Abstract
Background & Aims
The prevalence of diverticulosis differs with demographic features of patients, but evidence is limited. Well-defined demographic studies are necessary to understand diverticulosis biology. We estimated the prevalence of diverticulosis among patients of different ages, sexes, and races and ethnicities and calculated odds ratios.
Design
Using data from an endoscopic database, we identified 271,181 colonoscopy procedures performed from 2000 through 2012 at 107 sites in the United States. Our analysis included individuals 40 years and older who underwent colonoscopy examination for average-risk screening. The outcome was any reported diverticulosis on colonoscopy. Multivariate analyses were performed using logistic regression to estimate odds ratios (ORs) and 95% CI values, adjusting for confounding variables.
Results
The prevalence of diverticulosis increased with age in men and women of all races and ethnicities. Women 40–49 years old had significantly lower odds of any diverticulosis (OR, 0.71; 95% CI, 0.63–0.80) compared with men 40–49 years old, after adjustment. The strength of this association decreased with age. Compared with non-Hispanic white individuals, non-Hispanic black individuals (OR, 0.80; 95% CI, 0.77–0.83) and Asian/Pacific Islanders (OR, 0.38; 95% CI, 0.35–0.41) had lower odds of any diverticulosis. However, non-Hispanic black individuals (OR, 1.53, 95% CI, 1.44–1.62) had increased odds of any proximal diverticulosis, whereas Asian/Pacific Islanders (OR, 3.12; 95% CI, 2.67–3.66) had increased odds of only proximal diverticulosis.
Conclusions
In an analysis of data from 271,181 colonoscopy procedures, diverticulosis was less prevalent in women compared with men in the same age groups, indicating that sex hormones might affect pathogenesis. Differences in the odds of diverticulosis by race and ethnicity indicate a genetic contribution to risk.
Keywords: diverticular disease, diverticulitis, diverticular hemorrhage
Introduction
Colonic diverticulosis is a common incidental finding on colonoscopy.1 These defects form when colonic mucosa and submucosa herniate through the muscularis propria. Diverticula can hemorrhage, develop inflammation, and perforate.2 These complications are unpredictable, have limited treatment options, and cause substantial patient suffering.3, 4 Diverticular disease is one of the most common digestive diseases in the United States and is the indication for numerous ambulatory visits, hospital admissions, and surgical procedures.5, 6 Health care expenditures total $5.5 billion dollars annually.5
Developing diverticulosis is the first step in the diverticular disease cascade. While the etiopathogenesis of diverticulosis is poorly understood, there is emerging but limited evidence for endogenous sex hormones and genes in the biology of diverticulosis.7–11 We have reported that premenopausal age women are less likely to have diverticulosis than similar-age men, while postmenopausal age women and similar-age men appear to have the same risk.10 This single-center observation needs to be validated in a larger cohort. Moreover, there are unexplained disparities in the risk of diverticulitis12 and diverticular hemorrhage13 by age, sex, race, and ethnicity. Whether these differences are attributable to variation in the prevalence of diverticulosis has not been well studied.
Characterizing the demographics of individuals who develop colonic diverticulosis has the potential to improve understanding of diverticulosis biology and is important to interpreting disparities in diverticular disease risk. In the present study, we used a large national endoscopic database to determine the prevalence of diverticulosis by age, sex, race, and ethnicity in individuals undergoing an average-risk screening colonoscopy. We also determined whether diverticulosis odds differed by individual characteristics.
Methods
The Clinical Outcome Research Initiative (CORI) was established in 1995 to study outcomes of endoscopic gastrointestinal procedures in diverse practice settings across the United States. Physicians participating in the CORI consortium generated gastrointestinal endoscopy reports using a structured computer program developed specifically for the initiative. Data were de-identified prior to transmission to a central data repository, where they were assessed for completeness and accuracy. Practice sites included hospitals, ambulatory care centers, private practices, universities, and Veteran’s hospitals. Data from all participating practices were merged and stored in the National Endoscopic Database (NED). Data from the NED has been used previously to examine endoscopic findings.14–16
Using data from the NED, we included in our analysis all individuals 40 years and older who had a colonoscopy with an indication for average-risk screening performed between January 1, 2000 and December 31, 2012. Although average risk screening routinely begins at age 50, we included adults ages 40–49 to determine diverticulosis prevalence before the average age of menopause. We only included procedures with at least an adequate preparation. Adequate preparation included those judged by the endoscopist to be excellent, good, or fair but adequate. Use of the Boston Bowel Preparation Scale was recommended. We excluded any patient with an indication other than average risk screening. We extracted age at time of endoscopy, sex, race/ethnicity, endoscopy site and type for our analysis. Each endoscopist reported patient race/ethnicity. The primary outcome was the reporting of any colonic diverticulosis on colonoscopy. Among those with diverticulosis, 98.7% had a location documented. The category proximal diverticula included any diverticula reported in the cecum, ascending, hepatic, and/or transverse colon. The category distal diverticula included any diverticula reported in the splenic flexure, descending and/or sigmoid colon.
