Dear Editor,
The Coronavirus Disease 2019 (COVID-19) appeared in December 2019 in China and has infected more than 100,000 patients in China since then. After MDT (multi-disciplinary team treatment), more than 60,000 patients were cured and discharged from the isolation wards of designated hospitals. All of the discharged patients were negative as assayed by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) tests.
Based on Chinese government guidelines, these discharge patients needed to remain in isolation in the home for 2 weeks followed by additional follow-up nucleic acid testing and chest CT examination. However, some discharged patients have retested positive using nucleic acid tests. Reports of these scattered cases have drawn huge scrutiny. Unfortunately, there are some relevant issues needing resolution. First, the capacity for transmission between persons with these patients after positive diagnosis still needs to be determined. Second, the features of serial chest CT scans need to be analyzed to improve our awareness of these cases. Finally, the reason causing these positive retest results should be discussed.
We report here the serial CT examination features of two cluster transmission cases with positive follow-up nucleic acid test results after discharge.
1. Case report
1.1. Clinical evaluation and method
The two COVID-19 cases confirmed by the Jiangsu Province Center of Disease Control and Prevention (CDC) received antiviral treatment in the isolation ward of this institution between January 25 and February 9 (Fig. 1 ). According to the fifth and sixth edition guidelines on COVID-19 issued by the National Health Commission of the People's Republic of China [1,2], two consecutive negative RT-PCR test results in an interval at least one day apart is the standard necessary for discharge. These two patients met all of the discharge criteria and were given discharge permission by the MDT.
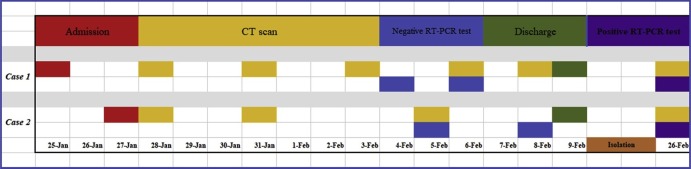
Fig. 1.
Timeline of the cases from admission to positive RT-PCR test after discharge. Isolation: isolation in home from Feb 10, 2020 to Feb 25, 2020 after discharge.
All of the relevant clinical history and laboratory results were retrieved from the electronic medical record system, and the details are presented in Table 1 .
Table 1.
Clinical and laboratory manifestation of the two cases with positive RT-PCR test after discharge.
| Clinical and laboratory manifestation | Case 1 | Case 2 |
|---|---|---|
| Sex | Male | Female |
| Age (years) | 56 | 21 |
| Body Temperature (°C)* | 39.5 | 38.2 |
| Cough and/or sputum | + | + |
| Fatigue | + | – |
| Interval between admission and CT scan (days) | 3 | 1 |
| Interval between admission and nucleic acid negativity (days) | 9 | 8 |
| White blood cell count (109/L) (normal range: 4.00–10.00) | 3.3 | 11.3 |
| Neutrophil count (109/L) (normal range: 2.00–7.00) | 1.98 | 8.27 |
| Lymphocyte count (109/L) (normal range: 0.80–4.00) | 1.0 | 2.4 |
| Eosinophil count (109/L) (normal range: 0.02–0.50) | 0.00 | 0.04 |
| CRP (normal range: 0–10 mg/L) | 42.2 | 6.8 |
| LDH (normal range: 109–245U/L) | 334 | 220 |
Note: CRP, C-reactive protein; LDH, Lactate dehydrogenase;* means the highest temperature before inpatient; + mean the positive symptoms; − mean no fatigue.
The axial, sagittal, and coronal thin slice (1.5 mm) reconstruction images from the lung (window width, 1500 HU; window level, −400 HU) and a mediastinal window (window width, 400 HU; window level, 40 HU) were used for evaluation, respectively. All of the imaging were analyzed, and a consensus was reached by two senior radiologists (K.X. and Y.K.M.) with more than 30 and 20 years of experience in interpreting chest CT imaging, respectively, who did not know detailed clinical, laboratory, epidemic or outcome information. The following image features were recorded: number, area, and density of lesion. The density and area of the largest lesion in each CT examination were also measured. For nodular lesions, the number of all lesions was also counted (Case 2) (Fig. 2, Fig. 4 ).
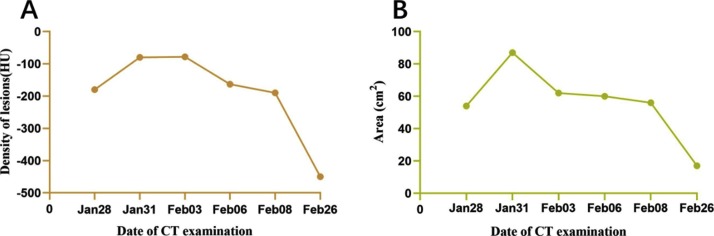
Fig. 2.
