Abstract
Background
Dementia with Lewy bodies (DLB) is more prevalent in men than in women. In addition, post-mortem studies found sex differences in underlying pathology. It remains unclear whether these differences are also present antemortem in in vivo biomarkers, and whether sex differences translate to variability in clinical manifestation. The objective of this study was to evaluate sex differences in cerebrospinal fluid (CSF) biomarker concentrations (i.e., alpha-synuclein (α-syn), amyloid β1-42 (Aβ42), total tau (Tau), phosphorylated tau at threonine 181 (pTau)) and clinical characteristics in DLB.
Methods
We included 223 DLB patients from the Amsterdam Dementia Cohort, of which 39 were women (17%, age 70 ± 6, MMSE 21 ± 6) and 184 men (83%, age 68 ± 7, MMSE 23 ± 4). Sex differences in CSF biomarker concentrations (i.e., α-syn, Aβ42, Tau, and pTau) were evaluated using age-corrected general linear models (GLM). In addition, we analyzed sex differences in core clinical features (i.e., visual hallucinations, parkinsonism, cognitive fluctuations, and REM sleep behavior disorder (RBD) and cognitive test scores using age- and education-adjusted GLM.
Results
Women had lower CSF α-syn levels (F 1429 ± 164 vs M 1831 ± 60, p = 0.02) and CSF Aβ42 levels (F 712 ± 39 vs M 821 ± 18, p = 0.01) compared to men. There were no sex differences for (p) Tau concentrations (p > 0.05). Clinically, women were older, had a shorter duration of complaints (F 2 ± 1 vs M 4 ± 3, p < 0.001), more frequent hallucinations (58% vs 38%, p = 0.02), and scored lower on MMSE and a fluency task (MMSE, p = 0.02; animal fluency, p = 0.006). Men and women did not differ on fluctuations, RBD, parkinsonism, or other cognitive tests.
Conclusions
Women had lower Aβ42 and α-syn levels than men, alongside a shorter duration of complaints. Moreover, at the time of diagnosis, women had lower cognitive test scores and more frequent hallucinations. Based on our findings, one could hypothesize that women have a more aggressive disease course in DLB compared to men. Future research should investigate whether women and men with DLB might benefit from sex-specific treatment strategies.
Keywords: Dementia with Lewy bodies, Sex differences, Cerebrospinal fluid biomarkers
Background
Dementia with Lewy bodies (DLB) is clinically characterized by cognitive decline, visual hallucinations, parkinsonism, cognitive fluctuations, and rapid eye movement (REM) sleep behavior disorder (RBD) [1]. Pathologically, DLB is characterized by the presence of cortical Lewy bodies, i.e., neuronal inclusions of alpha-synuclein proteins [2], frequently combined with Alzheimer’s disease (AD) pathology, i.e., amyloid plaques and neurofibrillary tangles (NFT) [3]. Most studies report a higher prevalence of DLB in men than in women [4–7], although a few report the opposite [8, 9]. In addition to the skewed distribution, there is evidence of differences in the underlying pathology between women and men with DLB. Post-mortem examinations showed that men were more likely to die from “pure” DLB pathology than women, and women were more likely to have mixed pathology (DLB + AD) [10, 11]. This is clinically relevant, as mixed pathology is linked to a more severe disease manifestation, with more cognitive disturbances, more frequent hallucinations, and shorter survival [12, 13]. Although post-mortem studies are important, a major drawback is that they reflect end-stage disease. In contrast, cerebrospinal fluid (CSF) biomarkers enable in vivo studies in ongoing pathological processes. Previous CSF biomarker studies in AD have shown sex differences in CSF (p) Tau concentrations, suggesting a higher antemortem neurofibrillary tangle (NFT) load in women with AD [14–16]. Literature regarding sex differences in CSF biomarkers in DLB, however, is still limited. One small study reported lower levels of CSF alpha-synuclein in DLB women compared to DLB men, AD, and controls [17]. In addition, apart from one study showing that visual hallucinations were more common in women [18], the relationship between clinical symptoms and sex in DLB has neither been studied extensively either. In order to provide biomarker-guided personalized medicine in the future, it is essential to further clarify sex differences in DLB biomarkers and symptomatology. Therefore, in the current study, we aimed to examine sex differences in CSF biomarkers and clinical symptomatology in a large well-defined cohort of DLB patients.
Methods
Participants
We included 223 DLB patients who visited the Alzheimer Center Amsterdam between 1999 and 2019 from the Amsterdam Dementia Cohort based on the availability of CSF [19]. All patients received standardized screening at baseline, which included a semi-structured medical history interview; physical, neurological, and neuropsychological examinations; magnetic resonance imaging (MRI); electroencephalography (EEG) or magnetoencephalography (MEG); and laboratory tests. Diagnoses were made in a multidisciplinary consensus meeting based on the results obtained from the standardized screening [19]. DLB patients were diagnosed clinically according to the current consensus criteria for probable DLB [1, 20]. FP-CIT single-photon emission computed tomography (DAT-SPECT) was available in 103 patients and was positive for DLB diagnosis in 92 patients. DLB was confirmed at autopsy in 3 patients, of which 2 did not have a DAT-SPECT scan. Written informed consent was obtained from all study participants for the use of clinical data and biomaterial for research purposes.
