Abstract
Background:
Hamstring injuries are prevalent in professional athletes and can lead to significant time loss, with recurrent injury being common. The efficacy of platelet-rich plasma (PRP) for augmentation of nonoperative treatment of partial musculotendinous hamstring injuries is not well established.
Hypothesis:
The addition of PRP injections to nonoperative treatment for acute partial musculotendinous hamstring injuries will lead to a shortened return to play in National Football League (NFL) players.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
NFL players from a single team who sustained acute grade 2 hamstring injuries, as diagnosed on magnetic resonance imaging (MRI) by a musculoskeletal radiologist from 2009 to 2018, were retrospectively reviewed. Average days, practices, and games missed were recorded. Players who did and did not receive PRP (leukocyte-poor) injections were compared. Those who received PRP did so within 24 to 48 hours after injury.
Results:
A total of 108 NFL players had MRI evidence of a hamstring injury, and of those, 69 athletes sustained grade 2 injuries. Thirty players received augmented treatment with PRP injections and 39 players underwent nonoperative treatment alone. Average time missed in those treated with PRP injections was 22.5 days, 18.2 practices, and 1.3 games. In those who did not receive PRP injections, time missed was 25.7 days (P = .81), 22.8 practices (P = .68), and 2.9 games (P < .05).
Conclusion:
Augmentation with PRP injections for acute grade 2 hamstring injuries in NFL players showed no significant difference in days missed or time to return to practice but did allow for faster return to play, with a 1 game overall difference. Owing to the possible large financial impact of returning to play 1 game sooner, PRP injections for treatment of grade 2 hamstring injuries may be advantageous in professional athletes.
Keywords: hamstring injury, platelet-rich plasma, autologous conditioned plasma, muscle injury, biologic enhancement
Hamstring injuries are among the most common lower extremity injuries in athletes, accounting for up to 29% of all injuries in various sports. In addition, these injuries may produce a prolonged impairment and a higher reinjury rate of 12% to 31%. Injuries range from mild muscle damage without loss of structural integrity to complete muscle tearing with fiber disruption.3
These muscle strains are a cause of considerable disability in American football players. Muscle strains in the National Football League (NFL) account for 46% of practice injuries and 22% of preseason game injuries. Hamstring strains are the second most common preseason injury in American football, with an injury rate of 1.79 per 1000 athlete-exposures for practices and 4.07 per 1000 athlete-exposures during games.8 Elliott et al7 concluded that the majority of these injuries occur during the preseason. In particular, the speed positions such as wide receivers (WRs) and defensive secondary, as well as players on the special teams units, are at elevated risk of injury.
Hamstring strains can lead to significant time missed from practices and games in the NFL and can have significant morbidity. Recurrence rates are also high, with 16% of hamstring injuries in the NFL being recurrent.17 The financial impact on players and teams can also be substantial.15,19 For these reasons, injury prevention and accelerated return to play with decreased risk of reinjury is desired. One promising adjunct to treatment is platelet-rich plasma (PRP), which is a concentrated source of autologous platelets, growth factors, and alpha granules.13 PRP has the potential to improve the healing process, and as such it has been proposed for the management of many musculoskeletal injuries, including hamstring strains.1,2,11,16,17,22 However, the literature is limited regarding its efficacy, particularly with regard to professional sports where missed time and reinjury are major concerns.
The purpose of this study was to evaluate return to play in professional American football players (NFL) with acute hamstring injuries after leukocyte-poor PRP (LP-PRP) injections. It was hypothesized that LP-PRP injections would lead to faster return to play when compared with a control group who underwent only nonoperative treatment.
Methods
NFL players from a single team who sustained acute midsubstance muscle hamstring injuries from 2009 to 2018 were retrospectively reviewed. All players had a positive plank and modified plank test as well as painful prone-resisted knee flexion.4 Magnetic resonance imaging (MRI) scans were obtained for all patients. Inclusion criteria were acute grade 2 hamstring injury as diagnosed on MRI by a musculoskeletal radiologist (J.D.T.) using the MRI classification of Cohen et al.5 Institutional review board approval was obtained before initiation of this study.
Individualized player decisions were made with regard to whether injections were given. Player desires as well as season status (off-season vs training camp vs regular season vs playoffs) were instrumental. Injections were more commonly performed if injuries occurred during the season or during the playoffs. More severe injuries, as determined on MRI, were also more likely to undergo injection treatment. The senior author (J.P.B.) began performing PRP injections for hamstring injuries in NFL players in January 2009 so all patients who sustained injuries previous to that date did not receive PRP.
