportions of diagnosed individuals globally.313 Despite this estimate, treatment uptake was low (2000–4000 people per year, or 1–2% of the infected population) in the era of interferon-based regimens.313 However, uptake has substantially increased following the Pharmaceutical Benefits Scheme, which, since March 1, 2016, has listed interferon-free, all-oral regimens of direct-acting antiviral drugs with no restrictions on the basis of the stage of liver disease or drug and alcohol intake.314 4400 incident patients were treated per month during the first four months of listing.315 By December, 2017, the number of patients starting therapy with direct-acting antiviral drugs had stabilised to about 1280 patients per month.315 Over the first 2 years of listing, 2016–18, 56 356 patients had been supplied with medication, and as of April 30, 2018, this number of patients was 58 941.315 The Australian Government has allocated $0·6 billion to fund this scheme over the subsequent 5 years. This treatment increase suggests that Australia could eliminate hepatitis C within the next 10–15 years if the current trend continues.316
The 2009 Australian Guidelines to Reduce Health Risks from Drinking Alcohol have led to some recommendations on reducing alcohol-related liver harms and on broader health aspects (table 4).317 Subsequent estimates suggest that Australians were drinking less alcohol in 2013–14 than in 1960, 50 years earlier.318 In 2014–15, 65·3% of Australians aged at least 15 years had sedentary lives or exercised rarely. This proportion comprises 33·8% sedentary people and 31·5% people with low levels of exercise below the “sufficiently active” threshold, defined as at least 30 min of moderate-intensity physical activity on most, preferably all, days.319 During the past two decades, frequent campaigns run by Federal and State agencies in Australia to promote healthy food intake and physical activity have been successful on the basis of improved general awareness about obesity, increased physical activity, and modification of dietary patterns (table 5).320, 321
New Zealand's Government is applying a nationwide wellbeing approach to policy and budget decision making. General wellbeing in the country is high, as reflected by OECD's economic health survey.322 According to the World Bank's income classification, New Zealand is a high-income country with GNI per capita of $37 190 in PPP terms in 2016.
New Zealand's health system is predominantly tax-funded and provides universal coverage. Health expenditure as a proportion of GDP increased from 6·8% in 1990 to 10·1% in 2010 (slightly above the OECD average of 9·5%). The population has a high health status overall but health inequalities are substantial in Pacific peoples and Māori.
In New Zealand, a hepatitis B vaccination programme started in 1985 and was first intended for infected expecting and lactating mothers. Universal vaccination of infants against hepatitis B was introduced in 1988. Lamivudine treatment was approved and funded for the management of patients with chronic hepatitis B in 2000 and, until 2015, almost 2500 patients had been treated. Adefovir was introduced in early 2003 and, subsequently, entecavir and tenofovir were also introduced.85 New Zealand has also implemented screening programmes for blood products and needle exchange programmes for intravenous drug users. The Pharmaceutical Management Agency (known as Pharmac) announced funding for direct-acting antiviral drug therapies for patients with HCV on June 9, 2016. From Oct 1, 2016, all prescribers including general practitioners were able to prescribe these drugs.316 Until February, 2019, an estimated 3000 patients with HCV have been treated with direct-acting antiviral drugs funded by Pharmac and another 2000 have been treated with such drugs provided through clinical trials.323
General practitioners in New Zealand are the primary health-care professionals responsible for monitoring patients for liver cancer, typically with a liver ultrasound. If cancer is suspected, a patient is referred for specialist care and further management. However, there are no data to indicate the quality of surveillance practices, even in specialist settings. Although a national registry would deal with this issue and improve surveillance, currently there is no political will to implement such a policy.
Several approaches are being taken to prevent and reduce hazardous drinking in New Zealand, including strengthening regulation through the Sale and Supply of Alcohol Act 2012 (table 4). This Act introduced a limit on alcohol vending hours, strengthened restrictions around irresponsible promotion of alcohol, and stricter laws on the supply of alcohol. It also increased the ability of communities to control alcohol licensing in their local area, run national social marketing campaigns to raise awareness about alcohol harms, expand school-based health services to improve early identification and treatment referrals for young people with an alcohol problem, provide self-help tools such as the Alcohol Drug Helpline, and support people to address their alcohol issues through primary care and specialist services.325
A Childhood Obesity Plan was launched in New Zealand in October, 2015, with three focus areas comprising 22 initiatives (table 5).326 These initiatives either expanded on already existing recommendations or were new, such as targeted interventions for obese individuals, increased support for people at risk of becoming obese, and broad approaches to make healthier choices easier for all New Zealanders. The focus of the plan is on food, the environment, and physical activity at each life stage, starting from pregnancy. The plan brings together initiatives across government agencies, the private sector, communities, schools, families, and whānau (Māori for extended family or community co-inhabiting an area as an economic unit). There have been many initiatives that encourage healthy eating, physical activity, and adequate sleep, such as Eating and Activity Guidelines for New Zealand Adults,327 Physical Activity guidelines,328 Clinical Guidelines for Weight Management for Adults,329 Clinical Guidelines for Weight Management for Children and Young People,330 Fruit in Schools,331 Green Prescriptions,332 and Active Families.333 The Fruit in Schools programme provides a piece of fruit each day to children from communities with low socioeconomic status. The Green Prescriptions initiative provides individual support for increased physical activity after a referral from a general practitioner or a practice. The Active Families initiative comprises community-based health initiatives designed to increase physical activity and improve nutrition in children and young people aged 5–18 years and in their whānau.325
The World Bank classifies Singapore as a high-income country, with GNI per capita of $85 050 in PPP terms in 2016. Singapore was ranked as the world's most competitive economy, according to the International Institute for Management Development's World Competitiveness Rankings for 2019.
Although Government health-care spending as a proportion of GDP is relatively low, Singapore is among the 25 countries with the highest per-capita health-care spending. In 2015, Singapore's Government spent 2·1% of GDP or $6·3 billion on health. Health-care financing is based on Singapore's 3M framework: MediSave (a compulsory national health savings account), MediShield Life (a government-funded universal health insurance plan), and MediFund (an endowment fund set up by the government to help Singaporeans who are unable to pay for their medical expenses).334 Under MediShield Life, even people with pre-existing conditions will be covered. The national health-care plan covers the entire population and ensures that all Singaporeans have access to medical care. Although public hospitals provide 80% of expensive tertiary care services, private sector practitioners account for 80% of primary health care, with government polyclinics that operate under the Ministry of Health accounting for the other 20%.334
Currently there is no national action plan for liver diseases in Singapore. Chronic hepatitis B is the most common cause of liver diseases and is primarily addressed the National Childhood Immunisation Programme implemented in 1987. Infant vaccination is given at birth followed by the second dose at 1 month of age and the third dose 6 months later. Hepatitis B serology is routinely tested as part of antenatal assessments. For surveillance, only acute hepatitis B and C are notifiable diseases to the Ministry of Health. Singapore's hepatitis B guidelines, which include chronic hepatitis B management, were introduced by the Ministry of Health in 2011.93 The Government also setup a Medication Assistance Fund to help eligible patients to pay for expensive drugs that are not in Singapore's standard drug list but have been assessed to be clinically cost-effective. Patients receive drug subsidies and assistance on the basis of their subsidy and means-test status and the scheme under which the drug is covered (ie, standard drug list vs Medication Assistance Fund). For patients with chronic hepatitis B, adefovir and lamivudine are the only drugs listed under the standard drug list. Entecavir and tenofovir are listed under the Medication Assistance Fund. Drug subsidies are provided for patients with HCV, including for pegylated interferon, ribavirin, and sofosbufir–velpatasvir.335 MediSave's list of chronic diseases for which patients can make claims does not include liver diseases. For MediShield Life, claims cover mainly expensive hospital procedures and inpatient treatment for liver disease. Outpatient claims for immunosuppression therapy for organ transplants is also covered.
Singapore's Liquor Control (Supply and Consumption) Act 2015 came into force on April 1, 2015 (table 4).336 The Act regulates the supply and consumption of alcoholic beverages in public places to minimise public disorder and disamenities arising from drinking in public, and prohibits the consumption of alcohol in public spaces from 2230 h to 0700 h every day. There are also restrictions on the sale, supply, and delivery of liquor.
Policies and programmes on obesity and NAFLD have been customised for different parts of the population and implemented in various settings in Singapore (ie, schools, workplaces, health-care institutions, and communities; table 5). There have been many initiatives to raise awareness through health education and communication including official dietary337 and physical activity338 guidelines by the Health Promotion Board; the Championing Efforts Resulting in Improved School Health (CHERISH) award for primary and secondary schools, junior colleges, and centralised academic institutions;339 workplace health promotion programmes (Healthier Canteen Certification Programme);340 the Singapore Helping Employees Achieve Lifetime Health (HEALTH) award for companies;341 various programmes in schools (model school tuck shop programme,342 Trim and Fit programme);343 and various community-wide programmes that promote healthy eating and physical activity (Healthier Hawker Program, Healthier Dining Programme, Lose to Win Programme).344, 345
Taiwan is included in the group of advanced economies by the International Monetary Fund. It is a high-income economy according to the World Bank, with GNI per capita of $45 582 in PPP terms in 2015. It is ranked 15th in the world by the Global Competitiveness Report of the World Economic Forum, is 22nd largest in the world in terms of PPP, and ranks as 18th by GDP at PPP per capita. Taiwan's national health expenditure accounted for 6·1% of GDP in 2015. The national health insurance system in Taiwan was launched in 1995 and currently provides coverage of about 99·7% of the population. As of June, 2016, 20 759 hospitals and health-care providers, or 93·0% of all health-care facilities in the country, were contracted by the national health insurance system. Taiwan's National Health Insurance Administration first started to reimburse treatment for chronic hepatitis B and C in 2003. Coverage of oral drug treatments for patients with hepatitis C has been approved since January, 2017.346
The Alternative Therapies programme for drug addiction, subsidised by Taiwan's Ministry of Health and Welfare, was introduced in 2006, and the Ministry's needle exchange programme was implemented in 2005.347 At the end of 2016, 179 institutions throughout Taiwan were providing alternative therapy for drug use. The Ministry of Health and Welfare also subsidised health institutions to provide treatment for drug and alcohol addiction in correctional facilities. In 2016, four health institutions offered services at five correctional facilities.
In 1984, the Taiwanese Government introduced the first control programme for viral hepatitis in infants globally.102 Initially, the programme focused on prevention of hepatitis B through immunisation, public education to avoid transmission, encouraging the use of disposable syringes, and blood safety. Only babies born to HBsAg-positive mothers were vaccinated because of high costs but, as of 1986, all infants weighing 2500 g or more were eligible. In the late 1980s, the programme was extended to preschool children, medical personnel, and elementary-school children, and from 1992 onward, unvaccinated teenagers and adults have been encouraged to be vaccinated on a fee-for-service basis. Around 2000, because of the availability of effective treatments for hepatitis B and C, treatment of chronic viral hepatitis was added to the programme. In 2003, treatment for chronic hepatitis B and C was reimbursed by the national health insurance, which has had a tremendous impact on the outcomes of patients with chronic hepatitis. A 2010 analysis showed a steady and substantial decrease of the mortality of patients with end-stage liver disease and hepatocellular carcinoma in Taiwan.348 In 2017, some of the direct-acting antivirals against HCV infection were covered by the national health insurance for the treatment of patients with chronic hepatitis C.
Although health insurance has been introduced in most countries of Asia-Pacific, overall coverage remains low in countries like India, Pakistan, and Bangladesh, with consequent high out-of-pocket expenditure. HBV vaccination programmes for infants have been implemented by all countries. The administration of a birth dose of HBV vaccine is still inadequate in many countries, especially in low-income and rural settings. Policies regarding mandatory screening of blood and blood products for HBV and HCV and safe injection practices are available in all countries (although nucleic-acid amplification testing is not mandatory in a few countries). Most countries have put HBV and HCV drugs on essential medicines lists. The costs of antiviral drugs have been brought down considerably by the availability of generic versions.
Except in Muslim-majority countries, alcoholic liver disease is a major public health issue, especially in China and India. Although many countries have policies on alcohol, major sociocultural and behavioural changes will be needed at the societal level to reduce overall consumption of alcohol.
Changes in patterns of obesity, physical inactivity, and diets is driving an increase in NAFLD across countries, irrespective of their income status. National food and nutrition policies in lower-middle-income countries has historically focused on combating undernutrition. Anti-obesity policies have been developed and implemented by some countries such as China, South Korea, Japan, Singapore, Australia, and New Zealand. Chinese anti-obesity policies, under the influence of large multinational food companies, have focused mainly on promoting physical activity, and less on nutritional measures.
Workforce and infrastructure
The number of professional health workers in mainland China increased from 3·63 per 1000 people in 2000 to 46·12 per 1000 people in 2016.242 In 2016, 32·2% of medical workers have an undergraduate or a higher degree.180 Health workers are unevenly distributed between urban and rural areas; highly qualified health workers concentrate in eastern China, which is more economically developed than other areas, and in tertiary hospitals, whereas there are inusfficient numbers of staff working on disease prevention and control or primary health facilities and in poorer provinces.349 Training programmes on liver diseases, as well as teleconsultation between primary care physicians and specialists, might improve the management of liver diseases. Most tertiary and some secondary hospitals are well equipped with materials and infrastructure needed to diagnose and treat liver diseases, such as biochemical, immunological, and nucleic acid assays; ultrasonography; CT and MRI scanning; and diagnostic and therapeutic endoscopy. However, these facilities and expertise might still be far from sufficient in western China.
Patients with infectious and non-infectious liver diseases are cared for by physicians specialising in infectious diseases, hepatology, or integrated traditional Chinese medicine. Resident training programmes for internal medicine have been well established in most parts of mainland China but fellowship programmes for specialists in hepatology are still to be established.
Over the past decade, enormous efforts have been made to address the legal and ethical issues in organ transplantation. Now, voluntary donation after cardiac death or living organ donation are the only means of organ transplantation in mainland China.350 Since 2011, the China Organ Transplant Response System has begun to allocate donor livers, which is based only on urgency and compatibility. Until December, 2011, 20 877 liver transplantations done between 1980 and 2011 in 81 certified transplantation centres had been reported to China's Liver Transplant Registry. Of the donated livers, 19 338 (92·6%) were procured from deceased donors, and 1539 (7·4%) were procured from voluntary living donors.351 In March, 2010, a new pilot project of organ donation from deceased donors was launched with the aim of reducing China's dependence on transplants from prisoners sentenced to death and expanding the pool of eligible donors into the general population.351 This pilot project made into a nationwide programme in 2013, and, as of Jan 1, 2015, all hospitals in China stopeed using organs from prisoners and currently exclusively rely on donations from the general public. Post-transplantation survival of recipients has improved substantially.351 Median post-transplantation follow-up was 14·7 months and the longest follow-up time was 192·5 months.351
India has 938 000 (one in 1320 people) doctors trained in modern medicine and 736 000 doctors (one in 1682 people) trained in traditional medicine, with an overall distribution of one doctor per 736 people and one nurse per 482 people.352 However, the number of health-care personnel (ie, doctors, nurses, technicians) trained to manage liver diseases is grossly insufficient. Several institutions in the country run 3-year training programmes in gastroenterology and hepatology (for internists or paediatricians), with a combined intake of around 200 students per year. Several academic centres in the country are also engaged in clinical and laboratory research in areas related to liver disease, and the country has a dedicated Institute of Liver and Biliary Sciences (New Delhi).
Provision of liver care services would require training of health-care personnel at various levels in the detection and initial management of liver diseases, and triage and referral of those at risk of progressive disease to specialised centres. Facilities for management of paediatric liver diseases are available in only a few centres. Online e-learning resources and telemedicine can facilitate such training, and also consultation between primary physicians and specialists, and should be encouraged.
Facilities for liver transplantation are available in major cities in India, with approximately 2500 transplants per year, mostly from living donors. To meet the need for liver transplant services, liver transplantation from deceased donors needs to be encouraged over living transplantation. The organ donation rate will need to increase from the current 0·5 per million people per year to 5–10 per million per year, and organ-sharing policies need to move from current ones that are based on waiting time or institutional rotation to a severity-based system. The Indian National Organ & Tissue Transplant Organisation is engaged in these activities.
In December, 2015, Indonesia had 9767 heath centres to deliver primary health care and 2488 hospitals (1593 public and 895 private hospitals). Specialised gastroenterology and hepatology services are available in tertiary care hospitals.32 In 2015, there were 876 984 health professionals in Indonesia, comprising 647 170 doctors and nurses (73·8%) and 229 814 (26·2%) health support workers. The few liver specialists (approximately 165) available to care for the more than 20 million patients with HBV or HCV represent a serious problem. Infrastructure capacity building, mentoring of health professionals, and technical training assistance to accelerate the decentralisation of service delivery from specialised medical centres to local hospitals and laboratories at or near the point of care has been proposed.32 In parallel, over 500 units of rapid molecular diagnostics with a point-of-care platform have been distributed to district laboratories to facilitate low-cost HCV detection and quantification and to scale up and converge testing in multiplex platforms with other diseases (eg, tuberculosis and HIV).
Pakistan is one of 57 countries with a serious deficiency in the health workforce.353 Pakistan has a doctor-to-patient ratio of 1:1300, doctor-to-nurse ratio of 1:2·7, and nurse-to-patient ratio of 1:20.354 There are many informal health-care providers in Pakistan, comprised of unqualified allopathic providers (eg, rural doctors or drug shop retailers), traditional healers, faith healers, Unani healers, and semi-qualified allopathic providers (eg, medical assistants, technicians, and community health workers). Although they are not a part of the mainstream health system, they are major health-care providers to poor rural populations, especially in remote and inaccessible areas. There are few medical professionals trained in managing liver diseases.
Pakistan's health-care facilities, such as basic health units (ie, facilities that cover 10 000 individuals) and rural health centres (ie, covering 30 000–45 000 individuals), are poorly maintained, equipped, and staffed, especially in rural areas. The health-care delivery system, therefore, relies hugely on private organisations that have advanced facilities but are unaffordable to most people. Public health-care institutions that provide advanced care are often only located in major towns and cities and private tertiary care hospitals are extremely expensive. Poor people in rural areas tend to consult local private doctors, with 70% of the population served by the private sector.355 The private sector operates through a fee-for-service system of hospitals, general practitioners, and homeopathic and traditional healers. Very few mechanisms exist to regulate the quality, standards, protocols, ethics, or prices in the private health sector. Additionally, opportunities for health-related research are few, and not many advanced technologies, such as molecular diagnostics and advanced endoscopic techniques, have been introduced in public-sector institutions in Pakistan. Training of health-care providers in the diagnosis and management of liver diseases, improvement in relevant infrastructure, and health-care affordability are crucial challenges.
The Government of Pakistan restructured its national health policy in 2001 after signing up to the Millenium Development Goals and began developing preventive health-care programmes.356 The Prime Minister's National Health Program of state-sponsored health insurance was launched in 2015, specifically aimed at Pakistani citizens living below the poverty line. Additionally, in the past decade, many digital start-up companies have been established to facilitate health-care delivery at all levels (eg, accessing health information, booking doctor appointments, ordering medications, or request laboratory tests and sample collection, and maintaining up-to-date medical records).
Pakistan's first liver transplantation was done in 2003 at the Sind Institute of Urology and Transplantation (Karachi). However, no other transplantations were done until 2011 when a single liver transplantation from a deceased donor was done in Lahore. From 2012 onward, several medical centres in Pakistan have attempted to develop programmes for transplantation from living donors.357 The most important impeding factor in developing high-volume transplantation programmes across Pakistan is the lack of skilled workforce. Shifa International Hospital (Islamabad) and the Shaikh Zayed Center of Liver Transplantation (Lahore) are the only two transplantation centres run by local teams, whereas others rely exclusively on international collaborators. Security concerns and visa delays make frequent travel by international teams difficult, and the reliance on international experts interrupts continuity of care. Thus, the presence of efficient local transplant teams is crucial to develop successful and sustainable transplantation programmes. Until February, 2017, only 539 liver transplantations had been done in Pakistan, and approximately 95% of these were done in the two locally run centres. A liver transplant from a living donor in Pakistan costs $35 000–45 000. Most patients are self-funded, and financial restrictions are one of the biggest hurdles to accessibility. The Human Organ and Transplantation Authority regulates legal and ethical aspects of liver transplantation in Pakistan, but its decentralisation with the 18th amendment of Pakistan's Constitution has moved various ministries, including the Ministry of Health, from central to provincial control.358 Those changes have given rise to five autonomous provincial bodies that regulate transplant activity, allowing for a stringent legal and regulatory process at the provincial level. Simultaneously, the current decentralised approach challenges the implementation of a future national transplant registry that might monitor transplantation activity and outcomes countrywide. The Government will have to consider innovative ideas including private–public sector partnerships and proper incentivisation of skilled medical personnel to make liver transplantation available in poor settings in Pakistan. The implementation of a national transplant registry is inevitable to ensure transparency in various steps of organ donation and outcome reporting while providing transplant services of international credibility.
A 2015 WHO report stated that there are 64 434 registered doctors, 6034 dentists, 30 516 nurses, and 27 000 nurse-midwives in Bangladesh.359 Additionally, the health workforce is skewed towards doctors, with a triple ratio of doctors to nurses to technologists of 1:0·4:0·24, by stark contrast with the WHO recommended ratio of 1:3:5. The involvement of the health workforce in the private sector has increased over the past two decades, as shown by the estimated 62% of medical doctors working in the private sector in 2013.176 Moreover, the private sector has seen tremendous growth in teaching institutions in that timeframe. There were no medical colleges or any private teaching institutions in 1996, but by 2011, 44 private medical colleges were established.359
Bangladesh has an extensive primary health-care infrastructure in its public health sector but facilities are inadequate. There is one bed for every 1699 people and a community clinic (n=12 527) for every 6000 people for primary health-care services.176, 359 However, these clinics lack facilities and expertise for the diagnosis and management of liver diseases.
Bangladesh has a long history of hepatology and related services and training programmes. Hepatology departments function in more than 15 public medical colleges and more are being developed. The country however, does not have a liver transplantation programme. Nevertheless, the hospital attendance of patients with liver disease has increased rapidly during the past couple of decades, and the sole medical university of Bangladesh experiences a tremendous burden of patients with hepatitis, at both its outpatient and inpatient departments.176 The number of hepatologists has increased several times over past two decades, but is not sufficient to cope with the increasing burden of patients with liver diseases.
Japan has one of the highest densities of hospitals globally, with a total of 7426 hospitals nationwide, of which 80% are privately owned.360 Hospitals in Japan are legally prohibited from for-profit management. Compared with OECD member countries, Japan has fewer medical doctors and more nurses. According to OECD data,361 there were 2·3 medical doctors per 1000 people in Japan in 2010. There were 10·4 nurses per 1000 people for the same year, which is average for OECD countries. The number of hospital beds in Japan in 2015 was 13·2 per 1000 people.362
The Japan Organ Transplant Network is an intermediary between donor and recipient for deceased donors. Transplantation from deceased donors was done in only 321 cases from 1964 to 2015 because of insufficient donors. Conversely, 8066 people from 1989 to 2015 received liver transplants from live donors. These cases are far fewer than in other Asian countries such as China, South Korea, and India.
Medical education is led by the Japanese Government. Of all medical universities in the country, 60% have been established by the central and local governments. A new system under the Japanese Medical Specialty Board was launched in 2018 to certify medical specialists under a common set of standards to upgrade the quality of health-care provision.363
In 2012, South Korea had 3298 hospitals and 514 687 hospital beds;301 86·9% of hospitals and 86·7% of beds were located in urban areas. The urban–rural disparity in the distribution of health facilities has been increasing.301 South Korea has a government-affiliated agency, the National Health Insurance Service, under the Korean Ministry of Health and Welfare that covers about 97% of the country's population and supervises all medical services. Additionally, for patients registered in the country's rare intractable diseases registry with autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, or post-liver transplantation, additional economic benefits, such as a reduction of their insurance excess is provided. Likewise, patients diagnosed with liver cancer receive additional economic assistance when registered with the Korea Central Cancer Registry.
