Abstract
Objectives:
In the United States (US), chronic bronchitis (CB) is common and is associated with substantial morbidity and mortality.Data on CB in the Hispanic/Latino population—a large, diverse US minority— are scarce.We aimed to test whether the prevalence of CB varies across Hispanic/Latino heritages and to identify CB risk factors including occupational exposures in this population.
Methods:
We analyzed data from the Hispanic Community Health Study/Study of Latinos, a US population-based probability sample of participants aged 18–74 years (N=16,415) including those with Mexican, Puerto Rican, Dominican, Cuban, Central American and South American heritages.Participants who had acompleted respiratory questionnaire and valid spirometric data were used for this analysis (N=13,259).CB, place of birth, heritage, occupational exposures, and other risk factors were based on standardized questionnaires.The prevalence of CB was estimated using survey logistic regression-conditional marginal analysis.
Results:
The estimated overall adjusted prevalence of CB was (mean [95%CI]) 12.1% [9.3–15.6], with a large variation across heritages.Dominican heritage had a five-fold higher prevalence than South American heritage.US-born participants had a higher adjusted prevalence than their non-US born counterparts (16.8% [12.5–22.1] vs.11.0% [8.5–14.10] P=0.022). Compared to non-exposed participants, those exposed to cleaning or disinfecting solutions had a higher adjusted prevalence of CB (12.6% [9.1–17.1] vs.11.8% [9.2–15.1] P=0.024).
Conclusions:
The prevalence of CB was higher among Dominicans than other Hispanic/Latino heritages.CB was more prevalent among US-born and those exposed to cleaning and disinfecting solutions.
Introduction
Chronic bronchitis (CB) is a common condition that is associated with worse quality of life and increased risk of all-cause mortality.1 CB affects all race/ethnic groups in the United States (US), with prevalence rates being highest among non-Hispanic Whites and Blacks (47.3/1000 and 48.6/1000, respectively).Approximately 942,000 Hispanics/Latinos in the US are affected by CB (prevalence rate 28.8/1000).1 The Hispanic/Latino population is the largest, youngest, and fastest-growing minority,2 numbering 58.9 million people or 18% of the US population (https://www.census.gov/newsroom/facts-for-features/2018/hispanic-heritage-month.html). Although they are assumed to be a homogeneous group, Hispanics/Latinos encompass people from different heritages with Mexican being the largest group —approximately two-thirds of all Hispanics.2 Despite their sizeable proportion, data on CB in Hispanics/Latinos are scarce.An early study showed that Puerto Ricans had the highest prevalence of CB;3 that study, however, included only three heritages and limited phenotypic information on smoking, place of birth, and occupational exposures.
While immigration to the US opens the possibility for new opportunities leading to improvement of Latino migrants’ quality of life, it might also imply a change in environmental exposures that increase the risk for chronic airway diseases.4 Indeed, Latino/Hispanics born in the US have higher risk of asthma than their non-US-born counterparts, suggesting that place of birth is an important risk factor for airway diseases in this population.5,6 Although the most established risk factor for CB is active smoking, several studies have shown CB to be present in 22% - 37% of never smokers.7,8 In the COPDGene study, CB was present at baseline and at a five-year follow-up in approximately 37% of those that haven’t smoked during that timeframe, showing that despite cessation of smoking, CB persisted.9 These data suggest that other exposures pose risk for the development of CB such as occupational exposures.Identifying occupational risk factors for CB is relevant to target prevention policies.Occupational exposure to dust, gases, and fumes as well as pesticides increased the risk of respiratory symptoms and CB,10,11 and cleaners have decreased lung function and a higher risk for the development of COPD, a disease that shares clinical characteristics with CB.12,13 Based on these data, we aimed to estimate the prevalence of CB across heritages in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL),14,15 and hypothesized that CB would be more prevalent in those born in the US and among exposed to occupational hazards.
Methods
The HCHS/SOL has been described previously.14,15 Briefly, itis a population-based study in 4 US communities (Bronx, NY; San Diego, CA; Miami, FL; and Chicago, IL).The goal of this study is to determine the protective and risk factors associated with major diseases.Self-identified Hispanic/Latino men and women aged 18–74 years were recruited from households selected in a random, multistage fashion. In this study, we used 18-year-old or older participants enrolled at baseline (between 2008 and 2011) who completed the respiratory questionnaire, performed valid spirometry, and had no missing data on heritage background.The household-level response rate of the identified households was 33.5%.Of 39,384 individuals who were selected, screened and met eligibility criteria, 41.7% were enrolled, representing 16,415 persons from 9,872 households.16 The participation rate for the respiratory questionnaire was 98.2%.5Questionnaires were in both English and Spanish and participants chose which language to use.Questionnaire responses and clinical measurements used in this analysis were collected at the baseline study visit. Informed consent was obtained from all study participants and HCHS/SOL was approved by each site’s IRB.The current study was approved by the Partners Human Research Committee (2017P001688/PHS).
