On December 31, 2019, a cluster of cases of severe respiratory syndrome was reported in patients with connections to a seafood market in Wuhan, Hubei Province, China.1 Within 1 week, Chinese health authorities were able to link these cases to a novel, enveloped RNA coronavirus, SARS-CoV-2, now commonly known to cause COVID-19.2 By February 14, 2020, over 66,000 cases of COVID-19 were reported in China.3 On January 19, a 35-year-old man returning from Wuhan to his home in Snohomish County, Washington, presented to urgent care with several days of cough and fever and ultimately tested positive for COVID-19, becoming the first case in the United States. The first COVID-related death occurred 4 weeks later, associated with a separate site, a long-term care facility in Kirkland, Washington, which rapidly became a cluster of 30 fatal cases as of March 16th. At the writing of this article, March 17th, there are 1012 confirmed cases in the state of Washington, with 52 deaths, primarily in King County. Evergreen Health, the major medical center in Kirkland, has recently declared that they have no remaining critical care capacity.
COVID-19 is now a global pandemic that is advancing at a pace that—without immediate attenuation—will rapidly overtake medical infrastructures. This has been painfully evinced in regions of Italy and Iran. For the United States, public health experts worry that this outbreak will continue to escalate, at least in the short term.4 With this backdrop, cancer care remains an essential clinical need, for which timely radiation therapy is a cornerstone modality. Concurrently, patients with cancer may have a 5-fold relative risk for severe manifestations (eg, requirement for invasive ventilation) and death, compared with the general population.5 In this article, we report our experience with delivering high-quality, patient-centered radiation therapy at an epicenter of the COVID-19 pandemic within the United States. Our aim is to describe policies and procedures that we have found helpful for our own patient population, staff, and community.
The Department of Radiation Oncology at the University of Washington (UW) comprises 7 sites of practice in both hospital-based and outpatient, including community, settings across the Seattle–Puget Sound area. On average, more than 220 patients are treated each day in our department, with cases ranging in complexity from whole-breast radiation therapy to immunocompromised, pediatric patients requiring anesthesia. Immediately after the public announcement of the presence of COVID-19 in our community, our department serially instituted policies and procedures that synthesized national, state, and institution-specific infection control guidance within a radiation oncology–appropriate model. Three overlapping goals to mitigate transmission while continuing to deliver high-quality treatments were identified: social distancing, preservation of the pool of health care providers, and conservation of personal protection equipment.
While pharmacologic interventions remain on the horizon, social distancing is the most effective known tool in curtailing the spread of this infection. Using an extended susceptible, latent, infectious, and removed constitutive model fitted to empirical data from the outbreak in China, biostatisticians at the Broad Institute and Harvard University have shown that social distancing methods, ranging in aggressiveness from a city-wide lockdown to centralized quarantine, were effective in dampening the reproductive number of COVID-19, ultimately controlling the outbreak in Wuhan.6 In our application, employees who can perform duties remotely (eg, research coordinators, research residents, administrative staff, and some medical physics staff) are instructed to work from home. The minimum level of staffing to maintain safe treatments at each practice site is deployed based on patient volume and complexity. Meetings have been limited to 5 persons or fewer, with at least 6 feet of distance between any 2 individuals. Nearly all tumor boards have transitioned to virtual conferencing, with the exception of small meetings with 5 persons or fewer and 1 tumor board in which in-person coordination was considered indispensable to patient care. In this regard, our institution has expanded teleconferencing capacity to be able to support up to 50,000 simultaneous online conferences. Crucially, during the relatively short roll-out of distancing policies, a relatively user-friendly teleconferencing solution was promulgated. This empowered any single user to initiate an individualized, Health Insurance Portability and Accountability Act–compliant teleconference session on demand.
To reduce exposure where possible, new patient consultations for treatment of indolent or benign conditions are deferred at the discretion of the radiation oncologist. Routine follow-ups are offered to patients via telephone or are postponed. At an institutional level, providers are being quickly certified for telemedicine, with proposals to temporarily relax billing standards.
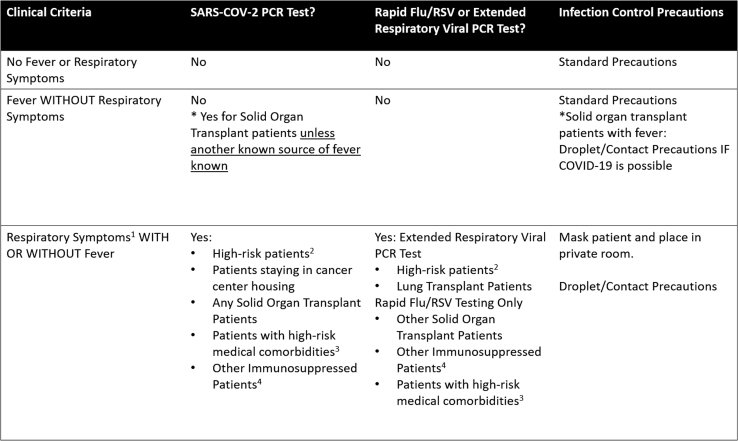
In terms of patient safety, the department has taken a number of early actions to limit the spread of COVID-19 to and from patients while still allowing treatments to continue. A site visit to our clinics by our institution’s infection control team was highly valuable, and this experience directly led to specific interventions that bolstered the continued treatment of patients while mitigating transmission risk. This session incorporated end-to-end patient tracing to identify opportunities to mitigate patient-to-patient, patient-to-staff, and staff-to-staff transmission. Screening of patients and staff for upper respiratory symptoms (fever, cough, rhinorrhea) is crucial for infection control. At many of our sites, there are multiple ports of entry into the clinic. As such, all patients are screened twice: once upon entering the building and again upon entering the department. Patients who are positive on screening for symptoms are asked to wear a mask, are placed in a private room where they are evaluated by a provider over telephone, and are appropriately triaged. Details of our testing algorithm specific to our patient population can be found in Figure 1. All patients are asked to either thoroughly wash their hands or use effective hand sanitizers upon entering and leaving an examination or treatment room.
