EXECUTIVE SUMMARY
In 2012 and 2013, the World Small Animal Veterinary Association (WSAVA) Vaccination Guidelines Group (VGG) undertook fact‐finding visits to several Asian countries, with a view to developing advice for small companion animal practitioners in Asia related to the administration of vaccines to dogs and cats. The VGG met with numerous first opinion practitioners, small animal association leaders, academic veterinarians, government regulators and industry representatives and gathered further information from a survey of almost 700 veterinarians in India, China, Japan and Thailand. Although there were substantial differences in the nature and magnitude of the challenges faced by veterinarians in each country, and also differences in the resources available to meet those challenges, overall, the VGG identified insufficient undergraduate and postgraduate training in small companion animal microbiology, immunology and vaccinology. In most of the countries, there has been little academic research into small animal infectious diseases. This, coupled with insufficient laboratory diagnostic support, has limited the growth of knowledge concerning the prevalence and circulating strains of key infectious agents in most of the countries visited.
Asian practitioners continue to recognise clinical infections that are now considered uncommon or rare in western countries. In particular, canine rabies virus infection poses a continuing threat to animal and human health in this region. Both nationally manufactured and international dog and cat vaccines are variably available in the Asian countries, but the product ranges are small and dominated by multi‐component vaccines with a licensed duration of immunity (DOI) of only 1 year, or no description of DOI. Asian practitioners are largely unaware of current global trends in small animal vaccinology or of the WSAVA vaccination guidelines. Consequently, most practitioners continue to deliver annual revaccination with both core and non‐core vaccines to adult animals, with little understanding that “herd immunity” is more important than frequent revaccination of individual animals within the population.
In this paper, the VGG presents the findings of this project and makes key recommendations for the Asian countries. The VGG recommends that (1) Asian veterinary schools review and increase as needed the amount of instruction in small animal vaccinology within their undergraduate curriculum and increase the availability of pertinent postgraduate education for practitioners; (2) national small animal veterinary associations, industry veterinarians and academic experts work together to improve the scientific evidence base concerning small animal infectious diseases and vaccination in their countries; (3) national small animal veterinary associations take leadership in providing advice to practitioners based on improved local knowledge and global vaccination guidelines; (4) licensing authorities use this enhanced evidence base to inform and support the registration of improved vaccine product ranges for use in their countries, ideally with DOI for core vaccines similar or equal to those of equivalent products available in western countries (i.e. 3 or 4 years).
The VGG also endorses the efforts made by Asian governments, non‐governmental organisations and veterinary practitioners in working towards the goal of global elimination of canine rabies virus infection. In this paper, the VGG offers both a current pragmatic and future aspirational approach to small animal vaccination in Asia. As part of this project, the VGG delivered continuing education to over 800 Asian practitioners at seven events in four countries. Accompanying this document is a list of 80 frequently asked questions (with answers) that arose during these discussions. The VGG believes that this information will be of particular value to Asian veterinarians as they move towards implementing global trends in small companion animal vaccinology.
INTRODUCTION
The World Small Animal Veterinary Association (WSAVA) Vaccination Guidelines Group (VGG) was established in 2004 with the task of producing globally applicable advice for small companion animal veterinary practitioners on best practice for vaccination of pet dogs and cats. The VGG first released vaccination guidelines for veterinarians in 2007 (Day et al. 2007) and these were updated in 2010 (Day et al. 2010). The 2010 revision was accompanied by a separate document providing information on vaccination for the owners and breeders of dogs and cats and by a series of infectious disease “fact sheets” designed to be used by veterinarians during an annual health check consultation (http://www.wsava.org/educational/vaccination-guidelines-group).
In 2012, the VGG began a new 2‐year project that focussed on the vaccination requirements of small companion animals in Asia. The project, which was completed in late 2013, was born of the recognition that there are many unique political, educational and scientific challenges in the Asian countries that may not have been addressed specifically by the previous documents produced by the VGG. The present paper represents the final outcome from this Asian study. It summarises the key challenges faced by small companion animal veterinary practitioners in those parts of Asia studied (many of which may be extrapolated to other Asian countries) and makes a series of recommendations for future actions that might benefit the profession, pet owners and dogs and cats in these countries.
METHODOLOGY
The membership of the VGG was revised for the duration of the Asian project. Core members of the committee (M. J. Day and R. D. Schultz) were joined by experts with first‐hand experience of the Asia‐Pacific region (H. Tsujimoto, R. Squires and U. Karkare). The principal aim of the project was to gather as much information concerning small companion animal practice, infectious disease and vaccination as possible, to form a firm basis for the recommendations to be made subsequently. To that end, in 2012 to 2013, the VGG undertook a series of fact‐finding visits to Japan (Tokyo and Osaka), India (Delhi and Mumbai), China (Beijing and Shanghai) and Thailand (Bangkok). Each of these visits was similarly structured and involved formal discussions with groups including (1) first opinion veterinary practitioners; (2) representatives of small animal veterinary associations and veterinary licensing boards; (3) veterinary academics teaching and conducting research in microbiology, immunology and companion animal medicine and the Deans of several veterinary schools; (4) government officials responsible for the assessment and licensing of small companion animal vaccines; and (5) representatives of international and national vaccine manufacturers and distributors. Given the importance of canine rabies in Asia, the VGG also met with the Deputy Director of the International Organisation for Animal Health (OIE) in the Asia‐Pacific region, the Chairman of the Animal Welfare Board of India, and the founder of a major non‐governmental organisation undertaking a rabies control programme in Sri Lanka (the Blue Paw Trust). The formal meetings were supplemented with site visits to 12 small animal practices (of a range of size and standards) in India and China. Outwith these committee visits, during 2013, the Chair of the VGG (M. J. Day) also discussed vaccination policy with the small animal veterinary association of South Korea and spoke with practitioners during visits to Hong Kong, Indonesia and Malaysia.
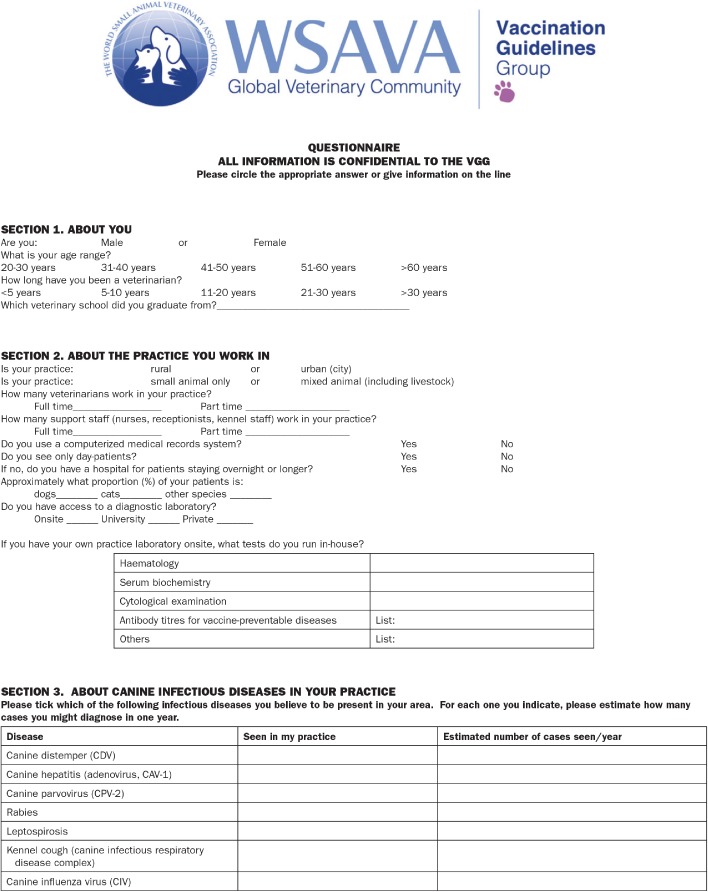
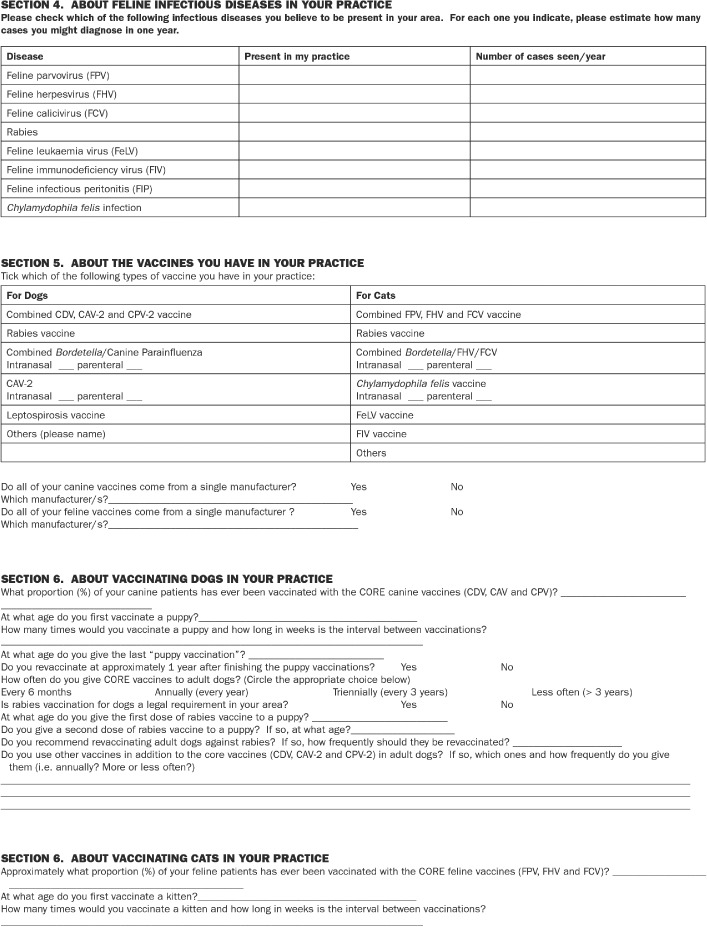
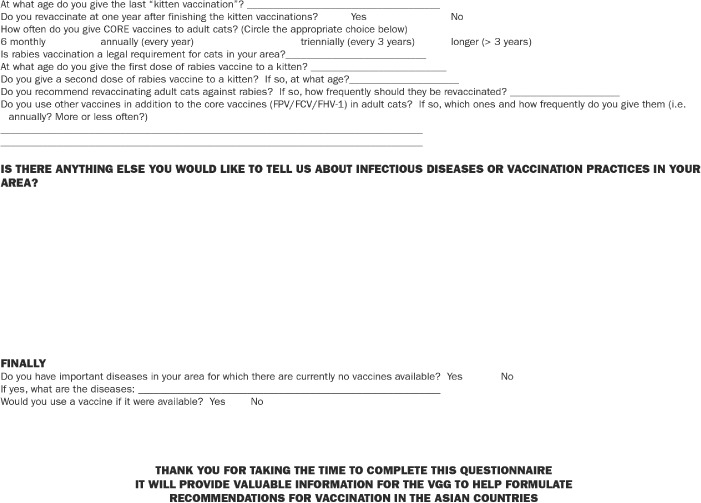
In order to expand the information gained from these face‐to‐face meetings, the VGG developed a questionnaire for distribution among first opinion practitioners in the various countries (Appendix VGG ASIAN QUESTIONNAIRE SURVEY). In each country surveyed, the questionnaire was translated, administered anonymously and the responses analysed and summarised (in English) by members of local small animal veterinary associations. Through these surveys, the VGG gathered information about (1) the responding practitioners, (2) veterinary practices and their diagnostic laboratory access, (3) canine and feline infectious diseases seen in the practices, and (4) canine and feline vaccines and vaccination protocols used in the practices. Responses to the surveys were excellent with data from 113 practitioners in Japan, 144 practitioners in India, 150 practitioners in China and 267 practitioners in Thailand. The questionnaire was also provided to small animal veterinary associations in Sri Lanka, Malaysia, Indonesia and Vietnam but no responses have been received to date.
