Abstract
The aim of this study was to investigate the utility of incorporating active matrix metalloproteinase-8 (aMMP-8) as a biomarker into the new periodontitis classification system (stage/grade) presented in 2018. This study included 150 Greek adults aged 25–78, of whom 74 were men and 76 women. Participants were tested with an aMMP-8 point-of-care mouthrinse test, after which a full-mouth clinical examination was performed to assess their periodontal and oral health. The aMMP-8 levels in mouthrinse were significantly lower among healthy patients compared with patients in more severe periodontitis stages and grades (Kruskal–Wallis test and Dunn–Bonferroni test for pairwise post-hoc comparisons; p < 0.01 and p < 0.05, respectively). Furthermore, aMMP-8 levels were less correlated with plaque levels than bleeding on probing (BOP) (Spearman’s rho = 0.269, p < 0.001; Spearman’s rho = 0.586, p < 0.001); respectively). Thus, aMMP-8 was more robust to the confounding effects of oral hygiene than traditional periodontal parameter bleeding on probing. The aMMP-8 point-of-care mouthrinse test can be utilized as an adjunctive and preventive diagnostic tool to identify periodontal disease, classified by stage and grade, and ongoing periodontal breakdown chairside in clinical practice in only 5 min. Overall, integrating aMMP-8 into the new periodontitis classification system seems beneficial.
Keywords: periodontitis, diagnosis, matrix metalloproteinase 8, biomarkers, molecular diagnostics, periodontal diseases, point-of-care testing
1. Main text
A new revised periodontitis case definition system was introduced in 2018 to define periodontitis more appropriately by its stage (the severity and extent of periodontal tissue destruction and complexity of management), and grade (the future risk of progression) [1]. One of its main goals is to provide dentists a framework for individualized identification, treatment and prevention of periodontitis in patients. In addition, it provides a necessary and very much needed framework for the introduction of diagnostic and prognostic biomarkers to extend and improve the information provided by the standard clinical measures.
As Tonetti et al. [1] note, there are some limitations regarding reliance on bleeding on probing (BOP) and other traditional measures in periodontitis diagnostics. For example, some of them are very much influenced by the level of training and experience of operator (i.e., periodontal probing) [1]. Furthermore, the clinical measurements provide mainly retrospective evidence of the severity and extent of periodontal breakdown but are limited methods to assess and predict the risk for on-going and future periodontal breakdown [2]. That stems from the nature of periodontitis to progress episodically, as the quiescent and active periods alternate [2]. Periodontal breakdown does not always follow such geometric or arithmetic calculations or linear patterns that are accurately measurable by radiographic bone loss and/or clinical attachment loss (CAL).
The new periodontitis classification system includes grading parameters to assess the future risk of periodontitis progression. Although they are associated with periodontitis and increase the likelihood of future periodontal breakdown, they cannot be considered to be reliable enough to indicate when periodontitis is in its active phase. This applies to even the grade modifiers smoking and diabetes that are well-known risk factors for periodontitis [3,4,5]. The current grading parameters are mainly able to predict that it is likely that the periodontal breakdown occurs in the future, but not the exact time when it is occurring. In this regard, the future inclusion of more robust biomarkers to the classification system is still anticipated in order to identify patients in active periods of periodontitis (= ongoing periodontal breakdown) and to be able to monitor disease progression and treatment responses more accurately [1].
Oral fluids have been studied intensively to find suitable biomarkers from saliva and gingival crevicular fluid (GCF) for the diagnostics of periodontitis. One of the most studied biomarkers is matrix metalloproteinase-8 (MMP-8). Several studies (for example Lee et al. [6], Romanelli et al. [7], Kiili et al. [8], Sorsa et al. [9], and Alassiri et al. [10]) have demonstrated how elevated levels of active matrix metalloproteinase-8 (aMMP-8), but not total or latent MMP-8, differentiate periodontitis from gingivitis, and precede periodontal attachment loss. Furthermore, active periodontal tissue destruction in progress (i.e., the active phase of periodontal disease) can be identified non-invasively in oral fluids as a pathological elevation of aMMP-8 levels [11,12,13]. Thus, it is no surprise that the aMMP-8 chairside/point-of-care (PoC) oral fluid tests have continuously been successful in identifying active periodontal tissue destruction and active periodontal disease (periodontitis, peri-implantitis, subclinical periodontitis) among adults and adolescents of different ethnic populations [10,12,14,15,16,17,18,19,20,21,22,23,24,25,26]. Similarly, previous longitudinal studies have shown that aMMP-8 assays with the same antibody can be used for predicting the progression of periodontitis and attachment loss, and monitoring treatment of periodontitis during the maintenance phase [27,28,29,30,31,32,33,34].
Many other potential biomarkers to detect periodontitis and related systemic diseases have been investigated as well [35,36,37,38,39,40,41,42,43]; these include, along with others, asymmetric dimethylarginine (ADMA), C-reactive protein, interferon gamma (IFN-γ), interleukin-6 (IL-6), macrophage inflammatory protein-1α (MIP-1α), PMN elastase, vitamin C and also antioxidants [35,36,37,38,39,40,41,42,43]. For example, vitamin C is linked to oxidative MMP-activation cascade by its recorded ability to prevent the oxidative activation of proMMP-8 [44]. According to a recent systematic review, aMMP-8/MMP-8 is currently the most accurate diagnostic biomarker in GCF for periodontitis in systemically healthy patients [35]. In saliva, aMMP-8/MMP-8 is also among the best five biomarkers, and the combination of aMMP-8/MMP-8 and IL-6 seems the most promising salivary diagnostic marker for periodontitis [36,37].