Statistical analysis
Proportions were calculated for categorical data. Age groups were created (40–49 years, 50–59 years, 60–69 years, 70–79 years, and over the age of 79 years). We calculated the prevalence of diverticulosis among average risk persons having a screening colonoscopy for each age category by demographics. Multivariate analyses were performed using logistic regression to estimate odds ratios and 95% confidence intervals while adjusting for confounding variables (age, sex, race/ethnicity, endoscopy site). Odds of diverticulosis by sex were modeled within age groups. Analyses were conducted using SAS version 9.4 (Cary, NC).
We followed the strengthening the reporting of observational studies in epidemiology (STROBE) guidelines for reporting observational studies.17 The University of North Carolina School of Medicine Institutional Review Board determined this study to be exempt from review.
Results
We identified 271,181 colonoscopy procedures with an indication for average-risk screening performed between 2000 and 2012 at 107 practice sites across the United States. These procedures represent 268,414 unique individuals. Among individuals who had an average-risk screening exam, 46% were women and 95% were between 50 and 79 years old (Table 1). The distribution of race/ethnicity in the cohort was 86% non-Hispanic white, 5% non-Hispanic black, 6% Hispanic and 2% Asian/pacific islander. Most (76%) of the procedures were performed in the community setting.
Table 1.
Characteristics
| Average-Risk Screening Colonoscopy | |
|---|---|
| N= 271,181 | |
| Age, years (%) | |
| 40–49 | 2% |
| 50–59 | 49% |
| 60–69 | 32% |
| 70–79 | 14% |
| 80+ | 2% |
| Sex (%) | |
| Women | 46% |
| Men | 54% |
| Race/Ethnicity (%) | |
| Non Hispanic White | 86% |
| Non Hispanic Black | 5% |
| Hispanic | 6% |
| Asian/Pacific Islander | 2% |
| Other/Unknown | 1% |
| Site type (%) | |
| Community | 76% |
| Health Maintenance Organization | 3% |
| Military | 2% |
| University | 9% |
| Veterans Affairs | 11% |
| Region of United States (%) | |
| North Central | 8% |
| North East | 15% |
| North West | 11% |
| South Central | 11% |
| South East | 17% |
| South West | 38% |
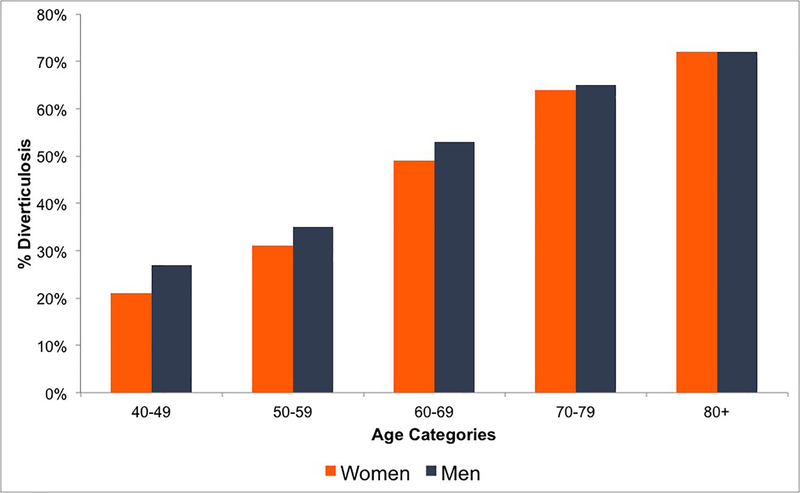
Diverticulosis was less prevalent in women compared with similar-age men until age 80 (Figure 1 and Table 2). Women 40–49 years old had a significantly reduced odds of any diverticulosis (OR 0.71, 95% CI 0.63 – 0.80) compared to men in the same age group after adjustment for race/ethnicity and endoscopy site (Table 2). Likewise, women 50–59 years old (OR 0.79, 95% CI 0.77 – 0.81), women 60–69 years old (OR 0.81, 95% CI 0.79 – 0.83) and women 70–79 years old (OR 0.91, 95% CI 0.87–0.95) had reduced odds of any diverticulosis compared to men. By the age of 80, there was no difference in the odds (OR 0.99, 95% CI 0.88 – 1.11) of diverticulosis.
