Abstract
Data on the efficacy of corticosteroids on respiratory picornavirus‐induced wheezing are limited. To determine whether prednisolone is effective in rhinovirus‐ or enterovirus‐induced recurrent wheezing, we conducted a controlled trial comparing oral prednisolone (2 mg/kg/day in three divided doses for 3 days) with placebo in hospitalized wheezing children and studied post hoc virus‐specific efficacy in early wheezing (<3 episodes, reported elsewhere) and in recurrent wheezing (≥3 episodes). Virus‐negative children where excluded. Our primary endpoint was the time until children were ready for discharge. Secondary endpoints included oxygen saturation and exhaled nitric oxide during hospitalization, duration of symptoms, blood eosinophil count, and impulse oscillometry 2 wk after discharge, and occurrence of relapses during the following 2 months. Virus‐specific effects were analyzed with interaction analysis in a multivariate regression model. During the study period, 661 patients were hospitalized, 293 randomized, and 59 were accepted in this analysis (mean age 2.6 yr, s.d. 1.3). Prednisolone did not significantly decrease the time until ready for discharge in all patients (prednisolone vs. placebo, medians, 18 vs. 24 h, p = 0.11). However, prednisolone decreased the time until ready for discharge in children with picornavirus infection (respectively, 12 vs. 24 h, p = 0.0022) and more specifically, in children with enterovirus infection (6 vs. 35 h, p = 0.0007). In the secondary endpoints, prednisolone decreased the duration of cough and dyspnea in rhinovirus‐affected children (p = 0.033 for both). Prospectively designed clinical trial is needed to test the hypothesis that prednisolone reduces symptoms in picornavirus‐affected wheezing children.
Keywords: asthma, child, enterovirus, prednisolone, rhinovirus, recurrent wheezing
Viral infection is detected in up to 88% of wheezing children (1, 2, 3). Corticosteroids are generally used in the treatment of wheezing. Whether the efficacy of systemic corticosteroid in childhood wheezing is dependent on the viral etiology has not been fully studied. In respiratory syncytial virus (RSV)‐induced wheezing in infants, nevertheless, it seems clear that systemic corticosteroid treatment with standard dosages is not effective (4, 5, 6, 7). Only mechanically ventilated infants suffering from RSV bronchiolitis may benefit from these agents (8, 9).
The efficacy studies focusing on viruses other than RSV have been scarce. As most exacerbations of pediatric asthma are related to respiratory picornavirus (i.e., rhinovirus or enterovirus) infections, and systemic corticosteroids are effective in children with acute asthma, these agents can be expected to be efficacious in wheezing induced by these viruses (1, 2, 3, 10). There is also indirect evidence available in early wheezing that certain children aged less than 3 yr, probably those suffering from non‐RSV infection, may benefit from these drugs (11, 12, 13). Furthermore, we have demonstrated that standard dose of prednisolone reduced relapses during a 2‐month period in early wheezing (1st or 2nd episode of wheezing in <3‐yr‐old children) associated with rhinovirus infection and/or blood eosinophils ≥0.2 × 109/l (14). Our study has been the only rhinovirus‐specific efficacy study in children to date. The effectiveness of prednisolone in rhinovirus‐induced wheezing is interesting, because early wheezing associated with rhinovirus has been shown to be the strongest predictor of subsequent third‐year wheezing and has even been related with school‐aged asthma (15, 16).
No virus‐specific efficacy studies are yet available on children suffering from recurrent wheezing or asthma. Here, we report the second post hoc analysis of our efficacy study, which focuses on the efficacy of prednisolone in the treatment of viral‐induced episode of recurrent wheezing (≥3 episodes of wheezing) or acute asthma in children aged less than 7 yr. Our main hypothesis was that the efficacy of prednisolone is associated with viral etiology. We expected prednisolone to be effective in acute wheezing induced by respiratory picornavirus infection.
Methods
Subjects
Children aged from 3 months to 16 yr, admitted to the Department of Pediatrics of Turku University Hospital between September 1, 2000 and May 31, 2002 for acute wheezing, were considered for the study (Fig. 1). The methods have been described in detail earlier (14, 17). Pre‐defined exclusion criteria were systemic corticosteroid treatment in the preceding 4 wk, chronic disease (other than asthma or allergy), severe wheezing necessitating intensive care unit treatment or previous participation in this study. For this analysis, we also excluded children with less than two previous wheezing attacks, as we wanted to focus on recurrent wheezing. In addition, a few children aged ≥7 yr were excluded to narrow down the age distribution. As in our previous report, we wanted to focus only on virus‐positive children. Atopy was defined as positive immunoglobulin E antibodies against common allergens (18). All asthma diagnoses fulfilled the criteria suggested by National Heart, Lung, and Blood Institute, USA (19). The study protocol was approved by the Ethics Committee of the Turku University Hospital, and written informed consents were obtained from the parents before commencing the study.
Figure 1.
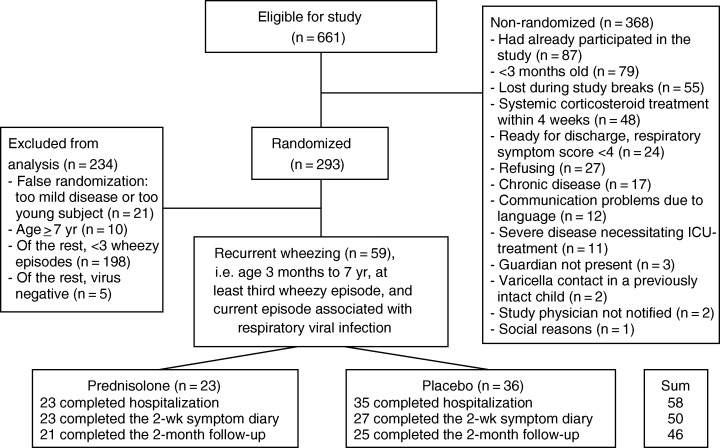
Study flow chart.
