Abstract
The purpose of this study was to assess if clinical indications, patient location, and imaging sites predict the viewing pattern of referring physicians for CT and MR of the head, chest, and abdomen. Our study included 166,953 CT/MR images of head/chest/abdomen in 2016–2017 in the outpatient (OP, n = 83,981 CT/MR), inpatient (IP, n = 51,052), and emergency (ED, n = 31,920) settings. There were 125,329 CT/MR performed in the hospital setting and 41,624 in one of the nine off-campus locations. We extracted information regarding body region (head/chest/abdomen), patient location, and imaging site from the electronic medical records (EPIC). We recorded clinical indications and the number of times referring physicians viewed CT/MR (defined as the number of separate views of imaging in the EPIC). Data were analyzed with the Microsoft SQL and SPSS statistical software. About 33% of IP CT and MR studies are viewed > 6 times compared to 7% for OP and 19% of ED studies (p < 0.001). Conversely, most OP studies (55%) were viewed 1–2 times only, compared to 21% for IP and 38% for ED studies (p < 0.001). In-hospital exams are viewed (≥ 6 views; 39% studies) more frequently than off-campus imaging (≥ 6 views; 17% studies) (p < 0.001). For head CT/MR, certain clinical indications (i.e., stroke) had higher viewing rates compared to other clinical indications such as malignancy, headache, and dizziness. Conversely, for chest CT, dyspnea-hypoxia had much higher viewing rates (> 6 times) in IP (55%) and ED (46%) than in OP settings (22%). Patient location and imaging site regardless of clinical indications have a profound effect on viewing patterns of referring physicians. Understanding viewing patterns of the referring physicians can help guide interpretation priorities and finding communication for imaging exams based on patient location, imaging site, and clinical indications. The information can help in the efficient delivery of patient care.
Keywords: CT, MR, Radiology reports, Referring physician, Patient location, Imaging use
Introduction
Modern electronic medical record systems enable radiologists to have access to key clinical information at the time of protocoling and interpreting imaging examinations. Likewise, the referring physicians can access and view radiology reports and studies from these systems. Such bidirectional interaction improves confidence, expediency, and communication between the providers.
With the rising use of cross-sectional imaging in clinical diagnosis and patient management, many referring physicians routinely review radiology reports and images of their patients to understand findings and make clinical decisions regarding their management. Several studies have assessed the role of image-rich and structured radiology reports to improve consistency amongst radiologists and help referring physicians recall and analyze important radiology findings [1, 2]. Research on radiology reports has also focused on physician compliance with suggestions or recommendations for follow up or additional imaging in the radiology reports [3]. There is also an increased use of radiology images as visual aids when discussing the diagnosis and treatment options with patients and their caregivers. Other studies have assessed the efficiency of communication of urgent and actionable radiology findings to the referring physicians [4–6]. Such investigations help understand and develop optimal ways for delivering radiology reports and studies related information to the referrers [7].
Understanding how the referring physicians and the caretaking team view radiology reports and studies of their patients may guide interpretation priorities for imaging exams based on patient location, imaging site, and clinical indications. Knowledge of viewing rates for different clinical indications and imaging tests can help create better ways of communicating and relaying imaging findings to the referring physicians. Thus, the purpose of our study was to assess if clinical indications, patient location, and imaging sites can predict the viewing pattern of referring physicians for CT and MR of the head, chest, and abdomen.
Methods and Materials
This retrospective, quality assurance study was exempted from Institutional Review Board approval and used de-identified patient information. One study co-author (MKK) received research grants from Siemens Healthineers and Riverain Inc. for unrelated research. None of the other co-authors have any financial disclosures. All study authors had complete and unrestricted access to the study data and manuscript.
Imaging Examinations
All included imaging examinations were performed in a single quaternary healthcare center. These examinations represented consecutive CT (n = 122,341) and MR (n = 44,612) of the head, chest, or abdomen of a total of 166,953 studies has been performed between April 2016 and August 2017. There were 36,657 head CT, 43,360 chest CT, and 42,324 abdomen CT in addition to 34,574 head MR, 418 chest MR, and 9620 abdomen MR. All studies regardless of the patients age, gender or race were included.
