Highlights
-
•
In this statement, the pathology, clinical diagnosis, and typical imaging characteristics of COVID-19 pneumonia are reviewed.
-
•
Chest CT plays an important role in diagnosis, in compliment with the RT-PCR test.
-
•
COVID-19 pneumonia has different imaging features in different stages.
Abbreviations: COVID-19, coronavirus disease 2019; GGO, ground glass opacity; RT-PCR, reverse transcription-polymerase chain reaction; CT, computed tomography
Keywords: COVID-19 pneumonia, Imaging features, Computed tomography
Abstract
Coronavirus disease 2019 (COVID-19) is highly contagious, mainly causing inflammatory lesions in the lungs, and can also cause damage to the intestine and liver. The rapid spread of the virus that causes coronavirus disease 2019 (COVID-19) pneumonia has posed complex challenges to global public health. Early detection, isolation, diagnosis, and treatment are the most effective means of prevention and control. At present, the epidemic situation of new coronavirus infection has tended to be controlled in China, and it is still in a period of rapid rise in much of the world. The current gold standard for the diagnosis of COVID-19 is the detection of coronavirus nucleic acids, but imaging has an important role in the detection of lung lesions, stratification, evaluation of treatment strategies, and differentiation of mixed infections. This Chinese expert consensus statement summarizes the imaging features of COVID-19 pneumonia and may help radiologists across the world to understand this disease better.
1. Introduction
A series of cases of pneumonia of unknown cause was reported in Wuhan, in late December 2019 [1]. Epidemiological data demonstrated person-to-person spread is the main mode of transmission, which resulted in a worldwide outbreak [2,3]. World Health Organization (WHO) designated COVID-19 as the official name [4,5]. The pathogen was confirmed to be severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a betacoronavirus [5]. Standard technique to confirm COVID-19 is nucleic acid testing with reverse transcription polymerase chain reaction (RT-PCR) and/or next-gen sequencing (NGS) methods [6,7]. Imaging features differ in different individuals and stages of the COVID-19 pneumonia, and they are also different from other infectious pulmonary diseases [8]. In order to improve the diagnosis and treatment, we first drew up the “Guideline for medical imaging in auxiliary diagnosis of coronavirus disease 2019”and participant in “Radiological diagnosis of new coronavirus infected pneumonitis: Expert recommendation from the Chinese Society of Radiology (First edition)” [9,10].Based on these previous advices, this current overview and consensus statement is meant to inform radiologists in the rest of the world based on the Chinese experience.
2. Pathological changes
In post-mortem cases, the lungs show consolidation in different degrees. Serum, fibrinous exudate, and transparent membrane formation are seen in the alveolar cavity; exudation cells are mainly monocytes and macrophages, and multinucleated giant cells are easily seen. Type 2 alveolar epithelial cells proliferated significantly, and some of the cells shed. Inclusion bodies can be seen in type 2 alveolar epithelial cells and macrophages. Alveolar septal vascular congestion and edema, monocyte and lymphocyte infiltration, and intravascular thrombosis can be seen. Focal hemorrhage and necrosis of lung tissue may occur with hemorrhagic infarction. Intra-alveolar fibrosis, resulting from organization of inflammatory exudates also can be found. The epithelium of the bronchial mucosa in lungs discards, and there is formation of mucus and mucus plugs in the cavity. Coronavirus particles can be seen in the bronchial mucosal epithelium and type 2 alveolar epithelial cells under an electron microscope [11,12].
3. Clinical features
The incubation period is 1∼14 days, mostly 3–7 days, based on the current epidemiological evidence [13]. Fatigue, and dry cough are the most common clinical onset symptoms. Nasal congestion, sore throat, and diarrhea are atypical clinical presentations [13]. Patients with mild or moderate type only demonstrate a low fever and mild fatigue without pneumonia in the early stage of the disease [13,14]. Most patients have a good prognosis, with few patients becoming critically ill. Prognosis is poor for the elderly and those with chronic underlying diseases, and the symptoms of children tend to be relatively mild [15,16]. Some critically patients may have elevation of troponin level, and an increase of C-reactive protein can be seen. Critically ill patients may develop acute respiratory distress syndrome, septic shock with metabolic acidosis and coagulation dysfunction that are difficult to correct [16,17]. For the clinical criteria, the first step is to ascertain the epidemiology history of suspected cases. Confirmed cases must be tested positive by RT-CPR assay or by NGS [18]. SARS-CoV-2 nucleic acids can be detected in nasopharyngeal swabs, sputum, or other lower respiratory tract secretions, blood, and stools [19].
4. There are four clinical types according to Chinese guideline on COVID-19 pneumonia [14]
Mild Type: Clinical symptoms are mild and no signs of pneumonia are seen on imaging.
Common Type: Fever, respiratory infections, and other symptoms; pneumonia can be seen on imaging.
