Abstract
During the past decade, substantial progress has been made in the field of the genetics of myelodysplastic syndromes (MDS). These comprise a group of chronic myeloid neoplasms with abnormal cell morphology and progression to acute myeloid leukemia (AML), where revolutionary sequencing technologies have played a major role. Through extensive sequencing of a large number of MDS genomes, a comprehensive registry of driver mutations involved in the pathogenesis of MDS has been revealed, along with their impacts on clinical phenotype and prognosis. The most frequently affected molecules are involved in DNA methylations, chromatin modification, RNA splicing, transcription, signal transduction, cohesin regulation, and DNA repair. These mutations show strong positive and negative correlations with each other, suggesting the presence of functional interactions between mutations, which dictate disease progression. Because these mutations are associated with disease phenotype, drug response, and clinical outcomes, it is essential to be familiar with MDS genetics not only for better understanding of MDS pathogenesis but also for management of patients.
Keywords: myelodysplastic syndromes (MDS), splicing factors, cohesin, secondary acute myeloid leukemia (sAML), next-generation sequencing
Introduction
Myelodysplastic syndromes (MDS) are a heterogeneous group of chronic myeloid neoplasms, which are characterized by refractory cytopenia with abnormal bone marrow (BM) morphology and frequent progression to acute myeloid leukemia (AML) (secondary AML [sAML]).1,2) Although AML progression, which is found in one-third of these patients, is a strong predictor of poor outcomes, many of the remaining patients also die from BM failure, which leads to fatal bleeding and infection.3) Recently, several new drugs, such as lenalidomide4) and hypomethylating agents,5) have been introduced into clinics, contributing improved outcomes for a subset of MDS patients. However, no curative therapy is available for MDS patients, except for allogeneic hematopoietic stem cell transplantation, which unfortunately is applicable only to younger patients, even though the vast majority of patients are elderly and not eligible to transplantation. Thus, there is an urgent need to understand the molecular pathogenesis of MDS to develop effective but less toxic therapies.
Little was known about relevant gene mutations that are implicated in MDS pathogenesis until early 2000s. This was in contrast to AML, whose molecular pathogenesis was intensively studied during the 1990s through the analysis of highly recurrent chromosomal translocations. In fact, only a handful of genes, including NRAS, TP53, ATRX, and RUNX1, were known to be mutated in MDS.6–10) The first breakthrough was brought about by the development of single nucleotide polymorphism (SNP) array-based genomic copy number analysis (or SNP array karyotyping), using millions of SNP probes, which enabled the comprehensive detection of genomic copy number abnormalities (CNAs) at an unprecedented resolution (∼several kilobase pairs) across the entire cancer genome.11,12) Thus, using SNP-array karyotyping, we and other groups identified a number of recurrent deletions, amplifications, and other allelic imbalances, such as copy neutral loss-of-heterozygosity (LOH) or uniparental disomies (UPDs),13) from which novel mutational/functional target genes were identified, including TET2,14,15) CBL,16) EZH2,17,18) CUX1,19) and ASXL1,20) which are targeted by common copy number lesions in 4q (UPD/deletion), 11q (UPD), 7q (UPD/deletion), and 20q (deletion), respectively. Other gene targets of common CNAs include NRAS and cMPL (1pUPD), FLT3 (13qUPD), TP53 (17qUPD/deletion), and RUNX1 (21qUPD/deletion).16)
It was not until the revolution in sequencing technologies were introduced into the genetic analysis of cancer that the entire picture of genetic alterations in MDS have been revealed and confirmed in large cohorts of MDS patients; followed by the first report of sequencing of an entire AML genome in 2008.21) Next-generation sequencing has been used for analyses of major human cancers, including MDS, to unveil the complete landscape of mutations and other genetic lesions.22,23) The power of this technology is highlighted by the discovery of mutations in DNMT3A and IDH1 on the basis of whole genome sequencing of an index AML case, which turned out to be among major mutations not only in AML but also in MDS.24,25)
Identification of splicing factor mutations in MDS using whole exome sequencing
To investigate novel mutational targets in MDS in an unbiased manner, we performed whole exome sequencing analysis of paired tumor/normal DNA from 29 cases with MDS and related myeloid neoplasms, including chronic myelomonocytic leukemia and sAML. On average, we identified 265 mutations (9 somatic mutations/sample).26) Most of the mutated genes were affected in a single sample, except for 13 genes shown in Table 1 (in bold), which were recurrently mutated in multiple samples, suggesting their role in MDS pathogenesis. Although 8 of these genes were well-known mutational targets in MDS, the remaining 4 were not reported previously, of which three genes (U2AF1(U2AF35), SRSF2, and ZRSR2) encode RNA splicing factors (SFs). Notably, also including an additional three genes (SF3A1, SF3B1, and PRPF40B), 16 out of 29 MDS cases analyzed had a mutated SF, suggesting that deregulated RNA splicing plays a central role in MDS pathogenesis.
Table 1.
Genes mutated in multiple samples
| Gene | Type | Chr | Mutation | A.A | Sample ID |
|---|---|---|---|---|---|
| ASXL1 | Nonsense | Chr20 | C > A | S852X | MDS-19 |
| ASXL1 | Nonsense | Chr20 | C > T | R693X | CMML-01 |
| BCOR | Frameshift | ChrX | */+C | V1351fs | MDS-19 |
| BCOR | Nonsense | ChrX | C > T | Q1187X | CMML-02 |
| DNMT3A | Missense | Chr2 | G > T | G543C | MDS-19 |
| DNMT3A | Missense | Chr2 | G > A | R882H | CMML-02 |
| EZH2 | Missense | Chr7 | A > C | D664A | tAML-01 |
| EZH2 | Frameshift | Chr7 | */−AA | K718fs | CMML-01 |
| KRAS | Missense | Chr12 | G > A | G12D | tAML-06 |
