Abstract
Purpose
To determine if weekly hours worked is associated with obesity among employed adults in US.
Design
Data from the 2015–2016 NHANES was used for this study. NHANES is a cross-sectional study.
Setting
NHANES is conducted annually by the National Center for Health Statistics (NCHS) designed to assess the health and nutritional status of citizens in the US.
Subjects
The final study sample size was 2,581.
Measures
The outcome was obesity status (Yes/No) and the exposure was the number of hours worked per week (<40, =40, >40 hours/week). Covariates of interest included in the analyses were income, age, education level, race, leisure physical activity, and gender.
Analysis
A weighted and adjusted logistic regression model was conducted in order to investigate the association between the number of hours worked at a job per week and obesity status. Descriptive statistics and weighted and adjusted odds ratios were produced with 95% confidence intervals.
Results
After controlling for the covariates of interest, people working 40 hours or 40+ hours a week had 1.403 (95% CI: 1.06–1.85) and 1.409 (95% CI: 1.03–1.93) times significantly greater odds of obesity than people who work < 40 hours a week, respectively.
Conclusion
Obesity is a complex and multifactorial disease with genetic and environmental interactions, including the number of hours a person works/week as a potential risk factor.
Purpose
Since 1990, the prevalence of obesity among United States (US) adults has been increasing.1 In 2000, 30.5% of Americans were obese and that proportion grew to 39.8% by 2016.1 For comparison purposes, the estimated global prevalence of obesity was 12% in 2017,2 which is much lower than the prevalence in the US. These contrasting statistics illustrate the significance of the obesity problem in the US specifically. In 1999, obesity was declared an epidemic in the US by health officials after a study published in the Journal for the American Medical Association observed a 6-percentage point increase (from 12% to 18%) in obesity from 1991 to 1998.3 According to the Centers for Disease Control (CDC),4 an epidemic refers to an increase, often sudden, in the number of cases of a disease above what is normally expected in that population. Obesity in adults has been identified as a risk factor for many chronic diseases including type 2 diabetes, coronary heart disease, high blood pressure, stroke, and certain forms of cancer.5 With obesity affecting over one-third of adults, the US faces a large economic and public health burden.6 Obesity is a complex and multifactorial disease with genetic and environmental interactions, which makes drawing conclusions about causes of obesity and solutions to prevent obesity difficult on a case-by-case basis.7 In the workplace, obesity and its coexisting chronic diseases contribute to excess costs associated with sick leave and absenteeism.8 Because the lack of physical activity is a risk factor for obesity,8 it is alarming that approximately one-third of US adults in 2007 were not meeting activity levels recommended for the promotion and maintenance of health.9 With about 25% of the population not engaging in daily leisure-time physical activity, it could explain why the US suffers from obesity and the chronic diseases associated with it.10
On average, working adults spend about one half of their work day sitting down, which is a substantial part of their waking hours.11–14 Among healthy adults above 20 years of age employed in high and low physical activity occupations, a high level of occupational physical activity (e.g. construction work) is associated with a decreased likelihood of being obese.15 This could be due to those people being physically active for a majority of the time that they’re awake.15
While previous literature investigated the association between occupational activity level and obesity, there is limited recent literature investigating the number of hours worked per week and its effect on obesity in the US on a nation-wide level. The literature mainly measured occupational activity level or leisure time activity level and the relationship with obesity as measured by Body Mass Index (BMI) or waist circumference. The number of hours worked per week were sometimes included in analysis but not as the main exposure of interest. For example, Cook and Gazmararian6 looked to investigate the association between long work hours, leisure time physical activity, and obesity across levels of occupational activity using data from the 2015 Georgia Behavioral Risk Factor Surveillance System. They found split results that work hours varied significantly across occupational activity groups, with employees in low physical activity occupations having the longest work hours, favoring the development of obesity, but no overall effect of long work hours on obesity.6 However, it is important to note that measuring occupational activity is known to not be accurate.6,15 Findings from Courtemanche16 show that longer work hours were associated with increased BMI and the probability of being obese among adults in the US during the time interval 1994 to 2004. Additionally, being that these data were collected 15 years ago in the US, there should be newer research to analyze if the findings are still relevant due to constantly changing lifestyle trends and nature of different occupations. Studies consistently show that excess sitting during leisure-time may have favorable associations for the development of overweight or obesity in adults, independent of physical activity level.17–19 Because of this consistent finding, it is important to consider reasons why people might be sitting in their leisure time instead of being active.