Measures
Clinical and cognitive features
We rated the core clinical features at baseline from preformatted questionnaires or retrospectively from patients’ medical charts. Hallucinations were scored according to the caregiver-rated neuropsychiatric inventory (NPI) that was available in 222 patients [21]. Parkinsonism was assessed with a preformatted checklist for extrapyramidal signs during the neurological exam (i.e., tremor, bradykinesia, and/or rigidity), data available for 216 patients. The semi-structured patient history interview was reviewed for information on fluctuations and RBD. Fluctuations were scored as being present when the patient or caregiver reported clear changes in attention and cognition during the day or between days. Information on fluctuations was available for 173 patients. REM sleep behavior disorder (RBD) was rated positive when caregivers reported that patients “act out” their dreams during their sleep. Information on RBD was available of 156 patients. Duration of complaints was systematically assessed during the patient history interview and was defined as the moment when the patient first noticed their cognitive complaints. Depressive symptoms were assessed using the 15-item Geriatric Depression Scale, with higher scores indicating more depressive symptoms [22]. Mini Mental State Examination (MMSE) was used to assess global cognition. Memory was assessed using the immediate and delayed recall of the Dutch version of the verbal learning test (RAVLT) [23]. Attention and speed was assessed using Trail Making Test (TMT)-A. Executive functioning was assessed using the ratio of TMT-B/TMT-A [24]. We calculated inverse scores for time-dependent tests (i.e., TMT-A and TMT-B), such that lower scores represent worse performance. Missing values of the TMT-B were imputed using the group ratio of TMT-B/TMT-A. Neuropsychological test scores were available for 205 patients, and test results were Z-transformed based on cognitively normal subjects (n = 533, 60 ± 10 years, 54%F, MMSE = 29 ± 1).
Apolipoprotein E genotyping
The QIAamp DNA blood isolation kit from Qiagen (Venlo, The Netherlands) was used to isolate DNA from 10-ml vacutainer tubes containing EDTA. This was followed by genotype determination using the LightCycler ApoE Mutation Detection Kit (Roche Diagnostics, GmbH, Mannheim, Germany). Subjects with at least one APOEe4 allele were defined as APOEe4 carriers, whereas no e4 allele defined subjects as APOEe4 non-carriers.
CSF analysis
For CSF collection and processing, standardized protocols were followed [25, 26]. CSF total α-syn concentrations were determined using a sandwich ELISA assay (developed by ADx NeuroSciences, Ghent, Belgium and commercialized by Euroimmun AG, Lübeck, Germany) [27]. To avoid blood contamination, α-syn measures with high hemoglobuline (Hb) concentrations (> 10 ng/ml) or high erythrocyte count (> 500 ery/ml) were excluded. CSF total α-syn was available for 127 patients. CSF Aβ1-42, Tau, and pTau concentrations were measured using a sandwich ELISA (Innotest, Fujirebio, Gent, Belgium), or the Elecsys Aβ42, Tau, and pTau (181P) CSF assays run on the cobas e601 analyzer (Roche Diagnostics GmbH). Elecsys values of Aβ42, Tau, and pTau were converted to Innotest values using previously described formulas [28]. Drift corrected continuous Aβ42 concentrations were used in the data analyses, and to define amyloid positivity, Aβ42 concentrations were dichotomized using a cutoff < 813 pg/ml [29]. CSF Aβ1-42, Tau, and pTau were available for all patients.
Statistical analysis
Demographic data were compared between women and men using chi-squared tests, independent t test, or Mann-Whitney U tests where appropriate. All variables were checked for outliers and normality of residuals using Q-Q plots. TMT-data and CSF (p) Tau levels were log-transformed to meet assumptions of normality. Other outcome variables met the assumption of normally distributed residuals. To evaluate sex differences in clinical outcome measures, we used general linear models (GLM) with sex as the factor and baseline cognitive data or core clinical features as main outcome measures. Analyses were adjusted for age (clinical data) or age and education (cognitive data). Next, we performed general linear models (GLM) with sex as the factor and CSF biomarkers (i.e., α-syn Aβ1-42, Tau, and pTau) as the main outcome measure for each of the four CSF biomarkers separately. Analyses were adjusted for age (model 1) or age and APOEe4 genotype (model 2). A p < 0.05 was considered significant. Analyses were conducted using R statistical program (version 3.5.2 “eggshell igloo”).