In this short communication, the aim is to study the usefulness of aMMP-8 as the stage and grade biomarker for the new periodontitis classification system [1]. Our hypothesis is that aMMP-8 levels among 150 Greek adults, measured by a quantitative aMMP-8 point-of-care (PoC)/chairside mouthrinse test, are positively associated with the severity of periodontal disease (stage) and possible risk for disease progression (grade).
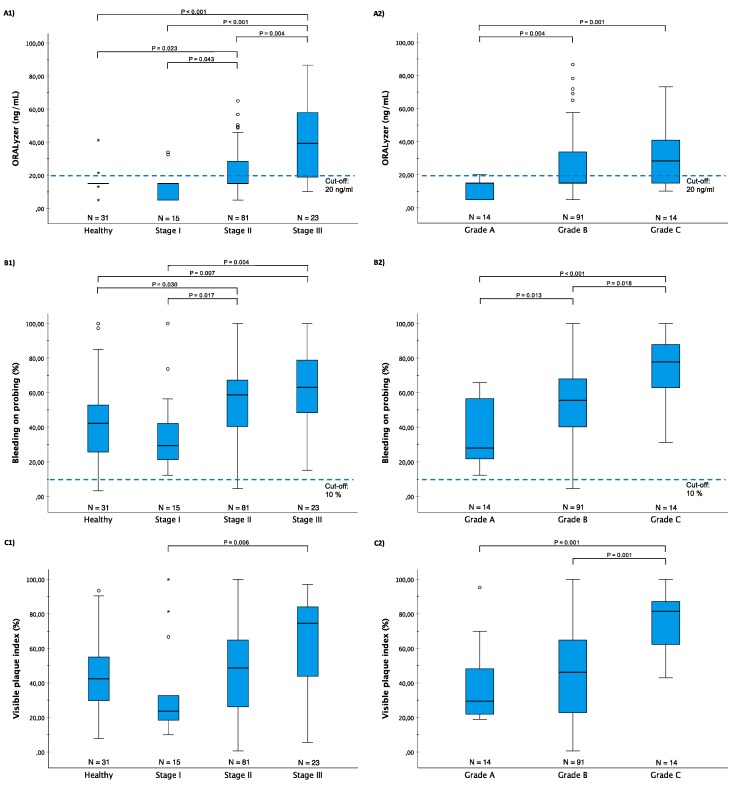
Figure 1 demonstrates the aMMP-8 levels, as well as bleeding on probing (BOP), and visual plaque index (VPI) levels among 150 Greek patients classified by the new classification system [1]. The participants were selected among the patients of the Periodontology University Clinic, Thessaloniki, Greece, as described earlier [26]. They had no underlying diseases and no medications (antibiotics, anti-inflammatory drugs etc.) were in use for the last 3 months before their examination (more information about patient characteristics in Table 1). Patients’ aMMP-8 levels were determined by the aMMP-8 PoC/chairside mouthrinse test, PerioSafe®, in combination with a digital reader, ORALyzer®, following the manufacturer’s instructions [10,14,24]. A.G. performed a full-mouth clinical examination for each patient to assess their periodontal and oral health, after which each patient’s aMMP-8 mouthrinse test result was read.
Figure 1.
(A) ORALyzer (ng/mL), (B) bleeding on probing (BOP) (%) and (C) visual plaque index (VPI) (%) vs. (1) periodontitis stages and (2) periodontitis grades (N = 150) described by Tonetti et al. [1]. Kruskal–Wallis test was significant (p < 0.01) for all the three variables in both cases. All significant (p < 0.05) pairwise post hoc comparisons (Dunn–Bonferroni test) are marked in the plots. The box-and-whiskers plots illustrate the median, quartiles, and extreme values. Previously validated cut-off of 20 ng/mL for aMMP-8 assays [10] and cut-off of 10% for BOP [1,49] marked in the figure.
Table 1.
Patient characteristics (N = 150 Greek adults).
| Healthy | Stage I | Stage II | Stage III | p-Value | Grade A | Grade B | Grade C | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Sex (N) | 0.003 a | ||||||||
| Women | 11 | 14 | 39 | 12 | 12 | 47 | 6 | 0.038 a | |
| Men | 20 | 1 | 42 | 11 | 2 | 44 | 8 | ||
| Age mean (SD) | 43.32 (12.78) | 61.64 (8.10) | 54.96 (9.83) | 56.00 (9.61) | <0.001 b | 60.64 (11.17) | 55.03 (9.54) | 57.21 (8.85) | 0.200 b |
| Education level (N) | <0.001 a | 0.065 a | |||||||
| Elementary | 0 | 1 | 2 | 0 | 0 | 1 | 2 | ||
| Middle | 2 | 8 | 41 | 19 | 10 | 48 | 10 | ||
| Post graduate Studies | 9 | 1 | 4 | 0 | 0 | 5 | 0 | ||
| Technical school | 0 | 0 | 3 | 31 | 0 | 4 | 0 | ||
| University | 20 | 5 | 31 | 3 | 4 | 33 | 2 | ||
| Annual dental visit (N) | 0.051 a | 0.680 a | |||||||
| Yes | 19 | 14 | 45 | 13 | 9 | 56 | 7 | ||
| No | 12 | 1 | 36 | 10 | 5 | 35 | 7 | ||
| Smoking (N) | 0.088 a | 0.290 a | |||||||
| Yes | 6 | 8 | 26 | 10 | 3 | 34 | 7 | ||
| No | 25 | 7 | 55 | 13 | 11 | 57 | 7 | ||
| Normal BMI (N) | 0.171 a | 0.641 a | |||||||
| Yes | 9 | 1 | 21 | 9 | 4 | 22 | 5 | ||
| No | 22 | 14 | 60 | 14 | 10 | 69 | 9 |
N: frequency; SD: standard deviation; BMI: body mass index; a Pearson Chi-squared test (asymptotic, 2-sided). b Welch t-test.
