Abstract
Endothelial cells are the main determinants of vascular function, since their dysfunction in response to a series of cardiovascular risk factors is responsible for disease progression and further consequences. Endothelial dysfunction, if not resolved, further aggravates the oxidative status and vessel wall inflammation, thus igniting a vicious cycle. We have furthermore to consider the physiological manifestation of vascular dysfunction and chronic low-grade inflammation during ageing, also known as inflammageing. Based on these considerations, knowledge of the molecular mechanism(s) responsible for endothelial loss-of-function can be pivotal to identify novel targets of intervention with the aim of maintaining endothelial wellness and vessel trophism and function. In this review we have examined the role of the detoxifying enzyme aldehyde dehydrogenase 2 (ALDH2) in the maintenance of endothelial function. Its impairment indeed is associated with oxidative stress and ageing, and in the development of atherosclerosis and neurodegenerative diseases. Strategies to improve its expression and activity may be beneficial in these largely diffused disorders.
Keywords: endothelial cells, oxidative stress, inflammageing, endothelial dysfunction, aldehyde dehydrogenase-2, cardiovascular disease, neurovascular disease
1. Introduction
We searched PubMed from its inception up to December, 2019, using the terms “ALDH2, endothelial cells, endothelial dysfunction, endothelial senescence, ageing, oxidative stress, inflammageing, cardiovascular diseases, neurovascular diseases” to identify publications in English that described the mechanism of action of ALDH2 activity in vascular function, preclinical evidence of beneficial effects of ALDH2 expression/activity for endothelial function, or clinical evidence of the benefit of ALDH2 activity modulation in cardio- or neuro-vascular diseases. We mostly selected publications from the past 10 years that we judged were relevant, but we did not exclude widely referenced and highly regarded older publications.
1.1. Endothelial Function and Dysfunction
Vascular function such as the heartbeat is an essential system for the good functioning of our body. Under normal conditions, endothelial cells (ECs) in blood vessels, through the release of vasoactive and anti-aggregatory mediators and the functioning of antioxidant systems, regulate blood pressure, protecting from hypertension and atherosclerosis. They also constitute a blood barrier, preventing leukocyte infiltration and inflammation into the vascular wall and surrounding tissues [1,2].
Conversely, endothelial dysfunction has been identified as a hallmark of most cardiovascular diseases. Dysfunction of ECs is correlated with an imbalance in the production of key regulators of the vascular homeostasis such as nitric oxide (NO) and growth factors, and/or impaired activity (uncoupling) of endothelial NO synthase (eNOS), associated with increased reactive oxygen species (ROS) levels and vascular oxidative stress [3,4]. Inflammatory factors such as inteleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), intercellular adhesion molecule 1 (ICAM-1) and loss of the antioxidant mechanism are among the most important causes of vascular dysfunction [5].
When endothelial dysfunction occurs, the ability of endothelium to perform one or all of these functions is decreased. In this condition, ECs switch to a pro-inflammatory profile, characterized by loss of barrier integrity, and reduced release of vasoactive molecules associated with increased release of pro-thrombotic mediators [2,5]. Our studies and those of others showed that endothelial dysfunction is linked to impaired endothelial cell survival and physiological angiogenic outcomes with a later rearrangement of the microcirculation that contributes to the onset of various diseases [6,7,8]. Both anti- and pro-angiogenic therapeutic strategies have been developed for treating human diseases. While angiogenesis inhibitors have been shown to have success in many diseases as cancer, few treatment protocols with the aim to stimulate angiogenesis in ischemia-associated diseases have reached the clinic. Indeed, since endothelial function has been proposed as “barometer for cardiovascular risk”, identification of the molecular determinants underlying endothelial integrity and functionality is a medical need [5,6,9,10,11]. In this scenario, risk factors for endothelial dysfunction are represented by pathological conditions as hypertension, diabetes and atherosclerosis, and lifestyles as high-fat diet, tobacco smoke, alcohol intake, and physical inactivity [12]. Since endothelium is a regulator of exchanges between the vascular wall and surrounding tissues, it is not surprising that dysfunctional ECs can lead to the impairment of other tissues [2,6,12]. Indeed, assessment of vascular function and structure, and in particular of endothelial dysfunction appears to play a crucial role in a broad array of human diseases as cardiovascular and neurodegenerative diseases, tumor growth and metastasis [2,5,8,9,10,11,12].
1.2. Endothelial Senescence
Cardiovascular diseases (CVDs) represent the major cause of disability and death in the elderly population of the Western World. As introduced above, a large number of risk factors plays a role in the development of CVDs, especially ageing which is associated with well-characterized phenotypes [8,13,14]. Over time, aged blood vessels become stiffer and thicker, and their ability to release vasoactive mediators, particularly NO, decreases, while vascular permeability increases, associated with the process of mild vessel inflammation, increased vessel thickness and compromised angiogenic response [14,15,16,17,18]. Of note, even if age remains the main determinant of vascular senescence, healthy vascular ageing can be achieved, and endothelial function is a key element of the heathy vasculature.
Senescent vascular endothelium and other tissues are frequently characterized by chronic mild inflammation [12,13]. In particular, the age-related low grade, chronic, and systemic inflammation is indicated by the term “inflammageing” [12,13]. The indicators of inflammageing include elevated levels of inflammatory mediators such as IL-1, IL-6 and TNF-α, which characterize many age-related pathological phenotypes. These indicators derive from an imbalance of the immune response (immunosenescence) [19].
A large population of senescent cells in organs has the potential to negatively impact organ renewal capabilities and functions, especially on ECs, accelerating the onset of several age-associated pathologies, as CVDs and cancer [15,20].
However, senescent cells may also exert various positive effects on individuals. As senescence is associated with irreversible growth arrest, it is considered to be a tumor suppressor process [21]. In particular, indirect evidence indicates that endothelial senescence plays a causal role in microvascular rarefaction and affects the ability of cells to proliferate and form capillary-like structures [20]. The timely and challenging issue for modern biomedical sciences focused on ageing is the identification of the biological targets and the pharmacological tools able to promote “healthy ageing”.