In response to the increasing demand for health services triggered by expanding insurance coverage, the health workforce of South Korea has also continuously expanded. The proportion of practicing doctors was 2·03 per 1000 people in 2011 (of whom there were 0·58 primary care doctors per 1000 people and 1·45 specialists per 1000 people), which was lower than the average for OECD countries (3·18 per 1000).301 The proportion of nurses in 2011 was 4·72 per 1000 people, which is much less than the average for OECD countries (8·70 per 1000).301
The Center for Korean Network for Organ Sharing supervises overall processes for organ donations, distributions, and transplantations. In 2016, 1417 liver transplantations were done. Of those, 963 cases were from living donors.364 Since June, 2016, the Model for End-Stage Liver Disease system has been used to match deceased liver donors to compatible patients, instead of the Child-Turcotte-Pugh score. 1-year graft survival in 1998 was 62% for patients with liver transplants from deceased donors and 80% for those with living donors. Survival outcomes had improved substantially by 2009, showing 1-year graft survival of 76% for patients with transplants from deceased donors and 90% for those with transplants from living donors, primarily because of developments in quality control and immunosuppression. In South Korea, liver transplantation from living donors is thought to be effective and feasible for patients needing a transplant. Transplantation from living donors has substantially increased over the past three decades because livers from deceased donors are scarce. Better understanding of the regeneration of partial grafts and various advances in surgical techniques have contributed to a marked improvement in patient and donor outcomes in cases of living-donor transplantation.
In Australia, there were 3·6 physicians per 1000 people in 2016 and 12·6 midwives and nurses per 1000 people for the same year.365, 366 There were 3·9 hospital beds per 1000 people in 2010.367 The shortages of health-care professionals persist despite the growth of the workforce. In New Zealand, in 2010, there were 2·6 physicians per 1000 people (below the OECD average of 3·1) and 10 nurses per 1000 people (above the OECD average of 8·7).368
Australia has made major progress in tackling blood-borne viruses and sexually transmissible infections over the past two decades. At the time of writing, the country could eliminate hepatitis C by 2030, and WHO reports369 that hepatitis B prevalence in children is less than 1%. The current health workforce needs to increase to promote primary providers' awareness and knowledge of hepatitis B and C, and an increase in support, training, and mentorship for health-care professionals is needed to ensure successful testing, management, and treatment in primary health care. Community organisations and the health-care workforce need to be supported to increase appropriate engagement with at-risk populations, improve health literacy, and maximise positive health outcomes. Conversely, to meet the growing demand for liver transplant services, organ donation in Australia needs to increase from the 20 donors per million people per year in 2016, and the 13 per million per year in New Zealand.
Liver transplantation is the one of the commonest solid organ transplants in Australia and New Zealand. Liver transplantation programmes were initiated in 1985 in Australia and in 1997 in New Zealand. 5000 liver transplants had been done in approximately 4500 patients from inception until January, 2015, with approximately 260 transplants annually. Liver transplant centres are based in major hospitals in five of Australia's states. Median survival in adult recipients is approximately 20 years, and more than 70% of paediatric recipients are alive 20 years after transplantation.370 According to the Australian Institute of Health and Welfare, in 2016 the second most common reason for hospital separations (ie, a hospital stay that results in change of the type of care) was alcohol-related liver disease.
There are increasingly more doctors in Singapore, from 1·5 doctors per 1000 people in 2008 to 2·2 per 1000 in 2016, with the number of specialists also increasing from 2962 in 2008 to 5047 in 2016.371 The infrastructure of medical services in Singapore is excellent. The Smart Health-Assist programme372 was introduced in 2015 as part of the Government's broader Infocomm Media 2025 Masterplan.373 The Smart Health-Assist programme investigates the use of technology to support new models of care, in both home and community settings. Telehealth is one such key focus area.374 Rather than simply reactively treating hospital inpatients, doctors can proactively reach out to patients, regardless of their location, because of Singapore's technological capabilities and robust broadband connectivity.
There are four liver transplantation centres in Singapore: two private and two public. From 2007 to 2016, 261 liver transplantations were done,375 105 from living donors and 156 from deceased donors. In 1987, Singapore introduced a presumed consent law for organ donation, referred to as the Human Organ Transplant Act.376 It applied only to people aged 21–60 years who had died from unnatural causes, met the criteria of brain or cardiac death, were not Muslim, and had not formally dissented from organ donation. Implementation began in 1988 and applied only to kidney donation. A 2004 amendment to the Act also permitted living organ donation and included other organs, such as livers, hearts, and corneas. The 2004 amendment further included all causes of death rather than solely death by accidental causes. Further legislative amendments in 2007 and 2009 were made with the firm intent of expanding the supply of transplantable organs and ensuring that organ donors are not exploited, unlawfully induced, or forced into organ retrieval by non-government actors.377 Another scheme is the Medical Therapy, Education, and Research,378 which operates on an opt-in basis, allowing people to pledge their organs or body parts for transplantation, education, or research after death. Additionally, the Ministry of Health subsidises at least 50% of the cost of liver transplantations. Together with the MediShield programme for immunosuppression, patients receiving liver transplants are well supported financially.
Taiwan has fewer doctors and nurses than OECD countries. In 2013, there were 1·7 doctors per 1000 and 5·7 nurses per 1000 people in Taiwan, compared with the median of 3·3 doctors and 8·6 nurses in OECD countries.379
The first successful liver transplantation from a deceased donor in Taiwan was done in 1984 in a patient with Wilson's disease. The first transplantation of a liver graft from a living donor to an adult patient was in 1999. Throughout the following decade, the number of transplantations from living donors in Taiwan increased much more quickly than those from deceased donors. Universal coverage by the Taiwan National Health Insurance enabled the establishment of clear guidelines for donor selection, indications, and transplantation timing. The Insurance's outcomes of organ transplantation to ensure public awareness and transparency were also regularly published.380 There were 24 centres approved by the Taiwanese Ministry of Health and Welfare that did 3017 liver transplantations between 2003 and 2012, with 3-year overall survival of 82%.380
In summary, inexperienced health-care workers (doctors, nurses, and technicians) and inadequate infrastructure to care for patients with liver diseases (at primary, secondary, and tertiary levels) is a problem in the Asia-Pacific, especially in countries with middle and high HDIs. There is very little information on the number of liver specialists in each country, which might represent a lack of focus on liver diseases and a paucity of hepatology specialists. Hepatology programmes urgently need to be established in most countries in the region. Few liver transplantation facilities are available in Pakistan, Bangladesh, and Indonesia. Even in countries with good facilities, liver transplants from deceased donors represent only a small proportion of all liver transplants. Although liver transplantation from living donors is broadly successful in Asia, there is a huge demand for new centres and training in the procedure.
Priorities to address the burden of liver diseases in the Asia-Pacific region
Health financing in China is not equitable. In 2011, the average total health expenditure per capita for urban areas was three times higher than it was for rural areas (¥2698 vs ¥879) but the share of out-of-pocket expenditure was 50% for urban residents and 36% for rural residents.381 Major disparities between the rural and urban health-care systems persist, mainly because of insufficient government stewardship and unequally distributed social determinants of health. The Chinese Government is moving the health-care system towards universal coverage for both rural and urban residents. The New Rural Cooperative Medical Scheme is the major medical insurance scheme in rural China. It aims to protect households from falling into poverty because of high treatment costs (ie, catastrophic health expenditure), and its principal objective is to provide universal coverage and improve equity of access to health care.382, 383 However, the main goal of preventing rural residents from falling into poverty because of severe illness is still far off. With the vast expansion of coverage between 2004 and 2007, reimbursement is falling as medical expenditure is increasing. In 2007, the real reimbursement rate (reimbursement amount divided by total expenditure on medical care) was around 19% for illnesses that required expenditures between ¥200 and ¥2000, but only 8% if expenditure was more than ¥10 000.384 The distribution of health workers is also uneven between rural and urban areas of China, with two-thirds of the health-care workforce situated in urban areas. Additionally, the educational or skill level of rural health workers is inferior to those in urban areas.385 A 2011 web report in Finance showed that there were still more than 300 million people without access to safe drinking water in rural China.386 Further progress must be guided by the principle of health equity and fairness and supported by cross-sectoral cooperation.
Diagnosis, treatment, and choice of optimal therapy for patients with HBV and HCV need to be improved in China. For HBV, nucleoside and nucleotide analogues such as lamivudine, adefovir, and telbivudine are not preferred by international guidelines but are still used in low-income areas,382, 387 although the first-line antiviral drugs entecavir and tenofovir disoproxil fumarate are recommended by practice guidelines and are already on the reimbursement list.388 As tenofovir becomes cheaper and generic versions of tenofovir and entecavir are approved, appropriate therapies should be increasingly prescribed. Similarly, for patients with HCV, cheaper interferon-free direct-acting antiviral regimens that are included in reimbursement lists are urgently needed.389, 390
Future efforts to reduce hepatitis-related morbidity and mortality in China should focus on preventive strategies, safe blood practices, public education, and training health staff for large-scale HBV and HCV testing and treatment provision.391 A strict action plan to reduce the harmful use of alcohol such as an excise tax on beer, wine, and spirits, and legally binding regulations on alcohol advertising should be implemented. The Government should also implement an operational policy to reduce unhealthy dietary practices and promote physical activity to prevent NAFLD.
Considering the current status of liver diseases in China, future research should focus on, but not be restricted to: improving the quality and completeness of incidence and prevalence reporting of acute and chronic hepatitis B and C; synthesising accurate disease burden information on the morbidity and mortality from cirrhosis and hepatocellular carcinoma attributable to HBV and HCV; and generating a definitive action plan with milestone targets and secured financing. It is also necessary to streamline clinical trials, to speed up approval for HBV and HCV drugs, and to substantially reduce their price and include them in reimbursement policies through independent cost-effectiveness analyses and negotiating with multiple stakeholders. Large-scale test-and-treat strategies for patients with hepatitis B and C must be optimised, and an optimal service delivery model and standard package for their diagnosis and treatment needs to be established and validated. Finally, accurate data generation on the prevalence of NAFLD and alcohol-related liver disease and their related morbidity and mortality, and research on effectiveness of various interventions to prevent these diseases are also needed.
In India, improving sanitation and providing safe drinking water is important to prevent HAV and HEV. The rural Indian population (about 70% of the total population) has mostly low literacy, lacks basic sanitary facilities, and is thus at high risk of faecal–oral transmission of hepatitis. Hygiene is also poor in urban areas, with poor disposal of solid and liquid waste (including excreta) and poor drainage systems. The Swachh Bharat Abhiyan (or Clean India Mission) is a nationwide campaign launched in 2014 for clean streets, roads, and other infrastructure. The campaign's objectives include eliminating open defecation through the construction of household-owned and community-owned toilets and establishing an accountability mechanism to monitor toilet use (ie, through a dedicated workforce using mobile phones and tablets). According to the Government of India, which runs the mission, 99% of rural villages were free from open defecation as of Oct 2, 2019.392, 393
Birth-dose immunisation against hepatitis B in India is low. Blood safety is a challenge in India because of the high prevalence of HIV, HCV, and HBV, the relatively low proportion of volunteer donors, and unstandardised screening procedures across blood collection centres.394 One study has estimated that nucleic-acid amplification testing could prevent 3272 infectious donations a year (including 818 HIV, 409 HCV, and 2454 HBV) from the approximate 5 million annual donations.395 Centralised screening centres for nucleic-acid amplification testing that serve all blood banks in a given city and report results electronically are hugely successful globally. This model has worked very well in Thailand, which has a fragmented blood-banking system similar to India and other countries in the region.
There are several factors in India and other developing countries that increase the risk of percutaneous needle stick injury and transmission of HBV and HCV. These include: severe disease requiring intravenous drugs; a preference to use injections over oral or other administration methods; use of hazardous equipment and procedures (eg, no disposable syringes, safe needle devices, and sharps disposal containers; inability or failure to use sharps containers immediately after injection; no personal protective equipment; inadequate staffing; reusing needles); and insufficient vaccination coverage against hepatitis B, availability of post-exposure prophylaxis against HBV, and adherence to standard precautions.396 In India, more than 93% of injections are unsafe.397 Inadequately sterilised needles and syringes are an important cause of transmission of blood-borne hepatitis in India.398 A large proportion of health-care workers in India are unvaccinated, many are unaware of their vaccination status, and are thus vulnerable to blood-borne infections.399 The implementation of safe injection practices in the Indian health-care system is urgently needed.
Although HAV vaccination is not included in the national immunisation schedule, it is available privately in high-income settings, as it is difficult to convincingly argue for its country-wide use. India has traditionally been an area of high HAV endemicity; however, studies have found evidence of an epidemiological shift to intermediate endemicity for people with high incomes in various cities.130, 400 In such cities, high-income areas are susceptible to HAV, but people living there are not likely to become infected, whereas most of the remaining population continue to get infected and transmit the virus. The hepatitis A vaccination strategy in susceptible high-income population groups would need to be reassessed. Introducing a hepatitis A vaccine in resource-poor populations is problematic because the resulting reduction in HAV transmission can have unintended consequences. Although it might reduce the risk of HAV infection, it also has the potential to increase the average age at which HAV infection occurs,401 thereby increasing the overall risk of acute disease. Thus, introducing vaccination with low coverage in a high-endemicity area would change the epidemiology to an intermediate-endemicity pattern, which is undesirable. By contrast, high-coverage vaccination in an intermediate-endemicity area would result in the desirable outcome of low endemicity.
Licensed versions of several direct-acting antiviral drugs with anti-HCV activity (including sofosbuvir, daclatasvir, sofosbuvir–ledipasvir, and sofosbuvir–velpatasvir) are available in India, and the price for a course of 3–6 months at the Government's expense is about $1 a day. A modelling study showed that treatment of HCV infection using generic direct-acting antiviral drugs is cost-saving.402 Provision of HBV oral drugs through the National Viral Hepatitis Control Program is currently in the planning stage.
Alcohol-related liver disease is likely to become an increasingly big problem, given that alcohol consumption in India is increasing. Measures to reduce alcohol-induced injuries are in place but are not strictly implemented. It might be possible to prevent NAFLD through various interventions at all societal levels, such as the 14·5% fat tax that the state of Kerala has already imposed on the consumption of certain foods.403 Far-reaching programmes to increase the awareness of the public and medical personnel on liver disease prevention are needed.
Research priorities on liver diseases in India need to focus on the quality of data collection regarding the incidence and prevalence of common causes of liver disorders and their risk factors. Data need to be generated on morbidity and mortality related to cirrhosis and hepatocellular carcinoma with various aetiologies. With the launch of the National Viral Hepatitis Control Program in 2018, research should also focus on the development of low-cost point-of-contact testing kits for viral hepatitis. The effectiveness of potential interventions to prevent and treat NAFLD and alcohol-related liver disease needs to be investigated. Finally, implementation research to improve the coverage and effectiveness of potential interventions and to improve awareness of these diseases in the general population is also needed.
In Indonesia, challenges persist in the programmes for control of viral hepatitis, including insufficient knowledge and awareness about viral hepatitis, inadequacy of available data, a large population spread over a vast archipelago, problems in diagnosis and treatment due to insufficient training of staff, few viral hepatitis specialists, and insufficiant health-care infrastructure and investment. Moreover, the need for viral quantification before, during, and after treatment, as well as the pretreatment determination of viral genotype as recommended by all existing guidelines, also pose problems that could threaten the success of Indonesia's National Health Insurance scheme. The scheme covers drugs for HBV and HCV, but does not cover the diagnostic tests needed to determine whether these drugs are needed. This discrepancy, along with the insufficient number of testing facilities, nullifies the potential benefit of accessible treatment for much of the population.36 A government strategic plan for disease prevention and increasing the uptake of services has been developed that integrates existing health programmes, such as mother-and-child health care, HIV-hepatitis co-infection management, public health-care insurance, public–private partnerships, and community engagement with civil society and the media.
The Indonesian Government has increasingly committed to fighting liver diseases, particularly viral hepatitis, but has not made this commitment into a formal priority. There is a paucity of reliable epidemiological and other data related to various liver diseases; such data are crucial to guide evidence-based policy development. The country needs to invest in research on liver diseases such as monitoring the epidemiological patterns of communicable and non-communicable liver diseases, including their prevalence, risk factors, pathogenesis, and natural history. Studies are needed on the impact of interventions, including assessment of preventive measures, guidelines, drug efficacy, and treatment. New tools for prevention, diagnosis, care, and treatment (eg, a new pilot project of catch-up vaccination for hepatitis B in vulnerable and high-risk groups and hepatitis B treatment for pregnant women) are needed.
In Pakistan, there are no publicly funded screening programmes for viral hepatitis. Such programmes are urgently needed to improve the National Hepatitis Strategic Framework274, 275 and implement prevention and treatment measures. Despite the high burden of hepatitis, less priority is given to it than to HIV, and there are no properly trained medical staff in small towns and villages. Therefore, improving compliance with HBV vaccination at birth is of great importance. An HAV vaccine is available but is not covered by any vaccination programmes, and there are no national guidelines on HAV vaccination. Donated blood is screened for hepatitis B and C but existing regulations for safe blood transfusion services are ineffective. Paid blood donation should be declared illegal. Community-based interventions to educate health-care providers and the public on the risks of HBV and HCV transmission associated with contaminated blood, unsafe injections, and reusing razors are needed. There are no widely available auto-disable or single-use syringes and strict implementation of strategies to avoid reusing needles or syringes. To prevent transmission, it is also important for the Government to provide safe drinking water and sanitation, and to educate the public on hygienic practices such as drinking boiled water. Opioid substitution programmes should be implemented, as should safe blood transfusion services that are easy to use and can be monitored according to international standards. Electronic media could be used to raise public awareness of viral hepatitis and to encourage patients to get screened and treated.
It is important to establish an integrated hepatitis surveillance and response system in Pakistan, with multiple sites across the country that provide laboratory testing for diagnosis and treatment. A publicly funded programme for HBV and HCV treatment is already established. Sofosbuvir and its generic versions are registered by the Drug Regulatory Authority of Pakistan; it is cheap but is entirely covered by patients' out-of-pocket expenses. Generic versions of daclatasvir are in their registration phase. Harm reduction strategies need to be implemented to provide treatment to users of injectable drugs, particularly in prisons. The Ministry of Health should consider early approval of hepatitis C medications already approved by the US Food and Drug Administration, monitoring the bioequivalence of generic drugs, and assessing the economic burden of hepatitis care, which is currently not being done. There is an urgent need for accurate epidemiological data assessing viral and other liver diseases. Developing strategies and studying their effect on prevention and treatment outcomes is another priority area of research. Research into ways to improve birth-dose HBV vaccination coverage is urgently required. Various modalities for training of the existing workforce in care of patients with liver diseases (on-site training, online training, teleconferencing, etc) also need to be investigated.
In Bangladesh, the prospect of achieving WHO's Global Health Sector Strategy on Eliminating Viral Hepatitis404 seems achievable and the Government has made it into an official priority. The Government is considering birth-dose and catch-up vaccination and vaccination of vulnerable groups against HBV, screening of at-risk groups such as pregnant women, and promoting access to health care by improving laboratory and imaging facilities in district-level government hospitals. Free treatment of individuals infected with HBV and HCV is pending pilot implementation and eventually expanded nationwide.
Although the cost of antiviral drugs has been reduced considerably in Bangladesh, the costs of diagnostic medical examinations are still extremely high. Additionally, patients are not sufficiently encouraged to get screened for hepatitis and to receive therapy. Awareness of hepatitis is increasing in urban areas, but rural areas are lagging in this respect. A study has shown that HBV DNA is prevalent in HBsAg-negative blood.405 Thus, the quality assurance of HBsAg testing kits and safety of HBsAg-negative blood, which has not been tested for anti-HBc or nucleic acids, needs Government attention. It might not be practical to test blood samples with nucleic-acid amplification as a preventive measure; however, testing for anti-HBc could be accommodated in Bangladesh to prevent HBV transmission through blood transfusion.
There have been substantial advances in research on liver diseases in Bangladesh and several epidemiological studies have been published in the past two decades.56, 57, 58, 59, 60, 61, 62, 149, 150, 152, 153, 154, 155, 156, 218, 219, 220, 223, 406, 407, 408 Still, baseline data on incidence, prevalence, risk factors, natural history, and the changing epidemiology of various causes of liver diseases need to be generated. Studies are needed to develop cheap, accessible, point-of-care testing for HBV and HCV, and on preventive measures and new drug treatments for NAFLD. Research to improve coverage of HBV vaccination for high-risk groups, particularly preventing HBV transmission from mother to baby, is needed. Strategies should be developed to improve general awareness about liver disease among the public and medical staff and training of existing health-care workers on managing liver diseases.
In Japan, as the prevalence of viral hepatitis decreases, cases of NASH and NAFLD are increasing. It is currently impossible to estimate how long this increase will continue and what preventive measures would be effective. Efforts to tackle NAFLD centre on the Government's extensive focus on obesity prevention and hepatocellular carcinoma through screening programmes and advances in treatment. Japan has a budget of $400 billion per year for overall health-care expenditure, accounting for 38·8% of the national governmental budget. Research must focus on the pathogenesis and treatment of NASH, autoimmune hepatitis, primary biliary cholangitis, and liver fibrosis, and on effective ways of delivering health-care education and information on prevention and treatment of NAFLD. Effective models of community-based care for patients with liver diseases, including cirrhosis and hepatocellular carcinoma, need to be investigated. Also, developing novel therapeutic targets for hepatitis B and treatment of hepatocellular carcinoma are major unmet needs. Research is needed into strategies to tackle increasing health costs and improve health equity.
In South Korea, HBV represents a major medical burden. According to a survey of 3000 people done by the Korea Association Study of Liver Disease (KASL), approximately half of the respondents (45·4%), aged between 15 and 69 years, had not had a HBsAg test or did not know whether they had had the test. Additionally, although antiviral therapy has been well supported by the national insurance reimbursement policy, there is still a gap between the HBV management guidelines proposed by KASL and government policy. Although screening tests for HBV infection are done for women who are preparing for pregnancy, army recruits, adults aged 40 years and older, and groups at high risk for hepatocellular carcinoma, a continuous management programme after HBV diagnosis requires further consideration, and the efficacy and cost-effectiveness of screening adults older than 40 years must be re-evaluated.
There is currently no screening programme for HCV in South Korea. One-off HCV screening and treatment of people aged 40–70 years is likely to be very cost-effective compared with the current practice of no screening.409 Importantly, to reduce the incidence of HCV-related end-stage liver-related complications and mortality, a national screening programme should include a national health policy aimed at managing HCV in the South Korean population.
According to a survey done by KASL in 2013 (Won H W, Korean Association for the Study of the Liver, personal communication), 79% of respondents who visited tertiary hospitals due to alcohol-related liver disease had not had the chance to join an abstinence programme or receive consultation from a psychologist. Only 3% of patients with alcohol-related liver disease had received specialised rehabilitation, which assists patients with returning to a normal social life. Hospital visits and treatments are mainly dependent on the will of the patient. Priority areas for addressing the burden of alcohol-related liver diseases in South Korea include research into helping people to adopt healthy lifestyles (ie, avoiding alcohol consumption, early detection of alcohol overuse and alcohol-related liver disease), effective strategies in helping people with alcohol-related liver disease to stop their alcohol consumption, and new therapeutic targets for alcohol-related liver diseases including severe hepatitis.
According to KNHANES 2009–13,410, 411 the number of people participating in intense physical activity is decreasing in South Korea, whereas caloric intake and the prevalence of diabetes, hypertension, obesity, and metabolic syndrome is increasing. According to the 2013 KASL survey (Won H W, Korean Association for the Study of the Liver, personal communication), 40% of respondents did not exercise even for 1 h per week, despite recognising that regular exercise is helpful for NAFLD management. Another issue is that national insurance does not support education programmes for optimal food intake and exercise, although lifestyle modification is the basis of NAFLD management. In many cases, doctors give patients who visit hospital general lifestyle modification recommendations, rather than specific guidelines. Priority areas for action for NAFLD in South Korea include research into noninvasive markers of NASH and fibrosis in NAFLD and on new therapies, ways to motivate people of all ages to adopt healthy lifestyles, and the pathological mechanisms of hepatocellular carcinoma in patients with NAFLD.
