1. Introduction
The novel coronavirus (SARS-CoV-2, COVID-19) was first identified in the province of Wuhan, China in December 2019 [1], following the emergence of new cases of pneumonia of unknown etiology. Since then, the manifestations of COVID-19 infections have ranged from asymptomatic to severe respiratory infections, with increased morbidity in older adults including those with co-morbidities and cancer [2,3]. Presently, global mortality is reported at 4.7%, but this varies widely by location, from 0.7% in Germany to 10.8% in Italy [4]. As of April 13, 2020, the number of infections continues to rise well beyond the 1.9 million cases, and approximately 120,000 COVID-19-related deaths that have already occurred globally [5].
Multiple myeloma (MM) is a malignant plasma cell dyscrasia which predominantly affects older and often frail adults. Although tremendous gains have been made for older adults with MM, infections, including respiratory infections, significantly impact the rate of early mortality in these patients [6,7]. Furthermore, older adults with MM have age-associated vulnerabilities leading to heterogeneity in outcomes [8]. The complexity of caring for older patients have increased substantially during this pandemic, due to concern about their risk of severe morbidity of COVID19 infection. Optimal strategies for these patients will involve staging the malignancy/aging, while simultaneously considering the local prevalence of COVID-19 infection. Herein, we discuss strategies for the risk reduction of COVID-19 transmission, treatment stratification of anti-myeloma therapy and discussion regarding goals of care for older adults with MM during the COVID-19 pandemic.
2. Risk Reduction Strategies of COVID-19 Transmission
Currently there is an absence of data regarding both the prevalence and outcomes for older adults with MM exposed to COVID-19. In non-cancer patients, chronological age has emerged as a risk-factor for poor outcomes with COVID-19, although there is wide variation in the estimates presented. Early estimates from China suggest an overall case fatality rate of 2%, increasing to 8% for those aged 70–79 years and 15% for those ≥80 years of age [1]. Recent estimates from an Italian series of 1591 patients admitted to the intensive care unit demonstrated that older adults (n = 786; age ≥ 64 years) had higher mortality compared to younger patients (n = 795; age ≤ 63 years) (36% vs 15%; difference, 21%, 95% Confidence Interval [CI], 17%–26%; P < .001) [9]. Similarly, in the United States, during March 1–28, 2020, the laboratory-confirmed COVID-19–associated hospitalization rate was 4.6 per 100,000 population with the highest rates among adults aged ≥65 years [10]. Increased number of overall comorbidities, including cardiovascular disease, diabetes, hypertension, chronic obstructive lung disease, accounted for the majority of severe COVID-19 infections and associated deaths [3,10,11]. Additionally, patients with increasing number of co-morbidities had worse outcomes [11], supporting the premise that the accumulation of vulnerabilities increases the risk of death, as is expected with other serious infections. Unfortunately, no data is available yet regarding other underlying geriatric impairments, such as functional dependence, in these patients.
With regards to prevalence/outcomes of the COVID-19 in adults with MM, there is a paucity of data and, apart from case reports [12], estimates need to be extrapolated from case series published for other patients with cancer [2,13,14] and accumulating clinical experience with patients with MM during this time. Most recently, Dai et al published a cohort of 338 hospitalized patients (n = 105 with cancer, n = 233 without cancer) which revealed that adults with cancer had a higher probability of death (Odds Ratio [OR] 2·88, 95% CI 1·20–6·89; P = 0·02), intensive care unit admission (OR 2·38, 95% CI 1·23–4·61; P = 0·01), or at least one severe or critical symptom (OR 2·60, 95% CI 1·53–4.41; P < 0·01) compared to those without cancer [14]. Another retrospective case series, identified anti-tumour receipt within the last 14 days as a significant risk factor for severe events defined as a condition requiring admission to an intensive care unit, the use of mechanical ventilation, or death (Hazard Ratio = 4.08, 95% CI 1.09–15.32; P = .04) [2].
The above estimates yield the assumption that older adults with myeloma are at increased risk for poor outcomes due to a combination of demographics (older chronological age at diagnosis which is associated with increased co-morbidities and additional age-related vulnerabilities), disease-related (higher risk of secondary immunodeficiency [15]) and treatment-related (anti-myeloma regimens that often require continuous administration) factors. While data confirming this assumption are needed, every effort should be made to decrease the risk of COVID-19 exposure in this patient population.