Results
Baseline characteristics are shown in Table 1. The majority of our sample consisted of men (f 17% vs m 83%). Women were older than men (f 70 vs m 68; p = 0.04), exhibited a shorter duration of complaints before diagnosis (f 2.3 vs m 3.5, p < 0.001), and more often reported visual hallucinations (f 58% vs m 38%, p < 0.02). Additionally, women more frequently carried the APOEe4 allele (f 70% vs m 52%, p = 0.08). No sex differences were found in other core clinical features, depressive symptoms, or years of education. After correcting for age and education, MMSE scores and animal fluency scores were lower in women than men. Performance on RAVLT (immediate and delayed recall), VAT, TMT-A, and TMT-B/A did not differ between sexes (Table 1).
Table 1.
Baseline characteristics
| Women, n = 39 | Men, n = 184 | p value | |
|---|---|---|---|
| Age | 70.1 ± 6.0 | 67.7 ± 7.3 | 0.04 |
| Education, years | 11.0 ± 2.8 | 11.4 ± 2.9 | 0.42 |
| Duration of complaints, years | 2.3 ± 1.2 | 3.5 ± 2.8 | < 0.001 |
| APOE ɛ4 carrier,n(%) | 22 (70%) | 86 (52%) | 0.08 |
| Geriatric Depression Scale (0–15) | 4 ± 3 | 4 ± 3 | 0.65 |
| Core clinical features,n(%) | |||
| Visual hallucinations, n = 222 | 23 (59%) | 69 (38%) | 0.02 |
| Parkinsonism, n = 216 | 23 (62%) | 130 (73%) | 0.28 |
| RBD, n = 156 | 11 (55%) | 99 (73%) | 0.17 |
| Cognitive fluctuations, n = 173 | 29 (94%) | 119 (84%) | 0.26 |
| Cognitive test scoresa,n = 205 | |||
| MMSE | 21 ± 6 | 23 ± 4 | 0.02 |
| RAVLT—immediate recall | − 1.94 ± 1.10 | − 2.00 ± 0.95 | 0.74 |
| RAVLT—delayed recall | − 1.80 ± 0.98 | − 1.72 ± 0.96 | 0.84 |
| VAT—12 items | − 6.20 ± 5.78 | − 4.87 ± 4.99 | 0.31 |
| TMT-Ab | − 5.47 ± 6.46 | − 4.60 ± 4.84 | 0.52 |
| TMT-B/Ab,c | − 6.93 ± 7.03 | − 5.33 ± 6.42 | 0.32 |
| Animal fluency | − 2.38 ± 1.02 | − 1.78 ± 0.99 | 0.002 |
| Biomarker status, abnormal/available,n(%) | |||
| DAT SPECT, n = 107 | 15/15 (100%) | 79/91 (87%) | 0.06 |
| CSF Aβ42 status | 30/39 (77%) | 104/186 (56%) | 0.02 |
| Abnormal Tau/Aβ42 ratio (> 0.52) | 21/38 (55%) | 55/185 (30%) | 0.002 |
Data represent mean ± SD, median [IQR] or n (%). Parkinsonism: bradykinesia, rigidity, or tremor
MMSE Mini Mental State Examination, RAVLT Raven auditory verbal learning test (Dutch version), VAT Visual Association Test, TMT Trail Making Test
aAdjusted for age and education. Data of RAVLT, VAT, TMT, and animal fluency represent z scores, based on cognitively healthy subjects
bData are inverted and log-transformed
cMissing values are imputed based on TMT-B/A ratio for n = 101
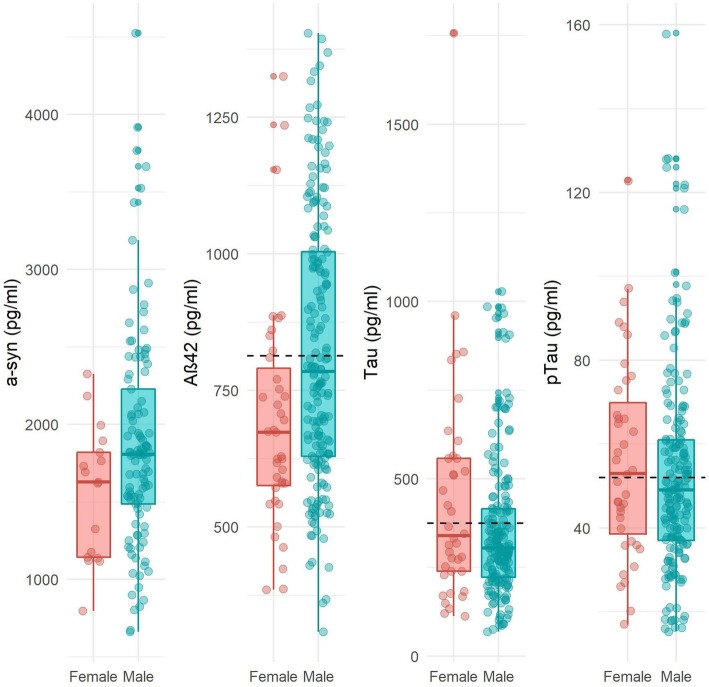
Next, we evaluated sex differences in CSF biomarker concentrations (Table 2; Fig. 1). Adjusted for age, women exhibited lower α-syn concentrations compared to men. Moreover, women had lower Aβ42 concentrations than men and exhibited more often abnormal CSF amyloid concentrations (f 77% vs m 56%, Table 1). No sex differences were found for CSF Tau or pTau concentrations. After adjusting for age and APOEe4 genotype, results for all CSF biomarkers remained largely similar (Table 2). When repeating the analyses in the subgroup with positive DAT-SPECT scans (n = 92; f 15 (16%), m 79 (84%)), we found similar effect sizes for all CSF biomarkers, although significance for α-syn was lost due to the loss of power (eTable 1).