The Korean Government started a national hepatocellular carcinoma examination project in 2003.412 The following factors need to be considered to improve the project: the target population; proper classification of hepatocellular carcinoma, as the International Classification of Diseases-10 code is inaccurate and does not provide appropriate guidelines on alcohol intake; and supportive hospital care programmes. Finally, lifestyle modifications for healthy bodyweight must be emphasised in the general population to prevent NAFLD.
Although support for research into liver diseases has increased substantially, it is still insufficient. Research priorities for liver diseases in South Korea include identifying barriers and facilitators, and developing strategies to increase awareness and education in the general population and physicians, for HBV and HCV testing and uptake of treatment, particularly in high-risk groups. A simple, accessible, cost-effective, and non-invasive test for NASH and strategies to help people to adopt healthy lifestyles are needed. Promoting awareness and education about alcohol misuse and evaluating successes and errors of abstinence and rehabilitation programmes for patients with alcohol-related liver disease is also necessary. An accurate risk model that incorporates newly identified risk factors and biomarkers must be developed for primary care providers. Additionally, research into the development of a simple and organised surveillance system for groups at high risk for hepatocellular carcinoma would facilitate making health care for these patients efficient and cost-effective.
Australia and New Zealand are multicultural countries, which turns diagnosing and treating people with hepatitis infection into a major challenge. The principal barrier to expanding patient coverage is that refugees and asylum seekers living with chronic hepatitis B have many other priorities, such as reuniting with their families and establishing a life in Australia and New Zealand, that are more important to them than health-seeking behaviours.396 Multiple other challenges include language and cultural differences and little disease-specific knowledge.413
Australia and New Zealand have low population densities, vast stretches of uninhabited land, and several urban centres distributed sparsely along the coast. The countries have problems addressing the health-care needs of remote communities, where the proportion of Indigenous people is high and geographical distances are extremely large.414 Inequalities in the social determinants of health between metropolitan and rural and regional populations influence the need for health care.415
Access to comprehensive primary health care involving specialists is considered ideal for the early and ongoing management of illness in rural areas.416 However, only 15% of Australian specialists have their main practice outside metropolitan areas, whereas 30% of Australians reside in rural areas.417 Rural specialist outreach services could help to overcome complex barriers to service access, mainly due to language and cultural differences, and avoid the cost and effort of seeking care away from home.418 Visiting liver specialists can meet many of the health service needs of rural areas (including prevention and management of liver diseases). Additionally, visiting specialists can also provide periodic procedural support for rural generalists, thereby increasing the clinical confidence and reducing the professional isolation of rural practices.419 Australia is the only country that, since 2000, has had a sustained national outreach policy that subsidises the outreach of medical specialists to rural areas; still, there is scope to improve outreach in hepatology services.420
There is also insufficient knowledge among health professionals of risk factors for the presence and progression of liver disease and the effect of liver disease on health and life expectancy. Waiting times for specialised liver centres are long, so patients cannot access services in a timely manner. The inability of primary care physicians to provide effective guidance and the lack of a management toolbox for primary care might also lead to their reduced interest in early intervention.
Another impediment to controlling hepatitis B and C is late notification of hepatitis, defined as late hepatitis diagnosis, which is mainly associated with old age. Late notification increases the risk of decompensated cirrhosis and hepatocellular carcinoma.421 Further, there is cultural resistance in migrant populations to accepting dietary and health advice from health service providers.422
The price of drug treatment and medical services that are not supported by the Pharmaceutical Benefits Scheme represents another barrier to tackling the burden of liver disease—eg, new obesity drugs such as naltrexone–bupropion. Policy makers need to recognise that liver diseases are chronic diseases and to establish nurse-led community-based models of care. Finally, enhancing funding for medical research to identify novel therapeutic targets for treating specific liver diseases, such as alcohol-related liver disease, NASH, and hepatitis B, and for implementation research is crucial.
The focus of HBV and HCV research in Australia and New Zealand should be on preventing transmission in people who inject drugs, including: evaluating novel methods to improve population estimates of injected drug use and hepatitis infections; evaluating implementation, effectiveness, and scale-up of existing prevention interventions for this population; identifying barriers and facilitators associated with HBV and HCV testing at the levels of the patient, provider, and health-care system; evaluating novel, point-of-care assays for HBV and HCV testing and treatment uptake that are highly sensitive and specific, simple, quick, and cheap; and evaluating the scale-up of strategies for improving the linkage to care for patients newly diagnosed with HBV and HCV.
New and effective therapies for patients with NAFLD and liver fibrosis need to be developed. An unmet clinical need is the identification of novel therapeutic targets for hepatitis B and liver cancer. Australia will also need to invest in research on liver diseases that are particularly common, including prevalence and risk factors, natural history, and effective methods for control and treatment. Further, there is a great need and potential for implementation research to improve the coverage and effectiveness of various interventions for liver diseases. Research needs to especially focus on Indigenous populations regarding prevention, treatment, models for engagement, and service delivery for various liver disorders.
In Singapore, identifying cases of hepatitis B and C is the biggest barrier to appropriate management of patients and control HBV and HCV infection. For hepatitis B, family screening is recommended under Singapore's hepatitis B guidelines. Once people are identified as having viral hepatitis, referring them to receive medical care might be difficult. Barriers to follow-up include insufficient reminders to patients, lack of physician time, cost of tests and treatment, and blood taking. In a study of patients with chronic hepatitis B who were offered health screening in 2003, 67% were not found to be followed up regularly.423 In a follow-up study, the barriers to regular follow-up included lack of education of the patient on the implications of not being followed up, cost of follow-up, blood taking, and lack of time.424
Regarding the management of non-viral hepatitis liver disease in Singapore, a strategy to target high-risk groups, particularly those with diabetes and those who are obese, would be the first step. Lifestyle interventions can be challenging to implement but much can be done by the Government to maximise disease control by introducing health-promoting public policies, infrastrucutre changes to facilitate healthy choices for living, working, studying, and recreation, and collaborative public–private partnerships. Alcohol-related liver disease represents an area that has not been addressed extensively, and expertise of medical staff around alcohol management, addiction behaviour, and support facilities needs improvement. Such improvement strategies might include developing multidisciplinary teams of psychiatrists, counsellors, psychologists, nurses, and social workers to provide individual, group, and family therapy; increasing addiction awareness in the community; and training for health-care and social service professionals and promoting addiction on research.
Research priorities for liver diseases in Singapore include: identifying barriers and facilitators associated with HBV and HCV testing and linkage to care and treatment; evaluating strategies that might be helpful in increasing testing (coverage and frequency) and uptake of treatment for HBV and HCV; and evaluating novel point-of-care assays and commercial serological and virological tests using dried blood-spot collection.
Priority research areas for NAFLD include finding a simple, accessible, cost-effective, and non-invasive test capable of finding cases in a large at-risk population and investigating the most effective ways to help people to adopt healthy lifestyles for the prevention and treatment of NAFLD. Research is also needed into the most effective ways of delivering health-care education and information about excessive alcohol consumption, the warning signs and risks of alcohol-related liver disease to different demographics (including young people), and the most effective strategies to reduce the risk of alcohol-related liver disease in heavy drinkers. Outcome measures of liver mortality, liver cirrhosis, and liver cancer need to be accurately collected with annual reports of their frequency to determine whether any measures taken against liver disease are improving outcomes.
The barriers to care for people with liver diseases in Taiwan are mainly financial. The Government is currently considering a public health programme to treat most, if not all, people infected with HCV. Public awareness and education on hepatitis B and C should be strengthened.425 General screening for HCV and HBV infection needs further efforts. Additionally, the data on people who have already been screened for HBV infection need to be retrieved from various large databases for integration into current treatment promotion.
The public health delivery system in Taiwan is robust, as exemplified by the successful national hepatitis B control programme that was launched 36 years ago. Taiwan aims to exceed the targets set by WHO of eliminating viral hepatitis as a public health threat by 2030 but more efforts need to be made by the Government to reach this goal. The most urgent of them is treating patients with chronic HCV infection with direct-acting antiviral drugs.
Priority research areas in Taiwan include strategies to increase awareness and education on the need for screening and regular monitoring and treatment of HBV, both in the general population and physicians, and to continuously evaluate the quality and effect of HBV vaccination. Research is also needed into the natural history and evolving epidemiology of HBV in Taiwan, to ensure that vaccination programmes are not missing any new risk groups that might arise over time. For example, although waning immunity of the vaccine after 15–20 years has not yet been observed to the extent that a booster is generally recommended after this time period, the possibility that this situation might change should be monitored closely.425 Research is also needed for strategies to overcome geographic and social inequities in access to care.
In summary, the major barriers to the care of patients with liver diseases in Asia-Pacific countries with middle and high HDIs include lack of baseline epidemiological data on various liver disorders, low coverage of birth-dose HBV vaccination, lack of awareness in the general population and health-care workers about liver diseases, lack of trained health professionals, and low public health expenditure. By contrast, the major barriers to care in high-HDI countries in Asia-Pacific include geographical and social inequalities to access to care, delivering HBV vaccination to new high-risk groups, delivering care to people infected with HBV and HCV who inject drugs, and increasing awareness in the general population to adopt healthy life styles. Research priorities need to be country-specific and should focus on specific barriers.
Discussion
Liver diseases are increasingly recognised as a major health challenge in developing countries, especially those in the Asia-Pacific region. Although viral hepatitis is a major cause of morbidity and mortality, the contribution of alcohol-related liver disease and NAFLD to the liver disease burden is rapidly increasing.
Viral hepatitis A and E are major causes of morbidity and mortality related to acute hepatitis in countries of the Asia-Pacific that have medium and high HDIs and whose populations have low access to clean drinking water and sanitation facilities (see panel 1 for a list of priority areas for liver diseases related to viral hepatitis). Of all deaths due to acute hepatitis in the region, 89% occur in medium-HDI countries, 9% in high-HDI countries, and 2% in countries with very high HDIs (figure 6 ). 95% of deaths related to acute HAV and HEV in the region occur in medium-HDI countries (figure 7 ). The SDGs, as part of the UN's 2030 Agenda for Sustainable Development, have ambitious goals in this regard. Goal 6 is to ensure availability and sustainable management of water and sanitation for all by 2030. Goal 6.1 calls to achieve universal and equitable access to safe and affordable drinking water for all, and Goal 6.2 aspires to achieve access to adequate and equitable sanitation and hygiene for all, as well as the end of open defecation.404 In the past decade, much progress has been made to increase access to drinking water and sanitation but still too many people lack access to a safe, sustainable water supply and sanitation services.
Panel 1. Priority areas of action for liver diseases related to viral hepatitis in the Asia-Pacific region.
Policy, planning, advocacy, and resource mobilisation (building infrastructure for sound policy and programme development)
National priority actions
-
•
Create an adequate statutory and regulatory environment for prevention and control of viral hepatitis
-
•
All heavily burdened countries to have fully funded control and elimination plans to achieve elimination by 2030
-
•
Advocate and mobilise resources for prevention and control of viral hepatitis
-
•
Create a fiscal space for new programmes with costed investment programmes and adopt domestic innovative finance tools where appropriate
International priority actions
-
•
Recognise the need to focus on countries with high viral hepatitis burdens and support national policy development
-
•
Support national policy makers in their activity (ie, WHO, Unitaid, non-governmental organisations) and provide international support for financing measures (ie, Unitaid, the Global Fund, corporate donors)
Viral hepatitis surveillance
National priority actions
-
•
Establish an effective surveillance system for viral hepatitis and improved capacity for complete and accurate disease reporting
-
•
Standardise data collection systems for core and targeted surveillance of viral hepatitis
-
•
Improve the epidemiological investigation and response capacity to outbreaks
-
•
Identify or develop and evaluate evidence-based interventions for prevention and control of viral hepatitis
International priority actions
-
•
Support national policy makers
Viral hepatitis prevention
National priority actions
-
•
Ensure all WHO elimination targets are addressed in plans
-
•
Emphasise the importance of sanitary conditions and personal hygiene
-
•
Ensure provision of harm reduction services, engage with marginalised groups (eg, prisoners, especially those who inject drugs), and ensure clear public health messages to encourage testing and treatment for HBV and HCV
-
•
Determine the need to include hepatitis A vaccination in routine childhood immunisation through periodic seroepidemiological surveys, disease surveillance, and modelling and cost-effectiveness analyses and formulate a hepatitis A vaccination policy for patients with chronic liver disease
-
•
Introduce hepatitis E vaccination in countries with high incidence of HEV infection
-
•
Address operational challenges in the delivery of birth-dose HBV vaccination
-
•
Promote the use of effective risk reduction interventions and strategies for HBV and HCV prevention
International priority actions
-
•
Support countries to decriminalise use of injected drugs and ensure equitable access to services for all (ie, non-governmental organisations, WHO, civil societies)
-
•
Ensure appropriate funding for HBV vaccination, including birth doses (ie, Gavi, WHO) and support research and development into HCV vaccine development (ie, research funders and pharmaceutical companies)
Viral hepatitis care and treatment
National priority actions
-
•
Develop standard procedures for management and guidelines on counselling, support, and care for patients with acute viral hepatitis
-
•
Assure timely access to chronic HBV and HCV diagnosis, care, treatment, and supportive services and their integration into primary care settings
-
•
Establish programmes to support care and treatment for marginalised individuals and populations
-
•
Focus on substantially scaling up testing for HBV and HCV
-
•
Create and evaluate simplified care pathways relevant to local settings and integrate them with existing services
-
•
Ensure that testing for HBV and HCV is integrated into the broad health-care system, rather than in centralised facilities
-
•
Promote task sharing and decentralisation of care through capacity building, training, and removal of requirements for specialised prescribing
-
•
Develop and regularly update guidelines for the clinical management, counselling, and care of patients with viral hepatitis
International priority actions
-
•
Support operational research into simplified pathways for screening, diagnosis, and treatment of viral hepatitis, integrated and improved service delivery, and linkage to social welfare programmes
-
•
Ensure access to quality diagnostics through an essential diagnostic list and prequalification of diagnostic tests for quality, performance, and safety (ie, WHO, funders)
-
•
Support scientific models of care and research and development into novel diagnostics, suitable for decentralised settings (ie, research funders, Foundation for Innovative New Diagnostics, industry)
Access to treatment
National priority actions
-
•
Ensure that all essential medicines for viral hepatitis are included in national programmes, with an emphasis on pangenotypic regimens
-
•
Apply comprehensive policy approaches to promoting access, including compulsory licensing
International priority actions
-
•
Ensure that all essential medicines are prequalified and either available through voluntary licensing or the Medicines Patent Pool (ie, WHO, non-governmental organisations, civil society, funders)
-
•
Support shared procurement mechanisms for treatment (ie, Pan American Health Organization)
Knowledge and awareness about viral hepatitis prevention, vaccination, risk factors, treatment, and management
National priority actions
-
•
Increase the knowledge about viral hepatitis in the general population and promote a healthy lifestyle in patients who are newly diagnosed or living with chronic viral hepatitis
-
•
Improve and expand the knowledge about viral hepatitis among health workers and carers
International priority actions
-
•
Support nations in their activities (ie, WHO, industry)
Monitoring progress
National priority actions
-
•
National plans need clearly defined, measurable objectives and new indices of national progress need to be developed
International priority actions
-
•
The progress of individual countries towards elimination goals needs to be closely monitored (ie, Polaris, WHO, creation a new elimination index)
Research on prevention and control of viral hepatitis
National priority actions
-
•
Research to monitor the changing epidemiological and virological patterns of hepatitis
-
•
Reduce the risk of transmission
-
•
Assess the impact of interventions and assess and develop new tools for prevention, diagnosis, care, and treatment
International priority actions
-
•
Support nations in their activities (ie, WHO, industry)
Figure 6.
Distribution of (A) all liver-related, (B) hepatitis-related, (C) cirrhosis-related, and (D) liver cancer-related deaths per HDI in the Asia-Pacific region1
HDI=Human Development Index.
Figure 7.
Distribution of (A) HBV-related and (B) HAV-related and HEV-related deaths from acute hepatitis per HDI in the Asia-Pacific region1
HDI=Human Development Index.
Hepatitis B and C are still responsible for a considerable fraction of morbidity and mortality due to liver diseases in almost all countries of the Asia-Pacific, although Taiwan has shown great success with HBV vaccination and reducing the burden of HBV in the past two decades. Overall, 86% of deaths related to acute HBV occur in medium-HDI countries (figure 7).1 Of all deaths due to cirrhosis in the Asia-Pacific, 66% occur in medium-HDI countries, 30% in high-HDI countries, and 4% in countries with very high HDIs (figure 6).1 63% of deaths due to HBV-related cirrhosis and 77% of deaths due to HCV-related cirrhosis occur in medium-HDI countries (figure 8 ).1 Of all deaths due to liver cancer in the Asia-Pacific, 74% occur in high-HDI countries, 18% in medium-HDI countries, and 8% in countries with very high HDIs (figure 6). 79% of those due to HBV-related liver cancer and 32% of those due to HCV-related liver cancer occur in high-HDI countries (figure 9 ).1 Preventing transmission of HBV and HCV is entirely achievable. HBV vaccination programmes for infants have been implemented by all countries. The administration of a birth dose of the HBV vaccine is still inadequate in many countries, especially in low-income and rural settings. Implementing policies on mandatory screening of blood and blood products for HBV and HCV and safe injection practices is still a challenge in many countries (eg, India and Pakistan). We strongly recommend a focus on harm reduction strategies that target people who inject drugs in all countries of the Asia-Pacific where these practices are prevalent. There has been progress in improving access to generic medications and reducing costs. The governments of many countries have put HBV and HCV drugs on their lists of essential medicines. There is an urgent need to make generic drugs available in all countries of the region and bring the costs of hepatitis C drugs to less than a dollar a day, following India's example.
Figure 8.
Distribution of deaths from cirrhosis due to (A) HBV infection, (B) HCV infection, (C) alcohol consumption, and (D) other causes per HDI in the Asia-Pacific region1
HDI=Human Development Index.
Figure 9.
Distribution of deaths from liver cancer due to (A) HBV infection, (B) HCV infection, (C) alcohol consumption, and (D) other causes per HDI in the Asia-Pacific region1
HDI=Human Development Index.
Since only a small proportion of patients with hepatitis B and C are ever diagnosed, the importance of screening and diagnostics need to be better emphasised. New approaches and tools are required for point-of-care diagnostics that are suitable for high-burden, low-resource countries. The 2018 establishment of a WHO Essential Diagnostics List426 is a welcome recognition of this importance. A greater focus is now needed on prequalification (ie, evaluating diagnostic tests with standardised protocols for their quality, performance, and safety to guide procurement decisions by actors such as WHO Member States or UN agencies) to ensure provision of high-quality diagnostics and clinical evidence for simplified management algorithms in settings where diagnostics are not available.4 We believe that governments should widely engage with all stakeholders, including individuals and organisations representing at-risk groups (eg, people who inject drugs, prisoners, and individuals with HIV), and also be liberal in approving and implementing new diagnostic devices.
International organisations have a key part in supporting national progress and they need to ensure that viral hepatitis is part of their remit, equal to other major infectious diseases such as tuberculosis, malaria, and HIV. Some organisations have led in this regard—notably WHO, Unitaid, and Clinton Health Access Initiative—but more can be done. There are several areas that organisations can prioritise to support viral hepatitis elimination efforts. Some are specific to viral hepatitis, for example the need to support the scale-up of birth-dose vaccination, which should be included in the remit of Gavi, the Vaccine Alliance, for support. Several other areas can leverage existing mechanisms that support other disease responses, notably HIV, to improve access to care and treatment for patients with viral hepatitis.4 We believe that governments should be increasingly accountable and take timely measures toward national viral hepatitis elimination strategies. Adequate enforcement of policies is also needed. Funding bodies should ask for evidence of the outcomes of their investments to improve accountability. Data on progress of achieving elimination targets should be regularly reported by WHO and other funders but more attention needs to be paid to each country's performance relative to others. Countries need to develop new fiscal spaces to accelerate the elimination of viral hepatitis, which will require innovative means of financing.4 Sponsoring the scale-up of blood testing is a key challenge and sustaining progress will require not only financing but also strong political will and unrelenting advocacy.
In 2015, WHO issued a draft Global Health Sector Strategy on Viral Hepatitis 2016–21, calling on all countries to aim to reach concrete targets towards the elimination of viral hepatitis.404 The policy response to viral hepatitis until now has been inadequate and considerable challenges exist, particularly in low-income and middle-income countries, which bear most of the burden of viral hepatitis (table 3). The Asia-Pacific region experiences a greater challenge from HBV and HCV infection than any other global region, having half of the 20 most heavily burdened countries.427 Countries in the Asia-Pacific with a high burden of viral hepatitis span the economic spectrum and there is a negative correlation between GNI and the prevalence of both HBV and HCV, with a greater burden in low-income countries.4 Countries need to define target screening populations, improve awareness among health-care workers regarding treatment options, subsidise the costs of drugs, and enhance access to them. Emulating Egypt and Georgia in managing HCV could be useful for countries in the Asia-Pacific region.428, 429 Infant HBV vaccination programmes have been implemented by all countries but often fall short of administering birth doses; Taiwan can be a positive example for HBV vaccination. Although policies on mandatory screening of blood and blood products for HBV and HCV are in place in all countries in the Asia-Pacific region (although nucleic-acid amplification testing is not mandatory in all), as are policies on safe injection practices, the lack of strong political commitment and effective regulations in low-to-middle income countries, especially in southeast Asia, limits the outcomes. Reuse of contaminated needles continues to cause outbreaks of hepatitis B and C in southeast Asia.46, 398 Harm reduction strategies targeting people who inject drugs need to be implemented, as has been done in Malaysia using the “Support. Don't punish” philosophy.430 The WHO's Global Health Sector Strategy404 on viral hepatitis called for elimination of viral hepatitis as a major public health threat by 2030 (ie, 90% reduction in incidence and 65% in mortality). Various targets have been proposed to achieve this, including three-dose coverage of hepatitis B vaccination in infancy (90%), receiving a timely birth dose (90%), blood safety (100%), injection safety (unsafe injections target of 0%), harm reduction (target for syringe and needle per person who injects drugs per year of 300), awareness of status of people infected with HBV and HCV (90%), and awareness of the status of infected people who were on HBV treatment or had started HCV treatment (80%). All countries in the Asia-Pacific should work towards achieving these targets in a time-bound manner.
Mortality in the Asia-Pacific region from alcohol-related cirrhosis correlates with per-capita alcohol consumption. Commensurate with an increase in mean incomes, per-capita alcohol consumption has increased in countries of the Asia-Pacific, such as China and India, which will increase their burden of alcohol-related liver disease. Overall, 65% of deaths due to alcohol-related cirrhosis occur in medium-HDI countries and 80% of deaths due to alcohol-related liver cancer occur in high-HDI countries (Figure 8, Figure 9). A systematic review182 reported that DALYs attributable to alcohol use have increased by more than 25% over 1990–2016 globally, driven primarily by increased consumption in south, southeast, and central Asia, in both men and women. The largest increases in exposure have been in countries in the low-middle quintile of the SDI.182 In 2016, alcohol use accounted for 4·0% (3·4–4·6) of age-standardised DALYs in southeast Asia.182 Unlike tobacco or drugs, governments have been discouraged from efforts to limit the availability of alcohol by trade agreements and disputes. Alcohol use is ranked as one of the leading risk factors, surpassing cholesterol, for total DALYs globally since 2010 compared with previous iterations of the GBD Study.182
The increasing burden of alcohol-related liver diseases can be ameliorated through government policies to control consumption and promote less harmful patterns of alcohol use (table 4). Alcohol policies can exist at the global, regional, international, national, or subnational levels. Effective alcohol strategies incorporate a multilevel, multicomponent approach, targeting multiple determinants of drinking and alcohol-related harms, such as availability, price, marketing, and criminalisation of drink-driving. We believe that these policies must be well implemented, enforced, and evaluated to be effective. We recommend that countries should develop their own capacities and set up national monitoring systems to complement national surveys and provide crucial information that allows them to evaluate alcohol policies and track alcohol consumption trends over time. Mongolia is a good example, where the President initiated the Alcohol Free Mongolia programme by advocating drinking a glass of milk instead of alcohol.431 SDG 3 aims to ensure healthy lives and promote wellbeing for all at all ages by 2030, and SDG 3.5 calls for strengthening the prevention and treatment of substance abuse, including narcotic drug use and harmful alcohol consumption. Although it is difficult to control alcohol use, several countries have added additional taxes on alcohol.
