Abstract
Objective:
Design, setting and participants: A randomised single‐blind controlled trial with a treatment duration of 3 days and a follow‐up period of 4 days was conducted at a sauna in Berlin, Germany. Between November 2007 and March 2008 and between September 2008 and April 2009, 157 patients with symptoms of the common cold were randomly assigned to an intervention group (n = 80) and a control group (n = 77).
Interventions: Participants in the intervention group inhaled hot dry air within a hot sauna, dressed in a winter coat, whereas participants in the control group inhaled dry air at room temperature within a hot sauna, also dressed in a winter coat.
Main outcome measures: Area under the curve (AUC) summarising symptom severity over time (Days 2, 3, 5 and 7), symptom severity scores for individual days, intake of medication for the common cold and general ill feeling.
Results: No significant difference between groups was observed for AUC representing symptom severity over time (intervention group mean, 31.2 [SEM, 1.8]; control group mean, 35.1 [SEM, 2.3]; group difference, − 3.9 [95% CI, − 9.7 to 1.9]; P = 0.19). However, significant differences between groups were found for medication use on Day 1 (P = 0.01), symptom severity score on Day 2 (P = 0.04), and participants’ ratings of the effectiveness of the therapy on Day 7 (P = 0.03).
Conclusion: Inhaling hot air while in a sauna has no significant impact on overall symptom severity of the common cold.
Trial registration: ClinicalTrials.gov identifier NCT00552981.
Keywords: Complementary therapies, Respiratory tract diseases
The common cold, mainly caused by rhinoviruses or coronaviruses, 1 , 2 is a frequent problem all over the world. Although the symptoms are generally benign, viral colds result in significant costs to the economy due to lost workdays and school attendance. 3 Convincing treatment options without side effects are not known. 4 Traditionally, the local application of heat is used to treat the symptoms of the common cold — for example, ingesting hot fluids such as tea or chicken soup, 5 or inhaling hot vapour. 6 Moreover, few clinical trials have been conducted to evaluate such treatment options. 6 ‐ 8 It has been suggested that local hyperthermia of the nasal mucosa can affect rhinovirus replication. 7 ‐ 9 A Cochrane review of six trials — one from Israel, two from the United Kingdom, and three from the United States — found that only the studies from Israel and UK showed that steam was beneficial for relief of common cold symptoms. 6 Results on symptom indices were equivocal; therefore, it was concluded that steam inhalation cannot be recommended for the routine treatment of common cold symptoms and further blind randomised controlled trials needed to be conducted.
In the German city of Essen, a sauna with dry air heated to 90°C exists (www.unperfekthaus.de/projekte/angezogen‐sauna) where people can visit dressed in street clothes for the relief of common cold symptoms. This type of sauna is widely available and offers enough dry air to heat the throat, and wetness of the skin is only caused by sweating, not by high humidity. With the aim of heating the throat, people stay in this sauna for only a short period to avoid sweating. Use of this type of sauna has little in common with that of a regular sauna, where one usually stays longer than 10 minutes and sweating is desired. If proven to be effective, a dry air sauna would be an interesting option for treating common cold symptoms.
On the basis of experiences with the sauna in Essen, the aim of our study was to test the hypothesis that inhaling hot dry air reduces common cold symptoms. To do this, we compared the efficacy of applying hot dry air versus dry air at room temperature to the throat of patients with a newly acquired common cold, using a symptom severity score.
Methods
Design
A randomised single‐blind controlled trial was conducted, in which participants were randomly assigned to an intervention group (inhaling hot air within a hot sauna) or a control group (inhaling air at room temperature within a hot sauna). Unstratified and unrestricted randomisation was applied by one of us (R L) using SAS/BASE software v9.1 (SAS Inc, Cary, NC, USA) and data were transferred into a secure Microsoft Office Access 2003 (Microsoft Corporation, Redmond, Wash, USA) database that was not accessible to any staff members or study physicians.
This study adhered to the principles of the Declaration of Helsinki and International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Guideline for Good Clinical Practice (ICH GCP), and was approved by the local ethics committee (Charité University Medical Center).
