Abstract
Nine of the fourteen states that have not expanded Medicaid are in the southern census region, and two other nonexpansion states border that region. Ongoing debate over the merits of Medicaid expansion in these states has focused, in part, on whether the safety net provides sufficient access for uninsured low-income Americans. We analyzed longitudinal survey and vital status data from the twelve-state Southern Community Cohort Study (SCCS) for 15,356 nonelderly adult participants with low incomes, 86 percent of whom were enrolled at community health centers. In difference-in-differences analyses, we compared changes in self-reported health between participants in four expansion and eight nonexpansion states before (2008–13) and after (2015–17) Medicaid expansion. We found that a higher proportion of SCCS participants in expansion states reported increases in Medicaid coverage (a differential change of 7.6 percentage points), a lower proportion experienced a health status decline (−1.8 percentage points), and a higher proportion maintained their baseline health status (1.4 percentage points). The magnitude of estimated reductions in health declines would meaningfully affect a nonexpansion state’s health ranking in our sample if that state elected to expand Medicaid. Our results suggest that for low-income adults in the South, Medicaid expansions yielded health benefits—even for those with established access to safety-net care.
Since 2014, thirty-four states have accepted federal Medicaid funding provided through the Affordable Care Act (ACA) to expand eligibility to adults with incomes up to 138 percent of the federal poverty level who are not pregnant, elderly, or disabled. Studies of the ACA’s Medicaid expansion have found clear improvements in access to care and reductions in financial strain among low-income populations.1–5 However, the effects of the expansion on the health of low-income adults remain unclear. While some studies have found modest improvements in self-reported health,6–12 a recent review determined that 60 percent of all assessments of health status did not find evidence of changes associated with Medicaid expansion.5
A possible explanation for the equivocal evidence of health improvements is that care financed by the Medicaid expansion was already accessible via safety-net providers and as uncompensated or charity care.13,14 Under this interpretation, Medicaid expansion may have shifted the financing of care without conferring additional health benefits. An alternative explanation is that studies of post-ACA Medicaid expansions have studied the general population of adults who are eligible for Medicaid, many of whom are young and relatively healthy.15 These studies may not have been able to detect health status changes among chronically or acutely ill adults who would forgo or delay getting medically necessary care without coverage.
In this study, we examined Medicaid expansions in the South, home to nearly half of the nation’s uninsured population before the ACA.16,17 Using longitudinal data from the Southern Community Cohort Study (SCCS), the largest epidemiologic study cohort of low-income adults recruited in the US, we assessed changes in mental and physical health after Medicaid expansion.18 Recruited primarily at community health clinics in twelve states, SCCS participants have particularly low incomes and are older and have considerably higher mortality, morbidity, and uninsurance rates than the low-income population in general. These characteristics, coupled with the variation in state decisions to implement the ACA’s Medicaid expansion, facilitated our assessment of the impact of Medicaid on health in a large sample of low-income adults with high health needs and established use of safety-net providers.
Study Data And Methods
Study Population
In the period 2001–09, the SCCS enrolled 84,513 participants ages 40–79 from twelve states: Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia. Two of these states (Kentucky and West Virginia) expanded their Medicaid programs in 2014, one (Arkansas) used Medicaid expansion funds starting in 2014 to subsidize private coverage for individuals and families with incomes less than 138 percent of poverty, one (Louisiana) expanded its Medicaid program in 2016, and one (Virginia) expanded its program in 2019. We categorized the four states that expanded before 2017 as expansion states for our analysis. Eighty-six percent of the participants were recruited in community health centers and completed a baseline survey in person at the time of enrollment via standardized computer-assisted interviews. The remaining 14 percent were recruited via sampling of the general population in SCCS states and completed the baseline survey by mail. People who did not speak English were excluded from recruitment into the SCCS. In addition, since a major goal of the SCCS was to capture incident cases of cancer, people who had been treated for cancer (excluding nonmelanoma skin cancer) during the year before possible enrollment were also excluded. The detailed baseline survey collected information on a broad set of social and health-related characteristics, including demographics, income, medical history, and health insurance coverage.
Subsequent information was obtained through mailed follow-up surveys and administrative linkages to vital status data. Participants who did not respond to mailed questionnaires were contacted by telephone up to eight times. Additional details on the recruitment and sampling of SCCS participants are reported elsewhere.18–20
The SCCS has fielded four follow-up surveys: Follow-up 1 was administered from 2008 to 2013, follow-up 2 from 2012 to 2015, follow-up 3 from 2015 to 2017, and follow-up 4 from 2018 to 2020. Our study sample included participants who responded to follow-up 1, the first participant survey that included the Medical Outcomes Study 12-Item Short-Form General Health Survey (SF-12).21 We used data from follow-up 3 to assess health insurance coverage and health status after the implementation of state Medicaid expansions. Neither the baseline nor follow-up 2 surveys included SF-12, and follow-up 4 was still in the field at the time of our analysis.
