Abstract
Background and aim
As a result of its rapid spread in various countries around the world, on March 11, 2020, WHO issued an announcement of the change in coronavirus disease 2019 status from epidemic to pandemic disease. The virus that causes this disease is indicated originating from animals traded in a live animal market in Wuhan, China. Severe Acute Respiratory Syndrome Coronavirus 2 can attack lung cells because there are many conserved receptor entries, namely Angiotensin Converting Enzyme-2. The presence of this virus in host cells will initiate various protective responses leading to pneumonia and Acute Respiratory Distress Syndrome. This review aimed to provide an overview related to this virus and examine the body’s responses and possible therapies.
Method
We searched PubMed databases for Severe Acute Respiratory Syndrome Coronavirus-2, Middle East respiratory syndrome-related coronavirus and Severe Acute Respiratory Syndrome Coronavirus. Full texts were retrieved, analyzed and developed into an easy-to-understand review.
Results
We provide a complete review related to structure, origin, and how the body responds to this virus infection and explain the possibility of an immune system over-reaction or cytokine storm. We also include an explanation of how this virus creates modes of avoidance to evade immune system attacks. We further explain the therapeutic approaches that can be taken in the treatment and prevention of this viral infection.
Conclusion
In summary, based on the structural and immune-evasion system of coronavirus, we suggest several approaches to treat the disease.
Keywords: COVID-19, SARS-CoV-2, Pandemic, ACE2, Wuhan
Abbreviations: MDA5, (Melanoma differentiation associated protein 5); DMVs, (double-membrane vesicles); MT, (Methyltransferase)
1. Introduction
Coronavirus disease 2019 (COVID-2019) is caused by a novel coronavirus known as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and was identified as a pandemic by the World Health Organization (WHO) on March 11, 2020 [1]. As of April 12, 2020, more than 1.8 million people were confirmed to have been infected and tested positive for COVID-19, with over 114,000 deaths worldwide [2]. This virus was first identified in the respiratory tract of patients with pneumonia in Wuhan, Hubei China, in December 2019 which was then indicated as a newly identified β-coronavirus (nCoV) [3,4].
SAR-CoV2 is an enveloped, non-segmented, positive sense RNA virus that is included in the sarbecovirus, ortho corona virinae subfamily which is broadly distributed in humans and other mammals [5,6]. Its diameter is about 65–125 nm, containing single strands of RNA and provided with crown-like spikes on the outer surface. SARS-CoV2 is a novel β-coronavirus after the previously identified SARS-CoV and MERS-CoV which led to pulmonary failure and potentially fatal respiratory tract infection and caused outbreaks mainly in Guandong, China and Saudi Arabia. In COVID-19 research, many studies have demonstrated that bats are suspected as the key reservoir of the viruses by finding as much as 96.2% identical genome sequencing of SARS-CoV-2 with bat CoV RaTG13 [3,7]. In this review, we hypothesize that since the COVID-19 virus has several complex immune-evasion components that contribute to its virulence, we suggest this more complete understanding can be used to develop an effective approach in the treatment of diseases caused by this virus.
2. Origin and structure of SARS-CoV2
A sample isolation from pneumonia patients who were some of the workers in the Wuhan seafood market found that strains of SARS-CoV-2 had a length of 29.9 kb [8]. Structurally, SARS-CoV-2 has four main structural proteins including spike (S) glycoprotein, small envelope (E) glycoprotein, membrane (M) glycoprotein, and nucleocapsid (N) protein, and also several accessory proteins [9]. The spike or S glycoprotein is a transmembrane protein with a molecular weight of about 150 kDa found in the outer portion of the virus. S protein forms homotrimers protruding in the viral surface and facilitates binding of envelope viruses to host cells by attraction with angiotensin-converting enzyme 2 (ACE2) expressed in lower respiratory tract cells. This glycoprotein is cleaved by the host cell furin-like protease into 2 sub units namely S1 and S2. Part S1 is responsible for the determination of the host virus range and cellular tropism with the receptor binding domain make-up while S2 functions to mediate virus fusion in transmitting host cells [3,10,11].
The nucleocapsid known as N protein is the structural component of CoV localizing in the endoplasmic reticulum-Golgi region that structurally is bound to the nucleic acid material of the virus. Because the protein is bound to RNA, the protein is involved in processes related to the viral genome, the viral replication cycle, and the cellular response of host cells to viral infections [12,13]. N protein is also heavily phosphorylated and suggested to lead to structural changes enhancing the affinity for viral RNA [10] (see Fig. 1 ).