Severe Type: Any of the following conditions:
-
1
Respiratory distress, RR ≥ 30 times/min
-
2
Resting-state oxygen saturation ≤93 %
-
3
Arterial oxygen partial pressure (PaO2)/oxygen concentration (FiO2) ≤ 300mmHg
Critical Type: Any of the following conditions:
-
1
Respiratory failure occurs and requires mechanical ventilation
-
2
Patient suffers from shock
-
3
Combined with other organ failure requiring ICU monitoring and treatment
5. Preparedness for the radiology department in the prevention and control of COVID-19
In Western countries, CT is not considered a screening examination for COVID-19 [[20], [21], [22]]. Due to various factors such as specimen collection technology, kit quality, and the diversity of disease evolution, the false-negative rate of nucleic acid detection is relatively high in China. In the situation of suspected crowds and limited medical resources, nucleic acid test negative but CT positive (highly suggestive of viral pneumonia) are also listed as medical isolation treatment criteria in China, which is more in line with the actual situation in Wuhan [18,9]. Thus, infection prevention and control is a new task and a serious challenge facing the radiology department in China. All members must fully understand the epidemic situation and fully grasp the knowledge of infection control. The work process and working mode must be changed in accordance with the requirements. The radiology department should prepare the requirements of COVID-19 imaging examination workflows, including but not limited to: (1) set up a special waiting area and examination room for COVID-19 patients; (2) require all radiologists, technologists, and nurses to master skills of prevention of COVID-19 infection; (3) formulate emergency CT examination specifications, procedures and disinfection measures for patients with suspected COVID-19; (4) require self-protection measures for all radiologists, technologists, and nurses; (7) regulate disposal of waste protective equipment. It should be emphasized that in order to prevent cross-infection, hospitals should clearly divide the polluted area, semi-polluted area, and clean area according to the requirements of nosocomial infection control, and set up independent inspection areas.
6. Recommendations for chest imaging techniques
Imaging, in particular chest X-ray and computed tomography (CT), is important in the detection of lung lesions, assessment of lesion size, density, and evolution. Chest X-ray examination is convenient and fast, and has been proven effective in diagnosing other coronaviruses, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [[23], [24], [25], [26]]. However, the sensitivity and specificity for mild type patients are relatively low [27]. It is not recommended for patients with early COVID-19 stage. Chest CT scans can demonstrate almost all abnormalities including early mild exudative lesions. Chest CT is the most valuable imaging tool for the clinical diagnosis of early stage COVID-19 pneumonia when patients’ symptoms are aspecific, especially in Wuhan with insufficient PCR tests in the early pandemic period [28,29]. It is recommended to use volume CT with a maximum acquisition slice thickness of 5 mm (≥16 slice multi-detector CT) and a reconstruction slice thickness of 1.0–1.5 mm [30]. Multi-planar reformats (transverse, sagittal, and coronal planes) are beneficial for the early detection of lesions in patients with negative nucleic acid tests [9].
7. Typical features on chest X-Ray
Multiple small patchy shadows and interstitial changes in the lower zone of lungs are typical imaging features in common type patients [9]. With the progression of the disease, it may manifest as a patchy distribution or multiple consolidations [13,27,31]. In severe and critical type COVID-19 pneumonia, multifocal or diffuse consolidation can be seen in both lungs, showing as "white lung" [16]. Chest X-ray is only suitable for primary hospitals without examination conditions and follow-up of critically ill patients.
8. Typical features on chest CT
Typical features on chest CT include ground-glass opacity with a cloud-like change on chest CT, not obscuring the accompanying pulmonary vascular structures in lungs [32,33]. Corresponding pathological changes are exudation in the alveolar cavity with partial filling of the air cavity, mainly from serous and fibrinous exudates, alveolar septal vascular congestion and edema. Disease progression mostly occurs in a course of 7–10 days, with enlarged and increased density of GGO, and consolidated lesions with air bronchogram sign [9,34,35]. GGOs from the early stage expand, and the density increases gradually. Consolidation shows increased lung parenchymal density, and blurred borders of the pulmonary blood vessels and airway walls due to the loss of air contrast. The lesion range can be acinar, leaflet, lung segment or lung lobe. Lesions are distributed as bilateral asymmetrical subpleural wedge-shaped or fan-shaped, mostly in the caudal regions of the lung and dorsal subpleural area [36]. When interlobular septa and intralobular interstitium are thickened, this is displayed as subpleural reticulation according to a "crazy paving" pattern [[38], [39], [40]]. The underlying pathological changes are pulmonary edema, protein exudation, thickening of intralobular interstitial, and multinucleated giant cells and macrophage infiltration in the alveolar cavity [37]. Critical stage disease may show further expansion of consolidations, with the whole lung showing increased opacity, a so-called "white lung" [9,35]. In recovery stage patients, the lesion area is reduced and absorbed, or only residual fibrous lesions are seen [38]. Less common findings include pleural effusion, stretch bronchiectasis, and thoracic lymphadenopathy (Imaging examples are shown in Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5 ).
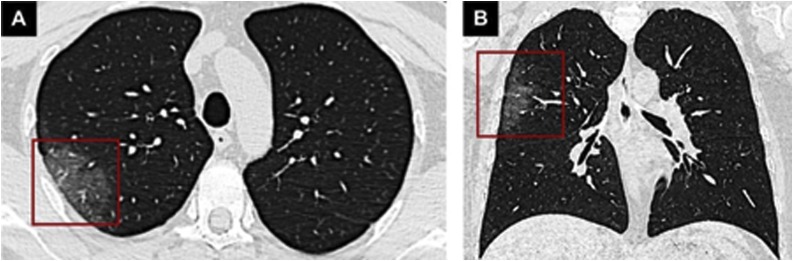
Fig. 1.