1.3. Aldehyde Dehydrogenase-2 (ALDH2)
The aldehyde dehydrogenase (ALDH) gene superfamily encodes enzymes that are mainly responsible for the irreversible oxidation of various aldehydes. Three major classes of mammalian ALDHs (classes 1, 2 and 3) have been identified. Classes 1 and 3 contain both constitutive and inducible cytosolic isozymes. Class 2 consists of constitutive mitochondrial isozymes [22,23]. ALDH2 is primarily involved in the detoxification of acetaldehyde, the first intermediate of ethanol metabolism, into acetate, a less active byproduct [23]. In addition to acetaldehyde, other aldehydes are metabolized by ALDH2 [23,24]. The sources of aldehydic substrates of ALDH2 can be endogenous or exogenous. Endogenous reactive aldehydes are generated as byproducts of cell metabolism and include malondialdehyde, 4-hydroxynonenal (4-HNE), DOPAL, and acrolein [23]. Exogenous aldehydes are found in industrial and environmental pollutants and may be produced during metabolism of xenobiotics. Among these, acrolein, acetaldehyde and formaldehyde are the major reactive species found in tobacco smoke and car exhaust [23,24]. Generally, aldehydes are toxic molecules that react rapidly with amino acid residues, e.g., thiols to form the genotoxic DNA- and protein-adducts in cells [23,24].
ALDH proteins are found in all cellular compartments, including cytosol, mitochondria, endoplasmic reticulum and the nucleus. Some proteins have more than one cellular location. Nevertheless, ALDHs also catalyze some reactions involved in the formation of bioactive molecules that regulate important physiological functions. This is the case of some ALDHs as ALDH1A1, 1A2 and 1A3 that convert retinal aldehyde in retinoic acid. In turn, retinoic acid acts as a ligand for retinoic X receptor (RXR) and nuclear retinoic receptor (RAR), participating in a number of growth and developmental processes [23,25,26].
ALDH2 arises as an important gatekeeper of ROS overproduction that a cell is able to tolerate. In fact, the main function of mitochondrial ALDH2 is to protect mitochondria and cells from the damaging effect of aldehydes, by oxidizing the substrates into their corresponding non-toxic carboxylic acids. Some studies distinguish between direct and indirect anti-oxidative properties of ALDH2. The direct anti-oxidative properties are assumed to depend on its potent reductase function with its highly activated sulfhydryl groups [27]. In addition to oxidative capabilities, ALDH2 possesses nitrate reductase activity responsible for the bioconversion of nitroglycerin to 1,2-glyceryl dinitrate (GDN), thus inducing NO release [28,29,30]. ALDH2 protein can be the substrate of various post-translational modifications, including oxidation, S-nitrosylation, phosphorylation, nitration, acetylation, glycosylation, and adduct formation, most of which reduce its activity [31].
In the present review, we describe the effects of oxidative stress-linked accumulation of aldehydes in the cells, focusing on ECs, and discuss the contribution of ALDH2 in several endothelium-dependent disorders, including senescence.
2. ALDH2 and Endothelial-Related Diseases
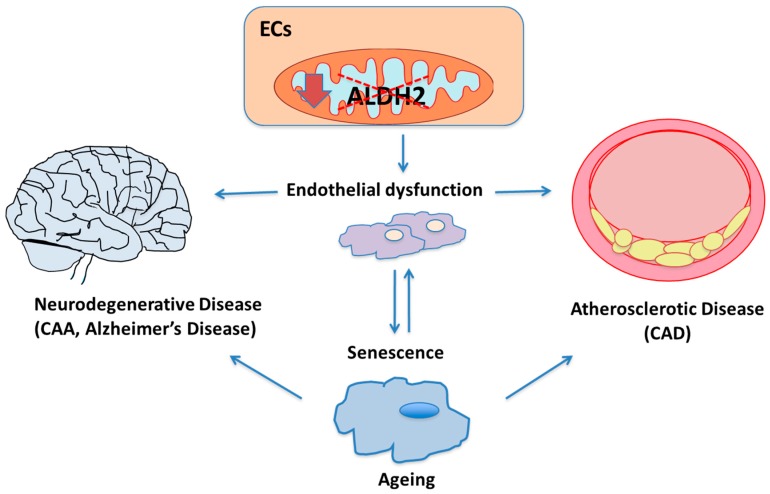
Different diseases have in common EC impairment and dysfunction and more precisely an alteration in ALDH expression and enzymatic activity, in turn responsible for changes in oxidative status and inflammation (Figure 1).
Figure 1.
The role of aldehyde dehydrogenase-2 (ALDH2) in endothelial function and endothelial-related diseases. ALDH2 downregulation (down arrow) and/or catalytic inactivation (dashed red lines) into mitochondria in endothelial cells (ECs), leading to inefficient aldehyde metabolism, is recognized to affect endothelial functions and make senescence occur faster. Senescence itself might further aggravate endothelial dysfunction. In turn, ALDH2 is believed to be involved in the ageing process, in particular ageing related-cardiovascular diseases, such as atherosclerosis and coronary artery disease (CAD), and affect the cerebrovascular unit, contributing to the etiology of neurovascular degenerative diseases, including Cerebral Amyloid Angiopathy (CAA).
2.1. ALDH2, Oxidative Stress and Ageing
Advanced age is an independent risk factor for life-threatening diseases, including coronary artery disease, stroke, and neurodegenerative diseases, which are directly related to ageing-associated EC dysfunction [32]. Despite senescence being studied deeply for many centuries and many steps in our understanding of it accomplished, the process of ageing remains largely difficult to remedy and remains, unfortunately, inevitable [33]. In addition to the “inflammageing” hypothesis, many theories have been proposed to explain the process of ageing [33]. In particular, the general free radical theory of ageing indicates that ageing is caused by ROS-dependent accumulation of damage [34]. In other words, the traditional view in the field of free radical biology is that free radicals and ROS are toxic and able to directly damage a large plethora of biological targets. Furthermore, the accumulation of damage leads to the process of ageing resulting in various diseases [35]. Recent findings revealed that the accumulation of toxic aldehydes plays a key role in ischemia-reperfusion injuries and in ageing as much as ROS from which they derive [36,37,38,39].
