TO 001
CABRINI SHARED CARE MODEL: EARLY REFERRAL AND ACCESS TO PALLIATIVE CARE FOR PATIENTS WITH COPD
O'Driscoll L
1Cabrini Health Respiratory Continuing Care Program, Oakleigh, Australia
Introduction
Chronic obstructive pulmonary disease (COPD) is a significant cause of death in Australia but access to Palliative Care is limited. In addition, previous studies indicate that patients with chronic lung disease are more likely to have their first encounter with palliative care in a critical care setting.
Aim
Cabrini Hospital developed a shared model of early referral and access to palliative care for patients with advanced COPD integrated across the Respiratory Continuing care program and Palliative Homecare team, through: Enabling patients to live as actively as possible with focus on quality of life; Reducing time in hospital and optimizing utilization of continuing care services to support preferred place of care; Optimizing function and comfort physically, psychosocially, emotionally and spiritually; Minimizing physical and psychosocial symptoms.
Providing adequate knowledge and open communication for patients and carers to help timely and informed decision‐making; Supporting carers throughout the person's illness; and Supporting patients and carers when death is inevitable and through the bereavement period.
Preliminary Results
Patient and families reported positive patient experience; improvement in preferred place of death; patients did not feel abandoned or “handed over' to another service; family end of life experience improved due to patient and family being well known to palliative homecare staff and respiratory nurses ; direct admission to inpatient palliative care services prevented a visit to emergency; prevention of hospital admission during final year of life improved quality of life; reduction in emergency calls to ambulance service due to breathlessness and anxiety;
Conclusion
A shared model of early referral and access to palliative care markedly improved quality of services for patients with advanced, non‐malignant lung disease. Training is required to support palliative homecare nurses to deliver care to patients with non‐malignant disease, and equally for chronic disease nurses to support and deliver a palliative care approach.
TO 002
WITHDRAWING/WEANING NON INVASIVE VENTILATION IN PALLIATIVE CARE PATIENTS WITH RESPIRATORY FAILURE
Lafferty, M1, Dunford, M1
1St George Hospital, Sydney, New South Wales, Australia
Introduction
Withdrawal of Non Invasive ventilation (NIV) at the end of life is extremely challenging with varying patient experience. There is little evidence describing medication titration prior to weaning/post NIV cessation, increasing the risk of an undignified death. St George Hospital palliative care service (SGHPS) receives referrals to assist in NIV withdrawal in patients failing to respond to treatment with both malignant and non‐malignant disease. It was recognized that there was a need to develop a more consistent way of weaning each patients NIV and titrating their medications depending on their level of dependency on the NIV.
Methods
In 2015/2016, SGHPC received 64 respiratory failure patient referrals receiving NIV. 35 were specifically referred for end of life care where treatment was deemed futile and there was a change in the direction of care with NIV to be weaned and ceased. We have identified 3 levels of NIV dependency at end of life (EOL) requiring different doses of medications/adjustments to ventilation during the weaning process to ensure a symptom free death. This led to the provision of more specific education to the respiratory medical and nursing staff in the units that use NIV. Effective withdrawal of NIV requires an integrated team approach to provide best practice care
Results
Provision of regular education and support of staff improved staff confidence and competence in caring for patients during the weaning process of NIV. 100% patients dying were on regular opioids and benzodiazepines at time of death. Number of days from referral to death ranged from 0‐8 with 25% dying on the referral day.
Conclusion
There is a need for further research and guidelines in palliative care NIV withdrawal with respiratory failure. A consistent collaborative approach from both the respiratory/palliative care services in optimal EOL management is encouraged.
Grant Support: Nil
TO 003
#O2THEFIX: SWIMMING BETWEEN THE FLAGS
Ncube N1, Chapman A1, Nand J1
1Waitemata District Health Board, Auckland, New Zealand
Introduction/Aim
Historically it has been common practice to administer oxygen regardless of need, without sufficient monitoring and adjustment. This has been consistently demonstrated by audits carried out at Waitemata District Health Board (Waitemata DHB) and other hospitals in New Zealand1,2.
The Thoracic Society of Australia and New Zealand (TSANZ) recently released guidelines for the acute use of oxygen in adults that promote prescribing of oxygen therapy to target a level between a prescribed range of oxygen saturations3. For example between 92% to 96% is appropriate for most patients. For patients that retain carbon dioxide, such as those with chronic obstructive pulmonary disease (COPD), oxygen should be titrated to 88‐92%
Methods
#O2TheFix: Swimming Between the Flags is an innovative multidisciplinary collaboration to improve the prescribing and safe administration of oxygen at Waitemata DHB. A campaign was planned to showcase the mix of utilising technology via electronic prescribing, social media and educational sessions sporting a catchy phrase: “O2 the Fix, Aim 92‐96. If high CO2, Aim 88‐92” to improve the awareness of oxygen with improved prescribing and administration.
Results
At baseline, only 12% of patients had their oxygen prescribed. The remaining patients were receiving oxygen without a prescription.
A re‐audit six months later showed an increase of oxygen prescribing from 12% to 49%.
Staff also report increased understanding of important safety concepts regarding oxygen and their delivery devices.
Conclusion
#O2TheFix has improved patient safety by raising awareness of oxygen and device prescribing, including specified target saturations ranges. The #O2TheFix team will continue to monitor oxygen and device prescribing while continuing to spread the important safety message.
Grant Support: nil
REFERENCES
Boyle M. Wong J. “Prescribing oxygen therapy. An audit of oxygen prescribing practices on medical wards at North Shore Hospital Auckland New Zealand” NZ Med J 2006:119; U2080
Holbourn A. Wong J. “Oxygen prescribing practice at Waikato Hospital does not meet guideline recommendations” Int Med J 2014 1231‐1234.
Beasley R, Chien J, Douglas J, Eastlake L, Farah C, King, G, Moore R, Pilcher J, Richards M, Smith S, Walters H. Thoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: ‘Swimming between the flags'. Respirology 2015; 20: 1182‐1191
TO 004
INTEGRATED CARE REVIEW OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE INPATIENT MANAGEMENT
Swami V1, Smith T1,2, Cho J1,3, Chawla A1, Roberts M1,3, Wheatley J1,2,3
1Department of Respiratory and Sleep Medicine, Westmead Hospital, Westmead, Australia, 2University of Sydney at Westmead Hospital, Westmead, Australia, 3Ludwig Engel Centre for Respiratory Research, Westmead Institute for Medical Research, Westmead, Australia
Introduction/Aim
In 2014–15, 66,540 patients were hospitalised with an acute exacerbation of COPD (AECOPD) in Australia. National and international guidelines to optimise inpatient management of COPD exist, however compliance to these remains unclear. In 2015 Westmead Hospital implemented a COPD Integrated Care Team (ICT) to review and optimise inpatient and outpatient management of COPD. To review management of AECOPD in inpatients admitted to a tertiary teaching hospital.
Methods
We developed an evidence‐based checklist to monitor the care of inpatients with AECOPD and the adherence to COPD national and international guidelines. We performed a retrospective chart review of checklist adherence for AECOPD admissions at Westmead Hospital from 2016 to 2017. ICT reviewed patients usually within 4 days of hospitalisation or step‐down from high dependency, recorded compliance with the checklist, and then provided advice to inpatient teams regarding optimisation of COPD management.
Results
We reviewed 276 inpatients with AECOPD (55% male; mean age 69.9±10.4 years). We identified good adherence to oxygen prescription on medication charts, early antibiotic rationalisation, and spirometry measurement (all>75% compliance). However, we found inhaler prescription errors in 37% of reviews including incorrect or missing prescriptions and duplication of inhaler classes. 36% of patients were still on nebulised therapy at ICT review, 30% of patients were current smokers and only half had been offered smoking cessation measures. Respiratory vaccinations were not up‐to‐date in 62% of patients, and only 5% had been offered pulmonary rehabilitation.
Conclusion
ICT has identified areas for improvement in inpatient management of AECOPD including inhaler therapy prescriptions, smoking cessation measures, referral to pulmonary rehabilitation and assessment of immunisation. There is a role for ICT in education, ongoing monitoring, and optimisation of inpatient AECOPD management. Further research is needed to understand the impact of improved compliance to AECOPD guidelines on long‐term ambulatory outcomes in patients with COPD.
TO 005
INNOVATIVE MULTI‐LINGUAL MOBILE APP TO IMPROVE KNOWLEDGE AND UNDERSTANDING OF ASTHMA AMONG INDIGENOUS CARERS OF CHILDREN WITH ASTHMA—PROTOCOL
Versteegh L1, Chang A1, Saunders J2, Chirwig S1, Sharma T1, McCallum G1
1Menzies School Of Health Research, Darwin, Australia, 2Asthma Foundation Northern Territory, Darwin, Australia
Introduction/Aim
Among Indigenous Australians, asthma is the most common self‐reported chronic respiratory problem. Asthma related health outcomes are also poorer among Indigenous than non‐Indigenous Australians. To address this, innovative interventions that are culturally‐appropriate are needed. We have developed a multi‐lingual mobile phone application (App) from our existing asthma flipchart, with ‘voice‐over' in local Indigenous languages, using a mixture of static and interactive formats. This study aims to evaluate whether the App improves health knowledge and understanding of asthma among Indigenous carers of children with asthma.
Methods
Evaluation of the app includes quantitative and qualitative methods in addition to the usability testing scheduled. The quantitative component involves a before and after study on asthma‐related knowledge based on our previous flipchart study. Eighty Indigenous carers of children with asthma will be enrolled. Carers will undergo a pre‐education questionnaire, followed by asthma education using the App. A post‐education questionnaire will be administered immediately post‐education session. A subset of carers will repeat the questionnaire two weeks later to determine short‐term knowledge retention. In the qualitative component, Indigenous health professionals with and without asthma will participate in semi‐structured interviews to ascertain perspectives of the functionality and usability of the App.
Results
Recruitment for this study will commence late October 2017 for 12 months.
Summary
Improving asthma related health outcomes is important, and requires a focused, multidisciplinary approach, particularly for at‐risk groups such as Indigenous Australians.
Education in the form of mobile Apps is an innovative method of communicating health messages to culturally and linguistically diverse groups, that moves towards reducing language and context barriers particularly faced by Indigenous people in rural or remote settings. The asthma App has the potential to improve community knowledge by increasing access and usability of health education once only delivered in health centres.
Declaration of interest: Nil
Grant Support: Asthma Australia
TO 006
HARNESSING HOPE, INSTILLING BELIEF: COPD SELF‐MANAGEMENT
Baird M1, Gullick J2
1Dubbo Health Service, Dubbo, New South Wales, Australia, and 2Sydney Nursing School, The University of Sydney, Camperdown, New South Wales, Australia
Introduction/Aim
Chronic Obstructive Pulmonary Disease (COPD) has a significant impact on the healthcare system and patient. Although literature worldwide supports the efficacy of self‐management, studies are traditionally entrenched in the economic model of supported self‐management with the primary outcome of decreasing healthcare utilisation. There is limited literature in a rural setting that explores COPD self‐management through the lens of patient experience.
This study aims to explore the concept of self‐management through the eyes of the patient with COPD, living in rural Western New South Wales (NSW); what their understanding of self‐management is and how they measure it?
Methods
A Heideggerian phenomenological inquiry formed the framework for this research, allowing exploration of the patients lived experience. In depth audio‐recorded semi‐structured interviews were conducted. A total of eight participants (four male, four female) with a reported diagnosis of COPD living in regional and rural Western NSW met the inclusion criteria. Interviews were transcribed verbatim, data was themed and analysed until thematic saturation was achieved (n=8).
Results
Findings unveiled four emerging themes: Adapt, Pace, Preserve and Ownership. Further exploration identified social, emotional and physical domains within the themes Adapt, Pace and Preserve. Exploring the phenomena through the patient lens, identified the true meaning of self‐management and their measures of success.
Conclusion
Exploring the patient's lived experience of COPD self‐management provides a meaningful and context‐driven explanation of patient's perceptions of self‐management, opening up the concept of subjective patient measures as an indicator of self‐management.
Grant Support: This research was supported by the NSW Ministry of Health, Rural Research Capacity Building Program and Western NSW LHD.
Conflict of Interest: COPD Nurse Presenter for Lung Foundation Australia, funded by Menarini.
TO 007
ARE INPATIENT SMOKERS CONSISTENTLY IDENTIFIED AND OFFERED SMOKING CESSATION INTERVENTIONS: A QUALITY IMPROVEMENT PROJECT
Reed N, Chan M, Bird T
Respiratory Nurses Interest group, Sydney, Australia
Introduction/Aim
Each year, smoking kills an estimated 18,000 Australians and costs Australia $31.5 billion in health and economic costs. Smoking harms nearly every organ in the body, causing disease and reducing quality of life and life expectancy. An inpatient care episode represents an opportunity to identify smokers with current health needs and to intervene consistently to improve health care outcomes. NSW Health Policy requires consistent identification of smokers and, as a minimum, brief intervention to manage their nicotine dependence. As health care systems transition from paper to electronic records, it is possible that documentation quality may suffer in areas such as this. The purpose of this audit was to determine the quality of our practice in this important area and whether documentation was compromised in the transition to an electronic medical record(EMR).