CT findings of early-stage COVID-19. A 36-year-old male with a history of close contact with comfirmed cases. Fever had been present for six days. Chest CT shows a unilateral pure GGO lesion (red rectangles) in the posterior segment of the right upper lobe on axial (A) and coronal view (B).
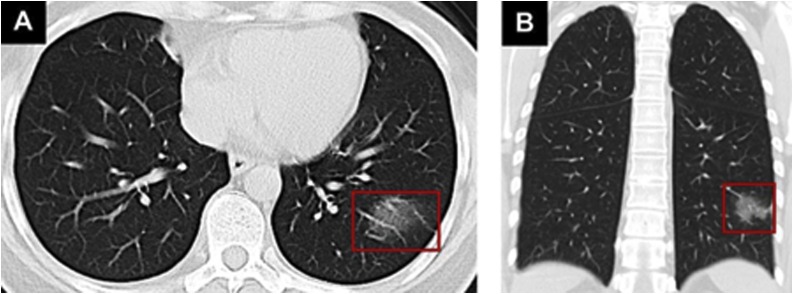
Fig. 2.
CT findings of early-stage COVID-19. A 43-year-old male with a history of travel to Wuhan presented with fever for 6 days. Axial (A) and coronal view (B) of chest CT shows a peripheral, unilateral GGO lesion in the posterobasal segment of the left lower lobe (red rectangles).
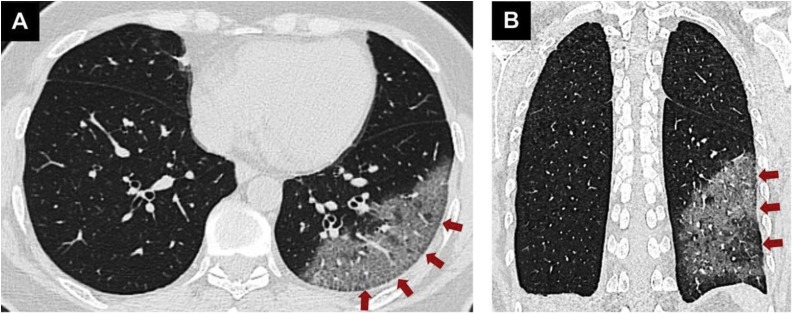
Fig. 3.
CT findings of COVID-19 in progressive stage. Diffuse GGO lesions associated with smooth interlobular and intralobular septal thickening (red arrows) are seen in the posterobasal segment of the left lower lobe in both axial (A) and coronal planes (B).
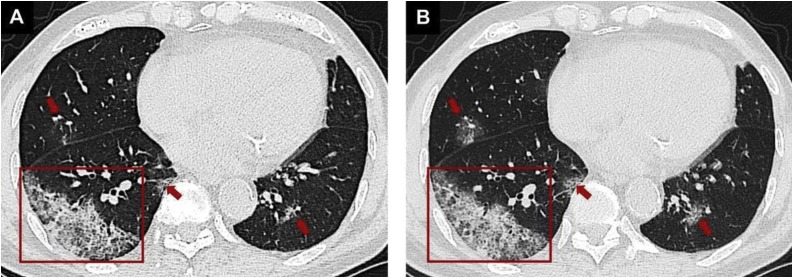
Fig. 4.
CT findings of COVID-19 in progressive stage. A 78-year-old male with a history of contact with COVID-19 patients. A crazy-paving pattern (A, red rectangle) across the subpleural area of the posterolateral segment of right lower lobe and multiple ill-defined GGOs (A, red arrows) in bilateral lungs can be seen. Repeat CT performed 4 days after admission shows that most of the lesions had improved (B, red rectangle and arrows) with an increased intensity inbothlungs.
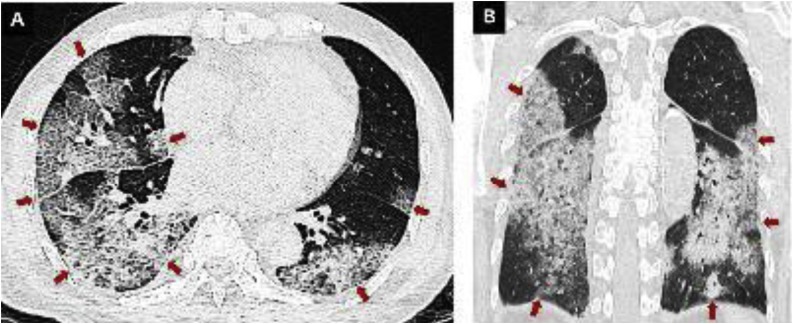
Fig. 5.
CT findings in critically ill COVID-19 patient. A 35-year-old male with severe COVID-19. The axial (A) and coronal view (B) of unenhanced chest CT images show diffuse GGO with multiple consolidations in both lungs, giving the white lung appearance as indicated by red arrows.
