Abstract
An entire, female, mixed‐breed cat of unknown age was presented with a 6‐week history of lethargy, anorexia and vomiting. There was an increase in the number of white blood cells in the blood, including neutrophils and eosinophils; moderate anaemia; ascites; and possible mesenteric peritonitis. Exploratory laparotomy revealed firm, multifocal small nodules in the mesentery. As the nodules were surgically unresectable, they were biopsied. Histologically, the nodules were composed of thin trabeculae of dense collagen fibres mixed with plump fibroblasts and numerous eosinophils, consistent with feline gastrointestinal eosinophilic sclerosing fibroplasia. Bacteria were not detected on histological examination of the nodules and cytology of the ascites. Remission of disease occurred following treatment with prednisolone and ciclosporin A for 22 days and antibiotics for 40 days. After remission, ciclosporin A was administered for 236 days and then discontinued. Eosinophilia also resolved after treatment with ciclosporin A. The cat is still alive and in good condition on day 689. This report describes what may be an atypical case of feline gastrointestinal eosinophilic sclerosing fibroplasia, lacking involvement of the gastrointestinal tract, and was apparently cured by treatment that involved ciclosporin A.
INTRODUCTION
Eosinophils are able to induce unique inflammatory diseases in cats, including eosinophilic plaque, eosinophilic granuloma, feline indolent ulcer and hypereosinophilic syndrome. Feline gastrointestinal eosinophilic sclerosing fibroplasia (FGESF) is a newly recognised eosinophilic inflammatory disease in cats and is characterised by a firm palpable abdominal mass of the gastrointestinal tract and associated lymph nodes (Craig et al. 2009, Linton et al. 2015). Histological features of the mass lesions include dense collagen trabeculae, large fibroblasts and numerous eosinophils (Craig et al. 2009). Intralesional bacteria were detected in more than 50% of cats with FGESF (Craig et al. 2009, Weissman et al. 2013, Linton et al. 2015) and FGESF‐like lesions (Ozaki et al. 2003). Intralesional fungi were also reported in a cat with FGESF (Grau‐Roma et al. 2014). However, the role of bacterial or fungal infection in the development of FGESF remains to be determined. It has been thought that immunological dysregulation by an unknown cause may be implicated in the pathogenesis of FGESF (Linton et al. 2015). Prednisolone was shown to prolong the survival time of cats with FGESF (Craig et al. 2009). Based on these features of FGESF, the suggested treatment is multimodal – consisting of prednisolone, immunomodulatory agents and antibiotics after surgical resection of the mass (Linton et al. 2015). However, the efficacy of the therapy has not been reported in cats with FGESF.
Here, we report a case of surgically unresectable FGESF‐like multifocal small nodules in the mesentery. Treatment with prednisolone, ciclosporin A and antibiotics was associated with remission, and ciclosporin A alone appeared to be effective for long‐term management. The present report describes what may be an atypical case of FGESF and a treatment option for this disease.
CASE HISTORY
An entire, female, mixed‐breed cat of unknown age (presumed to be more than 9 years old), weighing 2·6 kg, was presented with a 6‐week history of lethargy, anorexia and vomiting (day 1). The cat had a history of lung abscess that was not completely resected by surgery approximately 2 years before the current presentation. Physical examination revealed mildly pale mucous membranes and abdominal distension. A complete blood count (CBC) exhibited an increase in the number of white blood cells (WBCs) of 33·1 × 109 cells/L (reference interval, 5·5 to 19·5 × 109 cells/L), neutrophils of 27·1 × 109 cells/L (2·5 to 12·5 × 109 cells/L) and eosinophils of 3·3 × 109 cells/L (0 to 1·5 × 109 cells/L) and moderate anaemia with red blood cells of 4·7 × 1012/L (5·0 to 10·0 × 1012/L), haemoglobin of 70 g/L (80 to 150 g/L) and packed cell volume (PCV) of 19·4% (24·0 to 45·0%). Serum biochemical analysis detected an increase in the level of total protein (TP) of 92 g/L (57 to 78 g/L). Thoracic radiography revealed pulmonary mineralisation associated with the previous lung abscess in the right middle and caudal lobes. Abdominal radiography demonstrated reduced contrast. An abdominal ultrasound illustrated mild ascites and hyperechoic mesentery, suggesting mesenteric peritonitis. CT also demonstrated mild ascites. Radiography, ultrasonography and CT did not detect any abdominal masses. Inspection of ascitic fluid revealed a specific gravity of 1·038 and TP of 56 g/L, indicating an exudate. The cytology of the ascites demonstrated inflammatory cells, including neutrophils, lymphocytes and eosinophils. Bacteria and fungi were not detected in the ascitic fluid using light microscopy. The antibody titre for feline coronavirus in the sera (IDEXX Laboratories, Inc.) and the real‐time PCR analysis for the feline infectious peritonitis (FIP) virus in the ascites (IDEXX Laboratories, Inc.) were negative, ruling out FIP infection.