Fig. 1.
Structure of severe acute respiratory syndrome coronavirus 2 [12,13].
Another important part of this virus is the membrane or M protein, which is the most structurally structured protein and plays a role in determining the shape of the virus envelope. This protein can bind to all other structural proteins. Binding with M protein helps to stabilize nucleocapsids or N proteins and promotes completion of viral assembly by stabilizing N protein-RNA complex, inside the internal virion. The last component is the envelope or E protein which is the smallest protein in the SARS-CoV structure that plays a role in the production and maturation of this virus [12].
In supporting the process of entry of the virus into the host cell, SARS-CoV2 binds to the ACE2 receiver that is highly expressed in the lower respiratory tract such as type II alveolar cells (AT2) of the lungs, upper esophagus and stratified epithelial cells, and other cells such as absorptive enterocytes from the ileum and colon, cholangiocytes, myocardial cells, kidney proximal tubule cells, and bladder urothelial cells [14]. Therefore, patients who are infected with this virus not only experience respiratory problems such as pneumonia leading to Acute Respiratory Distress Syndrome (ARDS), but also experience disorders of heart, kidneys, and digestive tract.
3. Entry and life cycle of coronaviruses
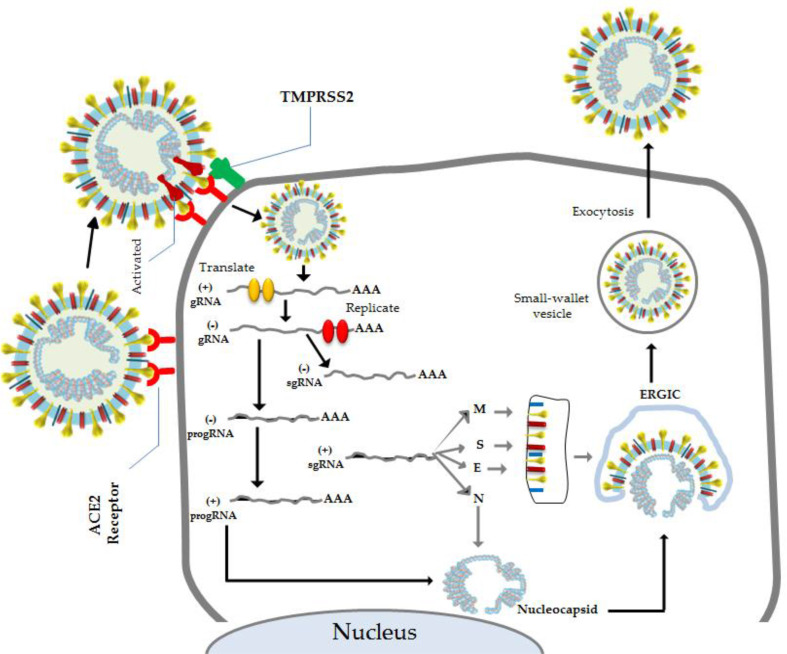
As a member of the Nidovirus family, coronavirus infection (SARS-CoV2) can be contracted from animals such as bats, and fellow humans. This virus can enter the human body through its receptors, ACE2 which are found in various organs such as heart, lungs, kidneys, and gastrointestinal tract, thus facilitating viral entry into target cells. The process of CoV entering into the host cell begins through the attachment of the S glycoprotein to the receptor, the ACE2 in the host cells (such as in type II pneumocytes in the lungs) [15]. This attachment occurs in the binding domain of S protein of SARS-CoV-2 receptors which are present at 331 to 524 residues, and can bind strongly to human ACE2 and bat ACE2 [13]. The entry and binding processes are then followed by fusion of the viral membrane and host cell [11].
After fusion occurs, the type II transmembrane serine protease (TMPRSS2) that is present on the surface of the host cell will clear the ACE2 and activate the receptor-attached spike-like, S proteins [15]. Activation of the S proteins leads to conformational changes and allows the virus to enter the cells [16]. Both of these proteins (TMPRSS2 and ACE2) are the main determinants of the entry of this virus. Based on the research of Sungnak et al. nasal epithelial cells, specifically goblet/secretory cells and ciliated cells, display the highest ACE2 expression throughout the respiratory tract [17]. Furthermore, entered-SARS-CoV-2 will subsequently release its genomic material in the cytoplasm and become translated in the nuclei (see Fig. 2 ).
