Abstract
Coronavirus disease 2019 (COVID-19) is a pandemic that has affected more than 1.8 million people worldwide, overwhelmed health care systems owing to the high proportion of critical presentations, and resulted in more than 100,000 deaths. Since the first data analyses in China, elevated cardiac troponin has been noted in a substantial proportion of patients, implicating myocardial injury as a possible pathogenic mechanism contributing to severe illness and mortality. Accordingly, high troponin levels are associated with increased mortality in patients with COVID-19. This brief review explores the available evidence regarding the association between COVID-19 and myocardial injury.
Key Words: COVID-19, Coronavirus, SARS, Troponin, Myocardial injury, Myocarditis
In December 2019, a series of pneumonia cases of unknown cause emerged in Wuhan, Hubei, China, with clinical presentations greatly resembling viral pneumonia.1 Deep sequencing analysis from lower respiratory tract samples indicated a novel coronavirus, which was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
As of April 14, 2020, a total of 1,844,863 cases of SARS-CoV-2 infection and 117,021 deaths have been confirmed by the World Health Organization.2 The most feared clinical presentation of coronavirus disease 2019 (COVID-19) is bilateral interstitial pneumonia, which may progress to acute respiratory distress syndrome. The latter occurs in approximately 3%–30% of hospitalized patients with COVID-19, depending on the cohort.1 , 3, 4, 5, 6, 7, 8
Analyzing the first reports from China, a considerable proportion of patients (12%–28%) presented elevated cardiac troponin levels.1 , 6 , 8 , 9 Compared with patients with normal levels, those with elevated troponins were older and had significantly higher rates of comorbidities including hypertension, coronary artery disease (CAD), and diabetes.6 Notably, patients with higher troponin levels were more likely to be admitted to intensive care1 , 5 and showed higher in-hospital mortality.6, 7, 8 , 10, 11, 12, 13
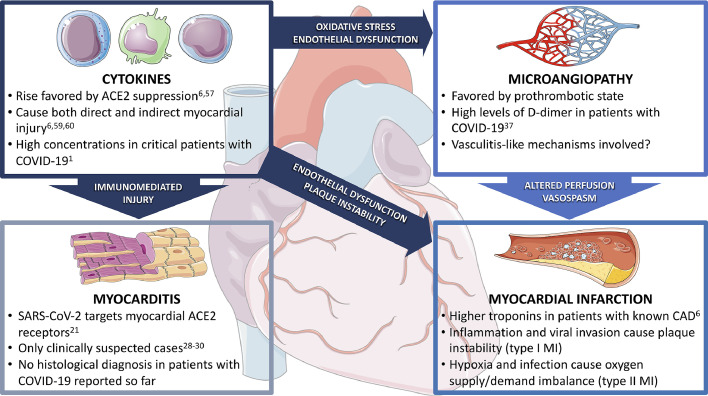
Acute respiratory infections as well as sepsis are often associated with an increase in troponin, which can be used as a marker of disease severity and predicts future cardiovascular events.14, 15, 16 Hypotheses on COVID-19–associated myocardial injury are consistent with previous observations relating to the outbreaks of SARS and Middle East respiratory syndrome. Several mechanisms have been proposed, which are summarized in Figure 1 . In this review, we provide an overview of the available evidence regarding the possible mechanisms of myocardial injury in COVID-19.
Fig. 1.