The information pertaining to these imaging examinations was extracted from our electronic medical record system (EPIC Systems Corporation, Verona, Wisconsin) using the Microsoft SQL program (Microsoft Inc., Redmond, Washington). In addition, we also obtained information pertaining to the location of the imaging equipment (on-site in the main hospital building versus nine off-campus outpatient satellite imaging centers) where each examination was performed. There were 125, 329 on-site exams and 41,624 off-campus exams (Table 1). Patient location (outpatient, inpatient, and emergency department) at the time of imaging was obtained (Table 1). We recorded the specified clinical indication and body region for imaging at the time of ordering of the imaging examination in the radiology order entry system portal within EPIC system.
Table 1.
Distribution of different imaging studies according to the location of the imaging equipment and patients
| Head CT | Head MR | Chest CT | Chest MR | Abdomen CT | Abdomen MR | ||
|---|---|---|---|---|---|---|---|
| Exam location | On-site | 33,892 | 23,887 | 29,972 | 201 | 31,491 | 5886 |
| Off campus | 2765 | 10,687 | 13,388 | 217 | 10,833 | 3734 | |
| Total | 36,657 | 34,574 | 43,360 | 418 | 42,324 | 9620 | |
| Patient location | Inpatient | 17,914 | 9395 | 10,921 | 24 | 11,186 | 1612 |
| Outpatient | 6680 | 21,066 | 27,653 | 384 | 20,390 | 7808 | |
| Emergency | 12,063 | 4113 | 4786 | 10 | 10,748 | 200 | |
| Total | 36,657 | 34,574 | 43,360 | 418 | 42,324 | 9620 |
Physician Views per Exam
Each review of the radiology images and/or images by the patient’s ordering physician or member of his or her caretaking team in EPIC was deemed as a “view.” For each imaging examination, we recorded the number of times the ordering or caretaking team viewed the radiology report and/or images within EPIC system over an average period time of 53 (± 79) days from the date of examination. The viewing frequency (1, 2, 3, 4, 5, 6, 7, 8, 9, and ≥ 10 times) were further stratified based on imaging exams, clinical indications, equipment location, and the patient location at the time of imaging. We classified the viewing frequency into three main subgroups (< 2 times, 2–5 times, and ≥ 6 times) for each clinical indication with at least 50 imaging examinations. The viewing frequency for the top three clinical indications for each imaging modality and imaged body region were estimated.
Statistical Analysis
Microsoft SQL was used for stratification of the number of views in EPIC based on different patient and imaging attributes. Descriptive statistics were performed in Microsoft Excel. All statistical analyses were performed by a qualified statistician (TC). The chi-square test (SPSS Statistical Software, IBM Inc.) for categorical variables was used to compare viewing frequency groups and scan-related characteristics. A weak association can result in near-zero p value due to the large sample size. Therefore, Cramer’s V was used to detect whether the relationships were strong enough to be practically meaningful. This value ranges from 0 to 1, with larger values of V indicating stronger associations in the variables (0.10–0.20 weak, 0.20–0.25 moderate, 0.30–0.35 strong, 0.45–0.99 redundant, 1.00 perfect relationship).
Results
Exam Types
Most exam types were reviewed once or twice (41%) regardless of the clinical indication and the exam type. About 17% of the imaging examinations garnered multiple views (> 10 or more). Head MR (20%), head CT (19%), and abdomen CT (19%) had the highest frequency of ≥ 10 views whereas chest CT (12%) and abdomen MR (9%) had the lowest frequency of multiple views. There were significant statistical differences between the distribution of viewing frequencies for different exam types (p < 0.0001).
Clinical Indications
The viewing frequencies for the top three most frequently specified clinical indications for different exam types are summarized in Table 2. CT examinations garnered higher viewing frequency as compared to MR examinations. Urgent or life-threatening clinical indications such as cerebrovascular accidents (head CT), dyspnea or hypoxia (chest CT), and abdominal pain (abdomen CT) had higher viewing frequency compared to non-urgent clinical indications. Different clinical indications for different imaging modalities had different viewing rates. The most commonly specified clinical indications often did not have the highest viewing frequency across different exam types in head, chest, and abdomen.
Table 2.