Firstly, aMMP-8 levels in mouthrinse were significantly lower among healthy patients compared with patients in more severe periodontitis stages and grades (Kruskal–Wallis test, p < 0.01; Figure 1), as would be expected from an effective diagnostic tool to classify periodontal health and disease [14,15,16,17,18,19,20,21,22,23,24,25,26]. This result is also in agreement with previous studies that have shown that aMMP-8 predicts very well future periodontal breakdown (positive predictive values range between 81.8%–94.7%) [35]. Secondly, BOP and VPI levels were also associated with the periodontitis stage and grade (Kruskal–Wallis test, p < 0.01); Figure 1), but these two parameters were also moderately correlated with each other (Spearman’s rho = 0.586, p < 0.001). The association between dental plaque levels and BOP levels and their potential confounding is well understood in the literature [45]. Previous studies have also shown that BOP poorly predicts future periodontal breakdown (positive predictive value for repeated incidence of BOP was ≤ 30%), but the continuous absence of BOP correlates much better with periodontal stability [2,45,46,47,48]. For example, Joss et al. [48] suggested a cut-off of 20% for BOP, while in the new classification system a threshold of 10% for BOP is suggested to define periodontal health [49]. However, as Figure 1 shows, despite the positive association between BOP and both stage and grade, the two cut-offs are likely to cause a large number of false positives. This seems to apply to VPI as well (see Figure 1), for example, when considering a good oral hygiene as a prerequisite for periodontal health and using a low cut-off for VPI. It is noteworthy that plaque assessments are not considered as an effective measure of periodontitis [50,51,52]. According to Lang et al. [45], dental plaque determines only 20% of the direct risk of the development of periodontitis.
Finally, in this sample, the range of BOP and VPI levels were wide among healthy patients compared with the diseased patients (stage I–III and Grades A–C). Regarding periodontitis patients, the same applies to BOP and VPI levels among Grade A patients when compared to Grade B patients (Figure 1). This kind of overlapping in BOP and VPI levels between different categories increases the risk for false positive diagnosis, as well. In contrast, the aMMP-8 levels did not exhibit similar overlapping, as BOP and VPI, between the same groups. Furthermore, aMMP-8 levels seemed much more immune to the confounding effects of dental plaque, as the link between aMMP-8 and VPI was somewhat negligible (Spearman’s rho = 0.269, p < 0.001). All in all, aMMP-8 was the preferable method for differentiating periodontal health and disease, because the risk of false positives seemed generally much lower for aMMP-8 than BOP or VPI (see Figure 1).
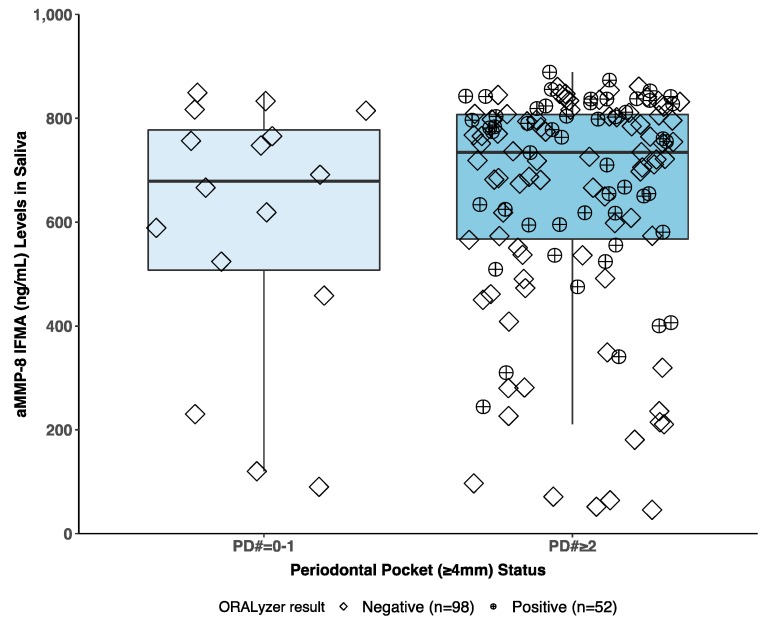
Our findings indicate that the aMMP-8 mouthrinse PoC/chairside test [10,12,14,15,16,17,18,19,20,21,22,23,24,25,26] can be implemented as the staging and grading biomarker in the new classification system of periodontitis [1]. In this regard, a previous study by Räisänen et al. [21] showed that mouthrinse aMMP-8 measurements are better and more precise in identifying periodontal health and disease among adolescents in comparison to saliva aMMP-8 measurements. The same result was repeated and further extended in this study by comparing the aMMP-8 PoC/chairside mouthrinse test to salivary aMMP-8 time-resolved immunofluorometric assay (IFMA) measurements, both methods utilizing the same antibody, among this sample of Greek adults (see Figure 2) [10,27,29]. The mouthrinse aMMP-8 measurements performed more precisely and gave no false positives (i.e., no positive aMMP-8 mouthrinse test results among healthy patients). In contrast, IFMA measurements of aMMP-8 levels in saliva offered a less definite classification of periodontal health and disease (Figure 2). As Räisänen et al. [21] suggest, mouthrinse aMMP-8 measurements seem the optimal way of measuring the active periodontal breakdown and risk of the future progression of periodontal disease.