The Global Strategy to Reduce the Harmful Use of Alcohol,432 negotiated and agreed by WHO Member States in 2010, represents international consensus that reducing the harmful use of alcohol and its associated health and social burden is a public health priority. The strategy provides guidance for action at all levels, including ten recommended target areas for policy and interventions for national action to reduce the harmful use of alcohol, and the main components for global action to support and complement activities at the country level.165
Given the magnitude and the complexity of the problem of reducing overall alcohol consumption in communities, concerted global and regional efforts must be in place to support countries and communities to reduce their harmful use of alcohol. International coordination and collaboration can create the necessary synergies and provide increased leverage for states to implement evidence-based measures. Local, national, and international monitoring and surveillance frameworks are needed to track the magnitude and trends of alcohol consumption and related harm, as well as monitor policy responses and analyse trends in alcohol consumption and its related disease burden. Such frameworks would be crucial to strengthen advocacy, adjust policy, and programme responses to the trends in alcohol-related harms and assess the effect of interventions. The ultimate goal of monitoring and surveillance is to provide, in a timely manner, relevant and reliable information to policy makers and decision makers for the effective prioritisation, implementation, and evaluation of policy options and interventions to reduce the harmful use of alcohol. WHO's Global Information System on Alcohol and Health serves that purpose and enables these processes.165 The UN's 2011 Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases mandated the development of a global monitoring framework, including indicators, and a set of voluntary global targets for the prevention and control of non-communicable diseases.433 This work yielded one voluntary target related to alcohol use: including at least a 10% relative reduction, as appropriate within the national context, in the harmful use of alcohol by 2025.
Obesity and NAFLD, although traditionally thought of as diseases of high-income countries, are increasingly recognised and have become epidemic in all countries of the Asia-Pacific region, irrespective of income status. Overall, 68% of deaths in Asia-Pacific due to NAFLD-related cirrhosis occur in medium-HDI countries, and 74% of deaths due to NAFLD-related liver cancer occur in high-HDI countries (Figure 8, Figure 9). Changing lifestyles and diet have contributed to the obesity and NAFLD epidemic in the Asia-Pacific. A systematic review and meta-analysis assessing the prevalence, incidence, and outcome of NAFLD disease in Asia found that even in people without obesity, the prevalence of NAFLD was 11·76%.240 A 2018 study suggested that so-called lean patients with NAFLD are more likely to develop progressive liver disease and die from causes related to liver disease than those with obesity-associated NAFLD, indicating that NAFLD is not a benign condition.434 Therefore, when a patient without obesity has abnormal anthropometric and laboratory measurements, and as the environment in Asia-Pacific continues to change, such awareness might become even more prudent.240 The prevalence of NAFLD in the Asia-Pacific is following similar trends to the prevalence reported in high-income countries, indicating that NAFLD is a global disease warranting the attention of primary care physicians, specialists, and health policy makers (panel 2 ). The high frequency of metabolic comorbidities in patients with NAFLD indicates that management of the increasing number of these patients might increase the strain on health systems. Furthermore, many patients with NAFLD develop progressive liver disease, which creates challenges for screening.240
Panel 2. Priority areas of action for liver diseases related to NAFLD in the Asia-Pacific region.
Policy, planning, advocacy, and resource mobilisation (building infrastructure for sound policy and programme development)
National priority actions
-
•
Create an adequate statutory and regulatory environment for prevention and control of obesity and NAFLD
-
•
Advocate and mobilise resources for prevention and control of obesity and NAFLD
-
•
Promote universal health coverage as a means of prevention and control of obesity and NAFLD
-
•
Integrate the prevention and control of obesity and NAFLD into health-planning processes and development plans
-
•
Forge multisectoral partnerships as appropriate, to promote cooperation at all levels among governmental, inter-governmental, and non-governmental organisations, civil society, and the private sector
-
•
Mobilise sustained resources, as appropriate to national context, and in coordination with relevant organisations and ministries
International priority actions
-
•
Facilitate coordination, collaboration, and cooperation among the main stakeholders including national governments, funds, programmes, and agencies of the UN, civil society, and the private sector
-
•
Support national policy makers in their activities (ie, WHO, UN, non-governmental organisations) and provide international support for financing measures (ie, Unitaid, Global Fund, corporate donors)
-
•
Facilitate the mobilisation of adequate, predictable, and sustained financial resources to advance universal coverage in national health systems, especially through primary health care
-
•
Facilitate quality and affordable secondary and tertiary health care, treatment facilities, and social protection mechanisms
Prevention of NAFLD and its modifiable risk factors
National priority actions
-
•
Implement legislative and regulatory measures, as appropriate, and health promotion interventions that engage state and non-state actors from within and outside the health sectors, to prevent physical inactivity, unhealthy diets, and obesity and protect children from the adverse impacts of marketing
-
•
Create supportive environments that promote healthy behaviour through multisectoral action (using incentives and disincentives, regulatory and fiscal measures, laws and other policy options, and health education, as appropriate within the national context), with a special focus on maternal health (including preconception, antenatal and postnatal care, and maternal nutrition), children, adolescents, and young adults, including prevention of childhood obesity
-
•
Develop guidelines, recommendations, or policy measures that engage different relevant sectors, such as food producers and processors and other commercial operators, as well as consumers
-
•
Develop policy measures in cooperation with relevant sectors to promote physical activity through activities of daily living (eg, active transport, recreation, leisure, and sport)
-
•
Strengthen institutional capacity and the workforce through training, appropriately deploy health services, social services, and the community workforce, and strengthen institutional capacity for implementing the national action plan (eg, include prevention and control of obesity and NAFLD in the teaching curricula for medical, nursing, and allied health personnel, and provide training and orientation to personnel in other sectors)
International priority actions
-
•
Provide technical assistance to countries to reduce modifiable risk factors
-
•
Publish and disseminate guidance toolkits on the implementation and evaluation of interventions at the country level (ie, WHO)
Early detection and treatment of NAFLD
National priority actions
-
•
Develop standard procedures for management of NAFLD and NASH and regularly updated guidelines on counselling, support, and care for patients with NAFLD and NASH
-
•
Improve access to care, treatment, and supportive services and integrate them into primary care settings
-
•
Create and evaluate simplified care pathways relevant to local settings and integrate them with existing services
-
•
Decentralise care through capacity building and training
International priority actions
-
•
Support operational research into simplified pathways
-
•
Promote capacity building at the national, regional, and global levels
-
•
Promote the development and dissemination of appropriate, affordable, and sustainable transfer of technology between countries and organisations on mutually agreed terms, particularly regarding intellectual property and licensing
Knowledge and awareness about NAFLD prevention, risk factors, and management
National priority actions
-
•
Increase knowledge about NAFLD and its risk factors in the general population
-
•
Improve and expand knowledge about NAFLD among health workers and carers
-
•
Empower communities and people to take responsibility for their own care
International priority actions
-
•
Support nations in their health-care activities (ie, WHO, industry)
Monitoring progress
National priority actions
-
•
National plans need clearly defined, measurable objectives and new indices of national progress need to be developed
-
•
Periodically assess epidemiological and resource needs (including workforce, institutional, and research capacity) of the health impact of policies in sectors beyond health (eg, agriculture, communication, education, employment, energy, environment, finance, industry and trade, justice, labour, sports, transport, and urban planning)
International priority actions
-
•
Progress of individual countries needs to be monitored
Research on prevention and control of NAFLD
National priority actions
-
•
Monitor the changing epidemiological patterns of NAFLD
-
•
Assess the impact of interventions and assess and develop new tools for prevention, diagnosis, care, and treatment
International priority actions
-
•
Provide support to countries in evaluating and implementing evidence-based options that suit their needs and capacities and in assessing the impact of public policies on health
Various steps need to be taken to promote healthy lifestyles to avoid overweight or obesity by increasing physical activity in schools and offices and regulating the food industry (eg, restricting the marketing of unhealthy foods and sugar-sweetened beverages, increasing taxation on unhealthy foods and beverages, labelling food with nutritional information and health facts, regulating the advertising of unhealthy foods, and promoting healthy foods; table 5). SDG 3.4 calls to reduce premature mortality from non-communicable diseases by a third through prevention and treatment by 2030. The 2011 UN high-level political declaration on non-communicable diseases433 included two voluntary targets potentially related to NAFLD, a 10% relative reduction, as appropriate nationally, in prevalence of insufficient physical activity and halting the increase of diabetes and obesity by 2025. Actions and interventions against NAFLD need to be urgently incorporated into WHO's Global Action Plan on non-communicable diseases,435 including public awareness (under Objective 1 of the Plan); screening for NAFLD; using simple, non-invasive biochemical markers to detect fibrosis in patients with NAFLD; early detection and weight management strategies including lifestyle modifications (dietary and physical activity); and interventions to prevent progression of NAFLD to cirrhosis and hepatocellular carcinoma.
The primary responsibility to prevent and control obesity and NAFLD lies with governments, although the engagement of all sectors of society, international collaboration, and cooperation are essential for success. Effective prevention and control of non-communicable diseases (including NAFLD) require leadership, coordinated multistakeholder engagement, and multisectoral action for health, both at the government level and at actor level. Such efforts would include health-in-all-policies and whole-of-government approaches across sectors such as health, agriculture, communication, education, employment, energy, environment, finance, food, foreign affairs, housing, justice and security, legislature, social welfare, social and economic development, sports, tax and revenue, trade and industry, transport, urban planning, and youth affairs, and partnership with relevant civil society and private sector entities. Opportunities to prevent and control NAFLD and its risk factors occur at multiple stages of life and interventions in early life often offer the best chance for primary prevention. People and communities should be empowered and involved in activities for prevention and control, including advocacy, policy, planning, legislation, service provision, education and training, monitoring, and research and evaluation of the effects of measures for the control and prevention of NAFLD. We believe that prevention is always better than cure; now is the time to push for prevention of NAFLD before its burden becomes overwhelming.
Other aspects that need urgent attention are inadequate infrastructure and facilities for liver transplantation and health-care personnel poorly trained in the management of liver diseases, including preventive aspects, especially in low-and-middle-income countries. The focus must be on early detection of liver diseases with timely referral and access to appropriate care by trained multidisciplinary teams. In this regard, SDG 3.9c calls to substantially increase health financing and the recruitment, development, training, and retention of the health workforce in developing countries.
Access to health insurance, affordable health care, and affordable essential medicines are also important issues in low-and-middle-income countries in the Asia-Pacific. SDG 3.8 aims to achieve universal health coverage, including protection from financial risk, access to good-quality, essential health-care services, and access to safe, effective, good-quality, and affordable essential medicines and vaccines for all by 2030. SDG 3.9b calls for the provision of access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS agreement and public health,436 which affirms the right of developing countries to fully use the provisions of the TRIPS agreement to provide access to medicines for all by 2030. To this end, health-financing systems should not only seek to raise sufficient funds for health provision but should also do so in a way that allows people to use services without risk of severe financial hardship or impoverishment.437 Three interrelated areas could bring health financing closer to universal health coverage: raising funds for health, reducing financial barriers to health-care access through prepayment and subsequent pooling of funds instead of direct out-of-pocket payments, and allocating or using funds in a way that promotes efficiency and equity. Public health systems and public–private partnerships need to be strengthened to face the challenges that an increasing burden of liver diseases could create, and measuring progress is an inherent part of any prevention and treatment strategy. We suggest a set of metrics to monitor the implementation of the various aspects of such a strategy (table 6 ).
Table 6.
Suggested metrics by target area to improve prevention, treatment, and care for patients with liver diseases in the Asia-Pacific region
| Metrics | |
|---|---|
| Viral hepatitis | |
| Improve coverage of hepatitis B immunisation, including a timely birth dose | Hepatitis B birth-dose vaccination (% coverage); three-dose hepatitis B vaccine for infants (% coverage); three-dose hepatitis B vaccine for health-care workers and other high-risk populations (% coverage) |
| Improve blood and injection safety | Blood donations screened with high-quality nucleic acid tests (% coverage); use safely engineered syringes and injection devices (% coverage) |
| Harm reduction for intravenous drug users | Number of sterile syringe or needle sets distributed per person per year for people who inject drugs |
| Improvements in sanitation and water quality | Households with an improved drinking water source (% coverage); households using improved sanitation facilities (% coverage) |
| Screening of high-risk groups for HBV and HCV in primary care settings | Proportion of patients in primary care who have been assessed for risk factors of HBV and HCV (% coverage); proportion of patients at high risk for HBV and HCV who have been tested (% coverage) |
| Increase the proportion of patients with chronic hepatitis B and C who have been diagnosed | Estimated proportion of patients with chronic hepatitis B and C who have not been diagnosed (% coverage) |
| Increase access to appropriate management and care for patients with chronic hepatitis B and C | Proportion of patients with chronic hepatitis B and C eligible for treatment with antiviral drugs (% coverage) |
| Monitor mortality related to acute and chronic hepatitis infections | Incidence of acute hepatitis A and E; mortality related to acute hepatitis A and E; incidence of acute hepatitis B and C; mortality related to acute hepatitis B and C; incidence of chronic HBV and HCV infections; mortality related to chronic HBV and HCV infection |
| Monitor morbidity related to chronic hepatitis infections | Number of patients with cirrhosis or hepatocellular carcinoma associated with HCV or HBV; number of liver transplantations for HCV or HBV; HBsAg prevalence in children younger than 5 years |
| Alcohol-related liver disease | |
| Reduce alcohol intake and ameliorate risky alcohol-related behaviours | Total (recorded and unrecorded) alcohol consumed per capita (ages ≥15 years) within a calendar year in L of pure alcohol; age-standardised prevalence of heavy episodic drinking in adolescents and adults |
| Early detection and treatment of alcoholic liver diseases | Proportion of adult patients in primary care who have had a measure of alcohol consumption or risk in the preceding year |
| Reduce the burden of liver diseases attributed to alcohol use | Alcohol-related morbidity and mortality in adolescents and adults; mortality related to alcohol-attributable cirrhosis; number of patients with alcohol-related cirrhosis or hepatocellular carcinoma; number of liver transplantations for alcohol-related liver disease |
| NAFLD | |
| Promoting physical activity | Prevalence of insufficient physically activity in adolescents (defined as <60 min of moderate to vigorous activity daily); age-standardised prevalence of insufficiently physical activity in people aged ≥18 years (defined as <150 min of moderate-intensity activity per week, or equivalent); per-capita travel (km per day) |
| Promoting healthy food consumption | Sugar consumption per capita (g per day); age-standardised mean proportion of total energy intake from saturated fat in people aged ≥18 years; age-standardised prevalence of people aged ≥18 years; consuming less than five total servings (400 g) of fruit and vegetables per day |
| Stopping the increase in diabetes, hyperlipidaemia, and obesity | Age-standardised prevalence of increased blood glucose or diabetes in children, adolescents, and adults; prevalence of overweight and obesity in children, adolescents, and adults; age-standardised prevalence of increased total cholesterol in children, adolescents, and adults |
| Early detection and treatment of NAFLD | Proportion of adult patients in primary care who have had their body-mass index recorded in the preceding year; prevalence of NAFLD or non-alcoholic steatohepatitis in patients in secondary care |
| Reducing the burden of liver disease attributed NAFLD | Number of patients with cirrhosis or hepatocellular carcinoma associated with NAFLD; number of liver transplantations for NAFLD |
| All liver diseases | |
| Increased facilities and expertise for diagnosis, treatment, and care of patients with liver disease | Proportion of secondary and tertiary care hospitals with a doctor trained in liver diseases; proportion of secondary care hospitals with 24 h endoscopy facilities; survival of hospital inpatients with liver disease by cause of admission |
| Improved access to liver transplantation facilities | Organ donations per million people per year; waiting time for liver transplants from deceased donors by blood group; proportion of liver transplants from living donors; proportion of publicly funded tertiary care hospitals equipped for liver transplantations |
| Increasing awareness of liver disease in the general population and governments | Existence of Government-supported national liver plans; existence of public health-sponsored public awareness campaigns (number per year); number of patient support groups and non-governmental organisations involved |
| Research into epidemiology, risk factors, prevention, and control of liver diseases | Number of research papers published on liver diseases in local journals per country; proportion of research papers published on liver disease in global journals per country |
Implementation of the recommendations of this Commission will depend less on technical capabilities and more on leadership and political will. Nevertheless, even when there is strong leadership and political will, the availability of finances, application of funds, and health-system capabilities will determine the magnitude and speed of the response. At the country level, public financing for health (as for any sector) is determined by the fiscal space available to the government. The fiscal space depends on the sources of finance available from improved economic growth that creates favourable macroeconomic conditions, such as revenues generated from new taxation or strengthened tax administration, borrowing from domestic and international sources, reprioritisation of health within the existing government budget, more effective and efficient allocation of available health resources, and innovative domestic and international financing.438
The high-level Taskforce on Innovative International Financing for Health Systems was set up in 2008.439 It recommended the creation of a common funding platform to strengthen health systems across the three global-scale innovative financing mechanisms—ie, the Global Fund, Gavi, and the World Bank. These innovative financing mechanisms link different elements of the financing value chain to mobilise funding from multiple sources (eg, governments, foundations, and the private sector), pool finances, and channel and allocate funds to health programmes through organisations and governments in low-income and middle-income countries. Outsourcing of services, such as diagnostic tests or management systems for health-care data, to non-government providers and encouraging the use of advanced market commitments (eg, vaccine purchases) can also be used to secure investment in health-care services from the private sector.439 The opportunity to link revenue generation to a global redistributive and environmental agenda should be sought via taxes on carbon, luxury items, or capital flow, and leveraging an increased domestic return on the natural resources and primary commodities of poor countries.440 Other financing mechanisms including global health bonds, debt-conversion instruments, market commitment instruments, social and development impact bonds, and global solidarity taxes and levies need to be invoked. Opportunity can be seized in the current political momentum within the G20 countries that is in favour of increased levies on currency transactions and additional financial transaction taxes that could be used to regulate the global financial system.440
The agenda of expanding the domestic resource base of low-income countries is also important for generating finances for health-care programmes. Many low-income countries could increase domestic public finance by reducing capital flight, promoting more effective tax policy, and improving their tax collection systems. Such an agenda would have the added benefit of focusing attention on the broad challenges of economic development and improving democratic and accountable governance. High-income countries should adhere to their responsibility to allocate 0·7% of their GNI to development aid. Principles and mechanisms need to be established for a systematic transfer of resources from high-income to low-income countries.440
There are some limitations to our analysis. First is the paucity and patchiness of data on liver diseases in the Asia-Pacific region. We did not include any countries with low HDI and thus our analysis is not wholly representative. Second, the tools for collecting, analysing, and reporting data in different countries are not homogenous. Therefore, it is possible that there are additional demands and concerns about staffing and financing needs and the requirements and timelines to reduce the burden of liver diseases. Despite these limitations, the Commission defines the unmet gaps and lays the foundation for collective thinking to eliminate viral hepatitis and control other liver disaeses, including NAFLD and alcohol-related disease, in the countries of the Asia-Pacific region.
In summary, this Commission provides an insight into the burden of liver diseases in the Asia-Pacific region and identifies potential causes of change in their underlying epidemiology and aetiology. Although viral hepatitis (both acute and chronic) is still a major cause of morbidity and mortality related to liver diseases in the Asia-Pacific region, efforts towards its elimination as a public health threat by 2030 should reduce this burden. Nevertheless, mortality from alcohol-related liver diseases remains high in mostly non-Muslim countries, especially China and India, and is expected to increase. Similarly, obesity and NAFLD-related liver diseases are common in all countries, irrespective of HDI, and are also expected to increase. We hope that the Commission provides an opportunity for countries to learn from each other to tackle the changing landscape of the burden of liver disease in the Asia-Pacific region and to achieve the targets set by the Sustainable Development Goals.
For e-Stat see https://www.e-stat.go.jp/en
This online publication has been corrected. The corrected version first appeared at thelancet.com/gastrohep on Feb 12, 2020
Acknowledgments
Acknowledgments
DHM thanks Pretty Multiharina Sasono, Wiendra Waworuntu, Naning Nugrahini, Sedya Dwisangka, and all staff of Sub-directorate of Hepatitis and Gastrointestinal Infection, Directorate General of Communicable Diseases, Ministry of Health, Indonesia, for providing data and discussions. SGL thanks Benjamin Ong, for reviewing the manuscript. ME and JG are supported by the Robert W Storr bequest to the Sydney Medical Foundation (University of Sydney, Sydney, Australia) and National Health and Medical Research Council of Australia (NHMRC) programme grant (1053206) and project grants (APP1107178 and APP1108422). MK and SKS thank Guresh Kumar (Institute of Liver and Biliary Sciences, New Delhi, India) for help in statistical analysis and figures.
Editorial note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contributors
SKS, MK, and RA wrote the sections on India. ME and JG wrote the sections on Australia and New Zealand. MAM and SMFA wrote the sections on Bangladesh. JJ and QT wrote the sections on China. DHM wrote the sections on Indonesia. MO and YO wrote the sections on Japan. K-HH and HWL wrote the sections on South Korea. WJ and ASB wrote the sections on Pakistan. CHC and SGL wrote the sections on Singapore. R-FP and D-SC wrote the sections on Taiwan. The Discussion and Introduction were written by SKS and MK.
Declaration of interests
MO reports grants from Bayer, Sumitomo Dainippon Pharma, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, EA Pharma, Eisai, Bristol-Myers Squibb, Japan Bio Products, Ono Pharmaceutical, Boehringer Ingelheim, GE Healthcare Japan, and Medtronic, outside the submitted work. SGL reports grants, personal fees, honorariums for advisory board membership, and speakers' fees from Gilead Sciences, Merck, Abbott Diagnostics, and Roche; personal fees, honorariums for advisory board membership, and speakers' fees from AbbVie and Spring Bank Pharmaceuticals; and personal fees from Dicerna Pharmaceuticals, outside the submitted work. All other authors declare no competing interests.
