Abstract
Objective
As periprosthetic knee fractures are becoming common with the increase in incidence of primary and revision total knee arthroplasty, their management and treatment have become important. The current study aims to evaluate the revision knee arthroplasty carried out due to the failure of primary treatment of periprosthetic femoral fractures.
Methods
The study was conducted from May 2012 to September 2019 at Orthopedics department of Xinjiang Medical University; out of 21 patients 11 were women and 10 men aged 44 to 80 (mean, 70.76 ± 8.31) years who underwent revision surgery for periprosthetic fractures of 19 distal femur, 1 patellar, and 1 proximal tibial fracture. Nineteen cases had definite trauma history leading to periprosthetic fracture, and 2 cases had fracture during post-operative functional exercise. All patients had revision surgery with extended stems with either constrained or limited condylar knee prosthesis.
Results
The duration of follow-up averaged 4.3 years. The Hospital for Special Surgery (HSS) knee score before fracture averaged 91 + 7.01 points (89–95 points) and 85.5 + 6.18 points (81–90 points) at the last follow-up. The average range of motion of knee joint before fracture was 115.7 [+7.6] (110 [~126]), and 101.3 [+9.8] (85 [~115]) at the last follow-up. There was no significant statistical difference. No complications such as infection, component loosening or nonunion. 2 patients had lower extremity vein thrombosis.
Conclusion
Revision surgery of the knee for the periprosthetic fractures with proper prosthetic selection can attain good outcomes after primary total knee arthroplasty. Reasonable and correct procedure is the main principle for a successful operation. The benefits and applicability of revision TKA is the reconstructive solution for the issues of prosthetic knee fractures, is highly recommended.
Keywords: Knee arthroplasty, Periprosthetic fractures, Revision total knee arthroplasty
1. Introduction
Total knee arthroplasty is a well-known reconstructive technique. In only USA, 700,000 such procedures are carried out each year. In the last few years, the rate of primary TKA has doubled in many countries.1 Consequently, the periprosthetic fractures around the knee have also increased tremendously over these years. The orthopedic surgeons have to increasingly deal with patients having periprosthetic fractures.2
As periprosthetic knee fractures are becoming common with the increase in prevalence of primary and revision total knee arthroplasty, their management and treatment have become important.3 The treatment of periprosthetic fractures is oriented to re-establish alignment and gain pain functional range of motion devoid of pain. Many strategies have been recommended to manage periprosthetic fractures in order to gain a stable, functional, and well aligned knee.4 The treatment of periprosthetic fractures is directed toward osteosynthesis through fixed plate fixation or retrograde nailing and revision with extended rod prosthesis.5 However, many non-modifiable risk factors have been found to complex the surgical treatment of periprosthetic fractures. This includes bone quality, comminuted fracture, and demographics of the patients.6
The present treatment with advanced fixation techniques gives union rate of 78%–100%. Previous research has shown non-union rate to be 9%, infection to be 3% and fixation failure to be 4% for failure of distal femoral periprosthetic fractures.7 Another study showed malunion rate of 7.6%–19.2% and non-union rate of 3.6%–9.2%. This work supported locked plating method and intra-medullary implants in place of old and traditional methods. Both the studies gave re-operation rate of 8.7%–16.7%.8 Various research works have reported varying results with different techniques to address complications that rise due to failure of first treatment.9 These complications include mal-union, non-union, inappropriate union, loss of bone stock, instability and stiffness.10
The loose or malaligned implants with or without bone loss associated with periprosthetic fractures, are usually treated with revision TKA. However, the clinical outcomes of revision TKA vary due to which controversy prevails regarding its use.11 The problems include non-union, loss of fixation, malrotation, malalignment, prosthetic loosening and infection.12 The fixation failure may result due to poor bone quality, distal femoral fractures and malaligned TKA implants.13 However, some benefits have also been associated with the use of revision Total knee arthroplasty including improvement in knee range of motion and early mobilization.14
The revision arthroplasty is extremely important and plays dynamic role in periprosthetic fractures.15 Despite this fact, the literature on utilization of revision arthroplasty due to failure of primary treatment is insufficient.16 The present study aims to assess the revision surgery carried out due to periprosthetic fractures after primary total knee arthroplasty.