| KRAS | Missense | Chr12 | A > G | K5E | CMML-01 |
| NRAS | Missense | Chr1 | G > A | G13D | MDS-19 |
| NRAS | Missense | Chr1 | G > A | G13D | MDS-20 |
| NRAS | Missense | Chr1 | G > A | G12S | MDS-20 |
| NRAS | Missense | Chr1 | G > A | G12S | tAML-05 |
| RUNX1 | Frameshift | Chr21 | */+G | L294fs | MDS-19 |
| RUNX1 | Missense | Chr21 | G > A | D171N | tAML-02 |
| SRSF2 | Missense | Chr17 | C > T | P95L | MDS-09 |
| SRSF2 | Missense | Chr17 | C > A | P95H | MDS-18 |
| SRSF2 | Missense | Chr17 | C > A | P95H | CMML-04 |
| SRSF2 | Deletion | Chr17 | — | P95HR103>R | tAML-07 |
| STAG2 | Nonsense | ChrX | C > T | R1012X | MDS-12 |
| STAG2 | Splice site | ChrX | G > A | Q399_spl | MDS-19 |
| TET2 | Frameshift | Chr4 | */−C | I340fs | MDS-06 |
| TET2 | Frameshift | Chr4 | */+C | Y1255Fs | MDS-16 |
| TET2 | Nonsense | Chr4 | C > T | Q323X | MDS-16 |
| TET2 | Nonsense | Chr4 | C > G | S825X | MDS-19 |
| TET2 | Frameshift | Chr4 | */+A | L1046fs | MDS-19 |
| TET2 | Nonsense | Chr4 | C > T | R550X | tAML-01 |
| TET2 | Frameshift | Chr4 | */−C | H994fs | tAML-01 |
| TET2 | Nonsense | Chr4 | C > T | Q1680X | tAML-07 |
| TET2 | Frameshift | Chr4 | */+A | S402Fs | tAML-07 |
| TET2 | Frameshift | Chr4 | */−AAAT | Q749fs | CMML-01 |
| TP53 | Missense | Chr17 | C > T | R116W | MDS-09 |
| TP53 | Frameshift | Chr17 | */−T | M1fs | tAML-03 |
| U2AF1 | Missense | Chr21 | A > G | Q157R | MDS-03 |
| U2AF1 | Missense | Chr21 | C > T | A26V | MDS-12 |
| U2AF1 | Missense | Chr21 | A > C | Q157P | MDS-15 |
| U2AF1 | Missense | Chr21 | A > G | Q157R | CMML-01 |
| U2AF1 | Missense | Chr21 | C > T | S34F | CMML-02 |
| ZRSR2 | Splice site | ChrX | G > A | K257splice | MDS-06 |
| ZRSR2 | Frameshift | ChrX | */−G | G323fs | MDS-08 |
| ZRSR2 | Nonsense | ChrX | G > T | E362X | MDS-16 |
| ZRSR2 | Missense | ChrX | A > T | N261Y | tAML-05 |
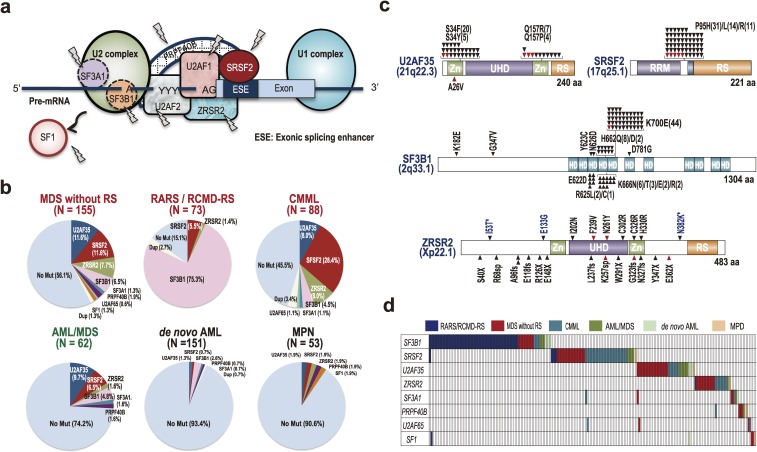
RNA splicing is a basic cellular apparatus ubiquitously found in all eukaryotes, which generates a wide variety of different splicing forms, enabling high-degrees of protein species expressed in eukaryotic organisms.27) The process begins with recognition of exon/intron boundaries, which is accomplished by U1 or U2 snRNP complex, followed by two trans-ester reactions and excision of the intronic sequence as a lariat structure. Of interest, except for PRPF40B, whose function is not well-established, all SFs mutated in 29 cases are included in the U2 RNP complex and involved in one of the initial steps of mRNA splicing, i.e., 5′ splice site recognition (Fig. 1a). To confirm these initial results from whole exome sequencing in the 29 cases, we performed extended mutation analysis in a large cohort of 582 cases with a wide variety of myeloid neoplasms, including not only different subtypes of MDS and sAML, but also de novo AML as well as classical myeloproliferative neoplasms, focusing on SFs involved in 5′ splice site recognition. Through this large-scale analysis, we confirmed that SF mutations were found in all subtypes of MDS, such as refractory anemia (RA), RA with excess blasts (RAEB), refractory cytopenia with multilineage dysplasia (RCMD) as well as RA with ringed sideroblasts (RARS) and refractory cytopenia with multilineage dysplasia and ringed sideroblasts (RCMD-RS), and also chronic myelomonocytic leukemia (CMML) at very high frequencies ranging from 45% to 85%, depending on subtype (Fig. 1b). Conspicuously, in two unique subtypes, RARS and RCMD-RS, which were characterized by elevated numbers of ring-sideroblasts (also known as sideroblastic anemia), >70% of the patients had SF3B1 mutations, making these mutations almost pathognomonic to these MDS subtypes, which was also confirmed in other studies.28,29) Moreover, SF mutations were also found in other myeloid neoplasms, including de novo and secondary AML as well as classical myeloproliferative neoplasm (MPN) cases, although mutation frequencies were largely <10%, except in sAML progressed from MDS, where an intermediate mutation frequency (∼25%) was observed. These findings strongly suggest that SF mutations are cardinal features of MDS and to a lesser extent, other myeloid neoplasms.30)
Figure 1.
Splicing factor mutations in MDS and related neoplasms. a. SFs involved in the recognition of 3′ (U1 complex) and 5′ (U2 complex) splice sites. SFs mutated in MDS and other myeloid malignancies are shown as arrows. b. Frequency of SF mutations in different subtypes of MDS and other myeloid neoplasms. c. Distribution of mutations in major SFs. Red arrowheads indicate confirmed somatic mutations. Zn: Zinc finger domain, RS: arginine/serine rich domain. d. Mutually exclusive pattern of mutations in myeloid neoplasms, in which samples are shown in horizontal columns. Cited from Yoshida et al., Nature, 2011.26)
SF mutations were found in at least 8 SFs, of which by far the most frequently affected were SF3B1, SRSF2, U2AF1, and ZRSR2.26) Among these, mutations in SF3B1, SRSF2, and U2AF1 showed prominent mutational hotspots (Fig. 1c); in SRSF2 most mutations affected the P95 residue between two functional domains, whereas mutations in U2AF1 exclusively affected two highly conserved amino-acids within Zinc-finger domains flanking the RNA binding domain (S34 and Q157).26,31,32) In addition, in SF3B1 nearly half of the mutations affected K700 and surrounding amino-acids.26) The presence of these prominent mutational hot spots strongly suggested that these cause neomorphic or gain-of-function mutations. By contrast, mutations in ZRSR2 were distributed along the entire protein, most of which resulted in a premature truncation, and thus were thought to cause loss-of-function. Additional important features of SF mutations in MDS and other myeloid neoplasms are that these mutations occurred in a mutually exclusive manner and that except for ZRSR2 mutations, all SF mutations were heterozygous with no homozygous mutations (Fig. 1d).26) These features suggest that multiple or homozygous SF mutations were lethal and not compatible with cell viability and positive selection of cells having SF mutations in such a manner.