Fig. 2.
Genome and nonstructural proteins of Severe Acute Respiratory Syndrome Coronavirus-2 [18].
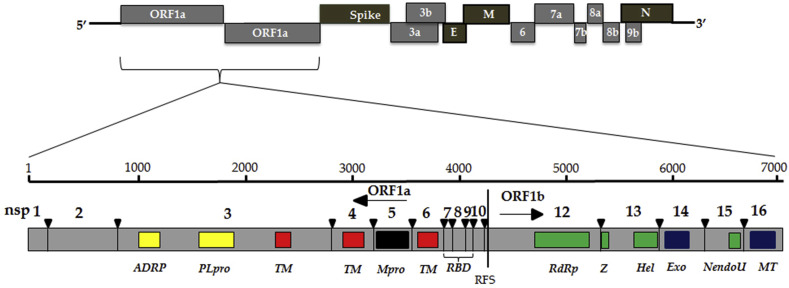
The genomic material released by this virus is mRNA that is ready to be translated into protein. In its genome range, this virus is complemented by about 14 open reading frames (ORF), each of which encodes a variety of proteins, both structural and non-structural that play a role in its survival as well as virulence power. In its phase of transformation, the gene segments that encode nonstructural polyproteins are the ones this process first translates into ORF1a and ORF1b to produce two large overlapping polyproteins, pp1a and pp1ab by contributing a ribosomal frame shifting event [19]. The polyproteins are supplemented by protease enzymes namely papain-like proteases (PLpro) and a serine type Mpro (chymotrypsin-like protease (3CLpro)) protease that are encoded in nsp3 and nsp 5. Subsequently, cleavage occurs between pp1a and pp1ab into nonstructural proteins (nsps) 1–11 and 1–16, respectively. The nsps play an important role in many processes in viruses and host cells (Table 1 ) [10,20,21] (see Fig. 3 ).
Table 1.
| Nonstructural Protein (nsp) | Function |
|---|---|
| nsp 1 & 3 | Inhibition of IFN signaling and blocking of host innate immune response by promotion of cellular degradation and blocks translation of host’s RNA |
| nsp 2 | Binding to prohibition protein |
| nsp3 & 5 | Promoting cytokine expression and cleavage of viral polyprotein |
| nsp 4 & 6 | Contribute to structure of DMVs as transmembrane scaffold protein (DMVs formation) |
| nsp 7/8 complex | Processivity clamp for RNA polymerase by arms hexadecameric complex |
| nsp9 | RNA binding protein phosphatase |
| nsp 10, 16 & 14 | Stimulation of ExoN and 2-O-MT activity |
| nsp 12 | Replication enzyme (RNA-dependent RNA polymerase) |
| nsp 13 | RNA helicase, 5′ triphosphatase |
| nsp 14 | Proofreading of viral genome |
| nsp 15 | Viral endoribonuclease and chymotrypsin-like protease |
| nsp 16 | Avoiding MDA5 recognition and inhibit innate immunity regulation |
Fig. 3.
Mechanism of entry and life cycle of Severe Acute Respiratory Syndrome Coronavirus [15,19].
Many of the nsps subsequently form replicase-transcriptase complex (RTC) in double-membrane vesicles (DMVs), which are mainly an assembly by RNA-dependent RNA polymerase (RdRp)- and helicase-containing subunits, the canonical RdRp domain residing of CoV nsp 12 and AV nsp9. Furthermore, the complex transcribes an endogenous genome template of viral entry to negative-sense genes of both the progeny genome and subgenomic RNA as intermediate products and followed by transcription to positive-sense mRNAs that are mainly mediated by RdRp [19,20,22].
Next, the subgenomic proteins become translated into structural and accessories proteins such as M, S, and E proteins that subsequently are insulated in the endoplasmic reticulum and then moved to the endoplasmic reticulum-Golgi intermediate compartment (ERGIC). Meanwhile, the previously replicated genome program can directly join the N protein to the nucleocapsid form and move into the ERGIC. In this compartment, nucleocapsids will meet with several other structural proteins and form small wallet vesicles to be exported out of the cell through exocytosis [10,19].