Of follow-up 1 respondents in nonexpansion and expansion states, 54.7 percent and 58.5 percent, respectively, responded to follow-up 3, 12.3 percent and 11.2 percent died before completing follow-up 3, and 33.0 percent and 30.3 percent did not respond to it. Consistent with low-income populations generally,22 the SCCS cohort reported highly variable annual household incomes, though most participants never reported an income above $50,000 (approximately 400 percent of poverty for an individual and 300 percent of poverty for a married couple). Therefore, we included in our sample follow-up 1 respondents who reported incomes of less than 400 percent of poverty, but not those with incomes below a lower poverty threshold consistent with Medicaid eligibility, to capture adults who were intermittently eligible for Medicaid and those who may have gained subsidized coverage as a result of Medicaid expansion outreach. We also limited the sample to people who were alive as of the earliest Medicaid expansion date (January 1, 2014) and were ages sixty-two or younger as of that date—thereby excluding people who aged into Medicare eligibility before 2016. All follow-up 1 respondents who died after January 1, 2014, were included in study cohort, whether or not they responded to follow-up 3. The final cohort included 15,356 adults (see figure e1 in the online appendix).23
The SCCS, including this ancillary study, was approved by Institutional Review Boards at Vanderbilt University Medical Center and Meharry Medical College. All participants provided written consent upon study enrollment.
Study Variables
Outcomes
The three primary outcomes were self-reported overall health status, physical health status, and mental health status. To derive effect estimates, we separately analyzed changes for each SF-12 item and averaged estimates across the items included in the overall, physical, and mental health composites (for details on our composite measures, seewe the appendix).23 We also analyzed survival and modeled death jointly with health status, as explained below. In addition, we examined self-reported health insurance coverage at the time of the survey, grouping respondents into mutually exclusive categories based on the following hierarchy: private insurance, Medicaid only, Medicare (including people dually eligible for Medicaid), military insurance, other insurance, and uninsured.
Covariates
From the baseline and follow-up 1 surveys, we obtained pre-expansion information on age, sex, marital status, race (African American, white, or other), education, employment status, and medical history (for a detailed list of medical history measures, see the appendix).23 Missing data on covariates due to item nonresponse (the rates ranged from 0.9 percent to 10.5 percent) were imputed using chained equations.24,25
Statistical Analysis
We conducted a difference-in-differences analysis to estimate changes in outcomes in the four expansion states relative to concurrent changes in outcomes in the eight nonexpansion states. Estimating the health effects of Medicaid expansions using the SF-12 presented two analytic challenges. First, responses to SF-12 questions are ordinal, which makes interpreting changes across different categories difficult. For example, the proportion reporting “good” general health in the post-expansion period reflects health maintenance (that is, remaining in good health), health improvements (for example, transitions to good health from fair or poor health), and health declines (such as transitions from excellent or very good health to good health). Second, only living participants can report their health status, and coverage expansions may have had different effects on participants in better versus those in worse health.26,27 If coverage expansions disproportionately improved survival among participants in fair or poor health, an analysis that ignored deaths (for example, by excluding decedents) might erroneously conclude that expansions worsened health status.
To address these challenges, we explicitly modeled health status transitions and incorporated death as a category for each categorical outcome. Specifically, for each SF-12 item, we jointly fitted a set of linear probability models that included a model for each of the possible response categories and a model for death (a linear equivalent of a multinomial model). These difference-in-difference models included interactions between respondents’ pre-expansion responses and all terms in the model, thereby estimating the differential change from each response category to each of the other categories.
From the adjusted estimates of differential changes for each transition type and the pre-expansion distribution across health status categories, we produced summary estimates of the differences between expansion and nonexpansion states in the percentages of the sample experiencing each of the following health status sequences: no change in health status, health improvement, and health decline. We considered death as a health decline in our main analysis and also analyzed deaths separately in a supplementary analysis (see eFigures 6 and 7 in the appendix).23
To estimate expansion-related differences in overall, physical, and mental health changes, we averaged these summary difference-in-difference estimates across the relevant SF-12 items. We also report estimates for each SF-12 item to describe their contribution to the overall estimates (see appendix tables e13 and e14).23 To convey the magnitude of difference-in-differences estimates, we examined how they would have altered a state’s ranking in the distribution of eight nonexpansion states’ rates of health declines or improvements in our sample.
Exact Inference Approach
Our statistical inferences were based on an exact inference procedure that allowed us to analyze our observational data like a cluster-randomized trial. We adopted this approach because the intervention was applied at the group (state) level and because standard inference approaches for group-level interventions yield high false discovery rates when the number of treated clusters is small.28–32 Specifically, for all estimates, we fitted the statistical model separately for all 495 possible combinations of four treated (expansion) states and eight untreated (nonexpansion) states (for more details on our inference approach, see the appendix).23 We quantified the extremeness of observed results based on percentile rank. Ranks of 100.0 (that is, 495 out of 495) or 0.2 (1 out of 495) were the most extreme values in the distribution.
