Abstract
OBJECTIVE: To report the number and timing of influenza A isolates, as well as overlapping respiratory viruses. Co‐circulating respiratory viruses may obscure the determination of influenza activity.
DESIGN: Prospective clinical surveillance for the new onset of respiratory illness followed by viral cultures during seven separate influenza seasons.
SETTING: The Wisconsin Veterans Home, a skilled nursing facility for veterans and their spouses.
RESULTS: Influenza A isolates were encountered in greater numbers than non‐influenza A isolates during three seasons. Seasonal variability is striking. In December 1992, we identified a large outbreak of respiratory illness. Influenza type B was cultured from 102 residents. In December 1995, influenza A was cultured from 285 people in Wisconsin. At that time, we identified outbreaks of respiratory illness in two of our four buildings. Based on statewide data, we suspected an influenza outbreak; however, 26 isolates of parainfluenza virus type 1 were cultured with no influenza. The potential importance of culturing at the end of the season was demonstrated in 1991–1992 when an outbreak of respiratory syn‐cytial virus (RSV) overlapped and extended beyond influenza A activity.
CONCLUSIONS: When interpreting new clinical respiratory illnesses as a basis for declaring an outbreak of influenza A, clinicians should realize that co‐circulating respiratory viruses can account for clinical illnesses. Clinicians might utilize healthcare dollars efficiently by performing cultures to focus the timing of influenza A chemoprophylaxis. Cultures could be performed when clinical outbreak criteria are approached to confirm an outbreak. Culturing of new respiratory illness could begin again before the anticipated discontinuation of prophylaxis (approximately 2 weeks). J Am Geriatr Soc 47:1087–1093,1999.
Keywords: nursing home, influenza outbreak
Mortality associated with influenza varies significantly from year to year.1 The Center for Disease Control tracked excess mortality in persons older than age 65 for 23 influenza seasons. No excess mortality was detected during four seasons. During the other 19 seasons, estimated influenza‐associated mortality ranged from 25 to >150 per 100,000 persons. Some years are outbreak years; in other years there are only sporadic cases. Early in the season, it is difficult to predict how contagious and virulent the circulating strain will be.
The Centers for Disease Control recommends, “When confirmed or suspected outbreaks of influenza A occur in institutions that house persons at high risk, chemoprophylaxis should be started as early as possible to reduce the spread of the virus.” 1 The suspicion of an outbreak of influenza A, however, does not confirm the existence of an outbreak. A critical clinician faced with increased rates of respiratory illness will want to know what proportion of illnesses are caused by influenza A and if subsequent attack rates and disease severity can be predicted from the clinical course of the suspected outbreak. Early recognition of explosive outbreaks with severe illness would seem to benefit most from aggressive institutional prophylaxis. However, it is unclear at what threshold sporadic influenza activity should elicit institutional chemoprophylaxis. Gomolin et al. have proposed criteria for a nursing home outbreak as a cluster of three individuals with new onset of respiratory illness and temperature elevation of more than 100CC on the same unit within 3 days when influenza has been laboratory‐confirmed in the facility. 2 Barker et al. proposed similar criteria with a cluster of two individuals within 2 days.1 Viral cultures should help clinicians to determine the outbreak threshold.
Outbreaks are suspected when regional laboratories report the isolation of influenza A and there is a clustering of new respiratory illnesses in the nursing facility. Unfortunately, new respiratory symptoms in nursing home patients have numerous etiologies, including other respiratory viruses (respiratory syncytial virus, influenza B, rhinovirus), chla‐mydia pneumoniae, bacterial infections, and aspiration events. 4 , 7 We have previously reported respiratory syncytial virus (RSV) activity superimposed on an influenza A outbreak. 4 Individual cases of influenza A could not be distinguished from RSV. The isolation of influenza can provide outbreak confirmation. In addition, cultures obtained from newly symptomatic residents during the final days of a planned course of chemoprophylaxis may suggest earlier termination of prophylaxis if influenza is no longer being isolated. During the seven influenza seasons covered in this report, we performed surveillance with viral cultures. We report the timing and numbers of influenza A isolates as well as overlapping viral respiratory isolates.