Table 2.
Cerebrospinal fluid concentrations at baseline
| Women, n = 39 | Men, n = 184 | Model 1a | Model 2b | |||
|---|---|---|---|---|---|---|
| Adjusted mean difference β coefficient (95%CI) | p value | Adjusted mean difference β coefficient (95%CI) | p value | |||
| α-sync | 1558 ± 431 | 1895 ± 707 | − 390 (− 731:− 48) | 0.03 | − 309 (− 657:− 40) | 0.08 |
| Aβ42 | 696 ± 210 | 824 ± 251 | − 108 (− 190:− 26) | 0.01 | −103 (− 191:− 14) | 0.02 |
| Taud | 5.9 ± 0.6 | 5.7 ± 0.5 | 0.10 (− 0.09:− 0.29) | 0.31 | 0.06 (− 0.14:− 0.03) | 0.55 |
| pTaud | 3.9 ± 0.5 | 3.9 ± 0.5 | 0.03 (− 0.13:0.19) | 0.74 | 0.01 (−0.15:0.17) | 0.90 |
Data presented as mean ± SD
aModel 1: adjusted for age
bModel 2: adjusted for age and APOEe4 genotype
cα-syn results were available for n = 117 (f = 17; m = 100)
dAnalyses were performed with LN transformed data to meet assumptions of normality
Fig. 1.
Sex differences in cerebrospinal fluid biomarker concentrations. Mean differences in CSF biomarker concentrations in picorgrams/milliliter between women and men. *p < 0.05. Abbreviations: CSF, cerebrospinal fluid; α-syn; alpha-synuclein; Aβ42; amyloid-β42; Tau, total tau; (p) Tau, tau phosphorylated at threonine 181. Dashed line reflects cutoffs for Aβ42 (813 pg/ml), Tau (375 pg/ml), and (p) Tau (52 pg/ml)
Discussion
In the present study, where DLB was more prevalent in men than in women, women had lower CSF Aβ42 and α-syn concentrations. In addition, women had more frequent hallucinations, had shorter duration of complaints before diagnosis, were older, and had lower scores on MMSE and fluency-tasks. Based on our findings, one could hypothesize that women have a more aggressive disease course compared to men.
When using predefined cutoffs for CSF Aβ42, 77% of women had amyloid pathology, in contrast to 56% of men. This suggests that women more often had concomitant AD pathology, whereas men more often had pure DLB pathology. These in vivo findings are in line with previous autopsy studies that observed that men were more likely to die with pure DLB pathology and women more often died with DLB + AD pathology [11, 30]. However, AD pathology is not only characterized by the presence of amyloid plaques, but also by NFT aggregation, which results in higher (p) Tau levels in CSF. As women in our study showed isolated lowered CSF Aβ42 levels, an alternative explanation could be that the lower levels of Aβ42 are directly related to the DLB disease process, rather than reflecting concomitant AD pathology. Previous studies have shown that Aβ42 induces the formation of high-molecular-weight α -syn, and vice versa [31]. Therefore, this synergistic interaction between Aβ42 and α -syn could lead to increased aggregation and accumulation of both α-syn and amyloid pathology in the women in our study compared to men [31–33].
Concomitant amyloid pathology in DLB has previously been related to a more severe clinical disease burden [12]. In line with these former findings, women in our cohort had lower MMSE and fluency test scores, and more frequent hallucinations, but a shorter duration of symptoms before diagnosis, suggesting a more aggressive disease course upon diagnosis in women with DLB. This could well be related to the amyloid-pathology that is more often encountered in DLB women. In our study, duration of complaints was estimated retrospectively; therefore, we cannot completely rule out that women with DLB were already in a later disease stage at the moment of diagnosis. Consistent with our hypothesis of a more aggressive disease course in women, one other study found that women with DLB have shorter survival after onset of dementia [34]. Prospective studies with longitudinal data are needed to further investigate sex differences in disease course over time.