9. Dynamic changes on chest CT
Chest CT can also evaluate the time course of COVID-19 and assess the evolution of disease severity. Chung et al. [34] evaluated each of the five lung lobes and determined the degree of involvement and rated the severity of each lobe. The patients who had the highest score (of 19) were admitted to the intensive care unit with multiple bilateral GGOs and subsegmental consolidation. Pan et al. [28] investigated the time course of lung changes during recovery from COVID-19 pneumonia. The results showed that with the evolution of the disease, GGO would enlarge with a crazy paving pattern and partial consolidation. Lung involvement reached a maximum at about the 10th day after the onset, and the crazy-paving pattern was resolved entirely in the absorption stage about the 14th day after the disease onset, which means that the crazy-paving pattern may become an important indicator for evaluation of disease evolution. Other studies focusing on the evolution of COVID-19 pneumonia concluded that the lung segments showed marked changes with decreasing of GGOs and increasing of crazy-paving pattern and consolidation [9,[39], [40], [41], [42]]. Patients recovering from COVID-19 can be tracked with CT to assess for long-term or permanent lung damage, including fibrosis. (Imaging examples are shown in Fig. 6, Fig. 7 ).
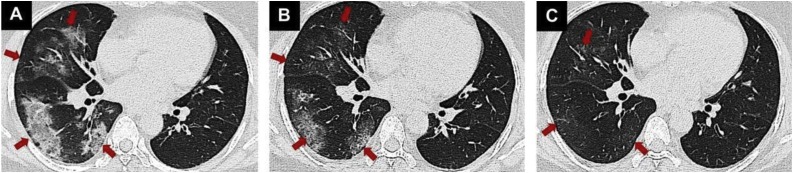
Fig. 6.
Temporal lung changes of a 56-year-old female with COVID-19. After three days of fever, lung findings on coronal non-contrast chest CT were multiple consolidations and patchy GGOs located in the subpleural area in the middle and lower lobes of the right lung (A, red arrows). Follow-up chest CT images obtained after one (B) and two (C) weeks show absorption of lesions (red arrows) with a gradual decrease in extent and density.
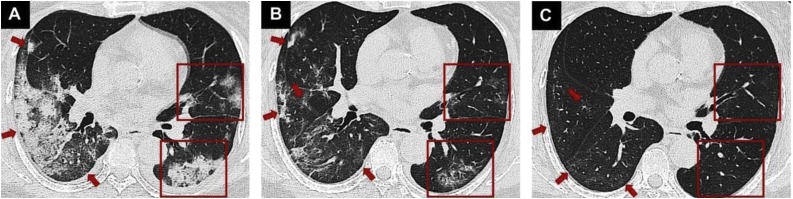
Fig. 7.
CT findings during the absorption period of COVID-19. A 68-year-old female presented with fever for six days. Lung findings on chest CT were patchy GGO and mass consolidation in both lungs (A, red rectangles and arrows). Lung lesions gradually absorbed on the CT five days later (B, red rectangles and arrows). After ten days, a few ill-defined GGOs remained in both lungs (C, red rectangles and arrows).
10. Differential diagnosis with other pneumonia
Although the imaging features of COVID-19 overlap with those of SARS and MERS, there are differences on imaging exams that set the COVID-19 pneumonia apart. It is essential to make a differential diagnosis for early identification of borderline patients and determination of the appropriate treatment. Viral pneumonia is characterized by alveolar wall edema and interstitial changes [43]. Streptococcus pneumonia is characterized by the consolidation of lobes or lobules without GGO [44]. Both mycoplasma and aspiration pneumonia distribute along the bronchovascular bundle [[45], [46], [47]], which is significantly different from COVID-19 pneumonia. In a study comparing chest CT from 219 patients with COVID-19 pneumonia in China and 205 patients with other causes of viral pneumonia in the United States, COVID-19 pneumonia cases were more likely to have a peripheral distribution (80 versus 57 percent), and GGO (91 versus 68 percent) [8]. COVID-19 patients more frequently had multifocal involvement on CT, compared with unifocal involvement in SARS and MERS [24,26,48]. Table 1 shows the differential diagnosis between COVID-19 pneumonia and other respiratory disease.
Table 1.
Differential Diagnosis between COVID-19 pneumonia and other Respiratory Disease.