A commercially available PRP system was used for all injections (Arthrex, autologous conditioned plasma [ACP]). Ten milliliters of venous blood was drawn by the senior author using the Arthrex ACP Double Syringe System, and centrifugation was done at 1500 rpm (350g) for 5 minutes. This system yields a low white blood cell product (LP-PRP) with 3× platelet concentration and a pH of 5.1. A volume of 2 to 5 mL of LP-PRP was obtained. No additives were used (ie, anticoagulant citrate dextrose [ACD-A] or bicarbonate) as the PRP was injected within 20 minutes of centrifugation. Samples were not tested for platelet concentration, as this is not allowed by the NFL Players Association. All PRP injections were performed by the senior author utilizing measurements from MRI and direct palpation. Those who received PRP did so within 24 to 48 hours of injury and received between 1 and 3 injections with 1 week in between based on the player’s response. This was dictated by symptoms, including pain, improvement of symptoms, and physical examination including tenderness and plank testing. Nonsteroidal anti-inflammatory drug use was restricted throughout this period to avoid the possibility of interference with the PRP injection.12
After injection, a rest period of 24 to 48 hours was given, with therapy focused on passive motion, cryotherapy, and modalities. All athletes underwent the same physical therapy regimen, focusing on regaining normal pain-free motion and resistance exercises for strengthening with a focus on eccentrics. Modalities, aerobic exercise, and foam roller therapy were also paramount. All athletes underwent the same return-to-play testing protocol, which included successful plank testing without pain, normal strength, normal range of motion, and normal position-specific functional testing.
Age, player position, tendon injured, and recurrence as well as average days, practices, and games missed were recorded. Players who did and did not receive PRP injections were compared. Statistical analysis was performed using Prism 7.0 (GraphPad). Categorical variables were assessed with the Fisher exact test, and continuous variables were compared using the Student t test. Statistical significance was defined as P < .05.
Results
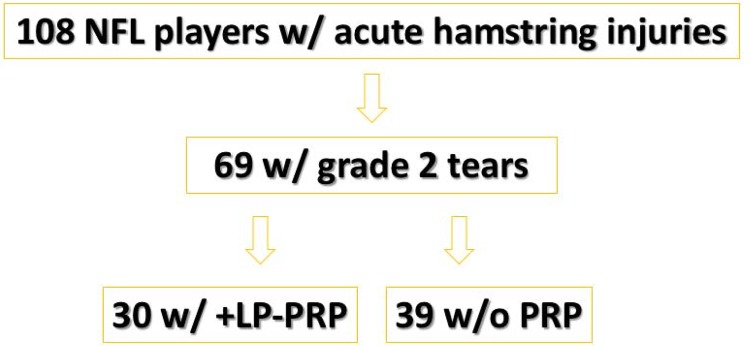
A total of 108 NFL players from a single team had MRI evidence of a hamstring injury, and of those, 69 athletes sustained grade 2 injuries based on MRI. Thirty players received augmented treatment with LP-PRP injections and 39 players underwent nonoperative treatment alone (Figure 1). Table 1 shows a comparison of characteristics between those who did and did not receive LP-PRP injections. The mean time missed in those treated with PRP injections was 22.5 days, 18.2 practices, and 1.3 games. In those who did not receive PRP injections, time missed was 25.7 days (P = .81), 22.8 practices (P = .68), and 2.9 games (P < .05) (Table 2). There was 1 recurrent injury in each group. The recurrence in the LP-PRP group occurred in a player who returned to play sooner than typically recommended because of a playoff game. No injection complications were seen (ie, nerve injury, loss of motion, infection, and significant local reaction). In the subset of those injured during the regular season, the average time missed for the PRP group (n = 21) was 11 days (P = .51), 6 practices (P = .79), and 1 game (P < .05) compared with the non-PRP group (n = 29), which was 14 days, 7 practices and 2 games.
Figure 1.
Study flowchart. All players underwent a standard physical therapy protocol. LP-PRP, leukocyte-poor platelet-rich plasma; NFL, National Football League; PRP, platelet-rich plasma.
Table 1.