Possible mechanisms explaining troponin elevation in patients with COVID-19. (Modified from Servier Medical Art, licensed under a Creative Common Attribution 3.0 Generic License. http://smart.servier.com/). ACE2, angiotensin-converting enzyme 2; CAD, coronary artery disease; COVID-19, coronavirus disease 2019; MI, myocardial infarction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Myocarditis
Myocarditis is an inflammatory disease of the myocardium diagnosed by established histologic, immunologic, and immunohistochemical criteria.17 Many viruses are cardiotropic, meaning that they bind directly on molecular targets in the myocardium. Myocardial damage may be due to different mechanisms. In the initial phase of viral myocarditis, direct virus-mediated lysis of cardiomyocytes occurs.18 This process is usually followed by a robust T-cell response, which can lead to further heart injury and ventricular dysfunction.19 , 20 In COVID-19, particular attention has been given to the role of angiotensin-converting enzyme 2 (ACE2), the binding receptor for SARS-CoV-2 cellular entry.21 ACE2 is highly expressed in pericytes of adult human hearts, which indicates an intrinsic susceptibility of the heart to SARS-CoV-2 infection.22 SARS-CoV-2 seems to not only gain initial entry through ACE2, but also to subsequently downregulate ACE2 expression, resulting in reduced conversion of angiotensin II (Ang-II) to angiotensin 1–7 (Ang-1–7). Ang-1–7 physiologically mediates protective cardiovascular effects in target organs.23 , 24
In autopsies of patients who died from the SARS outbreak in 2002, 35% of heart samples showed the presence of viral RNA in the myocardium, which in turn was associated with reduced ACE2 protein expression.25 SARS-CoV-2 may share the same mechanism with the first SARS coronavirus because the 2 viruses are highly homologous in genome.6 , 26 , 27 The consequences of ACE2 downregulation on the cardiovascular system is further expanded on.
Myocarditis represents one of the most challenging diagnoses in cardiology. Suspicion rises with the number of criteria fulfilled.17 However, diagnostic certainty is based on endomyocardial biopsy or autopsy, where histologic analyses (infiltration, lymphocytes, macrophages, cellular inflammatory types) or molecular methods of viral genome identification can be performed.
To the best of our knowledge, only 3 case reports of probable COVID-19 myocarditis are available to date,28, 29, 30 but none have been proven by biopsy. A fourth case describes the autopsy of a patient with severe COVID-19 who died from sudden cardiac arrest.31 Interestingly, there were no obvious histologic changes seen in the heart tissue.
The emergency setting of many hospital facilities during the pandemic together with strict hygienic measures intended to prevent further contagion may hinder large studies on biopsy specimens in patients with COVID-19 and the performance of autopsies. At present, no convincing evidence of histologically confirmed COVID-19 myocarditis has been published.
Microangiopathy
SARS-CoV-2 uses ACE2 as its entry receptor, and subsequently downregulates ACE2 expression. In addition to the heart and lung, ACE2 is localized in the intestinal epithelium, vascular endothelium, and the kidneys.32 , 33 In the renin–angiotensin–aldosterone system, ACE2 catalyzes the conversion of Ang-II to Ang-1–7, which opposes the vasoconstrictor, proinflammatory, pro-oxidant, proproliferative, and profibrotic actions exerted by Ang-II via AT1 receptors.34 As a result, suppression of ACE2 expression and subsequent increase in Ang-II35 levels may represent another threat to heart and vessels in patients with COVID-19. However, the role of Ang-II/Ang-1–7 imbalance in COVID-19 is extrapolated based on limited data from a different, albeit closely related, coronavirus (SARS-CoV).
