Abstract
ABSTRACT Objective: To describe responses of Chinese elderly living in Edmonton, Canada, during the severe acute respiratory syndrome (SARS) pandemic, and their use of Western and/or traditional Chinese medicine.
Design: A QUAL‐qual mixed method design, using grounded theory as the core method and ethnographic strategies are used to inform the cultural aspects of the study.
Sample: A purposeful sample of 19 Chinese elderly was interviewed and tape recorded. Four traditional Chinese Practitioners were also interviewed.
Methods: The interviews were transcribed and analyzed in Chinese and later translated into English. Data analysis utilized the constant comparison method.
Results: Participants experienced a 5‐stage process of protecting self, family, and others, responding according to the perceived threat of SARS. Participants used both Western and traditional Chinese strategies to combat SARS. Their desire to protect others took precedence under the moral code of filial piety. Once SARS was under control, the community remained vigilant and continued to monitor for its possible reoccurrence.
Conclusions: Cultural beliefs and practices within the Chinese population support the recommendations set by the health department for the protection of individuals and the community during the SARS pandemic. Therefore, the public health sector should become familiar with and support these Chinese cultural networks during pandemics.
Keywords: Chinese elderly, filial piety, SARS, severe acute respiratory syndrome, traditional Chinese medicine
In February 2003, the severe acute respiratory syndrome (SARS) epidemic occurred worldwide, and by March it had become a reality in Canada. The disease threatened the entire country and primarily affected the Chinese communities in Toronto. Medical and epidemiological research on infectious diseases including SARS generally focused on the identification of the pathogens (Drosten et al., 2003), understanding of its mode of transmission (Ksiazek et al., 2003; Peiris, Yuen, Osterhaus, & Stöhr, 2003) and the spread, treatment, and the clinical course of the disease (Lee et al., 2003). The causative agent for SARS is now confirmed to be a novel coronavirus and the predominant mode of its transmission is speculated to be large droplets or close or direct contact (Seto et al., 2003; Varia et al., 2003). To date, there is still no definitive treatment for SARS as its pathogenesis is still under investigation (Booth et al., 2003; Ho, 2003). Because of the speed of transmission with air travel, even though there were no diagnosed cases of SARS reported in Edmonton, Alberta, Canada, it is important to understand how communities responded and what preventive and protective strategies they used to combat SARS and to control the spread of the disease. This information may be incorporated into program to prevent uncontrolled pandemics in the future.
SARS first originated in the Province of Guangdong in southern China in November 2002 and remained isolated there until February 21, 2003 (Christian et al., 2004) when a physician from Guangdong became ill while visiting Hong Kong (Tsang et al., 2003). This physician became the index patient and infected 11 others staying in the same hotel. These index patients in turn carried SARS to Vietnam, Singapore, Ireland, Canada, and the United States (Wenzel & Edmond, 2003). The World Health Organization (WHO) declared SARS an evolving epidemic with 3,169 confirmed cases and 144 deaths (WHO, 2003) with a reported mortality rate of 4.9% (Wenzel & Edmond, 2003). SARS was reported and confirmed in Canada early March 2003 (Naylor, Chantler, & Griffiths, 2004) in five members of a multigenerational family of Chinese descent living in Toronto (Poutanen et al., 2003). The Canadian index patient stayed on the same floor at the same hotel as the index patient from Hong Kong. She was managed at home by her family doctor after she developed flu‐like symptoms and she died 3 days later. This patient's son who lived in the same house was admitted to hospital with pneumonia‐like symptoms, and he later died of multiorgan failure with a retrospective diagnosis of SARS (Poutanen et al., 2003). This was the first wave of SARS infection, in which five patients and almost 100 health care professionals were infected in three different hospitals in the Greater Toronto Area. The second wave of SARS infection in Canada occurred between April and June 2003 with a reported 74 cases of SARS at the North York General Hospital, which resulted in 90 confirmed SARS cases and more than 9,000 affected (Loutfy et al., 2004). These two epidemic waves of SARS resulted in a total of 251 probable and 187 suspected SARS cases and 43 deaths in Canada (St. John et al., 2005).
As patients with SARS were not immediately recognized and isolated on admission and no protective and preventive measures were implemented to control its spread, the majority of those affected by SARS in Canada were health care professionals (Donnelly et al., 2003; Wang & Jolly, 2003). This further establishes the importance of utilizing appropriate preventive and protective strategies against SARS, and is particularly important in the elderly population because the mortality for individuals above 65 years of age has been estimated at 55% worldwide (Donnelly et al., 2003).
Thus, the purpose of this study is to document the response of the Chinese elderly in Edmonton, Alberta, Canada, and to consider their views on SARS contagion from the perspective of traditional Chinese medicine (TCM). The Centre for Disease Control & Prevention in China has classified SARS as a type of Wan Bing ( ) (febrile diseases) in TCM, based on the similarities of the two diseases, and the existence of Wan Bing (
) (febrile diseases) in TCM, based on the similarities of the two diseases, and the existence of Wan Bing ( ) can be traced back 500 years (Hsu et al., 2006). Thus, TCM practitioners classified SARS as a reemerging disease, and the use of Chinese medicine to manage pandemics and epidemics has been documented in traditional Chinese medical textbooks for more than 1,800 years (Hsu et al., 2006).
) can be traced back 500 years (Hsu et al., 2006). Thus, TCM practitioners classified SARS as a reemerging disease, and the use of Chinese medicine to manage pandemics and epidemics has been documented in traditional Chinese medical textbooks for more than 1,800 years (Hsu et al., 2006).