Outcome
CB was based on participants’ responses to the respiratory questionnaire.CB was present if the participants said that they had a cough on most days/nights of the week or when waking up in the morning, both for at least 3 months in a row and at least the last 2 years.14
Covariates
Information on age, gender, place of birth, age at immigration, heritage background, acculturation, education attainment, health insurance, smoking history, and asthma history were also assessed by questionnaires.Participants were asked the following question to identify their country of birth, “In what country or territory were you born?” The answers were collapsed to US or non-US born.The age of immigration into the mainland US was defined as the current age minus the number of years living in the US.Heritage was asked with the following question: “Which best describes your Hispanic/Latino heritage?” The responses were then coded in 7 groups including Mexican, Cuban, Republic Dominican, Puerto-Rican, Central American, South American, and other/mixed heritage.Central Americans included Hondurans, Salvadorians, Guatemalans, and Nicaraguans.South Americans included Brazilians, Colombians, Ecuadorians, Peruvians, and Argentinians.Acculturation was measured with an acculturation score based on nativity, language spoken at home, and years of residence in the US.The score ranged from 0 to 5 with higher values indicating a higher acculturation level.17 Education attainment was classified as no high school or General Education Diploma (GED), at most high school or GED, and greater than high school or GED. Income was classified as less than 30,000dollars/year, 30,000 or more dollars/year, and missing. Insurance status was identified with the following questions: What type of health insurance coverage do you currently have? Do you have health insurance or other health care coverage? The variable was dichotomized as yes/no.5 Occupational exposures were asked with the following question: “In your current job(s) are you exposed to any of the following?” The options were as follows: “a) paints, varnishes, lacquers; b) glues, pastes or other adhesives; c) acids or alkalis d) pesticides; e) dusts; f) wood dust; g) cleaning or disinfecting solutions; h) petroleum products other than solvents (like grease, oil or fuel); i) cutting oils, machine oils, or metalworking fluids; j) smoke from burning wood; k) welding fumes; l) tobacco smoke; m) vehicle exhaust; n) cooking fumes; and o) solvents or degreasers.” Smoking status was classified as never, current, and former.Never smoking was defined as smoking fewer than 100 cigarettes ever.If participants did not smoke a cigarette in the previous 30 days, they were considered former smokers.If participants self-reported smoking of a cigarette in the previous 30 days, they were considered current smokers.Pack-years of smoking were calculated as the number of exposure years multiplied by the average number of cigarettes smoked per day divided by 20.This variable was categorized as 0–4.9, 5–9.9, and ≥10 pack-years.Second-hand smoke exposure was asked with the following questions “Before age 13, did you live with a regular cigarette smoker who smoked in your home?”, “Did your mother (or the primary female caregiver who lived in your home) smoke in your home?”, “Since age 13 have you ever lived with a regular cigarette smoker (not including yourself) who smoked in your home?” If the participant answered “yes” to any of those questions or answered 1 or more people to the question “Not counting yourself, how many people currently living in your household smoke regularly in the home?” then he/she was considered exposed to second-hand smoke.Asthma before age 18 years was present if the participants reported that they ever had asthma that was diagnosed by a doctor or health provider and still have this condition.5
Spirometry
Spirometry was performed according to the American Thoracic Society/European Respiratory Society guidelines using a dry rolling sealed spirometer with automated quality checks (Occupational Marketing, Houston, TX) with overreading by one investigator.5,18 All participants, except those with recent cardiovascular events or surgery, were asked to perform prebronchodilator spirometry.The median number of spirometric forced maneuvers was four.Participants with a prebronchodilator forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) ratio of 0.70 or less than the lower limit of normal met the criteria to perform post-bronchodilator spirometry.Prediction equations for the general US population were used to calculate predicted values.19 COPD was defined by a post-bronchodilator FEV1/FVC ratio of less than 0.70.5
Statistical Analysis
Means and prevalence rates were weighted to account for the sampling design, stratification, and clustering.14,15 Prevalence estimates of CB were computed by heritage background using a survey logistic regression-conditional marginal analysis.The variable selection was performed starting with univariable analyses for CB with the following risk factors: country of birth, acculturation score, education attainment, health insurance, age of immigration, smoking status (never, former, current), pack-years smoked, second-hand smoking, and asthma before 18 years.We then performed multivariable models starting with the significant factors from the univariate analysis. In this step, three variables were also added to the multivariable models: age, gender, and occupational exposures.The occupational exposures chosen were those with 10% or higher prevalence in the entire population. In the second step, backwards elimination was applied to reach the final model.Effect modifications of background in the relationships between CB and other significant variables were tested by including the appropriate interaction terms in the final model.Then the prevalence for each background was estimated with all other covariates at weighted average and interaction terms in the final model.The interpretation of these estimates was the prevalence of CB at the average of each covariate for the entire study population.Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Results
Of the 16,415 participants, 13,259 (81%) had respiratory questionnaire, valid spirometric, and heritage background data available (Figure 1).The Mexican and Puerto Rican heritages were the most common and South American and other/mixed were the lowest ones. Compared to the overall population, Cubans were older and Dominicans had a higher proportion of women.Those of Puerto Rican and other/mixed heritages had a higher proportion of US-born and immigrated to the mainland US at a younger age than the overall population.Puerto Ricans and Cubans had higher proportions of current smoking and higher pack-years smoked than the overall population.Puerto Ricans and Cubans had a higher prevalence of asthma onset before 18 years of age and COPD than the entire cohort (Table 1).
Figure 1.