Study design
The need for hospitalization was decided independent of the study by an on‐duty physician in the emergency room. In the ward, the eligible children were randomly assigned in a double‐blind fashion to receive either oral prednisolone (first dose 2 mg/kg, then 2 mg/kg/d in three divided doses for 3 days, maximum dose 60 mg/d, Prednisolon® 5 mg tablets, Leiras, Finland) or placebo after informed consent had been obtained. All patients received nebulized salbutamol 0.15 mg/kg (maximum single dose 5.0 mg) at 2 h intervals for the first 12 h, then at 4 h intervals while in the hospital. After discharge, β 2‐agonists were used on demand. During hospitalization, the patients received antibiotics (n = 29) or nebulized racemic epinephrine (n = 5) on demand. No other medication was used.
The study physicians (T.J. and P.L.) examined the patients on study entry and twice daily thereafter during their hospital stay and scored the respiratory symptoms. After the child's discharge, the guardian recorded the child's symptoms in a diary for 2 wk, which was followed by a follow‐up visit. After 2 months, the parents were contacted by phone to record any relapses necessitating a visit to a physician or hospitalization.
Outcome measures
Pre‐specified primary endpoint was the time until ready for discharge, which was defined as a duration of respiratory symptoms score >3 during hospital stay. The respiratory symptoms score, which was assessed every 12 h during hospitalization, is a summed score for the degree of dyspnea (0 = none, 1 = mild, 2 = moderate, 3 = severe), type of breathing (0 = normal, 1 =use of stomach muscles, 2 = use of intercostal muscles, 3 = nasal flaring), severity of auscultatory findings on wheezing (0 = none, 1 = expiratory, 2 = inspiratory and expiratory, 3 =audible without stethoscope), and assessment of expiratory:inspiratory time (0 = 1:2, 1 = 1:1, 2 = 2:1, 3 = 3:1). An estimation of 6 h was used for the last 12‐h period between hospital assessments, i.e., the period during which the patient became ready for discharge. Pre‐specified secondary endpoints were oxygen saturation and exhaled nitric oxide during hospital stay, wheeze and cough during 2 wk after discharge, impulse oscillometry with bronchodilation 2 wk after discharge, blood eosinophil counts at discharge and 2 wk later, and readmission to the out‐patient clinic or hospital for recurrent wheezing during a 2‐month period after discharge.
Sample collection and analysis
On admission, nasopharyngeal aspirates were obtained. Viral analyses were performed for rhinovirus, enteroviruses, RSV, adenovirus, influenza A and B viruses, parainfluenza virus types 1–4, coronavirus (strains OC43, 229, and NL63), and human metapneumovirus (14, 17). Blood samples for eosinophil analyses were collected on entry, and as described above, and analyzed according to the standard clinical routine in the Central Laboratory, Turku University Hospital, Turku, Finland. Exhaled NO was successfully collected with the tidal breathing offline collection procedure from 46 children (36 children with picornavirus and 10 with other virus infection on entry) according to the recommendations of the American Thoracic Society before randomization at the ward and analyzed in the Department of Clinical Physiology, Turku University Hospital (Sievers 280, Nitric Oxide Analyzer; Sievers Instruments Inc., Boulder, CO, USA) (14). Triple measurements of respiratory resistance (Rrs) at 5, 20, and 35 Hz were performed according to normal clinical protocol of our hospital (Master Screen IOS, Erich Jaeger GmbH, Würzburg, Germany) (20). Measurements were repeated after inhalation of 300 μg salbutamol.
Statistics
To allow detection of an 18 h difference (half the average duration of stay in our hospital) in the time until ready for discharge between the prednisolone‐treated group and the placebo groups (with an estimated standard deviation of 24 h) and to maintain an alpha error of 0.05 and a beta error of 0.20, the required size of the sample was 27 children for each treatment group (5). The normality of data distribution was tested using the Kolmogorov–Smirnov test. The t‐test or Mann–Whitney U test was used for continuous variables. Categorical data were analyzed using the chi‐square test or Fischer's exact test. The efficacy of prednisolone was analyzed using multivariate regression analysis (generalized linear model) with backward stepwise elimination model using negative binominal distribution and log‐link. The model included the study drug, age, atopic disease, blood eosinophil count at entry, duration of preceding respiratory symptoms, viral etiology (picornaviruses and RSV), and antibiotic treatment, i.e., the variables in which baseline difference was found between prednisolone and placebo groups or between picornavirus and non‐picornavirus groups. Interpretation of generalized linear model is carried out using the concept of risk ratio (RR), which means how much risk changes when an independent variable (if continuous) changes by one unit. In categorical explanatory variables, RR tells how great risk is in one group when compared with another group. Interaction between study drug and picornavirus, rhinovirus, or enterovirus positivity, blood eosinophil count on entry, presence of atopy, age, and severity of symptoms were also tested, i.e., one interaction in each model. E.g., the drug*picornavirus interaction term in the model refers to estimated differences in the drug effect in the picornavirus and non‐picornavirus groups. Furthermore, to estimate the drug effect in certain patient groups, e.g., in picornavirus and non‐picornavirus groups, contrast estimates were formulated to test the effect of the drug in each group. The effects of prednisolone on oxygen saturation and exhaled nitric oxide during the first 48 h of hospital stay were tested at 12 h intervals using the repeated measurements analysis of variance. Statistical significance was established at a p value lower than 0.05. The statistical analyses were carried out using SAS/STAT(r) software, Version 9.1.3 SP3 of the SAS System for Windows, SAS Institute Inc., Cary, NC, USA.
