Abstract
The SARS-CoV-2 infection (COVID-19), originally reported in Wuhan, China, has rapidly proliferated throughout several continents and the first case in the United States was reported on January 19, 2020. According to the ACR guidelines issued shortly after this disease was declared a pandemic, radiologists are expected to familiarize themselves with the CT appearance of COVID-19 infection in order to be able to identify specific findings of this entity. This case report discusses the relevant imaging findings of one of the first cases in the mid-western United States. It involves a 60-year-old man who presented with fever, dyspnea, and cough for 1 week and subsequently tested positive for COVID-19. The utility of the noncontrast CT chest in the diagnosis of COVID-19 has been controversial, but there are specific imaging findings that have been increasingly associated with this virus in the appropriate clinical context. The stages of imaging findings in COVID-19 are considered along with the implications of fibrosis throughout the stages. Future considerations include using artificial intelligence algorithms to distinguish between community acquired pneumonias and COVID-19 infection.
Abbreviations: ACR, American College of Radiology; CT, computed tomography; COVID-19, coronavirus disease 2019; COVNet, COVID-19 detection neural network; DAD, diffuse alveolar damage; GGO, ground-glass opacity; ICU, intensive care unit; PCR, polymerase chain reaction; rRT-PCR, real-time reverse transcriptase polymerase chain reaction; SARS-CoV-1 infection, severe acute respiratory syndrome coronavirus from the 2003 outbreak; SARS-CoV-2 infection, severe acute respiratory syndrome coronavirus 2; SDU, step down unit