4. Immune response to coronavirus infection
Generally, the body’s immune response to SARS-CoV2 and SARS-CoV is closely similar being mediated by cytokines [23]. A case report in Wuhan from 99 COVID-19 patients revealed that there was an increase in the total number of neutrophils, Interluekin-6 (IL-6) serum and c-reactive protein about 38%, 52% and 86%, respectively and 35% decrease of total lymphocytes [24]. Other research found increased expression of proinflammatory cytokines and chemokines IP-10, MCP-1, MIP-1A, and tumor necrosis factor-alpha (TNFα) [5]. The conditions are correlated with severity and mortality of this disease which suggest the potential of cytokines forming as found occurring in SARS-CoV and MERS-CoV infections [25].
The entry of the virus into the host cell triggers stimulation of the host’s immune response, which will first be encountered by innate immune system cells via antigen presenting cells (APC), e.g. dendritic cells and macrophages as frontline of the immune system [15,26]. APC have Pattern Recognition Receptors (PRR) including Toll-like receptors (TLRs), NOD-like receptors (NLRs), RIG-I-like receptors (RLRs) and other small free molecules that are located in various places in host cells such as plasma membranes, endosomal membrane, lysosomes, endocytolysosomes, and cytosol. They recognize PAMP comprised nucleic acids, carbohydrate moieties, glycoproteins, lipoproteins and other small molecules that are found in the structural components of viruses or intermediate products such as dsRNA and induce cascade signaling to produce immune system cell effectors. Each of the PRRs could induce a different biological response to subsequent protein activation [23,26].
For example, Toll like receptor 4 (TLR-4) might recognize the outer component of CoV, the protein spike. Furthermore, through mediation of MyD88, this introduction will trigger the activation of NF-κB transcription factors and the pathogen-activated protein kinases (MAPKs) pathway to induce proinflammatory proteins. Meanwhile, activation of endosomal receptors such as TLR-3 and TLR that could recognize the RNA or dsRNA genome of coronavirus leads to recruitment of TRIF adapter protein directly. TRIF subsequently activates the IRF3 and NF-κB transcription factors to induce proinflammatory cytokines such as interferon-α and TNF-β. Although the introduction of PAMP through TLR-4 can also recruit TRIF adapter proteins, the recruitment must be mediated by TRAM and TIRAM [15,[25], [26], [27]]. This secret of proinflammatory cytokines is the initial response in the first line of defense against virus infection. Furthermore, type I INF in turn will form complexes with its receptors, IFNAR and subsequently activate the JAK-STAT pathways. JAK1 and TYK2 kinases further phosphorylate STAT1 and 2 followed by its complexation with IRF9, and together they migrate into the nucleus to initiate the transcription of IFN-stimulated genes (ISGs) and lead to suppression of viral replication and prevent the severity of the disease [25]. However, excess releasing of pro-inflammatory cytokines such as IFN-α, IFN-γ, IL-1β, IL-6, IL-12, IL-18, IL-33, TNF-α, TGFβ, and chemokines CCL2, CCL3, CCL5, CXCL8, CXCL9, CXCL10 from immune effector cells causes hyperinflammation which will eventually lead to ARDS [28,29].
As the presenter of foreign antigens, the APC will present the antigen of CoV to the CD4 + T-helper cells by MHC class 1, and this leads to releasing of IL-12 as a co-stimulatory molecule to further stimulate the Th1 cell activation. In addition to Th1 stimulation, releasing of interleukin-12 and IFN-α, an increase in MHC Class I expression and NK cell activation is also needed for resistance of viral replication for the eradication of virus-infected cells. It also initiates production of proinflammatory cytokines via the NF-κB signaling pathway. IL-17 is a proinflammatory cytokine that also is increased when SARS-CoV2 infection occurs. These cytokines further recruit neutrophils and monocytes to the site of infection and activate several other pro-inflammatory cytokines and chemokines including IL-1, IL-6, IL-8, IL-21, TNF-β, and MCP-1 [15,26,30,31].
Next, activation of Th1 cells could stimulate CD8 + T cells, which are one of the effectors of T cells that will target and kill cells infected with CoV. At the same time, CD4 T cells could stimulate humoral immune responses by producing antigen-specific antibodies via activating T-dependent B cells [15,28,30].
The antibodies produced are generally IgM and IgG which have a unique presence pattern in response to the presence of coronavirus [28]. Generally, this infection will produce a specific IgM that can only last 12 weeks, but IgG with a longer period. In addition to the formation of antibodies, exposure to this virus also cause the formation of CD4 T cells and CD8 memory that can last for four years [32]. In fact, based on findings in patients who recovered six year after coronavirus infection, T cell memory was still able to hit the peptide spike when the first exposure occurred [33]. This further explains and directs researchers to the development of vaccines against the corona virus, especially to SARS-COV-2, which is now a pandemic outbreak in the worldwide [28].