Results
Characteristics of the children
During the study period, 661 children were hospitalized. Of these, 293 were randomized to receive prednisolone or placebo (Fig. 1). Of the 293 randomized children, 59 children were accepted for the analysis. The included children were 5 months to 6.1 yr old, had their ≥3rd wheezing episode, and confirmed respiratory viral infection. There was one drop‐out during hospitalization. Of the 58 children, who completed hospitalization, enterovirus was detected in 21 (36%) cases, rhinovirus in 20 (34%) cases, non‐typable rhino‐or enterovirus in 9 (16%) cases, RSV in 10 (17%) cases, adenovirus in 7 (12%) cases, parainfluenza virus type 1–4 in 3 (5%) cases, influenza A or B virus in 3 (5%) cases, coronavirus in 1 (2%) case, and metapneumovirus in 1 (2%) case. Mixed viral infection was detected in 17 (29%) cases.
Of these 58 children, 5 (9%) children were 5–12 month old, 33 (57%) children were 12–35 month old, and 20 (34%) children were 36 months to 6.1 yr old. Thirty children (52%) were atopic, and 25 children (44%) had asthma.
Children positive for respiratory picornavirus (i.e., rhinovirus or enterovirus) were more often atopic [picornavirus group vs. other virus group, 29/48 (60%) vs. 1/10 (10%), p = 0.0048], were more often sensitized to aeroallergens [respectively, 17/48 (35%) vs. 0/10 (0%), p = 0.0026], and had larger numbers of blood eosinophils on entry to the study [respectively, mean (SD), 0.63 (0.46) vs. 0.30 (0.20) × 109/l, p = 0.0015] than those positive for other viruses. Longer duration of preceding respiratory symptoms [respectively, mean (SD), 2.8 (2.3) vs. 8.4 (3.9) days, p < 0.001], antibiotic treatments [respectively, 20/48 (42%) vs. 9/10 (90%), p = 0.012], and detection of RSV [respectively, 4/48 (8%) vs. 6/10 (60%), p = 0.0008] were more common in the other virus group than in the picornavirus group. Otherwise, no differences were found between the virus groups in the variables mentioned in the 1, 2 (data not shown for different virus groups).
Table 1.
Patient characteristics in prednisolone and placebo groups
| Factor | Prednisolone (n = 23) | Placebo (n = 35) | p‐value |
|---|---|---|---|
| Age, years | 2.1 (1.1) | 2.9 (1.4) | 0.020 |
| Male, no. | 16 (70%) | 22 (63%) | 0.60 |
| Atopic, no. | 9 (39%) | 21 (60%) | 0.12 |
| Aeroallergen sensitization, no. | 7 (30%) | 10 (29%) | 0.88 |
| Asthma, no. | 10/22 (45%) | 15 (43%) | 0.85 |
| Wheezy episodes, no. | 4.6 (2.1) | 4.7 (2.1) | 0.79 |
| ICS at study entry, no. | 7 (30%) | 7 (20%) | 0.36 |
| ICS started/continued after discharge, no. | 12 (52%) | 16/32 (50%) | 0.87 |
| ICS started/continued 2 wk after discharge, no. | 17 (74%) | 22/32 (69%) | 0.68 |
| Parental asthma, no. | 7/22 (32%) | 10/34 (29%) | 0.85 |
| Parental allergy, no. | 13/22 (59%) | 18/34 (53%) | 0.65 |
| Previous cough, days | 2.3 (2.8) | 3.0 (3.0) | 0.35 |
| Previous wheezing, days | 1.9 (1.1) | 1.4 (0.7) | 0.31 |
ICS, inhaled corticosteroid.
Values are means (s.d.), unless otherwise noted. Analysis using t‐test or chi‐square test.
Table 2.