Density and area of lesions in Case 1 serial CT examinations. A: the curve of lesion density in different CT examinations. B: the curve of lesion area in serial CT examinations.
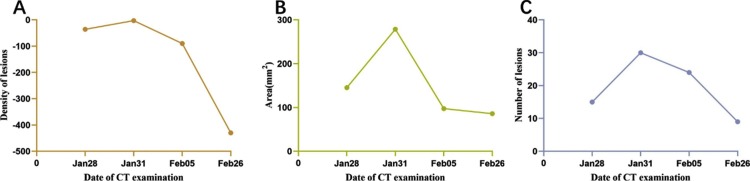
Fig. 4.
Curves of lesion density and number from Case 2 from a series of CT examinations. A: curve of lesion density. B: curve of lesion area. C: curve of lesion number.
1.1.1. Case 1
A 56-year-old male patient, who travelled from Guangzhou City, Guangdong Province to Xuzhou City, Jiangsu Province by train on January 14, 2020 and stayed for 6 h at Wuhan, Hubei Province Hankou Station, was the first confirmed COVID-19 case in our institution. The patient developed fever, fatigue, and cough on January 19, with the highest temperature reaching 39.5 °C, and was hospitalized in the isolation ward of our institution after 6 days (Jan 25).
Laboratory results showed decreased counts of white blood cells, neutrophils, lymphocytes, and eosinophils, and increased C-reactive protein (CRP) and lactate dehydrogenase (LDH) values (Table 1). After 9 days of treatment in the isolation ward and two consecutive negative nucleic acid tests, the patient was discharged. After isolation in his home for 17 days, the man performed throat and anus swab nucleic acid test, with positive results (Fig. 1).
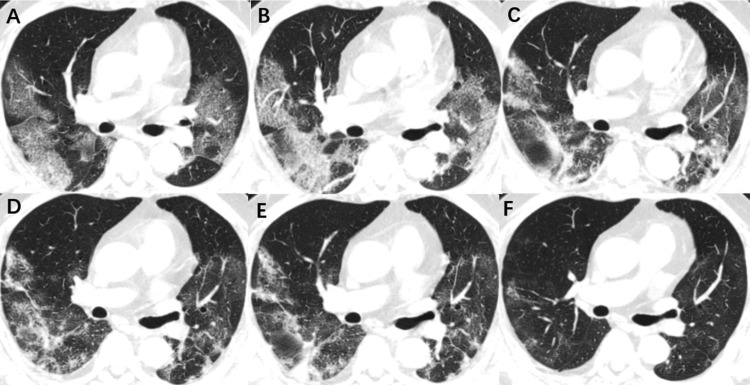
The patient received six CT scans throughout the course of the disease. We report here his series of chest CT curves. The initial CT after hospitalization (Jan 28, 2020) showed multi-focal patchy ground glass opacity (GGO) with a little fibrous tissue in both the lungs, involving all of the pulmonary lobes. The curve of density showed its highest value in the second examination, and then decreased in the first follow-up examination after discharge. The area of lesion also reached a peak value in the second imaging and then decreased. Compared with the admission CT examination, the density and area of lesion showed significant decrease in the first follow-up examination after discharge (Fig. 2, Fig. 3 ).
Fig. 3.
Axial chest CT images the Case 1. A: initial CT after admission isolation ward (Jan 28, 2020); B: second CT after admission to the isolation ward (Jan 31, 2020); C: third CT of hospitalization (Feb 03, 2020); D: fourth CT of hospitalization (Feb 06, 2020); E: final CT of hospitalization (Feb 08, 2020); and F: CT manifestation of significant absorbment of lesions after discharge (Feb 26, 2020).
1.1.2. Case 2
The 21-year-old female patient (Case 2) is the daughter of Case 1, who had close contact with her father with fever (the highest temperature: 38.2 °C) and a dry cough on January 24, 2020. The patient was also confirmed to be positive for COVID-19 and was admitted into our hospital on January 27. Laboratory results showed increased leukocyte and neutrophil counts and CRP values (Table 1). After two consecutive negative nucleic acid tests (interval one day), she was discharged to home isolation for two weeks. Seventeen days later, Case 2’s nucleic acid test results were determined to be positive by the Jiangsu Province CDC (Fig. 1).