Four studies on the effects of SARS in the Chinese elderly have been published. One studied factors influencing the practice of preventive behaviors among Chinese elderly (Tang & Wong, 2005) and the other investigated the level of knowledge and prevention against SARS among a group of elderly Chinese living in a nursing home in Hong Kong (Tse, Pun, & Benzie, 2003). Both studies involved interviewing a group of Chinese elderly to elicit their knowledge of SARS and their use of strategies against the disease. Tang and Wong (2005) reported that elderly who perceived greater vulnerability to SARS and those with a lower education level had more confidence in the health authority and were more likely to adopt the recommended strategies against SARS. Tse et al. (2003) did not investigate the type of strategies utilized by these elderly, and reported that the knowledge base of these elderly was extremely limited. Of the remaining two studies, Kong et al. (2003) addressed the importance of prevention and early diagnosis of SARS in the elderly population. Kong and his colleagues discussed the difficulties of diagnosing SARS in the elderly population and stressed the need to maintain proper surveillance strategies in the communities. Chung (2003) reported that Chinese elderly who lived alone and those with chronic diseases were more worried about contracting SARS. The majority of elderly in her study were fearful of becoming victims to SARS, and this fear was compounded by uncertainty.
In this study our aim was to generate a grounded theory describing the responses of Chinese elderly living in Edmonton to the threat of SARS. We asked:
-
1
What Western and or traditional Chinese strategies were used by the elderly Chinese to prevent and to protect themselves and others against SARS?
-
2
What was the rationale for the use of the different types of strategies?
-
3
Do the strategies used by the Chinese elderly vary according to the phases of the SARS epidemic?
Methods
Design
In this study, we used a QUAL‐qual mixed method design (Morse, 2003) using grounded theory to describe the process of Chinese elderly responding to the threat of SARS and ethnographic strategies were incorporated to elicit supplemental information about the cultural aspects of the phenomenon. The study was approved by the university's ethics board and permission was obtained from the various community organizations before conducting the research.
Sample
The study was conducted in a nursing home for Chinese elders, a Chinese multicultural organization, a Chinese seniors' lodge, and a Baptist church frequented by Chinese elderly. All four organizations were situated in or close to Edmonton Chinatown, and all organizations were meeting places for many Edmonton Chinese elderly. To elicit support of these institutions, the first author met with the managers and different groups of Chinese elderly in the three organizations to explain the purposes of the study and invited them to participate. Informed consent was obtained from all participants before data collection. Demographic data were obtained and included age, gender, marital status, a brief medical history, current medications, religious beliefs, recent travel to Hong Kong or other SARS‐infected countries. Further, the researchers ensured that participation was voluntary by ensuring that the participants had adequate time to ask questions. To ensure anonymity, each participant was assigned a number on the demographic data collection tool, the cassette tapes, and the transcripts. Only the investigators had access to the tapes and demographic data. Interviews were conducted either in participants' homes or in a room provided by one of the participating organizations.
A total of 19 participants were interviewed. Among the 19 participants, 8 lived with their children, 7 lived with their spouses, 2 lived in a nursing home, and 2 lived alone. The researcher also interviewed four traditional Chinese practitioners (three from Edmonton and one from Hong Kong) to elicit their understanding of the contagion of SARS and their views on protection and treatment of the disease from the perspective of TCM.
Data collection
After consent was obtained, the researcher approached the topic of investigation by asking the following statement: “Tell me what happened when you first heard of SARS,” and later focused the interview on more specific questions. The subsequent questions enabled the participants to elaborate on and clarify their experiences for protecting against and preventing SARS. All the interviews were audio‐taped and conducted by the first author in Cantonese (her first language and that of all the participants). The average time for interviews was approximately 1 hr. Elderly participants were asked to tell about their experiences during the SARS epidemic. They generally began to relate their stories from the time they first learned of SARS and continued to sequentially relate to the present time.
Examples of questions asked of the traditional Chinese practitioners were: “Why was the term che qi ( ) (evil air) used to explain SARS according to TCM?” and “What is the cause of diseases in TCM in relation to the seven emotions?” This information was vital, as their explanations on the cause of SARS and the use of herbs to prevent and treat the disease were important to aid the researcher in the understanding of the use of specific strategies pertaining to TCM among the participants.
) (evil air) used to explain SARS according to TCM?” and “What is the cause of diseases in TCM in relation to the seven emotions?” This information was vital, as their explanations on the cause of SARS and the use of herbs to prevent and treat the disease were important to aid the researcher in the understanding of the use of specific strategies pertaining to TCM among the participants.
Data analysis
Grounded theory data analysis occurred simultaneously with data collection. The interviews were initially transcribed and analyzed in Chinese and later translated into English. This was to ensure accuracy of data analysis without the loss of cultural meaning. The first author also provided the closest possible English definitions for specific terms used by the participants to describe their experiences with the threat of SARS. The constant comparison method was used to compare incidents within the transcripts. Using this method, incidents were compared and patterns identified until a core variable was identified. Initially, open coding using vivo codes in the participants' words were assigned to the data. These codes were later clustered into categories and the researcher described how the different categories related to each other. Once the core variable was identified, the researcher continued to code data around the core variable to develop a parsimonious theory that could be used to explain how the Chinese elderly protect and prevent SARS.