Figure 2.
The concentrations of aMMP-8 (ng/mL) in saliva measured by time-resolved immunofluorometric assay (IFMA) according to patient’s periodontal pocket (≥4 mm) status (zero or one [PD# = 0–1] vs. two or more periodontal pockets [PD# ≥ 2]) categorized by the corresponding ORALyzer test result (cut-off 20 ng/mL) measured from oral mouthrinse. A positive and negative ORALyzer results marked as diamonds and circle-plusses, respectively. N = 150 Greek patients.
The utility of mouthrinse measurements is based on a simple technique to collect and sample gingival crevicular fluid (GCF) [14,21,53], instead of using more laborious filter papers or micropipettes [54]. Moreover, previous studies have also presented a better diagnostic accuracy value of GCF in aMMP-8 measurements in comparison to saliva when classifying periodontal health and disease [35,36,37]. However, it should also be noted that not all commercial kits detect active forms of MMP-8, as the aMMP-8 PoC mouthrinse test and IFMA used in this study do [29]. Instead, some of them detect the total MMP-8, which is not able to detect periodontal breakdown or progression of periodontitis [55,56,57]. This fact may explain the variation in aMMP-8 and MMP-8 results in the literature, in addition to the type of oral fluid used in the testing.
Based on this evidence, therefore, we strongly support the call of Tonetti et al. [1] for a paradigm shift to also consider periodontitis in terms of the inflammatory mediators that are immunoassay measures, offering information that traditionally used diagnostic methods are not able to provide as accurately. We propose aMMP-8 as the biomarker and the aMMP-8 PoC/chairside mouthrinse testing to be incorporated into the new periodontal disease classification system by Tonetti et al. [1] (see Table 2: modified from Tonetti et al. [1]), to improve the diagnostic accuracy of periodontal diseases and their progression. The proposed aMMP-8 measurements by an aMMP-8 PoC mouthrinse test with a cut-off of 20 ng/mL allows this risk to be measured early enough, effectively and non-invasively in clinical practice within 5 min without the need to use laborious and time-consuming laboratory equipment [10,12,14,15,16,17,18,19,20,21,22,23,24,25,26]. The ability to identify active periods of periodontitis (=ongoing periodontal breakdown) chairside and in real-time is of great value to dentists trying to optimize patient treatment. It lets them to monitor disease progression, and treatment responses [10,11,12,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34], which should translate to better treatment outcomes as well. After all, periodontitis does have a negative effect not only to periodontium but also to the whole body by increasing the systemic inflammatory burden and the risk for certain systemic diseases like diabetes [2,4,58]. Finally, in addition to periodontitis, several studies have reported elevated aMMP-8 levels among patients with diabetes (type 1 and 2) [59,60,61,62]. In this regard, the recent study by Grigoriadis et al. [26] demonstrated that aMMP-8 PoC mouthrinse testing is also suitable for prediabetes/diabetes screening at the dental office.
Table 2.
Grading a periodontitis patient (modified from Tonetti et al. [1]) by active matrix metalloproteinase-8 (aMMP-8) as the main biomarker for active/progressing periodontal diseases.
| Grading a Periodontitis Patient by aMMP-8 | Grade A: Slow Rate of Progression | Grade B: Moderate Rate of Progression | Grade C: Rapid Rate of Progression | |
|---|---|---|---|---|
| Indicators of active periodontal tissue destruction/bone loss/clinical attachment loss | Mouthrinse, gingival crevicular fluid | No/slow = aMMP-8 level < 20 ng/mL | Moderate = aMMP-8 level ≥ 20 ng/mL | Rapid = aMMP-8 level > 30 ng/mL |
2. Patents
Timo Sorsa and Dirk-Rolf Gieselmann are inventors of US-patent 10 488 415 B2 and a Japanese patent 2016-554676.
Author Contributions
T.S. contributed by organizing the protocol, data analysis, preparation and revision of the manuscript. S.A. contributed by preparation and revision of the manuscript. A.G. contributed by organizing the protocol, data collection, preparation and revision of the manuscript. I.T.R. and P.P. contributed by data analysis, preparation and revision of the manuscript. S.O.N. and D.-R.G. contributed by preparation and revision of the manuscript. D.S. contributed by organizing the protocol, data collection, preparation and revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Open access funding provided by University of Helsinki. This work was supported by grants from the University of Helsinki Research Foundation (TYH 2016251, TYH 2017251, TYH 2018229, TYH 2019314, Y1014SL017, Y1014SL018, Y1014SULE1), Helsinki, Finland, and the Karolinska Institutet, Stockholm, Sweden, and Yrjö Jahnsson Foundation sr, The Paulo Foundation, Juhani Ahon Lääketieteen Tutkimussäätiö sr, Orion Research Foundation sr, and Helsingin Seudun Hammaslääkärit r.y. (Dentists of Helsinki Region Association), Finland.
Conflicts of Interest
Timo Sorsa and Dirk-Rolf Gieselmann are inventors of US-patent 10 488 415 B2 and a Japanese patent 2016-554676. Other authors report no conflicts of interest related to this study. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Ethical Approval
This study was approved by the Ethics Committee of the School of Dentistry, Aristotle University of Thessaloniki, Thessaloniki, Greece (#64, 12/6/2018), the local ethical committee of Stockholm Community, Sweden (2016-08-24/2016/1:8 and 2016-1-24), and the Helsinki University Central Hospital, Finland (nro260/13/03/00/13). All procedures performed in the present study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and informed written consent was obtained from all individual participants included in the study.