Methods
Records of Respiratory Medicine inpatients from January to May 2017 (paper‐based) and June‐October 2017 (EMR) were analysed for documentation of smoking status on admission to hospital and the offering of brief advice and pharmacotherapy or referral to specialist support services for current smokers.
Results
61 paper and 61 EMR records were analysed. 56(92%) of paper records identified smoking status. This fell significantly to 41(61%) [p<0.001;chi2 test] in EMR records. 7 of 13 smokers identified from paper records and 1 of 7 smokers from EMR were offered smoking cessation intervention[p=0.08].
Conclusion
Smoking status could be more consistently identified and recorded. Provision and/or documentation of smoking cessation interventions is poor. Transition to EMR may be a risk for poorer health service provision or documentation.
The audit has shown that there is a need for improvement in documentation by health professionals if smoking interventions as per NSW government guidelines are to be achieved.
Conflict of Interest: There is no conflict of interest.
Grant Support: NIL
Asthma & Allergy 1
TO 008
IRF7, CXCL9 AND CXCL10 PROTEIN LEVELS IN CHILDREN WITH ASTHMA
Coleman L1, Harris L1, Khoo S2,3, Franks K2, Bizzintino J2,3, Prastanti F2, Everard J2, Oo S1, Maciewicz R4, McCrae C4, Öberg L4, Le Souëf P1, Bosco A3, Laing I2,3
1School of Paediatrics and Child Health, University of Western Australia, Crawley, Australia, 2School of Biological Sciences, University of Western Australia, Crawley, Australia, 3Telethon Kids Institute, University of Western Australia, Subiaco, Australia, and 4Respiratory, Inflammation and Autoimmunity iMed, AstraZeneca, Gothenburg, Sweden
Introduction/Hypothesis
Rhinovirus (RV) species C infection is associated with increased severity of acute wheezing and asthma compared with other RV species. RVC utilises a different host cellular receptor to RVA and B, but the mechanisms and pathways activated by RVC and their contribution to the severity of disease are unknown. We have previously identified gene expression differences in nasal cell samples from children with acute asthma and wheezing who were infected with RVC versus RVA. RVC‐specific genes included IRF7, whereas CXCL9 and CXCL10 were identified in the RVA‐specific response. We hypothesised that protein levels for each of these genes would be different in nasal fluid from children having a respiratory exacerbation and infected with RVC versus RVA.
Methods
Nasal fluid samples were collected from 21 children with RVA and 37 with RVC presenting to our tertiary children's hospital Emergency Department with acute respiratory illness. CXCL10 and CXCL9 protein were measured as part of a multiplex ELISA (ThermoFisher), whereas IRF7 protein was measured using a single ELISA kit (Cusabio). Urea was measured using a quantitative chromatic assay (BioAssay Systems) and used to standardise the ELISA measurements (presented here as pg protein per μg urea).
Results
CXCL9 levels were not significantly different (Mann‐Whitney U=192, p=0.79) between RVA (median 13.27, range 0.34‐159.88, n=14) and RVC cases (median 20.66, range 0.37‐248.44, n=29). CXCL10 levels were also not significantly different (Mann‐Whitney U=234, p=0.90) between RVA (median 0.48, range 0.04‐11.41, n=16) and RVC cases (median 0.46, range 0.02‐41.19, n=30). IRF7 levels did not differ (Mann‐Whitney U=217, p=0.63) between RVA (median 1.88, range 0.15‐6.16, n=17) and RVC cases (median 1.62, range 0.19‐21.78, n=28).
Conclusion
CXCL9, CXCL10 and IRF7 gene expression in nasal cell samples collected during RVC vs RVA‐induced acute wheezing and/or asthma are different, but this has not translated to alterations in nasal fluid protein levels.
Grant Support: National Health and Medical Research Council, Telethon—Perth Children's Hospital Research Fund, University of Western Australia, Asthma Foundation of Western Australia, AstraZeneca
Declaration of Interest: none.
TO 009
GROWTH OF THE AIRWAY SMOOTH MUSCLE LAYER IN EARLY LIFE IS DUE TO CELL HYPERPLASIA
Elliot J1, Carvajal A2, Savigni D2, James A1,3, Noble P2,4
1Department of Pulmonary Physiology and Sleep Medicine, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia; 2School of Human Sciences, University of Western Australia, Perth, Western Australia, Australia; 3School of Medicine and Pharmacology, University of Western Australia, Perth, Western Australia, Australia; 4Centre for Neonatal Research and Education, School of Paediatrics and Child Health, University of Western Australia, Perth, Western Australia, Australia
Introduction/Aim
Thickening of the airway smooth muscle (ASM) layer is present in children with asthma which implicates a developmental origin. Little is known about the structural changes that occur in the airway and ASM layer from late gestation to adulthood. The aim of this study was to assess maturational changes in airway wall structure and examine mechanisms of ASM growth in terms of hyperplasia, hypertrophy and extracellular matrix (ECM).
Methods
Sheep were euthanized at late gestation (128 d), birth (150 d), post weaning (4 months) and sexual maturity (1 year). Lungs were fixed by instillation of formaldehyde and samples obtained from the trachea, main bronchus, segmental bronchus, sub‐segmental bronchus and peripheral airways. The area of the ASM layer, inner and outer wall and perimeter of basement membrane (Pbm) were measured by planimetry. The number and size of ASM cells was assessed by stereology and fractions of muscle, ECM and 'other' within the ASM layer were determined by point counting.
Results
The predominant period of airway maturation was from birth to 4 months of age. Airway size (Pbm) and airway wall areas (including ASM) were all increased in the trachea (p<0.05), segmental bronchus (p<0.05) and sub‐segmental bronchus (p<0.05). When wall areas were normalised to Pbm, there was no effect of age indicating that airway structure grew in proportion to airway size. Changes were less pronounced in more peripheral airways. The mechanism of ASM growth was due only to an increase in cell number and not as a result of cell hypertrophy or changes in the proportion of ECM.
Conclusion
Substantial airway growth occurs before weaning and this includes expansion of the ASM layer as a result of cell hyperplasia. Upregulation of ASM proliferation in infancy could facilitate thickening of the ASM layer and the development of asthma in childhood.
Grant Support: NHMRC (1077791)
Declaration of Interest Statement: None.
TO 010
LUNG FUNCTION AT 6 WEEKS OF AGE IS ASSOCIATED WITH THE RISK OF DEVELOPING BRONCHIOLITIS IN INFANTS BORN TO MOTHERS WITH ASTHMA DURING PREGNANCY
De Gouveia Beinelo P1, Jesson K1, Silva Sena C1, Collison A1, Murphy V1, D Robinson P2, Hardaker K2, D Sly P3, Gibson P4,5, Mattes J1,6
1Priority Research Group Growup Well, University Of Newcastle, Newcastle, Australia, 2Department of Respiratory Medicine, The Children's Hospital at Westmead, Sydney, Australia, 3Centre for Children's Health Research, University of Queensland, South Brisbane, Brisbane, Australia, 4Priority Research Centre Healthy Lungs, Hunter Medical Research Institute, University of Newcastle, Newcastle, Australia, 5Respiratory & Sleep Medicine Department, John Hunter Hospital, Newcastle, Australia, and 6Paediatric Respiratory & Sleep Medicine Department, John Hunter Children's Hospital, Newcastle, Australia
Introduction/Aim
FeNO‐guided asthma management during pregnancy was associated with a reduction in bronchiolitis episodes in the first year of life (Mattes et al., Thorax 2013). The aim of this analysis was to investigate an association between infant lung function at 6 weeks of age and bronchiolitis in the first 6 months of life in a cohort of babies born to women with asthma during pregnancy.
Methods
Tidal breathing flow‐volume loop (TBFVL) measurements were performed during quiet unsedated sleep in infants born to mothers who participated in an ongoing NHMRC‐funded multi‐centre RCT of FeNO‐guided asthma management versus usual care (Breathing for Life Trial). All researchers remain blinded in regards to the pregnancy intervention.
Results
Of 324 babies recruited to date, 289 attended a clinical assessment and 261 remained in quiet sleep during testing. 232 had TBFVL attempted (44% female; age 6 weeks SD 1.2), of which 209 (90%) tests were technically acceptable. At the time of abstract submission, 140/209 (67%) were 6 months old.
Infants with one episode of bronchiolitis in the first 6 months of life had a mean of time to Peak Tidal Expiratory Flow/time Expiratory Flow % (tPTEF/tE%) of 28.5 (SD 6.8; n=30) at 6 weeks of age. Infants with >1 episode of bronchiolitis had a mean tPTEF/tE% of 22.79 (SD 4.46; n=6) while those without bronchiolitis had a mean tPTEF/tE% of 32.34 (SD 9.4; n=104). There were no difference in respiratory rate (RR) between groups (1 episode: mean RR 44 breaths per minute; >1 episode: mean RR 42 breaths per minute; no bronchiolitis: mean RR 44 breaths per minute).
Conclusions
Lung function may be associated with the risk of developing bronchiolitis which could provide a linking mechanism for the effect of FeNO‐guided management on bronchiolitis prevalence.
Grant support: NHMRC, John Hunter Hospital, PRC GrowUpWell, HMRI and HCRF.
TO 011
ANTI G‐CSFR ANTIBODY TREATMENT SUPPRESSES NEUTROPHILIC AND TYPE‐2 LUNG INFLAMMATION IN AN ALLERGIC ASTHMA MODEL WORSENED BY NEONATAL CO‐INFECTION
Wang H1, FitzPatrick M2, Anthony D1, Reading P3, Wilson N5, Satzke C4,6,7, Dunne E6, Licciardi P6,7, Anderson G2, Vlahos R1, Bozinovski S1
#Equal contribution
1RMIT University, School of Health and Biomedical Sciences, Melbourne, Australia, 2The University of Melbourne, Lung Health Research Centre, Department of Pharmacology & Therapeutics, Parkville, Melbourne, Australia, 3The WHO Collaborating Centre for Reference and Research on Influenza, Victorian Infectious Diseases Reference Laboratory, at The Peter Doherty Institute for Infection and Immunity, Parkville, Melbourne, Australia, 4CSL Limited, Parkville, Melbourne, Australia, 5The University of Melbourne, Department of Microbiology and Immunology, at The Peter Doherty Institute for Infection and Immunity, Parkville, Melbourne, Australia, 6Pneumococcal Research, Murdoch Children's Research Institute, Parkville, Melbourne, Australia, 7The University of Melbourne, Department of Paediatrics, Parkville, Melbourne, Australia
Introduction/Aim
Early life respiratory infections are associated with the development of severe asthma, where the detection of both respiratory viruses and bacteria occur frequently in children with acute wheeze. However, the mechanistic interaction between neonatal respiratory infections and the establishment of allergic type‐2 and neutrophilic lung inflammation remains poorly understood in severe asthma. Our aim is to investigate the role of neonatal exposure to infectious pathogens in the development of allergen‐triggered asthmatic pathogenesis and airway remodelling.
Methods
Intranasal inoculation of Streptococcus pneumoniae (2000 CFU, EF3030)/saline and Influenza A virus (500 PFU, HKx31)/saline was performed on neonatal mice (female BALB/c) at the age of 8 days and 15 days respectively. At the age of 21 days, house dust mite (HDM)/saline was administered intranasally daily for 3 weeks.
In the therapeutic study, a separate cohort of mice was treated as described above. In the last week of HDM regime, 100 μg of anti‐G‐CSF receptor (G‐CSFR) /isotype antibody was injected intraperitoneally every second day.
Results
HDM challenge in mice co‐infected as neonates significantly increased pneumococcal lung infection, neutrophilic inflammation and mucus production. Neutrophilic lung inflammation was associated with an increase in interleukin‐17A and granulocyte‐colony stimulating factor (G‐CSF). Blocking G‐CSFR significantly reduced neutrophlic inflammation in the bronchoalveolar (BAL)‐fluid and myeloperoxidase activity in lung tissue without increasing pneumococcal lung load. In addition, elevated markers of netosis including neutrophil elastase and double‐stranded DNA were reduced in the BAL‐fluid of anti‐G‐CSFR treated mice. Anti‐G‐CSFR therapy also potently reduced type‐2 inflammation including BAL eosinophils, IL‐33/IL‐13 lung transcripts, CD4+IL4+ TH2 cells and mucus (muc5ac) production.
Conclusion
Disrupting G‐CSFR significantly reduced neutrophil mobilisation and netosis without worsening pneumococcal lung infection and furthermore, reduced type‐2 inflammation in allergic airways disease. Monoclonal antibodies against the G‐CSFR may represent a novel therapeutic target for mixed granulocytic severe asthma.
Grant Support: This work was supported by National Health and Medical Research Council of Australia (grant number APP1067547) and Australian Research Council (grant number FT130100654).