Our data are in line with former observations of a strong male-predominance in DLB, as 83% of patients in our cohort were men [4–7]. The strong male-predominance in DLB could be explained by hormonal differences between sexes. Several previous studies have shown that 17β-estradiol (E2) conveys neuroprotective effects in women [35]. In fact, a previous in vitro study has shown that estradiol exhibits dose-dependent inhibition of α-syn aggregation and destabilization of preformed α-syn, which is thought to be driven by the antioxidant properties of estrogens [36–39]. This suggests that until menopause occurs in women, at the average age of 55 years, they are protected against the development of diseases such as DLB and Parkinson’s disease. During the second half of menopause, however, women show a sudden drop of estradiol levels [40], thus triggering the aggregation of α-syn and impeding the breakdown of preformed α-syn. If this is the case, sex differences in prevalence are expected to be more balanced with increasing age. In line with this hypothesis, a recent study reported a higher DLB prevalence of men than women under the age of 75 years, which equalized between the ages of 75 and 80 years. Above the age of 80 years, however, DLB was more common in women [8]. Future studies will have to demonstrate whether this shift in prevalence is mediated by hormonal differences.
Another explanation for the higher prevalence of DLB in men could be that concomitant AD pathology seen in DLB women potentially introduces a bias towards diagnosing these women with AD rather than DLB, therefore underdiagnosing the true proportion of women with DLB. In line with this reasoning, one study found that concomitant AD pathology decreased diagnostic accuracy, as typical AD symptoms were more pronounced, in contrast to DLB symptoms [41]. Our results imply that clinicians should be conscious of the risk of underdiagnosing women with DLB.
Our study has several strengths, including our well-defined, large sample of DLB patients. The clinical diagnosis of DLB was largely supported by DAT-SPECT imaging. In addition, we had CSF α-syn available in a considerable part of patients and CSF AD biomarkers in all patients. Furthermore, CSF collection follows a highly standardized protocol, assuring that the possibility of pre-analytical confounders is minimized [19]. Among the limitations is the retrospective design of our study. Information on RBD and fluctuations was rated retrospectively based on patients’ medical charts. In some cases, these features were not reported, which could either mean that they were not present or that it was not asked by the medical doctor. Therefore, there was a relatively large number of missing values for these features and there is a risk of underreporting. Future prospective studies should use standardized methods to assess these symptoms. A second limitation is that CSF total α-syn is not yet validated as a clinically useful marker in DLB, and there might be differences in sensitivity between different α-syn species. For example, soluble α-syn oligomers could be more useful in DLB, because oligomeric forms of α-syn seem to play a more essential role in the pathogenesis of α-synucleinopathies than t-α-syn [42]. Another α-syn species of interest is α-syn phosphorylated at serine 129 (pSer129-α-syn), as approximately 90% of accumulated α-syn in Lewy bodies consists of pSer129-α-syn [43]. However, these species cannot yet be measured robustly with commercial assays as these have not yet been validated. A last limitation was that a small part of our patients had a normal DAT-SPECT scan, not supportive of DLB diagnosis. However, clinical diagnosis was made carefully in a tertiary memory clinic setting and false-negative DAT-SPECT scans in early disease stages have been previously described [44].
Conclusions
To conclude, our results indicate sex differences in DLB, wherein concomitant AD pathology was more frequent in women and CSF alpha-synuclein levels were lower in women compared to men. Concomitant pathology, combined with lower cognitive test scores and a shorter duration of complaints before diagnosis, could suggest a higher disease severity in women. Our results raise awareness among clinicians of the possibility that women are underdiagnosed and have the potential to aid in defining sex-specific personalized medicine strategies within DLB.
Supplementary information
Additional file 1: eTable 1. Cerebrospinal fluid concentrations at baseline in DAT SPECT positive subgroup.
Acknowledgements
Thanks to Cindy Francois (ADx, Neurosciences) for the preparation of the Hb ELISA kits.
Abbreviations
- DLB
Dementia with Lewy bodies
- CSF
Cerebrospinal fluid
- Aβ
Amyloid-β
- Aβ42
Amyloid β1-42
- α-syn
Alpha-synuclein
- Tau
Total tau
- pTau
Tau phosphorylated at threonine 181
- CV
Coefficient of variation
- MMSE
Mini Mental State Examination
- GLM
General linear models
- RBD
REM sleep behavior disorder
- NFT
Neurofibrillary tangles
- AD
Alzheimer’s disease
- MRI
Magnetic resonance imaging
- EEG
Electroencephalography
- DAT-SPECT
FP-CIT single-photon emission computed tomography
- NPI
Neuropsychiatric inventory
- TMT
Trail Making Test
- RAVLT
Verbal learning test
- Hb
Hemoglobuline
Authors’ contributions
MvdB and RBM were equally responsible for the study design, analysis and interpretation of data, and the writing of the manuscript. IvS was responsible for the study concept and design, review of the statistical analysis, and critical revision of the manuscript for important intellectual content. HvdS was responsible for critical revision of the manuscript for important intellectual content. PS was responsible for critical revision of the manuscript for important intellectual content. CET was responsible for critical revision of the manuscript for important intellectual content. AWL was responsible for the study concept and design and critical revision of the manuscript for important intellectual content. WMvdF was responsible for the study concept and design, the review of the statistical analysis, and the critical revision of the manuscript for important intellectual content. The authors read and approved the final manuscript.
