Abstract
Background
Foot‐and‐mouth disease virus (FMDV) causes a severe livestock disease, and the virus is an interesting target for virology and vaccine studies.
Materials and methods
Here we evaluated comparatively three different viral antigen‐encoding DNA sequences, delivered via two physical means (i.e., gene gun delivery into skin and electroporation delivery into muscle), for naked DNA‐mediated vaccination in a mouse system.
Results
Both methods gave similar results, demonstrating commonality of the observed DNA vaccine effects. Immunization with a cDNA vector expressing the major viral antigen (VP1) alone routinely failed to induce the production of anti‐VP1 or neutralizing antibodies in test mice. As a second approach, the plasmid L‐VP1 that produces a transgenic membrane‐anchored VP1 protein elicited a strong antibody response, but all test mice failed in the FMDV challenge experiment. In contrast, for mice immunized with the viral capsid precursor protein (P1) cDNA expression vector, both neutralizing antibodies and 80–100% protection in test mice were detected.
Conclusions
This strategy of using the whole capsid precursor protein P1 cDNA for vaccination, intentionally without the use of virus‐specific protease or other encoding genes for safety reasons, may thus be employed as a relevant experimental system for induction or upgrading of effective neutralizing antibody response, and as a convenient surrogate test system for DNA vaccination studies of FMDV and presumably other viral diseases. Copyright © 2005 John Wiley & Sons, Ltd.
Keywords: FMDV, DNA vaccine, viral clearance, capsid protein, immunogenicity
Introduction
Foot‐and‐mouth disease (FMD) has become a major problem affecting many livestock of agricultural importance in several countries across different continents. Because FMD spreads rapidly and widely and has grave economic consequences 1, it has become one of the animal diseases that livestock owners fear most. The outbreaks of FMD in cattle and swine during 2000 in the United Kingdom have more recently focused worldwide attention on this deadly animal disease 2. As a member of the family Picornavirus, foot‐and‐mouth disease virus (FMDV) is a non‐enveloped, icosahedral virus and the protein capsid encloses a single strand of positive sense RNA. After infection, the viral genome is translated and then cleaved via viral proteases into the mature structural and non‐structural proteins 3. The capsid consists of four proteins: VP1, VP2 and VP3 are assembled on the surface of the viral particle and fold as eight‐stranded β‐barrels, whereas VP4 is an internal core protein and less structurally conserved 4.
Immunological studies of FMDV have identified that linear and conformational sites are present on both empty capsids and virions 5, 6, 7, and that the antisera raised against empty capsids have serological specificity which is indistinguishable from that of sera prepared against FMD virions 8. The VP1 capsid protein has been shown to contain major antigenic determinants. In some instances of protein and peptide vaccines, although the total reactivity of antibodies is high, the level of neutralizing antibodies in comparison is low 9, 10. It was further proposed that the loop of VP1 in the naturally occurring virus could display multiple conformations, and this may elicit a different population of antibodies during immune responses 11, 12.
Due to the apparent complexities of various immune reactivities that can be generated against this virus, FMDV may serve as an attractive experimental model for studying gene‐based vaccines. Directing the immunogens encoded by the cDNA vectors to undergo the endogenous processing pathway after transgene expression in host cells may lead to an effective cell‐mediated (Th1) and humoral (Th2) protective immunity 13, 14. The immune response against FMDV has been shown as T‐cell‐dependent 15, and therefore the DNA vaccine strategy may also serve as a good strategy to solicit both humoral and cell‐mediated immune responses. In animals immunized with inactivated vaccines, a good correlation between neutralizing antibody and protection has been observed 16, and such a correlation has not been well established with animals immunized with non‐viral vaccine strategies. These limitations probably have reflected the difficulties of reproducing or mimicking the immunogenicity of an entire viral particle in using simple antigen preparations. Various pieces of evidence suggest that the simpler the epitopic composition of a vaccine, the lower the chances of conferring a solid protection against natural isolates of viruses 17, 18, 19, 20. Therefore, new vaccine strategies may need to employ many or most of the epitopes or in permutations to represent the virus particles.
Previously, Mason and colleagues have developed two types of DNA vaccine against the FMDV serotype A12 21, 22, 23. One contains a full‐length cDNA of the FMDV genome and the other a cDNA construct containing the P1‐2A and 3C (proteases) encoding regions which have been shown to elicit neutralizing antibody and have partially protected test pigs against viral infection 21, 22, 23. According to these cDNA constructs, it seems that capsid formation in situ is required for effective immunization 22, 23, 24, 25. The immunogens produced by capsid assembly may provide efficacious conformational epitopes 22, 24. Huang et al. 26 and Wong et al. 27 designed another approach, where several plasmids encoding various FMDV epitopes and leading signal peptide sequence were employed in the study. Swine inoculated with pCEIS plasmid encoding two major epitopes (site A and C) of FMDV serotype O and a host self immunoglobulin can provide protection against direct FMDV challenge 27.
To discriminate differences between vaccinated and virus‐infected animals and to reduce the potential risk of such DNA vaccines, we intentionally did not include the viral protease‐encoding genes (e.g. 2AB, 3BC) in the expression vector design. We evaluated three different strategies of cDNA constructs for transgenic expression of VP1 or the whole P1 capsid protein. Two physical means for direct DNA delivery in vivo were employed in this study, including gene‐gun‐ and electroporation‐mediated transfection into skin and muscle tissues, respectively. The possible applications of the current experimental system for future vaccine or virological studies of FMDV are discussed.
Materials and methods
Virus culture
Preparations of FMD serotype O Taiwan viruses from the 1997 epidemic strain were a generous gift from the National Institute for Animal Health (NIAH), Tansui, Taipei, Taiwan. FMDV was propagated in baby hamster kidney (BHK)‐21 cells. Host cells were first cultured in complete RPMI 1640 medium (Gibco) until a monolayer of approximately 80% confluence was formed; FMDV was then added to infect cells for 45 min. Conditioned culture medium was collected after 75% of the cytopathogenic effect of the BHK‐21 cells was reached. Fresh preparations were used within 1 day or stored frozen until use.