TO 012
GENETIC VARIANTS IN HUMAN RESPIRATORY VIRUS RECEPTORS WERE ASSOCIATED WITH INFECTION, RECOVERY AND RECURRENCE OF WHEEZING EXACERBATIONS IN CHILDREN
Harris L1,2, Allcock R3,4, Kresoje N3, Le Souëf P1, Laing I2,3
1Division of Paediatrics, The University of Western Australia, Perth, Australia, 2Telethon Kids Institute, Perth, Australia, 3School of Biomedical Sciences, the University of Western Australia, Perth, Australia, and 4Pathwest Laboratory Medicine WA, QEII Medical Centre, Perth, Australia
Introduction/Aim
Human rhinoviruses (RV) and respiratory syncytial virus (RSV) are common respiratory viruses in children with acute wheezing illnesses. Viruses use human receptors to enter host cells. RSV uses nucleolin (NCL), and RV uses intercellular adhesion molecule 1 (ICAM1), low density lipoprotein receptor (LDLR) or cadherin related family member 3 (CDHR3). We aimed to assess whether variants in viral receptor genes were associated with asthma severity.
Methods
Cohort: Children who presented to a tertiary children's hospital emergency department with acute asthma (n=50). Samples: Nasal samples for RV detection. DNA was extracted from peripheral blood. Analysis: Viral receptor genes were sequenced using Ion AmpliSeq primers (Thermo Fisher Scientific). Data collected included: (1) number of hours from presentation to discharge, (2) number of respiratory hospital presentations and admissions from birth and (3) number of salbutamol doses administered in the first 6 hours. Statistical analysis was completed using SPSS version 22. All analyses were adjusted for age and gender.
Results
The mean age of children was 8.44yrs, 60% male, 56% with detectable RV. Children with genotypes CDHR3 rs34426483 GC or CC and NCL rs7598759 CC were 0.161‐0.105 fold less likely to have rhinovirus detected at recruitment than children with the other genotypes (95% confidence interval (CI): 0.023‐1.11; p‐value: 0.064 and 95% CI: 0.009‐1.24; p‐value: 0.073, respectively). Children with ICAM1 rs281437 TT genotypes had 17.0 fold more hospital visits before recruitment (95% CI: ‐0.062‐23.5; p‐value: 0.002) and took 2.52 fold longer to be discharged from hospital (95% CI: 7.81‐129; p‐value: 0.019) compared to children with CC genotypes. Children with ICAM1 rs5498 GG genotypes had 0.593 fold fewer treatment doses in 6 hours (95% CI: ‐0.852‐12.1; p‐value: 0.013) than children with AA genotypes.
Conclusion
Gene variants in viral receptor genes may play a role in viral infection and treatment response, and thus recurrent respiratory illnesses requiring presentation to hospital.
Grant Support: NHMRC #1087700, Financial Markets Foundations for Children #2015‐314, University Postgraduate Award, UWA Safety‐Net Top‐Up Scholarship
Conflict of Interest: No.
Nomination: Nil.
TO 013
This abstract has been withdrawn
Paediatric
TO 014
ABNORMAL LUNG CLEARANCE INDEX (LCI) IN PRESCHOOL YEARS IS ASSOCIATED WITH LOWER SPIROMETRY LATER IN CHILDHOOD IN CYSTIC FIBROSIS (CF) CHILDREN
Panda H2, Hardaker K1,3, Hulme K2, Kennedy B1, Gustafsson P4, Cooper P1, Fitzgerald D1,3, Pandit C1,3, Selvadurai H1,3, Robinson P1,3
1The University of Sydney, Sydney, New South Wales, Australia, 2Department of Respiratory Medicine, The Children's Hospital at Westmead, Sydney, New South Wales, Australia, 3Discipline of Paediatrics and Child Health, Sydney Medical School, University of Sydney, Sydney, New South Wales, Australia, and 4Department of Paediatrics, Central Hospital, Skövde, Sweden
Introduction/Aim
Availability of robust commercial multiple breath nitrogen washout (MBNW) equipment offers improved feasibility for widespread preschool lung function testing in Cystic Fibrosis (CF) clinics. Clinical utility is emerging with this commercial equipment but the prognostic value of performing preschool MBW (defined as age 2‐6 years) remains unclear. We have previously shown an association between higher preschool Lung Clearance Index (LCI) values and greater medication use and incidence of bacterial isolation within our clinic. This study aimed to explore the association between those preschool LCI values and later spirometry, a well established clinical tool in older CF subjects.
Methods
Current spirometry values (FEV1, FEV1/FVC and FEF25‐75) were collated on the original 37 preschool children who had MBW performed at mean (SD) age 5.0 (1.2, range 2.8‐6.9) yrs: median (range) LCI 8.0 (6.5‐14.3). Spirometry results were expressed as z‐scores (GLI reference equations). Abnormal preschool LCI was defined based on recently published preschool healthy control data using identical equipment and testing protocol1 (ULN for LCI 8.0).
Results
Technically acceptable spirometry data were available in 35/37 (95%) (one had moved out of state, one has autism) at mean (SD; range) age 7.7 (1.4; 4.8‐9.8) years, which was 2.7 (0.4; 1.0‐3.3) years after the original MBW testing time point.
| Later spirometry (z scores) | |||
|---|---|---|---|
| FEV1 | FEV1/FVC | FEF25‐75 | |
| Overall cohort (n=35) | ‐0.18 (1.28) | ‐0.80 (1.06) | ‐0.82 (1.43) |
| Abnormal preschool LCI (n=17) | ‐0.53 (1.53) | ‐1.28 (1.17) | ‐1.05 (1.63) |
| Normal preschool LCI (n=18) | ‐0.02 (0.91) | ‐0.62 (0.78) | ‐0.63 (1.04) |
| p value (abnormal vs. normal LCI) | 0.07 | 0.02 | 0.03 |
Data presented as mean (SD).
Conclusion
Abnormal MBW‐derived LCI values in the preschool years are associated with later spirometry deficits. This suggests prognostic utility of MBW testing in this younger preschool age range to predict later spirometry values.
1 Stanojevic et al AJRCCM 2017;195:1216‐1225
Grant Support: CF fundraising, CHW
Conflict of interest: No conflicts of interest to declare.
TO 015
CAN A BRONCHOSCOPICALLY DEFINED BRONCHITIS TOOL IN CHILDREN BE VALIDLY DEVELOPED?
Thomas R1, Eg K1,2, Masters I1, McElrea M1, Chang A1,3
1Department of Respiratory and Sleep Medicine, Lady Cilento Children's Hospital, Children Centre for Health Research, Queensland University of Technology, Brisbane, Queensland, Australia, 2Department of Paediatrics, University of Malaya, Kuala Lumpur, Malaysia, and 3Child Health Division, Menzies School of Health Research, Charles Darwin University, Tiwi, Northern Territory, Australia
Introduction/Aim
Despite bronchitis being the most common finding at flexible bronchoscopy (FB) in many paediatric centres such as ours, no validated objective system exists. From previously recorded FB, we: (1) determined the correlation among the different macroscopic findings with airway neutrophilia (2) examined the inter‐rater repeatability of these findings and, (3) developed an experimental model of an objective FB‐derived bronchitis score (BScoreexp).
Methods
We reviewed 100 consecutive previous recordings (2016) from our database. We excluded FBs if: BAL data was unavailable, incomplete FB recording or FBs were on children who were immune‐compromised or had endotracheal tube, tracheostomy or foreign body. FB recordings were assessed (by 2 scorers independently,blinded to the clinical history) for 6 components: amount of secretions (scores 1‐6 from previous validated score), colour of secretions (0‐8 using BronkoTest), mucosal oedema (0‐3), ridging (0‐3), erythema (0‐3) and pallor (0‐3), based on pre‐determined criteria on a pictorial chart. The various models of BScoreexp were plotted against neutrophil% using a receiver operating characteristic (ROC) curve. Here we report our preliminary findings; on the first 65 children with valid FBs.
Results
Only secretion amount (rs=0.272, p=0.03) and colour (rs=0.342, p=0.005) significantly correlated with BAL %neutrophil but other macroscopic findings correlated with each other. For the 26 FBs examined for repeatability, kappa values for secretions (K=0.96, 95%CI 0.91‐1.0) and colour (K=0.84, 95%CI 0.73‐0.95) were excellent. Other K ranged from 0.38 to 0.67. Using BAL neutrophilia of 15% to define inflammation, the highest aROC (0.63, 95%CI 0.50‐0.76) was obtained by the giving three times weightage to secretion amount and colour and adding it to the other 4 components except pallor.
Conclusion
A repeatable FB‐defined bronchitis scoring system can be derived. However, a prospective study needs to be performed with larger numbers to further evaluate the different models to obtain aROC of >0.7.
Grant Support: KPE funded by an APSR Scholarship, ABC by NHMRC Practitioner Fellowship
Declaration of Interest statement: None.
TO 016
PROTRACTED BACTERIAL BRONCHITIS (PBB)—LONG‐TERM OUTCOMES AT FIVE YEARS: A COHORT STUDY
Ruffles T1, Marchant J1, Buntain H1, Mastera I1, Upham J2, Yerkovich S3, Gibson P4, Baines K4, Simpson J4, Pizzutto S5, Hodge G6, Hodge S6, Chang A1,5
1Department of Respiratory and Sleep Medicine, Lady Cilento Children's Hospital, Children Centre for Health Research, Queensland University of Technology, Brisbane, Australia, 2The School of Medicine, University of Queensland and Princess Alexandra Hospital, Brisbane, Australia, 3The Prince Charles Foundation, The Prince Charles Hospital, Chermside, Brisbane, Australia, 4The Respiratory and Sleep Medicine, School of Medicine and Public Health, Centre for Asthma and Respiratory Disease, The University of Newcastle, Callaghan, Newcastle, Australia, 5Child Health Division, Menzies School of Health Research, Darwin, Australia, 6The Chronic Inflammatory Lung Disease Research Laboratory, Department of Thoracic Medicine, Royal Adelaide Hospital and School of Medicine, University of Adelaide,, Adelaide, Australia
Introduction/Aim
PBB is a common cause of paediatric chronic cough and is defined as chronic wet cough (>4‐weeks) without specific signs or symptoms of an alternative cause which responds to 2‐weeks of appropriate antibiotic therapy. In this first 5‐year outcome data on children with PBB, we aimed to describe the long‐term clinical outcomes in children with PBB.
Methods
160 children (median age 25mths, range 2‐163mths) were recruited and followed for 5‐years with monthly contacts by research staff and when possible, annual physician clinical review. Flexible bronchoscopy, bronchoalveolar lavage and basic immune tests were performed at baseline. During follow‐up, chest CT was performed if clinical features were suggestive of bronchiectasis. Bronchiectasis was diagnosed when paediatric radiology criteria and clinical features were present. Spirometry was undertaken at the final follow‐up (5‐years) when possible. We present data on the initial 101 children (n PBB=82, controls=19) of the cohort with 5‐year follow‐up data.
Results
Of the 82 children with PBB (median age 23mths, range 5‐163mths; 65% boys), CT was undertaken in 26 children during the follow‐up period; 7 had bronchiectasis (7/82=8.5%). All were diagnosed within 28‐months. The frequency of recurrent PBB (>3/yr) decreased over the duration of the study from 54 (66%) at Yr‐1 to 10 (12%) at Yr‐5. Fifty‐seven (70%) of children with PBB had tracheomalacia and/or bronchomalacia on bronchoscopy, whilst 25 (30%) had visible evidence of bronchitis. At the Year‐5 point, the mean FEV1 was 94% predicted (SD 15.8) in both the PBB and control groups.
Conclusion
PBB is associated with a subsequent diagnosis of bronchiectasis in a proportion of children recognised within 28 months of initial PBB diagnosis. While recurrent PBB decreases over time, those with recurrent episodes should be reviewed for bronchiectasis. Spirometry values remains in the normal range in children diagnosed with PBB at long‐term follow‐up.
Grant Support: This work was supported by the National Health and Medical Research Council (APP1042601). PG, SP, SH and AC are supported by NHMRC fellowships. KB is supported by a lung foundation of Australia Fellowship.
TO 017
RESPIRATORY STATUS IN CHILDREN WITH SPINOMUSCULAR ATROPHY TYPE II & III
Parakh A1, Kapur N1,2,3, Deegan S1, Shackleton C1,3, Gauld L1,2,3
1Lady Cilento Children's Hospital, Brisbane, Australia, 2University of Queensland, Brisbane, Australia, and 3Center for Children's Health Research, Brisbane, Australia
Introduction
Spinomuscular atrophy (SMA) is an uncommon, progressive Neuromuscular Disorder (NMD) with significant respiratory morbidity and eventual respiratory failure. There are currently no clear guidelines for non‐invasive ventilation (NIV) instigation in this condition. Newer treatment options are likely to change current clinical practices but improved respiratory assessment methods are needed. Our objectives in this cohort were to (1) analyse the patterns of sleep breathing measured by polysomnography (PSG) and (2) determine early clinical and lung function predictors of nocturnal hypoventilation.
Methods
We retrospectively reviewed clinical records and PSG data of all children with genetically‐confirmed SMA II/III living in Queensland. Spirometry, Forced Oscillatory Technique (FOT), Lung Clearance Index (LCI), & respiratory muscle strength testing were prospectively performed/ measured. The prospective arm of the study is ongoing with complete data collection expected by November 2017.
