Abstract
Objectives:
Infective endocarditis (IE) among people who inject drugs is associated with high rates of mortality and repeat episodes of endocarditis. We sought to report on longer-term clinical outcomes of patients with IE who were offered buprenorphine or methadone treatment for opioid use disorder (OUD) at their initial hospital admission
Methods:
Individuals with OUD hospitalized between 2013 and 2015 with IE were included for the retrospective study. The following data were extracted from the medical record: sociodemographic data, mortality, repeat episodes of endocarditis, and evidence of ongoing buprenorphine and methadone treatment. The impact of medication use on mortality and repeat episode of endocarditis was examined using survival analysis.
Results:
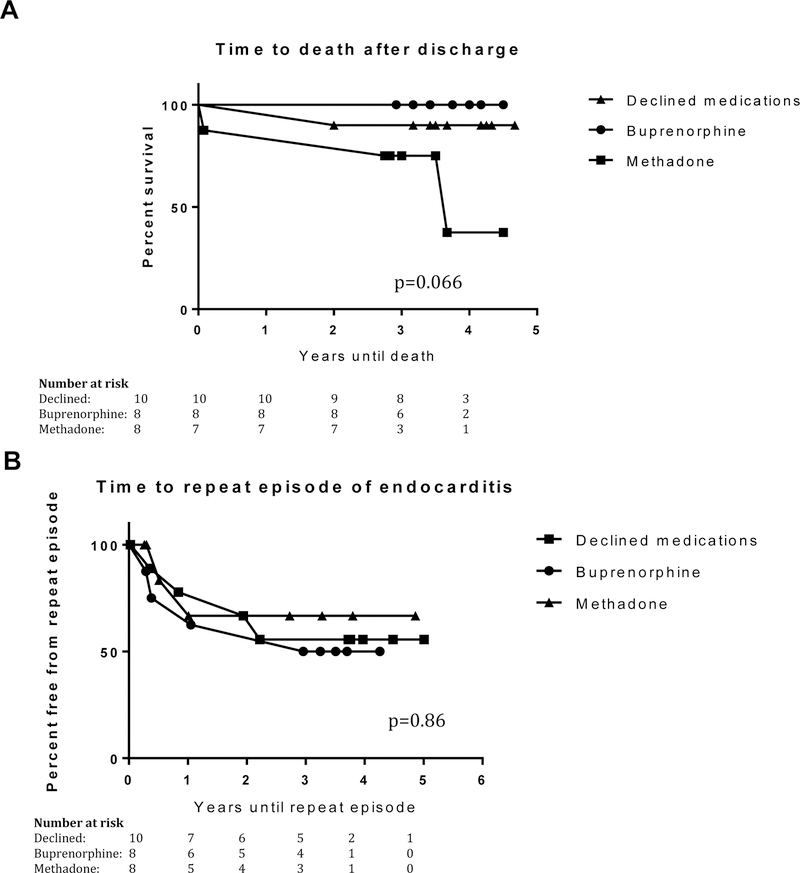
Overall 26 individuals were included in the study. The mean duration of follow-up was 45.0 months (SD 7.2, range 34.0 to 56.0). During the index admission, 8 received buprenorphine, 8 received methadone, and 10 declined medications. During the follow-up period, 4 (15.4%) individuals died, and 10 (38.5%) individuals experienced a repeat episode of endocarditis. Survival analysis of mortality (logrank p=0.066) and repeat episode of endocarditis (logrank p=0.86) comparing those who received buprenorphine, received methadone, and declined medication did not differ significantly.
Conclusions:
Initiation of medication treatment alone may not be sufficient to impact long-term mortality and rates of repeat episode of endocarditis. More research is needed to identify optimal treatment strategies for people who inject drugs with IE.
Keywords: opioid use disorder, people who inject drugs, infective endocarditis, buprenorphine, methadone
Introduction
Hospitalizations for infective endocarditis (IE) among people who inject drugs are increasing (Ronan and Herzig, 2016; Wurcel et al., 2016). Patients who develop endocarditis as a result of injection drug use, compared to those whose endocarditis is due to another cause, are much more likely to experience repeat episodes of endocarditis, require re-operation, and may have a higher mortality rate despite fewer comorbid cardiovascular diseases (Carozza et al., 2006; Kim et al., 2016; Rabkin et al., 2012). Although medication treatment with buprenorphine and methadone for the opioid use disorder (OUD) at the time of the initial hospital admission may be effective at reducing mortality and other adverse outcomes, longitudinal data are limited. In the only prior study so far examining long-term outcomes, initiation of medication for opioid use disorder (MOUD) during the initial hospitalization for endocarditis had no impact on mortality (Rodger et al., 2018).