Construction of cDNA expression vectors for DNA vaccine
In this study, we used the vector pIBSY1, which was modified from the p3224 mammalian expression vector containing the marker of kanamycin resistance for selection in E. coli, and an SV40 intron A sequence immediately following the CMV promoter for expression in mammalian cells, for construction and DNA immunization. In brief, plasmids pIBSY1‐VP1, pIBSY1‐L‐VP1 and pIBSY1‐P1 contained the capsid protein VP1 cDNA, a leader sequence of the pseudorabies virus glycoprotein C linked to the VP1 cDNA, and capsid precursor protein P1 (VP1‐4) cDNA gene of FMDV type O/Taiwan/97, respectively. The VP1 and P1 gene fragments were purified from agarose gel and subcloned into the EcoR I site and BamH I site of the pIBSY1 vector following the standard cloning procedure. The plasmid of pIBSY1‐L‐VP1 was subcloned from a plasmid containing a leader sequence of the pseudorabies virus glycoprotein C 28 (a generous gift from Dr. Ching‐Hua Chang) that was digested with Hind III and EcoR I and blunt‐end ligated into the pIBSY1‐VP1 vector. We prepared a pIBSY1‐P1 vector that contains all of the viral structural proteins. The resulting ligation mixture was used to transform E. coli DH5‐α competent cells (Gibco, Grand Island, NY, USA). Restriction endonuclease digestion mapping and authenticity of the sequence of inserted DNA was verified by an ABI 377 autosequence analysis. The constructed plasmids were subsequently purified using an EndoFree Plasmid Mega kit (Qiagen, CA, USA) and found to contain less than 4.5 EU/ml of endotoxin as determined by using the Limulus amoebocyte lysate analysis kit (QCL‐1000, BioWhittaker).
Expression and purification of recombinant viral protein VP1
The rVP1 capsid protein was expressed in E. coli, purified and refolded as described previously by Wang et al. 29. The concentration of purified viral protein was determined by measuring optical density at 280 nm, and the protein was subjected to Western blot analysis with anti‐FMDV antibody for verification of authenticity. Purified viral protein was then used in ELISA tests as an antigen source.
In vivo or in vitro gene‐gun‐mediated transgene expression
A helium gas‐driven gene gun was used for most in vivo and all in vitro DNA transfections as previously described 30. Plasmid DNA was precipitated onto 1 or 2 µm gold particles using the spermidine/CaCl2 coating method. The DNA/gold particle preparation was coated onto the inner surface of Tefzel tubing in the presence of 0.5 mg/ml polyvinylpyrrolidone (Sigma) and then cut into 0.5 inch segments to be used as DNA cartridges. Each DNA cartridge in this study was made to deliver 0.7 mg of gold particles and 1.75 µg of plasmid DNA. Gene transfer experiments were performed in BHK‐21 cells in culture or mouse and pig skin tissues of test animals. Aliquots of 5 × 105 cells per 35 mm dish were blasted in vitro by using the Helios gene gun (Bio‐Rad Laboratories, CA, USA) with a burst pressure of 150 psi. Particle‐mediated DNA delivery in vivo to the abdominal skin tissue of test mice and pigs was carried out at a discharge pressure of 350 and 500 psi, respectively. Transfected BHK‐21 cells, mouse and pig skin tissues were harvested at 24 h post‐bombardment, and expression of transgenic VP1 and P1 proteins was detected by immuno‐fluorescence staining and Western bolt analysis with rabbit anti‐VP1 polyclonal antibody.
Gene‐gun‐mediated DNA immunization into mice
DNA transfection into skin of test mice or pigs was carried out using the Helios gene gun system. Cartridges containing plasmid DNA (e.g. VP1, L‐VP1 and P1 vectors) were prepared as described above. Three test groups of 6‐ to 8‐week‐old BALB/cByJ (H‐2d) mice (Animal Care Center, Taipei, Taiwan) were immunized with the pIBSY1‐VP1, pIBSY1‐L‐VP1 or pIBSY1‐P1 expression vectors. Five mice per group were immunized with test DNA three to five times, each at an interval of 2 weeks.
Electroporation‐mediated DNA immunization into mice
Direct gene delivery by in vivo electroporation was performed as previously described by Kadowaki et al. 31. Plasmid DNAs (100 µg) in phosphate‐buffered saline (PBS) were injected into the tibialis anterior (TA) muscle of 10‐week‐old BALB/cByJ (H‐2d) and immediately electroporated with a pulse of electricity, using a two‐needle array electrode (BTX, San Diego, CA, USA) with 5 mm distances between them. The electrode was inserted longitudinally relative to the muscle fibers and six pulses of 100 V were given by a BTX square wave generator at a rate of one pulse per second, each lasting for 50 ms. Groups of mice (n = 4) were electroporated with plasmid DNAs at 3‐week intervals a total of four times. Serum samples of test mice were collected at day 0 or day 10 post‐vaccination. The vaccinated mice were challenged 3 weeks after the third boosting.
Test of antisera and challenge of adult mice with FMDV
Blood samples of test mice were collected for ELISA tests and virus challenge experiments were performed at day 10 post the booster injections. One group of mice was immunized with an injection of 0.1 ml of a commercially available, conventional FMDV vaccine (Aftopor, serotype O Taiwan; Merial Animal Health Ltd. Biological Laboratory, UK), serving as a positive control for this study, and yet another group of mice receiving no treatment served as negative control. For virus challenge experiments, adult BALB/cByJ mice (H‐2d) with or without prior vaccination treatments were injected intraperitoneally with a virus suspension (0.1 ml) containing 106 TCID50 virus particles of K strain O/Taiwan/97 FMDV. Blood was withdrawn from the test mice at 0, 1, 2, 3, 4 and 5 days post‐challenge. Individual blood samples (100 µl) were added to BHK‐21 cell cultures and incubated with gentle rocking at 37 °C for 60 min. The cell sheets were then washed twice with medium, and incubated with fresh medium supplemented with 2% fetal calf serum (FCS) for 3 days in the presence of 5% CO2. Presence of virus titer in sera of test mice was quantitatively determined by the appearance of cytopathic effect (CPE) of FMDV in BHK‐21 cell cultures. Virus clearance was determined by the absence of virus in sera of test mice at 1 to 2 days post‐challenge.