| Diseases | CT findings |
|---|---|
| Influenza A virus pneumonia | Bilateral diffuse GGO, confluent rapidly |
| Thickened bronchovascular bundle | |
| With or without consilidation | |
| Distributed along with the bronchial vascular bundle or subpleural region | |
| Streptococcus pneumoniae | Consolidation of lobes or lobules without GGO |
| Mycoplasma pneumonia | Bronchial wall Thickening |
| Patchy shadows along the bronchovascular bundle | |
| Accompany with CT signs like tree-in-budThe tree-in-bud sign | |
| Aspiration pneumonia | Bronchiectasis |
| Multifocal GGO | |
| GGO change quickly and be absorbed in a short time | |
| SARS | Unilateral or bilateral GGO, partially consolidate |
| Inter and intra lobular septal thickening and crazy-paving sign could be found | |
| Bilateral, basliar subpleural airspace | |
| MERS | Diffuse GGO |
| Lobular septal thickening and pleural effusions are atypical | |
| COVID-19 | Multifocal GGO associated with air bronchogram and/or crazy-paving pattern |
| The lesions can be segmental or lobular distribution, partially confluent | |
| Located in Subpleural | |
| Wedge-shaped or fanlike | |
| perpendicular to the bronchovascular bundle |
11. Application of artificial intelligence (AI) in COVID-19
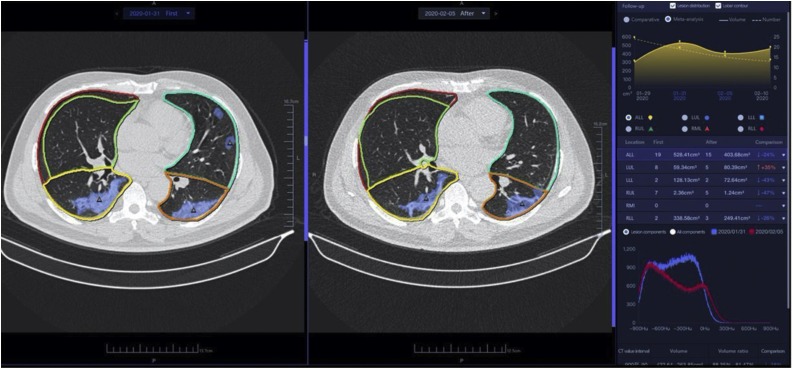
A large amount of CT images makes it difficult for radiologists to compare among serial studies. Thus, rapid detection, accurate location of lesions, and evaluation of lesion size, properties, and lesion dynamics are urgent issues that need to be addressed. An AI-assisted diagnostic system for COVID-19 has been developed in China. It takes about 15 s with an accuracy rate above 90 % [49]. The AI-system has outstanding performance in the detection of subtle GGO, which is the most easily missed typical CT feature of COVID-19. Also, it can precisely segment the lesion region, calculate the lesion volume, volume rates of lesions to total/left/right lung, and each lung lobe. Comparing CT scans of the same patient at several time points, the radiologist can use the system to measure changes in each lesion and track the progression of the disease (Fig. 8 ). Some researchers have tried to apply AI in CT image analysis to differentiate COVID-19 from other viral pneumonia patients [50]. With clinical symptoms, laboratory testing results, and contact or travel history, the AI system can help doctors identify patients with risk of progressing to a more severe disease state at the time of admission, for timely, precise, and effective treatment decisions. Hence, precise lesion labeling, segmentation, and quantification analysis of COVID-19 lesions is the future of AI.
Fig. 8.
The web client of an AI assisted COVID-19 diagnosis system. The lesion contours are labeled on the axial images of chest CT. In the follow-up module, the previous CT and subsequent CT images are on the left and right sides, along with a quantitative comparative analysis of the two CT lesions on the right information bar.
12. Conclusion
In general, combined chest CT, clinical symptoms, and laboratory tests facilitates the diagnosis of COVID-19. Increasing in-depth understanding of the disease, research, and the continuous improvement of AI technology will further promote the establishment of a comprehensive prevention and control system of early screening, diagnosis, isolation, and treatment of COVID-19 pneumonia.
Funding
This work was supported by National Science Foundation of China (No. 62041601, No.61936013, No.81771806, No.81930049). National Science and Technology Planning Project (2020ZX10001013).
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to thank the consensus statement committee, the members and their institutions are as follows
Consensus Statement Committee
Jianping Dai (Beijing Tiantan Hospital, Capital Medical University), Qiyong Guo (Shengjing Hospital of China Medical University), Ke Xu (The First Hospital of China Medical University), Zhengyu Jin (Peking Union Medical College Hospital), Kuncheng Li (Xuanwu Hospital Capital Medical University), Zhenchang Wang(Beijing Friendship Hospital, Capital Medical University), Min Chen (Beijing Hospital), Nan Hong (Peking University People’s Hospital), Hong Yu (Shanghai Chest Hospital, Shanghai Jiaotong University), Yali Wang (Hebei Yiling Hospital), Xuntao Yin (GuiZhou Provincial People’s Hospital), Jie Lu (Xuanwu Hospital Capital Medical University), Yibo Lu (The Forth Hospital Of Nanning), Jie Bian (The Second Hospital of Dalian Medical University), Guanxun Cheng (Peking University Shenzhen Hospital), Jinrong Qu (Henan Cancer Hospital), Yubo Lv (Jiahui International Hospital), Wenzhen Zhu (Zhongnan Hospital Of Wuhan University), Xiangyu Zhu (Shandong Medical Imaging Research Institute), Zhongwei Qiao (Children’s Hospital of Fudan University), Guoqing Qiao (DeZhou People’s Hospital), Qiang Liu (Shandong Medical Imaging Research Institute), Shiyuan Liu (Shanghai Changzheng Hospital), Wenya Liu (Xinjiang Medical University First Hospital), Yuanming Liu (Shenzhen Smart Imaging Healthcare Co.,Ltd / Texas State University), Jingzhe Liu (The First Hospitalo of Tsinghua University), Xinjiang Liu (Shanghai Pudong Hospital Fudan University Pudong Medical Center), Chuanjun Xu (The Second Hospital Of Nanjing), Jianrong Xu (Rnji Hospital, Shanghai Jiaotong University School of Medicine), Jiansong Ji (Lishui Hospital of Zhejiang University College (Lishui Center Hospital), Qun Lao (Hangzhou Children’s Hospital), Li Li (Beijing YouAn Hospital, Capital Medical University), Ping Li (The Second Affiliated Hospital Of Harbin Medical University), Xiaohu Li (The First Affiliated Hospital of Anhui Medical University), Hongjun Li (Beijing YouAn Hospital, Capital Medical University), Tongzeng Li (Beijing YouAn Hospital, Capital Medical University), Yonggang Li (The First Affiliated Hospital of Soochow University), Dechun Li (Xuzhou Central Hospital), Qi Yang (Beijing Chao-Yang Hospital, Capital Medical University), Yuxin Yang (Xinjiang Uygur Autonomous Region sixth people's hospital), Gaofeng Shi (The Fourth Hospital of Hebei Medical University, Hebei Cancer Hospital), Yuling He (The First Affiliated Hospital Of Nanchang University), Liya Wang (People’s Hospital Of Longhua, Shenzhen), Wei Song (Peking Union Medical College Hospital), Shuguang Chu (Shanghai East Hospital, Tongji University), Tong Zhang (The Fourth Affiliated Hospital Of Harbin Medical University), Yan Zhang (Shandong Medical Imaging Research Institute), Yuzhong Zhang (People’s Hospital Of Longhua, Shenzhen), Lina Zhang (The First Hospital Of China Medical University), Jinsong Zhang (Air Force Medical University of PLA), Guowei Zhang (Yantaishan Hospital, Yantai, PRChina), Xiaochun, Zhang (Zhongnan Hospital of Wuhan University), Huijuan Zhang (The South Branch of Fujian Provincial Hospital), Yong Lu (Ruijin Hospital, Shanghai Jiaotong University School of Medicine), Puxuan Lu (The Shenzhen Center for Chronic Disease Control), Feng Chen (The First Affiliated Hospital, College Of Medicine, Zhejiang University), Tianwu Chen (Affiliated Hospital Of North Sichuan Medical College), Kemin Chen (Ruijin Hospital, Shanghai Jiaotong University School Of Medicine), Lingbo Lin (Jinan Infectious Disease Hospital), Jizheng Lin (The Affiliated Hospital Of Qingdao University), Lin Luo (The First Affiliated Hospital of Baotou Medical College, Inner Mongolia University of Science and Technology), Jiawen Luo (The Second Hospital of Dalian Medical University), Xianwen Yue (Weifang Respiratory Disease Hospital), Jun Zhou (People’s hospital of Xishuangbanna Dai autonomous prefecture(Affiliated Hospital of Kunming University of Science and Technology)), Jun Zhou (The People’s Hospital Of The Xishuangbanna Dai Nationality Autonomous Prefecture), Yan Zhou (Hospital of Chengdu office of People’s Government of Tibetan Autonomous Region (Hospital C.T.)), Fei Shan (Shanghai Public Health Clinical Center), Jiaojiao Liu (Beijing YouAn Hospital, Capital Medical University), Zhonghui Duan (Beijing YouAn Hospital, Capital Medical University), Dailun Hou (Beijing Chest Hospital, Capital Medical University), Yuxin Shi (Shanghai Public Health Clinical Center), Chuanwu Jiang (Qingdao Hospital of Traditional Chinese Medicine(Qingdao Hiser hospital)), Liming Xia (Tongji Hospital, Tongji Medical College of HUST), Qiuzhen Xu (Zhongda Hospital, Southeast University), Haibo Xu (Zhongnan Hospital of Wuhan University), Xiaoping Yin (Affiliated Hospital of Hebei University), Jianbo Gao (The First Affiliated Hospital of Zhengzhou University), Youmin Guo (First Affiliated Hospital of Xi’an Jiaotong University), Yi Xiao (Shanghai Changzheng Hospital), Lianggeng Gong (The Second Affiliated Hospital of Nanchang University), Guangbin Cui (Tangdu Hospital, The Forth Military Medical University), Lianchun Liang (Beijing YouAn Hospital, Capital Medical University), Yun Peng (Beijing Children’s Hospital, Capital Medical University), Jingliang Chengb (The First Affiliated Hospital of Zhengzhou University), Hong Lu (Chongqin The Seventh People’s Hospital), Zhiyan Lu (Zhongnan Hospital of Wuhan University), Xianqiang Zeng (Nanyang Central Hospital), Haiyan Lou (The First Affiliated Hospital, College Of Medicine, Zhejiang University), Meiyan Liao (Zhongnan Hospital Of Wuhan University).