Supplementary Material
References
- 1.WHO Global Health Estimates 2015: deaths by cause, age, sex, by country and by region, 2000–2015. 2016. https://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000_2015/en/
- 2.World Bank Country profiles. 2017. https://datacatalog.worldbank.org/dataset/country-profiles
- 3.Ministry of Health Singapore Communicable diseases surveillance in Singapore 2016. 2017. https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/full-version.pdf
- 4.Cooke GS, Andrieux-Meyer I, Applegate TL. Accelerating the elimination of viral hepatitis: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol. 2019;4:135–184. doi: 10.1016/S2468-1253(18)30270-X. [DOI] [PubMed] [Google Scholar]
- 5.Shan S, Cui F, Jia J. How to control highly endemic hepatitis B in Asia. Liver Int. 2018;38(suppl 1):122–125. doi: 10.1111/liv.13625. [DOI] [PubMed] [Google Scholar]
- 6.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015;386:1546–1555. doi: 10.1016/S0140-6736(15)61412-X. [DOI] [PubMed] [Google Scholar]
- 7.Polaris Observatory Collaborators Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3:383–403. doi: 10.1016/S2468-1253(18)30056-6. [DOI] [PubMed] [Google Scholar]
- 8.Cui Y, Jia J. Update on epidemiology of hepatitis B and C in China. J Gastroenterol Hepatol. 2013;28(suppl 1):7–10. doi: 10.1111/jgh.12220. [DOI] [PubMed] [Google Scholar]
- 9.Cui F, Shen L, Li L. Prevention of chronic hepatitis B after 3 decades of escalating vaccination policy, China. Emerg Infect Dis. 2017;23:765–772. doi: 10.3201/eid2305.161477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang S, Ma Q, Liang S. Annual economic burden of hepatitis B virus-related diseases among hospitalized patients in twelve cities in China. J Viral Hepat. 2016;23:202–210. doi: 10.1111/jvh.12482. [DOI] [PubMed] [Google Scholar]
- 11.Qin Q, Smith MK, Wang L. Hepatitis C virus infection in China: an emerging public health issue. J Viral Hepat. 2015;22:238–244. doi: 10.1111/jvh.12295. [DOI] [PubMed] [Google Scholar]
- 12.Sun M, Xu N, Li C. The public health emergency management system in China: trends from 2002 to 2012. BMC Public Health. 2018;18:474–482. doi: 10.1186/s12889-018-5284-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu E, Yang M, Rao H. Temporal changes in the modes of hepatitis C virus transmission in the USA and northern China. Dig Dis Sci. 2017;62:2141–2149. doi: 10.1007/s10620-017-4619-6. [DOI] [PubMed] [Google Scholar]
- 14.Piao H-X, Yang A-T, Sun Y-M. Increasing newly diagnosed rate and changing risk factors of HCV in Yanbian Prefecture, a high endemic area in China. PLoS One. 2014;9 doi: 10.1371/journal.pone.0086190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lei JH, Liang J, Gong X, Xiao XQ, Chen Z, Peng F. Analysis of transmission routes of hepatitis C virus based on virus genotyping in 341 cases with different suspected initial infection time points in Hunan Province, China. Med Sci Monit. 2018;24:5232–5241. doi: 10.12659/MSM.907424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Islami F, Dikshit R, Mallath MK, Jemal A. Primary liver cancer deaths and related years of life lost attributable to hepatitis B and C viruses in India. Cancer Epidemiol. 2016;40:79–86. doi: 10.1016/j.canep.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Puri P. Tackling the hepatitis B disease burden in India. J Clin Exp Hepatol. 2014;4:312–319. doi: 10.1016/j.jceh.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thyagarajan SP, Jayaram S, Mohanavalli B. Prevalence of HBV in general population of India. In: Sarin SK, Singal AK, editors. Hepatitis B in India: prevention and management. CBS Publishers and Distributors; New Delhi: 2005. pp. 5–16. [Google Scholar]
- 20.Batham A, Narula D, Toteja T, Sreenivas V, Puliyel JM. Sytematic review and meta-analysis of prevalence of hepatitis B in India. Indian Pediatr. 2007;44:663–674. [PubMed] [Google Scholar]
- 21.Batham A, Gupta MA, Rastogi P, Garg S, Sreenivas V, Puliyel JM. Calculating prevalence of hepatitis B in India: using population weights to look for publication bias in conventional meta-analysis. Indian J Pediatr. 2009;76:1247–1257. doi: 10.1007/s12098-009-0246-3. [DOI] [PubMed] [Google Scholar]
- 22.Gupta S, Gupta R, Joshi YK, Singh S. Role of horizontal transmission in hepatitis B virus spread among household contacts in north India. Intervirology. 2008;51:7–13. doi: 10.1159/000118790. [DOI] [PubMed] [Google Scholar]
- 23.Pande C, Sarin SK, Patra S. Prevalence, risk factors and virological profile of chronic hepatitis B virus infection in pregnant women in India. J Med Virol. 2011;83:962–967. doi: 10.1002/jmv.22017. [DOI] [PubMed] [Google Scholar]
- 24.Jat SL, Gupta N, Kumar T. Prevalence of hepatitis D virus infection among hepatitis B virus-infected individuals in India. Indian J Gastroenterol. 2015;34:164–168. doi: 10.1007/s12664-015-0555-6. [DOI] [PubMed] [Google Scholar]
- 25.Puri P, Anand AC, Saraswat VA. Consensus statement of HCV Task Force of the Indian National Association for Study of the Liver (INASL). Part I: status report of HCV infection in India. J Clin Exp Hepatol. 2014;4:106–116. doi: 10.1016/j.jceh.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chowdhury A, Santra A, Chaudhuri S. Hepatitis C virus infection in the general population: a community-based study in west Bengal, India. Hepatology. 2003;37:802–809. doi: 10.1053/jhep.2003.50157. [DOI] [PubMed] [Google Scholar]
- 27.Singh M, Kotwal A, Gupta RM, Adhya S, Chatterjee K, Jayaram J. Sero-epidemiological and behavioural survey of HIV, HBV and HCV amongst Indian Armed Forces trainees. Med J Armed Forces India. 2010;66:50–54. doi: 10.1016/S0377-1237(10)80093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sood A, Sarin SK, Midha V. Prevalence of hepatitis C virus in a selected geographical area of northern India: a population based survey. Indian J Gastroenterol. 2012;31:232–236. doi: 10.1007/s12664-012-0251-8. [DOI] [PubMed] [Google Scholar]
- 29.Dhiman RK, Satsangi S, Grover GS, Puri P. Tackling the hepatitis C disease burden in Punjab, India. J Clin Exp Hepatol. 2016;6:224–232. doi: 10.1016/j.jceh.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solomon SS, Mehta SH, Srikrishnan AK. Burden of hepatitis C virus disease and access to hepatitis C virus services in people who inject drugs in India: a cross-sectional study. Lancet Infect Dis. 2015;15:36–45. doi: 10.1016/S1473-3099(14)71045-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muljono DH. Epidemiology of hepatitis B and C in Republic of Indonesia. Euroasian J Hepatogastroenterol. 2017;7:55–59. doi: 10.5005/jp-journals-l0018-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ministry of Health of the Republic of Indonesia Indonesia health profile 2016. 2016. http://ghdx.healthdata.org/record/indonesia-health-profile-2016
- 33.IndexMundi Indonesia demographics profile 2018. 2018. https://www.indexmundi.com/indonesia/demographics_profile.html
- 34.WHO Indonesia. 2015. http://www.who.int/countries/idn/en/
- 35.Purwono PB, Juniastuti, Amin M. Hepatitis B virus infection in Indonesia 15 years after adoption of a universal infant vaccination program: possible impacts of low birth dose coverage and a vaccine-escape mutant. Am J Trop Med Hyg. 2016;95:674–679. doi: 10.4269/ajtmh.15-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scrutton J, Wallace J, Wait S. Situation analysis of viral hepatitis in Indonesia: a policy report. 2018. http://www.healthpolicypartnership.com/wp-content/uploads/hepatitis/Situation_analysis_of_viral_hepatitis_in_Indonesia.pdf
- 37.Wijayadi T, Sjahril R, Turyadi Seroepidemiology of HBV infection among health-care workers in south Sulawesi, Indonesia. BMC Infect Dis. 2018;18:279. doi: 10.1186/s12879-018-3190-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agency for Health Research and Development (Indonesia) Indonesia Basic Health Research 2007–2008. http://ghdx.healthdata.org/record/indonesia-basic-health-research-2007-2008
- 39.Agency for Health Research and Development (Indonesia) Indonesia Basic Health Research. 2013. http://ghdx.healthdata.org/record/indonesia-basic-health-research-2013
- 40.Butt AS, Abbas Z, Jafri W. Hepatocellular carcinoma in Pakistan: where do we stand? Hepat Mon. 2012;12 doi: 10.5812/hepatmon.6023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Butt AS, Hamid S, Wadalawala AA. Hepatocellular carcinoma in native South Asian Pakistani population; trends, clinico-pathological characteristics & differences in viral marker negative & viral-hepatocellular carcinoma. BMC Res Notes. 2013;6:137–150. doi: 10.1186/1756-0500-6-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bosan A, Qureshi H, Bile KM, Ahmad I, Hafiz R. A review of hepatitis viral infections in Pakistan. J Pak Med Assoc. 2010;60:1045–1058. [PubMed] [Google Scholar]
- 43.Pervaiz A, Sipra FS, Rana TH, Qadeer I. Pre-donation screening of volunteer prisoner blood donors for hepatitis B and C in prisons of Punjab, Pakistan. J Ayub Med Coll Abbottabad. 2015;27:794–797. [PubMed] [Google Scholar]
- 44.Butt A, Jafri W, Janjua N, Pasha O. Seroprevalence and risk factors for hepatitis C infection among male prisoners in Karachi, Pakistan. Am J Gastroenterol. 2010;105:S112. [Google Scholar]
- 45.Qureshi H, Bile KM, Jooma R, Alam SE, Afridi HU. Prevalence of hepatitis B and C viral infections in Pakistan: findings of a national survey appealing for effective prevention and control measures. East Mediterr Health J. 2010;16(suppl):S15–S23. [PubMed] [Google Scholar]
- 46.Ahmed B, Ali T, Qureshi H, Hamid S. Population-attributable estimates for risk factors associated with hepatitis B and C: policy implications for Pakistan and other South Asian countries. Hepatol Int. 2013;7:500–507. doi: 10.1007/s12072-012-9417-9. [DOI] [PubMed] [Google Scholar]
- 47.Tanaka J, Koyama T, Mizui M. Total numbers of undiagnosed carriers of hepatitis C and B viruses in Japan estimated by age- and area-specific prevalence on the national scale. Intervirology. 2011;54:185–195. doi: 10.1159/000324525. [DOI] [PubMed] [Google Scholar]
- 48.National Institute of Infectious Diseases Acute hepatitis B, April 2006–December 2015. Inf Agent Surveill Rep. 2016;37:147–148. [Google Scholar]
- 49.August 2016 Infectious Agents Surveillance Report (IASR) 2016. https://www0.niid.go.jp/niid/idsc/iasr/37/438e.pdf
- 50.Okuda K, Ohtsuki T, Obata h. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer. 1985;56:918–928. doi: 10.1002/1097-0142(19850815)56:4<918::aid-cncr2820560437>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 51.Kudo M. Management of hepatocellular carcinoma in Japan as a world-leading model. Liver Cancer. 2018;7:134–147. doi: 10.1159/000484619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ikegami N, Yoo BK, Hashimoto H. Japanese universal health coverage: evolution, achievements, and challenges. Lancet. 2011;378:1106–1115. doi: 10.1016/S0140-6736(11)60828-3. [DOI] [PubMed] [Google Scholar]
- 53.Blaxell V. Yellow blood: hepatitis C and the modernist settlement in Japan. Asia Pac J. 2014;12:1–19. [Google Scholar]
- 54.Japanese Red Cross Society Haemovigilance by JRCS 2008. 2011. http://www.jrc.or.jp/mr/english/pdf/anzen_HVreport2008_en.pdf
- 55.Shiraki K. Vertical transmission of hepatitis B virus and its prevention in Japan. In: Nishioka K, Suzuki H, Mishiro S, Oda T, editors. Viral hepatitis and liver disease. Springer; Tokyo: 1994. [Google Scholar]
- 56.Afroz S, Mahtab MA, Rahman S, Khan M. Hepatitis B virus is the leading cause of cirrhosis of liver in Bangladesh. Hepatol Int. 2007;1(suppl 1):120. [Google Scholar]
- 57.Mahtab MA, Rahman S, Khan M, Ahmed F, Podder PK. Aetiology of SOL of liver in Bangladesh. Indian J Gastroenterol. 2007;26(suppl 2):76. [Google Scholar]
- 58.Mahtab MA, Rahman S, Karim MF. Epidemiology of hepatitis B virus in Bangladeshi general population. Hepatobiliary Pancreat Dis Int. 2008;7:595–600. [PubMed] [Google Scholar]
- 59.Ashraf H, Alam NH, Rothermundt C. Prevalence and risk factors of hepatitis B and C virus infections in an impoverished urban community in Dhaka, Bangladesh. BMC Infect Dis. 2010;10:208–216. doi: 10.1186/1471-2334-10-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Islam MN, Islam KM, Islam N. Hepatitis-B virus infection in Dhaka, Bangladesh. Bangladesh Med Res Counc Bull. 1984;10:1–6. [PubMed] [Google Scholar]
- 61.Mamun-Al-Mahtab, Akbar SM, Uddin H, Khan SI, Rahman S. Early termination of immune tolerance state of hepatitis B virus infection explains liver damage. World J Hepatol. 2014;6:621–625. doi: 10.4254/wjh.v6.i8.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mamun-Al-Mahtab, Karim F, Foster G, Akbar SMF, Rahman S. Prevalence and risk factors of asymptomatic HCV infection in Bangladesh. J Clin Exp Hepatol. 2011;1:13–16. doi: 10.1016/S0973-6883(11)60111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan SI, Reza MM, Crowe SM. People who inject drugs in Bangladesh–the untold burden! Int J Infect Dis. 2019;83:109–115. doi: 10.1016/j.ijid.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 64.Kim BK, Revill PA, Ahn SH. HBV genotypes: relevance to natural history, pathogenesis and treatment of chronic hepatitis B. Antivir Ther. 2011;16:1169–1186. doi: 10.3851/IMP1982. [DOI] [PubMed] [Google Scholar]
- 65.Park NH, Chung YH, Lee HS. Impacts of vaccination on hepatitis B viral infections in Korea over a 25-year period. Intervirology. 2010;53:20–28. doi: 10.1159/000252780. [DOI] [PubMed] [Google Scholar]
- 66.Cho EJ, Kim SE, Suk KT. Current status and strategies for hepatitis B control in Korea. Clin Mol Hepatol. 2017;23:205–211. doi: 10.3350/cmh.2017.0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee SS, Byoun YS, Jeong SH. Type and cause of liver disease in Korea: single-center experience, 2005–2010. Clin Mol Hepatol. 2012;18:309–315. doi: 10.3350/cmh.2012.18.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim DY, Kim IH, Jeong SH. A nationwide seroepidemiology of hepatitis C virus infection in South Korea. Liver Int. 2013;33:586–594. doi: 10.1111/liv.12108. [DOI] [PubMed] [Google Scholar]
- 69.Kim JY, Cho J, Hwang SH. Behavioral and healthcare-associated risk factors for chronic hepatitis C virus infection in Korea. J Korean Med Sci. 2012;27:1371–1377. doi: 10.3346/jkms.2012.27.11.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seong MH, Kil H, Kim YS. Clinical and epidemiological features of hepatitis C virus infection in South Korea: a prospective, multicenter cohort study. J Med Virol. 2013;85:1724–1733. doi: 10.1002/jmv.23661. [DOI] [PubMed] [Google Scholar]
- 71.National Centre for Immunisation Research and Surveillance History of immunisation in Australia. http://ncirs.org.au/health-professionals/history-immunisation-australia
- 72.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra: 2017. Cancer in Australia 2017. [Google Scholar]
- 73.Wan X, Mathews JD. Primary hepatocellular carcinoma in aboriginal Australians. Aust J Public Health. 1994;18:286–290. doi: 10.1111/j.1753-6405.1994.tb00246.x. [DOI] [PubMed] [Google Scholar]
- 74.Waziry R, Grebely J, Amin J. Trends in hepatocellular carcinoma among people with HBV or HCV notification in Australia (2000–2014) J Hepatol. 2016;65:1086–1093. doi: 10.1016/j.jhep.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 75.Kalisch DW. Australian Bureau of Statistics; Canberra: 2015. National Health Survey first results Australia 2014–15 4364.0.55.001. [Google Scholar]
- 76.McGregor S, McManus H, Gray R, Costello J. HIV, viral hepatitis and sexually transmitted infections in Australia: Annual surveillance report 2015. 2015. https://kirby.unsw.edu.au/sites/default/files/kirby/report/SERP_2015-Annual-Surveillance-Report.pdf
- 77.Butler JKR, Watson K, Watson A. Australian Centre for Economic Research on Health; Canberra: 2009. The impact of chronic hepatitis B in Australia: projecting mortality, morbidity and economic impact. [Google Scholar]
- 78.Graham S, Guy RJ, Cowie B. Chronic hepatitis B prevalence among Aboriginal and Torres Strait Islander Australians since universal vaccination: a systematic review and meta-analysis. BMC Infect Dis. 2013;13:403–413. doi: 10.1186/1471-2334-13-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.MacLachlan JH, Allard N, Towell V, Cowie BC. The burden of chronic hepatitis B virus infection in Australia, 2011. Aust N Z J Public Health. 2013;37:416–422. doi: 10.1111/1753-6405.12049. [DOI] [PubMed] [Google Scholar]
- 80.Ministerial Advisory Committee on AIDS. Sexual Health and Hepatitis. Hepatitis C Sub-Committee . Australian Government Department of Health and Ageing; Canberra: 2006. Hepatitis C Virus Projections Working Group: estimates and projections of the Hepatitis C virus epidemic in Australia. [Google Scholar]
- 81.The Gastroenterological Society of Australia/Australian Liver Association The economic cost and health burden of liver diseases in Australia. 2012. https://static1.squarespace.com/static/50ff0804e4b007d5a9abe0a5/t/53321aaee4b09f967eb0c7e5/1395792558684/gesa2013_revised%5B1%5D.pdf
- 82.Degenhardt L, Day C, Gilmour S, Hall W. The “lessons” of the Australian “heroin shortage”. Subst Abuse Treat Prev Policy. 2006;1:11–18. doi: 10.1186/1747-597X-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.The Kirby Insitute . The Kirby Institute and UNSW Australia; Sydney: 2015. Main findings, bloodborne viral and sexually transmitted infections in Aboriginal and Torres Strait Islander People: surveillance and evaluation report. [Google Scholar]
- 84.Vermunt J, Fraser M, Herbison P, Wiles A, Schlup M, Schultz M. Prevalence and knowledge of hepatitis C in a middle-aged population, Dunedin, New Zealand. World J Gastroenterol. 2015;21:10224–10233. doi: 10.3748/wjg.v21.i35.10224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Petousis-Harris H, Reynolds G, Poole T, Nowlan M. 2012 antigen review for the New Zealand National Immunisation Schedule: hepatitis B. 2015. http://ebooks.fmhs.auckland.ac.nz/2012-antigen-review-hepatitisb/
- 86.Ministry of Health . Ministry of Health; Wellington: 2012. Cancer: new registrations and deaths 2009. [Google Scholar]
- 87.Ministry of Health . Ministry of Health; Wellington: 2015. Cancer: new registrations and deaths 2012. [Google Scholar]
- 88.Blakely T, Bates M, Garrett N, Robson B. The incidence of hepatocellular carcinoma in New Zealand. N Z Med J. 1998;111:471–474. [PubMed] [Google Scholar]
- 89.Chamberlain J, Sarfati D, Cunningham R, Koea J, Gurney J, Blakely T. Incidence and management of hepatocellular carcinoma among Māori and non-Māori New Zealanders. Aust N Z J Public Health. 2013;37:520–526. doi: 10.1111/1753-6405.12108. [DOI] [PubMed] [Google Scholar]
- 90.Epidemiology & Disease Control Division . Ministry of Health; Singapore: 2014. Singapore Burden of Disease Study 2010. [Google Scholar]
- 91.Chang PE, Wong GW, Li JW, Lui HF, Chow WC, Tan CK. Epidemiology and clinical evolution of liver cirrhosis in Singapore. Ann Acad Med Singapore. 2015;44:218–225. [PubMed] [Google Scholar]
- 92.Lee HP, Chew L, Yew CK. National Registry of Diseases Office; Singapore: 2015. Singapore Cancer Registry Interim Annual Report: trends in cancer incidence in Singapore 2010–2014. [Google Scholar]
- 93.Ministry of Health Singapore The burden of disease in Singapore, 1990–2017: an overview of the Global Burden of Disease Study 2017 results. 2019. http://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Singapore_Report.pdf
- 94.Ang SF, Ng ES, Li H. The Singapore Liver Cancer Recurrence (SLICER) Score for relapse prediction in patients with surgically resected hepatocellular carcinoma. PLoS One. 2015;10 doi: 10.1371/journal.pone.0118658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ang LW, Cutter J, James L, Goh KT. Seroepidemiology of hepatitis B virus infection among adults in Singapore: a 12-year review. Vaccine. 2013;32:103–110. doi: 10.1016/j.vaccine.2013.10.057. [DOI] [PubMed] [Google Scholar]
- 96.Lim SG. Time for action on viral hepatitis. Ann Acad Med Singapore. 2016;45:27–30. [PubMed] [Google Scholar]
- 97.Phyo WW, Lim SG, Lee YW. Cross-sectional study on risk factors associated with hepatitis C (HCV) infection. 26th Annual Conference of APASL; Shanghai, China; Feb 15–19, 2017 (abstr PP1864).