Figure 1.
COVID-19 and influenza testing decision tree for the outpatient radiation therapy population. 1Respiratory symptoms: cough, shortness of breath, wheezing or chest tightness, sore throat. Consider excluding symptoms attributable to allergies. 2High-risk patients: all transplant and immunotherapy, all hematologic malignancy, all active chemotherapy, neutropenia (absolute neutrophil count < 500). 3Medical comorbidities: age >60 years, diabetes, chronic kidney dysfunction, pregnancy, lung cancer, chronic lung disease, cirrhosis. 4Other immunosuppressed: biologic agents for immunosuppression, steroids >0.5 mg/kg/d prednisone equivalent, congenital or acquired immunodeficiency.
Fortunately, although all radiation therapy patients are screened, few have required testing, and none have tested positive thus far. Because radiation therapy is often a necessary part of lifesaving cancer care, we anticipate treating patients with presumed or proven COVID-19. For the standard treatment, our institution has recommended droplet precautions (surgical mask, goggles, gloves, gown) and the use of a private waiting room. These patients will be treated at the end of the day, in a particular vault that is extensively decontaminated afterward. For treatments with anesthesia, the risk of aerosol transmission is high, and airborne precautions are required (N-95 mask, face shield, gloves, gown, and a personal respirator in some instances). At our main facility, a negative-pressure vault is available for treating patients requiring airborne precautions.
The rate of consumption of personal protective equipment (PPE) has been high and is expected to greatly increase in our facilities. Before implementing stringent conservation protocols, the University of Washington Medical Center exhausted 3 months of PPE supply in 3 days. To conserve PPE, we have instituted policies limiting the number of providers required to come into direct contact with patients with suspected or confirmed COVID-19.
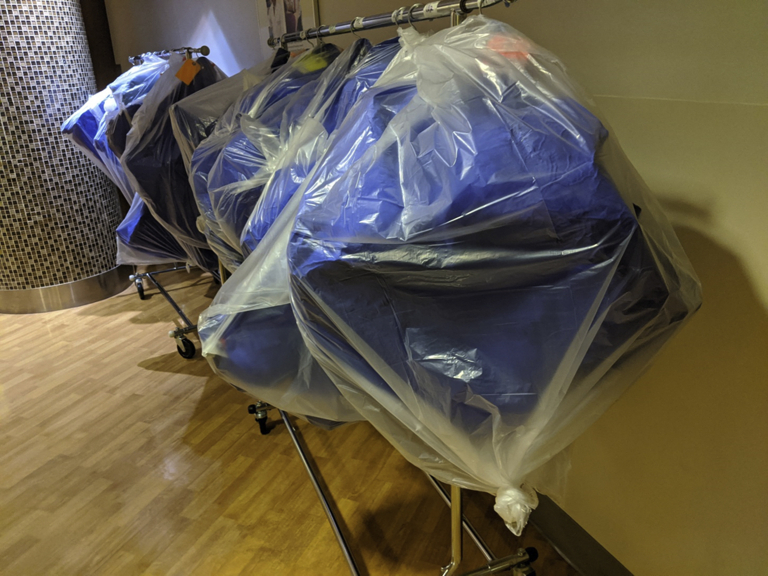
Recent data suggest that COVID-19 remains viable on plastic surfaces for up to 72 hours.7 Radiation treatment devices thus serve as a potential transmission nidus. To mitigate this risk, immobilization devices such as VakLok bags are individually disinfected and wrapped in a plastic bag that is sealed and changed after each daily use (Fig 2). Other hardware that comes into direct contact with patients, such as treatment tables and positioning aides, are extensively disinfected between uses. For respiratory motion management, we have developed a protocol for the use of the Active Breathing Controller (Elekta Inc), which is used at several centers. Some elements of this device cannot be decontaminated, so the device will not be used in patients with suspected or confirmed COVID-19 and abdominal compression will be used instead.
Figure 2.
Patient immobilization devices (VakLok molds) are individually sealed in plastic bags that are changed daily after treatment.