One of the specific aims of the project was to start to deliver continuing education (CE) in small companion animal vaccinology to Asian practitioners. Therefore, at each location visited, VGG members provided a half‐day of CE consisting of a series of lectures accompanied by written (and translated) notes. At each event, the results of the local questionnaire survey were presented by a representative of a local practitioner association. Over the course of the project, these events gave the VGG direct contact with over 800 Asian practitioners, with attendances of 370 in Japan, 180 in India, 180 in China and 80 in Thailand. During the active discussions that formed part of each meeting, a number of important “frequently asked questions” emerged and these (with answers) are given as an appendix (Appendix FREQUENTLY ASKED QUESTIONS) to this document.
CURRENT SITUATION IN ASIA
Veterinary education in Asia
Discussions with Deans, academic teachers and researchers from a total of 14 veterinary schools in the four countries revealed substantial differences between national curricula, in particular with respect to the inclusion of teaching related to small companion animal infectious disease, medicine and surgery. In India and China, veterinary schools are charged with providing practitioners to service the production animal industry and public health. Very little tuition related to small companion animal disease is provided and few academic staff have strong interest or expertise in small animal clinical studies. Therefore, practitioners working in this sector have largely gained their knowledge via postgraduate education. With the exception of some individuals who have worked abroad in other Asian countries or further afield, this postgraduate knowledge is largely gained from CE events provided by the veterinary associations. In Japan and Thailand, there is significantly greater development of small companion animal curricula, supported by well‐equipped teaching hospitals and designated academic staff; however, even in these countries, there are relatively few veterinary clinical specialists holding North American or European board certification, and the Asian Board of Veterinary Specialties, and associated speciality colleges, has only been established relatively recently. It was also notable that academics in the Japanese and Thai schools highlighted that there was less than optimal teaching of core clinical practice skills related to the client consultation and the delivery of vaccinations within that setting.
Small animal infectious disease in Asia
In the four countries visited, some common themes emerged concerning small companion animal infectious diseases. With the exception of canine rabies (which should be notified to the OIE, although it is widely recognised that gross under‐reporting occurs), there is little or no formal surveillance for small companion animal infectious diseases conducted by government, industry or academia. With some notable exceptions, particularly in Japan, there are very few academic staff who conduct research or publish in the area of small companion animal infectious diseases or vaccinology. This also means that practitioners in these countries have insufficient access to research‐led diagnostic laboratories that might help confirm diagnoses of infectious diseases in challenging, individual patients. Private diagnostic laboratories are also relatively uncommon in some countries; for example, an international group has only recently established the first veterinary diagnostic laboratory in Shanghai. In India, there are private laboratories only in Delhi and Mumbai. Many practitioners therefore rely on in‐practice diagnostic test kits, often manufactured in Asia, for detection of infectious agent antigen or antibody. The VGG identified few peer‐reviewed publications dealing with small companion animal infectious diseases and vaccinology that originated from India, China and Thailand. Some key manuscripts, brought to the attention of the VGG, are given as Appendix SELECTED KEY PAPERS HIGHLIGHTED TO THE VGG DURING MEETINGS. This situation, which is particularly acute in India and China, relates largely to two factors: (1) academics are not encouraged or supported to investigate diseases of small companion animals within institutions that have a production animal focus and (2) there are virtually no sources of research funding that might permit the investigation of small companion animal diseases.
In that respect, the data provided by the VGG survey questionnaire are particularly valuable. Although there are doubtless flaws in such questionnaire‐derived data, the collective experience of almost 700 first opinion practitioners provides a useful overview of the perceived occurrence of key infectious diseases in dogs and cats in these four countries (Tables 1 and 2). Practitioners in these countries continue to recognise small companion animal infectious diseases, many of which are now uncommon or rare in western countries.
Table 1.
Overview of vaccine‐preventable canine infectious diseases seen in veterinary practice
| Disease | % Practitioners reporting in Japan | % Practitioners reporting in India | % Practitioners reporting in Beijing | % Practitioners reporting in Shanghai | % Practitioners reporting in Thailand |
|---|---|---|---|---|---|
| CDV | 44 · 2 | 73 | 100 | 94 | 96 · 2 |
| CAV | 17 · 7 | 76 | 34 | 60 | 27 · 7 |
| CPV‐2 | 75 · 2 | 100 | 93 | 86 | 95 · 5 |
| Leptospirosis | 30 · 1 | 56 | 23 | 28 | 33 · 3 |
| Canine infectious respiratory disease complex | 76 · 1 | 28 | 87 | 66 | 70 · 8 |
| Rabies | 0 | 63 | 9 | 0 | 26 · 6 |
| Number of survey respondents | 113 | 144 | 100 | 50 | 267 |
Table 2.
Overview of vaccine‐preventable feline infectious diseases seen in veterinary practice
| Disease | % Practitioners reporting in Japan | % Practitioners reporting in India | % Practitioners reporting in Beijing | % Practitioners reporting in Shanghai | % Practitioners reporting in Thailand |
|---|---|---|---|---|---|
| FPV | 57 · 5 | 71 | 93 | 76 | 88 · 4 |
| FHV‐1 | 96 · 5 | Not reported | 86 | 62 | 71 · 2 |
| FCV | 88 · 5 | 29 | 86 | 38 | 71 · 5 |
| Feline leukaemia virus | 92 | 74 | 43 | 44 | 75 · 3 |
| Feline immunodeficiency virus | 96 · 5 | 15 | 34 | 36 | 68 · 9 |
| Rabies | 0 | 2 | 3 | 0 | 9 · 7 |
| Number of survey respondents | 113 | 144 | 100 | 50 | 267 |
The control of canine rabies is a major issue faced by small companion animal practitioners in many Asian countries. The disease has been eliminated in Japan and is rare in Thailand, but is still highly prevalent in India and, to a lesser extent, in China. There is a minimum estimate of 20,000 human deaths from rabies each year in India and the prevalence of disease relates to the challenges of controlling and vaccinating an estimated population of 25 million free‐roaming dogs in that country. The work of numerous NGOs working in various Asian countries has clearly shown that disease can be controlled where at least 70% of the free‐roaming dog population can be vaccinated, but this target has only been achieved in selected cities and regions. The veterinary practitioners met by the VGG in the various countries are all highly committed to the goal of global elimination of canine rabies virus infection and many of them are actively engaged in pro‐bono vaccination within their own practice areas.
Vaccines and vaccination practice in Asia
The small animal veterinary associations in the Asian countries visited, as members of WSAVA, were aware of the WSAVA vaccination guidelines and had discussed these in committee; however, the recommendations had not been actively promoted among association memberships. In Japan and Thailand, academic teachers were also well informed about the guidelines and some had started to include the WSAVA recommendations in their teaching. However, most first opinion practitioners in India and China were unaware of the global trends for change in small companion animal vaccination practice. In all of the Asian countries visited, most practitioners continue to adhere to an annual revaccination programme in which all core and non‐core components are administered, often with multi‐component products containing numerous antigens. In part, this is reinforced by the erroneous belief that in areas of “high infectious disease pressure”, individual animals may be better protected by more frequent administration of vaccines. Although practitioners understand the concept of “herd immunity” in the context of mass vaccination campaigns for the control of canine rabies, there is little sense that herd immunity applies also to other key infectious diseases.