Results
23 children (9F; 17 with SMA II, median age 108 months) were included. Median FVC% predicted (z score) was 61% (n=19, ‐3.32); Rrs8 z‐score: 2.19 (n=11); Xrs8 z‐score: ‐2.03 (n=11); SNIP z‐score: ‐2.53 (n=10) & LCI: 7.36 (n=12). Median (IQR) REM related Apnea‐hypopnea index (rAHI) was high at 5.9 (2.9‐17.5;n=19). 10 children (9 with SMA II) required long‐term nocturnal NIV initiated at a median age of 94 months; 5 (50%) after an acute respiratory illness. These children were older (127 vs 84 months; p=0.03) with significantly worse FVC‐z scores (‐4.8 vs ‐1.18; p<0.01); rAHI (26.5 vs. 4.2; p=0.05), LCI (8.8 vs. 7.1, p=0.01) & SNIP z‐scores (‐3.5 vs. ‐1.47 p=0.001). Predictors of NIV need will be analysed using a logistic regression model once the prospective arm is completed.
Conclusion
Most children with SMA II need nocturnal ventilatory support beginning in early childhood and FVC may be a predictor. FOT, SNIP and LCI were deranged and may help in predicting early respiratory insufficiency, particularly in early years.
Grant Support: None
Declaration of Interest: No conflicts of interest.
TO 018
AIRWAY SMOOTH MUSCLE CONTRACTION IS ENHANCED BY INTRA‐AMNIOTIC LIPOPOLYSACCHARIDE AND SUPPRESSED BY POSTNATAL DEXAMETHASONE IN A PRETERM OVINE MODEL
Savigni D1, Sorensen N1, Ahmadi‐Noorbakhsh S1, Pillow J1,2, Noble P1,2
1School of Human Sciences (Physiology), The University of Western Australia, Perth, Australia, and 2Centre for Neonatal Research and Education, School of Paediatrics and Child Health, The University of Western Australia, Perth, Australia
Introduction/Aim
Chorioamnionitis is associated with preterm birth and the development of airway disease in later life. Chorioamnionitis promotes lung inflammation, but its effect on airway smooth muscle (ASM) function is unknown. Postnatal steroids are given to preterm infants with severe lung disease and may have beneficial effects on airway development. This study examined the separate and combined effects of chorioamnionitis and postnatal steroids on ASM contraction in a preterm ovine model.
Methods
Chorioamnionitis was induced by ultrasound‐guided intra‐amniotic (IA) injection of lipopolysaccharide (LPS) into time‐mated ewes (127d gestation; term=150d). Postnatally, LPS‐exposed lambs received intravenous low‐dose dexamethasone (LPS/Dex) or saline (LPS/Sal: n=6) commencing within 2 h of birth. Postnatal controls received IA saline at 127d gestation and daily intravenous low‐dose dexamethasone (Sal/Dex: n=9) or saline (Sal/Sal: n=6) postnatally. Lambs were delivered via caesarean section at 129d gestation, receiving respiratory support as required, and euthanised after 7d (i.e., 136d postconceptional age). A fifth group of naïve fetal control lambs were euthanised immediately at 136d gestation as maturational controls. Bronchial rings were studied in organ bath chambers. Isometric force production to acetylcholine was measured and dose‐response curves constructed to determine maximal response, slope and sensitivity. ASM thickness was determined histologically after Masson's Trichrome.
Results
Maximal response, slope and sensitivity were similar between maturational and postnatal (placebo) controls, indicating ASM contraction was unaffected by preterm delivery. Maximal response was increased by IA LPS administration (p<0.05) and not significantly affected by postnatal dexamethasone. Dose‐response slope was reduced by postnatal dexamethasone (p<0.05) in LPS‐exposed lambs. ASM thickness was lower in animals treated postnatally with dexamethasone, irrespective of prior exposure to LPS (p<0.05).
Conclusion
ASM contraction is enhanced in offspring born to chorioamnionitis‐affected pregnancies, and this is suppressed by postnatal dexamethasone through reduced ASM thickness. Postnatal dexamethasone may reduce the incidence of future airway disease after chorioamnionitis.
Grant Support: NHMRC; TPCHRF; MHRIF
TO 019
CHARACTERISTICS OF CHILDREN WITH CHRONIC SUPPURATIVE LUNG DISEASE (CSLD): A PROSPECTIVE 10‐YEAR STUDY
McCallum G1, Chang A1,2, Byrnes C3, Mobberley C3, Morris P1, Redding G4, Grimwood K5, Singleton R6
1Menzies School of Health Research, Darwin, Australia, 2Children Centre for Health Research, Queensland University of Technology, Brisbane, Australia, 3The University of Auckland and Starship Children's Hospital, Auckland, New Zealand, 4University of Washington, Washington, USA, 5Griffith University and Gold Coast Health, Gold Coast, Australia, and 6Alaska Native Tribal Health Consortium, Anchorage, AK, USA
Introduction/Aim
While largely preventable, CSLD (including bronchiectasis), remains highly prevalent amongst disadvantaged Indigenous populations in high income countries. Adult studies with CSLD have shown that persistent airway infection and inflammation, and longer duration of chronic productive cough result in poorer clinical outcomes. There are however, no prospective studies in children with CSLD in the last 50‐years to help guide long‐term clinical care and management. We evaluated the long‐term clinical outcomes of Indigenous children with CSLD who participated in our previous study, ‘Multicentre Bronchiectasis Study (BOS)' (2004‐2012).
Methods
During 2015–17, we re‐assessed as many children as possible from BOS (Australia n=97, Alaska n=41, New Zealand n=42). Research staff administered standardised questionnaires and undertook medical note review, clinical examination and spirometry. Medical history was extracted from the original dataset and current medical records. Based on their clinical assessment, physicians classified children into 4 overall categories (well, better, stable, worse).
Results
120/180 (67%) children (current median age 11.5‐years (IQR 5.9‐18.6); 46% males) were reviewed. From birth until their current age, children had a median of 20 (IQR 14‐30) community‐treated acute lower respiratory infections and 4 (IQR 3‐7) respiratory hospitalisations. Respiratory infections decreased with age. At examination, wheeze was present in 10%, wet cough in 26% and digital clubbing in 17% of children. The children's summary clinical status were: well (22%); better (32%); stable (46%) or worse (0%). Airway obstruction on spirometry was present in 36% and restrictive pattern in 19%, with only 45% having normal spirometry values within population norms.
Conclusion
In a 10‐year follow‐up of children with CSLD and on‐going clinical care, most were stable or improved by adolescence. However, as many still experience respiratory symptoms and demonstrate impaired lung function, clinical follow‐up is recommended during adolescence to optimise clinical management.
Declaration of interest: Nil
Grant Support: NHMRC CRE for Lung Health APP1040830; GB and AC are supported by NHMRC fellowships.
Asthma & Allergy 2
TO 020
FREE FATTY ACID RECEPTORS 1 AND 4 MEDIATE DESENSITISATION‐RESISTANT BRONCHODILATION AND ARE EXPRESSED IN ASTHMATIC AIRWAYS
Angeles R1, Donovan C1, Royce S1,2, Bourke J1
1Department of Phamacology, Biomedicine Discovery Institute, Monash University, Clayton, Victoria, Australia, and 2Department of Medicine, Central Clinical School, Monash University, Clayton, Victoria, Australia
Introduction
Salbutamol opposes airway hyperresponsiveness in asthma but its efficacy is limited by β2‐adrenoceptor desensitisation. Free fatty acid receptors 1 and 4 (FFAR1, FFAR4) are expressed in mouse and human lungs (Mizuta et al., AJP Lung, 2015) and their agonists cause relaxation of mouse airways with greater efficacy than salbutamol (Bourke et al., AJRCMB, 2017).
Aims
To compare bronchodilation to salbutamol, GW9508 (FFAR1/FFAR4 agonist) and TUG891 (FFAR4 agonist) under conditions of β2‐adrenoceptor desensitisation, test potential FFAR1/FFAR4 desensitisation and assess FFAR expression in mouse airways from a model of chronic allergic airways disease and human airways from subjects with and without asthma.
Methods
Precision cut lung slices were prepared from 6‐8‐week‐old male BALB/C mice. Airway relaxation to GW9508, TUG891, and salbutamol were compared after overnight incubation with 10μM salbutamol, 100μM GW9508, or vehicle. Immunohistochemistry for FFARs was performed on lung sections from saline control (C) and ovalbumin (OVA)‐sensitised mice and airway biopsies from non‐asthmatic (NA) and asthmatic (A) subjects.
Results
Salbutamol and FFAR agonists relaxed airways pre‐contracted with methacholine (%relaxation: 10μM salbutamol 50±6%; 100μM GW9508 28±7%; 100μM TUG891 44±10%, n=7,4,6). Overnight incubation with salbutamol reduced subsequent relaxation to salbutamol (to 4±2%, n=7, p<0.0001 cf control), but not to GW9508 or TUG891 (27±6%, 42±10% respectively, n=6,5). GW9508 incubation did not affect salbutamol‐ or GW9508‐mediated relaxation (44±6%, 26±7% resepectively, n=6,6). Both FFAR1 and FFAR4 expression was similar in C and OVA mouse airways (FFAR4 positive pixel count/mm2: C 4.4±0.3x106; OVA 5.4±0.7x106, n=5,6) and both receptors were evident in airway smooth muscle and epithelium in NA and A human airways.
Conclusion
Relaxation to FFAR agonists was maintained under conditions of β2‐adrenoceptor desensitisation and resistant to homologous desensitisation. Expression of FFAR1 and FFAR4 in asthma context suggests that these receptors may be targeted for alternative or adjunct bronchodilator therapy.
TO 021
DETERMINANTS OF PHYSICAL ACTIVITY IN OBSTRUCTIVE AIRWAY DISEASES
Cordova‐Rivera L1,2, Gibson P1,2,3, Gardiner P5, McDonald V1,2,3,4
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute (HMRI), University of Newcastle, Newcastle, Australia, 2Centre of Excellence in Severe Asthma, Newcastle, Australia, 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, HMRI, Newcastle, Australia, 4The University of Queensland, Faculty of Medicine, Brisbane, Australia, and 5School of Nursing and Midwifery, University of Newcastle, Newcastle, Australia
Introduction/Aim
Severe asthma (SA), chronic obstructive pulmonary disease (COPD) and bronchiectasis are obstructive airway diseases (OAD) that share clinical characteristics that are likely to impair patients' physical activity (PA) level. However, PA has not been extensively studied in OAD, outside of COPD. We aimed to describe the prevalence of PA impairment in different OAD compared to controls, and to test whether in the OAD group, PA is associated with shared clinical characteristics of these diseases.
Method
A cross‐sectional study of adults with OAD (SA=62, COPD=67, bronchiectasis=60) and controls (n=63) was conducted. Participants underwent a multidimensional assessment involving measurement of body mass index (BMI), lung function, exercise capacity (6‐minute walk distance (6MWD)), health status (SGRQ) and systemic inflammation (hsCRP). PA (steps/day) was measured using the ActiGraph wGT3X‐BTaccelerometer.
Results
The OAD group included 189 participants (58.7% female), median [IQR] age 67 [58‐72] years and mean FEV1% predicted 69.4%. The control group included 63 participants (52.4% female), aged 55 [34‐64] years. Compared to controls, those with OAD accumulated less steps/day: median difference ‐4630 (COPD), ‐2255 (SA), and ‐2289 (bronchiectasis) (p≤0.001 all results). Compared to COPD, both SA and bronchiectasis accumulated more steps/day: median difference 2375 and 2341, respectively (p≤0.0001). No statistically significant differences were found between the SA and bronchiectasis groups. In separate adjusted regression models, 6MWD, FEV1% predicted and SGRQ were all associated with physical activity in participants with OAD. In the full multivariable model, 6MWD, FEV1% predicted and BMI remained significantly associated, explaining 47.4% of the adjusted variance of PA in people with OAD (p<0.0001).
Conclusion
People with OAD engage in lower levels of PA compared to controls. The degree of activity impairment differs by disease. Despite this, the level of activity is associated with shared clinical characteristics. Interventions to improve PA should be multifactorial, and target the OAD population, irrespective of diagnosis.
Grant Support: NHMRC, John Hunter Hospital Charitable Trust, HMRI
Conflict of Interest: VMM is supported by an NHMRC TRIP fellowship, has participated in educational symposia funded by GlaxoSmithKline, AstraZeneca, Menarini, and Novartis and has participated in advisory boards for GlaxoSmithKline, AstraZeneca and Menarini. PGG holds an NHMRC Practitioner Fellowship, has participated in educational symposia funded by AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline and Novartis, and has participated in studies funded by GlaxoSmithKline and AstraZeneca. PAG is supported by a NHMRC‐ARC Dementia Research Development Fellowship and has participated in an educational symposium funded by Boehringer Ingelheim.
TO 022
IL‐33 AND RHINOVIRUS EFFECTS ON IL‐33 RECEPTOR EXPRESSION IN ASTHMA
Upham J1,2, Jurak L2, Xi Y2
1Princess Alexandra Hospital, Brisbane, Australia, and 2University of Queensland Diamantina Institute, Brisbane, Australia
Background
Epithelial cell‐derived interleukin‐33 (IL‐33) appears to have an important role in polarizing type 2 immune responses to allergens, though whether IL‐33 can also modify responses to respiratory viruses in asthma is not clear.
Aim
Examine the effects of IL‐33 on anti‐viral cellular immunity in asthma, focusing on the role of the two chains of the IL‐33 receptor, interleukin 1 receptor like 1 (IL1RL1; also known as ST2) and IL‐1 receptor accessory protein (IL1RAP).
