Abstract
Background:
Medial meniscal extrusion (MME) is defined as displacement of the meniscus that extends beyond the tibial margin. Knee varus malalignment increases MME.
Purpose/Hypothesis:
The purpose of this study was to quantify MME before and after medial opening wedge high tibial osteotomy (HTO) and to correlate the reduction of MME with clinical outcomes and return to activity. It was hypothesized that MME would decrease after HTO and that patients with lower MME after surgery would have improved clinical outcomes and return to activity at short-term follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study included 66 patients who underwent HTO to correct the anatomic axis with a minimum follow-up of 2 years. MME was measured using magnetic resonance imaging preoperatively and 6 weeks after surgery (study protocol). Patients were assessed preoperatively and postoperatively with the Knee injury and Osteoarthritis Outcome Score (KOOS), visual analog scale (VAS) score for pain, and Tegner score.
Results:
The mean ± SD preoperative and postoperative MME values were 3.9 ± 0.6 mm and 0.9 ± 0.5 mm, respectively. At 2 years after surgery, KOOS, pain VAS, and Tegner scores were higher than those found preoperatively (P < .001). Patients with less than 1.5 mm of MME after surgery had better clinical outcomes and return to activity compared with patients who had MME of 1.5 mm or more (P < .05).
Conclusion:
Medial opening wedge HTO decreased MME after 6 weeks and improved clinical outcomes and return to activity at a minimum 2-year follow-up. Additionally, patients with postoperative MME of less than 1.5 mm had better clinical outcomes and return to activity compared with patients who had postoperative MME of 1.5 mm or more.
Keywords: meniscal extrusion, high tibial osteotomy, return to activities, knee function
Meniscal extrusion is characterized by the displacement of the meniscus beyond the tibial margin.17,19,23,26 Meniscal root tear, bucket-handle meniscal tear, joint space narrowing, and medial collateral ligament (MCL) injury may be among the causes of meniscal extrusion.1,7,21 A symptomatic meniscal extrusion is more frequent in the medial meniscus, measuring more than 3 mm at the midlevel of the MCL.5 Meniscal extrusion can disturb the mechanical capacity of the meniscus, increasing load stress and decreasing the contact area on the surface of the medial compartment of the knee.4
Knee varus malalignment can reduce the medial joint space, overloading this compartment.11,13 In eligible patients, surgical correction of varus alignment is an option to reduce the load of the medial tibiofemoral compartment and to correct malalignment. Yet, the advantages of reducing medial meniscal extrusion (MME) after medial opening wedge high tibial osteotomy (HTO) to correct malalignment of the knee are not completely understood.10,18
Therefore, the main objective of the present study was to quantify MME before and after medial opening wedge HTO and to correlate the reduction of MME with clinical outcomes and return to activity. It was hypothesized that MME would decrease after HTO and that patients with lower MME after surgery would have improved clinical outcomes and return to activity at short-term follow-up.
Methods
Institutional review board approval was obtained to conduct this study, and all patients signed an informed consent form. A longitudinal prospective cohort study was conducted with all patients who underwent medial opening wedge HTO with MME between 2005 and 2017.
Inclusion criteria were (1) age younger than 59 years, (2) a minimum follow-up of 2 years, (3) varus malalignment greater than 15°, (4) isolated medial compartment knee pain, (5) knee range of motion (ROM) greater than 120°, (6) no patellofemoral symptoms, (7) MME greater than 3 mm (pathological extrusion), and (8) medial knee osteoarthritis grades 1 to 3 according to the Kellgren-Lawrence classification.24 Patients were excluded for (1) obesity (body mass index >30); (2) surgical medial meniscal injury, previous meniscal surgery, or meniscal root tears; (3) unstable knee; (4) inflammatory and systemic disease; (5) concomitant surgery in the same knee; (6) other orthopaedic changes in the same limb; (7) loss to follow-up; and (8) refusal to participate. After screening criteria were applied, 66 patients were eligible for the study (Figure 1).
Figure 1.
