Abstract
A patient with coronavirus disease-2019 (COVID-19) developed sudden shortness of breath and hypoxia. She received a diagnosis of massive pulmonary embolism complicated by right-sided heart failure, which was successfully managed conservatively. This case marks the first report of COVID-19–induced pulmonary embolism in association with acute heart failure. (Level of Difficulty: Beginner.)
Key Words: COVID-19, heart failure, pulmonary embolism
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2
Graphical abstract
A patient with coronavirus disease-2019 (COVID-19) developed sudden shortness of breath and hypoxia. She received a diagnosis of massive pulmonary embolism…
History of Presentation
On March 16, 2020, a 59-year-old woman presented to the emergency department with reports of weakness and a mechanical fall. On presentation, she reported a mildly productive cough with yellowish sputum for the past week. Her mother had been similarly ill and had tested positive for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).
Learning Objectives
-
•
To make a differential diagnosis of pulmonary embolism in patients with COVID-19 with sudden onset of dyspnea and hypoxemia.
-
•
To understand the potential role of early anticoagulation in high-risk patients with COVID-19.
The patient was febrile (100.2°F) and tachycardic, with a heart rate of 120 beats/min. Her arterial oxygen saturation (Sao2) was 97% on 2 liters of supplemental oxygen. Physical examination demonstrated coarse crackles in the bilateral lower lung fields.
Past Medical History
Her past medical history included hypertension and diabetes mellitus.
Differential Diagnosis
The differential diagnosis included community-acquired pneumonia, atypical pneumonia, and coronavirus disease-2019 (COVID-19).
Investigations
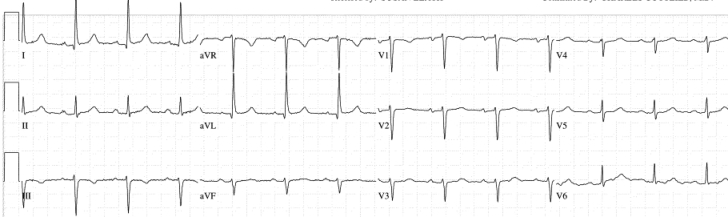
Laboratory investigation revealed leukopenia (2.6 K/μl), elevated lactate dehydrogenase of 812 U/l, C-reactive protein of 56 mg/l, and a D-dimer level of 1,280 ng/ml. The result of a rapid influenza test was negative. The electrocardiogram was unremarkable (Figure 1). Computed tomography of the chest revealed bilateral interstitial densities consistent with an infectious or inflammatory process and no evidence of pulmonary embolism (Figure 2A). She was started on intravenous fluids, a prophylactic dose of enoxaparin, and broad-spectrum antibiotics, including vancomycin, levofloxacin, and cefepime because of a high suspicion for pneumonia. She was also tested for COVID-19.
Figure 1.
Electrocardiogram on Day 1 Showing Normal Sinus Rhythm With Left Axis Deviation and No Ischemic Changes
Figure 2.
CT of the Chest and CT Pulmonary Angiography
(A) Axial unenhanced chest computed tomography (CT) scan obtained on day 1 after the onset of symptoms shows bilateral areas of ground-glass interstitial opacities. (B) Computed tomography pulmonary angiography demonstrates multiple bilateral filling defects involving lobar and segmental branches of the pulmonary artery (yellow arrow) and a linear saddle pulmonary embolus (red arrow).
The following day, her real-time fluorescence polymerase chain reaction result for SARS-CoV-2 returned positive. Her symptoms improved with supportive measures, antibiotics were discontinued, and a plan was made to discharge her home to self-quarantine. However, before discharge she developed sudden severe dyspnea while walking in her room. She was noted to be hypoxic, with her Sao2 dropping to 83%, with a resultant oxygen requirement of 6 liters by nasal cannula. Repeat computed tomography of the chest revealed large bilateral central and proximal segmental pulmonary artery emboli and a linear saddle pulmonary embolus (Figure 2B). Bedside transthoracic echocardiography revealed right ventricular dilatation with reduced function associated with severe tricuspid regurgitation (Figures 3A and 3B).