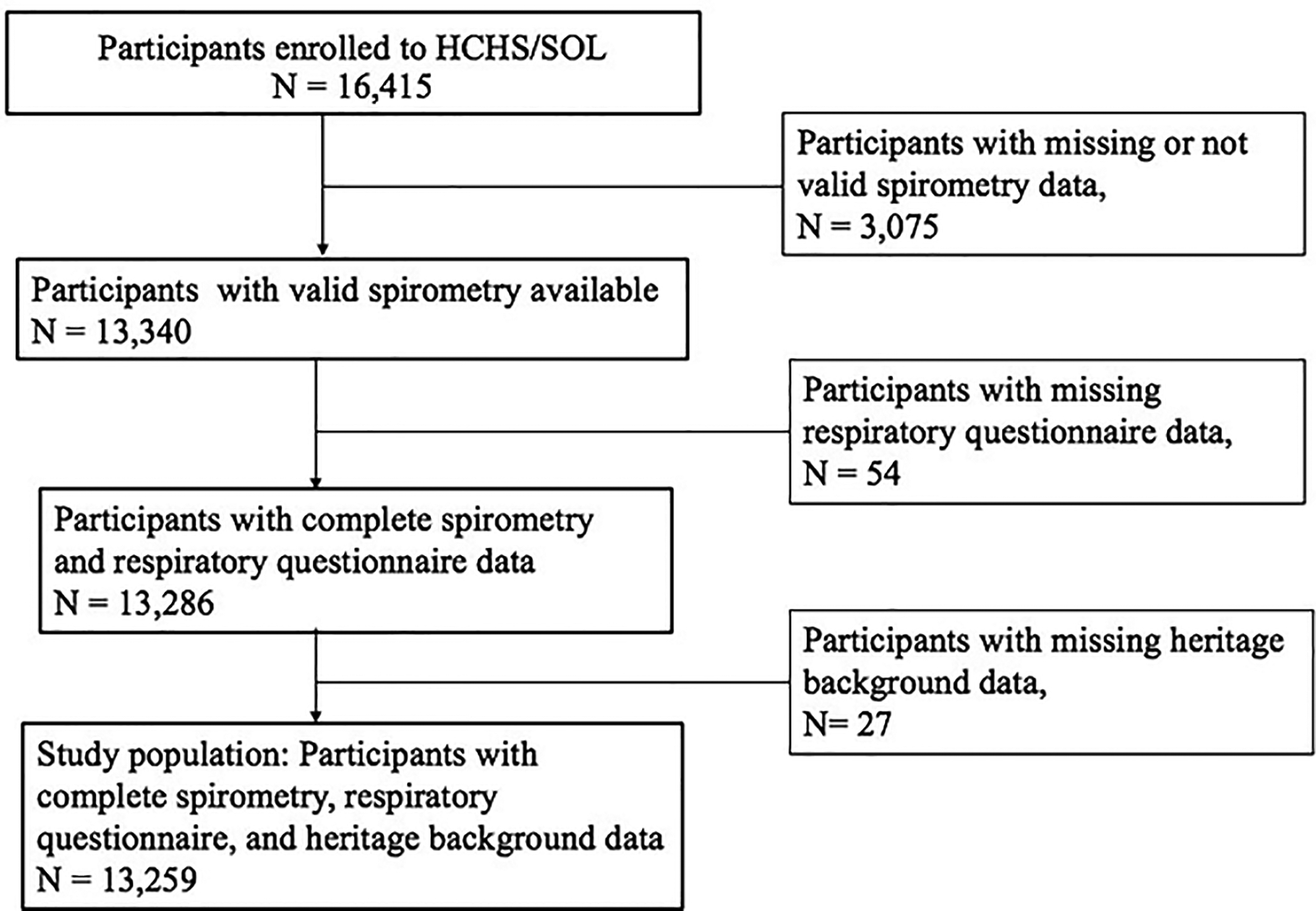
Flow chart of study participants selection
Table 1.
Characteristics of the Hispanic Community Health Study/Study of Latinos participants by heritage, 2008–2011
| Characteristic | Cuban | Dominican | Mexican | Puerto Rican | Central American | South American | Other/Mixed | Overall |
|---|---|---|---|---|---|---|---|---|
| Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | |
| Sample size, N | 2118 | 1202 | 4981 | 2214 | 1430 | 888 | 426 | 13259 |
| Age, yrs. | 46.5 (45.5–47.5) | 38.9 (37.5–40.3) | 38.5 (37.7–39.2) | 42.8 (41.7–43.8) | 39.7 (38.6–40.7) | 42.5 (40.8–44.1) | 34.5 (32.7–36.3) | 41 (40.5–41.5) |
| Male sex, % | 52.1 (49.9–54.2) | 39.7 (35.4–44.0) | 48.1 (45.9–50.3) | 52.1 (49.0–55.1) | 48.2 (44.7–51.7) | 46.2 (42.1–50.3) | 51.7 (44.2–59.3) | 48.8 (47.6–50.1) |
| US born, % | 7.5 (5.6–9.5) | 16.9 (12.6–21.1) | 24.7 (22.4–27.0) | 50.2 (46.9–53.4) | 7.6 (5.1–10.1) | 5.5 (3.4–7.5) | 54.2 (46.6–61.8) | 23.2 (21.5–24.9) |
| Age at Immigration, yrs. | 35 (34.0–35.9) | 25.4 (24.4–26.4) | 24.2 (23.3–25.0) | 18.4 (17.0–19.8) | 26.8 (26.0–27.7) | 29.5 (28.1–30.8) | 23.6 (20.1–27.1) | 27.1 (26.4–27.8) |
| Acculturation Score | 1 (0.9–1.2) | 1.8 (1.6–1.9) | 2 (1.9–2.1) | 3.3 (3.3–3.4) | 1.3 (1.2–1.5) | 1.2 (1.1–1.3) | 3 (2.8–3.3) | 1.9 (1.9–2.0) |
| Education Level, % | ||||||||
| No High School/GED, % | 22.1 (19.8–24.4) | 36.7 (32.8–40.7) | 34.8 (32.0–37.6) | 35 (31.9–38.1) | 38.7 (35.3–42.1) | 21.1 (17.1–25.1) | 20.4 (14.2–26.7) | 31.2 (29.8–32.7) |
| At most High School/GED, % | 29.7 (26.9–32.5) | 23 (19.1–26.9) | 30.5 (28.3–32.7) | 28.1 (25.5–30.6) | 25.5 (22.6–28.4) | 27.6 (23.6–31.5) | 23.7 (16.1–31.3) | 28.4 (27.2–29.6) |
| Greater Than High School/GED, % | 48.2 (45.2–51.1) | 40.2 (36.6–43.9) | 34.7 (31.4–38.1) | 36.9 (33.6–40.3) | 35.8 (32.3–39.3) | 51.3 (46.8–55.9) | 55.9 (48.0–63.8) | 40.4 (38.7–42.1) |
| Health Insurance, % | 41.5 (38.2–44.9) | 68.9 (64.6–73.2) | 42.9 (39.7–46.0) | 78.7 (76.1–81.3) | 30.8 (26.5–35.1) | 41.5 (36.8–46.1) | 56.8 (49.1–64.5) | 50.4 (48.5–52.3) |
| Smoking Status, % | ||||||||
| Never | 54 (51.1–57.0) | 77.8 (74.1–81.5) | 63.6 (61.3–65.8) | 49.3 (45.9–52.8) | 68.3 (64.8–71.8) | 64.2 (59.7–68.7) | 55.9 (48.2–63.6) | 60.7 (59.3–62.1) |
| Former | 19.2 (l7.2–21.2) | 10.1 (7.9–12.4) | 18 (16.4–19.7) | 17 (14.3–19.7) | 16.2 (13.5–18.9) | 21.7 (18.4–25.1) | 18.6 (13.3–23.9) | 17.4 (16.5–18.3) |
| Current | 26.8 (24.2–29.4) | 12.1 (8.6–15.6) | 18.4 (16.4–20.4) | 33.7 (30.5–36.9) | 15.4 (12.8–18.0) | 14 (10.7–17.3) | 25.5 (18.7–32.2) | 21.9 (20.7–23.1) |
| Pack-years Smoked Category*, % | ||||||||
| 0–4.9 | 1 (0.9–1.2) | 1.8 (1.6–1.9) | 2 (1.9–2.1) | 3.3 (3.3–3.4) | 1.3 (1.2–1.5) | 1.2 (1.1–1.3) | 3 (2.8–3.3) | 1.9 (1.9–2.0) |
| 5–9.9 | 5.2 (4.2–6.2) | 4.6 (3.1–6.2) | 5.4 (4.5–6.3) | 8.9 (7.1–10.7) | 5.2 (3.4–7.0) | 5.1 (3.2–6.9) | 5.8 (3.0–8.6) | 5.8 (5.2–6.3) |
| ≥10 | 28.4 (25.8–31.0) | 7.5 (5.9–9.1) | 7.1 (6.1–8.1) | 24.2 (21.3–27.2) | 9.7 (7.8–11.6) | 10.2 (7.9–12.6) | 11.2 (7.3–15.1) | 15.1 (13.9–16.2) |
| Second-hand Smoking, % | 78.9 (76.7–81.0) | 59.6 (55.2–64.0) | 57.7 (55.2–60.2) | 71.4 (68.2–74.6) | 55.4 (51.8–58.9) | 56.6 (52.5–60.7) | 68.1 (61.9–74.3) | 64.9 (63.5–66.4) |
| Asthma Onset Before Age 18 yrs., % | 17.7 (15.8–19.6) | 11.8 (9.0–14.6) | 5.7 (4.5–6.8) | 22.9 (20.1–25.8) | 9.7 (7.5–11.9) 4 | 6.3 (4.2–8.4) | 16.2 (10.9–21.5) | 12.4 (11.4–13.3) |