Together with insufficient education in vaccinology (both at the university and CE levels) and limited access to translated versions of WSAVA and other pertinent guidelines, there are other barriers that currently impede progress with respect to adoption of modern vaccination practices, as has occurred in many countries. The first of these relates to the availability of vaccines with a licensed duration of immunity (DOI) of more than 1 year and the availability of product ranges that permit separate administration of core vaccines (no more frequently than every 3 years) and non‐core vaccines (annually where a risk–benefit analysis deems that they are essential for the individual animal). In most Asian countries, vaccines are supplied by the major international companies and by national manufacturers. Most of the core vaccines produced by national manufacturers carry a 1‐year licensed DOI or lack a definitive description of DOI, as do the majority of international vaccines, despite the fact that the same international products in many other countries have a 3‐ or 4‐year licensed DOI.
The second major problem is that these issues are reinforced by the inflexibility of the national vaccine licensing authorities. In some countries, there appears to be a “protectionist” approach whereby nationally produced products are permitted but the equivalent international vaccines are not allowed to be imported. The international suppliers have challenges in bringing their products to these countries, where licensing authorities often demand a new and country‐specific data package, including epidemiological evidence that a particular infectious disease exists and is of significant concern in the country. Generating such data is difficult in the absence of an appropriate research infrastructure (as discussed earlier). This situation is exemplified by the fact that there are currently no licensed feline vaccines available in India. This has necessitated individual practitioners or distributors sourcing foreign vaccine and importing it into the country. Similarly, in China, there is only one international feline core vaccine combination available on the market.
There is also reluctance by licensing authorities to accept that an international vaccine with licensed 3‐year DOI in most countries should be used triennially in the local situation. This situation is particularly frustrating with respect to canine rabies vaccines. In many Asian countries, there is a legal requirement for annual rabies vaccination of dogs (but not cats) and this is sometimes linked to the registration of dogs. In a situation where a nationally produced vaccine with a 1‐year DOI is the only product available, this might be understandable; however, it is difficult to accept that international products, successfully used in triennial programmes in many other countries, must be administered annually to owned pet animals purely because of legal requirements.
A further issue, identified by the VGG during discussions and practice visits, relates to the concept of “vaccine husbandry” in some Asian countries. It is our belief that “vaccine failure” due to inappropriate storage or administration of products in the practice is common in some Asian countries and that this again reflects a lack of fundamental education in this area. In some countries, vaccines are transported long distances from the point of manufacture or importation to the veterinary practice. Most practitioners are well aware of the concept of the “cold chain”. However, practitioners may be too quick to blame a breakdown in the cold chain before delivery to the practice for vaccine failure and do not necessarily appreciate the monitoring measures that are put in place by the suppliers of international vaccines. The VGG has identified a number of practices related to vaccine storage and usage by practitioners, which have been highlighted in simple guidelines for correct vaccine husbandry (Table 3).
Table 3.
Vaccine husbandry: key points for veterinary practitioners
|
VGG RECOMMENDATIONS FOR ASIA
Education
The VGG believes that veterinary schools, or in some Asian countries those responsible for the content of a national veterinary curriculum, should consider the inclusion of increased curricular content in small animal infectious diseases, basic immunology and vaccinology. The inclusion or enhancement of teaching related to client communication skills and companion animal practice management should also be considered. Veterinary students should be taught practical vaccination approaches founded in the principles that underpin the WSAVA vaccination guidelines.
The VGG encourages the national small animal veterinary associations to promote the principles of the WSAVA vaccination guidelines to their membership. National associations should form their own expert committees to evaluate the WSAVA guidelines and use them as a basis to formulate national recommendations that account for differences in the field situation in each country. This process was widely adopted by other countries after the release of the 2007 WSAVA vaccination guidelines and reported in the 2010 document (Day et al. 2010).
The VGG recommends that, wherever possible, postgraduate education in small animal vaccinology should be made available to small animal practitioners in the Asian countries. The small animal associations should lead in this area in collaboration with industry veterinarians who might be encouraged to support financially the development of such CE.
Research
Academic veterinary microbiologists and immunologists in the Asian countries should be encouraged to work together with industry and practitioner associations to coordinate the generation of national data to provide fundamental knowledge about the prevalence of key infectious agents in the Asian countries. Such knowledge is currently not available and is often requisite for the introduction of vaccines into a country. In the specific case of leptospirosis, these groups should work together to determine the circulating serovars that are relevant in each country, in order to inform future vaccine development. Furthermore, collaborative research should be conducted that provides proof to veterinarians and governmental regulators as to the efficacy of international modified live virus (MLV) core vaccines when used less frequently than annually (e.g. every 3 or 4 years).
The importance of such research, particularly where it has a One Health dimension (i.e. for canine rabies or leptospirosis), should be recognised and suitably rewarded by academic institutions. Academics who choose to investigate small companion animal infectious diseases should not be regarded as performing research that is less significant than that related to production animal science.
Vaccine supply
The VGG suggests that veterinarians, animal owners and animals in Asian countries should be able to benefit from availability of companion animal vaccines produced by major global manufacturers that have been proven to be safe and efficacious. Restrictive practices by governments, which favour national producers or require the generation of national disease prevalence data, are unlikely to improve the welfare of pets.
Industry should be encouraged to increase the range of products they market within the Asian countries to enable practitioners to develop triennial core/annual non‐core programmes in accordance with WSAVA and other international guidelines. This would necessitate the introduction of vaccines with fewer components and separate core and non‐core vaccines, as are available in many other countries. Where these international products carry a 3‐ or 4‐year licensed DOI in other countries, industry should make every effort to work with local regulatory authorities to prove the efficacy of their products and to update the vaccine claims and datasheets in the Asian countries.
Vaccine husbandry
The VGG recommends that small companion animal practitioners in the Asian countries be educated in the fundamental aspects of storage and use of veterinary vaccines. To that end, we have produced a list of key requirements that we hope will be widely distributed to practitioners and taught within veterinary undergraduate curricula (Table 3).
An aspirational vaccination protocol for Asian practitioners
Veterinarians in Asian countries should be encouraged to implement the basic fundamentals of modern companion animal vaccinology as presented in the WSAVA vaccination guidelines (Day et al. 2010) (Table 4). In particular, practitioners should be educated in understanding the concept of core versus non‐core vaccines. Core vaccines are those that every dog or cat must receive as they protect the animal from prevalent diseases that may be lethal or induce significant morbidity. Non‐core vaccines are those that might be administered to individual animals whose geographical location or lifestyle places them at risk of contracting those particular infections. Non‐core vaccines are not required by every animal and should not be used where there is no evidence that the related disease exists in a country. The VGG also describes some vaccines as not recommended (where there is judged to be insufficient scientific evidence to justify their use). For individual‐owned pet animals in a domestic environment, the current WSAVA vaccination guidelines should be applied when quality‐assured MLV core vaccines are used in a practice. The VGG is unable to comment on whether nationally produced vaccines confer equivalent protection to those available internationally because of a lack of published, peer‐reviewed data.
Table 4.
An aspirational vaccination programme for Asian practitioners
| Type of vaccine | Puppy or kitten vaccination | Adult animal revaccination |
|---|---|---|
|
Quality‐assured core MLV vaccines For dogs including CDV, CAV‐2 and CPV‐2 For cats including FPV, FCV and FHV‐1 |
Start at 8 to 9 weeks of age with first vaccine; give a second vaccine 3 to 4 weeks later with a third vaccine to be given at 16 weeks of age or older A booster vaccine should be given 12 months later or at 12 months of age |
Revaccination with core, quality‐assured MLV vaccines should be no more frequent than every 3 years. Serology might be used to monitor protective immunity (for CDV, CAV, CPV and FPV) and aid decision making on revaccination intervals The single exception to this may be cats at high risk of contacting upper respiratory virus, in which these components may be given annually |
| Quality‐assured canine rabies vaccine for dogs or cats | According to datasheet recommendations; one dose from 12 weeks of age. The VGG recommends that in high‐risk areas a second dose may be given 4 weeks later | Quality‐assured canine rabies vaccines all carry a 3‐year licensed DOI in most countries outside of Asia |
|
Non‐core vaccines Examples for dogs: Leptospira, canine infectious respiratory disease complex (kennel cough) Examples for cats: feline leukaemia virus, Bordetella or Chlamydophila |
Give according to the manufacturer's recommendations: generally two doses 2 to 4 weeks apart | Non‐core vaccines are generally given annually unless the datasheet specifically recommends otherwise (e.g. some quality‐assured FeLV vaccines carry a longer DOI) |
|
Not recommended vaccines These include vaccines against coronavirus (canine or feline), feline immunodeficiency virus and Giardia |
The generic information in this table should be read in conjunction with the more detailed recommendations provided in the current WSAVA vaccination guidelines (Day et al. 2010). Vaccination according to WSAVA guidelines is possible only where available product ranges separate core from non‐core vaccine components. Note that these recommendations apply only to quality‐assured vaccines, most of which are produced by large, international companies
Increasing the frequency of vaccination does not provide greater protection to an individual animal and may increase the risk of an adverse reaction. In areas of high infectious disease pressure, it is much more important to ensure that as many of the target population as possible are vaccinated (i.e. increase herd immunity) than to increase the frequency of vaccinations given to individual animals. With respect to international core MLV vaccines, key changes to current protocols would be introduction of a final puppy and kitten primary core vaccination at or after 16 weeks of age and revaccination of adult dogs and cats with MLV core vaccines no more frequently than every 3 years. The unnecessary annual use of international MLV core revaccination may be regarded as an inappropriate use of limited client financial resources that may be better applied to address other health issues in the pet. Even though the international products in most Asian countries do not carry datasheet recommendations for use in this way, it would be useful if local professional guidance permitted practitioners to use these products “off label” with informed client consent. This approach was used successfully for a number of years in other countries before datasheet recommendations were updated. As discussed earlier, the VGG hopes that in due course the international core MLV vaccines will have datasheet changes made in the Asian countries.