Figure 1.
Diverticulosis on screening colonoscopy in average risk persons by age and sex. Women are in orange bars and men in navy blue.
Table 2.
Prevalence and Adjusted Odds of Any Diverticulosis by Sex Within Age Groups
| Age, years | Sex | n | Prevalence Diverticulosis % | Odds Ratio (95% Confidence Interval)1 |
|---|---|---|---|---|
| 40–49 | Men | 971 | 27% | Reference |
| Women | 617 | 21% | 0.71 (0.63, 0.80) | |
| 50–59 | Men | 24,841 | 35% | Reference |
| Women | 19,169 | 31% | 0.79 (0.77, 0.81) | |
| 60–69 | Men | 25,230 | 53% | Reference |
| Women | 18,796 | 49% | 0.81 (0.79, 0.83) | |
| 70–79 | Men | 13,059 | 65% | Reference |
| Women | 11,808 | 64% | 0.91 (0.87, 0.95) | |
| 80+ | Men | 2,256 | 72% | Reference |
| Women | 2,536 | 72% | 0.99 (0.88, 1.11) |
Adjusted for race/ethnicity and site
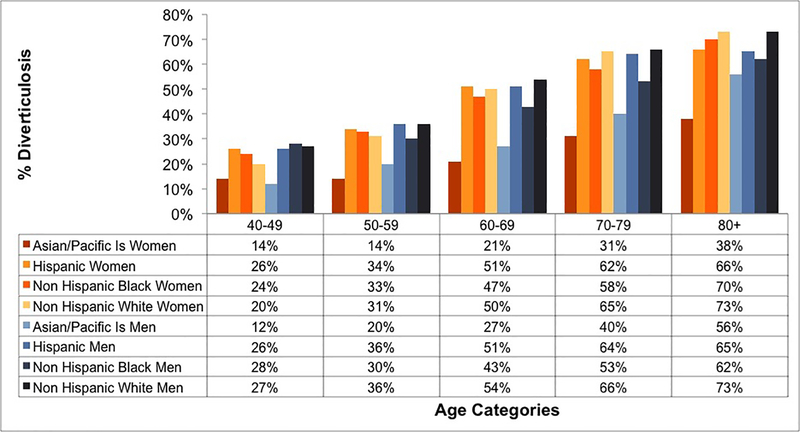
The prevalence of diverticulosis differed by age and race/ethnicity (Figure 2 and Table 3). There was a progressive increase in diverticulosis prevalence by age group (Table 3). Compared with non-Hispanic whites, Asian/pacific islanders (OR 0.38, 95% CI 0.35 – 0.41), non-Hispanic blacks (OR 0.80, 95% CI 0.77 – 0.83), and Hispanic individuals (OR 0.93, 95% CI 0.89 – 0.96) had lower odds of diverticulosis after adjustment for age, sex, and endoscopy site (Table 3). Asian/pacific islanders had the highest prevalence of proximal colon only diverticulosis (5%), while Non-Hispanic black individuals had the highest prevalence of any proximal diverticulosis (12%) (Table 4).
Figure 2.
Diverticulosis on screening colonoscopy in average risk persons by age, sex and race/ethnicity.
Table 3.