Assessing Assumptions Of Difference-In-Differences Analysis
Attributing differential changes to the coverage expansions assumed that changes in health over the study period would have been similar in expansion and nonexpansion states in the absence of expansions. To assess the plausibility of this assumption, we compared health trends for the SF-12 outcomes between expansion and nonexpansion states in the pre-expansion period. If the trends were similar, that would support the assumption. To assess preperiod trends, we leveraged the staggered timing of follow-up 1 for subgroups of the SCCS cohort from 2008 to 2011. We found no evidence of different trends between expansion and nonexpansion states (see the appendix).23 As a secondary check, we also tested whether pre-expansion mortality trends differed. This allowed us to assess differences in health trends between the groups that would have been manifested as differences in survival trends. We found no evidence for differences in survival in the pre-expansion period either (see appendix eTable 6 and eFigure 6).23 Finally, our approach to inference provided an additional assessment of the difference-in-differences assumptions. As we note regarding threats to validity of our difference-in-differences approach in the “Discussion” section, this method allowed us to gauge the plausibility of a scenario in which our results were due to differences in preperiod health trends or other time-varying confounders.
Sensitivity Analyses
We conducted several sensitivity analyses. First, we reestimated models without including participant covariates to gauge potential bias from regression to the mean when adjusting for baseline values of time-varying characteristics or from differential nonresponse to follow-up 3 when not adjusting for participant characteristics.33 Second, we added interactions between time and covariates found to differ at baseline to adjust for differences in health trends predicted by the covariates. Third, we reestimated models using survey nonresponse weights constructed from a wide array of participant characteristics collected by the baseline and follow-up 1 surveys. Fourth, we repeated our analysis with a multinomial logit differences-in-differences model, rather than a linear probability model as used in our main results. Fifth, we repeated our analyses including the sample of people alive as of January 1, 2010 (versus including only those alive as of January 1, 2014, as in our main results), which was the sample inclusion criteria used to assess mortality trends in the pre-expansion period. Sixth, we conducted an analysis that excluded Louisiana, since that state expanded Medicaid in mid-2016—about half-way through our post-expansion surveying period. Finally, in addition to our primary approach for addressing death as a competing risk, we also estimated models using principal stratification methods.27,34 This approach isolated estimates to the stratum of adults who would have survived with or without the Medicaid expansion and thereby minimized potential bias from death as a source of missing data on health outcomes (for more details on our principal stratification approach, see the appendix).23
Limitations
Our study had several limitations, some of which we take up in greater detail below in cases where our findings offer insights or can mitigate concerns. First, because the SCCS included limited assessments of health care use and barriers to care, we could not directly examine the potential mechanisms that could explain how expanding Medicaid improved the health trajectory of low-income adults.
Second, it is possible that the differential changes in self-reported health we report could be explained by unmeasured factors other than Medicaid expansion.
Third, we were limited to one pre-Medicaid expansion observation of health status, which limited our ability to investigate pre-expansion trend differences between expansion and nonexpansion states. We discuss approaches we used to investigate the potential role of nonparallel trends in our difference-in-differences study design in the “Discussion” section below and in greater detail in the appendix.23
Fourth, because of our focus on the SCCS cohort that was primarily recruited from community health centers, our findings may not be generalizable to low-income people who did not have a usual source of care.
Study Results
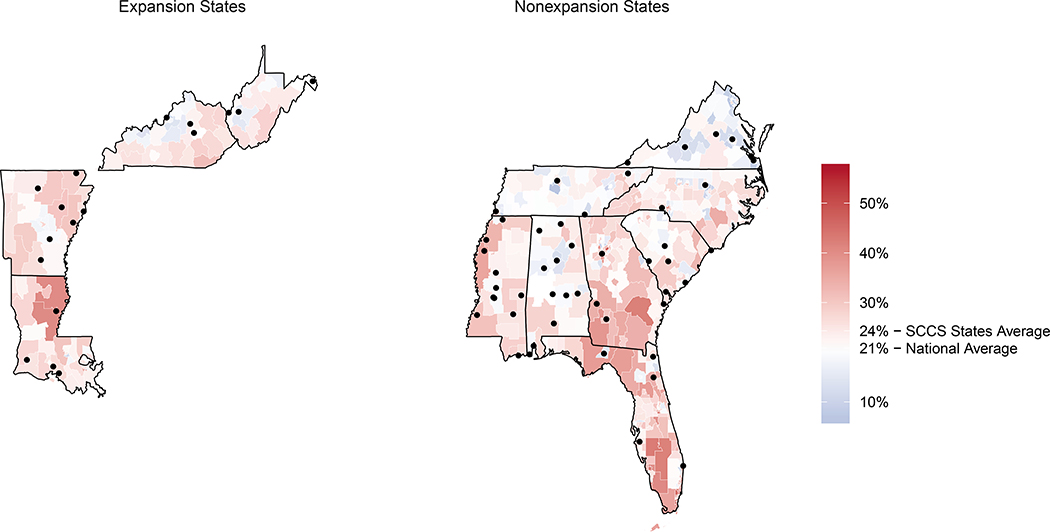
Exhibit 1 shows the geographic locations of SCCS recruitment clinics overlaid on local 2013 uninsurance rates among nonelderly adults. Baseline (pre-expansion) sociodemographic and health characteristics did not differ substantially between the SCCS expansion and nonexpansion state samples, with one exception: Owing to the concentration of nonexpansion states in the Deep South,35 African Americans were more prominently represented in nonexpansion states than in expansion states (73 percent versus 44 percent) (exhibit 2).