The use of non‐core vaccines in an individual animal should be based on available local knowledge of the prevalence of the pertinent infectious disease(s) and the risk of that individual animal's lifestyle placing it in contact with the pertinent infectious agent(s). These are currently difficult decisions for Asian practitioners, where there is such a small scientific evidence base related to the regional distribution of these infectious agents.
A pragmatic current vaccination protocol for Asian practitioners
The ability of small companion animal practitioners in Asia to adopt the current WSAVA vaccination guidelines is hampered by the issues of product availability, product licensed DOI and knowledge of infectious disease prevalence and risks. In many countries, there is a limited range of international multi‐component canine vaccines incorporating both core and non‐core antigens, and where feline vaccines are available at all, the product range is similarly limited. Practitioners should begin to understand that while current datasheet recommendations for international MLV core vaccines recommend annual revaccination of adult animals, the same vaccines are given triennially in many other countries. Practitioners and their national associations should therefore continue to lobby industry and government regulators for changes that will bring recommendations concerning international products into line with current global standards and practices. Table 5 presents some pragmatic recommendations that may assist Asian practitioners make the transition from the current situation to the newer global trends in small animal vaccinology.
Table 5.
A pragmatic vaccination programme for Asian practitioners in 2014
| Type of vaccine | Aim | Puppy or kitten vaccination | Adult animal revaccination |
|---|---|---|---|
| Core vaccines for dogs and cats |
Select a quality‐assured MLV product that allows the minimum combination of core antigens to be given (CDV, CAV‐2, CPV‐2 for dogs; FPV, FHV‐1, FCV for cats) Use an alternative diluent rather than reconstitute with a non‐core vaccine if that non‐core vaccine is not essential for that animal |
Start at 8 to 9 weeks of age with first vaccine; give a second vaccine 3 to 4 weeks later with a third vaccine to be given at 16 weeks of age or older A booster vaccine should be given 12 months later or at 12 months of age |
Discuss with clients the new global approach to core revaccination and obtain consent for administration of core quality‐assured MLV vaccine no more often than every 3 years The single exception to this may be cats at very high risk of contacting upper respiratory virus. These cats might be vaccinated annually, but be aware that the FPV component of the vaccine combination is not actually required |
| Canine rabies vaccine for dogs or cats | Select a quality‐assured product if available | According to datasheet recommendations; one dose from 12 weeks of age. The VGG recommends that in high‐risk areas a second dose may be given 4 weeks later | Conform to local legal requirements for annual revaccination, but continue to actively lobby associations and governments to allow triennial revaccination using quality‐assured products with a licensed 3‐year DOI. Continue to lobby industry to register these products with a 3‐year DOI in your country |
|
Non‐core vaccines Examples for dogs: Leptospira, canine infectious respiratory disease complex (kennel cough) Examples for cats: feline leukaemia virus, Bordetella or Chlamydophila |
Discuss the individual animal's lifestyle and exposure risk with the client – is the vaccine really necessary for this animal? Choose a quality‐assured product that contains just the desired antigen or the antigen in the least possible combination with other non‐essential components |
Give according to the manufacturer's recommendations: generally two doses 2 to 4 weeks apart | Non‐core vaccines are generally given annually unless the datasheet specifically recommends otherwise |
|
Not recommended vaccines These include vaccines against coronavirus (canine or feline), feline immunodeficiency virus and Giardia |
Consider whether these vaccines are required for the individual animal and whether there is sufficient scientific evidence to support their use |
The generic information in this table should be read in conjunction with the more detailed recommendations provided in the current WSAVA vaccination guidelines (Day et al. 2010).
Note that these recommendations apply only to quality‐assured vaccines, most of which are produced by large, international companies
Practitioners should opt for a quality‐assured vaccine product range that enables them to deliver core components [i.e. canine distemper virus (CDV), canine adenovirus‐2 (CAV‐2) and canine parvovirus‐2 (CPV‐2) for dogs; feline parvovirus (FPV), feline calicivirus (FCV) and feline herpesvirus‐1 (FHV‐1) for cats] in combination with the minimum number of non‐core antigens. Such products might be administered, where professional guidelines permit and with client consent, no more often than every 3 years to adult animals where the added benefit of the non‐core component is questionable (i.e. where the individual animal has minimal risk of coming into contact with that infectious agent). Where a non‐core component (e.g. canine Leptospira) can be separated from a multi‐component vaccine, and risk–benefit analysis suggests that the individual animal would benefit from that component, then that component must be given annually to adult animals. The VGG recognises that at the present time, such decisions can only be made by individual practitioners on the basis of the product ranges that they have available.
In the 2007 WSAVA vaccination guidelines, the VGG recognised that in many parts of the world, veterinary medical health care of owned individual pet animals is restricted by financial factors. The VGG proposed that where a pet owner might only be able to ever afford a single vaccine for their animal, that this should be one dose of quality‐assured MLV vaccine (and rabies vaccine) given at a time when that single dose might induce long‐term protective immunity in the absence of maternally derived antibody (i.e. at 16 weeks of age or older). This rule‐of‐thumb is likely to have particular resonance in many of the Asian countries.
Rabies control
The VGG was encouraged to see plans for further mass vaccination campaigns for the control of canine rabies virus infection in endemic areas of Asia. The VGG hopes that governments and NGOs will continue to work towards the goal of global elimination of canine rabies virus infection by 2030 as proposed by a recent joint statement from the WSAVA and OIE (http://www.wsava.org/sites/default/files/OIE-WSAVA%20Joint%20Statement%20November%202013_final-1.pdf).
The VGG admires the dedication of practitioners in Asian countries to the goal of elimination of canine rabies virus infection. In some countries, practitioners devote 10 to 20% of their working hours to pro‐bono vaccination of street dogs. This contribution should be encouraged and recognised by governments.
The VGG differentiates between rabies vaccination of individual‐owned and housed pet animals versus rabies vaccination delivered in the context of a mass vaccination campaign for free‐roaming dogs. In the case of vaccination of individual pet animals, the current pragmatic approach is to adhere to legislation that requires annual revaccination of adult dogs, while accepting that if quality‐assured international vaccines are used, they would protect that animal for a 3‐year period. Again, practitioners and the national associations should be lobbying for changes that permit use of international rabies vaccines (that have a 3‐year licensed DOI in other countries) to individual pet animals every 3 years. In the case of mass vaccination campaigns, the VGG accepts the logic of annual revaccination of populations within which long‐term identification of individual vaccinated animals is impractical. In such free‐roaming populations, there is often high turnover of the animals, with new puppies being born and older dogs dying during the period between vaccination campaigns. In order to achieve the requisite 70% vaccination coverage of these populations, annual revaccination should be maintained for such campaigns.
Finally, the VGG was surprised to learn of the widespread use of rabies postexposure prophylaxis (PEP) in rabies‐vaccinated dogs in some Asian countries. Instances of repeated administration of a complete five‐vaccination PEP protocol within short periods of time following repeated bites from free‐roaming dogs (in dogs that are already immune) may be considered unnecessary use of rabies vaccine that might better be used in vaccination of the free‐roaming dog population.
Application of the health check concept to Asian practice
An important part of the global change in vaccination practice has been the move towards delivering vaccination as one part of an annual health check and promoting to clients that their annual veterinary visit is for a holistic assessment of the animal's health and wellbeing, rather than simply to receive a vaccine booster. The annual health check concept is rapidly gaining popularity in many countries of the world, where it has been proven to be advantageous for the business of veterinary practice. There is no reason why this concept should not be equally well received by the affluent urban clients of Asian veterinary practitioners and the VGG would encourage the national associations to provide education in, and endorsement for, the concept. Even in a less affluent rural community, the small animal practitioner should consider aspects of nutrition and ecto‐ and endoparasite control at the same time as deciding on a vaccination protocol for the individual pet animal. In some parts of Asia, it has been observed that a high proportion of pups and kittens carry high parasitic burdens and that it would be a sensible approach to deal with these before vaccination, in order to achieve the greatest possible protective immune response following administration of a vaccine.
Conflict of interest
The VGG remains an independent committee of academic experts. Our meetings are not attended by our sponsors and our recommendations are made without the input of our sponsors.
Acknowledgements
The VGG gratefully acknowledges the time given by the large number of individuals who attended our meetings and contributed valuable data and local knowledge to the project. We are particularly grateful to the small animal associations and individuals who administered the questionnaire survey in the various countries, which was a demanding and time‐consuming task. In particular, we thank Dr Louis Liu (Beijing Small Animal Veterinary Association), Dr Geoffrey Chen (Shanghai Small Animal Veterinary Association) and Dr Walasinee Moonarmart (Veterinary Practitioners Association of Thailand). The work of the VGG continues to be sponsored by MSD Animal Health. We are enormously grateful for the incredible logistical support provided by the national offices of MSD Animal Health in the four countries that we visited and for the oversight given by David Sutton (MSD Global) and Dr Raphael Zwijnenberg (MSD Asia‐Pacific).