The goal of the current study is to determine whether there is an association between the number of hours worked per week and obesity on a nation-wide scale using recent US data. To this end, we examine the hypothesis that if a person works more than 40 hours a week, then the person is likely to spend their limited leisure time inactive, favoring the development of obesity. Conceivably, people may be too tired after a 40+ hour workweek to consistently be active in their leisure time, while people who have more free time (due to fewer hours in their workweek) may be more likely to have the energy, and anticipate having the time, to be physically active. The current investigation will be done using the 2015–2016 National Health and Nutrition Examination Survey (NHANES) data to investigate the association between hours worked per week and obesity status after adjusting for gender, race, education, income, leisure physical activity, and age.
Methods
Design
For the present study, publicly available data from the 2015–2016 wave of the National Health and Nutrition Examination Survey (NHANES) was used. The NHANES is a cross-sectional survey conducted annually by the National Center for Health Statistics (NCHS) designed to assess the health and nutritional status of citizens in the United States over the age of 2 months.10
Sample
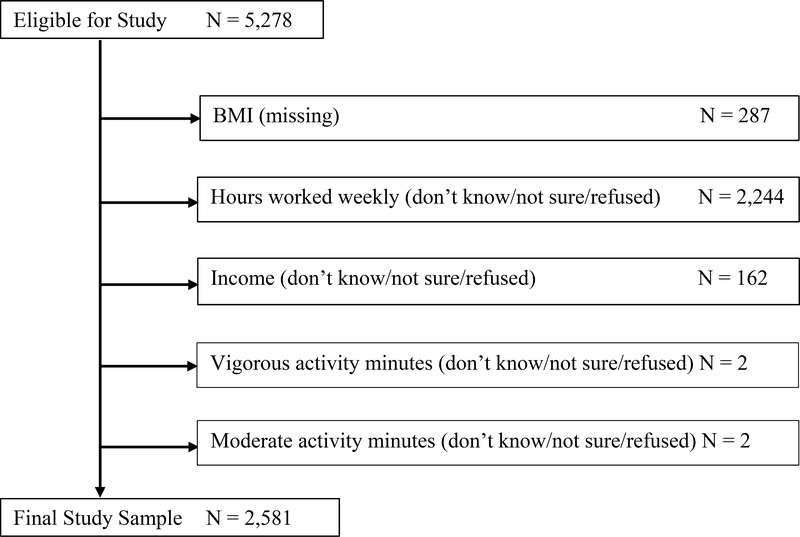
Of the initial 9,971 participants in the 2015–2016 cycle, data were used from 5,278 participants over the age of 25, who answered the questionnaire portion of the NHANES survey and were employed at the time of the survey (Figure 1). The sample size was restricted to adults over the age of 25 in order to account for students finishing up school and entering the workforce. It would be ideal to have a representative sample of adults who are in their careers, instead of a large number of students. From them, 4,991 had valid measurements taken in the Mobile Examination Center for BMI. Out of those who had valid measurements, several individuals had missing data on hours worked and income, and therefore were not included in the analyses, leading to the final study sample size of 2,581.
Figure 1.