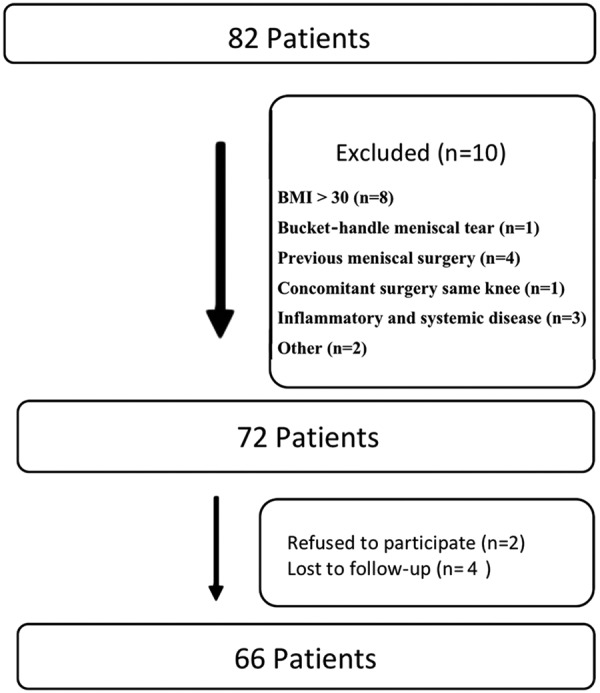
Flowchart of selection for all patients evaluated. BMI, body mass index. A few patients fulfill more than one exclusion criteria during sample selection.
MRI and Radiographic Evaluation
Varus deformity was measured with a single-cassette, full-length, anterior-posterior standing radiograph of the bilateral lower extremities. The weightbearing line method divides the tibial plateau from 0% to 100% (medial to lateral). The angle of desired correction is the angle formed by lines from a 62% point in the tibial plateau to (1) the center of the femoral head and (2) the center of the ankle.8
MME was measured before HTO and at 6-week follow-up (study protocol) through use of magnetic resonance imaging (MRI) by 2 experienced radiologists, both of whom were blinded to patient information. The measurements were made on the MRI coronal view of the medial meniscus showing the best image of the tibial eminence, in accordance with the techniques proposed by Hada et al14 and Roos et al.22 The intraclass correlation coefficient (ICC) was used for interrater and intrarater reliability analyses.20 To assess intrarater reliability, 1 radiologist repeated all measurements 2 weeks later. The ICC for meniscal extrusion was 0.89 (95% CI, 0.86-0.91) for interrater reliability and 0.94 (95% CI, 0.91-0.96) for intrarater reliability.
In the supine position, patients underwent MRI after a 2-hour rest.1 On a T2-weighted midcoronal plane—the slice with the largest area of the medial tibial eminence—a line was drawn connecting the femoral and tibial cortices.24 A second line was drawn tangential to the outermost edge of the medial meniscus. Extrusion was considered as the distance between the 2 lines (Figure 2).
Figure 2.
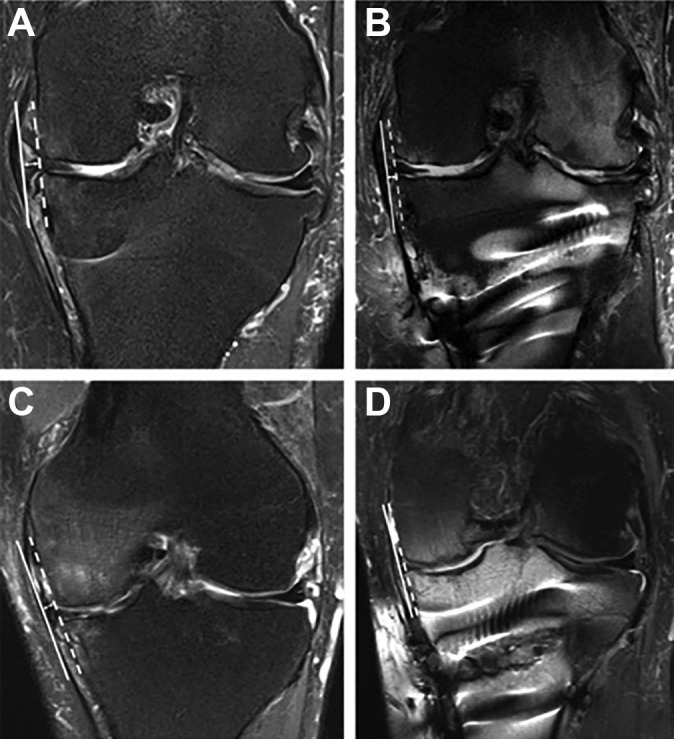
Preoperative (A and C) and postoperative (B and D) measurements of medial meniscal extrusion: coronal section of meniscus showing the best image of the tibial eminence. A tangent line was drawn from the edge of the medial tibial plateau to the medial femoral condyle (the white dashed line).