Case report
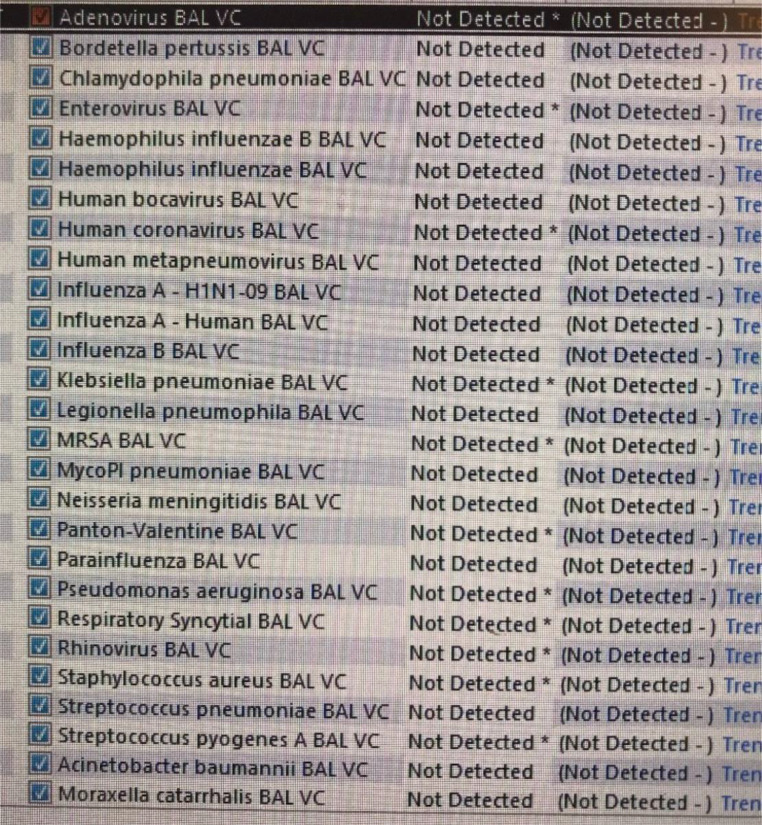
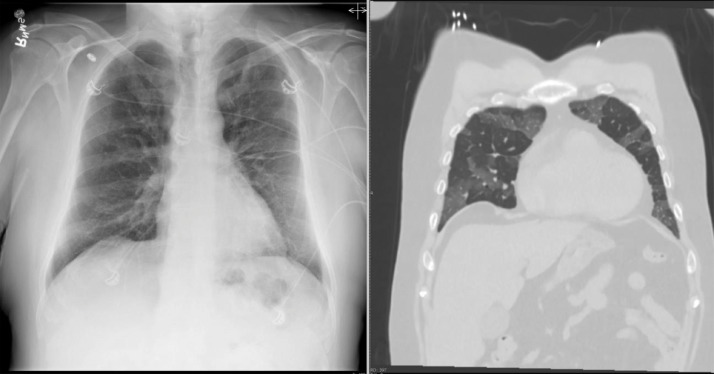
On March 8, 2020, a 60-year-old man presented to the emergency room with fever elevated to 38.1°C (100.5°F), cough, and shortness of breath. The patient did not have any significant comorbidities or contributory travel history. He was tested for several viral pathogens using a respiratory viral panel by PCR and was found to be negative for all of them (Fig. 1). A chest X-ray was ordered and initially read as normal (Fig. 2). However, in retrospect, there is a suggestion of subsegmental ground-glass opacities (GGO) beginning to become apparent given the onset of symptoms 7 days prior to admission. Of note, there is no evidence of lymphadenopathy or pleural effusions on this chest X-ray. While most patients imaged at 0-2 days after symptom onset had normal imaging, studies have shown limited specificity in diagnosing lower respiratory tract illnesses with chest X-ray [1].
Fig. 1.
Respiratory viral panel by PCR dated March 8, 2020: Nonreactive respiratory viral PCR panel (not including COVID-19 which was later found to be positive upon transfer).
Fig. 2.
PA chest X-ray dated March 8, 2020 (frontal view): There are patchy hazy subsegmental opacities noted bilaterally.
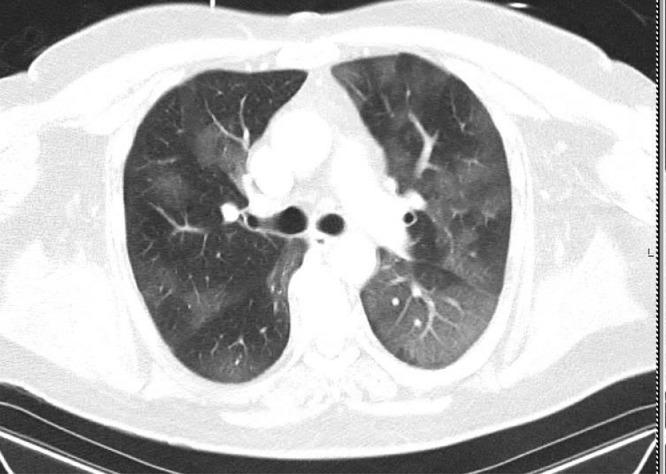