The clinical significance of this pathway in COVID-19 complications and any possible role of modulating this receptor are not yet fully known. A clinical trial testing recombinant human ACE2 as a treatment for patients with COVID-19 is currently ongoing (NCT04335136). This drug may play a double role, both by acting as a decoy and competitively decreasing viral cell entry, and by restoring ACE2 activity and its beneficial role.36
Endothelial dysfunction, cytokine storm, oxidative stress, and Ang-II upregulation may explain the coagulopathy frequently seen in severe coronavirus disease.37 A postmortem study from Singapore38 on patients with SARS reported that 4 of 8 patients had pulmonary thromboembolic lesions and 3 patients had deep vein thrombosis. To date, there is only 1 described case of COVID-19–associated pulmonary embolism,39 but approximately one-half of patients with COVID-19 present high levels of d-dimer,3 which is associated to disease severity and higher mortality.40 This marked increase in d-dimer may be due to intense inflammation stimulating intrinsic fibrinolysis in the lungs with spillover into the bloodstream.41
Another factor that may contribute to microangiopathy is vasculitis. Several studies have linked coronavirus infection with Kawasaki disease, especially in children.42, 43, 44 Furthermore, a case series of 3 deceased SARS patients in 2003 described findings of systemic vasculitis, including edema, localized fibrinoid necrosis, and infiltration of monocytes, lymphocytes, and plasma cells into vessel walls in the heart, lung, liver, kidney, adrenal gland, and the stroma of striated muscles.45 It has been suggested that, in patients with COVID-19, microvascular damage occurring in the heart causes perfusion defects, vessel hyperpermeability, and vasospasm, leading to myocardial injury.46 , 47 Notably, a considerable proportion of critically ill patients with COVID-19 present with acute kidney injury, which is associated with worse prognosis.8 , 48 The mechanism may be the same, with microangiopathy of renal vessels, but there is no strong supporting evidence to date. Worsening of troponin clearance in patients with acute kidney injury could also contribute to the elevated levels in those patients.
Myocardial Infarction
Patients with preexisting CAD and those with risk factors for atherosclerotic cardiovascular disease (CVD) are at an increased risk of developing an acute coronary syndrome during acute infections, as demonstrated previously in epidemiologic and clinical studies of influenza49, 50, 51 and other acute inflammatory conditions.52 This outcome could result from imbalance between oxygen supply and demand in the acute setting, so that the troponin elevation may be interpreted as a type 2 myocardial infarction (MI).53 Reduced oxygen supply in patients with COVID-19 is typically caused by hypoxic respiratory failure, a feature that is more common in deceased patients than in patients who recover10 and is a marker of disease severity.9 In contrast, infectious states are often accompanied by fever, tachycardia, and endocrine dysregulation, which lead to a marked increase in myocardial oxygen demand. Moreover, hypoxemia also leads to excessive intracellular calcium with consequent cardiac myocyte apoptosis.47
By definition, a type 2 MI can occur with or without underlying CAD. However, considering the higher prevalence of elevated troponin in patients with COVID-19 with previous CVD, it is possible that the type 2 MI when underlying stable coronary disease is unmasked by the acute infection.
Type 1 MI, caused by plaque rupture with thrombus formation, may also be precipitated by COVID-19.53 Circulating cytokines released during a severe systemic inflammatory stress could lead to atherosclerotic plaque instability and rupture.54 In addition, the suppression of ACE2 expression and Ang-II increase may elevate cardiovascular risk through mechanisms such as oxidative stress, endothelial dysfunction, and vasoconstriction. Moreover, because ACE2 is expressed in vascular endothelial cells,32 , 33 direct viral vascular infection leading to plaque instability may also play a role in type 1 MI in patients with COVID-19.
The occurrence of acute coronary syndrome and MI in infected patients during the first SARS outbreak has been described.38 , 55 However, there are very scarce data about symptoms and electrocardiogram changes related to MI in COVID-19. Chest pain has been broadly reported and is also associated with cardiac injury,7 but it has a very low specificity owing to the primary lung disease (ie, pleuritic pain). Interestingly, Guo et al6 reported that on admission no patients showed evidence of acute MI. No data regarding electrocardiogram changes on larger groups have been published to date.