Comparison of Characteristics of Patients With Grade 2 Hamstring Injuries Who Did and Did Not Undergo PRP Injectiona
| +LP-PRP | No PRP | |
|---|---|---|
| Number of players | 30 | 39 |
| Mean age, y | 28.8 | 25.7 |
| Player position | ||
| LB | 13 | 11 |
| WR | 7 | 10 |
| DB | 4 | 10 |
| RB | 4 | 6 |
| TE | 2 | 2 |
| Most common hamstring tendon injured | ||
| Biceps femoris | 22 | 24 |
| Semitendonosis | 7 | 8 |
| Semimembranosus | 1 | 7 |
| Number of PRP injections | ||
| 1 | 15 | |
| 2 | 10 | |
| 3 | 5 | |
| Injuries by time of the season, n | ||
| During season | 19 | 16 |
| During preseason | 6 | 20 |
| During off-season | 5 | 3 |
| Bilateral injuries during study period | 1 | 1 |
| Recurrences during study period | 1 | 1 |
aBoth +LP-PRP (players who received 2 to 3 LP-PRP injections) and No PRP (patients who did not receive PRP injections) groups underwent the same physical therapy and return-to-play protocol. DB, defensive back; LB, linebacker; +LP-PRP, leukocyte-poor platelet-rich plasma; PRP, platelet-rich plasma; RB, running back; TE, tight end; WR, wide receiver.
Table 2.
NFL Football Player Mean Time Missed: LP-PRP Injections vs No PRP Injectionsa
| Time Missed | +LP-PRP | No PRP | P |
|---|---|---|---|
| Days | 22.5 ± 20.1 | 25.7 ± 20.6 | .81 |
| Practices | 18.2 ± 9.2 | 22.8 ± 11.9 | .68 |
| Games | 1.3 ± 0.47 | 2.9 ± 1.1 | <.05b |
aPlayers who received LP-PRP injections (+LP-PRP) on average returned 1 game sooner than those who did not receive PRP injections (No PRP). LP-PRP, leukocyte-poor platelet-rich plasma injections; PRP, platelet-rich plasma.
bStatistically significant difference between the 2 treatments.
Discussion
Adjunctive LP-PRP injection treatment for acute grade 2 hamstring injuries led to a 1 game earlier return to play when compared with those who did not receive PRP injections in an NFL cohort. However, there was no statistically significant decrease in days or practices missed between treatment groups. Owing to the high morbidity and reinjury risk as well as the possible large financial impact of returning to play 1 game sooner, LP-PRP injections for treatment of grade 2 hamstring injuries may be advantageous in professional athletes.15,19
Possible explanations for the statistically significant improvement of 1 game earlier return to play in the PRP group versus the nonstatistically significant improvement of 3 days include different return to play desires based on the specific time within the season (preseason vs playoffs). This makes the days missed variable based on when the injury occurred. Further, coaches often require players to practice by a certain day of the week to be eligible to play in each week’s game. This leads to earlier return to play in practice, despite commonly being in a limited capacity, to ensure eligibility for the upcoming game.
Studies evaluating PRP injection treatment for hamstring injuries provide mixed results. This is likely because of the multiple different preparations of PRP used and compared. In 2011, Mejia and Bradley13 reported on their experience with PRP injections within 24 to 48 hours for acute hamstring injuries in 12 NFL players. This was the first evaluation of PRP treatment in NFL hamstring injuries. The same LP-PRP preparation and commercial system was used in the current study. Their results showed an earlier return to play of 3 days for grade 1 (n = 9) and 5 days for grade 2 injuries (n = 3), with an overall 1 game difference in return to play. The authors noted no recurrences compared with their baseline of 2 to 4 recurrences per year.13 The current study provides a larger sample size and a more meaningful and accurate evaluation of grade 2 injuries alone. The authors believe grade 2 injuries are those most likely to benefit from adjunctive treatment as grade 1 tears likely heal with traditional therapy alone, while grade 3 injuries are severe and typically indicate a more prolonged return to play no matter the additional treatment.
In a second NFL study investigating the effects of the addition of PRP to rehabilitation in acute hamstring injuries, Rettig et al17 reported no significant differences in recovery from hamstring injury between treatment with PRP (n = 5) and routine rehabilitation (n = 5). However, the PRP preparation used had high platelets (9.3 times baseline), were leukocyte rich (5.5 times baseline), and had additives, including ACD-A (3 mL added) and bicarbonate. In more recent studies, 6,18,20 it has been reported that leukocyte-rich PRP with high platelets is not ideal for acute muscle injuries as it may lead to an increased local reaction, possibly increasing scar formation. This is detrimental to hamstring injuries, as scar adjacent to normal tissue creates a stress riser, which may increase the risk of reinjury.21 Further, the 2013 study by Rettig et al is likely underpowered, with only 5 players in each group.17 Additives also dilute the PRP and its important growth substances.