METHODS
The Wisconsin Veterans Home is a skilled nursing facility for veterans and their spouses that is administered by the State of Wisconsin. The facility has four residential buildings (A‐D) and an activity building. Between 1991 and 1998, the average daily census was 712, 78.5% of residents were male, average age was 76 ± 10 years, and annual mortality was 17.4%. Beginning in the last week of October, vaccination of residents and staff was encouraged by announcements over the public address system and by memos from the Medical Director and Nursing Supervisors. The decision‐makers for incapacitated residents were asked to give consent for annual influenza vaccinations at the time of admission. Staff vaccination was encouraged to protect residents from a potentially lethal infection as well as to protect staff and their families from a miserable infection. Vaccination was offered to staff during all shifts in all buildings. Subsequently, vaccinations were offered to newly admitted residents and to new employees and reoffered to those who had refused.
During the seven influenza seasons covered in this report (with the exception of 1995‐1996), we conducted controlled studies designed to provide data on antiviral chemoprophy‐laxis. Prospective clinical surveillance with cultures was an integral part of our protocol.
Prospective surveillance began early in December and continued until the end of reported influenza activity in the state. Acute respiratory illness was defined as any new sign or symptom, including cough, sore throat, or runny nose. Nursing staff who provide routine care prepared daily reports of new respiratory symptoms for allresidents. These reports were reviewed by research nurses. Even afebrile residents with minor respiratory symptoms were cultured. A nasopha‐ryngeal and throat swab (two separate swabs) was obtained from all consenting residents by research nurses. Swabs were placed in transport media (veal broth with gentamicin, penicillin, streptomycin, and amphotericin), cooled to 4°C within 1 hour, transported cold (4 to 8°C) to the Wisconsin State Laboratory of Hygiene Virology Laboratory, and inoculated into cell cultures (24‐well plates of Madin Darby Canine Kidney (MDCK) cells; tubes of Primary rhesus Monkey Kidney, Hep‐2 and WI‐38 cells) for isolation of cultivable respiratory viruses within 30 hours of collection. MDCK cultures were incubated stationary at 35CC for 5 days. All tube cultures were incubated on a roller apparatus at 33CC for up to 14 days. Virus identification was performed using routine methods. During the 1995‐1996 season, all viral cultures were collected by clinical staff who performed throat cultures only. Therefore, clinical surveillance and cultures were performed by research staff under an identical protocol during six seasons and by clinical staff during one season. Chemo‐prophylaxis was initiated for all residents on a floor when influenza A had been cultured and 10% of the residents on a floor developed respiratory illness within a 7‐day period.
We report yearly vaccination rates for residents and staff, the number of clinical respiratory illness and cultures, and the timing of viral isolates for our entire four‐building facility. All viral infections cited in the Results section were culture‐confirmed.
RESULTS
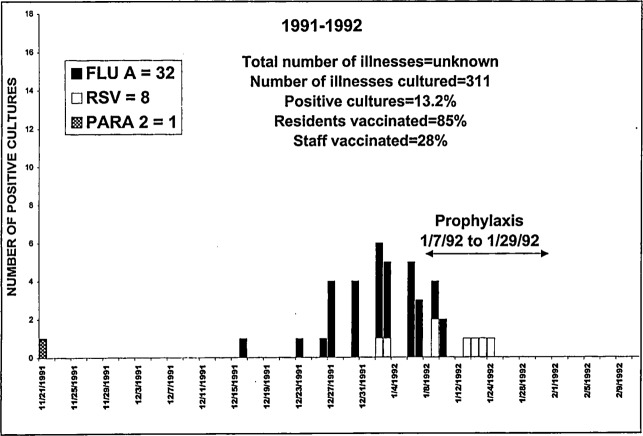
In 1991‐1992, 32 culture‐confirmed influenza A infections occurred over 25 days (Figure 1). “Prophylaxis” in the figures refers to the time period amantadine or rimantadine prophylaxis was administered on any of our 14 Nursing Units. A single parainfluenza 2 infection occurred 25 days earlier. Eight RSV infections overlapped and extended 14 days beyond the influenza period.
Figure 1.
Thirty‐two influenza A infections occurred over 25 days. One parainfluenza 2 infection occurred 25 days earlier. Eight RSV infections overlapped and extended 14 days beyond the influenza period.