Results
In qualitative research, the recruitment of participants continues until no new data is obtained from the interviews in this case. The sample consisted of 13 female and 6 male Chinese elderly residing in Edmonton Chinatown, and their ages ranged from 65 to 90 years.
A five‐stage model describing the process of using preventive and protective strategies SARS by the Chinese elderly emerged from the data (see Figure 1).
Figure 1.
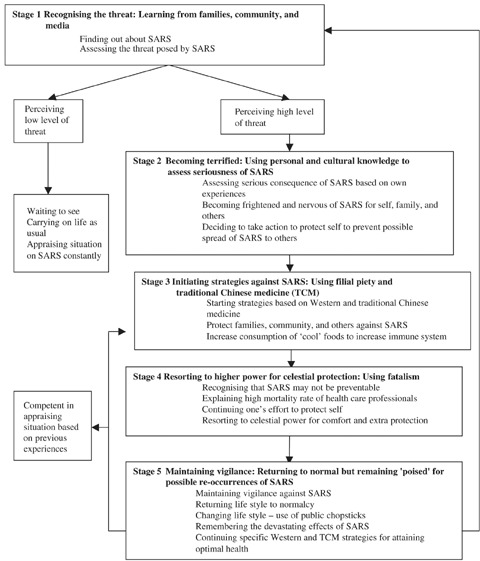
The Process of Protecting Against Severe Acute Respiratory Syndrome
Stage 1: Recognizing the threat: Learning from families, community, and media
All participants were aware of the SARS epidemic and its threat before the disease occurred in Canada. The primary source of information was the Edmonton community's Chinese newspapers, which are available free of charge. Individuals with compromised eyesight and those who were not able to read because of illiteracy chose to listen to the Chinese news on the radio. The Chinese media provided all the participants with information about SARS, but Chinese elderly with family members living in Hong Kong and/or China called their family regularly to get the latest developments on the SARS crisis, although their main reason for calling was to make sure that family members living in the affected areas were all right.
Also, many of the elderly still have relatives and family members living in Hong Kong, China and Taiwan and they were worried about their safety there. I know many of them will call their family members who live in those countries and ask about the condition and situation regarding SARS over there and to make sure they are safe.
Participants who belonged to specific community associations such as the Toishanese Women's Association and those who spent time at the multicultural center received news about SARS from other members of the associations who had recently returned from China or Hong Kong. Therefore, through the media and their association with various Chinese organizations, all the participants learned about the SARS crisis.
Besides the newspaper, I learned about SARS from friends at the Toishanese Women's Association as they told me that there was such incidence. We met regularly and talked about the latest happenings in Toishan and China.
None of the participants felt threatened by SARS initially as there were no confirmed cases in Canada, and they took comfort in the geographic distance between countries afflicted with SARS and Canada. They were not worried about SARS at the onset of the epidemic, as expressed in the following:
I personally did not do anything at first. I was in Canada and there was no need to be afraid or worried as there were no cases of SARS here at that time and we are so far away from Hong Kong and China.
Stage 2: Becoming terrified: Using personal and cultural knowledge to assess seriousness of SARS
Once cases of SARS were identified in Canada, participants in the study became terrified of the disease and were concerned about the risk of contracting SARS. The fear intensified when the high rate of infectivity among health care professionals who had donned full protective clothing against SARS became known. Participants began to assess the threat and seriousness of SARS by referring to their own experiences with other infectious diseases such as smallpox, tuberculosis, and AIDS.
My grandmother had smallpox and my mother still visited her at that time, it was a very long time ago … but it was not as dangerous as SARS. The doctors knew how to treat smallpox and they knew the cause for it as well. SARS was different, nothing was known and nothing was sure.
I think SARS was more serious and dangerous than other infectious diseases because people who contracted it could die very quickly. AIDS and TB were also infectious but they were treatable. SARS was more fatal than any other infectious diseases that I had previously experienced.
Participants began to feel frightened when the routes of transmission were unknown and the first case of SARS was identified in Toronto in an elderly Chinese woman recently returned from Hong Kong. They were nervous about SARS for self, family, and others, and began to recognize their vulnerability with SARS spreading quickly in Toronto, as the high mortality rate among the elderly group (close to 55%) became known. In particular, participants visiting Hong Kong at the time of the SARS crisis reported increased vulnerability to SARS, because Hong Kong was one of the epicentres of SARS outside of Mainland China. All participants became more worried about contracting SARS and then spreading to their families and others in the communities. The threat perceived by the participants and the fear of spreading the disease to family and others was more intense in individuals living with family members and in those living in the Chinese Elders' Mansions.
I am not afraid of contracting SARS because I am old and have lived my life the best way I could. … If I contracted SARS, I would not like my children to come and see me … I would like all my children to be safe and well. I do not want to infect them or others with the disease, as I would not be able to live with myself.
People were all scared of getting SARS in public places. I did not just think about myself. I am old and I really am not afraid of getting SARS, but I did not want to spread it to my son and the family.
Regardless of the level of perceived threat of SARS, all participants decided to take an active role in protecting themselves against SARS, as none of them were willing to be responsible for infecting others with SARS. They felt it was their obligation and moral duty to protect their family members and the community.