2. Material and methods
Records of 11 women and 10 men aged 44 to 80 (mean, 70.76 ± 8.31) years who underwent management for periprosthetic fractures of 19 distal femur, 1 patellar, and 1 proximal tibial fracture. There were 2 cases of Rorabeck type [1], 14 cases of type II and 4 cases of type III. One was classified as Felix type 2. Among them, 19 cases had definite trauma history leading to periprosthetic fracture, and 2 cases had fracture during functional exercise after operation. The median incision of knee joint was used to fix the fracture end with extension rod. Among them, 3 cases were severely comminuted fracture and internal fixation by locking plate was used to fix the fracture. 7 patients had constrained liner prosthesis and 14 with ordinary liner.
2.1. Operative indication
-
•
Supracondylar or intercondylar fractures around the joint
-
•
Implant loosening
-
•
Inappropriate place for internal fixation
-
•
Intolerance of bed for prolong time
2.2. Contraindication
-
•
Unfit for surgery due to poor general condition
-
•
Infection
-
•
limb dyskinesia
-
•
Low cardiac ejection fraction <40%
2.3. Preoperative preparation
Routine X-ray and CT scans of lower limbs were taken. By excluding the fracture and deformity angle of other parts of the fracture through full-length X-ray, CT was used to find out whether there was bone defect between the femoral condyles and the stability of the prosthesis. Blood routine, erythrocyte sedimentation rate and C-reactive protein were routinely examined before operation. The erythrocyte sedimentation rate and CRP were increased in some patients. Considering the relationship between ESR and CRP and trauma, the purpose of examination was to compare with the level of ESR and CRP after operation. Postoperative infection was excluded. All patients were treated with the second generation cephalosporin antibiotics 30 min before operation and 2–3 days after operation. Among them, 3 patients had exudation of the incision after operation and prolonged the use of antibiotics to 2 weeks. In order to prevent deep venous thrombosis of lower extremities, all patients were given anticoagulant therapy during perioperative period. Rivaroxaban was orally administered 8 h after operation, once a day for 3 weeks. At the same time, assistant physical therapy such as lower limb massage can prevent deep venous thrombosis of lower limbs.
2.4. Operative methods
Choose the original incision of the first operation and extend the exposure appropriately, dissect as little as possible to protect the blood supply of the fracture end, protect the soft tissue and knee extension device, and retain the original fragments and bone mass. Separate the interface between the prosthesis and bone cement with an oscillating saw, retain bone mass, thoroughly remove hematoma and granulation tissue, and clearly expose the fracture end and knee joint. Retain good fixation of the tibial component. If there is a mismatch between tibial prosthesis and femoral revision prosthesis, tibial prosthesis should be taken out. When dealing with one side of the femur, the distal femur is often free from the femoral shaft after complete debridement of the femoral prosthesis. The fractured end is temporarily fixed with Kirschner wire or bone holder. For comminuted fractures, locking plate can be added to assist fixation. Because of the fracture, it is difficult to locate the femoral prosthesis and use the osteotomy guide plate. All cases are guided to install the femoral prosthesis according to the supracondylar line or according to the position of the femoral medullary cavity rod. During the operation, attention should be paid to the integrity of the collateral ligament, and when necessary, the fixation should be strengthened by non-absorptive line. Thorough irrigation needed after fracture reduction. After traction restored limb length, for patients with different degrees of bone defect, autogenous bone from femoral osteotomy was used for bone grafting or cement filling. We have used condylar constrained knee prosthesis, NexGen condylar confinement prosthesis (Zimmer), LCCK + metaphyseal cone, (Fig. 1) legion (smith & Nephew), MBT (Depuy).