Measurement of antibody titers in serum
ELISA was used to determine the titer of anti‐VP1 antibodies. In brief, the purified recombinant VP1 protein in PBS was adsorbed directly onto the Nunc‐Maxisorb immunoplates at a concentration of 1 µg/well overnight at 4 °C. Plates were washed three times with PBST (PBS containing 0.1% Tween‐20) and blocked with 5% skim milk in PBS for 1 h at 37 °C. Sera were tested in fixed dilution series and incubated for 1 h at 37 °C. Plates were washed again and treated with a suitable concentration of biotinylated anti‐mouse or anti‐swine IgG antibodies for 1 h at 37 °C. Subsequently, the plates were washed and streptavidin‐peroxidase (1 : 3000 dilution, Vector, CA, USA) was added to the plates. After incubation for 1 h at 25 °C, the plates were washed again. The enzyme substrate 3,3′,5,5′‐tetramethylbenzidine (Sigma) was then added, and the reaction was carried out at room temperature for 10 min. Finally, an equal volume of 1 N H2SO4 was added to stop the reaction and absorbance at 450 nm was measured by an ELISA reader.
Assay for neutralizing antibodies
The method described previously by Wang et al. 32 was employed. In brief, sera from test animals were inactivated at 56 °C for 30 min. Test or control serum samples (50 µl) were added to wells at the end of each row of a 96‐well tissue culture plate, and then diluted in a two‐fold serial dilution across the plates. Fifty microliters of 100 TCID50 virus suspensions were added to each well, and the plate was vortexed for 1 min. After incubation at 37 °C in 5% CO2 for 90 min, 100 µl of BHK‐21 cell suspension (106 cells/ml) in Eagle's MEM containing 8% FCS were added to each well. The plate was incubated for an additional 48 h and the number of survived cells determined. The titer was expressed as the reciprocal of the final serum dilution that resulted in the neutralization of viral activity by 50%.
Immuno‐florescence staining
The adherent BHK‐21 cell layers grown on culture plates were washed with PBS and then incubated with polyclonal rabbit anti‐VP1 antibody for 45 min at room temperature. Samples were washed and stained with goat anti‐rabbit IgG‐fluorescein isothiocyanate (FITC). The samples were then analyzed by immuno‐fluorescence microscopy.
Western blot analysis
The transgenic expression of the FMDV structural protein precursor (P1) was detected immunologically by standard Western blotting analysis. In brief, transfected skin tissues were collected from test animals by excising a small uniform portion of the targeted, gene‐gun‐bombarded skin area. Skin samples were cut with scissors, minced and sonicated within extraction buffer [0.1% Triton X‐100 and protease inhibitor cocktail (Roche) in PBS] at 0 °C. Crude tissue extracts were spun at 10 000 g for 10 min and mixed with an equal volume of sample buffer. After boiling for 5 min, samples were subjected to 4–12% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS‐PAGE), and then transferred to a PVDF (polyvinylidene difluoride) membrane. The blots were blocked using 5% skim milk in PBS and incubated with a home‐made, polyclonal rabbit anti‐VP1 antibody (1 : 5000) in PBS for 1 h at 37 °C. Immuno‐blots were washed three times with PBST and then treated with goat biotinylated anti‐rabbit IgG antibodies (1 : 3000 dilution, Vector, CA, USA) for 1 h at 37 °C. Subsequently, the membranes were washed again and streptavidin‐peroxidase (1 : 3000 dilution) added to test blots. After incubation for 1 h at 25 °C, the membranes were washed again and stained with enhanced chemiluminescent (ECL™; Amersham Pharmacia Biotech).
Immuno‐florescence staining
The adherent BHK‐21 cell layers grown on culture plates were washed with PBS and then fixed with 3.7% formaldehyde in PBS for 10 min. After washing with PBS and blocking with normal horse serum, cell samples were incubated with home‐made polyclonal rabbit anti‐VP1 antibody (1 : 5000) and 0.1% saponin in PBS for 1 h at room temperature. Test samples were washed again and stained with goat anti‐rabbit IgG‐fluorescein isothiocyanate (FITC) as secondary antibody. Cell samples were then examined and photographed by immuno‐fluorescence microscopy using epilumination with an Olympus fluorescent scope.
Results
Construction of cDNA expression plasmid for FMDV vaccine
The original FMDV serotype O Taiwan preparations were officially and legally provided by the National Institute for Animal Health (Dr. Ming‐Hwa Jong, NIAH, Taiwan) and used for viral RNA extraction and cDNA fragment constructions. By using the P3 laboratory facility at NIAH, we cloned and isolated two FMDV cDNA gene fragments, including the 0.65 kb cDNA encoding the VP1 protein and the 2.2 kb cDNA encoding P1 (i.e. containing VP4, VP2, VP3, and VP1 viral proteins in sequence) as the whole capsid structural protein precursor. For both cDNA fragments, all of the 3′ protease genes and the subsequent 3′ terminal sequences were totally deleted, due to consideration of eliminating potential risks in such a viral DNA vaccine design. For potential future application to livestock animal DNA vaccination, we have adapted, functionally verified, and sequenced a CMV promoter/enhancer sequence and a ‘clinical trial‐grade’ mammalian gene expression vector system, i.e. the pIBSY1 plasmid vector or the pWRG 33, as guided for use by the Food and Drug Administration, USA, for recommended use in human gene therapy clinical trials. We then subcloned the two test FMDV viral protein cDNA clones into this expression plasmid.
Expression of cDNA expression vectors using gene‐gun‐ or electroporation‐mediated transfection for gene‐based vaccination
By using a luciferase transgene reporter assay, we demonstrated that this pIBSY1‐CMV promoter conferred approximately 35% more transient luciferase activity than a standard commercially available CMV promoter (pNAss; Clontech, Palo Alto, CA, USA), and the pIBSY1‐CMV promoter vector was hence employed for the rest of this study. In order to establish that the Bio‐Rad Helios gene gun system can be effectively applied to the current DNA vaccination experiment, we performed a number of reference tests to verify the efficiency of the mouse skin gene transfection system. With each 1.75 µg of a CMV‐luciferase (Lux) cDNA vector blasted onto mouse skin, 10–25 ng transgenic Lux protein per skin tissue site was obtained at 24 h post‐transfection. In comparison, about 90 ng transgenic Lux proteins per 1 × 106 BHK‐21 cells per 24 h were detected under in vitro transfection conditions. A dose of 1–5 ng hAAT cDNA expression vector was shown to produce about 1 ng of transgenic hAAT protein, and this induced readily detectable levels of antibodies against hAAT proteins in gene gun/skin immunized BALB/c mice. These results hence established the efficacy for DNA vaccination using the Helios gene gun. It is also important to note here that these levels of reporter transgene expression obtained with the Helios gun are very close to the levels we have previously established from the Accell® gene gun device 34.
