Abstract
Although advances in electronic image sharing have made continuity of patient care easier, currently, the majority of outside studies are received on CD. At our institution, there were 9 full-time employees (FTE) at three locations using three workflows to manually upload, schedule, and process studies to PACS. As the demand to view and store outside studies has grown, so has the processing turnaround time. To reduce turnaround time and the need for human intervention, we developed an automated workflow to import outside studies from a CD to our PACS and reconcile them with an internal accession number and exam code.
Keywords: EMR, Image exchange application, PACS, Outside CD, FTE, Auto-reconcile
Background
An “outside examination” is any study performed outside our radiology practice that needs to be imported and stored in the patient’s record. These studies are viewed as reference for a patient’s continuity of care, compared with studies performed at the receiving institution, or submitted for second-opinion review [1]. For continuity of care, it is ideal that outside studies are available promptly within PACS after import [2]. Many institutions import outside studies into PACS by uploading a disk directly into PACS or using an image-sharing application. Once the study is imported, some institutions choose to store them permanently with external demographics such as medical record number (MRN), accession number, and/or exam code. Permanently storing outside studies with external demographics does not properly tie studies into a patient’s record, may not give users confidence that the full imaging record can be viewed or searched, and may not locate archived studies for pre-fetch [3]. For these reasons, our institution chooses to reconcile outside studies with the patient’s internal demographics [4].
Three applications are required to reconcile the studies with internal identifiers and process them to PACS. Our electronic medical record (EMR) system has an integrated radiology information system (RIS), where orders are placed. The offers a dynamically generated URL that is configured within the EMR. The third application is the integration messaging engine that brokers Health Level Seven (HL7) messages between the two applications.
Our image-sharing software supports querying a DICOM modality worklist (MWL), which replaces the original institution’s patient demographics with our institution’s demographics taken from the outside study order, decreases the risk of error, and obviates the need for manual data entry [5]. Given the drawbacks of manually performing several steps in each of these applications, we developed an integrated automated workflow, which decreased the potential for error and made studies available promptly with internal study demographics and an accession number.
In the past, outside studies were processed using different image exchange applications at each of the three sites within our organization, and each required manual intervention upon import.
In this work, we describe a series of iterative improvements to the processing of submitted outside examinations that has culminated in a completely automated import workflow which also reconciles patient demographics to make outside exams available in PACS with any patient exams performed within our organization.
Methods
At our institution, the clinical team members managing processing studies to PACS are referred to as image processors, and as a whole are known as the Image Processing Department (IPD).
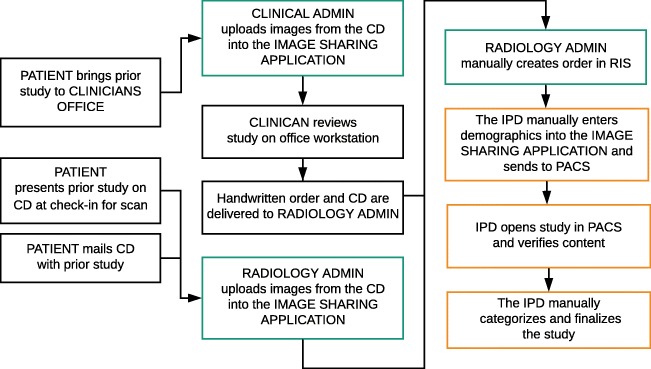
Original Approach to Importing Outside Examinations
Prior to the implementation of our current EMR and enterprise image-sharing application that utilizes a MWL, the workflow at the largest hospital within our health system comprised of departments delivering disks with handwritten orders to radiology reception. Radiology reception staff then would upload the disk to an image-sharing application and manually schedule the exam when not checking in patients for exams. Once a study was scheduled, an image processor would see the study on their RIS worklist, search for that patient in the image exchange application, manually update the patient demographics, and then, process the study to PACS. Once the study arrived in PACS, the image processor verified the study and completed the related order in the RIS. The order was completed with the date the study was performed and not the current date of day of import. Completing the study with the performed date allows the clinical team to sort the studies in the order they were acquired. There was a turnaround time of approximately 2 days from the time disk arrived in radiology reception to the study being available within PACS. Disks were then mailed back to the ordering office via interoffice mail, and often the ordering office would mail the disk to the patient. Our smaller sites did not utilize radiology reception to process outside examinations and disks were uploaded, scheduled, and processed to PACS by the local IPD (Fig. 1).