Participants
Employees of the Charité University Medical Center, medical students and people working near the Charité campus were recruited between November 2007 and March 2008 and between September 2008 and April 2009. Participants received €10 for each visit to cover transportation costs.
We included patients between 18 and 60 years of age, with at least two out of 10 common cold symptoms — cough, headache, hoarseness, muscle ache, nasal drainage (nasal drip), nasal congestion, scratchy throat, sore throat, sneezing and fever (> 38.5°C) for 24 hours or less 10 — and who were not planning to take medication for the cold. We excluded patients who had any of these cold symptoms for more than 24 hours, circulatory problems, severe chronic illness, or systolic blood pressure below 100 mmHg or above 160 mmHg, or who were pregnant.
Intervention
Participants in both groups sat in a sauna (dry air [20% humidity], 90°C) in Berlin (at the Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center) dressed in a winter coat (63% acrylic, 37% polyester, 1.5 cm thick), for about 3 minutes on 3 consecutive days. The short stay and the insulation provided by the winter coat should avoid circulatory imbalance and sweating. The intervention group sat in the hot sauna and inhaled the hot dry sauna air through the mouth via a mask. The control group sat in the hot sauna and inhaled dry air from outside the sauna (24°C) through the mouth via a mask (Box 1). Fitness of participants was assessed before every treatment in the sauna by measuring blood pressure and heart rate and by asking about fever symptoms.
Box 1.
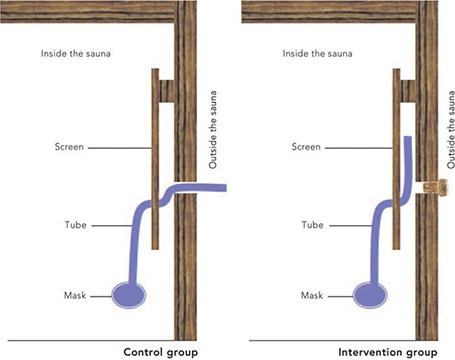
Sauna set‐up used for control and intervention groups
To have a comparable setting and enable maximum blinding in both groups, we used a face mask to cover the mouth and nose that was attached to a tube (80 cm long), similar to masks used for anaesthesia. The tube was lead through a screen, and the other end of the tube was either placed behind the screen (to allow inhalation of sauna air) or lead through the wall of the sauna (to allow inhalation of ambient air). After every application, the mask and tube were disinfected.
Outcome measures
The severity of each of the 10 symptoms used as inclusion criteria was rated by participants at baseline (on Day 1, before randomisation), after treatment episodes on Days 1, 2 and 3, and on Days 5 and 7, using a scale of 0 to 3 (0 = none, 1 = mild, 2 = moderate, 3 = severe). This scale has previously been used in a trial on the common cold. 10 The primary outcome measure was the area under the curve (AUC) which summarised symptom severity over time (on Days 2, 3, 5 and 7), based on a sum score from the 10 symptoms that were rated.
Secondary outcomes measured were symptom severity scores on Days 1, 2, 3, 5 and 7, use of medication for the common cold on Days 1–7, general ill feeling on a rating scale of 0 (completely healthy) to 10 (very ill) on Days 1, 2, 3, 5 and 7, and safety according to incidence of adverse events on Days 1–7 (eg, symptoms or events other than the 10 symptoms that were rated). In addition, participants rated expected outcomes of therapy and expected effectiveness of therapy at baseline, guessed which group they had been assigned to on Day 3, and provided ratings of outcomes and effectiveness on Day 7.
Outcomes were assessed using standardised questionnaires. Apart from the questionnaires completed on Days 5 and 7, which the participants took home, all questionnaires were completed at the study site.
Statistics
Each randomly assigned participant was included in the analysis regardless of adherence to the assigned treatment or the provision of a full set of data (intention‐to‐treat analysis). To detect a medium effect size (Cohen's d, 0.5) with 80% power and a two‐sided significance level of 5%, we planned to recruit 160 patients (128 participants plus 25% extra to allow for patient drop out).