References
- 1.WHO . 2020. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection Is Suspected.https://www.healthynewbornnetwork.org/resource/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-2019-ncovinfection-is-suspected [Google Scholar]
- 2.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., Seilmaier M., Drosten C., Vollmar P., Zwirglmaier K., Zange S., Wolfel R., Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Li M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T.K., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2005. Statement on the Second Meeting of the International Health Regulations.https://www.who.int/news-room/detail/30-01-2020-statement-onthe-second-meeting-of-the-international-health-regulations-(2005)-emergencycommittee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) [Google Scholar]
- 5.Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A., Haagmans B.L., Lauber C., Leontovich A.M., Neuman B.W., Penzar D., Perlman S., Poon L.L.M., Samborskiy D.V., Sidorov I.A., Sola I., Ziebuhr J. Coronaviridae Study Group of the International Committee on Taxonomy of, the species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020 doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K.W., Bleicker T., Brünink S., Schneider J., Schmidt M.L., Mulders D., Haagmans B.L., van der Veer B., van den Brink S., Wijsman L., Goderski G., Romette J.L., Ellis J., Zambon M., Peiris M., Goossens H., Reusken C., Koopmans M.P.G., Drosten C. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.Es.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reller L.B., Weinstein M.P., Murdoch D.R. Nucleic acid amplification tests for the diagnosis of pneumonia. Clin. Infect. Dis. 2003;36:1162–1170. doi: 10.1086/374559. [DOI] [PubMed] [Google Scholar]
- 8.Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L., Pan I., Shi L.-B., Wang D.-C., Mei J., Jiang X.-L., Zeng Q.-H., Egglin T.K., Hu P.-F., Agarwal S., Xie F., Li S., Healey T., Atalay M.K., Liao W.-H. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chinese Society of Radiology Radiological diagnosis of new coronavirus infected pneumonitis: expert recommendation from the Chinese Society of Radiology (First edition) Chin. J. Radiol. 2020;54:E001. doi: 10.3760/cma.j.issn.1005-1201.2020.0001. [DOI] [Google Scholar]
- 10.Radiology of Infection Sub-branch, Radiology Branch, Chinese Medical Association Guideline for medical imaging in auxiliary diagnosis of coronavirus disease 2019. Chin. J. Med. Imaging Technol. 2020;(36):321–331. doi: 10.13929/j.issn.1003-3289.2020.03.001. [DOI] [Google Scholar]
- 11.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.-S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020 doi: 10.1016/s2213-2600(20)30076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang T., Sun L.X., Feng R.E. Comparison of clinical and pathological features between severe acute respiratory syndrome and coronavirus disease 2019. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E040. doi: 10.3760/cma.j.cn112147-20200311-00312. [DOI] [PubMed] [Google Scholar]
- 13.Guan Wj., Ni Z.-y., Hu Y., Liang W.-h., Ou C.-q., He J.-x., Liu L., Shan H., Lei C.-l., Hui D.S.C., Du B., Li L.-j., Zeng G., Yuen K.-Y., Chen R.-c., Tang C.-l., Wang T., Chen P.-y., Xiang J., Li S.-y., Wang J.-l., Liang Z.-j., Peng Y.-x., Wei L., Liu Y., Hu Y.-h., Peng P., Wang J.-m., Liu J.-y., Chen Z., Li G., Zheng Z.-j., Qiu S.-q., Luo J., Ye C.-j., Zhu S.-y., Zhong N.-s. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.General Office of National Health Committee. Office of state administration of traditional Chinese medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial seventh edition). http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html.
- 15.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang X., Yu Y., Xu J., Shu H., Xia Ja., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020 doi: 10.1016/s2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.General Office of National Health Committee. Office of state administration of traditional Chinese medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial fifth edition). http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html.
- 19.Chan J.F., Yip C.C., To K.K., Tang T.H., Wong S.C., Leung K.H., Fung A.Y., Ng A.C., Zou Z., Tsoi H.W., Choi G.K., Tam A.R., Cheng V.C., Chan K.H., Tsang O.T., Yuen K.Y. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J. Clin. Microbiol. 2020 doi: 10.1128/JCM.00310-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mossa-Basha M., Meltzer C.C., Kim D.C., Tuite M.J., Kolli K.P., Tan B.S. Radiology department preparedness for COVID-19: radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simpson S., Kay F.U., Abbara S., Bhalla S., Chung J.H., Chung M., Henry T.S., Kanne J.P., Kligerman S., Ko J.P., Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol.: Cardiothorac. Imaging. 2020;2 doi: 10.1148/ryct.2020200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.British Society of Thoracic Imaging, Thoracic Imaging in COVID-19 Infection: Guidance for the Reporting Radiologist (Second edition). https://www.bsti.org.uk/standards-clinical-guidelines/clinical-guidelines/bsti-covid-19-guidance-for-the-reporting-radiologist/.