Functional consequence of SF mutations
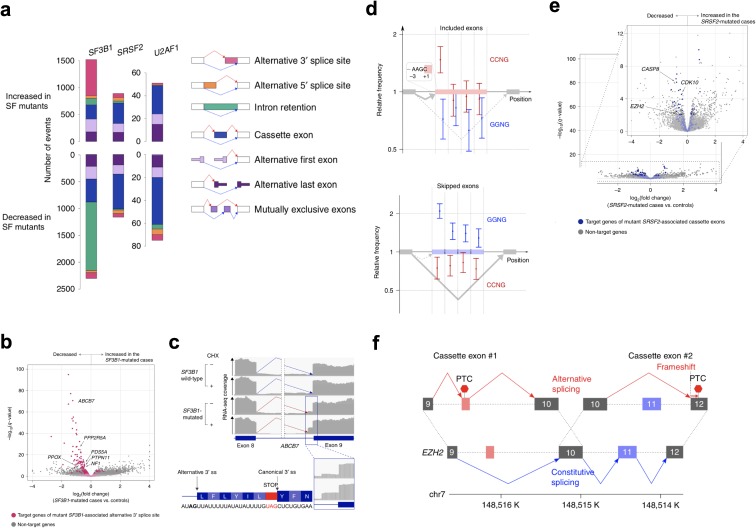
Several studies, including ours, addressed the effects of SF mutations on RNA splicing33–41) and biological phenotypes.36,38,42–45) To investigate the effects of SF mutations on RNA splicing, we performed RNA sequencing of CD34+ cells from a total of 100 MDS patients, including 32 cases with SF3B1 mutations and 23 with SRSF2 mutations. RNA from whole BM cells were also sequenced for 165 patients, which consisted of 54 SF3B1-mutated and 32 SRSF2-mutated, and 14 U2AF1-mutated cases.34,40) As expected, SF-mutated samples showed extensive changes in splicing compared with samples without any SF mutations (n = 41 for CD34+ cells and n = 66 for whole BM cells) (Fig. 2a). However, the patterns of splicing changes differed substantially depending on the mutated SF. For example, SF3B1-mutated samples showed significantly increased alternative 3′ splice sites, which were 5′ upstream of a canonical branch point, suggesting that they were caused by the recognition of an alternative 5′ branch point by the mutated SF3B1.34,40) SF3B1-mutated samples also exhibited a dramatically reduced number of retained introns (Fig. 2a).34,40) Of note many of these alternative splicing forms in SF3B1-mutated samples cause nonsense-mediated decay, leading to significantly reduced gene expression (Fig. 2b). A notable example is 3′ alternative splicing in ABCB7 encoding an iron transporter in mitochondria, haploinsufficiency of which is responsible for congenital sideroblastic anemia (Fig. 2c).34,40,46) By contrast, mutations in SRSF2, which binds to exonic splicing enhancer (ESEs) via consensus sequences (SSNG) and is implicated in the regulation of splicing efficiency, were associated with enhanced or suppressed cassette (or alternative) exons, where alternative exons containing the CCNG consensus have higher affinity to mutant SRSF2 tended to be more frequently included, whereas those carrying the consensus with less affinity were more often excluded (Fig. 2d).36,40) Splicing changes in U2AF1-mutated samples were dominated by alterations in cassette exons as seen in SRSF2-mutated samples. In contrast to a 3′ alternative splice site, alternative cassette exons seen in SRSF2 or U2AF1 mutants were less likely to influence gene expression. Nevertheless, some genes with mutant SRSF2- or U2AF1-associated alternative splicing resulted in reduced gene expression (Fig. 2e). An example is EZH2, a catalytic component of PRC2 frequently mutated in MDS, whose alternative exons in introns 10 and 11 are more frequently included or excluded caused a premature termination in SRSF2-mutated cells, of which the cassette exon in intron 10 is also included in the U2AF1 S34F mutants (Fig. 2f). Alternative splicing affecting EZH2 provides an example in which different SF mutants affected splicing of a common target, which was rarely seen despite large numbers of gene targets of SF mutant-associated alternative splicing. However, in general there were a few genes commonly mutated in MDS whose alternative splicing was caused by different SF mutants.
Figure 2.
(Color online) Abnormal splicing in SF-mutated cells. a. Types and numbers of splicing alterations significantly associated with each SF mutation. Bars in the upper half indicate alternative splicing events that were more frequently found in SF-mutated cases. Bars in the lower half are those that were more frequently found in the controls. Types of alternative splicing events are shown on the right, where cassette exon means inclusion or skipping of an exon. b, e. Volcano plots comparing expression levels of authentic transcripts between the (b) SF3B1- and (e) SRSF2-mutated CD34+ cells and those without known SF mutations. The number of samples in each group is shown in Fig. 1c. X-axis indicates fold changes in gene expression on a log 2 scale. Y-axis indicates q-values on a negative log10 scale. Target genes of mutant SF3B1-associated alternative 3′ splice sites are depicted in red (b). Those of mutant SRSF2-associated cassette exons are depicted in blue (e). c. Increased 3′ alternative splice site (3′ss) at exon 8/9 junction in ABCB7 in SF3B1-mutated cells compared with SF3B1-wild type cells, which becomes prominent by cyclohexamide (CHX) treatment. d. Forest plots show relative frequencies of CCNG and GGNG motifs within the differentially spliced exons in the SRSF2-mutated samples. Two panels show the exons that are more frequently included (n = 380) (top) and skipped (n = 645) (bottom) in SRSF2-mutated samples, respectively. Comparisons were made between the differentially spliced exons and constitutive ones (n = 72,002). Red and blue dots indicate relative frequencies of CCNG and GGNG, respectively. Bars indicate 95% confidence intervals. Relative frequencies are shown for exons divided into four segments with equal lengths. f. Two cassette exons in EZH2-associated with SRSF2 mutation. The left is alternative exon usage and the right is exon skipping. Gray boxes indicate constitutive exons. Red and blue boxes denote exons with increased and decreased usage in SRSF2-mutated samples, respectively. Cited from Shiozawa et al., Nature Communications, 2018.40)
We and other groups also investigated the biological consequences of mutant SFs using an engineered mouse model with conditional mutant SF alleles. However, even though targets of abnormal splicing of SF mutations overlapped with known mutational targets, the molecular pathogenesis of mutated SFs has not fully been elucidated. Indeed all these mouse models showed abnormal splicing of expected patterns, as seen in human samples, and developed dysplastic cell morphology as well as reduced production of mature blood cells. However, BM cells from these mice did not show any evidence of clonal advantage in competitive repopulation analysis; when equivalent numbers of BM cells from mutant and wild-type mice were transplanted into lethally irradiated recipients. When chimerism between wild-type and mutant SFs was evaluated, mutant cells unexpectedly showed a reduced rather than elevated chimerism, suggesting that SF-mutant BM cells have compromised repopulation capacity. One of the explanations might be an altered BM microenvironment favoring SF-mutant cells. Future studies are clearly warranted to clarify the exact mechanism of positive selection of SF-mutant cells in MDS patients.
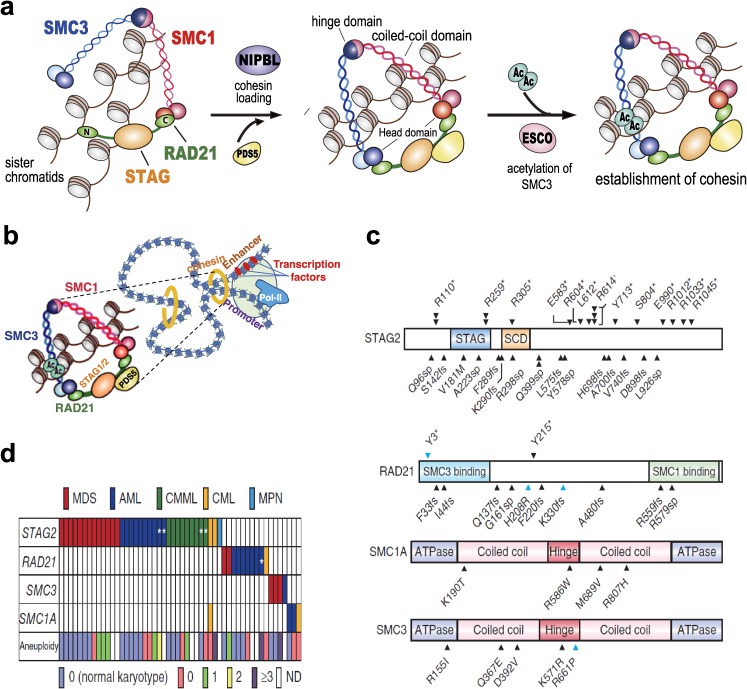
Cohesin mutations
An additional mutational targets mutated in MDS more frequently than expected only by chance (i.e. driver genes) were identified through exome sequencing of an extended cohort. Cohesin is a multimeric protein complex comprising RAD21, SMC1, SMC3, and a STAG protein (STAG1-3) (Fig. 3a).47) Taking a ring-like structure, these molecules are recruited on chromatin in concert with cohesin-associated molecules, such as NIPBL and ESCO proteins, to prevent sister chromatids from premature separation during cell division. However, these also participate in post-replicative DNA repair and long-range regulation of gene expression through the formation of large-scale chromatin structures (Fig. 3b).48,49) In MDS and other myeloid malignancies, approximately 10–15% of cases harbor mutations in cohesin and related molecules.50,51) Among these cohesin components, STAG2 was most frequently mutated, in which most mutations were truncating, leading to loss-of-function, and so were RAD21 mutations (Fig. 3c). As is the case with SF mutations, cohesin mutations are largely mutually exclusive (Fig. 3d), suggesting synthetic lethality of mutations in multiple cohesin components. Cohesin mutations were also reported in several solid tumors, including glioblastoma, melanoma, Ewing sarcoma, and colon cancers, where aneuploidy caused by loss of cohesin functions has been implicated in tumorigenesis.52) However, in myeloid malignancies, many of cohesin-mutated tumors had normal or near normal karyotypes (Fig. 3d), arguing against the role of aneuploid but supporting altered gene regulation as the mechanism of cohesin-mutated myeloid neoplasms. Recent studies showed that cohesin-deficient cells had altered chromatin structures that allowed for accessibility to a number of transcription factors, including RUNX1, GATA2, and ERG, suggesting functional interactions of cohesin mutations and these transcription factors.53)
Figure 3.