Physical distancing is the most pivotal and effective component of mitigating the risk. One of the great challenges of this pandemic has been limitations in access to testing for the virus, a barrier which, in concert with the risk of asymptomatic individuals can transmit the virus, has led to a situation where physical interaction with the healthcare system may present a patient's greatest risk for exposure to the virus. Until widespread testing is available, efforts should be made to decrease physical contact with the health care system [16]. Despite physical distance, continued contact with the health care system via audio or video technologies is imperative to ensure ongoing care is provided during this time of increased vulnerability. Disparities in both access and ability to utilize these advanced technologies among older adults needs to be recognized and, whenever possible, strategies devised to mitigate them. Alongside virtual visits, additional innovative strategies such as bloodwork-monitoring at home/local laboratories or couriering of medications to patients' home may also be required to further minimize risks. While risk-reduction strategies for COVID-19 should be emphasized, efforts should also be made to identify and address any other geriatric impairments such as nutrition, fall-risk, medication adherence, and mental-well-being using a multidisciplinary approach.
3. Treatment Stratification for Anti-Myeloma Therapy
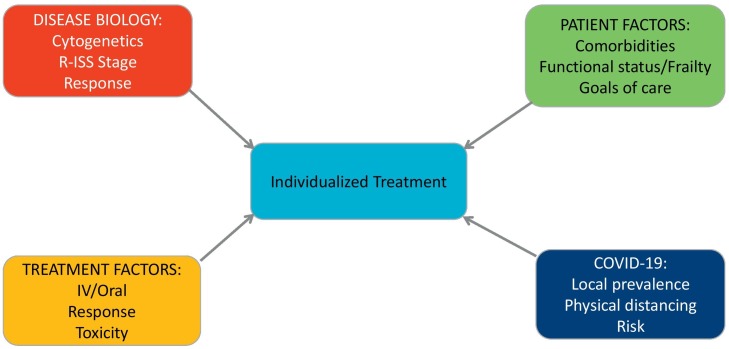
As clinicians struggle with optimizing care of older adults with MM during this pandemic, decisions regarding dose-reduction, regimen modification/interruption or continuation of therapy will need to be individualized based upon the concept of ‘staging the disease’ as well as ‘staging the aging,’ while adding in the complexity of the COVID pandemic.
‘Staging the disease,’ utilizing cytogenetics, Revised-International Staging System and response assessment, continues to hold prognostic value in older adults with NDMM [17,18] and therefore should inform treatment decision-making during this time. In addition, tremendous progress has been made over the past decade in understanding the heterogeneity of aging beyond chronological age alone, termed ‘staging the aging’. In MM, simple performance measures like Eastern Cooperative Oncology Group Performance Status (ECOG PS) contributes to the prognosis in older patients [19], but beyond ECOG PS, frailty (defined as the complex syndrome of physiological decline that increases vulnerability [20]) is a pivotal factor affecting outcomes in older patients, including progression-free survival, hospitalization, treatment-related toxicity, and overall survival [[21], [22], [23], [24]].
Myeloma-specific frailty indices, such as the International Myeloma Working Group frailty index and the Revised Myeloma Co-Morbidity Index, have emerged as powerful tools in the ‘personalization’ of therapy for older adults by identifying those ‘fit’ individuals who may benefit from more aggressive treatment measures while simultaneously identifying ‘frail’ patients at high-risk for adverse events [23,24]. Simple physical performances measures like the 4-meter walk test have also emerged as important strategies for risk-stratification of individuals with hematological malignancies, including MM [25]; however, require in-person assessment. Unfortunately, limited data exists on self-reported physical performance measures [26], which can potentially be done during virtual appointments, among patients with MM.
While none of the above tools for staging the disease or aging were devised or have been validated to account for the unexpected challenges of COVID-19, they can be utilized for conceptualizing the treatment of older adults with MM during this challenging time. Additionally, multiple international agencies have circulated guidance documents which are helpful as well [[27], [28], [29]]. Given the paucity of evidence-based data, treatment decisions need to be individualized as outlined in Fig. 1 while taking into account the rapid changes in COVID-19 risk in each geographic area. Potential strategies during this time are outlined below; however, the risk/benefit ratio will need to be carefully evaluated for each individual:
-
•
Timing of therapy initiation: Consider the timing of therapy initiation for both newly-diagnosed and relapsed patients. If possible, consider delaying with close follow-up if there is no imminent risk to the patients, such as diagnosis by SLiM criteria without any end organ damage [30] or the case of slow biochemical relapse. In the relapsed setting, the clinician should weigh the risk of increased patient interaction with the healthcare system due to a therapeutic change against the rate of progression [i.e. biologic progression, doubling time of paraprotein vs progression resulting in worsening end organ damage].