Cytokine Storm
Severe lung inflammation and impaired pulmonary gas exchange in COVID-19 has been suggested to be due to upregulation of proinflammatory cytokines.56 In healthy subjects, Ang-1–7 limits the synthesis of proinflammatory and profibrotic cytokines. Thus, downregulation of ACE2 by SARS-CoV-2, with a consequent decrease in Ang-1–7 levels, may magnify the cytokine storm, resulting in an overwhelming inflammatory response.6 , 57 Cytokines have been extensively studied in patients with heart failure owing to their role in inflammatory modulation, myocyte stress or stretch, myocyte injury and apoptosis, fibroblast activation, and extracellular matrix remodeling.58
In the study by Guo et al,6 plasma troponin levels had a significant positive linear correlation with plasma high-sensitivity C-reactive protein levels, indicating that myocardial injury may be closely associated with inflammatory pathogenesis during the progress of the disease. In addition to their direct effects on cardiomyocytes, high levels of circulating cytokines also lead to functional reprogramming of endothelial cells, endothelial dysfunction, and atherogenesis.6 , 59 , 60 In fact, endothelial cells are thought to play a primary role in the inflammatory response in viral infections.61
Thus, systemic inflammatory response with cytokine storm is a plausible cause of myocardial injury in the late phases of disease, usually associated with acute respiratory distress syndrome, multiorgan failure, and mortality. Overall, high cytokine levels may represent the key player of myocardial injury in COVID-19, being related to direct myocardial injury, endothelial dysfunction, destabilization of coronary plaque, and microthrombogenesis.
Future Perspectives
Troponin represents a useful marker of disease progression and prognosis in COVID-19. As noted by Guo et al,6 the 16% of their patients with underlying CVD but normal troponin levels had a relatively favorable outcome. Therefore, myocardial biomarkers should be evaluated in patients with CVD who develop COVID-19 for risk stratification purposes to potentially lead to earlier and more aggressive interventions.
Numerous therapies have been proposed worldwide to reduce COVID-19–associated morbidity and mortality. Some are antiviral drugs acting directly on SARS-CoV-2, with conflicting results to date.62 Other ongoing trials are testing immunomodulating agents, aimed at decreasing the excessive inflammatory response that characterizes severe disease progression. Because evidence of inflammatory cell infiltration has been reported in the alveoli of patients with acute respiratory distress syndrome associated with SARS-CoV-2 infection,31 this finding could justify the use of corticosteroids in patients with COVID-19. Another therapeutic possibility is drugs or biologics that act on the cytokine storm, especially targeting IL-163 and IL-6.64 Further observations on myocardial enzyme curves and imaging studies in patients treated with those drugs are needed to correlate immunomodulation with myocardial protection in COVID-19.
Another important issue in this disease is prevention of thrombotic complications. As noted, severe COVID-19 has been associated with high levels of d-dimer as a marker of a general prothrombotic state.37 Based on the immunothrombosis model, which highlights a bidirectional relationship between the immune system and thrombin generation, blocking thrombin by heparin may dampen the inflammatory response.65 Furthermore, heparin also has an anti-inflammatory function, which may be relevant in this setting.66 Several publications have demonstrated this property and some of the described mechanisms include binding to inflammatory cytokines, inhibition of neutrophil chemotaxis and leukocyte migration, neutralization of the positively charged peptide complement factor C5a, and sequestration of acute phase proteins.67, 68, 69, 70 A systematic review concluded that, in the clinical setting, heparin can decrease the level of inflammatory biomarkers but stressed the need for more data from larger studies.71
Conclusions
Elevated troponin levels are frequent in patients with COVID-19 and significantly associated with fatal outcomes. Several mechanisms may explain this phenomenon: viral myocarditis, cytokine-driven myocardial damage, microangiopathy, and unmasked CAD.
At present, none of these mechanisms have been definitely proven to be the main driver of troponin elevation and/or myocardial damage in patients with COVID-19. However, we posit that, although COVID-19 initially presents as a primarily respiratory condition, it quickly involves the cardiovascular system through an imbalance of the renin–angiotensin–aldosterone system mediated by ACE2 depletion. This mechanism may complicate the clinical course mediated through the inflammatory response, endothelial dysfunction and microvascular damage.
Additional study of these mechanisms is clearly needed and may influence the search for ways to prevent myocardial damage (eg, immunomodulating drugs). Given the impact of myocardial damage in the pathophysiology and prognosis of patients with COVID-19, the inclusion of cardiovascular end points in ongoing drug trials is essential.
It is reasonable to triage patients with COVID-19 according to the presence of underlying CVD and evidence of myocardial injury for prioritized treatment and even more aggressive treatment strategies in an effort to decrease mortality.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19) situation report – 85. Available at: https://reliefweb.int/report/world/coronavirus-disease-2019-covid-19-situation-report-85-14-april-2020.