Viewing frequency for the top three clinical indications for different exam types included in the study. The percentages refer to the proportion of viewing frequencies for the stated clinical indications
| Clinical indications | Total (%) | 1 view | 2–5 views | ≥ 6 views |
|---|---|---|---|---|
| Head CT | ||||
| CVA | 6074 (17%) | 490 (8%) | 1960 (32%) | 3624 (60%) |
| Trauma | 5770 (16%) | 1805 (31%) | 2423 (42%) | 1542 (27%) |
| Altered consciousness | 4288 (12%) | 1038 (24%) | 1966 (46%) | 1284 (30%) |
| Head MR | ||||
| Malignancy | 5468 (16%) | 1149 (21%) | 2581 (47%) | 1738 (32%) |
| Benign neoplasm | 3101 (9%) | 715 (23%) | 1532 (49%) | 854 (28%) |
| Focal neural deficit | 3025 (9%) | 545 (18%) | 1212 (40%) | 1268 (42%) |
| Chest CT | ||||
| Malignancy | 13,521(31%) | 5703 (42%) | 6156 (46%) | 1662 (12%) |
| Dyspnea-hypoxia | 4487 (10%) | 699 (16%) | 1815 (40%) | 1973 (44%) |
| Lung nodules | 3502 (8%) | 1256 (36%) | 1607 (46%) | 639 (18%) |
| Abdomen CT | ||||
| Abdominal pain | 11,119 (26%) | 2378 (21%) | 4115 (37%) | 4626 (42%) |
| Malignancy | 10,749 (25%) | 4265 (40%) | 4547 (42%) | 1937 (18%) |
| Kidney stone | 1408 (3%) | 308 (22%) | 697 (49%) | 403 (29%) |
| Abdomen MR | ||||
| Malignancy | 2061 (21%) | 647 (31%) | 1005 (49%) | 409 (20%) |
| Mass | 791 (8%) | 269 (34%) | 351 (44%) | 171 (22%) |
| Pain | 406 (4%) | 133 (33%) | 183 (45%) | 91 (22%) |
CVA cerebrovascular accident
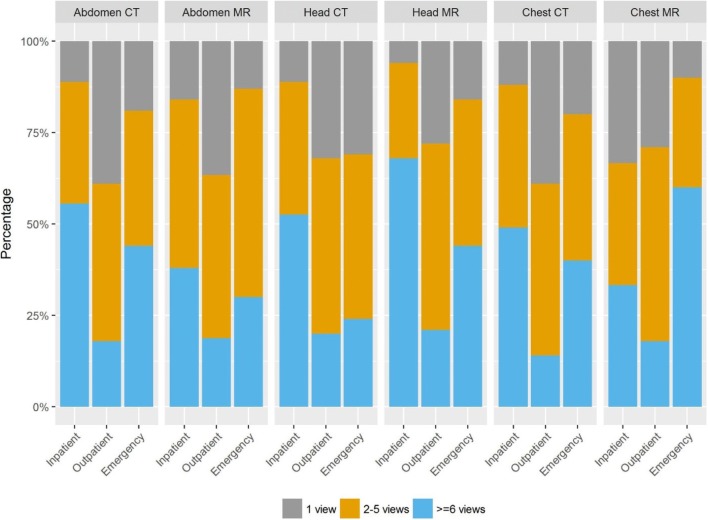
Imaging and Patient Location
The summarized viewing frequencies with row percentages are presented in Tables 3, 4, and 5, as well as in Figs. 1 and 2. The patient and exam locations were both significantly associated with viewing frequencies for different types of scans (p < 0.01), except for the exam locations of chest MR (p = 0.06). Cramer’s V values indicated that most associations were fairly strong (ranging from 0.24 to 0.31), except for exam locations of head CT and for both locations of chest MR and abdomen MR (Tables 3, 4, and 5).
Table 3.
