Dear Editor,
The unprecedented outbreak of the novel coronavirus (nCoV-19 or SARS-CoV-2), that emerged in Wuhan, China, in 2019 and spread all over Europe and the world, has forced French hospitals to reorganise and admit a large number of critically ill patients in a short period of time. Data from China reported up to 6% of patients overall [1] and 71% with severe COVID-19 [2] requiring mechanical ventilation. Median length of hospital stay was 12 days [1], but patients with severe disease may remain in intensive care units (ICUs) for 2 to 3 weeks, and survival time for non-survivors has been reported to be 1 to 2 weeks [2].
On March 23rd, 2020 in France, 2082 of 19,856 confirmed cases of COVID-19 needed intensive care [3]. Reports from Italy warned of the risk of ICU bed shortage [4]. New cases and especially severe ones are increasing exponentially following a similar evolution in Italy [5], with a risk of ICU saturation in many French regions. There is a growing need for ventilator weaning units that could help ICUs discharge ventilator-dependent patients with stable disease and no other organ failure but respiratory or neurological features. According to other physical medicine and rehabilitation societies worldwide, early evaluation and rehabilitation for these patients is mandatory [6], [7].
Here, we describe our organisation of this type of unit and our first feedback from its functioning, based on the experience in a French tertiary care university hospital. This weaning unit was set ex nihilo within 7 days and was ready for the first 4 patients by March 26th, 2020.
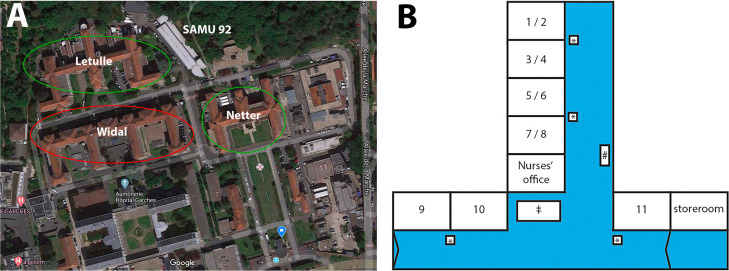
The pavilion architecture of our hospital allowed us to secure 2 buildings for COVID-19–free patients (from the conventional ICU and infectious diseases and neurorehabilitation units) and isolate one building for COVID-19 patients (Fig. 1 A) by March 13th, 2020. Two medical units are located on the first and second floors of this building, with a dedicated 28-bed ICU on the third floor (increased to 32 by April 10th). In the initial physical and rehabilitation medicine unit (first floor), 11 beds in 7 rooms were dedicated to post-ICU ventilator-dependent COVID-19 patients (Fig. 1B).
Fig. 1.
Architecture, topography and organisation of Raymond-Poincaré University Hospital and the newly established COVID-19 ventilator-weaning unit. A. Aerial view of Raymond-Poincaré Hospital showing the 3 main buildings, Netter, Letulle and Widal (screenshot from GoogleMaps, Mountain View, CA, USA). COVID-19–free buildings are circled in green, COVID-19–positive building is in red. B. Organisation of the weaning unit, with 4 double rooms and 3 single rooms. *: carts equipped with sanitary protection for COVID-19; #: location of the emergency cart; ‡: a cleaning place for reusable equipment such as protection goggles.
Each bed is equipped with a level-3 life support ventilator Astral 150® (ResMed, San Diego, CA, USA) and non-invasive continuous monitoring (oxygen saturation, heart rate, non-invasive blood pressure). Each ventilator has flow meters for perfusion and a nutrition pump for enteral feeding. We could not implement a full monitoring system in the nurses’ office, but ventilator alarms are repeated by using “babyphones” or with an independent remote alarm system. Finally, each room is equipped with a lift and harness for transfers (Fig. 2 ).
Fig. 2.

Picture of a double room fully equipped for ventilator-dependent patients within the rehabilitation department. 1: level-3 life support ventilator; 2: non-invasive continuous monitoring; 3: flow meters for perfusion; 4: nutrition pump for enteral feeding; 5: lift and harness for bed-to-chair transfers.
Medical staff consists of 3 senior and 2 junior physicians with ICU or ventilator training and expertise. Day shifts are organised so that 2 senior physicians and 1 resident are present each day. Night shifts include 3 additional senior physicians to ensure secured rotations. Paramedic staff consists of 3 rotations of 3 nurses and 3 caregivers per 24 hr. Nurses were recruited from ex-ICU nurses or individuals with experience in post-ICU care. They all underwent a full-day teaching program with the medical staff and a ventilation-specialised nurse before the opening of the unit. Finally, 2 physiotherapists are dedicated to motor and cardiorespiratory rehabilitation of patients. This rehabilitation staff is also assisted by part-time occupational and speech therapists to help with communication and early oral feeding of tracheotomised patients as well as 2 part-time psychologists.