Exhibit 1:
Locations of Southern Community Cohort Study (SCCS) recruitment health clinics and 2013 uninsurance rates among nonelderly adults, by study state Medicaid expansion status
SOURCE Authors’ analysis of Southern Community Cohort administrative data and 2013 data on uninsurance rates from the American Community Survey. NOTES The study states that expanded eligibility for Medicaid and those that did not are listed in the text. The circles indicate the clinic locations.
Exhibit 2:
Baseline characteristics of Medicaid expansion and nonexpansion study state samples
| Nonexpansion state sample (n = 11,679) | Expansion state sample (n = 3,677) | ||||
|---|---|---|---|---|---|
| Characteristic | No. or mean | % or SD | No. or mean | % or SD | Standardized mean difference |
| Mean age (years) | 51.6 | 4.1 | 51.7 | 4.3 | 0.036 |
| Male | 3,648 | 31.2% | 1,137 | 30.9% | 0.007 |
| African American | 8,565 | 73.3 | 1,601 | 43.5 | 0.634 |
| Highest level of education | 0.069 | ||||
| Less than high school | 2,436 | 20.9 | 668 | 18.2 | |
| High school or GED | 4,052 | 34.7 | 1,315 | 35.8 | |
| Vocational school or some college | 3,629 | 31.1 | 1,169 | 31.8 | |
| College degree or higher | 1,562 | 13.4 | 525 | 14.3 | |
| Marital status | 0.207 | ||||
| Married or living as married with a partner | 4,147 | 35.5 | 1,621 | 44.1 | |
| Separated or divorced | 3,886 | 33.3 | 1,188 | 32.3 | |
| Widowed | 754 | 6.5 | 215 | 5.8 | |
| Single, never married | 2,892 | 24.8 | 653 | 17.8 | |
| Employment status | 0.168 | ||||
| Working full time | 3,453 | 29.6 | 1,244 | 33.8 | |
| Working part time | 1,246 | 10.7 | 328 | 8.9 | |
| Unemployed | 2,228 | 19.1 | 542 | 14.7 | |
| On disability | 4,055 | 34.7 | 1,255 | 34.1 | |
| Retired | 254 | 0.2 | 110 | 3.0 | |
| Housewife | 443 | 3.8 | 198 | 5.4 | |
| Household income ($) | 0.197 | ||||
| 15,000 or less | 6,352 | 54.4 | 1,755 | 47.7 | |
| 15,001–25,000 | 2,402 | 20.6 | 725 | 19.7 | |
| 25,001–50,000 | 2,000 | 17.1 | 710 | 19.3 | |
| 50,001 or more | 925 | 7.9 | 487 | 13.2 | |
| General health status | 0.072 | ||||
| Excellent | 576 | 4.9 | 187 | 5.1 | |
| Very good | 2,073 | 17.7 | 694 | 18.9 | |
| Good | 4,300 | 36.8 | 1,326 | 36.1 | |
| Fair | 3,698 | 31.7 | 1,085 | 29.5 | |
| Poor | 1,032 | 8.8 | 385 | 10.5 | |
| History of: | |||||
| Cancer | 1,597 | 13.7 | 546 | 14.8 | 0.034 |
| Heart attack or myocardial infarction | 387 | 3.3 | 138 | 3.8 | 0.024 |
| Stroke | 315 | 2.7 | 89 | 2.4 | 0.018 |
| Diabetes | 3,404 | 29.1 | 995 | 27.1 | 0.046 |
| Takes aspirin | 4,441 | 38 | 1,476 | 40.1 | 0.043 |
SOURCE Authors’ analysis of Southern Community Cohort Study data. NOTES The study states that expanded eligibility for Medicaid and those that did not are listed in the text. SD is standard deviation.
Changes In Insurance Coverage
In the post-expansion period, 18.7 percent of expansion state SCCS participants reported having Medicaid coverage (data not shown). This was a differential increase of 7.6 percentage points compared to that in the nonexpansion states (exhibit 3). The estimated increase in Medicaid coverage in expansion states was the most extreme estimate among all possible combinations of the four treated and eight untreated states. Nearly all of the increase in Medicaid coverage was attributable to the differential decline in self-reported uninsured status of 7.0 percentage points.