Stage 3: Initiating strategies against SARS: Using filial piety and traditional Chinese medicine (TCM)
SARS was now a reality in Canada, and even though there were still no confirmed cases in Edmonton, the participants had decided to initiate strategies to fend off the disease. The participants were all willing to learn strategies against SARS, and were aware of the strategies recommended by the regional health authority. The media were the participants' main source of information, and strategies against SARS were broadcast by the Chinese radio stations and printed in newspapers published by the Edmonton Chinese community. During this time, the regional health authority began issuing pamphlets in English and Chinese listing the symptoms of SARS and recommended strategies against the disease to all businesses and institutions around Chinatown. These strategies included the use of masks, proper hand washing, maintaining personal hygiene, and avoidance of crowded places. Participants who had been in Hong Kong during the SARS outbreak all wore masks when they went out because it was recommended by the Health Department, but individuals also felt the pressure from the community to adhere to the practice.
People would wear a mask when they went out of the house basically, as it was strongly advised by the Health Department, so everyone listened and no one went out without a mask at that time. I guess you do not dare to go out without a mask, as everyone wears one so if you do not have one on, people will look at you in a strange way and of course stay clear of you as well. There was pressure I say to wear a mask when going out.
Besides learning about Western strategies against SARS, the Chinese elderly were knowledgeable about the use of strategies stemming from TCM. These strategies were mainly preventive in nature, including the use of herbs and special foods and exercise regimes such as qi gong and tai chi. Participants also revived the use of public chopsticks when dining out or when having guests over for dinner.
Well, we use kung fai (
) (public chopsticks) before but the outbreak of SARS really scared everyone. So, we thought it was a good idea to use them (meaning public chopsticks) again to protect others and ourselves against the SARS virus.
Other strategies utilized by the participants included avoiding crowded places (especially areas frequented by Chinese), meticulous hand washing, regular cleaning schedules, and isolation. These strategies were initiated on an individual basis. Institutions in Edmonton Chinatown such as restaurants, the multicultural center, and churches frequented by large number of Chinese also implemented their own regulations to protect residents, including restricting visitation, increased cleanliness, and closely monitoring the health of residents.
The most important thing was to pay attention to what you ate, as your health depends on the food that you eat and I believe what she [participant's friend] said. At that time I did not go to places where there were too many people and I stayed away from Chinatown. I was very careful with personal cleanliness and washed my hands more frequently.
At the beginning of the SARS epidemics, the management team here was very nervous and the cleaning staffs were cleaning all the time—they clean the corridors and the grounds around the gardens at least twice a day. They would clean the inside of the apartment buildings especially the doors and inside the elevators.
All participants utilized special foods to combat SARS, based on their belief that the SARS virus preferred the yang ( ) (hot) environment. Consumption of “cool” foods or herbs rich in ying (
) (hot) environment. Consumption of “cool” foods or herbs rich in ying ( ) (cool) constituents would render the body less appropriate for the SARS virus to duplicate. Special herbs were recommended by the universities in Hong Kong, and recipes using the herb ban lan gen (
) (cool) constituents would render the body less appropriate for the SARS virus to duplicate. Special herbs were recommended by the universities in Hong Kong, and recipes using the herb ban lan gen ( ) (Isatis indigotica) were printed in Chinese newspapers and discussed on radio and television programs. For this specific herb, many participants seek advice from traditional Chinese doctors, who are consulted regarding safety of use before using such herbs. S. Tse (personal communication, August 21, 2003) expressed the importance of seeking advice before starting ban lan gen (
) (Isatis indigotica) were printed in Chinese newspapers and discussed on radio and television programs. For this specific herb, many participants seek advice from traditional Chinese doctors, who are consulted regarding safety of use before using such herbs. S. Tse (personal communication, August 21, 2003) expressed the importance of seeking advice before starting ban lan gen ( ) (Isatis indigotica), which is liang (
) (Isatis indigotica), which is liang ( ) or cool in nature.
) or cool in nature.
Well, we already drink teas such as sugar cane, mua gun (
) [a “cold” Chinese herb] but I have never tried ban lan gen (
). The Chinese herbalist in Hong Kong recommended this herb to me, I heard of this by reading the newspaper and talking to others. I thought I was already taking the liang cha (
) [“cold tea”] and that should be enough.
I did not know but I know many people took the herbal tea—ban lan gen (
) for preventing SARS; they boiled the herbs to drink. I also boiled and included the Philippine maid; everyone drank it and the friends of my daughter. Everyone drank as the other might infect you; they said it was for prevention. … People said they were good so I boiled them to drink, I asked the chung yi (
) [“traditional Chinese doctor] and he said it was OK.
The use of special foods was more popular, and all participants were making soups with special ingredients that would render them more resistant to the SARS virus.
Well, during the SARS epidemic, I boiled kam gan fa (
) [a Chinese herb that aims at clearing the heat in the body, considered “cool” in nature] and boiled liang (
) soups, like soups made from fan guo [a type of Chinese gourd] and lentils regularly and I think it is also an effective preventive way against SARS as well people told me. … Well, these soups aim to rid of the heat and rid of the poison inside the body, like green bean. I would also boil the green bean soup dessert during the summer.
In addition to consuming herbs and foods recommended by friends and professionals, the Chinese elderly also engaged in regular exercises such as swimming, tai chi and qi gong. These activities all aimed to put the individual in the best position to combat against SARS. Participants believed these strategies boosted one's immune system and increased the body's ability to fight against the disease.
I go swimming every day with my neighbors. We start at 06:30 in the morning and will come home around 10:00. I have been doing this for the past 5 years and I feel great. It is necessary for me to have a schedule, some kind of routine. This will help to keep my immune system strong.
However, isolation was considered the ultimate protective strategy, and all four participants returned from Hong Kong underwent self‐imposed isolation, even though WHO had declared Hong Kong SARS‐free and there was no need to practice isolation.