- 3.Guan W., Ni Z., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28 doi: 10.1056/NEJMoa2002032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7 doi: 10.1001/jama.2020.1585. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 March 27 doi: 10.1001/jamacardio.2020.1017. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of Cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 March 25 doi: 10.1001/jamacardio.2020.0950. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 Feb 20 doi: 10.1016/S2213-2600(20)30079-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020 Mar 26 doi: 10.1136/bmj.m1091. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 March 3 doi: 10.1007/s00134-020-05991-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He X.W., Lai J.S., Cheng J., Wang M.W., Liu Y.J., Xiao Z.C. [Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients] Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E011. doi: 10.3760/cma.j.cn112148-20200228-00137. [DOI] [PubMed] [Google Scholar]
- 13.Wang L., He W., Yu X., Hu D., Bao M., Liu H. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020 Mar 30 doi: 10.1016/j.jinf.2020.03.019. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long B., Long D.A., Tannenbaum L., Koyfman A.An emergency medicine approach to troponin elevation due to causes other than occlusion myocardial infarction. Am J Emerg Med[Epub ahead of print]. [DOI] [PubMed]
- 15.Frencken J.F., van Baal L., Kappen T.H., Donker D.W., Horn J., van der Poll T. Myocardial injury in critically ill patients with community-acquired pneumonia. A cohort study. Ann Am Thorac Soc. 2019;16:606–612. doi: 10.1513/AnnalsATS.201804-286OC. [DOI] [PubMed] [Google Scholar]
- 16.Menéndez R., Méndez R., Aldás I., Reyes S., Gonzalez-Jimenez P., España P.P. Community-acquired pneumonia patients at risk for early and long-term cardiovascular events are identified by cardiac biomarkers. Chest. 2019;156:1080–1091. doi: 10.1016/j.chest.2019.06.040. [DOI] [PubMed] [Google Scholar]
- 17.Caforio A.L.P., Pankuweit S., Arbustini E., Basso C., Gimeno-Blanes J., Felix S.B. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–2648. doi: 10.1093/eurheartj/eht210. 2648a–8d. [DOI] [PubMed] [Google Scholar]
- 18.Maekawa Y., Ouzounian M., Opavsky M.A., Liu P.P. Connecting the missing link between dilated cardiomyopathy and viral myocarditis: virus, cytoskeleton, and innate immunity. Circulation. 2007;115:5–8. doi: 10.1161/CIRCULATIONAHA.106.670554. [DOI] [PubMed] [Google Scholar]
- 19.Lawson C.M. Evidence for mimicry by viral antigens in animal models of autoimmune disease including myocarditis. Cell Mol Life Sci CMLS. 2000;57:552–560. doi: 10.1007/PL00000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Badorff C., Knowlton K.U. Dystrophin disruption in enterovirus-induced myocarditis and dilated cardiomyopathy: from bench to bedside. Med Microbiol Immunol (Berl) 2004;193:121–126. doi: 10.1007/s00430-003-0189-7. [DOI] [PubMed] [Google Scholar]
- 21.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020:181. doi: 10.1016/j.cell.2020.02.052. 271–80.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen L., Li X., Chen M., Feng Y., Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020 mar 20 doi: 10.1093/cvr/cvaa078. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel V.B., Zhong J.-C., Grant M.B., Oudit G.Y. Role of the ACE2/angiotensin 1-7 axis of the renin-angiotensin system in heart failure. Circ Res. 2016;118:1313–1326. doi: 10.1161/CIRCRESAHA.116.307708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oudit G.Y., Kassiri Z., Jiang C., Liu P.P., Poutanen S.M., Penninger J.M. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu X., Chen P., Wang J., Feng J., Zhou H., Li X. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63:457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 March 27 doi: 10.1001/jamacardio.2020.1096. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zeng J.H., Liu Y.