Surgical Treatment
Indications for HTO surgeries were (1) age younger than 59 years, (2) varus malalignment more than 15°, (3) isolated medial compartment knee pain, (4) knee ROM greater than 120°, and (5) no patellofemoral symptoms. All surgeries were performed by single fellowship-trained knee surgeon. A medial opening wedge HTO was performed carefully to correct malalignment to the predetermined size. Fixation was carried out through use of either a Puddu plate (Arthrex) (38 patients) or a TomoFix plate (Synthes) (28 patients). All defects created by osteotomy were filled with iliac crest bone autograft. After surgery, ROM was not limited. Weightbearing was not allowed for 4 weeks. Cryotherapy was started within the first 24 hours, and continuous passive motion was used to increase knee ROM during the first 5 days, combined with exercises for quadriceps activation. Subsequently, rehabilitation exercises were carried out to strengthen the quadriceps, gain ROM, and improve proprioception. All patients underwent the same postoperative protocol. Return to sports was allowed at least 6 months after surgery.
Clinical and Functional Assessment
The Knee injury and Osteoarthritis Outcome Score (KOOS),22 visual analog scale (VAS) score for pain,15 and Tegner score25 were obtained preoperatively and 2 years after surgery. A second comparison with evaluated scores was made according to MME value after HTO surgery: <1.5 mm and ≥1.5 mm of MME.
Statistical Analysis
A descriptive analysis was carried out (means, standard deviations, quartiles, maximum and minimum values) for each variable. For qualitative variables, the absolute and relative frequencies were calculated. A paired t test was used to compare MME preoperatively and postoperatively.2 The Pearson correlation coefficient was used to measure the degree of relationship between scores.2 The statistical analysis was carried out using SPSS Version 17.0 for Windows (SPSS Inc). Considering the reduction of MME after HTO as the main analyzed outcome, for a power analysis of 80% with a 5% level of significance, a patient sample size of 62 was needed.
Results
Table 1 shows the final sample characteristics. The mean ± SD preoperative and postoperative MME values were 3.9 ± 0.6 mm and 0.9 ± 0.5 mm, respectively. Tegner scores, total KOOS, and all 5 KOOS subscales were higher and VAS scores were lower 2 years after surgery than preoperatively (P < .001) (Table 2). Patients with MME of less than 1.5 mm at 6 weeks after surgery had better postoperative KOOS (P < .001), postoperative VAS pain score (P < .001), and postoperative Tegner score (P < .001) than patients with MME of 1.5 mm or more (Table 3). No demographic differences were found between patients with MME less than 1.5 mm and those with MME 1.5 mm or more.
TABLE 1.
Patient Data (N = 66)a
| Value | P Value | |
|---|---|---|
| Sex | <.05 | |
| Male | 53 (80.3) | |
| Female | 13 (19.7) | |
| Knee side | >.05 | |
| Right | 35 (53) | |
| Left | 31 (47) | |
| Age, y | 47.5 ± 8.4 | |
| Follow-up, mo | 24 | |
| Body mass index, kg/m2 | 26 ± 3.2 |
aValues are presented as n (%) or mean ± SD.
TABLE 2.
Clinical Outcomes and Return to Activity After Medial Opening Wedge High Tibial Osteotomya
| Preoperative (N = 66) |
Postoperative (N = 66) |
P Value | |
|---|---|---|---|
| KOOS | 28.6 ± 3.2 | 76.7 ± 5.3 | <.001 |
| KOOS Symptoms | 29.6 ± 6.5 | 76.9 ± 7.6 | <.001 |
| KOOS Pain | 28.3 ± 5.5 | 75.2 ± 8.1 | <.001 |
| KOOS ADL | 28.9 ± 6.6 | 76.9 ± 7.6 | <.001 |
| KOOS Sport/Rec | 27.4 ± 8.1 | 77.3 ± 7.3 | <.001 |
| KOOS QOL | 28.9 ± 8.1 | 77.0 ± 7.6 | <.001 |
| Pain VAS | 8.3 ± 1.3 | 3.5 ± 1.7 | <.001 |
| Tegner | 1.4 ± 0.5 (min 1; max 2) |
4.2 ± 0.9 (min 2; max 6) |
<.001 |
aValues are presented as mean ± SD. ADL, Activities of Daily Living; Sport/Rec, Sports and Recreation; KOOS, Knee injury and Osteoarthritis Outcome Score; QOL, Quality of Life; VAS, visual analog scale.