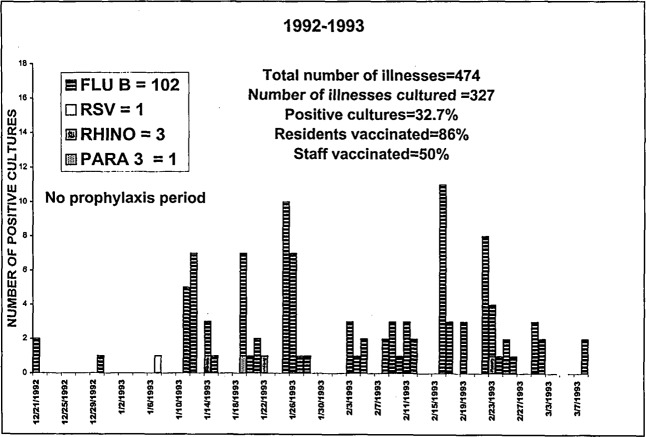
In 1992‐1993, 102 culture‐confirmed influenza B infections occurred over 86 days (Figure 2). In addition, five sporadic infections, including an RSV, a parainfluenza 3, and three rhinovirus infections, overlapped the influenza B period,.
Figure 2.
One hundred two influenza B infections occurred over 86 days, with five overlapping infections: RSV, parainfluenza 3, and three rhinovirus.
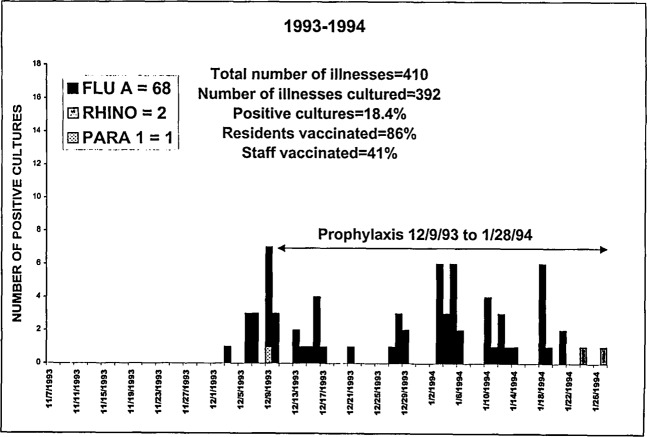
In 1993‐1994, 68 culture‐confirmed influenza A infections occurred over 47 days (Figure 3). Thirteen of 17 isolates from residents with disease onset after 1/08/94 were sent to the CDC for determination of amantadine sensitivity. Ten were resistant (CDC personal communication). There was a single overlapping parainfluenza 1 infection. Finally, two rhinovirus infections occurred in Building A 5 days after the influenza period.
Figure 3.
Sixty‐eight influenza A infections occurred over 47 days. A single overlapping parainfluenza 1 and 2 rhinovirus infections occurred 5 days after the influenza period.
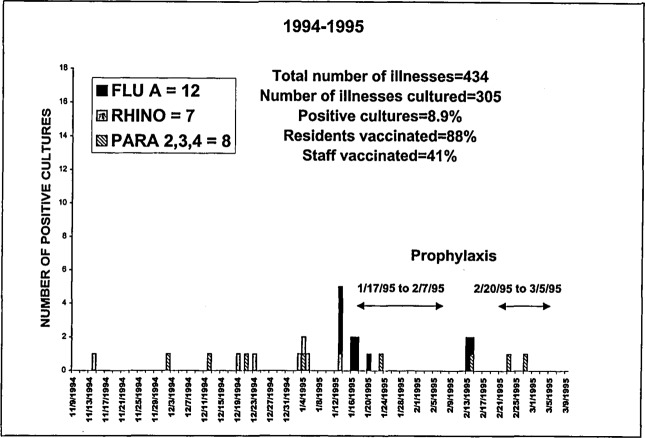
In 1994‐1995, 154 culture‐confirmed influenza A infections occurred over 32 days (Figure 4). There were seven rhinovirus infections, one parainfluenza 4 infection, one parainfluenza 2 infection, and two parainfluenza 3 infections before the influenza period. Four parainfluenza 3 infections overlapped and extended beyond the influenza period.
Figure 4.
Twelve influenza A infections occurred over 32 days. Seven rhinovirus, one parainfluenza 4, one parainfluenza 2, and two parainfluenza 3 infections occurred before the influenza period. Four parainfluenza 3 infections overlapped and extended beyond the influenza period.