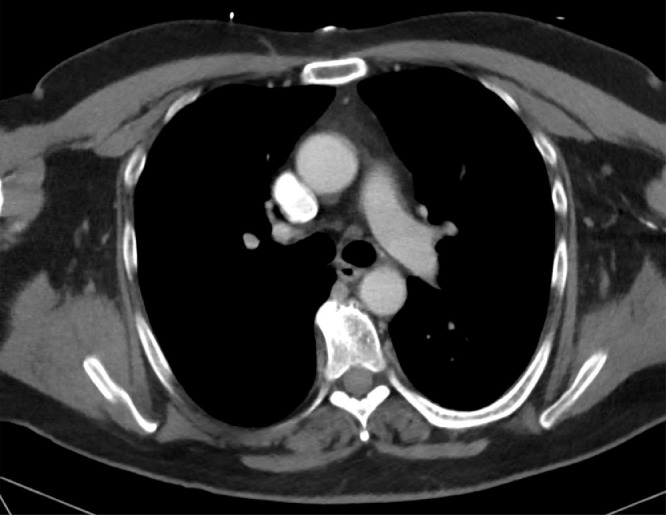
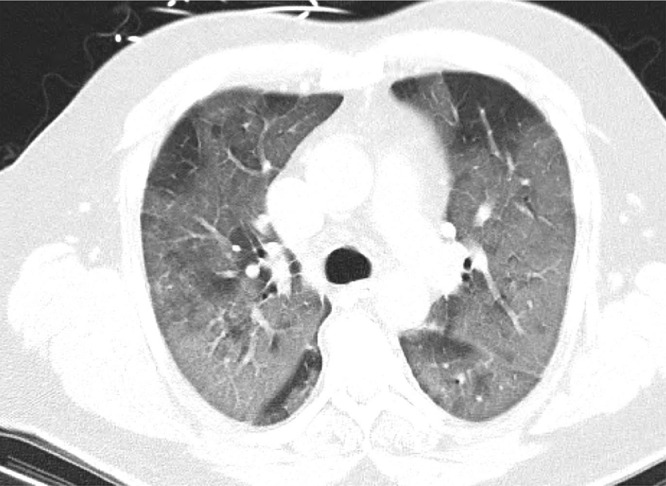
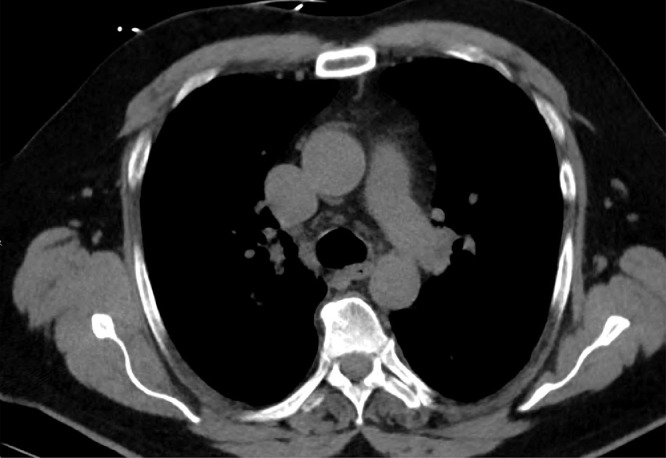
The next day, on March 9, 2020, a contrast-enhanced chest CT demonstrated subsegmental GGO extending to the periphery of the lungs without subpleural sparing (Fig. 3). There was no evidence of tree-in-bud opacities, pleural effusions, cavitation, or mediastinal/hilar lymphadenopathy (Fig. 4). The chest X-ray and coronal view of the early chest CT are 1 day apart and one can visualize to better advantage where there may have been GGO forming even on the chest X-ray a day earlier (Fig. 5). These findings along with the clinical symptoms suggested an early phase SARS-CoV-2 infection (COVID-19) and isolation protocols were followed based upon this suspicion.
Fig. 3.
Contrast-enhanced chest CT dated March 9, 2020 (axial view/lung window): Subsegmental ground glass opacities are noted extending to the periphery of the lungs without subpleural sparing.
Fig. 4.
Contrast-enhanced chest CT dated March 9, 2020 (axial view/soft-tissue window): There was no evidence of tree-in-bud opacities, pleural effusions, cavitation, or mediastinal/hilar lymphadenopathy.
Fig. 5.
Contrast-enhanced chest CT dated March 9, 2020 (axial view/lung window) and frontal CXR dated March 8, 2020: The coronal view of the early chest CT and the frontal chest X-ray are 1 day apart and one can visualize to better advantage where there may have been ground-glass opacities forming even on the early chest X-ray a day earlier.