Funding
Research of the Alzheimer Center Amsterdam is part of the Neurodegeneration research program of the Neuroscience Campus Amsterdam. The Alzheimer Center Amsterdam is supported by Alzheimer Nederland and Stichting VUMC funds. A.L. has received funding from stichting Dioraphte and ZonMW Memorabel (project #733050509).
Availability of data and materials
All data used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Written informed consent was obtained from all study participants for the use of clinical data and biomaterial for research purposes. This study was approved by the local medical ethical committee of the Amsterdam UMC, location VUmc.
Consent for publication
Not applicable.
Competing interests
Prof. Dr. Teunissen has a collaboration contract with ADx Neurosciences and performed contract research or received grants from Probiodrug, AC Immune, Biogen-Esai, CogRx, Toyama, Janssen prevention center, Boehringer, AxonNeurosciences, Fujirebio, EIP farma, PeopleBio, and Roche. Prof. Dr. Scheltens has acquired grant support (for the institution) from GE Healthcare and Piramal. In the past 2 years, he has received consultancy/speaker fees (paid to the institution) from Novartis, Probiodrug, Biogen, Roche, and EIP Pharma, LLC. Dr. Lemstra has received funding from stichting Dioraphte and ZonMW Memorabel (project #733050509). Research programs of Prof. Dr. Wiesje van der Flier have been funded by ZonMW, NWO, EU-JPND, Alzheimer Nederland, CardioVascular Onderzoek Nederland, Health~Holland, Topsector Life Sciences & Health, stichting Dioraphte, Gieskes-Strijbis fonds, stichting Equilibrio, Biogen MA Inc., Life-MI, AVID, and Combinostics. WF holds the Pasman chair. WF has performed contract research for Biogen MA Inc. All funding is paid to her institution. Van de Beek, Babapour Mofrad, van Steenoven, Dr. vanderStichele report no disclosures relevant to this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
M. van de Beek and R. Babapour Mofrad contributed equally to this work.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13195-020-00610-9.
References
- 1.McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor J-P, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies fourth consensus report of the DLB consortium. Neurology. 2017;89(1):88–100. doi: 10.1212/WNL.0000000000004058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vekrellis K, Xilouri M, Emmanouilidou E, Rideout HJ, Stefanis L. Pathological roles of α-synuclein in neurological disorders. Lancet Neurol. 2011;10(11):1015–1025. doi: 10.1016/S1474-4422(11)70213-7. [DOI] [PubMed] [Google Scholar]
- 3.van Steenoven I, Aarsland D, Weintraub D, Londos E, Blanc F, van der Flier WM, et al. Cerebrospinal fluid Alzheimer’s disease biomarkers across the Spectrum of Lewy body diseases: results from a large multicenter cohort. J Alzheimers Dis. 2016;54(1):287–295. doi: 10.3233/JAD-160322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane JP, Surendranathan A, Bentley A, Barker SA, Taylor J-P, Thomas AJ, et al. Clinical prevalence of Lewy body dementia. Alzheimers Res Ther. 2018;10(1):19. doi: 10.1186/s13195-018-0350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fereshtehnejad S-M, Religa D, Westman E, Aarsland D, Lökk J, Eriksdotter M. Demography, diagnostics, and medication in dementia with Lewy bodies and Parkinson’s disease with dementia: data from the Swedish dementia quality registry (SveDem) Neuropsychiatr Dis Treat. 2013;9:927. doi: 10.2147/NDT.S45840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Savica R, Grossardt BR, Bower JH, Boeve BF, Ahlskog JE, Rocca WA. Incidence of dementia with Lewy bodies and Parkinson disease dementia. JAMA Neurol. 2013;70(11):1396–1402. doi: 10.1001/jamaneurol.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Podcasy JL, Epperson CN. Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin Neurosci. 2016;18(4):437. doi: 10.31887/DCNS.2016.18.4/cepperson. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mouton A, Blanc F, Gros A, et al. Sex ratio in dementia with Lewy bodies balanced between Alzheimer’s disease and Parkinson’s disease dementia: a cross-sectional study. Alz Res Therapy. 2018;10:92. 10.1186/s13195-018-0417-4. [DOI] [PMC free article] [PubMed]
- 9.Price A, Farooq R, Yuan J-M, Menon VB, Cardinal RN, O’Brien JT. Mortality in dementia with Lewy bodies compared with Alzheimer’s dementia: a retrospective naturalistic cohort study. BMJ Open. 2017;7(11). [DOI] [PMC free article] [PubMed]