(Color online) Mutations in cohesin complex. a. Structure of the cohesin complex comprising SMC1, SMC3, RAD21, and one of STAG1-3 proteins. Taking a ring-like structure, cohesin is loaded onto two chromatin strands in concert with cohesin-associated molecules. b. Cohesin is thought to be involved in gene regulation through interaction with transcription factors and other transcriptional apparatus. c. Distribution of mutations in major cohesin components. d. Mutually exclusive distribution of mutations of different cohesin components. Cited from Kon et al., Nature Genetics, 2013.51)
Landscape of gene mutations in MDS
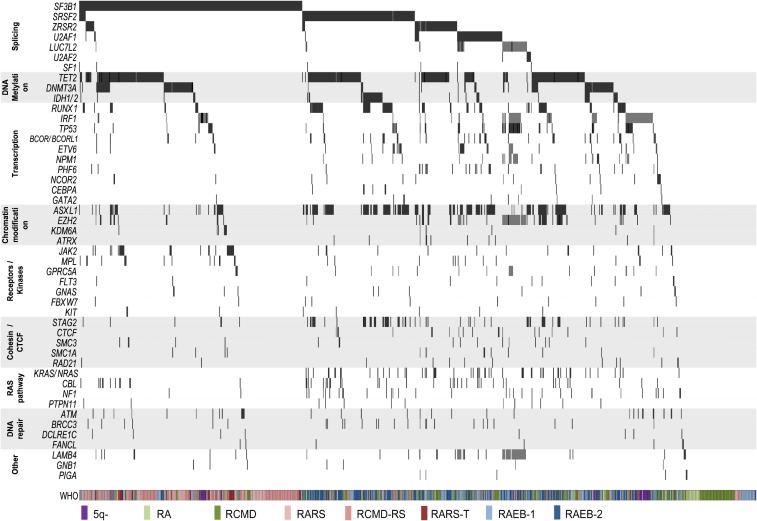
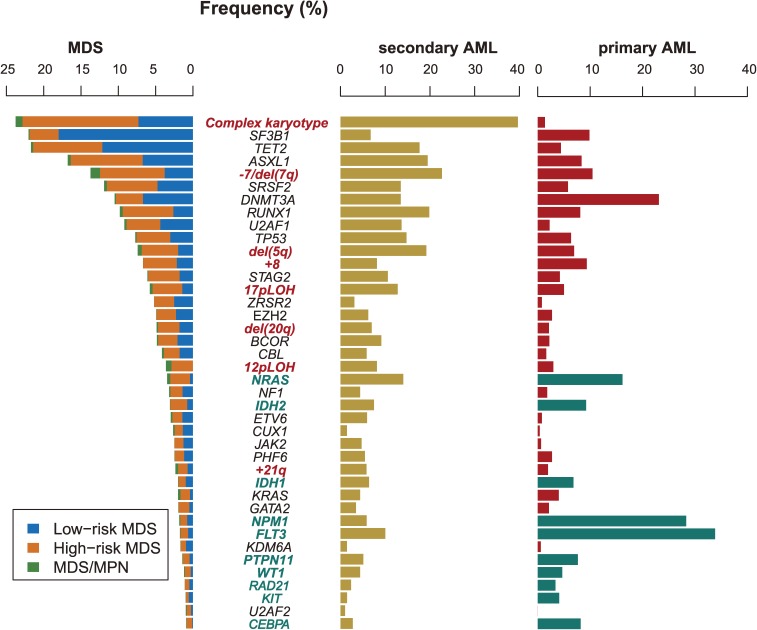
Other newly identified driver genes in MDS include BCOR/BCORL1,26,54) BRCC3,55,56) PHF6,26,57) ETV6, SETBP1,58,59) PRPF8,60) and RIT1.61) Thus, to elucidate the landscape of mutations in MDS, we conducted a comprehensive analysis of mutations in these major driver or candidate driver genes in a total of 944 MDS patients using targeted-capture sequencing. In total 47 genes were mutated at frequencies expected only by chance, where one or more of the 47 driver genes were mutated in as many as 864 (91.5%) of the 944 patients (Fig. 4).55) These driver genes were grouped into several discrete functional pathways, including RNA splicing, DNA methylation (TET2, DNMT3A, IDH1 and IDH2), chromatin modification (ASXL1, EZH2, and KDM6A), transcription (RUNX1, ETV6, BCOR/BCORL1, GATA2, CEBPA, and NPM1), receptor/tyrosine kinase, cohesin, RAS signaling (KRAS, NRAS, PTPN11, and CBL), and DNA repair (ATM, BRCC3, and FANCL). With a median of 3 per sample, the number of driver mutations increased with WHO risk. Among these, only 6 driver genes were mutated at 10% ≥ frequencies, followed by many low-frequency mutated genes. Most of the driver genes commonly mutated in MDS were also mutated in AML, but their frequency is substantially different between these malignancies (Fig. 5),62) suggesting that distinct pathogenesis between MDS and AML despite a substantial overlap in mutated drivers. In particular, a number of driver genes, including NRAS, FLT3, KRAS, PTPN11, IDH1, IDH2, WT1, RAD21, KIT, and CEBPA, were less frequently mutated in MDS compared with in primary AML (Fig. 5).63) This was also in line with the differences in the cytogenetic or copy number alteration profiles between AML and MDS. AML is characterized by frequent disease-specific reciprocal translocations, such as t(8;21)(q22;q22), inv(16)(p13q22), t(3;21)(q26;q22), t(15;17)(q22;q21) and other MLL(11q23)-affecting translocations, leading to RUNX1/RUNXT1, RUNX1/EVI1, PML/RARA, and a variety of MLL fusions, respectively. By contrast, most of the chromosomal lesions in MDS are unbalanced changes, which are caused by deletion and amplification of one or more chromosomal segments, including del(5q)/-5, del(7q)/-7, 12pLOH, del(20q), and 17pLOH (Fig. 5), most of which are seen in combinations as complex karyotypes in association with biallelic TP53 involvement. t(3;21)(q26;q22), inv(3)(q21q26), t(3;3)(q21;q26), t(1;3)(q36;q21), as well as t(6;9)(q22;q34) are typically seen in borderline cases between AML and MDS, predicting poor prognosis.63) Other abnormalities, such as +8, +21, are also seen in both AML and MDS at similar frequencies.
Figure 4.
(Color online) Landscape of gene mutations in 944 MDS cases. Mutations in 47 genes significantly mutated in 944 MDS cases are depicted. Driver genes are clustered according to their functions. Samples are shown in the horizontal axis with WHO classification in the indicated colors. Cited from Haferlach et al., Leukemia, 2014.55)
Figure 5.