Patient status, laboratory data, and medication at study entry in prednisolone and placebo groups
| Factor | Prednisolone (n = 23) | Placebo (n = 35) | p‐value |
|---|---|---|---|
| RSS, points† | 6.8 (1.6) | 6.6 (1.8) | 0.67 |
| O2‐saturation,% | 95.5 (2.1) | 95.1 (2.3) | 0.51 |
| Acute otitis media, no. | 9 (39%) | 15/34 (44%) | 0.71 |
| Blood eosinophils, ×109/l | 0.43 (0.57) | 0.49 (0.36) | 0.90 |
| Exhaled nitric oxide, ppb* | 5.9 (4.0–7.8) | 6.2 (4.9–11.4) | 0.22 |
| Rhinovirus, no. | 7 (30%) | 13 (37%) | 0.60 |
| Enteroviruses, no. | 9 (39%) | 12/32 (38%) | 0.90 |
| Nontypable rhino‐ or enterovirus, no. | 3 (13%) | 6 (17%) | 1.00 |
| Respiratory syncytial virus, no. | 5 (22%) | 5 (14%) | 0.50 |
| Adenovirus, no. | 2 (9%) | 5 (14%) | 0.69 |
| Parainfluenza virus types 1–4, no. | 1 (4%) | 2 (6%) | 1.00 |
| Influenza A or B virus, no. | 1/22 (5%) | 2 (6%) | 1.00 |
| Coronavirus. no. | 1 (4%) | 0 (0%) | 0.40 |
| Metapneumovirus, no. | 1 (4%) | 0 (0%) | 0.40 |
| Mixed viral infection, no. | 7 (30%) | 10 (29%) | 0.88 |
| Albuterol at ER, mg/kg | 0.31 (0.24) | 0.25 (0.21) | 0.35 |
| Antibiotic treatment, no.‡ | 11 (48%) | 18 (52%) | 0.79 |
| Amoxicillin, no. | 5 (22%) | 12/34 (35%) | 0.27 |
| Amoxicillin + clavulanic acid, no. | 1 (4%) | 2/34 (6%) | 1.00 |
| Ceftriaxone, no. | 3 (13%) | 0/34 (0%) | 0.061 |
| Macrolide, no. | 1 (4%) | 2/34 (6%) | 1.00 |
| Sulfa + trimetoprim, no. | 0 (0%) | 1/34 (3%) | 1.00 |
| Nitrofurantoin, no. | 1 (4%) | 0/34 (0%) | 0.40 |
ER, emergency room (before entry to the study).
Values are means (s.d.) or medians (interquartile range), unless otherwise noted. Analysis using t‐test, Mann–Whitney U test, chi‐square test, or Fischer's exact test when appropriate.
†Respiratory symptoms scores (RSS) were assessed on a scale from 0 (none) to 12 (severe).
*n = 20 for prednisolone group and n = 26 for placebo group.
‡Name of the antibiotic not available from one case. Antibiotics were administrated with standard dosages orally, except ceftriaxone with single dose 50 mg/kg i.m., maximum dose 500 mg, for those who could not take antibiotics orally.
When the baseline values of the treatment groups were compared, we found that the children in the prednisolone group were younger (p = 0.020) than those in the placebo group (Table 1). Otherwise, no differences were recorded in baseline characteristics between the prednisolone group and the placebo group (1, 2). In 26 children with successful impulse oscillometry, no difference in age was found between the treatment groups (prednisolone vs. placebo, means, 3.6 vs. 2.9 yr, p = 0.12).
Efficacy of prednisolone
In the univariate regression analysis, study drug was not associated with our primary endpoint, the time until ready for discharge (Table 3). However, significant interactions between study drug and age and picornavirus infection were found in the main endpoint. In secondary endpoints, prednisolone decreased blood eosinophil count at discharge in all patients. A significant interaction between study drug and rhinovirus infection was found in the duration of symptoms after discharge.
Table 3.
Univariate analysis of effects of prednisolone for primary and secondary outcomes
| Outcome | n | p‐values for prednisolone vs. placebo in all patients and for interactions between study drug and different variables | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All patients | Age | Atopy | B‐eos | Picornavirus | Rhinovirus | Enterovirus | RSS at entry* | ||
| Time until ready for discharge, h | 58 | 0.71 | 0.034 | 0.15 | 0.73 | 0.026 | 0.050 | 0.0002 | 0.20 |
| Duration of cough, days | 50 | 0.12 | 0.97 | 0.091 | 0.079 | 0.93 | 0.033 | 0.28 | 0.40 |
| Duration of dyspnea, days | 50 | 0.61 | 0.80 | 0.057 | 0.42 | 0.24 | 0.019 | 0.50 | 0.96 |
| Outpatient visit, no.† | 46 | 0.99 | 0.82 | 0.77 | 0.83 | 0.94 | 0.92 | 0.79 | 0.77 |
| Rehospitalized, no.† | 46 | 0.89 | 0.94 | 0.84 | 0.90 | 0.98 | 0.89 | 0.86 | 0.87 |
| B‐eos at discharge, ×109/l | 53 | <0.0001 | 0.71 | 0.80 | 0.22 | 0.79 | 0.72 | 0.60 | 0.41 |
| B‐eos 2 wk after discharge, ×109/l | 52 | 0.24 | 0.45 | 0.91 | 0.33 | 0.76 | 0.24 | 0.74 | 0.51 |
B‐Eos, blood eosinophils.
Values are medians (interquartile range) or number of subjects (%). Analysis using multivariate regression analysis.
*Respiratory symptoms scores (RSS) were assessed on a scale from 0 (none) to 12 (severe) at study entry.
†As a result of wheezing during 2 months after discharge.
In the step‐wise multivariate regression analysis, prednisolone did not significantly decrease our primary endpoint, the time until ready for discharge (prednisolone vs. placebo, medians, 18 vs. 24 h, p = 0.11, final model included study drug, antibiotic treatment, picornavirus infection, Table 4). However, prednisolone decreased the time until ready for discharge in children with respiratory picornavirus infection (respectively, 12 vs. 24 h for picornavirus group and 54 vs. 6 h for non‐picornavirus group, p = 0.0022 for interaction, final model included study drug, picornavirus infection, RSV‐infection, study drug*picornavirus infection; in picornavirus group, RR 1.91, 95% CI 1.22–3.00, p = 0.0048; in non‐picornavirus group, RR 0.30, 95% CI 0.11–0.82, p = 0.019) and more specifically, in children with enterovirus infection (respectively, 6 vs. 35 h for enterovirus group and 30 vs. 18 h for non‐enterovirus group, p = 0.0007 for interaction, final model included study drug, enterovirus infection, picornavirus infection, antibiotic treatment, study drug*enterovirus infection; in enterovirus group, RR 3.75, 95% CI 1.99–7.08, p < 0.0001; in non‐enterovirus group, RR 0.84, 95% CI 0.50–1.39, p = 0.49).