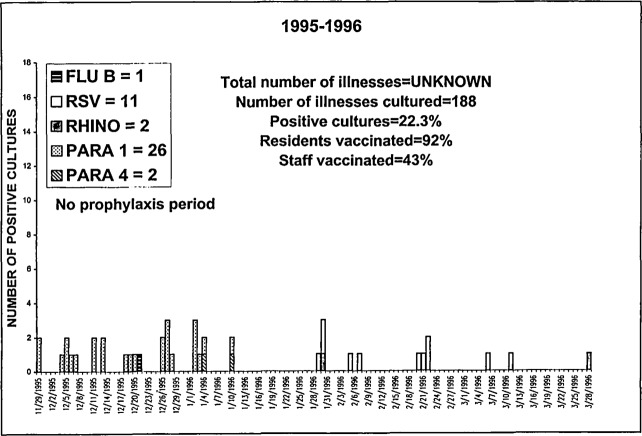
In 1995‐1996, a single culture‐confirmed influenza B infection occurred on 12/21 (Figure 5). There were 26 parainfluenza 1 infections over 43 days, and two parainfluenza 4 infections overlapped the end of the parainfluenza 1 period. This was followed by 11 RSV infections and two rhinovirus infections.
Figure 5.
A single influenza B infection occurred on 12/21. Twenty‐six parainfluenza 1 infections occurred over 43 days. Two parainfluenza 4 infections overlapped the parainfluenza 1 period, followed by 11 RSV and two rhinovirus infections.
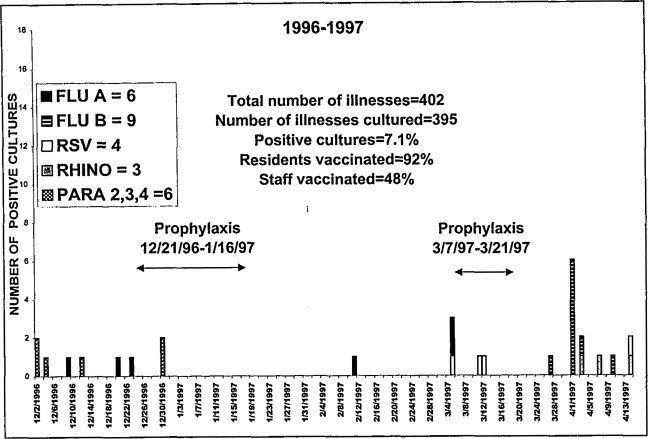
In 1996‐1997, six culture‐confirmed influenza A infections occurred over 86 days, followed by nine influenza B infections over 14 days. All influenza B infections occurred in a single building (Figure 6). There were six parainfluenza infections (3 type 2, 1 type 3, 2 type 4) between 12/02 and 12/30 that overlapped the influenza A period. Finally, four RSV infections and three rhinovirus infections were encountered after the influenza A period overlapping the influenza B period.
Figure 6.
Six influenza A infections occurred over 86 days, followed by nine influenza B infections over 14 days. Six parainfluenza infections (Types 2, 3, and 4) occurring between 12/02 and 12/30 overlapped the influenza A period. Four RSV and three rhinovirus infections overlapped the influenza B period.
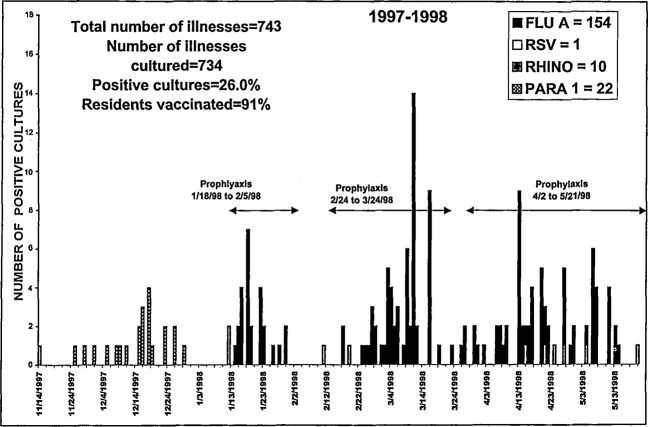
In 1997‐1998, 154 culture‐confirmed influenza A infections occurred over 123 days (Figure 7). Twenty‐two parainfluenza 1 infections were noted before the influenza period. There were 10 rhinovirus infections between 11/14 and 5/04. A single RSV infection overlapped the end of the influenza A period.
Figure 7.
One hundred fifty‐four influenza A infections occurred over 123 days. Twenty‐two parainfluenza 1 infections occurred before the influenza period. Ten rhinovirus infections occurred between 11/14 and 5/04, and a single RSV infection overlapped the influenza A period.