5. Immuno-evasion of coronaviruses
Generally, viruses including coronavirus have number of avoidance ways from onslaught of immune system cells to better survive and infect host cells [28,30]. The strategy can be applied to various processes, both at the time of introduction (before entering the cell) and when it has entered the host cell. During the recognition process, this virus can use avoidance strategies through the formation of double vesicles on the outside of the cell. The formation of these vesicles causes shield recognition of cytosolic PRRs to dsRNA as an intermediate product of replication virus [28].
In addition to the formation of a double vesicle, this virus has 8 proteins capable of avoiding the immune system through the blocking of INF. Nsp1 is a non-structural group of proteins from SARS-CoV that can suppress the work of INF–I through host translational machinery inactivation, RNA-Host degradation and inhibition of phosphorylation of STAT1. The mechanism could cause INF–I failure to induce replication and dissemination of viruses at an early stage and leads to increased severity of disease [25,27]. The composition of the viral RNA genome including SARS-CoV which has a 5 ′cap less than the host cell RNA makes it easy for immune system cells to recognize its presence and induce an immune response. To get around this, the virus developed a strategy of mimicking the host capping machinery. This strategy employs two non-structural proteins namely nsp 14 which initiates cap formation, and subsequently follows modifying the cap of viral RNAs by nsp 16 so that RNA viral seems similar to host cell RNA and avoids any PRRs recognition [27,34,35].
Other nonstructural proteins from coronavirus that also have the ability to prevent this virus from immune responses are nsp3 that encoded two functional proteins, macrodomains and PLpro (cleavage of nsps). Both of these proteins appear to be employed as actors in the evading of SARS-CoV from immune response-induce viruses. This possibility was supported by Fehr et al. in their in vivo study in BALB/c mice that were infected by SARS-CoV-lacking macrodomains. The findings of this study revealed that although there was an increase in expression of type I IFN, ISG15, CXCL10 and the proinflammatory cytokines IL-6 and TNF, followed by significantly higher survival, there was no lung pathology development in the mice [36]. The finding is closely similar to other studies conducted in mice demonstrating a lack of deubiquitinating enzyme (DUB) activity in MERS-CoV. DUB is another role of PLpro to help coronavirus evade attack from a host’s immune response by antagonizing the IFN response. From these findings, we hypothesized that the decline in function of the two proteins may lead to the direct introduction and sticking of immune troops to continuously infected cells and prevented the replication of the virus and the life cycle [37,38]. In addition to using nonstructural proteins, SARS-CoV could utilize its protein accessories to avoid immune responses. For example the gene segment located on ORF3b of this virus has the ability to antagonize the INF signaling pathway and cause inhibition of the effector cell activation cascade for eradication and inhibition of viral replication [39]. Equally of concern, the protein encoded in ORF6 could inhibit JAK-STAT signaling pathway by binding to karyopherin-α2, and tethers karyopherin-β1 on internal membranes to lead to blocking nuclear translocation of the transcription factor STAT1 [27].
6. Approach for SARS-CoV-2-related disease therapy
There is no specific treatment for eradication of the SARS-CoV2 virus in patients. Accordingly, the therapeutic approach that can be done is to use another β-coronavirus approach such as SARS-CoV or MERS-CoV treatments. Some possible therapies can be given according to the approaches including lopinavir/ritonavir, chloroquine, and hydroxychloroquine. Aerosol inhalation of alpha-interferon twice per night also could be used. In some cases coronaviruses (such as MERS-CoV) have commonly used combinations of interferon-α combined with ribavirin [40,41]. This therapy seems to be able to give results at the beginning of therapy, that is 14 days after being diagnosed, but this effect disappears when entering day 28. Furthermore, Loutfy et al. found that the combination of interferon with steroid drugs can accelerate lung repair and increase oxygen survival levels. Therapy using interferon-α is still confusing. Other studies have concluded that this therapy does not have a beneficial effect on patients [38,42].