Methods
Peripheral blood mononuclear cells were isolated from 16 people with mild/moderate allergic asthma and 16 healthy donors, exposed to IL‐33 (10ng/ml) and activated with rhinovirus (RV) serotype 16 for 24h. mRNA and protein expression were assessed by qPCR, flow cytometry and/or ELISA.
Results
In those with asthma, RV + IL‐33 induced greater type 2 cytokine production, whereas in control subjects, IL‐33 enhanced type 1 cytokine production. Both RV alone and RV + IL‐33 induced upregulation of IL1RL1/ST2 mRNA and surface protein expression in asthma (p=0.013 and p=0.034 respectively), but not in healthy participants. This was due to enhanced IL1RL1/ST2 expression on both type 2 innate lymphoid cells (ILC2) and conventional T‐cells. In contrast, neither RV nor IL‐33 had any effect on expression of IL1RAP expression. ILC2 cells were the major source of IL‐13 production.
Conclusion
These findings suggest dysregulation of the IL‐33 receptor IL1RL1/ST2 in asthma, and provide a mechanism by which RV infections might exacerbate type 2 inflammation in an IL‐33 rich tissue environment.
Grant Support: NHMRC and CRE for Severe Asthma
TO 023
This abstract has been withdrawn
TO 024
THE ROYAL MELBOURNE HOSPITAL THUNDERSTORM‐ASTHMA COHORT
Harun N1, Lachapelle P1,2, Bowatte G3, Lodge C3, Hinks T4, Braitberg G5, Irving L2,6, Dharmage S3,6, Douglass J1,6
1Department of Respiratory and Sleep Medicine, The Royal Melbourne Hospital, Melbourne, Victoria, Australia, 2Department of Immunology and Allergy, The Royal Melbourne Hospital, Melbourne, Victoria, Australia, 3Allergy and Lung Health Unit, School of Population and Global health, University of Melbourne, Melbourne, Victoria, Australia, 4Respiratory Medicine Unit, Nuffield Department of Medicine, University of Oxford, Oxford, UK, 5Department of Emergency Medicine, The Royal Melbourne Hospital, Melbourne, Victoria, Australia, and 6Lung Health Research Centre, University of Melbourne, Melbourne, Victoria, Australia
Introduction/Aim
We aimed to characterise people affected by the catastrophic thunderstorm‐asthma event in Melbourne, Australia in November 2016. We identified individual patient characteristics associated with hospital admission to inform research and practice in the management and prevention of the increasingly recognised and potentially fatal phenomenon of thunderstorm‐asthma.
Methods
Cross‐sectional, retrospective analysis of demographics of 240 patients presenting to The Royal Melbourne Hospital, an adult metropolitan university teaching hospital in Melbourne, and clinical characteristics of 70 of those patients who subsequently attended an outpatient clinic review.
Results
Patients were generally young adults (mean age 35 years), non‐Caucasian (60%), with seasonal rhinitis (96%) and universally (100%) sensitised to ryegrass pollen. Forty‐three patients (18%) required hospitalisation. Twenty‐six (37%) of these patients had no prior diagnosis of asthma. Amongst known asthmatics, preceding the event, 79% had active asthma symptoms. Forty‐four per cent of patients were receiving short‐acting β‐agonist therapy alone. Hospitalisation was associated with uncontrolled asthma symptoms in the month prior to the event (60%), and more symptomatic allergic rhinitis, lower lung function, higher total and ryegrass‐specific IgE and higher peripheral blood eosinophil counts measured at review.
Conclusion
Thunderstorm‐asthma affects people with seasonal rhinitis, ryegrass sensitisation and can occur without prior history of asthma, with a dramatic potential to rapidly inundate a healthcare system. Poor asthma control earlier in the hay fever season was associated with hospitalisation and inhaled corticosteroids should be considered prior to the high‐risk season in strongly sensitised individuals.
Grant Support: The authors have no potential conflict of interest to disclose.
TO 025
A SINGLE BOUT OF MODERATE‐INTENSITY EXERCISE REDUCES EOSINOPHILIC AIRWAY INFLAMMATION IN INACTIVE ADULTS WITH ASTHMA, WHILE VIGOROUS‐INTENSITY EXERCISE HAS NO EFFECT
Scott H1,2,3, Wood L2,3, Upham J4
1Lung and Allergy Research Centre, The University of Queensland, Woolloongabba, Queensland, Australia, 2School of Biomedical Sciences and Pharmacy, University of Newcastle, Callaghan, New South Wales, Australia, 3Centre for Healthy Lungs, University of Newcastle, New Lambton Heights, New South Wales, Australia, and 4Diamantina Institute, The University of Queensland, Woolloongabba, Queensland, Australia
Introduction/Aim
Exercise benefits general health, however its impact on asthma has received little attention, with the effects of exercise intensity not having been examined in this population. We previously found a single bout of moderate‐intensity exercise decreased exhaled nitric oxide in physically inactive, but not in physically active, adults with asthma. The aim of this study was to examine the acute effects of exercise intensity on airway inflammation in adults with asthma, and to examine whether this differs by usual exercise levels.
Methods
In a randomised controlled trial, adults with asthma were randomised to complete either 45 minutes of moderate‐intensity exercise (55‐70% HRmax) on a cycle ergometer (n=19), 30 minutes of vigorous‐intensity exercise (70‐85% HRmax) on a cycle ergometer (n=19) or 30 minutes of rest (n=18). Sputum cell counts were obtained the day prior to and 4 hours‐post exercise/rest.
Results
Sputum eosinophil count was lower following moderate‐intensity exercise [0 (‐26, 23]x106/mL) versus rest [9 (3, 42)x106/mL, p=0.0249]. However, sputum eosinophil count did not change following vigorous‐intensity exercise [8 (‐21, 47)x106/mL, p=0.380] versus rest. Participants who reported performing exercise causing breathlessness or sweating ≤once per week had a significant decrease in sputum eosinophil count [‐3 (‐89, 0) vs 7 (3, 142)x106/mL, p=0.006] and sputum %eosinophils [‐0.3 (‐0.7, 0)% vs 0.5 (0.1, 2.0)%, p=0.012] following moderate‐intensity exercise, compared to rest. Participants who became breathless or sweaty during exercise ≥twice/week had no change in sputum eosinophil count (p=0.395) or sputum %eosinophils (p=0.449) following the exercise challenge.
Conclusion
This study demonstrates that an acute bout of moderate‐intensity, but not vigorous‐intensity, exercise reduces sputum eosinophils in adults with asthma. This change was only evident in physically inactive participants, suggesting that regular physical activity may protect against airway inflammation.
Grant Support: TSANZ/Astra‐Zeneca Respiratory Research Fellowship; Asthma Australia Project Grant.
Cystic Fibrosis 1
TO 026
PRELIMINARY SAFETY AND EFFICACY OF TRIPLE‐COMBINATION CFTR MODULATOR REGIMENS
Tullis E1, Colombo C2, Davies J3, Wark P4, McKee C5, DeSouza C5, Waltz D5, Savage J5, Fisher M5, Shilling R5, Moskowitz S5, Tian S5, Taylor‐Cousar J6, Rowe S7
1St Michael's Hospital, ON, Canada, 2Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, University of Milan, Italy, 3Imperial College & Royal Brompton Hospital, UK, 4Department of Respiratory & Sleep Medicine, John Hunter Hospital, New South Wales, Australia, 5Vertex Pharmaceuticals Incorporated, MA, 6National Jewish Health, CO USA, and 7University of Alabama at Birmingham, AL, USA
Introduction/Aim
Prior studies with cystic fibrosis transmembrane conductance regulator (CFTR) modulators in patients heterozygous for F508del and a minimal function (MF) CFTR mutation (F508del/MF) have failed. One strategy to enhance clinical efficacy is to add a second corrector to established corrector/potentiator regimens. Safety and efficacy of 3 such next‐generation (NG) correctors (VX‐440, VX‐152, VX‐659) in triple‐combination therapy (TC) with tezacaftor (TEZ) and ivacaftor (IVA) were evaluated in patients with CF with F508del/MF or F508del/F508del genotypes.
Methods
Randomized, double‐blind, placebo‐ or active‐controlled studies of VX‐440 and VX‐152 (phase 2), and VX‐659 (phase 1) in TC were conducted in CF patients with F508del/MF (n=80) or F508del/F508del genotypes (n=40; the latter with VX‐152 and VX‐440 only; after 4 weeks of TEZ/IVA pretreatment). Primary objectives were safety and tolerability; efficacy and pharmacodynamic effects were assessed by absolute change in ppFEV1 and sweat chloride from baseline, respectively.
Results
Baseline characteristics were balanced. NG TC regimens were well tolerated; most adverse events (AEs) were mild or moderate. AEs leading to discontinuation included increased alanine aminotransferase/aspartate aminotransferase (VX‐440 TC, n=1), pneumonia (VX‐152 TC, n=1), and respiration abnormal/sputum increased (placebo, n=1). After 2 to 4 weeks, significant improvement from baseline in ppFEV1 of 9.6 to 12.0 percentage points was seen with all 3 NG TC regimens in F508del/MF patients, and significant improvement from baseline of 7.3 to 9.5 percentage points was seen with VX‐440 or VX‐152 TC on top of TEZ/IVA in F508del/F508del patients (vs TEZ/IVA baseline). Significant reductions from baseline in sweat chloride were also seen with TC regimens vs placebo or TEZ/IVA alone.
Conclusion
This is the first demonstration of substantial improvements with NG TC regimens in patients with CF with F508del/MF genotype, in whom previous CFTR modulators have failed, and in patients with CF with F508del/F508del genotype. Ongoing studies will guide development of TC regimens.
Grant Support: Sponsored by Vertex Pharmaceuticals Incorporated.
Conflict of Interest: PW was an investigator for the Next Gen clinical trial and has taken part in advisory boards for Vertex Pharmaceuticals.
TO 027
A PERIPHERAL BLOOD TRANSCRIPTIONAL PROFILE PREDICTS DISEASE SEVERITY AND THE RISK OF FUTURE EXACERBATIONS IN ADULTS WITH CYSTIC FIBROSIS (CF)
Goon K1, Baran R1, Baines K2, Wark P2
1Hunter New England Health, New Lambton Heights, Australia, and 2Hunter Medical Research Institute, New Lambton Heights, Australia
Introduction/Aim
To determine if a blood transcriptional gene signature could be used to predict risk of exacerbations in the next 12 months.
Methods
CF participants (n=21) were recruited when stable at annual review and followed for 12 months. Peripheral blood RNA was collected into Paxgene RNA tubes. RNA was extracted using the Paxgene Blood RNA Kit (Qiagen) and RNA quality and quantity was assessed using the Bioanalyser (Agilent Technologies). Transcriptional profiles were generated (Illumina HumanRef‐8 V4) and analysed using GeneSpring GX14.8.
Results
Participants had mean age 33years (13.5), mean FEV1 65% predicted (sd 22). Unsupervised hierarchical clustering of gene expression profiles revealed 2 distinct clusters. Cluster 2 (n=16) were characterised by significantly lower FEV1% predicted (p=0.036), higher residual volume % predicted (p=0.040), lower BMI (p=0.042), more frequent exacerbations requiring IV antibiotics (p=0.012), and increased presence of pseudomonas (p=0.011), compared with cluster 1 (n=5). This more severe phenotype in cluster 2 was associated with a reduction in the expression of 119 entities, including downregulation of immune regulatory genes such as IL‐10, IL‐17RD, and NLRP8.
Conclusion
Transcriptional profiles of peripheral blood can predict disease severity and future risk of exacerbations in the next 12 months.
Grant Support: n/a
TO 028
HYPERGLYCAEMIA IN YOUNG CHILDREN WITH CYSTIC FIBROSIS CORRELATES WITH INFECTION AND NEUTROPHIL BURDEN ON BRONCHOALVEOLAR LAVAGE
Prentice B1,2, Hameed S2,3, Verge C2,3, Ooi C2,4, Strachan R1, Waters S1,2, Widger J1,2
1Department of Respiratory Medicine, Sydney Children's Hospital, Sydney, New South Wales, Australia, 2School of Women's and Children's Health, The University of New South Wales, Sydney, New South Wales, Australia, 3Department of Endocrinology, Sydney Children's Hospital, Sydney, New South Wales, Australia, and 4Department of Gastroenterology, Sydney Children's Hospital, Sydney, New South Wales, Australia
Introduction
Cystic Fibrosis(CF) results in insulin deficiency from birth and progresses to Cystic Fibrosis‐related diabetes (CFRD)[1]. CFRD has a significant impact on lung function, respiratory infections, and nutrition, and leads to an increase in mortality[2]. However, the prevalence of early hyperglycaemia and impact on respiratory tract infections in young children with CF remains unknown.
Aims
To determine the prevalence of hyperglycaemia in children with CF using Continuous Glucose Monitoring (CGM) To correlate hyperglycemia on CGM with presence of CF pathogen and neutrophil percentage in routine bronchoalveolar lavage (BAL).