Accordingly, some studies support the close link between ALDH2 dysfunction and ageing, especially in the heart [40,41]. In particular, ALDH2 has been reported to protect ECs against oxidative stress events due to aldehydes, and cell senescence [41,42].
One of our recent works showed that inhibition of ALDH2 activity negatively impacted EC function. We demonstrated that ALDH2 silencing or inhibition significantly affected cell proliferation, migration and altered cellular permeability, in terms of reduced VE–cadherin and ZO-1 expression at cell–cell contacts and increased cellular permeability in human umbilical vein endothelial cells (HUVECs) [42]. Although the mechanism of action has not been fully elucidated, our results indicate that ROS production and 4-hydroxy-2-nonenal (4-HNE) accumulation, a secondary end-product of lipid peroxidation, contribute to mediate endothelial dysfunction and the onset of senescence in siALDH2 and daidzin-treated cells [42]. These findings were supported by the observation that exposure to the ROS scavenger, N-acetylcysteine, affected the pattern of 4-HNE adducts, reduced ROS and recovered cell survival in siALDH2 cells [42]. The aldehyde 4-HNE is a reactive molecule which forms adducts with proteins, lipids and DNA. Excessive 4-HNE adduct formation has been reported in ischemic cardiovascular tissue isolated from rodents and humans [43,44]. From a bioenergetic standpoint, we observed that ALDH2 attenuation reduced basal and maximal respiration and abolished mitochondrial reserve capacity in ECs [42]. Intriguingly, this latter finding suggested that ALDH2 supports mitochondrial bioenergetics by increasing basal, maximal and consequently reserve capacity. Further, the changes in cell morphology, from polygonal to an enlarged and irregular shape, evoked the senescent phenotype and this led us to explore further details. The analysis of typical senescent markers, such as p21/p53 expression and SA-β-gal, further suggested that siALDH2 or daidzin-treated ECs present early signs of senescence [42]. This scenario suggests a protective role of ALDH2 on endothelium. The inhibition of ALDH2 affects endothelial functions, bioenergetics and metabolism, and makes the acquisition of a senescent phenotype faster. The acquisition of a senescent phenotype might have a defensive role, but the expansion of senescent cells might itself further aggravate the damage and accelerate ageing.
From a mechanistic point of view, the accumulation of endogenous reactive aldehydes, including 4-HNE, and inhibition of ALDH2 by these reactive species increased cell vulnerability to aldehyde-induced damage [45]. Indeed, susceptibility to lipid peroxidation byproducts of ALDH2 enzymatic activity was reported [46]. It was observed that ALDH2 is inactivated by aldehydes at low concentrations (<10 μM) and ROS. ALDH inactivation may interfere with the detoxification of lipid aldehydes, promoting their accumulation, which, in turn, is known to trigger ROS production, amplifying oxidative damage in the cell. Specifically, in ECs inactivation of ALDH2 correlates with vascular damage, vasoconstriction, and thrombosis [47].
Moreover, evidence showed the role of acetaldehyde in tissue and cell damage. In particular, a study reported that ALDH2 prevented acetaldehyde-related toxic effects by alleviating oxidative stress and apoptosis in HUVECs [47]. For instance, it has been observed that in HUVEC, ALDH2 over-expression protects cells from the toxic effects of exposure to different concentrations of acetaldehyde. As a result, the generation of ROS is decreased, as well as apoptosis and activation of stress signaling molecules, such as signal-regulated extracellular kinases (ERK1/2), and the p38 mitogenic activated MAP kinase protein [47]. Of note, the acetaldehyde-induced ROS generation, apoptosis and activation of stress molecules were prevented by the ALDH2 transgene in a manner similar to antioxidant alpha-tocopherol, indicating that facilitation of acetaldehyde detoxification by ALDH2 transgene overexpression is able to counteract acetaldehyde-induced EC injury and activation of stress signals. These data consecutively highlight the therapeutic potential of ALDH2 in the prevention of cell damage induced by ethanol consumption [47], features of which are very similar to those of accelerated ageing.
Consistently, mutations in ALDHs genes as well as their downregulation or ALDHs catalytic inactivation, leading to inefficient aldehyde metabolism, may contribute in the etiology of various diseases including cardiopathies and neurovascular degenerative diseases, including the cerebral amyloid angiopathy (CAA) and Alzheimer’s disease (AD) [24,48].
2.2. ALDH2 and Atherosclerosis
Heart failure is a clinical manifestation characterized by alterations in cardiac morphology and functions that lead to reduced cardiac output and/or elevated intra-cardiac pressure at rest or during stress. Coronary artery disease (CAD), diabetes mellitus and alcohol abuse are common determinants of myocardial diseases, which result in ischemic injury, metabolic disorders or toxic damage [49]. Nevertheless, advanced ageing leads to alteration in morphology and function of the heart in the absence of other accompanying cardiovascular risk factors. In particular, ALDH2 is believed to be involved in the ageing process and ageing related-cardiovascular diseases. In fact, although ALDH2 is better known for its involvement in ethanol metabolism, it is also crucial for cardioprotection through the detoxification of reactive aldehydes such as 4-HNE and the bioconversion of nitrates into NO [27,29]. ALDH2 is largely seen as a critical enzyme involved in protecting the heart from ischemic injury. Much evidence, including meta-analysis, have assessed the associations between ALDH2 rs671 (ALDH2*2) polymorphism inactivating the enzymatic activity, and CAD [50]. Additionally, results from various studies conducted on Asian patients have highlighted the strong association between myocardial infarction and ALDH2 rs671 polymorphism [51]. In this context, the majority of studies focused on myocardium [52], with limited attention on ECs or vessels. Nonetheless, ALDH2 activity is impaired by oxidized low-density lipoproteins (ox-LDLs), possibly by post-translational modifications. In particular, ox-LDLs are found to exert an inhibitory effect on ALDH2 activity by preventing mitochondrial sirtuin 3 (SIRT3) expression [31]. SIRT3 is one of the members of the sirtuin family, which have a common core domain and an important role in ageing, stress resistance and metabolic regulation. In particular, SIRT3 has received much attention for its role in mitochondrial metabolism and ageing [53].