As a matter of fact, as with epidemics that have occurred before and since the death ratio caused by COVID 19 is quite high, mitigation methods need to be developed, one of which is through the development of vaccines that have not yet been found. Specific vaccines could be used to initiate the formation of specific antibodies against the SARS-CoV2 virus. This development is being temporarily developed in various parts of the world and is the focus of today’s global efforts. In fact, according to a news release from Jakarta Globe on March 27, 2019, the G20 has set aside about USD$ 4 billion for the development of the vaccine [40,43].
Spike or S protein-based vaccine is one approach to developing vaccines that has attracted the attention of many researchers in the discovery of the coronavirus vaccine. S protein has an RBD located in the S1 subunit of the virus that facilitates entry of the virus into the host cell by binding to its receptors on the host cell, ACE2. Furthermore, the existence of mapping and genomic characterization of these proteins has increasingly answered the puzzle in the development of this vaccine [44,45]. Research by Yang et al. that used combined DNA demonstrated protein S could activate the immune response through T cell production that subsequently form antibodies which can neutralize the virus in mice. Another study shown that this strategy was effective to elicit protective immunity producing neutralizing antibodies in mice [46,47]. Further studies with closely similar results conducted by Gao et al. and He et al. that used reconstructed vaccine which originated from S1 fragment of SARS-CoV revealed that it could stimulate immune response and induce highly potent neutralizing antibodies to blocking S protein binding and prevent SARS-CoV entry [48,49].
In addition, through recent developments in vaccine-based therapy for cancers and other diseases, therapeutic development efforts also focus on drug discovery that can stop the spread and replication of the virus in the host cell that is intended for patients who have already contracted an infection. These include camostat mesylate which is a serine protease inhibitor that can inhibit the performance of TMPRSS2 enzyme activity in the coronavirus entry process. This drug has been used clinically in the treatment of chronic pancreatitis so that it is considered to be a potential therapy for COVID-19 treatment [[50], [51], [52]]. In addition to the two therapeutic approaches above, other potential therapeutic development pathways for patients with this viral infection can be done through blocking ACE2 receptors and RNA interference using siRNA or microRNA [[52], [53], [54]].
It is now well-known that the pathogenesis of ARDS-induced coronaviruses involves microRNA in the cell nuclei. This discovery gave rise to new knowledge in the development of microRNA-based anti-coronavirus therapy approaches. MicroRNA-based therapy has been proven both in vitro, in vivo and clinically to cure diseases in the form of viral infections, cancer and other degenerative diseases [54,55].
7. Conclusions
In summary, we conclude that coronavirus has unique and complete components. Its immune-evasion components that contribute to evade from recognition of the immune system lead infectivity and fatality to host.
It is now well-known that the pathogenesis of disease-induced coronaviruses, the development of therapy will be more specific. For example the development of serine protease inhibitor or RBD-based vaccine also became coronavirus therapy approach. However, further research is necessary to develop these findings for clinical application in patients.
Author contribution
Indwiani Astuti: contributed masterplan of draft review and wrote introduction, origin and structure of coronavirus and entry and life cycle of coronaviruses; Ysrafil: contributed wrote immune response of coronavirus infection, immuno-evasion of coronaviruses, approaches for SARS-CoV-2-related disease therapy and figure design.
Funding
None declared.
Declaration of competing interest
None declared.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus W.H.O. WHO; 2020. COVID-19.https://who.sprinklr.com/ [Google Scholar]
- 3.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Military Medical Research. 2020;7:1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tian X., Li C., Huang A., Xia S., Lu S., Shi Z. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg Microb Infect. 2020;9:382–385. doi: 10.1080/22221751.2020.1729069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ul Qamar M.T., Alqahtani S.M., Alamri M.A., Chen L.-L. Structural basis of SARS-CoV-2 3CLpro and anti-COVID-19 drug discovery from medicinal plants. J Pharm Anal. 2020 doi: 10.1016/j.jpha.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu F., Zhao S., Yu B., Chen Y.-M., Wang W., Song Z.-G. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang S., Hillyer C., Du L. Neutralizing antibodies against SARS-CoV-2 and other human Coronaviruses. Trends Immunol. 2020 doi: 10.1016/j.it.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fehr A.R., Perlman S. Springer; New York: 2015. Coronaviruses: an overview of their replication and pathogenesis. Coronaviruses; pp. 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020 doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tai W., He L., Zhang X., Pu J., Voronin D., Jiang S. Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell Mol Immunol. 2020:1–8. doi: 10.1038/s41423-020-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu H., Zhong L., Deng J., Peng J., Dan H., Zeng X. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:1–5. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rabi F.A., Al Zoubi M.S., Kasasbeh G.A., Salameh D.M., Al-Nasser A.D. SARS-CoV-2 and Coronavirus Disease 2019: what we know so far. Pathogens. 2020;9:231. doi: 10.3390/pathogens9030231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simmons G., Zmora P., Gierer S., Heurich A., Pöhlmann S. Proteolytic activation of the SARS-coronavirus spike protein: cutting enzymes at the cutting edge of antiviral research. Antivir Res. 2013;100:605–614. doi: 10.1016/j.antiviral.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sungnak W, Huang N, Bécavin C, Berg M, Network H. SARS-CoV-2 entry genes are most highly expressed in nasal goblet and ciliated cells within human airways. arXiv preprint arXiv 2020.