The symptom severity score and general ill feeling data were evaluated using generalised estimation equation (GEE) regression models which modelled treatment group, time, group–time interaction, baseline values and participants’ initial expectations from treatment as covariates. This resulted in adjusted symptom severity scores from which the adjusted AUC was calculated via the trapezoid rule (ie, linear interpolation of data points and summing up the resulting trapezoid areas). All reported treatment effects, 95% confidence intervals and P values are based on this GEE model.
Similar GEE models were fitted to the dichotomous data on participants’ use of medication for the common cold during the treatment period, assuming a logit link function between covariates and response. Differences between the intervention and control groups are expressed as adjusted odds ratios.
Results
Participants
Of 287 people who expressed interest in the study, 157 were randomly assigned to the intervention or control arms of the study (intervention group: n = 80, control group: n = 77; Box 2). The mean age of these participants was 32.0 years (SD, 10.2 years; median, 28 years), and 93 participants (59.2%) were women. Mean age and body mass index differed significantly between groups (P = 0.03 and P = 0.003, respectively) but other baseline characteristics were comparable (Box 3).
Box 2.
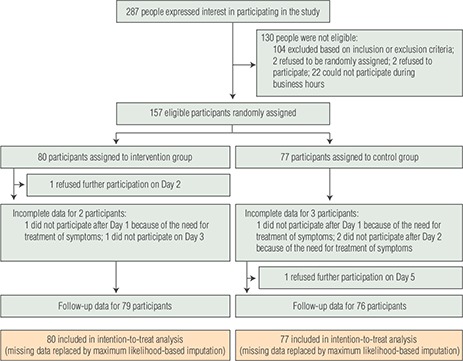
Recruitment, treatment and follow‐up of patients with a newly acquired common cold, November 2007 – March 2008 and September 2008 – April 2009
Box 3.
Baseline characteristics of study participants
|
Intervention (n = 80) |
Control (n = 77) |
P |
|||
|---|---|---|---|---|---|
|
Mean (SD) or no. (%) |
Median |
Mean (SD) or no. (%) |
Median |
||
| Women | 46 (58%) | 47 (61%) | 0.65 | ||
| Age (years) | 33.7 (10.8) | 30.0 | 30.2 (9.4) | 27.0 | 0.03 |
| Body mass index (kg/m 2 ) | 23.4 (4.0) | 22.8 | 21.8 (2.9) | 21.3 | 0.003 |
| No. of common colds in past 6 months | 0.9 (1.1) | 1 | 1.1 (1.5) | 1 | 0.63 |
| Duration of symptoms (h) | 19.0 (6.1) | 21.5 | 18.3 (5.9) | 19.0 | 0.44 |
| Symptom severity score | |||||
| Total | 9.4 (4.0) | 9 | 9.1 (3.1) | 9 | 0.92 |
| Cough | 0.9 (0.7) | 1 | 0.8 (0.8) | 1 | 0.24 |
| Headache | 1.1 (0.9) | 1 | 1.2 (1.0) | 1 | 0.47 |
| Hoarseness | 0.8 (0.8) | 1 | 0.7 (0.8) | 0 | 0.20 |
| Muscle ache | 0.6 (0.8) | 0 | 0.7 (0.7) | 1 | 0.33 |
| Nasal drainage | 1.5 (0.9) | 2 | 1.5 (0.9) | 2 | 0.84 |
| Nasal congestion | 1.1 (0.9) | 1 | 1.2 (0.9) | 1 | 0.65 |
| Scratchy throat | 1.3 (0.9) | 1 | 1.4 (0.7) | 1 | 0.52 |
| Sore throat | 1.1 (0.9) | 1 | 1.0 (0.9) | 1 | 0.30 |
| Sneezing | 0.9 (0.8) | 1 | 0.8 (0.8) | 1 | 0.69 |
| Fever | 0.2 (0.4) | 0 | 0.1 (0.3) | 0 | 0.01 |
| General ill feeling* | 3.8 (1.7) | 3 | 4.2 (1.6) | 4 | 0.08 |
| Use of medications for other diseases | 15 (19%) | 24 (31%) | 0.07 | ||
| Use of medications for common cold † | 15 (19%) | 14 (18%) | 0.93 | ||
| Consultation because of common cold | 0 | 1 (1%) | |||
| Expected outcome | 0.70 | ||||
| Recovery | 2 (3%) | 7 (9%) | |||
| Distinct improvement | 37 (46%) | 31 (40%) | |||
| Light improvement | 41 (51%) | 38 (49%) | |||
| No improvement | 0 | 1 (1%) | |||
| Expected effectiveness | 0.46 | ||||
| Very effective | 7 (9%) | 12 (16%) | |||
| Effective | 55 (69%) | 48 (62%) | |||
| Small effect | 18 (23%) | 17 (22%) | |||
| No effect | 0 | 0 | |||
* On a scale of 0 to 10 (0 = completely healthy; 10 = very ill).† Before the beginning of the study, during present common cold.