-
•
Transplant: Consider delaying autologous stem cell transplant (ASCT) for a finite period of time or, depending upon circumstances, omitting upfront ASCT for older adults with MM [28,31]. Additional cycles of the induction drug regimens may be continued in the interim; however, careful attention should be paid to ensure these do not affect the ability to subsequently harvest stem cells. If it is not possible to delay ASCT, then consideration should be given to screening patients for COVID-19 before both stem cell procurement and prior to ASCT in accordance with established guidelines (e.g. ASTC and EBMT) [30,33].
-
•
Drug regimens: While triplet regimens using a combination of drugs has led to significant improvements in outcomes for both transplant-eligible and -ineligible older adults, careful consideration will need to be given to regimen selection at this time weighing the risks/benefits. Patients with uncontrolled disease will need to be managed with appropriate anti-myeloma therapy to prevent myeloma-related morbidity or mortality. Given the significant burden on resources, health care providers will need to advocate for this patient group to ensure access to appropriate therapy, access to care, and management of toxicities.
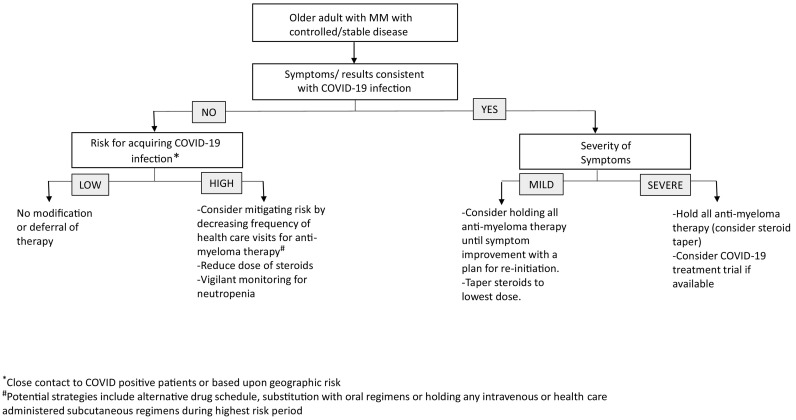
For adults with MM that is well-controlled, regimens that are well-tolerated should generally be continued, depending upon the presumed risk/severity of COVID-19 infection as outlined in Fig. 2 . If new regimens are employed, consideration should be given to orally-administered therapy, while remaining vigilant regarding any barriers affecting medication adherence. During any therapy switch or initiation, efforts should be made to decrease the risk of treatment-related adverse events, which can lead to dose reduction or cessation of therapy altogether, which is associated with poor outcomes [32]. Drug regimens associated with higher baseline risk of pulmonary toxicity need to be carefully considered in each individual case, weighing the pros and cons of therapy. Given the potential immunosuppressive effects of steroids, consideration should be given to lower doses or cessation of these agents. Additionally, given the decreased donation pool of blood products, efforts should be made to minimize therapy with may require platelet or red blood cell transfusions.
-
•
Supportive Care: While supportive care measures are a key component in the care of older adults, the risk versus benefit ratio will need to be carefully considered as many of these therapies may paradoxically increase contact with health care. Bisphosphonates such as zoledronate may be held for patients with stable disease and in the absence of significant bone related-disease. Additionally, efforts should be made to decrease risk of neutropenia using growth factor support, which, again, will need to be weighed against any increase in physical exposure to the health care system. Clinicians should be aware of risks of polypharmacy if additional supportive care medications, such as antibacterial or antiemetic prophylaxis, are added during this time. Efforts should be made to decrease other infectious risk factors for adults with MM by ensuring that other recommended vaccinations such as pneumococcal vaccines are administered.
-
•
Clinical Trials: Considerable effort has been made over the past few years in highlighting the disparities in access to clinical trials in older adults with MM [33]. As many new clinical trials for MM have halted or slowed enrollment, clinicians will need to advocate for patients in accessing bridging therapy during this time for disease control, with the hope that trial access will be available in the near future. Institution-, trial- and sponsor-specific protocol modification will need to be followed during this time. For older adults with MM, who do unfortunately have COVID-19-related complications, clinical trials for the prevention/management of the infection should be considered where appropriate.