A study corroborates the association between ALDH2 and SIRT3 [54]. This study strengthens the concept that moderate ethanol consumption is associated with a positive effect on eNOS activation that results in antiatherogenic actions. In particular, Xue and colleagues showed that in human aortic ECs (HAECs), low-dose ethanol resulted in SIRT3 inactivation, leading to rapid activation of ALDH2. ALDH2 activity mediates ethanol-induced eNOS activation and prevents ROS accumulation [54]. Thus, ALDH2 activation promoted by SIRT3 inactivation improves HAEC function, resulting in an anti-atherogenic effect. Consistent with this finding, another recent study showed that ALDH2 silencing or inhibition aggravated the atherosclerotic process. In ApoE−/− mice the silencing of the ALDH2 gene was associated with a severe inflammation of the vascular wall and the formation of larger and more unstable plaques [55]. In-vitro experiments with HUVECs further illustrated that inhibition of ALDH2 activity resulted in elevated inflammatory molecules, an enhanced nuclear translocation or phosphorylation of pro-inflammatory transcription factor such as NF-κB or AP-1 involved in vessel permeability and plaque development [55]. Of note, in ECs, we and other reported that several natural agents such as polyphenols of extra virgin olive oil modulate, beyond ROS production, the expression and activity of enzymes and transcription factors involved in atherogenesis [56,57]. These data support the assumption that metabolic cell redox state has a marked impact on the cell transcriptome and proteome, and, in turn, on cell functions. In this context, it would be of interest to know the effects of nutraceuticals on ALDH2 activity in controlling vessel integrity.
Overall, these data convincingly indicate that ALDH2 silencing or inhibition exacerbates the atherosclerosis process, increasing plaque development and vulnerability with aggravated inflammation. Nevertheless, further work is needed to fully understand the clinical value of ALDH2 and its activation in the prevention or treatment of atherosclerotic diseases, such as CAD.
2.3. ALDH2 and Neurodegenerative Diseases
Alzheimer’s disease (AD) is classified as a progressive neurodegenerative disorder, characterized by neuropathological changes in particular brain regions and in a variety of neuro-transmitter systems. The progressive neuronal degeneration that occurs in AD generally leads to dementia, the most common consequence, affecting cognitive functions in patients such as memory, thinking and reasoning [58]. Unfortunately, AD is becoming more prevalent as human lifespan increases. AD is a multifactorial disease driven by a combination of genetic and environmental factors and can be divided in two forms: familial and sporadic cases [59]. A characteristic feature of AD is the deposit of amyloid β peptides (mainly Aβ1-40 and Aβ1-42) in the brain that form extracellular amyloid plaques. These plaques lead to neuronal dysfunction, cell death, and loss of synaptic connections, notably due to the ensuing inflammation and oxidative stress [60]. Increased oxidative stress is reported to play a critical role in the pathogenesis of AD prior to the onset of Aβ deposition and cognitive impairment. Cerebrovascular dysfunction has emerged as a critical feature of neurodegenerative diseases [61]. Cerebral amyloid angiopathy (CAA), a cerebrovascular disease that is frequently associated with AD, is characterized by the accumulation of Aβ in cerebral microvessels. In CAA, the endothelial dysfunction is thought to alter Aβ homeostasis and to promote infiltration of the brain parenchyma with circulating toxic molecules [61]. At the same time, Aβ peptides, especially the vasculotropic isoform Aβ1–40, affect brain blood vessels, altering their fundamental functions, including impairment of vasoactive tone and barrier functions, vascular remodelling as well as suppression of the intrinsic angiogenic properties of endothelium [48,62,63,64]. Although CAA remains clinically distinct from AD, their common features have the potential to link cerebrovascular and neurodegenerative pathways in the ageing brain. The product 4-HNE is formed during oxidative stress, and is able to react with many molecules such as proteins, and to accumulate in the brain. Many studies have shown that 4-HNE covalently modifies Aβ via 1,4 conjugates, altering the function of Aβ and impairing cellular features such as metabolism, cell signaling and structural integrity [65]. Since ALDH2 protects mitochondrial functions through the detoxification of 4-HNE that accumulates in this organelle, it is not surprising that recent epidemiological studies showed a correlation between ALDH2*2 loss-of-function mutations in Asian patients and a higher incidence of AD in these people [24,45].
One potential intervention for the treatment of AD can be to reduce the toxicity caused by the Aβ peptides, particularly Aβ1-40. Previous studies from our lab elucidated the role of ALDH2 in the protection of endothelium against Aβ1-40 damage. In particular, the chronic exposure of cultured EC to Aβ results in profound modifications of cell pro-angiogenic functions, shifting their phenotype toward the senescence program and reducing its pro-angiogenic capability [66]. Aβ peptides also increase intracellular 4-HNE in ECs by impairment of mitochondrial ALDH2 activity [48]. Consistently, in an ALDH2−/− knockout null mouse model, mice exhibited both neuronal and vascular pathological changes associated with AD. In fact, mice exhibited progressive, age-related cognitive deficits in non-spatial and spatial working memory and other features, together with a multitude of AD-associated signs, including 4-HNE adducts as well as age-related increase in Aβ [67].
In addition to the observed AD-like changes in the brain, significant vascular alterations were found in cerebral microvessels (CMVs) of ALDH2−/− mice. In comparison to the wild type, CMVs of these mice displayed marked increases in HNE adducts and age-related increases in monomeric Aβ. Moreover, ALDH2−/− mice exhibited endothelial dysfunction, and increased Aβ deposits in microvessels [67].
From these studies it seems that ALDH2 activity may play a critical role for preserving endothelial function in cerebrovascular units and preventing age-related dysfunctions.
3. Conclusions
Global average lifespan is increasing as a result of many factors, such as lifestyle. But, as longevity continues to increase, ageing-related diseases and, consequentially, the need for new therapeutic interventions arise. Today, regenerative medicine plays a significant role relative to other therapies, including those for the treatment of CVD.