- 98.Winslow M, Subramaniam M, Ng WL, Lee A, Song G, Chan YH. Seroprevalence of hepatitis C in intravenous opioid users presenting in the early phase of injecting drug use in Singapore. Singapore Med J. 2007;48:504–508. [PubMed] [Google Scholar]
- 99.Chen DS. Fighting against viral hepatitis: lessons from Taiwan. Hepatology54: 381–92. [DOI] [PubMed]
- 100.Chiang CJ, Yang YW, You SL, Lai MS, Chen CJ. Thirty-year outcomes of the national hepatitis B immunization program in Taiwan. JAMA. 2013;310:974–976. doi: 10.1001/jama.2013.276701. [DOI] [PubMed] [Google Scholar]
- 101.Chen DS, Hsu NH, Sung JL. A mass vaccination program in Taiwan against hepatitis B virus infection in infants of hepatitis B surface antigen-carrier mothers. JAMA. 1987;257:2597–2603. [PubMed] [Google Scholar]
- 102.Chien YC, Jan CF, Kuo HS, Chen CJ. Nationwide hepatitis B vaccination program in Taiwan: effectiveness in the 20 years after it was launched. Epidemiol Rev. 2006;28:126–135. doi: 10.1093/epirev/mxj010. [DOI] [PubMed] [Google Scholar]
- 103.Ni YH, Chang MH, Jan CF. Continuing decrease in hepatitis B virus infection 30 years after initiation of infant vaccination program in Taiwan. Clin Gastroenterol Hepatol. 2016;14:1324–1330. doi: 10.1016/j.cgh.2016.04.030. [DOI] [PubMed] [Google Scholar]
- 104.Chen CL, Yang JY, Lin SF. Slow decline of hepatitis B burden in general population: results from a population-based survey and longitudinal follow-up study in Taiwan. J Hepatol. 2015;63:354–363. doi: 10.1016/j.jhep.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 105.Chen CH, Yang PM, Huang GT, Lee HS, Sung JL, Sheu JC. Estimation of seroprevalence of hepatitis B virus and hepatitis C virus in Taiwan from a large-scale survey of free hepatitis screening participants. J Formos Med Assoc. 2007;106:148–155. doi: 10.1016/S0929-6646(09)60231-X. [DOI] [PubMed] [Google Scholar]
- 106.Chang MH, You SL, Chen CJ. Long-term effects of hepatitis B immunization of infants in preventing liver cancer. Gastroenterology. 2016;151:472–480.e1. doi: 10.1053/j.gastro.2016.05.048. [DOI] [PubMed] [Google Scholar]
- 107.Su WJ, Liu CC, Liu DP. Effect of age on the incidence of acute hepatitis B after 25 years of a universal newborn hepatitis B immunization program in Taiwan. J Infect Dis. 2012;205:757–762. doi: 10.1093/infdis/jir852. [DOI] [PubMed] [Google Scholar]
- 108.Chen HL, Chang CJ, Kong MS. Pediatric fulminant hepatic failure in endemic areas of hepatitis B infection: 15 years after universal hepatitis B vaccination. Hepatology. 2004;39:58–63. doi: 10.1002/hep.20006. [DOI] [PubMed] [Google Scholar]
- 109.Chen DS, Kuo GC, Sung JL. Hepatitis C virus infection in an area hyperendemic for hepatitis B and chronic liver disease: the Taiwan experience. J Infect Dis. 1990;162:817–822. doi: 10.1093/infdis/162.4.817. [DOI] [PubMed] [Google Scholar]
- 110.Lee MH, Yang HI, Jen CL. Community and personal risk factors for hepatitis C virus infection: a survey of 23,820 residents in Taiwan in 1991–2. Gut. 2011;60:688–694. doi: 10.1136/gut.2010.220889. [DOI] [PubMed] [Google Scholar]
- 111.Wang JT, Wang TH, Lin JT, Lee CZ, Sheu JC, Chen DS. Effect of hepatitis C antibody screening in blood donors on post-transfusion hepatitis in Taiwan. J Gastroenterol Hepatol. 1995;10:454–458. doi: 10.1111/j.1440-1746.1995.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 112.Lin T, Chen CH, Chou P. Effects of combination approach on harm reduction programs: the Taiwan experience. Harm Reduct J. 2016;13:23–33. doi: 10.1186/s12954-016-0112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sun P, Su N, Lin FZ. Prevalence of hepatitis A viral RNA and antibodies among Chinese blood donors. Genet Mol Res. 2015;14:16431–16437. doi: 10.4238/2015.December.9.13. [DOI] [PubMed] [Google Scholar]
- 114.Zhu Y, Yuan Z, Zhao Q, Chen G, Xu B. Seroprevalence of hepatitis A virus antibody in a population aged 0–30 years in Shanghai, China: implications for hepatitis A immunization. Epidemiol Infect. 2013;141:556–562. doi: 10.1017/S0950268812001161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Han T, Li C, Zhang Y. The prevalence of hepatitis A virus and parvovirus B19 in source-plasma donors and whole blood donors in China. Transfus Med. 2015;25:406–410. doi: 10.1111/tme.12259. [DOI] [PubMed] [Google Scholar]
- 116.Yu P, Huang L, Li H. Epidemiological investigation of an outbreak of hepatitis A in rural China. Int J Infect Dis. 2015;33:191–195. doi: 10.1016/j.ijid.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 117.Jia Z, Yi Y, Liu J. Epidemiology of hepatitis E virus in China: results from the Third National Viral Hepatitis Prevalence Survey, 2005–2006. PLoS One. 2014;9 doi: 10.1371/journal.pone.0110837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cong W, Sui JC, Zhang XY, Qian AD, Chen J, Zhu XQ. Seroprevalence of hepatitis E virus among pregnant women and control subjects in China. J Med Virol. 2015;87:446–450. doi: 10.1002/jmv.24058. [DOI] [PubMed] [Google Scholar]
- 119.Gu G, Huang H, Zhang L, Bi Y, Hu Y, Zhou YH. Hepatitis E virus seroprevalence in pregnant women in Jiangsu, China, and postpartum evolution during six years. BMC Infect Dis. 2015;15:560–567. doi: 10.1186/s12879-015-1308-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Aye TT, Uchida T, Ma XZ. Complete nucleotide sequence of a hepatitis E virus isolated from the Xinjiang epidemic (1986–1988) of China. Nucleic Acids Res. 1992;20 doi: 10.1093/nar/20.13.3512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang L, Yan B, Xu A. A hepatitis E outbreak by genotype 4 virus in Shandong province, China. Vaccine. 2016;34:3715–3718. doi: 10.1016/j.vaccine.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 122.Zhu FC, Huang SJ, Wu T. Epidemiology of zoonotic hepatitis E: a community-based surveillance study in a rural population in China. PLoS One. 2014;9 doi: 10.1371/journal.pone.0087154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang X, An J, Tu A. Comparison of immune persistence among inactivated and live attenuated hepatitis a vaccines 2 years after a single dose. Hum Vaccin Immunother. 2016;12:2322–2326. doi: 10.1080/21645515.2015.1134069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang J, Zhang XF, Huang SJ. Long-term efficacy of a hepatitis E vaccine. N Engl J Med. 2015;372:914–922. doi: 10.1056/NEJMoa1406011. [DOI] [PubMed] [Google Scholar]
- 125.Jacobson KH. World Health Organization; Geneva: 2010. The global prevalence of hepatitis A virus infection and susceptibility: a systematic review. [Google Scholar]
- 126.Jindal M, Rana SS, Gupta RK, Das K, Kar P. Serological study of hepatitis A virus infection amongst the students of a medical college in Delhi & evaluation of the need of vaccination. Indian J Med Res. 2002;115:1–4. [PubMed] [Google Scholar]
- 127.Chadha MS, Lole KS, Bora MH, Arankalle VA. Outbreaks of hepatitis A among children in western India. Trans R Soc Trop Med Hyg. 2009;103:911–916. doi: 10.1016/j.trstmh.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 128.Goel A, Aggarwal R. Advances in hepatitis E—II: epidemiology, clinical manifestations, treatment and prevention. Expert Rev Gastroenterol Hepatol. 2016;10:1065–1074. doi: 10.1080/17474124.2016.1185365. [DOI] [PubMed] [Google Scholar]
- 129.Patra S, Kumar A, Trivedi SS, Puri M, Sarin SK. Maternal and fetal outcomes in pregnant women with acute hepatitis E virus infection. Ann Intern Med. 2007;147:28–33. doi: 10.7326/0003-4819-147-1-200707030-00005. [DOI] [PubMed] [Google Scholar]
- 130.Arankalle VA, Chadha MS, Chitambar SD, Walimbe AM, Chobe LP, Gandhe SS. Changing epidemiology of hepatitis A and hepatitis E in urban and rural India (1982–98) J Viral Hepat. 2001;8:293–303. doi: 10.1046/j.1365-2893.2001.00279.x. [DOI] [PubMed] [Google Scholar]
- 131.Mulyanto Viral hepatitis in Indonesia: past, present, and future. Euroasian J Hepatogastroenterol. 2016;6:65–69. doi: 10.5005/jp-journals-10018-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gunawan S, Muttaqin Z, Darti MW, et al. Prevalence of anti-HAV IgG among student in Mataram. Proceeding of Symposium Gastroenterohepatology, Mataram; Mataram, Indonesia; July 5–7, 2012 (abstr).
- 133.Corwin A, Putri MP, Winarno J. Epidemic and sporadic hepatitis E virus transmission in West Kalimantan (Borneo), Indonesia. Am J Trop Med Hyg. 1997;57:62–65. doi: 10.4269/ajtmh.1997.57.62. [DOI] [PubMed] [Google Scholar]
- 134.Corwin A, Jarot K, Lubis I. Two years' investigation of epidemic hepatitis E virus transmission in West Kalimantan (Borneo), Indonesia. Trans R Soc Trop Med Hyg. 1995;89:262–265. doi: 10.1016/0035-9203(95)90529-4. [DOI] [PubMed] [Google Scholar]
- 135.Sedyaningsih-Mamahit ER, Larasati RP, Laras K. First documented outbreak of hepatitis E virus transmission in Java, Indonesia. Trans R Soc Trop Med Hyg. 2002;96:398–404. doi: 10.1016/s0035-9203(02)90373-1. [DOI] [PubMed] [Google Scholar]
- 136.Utsumi T, Hayashi Y, Lusida MI. Prevalence of hepatitis E virus among swine and humans in two different ethnic communities in Indonesia. Arch Virol. 2011;156:689–693. doi: 10.1007/s00705-010-0883-x. [DOI] [PubMed] [Google Scholar]
- 137.Widasari DI, Yano Y, Utsumi T. Hepatitis E virus infection in two different regions of Indonesia with identification of swine HEV genotype 3. Microbiol Immunol. 2013;57:692–703. doi: 10.1111/1348-0421.12083. [DOI] [PubMed] [Google Scholar]
- 138.Wibawa ID, Suryadarma IG, Mulyanto Identification of genotype 4 hepatitis E virus strains from a patient with acute hepatitis E and farm pigs in Bali, Indonesia. J Med Virol. 2007;79:1138–1146. doi: 10.1002/jmv.20904. [DOI] [PubMed] [Google Scholar]
- 139.Viral Hepatitis Surveillance System—Pakistan: monthly acute viral hepatitis report, October 2014. 2014. http://emphnet.net/wpcontent/uploads/2015/05/Hepatitis-data-Oct-14.pdf
- 140.Aziz S, Muzaffar R. Helicobacter Pylori, hepatitis viruses A, C, E, antibodies, and HBsAg-Prevention and associated factors in pediatric communities of Karachi. J Coll Physicians Surg Pak. 2007;17:195–198. [PubMed] [Google Scholar]
- 141.Shah U, Habib Z, Kleinman RE. Liver failure attributable to hepatitis A virus infection in a developing country. Pediatrics. 2000;105:436–438. doi: 10.1542/peds.105.2.436. [DOI] [PubMed] [Google Scholar]
- 142.Butt AS, Sharif F. Viral Hepatitis in Pakistan: past, present, and future. Euroasian J Hepatogastroenterol. 2016;6:70–81. doi: 10.5005/jp-journals-10018-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Butt AS, Hamid S. Hepatitis E and acute-on-chronic liver failure: outcome and predictors of mortality in Asia pacific region. 26th Annual Conference of the Asian-Pacific Association for the Study of the Liver; Shanghai, China; Feb 15–19, 2017 (abstr PP0151).
- 144.Hamid SS, Atiq M, Shehzad F. Hepatitis E virus superinfection in patients with chronic liver disease. Hepatology. 2002;36:474–478. doi: 10.1053/jhep.2002.34856. [DOI] [PubMed] [Google Scholar]
- 145.Naru T, Yousuf F, Malik A, Naz S, Ismail H. Comparison of foeto-maternal outcome in pregnant women with hepatitis E—a review of 12 years. J Pak Med Assoc. 2017;67:538–543. [PubMed] [Google Scholar]
- 146.Iqbal T, Idrees M, Ali L. Isolation and characterization of two new hepatitis E virus genotype 1 strains from two mini-outbreaks in Lahore, Pakistan. Virol J. 2011;8:94–99. doi: 10.1186/1743-422X-8-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Khan A, Tanaka Y, Kurbanov F. Investigating an outbreak of acute viral hepatitis caused by hepatitis E virus variants in Karachi, South Pakistan. J Med Virol. 2011;83:622–629. doi: 10.1002/jmv.22036. [DOI] [PubMed] [Google Scholar]
- 148.Ahmad T, Waheed Y, Tahir S. Frequency of HEV contamination in sewerage waters in Pakistan. J Infect Dev Ctries. 2010;4:842–845. doi: 10.3855/jidc.612. [DOI] [PubMed] [Google Scholar]
- 149.Khan WI, Sultana R, Rahman M. Viral hepatitis: recent experiences from serological studies in Bangladesh. Asian Pac J Allergy Immunol. 2000;18:99–103. [PubMed] [Google Scholar]
- 150.Saha SK, Saha S, Shakur S. Community-based cross-sectional seroprevalence study of hepatitis A in Bangladesh. World J Gastroenterol. 2009;15:4932–4937. doi: 10.3748/wjg.15.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cuthbert JA. Hepatitis A: old and new. Clin Microbiol Rev. 2001;14:38–58. doi: 10.1128/CMR.14.1.38-58.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Amin MZ, Siddique LN, Satter MA, Biswas KK. Increasing incidence of hepatitis A in Bangladesh. Bangladesh J Sci Ind Res. 2012;47:309–312. [Google Scholar]
- 153.Harun-Or-Rashid M, Akbar SMF, Takahashi K. Epidemiological and molecular analyses of a non-seasonal outbreak of acute icteric hepatitis E in Bangladesh. J Med Virol. 2013;85:1369–1376. doi: 10.1002/jmv.23601. [DOI] [PubMed] [Google Scholar]
- 154.Labrique AB, Zaman K, Hossain Z. Epidemiology and risk factors of incident hepatitis E virus infections in rural Bangladesh. Am J Epidemiol. 2010;172:952–961. doi: 10.1093/aje/kwq225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Mamun-Al-Mahtab, Rahman S, Khan M, Karim F. HEV infection as an aetiologic factor for acute hepatitis: experience from a tertiary hospital in Bangladesh. J Health Popul Nutr. 2009;27:14–19. doi: 10.3329/jhpn.v27i1.3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mahtab MA, Rahman S, Khan M, Karim MF. Hepatitis E virus is a leading cause of acute-on-chronic liver disease: experience from a tertiary centre in Bangladesh. Hepatobiliary Pancreat Dis Int. 2009;8:50–52. [PubMed] [Google Scholar]
- 157.Sohn YM, Rho HO, Park MS. The changing epidemiology of hepatitis A in children and the consideration of active immunization in Korea. Yonsei Med J. 2000;41:34–39. doi: 10.3349/ymj.2000.41.1.34. [DOI] [PubMed] [Google Scholar]
- 158.Song MH, Lim YS, Song TJ. The etiology of acute viral hepatitis for last 3 years. Korean J Med. 2005;68:256–260. [Google Scholar]
- 159.Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention . Korea Centers for Disease Control and Prevention; Cheongju: 2017. Infectious diseases surveillance yearbook, 2016 (PHWR Vol 10–GL2017001) [Google Scholar]
- 160.Moon S, Han JH, Bae GR, Cho E, Kim B. Hepatitis A in Korea from 2011 to 2013: current epidemiologic status and regional distribution. J Korean Med Sci. 2016;31:67–72. doi: 10.3346/jkms.2016.31.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jeong SH. Current status of hepatitis e virus infection in Korea. Gut Liver. 2011;5:427–431. doi: 10.5009/gnl.2011.5.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Taniguchi M, Kim SR, Mishiro S. Epidemiology of hepatitis E in northeastern China, South Korea and Japan. J Infect. 2009;58:232–237. doi: 10.1016/j.jinf.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 163.The Kirby Institute HIV, viral hepatitis and sexually transmissible infections in Australia: Annual Surveillance Report 2011. 2011. https://kirby.unsw.edu.au/sites/default/files/kirby/report/SERP_2011-Annual-Surveillance-Report.pdf
- 164.Lopez L, Roos R, Cressey P, Horn B, Lee J. Ministry for Primary Industries; Wellington: 2016. Foodborne disease in New Zealand 2015. [Google Scholar]
- 165.WHO . World Health Organization; Geneva: 2018. Global status report on alcohol and health 2018. [Google Scholar]
- 166.Li YM, Chen WX, Yu CH. An epidemiological survey of alcoholic liver disease in Zhejiang province. Zhonghua Gan Zang Bing Za Zhi. 2003;11:647–649. (in Chinese). [PubMed] [Google Scholar]
- 167.Lu X-I, Tao M, Luo J-Y, Gen Y, Z PR, Z H-L. Epidemiology of alcoholic liver diseases in Xi'an. Shijie Huaren Xiaohua Za Zhi. 2003;11:719–722. (in Chinese). [Google Scholar]
- 168.Chen SL, Meng XD, Wang BY. An epidemiologic survey of alcoholic liver disease in some cities of Liaoning province. Zhonghua Gan Zang Bing Za Zhi. 2010;13:428–430. (in Chinese). [Google Scholar]
- 169.Yao JH, Zhao QD, Xiong PF. Investigation of alcoholic liver disease in ethnic groups of Yuanjiang county in Yunnan. Weichang Bingxue He Ganbingxue Za Zhi. 2011;20:1137–1139. (in Chinese). [Google Scholar]
- 170.Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol. 2013;28(suppl 1):11–17. doi: 10.1111/jgh.12036. [DOI] [PubMed] [Google Scholar]
- 171.Wang H, Ma L, Yin Q, Zhang X, Zhang C. Prevalence of alcoholic liver disease and its association with socioeconomic status in north-eastern China. Alcohol Clin Exp Res. 2014;38:1035–1041. doi: 10.1111/acer.12321. [DOI] [PubMed] [Google Scholar]
- 172.Huang A, Chang B, Sun Y. Disease spectrum of alcoholic liver disease in Beijing 302 Hospital from 2002 to 2013: a large tertiary referral hospital experience from 7422 patients. Medicine (Baltimore) 2017;96 doi: 10.1097/MD.0000000000006163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Chang B, Li B, Sun Y. Changes in etiologies of hospitalized patients with liver cirrhosis in Beijing 302 Hospital from 2002 to 2013. Mediators Inflamm. 2017;2017 doi: 10.1155/2017/5605981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bao XY, Xu BB, Fang K, Li Y, Hu YH, Yu GP. Changing trends of hospitalisation of liver cirrhosis in Beijing, China. BMJ Open Gastroenterol. 2015;2 doi: 10.1136/bmjgast-2015-000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Faridz D, Griffiths J. More than 80 dead from drinking bootleg alcohol in Indonesia. 2018. https://edition.cnn.com/2018/04/12/health/indonesia-fake-alcohol-intl/index.html
- 176.Rahman S, Ahmed MF, Alam MJ. Distribution of liver disease in Bangladesh: a cross-country study. Euroasian J Hepatogastroenterol. 2014;4:25–30. doi: 10.5005/jp-journals-10018-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kikuchi M, Horie Y, Ebinuma H, Taniki N, Nakamoto N, Kanai T. Alcoholic liver cirrhosis and significant risk factors for the development of alcohol-related hepatocellular carcinoma—Japan, 2012. Nihon Arukoru Yakubutsu Igakkai Zasshi. 2015;50:222–234. [PubMed] [Google Scholar]
- 178.Kweon S, Kim Y, Jang MJ. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra: 2011. Contribution of chronic disease to the gap in mortality between Aboriginal and Torres Strait Islander people and other Australians. [Google Scholar]
- 180.China Health and Family Planning Statistics Yearbook. 2017. http://www.yearbookchina.com/navibooklist-N2017120225-1.html
- 181.Tang YL, Xiang XJ, Wang XY, Cubells JF, Babor TF, Hao W. Alcohol and alcohol-related harm in China: policy changes needed. Bull World Health Organ. 2013;91:270–276. doi: 10.2471/BLT.12.107318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.GBD 2016 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Yu YC, Mao YM, Chen CW. CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hepatol Int. 2017;11:221–241. doi: 10.1007/s12072-017-9793-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Li Z, Xue J, Chen P, Chen L, Yan S, Liu L. Prevalence of nonalcoholic fatty liver disease in mainland of China: a meta-analysis of published studies. J Gastroenterol Hepatol. 2014;29:42–51. doi: 10.1111/jgh.12428. [DOI] [PubMed] [Google Scholar]
- 185.Fan JG, Zhu J, Li XJ. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol. 2005;43:508–514. doi: 10.1016/j.jhep.2005.02.042. [DOI] [PubMed] [Google Scholar]
- 186.Fan JG, Farrell GC. Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol. 2009;50:204–210. doi: 10.1016/j.jhep.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 187.Zhou YJ, Li YY, Nie YQ. Prevalence of fatty liver disease and its risk factors in the population of South China. World J Gastroenterol. 2007;13:6419–6424. doi: 10.3748/wjg.v13.i47.6419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Xu C, Yu C, Ma H, Xu L, Miao M, Li Y. Prevalence and risk factors for the development of nonalcoholic fatty liver disease in a nonobese Chinese population: the Zhejiang Zhenhai Study. Am J Gastroenterol. 2013;108:1299–1304. doi: 10.1038/ajg.2013.104. [DOI] [PubMed] [Google Scholar]
- 189.Estes C, Anstee QM, Arias-Loste MT. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69:896–904. doi: 10.1016/j.jhep.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 190.Amarapurkar DN, Hashimoto E, Lesmana LA, Sollano JD, Chen PJ, Goh KL. How common is non-alcoholic fatty liver disease in the Asia-Pacific region and are there local differences? J Gastroenterol Hepatol. 2007;22:788–793. doi: 10.1111/j.1440-1746.2007.05042.x. [DOI] [PubMed] [Google Scholar]
- 191.Duseja A, Singh SP, Saraswat VA. Non-alcoholic fatty liver disease and metabolic syndrome-position paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of Gastroenterology. J Clin Exp Hepatol. 2015;5:51–68. doi: 10.1016/j.jceh.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Amarapurkar D, Kamani P, Patel N. Prevalence of non-alcoholic fatty liver disease: population-based study. Ann Hepatol. 2007;6:161–163. [PubMed] [Google Scholar]
- 193.Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni CS. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009;84:84–91. doi: 10.1016/j.diabres.2008.11.039. [DOI] [PubMed] [Google Scholar]
- 194.Das K, Das K, Mukherjee PS. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology. 2010;51:1593–1602. doi: 10.1002/hep.23567. [DOI] [PubMed] [Google Scholar]
- 195.Majumdar A, Misra P, Sharma S, Kant S, Krishnan A, Pandav CS. Prevalence of nonalcoholic fatty liver disease in an adult population in a rural community of Haryana, India. Indian J Public Health. 2016;60:26–33. doi: 10.4103/0019-557X.177295. [DOI] [PubMed] [Google Scholar]
- 196.Siraj P, Kohli N, Srivastava VK, Natu SM. Distribution of nutrient intake among the subjects of non-alcoholic fatty liver disease in Lucknow district. Indian J Soc Res. 2012;3:37–41. [Google Scholar]
- 197.Bajaj S, Nigam P, Luthra A. A case-control study on insulin resistance, metabolic co-variates & prediction score in non-alcoholic fatty liver disease. Indian J Med Res. 2009;129:285–292. [PubMed] [Google Scholar]
- 198.Jali MV, Kambar S, Jali SM, Hiremath MB. Prevalence of non- alcoholic fatty liver disease among type-2diabetes mellitus patients–a cross-sectional hospital-based study. Al Ameen J Med Sci. 2015;8:50–54. [Google Scholar]
- 199.Kalra S, Vithalani M, Gulati G. Study of prevalence of nonalcoholic fatty liver disease (NAFLD) in type 2 diabetes patients in India (SPRINT) J Assoc Physicians India. 2013;61:448–453. [PubMed] [Google Scholar]
- 200.Patell R, Dosi R, Joshi H, Sheth S, Shah P, Jasdanwala S. Non-alcoholic fatty liver disease (NAFLD) in obesity. J Clin Diagn Res. 2014;8:62–66. doi: 10.7860/JCDR/2014/6691.3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Kumar R, Rastogi A, Sharma MK. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J Endocrinol Metab. 2013;17:665–671. doi: 10.4103/2230-8210.113758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Government of India Ministry of Health and Family Welfare National Family Health Survey 4 (NFHS-4) 2015–16. http://rchiips.org/NFHS/pdf/NFHS4/India.pdf
- 203.Chi NH, Whiting D, Forouhi N. IDF diabetes atlas, 7th edn. 2015. https://www.idf.org/component/attachments/attachments.html?id=1093&task=download
- 204.Duseja A, Das A, Das R. The clinicopathological profile of Indian patients with nonalcoholic fatty liver disease (NAFLD) is different from that in the West. Dig Dis Sci. 2007;52:2368–2374. doi: 10.1007/s10620-006-9136-y. [DOI] [PubMed] [Google Scholar]