Descriptive statistics of exam types, imaging location, patient location, and different number of views (head CT/MR). The p values compare the differences in viewing frequencies for given patient and exam locations for head CT and MR studies
| Location | Total | 1 view | 2–5 views | ≥ 6 views | p value | Cramer’s V | ||
|---|---|---|---|---|---|---|---|---|
| Head CT | Patient location |
Inpatient Outpatient Emergency |
17,914 6680 12,063 |
11% (2013) 32% (2111) 31% (3732) |
36% (6513) 48% (3237) 45% (5478) |
52% (9388) 20% (1332) 24% (2853) |
< 0.01 | 0.24 |
| Exam location |
Off Campus On-site |
2765 33,892 |
40% (1105) 20% (6751) |
45% (1240) 41% (13988) |
15% (420) 39% (13153) |
< 0.01 | 0.15 | |
| Head MR | Patient location |
Inpatient Outpatient Emergency |
9395 21,066 4113 |
6% (607) 28% (5950) 16% (656) |
26% (2400) 51% (10793) 40% (1656) |
68% (6388) 21% (4323) 44% (1801) |
< 0.01 | 0.31 |
| Exam location |
Off Campus On-site |
10,687 23,887 |
30% (3233) 17% (3980) |
51% (5436) 39% (9413) |
19% (2018) 44% (10494) |
< 0.01 | 0.25 |
Table 4.
Descriptive statistics of exam types, imaging location, patient location, and different number of views (chest CT/MR). The p values compare the differences in viewing frequencies for given patient and exam locations for chest CT and MR studies
| Location | Total | 1 view | 2–5 views | ≥ 6 views | p value | Cramer’s V | ||
|---|---|---|---|---|---|---|---|---|
| Chest CT | Patient location |
Inpatient Outpatient Emergency |
10,921 27,653 4786 |
12% (1291) 39% (10767) 20% (943) |
39% (4293) 47% (13035) 40% (1915) |
49% (5337) 14% (3851) 40% (1928) |
< 0.01 | 0.27 |
| Exam location |
Off Campus On-site |
13,388 29,972 |
42% (5652) 25% (7349) |
46% (6167) 44% (13076) |
12% (1569) 32% (9547) |
< 0.01 | 0.24 | |
| Chest MR | Patient location |
Inpatient Outpatient Emergency |
24 384 10 |
33% (8) 29% (111) 10% (1) |
33% (8) 53% (203) 30% (3) |
33% (8) 18% (70) 60% (6) |
< 0.01 | 0.13 |
| Exam location |
Off Campus On-site |
217 201 |
25% (54) 33% (66) |
57% (123) 45% (91) |
18% (40) 22% (44) |
0.06 | 0.12 |
Table 5.
Descriptive statistics of exam types, imaging location, patient location, and different number of views (abdomen CT/MR). The p values compare the differences in viewing frequencies for given patient and exam locations for abdomen CT and MR studies
| Location | Total | 1 view | 2–5 views | ≥ 6 views | p value | Cramer’s V | ||
|---|---|---|---|---|---|---|---|---|
| Abdomen CT | Patient location |
Inpatient Outpatient Emergency |
11,186 20,390 10,748 |
11% (1256) 39% (7862) 19% (2068) |
33% (3729) 43% (8856) 37% (3927) |
55% (6201) 18% (3672) 44% (4753) |
< 0.01 | 0.26 |
| Exam location |
Off Campus On-site |
10,833 31,491 |
42% (4502) 21% (6684) |
42% (4582) 38% (11930) |
16% (1749) 41% (12877) |
< 0.01 | 0.25 | |
| Abdomen MR | Patient location |
Inpatient Outpatient Emergency |
1612 7808 200 |
16% (260) 37% (2870) 13% (26) |
46% (734) 45% (3488) 57% (115) |
38% (618) 19% (1450) 30% (59) |
< 0.01 | 0.15 |
| Exam location |
Off Campus On-site |
3734 5886 |
36% (1333) 31% (1823) |
44% (1637) 46% (2700) |
20% (764) 23% (1363) |
< 0.01 | 0.05 |
Fig. 1.
Viewing frequency and imaging equipment location (off-site versus on-site) for head, chest, and abdomen CT and MR examinations
Fig. 2.
Viewing frequency and patient location (inpatient vs outpatient vs emergency department) for head, chest, and abdomen CT and MR examinations
With the exception of the abdomen MR examinations, on-site imaging had higher viewing frequency compared to those performed at off-site imaging location (p < 0.01). Malignancy was one of the top three frequently performed and viewed clinical indication regardless of the modality and body region in both on-site and off-site settings, except for on-site head CT. For the head CT, cerebrovascular accident (CVA) had higher frequency of viewing in both on and off-site settings. For the same clinical indications and exam type, most on-site exams had a higher viewing frequency compared to off-site exams.