In this review we showed that ALDH2 asserts a protective role in the endothelium against different types of stressors including age-associated dysfunctions. ALDH2 has emerged in recent years as a crucial guardian against several stressor or toxic insults, supporting its potential role in many diseases, including cardiovascular and cerebrovascular diseases that are linked to ageing (Table 1).
Table 1.
Summary of main findings of ALDH2 and ageing, atherosclerosis or neurodegenerative diseases.
| ALDH2 Status | Tissue/Cells | Molecular Mechanism | Function | Ref. |
|---|---|---|---|---|
| ALDH2 and vascular ageing | ||||
| ALDH2 activation | Heart (rat) | (−) aldehydic adducts (carbonylation) | (−) cardiac dysfunction | [28] |
| ALDH2 activation | Liver (rat) | (−) ROS (−) pro-inflammatory cytokines (−) 4-HNE and MDA |
(−) tissue apoptosis (+) mitochondrial membrane potential |
[30] |
| ALDH2 transgenic mice | Heart | (+) ROS (−) AMPK phosphorylation (−) SIRT1 |
(+) ageing-induced cardiac hypertrophy (+) apoptosis (+) mitochondrial injury |
[40] |
| ALDH2 activation | Heart (mouse) | (−) 4-HNE-protein adducts (−) protein carbonyls (+) autophagy flux (+) SIRT1 |
(+) cardiac function | [41] |
| ALDH2 gene silencing | Endothelial cells | (+) ROS (+) 4-HNE |
(−) respiration (+) senescence |
[42] |
| ALDH2 gene transfection | Endothelial cells | (−) ROS | (−) apoptosis (−) ERK/p38-MAPK |
[47] |
| ALDH2 and atherosclerosis | ||||
| ALDH2*2 loss-of-function | --- | (+) ox-LDLs | (+) coronary artery disease | [50,51,52] |
| ALDH2 gene silencing | ApoE−/− mice | (+) ROS | (+) vessel wall inflammation (+) plaque instability |
[55] |
| ALDH2 activation | Endothelial cells | (−) ROS; (+) eNOS (−) SIRT3 activation |
--- | [54] |
| ALDH2 inhibition | Endothelial cells | (+) NF-κB (+) AP-1 |
(+) permeability (+) plaque formation |
[55] |
| ALDH2 and neurodegenerative diseases | ||||
| ALDH2*2 loss-of-function | Brain | --- | (+) incidence of Alzheimer’s disease | [45] |
| ALDH2−/− mouse model | Brain | (+) 4-HNE adducts (+) Aβ |
(+) cognitive deficits (+) endothelial dysfunction (+) Aβ in microvessels |
[47] |
| ALDH2 inactivation | Endothelial cells | (+) 4-HNE | (−) angiogenesis (+) senescence |
[48] |
Since senescence-related endothelial dysfunction plays a crucial role in the pathogenesis of several diseases, further studies are necessary to fully elucidate the role and protective mechanisms of ALDH2 in the endothelium.
Author Contributions
G.N. wrote the manuscript and drew the figure; S.D., M.Z. and L.M. made substantial contribution in the revision process; L.M. gave approval of the submitted version. All authors have read and agreed to the published version of the manuscript All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Italian Ministry of Education, University and Research (MIUR- PRIN projects), grant number 2017XP72RF (to L.M.) and 20152HKF3Z (to M.Z.).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Wagner D.D., Frenette P.S. The vessel wall and its interactions. Blood. 2008;111:5271–5281. doi: 10.1182/blood-2008-01-078204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajendran P., Rengarajan T., Thangavel J., Nishigaki Y., Sakthisekaran D., Sethi G., Nishigaki I. The vascular endothelium and human diseases. Int. J. Biol. Sci. 2013;9:1057–1069. doi: 10.7150/ijbs.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daiber A., Oelze M., Wenzel P., Wickramanayake J.M., Schuhmacher S., Jansen T., Lackner K.J., Torzewski M., Münzel T. Nitrate tolerance as a model of vascular dysfunction: Roles for mitochondrial aldehyde dehydrogenase and mitochondrial oxidative stress. Pharmacol. Rep. 2009;61:33–48. doi: 10.1016/S1734-1140(09)70005-2. [DOI] [PubMed] [Google Scholar]
- 4.Monti M., Donnini S., Giachetti A., Mochly-Rosen D., Ziche M. deltaPKC inhibition or varepsilonPKC activation repairs endothelial vascular dysfunction by regulating eNOS post-translational modification. J. Mol. Cell. Cardiol. 2010;48:746–756. doi: 10.1016/j.yjmcc.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haybar H., Shahrabi S., Rezaeeyan H., Shirzad R., Saki N. Endothelial Cells: From Dysfunction Mechanism to Pharmacological Effect in Cardiovascular Disease. Cardiovasc. Toxicol. 2019;19:13–22. doi: 10.1007/s12012-018-9493-8. [DOI] [PubMed] [Google Scholar]
- 6.Donnini S., Cantara S., Morbidelli L., Giachetti A., Ziche M. FGF-2 overexpression opposes the beta amyloid toxic injuries to the vascular endothelium. Cell Death Differ. 2006;13:1088–1096. doi: 10.1038/sj.cdd.4401803. [DOI] [PubMed] [Google Scholar]