TABLE 3.
Clinical Outcomes and Return to Activity After Medial Opening Wedge High Tibial Osteotomy, Presented According to Amount of Medial Meniscal Extrusiona
| Assessment Point | <1.5 mm (n = 47) |
≥1.5 mm (n = 19) |
P Value | |
|---|---|---|---|---|
| KOOS | Preoperative | 26.6 ± 3.6 | 28.8 ± 2.1 | .6 |
| Postoperative | 79.6 ± 2.2 | 69.5 ± 3.3 | <.001 | |
| Pain VAS | Preoperative | 8.0 ± 1.4 | 8.5 ± 0.5 | .8 |
| Postoperative | 2.2 ±1.2 | 3.7 ± 1.2 | <.001 | |
| Tegner | Preoperative | 1.4 ± 0.5 | 1.4 ± 0.5 | .72 |
| Postoperative | 4.2 ± 0.9 | 3.2 ± 0.4 | <.001 |
aValues are presented as mean ± SD. KOOS, Knee injury and Osteoarthritis Outcome Score; VAS, visual analog scale.
No significant correlation was found between evaluated KOOS, VAS, and Tegner scores and the size of the opening wedge.
Discussion
The main finding of the present study was that medial opening wedge HTO decreased MME and improved clinical outcomes and return to activity.
MME is the result of increased pressure and repetitive stresses that can severely weaken the meniscus tissue during the inflammatory process caused by osteoarthritis.9,12 Although the results of most studies corroborate the hypothesis that MME is a risk factor for the development of osteoarthritis, there is no proven and accurate value that may differentiate meniscal extrusion as a pathological fact from a true pathological condition.
Crema et al7 aimed to establish a relationship between medial opening wedge HTO and the decrease of meniscal extrusion by using validated scores (KOOS, pain VAS, and Tegner) 2 years after surgery. Those investigators evaluated 2131 knees and found an association between knee varus malalignment and meniscal extrusion, inferring that MME is probably an effect of the complex interactions among joint tissues and mechanical stresses involved in osteoarthritis.3 However, little is known about the outcomes of meniscal extrusion correction and whether medial opening HTO changes MME. Bastard et al3 observed that 73.3% of patients submitted to medial opening HTO (mean follow-up, 1.3 years) resumed their sports activities at their preoperative level, and 23.3% resumed at a higher level. In a meta-analysis, Hoorntje et al16 concluded that 8 of 10 patients returned to sport and work after knee osteotomy. The time to return to work varied from 10 to 22 weeks, and almost all patients returned to the same or higher workload. In the present study, KOOS, pain VAS, and Tegner scores improved at 2 years of follow-up.
Previous research has arbitrarily divided extrusion as less than 3 mm and more than 3 mm, correlating with arthritic changes,6 but there is no strong evidence that this number should be considered as a cut-off to define a pathological MME.2,7,13 In the present study, all patients had postoperative MME of less than 3 mm, which can explain the improved clinical outcomes and return to activity after medial opening wedge HTO. We also evaluated the differences between values of less than 3 mm. Patients with postoperative MME of less than 1.5 mm had better KOOS, pain VAS, and Tegner scores compared with patients who had postoperative MME of 1.5 mm or more.
This study has limitations. One limitation is that MRI was performed with patients in the supine position rather than weightbearing, which may underestimate the amount of MME. However, no previous study has analyzed meniscal extrusion other than in the meniscus body; thus, only meniscal extrusion in the meniscus body was measured in the present study so that we could compare results with other studies on this subject in the literature.
Conclusion
In the present study, medial opening wedge HTO decreased MME after 6 weeks and improved clinical outcomes and return to activity at a minimum of 2 years of follow-up. Additionally, patients with postoperative MME of less than 1.5 mm had better clinical outcomes and return to activity compared with patients who had postoperative MME of 1.5 mm or more.