When I returned to Canada, it was already the end of July. Hong Kong had been declared SARS‐free by the WHO by then so I did not have to go into isolation for two weeks. I think it was a good thing that people coming from an infected country to isolate as I believe it was the only thing that would stop the spread of the disease.
The family and community played a major role in ensuring that individuals returning from a SARS‐infected country stayed away from others. Notices were posted and distributed to all individuals in churches, nursing homes, and senior apartment buildings.
Yeah, the management knows. People are asked to isolate themselves for at least 10 days after returning from Hong Kong. Everyone knows each other and they will monitor and make sure people are isolated when they returned from HK and other areas that are infected with SARS.
Participants observed all strategies used to protect and prevent SARS, and in turn they also acted to monitor to ensure that everyone was doing their part to prevent the spread of the disease. The main purpose of protecting themselves against SARS was to ensure that SARS would not spread to family members and others in the community. To the participants this is an issue of morality: that no one should do harm to others. None was willing to take the responsibility to harm people, whether it was intentional or unintentional.
Stage 4: Resorting to higher power for comfort and extra protection: Learning to accept one's fate
The Chinese elders proceeded to Stage 4 when they felt that they had done everything within their power in avoiding contracting SARS but there was still a chance for them to get the disease. The participants then resorted to fatalism and praying to higher powers for extra protection against SARS for themselves. They also utilized fatalism to explain the deaths of health care professionals who died from SARS.
In Hong Kong, it appears that most who died from SARS were the elderly and the younger people contracted it through direct contact like the health care professionals. So, this is about meng wen (
) [“destiny”], whether you believe or not meng wen (
) has its own arrangement. It is not possible for human to understand the tragedy … but people must learn to accept what had happened and move on, it is difficult to make sense, people would just say if bad things happen to decent people, why? No one knows it is the person's meng wen (
).
Praying and taking refuge in deities for extra protection against SARS was accepted by all participants because of the serious consequences of the disease. However, they concurred that individuals must adhere to the recommendations of the Health Departments to protect themselves against SARS.
The participants were aware that taking all recommended strategies and praying might not prevent an individual from contracting SARS. The participants had to resort to fatalism and a lack of luck to explain why previously young and healthy health care professionals contracted and succumbed to the disease.
But if you really contracted the disease, you can only consider yourself dao mei (
) [“unlucky”]. However, if you are dai ming (
) [“big life”], then you will be cured of the disease.
In this sense, participants agreed that believing and praying to higher powers did not guarantee that one would be protected from SARS. However, in the participants' minds, doing good deeds results in accumulating one's credit, which might help to protect an individual from harm.
Stage 5: Maintaining vigilance: Returning to normal but remaining “poised” for possible recurrence of SARS
The final stage of the model signifies the participants' attempt to normalize their lives when SARS was under control. The threat of SARS was no longer imminent and the participants were trying to resume their lives as before. However, they were aware of the need to remain vigilant and ready to initiate all strategies in case the epidemic returned.
I continue to pour bleach into the kitchen sink for disinfectant after I came back. I think it is a good idea to keep it clean and to kill germs as you just do not know. I feel that it is good so I continue to do it now. I do not do it every day like I did in Hong Kong, just once a week here, it's enough, it's enough, I think.
So, the only solution for people is that we should not say that because SARS did not occur here that it is guaranteed that it will not happen here. Having no cases in Edmonton does not mean that it will never happen, no cases means that we are lucky and that we need to make sure we pay attention and attend to hygiene. So, this is very important to keep one's hands clean. I intend to continue with this from now on with or without the threat of SARS.
The Chinese elderly continued to engage in preventive strategies aimed at improving and maintaining their immune systems to provide them a better chance to fight diseases including SARS. During this final stage, the participants tried to return their lives to normal, and all of them had established some changes to their routines because of the SARS outbreak.
Everything is back to normal. I went to yum cha (
) [“drink tea,” another term for dim sum] once a week. I rinsed all the cups and bowls with hot water. He said that he likes to see others and so I let him go. So, we go once a week to the restaurant to eat and that was what we have done before the SARS outbreak.
The participants became more conscientious about personal hygiene, cleanliness became a priority, and all employed the use of public chopsticks more often. They also placed the family and community first and said that it was important and that they would continue to observe the necessary strategies to keep SARS out.
I think everyone should continue to be clean and make sure the public areas are kept clean by not throwing garbage into the street and spitting as these will certainly spread diseases around. One needs to think of the community and to make sure that the best is done for oneself and others at the same time.
Discussion
The emergence of SARS in 2003 caused tremendous hardships worldwide. With no definitive cures available and a high mortality rate in individuals over the age of 60, knowledge of SARS and the use of preventive and protective strategies against the disease among the elderly are vital to controlling the spread of SARS.
All the participants in this study were extremely knowledgeable about the SARS epidemic and were aware of the recommended strategies to prevent the disease. This was in contrast to findings by Tse et al. (2003), in which Chinese elderly residing in a Hong Kong nursing home were less knowledgeable of SARS, and were not aware of the different strategies they could use to protect themselves against the disease despite access to media reports. One possible explanation is that the elderly in the study of Tse et al. resided in a nursing home, and they trusted the staff to take appropriate action to fend off SARS. They believed that they were taken care of, and that there was no need for them to know the details of strategies against SARS.