- 205.Madan K, Batra Y, Gupta SD. Non-alcoholic fatty liver disease may not be a severe disease at presentation among Asian Indians. World J Gastroenterol. 2006;12:3400–3405. doi: 10.3748/wjg.v12.i21.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ray G. Trends of chronic liver disease in a tertiary care referral hospital in Eastern India. Indian J Public Health. 2014;58:186–194. doi: 10.4103/0019-557X.138630. [DOI] [PubMed] [Google Scholar]
- 207.Asim M, Sarma MP, Kar P. Etiological and molecular profile of hepatocellular cancer from India. Int J Cancer. 2013;133:437–445. doi: 10.1002/ijc.27993. [DOI] [PubMed] [Google Scholar]
- 208.Kumar M, Kumar R, Hissar S. Risk factors analysis for hepatocellular carcinoma in patients with and without cirrhosis: a case-control study of 213 hepatocellular carcinoma patients from India. J Gastroenterol Hepatol. 2007;22:1104–1111. doi: 10.1111/j.1440-1746.2007.04908.x. [DOI] [PubMed] [Google Scholar]
- 209.Hasan I, Gani RA, Machmud R. Prevalence and risk factors for nonalcoholic fatty liver in Indonesia. J Gastroenterol Hepatol. 2002;17(suppl):S154. [Google Scholar]
- 210.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. Lancet. 2016;387:1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Younossi Z, Anstee QM, Marietti M. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 213.Pati GK, Singh SP. Nonalcoholic fatty liver disease in south Asia. Euroasian J Hepatogastroenterol. 2016;6:154–162. doi: 10.5005/jp-journals-10018-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Niaz A, Ali Z, Nayyar S, Fatima N. Prevalence of NAFLD in healthy and young male individuals. ISRN Gastroenterol. 2011;2011 doi: 10.5402/2011/363546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Abbas Z, Saeed A, Hassan SM. Non-alcoholic fatty liver disease among visitors to a hepatitis awareness programme. Trop Gastroenterol. 2013;34:153–158. doi: 10.7869/tg.119. [DOI] [PubMed] [Google Scholar]
- 216.Butt AS, Hamid S, Jafri W, Salih M, Javed A. Prevalence and risk factors for NAFLD among native south Asian Pakistani patients with type II diabetes and metabolic syndrome. United Eur Gastroenterol Week. 2011 Abstract No. 11–6979. [Google Scholar]
- 217.Butt AS, Hamid S, Haider Z, Salih M, Sharif F, Akhter J. NAFLD in newly diagnosed type 2 diabetes: prevalence and estimation of multiplicative effect for combination of various predicting factors. Hepatol Int. 2017;11(suppl 1):S1. [Google Scholar]
- 218.Alam S, Fahim SM, Chowdhury MAB. Prevalence and risk factors of non-alcoholic fatty liver disease in Bangladesh. JGH Open. 2018;2:39–46. doi: 10.1002/jgh3.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Rahman MM, Kibria G, Begum H. Prevalence and risk factors of nonalcoholic fatty liver disease in a rural community of south Asia. Gastroenterology. 2015;148:S145–S146. doi: 10.1136/bmjgast-2020-000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Biswas T, Garnett SP, Pervin S, Rawal LB. The prevalence of underweight, overweight and obesity in Bangladeshi adults: data from a national survey. PLoS One. 2017;12 doi: 10.1371/journal.pone.0177395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Bangladesh Demographic and Health Survey 2011 preliminary report. 2011. https://dhsprogram.com/pubs/pdf/PR15/PR15.pdf
- 222.Biswas T, Islam A, Rawal LB, Islam SM. Increasing prevalence of diabetes in Bangladesh: a scoping review. Public Health. 2016;138:4–11. doi: 10.1016/j.puhe.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 223.Alam S, Noor-E-Alam SM, Chowdhury ZR, Alam M, Kabir J. Nonalcoholic steatohepatitis in nonalcoholic fatty liver disease patients of Bangladesh. World J Hepatol. 2013;5:281–287. doi: 10.4254/wjh.v5.i5.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Tateishi R, Okanoue T, Fujiwara N. Clinical characteristics, treatment, and prognosis of non-B, non-C hepatocellular carcinoma: a large retrospective multicenter cohort study. J Gastroenterol. 2015;50:350–360. doi: 10.1007/s00535-014-0973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Park SH, Jeon WK, Kim SH. Prevalence and risk factors of non-alcoholic fatty liver disease among Korean adults. J Gastroenterol Hepatol. 2006;21:138–143. doi: 10.1111/j.1440-1746.2005.04086.x. [DOI] [PubMed] [Google Scholar]
- 226.Lee K, Sung JA, Kim JS, Park TJ. The roles of obesity and gender on the relationship between metabolic risk factors and non-alcoholic fatty liver disease in Koreans. Diabetes Metab Res Rev. 2009;25:150–155. doi: 10.1002/dmrr.924. [DOI] [PubMed] [Google Scholar]
- 227.Kojima S, Watanabe N, Numata M, Ogawa T, Matsuzaki S. Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J Gastroenterol. 2003;38:954–961. doi: 10.1007/s00535-003-1178-8. [DOI] [PubMed] [Google Scholar]
- 228.Lee HW, Kim BK, Kim SU. Prevalence and predictors of significant fibrosis among subjects with transient elastography-defined nonalcoholic fatty liver disease. Dig Dis Sci. 2017;62:2150–2158. doi: 10.1007/s10620-017-4592-0. [DOI] [PubMed] [Google Scholar]
- 229.Seo SH, Lee HW, Park HW. Prevalence and associated factors of nonalcoholic fatty liver disease in the health screen examinees. Korean J Med. 2006;70:26–32. [Google Scholar]
- 230.Access Economics The growing cost of obesity in 2008: three years on. 2008. http://www.diabetesaustralia.com.au/PageFiles/7830/FULLREPORTGrowingCostOfObesity2008.pdf
- 231.Burns J, Drew N, Elwel M. Overview of Aboriginal and Torres Strait Islander health status, 2018. 2019. https://healthinfonet.ecu.edu.au/healthinfonet/getContent.php?linkid=617557&title=Overview+of+Aboriginal+and+Torres+Strait+Islander+health+status+2018
- 232.Steering Committee for the Review of Government Service Provision . Productivity Commission; Canberra: 2016. Overcoming Indigenous disadvantage: key indicators 2016 report. [Google Scholar]
- 233.Ministry of Social Development The Social Report. 2004. http://socialreport.msd.govt.nz/2004/notes-references/endnotes.html#28
- 234.Ministry of Health . Ministry of Health; Wellington: 2016. Annual update of key results 2015/16: New Zealand Health Survey. [Google Scholar]
- 235.Coppell KJ, Miller JC, Gray AR, Schultz M, Mann JI, Parnell WR. Obesity and the extent of liver damage among adult New Zealanders: findings from a national survey. Obes Sci Pract. 2015;1:67–77. doi: 10.1002/osp4.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Khaw KB, Choi RH, Kam JH, Chakraborty B, Chow PK. Interval increase in the prevalence of symptomatic cholelithiasis-associated non-alcoholic fatty liver disease over a ten-year period in an Asian population. Singapore Med J. 2017;58:703–707. doi: 10.11622/smedj.2016189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Goh GB, Kwan C, Lim SY. Perceptions of non-alcoholic fatty liver disease–an Asian community-based study. Gastroenterol Rep. 2016;4:131–135. doi: 10.1093/gastro/gov047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Koh WP, Wang R, Jin A, Yu MC, Yuan JM. Diabetes mellitus and risk of hepatocellular carcinoma: findings from the Singapore Chinese Health Study. Br J Cancer. 2013;108:1182–1188. doi: 10.1038/bjc.2013.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Ministry of Health Singapore National health survey 2010. 2018. https://www.moh.gov.sg/resources-statistics/reports/national-health-survey-2010
- 240.Li J, Zou B, Yeo YH. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–398. doi: 10.1016/S2468-1253(19)30039-1. [DOI] [PubMed] [Google Scholar]
- 241.Purdie E. Tracking GDP in PPP terms shows rapid rise of China and India. 2019. https://blogs.worldbank.org/opendata/tracking-gdp-ppp-terms-shows-rapid-rise-china-and-india
- 242.China Statistical Yearbook 2017. 2017. http://www.stats.gov.cn/tjsj/ndsj/2017/indexch.htm
- 243.WHO China statistics summary (2002–present) 2019. http://apps.who.int/gho/data/node.country.country-CHN
- 244.WHO China key indicators. 2016. http://apps.who.int/gho/data/node.cco.ki-CHN?lang=en
- 245.WHO Country Cooperation Strategy at a glance: China. 2018. http://apps.who.int/iris/bitstream/handle/10665/137150/ccsbrief_chn_en.pdf?sequence=1
- 246.Hou J, Wang G, Wang F. Guideline of prevention and treatment for chronic hepatitis B (2015 update) J Clin Transl Hepatol. 2017;5:297–318. doi: 10.14218/JCTH.2016.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Chinese Society of Hepatology. Wei L, Chinese Society of Infection Diseases. Hou JL. The guideline of prevention and treatment for hepatitis C: a 2015 update. Zhonghua Gan Zang Bing Za Zhi. 2015;23:906–923. doi: 10.3760/cma.j.issn.1007-3418.2015.12.003. (in Chinese). [DOI] [PubMed] [Google Scholar]
- 248.Shan S, Wei W, Kong Y. China Registry of Hepatitis B (CR-HepB): protocol and implementation of a nationwide hospital-based registry of hepatitis B. Scand J Public Health. 2018 doi: 10.1177/1403494818772188. published online April 1. [DOI] [PubMed] [Google Scholar]
- 249.Greenhalgh S. Soda industry influence on obesity science and policy in China. J Public Health Policy. 2019;40:5–16. doi: 10.1057/s41271-018-00158-x. [DOI] [PubMed] [Google Scholar]
- 250.Ministry of Health and Family Welfare Government of India Situation analysis: backdrop to the National Health Policy. 2017. https://mohfw.gov.in/sites/default/files/71275472221489753307.pdf
- 251.Berman P, Ahuja R, Bhandari L. The impoverishing effect of health care payments in India: new methodology and findings. Econ Polit Wkly. 2010;45:65–71. [Google Scholar]
- 252.National Health Portal India National Viral Hepatitis Control Program (NVHCP) 2019. https://www.nhp.gov.in/national-viral-hepatitis-control-program-(nvhcp)_pg
- 253.WHO The Global Burden of Disease 2004 update. 2008. https://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf
- 254.Misra A, Sharma R, Gulati S. Consensus dietary guidelines for healthy living and prevention of obesity, the metabolic syndrome, diabetes, and related disorders in Asian Indians. Diabetes Technol Ther. 2011;13:683–694. doi: 10.1089/dia.2010.0198. [DOI] [PubMed] [Google Scholar]
- 255.Ministry of Health and Family Welfare Government of India National multisectoral action plan for prevention and control of common noncommunicable diseases (2017–2022) https://mohfw.gov.in/sites/default/files/National%20Multisectoral%20Action%20Plan%20%28NMAP%29%20for%20Prevention%20and%20Control%20of%20Common%20NCDs%20%282017-22%29.pdf
- 256.Food Safety & Standards Authority of India Guidelines–code of self-regulation in food advertisement. 2009. https://old.fssai.gov.in/Portals/0/Draft_code_for_selfregulation_October2009.pdf
- 257.Khandelwal S, Reddy KS. Eliciting a policy response for the rising epidemic of overweight-obesity in India. Obes Rev. 2013;14(suppl 2):114–125. doi: 10.1111/obr.12097. [DOI] [PubMed] [Google Scholar]
- 258.Food Safety and Standards Authority of India The prevention of food adulteration act & rules (as on 1·10·2004) http://www.old.fssai.gov.in/Portals/0/Pdf/pfa%20acts%20and%20rules.pdf
- 259.Maindola A. FSSAI aiming to reduce hydrogenated trans fats in Indian food to 2% 2019. https://www.fssai.gov.in/upload/media/FSSAI_News_Transfat_FNB_03_01_2019.pdf
- 260.The World Bank Population total Indonesia. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=ID
- 261.UN Office on Drugs and Crime Harm reduction advocacy programme with members of Indonesia's Parliament concludes. 2011. https://www.unodc.org/southeastasiaandpacific/en/2011/01/hiv-indonesia/story.html
- 262.Gunardi H, Zaimi LF, Soedjatmiko, Turyadi, Harahap AR, Muljono DH. Current prevalence of hepatitis B infection among parturient women in Jakarta, Indonesia. Acta Med Indones. 2014;46:3–9. [PubMed] [Google Scholar]
- 263.Ministry of Health Republic of Indonesia Regulation of Ministry of Health of the Republic of Indonesia number 53 of 2015 concerning the control of viral hepatitis. 2015. http://hukor.kemkes.go.id/uploads/produk_hukum/PMK_No._53_ttg_Penanggulangan_Hepatitis_Virus_.pdf (in Indonesian).
- 264.Ministry of Health Republic of Indonesia Regulation of Ministry of Health of the Republic of Indonesia number 52 of 2017 on triple elimination of mother-to-child transmission of HIV, syphilis and hepatitis B. 2017. http://hukor.kemkes.go.id/uploads/produk_hukum/PMK_No._52_ttg_Eliminasi_Penularan_HIV,_Sifilis,_dan_Hepatitis_B_Dari_Ibu_Ke_Anak_.pdf (in Indonesian).
- 265.Law of the Republic of Indonesia number 17 of 2007 on long-term national development plan of 2005–2025. https://policy.asiapacificenergy.org/sites/default/files/LONG-TERM%20NATIONAL%20DEVELOPMENT%20PLAN%20OF%202005-2025%20%28EN%29.pdf
- 266.Nugraha P. Healthy lifestyle movement launched in West Nusa Tenggara. 2017. https://www.thejakartapost.com/news/2017/03/29/healthy-lifestyle-movement-launched-in-west-nusa-tenggara.html
- 267.Asia Roundtable on Food Innovation for Improve Nutrition Tackling obesity in Asean: Indonesia's healthy eating campaign. 2018. http://www.arofiin.org/News/tid/83/Tackling-Obesity-in-ASEAN-Indonesia-s-Healthy-Eating-Campaign
- 268.O'Neill J. The “next eleven” and the world economy. 2018. https://www.project-syndicate.org/commentary/n-11-global-economy-by-jim-o-neill-2018-04?barrier=accesspaylog
- 269.World Bank Non-communicable diseases (NCDs)–Pakistan's next major health challenge. 2011. http://siteresources.worldbank.org/SOUTHASIAEXT/Resources/223546-1296680097256/7707437-1296680114157/NCD_PK_Policy_Feb_2011.pdf
- 270.WHO-UNICEF Pakistan: WHO and UNICEF estimates of immunization coverage: 2018 revision. 2019. https://www.who.int/immunization/monitoring_surveillance/data/pak.pdf
- 271.Waheed Y, Siddiq W. Elimination of hepatitis from Pakistan by 2030: is it possible? Hepatoma Res. 2018;4:45. [Google Scholar]
- 272.WHO Regional Office for the Eastern Meditteranean Pakistan: prevention and control of hepatitis. 2019. http://www.emro.who.int/pak/programmes/prevention-a-control-of-hepatitis.html
- 273.Centers for Disease Control and Prevention (CDC) Establishment of a viral hepatitis surveillance system–Pakistan, 2009–2011. MMWR Morb Mortal Wkly Rep. 2011;60:1385–1390. [PubMed] [Google Scholar]
- 274.WHO Pakistan: prevention and control of hepatitis. 2017. http://www.emro.who.int/pak/programmes/prevention-a-control-of-hepatitis.html
- 275.Maqbool S. Pakistan launchs its first Hepatitis Strategic Framework. 2017. https://www.thenews.com.pk/print/235844-Pakistan-launches-its-first-Hepatitis-Strategic-Framework
- 276.Niazi AK, Niazi SK, Baber A. Nutritional programmes in Pakistan: a review. J Med Nutr Nutraceut. 2012;1:98–100. [Google Scholar]
- 277.Ministry of Health Government of Pakistan, WHO Pakistan office, and Heartfile; Islamabad: 2004. National Action Plan for prevention and control of non-communicable diseases and health promotion in Pakistan. [Google Scholar]
- 278.Pakistan dietary guidelines for better nutrition: my plate. 2018. http://www.fao.org/3/ca1868en/CA1868EN.pdf
- 279.Huq NM, Abul Quasem Al-Amin AQ, Ranjan Howlander SR, Kabir MA. Paying out of pocket for healthcare in Bangladesh–a burden on poor? Iran J Public Health. 2015;44:1024–1025. [PMC free article] [PubMed] [Google Scholar]
- 280.Paul RC, Rahman M, Wiesen E. Hepatitis B surface antigen seroprevalence among prevaccine and vaccine era children in Bangladesh. Am J Trop Med Hyg. 2018;99:764–771. doi: 10.4269/ajtmh.17-0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Alam S, Azam G, Mustafa G, Alam M, Ahmad N. Past, present, and future of hepatitis B and fatty liver in Bangladesh. Gastroenterol Hepatol Open Access. 2017;6:00197. [Google Scholar]
- 282.UN Office on Drugs and Crime The Narcotics Control Act. 1990. https://www.unodc.org/res/cld/document/the-narcotic-control-act-1990_html/The_Narcotic_Drugs_and_Psychotropic_Substances_Control_Act_1990.pdf
- 283.Bangladesh National Plan of Action for Nutrition. 1997. https://extranet.who.int/nutrition/gina/en/node/8230
- 284.WHO A new Action Plan for nutrition in Bangladesh. 2019. http://www.searo.who.int/entity/nutrition/success-stories/bangladesh/en/
- 285.Ministry of Local Government. Rural Development and Cooperatives National Urban Health Strategy 2014. 2014. http://uphcp.gov.bd/cmsfiles/files/NUHS.pdf
- 286.Strategic plan for surveillance and prevention of non-communicable diseases in Bangladesh 2011–2015. 2011. http://www.searo.who.int/bangladesh/publications/strategic_plan_2011-15.pdf
- 287.World Bank Health, nutrition, and population sector program restructuring paper. 2010. http://documents.worldbank.org/curated/en/339291468201262694/Main-report
- 288.Planning Wing Ministry of Health and Family Welfare. Government of the People's Republic of Bangladesh Health, population, and nutrition sector development program (2011–2016) program implementation plan volume-I. 2011. http://www.dghs.gov.bd/index.php/en/mis-docs/important-documents/item/hpnsdp-2011-16
- 289.Zhang X, Oyama T. Investigating the health care delivery system in Japan and reviewing the local public hospital reform. Risk Manag Healthc Policy. 2016;9:21–32. doi: 10.2147/RMHP.S93285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Organisation for Economic Co-operation and Development Life expectancy at birth. 2019. https://data.oecd.org/healthstat/life-expectancy-at-birth.htm
- 291.Hashimoto H, Ikegami N, Shibuya K. Cost containment and quality of care in Japan: is there a trade-off? Lancet. 2011;378:1174–1182. doi: 10.1016/S0140-6736(11)60987-2. [DOI] [PubMed] [Google Scholar]
- 292.Tatara K, Okamoto E. Japan: health system review. 2009. http://www.euro.who.int/__data/assets/pdf_file/0011/85466/E92927.pdf
- 293.Oza N, Isoda H, Ono T, Kanto T. Current activities and future directions of comprehensive hepatitis control measures in Japan: the supportive role of the Hepatitis Information Center in building a solid foundation. Hepatol Res. 2017;47:487–496. doi: 10.1111/hepr.12897. [DOI] [PubMed] [Google Scholar]
- 294.Ujiie M, Sasaki K, Yoshikawa N, Enami T, Shobayashi T. Introduction of a hepatitis B vaccine into the national routine immunisation programme of Japan. Lancet Inf Dis. 2016;16 doi: 10.1016/S1473-3099(16)30463-7. [DOI] [PubMed] [Google Scholar]
- 295.Uchida S, Satake M, Kurisu A. Incidence rates of hepatitis C virus infection among blood donors in Japan: a nationwide retrospective cohort study. Transfusion. 2018;58:2880–2885. doi: 10.1111/trf.14951. [DOI] [PubMed] [Google Scholar]
- 296.Tanaka J, Mizui M, Nagakami H. Incidence rates of hepatitis B and C virus infections among blood donors in Hiroshima, Japan, during 10 years from 1994 to 2004. Intervirology. 2008;51:33–41. doi: 10.1159/000118794. [DOI] [PubMed] [Google Scholar]
- 297.McCurry J. Japan battles with obesity. Lancet. 2007;369:451–452. doi: 10.1016/S0140-6736(07)60214-1. [DOI] [PubMed] [Google Scholar]
- 298.Onishi N. Japan, seeking trim waists, measures millions. https://www.nytimes.com/2008/06/13/world/asia/13fat.html
- 299.Araujo C. XL problems: waistlines, gold and taxes. 2016. https://www.policy-shift.com/single-post/2016/02/17/XL-Problems-Waistlines-Gold-and-Taxes
- 300.Organisation for Economic Co-operation and Development Country note: how does health spending in Korea compare? 2015. https://www.oecd.org/els/health-systems/Country-Note-KOREA-OECD-Health-Statistics-2015.pdf
- 301.Kwon S, Lee T-J, Kim C-Y. World Health Organization; Geneva: 2015. Republic of Korea health system review. [Google Scholar]
- 302.Chu M. How bad are ‘mukbang’ shows, really? 2018. http://www.koreabiomed.com/news/articleView.html?idxno=3890
- 303.Credit Suisse Research Institute Global wealth report 2018. 2018. https://www.credit-suisse.com/media/assets/corporate/docs/about-us/research/publications/global-wealth-report-2018-en.pdf
- 304.Australian Taxation Office Medicare levy. 2019. http://www.ato.gov.au/Individuals/Medicare-levy/
- 305.Australian Institute of Health and Welfare Health expenditure Australia 2011–12: analysis by sector. 2014. https://www.aihw.gov.au/getmedia/32af8c90-feac-46dc-b974-ffb3c8aa3a59/16669.pdf.aspx?inline=true
- 306.Williams AH. Reduction in the hepatitis B related burden of disease–measuring the success of universal immunisation programs. Commun Dis Intell Q Rep. 2002:458–460. doi: 10.33321/cdi.2002.26.44. [DOI] [PubMed] [Google Scholar]
- 307.McCulloch K, Romero N, MacLachlan J, Allard N, Cowie B. Modeling progress toward elimination of hepatitis B in Australia. Hepatology. 2019 doi: 10.1002/hep.30899. published online Aug 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Olsen A, Wallace J, Maher L. Responding to Australia's National Hepatitis B Strategy 2010–13: gaps in knowledge and practice in relation to Indigenous Australians. Austr J Primary Health. 2013;20:134–142. doi: 10.1071/PY12162. [DOI] [PubMed] [Google Scholar]
- 309.European Association for the Study of the Liver EASL clinical practice guidelines: management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 310.Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261–283. doi: 10.1002/hep.28156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.WHO Hepatitis B control through immunization: a reference guide. 2014. https://www.who.int/immunization/sage/meetings/2015/october/8_WPRO_Hepatitis_B_Prevention_Through_Immunization_Regional_Reference_Guide.pdf
- 312.Australian Government Department of Health Third National Hepatitis B Strategy. 2018. https://www1.health.gov.au/internet/main/publishing.nsf/Content/ohp-bbvs-1/$File/Hep-B-Third-Nat-Strategy-2018-22.pdf
- 313.Hajarizadeh B, Grebely J, McManus H. Chronic hepatitis C burden and care cascade in Australia in the era of interferon-based treatment. J Gastroenterol Hepatol. 2017;32:229–236. doi: 10.1111/jgh.13453. [DOI] [PubMed] [Google Scholar]
- 314.The Kirby Institute Monitoring hepatitis C treatment uptake in Australia. 2017. https://kirby.unsw.edu.au/sites/default/files/kirby/report/Monitoring-hep-C-treatment-uptake-in-Australia_Iss8-DEC17.pdf
- 315.Australian Government Department of Health Direct acting antiviral medicines for the treatment of chronic hepatitis C. 2019. https://www.pbs.gov.au/info/industry/listing/participants/public-release-docs/2018-09/direct-acting-antiviral-medicines-for-hep-c
- 316.Wilkinson A. Australia's progress towards hepatitis C elimination: annual report 2019. 2019. https://kirby.unsw.edu.au/sites/default/files/_local_upload/others/Australia%27s-progress-on-hepatitis-C-elimination-2019-report.pdf
- 317.National Health and Medical Research Council Australian Government Australian guidelines to reduce health risks from drinking alcohol. 2009. https://www.nhmrc.gov.au/file/1646/download?token=pbOC6GL8329legislation.govt.nz/act/public/2012/0120/45.0/096be8ed80c4777d.pdf
- 318.Australian Bureau of Statistics Apparent consumption of alcohol, Australia, 2013–14. 2015. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Previousproducts/4307.0.55.001Main%20Features62013-14?opendocument&tabname=Summary&prodno=4307.0.55.001&issue=2013-14&num=&view=
- 319.Australian Bureau of Statistics National Health Survey first results: Australia 2014–2015. 2015. https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/CDA852A349B4CEE6CA257F150009FC53/Φle/national%20health%20survey%20first%20results,%202014-15.pdf