| COPD, % | 5.1 (4.2–6.1) | 2.2 (1.2–3.2) | 1.7 (1.1–2.2) | 4.3 (3.1–5.4) | 16 (0.9–2.3) | 2.2 (1.0–3.5) | 0.8 (0.1–1.4) | 2.9 (2.5–3.2) |
The estimates were calculated with PROC SURVEYMEANS and SURVEYFREQ procedures of SAS.The estimates account for sampling weight and study design.
Estimates are for smokers only.For variable descriptions and abbreviations see text.
Among subjects who were currently employed (N=6,859), the three most common current occupational exposures were cleaning or disinfecting solutions, dusts, and solvents or degreasers.Central Americans and Cubans had the highest and lowest exposure rates to cleaning or disinfecting solutions (Table 2).
Table 2.
Prevalence estimates of current occupational exposures from the Hispanic Community Health Study/Study of Latinos by heritage, 2008–2011
| Current Occupational Exposure | Cuban | Dominican | Mexican | Puerto Rican | Central American | South American | Other/Mixed | Overall |
|---|---|---|---|---|---|---|---|---|
| Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | Estimate (95%CI) | |
| Sample size, N | 902 | 624 | 2843 | 865 | 835 | 564 | 226 | 6859 |
| Paints, varnishes, lacquers, % | 17.9 (14.9–20.8) | 13.4 (10.0–16.9) | 16.8 (14.6–19.0) | 17.7 (14.1–21.2) | 21.2 (17.3–25.0) | 18.2 (13.8–22.6) | 17 (15.7–18.3) | |
| Glues, pastes or other adhesives, % | 14.2 (11.8–16.6) | 11 (7.7–14.4) | 16.3 (14.0–18.5) | 18.6 (15.1–22.1) | 17.4 (13.9–20.8) | 10.4 (7.1–13.8) | 7.8 (2.9–12.8) | 15 (13.8–16.3) |
| Acids or alkalis, % | 9.2 (7.0–11.5) | 4.7 (2.5–6.8) | 9.2 (7.6–10.8) | 9.2 (6.4–12.0) | 8.4 (6.1–10.6) | 5.3 (2.9–7.6) | 3.2 (0.7–5.7) | 8.2 (7.3–9.1) |
| Pesticides, % | 2.7 (1.6–3.7) | 5.5 (2.9–8.1) | 5.8 (4.2–7.5) | 7.3 (5.1–9.6) | 4.1 (2.3–5.8) | (2.5–6.8) | 7.1 (2.0–12.2) | 5.2 (4.4–6.1) |
| Dusts, % | 32.7 (28.9–36.5) | 29.2 (24.2–34.2) | 32.8 (29.5–36.2) | 42.6 (37.7–47.6) | 38.1 (34.0–42.3) | 29.2 (24.3–34.0) | 36.7 (26.3–47.0) | 34.1 (32.1–36.1) |
| Wood dust, % | 10.5 (8.3–12.7) | 13 (9.4–16.6) | 13.8 (11.7–15.9) | 17.8 (14.2–21.4) | l7.9 (14.2–21.6) | 13.9 (10.0–17.8) | 16 (9.5–22.4) | 14.1 (12.9–15.3) |
| Cleaning or disinfecting solutions, % | 32.1 (28.8–35.3) | 44 (37.9–50.2) | 40.8 (37.8–43.7) | 41.3 (36.4–46.2) | 46.3 (42.2–50.4) | 35.8 (30.4–41.3) | 37.4 (27.8–46.9) | 39.6 (37.8–41.4) |
| Petroleum products other than solvents, % | 11.8 (9.2–14.3) | 9 (6.0–11.9) | 13.9 (11.6–16.2) | 13.7 (10.5–17.0) | 13.5 (10.3–16.6) | 9 (6.1–11.9) | 9.5 (4.4–14.6) | 12.5 (11.3–13.7) |
| Cutting oils, machine oils or metalworking fluids, % | 9.4 (7.0–11.7) | 9.1 (5.7–12.5) | 129 (11.0–14.8) | 12.8 (9.7–15.9) | 13.5 (10.5–16.5) | 8.1 (5.4–10.9) | 10.6 (5.4–15.7) | 11.5 (10.4–12.6) |
| Smoke from burning wood, % | 2.8 (1.4–4.1) | 4.5 (2.2–6.8) | 56 (4.1–7.1) | 4.5 (2.9–6.1) | 5.1 (3.2–7.0) | 6 (3.2–8.7) | 3.8 (0.0–8.2) | 4.7 (4.0–5.5) |
| Welding fumes, % | 7.3 (5.2–9.3) | 5.1 (2.5–7.7) | 8.2 (6.8–9.7) | 9.3 (6.4–12.3) | 9.9 (6.9–12.8) | 6 (3.2–8.7) | 6 (2.2–9.7) | 7.8 (6.9–8.7) |
| Tobacco smoke, % | 11.8 (9.3–14.4) | 10.9 (7.4–14.5) | 14.3 (12.2–16.5) | 19.6 (15.8–23.3) | 17.6 (14.3–21.0) | 12.6 (9.3–16.0) | 19.9 (12.6–27.2) | 14.6 (13.4–15.9) |
| Vehicle exhaust, % | 12.9 (10.0–15.8) | 10.1 (7.0–13.2) | 12.4 (10.3–14.5) | 15.9 (12.3–19.5) | 10.5 (7.8–13.1) | 10 (6.5–13.5) | 12 (5.8–18.2) | 12.4 (11.2–13.6) |