- 18.Dandekar A.A., Perlman S. Immunopathogenesis of coronavirus infections: implications for SARS. Nat Rev Immunol. 2005;5:917–927. doi: 10.1038/nri1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020 doi: 10.1002/jmv.26234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun L., Xing Y., Chen X., Zheng Y., Yang Y., Nichols D.B. Coronavirus papain-like proteases negatively regulate antiviral innate immune response through disruption of STING-mediated signaling. PloS One. 2012;7 doi: 10.1371/journal.pone.0030802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Posthuma C.C., te Velthuis A.J., Snijder E. Nidovirus RNA polymerases: complex enzymes handling exceptional RNA genomes. Virus Res. 2017;234:58–73. doi: 10.1016/j.virusres.2017.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yi Y., Lagniton P.N., Ye S., Li E., Xu R.-H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020;16:1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prompetchara E., Ketloy C., Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38:1–9. doi: 10.12932/AP-200220-0772. [DOI] [PubMed] [Google Scholar]
- 26.Li G., Fan Y., Lai Y., Han T., Li Z., Zhou P. Coronavirus infections and immune responses. J Med Virol. 2020;92:424–432. doi: 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Totura A.L., Baric R.S. SARS coronavirus pathogenesis: host innate immune responses and viral antagonism of interferon. Curr Opin Virol. 2012;2:264–275. doi: 10.1016/j.coviro.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li X., Geng M., Peng Y., Meng L., Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020 doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen J., Lau Y.F., Lamirande E.W., Paddock C.D., Bartlett J.H., Zaki S.R. Cellular immune responses to severe acute respiratory syndrome coronavirus (SARS-CoV) infection in senescent BALB/c mice: CD4+ T cells are important in control of SARS-CoV infection. J Virol. 2010;84:1289–1301. doi: 10.1128/JVI.01281-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Janeway C., Murphy K., Travers P., Walport M. Garland Science; New York: 2008. Janeway’s immunobiology. [Google Scholar]
- 31.Zumla A., Hui D.S., Azhar E.I., Memish Z.A., Maeurer M. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet. 2020;395:e35–e36. doi: 10.1016/S0140-6736(20)30305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fan Y.-Y., Huang Z.-T., Li L., Wu M.-H., Yu T., Koup R.A. Characterization of SARS-CoV-specific memory T cells from recovered individuals 4 years after infection. Arch Virol. 2009;154:1093–1099. doi: 10.1007/s00705-009-0409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang F., Quan Y., Xin Z.-T., Wrammert J., Ma M.-J., Lv H. Lack of peripheral memory B cell responses in recovered patients with severe acute respiratory syndrome: a six-year follow-up study. J Immunol. 2011;186:7264–7268. doi: 10.4049/jimmunol.0903490. [DOI] [PubMed] [Google Scholar]
- 34.Chen Y., Cai H., Xiang N., Tien P., Ahola T., Guo D. Functional screen reveals SARS coronavirus nonstructural protein nsp 14 as a novel cap N7 methyltransferase. Proc Natl Acad Sci Unit States Am. 2009;106:3484–3489. doi: 10.1073/pnas.0808790106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daffis S., Szretter K.J., Schriewer J., Li J., Youn S., Errett J. 2′-O methylation of the viral mRNA cap evades host restriction by IFIT family members. Nature. 2010;468:452–456. doi: 10.1038/nature09489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fehr A.R., Athmer J., Channappanavar R., Phillips J.M., Meyerholz D.K., Perlman S. The nsp3 macrodomain promotes virulence in mice with coronavirus-induced encephalitis. J Virol. 2015;89:1523–1536. doi: 10.1128/JVI.02596-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Knaap R.C., Fernández-Delgado R., Dalebout T.J., Oreshkova N., Bredenbeek P.J., Enjuanes L. The deubiquitinating activity of Middle East respiratory syndrome coronavirus papain-like protease delays the innate immune response and enhances virulence in a mouse model. bioRxiv. 2019:751578. [Google Scholar]