The participants in this Edmonton study, however, chose to adopt a proactive role, and were strongly influenced by filial piety to doing no harm to their families, their communities, and society. Fifteen of the 19 participants in this study lived with either their children or their spouses, and these living arrangements prompted them to take the responsibility to protect their family members by learning everything about protection and prevention against SARS. Further, the concept of filial piety goes beyond the obligation of showing respect to one's parents. It is seen as an ethical principle that directs one's interpersonal relationships toward one's family and others in the community. In this case, filial piety suggested the “right and humane” way to act toward one's family and others in the community, and guided the Chinese elderly in their use of strategies against SARS. Therefore, filial piety was two‐tiered: what is expected of the participants at a personal level (to protect their families) and at a societal level (to undergo voluntary isolation upon return from Hong Kong). These actions were understandable because of the serious consequences of contracting SARS. There is no question that the use of protective and preventive strategies against SARS among Chinese elderly was clearly driven and influenced by filial piety, and that concept was central to this study. The Chinese elderly were so frightened of spreading SARS to their families and others that they took all effort to make sure they would not spread the disease, as they would not be able to live with themselves. In addition to using Confucianism, participants utilized fatalism and destiny to explain the unexplainable events. This provided explanation and comfort to the participants to explain the deaths of health care professionals. Participants were all proactive and engaged in all strategies against SARS, but enlisted extra protection from deities at the same time. Their main concerns were for the well being of family and community, and these were the motives behind the initiation of all protective and preventive strategies against SARS.
It has been shown that the extent of use of strategies against SARS was influenced by the stage of the epidemic. When the epidemic was at its peak, the participants would use recommended strategies for both protection and prevention of SARS, but the stress was on protective strategies, which included the use of masks, frequent hand washing, and avoiding areas frequented by Chinese.
Participants also employed traditional beliefs about food to increase immunity against diseases including SARS. The use of food is influenced by TCM, where foods are categorized either ying ( ) (cool) or yang (
) (cool) or yang ( ) (hot) class based on the food constituents. This explained the consumption of liang (
) (hot) class based on the food constituents. This explained the consumption of liang ( ) (cool) foods by the participants during the SARS outbreak, as it was believed that SARS virus proliferated more rapidly under the yang (
) (cool) foods by the participants during the SARS outbreak, as it was believed that SARS virus proliferated more rapidly under the yang ( ) (hot) body system. There were also differences on the types of herbs used by the participants. Those who were in Hong Kong during the SARS outbreak consumed ban lan gen (
) (hot) body system. There were also differences on the types of herbs used by the participants. Those who were in Hong Kong during the SARS outbreak consumed ban lan gen ( ) (Isatis indigotica), a herb that is considered extremely liang (
) (Isatis indigotica), a herb that is considered extremely liang ( ) (cool) in nature. Ban lan gen (
) (cool) in nature. Ban lan gen ( ) (Isatis indigotica) was recommended by traditional Chinese practitioners in Hong Kong (Leung, 2004; Leung & Ooi, 2003) for the prevention of SARS. However, individuals who were in Edmonton used herbs that were less liang (
) (Isatis indigotica) was recommended by traditional Chinese practitioners in Hong Kong (Leung, 2004; Leung & Ooi, 2003) for the prevention of SARS. However, individuals who were in Edmonton used herbs that were less liang ( ) (cool) in nature such as chrysanthemum and kam gan fa (
) (cool) in nature such as chrysanthemum and kam gan fa ( ), because ban lan gen (
), because ban lan gen ( ) (Isatis indigotica) might not be suitable for everyone. The use of different types of herbs is based on the knowledge of contagion of SARS as a type of Wan Bing (
) (Isatis indigotica) might not be suitable for everyone. The use of different types of herbs is based on the knowledge of contagion of SARS as a type of Wan Bing ( ) (febrile disease) from the TCM perspective. SARS was considered a reemerging disease that often occurred during (cusp) seasonal changes with extreme weather. Although the use of herbal medicines was recommended by TCM practitioners for the prevention of SARS, only participants who were in Hong Kong at the time of the epidemics actually consumed them. All other participants in the study consumed foods that possessed cooling effects and that were believed to place the body in a better position to fight the disease. The consumption of herbs or foods by the participants depended entirely on whether or not they had been abroad in a SARS‐infected country. The use of herbs was discussed with TCM practitioners, and this again reflected participants' concern about the benefits and risks of the use of herbs versus the use of food for prevention of diseases including SARS. Knowledge about the use of herbs and food to prevent diseases had been culturally acquired by these Chinese elders. They were not able to explain how they attained the knowledge, but tended to believe that it was part of their experience when they were growing up. Participants were knowledgeable about the use of both Western and TCM strategies against SARS, based on the recommendations of the various health authorities and their own knowledge of food therapy. Participants' use of both Western and TCM strategies was a course of action aimed at putting themselves in the best position to combat the disease.
) (febrile disease) from the TCM perspective. SARS was considered a reemerging disease that often occurred during (cusp) seasonal changes with extreme weather. Although the use of herbal medicines was recommended by TCM practitioners for the prevention of SARS, only participants who were in Hong Kong at the time of the epidemics actually consumed them. All other participants in the study consumed foods that possessed cooling effects and that were believed to place the body in a better position to fight the disease. The consumption of herbs or foods by the participants depended entirely on whether or not they had been abroad in a SARS‐infected country. The use of herbs was discussed with TCM practitioners, and this again reflected participants' concern about the benefits and risks of the use of herbs versus the use of food for prevention of diseases including SARS. Knowledge about the use of herbs and food to prevent diseases had been culturally acquired by these Chinese elders. They were not able to explain how they attained the knowledge, but tended to believe that it was part of their experience when they were growing up. Participants were knowledgeable about the use of both Western and TCM strategies against SARS, based on the recommendations of the various health authorities and their own knowledge of food therapy. Participants' use of both Western and TCM strategies was a course of action aimed at putting themselves in the best position to combat the disease.