Exhibit 3:
Changes in type of health insurance coverage among Southern Community Cohort Study participants in Medicaid expansion states associated with expansion
| Difference-in-differences | |||
|---|---|---|---|
| Type of insurance | Baseline (%) | Estimate | Percentile rank |
| Private | 30.8 | 0.06 | 52.3 |
| Medicaid | 10.6 | 7.6 | 100.0 |
| Medicare | 20.1 | −0.19 | 37.4 |
| Military | 2.3 | −0.63 | 0.2 |
| Other | 6.2 | 0.32 | 73.5 |
| Uninsured | 30.0 | −7.0 | 0.2 |
SOURCE Authors’ analysis of Southern Community Cohort Study data. NOTES The study states that expanded eligibility for Medicaid and those that did not are listed in the text. The difference-in-differences estimates are of the differential change in the category associated with the Medicaid expansion. The percentile ranks of the difference-in-differences estimates in the distribution of those estimates were generated from models fitted to all 495 possible combinations of four treated (expansion) and eight untreated (nonexpansion) states. The most extreme of the 495 values on each end of the distribution correspond to percentile ranks of 0.2 and 100.0. As noted in the text, mortality was included as a possible outcome category, but the estimates for mortality outcomes were excluded from this table. Separate estimates for mortality are reported in the appendix (see note 23 in text).
Changes In Health Status
Absent expansion, an expected 38.1 percent of cohort participants in expansion states would have experienced a health status decline (exhibit 4). Under expansion, however, 36.3 percent experienced a decline—a reduction of 1.8 percentage points (exhibit 4). This reduction in health status declines was explained by fewer transitions to health states with severe physical and mental health limitations as opposed to fewer transitions from health states with no limitations to health states with moderate limitations (see appendix eTables 9 and 10).23 Based on the distribution of rates of health declines from the pre to the post period among nonexpansion states (exhibit 5), this differential reduction in health declines would be analogous to the eighth (worst) ranked state (Tennessee) moving to the position of fifth, or the fourth ranked state (Mississippi) moving to the top position.
Exhibit 4:
Changes in health status among Southern Community Cohort Study participants in Medicaid expansion states from before to after expansion, by type of health
| Difference-in-differences | ||||
|---|---|---|---|---|
| Percentage experiencing change with expansion | Counterfactual percentage experiencing change without expansion | Estimate | Percentile rank | |
| Overall health | ||||
| No change | 40.2 | 38.8 | 1.4 | 100.0 |
| Improvement | 23.5 | 23.1 | 0.45 | 90.3 |
| Decline | 36.3 | 38.1 | −1.8 | 0.2 |
| Physical health | ||||
| No change | 41.5 | 39.6 | 1.9 | 100.0 |
| Improvement | 21.3 | 21.1 | 0.17 | 64.2 |
| Decline | 37.2 | 39.2 | −2.0 | 0.2 |
| Mental health | ||||
| No change | 37.8 | 36.3 | 1.5 | 100.0 |
| Improvement | 25.5 | 24.9 | 0.62 | 97.8 |
| Decline | 36.8 | 38.9 | −2.1 | 0.2 |
SOURCE Authors’ analysis of Southern Community Cohort Study data. NOTES The study states that expanded eligibility for Medicaid and those that did not are listed in the text. The counterfactual expected percentages are based on the observed change over time in the control group (which consisted of participants in nonexpansion states). The difference-in-differences estimates and percentile ranks are explained in the notes to exhibit 3. As noted in the text, mortality was included in the categories of declining health. Separate results for mortality are reported in the appendix (see note 23 in text).
Exhibit 5:
Changes in health status among Southern Community Cohort Study participants in Medicaid nonexpansion states from before to after expansion, by state
| Health status (%) | ||||
|---|---|---|---|---|
| No change | Improvement | Decline | State rank in declining health | |
| South Carolina | 43.3 | 23.3 | 33.4 | 1 |
| North Carolina | 42.4 | 22.9 | 34.7 | 2 |
| Virginia | 42.1 | 23.3 | 34.7 | 3 |
| Mississippi | 40.8 | 24 | 35.2 | 4 |
| Florida | 40.5 | 23.4 | 36.1 | 5 |
| Georgia | 40.6 | 22.6 | 36.8 | 6 |
| Alabama | 38.3 | 24.3 | 37.3 | 7 |
| Tennessee | 39.4 | 23.1 | 37.5 | 8 |
SOURCE Authors’ analysis of Southern Community Cohort Study data. NOTES Virginia had not yet expanded its Medicaid program during our study period, so it is included as a nonexpansion state here. As noted in the text, mortality was included in the category of declining health. Separate results for mortality are reported in the appendix (see note 23 in text).
We also found a 1.4-percentage-point differential increase in the proportion of participants reporting that they had maintained the same level of health (exhibit 4). Findings were similar for SF-12 items pertaining to physical and mental health.