- 7.Morbidelli L., Donnini S., Ziche M. Targeting endothelial cell metabolism for cardio-protection from the toxicity of antitumor agents. Cardio-Oncology. 2016;2:3. doi: 10.1186/s40959-016-0010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ungvari Z., Tarantini S., Kiss T., Wren J., Giles C.B., Griffin C.T., Murfee W.L., Pacher P., Csiszar A. Endothelial dysfunction and angiogenesis impairment in the ageing vasculature. Nat. Rev. Cardiol. 2018;15:555–565. doi: 10.1038/s41569-018-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caruso P., Signori R., Moretti R. Small vessel disease to subcortical dementia: A dynamic model, which interfaces ageing, cholinergic dysregulation and the neurovascular unit. Vasc. Health Risk Manag. 2019;15:259–281. doi: 10.2147/VHRM.S190470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trott D.W., Fadel P.J. Inflammation as a mediator of arterial ageing. Exp. Physiol. 2019;104:1455–1471. doi: 10.1113/EP087499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao Y.M., Yuan H.Q., Ren Z., Qu S.L., Liu L.S., Wei D.-H., Yin K., Fu M., Jiang Z.S. Endothelial to mesenchymal transition in atherosclerotic vascular remodeling. Clin. Chim. Acta. 2019;490:34–38. doi: 10.1016/j.cca.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Donato A.J., Machin D.R., Lesniewski L.A. Mechanisms of Dysfunction in the Ageing Vasculature and Role in Age-Related Disease. Circ. Res. 2018;123:825–848. doi: 10.1161/CIRCRESAHA.118.312563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dantas A.P., Jiménez-Altayó F., Vila E. Vascular ageing: Facts and factors. Front. Physiol. 2012;3:325. doi: 10.3389/fphys.2012.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghebre Y.T., Yakubov E., Wong W.T., Krishnamurthy P., Sayed N., Sikora A.G., Bonnen M.D. Vascular Ageing: Implications for Cardiovascular Disease and Therapy. Transl. Med. 2016;6 doi: 10.4172/2161-1025.1000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.North B.J., Sinclair D.A. The intersection between ageing and cardiovascular disease. Circ. Res. 2012;110:1097–1108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masi S., Colucci R., Duranti E., Nannipieri M., Anselmino M., Ippolito C., Tirotta E., Georgiopoulos G., Garelli F., Nericcio A., et al. Ageing Modulates the Influence of Arginase on Endothelial Dysfunction in Obesity. Arterioscler. Thromb. Vasc. Biol. 2018;38:2474–2483. doi: 10.1161/ATVBAHA.118.311074. [DOI] [PubMed] [Google Scholar]
- 17.Foote K., Reinhold J., Yu E.P.K., Figg N.L., Finigan A., Murphy M.P., Bennett M.R. Restoring mitochondrial DNA copy number preserves mitochondrial function and delays vascular ageing in mice. Ageing Cell. 2018;17:e12773. doi: 10.1111/acel.12773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Silva T.M., Li Y., Kinzenbaw D.A., Sigmund C.D., Faraci F.M. Endothelial PPARγ (Peroxisome Proliferator-Activated Receptor-γ) Is Essential for Preventing Endothelial Dysfunction with Ageing. Hypertension. 2018;72:227–234. doi: 10.1161/HYPERTENSIONAHA.117.10799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cannizzo E.S., Clement C.C., Sahu R., Follo C., Santambrogio L. Oxidative stress, inflamm-ageing and immunosenescence. J. Proteom. 2011;74:2313–2323. doi: 10.1016/j.jprot.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Campisi J., Andersen J.K., Kapahi P., Melov S. Cellular senescence: A link between cancer and age-related degenerative disease? Semin. Cancer Biol. 2011;21:354–359. doi: 10.1016/j.semcancer.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y., Lui K.O., Zhou B. Reassessing endothelial-to-mesenchymal transition in cardiovascular diseases. Nat. Rev. Cardiol. 2018;15:445–456. doi: 10.1038/s41569-018-0023-y. [DOI] [PubMed] [Google Scholar]
- 22.Vasiliou V., Thompson D.C., Smith C., Fujita M., Chen Y. Aldehyde dehydrogenases: From eye crystallins to metabolic disease and cancer stem cells. Chem. Biol. Interact. 2013;202:2–10. doi: 10.1016/j.cbi.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodríguez-Zavala J.S., Calleja L.F., Moreno-Sánchez R., Yoval-Sánchez B. Role of Aldehyde Dehydrogenases in Physiopathological Processes. Chem. Res. Toxicol. 2019;32:405–420. doi: 10.1021/acs.chemrestox.8b00256. [DOI] [PubMed] [Google Scholar]
- 24.Chen C.H., Ferreira J.C., Gross E.R., Mochly-Rosen D. Targeting aldehyde dehydrogenase 2: New therapeutic opportunities. Physiol. Rev. 2014;94:1–34. doi: 10.1152/physrev.00017.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rhinn M., Dollé P. Retinoic acid signalling during development. Development. 2012;139:843–858. doi: 10.1242/dev.065938. [DOI] [PubMed] [Google Scholar]
- 26.Ciccone V., Terzuoli E., Donnini S., Giachetti A., Morbidelli L., Ziche M. Stemness marker ALDH1A1 promotes tumor angiogenesis via retinoic acid/HIF-1α/VEGF signalling in MCF-7 breast cancer cells. J. Exp. Clin. Cancer Res. 2018;37:311. doi: 10.1186/s13046-019-1045-y. Correction in 2019, 38, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wenzel P., Hink U., Oelze M., Seeling A., Isse T., Bruns K., Steinhoff L., Brandt M., Kleschyov A.L., Schulz E., et al. Number of nitrate groups determines reactivity and potency of organic nitrates: A proof of concept study in ALDH-2−/− mice. Br. J. Pharmacol. 2007;150:526–533. doi: 10.1038/sj.bjp.0707116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun L., Batista Ferreira J.C., Mochly-Rosen D. ALDH2 activator inhibits increased myocardial infarction injury by nitroglycerin tolerance. Sci. Transl. Med. 2011;3:1–7. doi: 10.1126/scitranslmed.3002067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Opelt M., Eroglu E., Waldeck-Weiermair M., Russwurm M., Koesling D., Malli R., Graier W.F., Fassett J.T., Schrammel A., Mayer B. Formation of Nitric Oxide by Aldehyde Dehydrogenase-2 Is Necessary and Sufficient for Vascular Bioactivation of Nitroglycerin. J. Biol. Chem. 2016;291:24076–24084. doi: 10.1074/jbc.M116.752071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang T., Zhao Q., Ye F., Huang C.Y., Chen W.M., Huang W.Q. Alda-1 an ALDH2 activator, protects against hepatic ischemia/reperfusion injury in rats via inhibition of oxidative stress. Free Radic. Res. 2018;13:1–10. doi: 10.1080/10715762.2018.1459042. [DOI] [PubMed] [Google Scholar]