Outcome measures
For the AUC for symptom severity (Days 2, 3, 5 and 7), no significant differences between the groups were observed (adjusted group difference, − 3.9 [95% CI, − 9.7 to 1.9]); P = 0.19; Cohen's d, 0.13; Box 4, Box 5). Moreover, for the symptom severity score on Day 2, there was a significant difference between groups (adjusted group difference, − 1.0 [95% CI, − 2.0 to − 0.1]; P = 0.04; Box 4, Box 5). Additional adjustments for age and body mass index did not change the results.
Box 4.
Outcome measures for the intention‐to‐treat population
|
Intervention (n = 79) |
Control (n = 76) |
|||
|---|---|---|---|---|
|
Mean ± SEM (95% CI)* |
Mean ± SEM (95% CI)* |
Group difference (95% CI)* |
P* |
|
| Area under the curve for symptom severity on Days 2, 3, 5 and 7 | ||||
| 31.2 ± 1.8 (27.6 to 34.8) | 35.1 ± 2.3 (30.5 to 39.7) | − 3.9 (− 9.7 to 1.9) | 0.19 | |
| Symptom severity score | ||||
| Day 1 | 6.7 ± 0.3 (6.1 to 7.3) | 6.5 ± 0.2 (6.1 to 7.0) | 0.2 (− 0.6 to 0.9) | 0.69 |
| Day 2 | 6.5 ± 0.3 (5.9 to 7.2) | 7.6 ± 0.4 (6.9 to 8.3) | − 1.0 (− 2.0 to − 0.1) | 0.04 |
| Day 3 | 5.5 ± 0.4 (4.7 to 6.2) | 6.5 ± 0.5 (5.5 to 7.4) | − 1.0 (− 2.2 to 0.2) | 0.11 |
| Day 5 | 5.0 ± 0.4 (4.2 to 5.8) | 5.4 ± 0.5 (4.4 to 6.5) | − 0.5 (− 1.8 to 0.8) | 0.47 |
| Day 7 | 3.1 ± 0.4 (2.4 to 3.8) | 3.6 ± 0.5 (2.7 to 4.5) | − 0.5 (− 1.6 to 0.6) | 0.40 |
|
Percentage (95% CI)* |
Percentage (95% CI)* |
Odds ratio (95% CI)*† |
P* |
|
| Proportion of participants who took medication for common cold ‡ | ||||
| Day 1 | 3% (1% to 9%) | 15% (8% to 28%) | 0.2% (0.04% to 0.7%) | 0.01 |
| Day 2 | 6% (2% to 16%) | 9% (5% to 18%) | 0.6% (0.2% to 2%) | 0.47 |
| Day 3 | 9% (4% to 18%) | 12% (5% to 23%) | 0.7% (0.2% to 2%) | 0.56 |
| Day 4 | 9% (4% to 19%) | 12% (6% to 24%) | 0.7% (0.2% to 2%) | 0.51 |
| Day 5 | 10% (5% to 21%) | 9% (4% to 20%) | 1% (0.3% to 4%) | 0.85 |
| Day 6 | 7% (3% to 16%) | 7% (3% to 17%) | 1% (0.3% to 4%) | 0.94 |
| Day 7 | 5% (2% to 14%) | 8% (3% to 18%) | 0.7% (0.2% to 3%) | 0.56 |
|
No. (%) |
No. (%) |
P |
||
| Participant's rating of outcome on Day 7 | 0.56 | |||
| Recovery | 3 (4%) | 3 (4%) | ||
| Distinct improvement | 13 (16%) | 9 (12%) | ||
| Light improvement | 43 (54%) | 37 (49%) | ||
| No improvement | 20 (25%) | 27 (35%) | ||
| Participant's rating of effectiveness on Day 7 | 0.03 | |||
| Very effective | 2 (3%) | 1 (1%) | ||
| Effective | 30 (38%) | 22 (29%) | ||
| Small effect | 41 (52%) | 32 (42%) | ||
| No effect | 6 (8%) | 21 (28%) | ||
| Participant's guess of group allocation on Day 3 § | < 0.001 | |||
| Intervention | 41 (52%) | 14 (18%) | ||
| Control | 37 (47%) | 63 (82%) | ||
* Data were adjusted using a generalised estimation equation model.† Odds ratio < 1 indicates less medication use in intervention group.‡ From Days 1 to 7.§ Data missing for one participant in the intervention group on Day 3 (n = 79 for intervention group, n = 77 for control group).
Box 5.

Changes in adjusted symptom severity scores and general ill feeling scores over time*
B = baseline (on Day 1, before randomisation). * Data were reported by participants and adjusted using a generalised estimation equation model.
The general ill feeling score was not significantly different between groups (P > 0.05 for all days observed; Box 5). During the course of the common cold, the proportion of participants who took medication for the cold only differed significantly between groups on Day 1 (ie, after the first treatment episode) (odds ratio, 0.2 [95% CI, 0.04 to 0.7]; Box 4).