To determine the cause of anaemia, ascites and possible mesenteric peritonitis, an exploratory laparotomy was performed after a cross‐matched fresh whole blood transfusion (40 mL) on day 9. At laparotomy, multifocal small nodules were found in the mesentery (Fig 1A). The nodules were very firm. Gross inspection and palpation did not find any other lesions, including masses or lymphadenopathy. As it was impossible to surgically resect the multiple small nodules in the mesentery, excisional biopsies of a few nodules were performed for histological analysis (Fig 1B).
Figure 1.
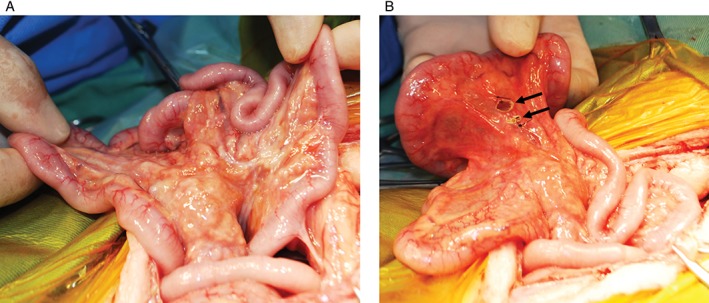
Gross findings at exploratory laparotomy. (A) Multifocal small nodules were found in the mesentery. (B) Excisional biopsies of a few nodules (the solid arrows indicate biopsy sites)
Histologically, the mesenteric nodular foci were composed of thin trabeculae of dense collagen fibres separated by densely cellular plump fibroblasts (Figs 2 and 3). The lesions contained numerous eosinophils and fewer lymphocytes, plasma cells and histiocytes (Fig 3). These histological characteristics were consistent with FGESF (Craig et al. 2009). No microbes were detected in the nodules.
Figure 2.
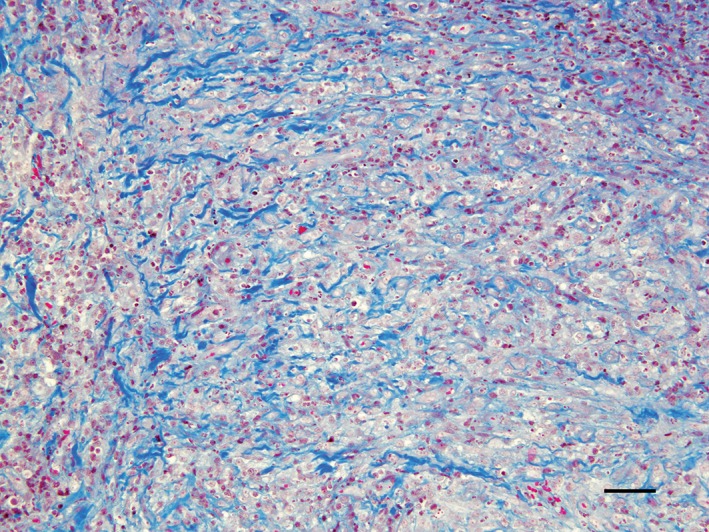
Photomicrograph of the mesenteric nodules. The foci were composed of thin trabeculae of dense collagen fibres, which were stained blue. Masson's trichrome stain; bar=50 μm
Figure 3.