- 10.Nelson PT, Jicha GA, Kryscio RJ, Abner EL, Schmitt FA, Cooper G, et al. Low sensitivity in clinical diagnoses of dementia with Lewy bodies. J Neurol. 2010;257(3):359–366. doi: 10.1007/s00415-009-5324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnes LL, Lamar M, Schneider JA. Sex differences in mixed neuropathologies in community-dwelling older adults. Brain Res. 2019;1719:11-6. [DOI] [PMC free article] [PubMed]
- 12.Lemstra AW, de Beer MH, Teunissen CE, Schreuder C, Scheltens P, van der Flier WM, et al. Concomitant AD pathology affects clinical manifestation and survival in dementia with Lewy bodies. J Neurol Neurosurg Psychiatry. 2017;88(2):113–118. doi: 10.1136/jnnp-2016-313775. [DOI] [PubMed] [Google Scholar]
- 13.Abdelnour C, van Steenoven I, Londos E, Blanc F, Auestad B, Kramberger MG, et al. Alzheimer’s disease cerebrospinal fluid biomarkers predict cognitive decline in Lewy body dementia. Mov Disord. 2016;31(8):1203–1208. doi: 10.1002/mds.26668. [DOI] [PubMed] [Google Scholar]
- 14.Hohman TJ, Dumitrescu L, Barnes LL, Thambisetty M, Beecham G, Kunkle B, et al. Sex-specific association of apolipoprotein e with cerebrospinal fluid levels of tau. JAMA Neurol. 2018;75(8):989–998. doi: 10.1001/jamaneurol.2018.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnes LL, Wilson RS, Bienias JL, Schneider JA, Evans DA, Bennett DA. Sex differences in the clinical manifestations of Alzheimer disease pathology. Arch Gen Psychiatry. 2005;62(6):685–691. doi: 10.1001/archpsyc.62.6.685. [DOI] [PubMed] [Google Scholar]
- 16.Mofrad RB, van der Flier WM. Nature and implications of sex differences in AD pathology. Nat Rev Neurol. 2019;15(1):6. doi: 10.1038/s41582-018-0115-7. [DOI] [PubMed] [Google Scholar]
- 17.Wennström M, Londos E, Minthon L, Nielsen HM. Altered CSF orexin and α-synuclein levels in dementia patients. J Alzheimers Dis. 2012;29(1):125–132. doi: 10.3233/JAD-2012-111655. [DOI] [PubMed] [Google Scholar]
- 18.Chiu PY, Teng PR, Wei CY, Wang CW, Tsai CT. Gender difference in the association and presentation of visual hallucinations in dementia with Lewy bodies: a cross-sectional study. Int J Geriatr Psychiatry. 2018;33(1):193–199. doi: 10.1002/gps.4706. [DOI] [PubMed] [Google Scholar]
- 19.van der Flier WM, Scheltens P. Amsterdam dementia cohort: performing research to optimize care. J Alzheimers Dis. 2018;62(3):1091–1111. doi: 10.3233/JAD-170850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKeith I, Dickson DW, Lowe J, Emre M, O'brien J, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies third report of the DLB consortium. Neurology. 2005;65(12):1863–1872. doi: 10.1212/01.wnl.0000187889.17253.b1. [DOI] [PubMed] [Google Scholar]
- 21.Cummings JL. The neuropsychiatric inventory assessing psychopathology in dementia patients. Neurology. 1997;48(5 Suppl 6):10S–16S. doi: 10.1212/WNL.48.5_Suppl_6.10S. [DOI] [PubMed] [Google Scholar]
- 22.Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist. J Aging Mental Health. 1986;5(1-2):165–73.
- 23.Saan R, Deelman B. De 15-woordentest A en B (een voorlopige handleiding). Groningen: Afdeling Neuropsychologie, AZG; 1986. [Google Scholar]
- 24.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8(3):271–276. doi: 10.2466/pms.1958.8.3.271. [DOI] [Google Scholar]
- 25.Mofrad RB, Bouwman FH, Slot RE, Timmers T, van der Flier WM, Scheltens P, et al. Lumbar puncture in patients with neurologic conditions. Alzheimers Dement. 2017;8:108–110. doi: 10.1016/j.dadm.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Campo M, Mollenhauer B, Bertolotto A, Engelborghs S, Hampel H, Simonsen AH, et al. Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: an update. Biomark Med. 2012;6(4):419–430. doi: 10.2217/bmm.12.46. [DOI] [PubMed] [Google Scholar]
- 27.Chiasserini D, Biscetti L, Eusebi P, Salvadori N, Frattini G, Simoni S, et al. Differential role of CSF fatty acid binding protein 3, α-synuclein, and Alzheimer’s disease core biomarkers in Lewy body disorders and Alzheimer’s dementia. Alzheimers Res Ther. 2017;9(1):52. doi: 10.1186/s13195-017-0276-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willemse EA, van Maurik IS, Tijms BM, Bouwman FH, Franke A, Hubeek I, et al. Diagnostic performance of Elecsys immunoassays for cerebrospinal fluid Alzheimer’s disease biomarkers in a nonacademic, multicenter memory clinic cohort: the ABIDE project. Alzheimers Dement. 2018;10:563–572. doi: 10.1016/j.dadm.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tijms BM, Willemse EA, Zwan MD, Mulder SD, Visser PJ, van Berckel BN, et al. Unbiased approach to counteract upward drift in cerebrospinal fluid amyloid-β 1–42 analysis results. Clin Chem. 2017;2017:281055. doi: 10.1373/clinchem.2017.281055. [DOI] [PubMed] [Google Scholar]