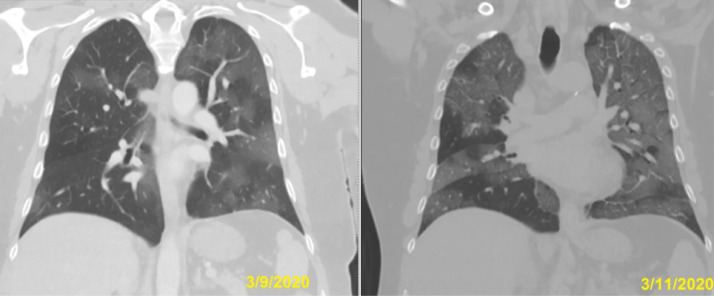
The patient demonstrated marked progression of dyspnea on March 11, 2020 and a follow-up noncontrast chest CT demonstrated significant progression of peripherally based GGO, now involving multiple segments of the lungs bilaterally. CT images of both lungs show multifocal GGO with consolidation scattered in peripheral zones of the lungs with poorly defined boundaries, vascular thickening, and associated intralobular septal thickening “crazy paving pattern” suggesting progressive phase COVID-19 infection (Fig. 6). Of note, no pleural effusions or lymphadenopathy had developed in the 2-day interval (Fig. 7). The correlation between the progression of clinical symptoms and imaging findings helped to exclude other noninfectious etiologies that can be seen with a peripheral pattern of lung disease (Figs. 8 and 9).
Fig. 6.
Contrast-enhanced chest CT dated March 11, 2020 (axial view/lung window): CT images of both lungs show progression of multifocal ground-glass opacities with developing consolidation scattered in the peripheral zones of the lungs. There are poorly defined boundaries, vascular thickening, and associated intralobular septal thickening “crazy paving pattern” suggesting progressive phase COVID-19 infection.
Fig. 7.
Contrast-enhanced chest CT dated March 11, 2020 (axial view/soft-tissue window): There was no evidence of tree-in-bud opacities, pleural effusions, cavitation, or mediastinal/hilar lymphadenopathy.
Fig. 8.
Comparison of contrast-enhanced chest CTs dated March 9, 2020 and March 11, 2020 (axial view/lung window): Interval progression from early phase to progressive phase COVID-19 infection within 3 days correlating with increasing dyspnea.
Fig. 9.
Contrast-enhanced chest CTs dated March 9, 2020 and March 11, 2020 (coronal view/lung window): Interval progression from early phase to progressive phase COVID-19 infection within 3 days correlating with increasing dyspnea.
The patient was subsequently transferred to an outside hospital where an rRT-PCR test was positive for COVID-19. The patient was admitted to the intensive care unit and placed on prone ventilation and started on remdesivir. The patient was followed with serial chest X-rays, but no imaging is available from this stay. On March 18, 2020, the patient remained dependent on a ventilator, but was beginning to stabilize using a combination of prone ventilation and remdesivir treatment. As of March 26, 2020, the patient had been extubated and transferred to the step down unit having demonstrated marked improvement in oxygen saturation. It remains unclear whether the drug treatment was responsible for this stability or if supportive care allowed the patient's immune system to respond appropriately. At the time of this submission, the patient remained admitted to the inpatient unit, but was recovering.
Discussion
The first documented case of community-acquired COVID-19 infection was a 35-year-old man in the state of Washington on January 19, 2020 [2]. Since the outbreak in Wuhan, China, it has been suggested that this disease appears to be more severe in male patients, patients over 60 years old, or patients with underlying respiratory or cardiac disease. The early symptoms, according to the CDC, include shortness of breath, fever, and cough. The pathologic diagnosis includes negative STAT rapid influenza and RSV PCR tests with a positive COVID-19 rRT-PCR test. However, at the time of this publication testing is not yet routinely available at all medical facilities throughout the country or to asymptomatic members of the general public. When COVID-19 rRT-PCR tests are available at a healthcare facility, obtaining results could vary between hours to 5 days.