Prevalence and Adjusted Odds of Any Diverticulosis by Age Group, Race, and Ethnicity
| n | Prevalence Diverticulosis % | Odds Ratio (95% Confidence Interval) | |
|---|---|---|---|
| Age group1 | |||
| 40–49 | 1,588 | 24% | Reference |
| 50–59 | 44,010 | 33% | 1.58 (1.50, 1.67) |
| 60–69 | 44,026 | 51% | 3.28 (3.11, 3.46) |
| 70–79 | 24,867 | 64% | 5.61 (5.31, 5.93) |
| 80+ | 4,792 | 72% | 7.97 (7.42, 8.56) |
| Race and Ethnicity2 | |||
| Non Hispanic White | 104,222 | 45% | Reference |
| Non Hispanic Black | 5,498 | 38% | 0.80 (0.77, 0.83) |
| Hispanic | 7,271 | 44% | 0.93 (0.89, 0.96) |
| Asian/Pacific Islander | 969 | 22% | 0.38 (0.35, 0.41) |
Adjusted for sex, race/ethnicity, and site
Adjusted for age, sex, and site
Table 4.
Prevalence and Adjusted Odds of Diverticulosis Location by Sex, Age Group, Race and Ethnicity
| Any Proximal | OR (95%CI) | Only Proximal | OR (95%CI) | Any Distal | OR (95%CI) | Only Distal | OR (95%CI) | |
|---|---|---|---|---|---|---|---|---|
| Sex1 | ||||||||
| Men | 9% | Reference | 1% | Reference | 44% | Reference | 37% | Reference |
| Women | 7% | 0.80 (0.78, 0.83) | 1% | 0.87 (0.81, 0.94) | 41% | 0.82 (0.81, 0.84) | 34% | 0.87 (0.86, 0.89) |
| Age group2 | ||||||||
| 40–49 | 5% | Reference | 1% | Reference | 23% | Reference | 19% | Reference |
| 50–59 | 6% | 1.32 (1.17, 1.48) | 1% | 1.38 (1.08, 1.77) | 32% | 1.55 (1.46, 1.64) | 27% | 1.54 (1.44, 1.64) |
| 60–69 | 10% | 2.26 (2.02, 2.54) | 1% | 1.41 (1.10, 1.82) | 50% | 3.26 (3.06, 3.46) | 41% | 2.86 (2.69, 3.05) |
| 70–79 | 13% | 3.29 (2.93, 3.70) | 1% | 1.42 (1.09, 1.84) | 63% | 5.58 (5.25, 5.94) | 51% | 4.20 (3.93, 4.48) |
| 80+ | 16% | 4.34 (3.80, 4.95) | 1% | 1.38 (0.99, 1.94) | 71% | 7.79 (7.19, 8.43) | 56% | 4.93 (4.55, 5.34) |
| Race and Ethnicity3 | ||||||||
| Non Hispanic White | 8% | Reference | 1% | Reference | 44% | Reference | 37% | Reference |
| Non Hispanic Black | 12% | 1.53 (1.44, 1.62) | 3% | 2.47 (2.19, 2.78) | 35% | 0.73 (0.70, 0.76) | 25% | 0.64 (0.61, 0.67) |
| Hispanic | 9% | 1.04 (0.97, 1.11) | 2% | 1.35 (1.16, 1.58) | 42% | 0.89 (0.86, 0.93) | 34% | 0.90 (0.86, 0.94) |
| Asian/Pacific Islander | 11% | 1.15 (1.03, 1.27) | 5% | 3.12 (2.67, 3.66) | 16% | 0.29 (0.27, 0.32) | 11% | 0.26 (0.24, 0.29) |
Odds ratio adjusted for age, race/ethnicity, and site
Odds ratio adjusted for sex, race/ethnicity, and site
Odds ratio adjusted for age, sex, and site
Among average-risk individuals having a colonoscopy for a screening indication, the prevalence of any diverticulosis increased with age in men and women of all races and ethnicities (Figure 2). The prevalence of distal diverticulosis increased with age, as did any proximal diverticulosis (Table 4). The prevalence of proximal only diverticulosis did not consistently increase with age (Table 4).
Discussion
Using 271,181 colonoscopy procedures with an indication for average-risk screening performed at sites across the United States, we found that diverticulosis was less prevalent in women compared with similar-age men. This difference was greatest before the average age of menopause and decreased with increasing age. Non-Hispanic black and Asian/Pacific Islander individuals were less likely to have diverticulosis, but more likely to have proximal diverticula. Asian/Pacific Islander individuals were most likely to have only proximal diverticula, while Non-Hispanic black had any proximal diverticula. Diverticulosis was common even before the age of 50 and the prevalence increased with age in men and women of all races and ethnicities.