Fig 1.
Original workflow
Workflow Automation: Phase 1
A thin-client image exchange application that utilized MWL eliminated the need to manually enter the study demographics. The previous application was a thick client which required installation on each workstation. Prior to the implementation of the new image-sharing application, some clinicians would view studies in their office on the thick-client application without having them processed to PACS for storage. The newer image-sharing application thin-client architecture allows it to be launched via a URL from any workstation on our network. The URL link was added to our organization’s intranet for convenience.
The integration workflow for the new thin-client application was deployed over several phases. The first phase allowed clinicians’ offices at our largest hospital to upload the disk directly from their workstations. The users were requested to nominate individual studies they wanted to be processed to PACS. The clinical radiology department also required the clinician’s office to place an order in the RIS; this new workflow decreased the processing time from 48 h to an average of 24 h, and only required radiology reception to upload disks provided by patients being checked in for radiology appointments.
Workflow Automation: Phase 2
The IPD located at our largest hospital received and processed the majority of outside studies, but was unable to keep up with the rapid increase in requests. Implementation of a new EMR provided the opportunity for change and led to the implementation of a unified workflow. One technologist RIS worklist shared between the three image processing sites was built within the EMR, and an e-mail distribution list allowed the three IPDs to communicate.
Following an announcement notifying departments that they could upload their disks directly from their workstation without the need to place the order in RIS, the demand to have studies stored increased. This in turn increased the IPD’s turnaround time. The self-submit workflow was deemed to be cumbersome as it required several clicks to process each study.
Workflow Automation: Phase 3
To reduce the number of clicks, we turned on a feature in our image processing application which auto-processed studies selected by the uploading user to PACS. The study was uploaded in the context of the patient, and the studies that were auto-processed to PACS were pre-pended with an acronym we provided. “PIX” (Penn Image Exchange), followed by an auto-generated accession number created by our image processing application. This acronym allowed the IPD to identify the studies and reconcile the exception created by the studies arriving in the PACS without a corresponding order placed in the RIS.
To reconcile these studies, the staff (1) created an image processing queue in PACS, (2) reviewed the study details and created a corresponding order within the RIS, (3) merged the study to the order in PACS, and (4) completed the order within the RIS. This feature was made possible with the use of a dynamically generated URL and an outbound HL7 message enabled in the RIS. This facility reduced the number of clicks by the uploading office and reduced the waiting time for a study to arrive in PACS. The end-user was able to identify the study in PACS by description and modality.
Workflow Automation: Phase 4
Despite all these iterations, eventually, the IPDs again became unable to keep up with the influx of outside studies, and processing turnaround increased from an average of 24 h to 7 days. For the next phase, a generic code and study description was introduced. Upon upload, all studies were labeled with the same study description, with “OT” as the modality. While this generic code helped resolve the overwhelming number of studies, the IPDs had to reconcile; there were still delays in identifying a study because they all appeared to be the same and there was no way to uniquely identify them. In many cases, a physician had to open up multiple studies in the patient’s jacket to find the desired exam.
Workflow Automation: Phase 5
Our final iteration of the workflow was implemented in two stages. First, we created a lookup table to match outside study and modality descriptions with our internal study and modality descriptions. The lookup table was created using historic information. The logs within our image-sharing application provided knowledge of previously assigned institution codes that were matched with the outside study description and modality code. Secondly, once we were satisfied that the lookup table accurately mapped the procedure code and modality, we auto-finalized the study as a reference, ending it with the date the study was performed. With our current method, we auto-reconcile the study. We did not purchase or build new software for the purposes of auto-reconciliation as we discovered functionality existed in the tools already implemented.
When the upload of an outside exam is performed, the EMR creates a dynamically generated URL to launch the image exchange application within the patient context. On upload, studies are labeled with patient’s name, date of birth, gender, and our enterprise master patient identifier. After uploading a study, the image exchange application sends an outbound HL7 order message to the enterprise integration engine.