References
- 1.Tonetti M.S., Greenwell H., Kornman K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Clin. Periodontol. 2018;45(Suppl. S20):S149–S161. doi: 10.1111/jcpe.12945. [DOI] [PubMed] [Google Scholar]
- 2.Kinane D.F., Stathopoulou P.G., Papapanou P.N. Periodontal diseases. Nat. Rev. Dis. Primers. 2017;3:17038. doi: 10.1038/nrdp.2017.38. [DOI] [PubMed] [Google Scholar]
- 3.Leite F.R.M., Nascimento G.G., Scheutz F., López R. Effect of Smoking on Periodontitis: A Systematic Review and Meta-regression. Am. J. Prev. Med. 2018;54:831–841. doi: 10.1016/j.amepre.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Cervino G., Terranova A., Briguglio F., De Stefano R., Famà F., D’Amico C., Amoroso G., Marino S., Gorassini F., Mastroieni R., et al. Diabetes: Oral Health Related Quality of Life and Oral Alterations. Biomed. Res. Int. 2019;2019:5907195. doi: 10.1155/2019/5907195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nascimento G.G., Leite F.R.M., Vestergaard P., Scheutz F., López R. Does diabetes increase the risk of periodontitis? A systematic review and meta-regression analysis of longitudinal prospective studies. Acta Diabetol. 2018;55:653–667. doi: 10.1007/s00592-018-1120-4. [DOI] [PubMed] [Google Scholar]
- 6.Lee W., Aitken S., Sodek J., McCulloch C.A. Evidence of a direct relationship between neutrophil collagenase activity and periodontal tissue destruction in vivo: Role of active enzyme in human periodontitis. J. Periodontal. Res. 1995;30:23–33. doi: 10.1111/j.1600-0765.1995.tb01249.x. [DOI] [PubMed] [Google Scholar]
- 7.Romanelli R., Mancini S., Laschinger C., Overall C.M., Sodek J., McCulloch C.A. Activation of Neutrophil Collagenase in Periodontitis. Infect. Immun. 1999;67:2319–2326. doi: 10.1128/IAI.67.5.2319-2326.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiili M., Cox S.W., Chen H.Y., Wahlgren J., Maisi P., Eley B.M., Salo T., Sorsa T. Collagenase-2 (MMP-8) and collagenase-3 (MMP-13) in adult periodontitis: Molecular forms and levels in gingival crevicular fluid and immunolocalisation in gingival tissue. J. Clin. Periodontol. 2002;29:224–232. doi: 10.1034/j.1600-051x.2002.290308.x. [DOI] [PubMed] [Google Scholar]
- 9.Sorsa T., Tjäderhane L., Konttinen Y.T., Lauhio A., Salo T., Lee H.M., Golub L.M., Brown D.L., Mäntylä P. Matrix metalloproteinases: Contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann. Med. 2006;38:306–321. doi: 10.1080/07853890600800103. [DOI] [PubMed] [Google Scholar]
- 10.Alassiri S., Parnanen P., Rathnayake N., Johannsen G., Heikkinen A.M., Lazzara R., van der Schoor P., van der Schoor J.G., Tervahartiala T., Gieselmann D., et al. The Ability of Quantitative, Specific, and Sensitive Point-of-Care/Chair-Side Oral Fluid Immunotests for aMMP-8 to Detect Periodontal and Peri-Implant Diseases. Dis. Mark. 2018;2018:1306396. doi: 10.1155/2018/1306396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorsa T., Gürsoy U.K., Nwhator S., Hernandez M., Tervahartiala T., Leppilahti J., Gürsoy M., Könönen E., Emingil G., Pussinen P.J., et al. Analysis of Matrix Metalloproteinases, Especially MMP-8, in Gingival Crevicular Fluid, Mouthrinse and Saliva for Monitoring Periodontal Diseases. Periodontol. 2000. 2016;70:142–163. doi: 10.1111/prd.12101. [DOI] [PubMed] [Google Scholar]
- 12.Al-Majid A., Alassiri S., Rathnayake N., Tervahartiala T., Gieselmann D.R., Sorsa T. Matrix metalloproteinase-8 as an inflammatory and prevention biomarker in periodontal and peri-implant diseases. Int. J. Dent. 2018;2018:7891323. doi: 10.1155/2018/7891323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L., Li X., Yan H., Huang L. Salivary matrix metalloproteinase (MMP)-8 as a biomarker for periodontitis: A PRISMA-compliant systematic review and meta-analysis. Medicine. 2018;97:e9642. doi: 10.1097/MD.0000000000009642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nwhator S.O., Ayanbadejo P.O., Umeizudike K.A., Opeodu O.I., Agbelusi G.A., Olamijulo J.A., Arowojolu M.O., Sorsa T., Babajide B.S., Opedun D.O. Clinical correlates of a lateral-flow immunoassay oral risk indicator. J. Periodontol. 2014;85:188–194. doi: 10.1902/jop.2013.130116. [DOI] [PubMed] [Google Scholar]
- 15.Izadi Borujeni S., Mayer M., Eickholz P. Activated matrix metalloproteinase-8 in saliva as diagnostic test for periodontal disease? A case-control study. Med. Microbiol. Immunol. 2015;204:665–672. doi: 10.1007/s00430-015-0413-2. [DOI] [PubMed] [Google Scholar]