Before opening the unit, we carefully defined criteria for patients to be admitted safely in this unit. Ventilator-dependent patients have to be tracheotomised at least 24 hrs before admittance but can be dependent 24/7 if the last prone decubitus session was ≥ 72 hrs and have PaO2/FiO2 ratio (FiO2 ≤ 45%) > 200 for at least 2 days. They have to be weaned from vasopressors for 48 hrs and have no other organ failure needing invasive support. Finally, before ICU discharge, patients are switched from an ICU ventilator to the weaning unit ventilator with clinical assessment and arterial blood gas analysis after 2 hrs.
Hence, between March 26th and April 9th, 10 patients (8 men, mean [SD] age 62 [14.9] years) were admitted in the unit: 2 were discharged to a conventional medical unit then home, and 2 were transferred back to the ICU because of secondary pulmonary critical exacerbation. Mean ICU length of stay before admission in the weaning unit was 11 (4.0) days (vs. 3 weeks in the Chinese series [2]). Mean length of stay in our unit was 6 (4.6) days. For successfully weaned patients, mean total duration of mechanical ventilation was 13 (6.3) days (range 8 to 22 days). Six patients had a history of hypertension and none were active or previous smokers. Three patients had post-ICU–acquired weakness, progressively regressive, and 1 had initial and transient brachiofacial paresis (intracerebral hemorrhage ruled out, but to date, MRI could not be performed). All had moderate to severely low serum albumin levels (< 25 g/L). All had mild to moderate post-ICU delirium, and 5 had persistent anxiety or post-traumatic stress.
By the date of final acceptance of this article (April 11), we counted 86,740 active cases of COVID-19 in France; 7004 patients were considered to have serious or critical disease and were in an ICU. This indicates an exponential increase of severe cases and confirms the past hypotheses of ICU-bed saturation (< 6000 before the epidemic). The survivors (approximately 60%) will need invasive ventilation for 3 weeks and early rehabilitation support. Our preliminary feedback on our set-up attests to the appropriateness of our approach.
The goal of the specific organisation we describe is to allow for early patient discharge from the ICU and increase ICU admission capacity over time during the COVID-19 crisis. It also allows for a physical medicine and rehabilitation holistic evaluation of post-critical COVID-19 patients. Hence, our first feedback strengthens the idea that our unit constitutes a possible intermediary stage between ICU and either home discharge or inward rehabilitation for patients with pulmonary, nutritional, neurological and psychological COVID-19–related and/or post-ICU impairments.
This set-up was made possible at our hospital in such short notice because of 3 main advantages:
-
•
the pavilion architecture and proximity of the ICU and conventional medical units within the same building;
-
•
the past and present experience of the post-ICU neuro-rehabilitation unit at our institution (Service de Rééducation Post-Réanimation);
-
•
the multidisciplinary medical team associating physiatrists, pulmonologists, physiologists and nurses with ICU and ventilator-weaning training.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
The authors thank ADEP assistance, Asten, ASV santé, LVL, SOS Oxygène and Resmed France for help in providing the necessary equipment to create this weaning unit.
References
- 1.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical caracteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [NEJMoa2002032] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. [S2213260020300795] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haut Conseil de la Santé Publique . 2020. Avis relatif aux recommandations thérapeutiques dans la prise en charge du COVID-19 (complémentaire à l’avis du 5 mars 2020) p. 23. https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=785. [Google Scholar]
- 4.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 doi: 10.1016/S0140-6736(20)30627-9. [S0140673620306279] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinross P., Suetens C., Gomes Dias J., Alexakis L., Wijermans A., Colzani E. Rapidly increasing cumulative incidence of coronavirus disease (COVID-19) in the European Union/European Economic Area and the United Kingdom, 1st January to 15th March 2020. Euro Surveill. 2020 doi: 10.2807/1560-7917. [ES.2020.25.11.2000285] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boldrini P., Bernetti A., Fiore P. Impact of COVID-19 outbreak on rehabilitation services and physical and rehabilitation medicine (PRM) physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER) Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06256-5. [DOI] [PubMed] [Google Scholar]
- 7.Negrini S., Ferriero G., Kiekens C., Boldrini P. Facing in real time the challenge of the COVID-19 epidemic for rehabilitation. Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06286-3. [DOI] [PubMed] [Google Scholar]