-X., Yuan J., Wang F.X., Wu W.B., Li J.X. First case of COVID-19 infection with fulminant myocarditis complication: case report and insights. Life Sci. 2020 March 11 doi: 10.20944/preprints202003.0180.v1. [Epub ahead of print] 11 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur Heart J. 2020 Mar 16 doi: 10.1093/eurheartj/ehaa190. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamming I., Timens W., Bulthuis M.L.C., Lely A.T., Navis G., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tikellis C., Bernardi S., Burns W.C. Angiotensin-converting enzyme 2 is a key modulator of the renin-angiotensin system in cardiovascular and renal disease. Curr Opin Nephrol Hypertens. 2011;20:62–68. doi: 10.1097/MNH.0b013e328341164a. [DOI] [PubMed] [Google Scholar]
- 34.Kuster G.M., Pfister O., Burkard T., Zhou Q., Twerenbold R., Haaf P. SARS-CoV2: should inhibitors of the renin–angiotensin system be withdrawn in patients with COVID-19? Eur Heart J. 2020 Mar 20 doi: 10.1093/eurheartj/ehaa235. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo J., Huang Z., Lin L., Lv J. Coronavirus disease 2019 (COVID‐19) and cardiovascular disease: a viewpoint on the potential influence of angiotensin‐converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.016219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yin S., Huang M., Li D., Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020 Apr 3 doi: 10.1007/s11239-020-02105-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chong P.Y., Chui P., Ling A.E., Franks T.J., Tai D.Y., Leo Y.S. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128:195–204. doi: 10.5858/2004-128-195-AODDTS. [DOI] [PubMed] [Google Scholar]
- 39.Danzi G.B., Loffi M., Galeazzi G., Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020 Mar 30 doi: 10.1093/eurheartj/ehaa254. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost JTH. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Idell S. Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit Care Med. 2003;31:S213–S220. doi: 10.1097/01.CCM.0000057846.21303.AB. [DOI] [PubMed] [Google Scholar]
- 42.Chang L.-Y., Lu C.-Y., Shao P.-L., Lee P.I., Lin M.T., Fan T.Y. Viral infections associated with Kawasaki disease. J Formos Med Assoc Taiwan Yi Zhi. 2014;113:148–154. doi: 10.1016/j.jfma.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shirato K., Imada Y., Kawase M., Nakagaki K., Matsuyama S., Taguchi F. Possible involvement of infection with human coronavirus 229E, but not NL63, in Kawasaki disease. J Med Virol. 2014;86:2146–2153. doi: 10.1002/jmv.23950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giray T., Biçer S., Küçük Ö., Çöl D., Yalvaç Z., Gürol Y. Four cases with Kawasaki disease and viral infection: aetiology or association. Infez Med. 2016;24:340–344. [PubMed] [Google Scholar]
- 45.Ding Y., Wang H., Shen H., Li Z., Geng J., Han H. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J Pathol. 2003;200:282–289. doi: 10.1002/path.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen Y., Li Y., Liu X. Potential pathophysiological mechanisms underlying COVID-19-induced myocardial injury. Chin J Pathophysiol. 2020;36:573–576. [Google Scholar]
- 47.Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pan X., Xu D., Zhang H., Zhou W., Wang L.H., Cui X.G. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020 Mar 31 doi: 10.1007/s00134-020-06026-1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Madjid M., Miller C.C., Zarubaev V.V., Marinich I.G., Kiselev O.I., Lobzin Y.V. Influenza epidemics and acute respiratory disease activity are associated with a surge in autopsy-confirmed coronary heart disease death: results from 8 years of autopsies in 34 892 subjects. Eur Heart J. 2007;28:1205–1210. doi: 10.1093/eurheartj/ehm035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nguyen J.L., Yang W., Ito K., Matte T.D., Shaman J., Kinney P.L. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1:274. doi: 10.1001/jamacardio.2016.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kwong J.C., Schwartz K.L., Campitelli M.A., Chung H., Crowcroft N.S., Karnauchow T. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 52.Smeeth L., Thomas S.L., Hall A.J., Hubbard R., Farrington P., Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611–2618. doi: 10.1056/NEJMoa041747. [DOI] [PubMed] [Google Scholar]