| Cooking fumes, % | 5.8 (4.1–7.5) | 9.6 (6.0–13.2) | 15.4 (13.2–17.6) | 11.2 (7.7–14.8) | 10.6 (8.3–12.9) | 15.3 (11.5–19.1) | 12.4 (5.6–19.2) | 12.1 (10.9–13.3) |
| Solvents or degreasers, % | 22.4 (19.4–25.4) | 7.5 (4.7–10.3) | 21 (18.6–23.4) | 11 (7.9–14.2) | 19.9 (16.4–23.4) | 18.3 (14.2–22.3) | 16.2 (9.3–23.1) | 18.3 (16.9–19.7) |
Population estimates are from the participants who reported having a current job (N=6859).The estimates were calculated with PROC SURVEYMEANS and SURVEYFREQ procedures.The estimates account for sampling weight and study design.
Prevalence of chronic bronchitis
The estimated overall adjusted prevalence was (mean [95% Confidence Interval]) 12.1% [9.3–15.6].There were substantial variations in the adjusted prevalence of CB across Hispanic/Latino heritages (Table 3).The prevalence was highest among Dominicans and Puerto Ricans, intermediate among Cubans, Mexicans, and Central Americans, and lowest among South Americans.When income was forced in the final model, it was not significant (P=0.76) and there were negligible changes in the estimates for the association between CB and Hispanic/Latino heritage background (data not shown).
Table 3.
Prevalence Estimates (%) of Chronic Bronchitis from the Hispanic Community Health Study/Study of Latinos by heritage, 2008–2011
| Cuban Estimate (95%CI) | Dominican Estimate (95%CI) | Mexican Estimate (95%CI) | Puerto Rican Estimate (95%CI) | Central American Estimate (95%CI) | South American Estimate (95%CI) | P-value |
|---|---|---|---|---|---|---|
| 9.6 (5.4–16.6) | 25.6 (14.5–41.0) | 9.5 (6.2–14.4) | 15.1 (10.4–21.4) | 7.9 (2.4–23.2) | 5.0 (1.4–16.6) | <.0001 |
The estimates account for sampling weight and study design.P-value comparing background was estimated with a survey logistic regression-conditional marginal Wald F test with 6 degrees of freedom.
The model was adjusted for age, US-born (reference US-born), smoking status (never, current, former; reference: never smoker), pack-years smoked (0–4.9, 5–9.9, and ≥10; reference: 0–4.9 category), exposure to cleaning or disinfecting solutions (reference: no exposure), asthma onset before age 18 years (reference: no asthma onset before age 18 years), background*US born, background*smoking status, and background*pack-years (heritage background reference: Mexican).Participants who reported not having a current job were assumed as non-exposed.All individual variables and interaction terms in this model were significant P≤0.0239).
Other/mixed heritage estimate from this model is not reported due to a low number of subjects for some covariate categories.
US-born and Chronic Bronchitis
The adjusted prevalence of CB in US-born participants was 16.8% (12.5–22.1) compared to 11.0% (8.5–14.10) among non-US-born participants (P=0.022).These differences were independent of age, smoking status, pack-year smoked, asthma onset before age 18 years, and exposure to cleaning and disinfecting solutions.We found no evidence of differences in the prevalence of CB according to the age of immigration.The heritage background modified the association between CB and US-born (P=0.0126 for the interaction).While most of the US-born heritages had a higher prevalence of CB, non-US-born South Americans had a slightly higher prevalence (Figure 2, Panel A).
Figure 2.