VGG ASIAN QUESTIONNAIRE SURVEY
FREQUENTLY ASKED QUESTIONS
| Questions about vaccine products |
| 1. Are Toxoplasma vaccines available in other countries? |
| There are no commercial Toxoplasma vaccines available for use in cats anywhere in the world. |
| 2. Canine coronavirus infection is quite common in our area. We often get positive reactions with commercial test kits for coronavirus. What does the VGG think of the use of coronavirus vaccine? |
| The VGG does not recommend the use of canine coronavirus vaccines as there is insufficient evidence that this vaccine is protective, or indeed that enteric coronavirus is a significant canine pathogen. Variant strains of this virus have been reported to cause disease in adult dogs and puppies in various parts of the world, but it is unclear that the available vaccines protect against these variants. The identification of coronavirus with a test kit does not necessarily mean it is the cause of disease. |
| 3. Is a monovalent vaccine better than a multi‐valent vaccine? |
| Vaccines with the fewest components possible enable practitioners to adhere to the WSAVA guidelines. Multi‐component core MLV vaccines (e.g. for CDV, CAV‐2 and CPV‐2) are ideal for delivery of core vaccinations, but it is best to have individual vaccines for non‐core antigens (e.g. Leptospira, canine infectious respiratory disease complex) so that these may be given only when risk–benefit analysis suggests that they will be of benefit. For Leptospira vaccines, multi‐component products may provide the best protection if their formulation is based on scientific evidence that justifies the inclusion of multiple serovars in the vaccine. |
| 4. Will the number of different antigens in multi‐valent vaccines adversely affect the efficacy of the vaccine? |
| No. For a multi‐valent vaccine to be licensed, the manufacturer must prove that each component of the vaccine can induce protective immunity, generally in challenge studies. |
| 5. Can you give all vaccinations at once to an adult dog presented with no previous history of vaccination? |
| This is a similar question to that above. Yes, a dog should be able to respond to multiple antigens delivered simultaneously. However, you should never mix different vaccines in the same syringe unless specifically indicated by the datasheet. From first principles, it would be good practice to deliver the different vaccines to different anatomical sites so that different lymph nodes are involved in generating the adaptive immune response, but no studies have formally proven this. |
| 6. What are the quality differences between MLV vaccines and “genetic” vaccines? |
| Genetic vaccines include virus vectored vaccines, genetically mutated (gene deleted) vaccines and naked DNA vaccines. These vaccines may theoretically be safer than certain MLV vaccines as there is no chance of “reversion to virulence”. These vaccines are also designed to produce an optimum immune response. |
| 7. Can killed vaccines “break through” MDA better than live? |
| There is little evidence for this, but what is known is that some of the newer genetic vaccines appear to be able to generate immunity in the presence of MDA earlier than traditional MLV vaccines. |
| 8. Small breeds of dogs commonly suffer from adverse reactions. Is it possible to reduce the dose of vaccine to avoid this? |
| No. Vaccine doses are not calculated on a milligram per kilogram basis, as are drugs. The entire antigenic load is needed to stimulate immunity effectively. You should not split vaccine doses, nor give reduced volumes to small dogs. In the USA, a new product has been released that is designed for small dogs. This is formulated as a 0 · 5 mL dose, but contains much the same amount of antigen as does a conventional 1 · 0 mL vaccine. |
| 9. Why don't we have suitable combinations of core vaccines available to allow them to be used in accordance with the guidelines? |
| Suitable products are available in some other countries. If you do not have them, then you and your national small animal veterinary association should lobby the manufacturers and government regulators to bring the suitable products to your marketplace. In many cases, industry would like to make new products available, but the block lies with the licensing authority. |
| 10. Why do we not have 3‐year DOI rabies vaccines? |
| As above, this may be because the manufacturers have chosen not to bring you these products or because the licensing authority has not permitted their introduction of a 3‐year labelling. In at least one Asian country, the only permitted rabies vaccine is a nationally produced product that only has a 1‐year licensed DOI. |
| 11. Do canine core vaccines in Asia have a DOI of at least 7 years as stated by Dr Schultz? |
| Many internationally marketed MLV vaccines that are quality assured have been independently tested by Dr Schultz, and shown to be protective, in a challenge study at 7 to 9 years (Schultz et al. 2010, Journal of Comparative Pathology, 142, S102–S108). The VGG does not know which of the nationally produced core vaccines may have similarly long DOI. |
| 12. A local 3‐way Leptospira vaccine is available in my country alongside the traditional bivalent products. Which one should I use? |
| If the local 3‐way vaccine contains a combination of “relevant” Leptospira serovars that usefully extends the breadth of protection provided by vaccination under your local conditions, then it is likely to be more effective and preferable to a traditional bivalent product. |
| 13. Currently there are no Bordetella vaccines available in Japan. Do the VGG think Bordetella vaccines are important in Japan? |
| Vaccines against Bordetella bronchiseptica are non‐core products. Bordetella is just one of numerous pathogens that can be involved in causing upper respiratory tract disease in dogs and cats. Bordetella bronchiseptica has been shown to be an important cause of canine respiratory disease in Japan, as in other countries, along with canine parainfluenza virus (Mochizuki et al. 2008, Journal of Veterinary Medical Science, 70, 563–569). Yes, the VGG suggests that vaccines against canine infectious respiratory disease could be very useful to Japanese practitioners and should be introduced. |
| 14. Some trivalent cat vaccines contain inactivated FPV and live FCV/FHV, can these still be used every 3 years? |
| Yes, this is a core vaccine. Inactivated FPV will still provide protection for a minimum of 3 years. |
| 15. Is it better to use vaccines containing local strains rather than international vaccines? |
| There is no evidence that international core vaccines are unable to provide good protection against CDV, CAV‐1, CAV‐2, CPV‐2, FPV, FHV‐1 and rabies virus, worldwide. In most instances, strain variation does not change the key protective antigens of the organism that are conserved between strains. In the case of Leptospira, inclusion of additional, locally important serovars or strains in a vaccine may lead to enhanced protection. |
| 16. A recent CPV outbreak in army dogs was shown to be caused by CPV‐2c. There are recommendations that vaccines should contain the latest strains, what's the VGG view on this? |
| Currently available international MLV vaccines contain CPV‐2 (original strain), CPV‐2a or CPV‐2b. These vaccines are expected to confer substantial cross‐protection against CPV‐2c challenge, and indeed some have been shown to do so, shortly after vaccination. At present, there does not seem to be a pressing need to change the formulation of canine parvovirus vaccines. |
| 17. How do practices know that vaccines delivered to them have been stored correctly and that they are still potent? Can vaccines be delivered with indicators to assure correct storage? |
| We have asked this question to the manufacturers and suppliers of international vaccines during our Asian meetings and have been assured that there is continuation of the cold chain from importation to practice delivery. International manufacturers do utilise temperature indication systems during the bulk delivery stages. |
| 18. There is no national policy in India giving advice and recommendations on canine vaccination. When will we get a local policy? |
| The WSAVA encourages all national small animal veterinary associations to develop national vaccination advice. This has already happened in many other countries. Some simply adopt and refer to the WSAVA guidelines, whereas others adapt the guidelines for the local situation. You should continue to lobby your national association to provide local guidance. |
| 19. How common is tetanus in dogs? Should we vaccinate against it? |
| In many parts of the world, tetanus is uncommon in dogs. There are no licensed vaccines for dogs, but in some areas deemed as being at high risk, veterinarians do use equine tetanus vaccine in dogs (off‐label use). Given that tetanus is nowadays considerably more frequently observed than canine infectious hepatitis and canine distemper in many parts of the world, development of a canine tetanus vaccine may be justifiable and commercially viable. |
| 20. Does the VGG recommend which vaccine brand should be used? |
| No. The VGG is an independent academic group that does not make product‐specific recommendations. However, in the case of international vaccines, the VGG knows that all of these products have undergone rigorous assessment of quality, safety and efficacy that has permitted their licensing in many countries. The VGG does not recommend the use of some vaccines – but this is based on a lack of adequate scientific evidence (i.e. peer‐reviewed scientific literature) that the vaccine is necessary or efficacious. Recommendations are reviewed and adjusted as needed periodically. |
| 21. If one wants to use just the DHPPi without the Leptospira component of a vaccine, what should be used to reconstitute the DHPPi? |
| You should ask this question to the manufacturer or supplier of the particular vaccine, but a suitable diluent may be sterile normal saline or sterile water for injection. If not, the manufacturer should be able to provide you with the specific diluent required. |
| 22. What about the use of rabies vaccine in small mammals (e.g. rabbits and guinea pigs)? |
| The VGG does not recommend rabies vaccination of these small mammals, except for ferrets. |
| 23. Should Leptospira vaccine be used 6‐monthly in high‐risk areas? |
| Yes, this is consistent with the VGG recommendations in the WSAVA guidelines. You should ideally have a good scientific evidence base for stating that your practice is in a high‐risk area. |
| 24. What happens if a dog is bitten by a free‐roaming dog after receiving the initial puppy rabies vaccine; should it receive PEP? What if that dog receives PEP and is then bitten again some weeks later, should it receive another course of PEP? |
| If the bitten puppy has been vaccinated properly, it should be protected against rabies. The VGG is aware that in India, PEP is used in this situation for the benefit of the puppy, and more importantly for the benefit of the human family. Repeated PEP is not justified. By that time the puppy will have received multiple vaccinations and further injections will provide no added benefit. |