Figure 3.
Bedside Transthoracic Echocardiography
(A) Parasternal short-axis view of the heart showing a dilated right ventricle (red arrow). (B) Doppler echocardiographic view of severe tricuspid regurgitation.
Management
The patient was started on therapeutic enoxaparin and was closely monitored for hemodynamic instability. She declined to take hydroxychloroquine, recommended by some experts for management for COVID-19. She remained hemodynamically stable and was transitioned to oral anticoagulant therapy (apixaban) with plans to continue anticoagulation for 6 months.
Discussion
The COVID-19 outbreak is an unprecedented global public health challenge. Since the end of December 2019, when the first cases of SARS-CoV-2 infection were detected in Wuhan, China, the disease has spread exponentially (1). On January 30, 2020, the World Health Organization declared COVID-19, the disease caused by the novel coronavirus, a public health emergency of international concern and later officially upgraded it to a global pandemic. As of April 24, 2020, more than 2,790,000 confirmed cases from more than 180 countries and more than 195,000 deaths have been documented worldwide. The projected U.S. death toll is >240,000, with an estimated total burden of more than 1 million COVID-19 cases.
In approximately 88% of cases, fever is the most common presentation, followed by cough (68%), vomiting (5%), and diarrhea (3.8%) (2). In up to 15% of patients, the natural course of the disease is complicated by severe interstitial pneumonia, which can lead to acute respiratory distress syndrome, multiorgan failure including acute kidney injury, disseminated intravascular coagulation, and death (2). To our knowledge, there have been no reported cases of COVID-19 complicated by massive pulmonary embolism and right-sided heart failure.
During the SARS-CoV-1 epidemic of 2014, the reported incidence of deep venous thrombosis and pulmonary embolism in affected patients was approximately 20% and 11%, respectively (3). So far, there have been no concrete data on the overall incidence of thrombosis in patients with SARS-CoV-2 infection (3). It is, however, estimated that approximately 50% of these patients have elevated D-dimer levels during disease progression, which is directly associated with the risk of increased thrombosis and poor prognosis of the disease (2,4). Multivariable regression showed increased odds of in-hospital death associated with D-dimer values >1 μg/ml (18.42, 2.64 to 128.55; p = 0.0033) (5). A higher risk of vessel thrombosis has been correlated with severity of the disease and multiorgan involvement, thus lending support to the argument for therapeutic anticoagulation in patients with COVID-19 who have elevated D-dimer levels (4).
The proposed mechanisms for COVID-19–induced thrombosis include a disease-specific hypercoagulable state, cytokine-mediated diffuse microvascular damage, and, in some cases, reactive thrombocytosis (6). The risk of thrombosis and pulmonary embolism can further be compounded by obesity, advanced age, and hospitalization-related immobilization. In the present case, the patient had elevated C-reactive protein and D-dimer levels with no other risk factor for pulmonary embolism, thereby indicating a COVID-19–related hypercoagulable state as a possible cause of thrombosis in the pulmonary vasculature.
Follow-Up
The patient remained asymptomatic with no further episodes of breathlessness or hypoxia at 1-week follow-up. She continues to take apixaban, with plans to follow up with a hematologist in 1 month.
Conclusions
Because patients with COVID-19 are admitted for treatment and isolation, it is imperative to follow prophylactic measures for avoiding venous thromboembolism. Sudden deterioration in respiratory status that is not explained by significant radiological changes in the lung fields, and especially in conjunction with high titers of D-dimers, should raise suspicion for pulmonary embolism. More studies are needed to determine the utility of therapeutic doses of anticoagulant agents in high-risk patients with COVID-19.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chong P.Y., Chui P., Ling A.E. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128:195–204. doi: 10.5858/2004-128-195-AODDTS. [DOI] [PubMed] [Google Scholar]
- 4.Tang N., Bai H., Chen X. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mei H., Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E002. doi: 10.3760/cma.j.issn.0253-2727.2020.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]