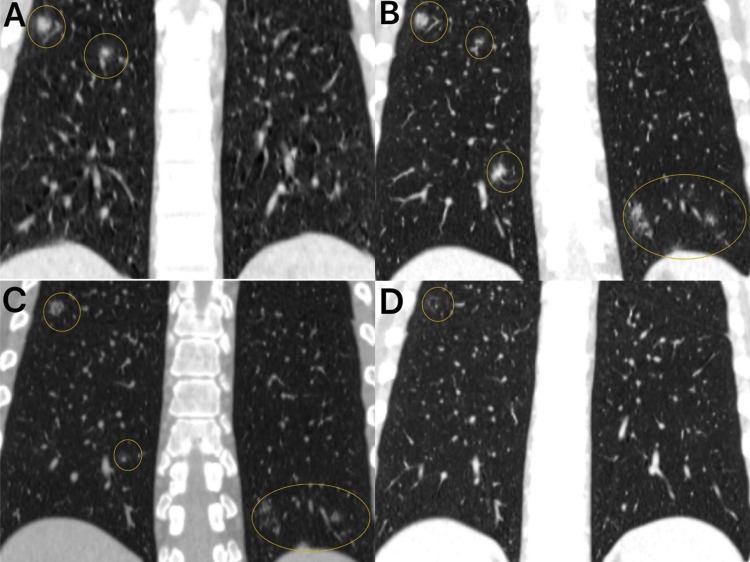
The patient received four CT scans throughout the course of the disease. The first CT scan (Jan 28, 2020) showed multiple nodular GGO in all pulmonary lobes. The curves of density, area and number showed their highest value at the second examination, and then decreased to different extents. Compared with the last CT examination from admission, the density and number showed significant decreases after the first follow-up CT post discharge (Fig. 4, Fig. 5 ). This area showed no significant change in two different examinations.
Fig. 5.
Coronal chest CT images of Case 2. A: first CT image after to the admission isolation ward (Jan 28, 2020); B: final CT during admission (Jan 31, 2020); C: CT upon release (Feb 5, 2020); and D: first follow-up CT after discharge with RT-PCR test positivity (Feb 26, 2020).
2. Discussion
Only scattered follow-up patients showed throat and anus swab nucleic acid positivity. As a community, we should pay attention to this fact. We did not know whether these cases had the capacity for promoting infection and whether these cases needed continued anti-viral treatment. We have two speculations for these positive retest results: (1) false negative rates of nucleic acid tests; (2) re-infection after discharge. For the two cases we reported, chest CT scan of the first follow-up after discharge showed significant changes compared to the last imaging during admission. Furthermore, these two cases performed strictly quarantine in home for more than two weeks after discharge. There was no evidence of re-infection and person-to-person transmission during this time.
Two consecutive negative nucleic acid tests over a one-day interval was the most important criteria for discharge from the isolation ward. We report here that these two cases met the criteria of the sixth guidelines of the national health commission. The false negative rate of this nucleic acid test has been previously documented [3,4]. Some patients manifested typical chest CT imaging of COVID-19, without positive nucleic acid results [4]. The experience of the diagnosing physician, the biopsy location, and the specific test kit used may impact the sensitivity of this test.
The serial CT images showed that there were still significant lesions that were not absorbed, especially in Case 1. The 7th edition of the guidelines revised and further emphasized the importance of CT examination in discharge criteria [5]. The acute bilateral pulmonary exudative lesions significantly diminishing was included in the new revision. We considered that this more strict criterium might compensate for the false negative rate of the nucleic acid test to some extent. Furthermore, the serial CT features may help evaluate the changes in lesions and offer more valuable clinical information. The density, however, was more likely to show changes in lesions rather than the number or area. By observing serial CT images, patients without significant decreases in lesions need additional time before repeated nucleic acid tests to diminish the false negative rate.
Thus, discharged isolation COVID-19 patients need strict follow-up with both nucleic acid testing and CT examination to reduce the insidious risk of persistent infection.
Declaration of Competing Interest
No potential conflicts of interest were disclosed.
Acknowledgments
We acknowledge all of our colleagues for their selfless help with this study. We also wish to pay tribute to all the medical personnel working on the frontline of the epidemic outbreak regardless of the risk to their lives.
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Contributor Information
Yankai Meng, Email: mengyankai@126.com.
Kai Xu, Email: xkpaper@163.com.
References
- 1.China National Health Commission . China National Health Commission; Beijing: 2020. Diagnosis and Treatment of Pneumonitis Caused by New Coronavirus (trial Version 5) [Google Scholar]
- 2.China National Health Commission . China National Health Commission; Beijing: 2020. Diagnosis and Treatment of Pneumonitis Caused by New Coronavirus (trial Version 6) [Google Scholar]
- 3.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020:2783. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie X., Zhong Z., Zhao W. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.China National Health Commission . China National Health Commission; Beijing: 2020. Diagnosis and Treatment of Pneumonitis Caused by New Coronavirus (trial Version 7) [Google Scholar]