| Questions about vaccine delivery to puppies and kittens |
| 25. Is it OK to mix different manufacturer's products during the primary course? |
| Core MLV vaccines from the different international suppliers are similar in composition and may be mixed during the primary course (e.g. if a puppy has an 8‐ to 9‐week vaccine from one veterinarian and then moves to another veterinarian who uses a different product range). Manufacturers will not support this practice (and will advise against it) because they have not undertaken studies to prove compatibility of their products with those of other manufacturers. It may also be acceptable to use non‐core vaccines from different manufacturers, with the exception of Leptospira vaccines where a first dose with a two‐serovar product, and a second dose with a four‐serovar product, would not induce immunity to the additional two serovars contained in the four‐way vaccine. |
| 26. In a puppy that has received inoculations at 6 and 9 weeks with one vaccine brand, and is then presented to a practice that uses another vaccine brand at 6 months, what should be given? |
| The second practice may give the international MLV core vaccine that they use routinely as described in the question above. If that puppy had not yet received a rabies vaccine, that should be given at 6 months as well (in a rabies endemic area). Remember that for puppies, some will not have responded to primary vaccination at either 6 or 9 weeks of age, and the VGG recommends a third vaccination at 16 weeks of age or greater. |
| 27. Often puppies or kittens are groomed before vaccination – is this OK? |
| As long as the puppy or kitten is in good health and not overly stressed by the grooming procedure, there is no reason not to vaccinate after grooming. |
| 28. Can you give rabies and DHPPi vaccine at the same time (concurrently)? |
| Yes, but unless the vaccines have a specific concurrent use claim on the product label, then this may be considered “off‐label” use. Ideally, the two vaccines used concurrently in this way should be given at different anatomical sites in order that vaccine antigens are carried to different lymph nodes in order to stimulate adaptive immunity at two distinct locations. |
| 29. Can one use rabies vaccine 1 week after DHPPi? |
| Yes, there is no problem in doing that. As discussed earlier, it would be sensible to inject this into a different location in order to stimulate immunity via a different lymph node. |
| 30. If a puppy suckles for more than 1 · 5 months, do you need to start the vaccination protocol later? |
| No. Remember that maternally derived antibody that interferes with puppy vaccination is only obtained from colostrum taken in during the first 24 to 48 hours of life. After that, entire antibody is not absorbed from the gastrointestinal tract. |
| 31. Why don't the VGG recommend Rabies vaccination until after 12 weeks of age? |
| This recommendation is consistent with the datasheets for the majority of international vaccines. |
| 32. Can we vaccinate puppies at less than 6 weeks of age? |
| In general, no. Puppies at this age will have MDA that blocks the ability of MLV vaccines to prime the immune system. Moreover, vaccine datasheets do not support this practice and there may be safety issues with giving MLV vaccine to very young animals (i.e. <4 weeks of age). One exception is the use of intranasal vaccines against canine infectious respiratory disease. These can be used safely from a very young age. Check product datasheets. |
| 33. There are some nationally manufactured rabies vaccines that are combined with DHPPi. Manufacturers recommend that these can be given from 8 weeks of age. How come these vaccine datasheets can say this? |
| A datasheet recommendation should be based on proven safety and efficacy studies performed to the requirements of the licensing authority. One can only assume that such studies have been done and support this recommendation. If in doubt, inquire with the manufacturer or government authorities. |
| 34. We have a core vaccine for puppies for which a final dose at 10 weeks is recommended. This seems contrary to the WSAVA guidelines. |
| Such “early finish” vaccines were introduced in order to encourage the early socialisation of puppies, which is very important for their development. We believe that 25% of the puppies still have blocking levels of MDA (particularly against parvovirus) at 10 weeks of age (and 10% at 12 weeks of age) and so there is a risk that not all puppies will be fully protected until they receive a 12‐month booster vaccine. The VGG recommends a final dose of puppy vaccine at 16 weeks of age or older. |
| 35. The 2010 WSAVA guidelines advise a 14‐ to 16‐week final dose, but should this be 14, 15 or 16 weeks? |
| We would recommend the final dose to be given at the 16‐week end of this range and in the current document, we have used the phrase “at 16 weeks of age or older”. For kittens, there are new studies that show persistence of MDA even beyond 16 weeks, and when we next revise the global WSAVA guidelines, we will consider this new evidence for kittens. |
| 36. In Thailand, the legal requirement is that puppies be vaccinated against rabies at 2 months of age – is this correct immunologically? |
| Most international canine rabies vaccines carry the recommendation for administration at 12 weeks of age, based on safety and efficacy studies. In this instance, the legal requirement would be in conflict with the datasheet recommendations if international vaccines are being used. Note that the WSAVA guidelines recommend a second vaccine be given (2 to 4 weeks later) in areas of high risk for rabies. |
| 37. If the pup has no MDA, when should you start vaccination? |
| In a practical setting, it would be difficult to prove that a pup had no MDA. This would necessitate knowing definitively that the pup did not take in colostrum. However, if this was known, then core vaccination may be given from 6 weeks of age. Certain MLV vaccines must not be given any earlier than 4 weeks of age as they may cause pathology in the pup. If this pup definitively had no MDA, it may respond adequately to a single dose of vaccine at 6 weeks of age; however, it may be pragmatic to give a second dose at 16 weeks of age. |
| 38. When can puppies go outside for proper socialisation? |
| There is no doubt that ensuring early socialisation is an important part of responsible puppy ownership. Owners should be made aware of the risks – that not every puppy will be fully protected against lethal (core) diseases until after the 16‐week vaccination (see Question 34). Owners should be advised about simple precautions; for example, only attending “puppy parties” where all of the dogs are vaccinated and attending such events on “clean territory” (e.g. not in the back room of the veterinary hospital). |
| 39. If the puppy sneezes after intranasal vaccination, is it necessary to vaccinate again? |
| Sneezing, with loss of some of the vaccine, is commonly observed after the use of intranasal products. These vaccines have been designed to allow for partial loss of the product and so it should not be necessary to revaccinate, unless it is clear that none or very little of the product was delivered successfully. |
| 40. What do we do if the animal is presented late for vaccination? |
| If this is a puppy, presented (for example) after 16 weeks of age, a single dose of international MLV core vaccine (CDV, CAV‐2 and CPV‐2) will be protective as will a single dose of rabies vaccine. Considering non‐core vaccines, it is necessary to give two doses 2 to 4 weeks apart. If this is an adult dog, presented for revaccination (for example) at 4 years rather than 3 years since its last core vaccination, the same would apply for core vaccines and canine rabies. Any adult dog that does not receive annual Leptospira vaccination should be treated as a puppy and receive two injections 2 to 4 weeks apart and then an annual vaccine. |
| Questions about vaccine delivery to adult animals |
| 41. Do you need to continue to vaccinate old dogs? |
| For MLV core vaccines (CDV, CAV‐2, CPV‐2), current international recommendations are for revaccination of adult dogs no more frequently than every 3 years. Canine rabies vaccines should be given every 3 years where an international product is used (with a 3‐year DOI) and that is consistent with local legal requirements. If non‐core vaccines are chosen for use in an individual dog, they must be given at least annually. |
| 42. At what age can one stop vaccinating dogs? |
| For core vaccines, the current recommendation is for lifelong revaccination no more frequently than every 3 years and if non‐core vaccines are chosen for use, these are generally given annually. One can use serological testing in any adult dog to confirm protection and elect not to revaccinate that animal. Current advice is that serological assessment is performed every 3 years, but in dogs older than 10 years, this should be done annually. In many Asian countries, there is also a legal requirement to vaccinate (currently annually) against rabies. |
| 43. For an adult dog with no CDV antibody, what's the recommended vaccination protocol? |
| An adult dog requires only one dose of international MLV core vaccine to generate a protective immune response. We would recommend vaccinating the dog and testing serologically 4 weeks later. An estimated 1 in every 5000 dogs may be a genetic non‐responder to CDV and may never be able to respond to vaccination. |
| 44. What protocol is recommended for an unvaccinated adult dog? |
| Core vaccination with a single dose of international MLV vaccine (CDV, CAV‐2, CPV‐2) plus rabies in endemic areas. Revaccination (or serological testing for CDV, CAV and CPV‐2) no more frequently than every 3 years thereafter. Non‐core vaccines should be selected based on a risk–benefit analysis for that individual animal. |
| 45. For an adult dog with an unknown Leptospira vaccination history, what's the recommended vaccination protocol? Is it still two doses 4 weeks apart as in puppies? |
| Yes, this dog would require two doses of vaccine given 2 to 4 weeks apart and then annual revaccination thereafter. |
| 46. How is it best to vaccinate a pregnant bitch? Is it best to give a booster vaccination before the pregnancy? |
| Vaccines should not be given during pregnancy unless specifically indicated in the datasheet. The best approach is to ensure that breeding bitches are vaccinated (with core vaccines), but it is unnecessary to give additional core vaccines to breeding bitches immediately before pregnancy – their standard vaccination schedule (e.g. triennial core revaccination) will provide adequate protective immunity and colostral antibody for the puppies. |
| 47. If rabies vaccine is given multiple times during a period (6 months), is this safe? |