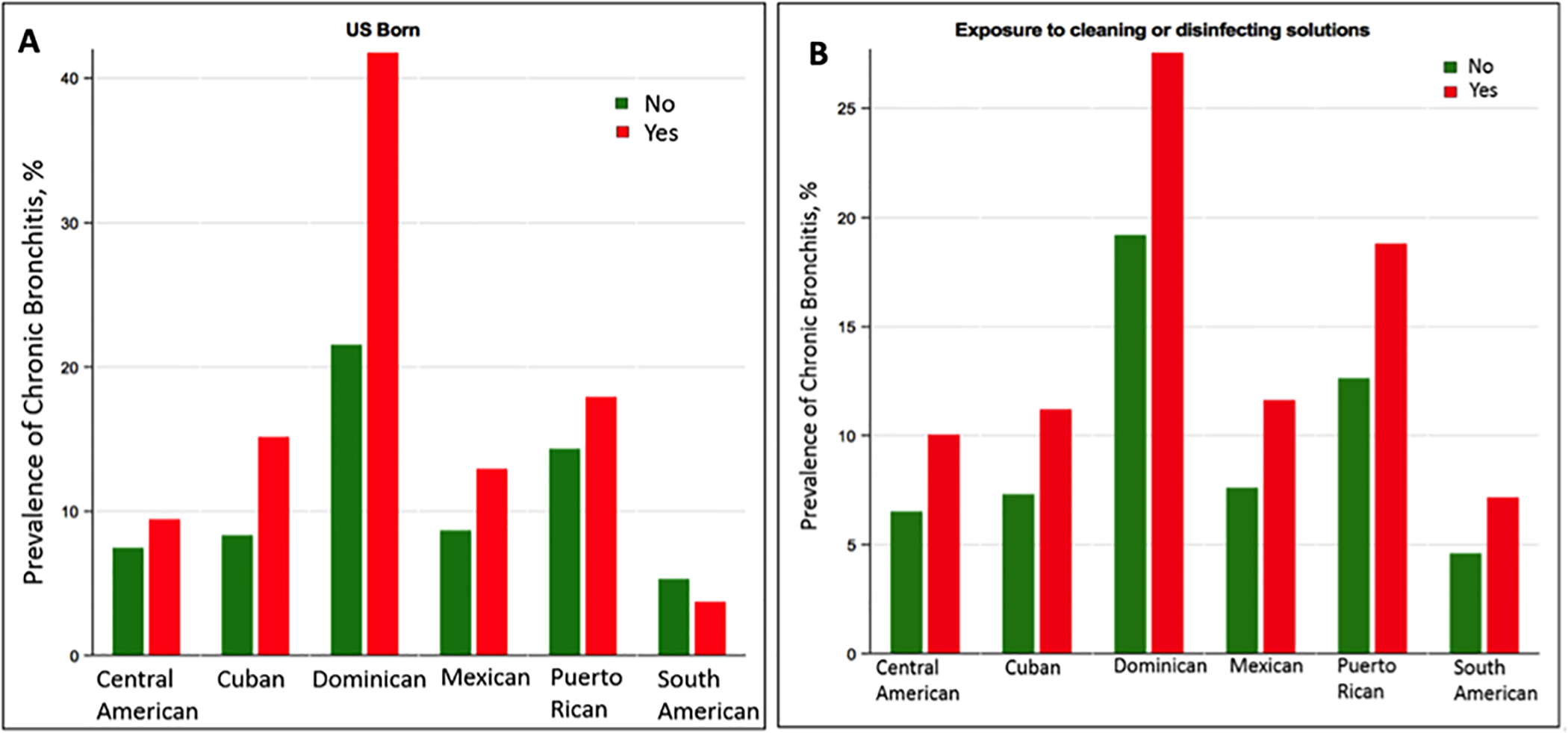
Estimated adjusted prevalence of chronic bronchitis by US-born (Panel A)and by exposure to cleaning or disinfecting solutions (Panel B) across heritages from the Hispanic Community Health Study/Study of Latinos.See the footnote of Table 3 for a description of the multivariable model.Other/mixed heritage estimate from this model is not reported due to a low number of subjects for some covariate categories.
Occupational Exposure and Chronic Bronchitis
Among the current occupational exposures asked the participants, those exposed to cleaning or disinfecting solutions had a higher adjusted prevalence of CB than those not exposed (12.6% [9.1–17.1] vs.11.8% [9.2–15.1] P=0.024).Both other individual current occupational exposures and the number of current occupational exposures were not significant in the final model.The background did not modify the association between CB and exposure to cleaning or disinfecting solutions (P=0.57), with the adjusted prevalence in exposed participants being consistently higher among all Hispanic/Latino heritages (Figure 2, Panel B).There was no interaction between exposure to cleaning or disinfecting solutions and place of birth (US-born/non-US-born) (P=0.52).
Subgroup Analysis
The risk factors for CB in the subset of subjects with COPD were similar to those of the entire population but both asthma onset before age 18 years and exposure to cleaning or disinfecting solutions were not significant in the final model (data not shown).Additional analyses showed that Dominicans and Puerto Ricans consistently had the highest prevalence of CB among participants without COPD and those without asthma.Dominicans also had the highest prevalence of CB among never-smoker participants, while Puerto Ricans ranked third in this subgroup.The estimates of the prevalence of CB for the heritage backgrounds across those subgroups were variable.For example, for Dominicans, the prevalence of CB ranged from 25.4% among non-COPD participants to 12.0% in non-asthma participants.
Discussion
We showed in a large population-based study of US Hispanics/Latinos a striking variation in the prevalence of CB across heritages, with Dominicans having up to five-fold higher prevalence than other Latinos/Hispanics.We also have shown that US-born and current exposure to cleaning and disinfecting solutions are risk factors for CB.
US Hispanics/Latinos are a diverse group based on heritage, nativity (US-born and non-US-born), and exposure to CB risk factors.2 In this study, the largest on CB in this population, we found striking variability in the prevalence of CB, with Dominicans and Puerto Ricans having the highest prevalence in adjusted models.A prior study limited to three Hispanic heritages showed that Puerto Ricans had the greatest prevalence of CB, although the estimate was lower than the current one.3 Unlike the prior study, the present one had a broader representation of the Hispanic heritages and used more factors influencing CB such as nativity, measures of socioeconomic status (i.e., education attained and yearly income), smoking status, smoking intensity, and current occupational exposures.Our finding keeps with other small and large studies that have also found large variability in the prevalence of other airway diseases such as asthma and COPD across heritages.For instance, Barr and colleagues using HCHS/SOL data reported that Puerto Ricans had the highest prevalence of asthma (36.5%) among US Hispanics/Latinos, and Menezes and associates using data from a Latin American cohort showed that Mexicans had the lower prevalence of COPD compared to other South American countries.5,20 While our study does not address the mechanisms underlying these differences in the prevalence of CB, they might be due in part to differences in early-life exposures, unmeasured socioeconomic factors, other environmental exposures, and genetics.Dominicans and Puerto Ricans have a higher proportion of African ancestry than other heritages.21 A greater African ancestry percent has been related to lower lung function22, suggesting a potential susceptibility for airway diseases.