The groups did not differ significantly in terms of incidence of adverse events (11 participants [13.8%] in intervention group v nine participants [11.7%] in control group, P = 0.70). The most common adverse event was a cough directly stimulated by the intervention (intervention group, 2; control group, 1).
Expected outcomes according to participants had no significant impact on the AUC for symptom severity (P = 0.43).
Discussion
Participants who had inhaled hot air in the sauna did not show significantly different common cold symptoms compared with participants who had inhaled air at room temperature.
The main strengths of this trial are the rigorous study design, large sample size, high compliance and follow‐up rates, and the clear research hypothesis. Moreover, the sauna set‐up was very similar for the intervention and control groups, and the groups were comparable at baseline.
We might have underestimated the effect of sitting in the sauna. For example, some participants experienced pleasant warming of the face and relaxation while sitting in the sauna and less headache afterwards. The warm feeling in a sauna during a cold might have more impact on symptoms than inhaling hot air, resulting in similar treatment outcomes in both groups. If so, we might have chosen the wrong research hypothesis.
A short stimulus of 3 minutes was used to avoid sweating and drying of the mucus in the throat. The duration of each sauna stay in our study may have been too short, and the sauna stays may not have been frequent enough to cause a substantial effect. Also, blinding for the air temperature was difficult. In addition, the outcome measures we used were based only on participants’ reports. We did not include any objective outcome measures, such as plasma cytokine levels 10 , 11 or nasal airflow resistance. 5
Participants in our study started with a severity score of about 9 and reached a score of about 3 on Day 7. This course of disease is comparable with results from placebo groups in studies used to evaluate the efficacy of zinc acetate. 10 , 11 After enrolment in the study, the severity score lowered without the initial worsening of symptoms that one would expect within the first 48 hours of a common cold. 12 Perhaps the peak of symptom severity had already been reached. However, initial worsening is often only observable in studies where participants suffer from an experimentally induced common cold. 13 Taking this lack of initial worsening as an indication of longer disease duration (ie, greater than 24 hours at the start of the study), our intervention might have been too late to have had an impact on the course of the disease. However, the context effect 14 or placebo effect 15 , 16 may explain the initial improvement of symptoms. The placebo effect may also explain the significant group differences for the participants’ ratings of symptom severity on Day 2, medication intake on Day 1, and ratings of the effectiveness of the therapy on Day 7. As more participants in the control group guessed correctly that they were in the control group, the placebo effect might have been higher in the intervention group. Although we used dry air to heat the throat, instead of humidified air in the nose as done in most studies evaluated in the Cochrane review,6 we support the view that steam inhalation cannot yet be recommended for the routine treatment of common cold symptoms.