- 31.Wei S.J., Xing J.H., Wang B.L., Xue L., Wang J.L., Li R., Qin W.D., Wang J., Wang X.P., Zhang M.X., et al. Poly(ADPribose) polymerase inhibition prevents reactive oxygen species induced inhibition of aldehyde dehydrogenase2 activity. Biochem. Biophys. Acta. 2013;1833:479–486. doi: 10.1016/j.bbamcr.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 32.Tian X.L., Li Y. Endothelial cell senescence and age-related vascular diseases. J. Genet. Genom. 2014;41:485–495. doi: 10.1016/j.jgg.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Sergiev P.V., Dontsova O.A., Berezkin G.V. Theories of ageing: An ever-evolving field. Acta Nat. 2015;7:9–18. doi: 10.32607/20758251-2015-7-1-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gladyshev V.N. The free radical theory of ageing is dead. Long live the damage theory! Antioxid. Redox. Signal. 2014;20:727–731. doi: 10.1089/ars.2013.5228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liochev S.I. Reactive oxygen species and the free radical theory of ageing. Free Radic. Biol. Med. 2013;60:1–4. doi: 10.1016/j.freeradbiomed.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 36.Gomes K.M., Campos J.C., Bechara L.R., Queliconi B., Lima V.M., Disatnik M.H., Magno P., Chen C.H., Brum P.C., Kowaltowski A.J., et al. Aldehyde dehydrogenase 2 activation in heart failure restores mitochondrial function and improves ventricular function and remodelling. Cardiovasc. Res. 2014;103:498–508. doi: 10.1093/cvr/cvu125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gomes K.M., Bechara L.R., Lima V.M., Ribeiro M.A., Campos J.C., Dourado P.M., Kowaltowski A.J., Mochly-Rosen D., Ferreira J.C. Aldehydic load and aldehyde dehydrogenase 2 profile during the progression of post-myocardial infarction cardiomyopathy: Benefits of Alda-1. Int. J. Cardiol. 2015;179:129–138. doi: 10.1016/j.ijcard.2014.10.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Panisello-Roselló A., Lopez A., Folch-Puy E., Carbonell T., Rolo A., Palmeira C., Adam R., Net M., Roselló-Catafau J. Role of aldehyde dehydrogenase 2 in ischemia reperfusion injury: An update. World J. Gastroenterol. 2018;24:2984–2994. doi: 10.3748/wjg.v24.i27.2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kimura M., Yokoyama A., Higuchi S. Aldehyde dehydrogenase-2 as a therapeutic target. Expert Opin. Ther. Targets. 2019;23:955–966. doi: 10.1080/14728222.2019.1690454. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Y., Mi S.L., Hu N., Doser T.A., Sun A., Ge J., Ren J. Mitochondrial aldehyde dehydrogenase 2 accentuates ageing-induced cardiac remodeling and contractile dysfunction: Role of AMPK, Sirt1, and mitochondrial function. Free Radic. Biol. Med. 2014;71:208–220. doi: 10.1016/j.freeradbiomed.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu B., Yu L., Wang Y., Wang H., Li C., Yin Y., Yang J., Wang Z., Zheng Q., Ma H. Aldehyde dehydrogenase 2 activation in aged heart improves the autophagy by reducing the carbonyl modification on SIRT1. Oncotarget. 2016;7:2175–2188. doi: 10.18632/oncotarget.6814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nannelli G., Terzuoli E., Giorgio V., Donnini S., Lupetti P., Giachetti A., Bernardi P., Ziche M. ALDH2 Activity Reduces Mitochondrial Oxygen Reserve Capacity in Endothelial Cells and Induces Senescence Properties. Oxid. Med. Cell Longev. 2018;2018:9765027. doi: 10.1155/2018/9765027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Uchidaand K., Stadtman E.R. Modification of histidine residues in proteins by reaction with 4-hydroxynonenal. Proc. Natl. Acad. Sci. USA. 1992;89:4544–4548. doi: 10.1073/pnas.89.10.4544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chung F.-L., Nath R.G., Ocando J., Nishikawa A., Zhang L. Deoxyguanosine Adducts of t-4-Hydroxy-2-nonenal Are Endogenous DNA Lesions in Rodents and Humans: Detection and Potential Source. Cancer Res. 2000;60:1507–1511. [PubMed] [Google Scholar]
- 45.Chen C.H., Joshi A.U., Mochly-Rosen D. The Role of Mitochondrial Aldehyde Dehydrogenase 2 (ALDH2) in Neuropathology and Neurodegeneration. Acta Neurol. Taiwan. 2016;25:111–123. [PMC free article] [PubMed] [Google Scholar]
- 46.Yoval-Sánchez B., Rodríguez-Zavala J.S. Differences in susceptibility to inactivation of human aldehyde dehydrogenases by lipid peroxidation byproducts. Chem. Res. Toxicol. 2012;25:722–729. doi: 10.1021/tx2005184. [DOI] [PubMed] [Google Scholar]
- 47.Li S.Y., Gomelsky M., Duan J., Zhang Z., Gomelsky L., Zhang X., Epstein P.N., Ren J. Overexpression of aldehyde dehydrogenase-2 (ALDH2) transgene prevents acetaldehyde-induced cell injury in human umbilical vein endothelial cells: Role of ERK and p38 mitogen-activated protein kinase. J. Biol. Chem. 2004;279:11244–11252. doi: 10.1074/jbc.M308011200. [DOI] [PubMed] [Google Scholar]