Cohort Diagram of the Final Study Sample
Note: BMI stands for body mass index (kg/m2)
Measures
The exposure of interest for this investigation was the number of hours worked per week. This variable was collected on a continuous scale of hours ranging from 1 to 79 hours per week and was top-coded at 80. For the purpose of this study, the variable was then divided into 3 categories of <40 hours, equal to 40, and >40 hours. In 1938, the Fair Labor Standards Act was passed and set maximum hours at 40 per week.20 Since then, this standard has remained unchanged, evolving as the social and cultural norm of working 40 hours per week.22
The outcome of interest for this study was obesity status. Obesity status was measured by using the Body Mass Index (BMI) cutoff point of ≥ 30 (kg/m2) which defines obesity, according to the CDC.21 The BMI is calculated as body weight measured in kilograms divided by the squared value of the body height, measured in meters squared.22 Trained health technicians directly measured participants’ height and weight in the Mobile Examination Center component of NHANES, and as such these measures, including the BMI, are more reliable than self-reported measures.
Covariates of interest used in this investigation were age, sex, race, income, leisure physical activity, and education level.
Participants reported their gender in the questionnaire portion as either male or female. Participants reported their race by selecting one of six categories: Mexican American, Other Hispanic, Non-Hispanic Black, Non-Hispanic White, Non-Hispanic Asian, or other race (including multi-racial). These categories were collapsed into Mexican American/Hispanic, Non-Hispanic Black, Non-Hispanic White, Non-Hispanic Asian, and Other.
Participants reported their annual household income by selecting one of 14 categories of US dollar ranges, ranging in equal intervals from less than $5,000 (5K) to over $100,000 (100K). These categories were then collapsed into four groups of income: less than 25K, 25K-45K, 45K to 75K, and more than 75K.
Participants reported their education by selecting between 5 categories: less than 9th grade, 9th to 11th (includes 12th with no diploma), high school graduate/GED equivalent, some college or AA degree, college graduate or above. These categories were collapsed into three categories: less than high school, high school diploma or GED equivalent, and continued education.
Participants also indicated their age at the time of the survey. Age was collected and used as a continuous variable in the analyses.
The leisure physical activity variable was created using variables that measured vigorous and moderate recreational activity from the NHANES dataset. The distinction between vigorous and moderate activity was described to the participant as vigorous activity causing large increases in breathing or heart rate for at least 10 minutes continuously and moderate activity as small increases in breathing or heart rate for 10 minutes continuously. Metabolic equivalent (MET) was calculated by multiplying the number of days of vigorous or moderate leisure activity and the average number of minutes of activity by 8 or 4 depending on intensity, as suggested by NHANES, and then added together. This MET variable included both vigorous-intensity leisure activity and moderate-intensity weekly activity during leisure time, to give an average weekly leisure physical activity expenditure.
Analysis
Descriptive statistics were produced including weighed median and interquartile range (IQR) for the continuous variables and unweighted counts, weighted percent and 95% confidence intervals (CI) for the percent, for the categorical variables (Table 1). The interaction effect was analyzed between leisure physical activity MET and hours worked. Unadjusted weighted associations between each of the independent variables and the outcome of interest were investigated. Weighted logistic regressions were used to investigate the unadjusted association between continuous variables and obesity status. The association between categorical variables and obesity status was investigated using the Rao-Scott Chi-square test, which is the survey-weighted equivalent of the Pearson Chi-square test. A weighted and adjusted logistic regression model was conducted in order to investigate the association between the number of hours worked per week and obesity status, while adjusting for the covariates of interest. Weighed and adjusted odds ratios (OR) with corresponding 95% confidence intervals (CI) are presented in Table 2. All analyses were performed using R Studio statistical software. The statistical significance level was set at 0.05.
Table 1.