During the 7 years covered in this report, 2652 cultures were performed, and 19.1% of these revealed a viral pathogen, which included 270 influenza A, 112 influenza B, 25 RSV, 50 parainfluenza 1, five parainfluenza 2, eight parainfluenza 3, five parainfluenza 4, and 32 rhinovirus infections.
DISCUSSION
There was striking annual variability in the number of influenza A cases (0–154) and in the duration of activity (25‐123 days). Influenza A isolates were encountered in greater numbers than non‐influenza isolates during three of seven seasons. These three seasons included the largest numbers of influenza A isolates (154, 68, 32). During other seasons, our experience was similar to Nicholson's, who performed prospective surveillance of 515 beds in English homes for the elderly. Individuals with new respiratory symptoms were identified, viral cultures and serological studies were performed, and 41 cases were laboratory‐confirmed, including five with influenza A and 11 with coronavirus, which can only be diagnosed serologically. The proportion of non‐influenza cases in the present study would probably be greater if corona virus serology had been included. The English investigators concluded, “Respiratory symptoms in the study population evidently were caused mostly by pathogens other than influenza during the influenza period documented nationally.” 8 Serie et al. also reported 17 influenza B isolates overlapping the beginning and end of influenza A activity in a large geriatric hospital. 9 When interpreting numbers of new clinical respiratory illnesses as a basis for an outbreak of influenza A, clinicians should realize that co‐circulating respiratory viruses can account for clinical illnesses.
Influenza surveillance should be intensified after a regional surveillance system has identified influenza. However, Arroyo et al. reported a nursing home outbreak that included the first isolates in South Carolina.10 The importance of cultures early in the season was underscored in December, 1995 when 285 cases of influenza A were cultured in the state of Wisconsin, and an outbreak of respiratory illness was encountered in two of our buildings. However, 26 isolates of parainfluenza 1 were cultured with no influenza A. If cultures had not been obtained, antiviral chemoprophylaxis could have been started unnecessarily. Osterweil and Norman reported the use of amantadine prophylaxis for an outbreak that was later serologically proven to be caused by RSV.11 In December 1992, we identified a large outbreak of respiratory illness, but it was caused by influenza B. A need for a precise diagnosis of influenza A and/or B will be more important when antiviral agents with activity against influenza B become available. During the 1996‐1997 season, 22 non‐influenza A cases were identified in the face of six culture‐confirmed influenza A cases. Confusion regarding influenza A activity was possible without cultures. These observations underscore that if chemoprophylaxis is initiated because of a suspected outbreak, continued antiviral chemoprophylaxis should require laboratory confirmation.
Despite our extensive experience, we are not able to predict how a given outbreak will proceed. During our largest outbreak (1997–1998), team members often speculated on future influenza activity. The standard response became “only a fool would predict.” The timing of chemoprophylaxis termination is problematic inasmuch as reliable information on the duration of influenza activity in the community may not be available or germane to what is happening within the facility. In 1997‐1998, the last cases at the Home occurred 1 week afterthe last cases in the rest of the state of Wisconsin. The duration of antiviral prophylaxis should be guided by ongoing surveillance within the facility. The importance of culturing at the end of the influenza season was suggested in 1991‐1992 when we identified significant RSV activity at the end of the outbreak. We could have continued prophylaxis unnecessarily, based on the continued occurrence of clinical respiratory illnesses, had we not had surveillance culturing in place. In addition, the isolation of influenza A from a resident whose respiratory illness began in the second week of chemoprophylaxis (as occurred during the 1993‐1994 season) suggests a resistant strain and might prompt a switch to an alternate antiviral when they become available.12 Timely and accurate information regarding influenza activity within the facility could allow a more focused duration of prophylaxis.