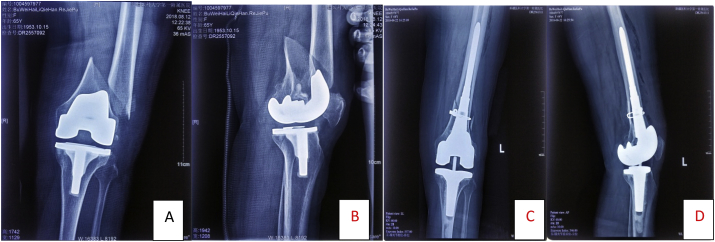
Fig. 1.
73yrs Male (A&B) shows with periprosthesis fractures, (C&D) shows Revision with extended stem TKA and cones.
Postoperatively, physiotherapy was started. Active and passive exercises were done. Non weight bearing mobilization was allowed which was progressively followed by full weight bearing after radiological evidence of bone healing. B-mode ultrasonography of lower extremity vessels was reviewed before discharge to exclude deep venous thrombosis of lower extremity. The patients were followed up regularly for 3 months, 6 months and 12 months after operation and once a year thereafter. Follow-up included The Hospital for Special Surgery (HSS) knee score, knee flexion and extension activity, full-length standing X-ray film of both lower extremities and anterolateral film of knee joint to measure and evaluate the force line of lower extremities, prosthesis position and fracture healing.
3. Results
The mean age of patients was 70.76 ± 8.31 years ranging from 44 to 80 years. The percentage of male and female was 47.6% and 52.4% respectively (Table 1).Rorabeck 2 was the most common classification (66.7%). Rorabeck 3 was the second most common (19%) and Rorabeck 1 was the third most common classification (9.5%). Other Felix classification each constituted 4.8% (Table 2). Seven cases had constrained condylar prosthesis (33.3%) and 11 had limited condylar prosthesis (52.4%) and three combine with locking plate due to communited fracture of distal femur(Table 3). The operation time of this group was 70–125 min, with an average of 89 min. All the patients were followed up. The follow-up period ranged from 8 months to 7 years, with an average of 4.3 years. The Hospital for Special Surgery (HSS) knee score before fracture averaged 91 + 7.01 points (89–95 points) and 85.5 + 6.18 points (81–90 points) at the last follow-up. The average range of motion of knee joint before fracture was 115.7 [+7.6] (110 [~126]), and 101.3 [+9.8] (85 [~115]) at the last follow-up. There were no complications such as infection, loosening and fracture nonunion. Three patients with incision exudation were treated with prolonged antibiotics for 2 weeks, and the incision healed. Intermuscular venous thrombosis was found by B-mode ultrasonography in 2 patients after operation. Rivaroxaban was taken orally for anticoagulation and the thrombosis disappeared within a month. Fractures healed about 6 months after operation. The other patients had no complications such as infection, instability of knee joint and unequal length of lower limbs.
Table 1.
Age and sex distribution of patients.
| Age and sex | n = 21 |
|---|---|
| Age in years, mean ± SD (Range) | 70.76 ± 8.31 (44–80) |
| Sex, no. (%) | |
| Male | 10 (47.6) |
| Female | 11 (52.4) |
Table 2.
Distribution of patients according to Lewis and Rorabeck classification.
| Rorabeck classification | No. (n = 21) | % |
|---|---|---|
| Rorabeck 1 | 2 | 9.5 |
| Rorabeck 2 | 13 | 61.9 |
| Rorabeck 2+goldberg 2 | 1 | 4.8 |
| Rorabeck 3 | 4 | 19.0 |
| FELIX 2 | 1 | 4.8 |
Table 3.