Descriptive statistics of the final study sample
| Overall (N=2,581) | Obesity | p-value* | ||||||
| Unweighted counts | Weighted | Yes (N= 1,063) | No (N= 1,518) | |||||
| Median | Interquartile range | Median | Interquartile range | Median | Interquartile range | |||
| Age at survey | 2,581 | 45 | 34 – 54 | 45 | 36 – 55 | 44 | 32–54 | 0.070 |
| Number of hours spent at work | 2,581 | 40 | 35 – 50 | 40 | 38 – 50 | 40 | 35 – 50 | 0.082 |
| Leisure physical activity | 2,581 | 360 | 0 – 1440 | 240 | 0 – 960 | 480 | 0 – 1680 | < 0.001 |
| Overall (N=2,581) | Obesity | |||||||
| Unweighted counts | Weighted | Yes (N= 1,063) | No (N= 1,518) | p-value** | ||||
| Percent | 95% CI for percent | Percent | 95% CI for percent | Percent | 95% CI for percent | |||
| Categorical number of hours spent at work | ||||||||
| < 40 hours | 793 | 28.51 | 25.69 – 31.34 | 25.55 | 21.28 – 29.81 | 30.60 | 27.53 – 33.66 | 0.112 |
| 40 hours | 806 | 29.59 | 27.13 – 32.04 | 30.95 | 26.78 – 35.13 | 28.63 | 26.14 – 31.11 | |
| > 40 hours | 982 | 41.90 | 38.28 –45.52 | 43.50 | 38.92 – 48.09 | 40.78 | 36.61 – 44.95 | |
| Gender | ||||||||
| Female | 1,230 | 46.73 | 44.79 – 48.66 | 49.00 | 45.50 – 52.51 | 45.13 | 41.98 – 48.28 | 0.178 |
| Male | 1,351 | 53.28 | 51.34 – 55.21 | 51.00 | 47.49 – 54.50 | 54.87 | 51.72 – 58.02 | |
| Race | ||||||||
| Non-Hispanic White | 815 | 65.15 | 56.81 – 73.48 | 63.72 | 54.56 – 72.87 | 66.15 | 57.78 – 74.53 | < 0.001 |
| Non-Hispanic Black | 568 | 11.01 | 6.70 – 15.32 | 13.47 | 7.78 – 19.16 | 9.28 | 5.73 – 12.84 | |
| Non-Hispanic Asian | 350 | 5.84 | 3.16 – 8.53 | 1.57 | 0.80 – 2.33 | 8.85 | 4.93 – 12.76 | |
| Hispanic | 768 | 14.91 | 9.56 – 20.26 | 17.39 | 11.78 – 23.00 | 13.17 | 7.87 – 18.47 | |
| Other | 80 | 3.08 | 2.18 – 4.00 | 3.85 | 2.38 – 5.32 | 2.55 | 1.75 – 3.35 | |
| Education | ||||||||
| Less than High School Education | 480 | 11.57 | 8.49 – 14.65 | 10.82 | 8.08 – 13.56 | 12.10 | 8.38 – 15.82 | < 0.001 |
| High School Education/GED | 509 | 17.26 | 14.61 – 19.91 | 18.23 | 15.70 – 20.76 | 16.58 | 13.03 – 20.14 | |
| Continued Education | 1,592 | 71.17 | 66.67 – 75.67 | 70.95 | 66.86 – 75.05 | 71.32 | 65.45 – 77.19 | |
| Annual income | ||||||||
| < $25,000 | 300 | 6.90 | 5.44 – 8.37 | 6.73 | 4.98 – 8.48 | 7.03 | 5.37 – 8.69 | 0.854 |
| $25,000 – $44,999 | 766 | 21.99 | 19.42 – 24.55 | 22.09 | 18.51 – 25.67 | 21.91 | 19.38 – 24.45 | |
| $45,000 – $74,999 | 609 | 22.50 | 19.52 – 25.48 | 23.31 | 18.22 – 28.40 | 21.93 | 18.25 –25.61 | |
| > $75,000 | 906 | 48.61 | 43.07 – 54.15 | 47.87 | 40.53 – 55.21 | 49.13 | 43.50 – 54.75 | |
Based on weighted logistic regression significant at p-value < 0.05
Based on the Rao-Scott Chi-square test, which is the design adjusted equivalent of the Pearson Chi-square test significant at p-value < 0.05
Note: Significant p-value is bolded in the table
Table 2. The association between hours worked per week and obesity status among working adults:
Weighted and adjusted odds ratios (OR) and corresponding 95% Confidence Intervals (CI)
| Independent variable | Weighted OR | Weighted 95% CI |
|---|---|---|
| Number of hours spent at work | ||
| < 40 hours | REFERENCE | REFERENCE |
| 40 hours | 1.403 | 1.06 – 1.85 |
| > 40 hours | 1.409 | 1.03 – 1.93 |
| Gender | ||
| Male | REFERENCE | REFERENCE |
| Female | 1.171 | 0.92 – 1.49 |
| Race | ||
| Non-Hispanic White | REFERENCE | REFERENCE |
| Non-Hispanic Black | 1.598 | 1.25 – 2.05 |
| Non-Hispanic Asian | 0.177 | 0.13 – 0.25 |
| Hispanic | 1.611 | 1.16 – 2.24 |
| Other | 1.769 | 1.09 – 2.87 |
| Education | ||
| Less than High School Education | REFERENCE | REFERENCE |