- 38.Nelemans T., Kikkert M. Viral Innate immune evasion and the pathogenesis of emerging RNA virus infections. Viruses. 2019;11:961. doi: 10.3390/v11100961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freundt E.C., Yu L., Park E., Lenardo M.J., Xu X.-N. Molecular determinants for subcellular localization of the severe acute respiratory syndrome coronavirus open reading frame 3b protein. J Virol. 2009;83:6631–6640. doi: 10.1128/JVI.00367-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; 2020. Features, evaluation and treatment coronavirus (COVID-19) StatPearls [Internet] [PubMed] [Google Scholar]
- 41.Falzarano D., De Wit E., Martellaro C., Callison J., Munster V.J., Feldmann H. Inhibition of novel β coronavirus replication by a combination of interferon-α2b and ribavirin. Sci Rep. 2013;3:1686. doi: 10.1038/srep01686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Loutfy M.R., Blatt L.M., Siminovitch K.A., Ward S., Wolff B., Lho H. Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: a preliminary study. J Am Med Assoc. 2003;290:3222–3228. doi: 10.1001/jama.290.24.3222. [DOI] [PubMed] [Google Scholar]
- 43.Yasmin N. Jakarta Globe; Jakarta: 2020. G20 to raise $4b for covid-19 vaccine development. Jakarta Globe. [Google Scholar]
- 44.Zhu X., Liu Q., Du L., Lu L., Jiang S. Receptor-binding domain as a target for developing SARS vaccines. J Thorac Dis. 2013;5:S142. doi: 10.3978/j.issn.2072-1439.2013.06.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang Z-y, Kong W-p, Huang Y., Roberts A., Murphy B.R., Subbarao K. A DNA vaccine induces SARS coronavirus neutralization and protective immunity in mice. Nature. 2004;428:561–564. doi: 10.1038/nature02463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Du L., He Y., Zhou Y., Liu S., Zheng B.-J., Jiang S. The spike protein of SARS-CoV—a target for vaccine and therapeutic development. Nat Rev Microbiol. 2009;7:226–236. doi: 10.1038/nrmicro2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gao W., Tamin A., Soloff A., D’Aiuto L., Nwanegbo E., Robbins P.D. Effects of a SARS-associated coronavirus vaccine in monkeys. Lancet. 2003;362:1895–1896. doi: 10.1016/S0140-6736(03)14962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.He Y., Zhou Y., Liu S., Kou Z., Li W., Farzan M. Receptor-binding domain of SARS-CoV spike protein induces highly potent neutralizing antibodies: implication for developing subunit vaccine. Biochem Biophys Res Commun. 2004;324:773–781. doi: 10.1016/j.bbrc.2004.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kawase M., Shirato K., van der Hoek L., Taguchi F., Matsuyama S. Simultaneous treatment of human bronchial epithelial cells with serine and cysteine protease inhibitors prevents severe acute respiratory syndrome coronavirus entry. J Virol. 2012;86:6537–6545. doi: 10.1128/JVI.00094-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou Y., Vedantham P., Lu K., Agudelo J., Carrion R., Jr., Nunneley J.W. Protease inhibitors targeting coronavirus and filovirus entry. Antivir Res. 2015;116:76–84. doi: 10.1016/j.antiviral.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu C., Zhou Q., Li Y., Garner L.V., Watkins S.P., Carter L.J. ACS Publications; Mashington, D.C.: 2020. Research and development on therapeutic agents and vaccines for COVID-19 and related human coronavirus diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rossbach M. Small non-coding RNAs as novel therapeutics. Curr Mol Med. 2010;10:361–368. doi: 10.2174/156652410791317048. [DOI] [PubMed] [Google Scholar]
- Ysrafil Y., Astuti I., Anwar S.L., Martien R., Fan Sumadi, Wardhana T. MicroRNA -155-5p diminishes in vitro ovarian cancer viability by targeting HIF1α expression. Adv Pharmaceut Bull. 2020 doi: 10.34172/apb.2020.076. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]