Despite having no COVID-19–positive patients undergoing radiation therapy as of yet at our centers, health care provider depletion is becoming a pressing issue. Within our department, at least 4 physicians were required to undergo testing after a self-administered online survey for low-grade symptoms. Although they were all ultimately found to be uninfected, this process removed them from patient care for at least 48 hours. These disruptions can be expected to continue and will likely increase.
In these trying times, the training of medical and physics residents remains fundamental to our department’s mission. Balancing training and the principles of social distancing, provider preservation, and PPE conservation is a delicate task. Although immersion and availability have been beneficial tenets of training, they are subsumed by the need to mitigate transmission. Residents on a research block or on days without patient visits are instructed to work from home. All lectures and didactic activities have moved to videoconference. Most difficult of all in light of our collective appreciation of time with patients, minimization of redundant encounters requiring both residents and attendings to see the patient is encouraged. With specific focus on trainees, there are valuable lessons from prior viral epidemics. After the 2003 SARS epidemic in Toronto, trainees who were quarantined reported high levels of psychological distress, particularly those who were not contacted for wellness checks during their isolation.8 Effective rather than effusive communication from hospital leadership was found to facilitate coping. Coherent communication is uniquely important to trainees, who often straddle all sites of practice within a radiation oncology program. Empowering trainees to stay home if they have symptoms should be of utmost concern; during the 2009 H1N1 outbreak, 67% of residents with influenza-like illness still reported to work at a US training hospital, despite perceiving the risk of H1N1 transmission to be high.9 It is imperative to have clear messaging from departmental leadership regarding expectations while simultaneously allaying concerns of any detriment to professional development as a result of missing work.
The potential disruptions to training and professional development are understandably a source of anxiety for trainees. At UW, we attempt to allay some of these concerns by regular, quarterly meetings as well as one-on-one meetings between the residents and the chair. Our department also recognizes that many of our residents and faculty have young children and face tremendous challenges as schools and childcare services have begun shutting down in the Seattle area. Furthermore, some have partners who are internal medicine trainees and have already been asked to directly care for COVID-19 patients or to cover clinics so others may care for COVID-19 patients as the health care provider pool becomes depleted. Many trainees have neither the resources to hire personal back-up care nor the social network to summon pro bono care. As a response, we have initiated a grassroots effort to pool childcare resources within the UW medical community. Many university and medical students on academic furlough due to the pandemic have volunteered to serve as childcare resources specifically for health care providers.
We intend these experiences to be descriptive rather than prescriptive and strongly encourage everyone to follow guidance from The Centers for Disease Control and the State Department of Health, as well as guidelines from their home institution, hospital, or clinic. This pandemic, along with our institutions’ response to it, are dynamic in nature. Thus, a nimble set of solutions, tailored to the specific needs of any single institution’s patient population and those of its health care community, is required. The strengths of the field of radiation oncology remain incandescent in the face of this approaching storm: team-based care, evidence-based practice, and a community of talented, dedicated, and compassionate professionals. Despite the unprecedented challenge, we intend to come together to deliver the best possible care for the patients who depend on us. We must also remember to support as well as to lean on one another during this historic trial.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
Research data are stored in an institutional repository and will be shared upon request to the corresponding author.
References
- 1.World Health Organization . WHO; 2020. Pneumonia of unknown cause – China.https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ Available at: [Google Scholar]
- 2.Guan W, Ni Zy, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China [e-pub ahead of print]. N Engl J Med.https://doi.org/10.1056/NEJMoa2002032. Accessed March 17, 2020. [DOI] [PMC free article] [PubMed]
- 3.Johns Hopkins University Center for Systems Science and Engineering (CSSE) Wuhan coronavirus (2019-nCoV) global cases. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Available at:
- 4.Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the uncharted [e-pub ahead of print]. N Engl J Medhttps://doi.org/10.1056/NEJMe2002387. Accessed March 17, 2020. [DOI] [PMC free article] [PubMed]
- 5.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin X. 2020. Analysis of 25,000 Lab-Confirmed COVID-19 Cases in Wuhan: Epidemiological Characteristics and Non-Pharmaceutical Intervention Effects. Available at: https://docs.google.com/file/d/14tGJF9tdv4osPhY1-fswLcSlWZJ9zx45/edit?usp=docslist_api&filetype=mspresentation. Accessed March 17, 2020. [Google Scholar]
- 7.van Doremalen N, Morris DH, Holbrook MG, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1 [e-pub ahead of print]. N Engl J Med.https://doi.org/10.1056/NEJMc2004973. Accessed March 17, 2020. [DOI] [PMC free article] [PubMed]
- 8.Rambaldini G, Wilson K, Rath D, et al. The Impact of Severe Acute Respiratory Syndrome on medical house staff: A qualitative study [e-pub ahead of print]. J Gen Intern Med.https://doi.org/10.1111/j.1525-1497.2005.0099.x. Accessed March 17, 2020. [DOI] [PMC free article] [PubMed]
- 9.May L., Katz R., Johnston L., Sanza M., Petinaux B. Assessing physicians’ in training attitudes and behaviors during the 2009 H1N1 influenza season: A cross-sectional survey of medical students and residents in an urban academic setting. Influenza Other Respi Viruses. 2010;4:267–275. doi: 10.1111/j.1750-2659.2010.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]