| The international rabies vaccines are very safe, but there is no need to administer them to individual‐owned pet dogs more frequently than every 3 years. The VGG is aware that in some Asian countries, the vaccine is used in a postexposure prophylaxis (PEP) protocol when a pet dog is bitten by a free‐roaming dog. If the pet dog is vaccinated and already protected, this procedure should not be encouraged. |
| 48. What protocol is recommended for an unvaccinated adult cat? |
| For an adult cat that has never been vaccinated, the VGG recommends core vaccination with two doses of international MLV vaccine (FPV, FCV, FHV‐1) plus one dose of rabies vaccine in endemic areas. Revaccination (or serological testing for FPV) no more frequently than every 3 years thereafter. Non‐core vaccines should be selected based on a risk–benefit analysis for that individual animal. |
| 49. A bitch that was initially vaccinated as a pup, but has not received booster vaccination since then was presented by the owners before breeding. Should she be revaccinated? |
| Yes. The bitch should receive one dose of international MLV core vaccine (CDV, CAV‐2 and CPV‐2) and in an endemic area also canine rabies vaccine. |
| Questions about vaccine husbandry and general vaccination |
| 50. Is it OK to swab the vaccination site with spirit before vaccinating? |
| No, alcohol or other disinfectant might inactivate modified live virus in core vaccines. |
| 51. Can you vaccinate and dose with anthelmintic at the same time? |
| There is no reason not to do this. |
| 52. Should FIV‐positive cats be vaccinated? |
| It is suggested that FIV‐positive cats may not be able to respond adequately to vaccination and may also be more susceptible to develop a vaccine‐induced disease following MLV vaccination. The vaccination requirements of an FIV‐positive cat should be considered carefully. Such animals would be best housed indoors away from other cats and not permitted outdoor access. If core vaccination is essential, then use of a killed rather than MLV core vaccine is recommended. |
| 53. Should a cat be vaccinated if it already has signs of upper respiratory disease? |
| A cat with current clinical disease should not be vaccinated. Once it has recovered, the cat should have some natural immunity to FCV or FHV (or both if both agents were involved in causing the respiratory disease), but such immunity is never sterilising (even after vaccination). There is no indication NOT to vaccinate a cat that has recovered from a respiratory viral infection. A trivalent vaccine will protect against FPV and also against the respiratory virus (FHV‐1 or FCV) that was not involved in causing the earlier respiratory disease. |
| 54. Should you vaccinate E. canis‐infected dogs since these dogs can be immunosuppressed? |
| There is no evidence that a dog with monocytic ehrlichiosis cannot respond adequately to vaccination or that protective antibody titres against core vaccine components diminish in E. canis‐infected dogs. Ideally, the dog would be treated and any essential vaccination performed after the cessation of therapy. It may be a legal requirement to give rabies vaccine to such cases in any event. |
| 55. Should one vaccinate an animal that is diseased or stressed? |
| No. This is contrary to good practice and the advice on most vaccine datasheets. |
| 56. How should dogs on medication for immune‐mediated disease be vaccinated? |
| Antineoplastic drugs, and some of the most potent drugs used to treat immune‐mediated diseases, interfere with a dog's ability to respond immunologically to vaccination, but standard immunosuppressive doses of glucocorticoid have relatively little effect. Nevertheless, vaccines should not be administered to animals with significant disease and animals receiving high doses of glucocorticoid for immune‐mediated disease fall into this category. Vaccination should be delayed until after the drugs have been tapered or stopped. Most dogs receiving such therapy will be adult animals that will already have acquired long‐term immunological memory to core vaccine antigens and should be on a revaccination schedule of not more often than every 3 years for these core vaccines. |
| 57. Does vaccination at different subcutaneous sites have the same efficacy? |
| This is an interesting question that has come about due to recommendations to vaccinate cats in locations other than the scruff of the neck in order to avoid the occurrence of a surgically challenging feline injection site sarcoma. In the USA, recommendations for vaccination of cats in the distal hindlimbs are made. The WSAVA vaccination guidelines propose vaccination into the skin of the lateral abdomen. In a recent pilot study, investigators vaccinated cats into the distal tail and actually addressed the question of efficacy by showing that such cats made protective serological responses to FPV and rabies virus (Hendricks et al. 2014, Journal of Feline Medicine and Surgery, 16, 275–280). It has been suggested that further work is needed to ensure injection of heavily adjuvanted vaccines into the tails of cats is safe: it is feared that swelling in such a tight area may lead to development of “compartment syndrome” in some cats. However, this was not noted in the pilot study. |
| 58. Power cuts are not uncommon in parts of our country and they can last for 2 to 3 days. What should one do as regards any vaccine in the fridge at the time – is it OK to use? |
| MLV vaccine that has not been stored at appropriate temperature for 2 to 3 days should not be used. Some of the components of these vaccines (e.g. CDV) are temperature sensitive and there may have been inactivation of the virus. |
| Questions about the use of serological testing |
| 59. How long after CPV‐2/CDV vaccination should you wait before measuring protective antibody concentrations using in‐clinic tests? |
| This question is most relevant for puppies, because adult dogs are likely already to have serum antibodies present at the time of booster vaccination, regardless of how long an interval there has been since they were last vaccinated. If a puppy receives its final primary vaccine at 16 weeks of age, then it may be tested from 20 weeks of age onwards. Any antibody present at that stage cannot be of passive, maternal origin and therefore indicates that the puppy is actively protected. |
| 60. Why don't the VGG recommend that you do a rabies antibody test? |
| For many Asian veterinarians, this question may be of little practical consequence, as regular rabies vaccination of dogs and cats is a legal requirement in many countries, irrespective of any titre results. Rabies antibody testing is only required in certain situations related to international pet travel. The international rabies vaccines are highly efficacious and it is generally considered that there is no need to demonstrate immunity post vaccination. |
| 61. Can we use antibody tests (CDV, CPV‐2 and CAV) to test the MDA in order to decide the first vaccination time? |
| Theoretically, this would be possible and years ago a “nomogram” was often used to estimate when pups might best respond to vaccination on the basis of the titre of antibody in the serum of the bitch. In practice, it would be very difficult and expensive to repeatedly sample and test young puppies in order to monitor the decline of MDA. |
| 62. What happens to the antibody titre over the 3‐year period post vaccination? |
| For CDV, CAV‐2, CPV‐2 and FPV, the antibody titre will be consistently present at similar titre. This has been shown in numerous field serological surveys of dogs last vaccinated up to 9 years previously and in experimental studies for dogs last vaccinated up to 14 years previously. For Leptospira, the titres will decline rapidly after vaccination and in any case are not well correlated with protection. Serum antibody titres are less relevant for FCV and FHV‐1 where the most important type of immunity is mucosal and cell‐mediated, respectively. |
| 63. In an animal that has completed its puppy/kitten shots, is a higher antibody titre required to protect against heavy disease challenge? |
| For CDV, CAV‐2, CPV‐2 and FPV, the answer is no. The presence of antibody (no matter what the titre) indicates that protective immunity and immunological memory is present in that animal. Giving more frequent vaccines to animals in an attempt to increase antibody titre is a pointless exercise. It is impossible to create “greater immunity” by attempting to increase an antibody titre. |
| 64. Can we test dogs as an alternative to annual vaccination? We are concerned about the advice to only boost every 3 years. |
| Yes, certainly. There are now well‐validated in‐practice serological test kits that permit determination of the presence of protective serum antibody specific for CDV, CAV, CPV‐2 and FPV. In other countries, these kits are used to confirm protection at 3‐year intervals (instead of automatic revaccination for core diseases). You may perform serology annually, but if you collect and analyse the data that you generate within your practice, you will soon find that annual testing is not necessary. |
| Questions about the annual health check |
| 65. In the annual health check, what tests/examinations should you do? |
| The annual health check should focus on the basic physical examination (including body temperature, cardiac auscultation and palpation). An excellent history should be taken to understand the lifestyle and disease risks (e.g. travel, boarding, indoor versus outdoor exposure). The fundamentals of nutrition and parasite control should be discussed with the owners. |
| 66. Some owners may be reluctant to come back just for an annual health check. What advice can be provided to promote the health check concept in order to improve owner compliance? |
| This is all a matter of education. Clients should realise that the health check examines all aspects of the health and wellbeing of their pet and may pick up the early stages of clinical problems. In terms of vaccination, the health check examination might include serology (every 3 years for core vaccine antigens) or the annual administration of non‐core vaccine if such vaccines are required. |
| 67. The costs of an annual health check are far too high for my clients. |
| The annual health check may be as simple as an excellent clinical history and physical examination – the costs for which are purely the professional time of the veterinarian. Fundamentally, the concept of an “annual health check” is a new way of delivering what most practitioners already offer as a “vaccination booster and physical examination”. For more affluent clientele, the annual health check has proven a means of offering other veterinary services and increasing practice profitability. This is also an example of practicing better quality medicine and about redefining the veterinarian–client relationship. |
| Questions about vaccine adverse effects |
| 68. In case of a mild allergic reaction to a vaccine, can you use steroids to treat? |