Changes In Survival
We did not find evidence of differences in survival between expansion and nonexpansion states in the post-expansion period when we used a parametric regression approach (the difference-in-differences estimate for expansion versus nonexpansion states was an increase of 0.23 percentage points, and the percentile rank was 33.5) or nonparametric (Kaplan-Meier) methods (the difference in survival was an increase of 0.20 percentage points, and the percentile rank was 84.0) (see appendix eFigure 7).23
Sensitivity Analyses
Differential changes in many of the individual SF-12 items contributed to our summary estimates of self-reported health changes (see appendix eTables 13 and 14).23 For example, estimates of reductions in health declines of 1.0 percentage points or more were observed for ten of the twelve SF-12 items. Results and inferences were substantively similar when we used a multinomial logit model specification (appendix eTable 2),23 excluded all baseline covariates from the analysis (appendix eTable 15),23 added an interaction between race and time to account for possible time-varying confounding linked with racial differences in our sample (appendix eTable 15),23 and used principal stratification to address truncation of health outcomes by death (appendix eTable 8).23 Finally, our estimates for health status declines (−2.3 percentage points, with a percentile rank of 0.2), health status improvements (0.72 percentage points, with a percentile rank of 100.0), and maintenance of health status (1.5 percentage points) were larger in magnitude when we excluded participants from Louisiana, which expanded Medicaid half-way through our post-2014 surveying period (appendix eTable 15).23
Discussion
In a low-income cohort of older nonelderly adults in the South with high rates of disability, poor health, chronic disease, and uninsurance, self-reported health declined more slowly over time for people who lived in states that implemented ACA provisions to expand Medicaid than for people in other southern states. Adults in expansion states also were more likely to maintain their baseline health status.
We observed favorable differential changes in health in expansion states for measures of both mental and physical health, including SF-12 items that assessed limitations in physical activities (for example, pushing a vacuum cleaner) and limitations from pain. These items related to physical functioning may be less likely than mental health items to be influenced by improvements in financial security or access to care without accompanying changes in clinical outcomes. Thus, our findings build on prior studies that found improvements in self-reported health status associated with Medicaid expansions.6,8–12 Those studies were limited in their ability to assess effects of the expansions on physical functioning or clinical outcomes because they lacked either measures of specific functional limitations or lacked statistical power to detect meaningful changes in chronic disease control.
Our findings raise the natural question of what mechanisms could explain how expanded Medicaid improved the health trajectory of low-income adults. One such mechanism is expanded access to specialty care. Safety-net clinics, including community health clinics and federally qualified health centers, primarily provide primary care services. Although up to 25 percent of visits to safety-net clinics identified the need for specialty follow-up care,36,37 access to specialty care among uninsured patients of safety-net providers is poor.38 Often, access to specialty care services is conditional on the ability of uninsured people to pay for care up front. In contrast, specialty care is a covered benefit with limited or no cost sharing under Medicaid. Similarly, uninsured adults cannot rely on outpatient safety-net clinics for inpatient care, many procedures, or prescription drugs.
A related mechanism is expanded access to transportation services under Medicaid. Access to both primary and specialty care services is poor in rural and underserved areas, and the lack of viable transportation options is a frequently cited reason for delays in seeking care.39 Importantly, transportation services are a covered benefit under Medicaid. More timely use of care and fewer delays in seeking treatment due to expanded access to transportation services under Medicaid also could have contributed to our findings. Because the SCCS included limited assessments of health care use and barriers to care, we could not examine these potential mechanisms empirically.
As noted above, our study had several other limitations. First, it is possible that differential improvements in self-reported health were due to changes in factors other than Medicaid expansion. For example, the baseline racial composition of our sample differed across state expansion status. Differences in race may predict different changes in health for expansion and nonexpansion states. Population characteristics may have differentially changed in expansion states relative to nonexpansion states. However, our findings were nearly identical in sensitivity analyses that excluded all patient controls (including race) and that adjusted for differences in health trends associated with differences in race. Moreover, the lower rate of health declines in expansion states was the most extreme value in the distribution of estimates generated by permuting state expansion status in our main results and in all sensitivity analyses. Thus, to explain the “extremeness” of our findings, an unmeasured time-varying confounder would have to be ordered perfectly with state expansion decisions.
Second, health status was assessed in the SCCS cohort only once per respondent before the ACA’s Medicaid expansion. Nevertheless, we did not find evidence of differing pre-expansion trends between expansion and nonexpansion states in health reported by subsamples surveyed from 2008 to 2011. Trends in mortality also did not differ over the four-year pre-expansion period. In addition, the “extremeness” of our estimates relative to all possible expansion state combinations also makes it unlikely that the continuation of differences in pre-expansion health trends (a time-varying confounder) could fully explain our findings. Such an explanation would require the four SCCS states with the most favorable pre-expansion health trends to be the four that elected to expand Medicaid. It is unlikely that expansion decisions sorted systematically with health trends, because state expansion decisions were mostly political.
Finally, our analysis produced estimates of the effects of Medicaid expansion averaged across the low-income, non-elderly SCCS cohort, only some of whom obtained coverage due to expansion. Overall, we found that expansion was associated with a 7.0-percentage-point differential decline in uninsured status and a 1.8-percentage-point differential decline in the probability of experiencing worsening health status. If these health changes are attributable entirely to gains in coverage among the otherwise uninsured, this implies that 257 fewer people experienced a health status decline for every 1,000 people who gained coverage ([1.8/7.0] × 1,000)]. However, Medicaid expansion both increased coverage among the previously uninsured and improved continuity of coverage among those already insured.40–42 Both of these factors could plausibly affect health, so assuming health status changes were mediated entirely by differential gains in coverage may overstate the magnitude of health changes attributable to gains in coverage. Expressing the differential reduction in health declines in terms of state rankings provides a more conservative and interpretable assessment of the population health benefits associated with expansion.