| High School Education/GED | 1.381 | 1.07 – 1.79 |
| Continued Education | 1.428 | 1.01 – 2.02 |
| Annual income | ||
| < $25,000 | REFERENCE | REFERENCE |
| $25,000 – $44,999 | 1.031 | 0.82 – 1.31 |
| $45,000 – $74,999 | 1.126 | 0.78 – 1.66 |
| > $75,000 | 1.130 | 0.83 – 1.59 |
| Age | 1.008 | 1.00 – 1.02 |
| Leisure physical activity | 1.000 | 1.00 – 1.00 |
Note: Significant OR with a corresponding CI is bolded in the table.
Note: The lower 95% confidence level for age was 0.998, indicating non-significance.
Results
The characteristics of the final study sample are presented in Table 1. The median age of the study participants was approximately 44 years with an IQR of 34–54 years. The median number of hours worked per week was 40 with an IQR of 35 to 50. Among adults aged 25 and older there was a marginally significant association between obesity status and age at survey (p= 0.07) as well as the number of hours spent at work (p= 0.088). In basic univariable statistical analyses between categorical independent variables and obesity – the outcome of interest, there was a statistically significant association between race (p < 0.00001) and obesity, as well as between education (p < 0.0001) and obesity. There was no significant interaction effect between leisure physical activity and hours worked per week. The weighted and adjusted odds of being obese were significantly greater for non-Hispanic Blacks (OR=1.598; 95% CI: 1.25–2.05), Hispanics (OR=1.611; 95% CI: 1.16 – 2.24), and Other races (OR=1.769; 95% CI: 1.09 – 2.87) when compared to non-Hispanic Whites (Table 2). The weighted and adjusted odds of obesity among individuals with a high school education or GED equivalent were 38.1% significantly greater (OR=1.381; 95% CI: 1.07 – 1.79) than those with less than a high school education. The weighted and adjusted odds for obesity were 42.8% significantly greater for those with continued education (OR=1.428; 95% CI: 1.01–2.02) compared to those with less than high school education (Table 2).
After adjusting for gender, race, education, annual income, leisure physical activity, and age, the weighted and adjusted odds of obesity among individuals working more than 40 hours a week, or exactly 40 hours a week, were 40.9% significantly greater (OR=1.409; 95% CI: 1.03–1.93), or 40.3% significantly greater (OR=1.403; 95% CI: 1.03–1.85), respectively, than the odds of obesity among individuals working < 40 hours a week (Table 2). This suggests that working 40 hours or more a week is significantly associated with obesity when compared to individuals working < 40 hours a week. The results from the logistic regression also indicated that the odds of obesity among individuals who graduated high school or obtained their GED were 38.1% significantly greater than the odds of obesity for individuals having less than a high school education level (OR=1.381; 95% CI: 1.07–1.79). The odds of obesity were significantly greater for participants who identified as Non-Hispanic Black (OR 1.598, 95% CI: 1.25–2.05) or Hispanic (OR 1.611, 95% CI: 1.16–2.24) compared to participants who identified as Non-Hispanic White, after adjusting for all the other independent variables in the model. In addition, the odds of obesity for those who identified as Non-Hispanic Asian were 82.3% (OR=0.177; 95% CI: 0.13–0.25) significantly lower than the odds of obesity among participants who identified as Non-Hispanic White. Physical activity was taken into account in the analysis in the form of MET for leisure, and physical activity was significantly associated with the outcome of interest (OR=0.9997; 95% CI: 0.9997– 0.9998).