Different mutation frequency between MDS, sAML, and primary AML. Frequency of major driver genes mutated in common in different myeloid malignancies, including MDS, sAML, and de novo primary AML. Risks of MDS are indicated by color. Mutations commonly seen in primary AML but only rarely in MDS are shown in dark blue in the AML panel. Cited from Ogawa, Blood, 2019.63)
Co-occurring and mutually exclusive mutations
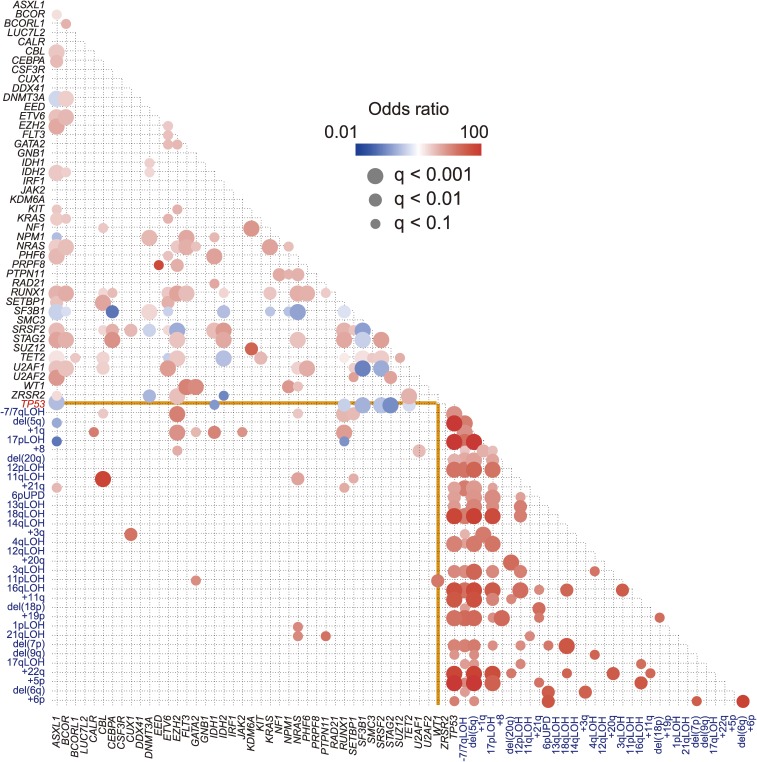
Among these driver mutations and copy number alterations, there exist strong positive and negative correlations. By exhaustively interrogating pairwise combination of mutations among the 944 patients, we detected a total of 82 significant (q < 0.01) combinations of mutations (Fig. 6), suggesting strong functional interactions between these mutations. Most of these significant combinations of mutations showed excellent concordance with those detected by analysis of independent MDS cohorts (Table 2), confirming the validity of these mutational combinations.64) For example, SF mutations are almost mutually exclusive with each other and so are mutations in components of the cohesin complex, likely due to synthetic lethality of multiple mutations in these pathways and complexes. By contrast, STAG2 mutations significantly cooccurred with mutations in RUNX1, SRSF2, ASXL1, EZH2, BCOR, and IDH2.55,64) Mutations and copy number alterations are largely mutually exclusive with some exceptions, of which significant correlations between copy number alterations and TP53 mutations. TP53 mutations, particularly when biallelic, are tightly associated with complex karyotypes with aneuploidy, which uniformly shows very poor prognosis resistant even to allogeneic stem cell transplantation, whereas TP53 mutations tend to be mutually exclusive with other mutations (Fig. 6).63)
Figure 6.
Genetic interactions between major driver mutation. Correlation-coefficients and corresponding q value are shown by color gradient and size of circle for all combinations of mutations in the indicated major drivers in 944 MDS cases. TP53 mutation and CNAs are shown in red and blue, respectively. Cited from Ogawa, Blood, 2019.63)
Table 2.
High concordance of coexisting mutations between independent studies
| Haferlach et al., Leukemia 201455) (N = 944) | Papaemmanuil et al., Blood 201364) (N = 738) | |
|---|---|---|
| TET2 | ZRSR2 (q < 0.0001), SRSF2, CBL (q < 0.001) | SRSF2, ZRSR2 (q < 0.01) |
| SF3B1 | DNMT3A, JAK2 (q < 0.01) | DNMT3A (q < 0.01) |
| SRSF2 | STAG2, ASXL1, RUNX1, IDH2 (q < 0.0001), TET2 (q < 0.001), CBL (q < 0.01) | STAG2, IDH2, CUX1, ASXL1, TET2, RUNX1 (q < 0.01) |
| U2AF1 | ASXL1 (q < 0.0001), PHF6, ETV6 (q < 0.01) | ASXL1 (q < 0.05) |
| ZRSR2 | TET2 (q < 0.0001), PHF6 (q < 0.01) | TET2 (q < 0.01) |
| STAG2 | ASXL1, RUNX1, SRSF2, NRAS, BCOR (q < 0.0001), IDH2 (q < 0.001), EZH2 (q < 0.01) | SRSF2, RUNX1 (q < 0.01), ASXL1 (q < 0.05), IDH2, EZH2 (q < 0.1) |
| DNMT3A | SF3B1 (q < 0.001) | SF3B1 (q < 0.01), BCOR (q < 0.05) |
| RUNX1 | SRSF2, ASXL1, EZH2, STAG2, BCOR (q < 0.0001) | STAG2, ASXL1, SRSF2 (q < 0.01), EZH2 (q < 0.05), NRAS (q < 0.1) |
| ASXL1 | SRSF2, U2AF1, STAG2, IDH2, EZH2, RUNX1, NRAS (q < 0.0001), CBL (q < 0.01) | SRSF2, RUNX1 (q < 0.01), JAK2, U2AF1, STAG2 (q < 0.05), IDH2, NRAS, CUX1 (q < 0.1) |
| EZH2 | RUNX1, ASXL1, TP53, LAMB4, LUC7L2, NPM1, ETV6 (q < 0.0001), NRAS (q < 0.001), STAG2 (q < 0.01) | RUNX1 (q < 0.05), STAG2 (q < 0.1) |
Significant correlations in both studies are shown in bold.
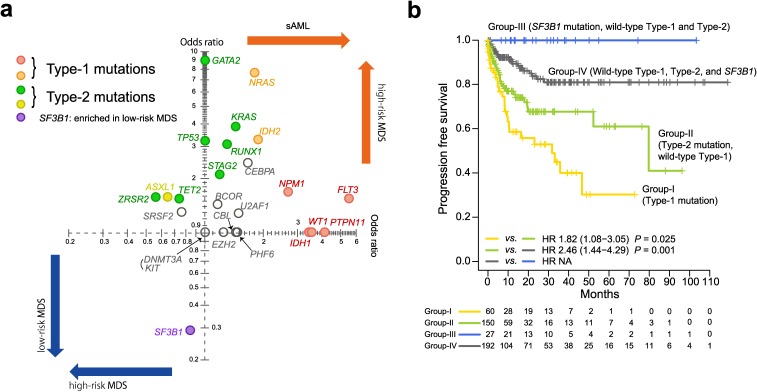
Moreover, not only combinations of mutations but also their order of acquisition is not totally random, but there is a strong trend that some mutations tend to precede others, frequently associated with progression from low-risk to high-risk diseases and to sAML. To examine this, we interrogated significant enrichment of mutations between low- and high-risk MDS and also between high-risk MDS and sAML in a cohort of 2,250 MDS cases.65) As shown in Fig. 7a, there was a significant enrichment of SF3B1 mutations in low-risk vs. high-risk MDS cases, whereas mutations in TP53, GATA2, RUNX1, KRAS, STAG2, ASXL1, ZRSR2, and TET2 (Type-2 mutations) were significantly enriched in high-risk compared with low-risk MDS. Between high-risk and sAML cases, there was a significant enrichment of mutations in FLT3, PTPN11, WT1, IDH1, NPM1, IDH2, and NRAS (Type-1 mutations) (Fig. 7a). These results suggested that Type-2 and Type-1 mutations are associated with progression from low-risk to high-risk MDS and high-risk MDS to sAML, respectively. To see this, we investigated the impact of Type-1 and Type-2 mutations on progression to sAML. We found that patients carrying one or more of Type-1 mutations at the time of diagnosis tended to progress to sAML earlier than those cases with Type-2 mutations alone (Fig. 7b). Patients with SF3B1 mutations but not Type-1 or Type-2 mutations rarely progressed to sAML and those without of Type-1 or Type-2 mutations displayed an intermediate risk of AML progression. Notably, all Type-1 mutations were also strongly enriched in primary AML, compared with MDS.63) Of further interest, upon progression to sAML, acquisition of one or more Type-1 mutations was confirmed in some patients with Type-2 mutations alone. These Type-1 and Type-2 mutations demonstrated significant co-occurrence between each other, suggesting that mutations are associated with disease progression. Recent studies more closely described the dynamics of clones during progression from MDS to AML using longitudinal samples for deep sequencing and single-cell sequencing. The presence of multiple clones in MDS, particularly in immature stem cell fractions, from which a clone evolves to sAML, while swiping other clones.65–67)
Figure 7.