Table 4.
Multivariate analysis of effects of prednisolone for primary and secondary outcomes
| Outcome | n | Int. | All patients | p‐value | Interactions between study drug and viral groups | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rhinovirus | p‐value | Enterovirus | p‐value | |||||||
| Yes | No. | Yes | No | |||||||
| Time until ready for discharge, h | 58 | Pred. | 18 (6–34) | 0.11 | 6 (6–30) | 21 (6–42) | 0.37 | 6 (6–18) | 30 (6–42) | 0.0007* |
| Pl. | 24 (6–42) | 28 (18–54) | 21 (6–39) | 35 (21–58) | 18 (6–30) | |||||
| Duration of cough, days | 50 | Pred. | 5 (2–9) | 0.26 | 2 (0–7) | 6 (4–10) | 0.033† | 6 (5–11) | 4 (2–7) | 0.10 |
| Pl. | 7 (4 to13) | 10 (4–13) | 7 (3–12) | 7 (4–14) | 8 (4–12) | |||||
| Duration of dyspnea, days | 50 | Pred. | 2 (0–4) | 0.61 | 0 (0–2) | 4 (0–5) | 0.033‡ | 2 (0–2) | 3 (0–4) | 0.89 |
| Pl. | 2 (0–4) | 2 (0–4) | 2 (0–3) | 3 (0–4) | 1 (0–3) | |||||
| Outpatient visit, no.§ | 46 | Pred. | 3/21 (14%) | 0.61 | 1/5 (20%) | 2/16 (13%) | 0.99 | 2/9 (22%) | 1/12 (8%) | 0.49 |
| Pl. | 5/25 (20%) | 2/8 (25%) | 3/17 (18%) | 4/11 (36%) | 1/14 (7%) | |||||
| Rehospitalized, no.§ | 46 | Pred. | 2/21 (10%) | 0.79 | 0/5 (0%) | 2/17 (12%) | 0.97 | 2/9 (22%) | 0/12 (0%) | 0.97 |
| Pl. | 3/25 (12%) | 1/8 (13%) | 2/17 (12%) | 2/11 (18%) | 1/14 (7%) | |||||
| B‐eos at discharge, ×109/l | 53 | Pred. | 0.00 (0.00–0.10) | <0.0001¶ | 0.00 (0.00–0.10) | 0.00 (0.00–0.10) | 0.52 | 0.050 (0.00–0.10) | 0.00 (0.00–0.10) | 0.16 |
| Pl. | 0.50 (0.30–0.80) | 0.40 (0.30–0.50) | 0.70 (0.50–1.2) | 0.70 (0.50–1.20) | 0.40 (0.20–0.80) | |||||
| B‐eos 2 wk after discharge, ×109/l | 52 | Pred. | 0.45 (0.30–0.70) | 0.084 | 0.50 (0.60–0.70) | 0.40 (0.20–1.30) | 0.94 | 0.85 (0.40–1.30) | 0.40 (0.30–0.60) | 0.23 |
| Pl. | 0.30 (0.30–0.50) | 0.30 (0.20–0.35) | 0.40 (0.30–0.60) | 0.40 (0.30–0.70) | 0.30 (0.20–0.50) | |||||
Int., intervention; B‐Eos, blood eosinophils; pred., prednisolone; pl., placebo.
Values are medians (interquartile range) or number of subjects (%). Analysis using multivariate regression analysis.
*In enterovirus group, RR 3.75, 95% CI 1.99–7.08, p < 0.0001. In non‐enterovirus group, RR 0.84, 95% CI 0.50–1.39, p = 0.49.
†In rhinovirus group, RR 2.71, 95% CI 1.34–5.47, p = 0.0053. In non‐rhinovirus group, RR 1.06, 95% CI 0.67–1.68, p = 0.80.
‡In rhinovirus group, RR 4.31, 95% CI 1.12–16.64, p = 0.034. In non‐rhinovirus group, RR 0.77, 95% CI 0.33–1.78, p = 0.54.
§As a result of wheezing during 2 months after discharge.
¶RR 10.87, 95% CI 3.84–30.78.
In the secondary endpoints, prednisolone decreased the duration of symptoms in rhinovirus‐affected children in the multivariate model (Table 4). In these children, prednisolone decreased the duration of cough (prednisolone vs. placebo, medians, 2 vs. 10 days for rhinovirus group and 6 vs. 7 days for non‐rhinovirus group, p = 0.033 for interaction, final model included study drug, rhinovirus infection, study drug*rhinovirus infection; in rhinovirus group, RR 2.71, 95% CI 1.34–5.47, p = 0.0053; in non‐rhinovirus group, RR 1.06, 95% CI 0.67–1.68, p = 0.80) and dyspnea (respectively, 0 vs. 2 days for rhinovirus group and 4 vs. 2 days for non‐rhinovirus group, p = 0.033 for interaction, final model included study drug, rhinovirus infection, age, study drug*rhinovirus infection; in rhinovirus group, RR 4.31, 95% CI 1.12–16.64, p =0.034; in non‐rhinovirus group, RR 0.77, 95% CI 0.33–1.78, p = 0.54). Prednisolone also decreased blood eosinophils at discharge in all children (respectively, 0.00 vs. 0.50 × 109/l, RR 10.87, 95% CI 3.84–30.78, p < 0.0001, final model included study drug). The effect was no longer present 2 wk after discharge. No other significant differences or interactions were found (data partly shown in Table 4).