Here we describe longer-term clinical outcomes of IE among people who inject drugs who were offered buprenorphine or methadone treatment for OUD at their initial hospital admission (Suzuki, 2016).
Methods
Setting:
Individuals included in this report were initially admitted for the treatment of IE to Brigham and Women’s Hospital in Boston, MA between 2013 and 2015. The Partners HealthCare Human Research Committee approved the study.
Participants:
Study participants were the subject of a prior retrospective chart review of 29 consecutive patients admitted to Brigham and Women’s Hospital between May 2013 and July 2015 for the treatment of IE and referred for an addiction consultation (Suzuki, 2016). The addiction consultation team consisted of addiction psychiatrists and social workers. In addition to helping to resolve the ambivalence for treatment using motivational interviewing strategies, all patients were evaluated by the consultation team for the suitability of initiating MOUD. If the patient was suitable for and preferred buprenorphine, then it was initiated during the hospitalization, and a referral made to an outpatient prescriber. A prescription was provided if needed by the rehabilitation facility, or to bridge to the outpatient appointment. If methadone was chosen, then methadone was initiated during the hospitalization at no more than 30mg on the first day, and referral made to a clinic following the day of anticipated discharge. If being discharged to home, due to regulatory constraints, methadone was tapered off prior to discharge, typically by reducing the dose by no more than 5mg per day. If the patient was being transferred to a rehabilitation facility instead, recommendations were provided to continue the methadone at the facility. For all patients, every effort was made to schedule a follow-up visit with outpatient addiction treatment as close as possible to the anticipated discharge date to minimize disruptions in treatment. For those who had not yet identified a suitable buprenorphine provider at the time of discharge from the hospital or the rehabilitation facility, patients were offered weekly visits for up to a month at the hospital to assist patients in finding a prescriber. Data from 26 individuals were available for examination from the electronic medical records.
Data extraction:
Data extracted from the electronic medical record included: sociodemographic data (age, gender, self-report race/ethnicity), mortality, repeat episodes of endocarditis, and evidence of buprenorphine and methadone treatment for the opioid use disorder (documentation by prescription or free text in progress notes). Psychiatric, substance use, and medical histories were extracted from the previous study (Suzuki, 2016).
Analytic strategy:
Demographic and clinical variables were compared between patients who received buprenorphine, received methadone, and declined medications at initial hospitalization, using chi-square and Fisher’s exact test for categorical variables, and student’s t-test for continuous variables. We examined associations between baseline demographic and clinical variables with mortality and repeat episodes of endocarditis, respectively using chi-square and Fisher’s exact test for categorical variables, and student’s t-test for continuous variables. Kaplan-Meier curves were plotted for survival and freedom from repeat episodes of endocarditis for those who received buprenorphine, received methadone or declined medications. For the survival analysis of repeat episode of endocarditis, data for those who died were censored at the time of their death. Log-rank test compared the time to death and time to repeat episode of endocarditis among these 3 groups (2 degrees of freedom).
Results
Baseline characteristics:
The demographic and clinical variables comparing those who received buprenorphine, received methadone, or declined medications are summarized in Table 1. All endorsed opioids as the primary drugs used for injection use, including heroin, prescription opioids, and buprenorphine. No significant differences in demographic and clinical variables, including duration of follow-up, were identified between those who received buprenorphine, received methadone, or declined medications. The mean duration of follow-up was 45.0 months (SD 7.2, range 34.0 – 56.0 months). The maximum dose that patients received during the index admission averaged 15.1mg (SD 5.1, range 8–24mg) for buprenorphine, and 29.4mg (SD 20.6, range 10–70mg) for methadone.