Distribution of patients according to surgical materials used.
| Surgical materials used | No. (n = 21) | % |
|---|---|---|
| Constrained condylar prosthesis | 7 | 33.3 |
| Limited condylar prosthesis | 11 | 52.4 |
| Limited condylar prosthesis + LISS | 3 | 14.3 |
4. Discussion
As the number of individuals taking primary or revision TKA is increasing, the relevant complications are also at increase. There are many causes of periprosthetic fracture after knee arthroplasty, which are mainly divided into patient factors such as age, female, trauma, aggressive activity, chronic use of steroids/corticoid therapy, rheumatoid arthritis and other risk factors is surgical factors such as excessive anterior femoral notching, forceful manipulation. According to an estimate, the risk of periprosthetic knee fracture ranges from 1.1% to 2.1% for primary knee arthroplasty, whereas, for revision TKA it has range of 0.7%–1.5%.17 Internal fixation is widely used to address acute periprosthetic knee fractures, which renders advantage over non-operative techniques. Anyhow, various factors make operative techniques challenging and perplexing for surgeon.18 These factors include implant types, fracture displacement, amount and quality of bone available, position, and fixation.19
In order to avoid loss of mobility in patients with periprosthetic fractures, timely fracture union is important. The previous research works have achieved this goal with the use of various conventional plating techniques.20 On the other hand, others have addressed to perplexities of salvage procedures in case of implant failure, non-union or mal-union. In a study performed by Deshmukh et al.,21 two out of thirty femoral cases showed delayed union had been addressed through revision fixation and bone grafting. The study of Abbas and Morgan-Jones22 showed higher levels of failure due to internal fixation and open reduction. Majority of the patients required repeated open reduction, and revision TKA. The work of Horneff et al.23 utilized supplemental strut grafting to the failed fixations and claimed good results in majority of the cases. Previous research works have pointed out towards various complications associated with fracture union.24 These complications are addressed with the help of different modern techniques of locked plating. However, the success rate may vary in accordance with the treatment strategies adopted to counter with the complications of failed primary treatment.25 Many factors exists that influence the revision fracture fixation. They may include secondary implant loosening, loss of bone stock and impaired vascularity.26 The fixation and stability of revision arthroplasty also get effected by loss of metaphyseal bone. To address this issue, distal femoral arthroplasty has widely been used by many researchers, especially in the low demand subgroup of individuals.27 Anyhow, many complications are associated with this method, when used to counter primary treatment failure.28
The revision TKA is a conventional method used for periprosthetic fractures. Indications for the technique include component malposition, component loosening, instability, loss of bone stock and wear.29 Despite its importance, only few research works have elaborated use of reivion TKA for managing mal-union or non-union of periprosthetic fractures.30 A previous study reported successful treatment of femoral non-unions with the help of bone grafting and long stem primary knee arthroplasty.31 However, the literature shows varying results for revision arthroplasty, when used to address failed primary fixation or non-union of periprosthethic knee fractures.