Discussion
The findings of this study show that there are decreased odds of obesity when working less than 40 hours a week compared to the standard 40-hour workweek and overtime, which is consistent with findings from Courtamanche for a cohort followed from 1979 to 2004.16 After testing for interaction, it was found that physical activity status does not significantly modify the association between the number of hours worked and obesity.
One potential explanation for this relationship between hours worked per week and obesity status is that the prevalence of obesity has been growing in the United States because people are less physically active in their jobs than they used to be.23,34 Philipson and Posner suggested that technology increased the efficiency of food production, thereby lowering food prices resulting in increased food consumption.24 The combination of increased food consumption and less physical activity at work widens the gap between calories consumed and calories burned, favoring the development of obesity.24,25 With people moving less overall in their jobs (which are a substantial part of their waking hours), they are more likely to be at risk for obesity. In 1950, there were about 30% more persons in high-activity occupations than low-activity occupations, but by 2000 there were approximately twice as many people in low-activity populations than high activity populations.26 If a person is using extra hours in the day to be at work, the number of hours left for leisure is reduced. Common explanations reported for inactivity are “lack of time” and “work demands.”27 These factors could potentially lead to individuals being more focused on relaxing and sedentary activities instead of physically demanding activities that take up energy and time.
There are studies that show similar conclusions of a consistent relationship between hours worked and factors favoring the development of obesity.6,27,28 One study by Au, Hack, and Hollingsworth28 used data from 1998 in Australia and found that among employed women aged 45–50, those who worked 35–40 hours per week were more likely to engage in no physical activity (29.4%) compared to women who worked fewer hours (24.7%).28 The authors concluded that women who work over 40 hours a week are more likely to make lifestyle choices associated with weight gain.28 Another study done in Australia by Burton and Turrell27 used data from 1995 and had findings that differed by gender, with females having a higher rate of insufficient activity for recommended levels than males in the study. Among males, the findings suggested a relationship between working more than 40 hours per week and an increased proportion of participants being insufficiently active (at the bivariate level), which could favor the development of obesity.27 A study done by Cook and Gazmararian6 using Georgia BRFSS data from 2015 suggests that the physical activity level at work in combination with hours spent at work may have an effect on obesity.6 They found that work hours varied significantly across occupational activity groups with employees in low physical activity occupations having the longest work hours, favoring the development of obesity. One of the limitations of Cook and Gazmararian6 article is that the analyses used BMI values calculated based on respondents’ self-reported measurements of weight and height, introducing bias and potentially an underestimation in overall prevalence of obesity in their sample. The current study confirms and extends the work of Cook and Gazmararian by using a national data set and reliable measures of height and weight in NHANES.
Inconsistent with the results found in the current study, Burton and Turrell concluded that regardless of gender, Australians in blue collar occupations (manual labor) were more likely to be insufficiently active, favoring the development of obesity, compared to those in professional occupations (managers and administrators, professionals, and paraprofessionals) from 1995 data.27 This is counterintuitive because the level of typical occupational physical activity for blue collar workers was higher compared to white collar workers (clerks, salespersons, and personal service workers) and the variability was not explained by the time spent in work.27 The findings from the current study are inconsistent with this finding in that those with more than high school education, therefore typically having more professional occupations, are more likely to be obese compared to those with less than a high school degree.