A randomized study2 including athletes from different sports compared 28 patients with grade 2 hamstring injuries who received a single LR-PRP injection versus rehabilitation alone. These authors reported earlier return to play (26.7 vs 42.5 days; P = .02) and lower pain scores with PRP. In a double-blinded randomized study, Hamilton et al9 compared a single LR-PRP injection, platelet-poor plasma (PPP) injection, and rehabilitation alone in 90 professional athletes with MRI evidence of hamstring injury. The authors found no difference between a single PRP injection and rehabilitation alone but reported a significantly earlier return to sport in the PRP group (21 days) compared with the PPP group (21 vs 27 days; P = .01). They found no difference in reinjury rates at 2- or 6-month follow-up.9 The ideal number of injections and formulation of PRP are not clear. More well-designed prospective randomized trials are needed to better elucidate the clinical results of PRP treatment.
Before biologic treatments were available, Levine et al10 promoted steroid injections for hamstring injuries in NFL players. That group injected 58 hamstrings less than 72 hours after injury and reported a mean return to sport of 7.6 days (range, 0-24 days) with no reruptures. They had no comparison group of players not receiving a corticosteroid injection. As a different MRI-based classification was used in the current study, direct comparison may not be accurate. Nevertheless, days missed in the current study were 11 with PRP treatment. More severe injuries are likely included in the current study as well as in a recent comparison of 32 patients who received PRP with 24 who received steroid injections for grade 2 injuries. This group found superior outcomes in the PRP group and recommended against steroid injection in favor of PRP.16
Although the current study evaluates an NFL cohort, hamstring injuries are very common in all sports. Reducing pain, time to return to sport, and recurrence are advantageous in all athletes, as hamstring injuries can be quite disabling. Currently, limited treatments addressing these issues exist. PRP may be a useful adjunct for treatment of hamstring muscle injuries in athletes of all levels, with the hope of creating more normal architecture, thus allowing successful return to play with less risk of reinjury.
As mentioned, various plasma separation devices exist in clinical use, with each device having slightly different preparation steps and end products. The main differences among the current systems include the volume of blood required and the technical handling of the specimen during the centrifugation and separation process. Platelet concentration yield and leukocyte concentration differ based on preparation. These differences in PRP are vital, and their understanding is essential for appropriate treatment of injuries. For this reason, analysis of the PRP product used is recommended.
Preparations of PRP vary greatly among the current studies in the literature, which likely explains their mixed results. The authors recommend PRP with low leukocyte count and relatively low platelet count (3×) without additives (ie, ACD-A or bicarbonate), as the addition of other products leads to dilution of the PRP. The authors recommend avoiding PRP preparations with high leukocytes and high platelets in hamstrings, as scarring may ensue. These preparations are rather recommended for tendinopathy. Condition-specific PRP preparations are essential as are appropriate rehabilitation and injury prevention programs.6,14
Limitations
The current study may be underpowered to detect differences in practices and days missed; hence, a larger sample size would be beneficial. The variations in the number of PRP injections given also make it difficult to recommend the appropriate number of injection treatments. The number of patients in these groups does not allow for comparison between the number of injections. Player position was also not compared between groups. Significant differences may exist because of the requirements of different positions (ie, linebackers may return quicker than speed positions such as WR/defensive back). The current modern rehabilitation program may confound the results, as the recurrence rate reported for both groups is less than that previously reported. This may account for much of the benefit for both hamstring groups. Further, follow-up MRI, which was not obtained in this study, may provide interesting information regarding scarring and healing response.
Players were unable to be randomized between groups because of their professional level of play. Players both in and out of season were included in the current study. This may lead to an overestimation of days, practices, and games missed as there may be little urgency for return to play in many veteran players in the off-season or preseason. However, this is not the case for nonveterans and players vying for a roster spot. For this reason, all players were included in an attempt to provide the most complete picture of hamstring recovery. However, when evaluating players only in season, the number of days, practices, and games missed were also decreased with PRP treatment, but a 1 game earlier return to play was the only statistically significant finding.
Conclusion
Augmentation with LP-PRP injections for acute grade 2 hamstring injuries in NFL players showed no significant difference in days missed or time to return to practice but did allow for faster return to play with a 1 game overall difference. Owing to the possible large financial impact of return to play 1 game sooner, LP-PRP injections for treatment of grade 2 hamstring injuries may be advantageous in professional athletes.