- 48.Solito R., Corti F., Chen C.H., Mochly-Rosen D., Giachetti A., Ziche M., Donnini S. Mitochondrial aldehyde dehydrogenase-2 activation prevents β-amyloid-induced endothelial cell dysfunction and restores angiogenesis. Pt 9J. Cell Sci. 2013;126:1952–1961. doi: 10.1242/jcs.117184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pang J., Wang J., Zhang Y., Xu F., Chen Y. Targeting acetaldehyde dehydrogenase 2 (ALDH2) in heart failure-Recent insights and perspectives. Biochem. Biophys. Acta Mol. Basis Dis. 2017;1863:1933–1941. doi: 10.1016/j.bbadis.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 50.Zhang L.L., Wang Y.Q., Fu B., Zhao S.L., Kui Y. Aldehyde dehydrogenase 2 (ALDH2) polymorphism gene and coronary artery disease risk: A meta-analysis. Genet. Mol. Res. 2015;14:18503–18514. doi: 10.4238/2015.December.23.38. [DOI] [PubMed] [Google Scholar]
- 51.Wang Q., Zhou S., Wang L., Lei M., Wang Y., Miao C., Jin Y. ALDH2 rs671 Polymorphism and coronary heart disease risk among Asian populations: A meta-analysis and meta-regression. DNA Cell Biol. 2013;32:393–399. doi: 10.1089/dna.2013.1995. [DOI] [PubMed] [Google Scholar]
- 52.Yasue H., Mizuno Y., Harada E. Association of East Asian Variant Aldehyde Dehydrogenase 2 Genotype (ALDH2*2*) with Coronary Spasm and Acute Myocardial Infarction. Adv. Exp. Med. Biol. 2019;1193:121–134. doi: 10.1007/978-981-13-6260-6_7. [DOI] [PubMed] [Google Scholar]
- 53.Kincaid B., Bossy-Wetzel E. Forever young: SIRT3 a shield against mitochondrial meltdown, ageing, and neurodegeneration. Front. Ageing Neurosci. 2013;5:48. doi: 10.3389/fnagi.2013.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xue L., Xu F., Meng L., Wei S., Wang J., Hao P., Bian Y., Zhang Y., Chen Y. Acetylation-dependent regulation of mitochondrial ALDH2 activation by SIRT3 mediates acute ethanol-induced eNOS activation. FEBS Lett. 2012;586:137–142. doi: 10.1016/j.febslet.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 55.Pan C., Xing J.H., Zhang C., Zhang Y.M., Zhang L.T., Wei S.J., Zhang M.X., Wang X.P., Yuan Q.H., Xue L., et al. Aldehyde dehydrogenase 2 inhibits inflammatory response and regulates atherosclerotic plaque. Oncotarget. 2016;7:35562–35576. doi: 10.18632/oncotarget.9384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Terzuoli E., Nannelli G., Giachetti A., Morbidelli L., Ziche M., Donnini S. Targeting endothelial-to-mesenchymal transition: The protective role of hydroxytyrosol sulfate metabolite. Eur. J. Nutr. 2019 doi: 10.1007/s00394-019-01920-x. [DOI] [PubMed] [Google Scholar]
- 57.Tressera-Rimbau A., Arranz S., Eder M., Vallverdú-Queralt A. Dietary Polyphenols in the Prevention of Stroke. Oxid. Med. Cell. Longev. 2017;2017:7467962. doi: 10.1155/2017/7467962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wenk G.L. Neuropathologic changes in Alzheimer’s disease. J. Clin. Psychiatry. 2003;64:7–10. [PubMed] [Google Scholar]
- 59.Piaceri I., Nacmias B., Sorbi S. Genetics of familial and sporadic Alzheimer’s disease. Front. Biosci. 2015;5:167–177. doi: 10.2741/e605. [DOI] [PubMed] [Google Scholar]
- 60.Zhao Y., Zhao B. Oxidative stress and the pathogenesis of Alzheimer’s disease. Oxid. Med. Cell Longev. 2013;2013:316523. doi: 10.1155/2013/316523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lyros E., Bakogiannis C., Liu Y., Fassbender K. Molecular links between endothelial dysfunction and neurodegeneration in Alzheimer’s disease. Curr. Alzheimer Res. 2014;11:18–26. doi: 10.2174/1567205010666131119235254. [DOI] [PubMed] [Google Scholar]
- 62.Revesz T., Ghiso J., Lashley T., Plant G., Rostagno A., Frangione B., Holton J.L. Cerebral amyloid angiopathies: A pathologic, biochemical, and genetic view. J. Neuropathol. Exp. Neurol. 2003;62:885–898. doi: 10.1093/jnen/62.9.885. [DOI] [PubMed] [Google Scholar]
- 63.Patel N.S., Mathura V.S., Bachmeier C., Beaulieu-Abdelahad D., Laporte V., Weeks O., Mullan M., Paris D. Alzheimer’s beta-amyloid peptide blocks vascular endothelial growth factor mediated signaling via direct interaction with VEGFR-2. J. Neurochem. 2010;112:66–76. doi: 10.1111/j.1471-4159.2009.06426.x. [DOI] [PubMed] [Google Scholar]
- 64.Solito R., Corti F., Fossati S., Mezhericher E., Donnini S., Ghiso J., Giachetti A., Rostagno A., Ziche M. Dutch and Arctic mutant peptides of beta amyloid(1-40) differentially affect the FGF-2 pathway in brain endothelium. Exp. Cell Res. 2009;315:385–395. doi: 10.1016/j.yexcr.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Siegel S.J., Bieschke J., Powers E.T., Kelly J.W. The oxidative stress metabolite 4-hydroxynonenal promotes Alzheimer protofibril formation. Biochemistry. 2007;46:1503–1510. doi: 10.1021/bi061853s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Donnini S., Solito R., Cetti E., Corti F., Giachetti A., Carra S., Beltrame M., Cotelli F., Ziche M. Abeta peptides accelerate the senescence of endothelial cells in vitro and in vivo, impairing angiogenesis. FASEB J. 2010;24:2385–2395. doi: 10.1096/fj.09-146456. [DOI] [PubMed] [Google Scholar]
- 67.D’souza Y., Elharram A., Soon-Shiong R., Andrew R.D., Bennett B.M. Characterization of Aldh2−/− mice as an age-related model of cognitive impairment and Alzheimer’s disease. Mol. Brain. 2015;8:27. doi: 10.1186/s13041-015-0117-y. [DOI] [PMC free article] [PubMed] [Google Scholar]