Imaging has played a controversial role in the diagnosis and management of COVID-19. There have been several publications that indicate a role for chest CT in early detection of COVID-19 when combined with clinical suspicion and high pretest probability [3]. For example, one study published in the American Journal of Roentgenology on February 20, 2020 found that there was a low miss rate for COVID-19 on chest CT (3.9% 2/51 cases). Therefore, a negative chest CT may assist in management by allowing physicians to determine whether quarantine is warranted when the patient is within the incubation window [4]. However, in mid-March of 2020, the ACR issued an official statement on this topic and acknowledged that under current shortages and delays in testing: "some medical practices are requesting chest CT to inform decisions on whether to test a patient for COVID-19, admit a patient or provide other treatment. The ACR strongly urges caution in taking this approach. A normal chest CT does not mean a person does not have COVID-19 infection - and an abnormal CT is not specific for COVID-19 diagnosis. A normal CT should not dissuade a patient from being quarantined or provided other clinically indicated treatment when otherwise medically appropriate” [5].
There is minimal utility in obtaining a chest X-ray in the early stages of an acute lower tract infection except to exclude other etiologies of dyspnea. However, early chest X-rays (0-2 days within symptom onset) tend to be normal or demonstrate increased bronchovascular markings [1]. Later stages of the disease tend to be less specific for COVID-19 as secondary complications may look more like pneumonia than a typical viral infection and the role for serial chest X-rays appears to have more utility in establishing a baseline to assess improvement of aeration and ascertain the locations of tubes and lines in the intensive care unit.
Chest CT has some findings that appear common across multiple cases of COVID-19 and are similar to SARS-CoV-1. The most common findings described include patchy subsegmental GGO with peripheral and bilateral distributions which do not spare the periphery. Consolidative airspace disease occurs in later phases of the infection [6]. Crazy-paving is also associated with the disease, representing regions of interlobular and intralobular septal thickening. Airway and bronchovascular thickening can be seen in both early and later stages with later stage features evolving to bronchiectasis and potentially traction bronchiectasis. While some of the features may overlap stages depending on the patient's comorbidities, there are 4 stages of the disease to consider in recognizing the pattern of disease associated with COVID-19 (Table 1) [7].
Table 1.
The 4 stages of COVID-19
| Early/initial stage (0-4 days) |
| Progressive stage (5-8 days) |
| Peak stage (10-13 days) |
| Absorption stage (≥14 days) |
The early/initial stage (0-4 days) demonstrates the previously described and most well-recognized features of COVID-19 infection, consisting of peripherally-based GGOs without subpleural sparing as in our case (Fig. 3). Alternatively, as mentioned in the ACR's statement, this stage can have a normal CT chest appearance. Some features that are not usually present in early examples of COVID-19 include pleural effusions, cavitary airspace disease, typical tree-in-bud opacities, pneumothorax, or thoracic lymphadenopathy. However, many of these features can be seen in later stages of the disease as secondary complications.
The progressive stage of the disease (5-8 days) demonstrates an increased amount of GGO relative to the early phase. These opacities can be distributed in a bilateral, multifocal, and multilobular pattern with poorly defined boundaries. There is vascular thickening and associated intralobular septal thickening “crazy paving pattern,” as noted in the case report (Figs. 6 and 9b).
The peak stage (10-13 days) includes consolidation and can include secondary complications of the disease. This phase can have an even less specific pattern. For example, 1 study found a pattern similar to organizing pneumonia, previously referred to as cryptogenic organizing pneumonia, appeared in this late stage [8]. Organizing pneumonia, while idiopathic in etiology, can resemble many types of pneumonia with bilateral, peripherally based patchy alveolar airspace opacities and a “reverse halo” sign in which a GGO is surrounded by denser crescentic or ring shape consolidation [9].