Footnotes
Final revision submitted November 27, 2019; accepted December 3, 2019.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital Israelita Albert Einstein–São Paulo (ref No. 3.183.085).
References
- 1. Achtnich A, Petersen W, Willinger L, et al. Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2282–2288. [DOI] [PubMed] [Google Scholar]
- 2. Antony B, Driban JB, Price LL, et al. The relationship between meniscal pathology and osteoarthritis depends on the type of meniscal damage visible on magnetic resonance images: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2017;25(1):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bastard C, Mirouse G, Potage D, et al. Return to sports and quality of life after high tibial osteotomy in patients under 60 years of age. Orthop Traumatol Surg Res. 2017;103(8):1189–1191. [DOI] [PubMed] [Google Scholar]
- 4. Bloecker K, Guermazi A, Wirth W, et al. Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing—data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2013;21:419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boxheimer L, Lutz AM, Treiber K, Goepfert K, Crook DW. MR imaging of the knee: position related changes of the menisci in asymptomatic volunteers. Invest Radiol. 2004;39:254–263. [DOI] [PubMed] [Google Scholar]
- 6. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183:17–23. [DOI] [PubMed] [Google Scholar]
- 7. Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology. 2012;264(2):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248–264. [PubMed] [Google Scholar]
- 9. Ekhtiari S, Haldane CE, de Sa D, Simunovic N, Musahl V, Ayeni OR. Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am. 2016;98(18):1568–1577. [DOI] [PubMed] [Google Scholar]
- 10. Erquicia J, Gelber PE, Cardona-Muñoz JI, Pelfort X, Tey M, Monllau JC. There is no relation between mild malalignment and meniscal extrusion in trauma emergency patients. Injury. 2012;43(2):68–72. [DOI] [PubMed] [Google Scholar]
- 11. Falah M, Nierenberg G, Soudry M, Hayden M, Volpin G. Treatment of articular cartilage lesions of the knee. Int Orthop. 2010;34(5):621–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Faschingbauer M, Nelitz M, Urlaub S, Reichel H, Dornacher D. Return to work and sporting activities after high tibial osteotomy. Int Orthop. 2015;39(8):1527–1534. [DOI] [PubMed] [Google Scholar]
- 13. Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29(4):295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hada S, Ishijima M, Kaneko H, et al. Association of medial meniscal extrusion with medial tibial osteophyte distance detected by T2 mapping MRI in patients with early-stage knee osteoarthritis. Arthritis Res Ther. 2017;19(1):201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heller GZ, Manuguerra M, Chow R. How to analyze the visual analogue scale: myths, truths and clinical relevance. Scand J Pain. 2016;13:67–75. [DOI] [PubMed] [Google Scholar]
- 16. Hoorntje A, Witjes S, Kuijer PPFM, et al. High rates of return to sports activities and work after osteotomies around the knee: a systematic review and meta-analysis. Sports Med. 2017;47(11):2219–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kijima H, Yamada S, Nozaka K, Saito H, Shimada Y. Relationship between pain and medial meniscal extrusion in knee osteoarthritis. Adv Orthop. 2015;2015:210972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim SJ, Choi CH, Chun YM, et al. Relationship between preoperative extrusion of the medial meniscus and surgical outcomes after partial meniscectomy. Am J Sports Med. 2017;45(8):1864–1871. [DOI] [PubMed] [Google Scholar]
- 20. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Narazaki S, Furumatsu T, Tanaka T, Fujii M, Miyazawa S, Inoue H. Postoperative change in the length and extrusion of the medial meniscus after anterior cruciate ligament reconstruction. Int Orthop. 2015;39(12):2481–2487. [DOI] [PubMed] [Google Scholar]
- 22. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 23. Saier T, Minzlaff P, Feucht MJ, et al. Health-related quality of life after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):934–942. [DOI] [PubMed] [Google Scholar]
- 24. Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–124. [DOI] [PubMed] [Google Scholar]
- 25. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 26. Zhang F, Kumm J, Svensson F, Turkiewicz A, Frobell R, Englund M. Risk factors for meniscal body extrusion on MRI in subjects free of radiographic knee osteoarthritis: longitudinal data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2016;24(5):801–806. [DOI] [PubMed] [Google Scholar]