To evaluate the efficacy of gene gun versus electroporation transfection for transgene expression and (DNA) immunization (e.g. the production of antibodies), we used a CMV‐luciferase reporter system and human α‐antitrypsin (hAAT) cDNA vaccination, respectively. The abdominal skin tissues of BALB/cByJ mice (n = 5) were transfected with 6 µg of CMV‐luciferase plasmid DNA with gene gun. Alternatively, muscle tissues of two hind legs of BALB/cByJ mice were transfected with 100 µg of luciferase plasmid DNA (50 µg/leg) via intramuscular injection followed by electroporation. At 20 h post‐transfection, test tissue samples were extracted and luminometer assays performed for luciferase activity. For DNA immunization, CMV‐hAAT cDNA was similarly transfected into mice using these two methods, and mean serum titers of anti‐hAAT antibodies in test mice (n = 5) were assayed with ELISA. From these two experiments (n = 5 mice/test group), we observed that (1) a 1.9‐fold higher transgenic CMV‐Lux activity was obtained from the electroporation method (i.e. 5.53 ± 0.4 × 107 RLU/site) as compared with the gene gun method (i.e. 2.85 ± 0.26 × 107 RLU/site), and (2) a 44‐fold higher anti‐hAAT antibody titer was obtained from the electroporation method (i.e. reciprocal titer at 1142.9 ± 362.8) as compared with the gene gun method (i.e. reciprocal titer at 25.7 ± 9.8). These results imply that transient expression levels of test reporter DNA vaccine transgenes obtained from different DNA delivery methods may not, as an effect on vaccination, reflect proportionally to their efficacy in production of antibodies.
A verified hyper‐immune pig serum provided by NIAH was used as our antibody source. For this study, we generated a recombinant VP1 protein in E. coli, and it was purified, refolded and used as an antigen protein for producing anti‐VP1 antibody. Standard ELISA and Western blot analysis were used for verification and quantification of the transgenic VP1 or other viral proteins. As shown in Figure 1, transgenic expression of VP1 protein was effectively detected in BHK‐21 cells (Figures 1A and 1B) and mouse skin tissue (Figures 1C and 1D) when they were gene‐gun‐transfected using the VP1 cDNA expression vector (pIBSY1‐VP1). One day after transfection, in vivo expression of transgenic FMDV VP1 and P1 polypeptide in pig skin tissue had an apparent molecular weight of 26 000 and 81 000, respectively, as predicted and experimental results obtained by Western blot analysis with anti‐VP1 antibody (Figure 2). Since only the anti‐VP1 antiserum was available for this study, we were unable to evaluate the expression of VP2, VP3 and VP4 proteins in our experiments.
Figure 1.
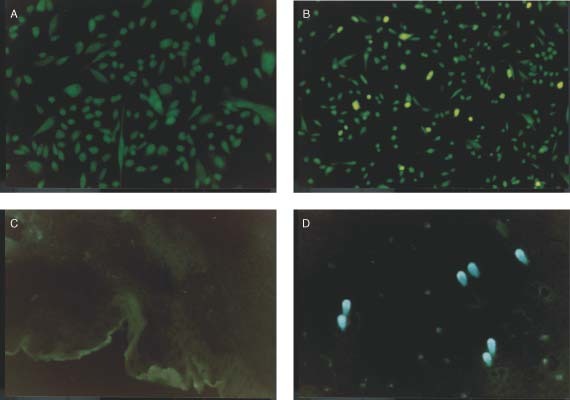
Transgenic expression of FMDV/VP1 protein in vitro (A, B) in baby hamster kidney (BHK‐21) cell cultures and in vivo (C, D) in mouse skin tissues, as detected by indirect immuno‐fluorescence staining. Control (empty) cDNA vector (A, C) and VP1‐expressing cDNA vector (B, D) were transfected into correspondent target cells/tissues. Transfected BHK‐21 cells and mouse skin tissues were harvested 24 h post‐bombardment, and expression of transgenic VP1 protein was detected by immuno‐fluorescence staining with polyclonal rabbit anti‐VP1 antibody. Details of experimental procedures/assays are as described in ‘Materials and methods’
Figure 2.
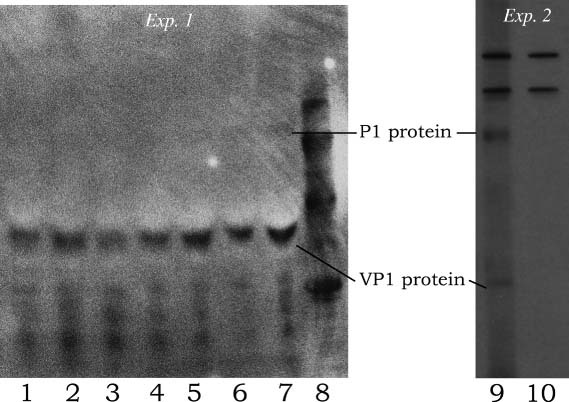
Western blot analysis of transgenic FMDV VP1 and P1 proteins via gene‐gun‐mediated transfection into pig skin tissue. The VP1 cDNA (lanes 1–4), and P1 cDNA expression plasmids (lanes 5–7 and 9), were transfected into pig abdominal skin tissue via gene gun delivery. Lanes 8 and 10 were molecular markers (94, 67, 45 and 20.1 kDa) and control, respectively. The blasted skin tissues were collected 24 h post‐bombardment, and transgenic expression of VP1 and P1 polypeptide detected by Western blot analysis as described in ‘Materials and methods’. Expression of P1 protein in experiment 2 was detected at a much increased abundance as compared to those detected in experiment 1. Apparent non‐specific binding of two high molecular weight bands was detected for both untreated and P1‐transfected pig skin tissues in experiment 2
An adult mouse system for virus challenge and clearance of FMDV
Previously, researchers have reported the use of pigs 35, guinea pigs 26, 36 or suckling mice 37 as animal models for vaccination and viral challenge experiments with FMDV. FMDV replicates in the cytoplasm of host cells and new virus particles are generated in large numbers within the cytosol. With time, the infected cells are destroyed and new virus particles released to infect other cells. In this study on an adult mouse (2–3 month old) system, we found that infecting FMDV first appeared in test mouse blood for only a few minutes, and replicated in the blood at 8–15 h post‐inoculation with 106 TCID50 virus particles via intraperitoneal (IP) injection. However, the virus titer then decreased and was eventually cleared in the serum of test mice after an additional 3–5 days. We then found that BALB/c mice first immunized with a commercially available, killed virus vaccine or the current DNA vaccine strategy and then inoculated with highly infectious FMD virus, viremia, cleared the virus in 1–2 days, instead of the 3–5 days in the control or non‐vaccinated mice (Figure 3). As no symptoms were detectable in FMDV‐infected mice, this adult mouse challenge model was based on the cytopathic effect (CPE) assay of the clearance of virus particles in serum collected 1–6 days post‐intraperitoneal injection of the challenging FMDV. Using this protocol, we observed that virus particles were routinely and totally cleared in 1–2 days for 100% of test mice vaccinated with commercially obtained killed virus vaccines. In contrast, both the naive and the empty vector‐immunized mice routinely (70–100%) still suffered high or medium levels of viremia during the first 1–3 days after viral challenge (Figure 3). This result suggested strongly that there was little or no virus replication in the vaccinated mice. This adult mouse system thus provided a convenient and quick assay for the evaluation of molecular DNA vaccine strategies against FMDV (see below).