Policy Implications And Conclusion
As of late 2019, nine of the fourteen remaining nonexpansion states are in the southern census region, and two other nonexpansion states border that region. Ongoing debate over the merits of Medicaid expansion in these states has focused, in part, on whether the safety net and other forms of implicit insurance (for example, charity and uncompensated care as well as the US bankruptcy system) provide sufficient financial protection for uninsured low-income Americans.
Our study was ideally suited to answer this question because the study cohort was mostly recruited from community health centers in primarily rural areas of the South. In addition, the adult population we considered was older and sicker than general uninsured populations are. Within this population with established safety-net access and high health care needs, we found that Medicaid expansion was associated with lower rates of self-reported health declines and a higher likelihood of maintaining baseline health status over time. These findings suggest that access to safety-net providers in southern states is an inadequate substitute for health insurance coverage. Thus, nonexpanding southern states could improve the health of their low-income residents by accepting expansion funds or otherwise extending coverage to low-income residents.
Supplementary Material
Acknowledgment
An earlier version of this article was presented at the 2019 AcademyHealth Annual Research Meeting in Washington, DC. This work was funded by the National Cancer Institute (Grant No. NIH 5R01 CA189152-05). The authors are grateful for research support from Zilu Zhou, who provided analytic support for this project. The authors also thank Mark Steinwandel and anonymous reviewers from the Southern Community Cohort Study manuscript and statistical review panel for helpful guidance and comments on this work.
Bios for 2019-00929_Graves
Bio 1: John A. Graves (john.graves@vanderbilt.edu) is an associate professor in the Department of Health Policy, Vanderbilt University School of Medicine, in Nashville, Tennessee.
Bio 2: Laura A. Hatfield is an associate professor in the Department of Health Care Policy, Harvard Medical School, in Boston, Massachusetts.
Bio 3: William Blot is a professor of medicine in the Vanderbilt University School of Medicine.
Bio 4: Nancy L. Keating is a professor of health care policy and medicine in the Department of Health Care Policy, Harvard Medical School and the Division of General Internal Medicine at Brigham and Women’s Hospital, both in Boston.
Bio 5: J. Michael McWilliams is the Warren Alpert Foundation Professor of Health Care Policy, Department of Health Care Policy, Harvard Medical School.
Notes
- 1.Hu L, Kaestner R, Mazumder B, Miller S, Wong A. The effect of the Affordable Care Act Medicaid expansions on financial wellbeing. J Public Econ. 2018;163:99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller S, Hu L, Kaestner R, Mazumder B, Wong A. The ACA Medicaid expansion in Michigan and financial health [Internet]. Cambridge (MA): National Bureau of Economic Research; [revised 2019 Sep; cited 2019 Nov 5]. (NBER Working Paper No. 25053). Available from: https://www.nber.org/papers/w25053.pdf [Google Scholar]
- 3.Brevoort K, Grodzicki D, Hackmann MB. Medicaid and financial health [Internet]. Cambridge (MA): National Bureau of Economic Research; 2017. November [cited 2019 Nov 5]. (NBER Working Paper No. 24002). Available from: https://www.nber.org/papers/w24002.pdf [Google Scholar]
- 4.Caswell KJ, Waidmann TA. The Affordable Care Act Medicaid expansions and personal finance. Med Care Res Rev. 2019;76(5):538–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazurenko O, Balio CP, Agarwal R, Carroll AE, Menachemi N. The effects of Medicaid expansion under the ACA: a systematic review. Health Aff (Millwood). 2018;37(6):944–50. [DOI] [PubMed] [Google Scholar]
- 6.Sommers BD, Maylone B, Blendon RJ, Orav EJ, Epstein AM. Three-year impacts of the Affordable Care Act: improved medical care and health among low-income adults. Health Aff (Millwood). 2017;36(6):1119–28. [DOI] [PubMed] [Google Scholar]
- 7.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–9. [DOI] [PubMed] [Google Scholar]
- 8.Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2):390–417. [DOI] [PubMed] [Google Scholar]
- 9.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early effects of the Affordable Care Act on health care access, risky health behaviors, and self-assessed health. South Econ J. 2018;84(3):660–91. [Google Scholar]
- 10.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947–56. [DOI] [PubMed] [Google Scholar]
- 11.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein A, Taubman S, Wright B, Bernstein M, Gruber J, Newhouse JP, et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finkelstein A, Hendren N, Luttmer EFP. The value of Medicaid: interpreting results from the Oregon Health Insurance Experiment [Internet]. Cambridge (MA): National Bureau of Economic Research; 2015. June [cited 2019 Nov 5]. (NBER Working Paper No. 21308). Available from: https://www.nber.org/papers/w21308.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finkelstein A, Mahoney N, Notowidigdo MJ. What does (formal) health insurance do, and for whom? [Internet]. Cambridge (MA): National Bureau of Economic Research; 2017. August [cited 2019 Nov 5]. (NBER Working Paper No. 23718). Available from: https://www.nber.org/papers/w23718.pdf [Google Scholar]
- 15.Institute of Medicine. Coverage matters: insurance and health care. Chapter 3: who goes without health insurance? Who is most likely to be uninsured? Washington (DC): National Academies Press; 2001. [PubMed] [Google Scholar]
- 16.Henry J Kaiser Family Foundation. Health insurance coverage of the total population [Internet]. San Francisco (CA): KFF; 2017. [cited 2019 Nov 5]. Available from: http://kff.org/other/state-indicator/total-population/?currentTimeframe=0&selectedDistributions=non-group [Google Scholar]
- 17. For this analysis we aggregated the total 2013 uninsured population in the southern census region, which consists of sixteen states plus the District of Columbia. However, as noted in the text, our analysis focused on the twelve states covered in the Southern Community Cohort (listed in text).