Footnotes
Final revision submitted February 5, 2020; accepted February 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.P.B. has received consulting fees from DJO and royalties from Arthrex. T.J.L. has received grant support from Arthrex; educational support from Arthrex, Smith & Nephew, and Steelhead Surgical; and hospitality payments from Acumed, DePuy Synthes, Wright Medical, and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Pittsburgh Institutional Review Board (ID No. PRO18040336).
References
- 1. A Hamid M, Mohamed Ali MR, Yusof A, George J. Platelet-rich plasma (PRP): an adjuvant to hasten hamstring muscle recovery. A randomized controlled trial protocol (ISCRTN66528592). BMC Musculoskelet Disord. 2012;13:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. A Hamid M, Mohamed Ali MR, Yusof A, George J, Lee LP. Platelet-rich plasma injections for the treatment of hamstring injuries: a randomized controlled trial. Am J Sports Med. 2014;42(10):2410–2418. [DOI] [PubMed] [Google Scholar]
- 3. Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41(12):2933–2947. [DOI] [PubMed] [Google Scholar]
- 4. Arner JW, McClincy MP, Bradley JP. Hamstring injuries in athletes: evidence-based treatment. J Am Acad Orthop Surg. 2019;27(23):868–877. [DOI] [PubMed] [Google Scholar]
- 5. Cohen SB, Towers JD, Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3(5):423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dragoo JL, Braun HJ, Durham JL, et al. Comparison of the acute inflammatory response of two commercial platelet-rich plasma systems in healthy rabbit tendons. Am J Sports Med. 2012;40(6):1274–1281. [DOI] [PubMed] [Google Scholar]
- 7. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843–850. [DOI] [PubMed] [Google Scholar]
- 8. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597–1603. [DOI] [PubMed] [Google Scholar]
- 9. Hamilton B, Tol JL, Almusa E, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial. Br J Sports Med. 2015;49(14):943–950. [DOI] [PubMed] [Google Scholar]
- 10. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT. 3rd. Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. Am J Sports Med. 2000;28(3):297–300. [DOI] [PubMed] [Google Scholar]
- 11. Manduca ML, Straub SJ. Effectiveness of PRP injection in reducing recovery time of acute hamstring injury: a critically appraised topic. J Sport Rehabil. 2018;27(5):480–484. [DOI] [PubMed] [Google Scholar]
- 12. Mannava S, Whitney KE, Kennedy MI, et al. The influence of naproxen on biological factors in leukocyte-rich platelet-rich plasma: a prospective comparative study. Arthroscopy. 2019;35(1):201–210. [DOI] [PubMed] [Google Scholar]
- 13. Mejia H, Bradley JP. The effects of platelet-rich plasma on muscle: basic science and clinical application. Op Tech Sports Med. 2011;19(3):149–153. [Google Scholar]
- 14. Miroshnychenko O, Chang WT, Dragoo JL. The use of platelet-rich and platelet-poor plasma to enhance differentiation of skeletal myoblasts: implications for the use of autologous blood products for muscle regeneration. Am J Sports Med. 2017;45(4):945–953. [DOI] [PubMed] [Google Scholar]
- 15. Navarro SM, Sokunbi OF, Haeberle HS, et al. Short-term outcomes following concussion in the NFL: a study of player longevity, performance, and financial loss. Orthop J Sports Med. 2017;5(11):2325967117740847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park PYS, Cai C, Bawa P, Kumaravel M. Platelet-rich plasma vs. steroid injections for hamstring injury-is there really a choice? Skeletal Radiol. 2018;48(4):577–582. [DOI] [PubMed] [Google Scholar]
- 17. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rossi LA, Molina Rómoli AR, Bertona Altieri BA, Burgos Flor JA, Scordo WE, Elizondo CM. Does platelet-rich plasma decrease time to return to sports in acute muscle tear? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3319–3325. [DOI] [PubMed] [Google Scholar]
- 19. Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes. Orthop J Sports Med. 2016;4(8):2325967116663921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Setayesh K, Villarreal A, Gottschalk A, Tokish JM, Choate WS. Treatment of muscle injuries with platelet-rich plasma: a review of the literature. Curr Rev Musculoskelet Med. 2018;11(4):635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wangensteen A, Tol JL, Witvrouw E, et al. Hamstring reinjuries occur at the same location and early after return to sport: a descriptive study of MRI-confirmed reinjuries. Am J Sports Med. 2016;44(8):2112–2121. [DOI] [PubMed] [Google Scholar]
- 22. Zanon G, Combi F, Combi A, Perticarini L, Sammarchi L, Benazzo F. Platelet-rich plasma in the treatment of acute hamstring injuries in professional football players. Joints. 2016;4(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]