The integration engine creates an HL7 order message obtaining the procedure code using a lookup table. The lookup table contains a comprehensive list of historical outside study descriptions and the mapped procedure code. If a description does not exist in the table, it is then matched using logic based on the modality and keywords within the original description text. The order message is sent to the EMR’s inbound orders interface.
The EMR verifies the content of the order message, creates an internal accession number, and sends the Order Schedule Message to the integration engine. The EMR then auto-arrives the patient.
The integration engine modifies the structure of the Order Schedule Message to include the image exchange identifier, then sends this version of the message to the image exchange application and sends the original message to PACS. Once the image exchange application receives the modified order message, it labels the study with the accession number and procedure description; concurrently, the EMR sends an order arrived message to the interface engine.
The interface engine modifies the order arrived message to create an order end message. Finally, the exam end message triggers an auto-final message in the EMR, creating a canned report.
Our systems implement multiple Integrating the Healthcare Enterprise (IHE) profiles. The Portable Data for Imaging (PDI) profile helped address the compatibility challenge often faced when importing outside studies by establishing a protocol for media [6, 7]. Without this profile, our rate of failure would be significantly higher. We also adhere to the Import Reconciliation Workflow (IRWF) and the Scheduled Workflow (SWF) profiles [6, 8]. The IRWF was designed to ensure imported data is reliable. One of the benefits put in place with this workflow is the focus on data reconciliation to reduce the potential for error, which was the driver for our current process. With the SWF using HL7 to place radiology orders, help prevent the duplication of orders, and provide consistency, this is something we heavily relied on while coding our messages in the interface [6, 9] (Fig. 2).
Fig 2.
Integrated workflow
With our automated workflow, all studies across the health system are originally uploaded as reference. In order to obtain a second opinion, an order must be placed by a clinician.
We ask that orders for second-opinion interpretation be placed after the study has been uploaded and an image of the original outside report has been stored into our EMR. Once the order is placed, it arrives on an outside study MWL in the RIS, which is now solely managed by the IPD at our largest hospital. Prior to processing a second opinion, the image processing coordinator reviews the patient’s jacket to ensure the same study had not been performed within 6 months. If that is found to be the case, the ordering clinician is notified that the study will be stored as a reference. Exceptions are made if the ordering clinician presents extenuating circumstances as to why a second interpretation is needed; otherwise, an addendum will be made to the report if appropriate or the clinician may opt to order another scan if they deem necessary.
If the patient has not had the same study performed within 6 months, the image processor associates a scanned version of the original report to the second-opinion order within the EMR. Then, the reference images within the PACS are updated with the second-opinion order’s accession number.
Results
We were able to reduce the number of full-time FTEs from 9 to 3, allowing images to be processed and released to PACS in an average of 1 min. Upon upload, the outside study immediately arrives in PACS with our institutional accession number and exam code.
With our old methodology, approximately 48,000 outside studies were uploaded a year. These uploads were performed across three hospitals and several remote community radiology sites. While the majority of studies were uploaded at our largest hospital, we are not able to track the exact number of uploads since during this time, our other sites used various applications to upload and reconcile the outside studies.
In 2013, we began utilizing our thin-client image-sharing application which eliminated the need to manually enter the study demographics. In 2014, after a full year of the phase 2 workflow with departments uploading exams directly from their workstations, the number of studies uploaded rose to 125,007.
Over the next 2 years, we underwent the remaining aforementioned iterations before arriving at the current (phase 5) workflow. Three stand out as having the most significant impact on the number of studies we imported: (1) having the IPDs create the reference orders as opposed to the departments, (2) having studies directly processed to PACS with an auto-generated accession number, and (3) automatically reconciling external and internal study descriptions to further automate reconciliation to internal identifiers. We had a total of 159,911 exams uploaded in 2015, 190,786 uploaded in 2016 and 199,017 in 2017.
The last phase of automation was initiated in 2017, and after the cardiology department began utilizing our image sharing upload application, the total number of disks uploaded rose to 206,804 in 2018.