(Color online) Major role of driver mutation in disease progression. a. Enrichment of driver mutations in sAML and high-risk MDS relative to high-risk and low-risk MDS, respectively. Enrichment is expressed as an odds ratio (OR) of mutation rates in sAML (n = 360) vs. high-risk MDS (n = 683) on the x axis and high-risk (n = 683) vs. low-risk (n = 1,207) on the y axis. Logistic regression analysis was applied to 25 driver genes measured in whole cohorts in 2,250 MDS and sAML patients, and the best model was selected by the least absolute shrinkage and selection operator. Mutations showing significant enrichment in either comparison are indicated by colors according to OR 95% CI limits being above (if OR >1) or below (if OR <1). According to their distinct enrichment patterns, mutations are classified into Type 1 or Type 2, as indicated. b. Progression-free survival of 429 patients with Type-1 mutations (group I), with Type-2 but not Type-1 mutations (group II), with SF3B1 but no Type-1 or Type-2 mutations (group III), and other patients with no Type-1, Type-2, or SF3B1 mutations (group IV). Cited from Makishima et al., Nature Genetics, 2017.65)
Clinical impact of mutations
Finally, we evaluated the impact of mutations on survivals of 944 MDS patients. To examine the impact of gene mutations, we generated two Cox proportional hazard models, in which the model was constructed using mutation alone (Model-II) or both clinical factors and mutations (Model-I), including complete blood counts, BM blast%, and cytogenetics, which were compared with IPSS and IPSS-R conventionally used for prognostication of MDS patients, using LASSO for selection of variables. In univariate analysis, mutations in 25 genes were significantly associated with overall survival (OS), of which only SF3B1 mutations predicted a better OS. The model combining clinical and gene mutations significantly outperformed traditional IPSS and IPSS-R models, which was in agreement with other studies,55) but in accordance of an earlier studies evaluating the clinical effects of mutations in MDS.68)
Conclusions
During the past two decades, our knowledge about the genetics of MDS has improved dramatically, with the revolution in genomics, particularly next-generation sequencing, providing a comprehensive registry of driver mutations in MDS, their frequency, and mutual correlations, as well as their impacts on disease phenotypes and prognosis. Now, allied efforts are in progress by the international working group for the prognosis of MDS (IWG-PM), in which thousands of MDS patients are being investigated for major driver mutations to confirm and further extend these initial findings. These studies provide a solid basis for novel molecular classifications of MDS, which help accurate diagnosis and prognostication, as well as better choice of therapies to ultimately improve patients’ clinical outcomes. Finally, despite a large number of newly revealed driver mutations, their functional roles in MDS pathogenesis remain to be elucidated for many drivers. For example, as seen above, SF mutations unequivocally play critical roles in MDS pathogenesis, whereas no functional evidence has been demonstrated for how SF-mutated hematopoietic cells achieve a clonal dominance; SF-mutated stem cells show a compromised competitive repopulation potential over normal stem cells in mouse models.36,42–45) The importance of understanding of the functional/molecular mechanisms of these driver mutations identified through genetic analyses cannot be underestimated.
Acknowledgement
This work is supported by Grants-in-Aid for Scientific Research (MEXT/JSPS KAKENHI JP26221308 and JP26253060), a Grant-in-Aid from the Japan Agency for Medical Research and Development (Project for Development of Innovative Research on Cancer Therapeutics [16cm0106501h0001], and Practical Research for Innovative Cancer Control Project [15ck0106073h0002 and 16ck0106073h0003]), and grants from the Takeda Science Foundation.
Profile
Seishi Ogawa was born in Okayama Prefecture in 1962 and graduated from Medical School at the University of Tokyo in 1988 and then from the Graduate School of Medicine, the University of Tokyo in 1993. He became Professor at Kyoto University in 2013. He has been the Head of the Department of Pathology and Tumor Biology since 2013 developing work on genome analysis of human cancers. Since 2017, he has been a guest professor at the Department of Medicine, Center for Hematology and Regenerative Medicine, Karolinska Institute, Stockholm, Sweden. He is a member of the Institute for the Advanced Study of Human Biology (WPI-ASHBi), Kyoto University since 2018. His scientific contributions have been central to understanding the pathogenesis of myelodysplastic syndromes, clear cell renal carcinoma, neuroblastoma, and other hematological cancers through the identification of key genetic alterations and mutations. He has exploited various approaches from the development of genome analysis tools, including the use of massively parallel sequencing technologies to comprehensively explore cancer genomes, giving rise to a series of publications (over 400 peer-reviewed papers). His work has also addressed the implication of these findings for cancer biology. He has received numerous prestigious awards, most recently, Education, Culture, Sports, Science and Technology Minister’s Commendation (2017), Uehara Prize (2017), Princes Takamatsu Cancer Research Fund Prize (2017), Takamine Prize (2018), Medal with Purple Ribbon (2018), and Erwin von Baelz Prize (2018). His work has received continuous funding support, including Gant-in-aids from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
References
- 1).Nimer S.D. (2008) Myelodysplastic syndromes. Blood 111, 4841–4851. [DOI] [PubMed] [Google Scholar]
- 2).Tefferi A., Vardiman J.W. (2009) Myelodysplastic syndromes. N. Engl. J. Med. 361, 1872–1885. [DOI] [PubMed] [Google Scholar]
- 3).Corey S.J., Minden M.D., Barber D.L., Kantarjian H., Wang J.C., Schimmer A.D. (2007) Myelodysplastic syndromes: The complexity of stem-cell diseases. Nat. Rev. Cancer 7, 118–129. [DOI] [PubMed] [Google Scholar]
- 4).List A., Kurtin S., Roe D.J., Buresh A., Mahadevan D., Fuchs D., et al. (2005) Efficacy of lenalidomide in myelodysplastic syndromes. N. Engl. J. Med. 352, 549–557. [DOI] [PubMed] [Google Scholar]
- 5).Fenaux P., Mufti G.J., Hellstrom-Lindberg E., Santini V., Finelli C., Giagounidis A., et al. (2009) Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: A randomised, open-label, phase III study. Lancet Oncol. 10, 223–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Hirai H., Kobayashi Y., Mano H., Hagiwara K., Maru Y., Omine M., et al. (1987) A point mutation at codon 13 of the N-ras oncogene in myelodysplastic syndrome. Nature 327, 430–432. [DOI] [PubMed] [Google Scholar]
- 7).Sugimoto K., Hirano N., Toyoshima H., Chiba S., Mano H., Takaku F., et al. (1993) Mutations of the p53 gene in myelodysplastic syndrome (MDS) and MDS-derived leukemia. Blood 81, 3022–3026. [PubMed] [Google Scholar]