- 18.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21(1, Suppl):26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conway BN, Han X, Munro HM, Gross AL, Shu XO, Hargreaves MK, et al. The obesity epidemic and rising diabetes incidence in a low-income racially diverse southern US cohort. PLoS One. 2018;13(1):e0190993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warren Andersen S, Blot WJ, Shu XO, Sonderman JS, Steinwandel M, Hargreaves MK, et al. Associations between neighborhood environment, health behaviors, and mortality. Am J Prev Med. 2018;54(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ware J Jr, Kosinski M, Keller SDA. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 22.Graves JA. Better methods will be needed to project incomes to estimate eligibility for subsidies in health insurance exchanges. Health Aff (Millwood). 2012;31(7):1613–22. [DOI] [PubMed] [Google Scholar]
- 23. To access the appendix, click on the Details tab of the article online.
- 24.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99. [DOI] [PubMed] [Google Scholar]
- 26.McConnell S, Stuart EA, Devaney B. The truncation-by-death problem: what to do in an experimental evaluation when the outcome is not always defined. Eval Rev. 2008;32(2):157–86. [DOI] [PubMed] [Google Scholar]
- 27.Zhang JL, Rubin DB. Estimation of causal effects via principal stratification when some outcomes are truncated by “death.” J Educ Behav Stat. 2003;28(4):353–68. [Google Scholar]
- 28.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. J Hum Resour. 2015;50(2):317–72. [Google Scholar]
- 29.Cameron AC, Miller DL. Robust inference with clustered data. Davis (CA): University of California Department of Economics; 2010. (Working Paper No. 10–7). [Google Scholar]
- 30.Rosenbaum PR. Observational studies. 2nd ed. New York (NY): Springer; 2002. p. 1–17. [Google Scholar]
- 31.Garthwaite C, Gross T, Notowidigdo M, Graves JA. Insurance expansion and hospital emergency department access: evidence from the Affordable Care Act. Ann Intern Med. 2017;166(3):172–9. [DOI] [PubMed] [Google Scholar]
- 32.Rokicki S, Cohen J, Fink G, Salomon JA, Landrum MB. Inference with difference-in-differences with a small number of groups: a review, simulation study, and empirical application using SHARE data. Med Care. 2018;56(1):97–105. [DOI] [PubMed] [Google Scholar]
- 33.Daw JR, Hatfield LA. Matching and regression to the mean in difference-in-differences analysis. Health Serv Res. 2018;53(6):4138–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ding P, Lu J. Principal stratification analysis using principal scores. J R Stat Soc Series B Stat Methodol. 2017;79(3):757–77. [Google Scholar]
- 35. The Deep South refers to areas historically dependent on slavery, specifically Alabama, Georgia, Louisiana, Mississippi, and South Carolina. According to 2017 data from the American Community Survey, the fraction of the population that was African American in Deep South states (30 percent) was much higher than that in other states in the southern census region (15 percent). See: [please provide].
- 36.Gusmano MK, Fairbrother G, Park H. Exploring the limits of the safety net: community health centers and care for the uninsured. Health Aff (Millwood). 2002;21(6):188–94. [DOI] [PubMed] [Google Scholar]
- 37.Cook NL, Hicks LS, O’Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access to specialty care and medical services in community health centers. Health Aff (Millwood). 2007;26(5):1459–68. [DOI] [PubMed] [Google Scholar]
- 38.Felt-Lisk S, McHugh M, Howell E. Monitoring local safety-net providers: do they have adequate capacity? Health Aff (Millwood). 2002;21(5):277–83. [DOI] [PubMed] [Google Scholar]
- 39.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frean M, Gruber J, Sommers BD. Premium subsidies, the mandate, and Medicaid expansion: coverage effects of the Affordable Care Act. J Health Econ. 2017;53:72–86. [DOI] [PubMed] [Google Scholar]
- 41.Graves JA, Nikpay SS. The changing dynamics of US health insurance and implications for the future of the Affordable Care Act. Health Aff (Millwood). 2017;36(2):297–305. [DOI] [PubMed] [Google Scholar]
- 42.Frean M, Gruber J, Sommers BD. Disentangling the ACA’s coverage effects—lessons for policymakers. N Engl J Med. 2016;375(17):1605–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.