- 16.Johnson N., Ebersole J.L., Kryscio R.J., Danaher R.J., Dawson D., 3rd, Al-Sabbagh M., Miller C.S. Rapid assessment of salivary MMP-8 and periodontal disease using lateral flow immunoassay. Oral Dis. 2016;22:681–687. doi: 10.1111/odi.12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heikkinen A.M., Nwhator S.O., Rathnayake N., Mäntylä P., Vatanen P., Sorsa T. Pilot study on oral health status as assessed by an active matrix metalloproteinase-8 chairside mouthrinse test in adolescents. J. Periodontol. 2016;87:36–40. doi: 10.1902/jop.2015.150377. [DOI] [PubMed] [Google Scholar]
- 18.Heikkinen A.M., Raivisto T., Kettunen K., Kovanen L., Haukka J., Pakbaznejad Esmaeili E., Elg J., Gieselmann D.R., Rathnayake N., Ruokonen H., et al. Pilot study on the genetic background of an active matrix metalloproteinase-8 test in Finnish adolescents. J. Periodontol. 2017;88:464–472. doi: 10.1902/jop.2016.160441. [DOI] [PubMed] [Google Scholar]
- 19.Lorenz K., Keller T., Noack B., Freitag A., Netuschil L., Hoffmann T. Evaluation of a novel point-of-care test for active matrix metalloproteinase-8: Agreement between qualitative and quantitative measurements and relation to periodontal inflammation. J. Periodontal Res. 2017;52:277–284. doi: 10.1111/jre.12392. [DOI] [PubMed] [Google Scholar]
- 20.Leppilahti J.M., Harjunmaa U., Järnstedt J., Mangani C., Hernández M., Tervahartiala T., Lopez R., Ashorn U., Ashorn P., Gieselmann D.R., et al. Diagnosis of newly delivered mothers for periodontitis with a novel oral-rinse aMMP-8 point-of-care test in a rural Malawian population. Diagnostics. 2018;8:67. doi: 10.3390/diagnostics8030067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Räisänen I.T., Heikkinen A.M., Nwhator S.O., Umeizudike K.A., Tervahartiala T., Sorsa T. On the diagnostic discrimination ability of mouthrinse and salivary aMMP-8 point-of-care testing regarding periodontal health and disease. Diagn. Microbiol. Infect. Dis. 2019;95:114871. doi: 10.1016/j.diagmicrobio.2019.114871. [DOI] [PubMed] [Google Scholar]
- 22.Räisänen I.T., Heikkinen A.M., Pakbaznejad Esmaeili E., Tervahartiala T., Pajukanta R., Silbereisen A., Bostanci N., Sorsa T. A point-of-care test of active matrix metalloproteinase-8 (aMMP-8) predicts triggering receptor expressed on myeloid cells-1 (TREM-1) levels in saliva. J. Periodontol. 2019 doi: 10.1002/JPER.19-0132. [DOI] [PubMed] [Google Scholar]
- 23.Räisänen I.T., Heikkinen A.M., Siren E., Tervahartiala T., Gieselmann D.R., van der Schoor G.J., van der Schoor P., Sorsa T. Point-of-care/chairside aMMP-8 analytics of periodontal diseases’ activity and episodic progression. Diagnostics. 2018;8:74. doi: 10.3390/diagnostics8040074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Räisänen I.T., Sorsa T., van der Schoor G.-J., Tervahartiala T., van der Schoor P., Gieselmann D.R., Heikkinen A.M. Active matrix metalloproteinase-8 point-of-care (PoC)/chairside mouthrinse test vs bleeding on probing in diagnosing subclinical periodontitis in adolescents. Diagnostics. 2019;9:34. doi: 10.3390/diagnostics9010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmalz G., Hübscher A.E., Angermann H., Schmidt J., Schmickler J., Legler T.J., Ziebolz D. Associations of chairside salivary aMMP-8 findings with periodontal parameters, potentially periodontal pathogenic bacteria and selected blood parameters in systemically healthy adults. Diagn. Microbiol. Infect. Dis. 2019;95:179–184. doi: 10.1016/j.diagmicrobio.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Grigoriadis A., Sorsa T., Räisänen I., Pärnänen P., Tervahartiala T., Sakellari D. Prediabetes/diabetes can be screened at the dental office by a low-cost and fast chair-side/point-of-care aMMP-8 immunotest. Diagnostics. 2019;9:151. doi: 10.3390/diagnostics9040151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mäntylä P., Stenman M., Kinane D.F., Tikanoja S., Luoto H., Salo T., Sorsa T. Gingival crevicular fluid collagenase-2 (MMP-8) test stick for chair-side monitoring of periodontitis. J. Periodontal Res. 2003;38:436–439. doi: 10.1034/j.1600-0765.2003.00677.x. [DOI] [PubMed] [Google Scholar]
- 28.Mäntylä P., Stenman M., Kinane D., Salo T., Suomalainen K., Tikanoja S., Sorsa T. Monitoring periodontal disease status in smokers and nonsmokers using a gingival crevicular fluid matrix metalloproteinase-8-specific chair-side test. J. Periodontal Res. 2006;41:503–512. doi: 10.1111/j.1600-0765.2006.00897.x. [DOI] [PubMed] [Google Scholar]
- 29.Sorsa T., Hernández M., Leppilahti J., Munjal S., Netuschil L., Mäntylä P. Detection of gingival crevicular fluid MMP-8 levels with different laboratory and chair-side methods. Oral Dis. 2010;16:39–45. doi: 10.1111/j.1601-0825.2009.01603.x. [DOI] [PubMed] [Google Scholar]