Methods
A single‐centre study of children with CF <5years. The CGM device (CGM Medtronic MiniMed) was inserted when clinically well during routine bronchoscopy/BAL and worn for 3 days. CGM outcomes included peak glucose, time spent >7.8mmol/L and Area Under Curve (AUC) >7.8mmol/L. BAL samples were cultured and cell count and differential determined. A t‐test and regression analysis was undertaken to examine the relationship between hyperglycaemia and the presence of CF pathogen, and neutrophil percentage on BAL.
Results
14 children (3 female) had CGMs performed, 12/14 had neutrophil percentage results available. Median age 2.44 years (range 1‐ 5.5). 3 day glucose mean=5.89±0.49mmol/L (mean± SD). 43% (6/14) had diabetic range (≥11.1mmol/L) glucose levels. Participants who had positive cultures spent a greater period of time >7.8mmol/L on CGM (mean time 9.9%) compared with culture negative participants (3%, p=0.02), and had a greater glucose AUC>7.8mmol/L (p=0.04). There was a positive correlation with peak glucose (r2=0.4, p=0.02) and AUC>7.8mmol/L (r2=0.4, p= 0.04) with neutrophil burden on lavage.
Conclusion
Young children with CF have demonstrated diabetic range hyperglycaemia on CGM. CF pathogens are more likely to be present when glucose abnormalities are more severe and a significant correlation between neutrophil count and hyperglycemia was demonstrated. Further research is underway to determine whether abnormalities on CGM in this cohort has an impact on nutrition, pulmonary inflammation and lung function.
REFERENCES
Milner AD. Blood glucose and serum insulin levels in children with cystic fibrosis. Archives of Disease in Childhood. 1969;44(235):351‐355.
Antoinette Moran et al. Cystic Fibrosis–Related Diabetes: Current Trends in Prevalence, Incidence, and Mortality. Diabetes Care Sep 2009, 32 (9) 1626‐1631.
Grant Support/Declaration of Interest: SH and CFV are grateful for funding assistance from the National Health and Medical Research Council of Australia, the Australasian Cystic Fibrosis Research Trust, Regional Diabetes Support Scheme, Sydney Children's Hospital Foundation, Australasian Pediatric Endocrine Care Grant from Pfizer, and for Industry support from Novo Nordisk, Medtronic, Abbott Diagnostics. BP was awarded the TSANZ/Vertex Cystic Fibrosis Paediatric Clinical fellowship in 2016.
TO 029
GREATER SLEEP FRAGMENTATION IS ASSOCIATED WITH LESS PHYSICAL ACTIVITY IN ADULTS WITH CYSTIC FIBROSIS
Cox N1,2, Pepin V3, Holland A1,2,4
1La Trobe University, Melbourne, Australia, 2Institute for Breathing and Sleep, Melbourne, Australia, 3Concordia University & Hôpital du Sacré‐Coeur de Montréal, Montreal, Canada, and 4Alfred Health, Melbourne, Australia
Introduction/Aim
Sleep quality in people with cystic fibrosis (CF) is known to be poor, while regular physical activity participation is associated with less decline in lung function (FEV1). The relationship between sleep quality and physical activity in people with CF is unknown. We aimed to explore any association between sleep pattern and physical activity participation in young adults with CF.
Methods
This is a secondary analysis of sleep and activity data collected via actigraphy. Adults with CF in stable health, participating in a study of physical activity (including assessment of exercise capacity), completed 7 days of activity and sleep assessment (SenseWear Armband (SWA), Bodymedia USA). Sleep characteristics were derived from accelerometer positional data and registration of sleep state by the SWA, determined by energy expenditure.
Results
Sleep and activity data were available for 47 participants (n=28 male; mean (SD) age 29(8) years; median (IQR) FEV1 60 (50 to 82) %predicted). More fragmented sleep was associated with poorer exercise capacity (rs=‐0.303, p=0.04), time spent in moderate‐vigorous physical activity (MVPA) (rs=‐0.337, p=0.020), and poorer FEV1 (rs=‐0.344, p=0.018). In a stepwise multiple regression model that included age, sex, body mass index and FEV1, models including wake after sleep onset (WASO) were significant for predicting total activity time and total MVPA time (R2=0.30 and 0.26 respectively, p<0.02). Less WASO significantly predicted more total daily activity time (ß=‐1.0, SE of ß=0.4, p=0.02), and trended toward significance for predicting greater MVPA time (ß=‐0.3, SE of ß=‐0.26, p=0.08). Greater total sleep time and sleep efficiency were related to better exercise capacity and lung function (p<0.05).
Conclusion
This analysis demonstrated a modest relationship between sleep parameters and physical activity and exercise capacity in adults with CF. Future studies of interventions to promote physical activity participation in this group should consider the relationship between sleep and activity performance.
Grant Support: NHMRC (Early Career Fellowship: 1119970); La Trobe University Research Collaboration Grant 2015
TO 030
NON‐INVASIVE MUCOCILIARY TRANSIT ASSESSMENT IN LIVE PIG TRACHEA
Donnelley M1,2, Klein M3, Hausermann D3, Hall C3, Maksimenko A3, Morgan K4,5, Parsons D1,2
1Robinson Research Institute and Adelaide Medical School, University of Adelaide, Adelaide, Australia, 2Respiratory and Sleep Medicine, Women's and Children's Hospital, North Adelaide, Australia, 3Imaging and Medical Beamline, Australian Synchrotron, Clayton, Australia, 4School of Physics, Monash University, Clayton, Australia, and 5Institute for Advanced Study, Technische Universität München, Munich, Germany
Introduction/Aim
The Imaging and Medical Beamline (IMBL) at the Australian Synchrotron was designed to be the world's widest synchrotron x‐ray beam, to facilitate clinical imaging and therapeutic applications in humans, as well as for imaging large animal models. Our group is currently interested in imaging the airways of newly‐developed CF animal models that display human‐like lung disease, such as the CF pig. We hypothesise that the ability of the lung to clear inhaled particulates by mucociliary transit (MCT) can be used as an outcome measure for assessing the effectiveness of CF airway therapies. This study extends findings from ex vivo sheep and pig tracheal tissue studies previously performed at the IMBL, and was designed to determine whether the design of the IMBL is suitable for imaging pig airways.
Methods
A small sample of 200 μm diameter high refractive index (HRI) glass bead marker particles were delivered into the tracheal airway surface of eight live piglets. Automated analysis algorithms were used to track and quantify deposited‐particle motion, including the response to aerosol delivery of hypertonic saline. A high‐resolution computed tomographic (CT) whole‐animal post‐mortem scan of one pig was also performed to verify the large‐sample CT capabilities of the IMBL.
Results
MCT tracking particles were visible in all animals, and our automated MCT tracking algorithms were able to identify and track particles. A CT of the whole animal was successfully acquired, and visualisations were successfully made from the CT dataset. Due to unexpected IMBL technical and equipment issues shuttering of the X‐ray bean was sometimes poorly controlled, resulting in high radiation doses for some animals.
Conclusion
This study demonstrated that the IMBL is suitable for large animal tracheal MCT imaging and CT. Radiation doses must be carefully and reliably controlled for future non‐recovery studies, and will enable estimation of the minimum achievable doses with this experiment design.
Acknowledgements: WCH Foundation, NHMRC Project Grant APP1079712, and http://www.cure4cf.org. Australian Synchrotron proposal number AS162/IMBL/10788.
TO 031
ABSENTEEISM AND PRESENTEEISM IMPACT WORK IN ADULTS WITH CYSTIC FIBROSIS
Lian R1, Cavalheri V1,2, Wood J1,3, Jenkins S1,2,3, Straker L1, Hill K1,2
1Curtin University, Bentley, Australia, 2Institute for Respiratory Health, Sir Charles Gairdner Hospital, Nedlands, Australia, and 3Physiotherapy Department, Sir Charles Gairdner Hospital, Perth, Australia
Introduction/Aim
People with cystic fibrosis (CF) are living longer and thus facing issues related to work. The aims of this study were to, in people with CF living in Western Australia (i) report work status and self‐reported absenteeism (absence from work due to illness) and presenteeism (loss of performance at work due to illness); and (ii) explore factors related to work status and absenteeism and presenteeism.
Methods
Secondary analyses of a larger study were conducted. Measures were collected of work status, absenteeism and presenteeism (World Health Organisation's Health Performance Questionnaire), airflow obstruction (FEV1), health‐related quality of life (HRQoL; CF Questionnaire‐Revised) and level of education. Adults with CF were grouped by work status (full‐time versus part‐time/unemployed) and self‐reported absenteeism/presenteeism (substantial versus no substantial). Between‐group differences were explored and factors related to work status and absenteeism/presenteeism were evaluated using logistic regression.
Results
Of the 50 participants (30 [25‐36]yr, percent predicted FEV1 60±18[SD]%), 34 (68%) worked full‐time. Participants reported working 30±14(SD)hr/week. Compared to those part‐time/unemployed, participants working full‐time were older (median [IQR] 33 [27 to 38]yr versus 26 [22 to 32]yr; p=0.048) and had higher levels of education (79% versus 31% completed university or other tertiary studies; p=0.002). Higher education level was associated with reduced odds of working part‐time/being unemployed (OR 0.26 95%CI [0.11 to 0.64]). Substantial absenteeism and substantial presenteeism were reported by 47% and 16% of participants, respectively. Those reporting substantial absenteeism had worse HRQoL (median [IQR] role domain score 92 [75 to 100] no substantial absenteeism versus 83 [60 to 90] substantial absenteeism; p=0.018). No associations were found for substantial presenteeism.
Conclusion
Despite moderate disease severity, most participants reported working full‐time. Cystic fibrosis may have a greater impact upon absenteeism than presenteeism; however, larger studies are needed to determine the reasons for this greater impact.
Grant Support: This study was partially funded by a Sir Charles Gairdner Group Research Advisory Council Grant.
Declaration of Interest: Nil.
Declaration of Interest: Nil.
Occupational & Environmental Lung Disease / Population Health
TO 032
SMOKING, FAMILY HISTORY AND ASBESTOS EXPOSURE ARE ASSOCIATED WITH IPF
Abramson M1, Murambadoro T1, Alif S1, Benke G1, Dharmage S2, Ellis S3, Glaspole I4, Hopkins P5, Hoy R1,4, Klebe S6, Miller A7, Moodley Y8, Ng B3, Rawson S1, Reynolds P9, Rouse H10, Wolfe R1, Walters E11, Corte T12
1Public Health & Preventive Medicine, Monash University, Melbourne, Australia, 2Population & Global Health, University of Melbourne, Parkville, Australia, 3Radiology, The Alfred, Prahran, Australia, 4Respiratory Medicine, The Alfred, Prahran, Australia, 5The Prince Charles Hospital, Chermside, Australia, 6Anatomical Pathology, Flinders Medical Centre, Bedford Park, Australia, 7Radiology, Royal North Shore Hospital, St Leonards, Australia, 8University of Western Australia, Claremont, Australia, 9Royal Adelaide Hospital, Adelaide, Australia, 10Medical Imaging, St Vincents Hospital, Fitzroy, Australia, 11Medicine, University of Tasmania, Hobart, Australia, and 12Royal Prince Alfred Hospital, Camperdown, Australia
Introduction/Aim
Idiopathic Pulmonary Fibrosis(IPF) is a progressive scarring lung disease of unknown cause with limited treatment and a median survival of 2‐3 years. Our aim was to identify potential occupational and environmental exposures associated with development of IPF in Australia.
Methods
Cases were recruited by the Australian IPF registry. Patients completed a questionnaire about demographics, smoking, family history, environmental and occupational exposures, and medical history. Clinical, radiological and histopathological data were reviewed by a multidisciplinary panel. Population based controls were recruited by random digit dialling, frequency matched on age, sex and state, and interviewed to collect comparable data. Multivariate logistic regression was used to assess associations with IPF as Odds Ratios(OR) and 95% confidence intervals(95%CI), adjusted for age, sex and smoking.
Results
Data were from 374 cases assessed by multidisciplinary discussion as definite, probable or possible IPF, and 902 controls. The mean±SD age of cases was 71.2±7.8 and controls 70.8±8.4 years. 72% cases and 69% controls were male. Current or past tobacco smoking was associated with increased risk of IPF: OR=2.24 (95%CI 1.72, 2.91), but marijuana use appeared protective: 0.43 (0.26, 0.70). A family history of pulmonary fibrosis was associated with 14.1 (7.14, 27.9) fold increased risk of IPF. No domestic environmental exposures were associated with increased risk, but pet birds or standing water appeared protective (OR=0.51; 0.34, 0.78 and 0.57; 0.36, 0.89 respectively). Self‐reported occupational exposure to asbestos was associated with increased risk: OR=1.38 (1.06, 1.79), but silica appeared protective: 0.60 (0.42, 0.85). Self‐reported occupational exposures to gases, fumes, chemicals or dust were not associated with IPF.
Conclusion
Preliminary findings suggest that the burden of IPF could be reduced by continued tobacco control measures and preventing ongoing exposure to asbestos. More detailed assessment of occupational exposures will be undertaken using the Finnish job exposure matrix(FINJEM).