Fig. 1.
Conceptual approach for care of older adults with multiple myeloma during the COVID-19 Pandemic.
Fig. 2.
Guidance for anti-myeloma therapy in older adults with stable multiple myeloma during the COVID-19 Pandemic.
4. Goals-of-Care Discussion
It is inevitable that some older adults with MM will face insurmountable challenges in the upcoming few months with the possibility of morbidity and mortality. Oncology providers will need to engage in effective communication strategies regarding decision-making for both individual treatment trajectory as well as end-of-life conversations. Alternative and innovative methods of communication may need to be employed, such as multi-person video conferencing, to decrease the burden of social isolation by ensuring caregivers and other loved ones can participate during these difficult discussions. Documentation regarding goals-of-care should be clearly outlined and easily retrievable during a crisis situation, to ensure that any treatment goals are managed according to individual patient preferences.
5. Forging Ahead
In conclusion, as both clinicians and older adults with MM face this challenging time, shared decision-making has never been more important to personalize treatment during this pandemic, focusing on disease status as well as any aging-associated vulnerabilities. To further address the unique challenges faced by adults with MM and COVID-19 infection, ongoing efforts for collating data, such as those by the American Society of Hematology's Research Collaborative data hub COVID-19 Registry and the international COVID-19 and Cancer Consortium database, will be critical to filling the existing knowledge gaps about the epidemiology and outcomes of COVID-19 for subgroups of patients [34,35]. Additionally, building new and innovative research platforms globally will allow us to not only meet the challenge of this pandemic but to also inform strategies for any future health care challenges among older adults with cancer.
Acknowledgments
Acknowledgement
Dr. Kah Poh (Melissa) Loh for her Editorial review.
Author contributions
| Study concepts | Mian, Wildes |
| Study design | Mian, Wildes |
| Data acquisition | Mian, Wildes |
| Quality control of data and algorithms | Mian, Wildes |
| Data analysis and interpretation | Mian, Grant, Engelhardt, Pawlyn, Bringhen, Zweegman, Stege, Rosko, von Lilienfeld-Toal, Wildes |
| Statistical analysis | Mian, Grant, Engelhardt, Pawlyn, Bringhen, Zweegman, Stege, Rosko, von Lilienfeld-Toal, Wildes |
| Manuscript preparation | Mian, Grant, Engelhardt, Pawlyn, Bringhen, Zweegman, Stege, Rosko, von Lilienfeld-Toal, Wildes |
| Manuscript editing | Mian, Grant, Engelhardt, Pawlyn, Bringhen, Zweegman, Stege, Rosko, von Lilienfeld-Toal, Wildes |
| Manuscript review | Mian, Grant, Engelhardt, Pawlyn, Bringhen, Zweegman, Stege, Rosko, von Lilienfeld-Toal, Wildes |
Funding/conflict of interest
HM: Honoraria/Consultancy fees: Amgen, Celgene, Takeda, Janssen, Sanofi.
SJG:receives research support from National Heart Lung and Blood Institute (Grant No: 5T32HL007093), PI: Janis L. Abkowitz.
ME: Grant support from German Cancer Aid (DKH).
CP: Honoraria/Consultancy fees: Amgen, Celgene, Takeda, Janssen.
SB: reports honoraria from Amgen, Bristol-Myers Squibb, Celgene, and Janssen; and reports a consultancy/advisory role for Celgene, Janssen, Karyopharm, and Takeda.
SZ: research support from Janssen, Celgene and Takeda; serves in advisory boards for Janssen, Celgene and Takeda.
CS: No conflicts reported.
AR: Research Funding: Janssen, Regeneron, Millenium.
MLT: Honoraria/Consulting fees: Celgene, Janssen, Takeda, Amgen, Oncopeptides, Cancer Drug Development Forum, Gilead, Merck, BMS, Research Funding: Celgene, Gilead, Novartis, Deutsche Krebshilfe (German Cancer Aid).