Table 1:
Summary of demographic and clinical variables, mortality, and repeat episode of endocarditis among those who received buprenorphine, received methadone, or declined MOUD during the index admission
| Total (n=26) | Received buprenorphine (n=8) | Received methadone (n=8) | Declined MOUD (n=10) | p | |
|---|---|---|---|---|---|
| Age, M (SD) | 33.8 (SD 12.0) | 31.1 (SD 10.6) | 38.9 (SD 14.4) | 31.9 (SD 11.3) | NS |
| Gender | |||||
| Female | 13 (50%) | 5 (62.5%) | 5 (62.5%) | 3 (30%) | NS |
| Male | 13 (50%) | 3 (37.5%) | 3 (37.5%) | 7 (70%) | |
| Race | |||||
| White | 22 (84.6%) | 7 (87.5%) | 7 (87.5%) | 8 (80.0%) | NS |
| Black | 1 (3.8%) | 0 | 1 (12.5%) | 0 | |
| Asian | 1 (3.8%) | 1 (12.5%) | 0 | 0 | |
| Unknown | 2 (7.7%) | 0 | 0 | 2 (20.0%) | |
| Ethnicity | |||||
| Not Hispanic or Latino | 24 (92.3%) | 8 (100%) | 8 (100.0%) | 8 (80.0%) | NS |
| Hispanic or Latino | 0 | 0 | 0 | 0 | |
| Unknown | 2 (7.7%) | 0 | 0 | 2 (20.0%) | |
| Psychiatric history | |||||
| History of psychiatric admission | 8 (30.8%) | 3 (37.5%) | 3 (37.5%) | 2 (20.0%) | NS |
| On psychiatric medications | 11 (42.3%) | 2 (25.0%) | 4 (50.0%) | 5 (50.0%) | NS |
| Any psychiatric disorder | 15 (57.7%) | 4 (50.0%) | 5 (62.5%) | 6 (60.0%) | NS |
| Mood disorder | 11 (42.3%) | 4 (50.0%) | 3 (37.5%) | 4 (40.0%) | NS |
| Anxiety disorder | 11 (42.3%) | 4 (50.0%) | 3 (37.5%) | 4 (40.0%) | NS |
| PTSD | 4 (15.4%) | 1 (12.5%) | 2 (25.0%) | 1 (12.5%) | NS |
| SUD history | |||||
| Opioid use disorder | 26 (100.0%) | 8 (100.0%) | 8 (100.0%) | 10 (100.0%) | NS |
| IV heroin | 24 (92.3%) | 8 (100.0%) | 7 (87.5%) | 9 (90.0%) | NS |
| IV prescription opioid | 4 (15.4%) | 0 | 2 (25.0%) | 2 (20.0%) | NS |
| IV buprenorphine | 4 (15.4%) | 1 (12.5%) | 2 (25.0%) | 1 (10.0%) | NS |
| Cocaine/stimulant use disorder | 13 (50.0%) | 4 (50.0%) | 3 (37.5%) | 6 (60.0%) | NS |
| Cannabis use disorder | 8 (30.8%) | 3 (37.5%) | 2 (25.0%) | 3 (30.0%) | NS |
| Alcohol use disorder | 8 (30.8%) | 5 (62.5%) | 1 (12.5%) | 2 (20.0%) | NS |
| Prior overdose | 3 (11.5%) | 0 | 2 (25.0%) | 1 (10.0%) | NS |
| Prior MOUD | 14 (53.9%) | 5 (62.5%) | 5 (62.5%) | 4 (40.0%) | NS |
| Medical history | |||||
| Chronic pain | 7 (26.9%) | 1 (12.5%) | 4 (50.0%) | 2 (20.0%) | NS |
| Hepatitis C | 15 (57.7%) | 6 (75.0%) | 4 (50.0%) | 5 (50.0%) | NS |
| HIV | 0 | 0 | 0 | 0 | NS |
| Previous endocarditis | 8 (30.8%) | 3 (37.5%) | 3 (37.5%) | 2 (20.0%) | NS |
| Prosthetic valve | 6 (23.1%) | 3 (37.5%) | 2 (25.0%) | 1 (10.0%) | NS |
| Transferred from another hospital at index admission | 15 (57.7%) | 5 (62.5%) | 5 (62.5%) | 5 (50.0%) | NS |
| Site of infection | |||||
| Tricuspid | 12 (48.0%) | 5 (62.5%) | 4 (57.1%) | 3 (30.0%) | NS |
| Pulmonary | 1 (4.0%) | 1 (12.5%) | 0 | 0 | |
| Mitral | 5 (20.0%) | 1 (12.5%) | 3 (42.9%) | 1 (10.0%) | |
| Aortic | 6 (24.0%) | 1 (12.5%) | 0 | 5 (50.0%) | |
| No vegetations | 1 (4.0%) | 0 | 0 | 1 (10.0%) | |
| Prosthetic valve infection | 6 (23.1%) | 3 (37.5%) | 2 (25.0%) | 1 (10.0%) | NS |
| Bacteria | |||||
| MRSA | 5 (19.2%) | 2 (25.0%) | 1 (12.5%) | 2 (20.0%) | NS |
| MSSA | 13 (50.0%) | 4 (50.0%) | 6 (75.0%) | 3 (30.0%) | |
| Streptococcus | 4 (15.4%) | 1 (12.5%) | 0 | 3 (30.0%) | |
| Enterococcus | 3 (11.5%) | 0 | 1 (12.5%) | 2 (20.0%) | |
| Unknown | 1 (3.9%) | 1 (12.5%) | 0 | 0 | |