Similar to a recent colonoscopy-based study,10 women were less likely to have colonic diverticulosis compared with similar age men. In contrast with the prior study, the large number of procedures in this analysis allowed us to look at the association with greater confidence across multiple age categories. Our results suggest that endogenous ovarian steroid hormones may reduce the risk of developing diverticulosis. Given the time it takes for diverticulosis to develop, there may even be a carryover of the protective effect after the age of menopause.
Mechanistically, steroid hormones may have a protective effect on connective tissues. Dysfunctional connective tissues and associated genes have been implicated in diverticulosis biology. 7–9, 18–23 Despite finding a lower prevalence of diverticulosis in women overall, there is evidence that women over the age of 60 have a significantly increased risk of incident diverticulitis compared with men.12 This sex-specific difference in diverticulitis risk cannot be explained by an increased prevalence of diverticulosis. Instead, there must be a sex-specific factor that disproportionally drives diverticulitis risk in women over the age of 60. This disparity may be due to environmental factors. Obesity and nonsteroidal anti-inflammatory drug use increase diverticulitis risk24, while vigorous physical activity25 reduces the risk. Menopause is associated with an increased risk of visceral fat accumulation. Furthermore, women are more likely than men to be obese (women 40% versus men 35%) and are almost twice as likely to have the most severe class of obesity (women 10% versus men 6%).26 Women are also less likely to be physically active and more likely to use nonsteroidal anti-inflammatory drugs compared to men. 27, 28
There are also unexplained racial disparities in the risk of diverticulitis12 and diverticular hemorrhage.13 In the U.S., white individuals experienced the highest prevalence of hospital admissions for diverticulitis compared with black and Hispanic individuals. Asian/Pacific Islander individuals experience a much lower prevalence compared with all other races. Some of these disparities may be attributable to underlying variation in the prevalence of diverticulosis. Diverticulitis is most common in the distal colon. This study shows that non Hispanic whites have a higher prevalence of distal diverticulosis compared with non Hispanic black and Asian/Pacific Islanders, which could explain a higher incidence of diverticulitis in white individuals.
Diverticular hemorrhage is an arterial bleed that more commonly occurs in proximal diverticula compared to distal diverticula. Proximal diverticula are either congenital or acquired. Congenital diverticula are usually true diverticula that involve all three layers of the bowel wall. True diverticula may be less likely to hemorrhage compared to acquired diverticula. Acquired diverticula are mechanically vulnerable and form when the colonic mucosa and submucosa herniate through vascular portals in the muscularis propria. Similar to prior work29, 30 non Hispanic black individuals have the highest prevalence of any proximal diverticula, the majority of which are likely acquired diverticula and at risk of hemorrhage. This disparity in diverticulosis prevalence may explain why black individuals experience the highest prevalence of diverticular hemorrhage compared to other races. In contrast, Asian/Pacific Islanders have the highest prevalence of proximal only diverticulosis but are less likely to experience diverticular hemorrhage. Because the prevalence of proximal only diverticulosis did not increase with age, these diverticula are likely congenital, involve all three layers of the bowel wall, and are less likely to hemorrhage.
This work has limitations. Colonic diverticulosis is a common incidental finding on screening colonoscopy and reporting is optional. While diverticulosis was likely underreported, this reporting is unlikely to vary by age, sex and/or race/ethnicity. This type of non-differential misclassification would bias our results towards the null. Because there was significant variation in reporting diverticulosis, we included endoscopy site in our models, with no change in our results. The burden of colonic diverticulosis was not reported in this database. Therefore, we could not determine associations between demographics and number of diverticula. The burden of diverticula may drive some of the risk of complications. The accuracy of reporting diverticulosis location in the colon is unknown; as such, we categorized location into the two broad and clinically significant categories of proximal and distal. Each endoscopist reported patient race/ethnicity, which may result in misclassification of this variable. Additionally, the sites participating in CORI are not necessarily representative of all endoscopy practices in the United States. VA facilities and academic medical centers are likely over-represented. Because we included data from VA facilities, men make up more than half (54%) of our cohort. Furthermore, the majority (86%) of patients included in this study are non-Hispanic white, a proportion that differs from the U.S. population (60.4% 2010 U.S. Census). Individuals who participate in colorectal screening are generally healthier than those who do not participate in screening. Differential screening rates may contribute to differences in diverticulosis, as those who are more or less likely to get screening may also be more or less likely to get diverticulosis. Because obesity increases the risk of diverticulosis in women10, the prevalence of diverticulosis in women may be higher in the general population.