The incidence of fracture in patients over 70 years old was 1.6 times higher than that in young patients, while the incidence in female patients was higher than that in male patients. The average age of this group was 70 years old. There were 11 female patients, accounting for 52.4% of all patients. This was consistent with the literature. The main reasons are the decline of muscle strength, poor compensatory ability of cardiopulmonary function, weakening of patient's activity, prone to falls, sprains and other accidents. Low-energy injury can lead to serious periprosthetic fracture of knee joint. In this group, 2 patients had periprosthetic fracture of distal femur during functional exercise after operation. Excess anterior femoral notching in knee arthroplasty weakened the strength of anterior and posterior femoral cortex. It should be avoided as far as possible during operation. Therefore, the causes of periprosthetic fracture of distal femur after knee arthroplasty are various. Patients often have multiple risk factors for such complications. In order to avoid the occurrence of fracture, it is necessary to prevent from the internal and external causes of patients, so as to reduce the pain of patients. According to the patient's bone condition, fracture type and stability of the prosthesis, the treatment of periprosthetic fracture of after knee arthroplasty includes conservative treatment, mainly for patients with no displacement of fracture or absolute contraindication of operation; open reduction and internal fixation includes locking plate and intramedullary nail fixation, mainly for patients without loosening of prosthesis. Patients with enough space for fixation at the fracture end but revision knee arthroplasty is mainly used for patients with prosthesis loosening and comminuted fracture without possibility of internal fixation. A large number of literatures have described the treatment of open reduction and internal fixation, including locking compression plate and retrograde intramedullary nail fixation. For patients with good bone prosthesis stability, according to the type of fracture, there is no significant difference in the time of bed rest, complications and joint function recovery. However, there are nonunions and deformities in both methods. For elderly patients, in order to avoid the complications caused by bed rest and the risk of secondary operation of nonunion and malunion, many surgeons have proposed revision of knee joint or special prosthesis for periprosthetic knee fractures in recent years, which can carry out early weight-bearing activities, retain knee joint function, quick recovery and improve patients' quality of life. In this group of 21 cases, we used knee revision surgery, see (Fig. 2, Fig. 3) instead of using custom-made distal femur prosthesis and rotating hinge knee prosthesis, the authors of the literature used constrained condylar prosthesis. During the operation the fracture end was fixed with extension rod, similar to the effect of intramedullary nail, which shortened the operation time and allowed the patients to move early and perform functional exercises. This method can reduce the complications and mortality of patients especially for elderly patients with severe comminuted periprosthetic fracture with osteoporosis.
Fig. 2.
65 yrs F with fig (a & b)Rorabeck type 3 treated by revision surgery fig (c&d).
Fig. 3.
80yrs Male (a) Felix fracture (b&c) revision surgery done extended stemmed TKA.
In the present research work, all individuals showed pain free mobility at last follow-up visit. Moreover, improvement in knee score and functional score was observed along with knee range of motion. These findings indicate the benefits and applicability of revision TKA. The use of revision TKA, as a reconstruction solution for the issues of mal-union and non-union of prosthetic knee fractures, is highly recommended. The problems of alignment, stability and bone loss can be well addressed through adequate use of constraint levels, intramedullary stems and metaphyseal sleeves.
4.1. Prosthetic selection
When TKA is performed on patients with distal femoral periprosthetic fracture, the type of prosthesis should be selected according to the degree of bone defect of distal femur, age and activity of patients. Hinged knee joint, rotating hinge knee joint and specially customized knee joint with distal femur are commonly used, but the loosening rate of prosthesis is higher. Springer et al.32 reported that 69 cases of old femoral supracondylar fracture were treated with knee joint revision and TKA for the first time. The short-term effect was satisfactory. 30% of the cases had complications such as infection, fracture and loosening after 5 years of follow-up. Hinged knee prosthesis is not used in this group because it avoids removing more bone and is more conducive to future revision. We have selected following prosthesis for knee revision: LCCK (Zimmer), Legion (Smith Nephew) and MBT (Depuy) The advantages of these prosthesis with extension handle are1: automatic alignment, inserting extension rod into cortical bone after full extension, and then determining the force line2; design of extension rod with different lengths, which can play a good role in fracture fixation and support through the fracture end, allowing early mobilization. The aim was to increase the stability of the knee joint, prevent early complications such as loosening of the prosthesis due to the instability of the knee joint, and improve the survival rate of the prosthesis.
5. Conclusion
Knee revision surgery for periprosthetic fracture of distal femur after knee arthroplasty is a challenging problem for joint surgeons, and it is also one of the complex operations. Only surgeons with rich clinical skill can successfully complete the operation after detailed and comprehensive preoperative planning. The revision of knee joint for the treatment of periprosthetic fracture after TKA can achieve good surgical outcomes, with improved functionality and good follow-up results. In case of bone loss the use of metaphyseal sleeves is also an effective option in the setting of revision TKA.
Funding
No funding was received for this research.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of competing interest
No conflicts of interest were declared by the authors.