The use of “public chopsticks” as a protective strategy against SARS applied to dining out or when there were guests coming to dinner. Public chopsticks are equivalent to serving spoons in Western culture. Generally, public chopsticks are not employed when dining with members of a family. These chopsticks are expected at restaurants and ensure a certain level of hygienic practice to prevent cross‐contamination among individuals.
Components in the model of Protecting Self, Family, and Others could be confirmed in other research, and the findings could be used in the context of prevention and protection of other infectious diseases. SARS has no definitive treatment to date, making protection and prevention the main canon to controlling this disease. Increased understanding of the behaviors of minority groups in response to the threat of SARS would be beneficial for health care professionals planning interventions for these groups. Thus, one of the major implications of this study is for health authorities to consider integrating traditional beliefs and strategies into the fight against infectious diseases including SARS.
This study was conducted with a very specific group of Chinese elders in Edmonton. All participants in this study received support from either their immediate families or from church groups and associations to which they belonged. These Chinese elderly lived by themselves, with their children, or in the Seniors' Lodge, and they had few or no financial concerns. The findings of this study reflected the Chinese values of filial piety and responsibilities toward family, community, and society, and the use of TCM. This study group has resided in Canada for one generation, and the applicability of the findings would vary according to the level of acculturation of Chinese families and community, with the level of adherence to these traditional values changing over time.
The importance of prevention of infectious diseases has gained recognition in recent years with the SARS outbreak in 2003 and the threat of an avian influenza (H5N1) pandemic predicted by WHO (2006). Scientists and government agencies such as WHO and CDC have put forth their recommendations on how to manage H5N1 in event of an outbreak. Preparedness plans for avian influenza generally involve the public sector, with the medical sector taking the lead. The plan is often a top‐down approach, and usually does not include individual efforts to fend off diseases nor consider cultural systems used to resist the spread of disease.
We have identified a model that explains the behaviors and the use of protective and preventive strategies by Chinese elderly faced with a serious disease, using SARS as an example. While this study only included a small group of Chinese elderly living in Edmonton, the cultural patterning of their behavior, including the use of traditional Chinese strategies that incorporate cultural beliefs, suggests that these behaviors were widespread. In addition, supplemental strategies recommended by Western medicine were also deployed by the elderly. Thus, this study increases our understanding of Chinese elders' use of protective and preventive strategies against SARS, an area that had been almost unexplored.
Health care professionals should take into consideration the cultural beliefs of individual minority groups. With respect to the threat of H5N1, it is our hope that this study may stimulate further research into the use of other traditional beliefs and practices to combat diseases by studying the responses of other cultural groups to the threat of infectious disease. In particular, public health nurses should explore the cultural components of minority groups to better understand and support the use of additional disease prevention strategies based on the health beliefs of these groups. Understanding the contagion of diseases from the individual's cultural perspective is vital if one is to provide education about the use of specific strategies in preventing the spread of diseases. Strategies recommended by health authorities must be congruent with the health beliefs of the minority group in order to encourage adherence to protocols for control of infectious diseases in the future. We trust that this study exemplifies the importance of incorporating culture as a means of revealing and interpreting responses to an urgent and immediate threat to health. A comparative study involving Chinese elderly from different countries would be valuable, as factors affecting the use of strategies against SARS and similar infectious diseases may differ in other regions.
Acknowledgments
The authors thank Dr. Anne Neufeld and Dr. Norah Keating for their contributions. This research was taken from the first author's dissertation conducted as part of the requirements for the doctoral degree.
References
- Booth, C. M. , Matukas, L. M. , Tomlinson, G. A. , Rachlis, A. R. , Rose, D. B. , Dwosh, H. A. , et al (2003). Clinical features and short term outcomes of 144 patients with SARS in the greater Toronto area. Journal of American Medical Association, 289 (21), 2801–2809. [DOI] [PubMed] [Google Scholar]
- Christian, M. D. , Loutfy, M. , McDonald, G. , Martinez, K. F. , Ofner, M. , Wong, T. , et al (2004). Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerging Infectious Disease, 10 (2), 287–293. Retrieved May 13, 2004, from http://www.cdc.gov/ncidod/EID/vol10no2/03-0700.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, J. C. C. (2003). How do older people react to severe acute respiratory syndrome? Journal of the American Geriatrics Society, 51 (8), 1183–1184. [DOI] [PubMed] [Google Scholar]
- Donnelly, C. A. , Ghani, A. C. , Leung, G. M. , Hedley, A. J. , Fraser, C. , Riley, S. , et al (2003). Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet, 361 (9371), 1761–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drosten, C. , Gunther, S. , Preiser, W. , Van der Werf, S. , Brodt, H.‐R. , Becker, S. , et al (2003). Identifications of a novel coronavirus in patients with severe acute respiratory syndrome. New England Journal of Medicine, 348 (20), 1967–1976. [DOI] [PubMed] [Google Scholar]
- Ho, W. (2003). Guidelines on management of severe acute respiratory syndrome (SARS). Lancet, 361 (9371), 1313–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, C.‐H. , Hwang, K.‐C. , Chao, C.‐L. , Chang, S. G. N. , Ho, M.‐S. , & Chou, P. (2006). Can herbal medicine assist against Avian flu? Learning from the experience of using supplementary treatment with Chinese medicine on SARS or SARS‐like infectious disease in 2003. The Journal of Alternative and Complementary Medicine, 12 (6), 505–506. [DOI] [PubMed] [Google Scholar]
- Kong, T. K. , Dai, D. L. K. , Leung, M. F. , Au, S. Y. , Yung, R. , & Chan, M. H. (2003). Severe acute respiratory syndrome (SARS) in elders. Journal of the American Geriatrics Society, 51 (8), 1182–1183. [DOI] [PubMed] [Google Scholar]
- Ksiazek, T. G. , Erdman, D. , Goldsmith, C. S. , Zaki, S. R. , Peret, T. , Emery, S. , et al (2003). A novel coronoavirus associated severe acute respiratory syndrome. New England Journal of Medicine, 348 (20), 1953–1966. [DOI] [PubMed] [Google Scholar]
- Lee, N. , Hui, D. , Wu, A. , Chan, P. , Cameron, P. , Joynt, G. , et al (2003). A major outbreak of severe acute respiratory syndrome in Hong Kong. New England Journal of Medicine, 348 (20), 1986–1994. [DOI] [PubMed] [Google Scholar]
- Leung, P. C. (2004). Herbal medicine and atypical pneumonia. Unpublished manuscript.