Figure 3.
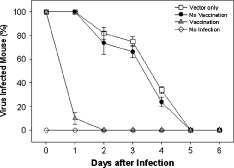
Vaccination and virus challenge with FMDV in an adult mouse system. Adult BALB/cByJ mice were treated with or without prior vaccination with commercially available, inactivated vaccine, and then injected intraperitoneally with a suspension containing 106 TCID50 virus particles of K strain O/Taiwan/97 FMDV. Blood samples were withdrawn from test mice at 0, 1, 2, 3, 4, 5 and 6 days post‐challenge. Individual blood samples (100 µl) were added to BHK‐21 monolayer cultures and the presence of virus in sera of test mice was determined by the appearance of cytopathic effect of FMDV in BHK‐21 cells as described in ‘Materials and methods’
Immunogenicity and potency of DNA vaccine
Six‐ to eight‐week‐old, cohort BALB/c mice were systematically vaccinated using the Helios gene gun with VP1, L‐VP1 or P1 cDNA expression vectors. More than 200 BALB/c or C57 mice under various experimental conditions have been skin‐vaccinated via gene gun in a series of experiments, with a regime of one prime (day 0) and two booster (days 14 and 28) DNA transfections. Test mice were monitored, and pre‐immune and post‐immune sera collected and analyzed for transgenic VP1 antigen protein expression, and for production of neutralizing antibodies in test mice. We observed that DNA vaccination with plasmid vector expressing VP1 alone routinely induced very low levels of anti‐VP1 antibodies and no detectable levels of virus‐neutralizing antibody activities in all test mice, providing a very important negative baseline for this study (Tables 1 and 2). Replicate (>6) experiments were performed and up to 60 mice tested for the VP1 results shown in Table 2; similar results were always obtained. In contrast, however, skin DNA vaccination with a cDNA construct expressing the precursor polypeptide of the four FMDV capsid proteins (VP4‐1), namely P1, induced antibodies against the VP1 protein as well as neutralizing antibodies against the FMDV, and resulted in a significant protective immunity (virus clearance) in test mice (Table 2). Other than gene‐gun‐mediated in vivo gene transfer, intramuscular injection of DNA followed by in situ electroporation is another physical means for effective gene vaccination in experimental animal systems. Table 3 shows that a very similar result was obtained from the electroporation‐mediated DNA immunization method as compared with the gene gun method. Neutralizing antibody titers and virus clearance in test mice were detected after immunization with P1 cDNA plasmids by in vivo electroporation delivery into muscle tissue. Furthermore, these results, obtained from two independent gene delivery methods, were obtained without the use of FMDV viral protease‐encoding genes in DNA co‐transfection/vaccination, i.e. the 2A or 3ABC protease‐expressing cDNA genes of FMDV were not included for transgene expression in the current vaccinating‐DNA vector construct. In one P1 cDNA immunized mouse in this experiment, the anti‐VP1 antibody ELISA titers and the anti‐viral neutralizing antibody titers were found to be as high as 26 500 and 256, respectively. In the mouse challenge experiment, 80–100% mice immunized with this P1 cDNA expression plasmid were found to be effectively and quickly cleared of the infecting FMDV particles, whereas control animals could not clear virus rapidly (Tables 2 and 3).
Table 1.
Comparison of antibody response levels in test mice following gene‐gun‐mediated skin transfection with expression plasmids encoding VP1, L‐VP1 or P1 cDNA of FMDV
| cDNA vector | Relative antibody level in sera of 6 different test micea | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| None | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Vector only | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| pIBSY1‐VP1 (soluble form) | 0.01 | 0.00 | 0.01 | 0.01 | 0.00 | 0.04 |
| pIBSY1‐L‐VP1 (membrane‐bound form) | 0.26 | 0.22 | 0.31 | 0.30 | 1.80 | 2.30 |
| pIBSY1‐P1 (capsid precursor protein) | 0.36 | 0.30 | 0.32 | 0.20 | 0.25 | 1.60 |
Recombinant VP1 proteins were coated at 1 µg/well to 96‐well microplates. Mouse sera were prepared from blood samples and added to microwells at 1 : 100 dilutions. ELISA tests were developed using 3,3′,5,5′‐tetramethylbenzidine (TMB) as substrate for peroxidase, and stopped with 1 N H2SO4, and absorbance values read at OD 450 nm.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Table 2.
Neutralizing antibody titer and virus clearance in mice receiving cDNA plasmids by in vivo gene gun delivery post 3rd boosting
| cDNA vector | Anti‐rVP1 titer | NA titera | Virus clearanceb |
|---|---|---|---|
| None | 30 ± 5 | 0 | 0/5 (0%) |
| pIBSY1 | 30 ± 5 | 0 | 0/5 (0%) |
| pIBSY1‐VP1 | 98 ± 79 | 0 | 0/5 (0%) |
| pIBSY1‐P1 | 5420 ± 11 784 | 52 ± 114 | 4/5 (80%) |
The titer of neutralizing antibodies (NA titer) of each test mouse is expressed as a reciprocal of the final dilution of test serum that caused a 50% reduction in test virus titer as described in ‘Materials and methods’. The background (negative control) value of our CPE test in NA titer assay (as detected at the highest serum concentration tested) was measured at ≤3, and this value was used as a background for substration of the NA titers of other tested samples.