Of these studies uploaded an average of 13,000 are submitted for radiology second opinion each year (Fig. 3).
Fig. 3.
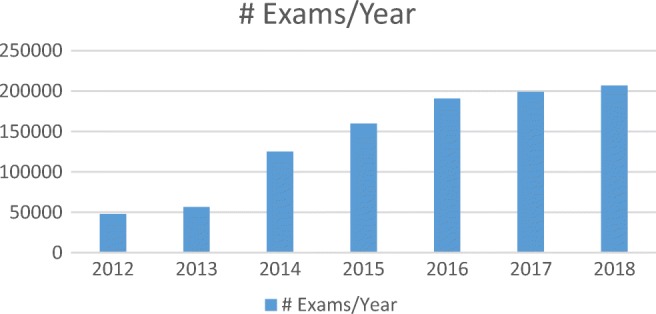
Exam by year
Discussion
Initially, we attempted to decrease turnaround time by sharing the Image Processing Department’s task with the ordering departments; however, the increase in demand increased the manual efforts on both parties and eventually increased the turnaround time.
Next, we attempted to automatically process the studies to PACS in the context of the patient and then, reconcile the study with our internal accession number. Although this workflow made studies readily available in PACS within the patient’s folder, study reconciliation was a time-consuming process. We did not consider storing studies with the external procedure description and accession number and option because we could not readily identify all of them, and it could affect the ability to properly retrieve archived studies based on our PACS pre-fetch rules.
We also attempted to solve our issue by creating a generic procedure code and automatically assigning it to each outside study. This method increased the effort of the IPDs and the clinicians to identify the correct study in PACS.
The current workflow auto-reconciles the uploaded studies and processes them to PACS with an internal procedure code and accession numbers that are in sequence with studies acquired internally, which reduces turnaround time as well as the number of FTEs required to process studies.
Occasionally, we receive studies without a description. Such studies cannot be matched to an internal study code, and a generic order is created, but the study is not released to PACS. The IPD reviews studies that fall into this category from a worklist created in our EMR, locates them in our image exchange application, and manually processes them to PACS. The IPD also manually processes studies that fail to process to PACS due to the format of the study or an incomplete disk upload.
Industries are making a continuous effort to move away from disk [10]. In healthcare, electronic image transfer helps provide the best continuity of care, allowing clinical teams to prep before a patient’s arrival, saving useful time, especially in instances of stroke, aortic rescue, and other emergent cases [11].
While we worked to perfect the workflow of uploading outside examinations via disk, we also recognize the need for seamless electronic image sharing in order to provide optimal patient care. One of the reasons we did not want to purchase or create new software is because we realize this is a temporary solution, as our ultimate goal is to remove our reliance on disk media altogether.
Recently, policy changes were proposed to make data easily and safely accessible to patients online by the Center for Medicare and Medicaid Services (CMS) and the Office of the National Coordinator for Health IT (ONC) [8]. With access to their images and other health-related data, patients can efficiently share images with the physician and facility of their choice. #DitchTheDisk is a movement focused eliminated disk to help a providing facility obtain a patient’s full medical history while saving both time and money [9, 11].
The RSNA Image Share Validation—the Sequoia Project—was established to help enforce standards in electronic image sharing for reliable and efficient access to outside studies. Through this program, electronic image exchange application vendors are invited to participate in a validation process of the established IHE Cross-Enterprise Document Sharing (XDS) family of profiles. The program supports #DitchTheDisk and is focused on eliminating disks while finding other means to help a care facility obtain a patient’s full medical history and saving both time and money [7]. The American College of Radiology (ACR) recognizes that disks remain the most common method to upload outside studies and collaborates with RSNA to help promote the movement [12, 13].
The IHE workflow Import and Display of External Priors (IDEP), which is currently in development, expands upon the complications of manually importing outside studies which need to be readily available for comparison. The goal of this proposed workflow intends to resolve the issue by using tools that already exist, keeping it as simple as possible [14].
Conclusion
We developed an automated workflow to upload outside studies from CDs, which freed up 6 FTEs for other roles in the department and enabled near real-time availability of outside examinations despite quadrupling the increase in the volume of cases submitted annually. Studies are now viewable in PACS with an institutional accession number and exam code within a matter of minutes.