The cost of 7 days of generic amantadine (100 mg qd) is $2.56, whereas a similar dose and duration of rimantadine is $12.23. (Red Book, 1999) A 1997 Medical Letter stated that rimantadine had “gastrointestinal adverse effects similar to those of amantadine, but a lower risk of CNS adverse effects.”13 We, therefore, prefer rimantadine. The cost of 7 days of rimantadine for 200 residents is approximately $2450.00. Our current cost for an influenza culture is approximately $50.00. One week of rimantadine in a 200‐bed facility, therefore, has a cost similar to 40 viral cultures. Our system of intensive surveillance with cultures is unlikely to become the standard of care. Greater economy might include cultures restricted to febrile respiratory illness after influenza A has been cultured by a regional laboratory. If clinical criteria for an outbreak were approached, all residents with respiratory illness of recent onset could be cultured and antiviral prophylaxis initiated pending culture results. Culturing of any new respiratory illnesses could begin again before the anticipated discontinuation of prophylaxis (14 days) to determine if influenza activity was continuing. 14
Clinical recognition of an outbreak of respiratory illness is not difficult. Declaring an outbreak of Influenza A, however, may be difficult because other winter respiratory viruses are capable of producing severe illness (i.e., influenza B, RSV, and parainfluenza 1). Each clinician must assess the relevance of his/her viral culture monitoring system for timeliness and proximity, as well as the proportion of respiratory illnesses culture‐confirmed as influenza A, when initiating antiviral chemoprophylaxis. We do not wish to discourage clinicians from initiating timely, lifesaving chemoprophylaxis. We consider the response to a winter outbreak of respiratory illness to be analogous to the timely response to a severe febrile illness. The clinician should obtain appropriate cultures and simultaneously initiate antimicrobial coverage pending the results of cultures. We recommend that clinicians perform surveillance for new respiratory symptoms, followed by laboratory confirmation, to determine an outbreak's beginning and end, thus enabling them to limit prophylaxis to the shortest effective duration.
Supported by NIH Grants AG 09632 and AG 00548 to Dr. Gravenstein, and by Glaxo‐Wellcomc, Research Triangle Park, South Carolina, to Dr Gravenstein and Dr. Drinka.
REFERENCES
- 1. Advisory Committee on Immunization Practices (ACIP) Prevention and Control of Influenza. Recommendations of the ACIP. MMWR 1998;47:1–26. [PubMed] [Google Scholar]
- 2. Gomolin IH, Leib HB, Arden NH, Sherman FT. Control of influenza outbreaks in the nursing home: Guidelines for diagnosis and management. J Am Geriatr Soc 1995;43:71–74. [DOI] [PubMed] [Google Scholar]
- 3. Barker WH, Borisute H, Cox C. A study of the impact of influenza on the functional status of frail older people. Arch Intern Med 1998;158:645–650. [DOI] [PubMed] [Google Scholar]
- 4. Wald TG, Miler BA, Shult P et al. Can respiratory syncytial virus and influenza A be distinguished clinically in institutionalized older persons? J Am Geriatr Soc 1995;43:170–174. [DOI] [PubMed] [Google Scholar]
- 5. Drinka PJ, Gravenstein S, Krause P et al. Outbreaks of influenza A and B in a highly immunized nursing home population. J Fam Pract 1997;45:509–514. [PubMed] [Google Scholar]
- 6. Wald TG, Shult P, Krause P et al. A rhinovirus outbreak among residents of a long‐term care facility. Ann Intern Med 1995;123:588–593. [DOI] [PubMed] [Google Scholar]
- 7. Troy CJ, Peeling RW, Ellis AG et al. Chlamydia pneumoniaeas a new source of infectious outbreaks in nursing homes. JAMA 1997;277:1214–1218. [PubMed] [Google Scholar]
- 8. Nicholson KG, Baker DJ, Farquhar A et al. Acute upper respiratory tract viral illness and influenza immunization in homes for the elderly. Epidemiol Infect 1990;105:609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Serie C, Barme M, Hannoun C et al. Effects of vaccination on an influenza epidemic in a geriatric hospital. Dev Biol Stand 1977;39:317–321. [PubMed] [Google Scholar]
- 10. Arroyo JC, Postic, Brown H et al. Influenza A/Philippines/2/82 outbreak in a nursing home. Limitations of influenza vaccination in the aged. Am J Infect Control 1984;12:329–334. [DOI] [PubMed] [Google Scholar]
- 11. Osterweil D, Norman D. An outbereak of an influenza‐like illness in a nursing home. J Am Geriatr Soc 1990;38:659–662. [DOI] [PubMed] [Google Scholar]
- 12. Hayden FG, Osterhaus AD, Treanor JJ et al. Efficacy and safety of the neur‐aminidase inhibitor Zanamivir in the tratment of nifluenza virus infections. N Engl J Med 1997;337:874–880. [DOI] [PubMed] [Google Scholar]
- 13. Drugs for non‐HIV infections. Med Lett Drugs Ther 1997;39:69–76. [PubMed] [Google Scholar]
- 14. Drinka PJ, Gravenstein S, Krause P et al. Duration of influenza A chemoprophylaxis: A comparison of 2 protocols. Arch Intern Med 1998;158:2155–2159. [DOI] [PubMed] [Google Scholar]