The clearance of virus was determined by the absence of virus in the serum of test mice at 48 h after FMDV challenge and expressed as a ratio of the number of viremia‐free mice/number of challenged mice.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Table 3.
Neutralizing antibody titer and virus clearance in mice receiving DNA plasmids by in vivo electroporation delivery post 3rd boosting
| cDNA vector | Anti‐rVP1 titer | NA titera | Virus clearanceb |
|---|---|---|---|
| None | N.D. | 0 | 0/5 (0%) |
| pIBSY1 | 30 ± 5 | 0 | 0/5 (0%) |
| pIBSY1‐VP1 | 2029 ± 999 | 0 | 0/5 (0%) |
| pIBSY1‐P1 | 1364 ± 2680 | 10 ± 22 | 8/8 (100%) |
The assays and analyses of NA titera and virus clearanceb are the same as described under Table 2. N.D.: not determined.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Discussion
Since DNA vaccine by design often makes use of only a limited fragment of the viral genomic cDNA, there is hence little chance for ‘live’ viral infection that would otherwise often happen by the contamination of live virus that escapes during the inactivation process for making vaccines. The reason we designed the DNA vaccine vector without incorporating the protease‐encoding genes was based on safety considerations, because an exact processing of the viral capsid proteins can create authentic viral capsids by processing with specific viral proteases, and we envision this in turn might generate novel recombinant virus in the host with other types of virus, e.g. at the virus assembly level. There are speculations that the severe acute respiratory syndrome (SARS) virus may be generated as a ‘hybrid’ virus between human and wild animal coronaviruses 38. The current DNA vaccine strategy we believe may eliminate such a remote possibility.
The suckling mice protection assay has previously been employed as a useful method in vaccine studies of FMDV, by serving as an indicator of neutralizing antibodies present in the adult test mouse serum, and it has been shown to confer a good correlation with the protection assay 37. In this study, we instead have established a similar but more convenient and faster assay method for the challenge and clearance of FMDV using only the adult mouse system. As seen in Figure 3, we have repeatedly observed that, as compared with the control set mice (no vaccination), a virus clearance that is 2 to 3 days earlier, or a total lack of FMD virus titer, can be effectively obtained from vaccinated mice that are either immunized with the current P1 DNA vaccine or the commercially available, inactivated virus vaccine. This assay, just like a 1–3 day transient transgenic luciferase activity assay, may hence serve as an efficient, large sample number, surrogate assay system for future studies on virus challenge, clearance and protection against the FMDV systems.
As we have shown in Figure 3 and other related experiments, this short viremia period was detected in our study by using a protocol of employing a virus titer (dosage) of 106 TCID50 virus particles of K strain O/Taiwan/97 FMDV and the adult BALB/cBYJ (H‐2d) mice as host animals. In the present study, the 2–3 day shorter period for viral clearance has proved as experimentally distinguishable and useful in our assays of not just DNA vaccines, but also in studies of peptide vaccines against FMDV, as we previously reported 26. These results show that this assay is sensitive enough for a spectrum of studies on vaccine efficacy. It would be interesting to investigate in future studies whether various anti‐FMDV vaccines or vaccines at different vaccination dosages that confer a substantial difference in viral clearance activities or vaccine efficacy in pigs could also be effectively distinguished from each other within very specific time points of this 2–3 day period of our current mouse model. So far, we have not accumulated enough data to evaluate this possibility. Since there is an apparent correlation between the viral clearance activity and the production of neutralizing antibodies 29, we believe it may also be desirable to correlate the viral clearance time with the titers of neutralizing antibodies. Future experiments will be necessary to assess these possibilities.
With the current adult mouse system, we show that the whole P1 of the FMDV capsid protein‐encoding cDNA sequence without the presence (i.e. co‐expression) of viral proteases, but not the VP1 protein by itself, can elicit a significant level of neutralizing antibodies and confer an effective level of protection against viral challenge with FMDV. Previous studies have shown that the whole virus particle or an ‘authentic’ empty capsid assembly was very important for induction of neutralizing antibodies and protection against viral challenge 21, 22, 23. In comparison, our current result on the efficacy of P1 DNA vaccine but the lack of it for the VP1 DNA vaccine may be explained by the following possibilities. Firstly, the transgenic VP1 protein produced in mouse epidermal cells cannot serve as an effective immunogen in our study, yet, in contrast, the VP1 and/or P1 protein moiety(s) from the multiple subunit polyprotein of VP‐4, ‐2, ‐3 and ‐1 (as a single chain transgenic P1 protein) can however serve as a potent immunogen, presumably by presenting as a different protein folding as the ‘free or single unit’ VP1 transgenic protein. Secondly, the transgenic P1 protein, consisting all of the FMD protein components of the virus capsid, may be able to form some kind of modified capsid‐like structural assemblies or protein aggregates in test mouse skin cells, effecting as a strong viral immunogen. A third possibility is that endogenous protease (e.g. chymotrypsin) activities of mouse host cells may process the P1 transgenic protein into efficacious configurations or conformations, resulting in production of VP1, P1 or other viral proteins with novel (non‐authentic) foldings, and these can serve as potent viral protein epitopes. Western blot analyses (Figure 2) showed that the P1 precursor polypeptide can be transiently expressed between low (for Exp.‐1) to readily (for Exp.‐2) detectable levels. In Exp.‐2, different animals from Exp.‐1 were used, and we observed an increased abundance of P1 protein. For both experiments, correct size and transgenic VP1 protein, derived by ‘host cell’ processing, were clearly detected at high levels in test pig skin tissues that were gene‐gun‐transfected with the P1 cDNA expression constructs. These results suggest that authentic and intact transgenic P1 and VP1 viral proteins were produced in immunized animals. Xing et al. 39 have studied the interactive, multiple domains of the FMDV for involvement of VP3, ‐2 and ‐1 proteins on the topical structure of FMDV. Their findings and our collaboration with them in this study led us to suggest that capsid‐like protein aggregates or ‘virus‐like particles’ (VLP) from transgenic P1 products may exist transiently or at relatively low frequency. Future studies using scanning electron microscopy and protein biochemistry techniques will be required to discern the actual molecular mechanism.