Grant Support
NHMRC
TO 033
LONGITUDINAL SURVEILLANCE OF METROPOLITAN FIREFIGHTERS INDICATES NORMAL LUNG FUNCTION DECLINE
Slattery F1, Johnston K2, Paquet C2, Crockett A1
1Alliance for Research in Exercise, Nutrition and Activity (ARENA), Sansom Institute, School of Health Sciences, University of South Australia, Adelaide, Australia, and 2School of Health Sciences, Sansom Institute for Health Research, University of South Australia, Adelaide, Australia
Introduction/Aim
Longitudinal surveillance of firefighter lung function is highly valuable, especially considering its utility in determining changes in function following disastrous exposures. Studies investigating the long‐term rate of change in lung function parameters of firefighters, however, have produced mixed findings. We aimed to determine the rate of change in FEV1 and FVC of a contemporary cohort professional South Australian Metropolitan Fire Service (SAMFS) firefighters.
Methods
Spirometry was conducted in 5 stages between 2007 and 2016 on all available and consenting full‐time firefighting staff, in accordance with ATS/ERS criteria using a Viasys MasterScreen® spirometry system. We examined serial FEV1 and FVC measurements to determine the average rate of change using linear mixed effects modelling.
Results
Participation at each stage of data collection ranged from approximately 48‐64%. Data from 838 individual male firefighters, each contributing an average of 2.6 ± 1.1 (range 1‐5) measurements, were included in the analysis. Fifty per cent of included firefighters had at least three measurements. Preliminary analyses show that the proportion of firefighters below the lower limit of normal (LLN) at baseline was 0.7% for FEV1, 0.0% for FVC and 14.2% for FEV1/FVC, while longitudinally, FEV1 (adjusted for baseline age and height) declined by 34 (95% CI, 30 to 37) mL/yr while FVC declined by 24 (95% CI, 20 to 29) mL/yr.
Conclusion
The SAMFS firefighters observed in this study showed normal levels of FEV1 and FVC at baseline; unsurprising given that they are selected, in part, based on their physical fitness. Early results indicate that the cohort have a normal rate of change in FEV1 and FVC, suggesting that their lung function remains relatively unaffected by their occupation.
Grant Support
This research was supported by the South Australian Metropolitan Fire Service and an Australian Government Research Training Program Scholarship (FS).

TO 034
ASSESSING THE SUITABILITY OF FRACTIONAL EXHALED NITRIC OXIDE (FENO) CUT‐OFF RANGES FOR ABORIGINAL AND/OR TORRES STRAIT ISLANDER CHILDREN AND YOUNG ADULTS
Blake T1,2,3, Chang A2,3, Chatfield M4, Petsky H5, McElrea M1,2,3
1Centre For Children's Health Research, South Brisbane, Australia, 2Indigenous Respiratory Outreach Care (IROC) Program, Chermside, Australia, 3Department of Respiratory and Sleep Medicine, Lady Cilento Children's Hospital, South Brisbane, Australia, 4QIMR Berghofer Medical Research Institute, Herston, Australia, and 5School of Nursing and Midwifery, Griffith University, Nathan, Australia
Introduction/Aim
Fractional exhaled nitric oxide (FeNO) is used as a non‐invasive measure of eosinophilic airway inflammation. It is unknown how appropriate the recommended FeNO cut‐off ranges are for Aboriginal and/or Torres Strait Islander patients. Our aim was to assess the distribution of healthy Aboriginal and/or Torres Strait Islander FeNO results according to current American Thoracic Society cut‐off guidelines.
Methods
We measured FeNO (using Aerocrine NioxMINO) in 991 Indigenous children and young adults (aged 3 to 25 years) from seven Queensland communities. Questionnaires and medical charts were reviewed to identify healthy participants (no respiratory and/or atopic illness ever).
Results
Acceptable FeNO measurements were achieved by 553 children (≤12 years) and 288 adults (>12 years). Participants with a history of respiratory and/or atopy conditions were excluded resulting in a healthy cohort of children (n=401, 72.5%) and adults (n=193, 67%). The geometric mean FeNO results for children and adults were 11.1ppb and 12.5ppb respectively. Table 1 summarises the distribution of healthy FeNO results for each ethnic group according to current cut‐off ranges.
Conclusion
Although the majority of participants had FeNO results within the age‐respective normal ranges, we found a proportion of healthy participants with elevated FeNO results in all groups. The greatest proportion of elevated results was seen in Torres Strait Islander children and adults, and Aboriginal/Torres Strait Islander children. This suggests that the recommended cut‐off ranges may not be appropriate for these groups. Further investigation is still needed.
Grant Support
IROC Program (Qld Health) and CRE for Indigenous Lung Health in Children. NHRMC PhD Scholarship (TB), NHMRC Practitioner Fellowship (AC).
TO 035
LUNG CANCER SCREENING IN THE WESTERN AUSTRALIAN ASBESTOS REVIEW PROGRAM
Harris E1,2, Murray C3, Franklin P4, Sodhi‐Berry N4, Reid A5, Olsen N4, Hall D1, De Klerk N4, Musk A1,4, Brims F1,2,6
1Sir Charles Gairdner Hospital, Perth, Australia, 2Curtin Medical School, Curtin University, Perth, Australia, 3Royal Perth Hospital, Perth, Australia, 4School of Population and Global Health, University of Western Australia, Perth, Australia, 5School of Public Health, Curtin University, Perth, Australia, and 6Institute for Respiratory Health, Perth, Australia
Introduction
Asbestos exposure increases the risk of lung cancer, especially in smokers. Western Australia (WA) has the highest rates of asbestos‐related diseases in the world, due to crocidolite mining in the Pilbara town of Wittenoom and the widespread use of asbestos throughout WA. Early diagnosis utilising low dose CT (LDCT) scans have been shown to reduce mortality from lung cancer.
Aim
To analyse the efficacy of LDCT in detection of lung cancer in an asbestos‐exposed population over a 5‐year period.
Methods
In 2012, the Asbestos Review Program (based at Sir Charles Gairdner Hospital) began performing annual LDCT to screen an asbestos‐exposed population for asbestos related lung disease and lung cancer. Population: Wittenoom miners and residents, other individuals with >3 months cumulative full time exposure. All participants had a prone LDCT scan with annual health questionnaire (including smoking status), spirometry and gas transfer.
Results
5907 LDCT scans were performed on 1760 individuals with a median age of 70 years (IQR 63‐76), 1490 (85.1%) were male and 1115 (63.7%) were ever‐smokers. Lung cancer was diagnosed in 17 participants (0.97% of the cohort), 15 (pre‐operative stage 1a or b) underwent treatment with curative intent, 2 underwent non‐curative chemo‐radiation. Lung cancer was prevalent in 10 (59%), and incident in 7 (41%) individuals (see Table 1). One participant died 4 months after surgery (found to have M1a disease during operation); no participants treated curatively have had reoccurrence to date. Mesothelioma was diagnosed in 7 other individuals. Asbestosis was present in 40.3% of the ARP population and 64.0% had pleural plaques, confirming significant asbestos exposure. The median radiation exposure per LDCT was 0.20mSv (IQR 0.14‐0.52).
Conclusions
A carefully controlled LDCT screening program is effective at diagnosing and treating early‐stage lung cancer in this population. Occupational exposure to asbestos should be accounted for in assessing risk for lung cancer.
Table. 1. Characteristics of ARP participants diagnosed with lung cancer

TO 036
NITROGEN DIOXIDE IS ADVERSELY ASSOCIATED WITH TRANSFER FACTOR OF CARBON MONOXIDE IN A DOSE‐RESPONSE MANNER
Perret J1, Bowatte G1, Knibbs L2, Lodge C1, Johns D3, Lowe A1, Thomas P4, Giles G5, Morrison S2, Walters E1, Abramson M6, Dharmage S1
1The University Of Melbourne, Melbourne, Australia, 2University of Queensland, Brisbane, Australia, 3University of Tasmania, Hobart, Australia, 4University of New South Wales, Sydney, Australia, 5Cancer Council Victoria, Melbourne, Australia, and 6Monash University, Melbourne, Australia
Introduction/Aim
While air pollution exposure can contribute to the development of chronic obstructive pulmonary disease (COPD), previous studies have not examined lung function beyond the airways. We aimed to examine relationships between exposure to nitrogen dioxide (NO2, a gaseous air pollutant) and complex post‐bronchodilator (post‐BD) lung function measures in middle‐aged Australians.
Methods
Cross‐sectional data were obtained from the Tasmanian Longitudinal Health Study (n=1,389) when participants were 45 years of age. Annual outdoor mean NO2 concentrations at participants' residential addresses were estimated using a validated satellite‐based, land‐use regression model. Multivariable regression used post‐BD spirometry, carbon monoxide transfer factor (TLco) and static lung volumes as continuous outcomes.
Results
Median NO2 exposure was 3.66 [interquartile range 2.95, 5.22] parts per billion. Increasing exposure to NO2 was associated with reduced TLco in a dose‐response manner [p‐for‐trend<0.001]. Compared with the lowest quartile of NO2 exposure, the reduction in TLco was equivalent to 7.7% of predicted for the highest NO2 quartile (95%CI: −10.8 to −4.5) independent of smoking, and was significantly lower for those with current asthma [p(interaction)=0.005]. There was a trend to reduced TLC [p‐for‐trend=0.02], and reductions in post‐BD FVC for non‐ and past but not current smokers exposed to the highest NO2 quartile [non‐smokers −2.6% pred, p=0.042, p(interaction)=0.056]. There were no statistically significant relationships with post‐BD FEV1/FVC, FEF25‐75% or gas trapping (RV/TLC).
Conclusion
We provide evidence for a moderate adverse association between NO2 exposure and TLco at relatively low pollution levels, that varies with current asthma status. Other non‐obstructive features favour a lung parenchymal process, although co‐existent small airway narrowing may be masked by reduced FVC levels. This new knowledge supports environmental policy to reduce NO2 levels to as low as feasible.
Grant Support
NHMRC including Centre for Air quality, health Research and evaluation (CAR); Clifford Craig Foundation; Asthma Foundations (TAS VIC QLD)
TO 037
MIDDLE‐AGE LUNG FUNCTION DECLINE IS PREDOMINANTLY INFLUENCED BY ADULT FACTORS AND THEIR INTERACTIONS WITH CHILDHOOD AND GENETIC FACTORS
Bui D1, Walters H1, Burgess J1, Bui M1, Perret J1, Bowatte G1, Lowe A1, Graham G2, Erbas B3, Morrison S4, Feather I5, James A6, Thomas P7, Hamilton G8,9, Abramson M10, Lodge C1, Dharmage S1
1The University Of Melbourne, Melbourne, Australia, 2Cancer Epidemiology Centre, Cancer Council Victoria, Melbourne, Australia, 3School of Psychology and Public Health, La Trobe University, Melbourne, Australia, 4University of Queensland, Brisban, Australia, 5Gold Coast Hospital, Gold Coat, Australia, 6Sir Charles Gairdner Hospital, Perth, Australia, 7University of New South Wales, Sydney, Australia, 8Monash Lung and Sleep, Monash Health, Melbourne, Australia, 9School of Clinical Sciences, Monash University, Melbourne, Australia, and 10School of Public Health & Preventive Medicine, Monash University, Melbourne, Australia
Introduction/Aim
Accelerated adult lung function decline is a major pathway to chronic obstructive pulmonary disease. We sought to investigate associations and interactions between life span factors and lung function decline during middle age.
Methods
Post‐bronchodilator lung function was measured at 45 and 53 years in 842 participants from the Tasmanian Longitudinal Health Study. We used multivariate linear regression to investigate associations of factors in adulthood (current asthma, smoking, atopy, BMI, BMI change, occupational exposures and traffic related air pollution), childhood (pneumonia, asthma, parental asthma and parental smoking) and Glutathione S‐transferase gene polymorphisms, with the rate of lung function decline between 45 and 53 years. Interactions between factors were also investigated.
Results
Current asthma (‐6; 95%CI: ‐11,‐1 mL/year), current smoking (‐16; ‐21,‐10 mL/year), atopy (‐5; ‐9,‐0.7 mL/year), all at 45 years, lifetime occupational exposure to vapour/gas/dust/fumes (‐6; ‐11,‐1 mL/year) and increased BMI during the follow‐up period (‐2; ‐2.6,‐1.5 mL/year per kg/m2 increase) were independently associated with accelerated FEV1 decline after controlling for age, height, sex, socioeconomic status and lung function at baseline (45 years). Current smoking (‐12; ‐18,‐6 mL/year) and BMI change (‐2.5; ‐3.2,‐1.9 mL/year per kg/m2 increase) were associated with greater FVC decline. GTTM1 polymorphism modified the effect of occupational exposure (p=0.06 and 0.07), and heavy maternal smoking during childhood modified the effect of personal smoking (p=0.03 and 0.02) on both FEV1 and FVC decline. The effect of occupational exposure was only significant for carriers of the GSTM1 null genotype, and the effect of personal smoking was augmented in those also exposed to maternal smoking.
Conclusion
Lung function decline in this middle‐aged sample was predominantly influenced by adult factors. Exposure to maternal smoking during childhood and genetic susceptibility may predispose people to being more susceptible to adulthood exposures.
Grant Support
National Health and Medical Research Council of Australia, Clifford Craig Medical Research Trust of Tasmania; Victorian, Queensland & Tasmanian Asthma Foundations
Declaration of Interest Statement
There is no conflict of interest.
