Dear Editor,
The first confirmed case of SARS-CoV-2 in the city of Barcelona, Spain, was identified on February 25th, 2020. Since then, the epidemic spread countrywide, and Spain has become the second most affected country worldwide (130,759 cases, on April 5th) after the United States, and the second in the number of deaths (12,418 deaths, on April 5th) after Italy (Our World in Data, 2020). The regions most affected are Madrid and Catalonia, where Barcelona is located (Supplementary Fig. 1).
The transmission of coronaviruses can be affected by several factors, including the climate (Hemmes et al., 1962). Therefore, it is essential to understand the role that weather conditions could have on the transmission of COVID-19. However, there is still a lack of evidence. A previous study in the four major Chinese cities suggested that the SARS outbreak was significantly associated with the temperature, increasing the daily incidence rate with lower temperatures (Tan et al., 2005). Recent preprint studies using national data from countries affected by COVID-19 reported that low temperature is beneficial to the viral transmission (Triplett, 2020; Wang et al., 2020a, 2020b). However, these should be taken with caution since have not yet been peer reviewed.
We collected daily incidence rate of diagnosed cases confirmed from PCR tests in the Barcelona's Health Region (Regió Sanitària de Barcelona), between March 2nd and April 5th, 2020. Data was collected from the COVID-19 registry of PCR tests by the Health Evaluation and Quality Agency of Catalonia (AQuAs, 2020). Daily maximum temperature was provided by the Meteorological Service of Catalunya (MeteoCat). We fitted a quasi-Poisson regression model allowing for features specific to the infectious disease context (Imai et al., 2015). We adjusted for linear and quadratic trends, weekends, and tthe lookdown period (after March 16th). We accounted for residual autocorrelation by adjusting for the logarithm of lagged outcome (Brumback et al., 2000). Since the median incubation period for COVID-19 is over 5–6 days (Lauer et al., 2020), we used a one week distributed lag model (Gasparrini et al., 2010).
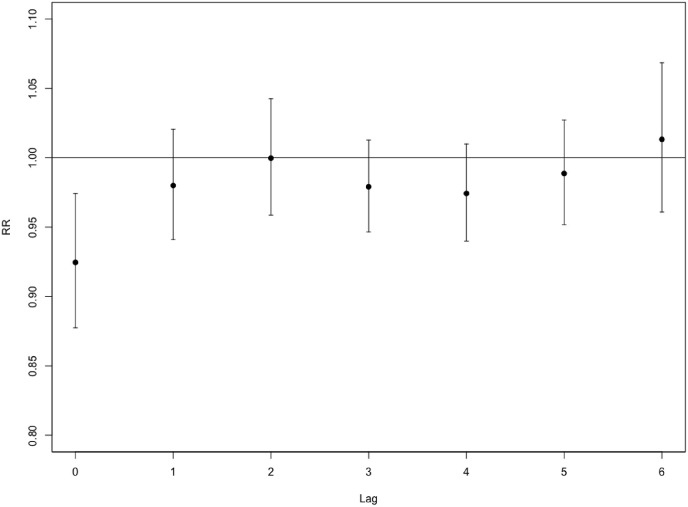
The incidence rate of a positively diagnosed cases of COVID-19 ranged from 0 to 60% and daily maximum temperature between 12.2 °C and 22.8 °C (Supplementary Fig. 2). An average increase of 1 °C of maximum temperature decreased the incidence rate by −7.5% (95%CI = [−12.3; −2.6]) on the same day (lag 0) (Fig. 1 ). Afterward, the temperature effect almost disappears, being substantially reduced from lag 1 to lag 6. We evaluated the linearity of the associations without observing evidence of departure from linearity (Supplementary Fig. 3).
Fig. 1.
Risk increase of daily incidence rate of positively diagnosed cases of COVID-19 for a rise of 1 °C of maximum temperature from lag 0 to lag 6.
Temperature is an essential factor in people's living environment, which can play a significant role in public health in terms of epidemic development and control (McMichael et al., 2008). There is a specific temperature that best fits the benefit of the virus and that lower temperatures contribute to the transmission because it is when the vulnerability increases. Thus, the arrival of summer could reduce the transmission of the COVID-19. Our result agreed with those already reported in other geographical locations, showing how the number of diagnosed cases increase below a maximum temperature of 10 °C and linearly decreasing afterward (Triplett, 2020; Wang et al., 2020b). However, these are cross-sectional studies at the country scale, which might have some measurement error due to high spatial variability when estimating a fixed temperature exposure for large geographic areas (Soares et al., 2012). Our study considers a smaller area, mainly defined by Barcelona's metropolitan area, where the daily variability of maximum temperature can be estimated more accurately. However, we have not been able to account for socioeconomic status or other meteorological factors, such as ultraviolet radiation or absolute humidity. While daily mortality could be a more robust indicator of the virus behavior, because it is not affected by the number of people tested, mortality may have different incident lag, from days to weeks from the diagnostic. We used instead of the daily incidence rate of positively diagnosed cases of COVID-19 confirmed from PCR tests.
Although we adjusted for time-trends and accounted for residual autocorrelation, typical for infectious diseases (Imai et al., 2015), we are concerned that our finding could still be a spurious relationship due to the small number of days considered in our analysis. Our result has to be further explored; however, it could provide a first clue to understanding the temperature-transmission relation of COVID-19 since it shares genetic similarities with SARS (Benvenuto et al., 2020).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments:
To Joe Brew for providing Online Appendix Fig. 1.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.109553.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- AQuAs Registre de test de COVID-19 realitzats a Catalunya. Segregació per sexe i àrea bàsica de salut (ABS). Dades Obertes Catalunya. Generalitat de Catalunya. 2020. https://analisi.transparenciacatalunya.cat/Salut/Registre-de-test-de-COVID-19-realitzats-a-Cataluny/xuwf-dxjd Available from:
- Benvenuto D. The 2019-new coronavirus epidemic: evidence for virus evolution. J. Med. Virol. 2020;92:455–459. doi: 10.1002/jmv.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumback B.A. Transitional regression models, with application to environmental time series. J. Am. Stat. Assoc. 2000;95 [Google Scholar]
- Gasparrini A. Distributed lag non-linear models. Stat. Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmes J.H. Virus survival as a seasonal factor in influenza and poliomylitis. Antonie Leeuwenhoek. 1962;28:221–233. doi: 10.1007/BF02538737. [DOI] [PubMed] [Google Scholar]
- Imai C. Time series regression model for infectious disease and weather. Environ. Res. 2015;142:319–327. doi: 10.1016/j.envres.2015.06.040. [DOI] [PubMed] [Google Scholar]
- Lauer S.A. The Incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael A.J. International study of temperature, heat and urban mortality: the 'ISOTHURM' project. Int. J. Epidemiol. 2008;37:1121–1131. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- Our World in Data Coronavirus disease (COVID-19) – statistics and research. 2020. https://ourworldindata.org/coronavirus/ Oxford Martin School, The University of Oxford, Global Change Data Lab. Available from:
- Soares P.M.M. WRF high resolution dynamical downscaling of ERA-Interim for Portugal. Clim. Dynam. 2012;39:2497–2522. [Google Scholar]
- Tan J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59:186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triplett M. Evidence that higher temperatures are associated with lower incidence of COVID-19 in pandemic state, cumulative cases reported up to March 27. 2020. medRxiv preprint. [DOI]
- Wang J. High temperature and high humidity reduce the transmission of COVID-19. SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3551767. [DOI] [Google Scholar]
- Wang M. Temperature significantly change COVID-19 transmission in 429 cities. 2020. medRxiv preprint. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.