The immunogenicity of capsid protein VP1 has been shown to be conferred mostly from the G‐H loop of VP1 40, 41. In comparison with our previous work on the immune response obtained from the E. coli‐produced, recombinant capsid protein VP1 29, we have observed in this study that the DNA vaccines encoding VP1 or P1 protein were much (10–100‐fold) less immunogenic than an equivalent dose of the VP1 antigen preparation administered in the form of recombinant protein in mice. Throughout multiple independent experiments, using both gene‐gun‐ and electroporation‐mediated DNA vaccinations with a plasmid vector expressing only the VP1 cDNA, no detectable effect on the production of anti‐viral neutralizing antibodies and virus clearance in a total of 60 VP1 tested mice has been seen (Tables 2 and 3). The lack of any immune response to the VP1 cDNA vaccine, as compared to the P1 cDNA vaccine, may due to a number of reasons: first, the lack of appropriate folding of transgenic VP1 in test mouse skin tissue or tibialis anterior (TA) muscle; second, antigen presentation of the VP1 protein is not favored in test skin or muscle tissues; third, a very short half‐life or inappropriate transgenic protein processing of the expressed VP1 antigen in test host cells; and fourth, the immune response of the Th2 pathway in skin tissue or TA muscles may be too low to result in a threshold activity. Future studies will be needed to investigate these possibilities.
In summary, we have shown that FMDV can replicate in the blood of test mice after an infection with an intraperitoneal injection of 106 TCID50 virus particles. By expressing only a four FMDV capsid protein sequence as a single polypeptide molecule (P1) from a cDNA vector via skin or muscle DNA vaccination, we could elicit a significant immune response (i.e. neutralizing antibody) against FMDV, providing protection against viral challenge in an adult BALB/c mouse system. The current experimental system creates the potential for future studies on a complete set of viral capsid proteins as precursor molecules for DNA vaccination. This and related molecular strategies for developing future FMDV or other virus DNA vaccines, and for research into molecular mechanisms of the target virus (e.g. host cell processing and assembling of P1 protein components without viral proteases), could be investigated using the current gene delivery/mouse evaluation system.
Acknowledgements
This work was supported by grants from Academia Sinica and by National Science Council of the Republic of China (NSC 88‐2173‐B‐001‐005).
References
- 1. Yang PC, Chu RM, Chung WB, Sung HT. Epidemiological characteristics and financial costs of the 1997 foot‐and‐mouth disease epidemic in Taiwan. Vet Rec 1999; 145: 731–734. [DOI] [PubMed] [Google Scholar]
- 2. Stone R. Report Urges U.K. to vaccinate herds. Science 2002; 297: 319–321. [DOI] [PubMed] [Google Scholar]
- 3. Rueckert RR. Picornaviridae: the viruses and their replication In Virology, Fields BN, Knipe DM, Howley PH. (eds). Lippincott‐Raven Publishers: Philadelphia, PA, 1996; 609–654. [Google Scholar]
- 4. Acharya R, Fry E, Stuart D et al. The three‐dimensional structure of foot‐and‐mouth disease virus at 2.9 A resolution. Nature 1989; 337: 709–716. [DOI] [PubMed] [Google Scholar]
- 5. Doel TR, Chong WKT. Comparative immunogenicity of 146S, 75S, and 12S particles of foot‐and‐mouth disease virus. Arch Virol 1982; 73: 185–191. [DOI] [PubMed] [Google Scholar]
- 6. Grubman MJ, Morgan DO, Kendall J, et al. Capsid intermediates assembled in a foot‐and‐mouth disease virus genome RNA‐programmed cell‐free translation system and in infected cells. J Virol 1985; 56: 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rowlands DJ, Sangar DV, Brown F. A comparative chemical and serological study of the full and empty particles of foot‐and‐mouth disease virus. J Gen Virol 1975; 26: 227–238. [DOI] [PubMed] [Google Scholar]
- 8. Rweyemamu MM, Terry G, Pay TWF. Stability and immunogenicity of empty particles of foot‐and‐mouth disease virus. Arch Virol 1979; 59: 69–79. [DOI] [PubMed] [Google Scholar]
- 9. Petit MC, Benkirane N, Guichard G, et al. Solution structure of a retro‐inverso peptide analogue mimicking the foot‐and‐mouth disease virus major antigenic site. Structural basis for its antigenic cross‐reactivity with the parent peptide. J Biol Chem 1999; 274: 3686–3692. [DOI] [PubMed] [Google Scholar]
- 10. Brown F, Benkirane N, Limal D, et al. Delineation of a neutralizing subregion within the immunodominant epitope (GH loop) of foot‐and‐mouth disease virus VP1 which does not contain the RGD motif. Vaccine 1999; 18: 50–56. [DOI] [PubMed] [Google Scholar]
- 11. Harrison SC. Picornaviruses. Finding the receptors. Nature 1989; 388: 205–206. [DOI] [PubMed] [Google Scholar]
- 12. Mateu MG, Martinez MA, Capucci L, et al. A single amino acid substitution affects multiple overlapping epitopes in the major antigenic site of foot‐and‐mouth disease virus of serotype C. J Gen Virol 1990; 71: 629–637. [DOI] [PubMed] [Google Scholar]
- 13. Liu MA, Ulmer JB. Gene‐based vaccines. Mol Ther 2000; 1: 497–500. [DOI] [PubMed] [Google Scholar]
- 14. Oshikawa K, Rakhmilevich AL, Shi F, et al. Interleukin 12 gene transfer into skin distant from the tumor site elicits antimetastatic effects equivalent to local gene transfer. Hum Gene Ther 2001; 12: 149–160. [DOI] [PubMed] [Google Scholar]
- 15. Collen T, Baron J, Childerstone A, et al. Heterotypic recognition of recombinant FMDV proteins by bovine T‐cells: the polymerase (P3Dpol) as an immunodominant T‐cell immunogen. Virus Res 1998; 56: 125–133. [DOI] [PubMed] [Google Scholar]
- 16. Mulcahy G, Pullen LA, Gale C, et al. Mouse protection test as a predictor of the protective capacity of synthetic foot‐and‐mouth disease vaccines. Vaccine 1991; 9: 19–24. [DOI] [PubMed] [Google Scholar]