- 30.Sorsa T., Mäntylä P., Tervahartiala T., Pussinen P.J., Gamonal J., Hernandez M. MMP activation in diagnostics of periodontitis and systemic inflammation. J. Clin. Periodontol. 2011;38:817–819. doi: 10.1111/j.1600-051X.2011.01753.x. [DOI] [PubMed] [Google Scholar]
- 31.Leppilahti J.M., Kallio M.A., Tervahartiala T., Sorsa T., Mäntylä P. Gingival crevicular fluid matrix metalloproteinase-8 levels predict treatment outcome among smokers with chronic periodontitis. J. Periodontol. 2014;85:250–260. doi: 10.1902/jop.2013.130156. [DOI] [PubMed] [Google Scholar]
- 32.Leppilahti J.M., Hernández-Ríos P.A., Gamonal J.A., Tervahartiala T., Brignardello-Petersen R., Mantyla P., Sorsa T., Hernández M. Matrix metalloproteinases and myeloperoxidase in gingival crevicular fluid provide site-specific diagnostic value for chronic periodontitis. J. Clin. Periodontol. 2014;41:348–356. doi: 10.1111/jcpe.12223. [DOI] [PubMed] [Google Scholar]
- 33.Leppilahti J.M., Sorsa T., Kallio M.A., Tervahartiala T., Emingil G., Han B., Mäntylä P. The utility of gingival crevicular fluid matrix metalloproteinase-8 response patterns in prediction of site-level clinical treatment outcome. J. Periodontol. 2015;86:777–787. doi: 10.1902/jop.2015.140421. [DOI] [PubMed] [Google Scholar]
- 34.Raivisto T., Sorsa T., Räisänen I., Kauppila T., Ruokonen H., Tervahartiala T., Haukka J., Heikkinen A.M. Active Matrix Metalloproteinase-8 Chair Side Mouth Rinse Test, Health Behaviour and Oral Health in Finnish Adolescent Cohort. J. Clin. Diagn. Res. 2019 doi: 10.7860/JCDR/2020/43031.13467. [DOI] [Google Scholar]
- 35.Arias-Bujanda N., Regueira-Iglesias A., Balsa-Castro C., Nibali L., Donos N., Tomás I. Accuracy of single molecular biomarkers in gingival crevicular fluid for the diagnosis of periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2019;46:1166–1182. doi: 10.1111/jcpe.13188. [DOI] [PubMed] [Google Scholar]
- 36.Arias-Bujanda N., Regueira-Iglesias A., Balsa-Castro C., Nibali L., Donos N., Tomás I. Accuracy of single molecular biomarkers in saliva for the diagnosis of periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2020;47:2–18. doi: 10.1111/jcpe.13202. [DOI] [PubMed] [Google Scholar]
- 37.Sukriti K.C., Wang X.Z., Gallagher J.E. Diagnostic sensitivity and specificity of host-derived salivary biomarkers in periodontal disease amongst adults: Systematic review. J. Clin. Periodontol. 2019 doi: 10.1111/jcpe.13218. [DOI] [PubMed] [Google Scholar]
- 38.Ebersole J.L., Nagarajan R., Akers D., Miller C.S. Targeted salivary biomarkers for discrimination of periodontal health and disease(s) Front. Cell. Infect. Microbiol. 2015;5:62. doi: 10.3389/fcimb.2015.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fiorillo L., Cervino G., Herford A.S., Lauritano F., D’Amico C., Lo Giudice R., Laino L., Troiano G., Crimi S., Cicciù M. Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. Int. J. Mol. Sci. 2018;19:1908. doi: 10.3390/ijms19071908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Isola G., Polizzi A., Muraglie S., Leonardi R., Lo Giudice A. Assessment of Vitamin C and Antioxidant Profiles in Saliva and Serum in Patients with Periodontitis and Ischemic Heart Disease. Nutrients. 2019;11:2956. doi: 10.3390/nu11122956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Isola G., Alibrandi A., Currò M., Matarese M., Ricca S., Matarese G., Ientile R., Kocher T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020 doi: 10.1002/JPER.19-0446. [DOI] [PubMed] [Google Scholar]
- 42.Gul S.S., Douglas C.W.I., Griffiths G.S., Rawlinson A. A pilot study of active enzyme levels in gingival crevicular fluid of patients with chronic periodontal disease. J. Clin. Periodontol. 2016;43:629–636. doi: 10.1111/jcpe.12568. [DOI] [PubMed] [Google Scholar]
- 43.Tada A., Miura H. The Relationship between Vitamin C and Periodontal Diseases: A Systematic Review. Int. J. Environ. Res. Public Health. 2019;16:2472. doi: 10.3390/ijerph16142472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suomalainen K., Sorsa T., Lindy O., Saari H., Konttinen Y.T., Uitto V.J. Hypochlorous acid induced activation of human neutrophil and gingival crevicular fluid collagenase can be inhibited by ascorbate. Scand. J. Dent. Res. 1991;99:397–405. doi: 10.1111/j.1600-0722.1991.tb01047.x. [DOI] [PubMed] [Google Scholar]
- 45.Lang N.P., Bartold P.M. Periodontal health. J. Periodontol. 2018;89(Suppl. S1):S9–S16. doi: 10.1002/JPER.16-0517. [DOI] [PubMed] [Google Scholar]