- 30.Nelson PT, Schmitt FA, Jicha GA, Kryscio RJ, Abner EL, Smith CD, et al. Association between male gender and cortical Lewy body pathology in large autopsy series. J Neurol. 2010;257(11):1875–1881. doi: 10.1007/s00415-010-5630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clinton LK, Blurton-Jones M, Myczek K, Trojanowski JQ, LaFerla FM. Synergistic interactions between Aβ, tau, and α-synuclein: acceleration of neuropathology and cognitive decline. J Neurosci. 2010;30(21):7281–7289. doi: 10.1523/JNEUROSCI.0490-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Irwin DJ, Lee VM-Y, Trojanowski JQ. Parkinson’s disease dementia: convergence of α-synuclein, tau and amyloid-β pathologies. Nat Rev Neurosci. 2013;14(9):626. doi: 10.1038/nrn3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colom-Cadena M, Gelpi E, Charif S, Belbin O, Blesa R, Martí MJ, et al. Confluence of α-synuclein, tau, and β-amyloid pathologies in dementia with Lewy bodies. J Neuropathol Exp Neurol. 2013;72(12):1203–12. doi: 10.1097/NEN.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 34.Williams MM, Xiong C, Morris JC, Galvin JE. Survival and mortality differences between dementia with Lewy bodies vs Alzheimer disease. Neurology. 2006;67(11):1935–1941. doi: 10.1212/01.wnl.0000247041.63081.98. [DOI] [PubMed] [Google Scholar]
- 35.Liu B, Dluzen DE. Oestrogen and nigrostriatal dopaminergic neurodegeneration: animal models and clinical reports of Parkinson's disease. Clin Exp Pharmacol Physiol. 2007;34(7):555–565. doi: 10.1111/j.1440-1681.2007.04616.x. [DOI] [PubMed] [Google Scholar]
- 36.Hirohata M, Ono K, Morinaga A, Ikeda T, Yamada M. Anti-aggregation and fibril-destabilizing effects of sex hormones on α-synuclein fibrils in vitro. Exp Neurol. 2009;217(2):434–439. doi: 10.1016/j.expneurol.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Zhu M, Rajamani S, Kaylor J, Han S, Zhou F, Fink AL. The flavonoid baicalein inhibits fibrillation of α-synuclein and disaggregates existing fibrils. J Biol Chem. 2004;279(26):26846–26857. doi: 10.1074/jbc.M403129200. [DOI] [PubMed] [Google Scholar]
- 38.Ono K, Yamada M. Antioxidant compounds have potent anti-fibrillogenic and fibril-destabilizing effects for α-synuclein fibrils in vitro. J Neurochem. 2006;97(1):105–115. doi: 10.1111/j.1471-4159.2006.03707.x. [DOI] [PubMed] [Google Scholar]
- 39.Ehrnhoefer DE, Bieschke J, Boeddrich A, Herbst M, Masino L, Lurz R, et al. EGCG redirects amyloidogenic polypeptides into unstructured, off-pathway oligomers. Nat Struct Mol Biol. 2008;15(6):558. doi: 10.1038/nsmb.1437. [DOI] [PubMed] [Google Scholar]
- 40.Mielke MM, Vemuri P, Rocca WA. Clinical epidemiology of Alzheimer’s disease: assessing sex and gender differences. Clin Epidemiol. 2014;6:37. doi: 10.2147/CLEP.S37929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Merdes A, Hansen L, Jeste D, Galasko D, Hofstetter C, Ho G, et al. Influence of Alzheimer pathology on clinical diagnostic accuracy in dementia with Lewy bodies. Neurology. 2003;60(10):1586–1590. doi: 10.1212/01.WNL.0000065889.42856.F2. [DOI] [PubMed] [Google Scholar]
- 42.van Steenoven I, Majbour NK, Vaikath NN, Berendse HW, van der Flier WM, van de Berg WD, et al. α-Synuclein species as potential cerebrospinal fluid biomarkers for dementia with lewy bodies. Mov Disord. 2018;33(11):1724–1733. doi: 10.1002/mds.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson JP, Walker DE, Goldstein JM, De Laat R, Banducci K, Caccavello RJ, et al. Phosphorylation of Ser-129 is the dominant pathological modification of α-synuclein in familial and sporadic Lewy body disease. J Biol Chem. 2006;281(40):29739–29752. doi: 10.1074/jbc.M600933200. [DOI] [PubMed] [Google Scholar]
- 44.van der Zande JJ, Booij J, Scheltens P, Raijmakers PG, Lemstra AW. [(123)]FP-CIT SPECT scans initially rated as normal became abnormal over time in patients with probable dementia with Lewy bodies. Eur J Nucl Med Mol Imaging. 2016;43(6):1060–1066. doi: 10.1007/s00259-016-3312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: eTable 1. Cerebrospinal fluid concentrations at baseline in DAT SPECT positive subgroup.
Data Availability Statement
All data used and/or analyzed during the present study are available from the corresponding author on reasonable request.