| Hospital length of stay, Mean days (SD) | 17.8 (SD 13.9) | 16.6 (SD 11.7) | 15.0 (SD 7.7) | 21,0 (19.1) | NS |
| Surgical treatment at index admission | 8 (30.8%) | 3 (37.5%) | 1 (25.0%) | 3 (30.0%) | NS |
| Antibiotic treatment | |||||
| Completion of antibiotic course | 24 (92.3%) | 8 (100.0%) | 6 (75.0%) | 10 (100.0%) | NS |
| Transferred to nursing facility | 23 (88.5%) | 7 (87.5%) | 7 (87.5%) | 9 (90.0%) | NS |
| Duration of follow-up, Mean months, (SD, range) | 45.0 (SD 7.2, range 34–56) | 45.8 (SD 7.0, 35–54) | 43.8 (SD 8.7, 34–54) | 45.3 (SD 6.7, 35–56) | NS |
| Mortality (% deceased) | 15.4% | 0 | 3 (37.5%) | 1 (10%) | NS |
| Repeat episode of endocarditis | 10 (38.5%) | 4 (50.0%) | 2 (25%) | 4 (40%) | NS |
| Evidence of MOUD after index admission during follow-up | 16 (61.5%) | 7 (87.5%) | 4 (50%) | 5 (50%) | NS |
MOUD = Medications for opioid use disorder
PTSD = Post-traumatic stress disorder
MRSA = Methicillin-Resistant Staphylococcus Aureus
MSSA = Methicillin-Susceptible Staphylococcus Aureus
Mortality:
Four (15.4%) individuals died during the follow-up period. Those who died were more likely to have received psychiatric medications (p=0.02) and to have a history of chronic pain (p=0.047). Survival analysis of mortality utilizing log-rank test comparing those who received buprenorphine, received methadone, and declined medication did not differ significantly (p=0.066) (Figure 1a).
Figure 1.
(A) Kaplan-Meier curve for time to death (B) and time to repeat episode of endocarditis comparing those who declinded medications, initiated buprenorphine, and initiated methadone.
Repeat episode of endocarditis:
A total of 10 (38.5%) individuals experienced a repeat episode of endocarditis during the follow-up period. None of the demographic or clinical variables were significantly correlated with individuals who experienced a repeat episode of endocarditis. Survival analysis of repeat episodes of endocarditis utilizing log-rank test comparing those who received buprenorphine, received methadone, and declined medication did not differ significantly (p=0.86) (Figure 1b).
Engagement with medication treatment for OUD after discharge:
Overall, the majority (62.5%) had evidence of ongoing treatment for OUD during the follow-up period.
Discussion
This study confirms that injection-drug-related IE continues to be a severe and life-threatening illness, with high rates of mortality and repeat infection to endocarditis despite the involvement of addiction consultants during the initial hospitalization. Results also suggest that initiation of medication treatment for OUD during the initial hospitalization may not significantly impact long-term mortality rate nor repeat endocarditis infection. Indeed, in the only other published report that examined the impact of initiating medication treatment during the initial hospital admission, medications had no impact on mortality among people who inject drugs with IE (Rodger et al., 2018). Similarly, initiation of medication treatment for OUD alone may not alter the likelihood of experiencing repeat episodes of endocarditis. However, these results remain preliminary given the small size, and more research is needed to better understand the long-term impact of medication treatment for OUD during hospitalization for infective endocarditis.