The major limitation of this study is that occupational activity level was not included in the analysis. The closest variable in the NHANES dataset for the 2015–2016 wave was vigorous or moderate “work activity”. The term “work” in the context of this variable refers to things that you have to do such as paid and unpaid work, household chores, and yard work. Thus, this variable does not specifically capture occupational activity. Even if it did, occupational activity variables have been shown to not be valid or reliable. Cook and Gazmararian stated that evidence of the validity of inferences comparing the BRFSS physical activity questionnaire with accelerometer data they used were fair to poor across all measures of occupational activity.6 King used definitions from the US Department of Labor as a reference to assign each of the 40 occupational categories into three groups being high occupational activity (OA) (7), low OA (10), and the remaining 23 occupational groups were labeled as an unclassified amount of OA, which was then excluded from analysis.15 In his limitations he noted that actual intensity level of an occupation was not measured and energy cost was not quantified in his variable of occupational activity.15 Additionally, diet indicators should have been included as potential covariates because they are important to look at in conjunction with obesity. In addition, the type of occupation and shift work was not included in the analyses since this information was not available in the dataset. Lastly, the nature of the data collection was cross-sectional which limits the causal inference of the finding. It could be that individuals self-select into the different activity level jobs due to physical limitations from disability and injury which could prevent them from working in an occupation that is more physically demanding. It could also be that those who work longer hours were less likely to take the survey due to higher work demands. This scenario would end up underestimating the effect of long hours on obesity.
Some strengths of this study include that the survey itself was a robust instrument distributed and randomized at the national level. Findings can be generalized because the selection process for NHANES is well-designed and the sample is representative of the study population. It was beneficial that along with the questionnaire, there were trained technicians who worked in the mobile examination unit to get objective body measurements that were then translated into BMI instead of being self-reported. Another strength is that the final study sample size of 2,581 is relatively large.
SO WHAT?
What is already known about this topic?
US residents’ health may be suffering from being overworked. Obesity may be rampant in the US also because adults are so overworked not having the energy/time to choose active pastimes.
What does this article add?
This research displays the need to offer support for health promotion interventions to increase physical activity in the workplace and/or active transport options to increase activity levels.6,30
What are the implications for health promotion practice or research?
Ease of access to healthier food options and health benefits of shorter work week hours needs to be longitudinally investigated. Future research will also need to examine whether this association between hours worked per week and obesity status is mediated by specific dietary factors since being overworked may affect substituting home-made meals with convenient fast food and pre-packaged/processed meals16, resulting in higher levels of calorie consumption and obesity.29
Acknowledgments
Funding
This work was supported in part by the National Institute for General Medical Sciences (NIGMS) in the National Institutes of Health (NIH), grant number P20GM121341. This content is solely the responsibility of the authors and does not necessarily represent the official views of the NIGMS or NIH.
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016 NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics; 2017 [PubMed] [Google Scholar]
- 2.Gregg EW, Shaw JE. Global health effects of overweight and obesity. The New England Journal of Medicine. 2017;377(1):80–81. [DOI] [PubMed] [Google Scholar]
- 3.Journal of the National Medical Association. Obesity declared an epidemic in the United States. Journal of the National Medical Association. 1999;91(12):645.10628122 [Google Scholar]