- 8).Osato M., Asou N., Abdalla E., Hoshino K., Yamasaki H., Okubo T., et al. (1999) Biallelic and heterozygous point mutations in the runt domain of the AML1/PEBP2αB gene associated with myeloblastic leukemias. Blood 93, 1817–1824. [PubMed] [Google Scholar]
- 9).Imai Y., Kurokawa M., Izutsu K., Hangaishi A., Takeuchi K., Maki K., et al. (2000) Mutations of the AML1 gene in myelodysplastic syndrome and their functional implications in leukemogenesis. Blood 96, 3154–3160. [PubMed] [Google Scholar]
- 10).Steensma D.P., Higgs D.R., Fisher C.A., Gibbons R.J. (2004) Acquired somatic ATRX mutations in myelodysplastic syndrome associated with α thalassemia (ATMDS) convey a more severe hematologic phenotype than germline ATRX mutations. Blood 103, 2019–2026. [DOI] [PubMed] [Google Scholar]
- 11).Nannya Y., Sanada M., Nakazaki K., Hosoya N., Wang L., Hangaishi A., et al. (2005) A robust algorithm for copy number detection using high-density oligonucleotide single nucleotide polymorphism genotyping arrays. Cancer Res. 65, 6071–6079. [DOI] [PubMed] [Google Scholar]
- 12).Yamamoto G., Nannya Y., Kato M., Sanada M., Levine R.L., Kawamata N., et al. (2007) Highly sensitive method for genomewide detection of allelic composition in nonpaired, primary tumor specimens by use of affymetrix single-nucleotide-polymorphism genotyping microarrays. Am. J. Hum. Genet. 81, 114–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Sato-Otsubo A., Sanada M., Ogawa S. (2012) Single-nucleotide polymorphism array karyotyping in clinical practice: Where, when, and how? Semin. Oncol. 39, 13–25. [DOI] [PubMed] [Google Scholar]
- 14).Delhommeau F., Dupont S., Della Valle V., James C., Trannoy S., Masse A., et al. (2009) Mutation in TET2 in myeloid cancers. N. Engl. J. Med. 360, 2289–2301. [DOI] [PubMed] [Google Scholar]
- 15).Langemeijer S.M., Kuiper R.P., Berends M., Knops R., Aslanyan M.G., Massop M., et al. (2009) Acquired mutations in TET2 are common in myelodysplastic syndromes. Nat. Genet. 41, 838–842. [DOI] [PubMed] [Google Scholar]
- 16).Sanada M., Suzuki T., Shih L.Y., Otsu M., Kato M., Yamazaki S., et al. (2009) Gain-of-function of mutated C-CBL tumour suppressor in myeloid neoplasms. Nature 460, 904–908. [DOI] [PubMed] [Google Scholar]
- 17).Ernst T., Chase A.J., Score J., Hidalgo-Curtis C.E., Bryant C., Jones A.V., et al. (2010) Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nat. Genet. 42, 722–726. [DOI] [PubMed] [Google Scholar]
- 18).Nikoloski G., Langemeijer S.M., Kuiper R.P., Knops R., Massop M., Tönnissen E.R., et al. (2010) Somatic mutations of the histone methyltransferase gene EZH2 in myelodysplastic syndromes. Nat. Genet. 42, 665–667. [DOI] [PubMed] [Google Scholar]
- 19).Thoennissen N.H., Lasho T., Thoennissen G.B., Ogawa S., Tefferi A., Koeffler H.P. (2011) Novel CUX1 missense mutation in association with 7q- at leukemic transformation of MPN. Am. J. Hematol. 86, 703–705. [DOI] [PubMed] [Google Scholar]
- 20).Gelsi-Boyer V., Trouplin V., Adelaide J., Bonansea J., Cervera N., Carbuccia N., et al. (2009) Mutations of polycomb-associated gene ASXL1 in myelodysplastic syndromes and chronic myelomonocytic leukaemia. Br. J. Haematol. 145, 788–800. [DOI] [PubMed] [Google Scholar]
- 21).Ley T.J., Mardis E.R., Ding L., Fulton B., McLellan M.D., Chen K., et al. (2008) DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome. Nature 456, 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Meyerson M., Gabriel S., Getz G. (2010) Advances in understanding cancer genomes through second-generation sequencing. Nat. Rev. Genet. 11, 685–696. [DOI] [PubMed] [Google Scholar]
- 23).Vogelstein B., Papadopoulos N., Velculescu V.E., Zhou S., Diaz L.A., Jr., Kinzler K.W. (2013) Cancer genome landscapes. Science 339, 1546–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Mardis E.R., Ding L., Dooling D.J., Larson D.E., McLellan M.D., Chen K., et al. (2009) Recurring mutations found by sequencing an acute myeloid leukemia genome. N. Engl. J. Med. 361, 1058–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Ley T.J., Ding L., Walter M.J., McLellan M.D., Lamprecht T., Larson D.E., et al. (2010) DNMT3A mutations in acute myeloid leukemia. N. Engl. J. Med. 363, 2424–2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Yoshida K., Sanada M., Shiraishi Y., Nowak D., Nagata Y., Yamamoto R., et al. (2011) Frequent pathway mutations of splicing machinery in myelodysplasia. Nature 478, 64–69. [DOI] [PubMed] [Google Scholar]
- 27).Wahl M.C., Will C.L., Luhrmann R. (2009) The spliceosome: Design principles of a dynamic RNP machine. Cell 136, 701–718. [DOI] [PubMed] [Google Scholar]
- 28).Papaemmanuil E., Cazzola M., Boultwood J., Malcovati L., Vyas P., Bowen D., et al. (2011) Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N. Engl. J. Med. 365, 1384–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Malcovati L., Karimi M., Papaemmanuil E., Ambaglio I., Jädersten M., Jansson M., et al. (2015) SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood 126, 233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Yoshida K., Ogawa S. (2014) Splicing factor mutations and cancer. Wiley Interdiscip. Rev. RNA 5, 445–459. [DOI] [PubMed] [Google Scholar]
- 31).Meggendorfer M., Roller A., Haferlach T., Eder C., Dicker F., Grossmann V., et al. (2012) SRSF2 mutations in 275 cases with chronic myelomonocytic leukemia (CMML). Blood 120, 3080–3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32).Graubert T.A., Shen D., Ding L., Okeyo-Owuor T., Lunn C.L., Shao J., et al. (2012) Recurrent mutations in the U2AF1 splicing factor in myelodysplastic syndromes. Nat. Genet. 44, 53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33).Shao C., Yang B., Wu T., Huang J., Tang P., Zhou Y., et al. (2014) Mechanisms for U2AF to define 3′ splice sites and regulate alternative splicing in the human genome. Nat. Struct. Mol. Biol. 21, 997–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34).Darman R.B., Seiler M., Agrawal A.A., Lim K.H., Peng S., Aird D., et al. (2015) Cancer-associated SF3B1 hotspot mutations induce cryptic 3′ splice site selection through use of a different branch point. Cell Rep. 13, 1033–1045. [DOI] [PubMed] [Google Scholar]