Inhaling hot dry air while in a sauna does not have a significant impact on the symptom severity of a common cold.
Acknowledgements
We thank Beatrice Eden and Iris Bartsch for their support with daily patient management, and Reinhard Wiesemann who developed the idea for this setting and provided the sauna cabin.
Competing Interests
The study was funded by the Karl und Veronica Carstens Foundation.
References
- 1. Heikkinen T, Jarvinen A. The common cold. Lancet 2003; 361: 51–59. 12517470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Papadopoulos NG, Sanderson G, Hunter J, Johnston SL. Rhinoviruses replicate effectively at lower airway temperatures. J Med Virol 1999; 58: 100–104. 10223554. [DOI] [PubMed] [Google Scholar]
- 3. Roxas M, Jurenka J. Colds and influenza: a review of diagnosis and conventional, botanical, and nutritional considerations. Altern Med Rev 2007; 12: 25–48. 17397266. [PubMed] [Google Scholar]
- 4. Arroll B. Non‐antibiotic treatments for upper‐respiratory tract infections (common cold). Respir Med 2005; 99: 1477–1484. 16291073. [DOI] [PubMed] [Google Scholar]
- 5. Saketkhoo K, Januszkiewicz A, Sackner MA. Effects of drinking hot water, cold water, and chicken soup on nasal mucus velocity and nasal airflow resistance. Chest 1978; 74: 408–410. 359266. [DOI] [PubMed] [Google Scholar]
- 6. Singh M. Heated, humidified air for the common cold. Cochrane Database Syst Rev 2006; (3): CD001728. 16855975. [DOI] [PubMed] [Google Scholar]
- 7. Tyrrell D, Barrow I, Arthur J. Local hyperthermia benefits natural and experimental common colds. BMJ 1989; 298: 1280–1283. 2500196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Conti C, De MA, Mastromarino P, et al. Antiviral effect of hyperthermic treatment in rhinovirus infection. Antimicrob Agents Chemother 1999; 43: 822–829. 10103186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lwoff A. Death and transfiguration of a problem. Bacteriol Rev 1969; 33: 390–403. 4313270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prasad AS, Fitzgerald JT, Bao B, et al. Duration of symptoms and plasma cytokine levels in patients with the common cold treated with zinc acetate. A randomized, double‐blind, placebo‐controlled trial. Ann Intern Med 2000; 133: 245–252. 10929163. [DOI] [PubMed] [Google Scholar]
- 11. Prasad AS, Beck FW, Bao B, et al. Duration and severity of symptoms and levels of plasma interleukin‐1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis 2008; 197: 795–802. 18279051. [DOI] [PubMed] [Google Scholar]
- 12. Gwaltney JM Jr, Hendley JO, Simon G, Jordan WS Jr. Rhinovirus infections in an industrial population. II . Characteristics of illness and antibody response. JAMA 1967; 202: 494–500. 4293015. [PubMed] [Google Scholar]
- 13. Gwaltney JM Jr, Hendley JO, Patrie JT. Symptom severity patterns in experimental common colds and their usefulness in timing onset of illness in natural colds. Clin Infect Dis 2003; 36: 714–723. 12627355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Di Blasi Z, Kleijnen J. Context effects. Powerful therapies or methodological bias? Eval Health Prof 2003; 26: 166–179. 12789710. [DOI] [PubMed] [Google Scholar]
- 15. Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet 1998; 351: 1722–1725. 9734904. [DOI] [PubMed] [Google Scholar]
- 16. Brinkhaus B, Pach D, Lüdtke R, Willich SN. Who controls the placebo? Introducing a placebo quality checklist for pharmacological trials. Contemp Clin Trials 2008; 29: 149–156. 17669693. [DOI] [PubMed] [Google Scholar]