There are several possible explanations for the failure to find any significant differences in mortality and repeat infection between those who initiated buprenorphine, methadone or declined treatment. The high rate of engagement with medication treatment for OUD during the follow-up even among those who declined initial treatment may be one reason. The majority of patients had evidence of ongoing treatment with the same medication they had chosen during the index admission. Another may be that the addiction psychiatry consultation service provided referrals to treatment for all patients, and were encouraged to seek treatment utilizing motivational interviewing strategies. Additionally, people who inject drugs with IE may require more intensive treatment for their OUD to impact longer-term outcomes. More research is needed to examine if initiation of medications for OUD during the index admission can impact longer-term outcomes.
Given that medications for OUD have been shown to reduce overall mortality and suppress illicit opioid use (Larochelle et al., 2018; Mattick et al., 2014; Sordo et al., 2017), medications should be offered to every OUD patient during the initial hospitalization. In our study, over 60% of all OUD patients with IE accepted the initiation of buprenorphine or methadone treatment during the initial hospitalization, and a similar majority of patients had evidence of ongoing treatment during the follow-up period. Unfortunately, hospitalizations are rarely used as opportunities to initiate medication treatment for the underlying OUD among those with infectious complications (Fanucchi and Lofwall, 2016). Prior studies have demonstrated that implementation of an addiction consultation service may facilitate the initiation of medications for OUD and referral to treatment after discharge (Trowbridge et al., 2017; Wakeman et al., 2017). Future research should investigate whether hospital-based addiction consultation services can help facilitate patients to initiate medications for OUD and to engage with ongoing addiction treatment after discharge.
The difference between utilizing buprenorphine and methadone during the index admission warrants further comment. Those who accepted buprenorphine were not only initiated onto buprenorphine but also were provided with a prescription to ensure could continue this medication while awaiting to initiate outpatient treatment in the community. In contrast, due to administrative and regulatory constraints, methadone was discontinued prior to discharge to home for those who opted for methadone. Even if methadone was continued at the rehabilitation facility, methadone was likely to have been tapered off prior to discharge to home. Federal law permits methadone to be administered for the treatment of OUD during the hospitalization, but the law does not permit for a prescription of methadone to be written if it is being utilized for the treatment of OUD. An intake at the methadone clinic was arranged as close as possible to the anticipated discharge date, but this likely created gaps in treatment. This suggests, therefore, that those who initiated methadone were more similar to patients who declined medications because both were discharged from the hospital or rehabilitation facility with no MOUD. As such, individuals who initiated methadone may be more accurately described as receiving a methadone withdrawal protocol with plans for outpatient linkage. Nevertheless, post-hoc survival analysis comparing individuals who initiated buprenorphine to individuals who either initiated methadone or declined medications found no differences on either mortality or repeat episode of endocarditis.
There are several limitations to this study. The study was of a small sample size, providing limited power to detect small but clinically meaningful differences in outcomes. This was an observational study, and there are likely confounders among patients who chose buprenorphine, methadone, and who declined MOUD that impacted the outcomes. The study was conducted at a single academic institution, limiting the ability to generalize our results to other populations and settings. Given that the majority of patients were initially admitted to another facility, individuals in this cohort may represent those with greater severity of illness, and treatment of their opioid withdrawal could have been delayed until after transfer. While specific reasons for the refusal of MOUD were not collected, the acceptance of buprenorphine may have been influenced by concerns for inadequate management of acute pain. The individuals included in this study were limited to those who accepted an addiction consultation, who may be different from patients who either declined the consultation, or for whom the team felt no need to request a consultation. Initiation of methadone was distinct from initiation of buprenorphine because instead of providing a prescription in order to continue treatment, individuals who chose methadone received a withdrawal protocol with plan for outpatient linkage. Finally, we were limited in identifying deaths, repeat infections to endocarditis, and ongoing OUD treatment only from medical records of our own healthcare system, leading to an underestimation of the number of these events.