TW: Research Funding: Janssen; Consulting: Carevive Systems, Seattle Genetics.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L., Zhu F., Xie L., Wang C., Wang J., Chen R., et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020 Mar 26 doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang L., He W., Yu X., Hu D., Bao M., Liu H., et al. Coronavirus Disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020 Mar;30 doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omer S.B., Malani P., Del Rio C. The COVID-19 pandemic in the US: a clinical update. JAMA. 2020 Apr;6 doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- 5.Coronavirus Resource Center: John Hopkins University and Medicine https://coronavirus.jhu.edu/map.html [accessed 13 April 2020]
- 6.Holmstrom M.O., Gimsing P., Abildgaard N., Andersen N.F., Helleberg C., Clausen N.A., et al. Causes of early death in multiple myeloma patients who are ineligible for high-dose therapy with hematopoietic stem cell support: a study based on the nationwide Danish Myeloma Database. Am J Hematol. 2015 Apr;90(4):E73–E74. doi: 10.1002/ajh.23932. [DOI] [PubMed] [Google Scholar]
- 7.Blimark C., Holmberg E., Mellqvist U.H., Landgren O., Bjorkholm M., Hultcrantz M., et al. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015 Jan;100(1):107–113. doi: 10.3324/haematol.2014.107714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelhardt M., Ihorst G., Duque-Afonso J., Wedding U., Spät-Schwalbe E., Goede V., et al. Structured assessment of frailty in multiple myeloma as a paradigm of individualized treatment algorithms in cancer patients at advanced age. Haematologica. 2020 Apr 2 doi: 10.3324/haematol.2019.242958. haematol.2019.242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020 Apr 6 doi: 10.1001/jama.2020.5394. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg S.K.L., Whitaker M., O’Halloran A., Cummings C., Holstein R., et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020 doi: 10.15585/mmwr.mm6915e3. ePub: 8 April 2020. [accessed 10 April 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Characteristics of COVID-19 patients dying in Italy Report based on available data on April 9th, 2020. Istituto Superiore di Sanità; 2020. https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-analysis-of-deaths [Accessed April 12, 2020] [Google Scholar]
- 12.Zhang X., Song K., Tong F., Fei M., Guo H., Lu Z., et al. First case of COVID-19 in a patient with multiple myeloma successfully treated with tocilizumab. Blood Adv. 2020;4(7):1307–1310. doi: 10.1182/bloodadvances.2020001907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang W., Guan W., Chen R., Wang W., Li J., Xu K., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020 Mar;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai M.-Y., Liu D., Liu M., Zhou F.-X., Li G.-L., Chen Z., Zhang Z.-A., You H., Wu M., Zhen Q.-C., Xiong Y., Xiong H.-H., Wang C., Chen C.-C., Xiong F., Zhang Y., Peng Y.-Q., Ge S.-P., Zhen B., Yu T.-T., Wang L., Wang H., Liu Y., Chen Y.-S., Mei J.-H., Gao X.-J., Li Z.-Y., Gan L.-J., He C., Li Z., Shi Y.-Y., Qi Y.-W., Yang J., Tenen D.G., Chai L., Mucci L.A., Santillana M., Cai H.-B. 2020. Patients with Cancer Appear More Vulnerable to S.-C.-2: A M.-C. Study During the COVID-19 Outbreak (3/17/2020) Available at SSRN: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schutt P., Brandhorst D., Stellberg W., Poser M., Ebeling P., Muller S., et al. Immune parameters in multiple myeloma patients: influence of treatment and correlation with opportunistic infections. Leuk Lymphoma. 2006 Aug;47(8):1570–1582. doi: 10.1080/10428190500472503. [DOI] [PubMed] [Google Scholar]
- 16.Reusken C.B., Buiting A., Bleeker-Rovers C., Diederen B., Hooiveld M., Friesema I., et al. Rapid assessment of regional SARS-CoV-2 community transmission through a convenience sample of healthcare workers, the Netherlands, March 2020. Euro Surveill. 2020 Mar;25(12) doi: 10.2807/1560-7917.ES.2020.25.12.2000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kastritis E., Terpos E., Roussou M., Gavriatopoulou M., Migkou M., Eleutherakis-Papaiakovou E., et al. Evaluation of the Revised International Staging System in an independent cohort of unselected patients with multiple myeloma. Haematologica. 2017;102(3):593–599. doi: 10.3324/haematol.2016.145078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gay F., Larocca A., Wijermans P., Cavallo F., Rossi D., Schaafsma R., et al. Complete response correlates with long-term progression-free and overall survival in elderly myeloma treated with novel agents: analysis of 1175 patients. Blood. 2011;117(11):3025–3031. doi: 10.1182/blood-2010-09-307645. [DOI] [PubMed] [Google Scholar]