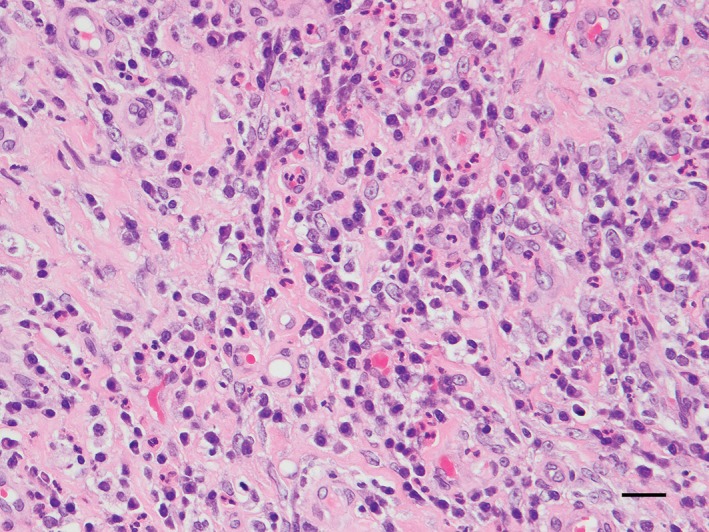
Photomicrograph of the mesenteric nodules. The foci were composed of thin trabeculae of dense collagen fibres mixed with fibroblasts, numerous eosinophils and fewer lymphocytes, plasma cells and histiocytes. Haematoxylin and eosin stain, bar=20 μm
Because bacterial infection was not investigated by culture, PCR or fluorescence in situ hybridisation (FISH), bacteria might have been implicated in the development of FGESF‐like lesions in the cat. Therefore, the cat was subcutaneously (sc) injected with 5 mg/kg enrofloxacin (Baytril®; Bayer) once daily on days 8, 9 and 10 and intravenously (iv) injected with 30 mg/kg ampicillin sodium (Ampicillin Na KS; Kyoritsu Seiyaku) twice daily on day 9. After the cat was discharged on day 11, it was sc injected with 8 mg/kg cefovecin sodium (Convenia®; Zoetis Japan) on days 11, 23 and 47.
Based on the histological diagnosis, oral administration of 1 mg/kg prednisolone (Prednisolone; Pfizer) every 24 hours and 7 mg/kg ciclosporin A (Atopica™; Kyoritsu Seiyaku) every 24 hours was initiated on day 23. After initiation of treatment with prednisolone and ciclosporin A, lethargy, anorexia and vomiting improved, and ascites diminished. Prednisolone was discontinued on day 44 due to the difficulty of oral administration. Ciclosporin A was administered without concurrent medicine until day 280, and it was then discontinued at the owner's request. The cat was in good condition during treatment with ciclosporin A and remained in good condition after discontinuation. A CBC examined on day 469 revealed that the numbers of WBCs (15·9 × 109 cells/L) and eosinophils (0·7 × 109 cells/L) had returned to within the reference intervals, although the number of neutrophils (14·3 × 109 cells/L) was slightly above the upper reference boundary. The moderate anaemia found on day 1 was improved, with RBCs of 10·0 × 1012/L, haemoglobin of 115 g/L and PCV of 32·5%. The serum level of TP remained elevated (105 g/L). The cat remained in good condition at the time of submission of this report (day 689).
DISCUSSION
A palpable abdominal mass is a clinical feature of FGESF and has been detected in a substantial proportion of cats with FGESF, but not in all (Craig et al. 2009, Linton et al. 2015). The cat in this case report did not have an abdominal mass but had firm multifocal small nodules in the mesentery. Histological findings were consistent with FGESF. The cat also displayed weight loss, chronic vomiting and peripheral eosinophilia, which are typical historical and haematological abnormalities observed in cats with FGESF (Craig et al. 2009, Linton et al. 2015). These findings suggest that the cat in the present report may have had an atypical type of FGESF.