- 17. Barteling SJ, Woortmeyer R. Multiple variants in foot‐and‐mouse disease virus (FMDV) populations: the Achilles heel for peptide and rec. DNA vaccines? Dev Biol Stand 1987; 66: 511–521. [PubMed] [Google Scholar]
- 18. Domingo E, Verdaguer N, Ochoa WF, et al. Biochemical and structural studies with neutralizing antibodies raised against foot‐and‐mouth disease virus. Virus Res 1999; 62: 169–175. [DOI] [PubMed] [Google Scholar]
- 19. Weidt G, Deppert W, Utermohlen O, et al. Emergence of virus escape mutants after immunization with epitope vaccine. J Virol 1995; 69: 7147–7151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Taboga O, Tami C, Carrillo E, et al. A large‐scale evaluation of peptide vaccines against foot‐and‐mouth disease: lack of solid protection in cattle and isolation of escape mutants. J Virol 1997; 71: 2606–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ward G, Rieder E, Mason PW. Plasmid DNA encoding replicating foot‐and‐mouth disease virus genomes induces antiviral immune responses in swine. J Virol 1997; 71: 7442–7447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chinsangaram J, Beard C, Mason PW, et al. Antibody response in mice inoculated with DNA expressing foot‐and‐mouth disease virus capsid proteins. J Virol 1998; 72: 4454–4457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beard C, Ward G, Rieder E, et al. Development of DNA vaccines for foot‐and‐mouth disease, evaluation of vaccines encoding replicating and non‐replicating nucleic acids in swine. J Biotechnol 1999; 73: 243–249. [DOI] [PubMed] [Google Scholar]
- 24. Benvenisit L, Rogel A, Kuznetzova L, et al. Gene gun‐mediated DNA vaccination against foot‐and‐mouth disease virus. Vaccine 2001; 19: 3885–3895. [DOI] [PubMed] [Google Scholar]
- 25. Cedillo‐Barron L, Foster‐Cuevas M, Belsham GJ, et al. Induction of a protective response in swine vaccinated with DNA encoding foot‐and‐mouth disease virus empty capsid proteins and the 3D RNA polymerase. J Gen Virol 2001; 82: 1713–1724. [DOI] [PubMed] [Google Scholar]
- 26. Huang H, Yang Z, Xu Q, et al. Recombinant fusion protein and DNA vaccines against foot and mouth disease virus infection in guinea pig and swine. Viral Immunol 1999; 12: 1–8. [DOI] [PubMed] [Google Scholar]
- 27. Wong HT, Cheng SCS, Chan EWC, et al. Plasmids encoding foot‐and‐mouth disease virus VP1 epitopes elicited immune responses in mice and swine and protected swine against viral infection. Virology 2000; 278: 27–35. [DOI] [PubMed] [Google Scholar]
- 28. Robbins AK, Watson RJ, Whealy ME, et al. Characterization of a pseudorabies virus glycoprotein gene with homology to herpes simplex virus type 1 and type 2 glycoprotein C. J Virol 1986; 58: 339–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang J‐H, Liang CM, Peng JM, et al. Induction of immunity in swine by purified recombinant VP1 of foot‐and‐mouth disease virus. Vaccine 2003; 21: 3721–3729. [DOI] [PubMed] [Google Scholar]
- 30. Kuo C‐F, Wang J‐H, Yang N‐S. Direct gene transfer and vaccination via skin transfection using a gene gun, In Methods in Molecular Medicine, vol. 69, Gene Therapy Protocols, (2nd edn), Morgan JR. (ed). Humana Press Inc.: Totowa, NJ, 2002; 137–147. [DOI] [PubMed] [Google Scholar]
- 31. Kadowaki S, Chen Z, Asanuma H, et al. Protection against influenza virus infection in mice immunized by administration of hemagglutinin‐expressing DNAs with electroporation. Vaccine 2000; 18: 2779–2788. [DOI] [PubMed] [Google Scholar]
- 32. Wang CY, Chang TY, Walfield AM, et al. Synthetic peptide‐based vaccine and diagnostic system for effective control of FMD. Biologicals 2001; 29: 221–228. [DOI] [PubMed] [Google Scholar]
- 33. Mahvi D, Burkholder JK, Tuner J, et al. Particle‐mediated gene transfer of GM‐CSF cDNA to tumor cells: implications for a clincally relevant tumor vaccine. Hum Gene Ther 1996; 7: 1535–1543. [DOI] [PubMed] [Google Scholar]
- 34. Qiu P, Ziegelhoffer P, Sun J, et al. Gene gun delivery of mRNA in situ results in efficient transgene expression and genetic immunization. Gene Ther 1996; 3: 262–268. [PubMed] [Google Scholar]
- 35. Mayr GA, O'Donnell V, Chinsangaram J, et al. Immune responses and protection against foot‐and‐mouth disease virus (FMDV) challenge in swine vaccinated with adenovirus‐FMDV constructs. Vaccine 2001; 19: 2152–2162. [DOI] [PubMed] [Google Scholar]
- 36. Dunn CS, Samuel AR, Pullen LA, et al. The biological relevance of virus neutralisation sites for virulence and vaccine protection in the guinea pig model of foot‐and‐mouth disease. Virology 1998; 247: 51–61. [DOI] [PubMed] [Google Scholar]
- 37. Wigdorovitz A, Carrillo C, Dus Santos MJ, et al. Induction of a protective antibody response to foot and mouth disease virus in mice following oral or parenteral immunization with alfalfa transgenic plants expressing the viral structural protein VP1. Virology 1999; 255: 347–353. [DOI] [PubMed] [Google Scholar]
- 38. Anand K, Ziebuhr J, Wadhwani P, et al. Coronavirus main proteinase (3CLpro) structure: basis for design of anti‐SARS drugs Science 2003; 300: 1763–1767. [DOI] [PubMed] [Google Scholar]
- 39. Xing L, Tjarnlund K, Lindquist B, et al. Distinct cellular receptor interactions in poliovirus and rhinoviruses. EMBO J 2000; 19: 1207–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bittle JL, Houghten RA, Alexander H, et al. Protection against foot‐and‐mouth disease by immunization with a chemically synthesized peptide predicted from the viral nucleotide sequence. Nature 1982; 298: 30–33. [DOI] [PubMed] [Google Scholar]
- 41. Kitson JD, McCahon D, Belsham GJ. Sequence analysis of monoclonal antibody resistant mutants of type O foot and mouth disease virus: evidence for the involvement of the three surface exposed capsid proteins in four antigenic sites. Virology 1990; 179: 26–34. [DOI] [PubMed] [Google Scholar]