- 4.Dicker RC, Coronado F, Koo D, Parrish RG. Principles of epidemiology in public health practice; an introduction to applied epidemiology and biostatistics. Centers of Disease Control and Prevention, Atlanta, GA: (2006) [Google Scholar]
- 5.Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89(6):2583–2589. [DOI] [PubMed] [Google Scholar]
- 6.Cook MA, Gazmararian J. The association between long work hours and leisure-time physical activity and obesity. Prev Med Rep 2018;10:271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pigeyre M, Rousseaux J, Trouiller P, et al. How obesity relates to socio-economic status: Identification of eating behavior mediators. Int J Obes (Lond). 2016;40(11):1794–1801. [DOI] [PubMed] [Google Scholar]
- 8.Bonauto DK, Lu D, Fan ZJ. Obesity prevalence by occupation in Washington State, Behavioral Risk Factor Surveillance System. Prev Chronic Dis 2014;11:130219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Prevalence of self-reported physically active adults--United States, 2007. MMWR Morb Mortal Wkly Rep 2008;57(48):1297–1300. [PubMed] [Google Scholar]
- 10.Steeves JA, Bassett DR, Thompson DL, Fitzhugh EC. Relationships of occupational and non-occupational physical activity to abdominal obesity. Int J Obes (Lond). 2012;36(1):100–106. [DOI] [PubMed] [Google Scholar]
- 11.Jans MP, Proper KI, Hildebrandt VH. Sedentary behavior in Dutch workers: Differences between occupations and business sectors. Am J Prev Med 2007;33(6):450–454. [DOI] [PubMed] [Google Scholar]
- 12.Ki M, Pouliou T, Li L, Power C. Physical (in)activity over 20 y in adulthood: associations with adult lipid levels in the 1958 British birth cohort. Atherosclerosis. 2011;219(1):361–367. [DOI] [PubMed] [Google Scholar]
- 13.Miller R, Brown W. Steps and sitting in a working population. Int J Behav Med 2004;11(4):219–224. [DOI] [PubMed] [Google Scholar]
- 14.Mummery WK, Schofield GM, Steele R, Eakin EG, Brown WJ. Occupational sitting time and overweight and obesity in Australian workers. Am J Prev Med 2005;29(2):91–97. [DOI] [PubMed] [Google Scholar]
- 15.King GA, Fitzhugh EC, Bassett DR, et al. Relationship of leisure-time physical activity and occupational activity to the prevalence of obesity. Int J Obes Relat Metab Disord. 2001;25(5):606–612. [DOI] [PubMed] [Google Scholar]
- 16.Courtemanche C Longer hours and larger waistlines? The relationship between work hours and obesity. Forum for Health Economics and Policy. 2009. Vol. 12, No.2 [Google Scholar]
- 17.Dunton GF, Berrigan D, Ballard-Barbash R, Graubard B, Atienza AA. Joint associations of physical activity and sedentary behaviors with body mass index: Results from a time use survey of US adults. Int J Obes (Lond). 2009;33(12):1427–1436. [DOI] [PubMed] [Google Scholar]
- 18.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugiyama T, Healy GN, Dunstan DW, Salmon J, Owen N. Joint associations of multiple leisure-time sedentary behaviours and physical activity with obesity in Australian adults. Int J Behav Nutr Phys Act 2008;5:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lebowitz S Here’s how the 40-hour workweek became the standard in America. Business Insider; 2015;24:2015 [Google Scholar]
- 21.Centers for Disease Control and Prevention. Defining adult overweight and obesity. https://www.cdc.gov/obesity/adult/defining.html. Accessed Mar 15, 2019.
- 22.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: 2011–2012 Data Documentation, Codebook, and Frequencies. 2015. [Google Scholar]
- 23.Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010;85(12):1138–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Philipson TJ, Posner RA. The long-run growth in obesity as a function of technological change. Perspect Biol Med. 2003;46(3 Suppl):S87–107. [PubMed] [Google Scholar]
- 25.Lakdawalla D and Philipson T The growth of obesity and technological change: a theoretical and empirical examination.” National Bureau of Economic Research; 2002. (No. w8946). [Google Scholar]
- 26.Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421–443. [DOI] [PubMed] [Google Scholar]
- 27.Burton NW, Turrell G. Occupation, hours worked, and leisure-time physical activity. Prev Med. 2000;31(6):673–681. [DOI] [PubMed] [Google Scholar]
- 28.Au N, Hauck K, Hollingsworth B. Employment, work hours and weight gain among middle-aged women. Int J Obes (Lond). 2013;37(5):718–724. [DOI] [PubMed] [Google Scholar]
- 29.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tigbe WW, Lean ME, Granat MH. A physically active occupation does not result in compensatory inactivity during out-of-work hours. Prev Med. 2011;53(1–2):48–52. [DOI] [PubMed] [Google Scholar]