- 320.Ridoutt B, Baird D, Bastiaans K. Changes in food intake in Australia: comparing the 1995 and 2011 National Nutrition Survey results disaggregated into basic foods. Foods. 2016;5:40–53. doi: 10.3390/foods5020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Brand-Miller JC, Barclay AW. Declining consumption of added sugars and sugar-sweetened beverages in Australia: a challenge for obesity prevention. Am J Clin Nutr. 2017;105:854–863. doi: 10.3945/ajcn.116.145318. [DOI] [PubMed] [Google Scholar]
- 322.Organisation for Economic Co-operation and Development OECD economic surveys New Zealand. 2019. http://www.oecd.org/economy/surveys/new-zealand-2019-OECD-economic-survey-overview.pdf
- 323.Ministry of Health Hepatitis C. 2019. https://www.health.govt.nz/our-work/diseases-and-conditions/hepatitis-c
- 325.Ministry of Health Improving the health of New Zealanders. 2019. https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/surveys/new-zealand-health-survey/improving-health-new-zealanders#alcohol
- 326.Ministry of Health Childhood obesity plan. 2019. https://www.health.govt.nz/our-work/diseases-and-conditions/obesity/childhood-obesity-plan
- 327.Ministry of Health Eating and activity guidelines for New Zealand adults. 2015. https://www.health.govt.nz/system/files/documents/publications/eating-activity-guidelines-for-new-zealand-adults-oct15_0.pdf
- 328.Ministry of Health Physical activity. 2017. https://www.health.govt.nz/our-work/preventative-health-wellness/physical-activity
- 329.Ministry of Health Clinical Guidelines for Weight Management in New Zealand Adults. 2018. https://www.health.govt.nz/publication/clinical-guidelines-weight-management-new-zealand-adults
- 330.Ministry of Health Clinical Guidelines for Weight Management in New Zealand Children and Young People. 2016. https://www.health.govt.nz/system/files/documents/publications/clinical-guidelines-weight-management-nz-children-young-people-dec16.pdf
- 331.Ministry of Health Fruit in Schools programme. 2017. https://www.health.govt.nz/our-work/life-stages/child-health/fruit-schools-programme
- 332.Ministry of Health How the Green Prescription works. 2017. https://www.health.govt.nz/our-work/preventative-health-wellness/physical-activity/green-prescriptions/how-green-prescription-works
- 333.Ministry of Health Active Families. 2018. https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/green-prescriptions/active-families
- 334.Theseira L. Singapore: healthcare overview. 2015. files.export.gov/x_5985.pdf
- 335.Ministry of Health Singapore Drug subsidies & schemes. 2019. https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/drug-subsidies-schemes
- 336.Liquor control (supply and consumption) act 2015. 2015. https://sso.agc.gov.sg/Act/LCSCA2015
- 337.Lee BL. Dietary guidelinies in Singapore. Asia Pac J Clin Nutr. 2011;20:472–476. [PubMed] [Google Scholar]
- 338.Health Promotion Board National physical activity guidelines: summary guide for professionals. 2011. https://www.healthhub.sg/sites/assets/Assets/PDFs/HPB/PhysicalActivityPDFs/NPAG_Summary_Guide.pdf
- 339.Health Promotion Board The CHERISH Award. 2018. https://www.hpb.gov.sg/article/the-cherish-award
- 340.MyKenzen Healthy canteen program. http://www.mykenzen.com/whp-nutrition-services/507-healthy-canteen-program.html
- 341.The Singapore Contractors Association Circular: Health Promotion Board (HPB)–Singapore HEALTH Award 2017. 2017. https://www.scal.com.sg/info-details/hpb-Singapore-HEALTH-Award-2017/
- 342.Health Promotion Board Healthy Meals in Schools Programme. 2019. https://www.hpb.gov.sg/schools/school-programmes/healthy-meals-in-schools-programme
- 343.Lee W. Fighting fat: with TAF in Singapore. Diabetes Voice. 2003;48:49–50. [Google Scholar]
- 344.Health Promotion Board Healthier Dining Programme extended to include food in hawker centres and coffee shops. 2018. https://www.hpb.gov.sg/article/healthier-dining-programme-extended-to-include-food-in-hawker-centres-and-coffee-shops
- 345.Health Promotion Board Physical activity programmes. 2018. https://www.hpb.gov.sg/healthy-living/physical-activity/physical-activity-programmes
- 346.National Health Insurance Administration Ministry of Health and Welfare Conditional inclusion of oral drug treatment for hepatitis C in the national health insurance coverage as of January 24, 2017. 2017. https://www.nhi.gov.tw/english/News_Content.B4B5DC48343&sms=F0EAFEB716DE7FFA&s=5B9044CF1188EE23
- 347.Ministry of Justice. Ministry of Health and Welfare. Ministry of Education 2016 anti-drug report. https://www.fda.gov.tw/tc/includes/GetFile.ashx?id=f636694179152393293
- 348.Chiang CJ, Yang YW, Chen JD. Significant reduction in end-stage liver diseases burden through the national viral hepatitis therapy program in Taiwan. Hepatology. 2015;61:1154–1162. doi: 10.1002/hep.27630. [DOI] [PubMed] [Google Scholar]
- 349.WHO Health data and health information systems in the Western Pacific. http://www.wpro.who.int/health_services/health_service_delivery_profiles/en/
- 350.Huang JF, Wang HB, Zheng SS. Advances in China's organ transplantation achieved with the guidance of law. Chin Med J (Engl) 2015;128:143–146. doi: 10.4103/0366-6999.149183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Wang H, Jiang W, Zhou Z, Long J, Li W, Fan ST. Liver transplantation in mainland China: the overview of CLTR 2011 annual scientific report. Hepatobiliary Surg Nutr. 2013;2:188–197. doi: 10.3978/j.issn.2304-3881.2013.08.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Central Bureau of Health Intelligence National Health Profile 2018 13th issue. 2018. http://www.cbhidghs.nic.in/Ebook/National%20Health%20Profile-2018%20(e-Book)/files/assets/common/downloads/files/NHP%202018.pdf
- 353.Rana SA, Sarfraz M, Kamran I, Jadoon H. Preferences of doctors for working in rural Islamabad capital territory, Pakistan: a qualitative study. J Ayub Med Coll Abbottabad. 2016;28:591–596. [PubMed] [Google Scholar]
- 354.Nishtar S. The Gateway Paper: health systems in Pakistan, a way forward. J Pak Psychiatric Soc. 2006;3:54. [Google Scholar]
- 355.Akbari AH, Rankaduwa W, Kiani AK. Demand for public health care in Pakistan. Pakistan Dev Rep. 2009;48:141–153. [Google Scholar]
- 356.Kurji Z, Premani ZS, Mithani Y. Analysis of the health care system of Pakistan: lessons learnt and the way forward. J Ayub Med Coll Abbottabad. 2016;28:601–604. [PubMed] [Google Scholar]
- 357.Hafeez Bhatti AB, Saud Dar F. Living donor liver transplantation in Pakistan. Transplantation. 2017;101:1507–1508. doi: 10.1097/TP.0000000000001737. [DOI] [PubMed] [Google Scholar]
- 358.Constitution (Eighteenth Amendment) Act, 2010. 2010. http://www.pakistani.org/pakistan/constitution/amendments/18amendment.html
- 359.Ahmed SM, Alam BB, Anwar I. Bangladesh health system review. 2015. http://apps.searo.who.int/PDS_DOCS/B5409.pdf
- 360.Matsuda S. Health policy in Japan–current situation and future challenges. JMA J. 2019;2:1–10. doi: 10.31662/jmaj.2018-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Japan International Cooperation Agency Japan's experience with human resources and health policies. 2013. https://www.jica.go.jp/english/news/field/2013/c8h0vm00006f7nc3-att/20130619_01.pdf
- 362.Organisation for Economic Co-operation and Development Health care resources. 2019. https://stats.oecd.org/index.aspx?DataSetCode=HEALTH_REAC#
- 363.Training and certifying medical specialists. 2018. https://www.japantimes.co.jp/opinion/2018/04/15/editorials/training-certifying-medical-specialists/#.W0M7o9UzbIU
- 364.Lee SG, Moon DB, Hwang S. Liver transplantation in Korea: past, present, and future. Transplant Proc. 2015;47:705–708. doi: 10.1016/j.transproceed.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 365.World Bank Physicians (per 1000 people)–Australia. 2019. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=AU
- 366.World Bank Nurses and midwives (per 1000 people)–Australia. 2019. https://data.worldbank.org/indicator/SH.MED.NUMW.P3?locations=AU
- 367.WHO WHO global health workforce statistics database. 2018. http://www.who.int/hrh/statistics/hwfstats/
- 368.Cumming J, McDonald J, Barr C, Martin G, Gerring Z, Daube J. World Health Organization; Manila: 2014. New Zealand health system review. [Google Scholar]
- 369.Kwon JA, Dore GJ, Grebely J. Australia on track to achieve WHO HCV elimination targets following rapid initial DAA treatment uptake: a modelling study. J Viral Hepat. 2019;26:83–92. doi: 10.1111/jvh.13013. [DOI] [PubMed] [Google Scholar]
- 370.McCaughan GW, Munn SR. Liver transplantation in Australia and New Zealand. Liver Transpl. 2016;22:830–838. doi: 10.1002/lt.24446. [DOI] [PubMed] [Google Scholar]
- 371.Chart of the day: Singapore's number of doctors lower range for developed countries. 2018. https://sbr.com.sg/healthcare/news/chart-day-singapores-number-doctors-in-lower-range-developed-countries
- 372.Ministry for Communications and Information Singapore Smart Health-Assist. https://www.mci.gov.sg/∼/media/mcicorp/doc/infocomm%20media%20prelim%20ideas/smart%20health-assist.pdf?la=en
- 373.Ministry for Communications and Information Singapore Infocomm meda 2025. https://www.mci.gov.sg/∼/media/data/mci/docs/imm%202025/infocomm%20media%202025%20full%20report.pdf
- 374.EDB Singapore How Singapore is working towards a healthier tomorrow–smartly. 2017. https://www.edb.gov.sg/en/news-and-events/insights/innovation/how-singapore-is-working-towards-a-healthier-tomorrow-smartly.html
- 375.Muthiah M, Chong CH, Lim SG. Liver disease in Singapore. Euroasian J Hepatogastroenterol. 2018;8:66–68. doi: 10.5005/jp-journals-10018-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Prabhakar KS. Cadaveric & living organ donation. Natural limitations. Possible solutions. Singapore experience. Ann Transplant. 2004;9:31–33. [PubMed] [Google Scholar]
- 377.Singapore Government Human Organ Transplant (amendment) Act 2009. 2009. https://sso.agc.gov.sg/Acts-Supp/14-2009/Published/20090415?DocDate=20090415
- 378.Ministry of Health Singapore The Medical (therapy, education and research) Act (MTERA) 2019. https://www.moh.gov.sg/policies-and-legislation/the-medical-(therapy-education-and-research)-act-(mtera)
- 379.Cheng T-M. Taiwan's health care system: the next 20 years. 2015. https://www.brookings.edu/opinions/taiwans-health-care-system-the-next-20-years/
- 380.Pillai VG, Chen CL. Living donor liver transplantation in Taiwan–challenges beyond surgery. Hepatobiliary Surg Nutr. 2016;5:145–150. doi: 10.3978/j.issn.2304-3881.2015.08.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Long Q, Xu L, Bekedam H, Tang S. Changes in health expenditures in China in 2000s: has the health system reform improved affordability. Int J Equity Health. 2013;12:40. doi: 10.1186/1475-9276-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Liang X, Guo H, Jin C, Peng X, Zhang X. The effect of new cooperative medical scheme on health outcomes and alleviating catastrophic health expenditure in China: a systematic review. PLoS One. 2012;7 doi: 10.1371/journal.pone.0040850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Yang W. China's new cooperative medical scheme and equity in access to health care: evidence from a longitudinal household survey. Int J Equity Health. 2013;12:20. doi: 10.1186/1475-9276-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Yi H, Zhang L, Singer K, Rozelle S, Atlas S. Health insurance and catastrophic illness: a report on the New Cooperative Medical System in rural China. Health Econ. 2009;18(suppl 2):S119–S127. doi: 10.1002/hec.1510. [DOI] [PubMed] [Google Scholar]
- 385.Wang HHX, Wang JJ, Zhou ZH, Wang XW, Xu L. General practice education and training in southern China: recent development and ongoing challenges under the health care reform. Malays Fam Physician. 2013;8:2–10. [PMC free article] [PubMed] [Google Scholar]
- 386.Weng S, Gao S. A new account of rural drinking water safety. 2011. http://finance.sina.com.cn/chanjing/sdbd/20110908/090010452522.shtml (in Chinese).
- 387.Lim SG, Amarapurkar DN, Chan HL. Reimbursement policies in the Asia-Pacific for chronic hepatitis B. Hepatol Int. 2015;9:43–51. doi: 10.1007/s12072-014-9593-x. [DOI] [PubMed] [Google Scholar]
- 388.National Healthcare Security Administration National drug catalogue for basic medical insurance, work-related injury insurance and maternity insurance. 2019. http://www.nhsa.gov.cn/art/2019/8/20/art_37_1666.html
- 389.Bian DD, Zhou HY, Liu S. Current treatment status and barriers for patients with chronic HCV infection in mainland China: a national multicenter cross-sectional survey in 56 hospitals. Medicine (Baltimore) 2017;96 doi: 10.1097/MD.0000000000007885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Lim SG, Aghemo A, Chen PJ. Management of hepatitis C virus infection in the Asia-Pacific region: an update. Lancet Gastroenterol Hepatol. 2017;2:52–62. doi: 10.1016/S2468-1253(16)30080-2. [DOI] [PubMed] [Google Scholar]
- 391.Zu J, Li M, Zhuang G. Estimating the impact of test-and-treat strategies on hepatitis B virus infection in China by using an age-structured mathematical model. Medicine (Baltimore) 2018;97:e0484. doi: 10.1097/MD.0000000000010484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Major initiatives: Swachh Bharat Mission. www.pmindia.gov.in/en/major_initiatives/swachh-bharat-abhiyan
- 393.India Today Is India really open defecation free? 2019. https://www.indiatoday.in/india/story/is-india-really-open-defecation-free-1605716-2019-10-02
- 394.Kapoor D, Saxena R, Sood B, Sarin SK. Blood transfusion practices in India: results of a national survey. Indian J Gastroenterol. 2000;19:64–67. [PubMed] [Google Scholar]
- 395.Makroo RN, Choudhury N, Jagannathan L. Multicenter evaluation of individual donor nucleic acid testing (NAT) for simultaneous detection of human immunodeficiency virus -1 & hepatitis B & C viruses in Indian blood donors. Indian J Med Res. 2008;127:140–147. [PubMed] [Google Scholar]
- 396.Rajasekaran M, Sivagnanam G, Thirumalaikolundusubramainan P, Namasivayam K, Ravindranath C. Injection practices in southern part of India. Public Health. 2003;117:208–213. doi: 10.1016/S0033-3506(03)00065-9. [DOI] [PubMed] [Google Scholar]
- 397.Anand K, Pandav CS, Kapoor SK. Injection use in a village in north India. Natl Med J India. 2001;14:143–144. [PubMed] [Google Scholar]
- 398.Patel DA, Gupta PA, Kinariwala DM, Shah HS, Trivedi GR, Vegad MM. An investigation of an outbreak of viral hepatitis B in Modasa town, Gujarat, India. J Glob Infect Dis. 2012;4:55–59. doi: 10.4103/0974-777X.93762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Sukriti, Pati NT, Sethi A. Low levels of awareness, vaccine coverage, and the need for boosters among health care workers in tertiary care hospitals in India. J Gastroenterol Hepatol. 2008;23:1710–1715. doi: 10.1111/j.1440-1746.2008.05483.x. [DOI] [PubMed] [Google Scholar]
- 400.Mall ML, Rai RR, Philip M. Seroepidemiology of hepatitis A infection in India: changing pattern. Indian J Gastroenterol. 2001;20:132–135. [PubMed] [Google Scholar]
- 401.Khanna S, Vohra P, Jyoti R. Changing epidemiology of acute hepatitis in a tertiary care hospital in Northern India. Indian J Gastroenterol. 2006;25:101–102. [PubMed] [Google Scholar]
- 402.Aggarwal R, Chen Q, Goel A. Cost-effectiveness of hepatitis C treatment using generic direct-acting antivirals available in India. PLoS One. 2017;12 doi: 10.1371/journal.pone.0176503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Bhushan R, Bailay R, Sanandakumar S. In a first, Kerala imposes 14·5% ‘fat tax’ on junk food. 2016. http://economictimes.indiatimes.com/news/politics-and-nation/in-a-first-kerala-imposes-14–5-fat-tax-on-junk-food/articleshow/53113799.cms
- 404.WHO . World Health Organization; Geneva: 2015. Draft global health sector strategy on viral hepatitis, 2016–2021. [Google Scholar]
- 405.Jahan M, Islam MA, Akbar SM. Anti-HBc screening of blood donors in Bangladesh: relevance to containment of HBV propagation. J Clin Exp Hepatol. 2016;6:115–118. doi: 10.1016/j.jceh.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Mahtab MA, Rahman S, Khan M, Karim F, Sharif NM, Shrestha A. Genotypes of HCV in Bangladesh: experience from a tertiary centre. Hungarian Med J. 2008;2:577–581. [Google Scholar]
- 407.Uz-Zaman MH, Rahman A, Yasmin M. Epidemiology of hepatitis B virus infection in Bangladesh: prevalence among general population, risk groups and genotype distribution. Genes. 2018;9:E541. doi: 10.3390/genes9110541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Mahmud S, Hussain M, Ahmed SS, Rahman M, Tasneem F, Afroz M. Burden of HCV in Bangladesh: warrants the screening of blood donors. Acad J Ped Neonatol. 2017;4 [Google Scholar]
- 409.Kim DY, Han KH, Jun B. Estimating the cost-effectiveness of one-time screening and treatment for hepatitis C in Korea. PLoS One. 2017;12 doi: 10.1371/journal.pone.0167770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Park J, Shin A, Lee M. Prevalence of participating in physical activity from 2 Korean surveillance systems: KNHANES and KCHS. J Phys Act Health. 2018;15:763–773. doi: 10.1123/jpah.2017-0428. [DOI] [PubMed] [Google Scholar]
- 411.Tran BT, Jeong BY, Oh J-K. The prevalence trend of metabolic syndrome and its components and risk factors in Korean adults: results from the Korean National Health and Nutrition Examination Survey 2008–2013. BMC Public Health. 2017;17:71. doi: 10.1186/s12889-016-3936-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Yoon SK, Chun HG. Status of hepatocellular carcinoma in South Korea. Chin Clin Oncol. 2013;2:39. doi: 10.3978/j.issn.2304-3865.2013.11.08. [DOI] [PubMed] [Google Scholar]
- 413.Sievert K, O'Neill P, Koh Y, Lee JH, Dev A, Le S. Barriers to accessing testing and treatment for chronic hepatitis B in Afghan, Rohingyan, and South Sudanese populations in Australia. J Immigr Minor Health. 2018;20:140–146. doi: 10.1007/s10903-017-0546-z. [DOI] [PubMed] [Google Scholar]
- 414.Carson PJ. Providing specialist services in Australia across barriers of distance and culture. World J Surg. 2009;33:1562–1567. doi: 10.1007/s00268-009-0088-1. [DOI] [PubMed] [Google Scholar]
- 415.Gruen RL, Bailie RS, Wang Z, Heard S, O'Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. Lancet. 2006;368:130–138. doi: 10.1016/S0140-6736(06)68812-0. [DOI] [PubMed] [Google Scholar]
- 416.Garne DL, Perkins DA, Boreland FT, Lyle DM. Frequent users of the Royal Flying Doctor Service primary clinic and aeromedical services in remote New South Wales: a quality study. Med J Aust. 2009;191:602–604. doi: 10.5694/j.1326-5377.2009.tb03344.x. [DOI] [PubMed] [Google Scholar]
- 417.Australian Institute of Health and Welfare Medical workforce 2011. 2013. https://www.aihw.gov.au/getmedia/1a9d981d-a5a5-4bac-b8fc-f885deb3a01c/14395-20130409.pdf.aspx
- 418.Rankin SL, Hughes-Anderson W, House AK, Heath DI, Aitken RJ, House J. Costs of accessing surgical specialists by rural and remote residents. ANZ J Surg. 2001;71:544–547. doi: 10.1046/j.1440-1622.2001.02188.x. [DOI] [PubMed] [Google Scholar]
- 419.Robinson M, Slaney GM, Jones GI, Robinson JB. GP Proceduralists: ‘the hidden heart’ of rural and regional health in Australia. Rural Remote Health. 2010;10 [PubMed] [Google Scholar]
- 420.O'Sullivan BG, Joyce CM, McGrail MR. Adoption, implementation and prioritization of specialist outreach policy in Australia: a national perspective. Bull World Health Organ. 2014;92:512–519. doi: 10.2471/BLT.13.130385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Alavi M, Law MG, Grebely J. Time to decompensated cirrhosis and hepatocellular carcinoma after an HBV or HCV notification: a population-based study. J Hepatol. 2016;65:879–887. doi: 10.1016/j.jhep.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 422.Patel M, Phillips-Caesar E, Boutin-Foster C. Barriers to lifestyle behavioral change in migrant South Asian populations. J Immigr Minor Health. 2012;14:774–785. doi: 10.1007/s10903-011-9550-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Wai CT, Mak B, Chua W, Lim SG. The majority of hepatitis B carriers are not on regular surveillance in Singapore. Singapore Med J. 2004;45:423–426. [PubMed] [Google Scholar]
- 424.Wai CT, Mak B, Chua W. Misperceptions among patients with chronic hepatitis B in Singapore. World J Gastroenterol. 2005;11:5002–5005. doi: 10.3748/wjg.v11.i32.5002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Wait S, Chen DS. Towards the eradication of hepatitis B in Taiwan. Kaohsiung J Med Sci. 2012;28:1–9. doi: 10.1016/j.kjms.2011.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.WHO First-ever WHO list of essential diagnostic tests to improve diagnosis and treatment outcomes. 2018. https://www.who.int/news-room/detail/15-05-2018-first-ever-who-list-of-essential-diagnostic-tests-to-improve-diagnosis-and-treatment-outcomes
- 427.Williams R, Aspinall R, Bellis M. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet Gastroenterol Hepatol. 2014;384:1953–1997. doi: 10.1016/S0140-6736(14)61838-9. [DOI] [PubMed] [Google Scholar]
- 428.WHO Egypt steps up efforts against hepatitis C. 2014. http://www.who.int/features/2014/egypt-campaign-hepatitisc/en/
- 429.WHO Georgia sets sights on eliminating hepatitis C. 2015. http://www.euro.who.int/en/countries/georgia/news/news/2015/07/georgia-sets-sights-on-eliminating-hepatitis-c
- 430.Malaysia Ministry of Health . Malaysia Ministry of Health; Kuala Lumpur: 2014. Malaysia 2014 country response to HIV/AIDS. Reporting period: January 2013 to December 2013. [Google Scholar]
- 431.WHO Alcohol initiative. http://www.wpro.who.int/mongolia/mediacentre/alcohol/en/
- 432.WHO . World Health Organization; Geneva: 2010. Global strategy to reduce the harmful use of alcohol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.UN Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. 2012. http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf
- 434.Hagström H, Nasr P, Ekstedt M. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol Commun. 2017;2:48–57. doi: 10.1002/hep4.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.WHO Global Action Plan for the Prevention and Control of NCDs 2013–2020. 2019. http://www.who.int/nmh/events/ncd_action_plan/en/
- 436.World Trade Organization Declaration on the TRIPS agreement and public health. 2001. https://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm
- 437.WHO Health systems financing. https://www.who.int/healthsystems/topics/financing/en/
- 438.Heller PS. The prospects of creating ‘fiscal space’ for the health sector. Health Policy Plan. 2006;21:75–79. doi: 10.1093/heapol/czj013. [DOI] [PubMed] [Google Scholar]
- 439.Taskforce on Innovative International Financing for Health Systems More money for health, and more health for the money. 2009. http://www.internationalhealthpartnership.net//CMS_files/documents/taskforce_report_EN.pdf
- 440.McCoy D, Brikci N. Taskforce on Innovative International Financing for Health Systems: what next? 2010. https://www.who.int/bulletin/volumes/88/6/09-074419/en/ [DOI] [PMC free article] [PubMed]
Uncited Reference
- 324.New Zealand Government Sale and Supply of Alcohol Act 2012. 2012. http://www.legislation.govt.nz/act/public/2012/0120/latest/DLM3339333.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.