- 19.Pawlyn C., Cairns D., Kaiser M., Striha A., Jones J., Shah V., et al. The relative importance of factors predicting outcome for myeloma patients at different ages: results from 3894 patients in the Myeloma XI trial. Leukemia. 2020;34(2):604–612. doi: 10.1038/s41375-019-0595-5. 2020/02/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rockwood K. Frailty and its definition: a worthy challenge. J Am Geriatr Soc. 2005 Jun;53(6):1069–1070. doi: 10.1111/j.1532-5415.2005.53312.x. [DOI] [PubMed] [Google Scholar]
- 21.Cook G., Royle K.L., Pawlyn C., Hockaday A., Shah V., Kaiser M.F., et al. A clinical prediction model for outcome and therapy delivery in transplant-ineligible patients with myeloma (UK Myeloma Research Alliance Risk Profile): a development and validation study. Lancet Haematol. 2019 Mar;6(3):e154–e166. doi: 10.1016/S2352-3026(18)30220-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mian H.S., Wildes T.M., Fiala M.A. Development of a medicare health outcomes survey deficit-accumulation frailty index and its application to older patients with newly diagnosed multiple myeloma. JCO Clin Cancer Inform. 2018;2 doi: 10.1200/CCI.18.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engelhardt M., Domm A.-S., Dold S.M., Ihorst G., Reinhardt H., Zober A., et al. A concise revised Myeloma Comorbidity Index as a valid prognostic instrument in a large cohort of 801 multiple myeloma patients. Haematologica. 2017;102(5):910–921. doi: 10.3324/haematol.2016.162693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palumbo A., Bringhen S., Mateos M.-V., Larocca A., Facon T., Kumar S.K., et al. Geriatric assessment predicts survival and toxicities in elderly myeloma patients: an International Myeloma Working Group report. Blood. 2015;125(13):2068–2074. doi: 10.1182/blood-2014-12-615187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu M.A., DuMontier C., Murillo A., Hshieh T.T., Bean J.F., Soiffer R.J., et al. Gait speed, grip strength, and clinical outcomes in older patients with hematologic malignancies. Blood. 2019 Jul 25;134(4):374–382. doi: 10.1182/blood.2019000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newell A.M., VanSwearingen J.M., Hile E., Brach J.S. The modified Gait Efficacy Scale: establishing the psychometric properties in older adults. Phys Ther. 2012 Feb;92(2):318–328. doi: 10.2522/ptj.20110053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myeloma Patient Safety and the Coronovirus: International Myeloma Foundation https://www.myeloma.org/covid19-myeloma-patients [accessed 6 April 2020]
- 28.American Society of Transplantation and Cellular Therapy: Reponse to COVID-19 https://www.astct.org/connect/astct-response-to-covid-19 [accessed 6 April 2020]
- 29.COVID -19 and Multiple Myeloma: Frequently Asked Questions (American Society of Hematology) https://www.hematology.org/covid-19/covid-19-and-multiple-myeloma [accessed 6 April 2020]
- 30.Rajkumar S.V., Dimopoulos M.A., Palumbo A., Blade J., Merlini G., Mateos M.V., et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014 Nov;15(12):e538–e548. doi: 10.1016/S1470-2045(14)70442-5. [DOI] [PubMed] [Google Scholar]
- 31.Coronavirus Disease Covid-19: European Society for Blood and Marrow Transplant https://www.ebmt.org/ebmt/news/coronavirus-disease-covid-19-ebmt-recommendations-update-march-23-2020 [accessed 6 April 2020]
- 32.Bringhen S., Mateos M.V., Zweegman S., Larocca A., Falcone A.P., Oriol A., et al. Age and organ damage correlate with poor survival in myeloma patients: meta-analysis of 1435 individual patient data from 4 randomized trials. Haematologica. 2013 Jun;98(6):980–987. doi: 10.3324/haematol.2012.075051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duma N., Azam T., Riaz I.B., Gonzalez-Velez M., Ailawadhi S., Go R. Representation of minorities and elderly patients in multiple myeloma clinical trials. Oncologist. 2018;23(9):1076–1078. doi: 10.1634/theoncologist.2017-0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.ASH RC COVID-19 Registry for Hematologic Malignancy https://www.ashresearchcollaborative.org/covid-19-registry/ [accessed 9 April 2020]
- 35.The COVID-19 and Cancer Consortium https://ccc19.org/ [accessed 9 April 2020]