The hallmark of the absorption stage (≥14 days) was improved aeration of the lungs with resolving features of “crazy paving,” continued resolution of GGO, and parenchymal bands. Additionally, there may be changes of fibrosis found at this stage. In 2004, after SARS-CoV-1, postmortem histological examinations revealed that there were features of diffuse alveolar damage in all patients, pronounced pulmonary edema, and hyaline membrane formation. Changes of fibrosis, including focal honeycombing fibrosis, were also found in what would now be considered the progressive stages, peak stages, and absorption stages [10]. However, the role that fibrosis plays in prognostication has been controversial. For example, 1 study suggested that patients with fibrous stripes and lesions are forming these during healing and that fibrosis could indicate stabilization. Another study suggested that fibrosis could indicate a poor outcome in the case of SARS-CoV-2 (COVID-19) and, when seen in earlier stages, could imply an impending progression to the peak stage [11].
In summary, this case demonstrates some of the most common imaging findings in early and progressive stage COVID-19 infection. It also highlights the necessity of recognizing the patterns of COVID-19 infection in the early phase if presented with that opportunity. The management implications for identifying common features of viral pneumonia are becoming more clear. Further, it is not entirely unprecedented for radiologists to need to be this specific about an organism on imaging as the accurate diagnosis of tuberculosis carries a similar importance. However, tuberculosis is not as common and it is possible that this will be considered the tuberculosis of this generation of radiologists. One of the most common arguments for not utilizing CT chest for this diagnosis remains the nonspecific features of COVID-19 suggesting the overlap with other peripherally based airspace patterns such as organizing pneumonia. However, at the time of this submission, the chest CT is one of the primary tools used for diagnosis of symptomatic COVID-19 infection along with rRT-PCR and clinical symptoms. It seems practical that identifying and documenting the pertinent negatives of viral pneumonia well enough to suspect COVID-19 infection will remain an important role for the radiologist. Additionally, patients may have comorbidities that can decrease the specificity of chest CT for COVID-19, but this appears to represent a time where advanced cooperation between the radiologist and clinician is one of the most important factors in ascertaining an accurate diagnosis.
Given the controversial role the radiologist plays in diagnosis of COVID-19, future consideration should include the use of artificial intelligence and deep learning. Deep learning algorithms have already shown some success in rapidly identifying patterns associated with this infection via the COVID-19 detection neural network (COVNet) [12]. Additionally, at the time of this submission, there is an ACR Data Science Institute use case for artificial intelligence algorithms which addresses the pertinent findings of COVID-19. The ACR Data Science Institute use cases are created by radiologists and are meant to be used as open-source guidelines for data scientists who wish to design neural network architecture to identify features or patterns of radiographic pathology [13].
Footnotes
Acknowledgments: Healthcare workers involved in the care of this patient.
Competing interest: None.
References
- 1.Cao A.M., Choy J.P., Mohanakrishnan L.N., Bain R.F., van Driel M.L. Chest radiographs for acute lower respiratory tract infections. Cochrane Database Sys Rev. 2013;(12) doi: 10.1002/14651858.CD009119.pub2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464822/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. https://www.nejm.org/doi/full/10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y., Xia L. Coronavirus Disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020 doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 5.“American College of Radiology, ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection.” Am Coll Radiol, 2020. www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection.
- 6.Kong W., Agarwal P. Chest imaging appearance of COVID-19 infection. Radiol Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200028. https://pubs.rsna.org/doi/10.1148/ryct.2020200028 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan F., Ye T., Sun P., Gui S., Liang B., Lingli L. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. Published online February 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins J. Cryptogenic organizing pneumonia. In: Stern Eric J., editor. Chest radiology, the essentials. 3rd ed. Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 10.Tse G.M.K., To K.F., Chan P.K.S., Lo A.W.I., Ng K.-C., Wu A. Pulmonary pathological features in coronavirus associated severe acute respiratory syndrome (SARS) J Clin Pathol. 2004;57:260–265. doi: 10.1136/jcp.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li L, Qin L, Xu Z, Yin Y, Wang X, Kong B. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200905. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stern EJ, Bernheim A, Chung M. COVID-19 compatible chest CT pattern. Am Coll Radiol, 2020. www.acrdsi.org/DSI-Services/Define-AI/Use-Cases/COVID-19-Compatible-Chest-CT-Pattern.