Acknowledgments
The authors would like to thank Carolyn Cicilia from the Applications Integration Team, Dr. Neil Malhotra from the Department of Neurosurgery, Ann Costello, the Director of Clinical Radiology, Kristen Martin from the Clinical Imaging Management Team, and the Image Processing Departments. The authors would also like to acknowledge the Penn Medicine Radiology PACS Team, the PennChart Radiant Team, and Clinical Imaging IS Leadership with special thanks for their help and efforts.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kuzmak PM, Dayhoff RE, Gavrilov S, Cebelinski G, Shovestul ML, Casertano A. Streamlining importation of outside prior DICOM studies into an imaging system. J Digit Imaging. 2012 Feb;25(1):70-7. doi: 10.1007/s10278-011-9406-x. PubMed PMID: 21809172; PubMed Central PMCID: PMC3264724. [DOI] [PMC free article] [PubMed]
- 2.Sodickson A, Opraseuth J, Ledbetter S. Outside imaging in emergency department transfer patients: CD import reduces rates of subsequent imaging utilization. Radiology. 2011 Aug;260(2):408-13. doi: 10.1148/radiol.11101956. Epub 2011 Apr 19. [DOI] [PubMed]
- 3.Hagiwara H, Nemoto A, Inoue T. Burden on university hospitals of handling portable data for imaging (PDI) media. Appl Clin Inform. 2014 Jan 15;5(1):46-57. doi: 10.4338/ACI-2013-07-RA-0052. eCollection 2014. PubMed PMID: 24734123; PubMed Central PMCID: PMC3974247. [DOI] [PMC free article] [PubMed]
- 4.Erickson BJ. Experience with importation of electronic images into the medical record from physical media. J Digit Imaging. 2011 Aug;24(4):694-9. doi: 10.1007/s10278-011-9364-3. PubMed PMID: 21286776; PubMed Central PMCID: PMC3138924. [DOI] [PMC free article] [PubMed]
- 5.Lu MT, Tellis WM, Fidelman N, Qayyum A, Avrin DE. Reducing the rate of repeat imaging: import of outside images to PACS. AJR Am J Roentgenol. 2012;198(3):628–634. doi: 10.2214/AJR.11.6890. [DOI] [PubMed] [Google Scholar]
- 6.Integrating the Healthcare Enterprise (IHE), 2019 Retrieved from https://www.ihe.net/ihe_domains/radiology/. Accessed Sept 2019
- 7.Integrating the Healthcare Enterprise. Portable Data for Imaging (PDI), 2018, May. Retrieved from https://wiki.ihe.net/index.php/Portable_Data_for_Imaging. Accessed Sept 2019
- 8.Integrating the Healthcare Enterprise. Import Reconciliation Workflow (IRWF), 2018, May. Retrieved from https://wiki.ihe.net/index.php/Import_Reconciliation_Workflow. Accessed Sept 2019
- 9.Integrating the Healthcare Enterprise Scheduled Workflow (SWF), 2018, May. Retrieved from https://wiki.ihe.net/index.php/Scheduled_Workflow. Accessed Sept 2019
- 10.Flanders AE. Medical image and data sharing: are we there yet? Radiographics 2009 Sep-Oct;29(5):1247-51. doi: 10.1148/rg.295095151. Review. [DOI] [PubMed]
- 11.HealthIT.gov, 2019, February. Retrieved from https://www.healthit.gov/topic/about-onc. Accessed Sept 2019
- 12.Sequoia Project. 2019 Retrieved from https://sequoiaproject.org/rsna/. Accessed Sept 2019
- 13.How We Can #DitchTheDisk & Share Images Electronically, 2019 July. Retrieved from https://carequality.org/how-we-can-ditchthedisk-share-images-electronically/. Accessed Sept 2019
- 14.Integrating the Healthcare Enterprise. Proposed Workitem: Import and Display of External Priors (IDEP), 2018 September Retrieved from https://wiki.ihe.net/index.php/Import_and_Display_of_External_Priors-_Proposal. Accessed Sept 2019