- 46.Lang N.P., Joss A., Orsanic T., Gusberti F.A., Siegrist B.E. Bleeding on probing. A predictor for the progression of periodontal disease? J. Clin. Periodontol. 1986;13:590–596. doi: 10.1111/j.1600-051X.1986.tb00852.x. [DOI] [PubMed] [Google Scholar]
- 47.Lang N.P., Adler R., Joss A., Nyman S. Absence of bleeding on probing. An indicator of periodontal stability. J. Clin. Periodontol. 1990;17:714–721. doi: 10.1111/j.1600-051X.1990.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 48.Joss A., Adler R., Lang N.P. Bleeding on probing. A parameter for monitoring periodontal conditions in clinical practice. J. Clin. Periodontol. 1994;21:402–408. doi: 10.1111/j.1600-051X.1994.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 49.Tonetti M.S., Sanz M. Implementation of the new classification of periodontal diseases: Decision-making algorithms for clinical practice and education. J. Clin. Periodontol. 2019;46:398–405. doi: 10.1111/jcpe.13104. [DOI] [PubMed] [Google Scholar]
- 50.Claffey N., Nylund K., Kiger R., Garrett S., Egelberg J. Diagnostic predictability of scores of plaque, bleeding, suppuration and probing depth for probing attachment loss. 3 1/2 years of observation following initial periodontal therapy. J. Clin. Periodontol. 1990;17:108–114. doi: 10.1111/j.1600-051X.1990.tb01071.x. [DOI] [PubMed] [Google Scholar]
- 51.Grossi S.G., Zambon J.J., Ho A.W., Koch G., Dunford R.G., Machtei E.E., Norderyd O.M., Genco R.J. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J. Periodontol. 1994;65:260–267. doi: 10.1902/jop.1994.65.3.260. [DOI] [PubMed] [Google Scholar]
- 52.Hujoel P.P., Cunha-Cruz J., Loesche W.J., Robertson P.B. Personal oral hygiene and chronic periodontitis: A systematic review. Periodontol. 2000. 2005;37:29–34. doi: 10.1111/j.1600-0757.2004.03795.x. [DOI] [PubMed] [Google Scholar]
- 53.Gangbar S., Overall C.M., McCulloch C.A., Sodek J. Identification of polymorphonuclear leukocyte collagenase and gelatinase activities in mouthrinse samples: Correlation with periodontal disease activity in adult and juvenile periodontitis. J. Periodontal. Res. 1990;25:257–267. doi: 10.1111/j.1600-0765.1990.tb00914.x. [DOI] [PubMed] [Google Scholar]
- 54.Rathnayake N., Gieselmann D.R., Heikkinen A.M., Tervahartiala T., Sorsa T. Salivary diagnostics-point-of-care diagnostics of MMP-8 in dentistry and medicine. Diagnostics. 2017;7:7. doi: 10.3390/diagnostics7010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leppilahti J.M., Ahonen M.M., Hernández M., Munjal S., Netuschil L., Uitto V.J., Mäntylä P. Oral rinse MMP-8 point-of-care immuno test identifies patients with strong periodontal inflammatory burden. Oral Dis. 2011;17:115–122. doi: 10.1111/j.1601-0825.2010.01716.x. [DOI] [PubMed] [Google Scholar]
- 56.Romero-Castro N.S., Vázquez-Villamar M., Muñoz-Valle J.F., Reyes-Fernández S., Serna-Radilla V.O., García-Arellano S., Castro-Alarcón N. Relationship between TNF-α, MMP-8, and MMP-9 levels in gingival crevicular fluid and the subgingival microbiota in periodontal disease. Odontology. 2019 doi: 10.1007/s10266-019-00435-5. [DOI] [PubMed] [Google Scholar]
- 57.Sorsa T., Gieselmann D.-R., Korvuo A., Maier K., Mäntylä P., Råman I., Tiisala S. MMP-8 Activation Product, Its Determination and Use. No. 10,488,415. U.S. Patent. 2019 Nov 26;
- 58.Fiorillo L. Oral Health: The First Step to Well-Being. Medicina. 2019;55:676. doi: 10.3390/medicina55100676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sorsa T., Ingman T., Suomalainen K., Halinen S., Saari H., Konttinen Y.T., Uitto V.-J., Golub L.M. Cellular source and tetracycline-inhibition of gingival crevicular fluid collagenase of patients with labile diabetes mellitus. J. Clin. Periodontol. 1992;19:146–149. doi: 10.1111/j.1600-051X.1992.tb00454.x. [DOI] [PubMed] [Google Scholar]
- 60.Ryan M.E., Ramamurthy N.S., Sorsa T., Golub L.M. MMP-mediated events in diabetes. Ann. N. Y. Acad. Sci. 1999;878:311–334. doi: 10.1111/j.1749-6632.1999.tb07692.x. [DOI] [PubMed] [Google Scholar]
- 61.Safkan-Seppälä B., Sorsa T., Tervahartiala T., Beklen A., Konttinen Y.T. Collagenases in gingival crevicular fluid in type 1 diabetes mellitus. J. Periodontol. 2006;77:189–194. doi: 10.1902/jop.2006.040322. [DOI] [PubMed] [Google Scholar]
- 62.Rathnayake N., Akerman S., Klinge B., Lundegren N., Jansson H., Tryselius Y., Sorsa T., Gustafsson A. Salivary biomarkers for detection of systemic diseases. PLoS ONE. 2013;8:e61356. doi: 10.1371/journal.pone.0061356. [DOI] [PMC free article] [PubMed] [Google Scholar]