Abstract
Hiccups (singultus) are reflex inspiratory movements that involve the swallowing reflex arc and can be classified as acute (<48 h) or persistent (>48 h). A 62-year-old man with no history of malignancy or pulmonary disease presented to the Emergency Department with a four-day history of persistent hiccups. Other than episodic hiccupping, his physical examination was otherwise unremarkable. An abnormal chest X-ray led to a CT scan of the chest with IV contrast, which demonstrated regional, peripheral groundglass opacities of the upper lobes with small focal groundglass opacities scattered throughout the lungs. He was tested for COVID-19 per admission protocol, started on hydroxychloroquine, his hiccups improved, and he was discharged to home after 3 days. An emergency medicine physician should keep COVID-19 on the differential and be vigilant of exposure in atypical presentations.
1. Introduction
Hiccups are involuntary, spasmodic contractions of the diaphragm and intercostal muscles [1]. The majority of hiccup bouts (<48 h) are transient and resolve spontaneously, however, prolonged hiccups lasting >48 h may be attributable to serious underlying pathology and affect quality of life [2]. Although a specific etiology is often not found, a detailed history, physical examination, and diagnostic testing should be pursued to rule out underlying disease and target therapeutic intervention [3].
In December of 2019, a novel coronavirus (COVID-19) was discovered in Wuhan, Hubei Province in China and has since spread throughout the world. To date, >750,000 confirmed cases of COVID-19 have been reported globally [4]. A case report of 138 COVID-19 positive patients in Wuhan, China described fever, fatigue, and dry cough as the most common presenting symptoms, although a wide array of presenting complaints have been identified, including but not limited to myalgias, headache, hemoptysis, and isolated gastrointestinal symptoms among others [5,6]. Here we describe a case report of a male patient who presented with persistent hiccups as his chief complaint and was found to be COVID (+) with ground glass opacities on computed tomography (CT) of his chest.
2. Case report
A 62-year-old male with a past medical history of diabetes, hypertension, and coronary artery disease presented to the Emergency Department (ED) with a chief complaint of weight loss and hiccups. He endorsed a twenty-five-pound unintentional weight loss over the last four months, and more recently, persistent hiccups for four days prompting his visit to the ED. He denied a history of cancer or current cigarette use. He denied fevers, nasal congestion, sore throat, chest pain, or shortness of breath that was different from baseline. He denied recent travel or sick contacts.
On arrival to the ED, vital signs were temperature 37.3 °C, heart rate 96 beats per minute, blood pressure 137/70, 20 respirations per minute, and oxygen saturation 97% on room air. Lung examination was notable for non-labored respirations with clear breath sounds bilaterally. The reminder of his physical examination was unremarkable.
The ED treatment team pursued imaging to rule out a mediastinal mass in the setting of persistent hiccups and weight loss. A chest X-ray showed new groundglass opacities in the right upper lung, left mid and lower lungs, and right costophrenic angle (Fig. 1 ). A CT chest with contrast demonstrated regional, peripheral groundglass opacities of the upper lobes with small focal groundglass opacities scattered throughout the lungs (Fig. 2, Fig. 3 ). Laboratory values were notable for a leukopenia of 4200 cells and thrombocytopenia of 15,000 platelets. He was found to be hyponatremic (131) and hypochloremic (98), otherwise the remainder of his laboratory studies including his troponin, metabolic panel, lactate, and urine studies were non-contributory. The patient was subsequently moved to an isolation room and received 1 g of ceftriaxone and 500 mg of azithromycin intravenously for possible pneumonia. A respiratory viral panel and COVID-19 swab were sent, and he was admitted to the COVID medical unit as a person under investigation.
Fig. 1.
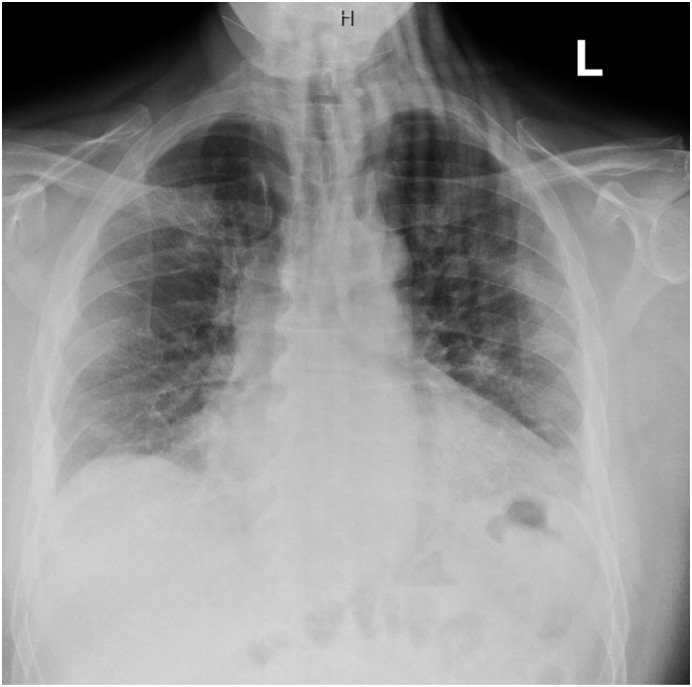
A chest radiograph demonstrating groundglass opacities in the right upper lung, left mid and lower lungs, and right costophrenic angle.