In this study, two factors were associated with an increasing prevalence of CB in this population: place of birth and occupational exposure to cleaning and disinfecting solutions.We found that non-South American Hispanics/Latinos born in the US had a higher prevalence of CB than their non-US counterparts.This finding is in agreement with prior reports showing an increased higher prevalence of asthma in US-born Hispanics/Latinos and United Kingdom-born Whites than Hispanic/Latino and White immigrants, respectively.5,23,24 These differences might be due to unmeasured factors including differences in exposure to air pollution. In the US, 28.3% of Hispanics/Latinos live near a major highway and 80% live in neighborhoods that do not meet at least one Environmental Protection Agency air-quality standard.2,25 Long-term exposure to outdoor environments with high pollution may increase the prevalence of CB.Another explanation is that US-born Hispanics/Latinos have more access to regular health care than immigrants,2 being more likely to be diagnosed with CB. Additionally, immigrants tend to be healthier than their home-country population (the healthy migrant effect), which may also explain the lower prevalence of CB in this group.Further studies are needed to test the place of birth as a potential risk factor for CB.
In this study, we also found that participants exposed to cleaning and disinfecting solutions at work had a higher prevalence of CB.This finding expands upon prior evidence on a variety of occupations such as farming and livestock farming and occupational exposures including vapors, dusts, gases, solid fuel, metals, and agricultural pesticides that have been linked to CB.10,26–30 Our finding is further supported by research showing an increased risk of COPD among US workers employed in the “Building and grounds cleaning and maintenance” occupations.12 Although our study does not address the mechanisms of this association, it has been suggested that cleaning agents irritate the airways.13 Thus, repeated exposures to these agents might induce hypertrophy and/or hyperplasia of mucus-producing cells leading to an increased mucus production, which manifests as cough and phlegm, the defining symptoms of CB.Regardless of the underlying mechanism, in 2018, 5.8 million people (38.8% Hispanics/Latinos) worked in the “Building and grounds cleaning and maintenance” occupations, according to the US Department of Labor (https://www.bls.gov/cps/cpsaat11.htm), and were likely exposed to cleaning and disinfecting solutions. Thus, we believe that the prior and present findings are helpful to inform occupation-specific policies of respiratory disease prevention.They also highlight the need to consider occupational exposures when evaluating patients with CB.
This study has limitations. First, the study response rate was low, which might reflect the challenges of recruiting minorities to epidemiological studies in the US.To reduce the potential bias of estimates due to study non-participation, the HCHS/SOL team used a widely accepted statistical adjustment protocol. Also, HCHS/SOL is a predominantly urban population sampling of a few cities. Thus, certain exposures such as pesticides might be lower in urban compared to rural settings.Because of all the above factors above, caution should be exercised when extrapolating these findings to the entire US Hispanic/Latino population.Another potential limitation of this study is the healthy worker effect.Because of the study design, workers with poor health status are likely underrepresented in this cohort. Thus, we may have underestimated(or not detected) the effects of different occupational exposures on CB.This cohort has no control group by HCHS/SOL design, preventing comparison with non-Hispanic/Latino groups; however, our results do fill a gap in knowledge of CB for this minority.We did not have data available for air pollution making itimpossible to account for this risk factor.Hispanic heritage, occupational exposures, and CB ascertainment were all self-reported.Although recent studies have shown a strong correlation between self-reported heritage and genetic markers,21 it is possible that there were exposure and symptom misclassifications. Finally, data on occupational exposure lacked key information such as cumulative exposure time to the current occupational exposures, preventing us from performing a more comprehensive analysis of the relationships between occupational factors and CB.
In summary, in this large population-based study we have demonstrated that the prevalence of CB varies across heritage backgrounds, highest among Dominicans and Puerto Ricans, and that place of birth and occupational exposure to cleaning and disinfecting solutions are factors associated with increased prevalence of CB in US Hispanics/Latinos.
What is already known about this subject?
Chronic bronchitis is associated with increased morbidity and mortality.The most established risk factor is smoking.The prevalence and risk factors associated with chronic bronchitis among US Hispanics/Latinos have not been well described.
What are the new findings?
The prevalence of chronic bronchitis among US Hispanics/Latinos varied widely across heritages, and there was an increased prevalence among those born in the US and those exposed to cleaning or disinfecting solutions, independent of smoking status.
How might this impact on policy or clinical practice in the foreseeable future?
The clinician should have heightened awareness of the risks associated with exposure to cleaning and disinfecting solutions in the development of chronic bronchitis, and respiratory protective masks should be given to those exposed to cleaning and disinfecting solutions.
Acknowledgments
The authors thank the staff and participants of HCHS/SOL for their important contributions.A complete list of staff and investigators has been published previously15 and is also available on the study website (http://www.cscc.unc.edu/hchs/).Statistical analyses were performed at the Brigham and Women’s Hospital following the directions of HCHS/SOL documentation.The authors also thank the National Heart, Lung, and Blood Institute BioLINCC staff for making the data available for this analysis.
Funding/Support: Dr.Diaz receives funding support from the National Heart, Lung, and Blood Institute of the NIH under award number R01-HL133137 and the Brigham and Women’s Hospital Minority Faculty Career Development Award.
Role of the Funder/Sponsor: The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures:
Dr.Kim has received personal fees from Medscape, Gala Therapeutics, AstraZeneca, Boehringer Ingelheim, and the American Board of Internal Medicine over the last three years, outside of the submitted work.Dr.Wang has no conflicts to disclose.Dr.Mannino is an employee and shareholder of GlaxoSmithKline.Dr.Diaz reported receipt of grant funding from the National Institutes of Health (NIH) and the Brigham and Women’s Hospital Minority Faculty Career Development Award.
Publisher's Disclaimer: Disclaimer: This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.The authors used the public data sets of HCHS/SOL, which may differ from those used for HCHS/SOL in their publications.