The efficacy of prednisolone tended to be associated with atopy and increased blood eosinophil count. In atopic children, prednisolone tended to decrease the duration of cough [prednisolone vs. placebo, medians (interquartile range), 2 (2–7) vs. 9 (4–14) days for atopic and 6 (4–9) vs. 4 (3–12) days for non‐atopic children, p = 0.091 for interaction, final model included study drug, atopy, study drug*atopy and dyspnea [respectively, 0 (0–2) vs. 1 (0–3) days for atopic children and 4 (0–5) vs. 2 (0–4) days for non‐atopic children, p = 0.057 for interaction, final model included study drug, atopy, age, study drug*atopy]. In children with increased blood eosinophil count, prednisolone also tended to decrease the duration of cough [respectively, medians, 5 (4–6) vs. 7 (4–12) days for blood eosinophils ≥0.3 × 109/l and 7 (3–11) vs. 9 (4–13) days for blood eosinophils <0.3 × 109/l, p =0.079 for interaction, final model included study drug, blood eosinophils ≥0.3 × 109/l, study drug*blood eosinophils ≥0.3 × 109/l). The median was used as cut‐off point for blood eosinophils.
No differences were found in oxygen saturation or exhaled nitric oxide measurements during hospital stay between the treatment groups (respectively, repeated measurements analysis of variance, p = 0.53 and 0.77, data not shown). Neither differences were found in impulse oscillometry measurements 2 wk after discharge between the treatment groups [Rrs5, prednisolone vs. placebo, median (interquartile range), 1.27 (1.17–1.38) vs. 1.21 (1.05–1.31), p = 0.68; difference in Rrs5 after 0.3 mg salbutamol inhalation, −41% (−26% to −49%) vs. −25% (−10% to −41%), p = 0.87].
The prednisolone treatment was well tolerated. No clinically significant adverse effects occurred.
Discussion
We were not able to demonstrate a benefit of prednisolone treatment with standard dosages in children hospitalized for recurrent wheezing or acute asthma in any of our clinical endpoints. However, we demonstrated efficacy of the treatment in our primary outcome, the time until ready for discharge, in respiratory picornavirus‐associated episode of wheezing. We also found that prednisolone reduced the duration of cough and dyspnea in rhinovirus‐affected children. Prednisolone effectively decreased blood eosinophil count at discharge in all patients, but the effect was lost within 2 wk.
Efficacy studies focusing on natural respiratory picornavirus infections are difficult to design and conduct because of the delays in viral diagnosis, which necessitate inclusion of a large number of patients and subsequent analysis of the results. Although there are no other virus‐specific efficacy studies available in children suffering from recurrent wheezing or asthma, the efficacy of prednisolone in rhino‐ and enterovirus‐induced wheezing was what was to be expected on the basis of the high detection rate of respiratory picornaviruses in acute childhood asthma and separate studies showing the efficacy of systemic corticosteroids in this patient group (1, 3, 10). However, we were surprised by the finding that prednisolone also decreased the duration of hospitalization in picornavirus affected children because previous studies on pediatric asthma have had difficulties demonstrating it. A recent meta‐analysis of these studies have shown efficacy in the discharge rate at the first re‐examination in the outpatient ward, in the improvement of clinical severity scores, and in the number of relapses over 1–3 months after discharge, but not in the duration of hospitalization (10). The rapid resolution of wheezing (median of 18 h in our children) makes it difficult to demonstrate a decrease in hospitalization time. The negative clinical outcomes in all patients may be, thus, because of the different viral etiologies of illness, or in broader scope, because of the association of certain host characteristics with picornavirus infections.
There is evidence that certain children suffering from early wheezing, but not those with RSV infection, may benefit from systemic corticosteroids. Daugbjerg et al. (11) studied 123 wheezing children aged 1.5–18 months and found shorter duration of hospitalization in prednisolone than placebo group. Only 31% of children were RSV‐positive. Goebel et al. (12) studied 51 first‐time wheezers aged less than 2 yr and showed lower symptom scores in prednisolone group than in placebo group. Only 35% of children were RSV‐positive. Schuh et al. (13) showed marked effects with a single dose of dexamethasone in 70 first‐time wheezers aged 8 wk to 23 months in an emergency room setting. Half the number of children were RSV‐positive. More recently, a Finnish study showed shorter hospital stays and a shorter duration of symptoms in 230 wheezing children aged 6–35 months treated with prednisolone (21). Although no viral diagnostics were used in that study, many of the children were older than those typically infected by RSV. As RSV‐positive children have clearly not benefited from corticosteroids (4, 5, 6, 7) and rhinovirus has been detected in 20–40% and enteroviruses in 10–20% of the cases bronchiolitis cases (1, 2, 15, 22), these earlier studies support the view that systemic corticosteroids may be effective in respiratory picornavirus‐affected children. Finally, we have demonstrated in our earlier report that standard dose of prednisolone reduced relapses during a 2‐month period after first or second episode of wheezing associated with rhinovirus infection and/or blood eosinophils ≥0.2 × 109/l, but not with RSV infection, in 78 children aged 3–35 months (14). These previous studies on early wheezing are in agreement with the current report on recurrent wheezing.