Fig. 2.
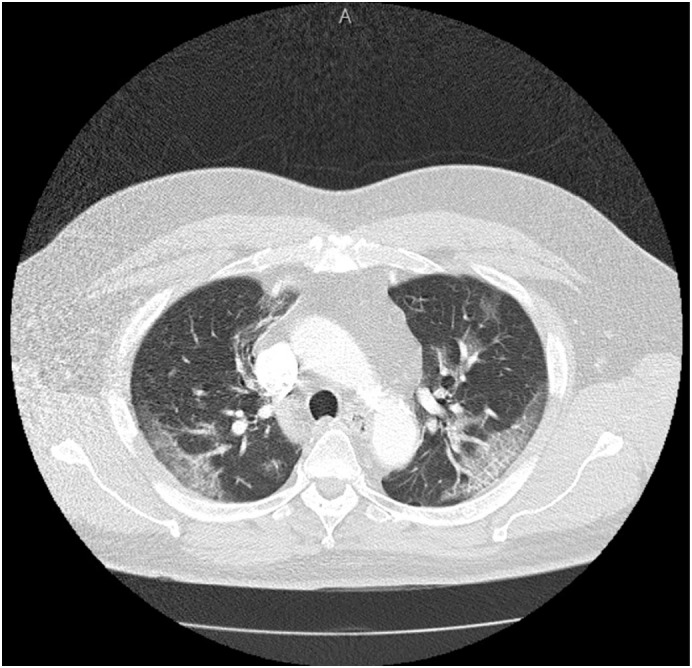
A computed tomography scan of the chest demonstrating peripheral groundglass opacities of the upper lung lobes.
Fig. 3.
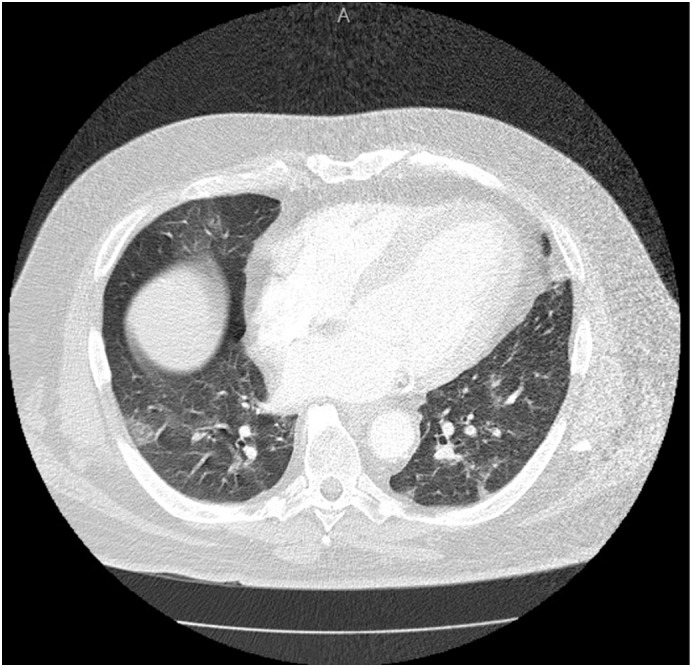
A computed tomography scan of the chest demonstrating scattered ground glass opacities in the lower lung lobes.
On arrival to the medical unit he was febrile to 38.4 °C and mildly tachycardic with a heart rate of 104 beats per minute. He placed on contact and airborne isolation and started on hydroxychloroquine 400 mg BID for one day, followed by 200 mg BID for 5 days for suspected COVID-19 infection. The following day the patient was found to be COVID positive. Symptomatic care was continued and the patient was discharged three days after admission in stable condition.
3. Discussion
Information regarding the clinical characteristics of COVID-19 is rapidly evolving as data continues to emerge throughout the world. Here we present a case of persistent hiccups as the presenting symptom of a COVID-19 infection in a 62-year-old man. To our knowledge, this is the first case report of persistent hiccups as the presenting complaint in a COVID-19 positive patient in emergency medicine literature.
This case report highlights two important issues: first, it stresses the importance of a detailed evaluation in those presenting with hiccups, at a minimum taking a thorough history, physical exam, obtaining basic laboratory work, and getting a chest X-ray. Second, physicians should keep COVID-19 infection on their differential as more cases are discovered through atypical presentations. Providers must be vigilant and maintain personal protective equipment to avoid exposure from the undifferentiated patient.
Meetings/funding/conflicts of interest
None.
Author contributions
N/A.
Contributor Information
Garrett Prince, Email: garrett.prince@cookcountyhhs.org.
Michelle Sergel, Email: msergel@cookcountyhhs.org.
References
- 1.Federspil P.A., Zenk J. Hiccup. HNO. 1999 Oct;47(10):867–875. doi: 10.1007/s001060050527. [DOI] [PubMed] [Google Scholar]
- 2.Smith H.S., Busracamwongs A. Management of hiccups in the palliative care population. Am J Hosp Palliat Care. 2003;20:149. doi: 10.1177/104990910302000214. [DOI] [PubMed] [Google Scholar]
- 3.Rousseau P. Hiccups. South Med J. 1995;85:175. doi: 10.1097/00007611-199502000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Johns Hopkins University Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu/map.html
- 5.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan China. Lancet. 2020;395:497. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