In conclusion, we found that diverticulosis was less prevalent in women compared with similar-age men in a large national endoscopic database, supporting a role for sex hormones in diverticulosis pathogenesis. Asian/Pacific Islander individuals were most likely to have proximal only diverticula, while Non-Hispanic black individuals had both distal and proximal diverticula. Differences in the risk of diverticulosis by race/ethnicity are congruent with genetic contribution to risk and account for some proportion of variation in diverticular disease risk. However, it remains unclear why women 60 years or older have a greater burden of diverticulitis than men of the same age.
Need to Know.
Background
We estimated the prevalence of diverticulosis among patients of different ages, sexes, and races and ethnicities and calculated odds ratios.
Findings
In an analysis of data from 271,181 colonoscopy procedures, the prevalence of diverticulosis increased with age in men and women of all races and ethnicities. Diverticulosis was less prevalent in women compared with similar-age men. There were also differences in the prevalence and distribution of diverticulosis by race/ethnicity.
Implications for Patient Care
Differences in diverticulosis prevalence by age and race account for some proportion of variation in diverticular disease risk. However, it not clear why women 60 years or older have a greater burden of diverticulitis than men of the same age.
Acknowledgements
The Clinical Outcomes Research Initiative was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The data from the Clinical Outcomes Research Initiative reported here were supplied by the NIDDK Central Repositories. This manuscript was not prepared in collaboration with Investigators of the Clinical Outcomes Research Initiative study and does not necessarily reflect the opinions or views of the Clinical Outcomes Research Initiative study, the NIDDK Central Repositories, or the NIDDK.
Grant Support: This research was supported in part by grants from the National Institutes of Health K23DK113225, R01DK09473, and P30 DK034987
Footnotes
Conflicts of Interest/Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology. 2009;136(2):376–86. Epub 2009/01/07. [DOI] [PubMed] [Google Scholar]
- 2.Strate LL, Morris AM. Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology. 2019; 156(5):1282–98 el. Epub 2019/01/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strate LL, Peery AF, Neumann I. American Gastroenterological Association Institute Technical Review on the Management of Acute Diverticulitis. Gastroenterology. 2015;149(7):1950–76 e12. Epub 2015/10/11. [DOI] [PubMed] [Google Scholar]
- 4.van Dijk ST, Daniels L, de Korte N, et al. Quality of Life and Persistent Symptoms After Uncomplicated Acute Diverticulitis. Dis Colon Rectum. 2019;62(5):608–14. Epub 2019/02/27. [DOI] [PubMed] [Google Scholar]
- 5.Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156(1):254–72 e11. Epub 2018/10/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zogg CK, Najjar P, Diaz AJ, et al. Rethinking Priorities: Cost of Complications After Elective Colectomy. Ann Surg. 2016;264(2):312–22. Epub 2015/10/27. [DOI] [PubMed] [Google Scholar]
- 7.Schafmayer C, Harrison JW, Buch S, et al. Genome-wide association analysis of diverticular disease points towards neuromuscular, connective tissue and epithelial pathomechanisms. Gut. 2019;68(5):854–65. Epub 2019/01/21. [DOI] [PubMed] [Google Scholar]