Malignancy was the lead indication for outpatient body exams, while trauma, pain, and hypoxia were the lead clinical indications for inpatient imaging examinations. There were significant differences between viewing rates of imaging exams for similar clinical indications in different patient location (outpatient versus inpatient versus emergency settings) (p < 0.01).
Discussion
We found that the imaging site, patient location, and clinical indications were significant predictors of viewing frequency of radiology reports in the electronic medical records. Chronic diseases such as malignancy were the most frequent indications for MR exams in head, chest, and abdomen and had the highest viewing frequencies. Conversely, regardless of the body part, CT for acute clinical indications such as stroke, dyspnea-hypoxia, abdominal pain, and renal colic had higher viewing frequencies compared to those associated with malignancies. Interestingly, radiology reports of exams performed on-site had higher viewing frequency as compared to those performed at off-site imaging facilities when imaging exam, clinical indication, and body regions were matched. This may have been related to the fact that patients imaged on-site may be sicker and/or have multiple caretaking healthcare providers as compared to patients imaged at off-site facilities. These reasons likely apply to the variations in viewing frequency for imaging exams performed for different patient locations. Viewing frequencies for exams with similar clinical indications amongst inpatients and emergency department patients were higher when compared to the corresponding imaging exams in outpatients.
To the best of our knowledge, there are no published studies on physicians’ viewing frequencies of radiology reports in the electronic medical records. However, in a study from 2002, McEnery et al. reported on the use of radiology image retrieval from an enterprise level archive [8]. In that study, most imaging retrievals (51.5%) were for those less than 72 h old, although 9.9% of retrievals pertained to imaging exams older than 100 days. Furthermore, the authors also reported that CT studies were less frequently retrieved (16.9%) as compared to MR (44.5%) [8]. The image retrieval experience in this study [8] is at odds with the higher viewing frequency for CT reports than for MR in our study. This could be explained based on the fact that the PACS retrieval of images may be greater for more complex MR studies than for CT amongst the assessed radiologists in the earlier publication [8] as compared to the viewing frequency of radiology reports in EPIC assessed in our study. Indeed, CT is more commonly used for such acute clinical indications as compared to MR, which may explain why the viewing frequency is higher for CT than for MR. Furthermore, greater familiarity and understanding with CT as compared to MR amongst viewing physicians may also have been responsible for the higher viewing frequency for CT.
The primary implication of our study pertains to the understanding of viewing patterns of the referring physicians based on specific clinical indications, patient location (inpatient, outpatient, emergency department), imaging site (on-site versus off-site), imaging modality (CT versus MR), and body region (head, chest, abdomen). While it is not surprising that imaging tests performed in inpatients and emergency department had a higher viewing frequency, understanding viewing frequency based on specific clinical indications can help improve efficiency. For example, such information can help prioritize the interpretation of specific imaging exams and clinical indications over others with a lower viewing frequency. Preferential interpretation of such exams in busy imaging practices might help improve physician satisfaction and patient care. Radiology information system (RIS) or electronic medical records can be adapted to deliver the radiology reports of imaging exams, clinical indications, patient location and imaging sites with high viewing frequencies in a prompt, efficient, secure, and accessible manner. This is of importance if a higher viewing frequency of radiology reports takes the physician or their time away from actual patient interaction, examination, or care. In fact, Harvey et al. have argued in favor of a task-specific and a data-driven electronic medical record user interface to improve the efficiency and safety of healthcare [9]. Conversely, for radiology reports with low viewing frequencies, our study raises questions. One hypothesis is that less frequently viewed imaging study may be more likely to be normal and thus less “interesting” to view. Were such imaging examinations necessary? Did they help in patient care or outcome? What were the cost implications of such imaging examinations? Can algorithms including deep learning and/or natural language processing automate radiology exam lists for preferential interpretation of high viewing frequency exams? And ultimately, can such algorithm enable better integration and extraction of radiology reports from the medical records and avoid multiple clicks associated with radiology reports that garner multiple views within the electronic medical records?