In addition to prednisolone, the concurrent use of immunomodulatory drugs, including ciclosporin A, has been suggested as treatment for FGESF (Linton et al. 2015). Ciclosporin A suppresses eosinophil‐mediated inflammatory responses such as degranulation, cytokine secretion and recruitment to sites of inflammation (Kovalik et al. 2012). However, the efficacy of ciclosporin A on FGESF has never been reported. The cat in this report received ciclosporin A and prednisolone for 22 days and then received ciclosporin A without any other medications for 236 days. Clinical signs were improved after initiation of prednisolone and ciclosporin A, and good condition was maintained during and after treatment with ciclosporin A. Furthermore, the number of eosinophils in the peripheral blood returned to within the reference interval after treatment with ciclosporin A. These results suggest that the concurrent use of prednisolone and ciclosporin A induced remission, and subsequent administration of ciclosporin A without any medication was effective for the long‐term remission of clinical signs associated with FGESF‐like lesions in the cat. However, marked hyperproteinaemia was still demonstrated after the end of treatment (day 469), suggesting that an underlying predisposition to this disease persisted.
In previous studies, bacteria were isolated from abdominal lesions in more than 50% of cats with FGESF (Craig et al. 2009, Linton et al. 2015), although it is unclear how bacteria contributed to the development of the disease. In this report, bacteria were not detected on histological examination of the nodules and cytology of the ascites. However, bacterial infection was not determined by culture, eubacterial PCR or FISH using eubacterial primers. In addition, several antibiotics were injected during and after the laparotomy. Therefore, we cannot rule out the possibility that bacteria might also have contributed to the lesions in this individual.
In conclusion, the current case report may represent an atypical type of FGESF, and it appears that multimodal therapy, consisting of prednisolone, ciclosporin A and antibiotics, was effective for surgically unresectable FGESF‐like lesions.
Conflict of interest
None of the authors of this article has a financial or personal relationship with other people or organisations that could inappropriately influence or bias the content of the paper.
References
- Craig, L. E. , Hardam, E. E. , Hertzke, D. M. , et al (2009) Feline gastrointestinal eosinophilic sclerosing fibroplasia. Veterinary Pathology 46, 63‐70 [DOI] [PubMed] [Google Scholar]
- Grau‐Roma, L. , Galindo‐Cardiel, I. , Isidoro‐Ayza, M. , et al (2014) A case of feline gastrointestinal eosinophilic sclerosing fibroplasia associated with phycomycetes. Journal of Comparative Pathology 151, 318‐321 [DOI] [PubMed] [Google Scholar]
- Kovalik, M. , Thoday, K. L. & van den Broek, A. H. (2012) The use of ciclosporin A in veterinary dermatology. The Veterinary Journal 193, 317‐325 [DOI] [PubMed] [Google Scholar]
- Linton, M. , Nimmo, J. S. , Norris, J. M. , et al (2015) Feline gastrointestinal eosinophilic sclerosing fibroplasia: 13 cases and review of an emerging clinical entity. Journal of Feline Medicine and Surgery 17, 392‐404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozaki, K. , Yamagami, T. , Nomura, K. , et al (2003) Abscess‐forming inflammatory granulation tissue with Gram‐positive cocci and prominent eosinophil infiltration in cats: possible infection of methicillin‐resistant Staphylococcus. Veterinary Pathology 40, 283‐287 [DOI] [PubMed] [Google Scholar]
- Weissman, A. , Penninck, D. , Webster, C. , et al (2013) Ultrasonographic and clinicopathological features of feline gastrointestinal eosinophilic sclerosing fibroplasia in four cats. Journal of Feline Medicine and Surgery 15, 148‐154 [DOI] [PMC free article] [PubMed] [Google Scholar]