- 8.Sigurdsson S, Alexandersson KF, Sulem P, et al. Sequence variants in ARHGAP15, COLQ and FAM155A associate with diverticular disease and diverticulitis. Nat Commun. 2017;8:15789 Epub 2017/06/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maguire LH, Handelman SK, Du X, et al. Genome-wide association analyses identify 39 new susceptibility loci for diverticular disease. Nat Genet. 2018;50(10):1359–65. Epub 2018/09/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peery AF, Keil A, Jicha K, et al. Association of Obesity With Colonic Diverticulosis in Women. Clin Gastroenterol Hepatol. 2019. Epub 2019/05/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camilleri M, Sandler RS, Peery AF. Etiopathogenetic Mechanisms in Diverticular Disease of the Colon. Cell Mol Gastroenterol Hepatol. 2019. Epub 2019/07/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal Trends in the Incidence and Natural History of Diverticulitis: A Population-Based Study. Am J Gastroenterol. 2015;110(11):1589–96. Epub 2015/09/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheat CL, Strate LL. Trends in Hospitalization for Diverticulitis and Diverticular Bleeding in the United States From 2000 to 2010. Clin Gastroenterol Hepatol. 2016;14(1):96–103 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lieberman DA, Holub J, Eisen G, et al. Utilization of colonoscopy in the United States: results from a national consortium. Gastrointest Endosc. 2005;62(6):875–83. Epub 2005/11/23. [DOI] [PubMed] [Google Scholar]
- 15.Lieberman DA, Williams JL, Holub JL, et al. Race, ethnicity, and sex affect risk for polyps >9 mm in average-risk individuals. Gastroenterology. 2014;147(2):351–8; quiz e14–5. Epub 2014/05/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lieberman DA, Holub JL, Moravec MD, et al. Prevalence of colon polyps detected by colonoscopy screening in asymptomatic black and white patients. JAMA. 2008;300(12): 1417–22. Epub 2008/09/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7. Epub 2007/10/17. [DOI] [PubMed] [Google Scholar]
- 18.Stumpf M, Cao W, Klinge U, et al. Increased distribution of collagen type III and reduced expression of matrix metalloproteinase 1 in patients with diverticular disease. Int J Colorectal Dis. 2001;16(5):271–5. Epub 2001/11/01. [DOI] [PubMed] [Google Scholar]
- 19.Wess L, Eastwood MA, Wess TJ, et al. Cross linking of collagen is increased in colonic diverticulosis. Gut. 1995;37(1):91–4. Epub 1995/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomson HJ, Busuttil A, Eastwood MA, et al. Submucosal collagen changes in the normal colon and in diverticular disease. Int J Colorectal Dis. 1987;2(4):208–13. Epub 1987/11/01. [DOI] [PubMed] [Google Scholar]
- 21.Hellwig I, Bottner M, Barrenschee M, et al. Alterations of the enteric smooth musculature in diverticular disease. J Gastroenterol. 2014;49(8):1241–52. Epub 2013/10/12. [DOI] [PubMed] [Google Scholar]
- 22.Altadill A, Eiro N, Gonzalez LO, et al. Comparative analysis of the expression of metalloproteases and their inhibitors in resected crohn’s disease and complicated diverticular disease. Inflamm Bowel Dis. 2012;18(1):120–30. Epub 2011/03/26. [DOI] [PubMed] [Google Scholar]
- 23.Bode MK, Karttunen TJ, Makela J, et al. Type I and III collagens in human colon cancer and diverticulosis. Scand J Gastroenterol. 2000;35(7):747–52. Epub 2000/09/06. [DOI] [PubMed] [Google Scholar]
- 24.Ma W, Jovani M, Liu PH, et al. Association Between Obesity and Weight Change and Risk of Diverticulitis in Women. Gastroenterology. 2018;155(1):58–66 e4. Epub 2018/04/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strate LL, Liu YL, Aldoori WH, et al. Physical activity decreases diverticular complications. Am J Gastroenterol. 2009;104(5):1221–30. Epub 2009/04/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91. Epub 2016/06/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davis JS, Lee HY, Kim J, et al. Use of non-steroidal anti-inflammatory drugs in US adults: changes over time and by demographic. Open Heart. 2017;4(1):e000550 Epub 2017/07/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. Epub 2007/12/20. [DOI] [PubMed] [Google Scholar]
- 29.Peery AF, Keku TO, Martin CF, et al. Distribution and Characteristics of Colonic Diverticula in a United States Screening Population. Clin Gastroenterol Hepatol. 2016;14(7):980–5 e1. Epub 2016/02/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Golder M, Ster IC, Babu P, et al. Demographic determinants of risk, colon distribution and density scores of diverticular disease. World J Gastroenterol. 2011;17(8):1009–17. Epub 2011/03/31. [DOI] [PMC free article] [PubMed] [Google Scholar]