Our study has limitations. Although our study has a large sample size, certain exam types such as chest MR had fewer cases compared to the other more common exam types. While most physicians affiliated with our hospital review the imaging results in the electronic medical records system used in our study, the outside-hospital physicians do not have access to our electronic medical records. Therefore, their viewing pattern was not captured in our study. However, this should not affect our results substantially since most CT and MR examinations performed at our institutions are referred by physicians affiliated to our hospital with access to our hospital electronic medical records system. Our study also did not capture the physicians’ intent for viewing radiology reports. While all included imaging examinations were performed for clinically indicated reasons, we could not capture the information regarding the exact reasons why physicians viewed some exams differently as compared to others. Likewise, we could not capture the information related to the proportion of actionable or positive findings and/or recommendations in radiology reports with higher and lower viewing frequencies.
The large variability and overlapping of clinical indications for different body regions and imaging modalities also challenged our study. Some imaging studies were performed for more than one clinical indication (for example, known case of renal cell carcinoma and chest pain as clinical indications for chest CT). For such cases, we focused on the first clinical indication. We did not evaluate the difference in the viewing frequency for initial and follow-up imaging examinations since such information were not available for exams performed prior to the implementation of the current electronic medical records system used in our study. Another limitation of our study pertains to the lack of information on the viewing frequency of the specific member types (residents, fellows, type of physicians (radiologists, non-radiology physicians including specialized versus primary care), nurses, or physician assistants).
In summary, imaging examinations for the acute clinical indications generate greater viewing frequency in the medical records compared to the non-acute indications. For similar exam types and clinical indications, the on-site and inpatient imaging exams have higher viewing frequency compared to those performed at the off-site imaging sites and/or at outpatient locations. Understanding viewing patterns of the referring physicians and the predictors (exam types, imaging site and the patient location at the time of imaging) of viewing frequencies can help guide interpretation priorities and communication strategies for imaging exams based on imaging modality, patient location, and clinical indications. This can help deliver efficient patient care.
Funding Information
One study co-author (MKK) received research grants from Siemens Healthineers and Riverain Inc. for unrelated research.
Compliance with Ethical Standards
This retrospective, quality assurance study was exempted from Institutional Review Board approval and used de-identified patient information.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maros ME, Wenz R, Förster A, Froelich MF, Groden C, Sommer WH, Schönberg SO, Henzler T, Wenz H. Objective comparison using guideline-based query of conventional radiological reports and structured reports. In Vivo. 2018;32:843–849. doi: 10.21873/invivo.11318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinto Dos Santos D, Hempel JM, Mildenberger P, Klöckner R, Persigehl T. Structured reporting in clinical routine. Rofo. 2019;191:33–39. doi: 10.1055/a-0636-3851. [DOI] [PubMed] [Google Scholar]
- 3.Mabotuwana T, Hombal V, Dalal S, Hall CS, Gunn M. Determining adherence to follow-up imaging recommendations. J Am Coll Radiol. 2018;15(3):422–428. doi: 10.1016/j.jacr.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 4.Meng X, Ganoe CH, Sieberg RT, Cheung YY, Hassanpour S. Assisting radiologists with reporting urgent findings to referring physicians: a machine learning approach to identify cases for prompt communication. J Biomed Inform. 2019;93:103169. doi: 10.1016/j.jbi.2019.103169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatti ZS, Brown RKJ, Kazerooni EA, Davenport MS. Communicating radiology test results: are our phone calls excessive, just right, or not enough? Acad Radiol. 2018;25:365–371. doi: 10.1016/j.acra.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Duncan KA, Drinkwater KJ, Dugar N, Howlett DC, Royal College of Radiologists’ Clinical Radiology Audit Committee Audit of radiology communication systems for critical, urgent, and unexpected significant findings. Clin Radiol. 2016;71:265–270. doi: 10.1016/j.crad.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 7.Larson PA, Berland LL, Griffith B, Kahn CE, Jr, Liebscher LA. Actionable findings and the role of IT support: report of the ACR Actionable Reporting Work Group. J Am Coll Radiol. 2014;11:552–558. doi: 10.1016/j.jacr.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 8.McEnery KW, Suitor CT, Thompson SK, et al. Enterprise utilization of “always on-line” diagnostic study archive. J Digit Imaging. 2002;15(Suppl 1):81–86. doi: 10.1007/s10278-002-5077-y. [DOI] [PubMed] [Google Scholar]
- 9.Harvey HB, Krishnaraj A, Alkasab TK. A software system to collect expert relevance ratings of medical record items for specific clinical tasks. JMIR Med Inform. 2014;2:e3. doi: 10.2196/medinform.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]