References
- 1.Kim V, Criner GJ.The chronic bronchitis phenotype in chronic obstructive pulmonary disease: features and implications.Curr Opin Pulm Med 2015;21:133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diaz AA, Celli B, Celedon JC.Chronic Obstructive Pulmonary Disease in Hispanics.A 9-Year Update.Am J Respir Crit Care Med 2018;197:15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bang KM, Gergen PJ, Carroll M.Prevalence of chronic bronchitis among US Hispanics from the Hispanic Health and Nutrition Examination Survey, 1982–84.Am J Public Health 1990;80:1495–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diaz AA, Come CE, Mannino DM, et al. Obstructive lung disease in Mexican Americans and non-Hispanic whites: an analysis of diagnosis and survival in the National Health and Nutritional Examination Survey III Follow-up Study.Chest 2014;145:282–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barr RG, Aviles-Santa L, Davis SM, et al. Pulmonary Disease and Age at Immigration among Hispanics.Results from the Hispanic Community Health Study/Study of Latinos.Am J Respir Crit Care Med 2016;193:386–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rose D, Mannino DM, Leaderer BP.Asthma prevalence among US adults, 1998–2000: role of Puerto Rican ethnicity and behavioral and geographic factors.Am J Public Health 2006;96:880–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pelkonen M, Notkola IL, Nissinen A, Tukiainen H, Koskela H.Thirty-year cumulative incidence of chronic bronchitis and COPD in relation to 30-year pulmonary function and 40-year mortality: a follow-up in middle-aged rural men.Chest 2006;130:1129–37. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Garcia M, Caballero A, Jaramillo C, Torres-Duque CA.Chronic bronchitis: High prevalence in never smokers and underdiagnosis- A population-based study in Colombia.Chron Respir Dis 2019;16:1479972318769771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim V, Zhao H, Boriek AM, et al. Persistent and Newly Developed Chronic Bronchitis Are Associated with Worse Outcomes in Chronic Obstructive Pulmonary Disease.Annals of the American Thoracic Society 2016;13:1016–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sunyer J, Zock JP, Kromhout H, et al. Lung function decline, chronic bronchitis, and occupational exposures in young adults.Am J Respir Crit Care Med 2005;172:1139–45. [DOI] [PubMed] [Google Scholar]
- 11.Negatu B, Kromhout H, Mekonnen Y, Vermeulen R.Occupational pesticide exposure and respiratory health: a large-scale cross-sectional study in three commercial farming systems in Ethiopia.Thorax 2017;72:498–9. [DOI] [PubMed] [Google Scholar]
- 12.Doney B, Hnizdo E, Syamlal G, et al. Prevalence of chronic obstructive pulmonary disease among US working adults aged 40 to 70 years.National Health Interview Survey data 2004 to 2011.J Occup Environ Med 2014;56:1088–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Svanes O, Bertelsen RJ, Lygre SHL, et al. Cleaning at Home and at Work in Relation to Lung Function Decline and Airway Obstruction.Am J Respir Crit Care Med 2018;197:1157–63. [DOI] [PubMed] [Google Scholar]
- 14.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos.Ann Epidemiol 2010;20:642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos.Ann Epidemiol 2010;20:629–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Afshar M, Wu D, Durazo-Arvizu R, et al. Association of Serum Lipids and Obstructive Lung Disease in Hispanic/Latino Adults of Diverse Backgrounds.J Pulm Respir Med 2017;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA).Diabetes Care 2008;31:1621–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests.Eur Respir J 2005;26:948–68. [DOI] [PubMed] [Google Scholar]
- 19.Hankinson JL, Odencrantz JR, Fedan KB.Spirometric reference values from a sample of the general U.S.population.Am J Respir Crit Care Med 1999;159:179–87. [DOI] [PubMed] [Google Scholar]
- 20.Menezes AM, Perez-Padilla R, Jardim JR, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study.Lancet 2005;366:1875–81. [DOI] [PubMed] [Google Scholar]
- 21.Conomos MP, Laurie CA, Stilp AM, et al. Genetic Diversity and Association Studies in US Hispanic/Latino Populations: Applications in the Hispanic Community Health Study/Study of Latinos.Am J Hum Genet 2016;98:165–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar R, Seibold MA, Aldrich MC, et al. Genetic ancestry in lung-function predictions.N Engl J Med 2010;363:321–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holguin F, Mannino DM, Anto J, et al. Country of birth as a risk factor for asthma among Mexican Americans.Am J Respir Crit Care Med 2005;171:103–8. [DOI] [PubMed] [Google Scholar]
- 24.Netuveli G, Hurwitz B, Sheikh A.Ethnic variations in incidence of asthma episodes in England & Wales: national study of 502,482 patients in primary care.Respir Res 2005;6:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wernette DR, Nieves LA.Breathing polluted air: minorities are disproportionately exposed.EPA J 1992;18:16–7. [Google Scholar]
- 26.Tual S, Clin B, Leveque-Morlais N, Raherison C, Baldi I, Lebailly P.Agricultural exposures and chronic bronchitis: findings from the AGRICAN (AGRIculture and CANcer) cohort.Ann Epidemiol 2013;23:539–45. [DOI] [PubMed] [Google Scholar]
- 27.Eduard W, Pearce N, Douwes J.Chronic bronchitis, COPD, and lung function in farmers: the role of biological agents.Chest 2009;136:716–25. [DOI] [PubMed] [Google Scholar]
- 28.Mamane A, Baldi I, Tessier JF, Raherison C, Bouvier G.Occupational exposure to pesticides and respiratory health.Eur Respir Rev 2015;24:306–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG.COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis.Thorax 2010;65:221–8. [DOI] [PubMed] [Google Scholar]
- 30.Lytras T, Kogevinas M, Kromhout H, et al. Occupational exposures and incidence of chronic bronchitis and related symptoms over two decades: the European Community Respiratory Health Survey.Occup Environ Med 2019;76:222–9. [DOI] [PubMed] [Google Scholar]