- 35).Ilagan J.O., Ramakrishnan A., Hayes B., Murphy M.E., Zebari A.S., Bradley P., et al. (2015) U2AF1 mutations alter splice site recognition in hematological malignancies. Genome Res. 25, 14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36).Kim E., Ilagan J.O., Liang Y., Daubner G.M., Lee S.C., Ramakrishnan A., et al. (2015) SRSF2 mutations contribute to myelodysplasia by mutant-specific effects on exon recognition. Cancer Cell 27, 617–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37).Alsafadi S., Houy A., Battistella A., Popova T., Wassef M., Henry E., et al. (2016) Cancer-associated SF3B1 mutations affect alternative splicing by promoting alternative branchpoint usage. Nat. Commun. 7, 10615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38).Fei D.L., Motowski H., Chatrikhi R., Prasad S., Yu J., Gao S., et al. (2016) Wild-type U2AF1 antagonizes the splicing program characteristic of U2AF1-mutant tumors and is required for cell survival. PLoS Genet. 12, e1006384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Kesarwani A.K., Ramirez O., Gupta A.K., Yang X., Murthy T., Minella A.C., et al. (2017) Cancer-associated SF3B1 mutants recognize otherwise inaccessible cryptic 3′ splice sites within RNA secondary structures. Oncogene 36, 1123–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40).Shiozawa Y., Malcovati L., Galli A., Sato-Otsubo A., Kataoka K., Sato Y., et al. (2018) Aberrant splicing and defective mRNA production induced by somatic spliceosome mutations in myelodysplasia. Nat. Commun. 9, 3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41).Madan V., Kanojia D., Li J., Okamoto R., Sato-Otsubo A., Kohlmann A., et al. (2015) Aberrant splicing of U12-type introns is the hallmark of ZRSR2 mutant myelodysplastic syndrome. Nat. Commun. 6, 6042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Shirai C.L., Ley J.N., White B.S., Kim S., Tibbitts J., Shao J., et al. (2015) Mutant U2AF1 expression alters hematopoiesis and pre-mRNA splicing in vivo. Cancer Cell 27, 631–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43).Obeng E.A., Chappell R.J., Seiler M., Chen M.C., Campagna D.R., Schmidt P.J., et al. (2016) Physiologic expression of Sf3b1K700E causes impaired erythropoiesis, aberrant splicing, and sensitivity to therapeutic spliceosome modulation. Cancer Cell 30, 404–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44).Kon A., Yamazaki S., Nannya Y., Kataoka K., Ota Y., Nakagawa M.M., et al. (2018) Physiological Srsf2 P95H expression causes impaired hematopoietic stem cell functions and aberrant RNA splicing in mice. Blood 131, 621–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45).Mupo A., Seiler M., Sathiaseelan V., Pance A., Yang Y., Agrawal A.A., et al. (2017) Hemopoietic-specific Sf3b1-K700E knock-in mice display the splicing defect seen in human MDS but develop anemia without ring sideroblasts. Leukemia 31, 720–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46).Dolatshad H., Pellagatti A., Liberante F.G., Llorian M., Repapi E., Steeples V., et al. (2016) Cryptic splicing events in the iron transporter ABCB7 and other key target genes in SF3B1-mutant myelodysplastic syndromes. Leukemia 30, 2322–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47).Gruber S., Arumugam P., Katou Y., Kuglitsch D., Helmhart W., Shirahige K., et al. (2006) Evidence that loading of cohesin onto chromosomes involves opening of its SMC hinge. Cell 127, 523–537. [DOI] [PubMed] [Google Scholar]
- 48).Nasmyth K., Haering C.H. (2009) Cohesin: Its roles and mechanisms. Annu. Rev. Genet. 43, 525–558. [DOI] [PubMed] [Google Scholar]
- 49).Phillips-Cremins J.E., Sauria M.E., Sanyal A., Gerasimova T.I., Lajoie B.R., Bell J.S., et al. (2013) Architectural protein subclasses shape 3D organization of genomes during lineage commitment. Cell 153, 1281–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50).Welch J.S., Ley T.J., Link D.C., Miller C.A., Larson D.E., Koboldt D.C., et al. (2012) The origin and evolution of mutations in acute myeloid leukemia. Cell 150, 264–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Kon A., Shih L.Y., Minamino M., Sanada M., Shiraishi Y., Nagata Y., et al. (2013) Recurrent mutations in multiple components of the cohesin complex in myeloid neoplasms. Nat. Genet. 45, 1232–1237. [DOI] [PubMed] [Google Scholar]
- 52).Solomon D.A., Kim T., Diaz-Martinez L.A., Fair J., Elkahloun A.G., Harris B.T., et al. (2011) Mutational inactivation of STAG2 causes aneuploidy in human cancer. Science 333, 1039–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53).Noutsou M., Li J., Ling J., Jones J., Wang Y., Chen Y., et al. (2017) The cohesin complex is necessary for epidermal progenitor cell function through maintenance of self-renewal genes. Cell Rep. 20, 3005–3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54).Damm F., Chesnais V., Nagata Y., Yoshida K., Scourzic L., Okuno Y., et al. (2013) BCOR and BCORL1 mutations in myelodysplastic syndromes and related disorders. Blood 122, 3169–3177. [DOI] [PubMed] [Google Scholar]
- 55).Haferlach T., Nagata Y., Grossmann V., Okuno Y., Bacher U., Nagae G., et al. (2014) Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 28, 241–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56).Huang D., Nagata Y., Grossmann V., Radivoyevitch T., Okuno Y., Nagae G., et al. (2015) BRCC3 mutations in myeloid neoplasms. Haematologica 100, 1051–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57).Mori T., Nagata Y., Makishima H., Sanada M., Shiozawa Y., Kon A., et al. (2016) Somatic PHF6 mutations in 1760 cases with various myeloid neoplasms. Leukemia 30, 2270–2273. [DOI] [PubMed] [Google Scholar]
- 58).Makishima H., Yoshida K., Nguyen N., Przychodzen B., Sanada M., Okuno Y., et al. (2013) Somatic SETBP1 mutations in myeloid malignancies. Nat. Genet. 45, 942–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59).Sakaguchi H., Okuno Y., Muramatsu H., Yoshida K., Shiraishi Y., Takahashi M., et al. (2013) Exome sequencing identifies secondary mutations of SETBP1 and JAK3 in juvenile myelomonocytic leukemia. Nat. Genet. 45, 937–941. [DOI] [PubMed] [Google Scholar]
- 60).Kurtovic-Kozaric A., Przychodzen B., Singh J., Konarska M.M., Clemente M.J., Otrock Z.K., et al. (2015) PRPF8 defects cause missplicing in myeloid malignancies. Leukemia 29, 126–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61).Gomez-Segui I., Makishima H., Jerez A., Yoshida K., Przychodzen B., Miyano S., et al. (2013) Novel recurrent mutations in the RAS-like GTP-binding gene RIT1 in myeloid malignancies. Leukemia 27, 1943–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62).Papaemmanuil E., Gerstung M., Bullinger L., Gaidzik V.I., Paschka P., Roberts N.D., et al. (2016) Genomic classification and prognosis in acute myeloid leukemia. N. Engl. J. Med. 374, 2209–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63).Ogawa S. (2019) Genetics of MDS. Blood 133, 1049–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64).Papaemmanuil E., Gerstung M., Malcovati L., Tauro S., Gundem G., Van Loo P., et al. (2013) Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood 122, 3616–3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65).Makishima H., Yoshizato T., Yoshida K., Sekeres M.A., Radivoyevitch T., Suzuki H., et al. (2017) Dynamics of clonal evolution in myelodysplastic syndromes. Nat. Genet. 49, 204–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66).da Silva-Coelho P., Kroeze L.I., Yoshida K., Koorenhof-Scheele T.N., Knops R., van de Locht L.T., et al. (2017) Clonal evolution in myelodysplastic syndromes. Nat. Commun. 8, 15099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67).Chen J., Kao Y., Sun D., Todorova T., Reynolds D., Narayanagari S.-R., et al. (2019) Myelodysplastic syndrome progression to acute myeloid leukemia at the stem cell level. Nat. Med. 25, 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68).Bejar R., Stevenson K., Abdel-Wahab O., Galili N., Nilsson B., Garcia-Manero G., et al. (2011) Clinical effect of point mutations in myelodysplastic syndromes. N. Engl. J. Med. 364, 2496–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]