References
- 1.Duncan C., Haddad F. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Joint Lett J. 2014;96:713–716. doi: 10.1302/0301-620X.96B6.34040. [DOI] [PubMed] [Google Scholar]
- 2.Bukata S., DiGiovanni B., Friedman S. A guide to improving the care of patients with fragility fractures. Geriatr. Orthop. Surg. Rehabil. 2011;2:5–37. doi: 10.1177/2151458510397504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Streubel P. Mortality after periprosthetic femur fractures. J Knee Surg. 2013;26:27–30. doi: 10.1055/s-0033-1333905. [DOI] [PubMed] [Google Scholar]
- 4.Lee S., Lim S., Moon Y. Outcomes of long retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134:47. doi: 10.1007/s00402-013-1890-7. [DOI] [PubMed] [Google Scholar]
- 5.Ristevski B., Nauth A., Williams D. Systematic review of the treatment of periprosthetic distal femur fractures. J Orthop Trauma. 2014;28:307. doi: 10.1097/BOT.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal S., Azam A., Morgan-Jones R. Metal metaphyseal sleeves in revision total knee replacement. Bone Joint Lett J. 2013;95:1640. doi: 10.1302/0301-620X.95B12.31190. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal S., Sharma R., Jain J. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg. 2014;22:24–29. doi: 10.1177/230949901402200108. [DOI] [PubMed] [Google Scholar]
- 8.Weiser L., Korecki M., Sellenschloh K. The role of inter-prosthetic distance, cortical thickness and bone mineral density in the development of interprosthetic fractures of the femur: a biomechanical cadaver study. Bone Joint Lett J. 2014;96:1378–1384. doi: 10.1302/0301-620X.96B10.33461. [DOI] [PubMed] [Google Scholar]
- 9.Kancherla V., Nwachuku C. The treatment of periprosthetic femur fractures after total knee arthroplasty. Orthop Clin N Am. 2014;45:457–467. doi: 10.1016/j.ocl.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Aldrian S., Schuster R., Haas N. Fixation of supracondylar femoral fractures following total knee arthroplasty: is there any difference comparing angular stable plate fixation versus rigid interlocking nail fixation? Arch Orthop Trauma Surg. 2013;133:921. doi: 10.1007/s00402-013-1730-9. [DOI] [PubMed] [Google Scholar]
- 11.Saidi K., Ben-Lulu O., Tsuji M., Safir O., Gross A., Backstein D. Supracondylar periprosthetic fractures of the knee in the elderly patients: a comparison of treatment using allograft-implant composites, standard revision components, distal femoral replacement prosthesis. J Arthroplasty. 2014;29:110–114. doi: 10.1016/j.arth.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Jassim S., McNamara I., Hopgood P. Distal femoral replacement in periprosthetic fracture around total knee arthroplasty. Injury. 2014;45:550–553. doi: 10.1016/j.injury.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 13.Streubel P., Gardner M., Morshed S., Collinge C., Gallagher B., Ricci W. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br. 2010;92:527–534. doi: 10.1302/0301-620X.92B3.22996. [DOI] [PubMed] [Google Scholar]
- 14.Cannon S. The use of megaprosthesis in the treatment of periprosthetic knee fractures. Int Orthop. 2015;39:1945–1950. doi: 10.1007/s00264-015-2969-2. [DOI] [PubMed] [Google Scholar]
- 15.Johnston A., Tsiridis E., Eyres K., Toms A. Periprosthetic fractures in the distal femur following total knee replacement: a review and guide to management. Knee. 2012;19:156–162. doi: 10.1016/j.knee.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Chen A., Choi L., Colman M. Primary versus secondary distal femoral arthroplasty for treatment of total knee arthroplasty periprosthetic femur fractures. J Arthroplasty. 2013;28:1580–1584. doi: 10.1016/j.arth.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 17.Meek R., Norwood T., Smith R., Brenkel I., Howie C. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011;93:96–101. doi: 10.1302/0301-620X.93B1.25087. [DOI] [PubMed] [Google Scholar]