- 53.Thygesen K., Alpert J.S., Jaffe A.S., Chaitman B.R., Bax J.J., Morrow D.A. Fourth universal definition of myocardial infarction (2018) Eur Heart J. 2018;72:2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 54.Bonow R.O., Fonarow G.C., O'Gara P.T., Yancy C.W. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020 Mar 27 doi: 10.1001/jamacardio.2020.1105. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 55.Peiris J., Chu C., Cheng V., Chan K.S., Hung I.F., Poon L.L. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xiong T.-Y., Redwood S., Prendergast B., Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020 Mar 18 doi: 10.1093/eurheartj/ehaa231. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peiró C., Moncada S. Substituting angiotensin-(1-7) to prevent lung damage in SARSCoV2 infection? Circulation. 2020 Apr 3 doi: 10.1161/CIRCULATIONAHA.120.047297. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stanciu A.E. Advances in clinical chemistry. Elsevier; New York: 2019. Cytokines in heart failure; pp. 63–113. [Google Scholar]
- 59.Kofler S., Nickel T., Weis M. Role of cytokines in cardiovascular diseases: a focus on endothelial responses to inflammation. Clin Sci Lond Engl 1979. 2005;108:205–213. doi: 10.1042/CS20040174. [DOI] [PubMed] [Google Scholar]
- 60.Mirzaei H., Ferns G.A., Avan A. Advances in clinical chemistry. Elsevier; New York: 2019. Cytokines and MicroRNA in coronary artery disease; pp. 47–70. [DOI] [PubMed] [Google Scholar]
- 61.Teijaro J.R., Walsh K.B., Cahalan S., Fremgen D.M., Roberts E., Scott F. Endothelial cells are central orchestrators of cytokine amplification during influenza virus infection. Cell. 2011;146:980–991. doi: 10.1016/j.cell.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020 Mar 18 doi: 10.1056/NEJMoa2001282. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Conti P., Gallenga C.E., Tetè G., Caraffa A., Ronconi G., Younes A. How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1. J Biol Regul Homeost Agents. 2020 Mar 31 doi: 10.23812/Editorial-Conti-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 64.Zhang C., Wu Z., Li J.-W., Zhao H., Wang G.Q. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. 2020 Mar 29 doi: 10.1016/j.ijantimicag.2020.105954. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gaertner F., Massberg S. Blood coagulation in immunothrombosis-At the frontline of intravascular immunity. Semin Immunol. 2016;28:561–569. doi: 10.1016/j.smim.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 66.Thachil J. The versatile heparin in COVID-19. J Thromb Haemost. 2020 Apr 2 doi: 10.1111/jth.14821. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Young E. The anti-inflammatory effects of heparin and related compounds. Thromb Res. 2008;122:743–752. doi: 10.1016/j.thromres.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 68.Li J.-P., Vlodavsky I. Heparin, heparan sulfate and heparanase in inflammatory reactions. Thromb Haemost. 2009;102:823–828. doi: 10.1160/TH09-02-0091. [DOI] [PubMed] [Google Scholar]
- 69.Esmon C.T. Targeting factor Xa and thrombin: impact on coagulation and beyond. Thromb Haemost. 2014;111:625–633. doi: 10.1160/TH13-09-0730. [DOI] [PubMed] [Google Scholar]
- 70.Poterucha T.J., Libby P., Goldhaber S.Z. More than an anticoagulant: do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017;117:437–444. doi: 10.1160/TH16-08-0620. [DOI] [PubMed] [Google Scholar]
- 71.Mousavi S., Moradi M., Khorshidahmad T. Anti-inflammatory effects of heparin and its derivatives: a systematic review. Adv Pharmacol Sci. 2015;2015 doi: 10.1155/2015/507151. [DOI] [PMC free article] [PubMed] [Google Scholar]