| Yes; reactions such as facial oedema and pruritus may be treated with anti‐inflammatory (not immunosuppressive) doses of oral glucocorticoid (e.g. prednisolone) and/or with antihistamines. |
| 69. If an animal suffers an allergic reaction post vaccination, what should you do when the next vaccination is due? |
| In this situation, there is a risk that revaccination will trigger the same allergic reaction. The answer to the question depends on the age of the dog and the stage of the vaccination programme, and the type of vaccine under consideration. For core vaccines, it is important that the animal receives one dose at 16 weeks or greater to induce protective immunity. An antihistamine or an anti‐inflammatory dose of glucocorticoid may be administered to such animals in advance of vaccination, and they should be closely monitored immediately afterwards. Thereafter, such an animal might be serologically tested to demonstrate protective immunity rather than automatically revaccinated. If the reaction occurred in an adult dog, serological testing may be used instead of core revaccination. If the reaction is thought to have been triggered by a non‐core vaccine, consideration should be given as to whether the animal really requires that vaccine in the future. |
| 70. Is there evidence that cutaneous vasculitis can be caused by vaccination? |
| Yes, this is a very rare, but recognised, adverse reaction following vaccination, particularly rabies vaccination. |
| 71. What are adverse hypersensitivity reactions and how can these be differentiated clinically? |
| The most common such reactions are facial oedema and cutaneous pruritus occurring within an hour (generally less) of vaccination. The temporal relationship suggests that the vaccine has triggered the reaction. |
| 72. Do we see signs of cutaneous allergic reactions in cats as in dogs? |
| Yes. Cats may present with the same manifestations of type I hypersensitivity post vaccination as dogs (e.g. facial oedema and cutaneous pruritus). |
| 73. How do we know that a feline sarcoma was caused by a vaccine? How do we deal with this type of sarcoma? |
| A feline injection site sarcoma (FISS) arises at an anatomical location into which injectable product has been delivered previously. It is suspected that a wide range of injectables, including vaccines, may potentially trigger these tumours. It is important to record the site of vaccination in cats in the medial record of the animal and the WSAVA guidelines give advice on suggested best locations for vaccinating cats. Unfortunately, these sarcomas are very aggressive. They infiltrate widely and around 20% may metastasise. They require significant surgical resection that is often best performed by a specialist. |
| 74. Why are there more hypersensitivity cases caused by rabies vaccine than before? Why is this more common among toy poodle dogs? |
| Hypersensitivity reactions may be caused by any type of vaccine, but killed adjuvanted products may be particularly associated with this type of reaction. We now know that a dominant antigen that causes these reactions is bovine serum albumin (BSA) that is incorporated into vaccines during their production. Manufacturers are now trying to reduce the concentration of BSA in animal vaccines. Such reactions are more common in many toy breeds, and in many countries, these breeds are now particularly popular. There is likely to be a genetic susceptibility, but this is poorly understood. |
| 75. Why do some dog breeding kennels continually have problems with dogs dying from CDV and CPV‐2 infections? |
| The most likely cause for this scenario is that the breeding stock is not adequately vaccinated. Outbreaks might occur among puppies that did not obtain sufficient MDA as the bitch was not effectively vaccinated. In contrast, where puppy vaccination is not performed according to WSAVA guidelines (i.e. with a final puppy vaccine at 16 weeks of age or older), there is a risk that some puppies may be unprotected if the bitch does have a high level of MDA. Finally, there are some breeds of dog (e.g. Rottweiler, Dobermann) that have a greater risk of being genetic non‐responders to these vaccines. Good husbandry, hygiene and nutrition all play a role in minimising disease outbreaks in kennels. |
| 76. Can a modified live virus revert to virulence? Will a dog be infected by an MLV vaccine? |
| Yes, an MLV vaccine strain can theoretically revert to virulence, but this is exceedingly rare. Yes, MLV vaccines are called “infectious vaccines” because they work by inducing a low level of infection (and virus replication) in the dog, sufficient to induce immunity, but not disease. In the case of canine parvovirus, vaccinated dogs might shed the MLV vaccine strain of virus in the faeces for a short period after vaccination. This does not pose a risk to other dogs. |
| 77. Some pups were vaccinated at 6 weeks of age with DHPPi and went down with infectious hepatitis at 7 weeks of age; why did this happen? |
| The most common reason for this occurrence (i.e. infection in a vaccinated pup) is that the animal was already incubating infectious virus before it was vaccinated. It is possible that these pups might have been infected during the “window of susceptibility” when they no longer had sufficient MDA to fully protect them against virulent street virus, but the MDA that was present was still sufficient to interfere with their immune response to a recently administered vaccine. |
| 78. Apart from the (very small) risk of adverse reaction, what are the other risks of annual vaccination? |
| The risks of adverse reaction following vaccination are indeed relatively small. For dogs and cats, this is in the order of 30 to 50 reactions for every 10,000 animals vaccinated, respectively, and the vast majority of these are non‐serious reactions (e.g. transient pyrexia and lethargy, allergic reactions). However, if a serious reaction occurs in one of your client's animals – that is a difficult discussion to have. Adoption of new guidelines is not simply about minimising the risk of adverse reactions – it is about practicing better, evidence‐based veterinary medicine and only performing a medical procedure (i.e. vaccination) when this is required. |
| 79. Some dogs are genetically poor responders (e.g. Rottweilers). How should one vaccinate these breeds? |
| The WSAVA guidelines contain a useful flow diagram that helps you identify non‐responder dogs. All puppies should be vaccinated in the same way (with a final vaccination at 16 weeks of age or older) and if you are concerned about the breed and the potential for lack of response, you should serologically test at 20 weeks of age. Most non‐responders will fail to seroconvert to just one of the core vaccine antigens (i.e. CDV, CAV or CPV‐2). You may attempt to revaccinate and retest that dog, but a true non‐responder (or low‐responder) may still not respond to revaccination. Such animals simply lack the immunological ability to make an immune response to that particular antigen and will never respond to that vaccine component. Owners should be made aware that these dogs will be at risk, and ideally, they should not be used for breeding. |
| 80. How should we analyse the risk–benefit of vaccinations? |
| Risk–benefit analysis really only applies to the choice of non‐core vaccines, as it is taken as given that all dogs and cats (no matter where or how they live) should receive core vaccines (including rabies in endemic areas). The risk–benefit analysis is made for the individual animal, taking into consideration what the owner has told you about its housing, indoor–outdoor access, travel and boarding frequency, exposure to other animals (e.g. part of a multi‐pet household) etc. The risks to consider are (1) the risk of adverse reaction following vaccination, (2) the risk that you will be performing an unnecessary medical procedure, (3) the risk that the animal will become infected with the infectious agent based on scientific knowledge about the prevalence of disease in your area, and (4) the risk of developing clinical disease following that infection. The possible benefits to consider are (1) whether the vaccine might protect the animal from infection if its lifestyle or geographical location means it is likely to be exposed to that infectious agent, (2) whether the vaccine might reduce the severity of clinical signs should that animal become infected, and (3) whether the animal being vaccinated contributes to herd immunity among the population. |
SELECTED KEY PAPERS HIGHLIGHTED TO THE VGG DURING MEETINGS
| This list does not represent an exhaustive review of the literature but provides examples of local research related to vaccine‐preventable infectious diseases of dogs and cats that was considered to be of national significance by key opinion leaders attending the VGG meetings. |
|
Abhinay, G., Joseph, S. & Ambily, R. (2012) Seroprevalence of canine leptospirosis. Indian Veterinary Journal 89, 72‐73 Iwamoto, E., Wada, Y., Fujisaki, Y., et al. (2009) Nationwide survey of Leptospira antibodies in dogs in Japan: results from microscopic agglutination test and enzyme‐linked immunosorbent assay. Journal of Veterinary Medical Science 71, 1191‐1199 Lin, Y., Zhao, Y.‐B., Zeng, X.‐J., et al. (2012) Complete genome sequence of an H3N2 canine influenza virus from dogs in Jiangsu, China. Journal of Virology 86, 11402 Manickam, R., Basheer, M. D., & Jayakumar, R. (2008) Post‐exposure prophylaxis (PEP) of rabies‐infected Indian street dogs. Vaccine 26, 6564‐6568 Meeyam, T., Tablerk, P., Petchanok, B., et al. (2006). Seroprevalence and risk factors associated with leptospirosis in dogs. Southeast Asian Journal of Tropical Medicine and Public Health 37, 148‐153 Miyaji, K., Suzuki, A., Shimakura, H., et al. (2012) Large‐scale survey of adverse reactions to canine non‐rabies combined vaccines in Japan. Veterinary Immunology and Immunopathology 145, 447‐452 Nakamura, Y., Nakamura, Y., Ura, A., et al. (2010). An updated nationwide epidemiological survey of feline immunodeficiency virus (FIV) infection in Japan. Journal of Veterinary Medical Science 72, E1 Song, Y., Li, Y., Lv, Y., et al. (2008). Sequence analysis of canine parvovirus VP2 gene. Chinese Agricultural Science Bulletin 24, 26‐31 Tsai, H.‐J., Pan, M.‐J., Cheng, Y.‐H., et al. (2009) Investigation of leptospirosis in dogs with acute renal failure or icterus. Taiwan Veterinary Journal 35, 36‐42 Watanabe, S., Kawamura, M., Odahara, Y., et al. (2013). Phylogenetic and structural diversity in the feline leukemia virus Env gene. Plos ONE, 8, e61009 Zhang, C., Wang, H., & Yan, J. (2012) Leptospirosis prevalence in Chinese populations in the last two decades. Microbes and Infection 14, 317‐323 |
References
- Day, M. J. , Horzinek, M. & Schultz, R. D. (2007) Guidelines for the vaccination of dogs and cats. Journal of Small Animal Practice 48, 528‐541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day, M. J. , Horzinek, M. & Schultz, R. D. (2010). Guidelines for the vaccination of dogs and cats. Journal of Small Animal Practice 51, 338‐356 [DOI] [PMC free article] [PubMed] [Google Scholar]