- 18.Sarmah S., Patel S., Reading G. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012;94:302. doi: 10.1308/10.1308/003588412X13171221592537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nauth A., Ristevski B., Bégué T., Schemitsch E. Periprosthetic distal femur fractures: current concepts. J Orthop Trauma. 2011;25:S82–S85. doi: 10.1097/BOT.0b013e31821b8a09. [DOI] [PubMed] [Google Scholar]
- 20.Gavaskar A., Tummala N., Subramanian M. The outcome and complications of the locked plating management for the periprosthetic distal femur fractures after a total knee arthroplasty. Clin Orthop Surg. 2013;5:124. doi: 10.4055/cios.2013.5.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deshmukh A., Thakur R., Rasquinha V., Rodriguez J. Femoral revision arthroplasty for Su type 3 supracondylar periprosthetic knee fractures. J Knee Surg. 2015;28(4):349–353. doi: 10.1055/s-0034-1390029. [DOI] [PubMed] [Google Scholar]
- 22.Abbas A., Morgan-Jones R. Revision total knee arthroplasty for failure of primary treatment of periprosthetic knee fractures. J Arthroplasty. 2014;29:1996–2001. doi: 10.1016/j.arth.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 23.Horneff J., Scolaro J., Jafari S. Intramedullary nailing versus locked plate for treating supracondylar periprosthetic femur fractures. Orthopedics. 2013;36:561. doi: 10.3928/01477447-20130426-16. [DOI] [PubMed] [Google Scholar]
- 24.Hoffmann M., Jones C., Sietsema D., Koenig S., Tornetta P. Outcome of periprosthetic distal femoral fractures following knee arthroplasty. Injury. 2012;43:1084–1089. doi: 10.1016/j.injury.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 25.Singh J., Jensen M., Lewallen D. Predictors of periprosthetic fracture after total knee replacement: an analysis of 21,723 cases. Acta Orthop. 2013;84:170–177. doi: 10.3109/17453674.2013.788436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scolaro J., Schwarzkopf R. Management of interprosthetic femur fractures. J Am Acad Orthop Surg. 2017;25:e63–e69. doi: 10.5435/JAAOS-D-15-00664. [DOI] [PubMed] [Google Scholar]
- 27.Hou Z., Bowen T., Irgit K. Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma. 2012;26:427. doi: 10.1097/BOT.0b013e31822c050b. [DOI] [PubMed] [Google Scholar]
- 28.Höll S., Schlomberg A., Gosheger G. Distal femur and proximal tibia replacement with megaprosthesis in revision knee arthroplasty: a limb-saving procedure. Knee Surg Sports Traumatol Arthrosc. 2012;20:2513. doi: 10.1007/s00167-012-1945-2. [DOI] [PubMed] [Google Scholar]
- 29.Kim Y., Park J., Kim J., Oh H. Longterm clinical outcomes and survivorship of revision total knee arthroplasty with use of a constrained condylar knee prosthesis. J Arthroplasty. 2015;30:1804–1809. doi: 10.1016/j.arth.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Hou Z., Moore B., Bowen T. Treatment of interprosthetic fractures of the femur. J Trauma. 2011;71:1715–1719. doi: 10.1097/TA.0b013e31821dd9f1. [DOI] [PubMed] [Google Scholar]
- 31.Derome P., Sternheim A., Backstein D., Malo M. Treatment of large bone defects with trabecular metal cones in revision total knee arthroplasty: short term clinical and radiographic outcomes. J Arthroplasty. 2014;29:122–126. doi: 10.1016/j.arth.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 32.Springer B.D., Hanssen A.D., Sim F.H. The kinematic rotating hinge prosthesis for complex knee arthroplasty[J] Clin Orthop. 2001;392:283–291. doi: 10.1097/00003086-200111000-00037. [DOI] [PubMed] [Google Scholar]