The beneficial effects of systemic corticosteroids in acute childhood wheezing induced by respiratory picornaviruses are not supported by the studies on experimental rhinovirus infection in adults. In these studies, systemic, inhaled, or nasal corticosteroids administered to non‐atopic adults and atopic adults with mild asthma have not clearly reduced symptoms or airway responsiveness (23, 24, 25). We argue that the experimental infections in adults with mild asthma are not comparable to natural viral infection in children, especially to moderate‐to‐severe cases necessitating hospitalization. Children susceptible to rhinovirus‐induced moderate‐to‐severe wheezing may not just present a case of any viral illness. Instead, these cases may reveal children with underlying immunologic anomaly predisposing them to more severe outcome of rhinovirus infections (26, 27). We speculate that markedly elevated baseline eosinophil counts and higher prevalence of atopy found in rhinovirus‐affected children when compared with children affected by other viruses may also increase susceptibility for more severe diseases (14, 28). However, there was no significant interaction between the study drug and blood eosinophil count on entry, atopy, or age in the current study.
Systemic corticosteroids effectively decrease inflammatory markers, including blood eosinophils, in acute asthma, but the reports concerning the duration of this effect are limited. In asthmatic children, the eosinopenic effect has been reported to last at least 5 days after the discontinuation of a 5‐day treatment with prednisolone (29). In asthmatic adults, blood eosinophils have returned to baseline level 1 wk after a 12‐day treatment with prednisolone (30). In our study, no difference in eosinophil levels was found 2 wk after the prednisolone treatment. It appears that the eosinopenic effect of 3‐day course of prednisolone is lost within 2 wk. This is in agreement with our previous report on early wheezing (14).
Several limitations of this study must be taken into account. As a result of difficulties designing picornavirus‐specific studies in children, our analyses were carried out post hoc. The power calculation was based on RSV‐infection, because previous data on rhinovirus‐specific efficacy were not available. The final sample size was quite small, and it could account for some negative findings, e.g., the efficacy associated with atopy and increased blood eosinophils. Despite intensive search, the detection of other than respiratory picornavirus infections was low. It is the most likely reason for the prolonged time until ready for discharge in non‐picornavirus‐affected children receiving prednisolone when compared with placebo. The reliability of a positive PCR test in the detection of an active viral infection may be questioned (1). We have previously shown in our wheezing patients that cases of positive picornavirus PCR markedly decreased within 2–3 wk and disappeared within 5–6 wk after acute wheezing, suggesting that PCR positivity is related to acute infection (31). In the current study, viral load was not assessed. Balanced randomization was lost because of exclusion of many subjects before analysis. It should be noted that virus‐specific results come from various subgroup analyses and are only secondary outcomes. Finally, we studied only hospitalized children receiving abundant bronchodilating medication and excluded children requiring intensive care. The strengths of this study include careful recording of risk factors, detailed viral diagnostics, and prospective follow‐up.
In conclusion, our findings support the view that systemic corticosteroids in the dosages used are effective in children suffering from rhinovirus‐ or enterovirus‐induced episode of recurrent wheezing or asthma. In these patients, prednisolone treatment reduced the severity or the duration of the disease. Prospectively designed clinical trial, appropriately powered, is needed to test the hypothesis that prednisolone reduces symptoms in rhinovirus or enterovirus‐affected wheezing children.
Acknowledgments
This study was supported by the Academy of Finland, the Foundation for Pediatric Research, the Finnish Cultural Foundation, and the Paulo Foundation. Prednisolone and placebo were provided by Leiras Pharmaceuticals Inc., Turku, Finland.
References
- 1. Rakes GP, Arruda E, Ingram JM, et al. Rhinovirus and respiratory syncytial virus in wheezing children requiring emergency care. IgE and eosinophil analyses. Am J Respir Crit Care Med 1999: 159: 785–90. [DOI] [PubMed] [Google Scholar]
- 2. Papadopoulos NG, Moustaki M, Tsolia M, et al. Association of rhinovirus infection with increased disease severity in acute bronchiolitis. Am J Respir Crit Care Med 2002: 165: 1285–9. [DOI] [PubMed] [Google Scholar]
- 3. Rawlinson WD, Waliuzzaman Z, Carter IW, Belessis YC, Gilbert KM, Morton JR. Asthma exacerbations in children associated with rhinovirus but not human metapneumovirus infection. J Infect Dis 2003: 187: 1314–8. [DOI] [PubMed] [Google Scholar]
- 4. Roosevelt G, Sheehan K, Grupp Phelan J, Tanz RR, Listernick R. Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet 1996: 348: 292–5. [DOI] [PubMed] [Google Scholar]
- 5. De Boeck K, Van der Aa N, Van Lierde S, Corbeel L, Eeckels R. Respiratory syncytial virus bronchiolitis: a double‐blind dexamethasone efficacy study. J Pediatr 1997: 131: 919–21. [DOI] [PubMed] [Google Scholar]
