A 52-year-old male patient developed chills, fever and generalized pain 8 days earlier. The following symptoms were denied: sore throat, fatigue, cough, nausea, abdominal distention or abdominal pain. The patient and 4 of his family members tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on nucleic acid tests performed by the Suining Center for Disease Control & Prevention, and then they were transferred to our hospital for quarantine and specialized treatment.
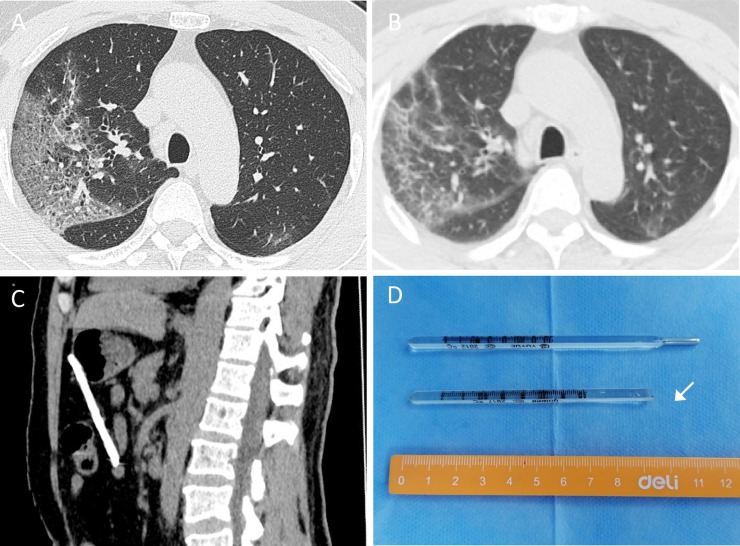
The patient’s characteristics included the following: temperature, 37.8 °C; pulse, 101/min; respiration, 20/min; and blood pressure, 137/92 mmHg. Arterial blood gas analysis showed the following: pH, 7.53; partial pressure of oxygen (PaO2), 76 mmHg; partial pressure of carbon dioxide (PCO2), 35 mmHg; and fraction of inspired oxygen (FiO2), 28 %. A full blood count showed a white blood cell (WBC) count of 4.8 × 10⁹/L, a neutrophil count of 2.78 × 10⁹/L and a lymphocyte count of 1.33 × 10⁹/L. The C-reactive protein (CRP) level was 0.52 mg/L (normal 0–10), and the procalcitonin (PCT) level was 0.06 ng/mL (normal 0−0.5). On admission, computed tomography (CT) images showed ground-glass opacity (GGO) and consolidation in multiple lobes, along with double emphysema signs and scattered fibrous foci in both lungs (Fig. 1 A).
Fig. 1.
The patient’s CT and the foreign body in the abdomen.
The chest CT presentation at admission showed multiple GGO changes with consolidation in both lungs, with air bronchogram, blood vessel thickening in the foci, signs of emphysema, and scattered fibrous foci (1A). Compared with the CT at admission, the chest CT manifestations at discharge indicated that pulmonary consolidation was resolved, while the fibrosis was more obvious (1B). The appearance of the foreign body on the abdominal plain CT scan (1C). The foreign body was a thermometer (white arrow) without a mercury tip (1D).
On the fourth day after admission, chest CT was repeated and showed that a high-density shadow was present in the anterior wall of the stomach, but the whole shadow could not be observed. The patient had not yet disclosed any relevant information to a doctor. During a physical examination, a 3-mm-diameter wound with little pus that was covered with a band aid was seen under the xiphoid of the patient. There was no tenderness, rebound tenderness, or high muscular tension in the upper abdomen, and no foreign body was palpable. On the fourth night, the CT was repeated and showed a columnar high-density shadow localized in the upper abdominal cavity (Fig. 1C). Subsequently, the medical staff performed exploratory laparotomy under strict protective measures after a negative-pressure operating room was prepared. During the operation, a 3-mm irregular skin-penetrating wound was found under the xiphoid, and the omentum was damaged approximately 1 cm away from the greater curvature of the stomach. There was a 4-cm × 3-cm haematoma in the omentum. A 9-cm thermometer was found in the omental sac. The mercury tip of the thermometer had disappeared (Fig. 1D). No pus or food residue was found in the abdominal cavity. After the operation, tetanus antitoxin was injected, and piperacillin sodium and tazobactam sodium were intravenously infused as antibacterial therapy (3.375 g q8h).
Although the patient had no history of depression, he thought that his own negligence had led to several family members becoming infected by SARS-CoV-2. Therefore, he had a strong sense of guilt and was worried about being discriminated against by society. After effective psychotherapy, the patient's depression improved, and he was willing to cooperate with the examination and treatment. We used the Impact of Events Scale – Revised (IES-R) to evaluate the post-traumatic stress disorder (PTSD) of the patient at that time. The three subscale scores were as follows: intrusion subscale, 14 points; avoidance subscale, 12 points; and hyperarousal subscale, 9 points. The total score of the IES-R scale was 35, which is significantly higher than the diagnostic standard of 20 (Hawryluck et al., 2004; Wu et al., 2005). After the evaluation, a senior psychologist was arranged to provide him with regular psychological counselling, and we also increased the nursing management. Considering that the psychological pressure of the patient had been relieved, we did not give him antidepressants.
Five days after admission, the nucleic acid test results for SARS-CoV-2 became negative. Nine days after admission, chest CT showed that the consolidations of the bilateral lungs were partially resolved (Fig. 1B). On the 11th day of hospitalization, the patient was discharged and was advised to quarantine at home for 14 days and receive regular follow up.
Although many studies have reported the clinical characteristics of COVID-19 patients, few have described changes in the mental state of the patients. Previous studies have reported that 10 %–42 % of Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) patients were afflicted by anxiety, depression and other mental symptoms (Han et al., 2003; Kim et al., 2018; Lee et al., 2018), which are closely related to the quarantine state in addition to the diseases themselves. The adverse effects of mental illness on the recovery of COVID-19 patients should be considered, including the possibility of death in a few patients (Goyal et al., 2020). Therefore, psychotherapy should be considered as an important treatment measure for patients suffering from infectious diseases that are characterized by severe social harm. It is especially important to provide timely and effective psychological counselling for patients who believe they may be responsible for disease transmission.
Ethics approval and consent to participate
The use of the data from the case in the present study was approved by the Institutional Review Board (IRB) of Suining Central Hospital. Informed consent was obtained from the patient.
Role of funding source
The authors have not received any financial support for this article.
Availability of data and materials
Not applicable.
We were all involved in the medical care of the patient and in writing and reviewing the manuscript. All listed authors approved the final version of the submitted manuscript.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgement
Not applicable.
References
- Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: first suicidal case in India. Asian J. Psychiatry. 2020;49:101989. doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y., Geng H., Feng W., et al. A follow-up study of 69 discharged SARS patients. J. Tradit. Chin. Med. 2003;23(3):214–217. [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.C., Yoo S.Y., Lee B.H., Lee S.H., Shin H.S. Psychiatric findings in suspected and confirmed middle east respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Invest. 2018;15(4):355–360. doi: 10.30773/pi.2017.10.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress after SARS. Emerg. Infect. Dis. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
We were all involved in the medical care of the patient and in writing and reviewing the manuscript. All listed authors approved the final version of the submitted manuscript.