- 23.Franks T.J., Chong P.Y., Chui P., Galvin J.R., Lourens R.M., Reid A.H., Selbs E., McEvoy C.P., Hayden C.D., Fukuoka J., Taubenberger J.K., Travis W.D. Lung pathology of severe acute respiratory syndrome (SARS): a study of 8 autopsy cases from Singapore. Hum. Pathol. 2003;34:743–748. doi: 10.1016/s0046-8177(03)00367-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaw G.J., Tan D.Y., Leo Y.S., Tsou I.Y., Wansaicheong G., Chee T.S. Chest radiographic findings of a case of severe acute respiratory syndrome (SARS) in Singapore. Singapore Med. J. 2003;44:201–204. [PubMed] [Google Scholar]
- 25.Tsou I.Y., Loh L.E., Kaw G.J., Chan I., Chee T.S. Severe acute respiratory syndrome (SARS) in a paediatric cluster in Singapore. Pediatr. Radiol. 2004;34:43–46. doi: 10.1007/s00247-003-1042-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmed A.E., Al-Jahdali H., Alshukairi A.N., Alaqeel M., Siddiq S.S., Alsaab H., Sakr E.A., Alyahya H.A., Alandonisi M.M., Subedar A.T., Aloudah N.M., Baharoon S., Alsalamah M.A., Al Johani S., Alghamdi M.G. Early identification of pneumonia patients at increased risk of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int. J. Infect. Dis. 2018;70:51–56. doi: 10.1016/j.ijid.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Liu L., Shan H., Lei C.L., Hui D.S.C., Du B., Li L.J., Zeng G., Yuen K.Y., Chen R.C., Tang C.L., Wang T., Chen P.Y., Xiang J., Li S.Y., Wang J.L., Liang Z.J., Peng Y.X., Wei L., Liu Y., Hu Y.H., Peng P., Wang J.M., Liu J.Y., Chen Z., Li G., Zheng Z.J., Qiu S.Q., Luo J., Ye C.J., Zhu S.Y., Zhong N.S. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pan Y., Guan H., Zhou S., Wang Y., Li Q., Zhu T., Hu Q., Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur. Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiong Y., Sun D., Liu Y., Fan Y., Zhao L., Li X., Zhu W. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest. Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiao-yuan T.M.F. Expert consensus on imaging diagnosis and infection control for COVID-19. Chin. Comput. Med. Imag. 2020;26 doi: 10.19627/j.cnki.cn31-1700/th.20200309.001. [DOI] [Google Scholar]
- 31.Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L., Li S.B., Wang H.Y., Zhang S., Gao H.N., Sheng J.F., Cai H.L., Qiu Y.Q., Li L.J. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Webb W.R. Thin-Section CT of the Secondary Pulmonary Lobule: Anatomy and the Image—The 2004 Fleischner Lecture. Radiology. 2006;239:322–338. doi: 10.1148/radiol.2392041968. [DOI] [PubMed] [Google Scholar]
- 33.Koo H.J., Lim S., Choe J., Choi S.H., Sung H., Do K.H. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–739. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 34.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A., Jacobi A., Li K., Li S., Shan H. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020 doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kong W., Agarwal P.P. Chest imaging appearance of COVID-19 infection. Radiol.: Cardiothorac. Imaging. 2020;2 doi: 10.1148/ryct.2020200028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lei J., Li J., Li X., Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Franquet T. Imaging of pulmonary viral pneumonia. Radiology. 2011;260:18–39. doi: 10.1148/radiol.11092149. [DOI] [PubMed] [Google Scholar]
- 38.Duan Y.N., Qin J. Pre- and posttreatment chest C.T. findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yoon S.H., Lee K.H., Kim J.Y., Lee Y.K., Ko H., Kim K.H., Park C.M., Kim Y.H. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J. Radiol. 2020 doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shi H., Han X., Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology. 2020 doi: 10.1148/radiol.2020200269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H., Ling Y., Jiang Y., Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ng M.-Y., Lee E.Y., Yang J., Yang F., Li X., Wang H., Lui M.M.-s., Lo C.S.-Y., Leung B., Khong P.-L. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol.: Cardiothorac. Imaging. 2020;2 doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paul N.S., Roberts H., Butany J., Chung T., Gold W., Mehta S., Konen E., Rao A., Provost Y., Hong H.H., Zelovitsky L., Weisbrod G.L. Radiologic pattern of disease in patients with severe acute respiratory syndrome: the toronto experience. RadioGraphics. 2004;24:553–563. doi: 10.1148/rg.242035193. [DOI] [PubMed] [Google Scholar]
- 44.Okada F., Ando Y., Matsushita S., Ishii R., Nakayama T., Morikawa K., Ono A., Maeda T., Mori H. Thin-section CT findings of patients with acute Streptococcus pneumoniae pneumonia with and without concurrent infection. Br. J. Radiol. 2012;85:e357–e364. doi: 10.1259/bjr/18544730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kashyap S., Sarkar M. Mycoplasma pneumonia: clinical features and management. Lung India. 2010;27:75–85. doi: 10.4103/0970-2113.63611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guo W.-L., Wang J., Zhu L.-Y., Hao C.-L. Differentiation between mycoplasma and viral community-acquired pneumonia in children with lobe or multi foci infiltration: a retrospective case study. BMJ Open. 2015;5:e006766. doi: 10.1136/bmjopen-2014-006766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee J.S., Gong G., Lim T.H. Squalene aspiration pneumonia: thin-section CT and histopathologic findings. J. Korean Radiol. Soc. 2020;38 [Google Scholar]
- 48.Ajlan A.M., Ahyad R.A., Jamjoom L.G., Alharthy A., Madani T.A. Middle east respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings. Am. J. Roentgenol. 2014;203:782–787. doi: 10.2214/AJR.14.13021. [DOI] [PubMed] [Google Scholar]
- 49.Elise Mak, China uses AI in medical imaging to speed up COVID-19 diagnosis. https://www.bioworld.com/articles/433530-china-uses-ai-in-medical-imaging-to-speed-up-covid-19-diagnosis.
- 50.Chassagnon G., Vakalopoulou M., Paragios N., Revel M.P. Artificial intelligence applications for thoracic imaging. Eur. J. Radiol. 2020;123 doi: 10.1016/j.ejrad.2019.108774. [DOI] [PubMed] [Google Scholar]