- 6. Bülow SM, Nir M, Levin E, et al. Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics 1999: 104: e77. [DOI] [PubMed] [Google Scholar]
- 7. Van Woensel JB, Kimpen JL, Sprikkelman AB, Ouwehand A, Van Aalderen WM. Long‐term effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol 2000: 30: 92–6. [DOI] [PubMed] [Google Scholar]
- 8. Van Woensel JB, Wolfs TF, Van Aalderen WM, Brand PL, Kimpen JL. Randomised double blind placebo controlled trial of prednisolone in children admitted to hospital with respiratory syncytial virus bronchiolitis. Thorax 1997: 52: 634–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van Woensel JB, Van Aalderen WM, De Weerd W, et al. Dexamethasone for treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus. Thorax 2003: 58: 383–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith M, Iqbal S, Elliott TM, Everard M, Rowe BH. Corticosteroids for hospitalised children with acute asthma. Cochrane Database Syst Rev 2003: 2: CD002886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daugbjerg P, Brenoe E, Forchhammer H, et al. A comparison between nebulized terbutaline, nebulized corticosteroid and systemic corticosteroid for acute wheezing in children up to 18 months of age. Acta Paediatr 1993: 82: 547–51. [DOI] [PubMed] [Google Scholar]
- 12. Goebel J, Estrada B, Quinonez J, Nagji N, Sanford D, Boerth RC. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr (Phila) 2000: 39: 213–20. [DOI] [PubMed] [Google Scholar]
- 13. Schuh S, Coates AL, Binnie R, et al. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr 2002: 140: 27–32. [DOI] [PubMed] [Google Scholar]
- 14. Jartti T, Lehtinen P, Vanto T, et al. Evaluation of the efficacy of prednisolone in early wheezing induced by rhinovirus or respiratory syncytial virus. Pediatr Infect Dis J 2006: 25: 482–8. [DOI] [PubMed] [Google Scholar]
- 15. Kotaniemi‐Syrjänen A, Vainionpää R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus‐induced wheezing in infancy – the first sign of childhood asthma? J Allergy Clin Immunol 2003: 111: 66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lemanske RF, Jackson DJ, Gangnon RE, et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol 2005: 116: 571–7. [DOI] [PubMed] [Google Scholar]
- 17. Jartti T, Lehtinen P, Vuorinen T, et al. Respiratory picornaviruses and respiratory syncytial virus as causative agents of acute expiratory wheezing in children. Emerg Infect Dis 2004: 10: 1095–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johansson SG, Bieber T, Dahl R, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004: 113: 832–6. [DOI] [PubMed] [Google Scholar]
- 19. NAEPP Expert Panel Report . Guidelines for the Diagnosis and Management of Asthma – Update on Selected Topics 2002. Update 2002. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/index.htm [Google Scholar]
- 20. Malmberg LP, Pelkonen A, Poussa T, Pohianpalo A, Haahtela T, Turpeinen M. Determinants of respiratory system input impedance and bronchodilator response in healthy Finnish preschool children. Clin Physiol Funct Imaging 2002: 22: 64–71. [PubMed] [Google Scholar]
- 21. Csonka P, Kaila M, Laippala P, Iso‐Mustajärvi M, Vesikari T, Ashorn P. Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection‐induced lower airway disease: a randomized, placebo‐controlled trial. J Pediatr 2003: 143: 725–30. [DOI] [PubMed] [Google Scholar]
- 22. Jacques J, Bouscambert‐Duchamp M, Moret H, et al. Association of respiratory picornaviruses with acute bronchiolitis in French infants. J Clin Virol 2006: 35: 463–6. [DOI] [PubMed] [Google Scholar]
- 23. Farr BM, Gwaltney JM JR, Hendley JO, et al. A randomized controlled trial of glucocorticoid prophylaxis against experimental rhinovirus infection. J Infect Dis 1990: 162: 1173–7. [DOI] [PubMed] [Google Scholar]
- 24. Gustafson LM, Proud D, Hendley JO, Hayden FG, Gwaltney JM Jr. Oral prednisone therapy in experimental rhinovirus infections. J Allergy Clin Immunol 1996: 97: 1009–14. [DOI] [PubMed] [Google Scholar]
- 25. Grunberg K, Sharon RF, Sont JK, et al. Rhinovirus‐induced airway inflammation in asthma: effect of treatment with inhaled corticosteroids before and during experimental infection. Am J Respir Crit Care Med 2001: 164: 1816–22. [DOI] [PubMed] [Google Scholar]
- 26. Wark PA, Johnston SL, Bucchieri F, et al. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med 2005: 201: 937–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Xatzipsalti M, Kyrana S, Tsolia M, et al. Rhinovirus viremia in children with respiratory infections. Am J Respir Crit Care Med 2005: 172: 1037–40. [DOI] [PubMed] [Google Scholar]
- 28. Jartti T, Mäkelä M, Vanto T, Ruuskanen O. The link between bronchiolitis and asthma. Infect Dis Clin North Am 2005: 19: 667–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sahid El‐Radhi A, Hogg CL, Bungre JK, Bush A, Corrigan CJ. Effect of oral glucocorticoid treatment on serum inflammatory markers in acute asthma. Arch Dis Child 2000: 83: 158–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wilson AM, McFarlane LC, Lipworth BJ. Systemic bioactivity profiles of oral prednisolone and nebulized budesonide in adult asthmatics. Chest 1998: 114: 1022–7. [DOI] [PubMed] [Google Scholar]
- 31. Jartti T, Lehtinen P, Vuorinen T, Koskenvuo M, Ruuskanen O. Persistence of rhinovirus and enterovirus RNA after acute respiratory illness in children. J Med Virol 2004: 72: 695–9. [DOI] [PubMed] [Google Scholar]