- Leung, P. C. , & Ooi, E. E. (2003). SARS war: Combating the disease. Singapore: World Scientific Publishing Co. Ltd. [Google Scholar]
- Loutfy, M. R. , Wallington, T. , Rutledge, T. R. , Mederski, B. , Rose, K. , Kwolek, S. , et al (2004). Hospital preparedness and SARS. Emerging Infectious Disease, 10 (5), 771–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse, J. M. (2003). Principles of mixed method and multi‐method research design In Teddlie C., & Tashakkori A. (Eds.), Handbook of mixed methods in social and behavioural research (pp. 189–208). London: Sage Publications. [Google Scholar]
- Naylor, C. D. , Chantler, C. , & Griffiths, S. (2004). Learning from SARS in Hong Kong and Toronto. Journal of American Medical Association, 29 (20), 2483–2487. [DOI] [PubMed] [Google Scholar]
- Peiris, J. S. M ., Yuen, K. Y. , Osterhaus, A. D. M. E ., & Stöhr, K. (2003). The severe acute respiratory syndrome. New England Journal of Medicine, 349 (25), 2431–2441. [DOI] [PubMed] [Google Scholar]
- Poutanen, S. M. , Low, D. , Henry, B. , Finkelstein, S. , Rose, D. , Green, K. , et al (2003). Identification of severe acute respiratory syndrome in Canada. New England Journal of Medicine, 348 (20), 1995–2005. [DOI] [PubMed] [Google Scholar]
- Seto, W. H. , Tsang, D. , Yung, R. W. H. , Ching, T. Y. , Ng, T. K. , Ho, M. , et al (2003). Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet, 361 (9368), 1519–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. John, R. K. , King, A. , De Jong, D. , Bodie‐Collins, M. , Squires, S. G. , & Tam, T. W. S. (2005). Border screening for SARS. Emerging Infectious Disease, 11 (1), 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, C. S. , & Wong, C. (2005). Psychosocial factors influencing the practice of preventive behaviors against severe acute respiratory syndrome among older Chinese in Hong Kong. Journal of Aging and Health, 17 (4), 490–506. [DOI] [PubMed] [Google Scholar]
- Tsang, K. W. , Ho, P. L. , Ooi, G. C. , Yee, W. K. , Wang, T. , Chan‐Yeung, M. , et al (2003). A cluster of cases of severe acute respiratory syndrome in Hong Kong. New England Journal of Medicine, 348 (20), 1977–1985. [DOI] [PubMed] [Google Scholar]
- Tse, M. M. , Pun, S. P. , & Benzie, I. I. (2003). Experiencing SARS: Perspectives of the elderly residents and health care professionals in a Hong Kong nursing home. Geriatric Nursing, 24 (5), 266–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varia, M. , Wilson, S. , Sarwal, S. , McGeer, A. , Gournis, E. , Galanis, E. , et al (2003). Investigation of a nosocomial outbreak of severe acute respiratory syndrome (SARS) in Toronto, Canada. Canadian Medical Association Journal, 169 (4), 285–292. [PMC free article] [PubMed] [Google Scholar]
- Wang, M.‐D. , & Jolly, A. M. (2003). Changing virulence of the SARS virus: The epidemiological evidence. Bulletin of the World Health Organization, 82 (7), 547–549. [PMC free article] [PubMed] [Google Scholar]
- Wenzel, R. P. , & Edmond, M. B. (2003). Managing SARS amidst uncertainty. New England Journal of Medicine, 348 (20), 1947–1948. [DOI] [PubMed] [Google Scholar]
- World Health Organization [WHO]. (2003). Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Retrieved March 2, 2004, from http://who.int/csr/sars/country/table2004_04_21/en/index.html
- World Health Organization [WHO]. (2006). WHO activities in avian influenza and pandemic influenza preparedness from January to December 2006. Retrieved July 2, 2007, from http://www.who.int/csr/disease/avian_influenza/WHOactivitiesavianinfluenza/en/index.html