Infective endocarditis among people who inject drugs is a severe and life-threatening illness. While initiation of medications such as buprenorphine and methadone for the underlying OUD may increase the number of such patients engaging in ongoing treatment, more research is needed to determine the impact of these medications on longer-term outcomes including mortality and repeat episodes of endocarditis. Future research should employ a larger prospective study design to better characterize the cohort, exposure to ongoing treatments, and the incidence of adverse outcomes. Research should also examine the impact of addiction consultation service, interventions to enhance linkage to and retention in outpatient treatment, and treatments for any psychiatric or medical co-morbidities. This preliminary study suggests that new and innovative methods to enhance the therapeutic impact of medications may be needed for patients with OUD and infective endocarditis.
Acknowledgements:
The authors would like to acknowledge Bianca Martin for her assistance with data extraction.
Funding: This work was supported by National Institutes of Health [grant numbers K23DA042326 (JS), K24DA022288 (RW)]
References
- Carozza A, De Santo LS, Romano G, Della Corte A, Ursomando F, Scardone M, Caianiello G, Cotrufo M, 2006. Infective endocarditis in intravenous drug abusers: patterns of presentation and long-term outcomes of surgical treatment. J. Heart Valve Dis 15, 125–131. [PubMed] [Google Scholar]
- Fanucchi L, Lofwall MR, 2016. Putting Parity into Practice - Integrating Opioid-Use Disorder Treatment into the Hospital Setting. N. Engl. J. Med 375, 811–813. 10.1056/NEJMp1606157 [DOI] [PubMed] [Google Scholar]
- Kim JB, Ejiofor JI, Yammine M, Ando M, Camuso JM, Youngster I, Nelson SB, Kim AY, Melnitchouk SI, Rawn JD, MacGillivray TE, Cohn LH, Byrne JG, Sundt TM, 2016. Surgical outcomes of infective endocarditis among intravenous drug users. J. Thorac. Cardiovasc. Surg 152, 832–841.e1. 10.1016/j.jtcvs.2016.02.072 [DOI] [PubMed] [Google Scholar]
- Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, Bagley SM, Liebschutz JM, Walley AY, 2018. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann. Intern. Med 10.7326/M17-3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst. Rev 2, CD002207. 10.1002/14651858.CD002207.pub4 [DOI] [PubMed] [Google Scholar]
- Rabkin DG, Mokadam NA, Miller DW, Goetz RR, Verrier ED, Aldea GS, 2012. Long-term outcome for the surgical treatment of infective endocarditis with a focus on intravenous drug users. Ann. Thorac. Surg 93, 51–57. 10.1016/j.athoracsur.2011.08.016 [DOI] [PubMed] [Google Scholar]
- Rodger L, Glockler-Lauf SD, Shojaei E, Sherazi A, Hallam B, Koivu S, Gupta K, Hosseini-Moghaddam SM, Silverman M, 2018. Clinical Characteristics and Factors Associated With Mortality in First-Episode Infective Endocarditis Among Persons Who Inject Drugs. JAMA Netw. Open 1, e185220 10.1001/jamanetworkopen.2018.5220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronan MV, Herzig SJ, 2016. Hospitalizations Related To Opioid Abuse/Dependence And Associated Serious Infections Increased Sharply, 2002–12. Health Aff. Proj. Hope 35, 832–837. 10.1377/hlthaff.2015.1424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R, 2017. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 357, j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki J, 2016. Medication-assisted treatment for hospitalized patients with intravenous-drug-use related infective endocarditis. Am. J. Addict 25, 191–194. 10.1111/ajad.12349 [DOI] [PubMed] [Google Scholar]
- Trowbridge P, Weinstein ZM, Kerensky T, Roy P, Regan D, Samet JH, Walley AY, 2017. Addiction consultation services - Linking hospitalized patients to outpatient addiction treatment. J. Subst. Abuse Treat 79, 1–5. 10.1016/j.jsat.2017.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA, 2017. Inpatient Addiction Consultation for Hospitalized Patients Increases Post-Discharge Abstinence and Reduces Addiction Severity. J. Gen. Intern. Med 10.1007/s11606-017-4077-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurcel AG, Anderson JE, Chui KKH, Skinner S, Knox TA, Snydman DR, Stopka TJ, 2016. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open Forum Infect. Dis 3, ofw157. 10.1093/ofid/ofw157 [DOI] [PMC free article] [PubMed] [Google Scholar]