Primary Care/ Palliative Care/ Tobacco
TO 038
PERSONAL VAPORIZER E‐JUICES AND AEROSOLS VARY WIDELY IN PHYSICOCHEMICAL PROPERTIES
Chivers E1, Mullins B2, Musk B3, Huxley R4, Franklin P3,5, Larcombe A1,2
1Respiratory Environmental Health, Telethon Kids Institute, Perth, Australia, 2Occupation & Environment, School of Public Health, Curtin University, Perth, Australia, 3School of Population Health, University of Western Australia, Crawley, Crawley, Australia, 4College of Science, Health & Engineering, La Trobe University, Melbourne, Australia, and 5Environmental Health Directorate, Department of Health, Perth, Australia
Introduction/Aim
Personal vaporizers (“electronic‐cigarettes”) aerosolise a liquid “e‐juice” producing an aerosol which is inhaled. There is no regulation of e‐juice ingredients. There are tens‐of‐thousands of different flavours, nicotine concentrations and excipient blends available from thousands of suppliers. Furthermore, while many ingredients are approved as food additives, inhalation toxicology data may be unavailable. We aimed to test the physico‐chemical properties of a range of e‐juices and aerosols to (i) identify potentially toxic substances and (ii) to see whether ingredients match labelling.
Methods
18 e‐juices were obtained from Australian and US retailers. E‐juice chemistry was analysed via GC‐MS. Aerosols were generated using a custom‐made device based on an Innokin MVP2 vaporizer / Innokin iClear30 cartomizers set at 2.1Ω and 4.2V. Aerosols were collected for 30 minutes using appropriate filters and collection tubes. We assessed levels of carbonyls, volatile organics, polycyclic‐aromatics, nicotine, particulate matter and metals. Aerosol mass and size distributions were measured using an optical particle spectrometer.
Results
28 different chemicals were detected in e‐juices including known respiratory irritants such as 2‐chlorophenol and 1,2,3‐butantriol. Nicotine was detected in 6 apparently “nicotine‐free” juices. Seven metals were identified in aerosols, including titanium, chromium and nickel. We also identified 7 carbonyls, however only formaldehyde, acetaldehyde and acetone were common. Sixteen volatile organics were identified. The solvents hexane and 2‐ethoxy ethanol were ubiquitous in all samples. No poly‐cyclic aromatics were detected. Aerosols contained particulate matter at hugely varying levels (3.3 to 63mg/m3) and particle size distributions also varied considerably, apparently based on the excipient mixture.
Conclusion
The physico‐chemical properties of e‐juices and aerosols vary widely and hence their potential to impact health is also likely to vary. Importantly, nicotine was found in many “nicotine‐free” juices, which has implications for addiction.
Grant Support: Department of Health, WA, Telethon Kids Institute, Curtin University, NH&MRC and the ACCC
TO 039
PHARMACIST‐LED SMOKING CESSATION INTERVENTION IN AUSTRALIAN PRIMARY CARE TARGETING SMOKERS AT RISK OF DEVELOPING COPD
Liang J1, Abramson M2, Zwar N3, Russell G4, Holland A5, Bonevski B6, Mahal A7, Phillips K8, Eustace P9, Paul E2, George J1
1Centre for Medicine Use and Safety, Monash University, Australia, 2Department of Epidemiology and Preventive Medicine, Monash University, Australia, 3School of Medicine, University of Wollongong, Australia, 4School of Primary Health Care, Monash University, Australia, 5Department of Physiotherapy, La Trobe University, Australia, 6School of Medicine and Public Health, University of Newcastle, Australia, 7Nossal Institute of Global Health, University of Melbourne, Australia, 8Lung Foundation Australia, , Australia, and 9Eastern Melbourne PHN, Australia
Introduction
Tobacco smoking is the most preventable risk factor in the development of COPD. Approximately one in five patients attending general practice is a smoker. We describe a pharmacist‐led smoking cessation intervention as part of an interdisciplinary model of care (RADICALS) aimed at reducing the burden of COPD and smoking in Australian primary care.
Methods
General practices (n=43) were block‐randomised into ICG (interdisciplinary care group) or UCG (usual care group). Patients aged ≥40 years and self‐reporting being current or ex‐smokers with a smoking history of ≥10 pack years, and/or those who were managed as having COPD were invited to participate. Participants in UCG practices received routine care from their GP and Quitline referral, if appropriate. In ICG, individualised smoking cessation support was coordinated by a pharmacist on‐site and offered to participants who were current smokers. Smoking cessation support was also provided by a consultant pharmacist during a home medicines review in participants with COPD. Pharmacotherapy was recommended and discussed with the participant's GP, if appropriate. Exhaled CO‐verified 7‐day point prevalence abstinence and changes in nicotine dependence at 6 and 12 months from baseline are outcomes.
Results
A total of 1,055 participants with a range of demographic and clinical characteristics were recruited. Of these, 693 (65.7%) were current smokers; almost all smoked daily (649, 93.7%). Median exhaled CO was 21ppm [IQR 13‐28]. Smokers in ICG practices (n=373) were at various readiness‐to‐quit stages. Tailored pharmacist interventions ranged from motivational counselling/Quitline referral to advising on nicotine replacement therapy/varenicline use. Six month follow‐ups are now complete (n=370); 12 month follow‐ups will be completed by February 2018.
Conclusion
Pharmacists working with GPs can assist smokers attending general practices to quit using pharmacotherapy and non‐pharmacological approaches.
Grant/in‐kind support: NHMRC, Lung Foundation Australia, Boehringer Ingelheim, Eastern Melbourne PHN, Cyril Tonkin Scholarship
TO 040
AUSTRALASIAN MALIGNANT PLEURAL EFFUSION (AMPLE)‐1 RANDOMIZED CONTROLLED TRIAL OF INDWELLING PLEURAL CATHETER VERSUS TALC PLEURODESIS
Lee Y1,2,3, Fysh E1,2,3, Smith N4, Lee P5, Kwan B6, Yap E7, Horwood F7, Piccolo F8, Lam D9, Garske L10, Shrestha R11, Kosky C2,12, Read C3, Murray K13, Thomas R1,2,3
1Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Australia, 2School of Medicine & Pharmacology, University of Western Australia, Perth, Australia, 3Pleural Medicine Unit, Institute for Respiratory Health, Perth, Australia, 4Medical Research Institute of New Zealand, Wellington, New Zealand, 5Division of Respiratory & Critical Care Medicine, Department of Medicine, Yong Loo Lin Medical School, National University of Singapore, Singapore, Singapore, 6Department of Respiratory Medicine, St George Hospital & Sutherland Hospital, Sydney, Australia, 7Department of Respiratory Medicine, Middlemore Hospital, Auckland, New Zealand, 8Department of Internal Medicine, St John of God Midland Hospital, Perth, Australia, 9Department of Medicine, University of Hong Kong, Hong Kong, China, 10Department of Respiratory and Sleep Medicine, Princess Alexandra Hospital, Brisbane, Australia, 11Department of Respiratory Medicine, Fiona Stanley Hospital, Perth, Australia, 12Department of Pulmonary Physiology & Department of General Medicine, Sir Charles Gairdner Hospital, Perth, Australia, and 13School of Population and Global Health, University of Western Australia, Perth, Australia
Introduction
Hospital admissions and multiple pleural interventions for symptom relief are often required in the management of malignant pleural effusions (MPEs). Current literature suggested that talc pleurodesis and indwelling pleural catheter (IPC) offer similar quality‐of‐life benefits, resulting in equipoise. No studies have previously examined hospitalization of MPE patients in their remaining lifespan as the principle endpoint, an outcome of significance to these patients who often have limited prognoses.
Method
An open‐labelled, randomized controlled trial: ACTRN12611000567921. Nine units from Australia, New Zealand, Singapore and Hong Kong recruited 146 MPE patients randomized (1:1) to IPC or talc slurry pleurodesis; minimized by Australasia vs Asia, mesothelioma vs metastatic malignancies, and trapped lung (vs not). The primary endpoint is total days of hospitalization from treatment to death, or 12‐month follow‐up.
Results
The IPC group spent significantly fewer days in hospital than the Pleurodesis group: median (IQR) 10.0 (14) vs 12.0 (14) days, p=0.026, which represented 6.2 (13.8)% vs 11.1 (33.7)% of their remaining lifespan in hospital respectively, p=0.01. Mean reduction in hospitalization days was 3.6 days/patient: 12.7 (IPC) vs 16.3 (Pleurodesis) days. The reduction was mainly in effusion‐related hospitalizations: median 1.0 (IPC) vs 4.0 (Pleurodesis) days, p<0.001, though fewer non‐effusion related hospitalization days were observed with IPC treatment. Fewer IPC‐treated patients required further invasive pleural drainages (4.1% vs 22.5%, 95% CI 7.7‐29.2%). Both treatments provided significant improvement in breathlessness (assessed by Visual Analog Score) and quality‐of‐life (EQ5D), and had comparable complication rates.
Conclusion
Treatment of MPE with IPC can reduce lifetime hospitalization days and further invasive pleural procedures compared with conventional talc pleurodesis, without compromising on symptomatic improvement. These data will inform patients' decision on treating options. Extrapolating from this result, use of IPC (instead of talc slurry pleurodesis) for MPE can save up to 14,000 bed days in Australia each year.
Grant Support: Project grants from Cancer Council Western Australia and Sir Charles Gairdner RAC. Fellowship funding from NHMRC (YCGL & RT), Cancer Council WA (RT) and Raine Foundation (ET)
Declaration: Rocket Med Ltd has provided free IPC drainage kits and an unrestricted educational grant for previous trials led by YCGL. YCGL has served on advisory boards of Carefusion/BD and Sequana Med Ltd.
TO 041
PALLIATION AND THE USE OF DIAGNOSTIC TESTS IN PATIENTS DYING IN HOSPITAL FROM COPD
Ross L1, Taverner J1, Bartlett C1, Irving L1, Philip J2, Smallwood N1
1Royal Melbourne Hospital, Parkville, Australia, and 2St Vincent's Hospital, Melbourne, Fitzroy, Australia
Introduction/Aim
COPD is an incurable, progressive illness, with associated significant morbidity and mortality. Accurately determining prognosis in severe COPD is well‐recognised to be challenging, as is diagnosing “active dying”.
Aim
To audit the use of diagnostic tests in both recognising active dying and after establishing the “Goal of Care” (GOC) was palliation in COPD patients dying in hospital.
Method
A retrospective audit of 475 consecutive patients who died from COPD at an Australian teaching hospital between 2004‐2016.
Results
Of 221 patients included: 136 (60%) male, median age 80 years; median respiratory function: FEV1 0.8L (41%), FVC 2.0L (73%) and DLco 9 (41%); and 109 (49%) used home oxygen. 63 (29%) patients had palliative care involvement prior to the final admission.
During the terminal admission patients received on average 7 episodes of venepuncture, 9 Arterial Blood Gas tests and 3 chest radiographs. Receiving increased diagnostic tests was associated with age <70years, admission under respiratory medicine team, ICU admission, and radiological evidence of pneumonia on admission.
For 187 (85%) patients, the GOC was documented as palliation during the final admission, a median of 1.8 days prior to death. 131 (70%) patients had diagnostic tests performed on the day palliation was initiated, and despite the change in GOC 22 (12%) patients had further tests following palliation. 70 (32%) had tests on the day they died.
Conclusion
Excessive, unnecessary diagnostic tests were performed in one third of inpatients dying from COPD, including those following a clear decision to palliate. Failure to clinically diagnose active dying imposes an unnecessary burden of diagnostic tests on those in their final hours.
Key Words
Palliation, COPD, diagnostic tests
Nomination for New Investigator Award: N/A
Grant Support: N/A
TO 042
A CLUSTER RANDOMIZED TRIAL OF AN INTERDISCIPLINARY INTERVENTION FOR COPD IN AUSTRALIAN PRIMARY CARE
Liang J1, Abramson M2, Zwar N3, Russell G4, Holland A5, Bonevski B6, Mahal A7, Phillips K8, Eustace P9, Paul E2, George J1
1Centre for Medicine Use and Safety, Monash University, Victoria, Australia, 2Department of Epidemiology and Preventive Medicine, Monash University, Victoria, Australia, 3School of Medicine, University of Wollongong, New South Wales, Australia, 4School of Primary Health Care, Monash University, Victoria, Australia, 5Department of Physiotherapy, La Trobe University, Victoria, Australia, 6School of Medicine and Public Health, University of Newcastle, New South Wales, Australia, 7Nossal Institute of Global Health, University of Melbourne, Victoria, Australia, 8Lung Foundation of Australia, Queensland, Australia, and 9Eastern Melbourne PHN, Victoria, Australia
Introduction
Interdisciplinary practice‐based interventions could potentially benefit patients with COPD in primary care. We describe the RADICALS (Review of Airway Dysfunction and Interdisciplinary Community‐based care of Adult Long‐term Smokers) model of care delivered in Australian general practices.
Methods
General practices (n=43) were block‐randomised into ICG (interdisciplinary care group) or UCG (usual care group). Patient participants with spirometry‐confirmed COPD in UCG practices received routine care from their GP and Quitline referral, if appropriate. ICG participants received the RADICALS model of care, coordinated by a research assistant, GPs and staff at each clinic. The model comprised individualised smoking cessation support, a home medicines review (HMR) from a consultant pharmacist, and home‐based pulmonary rehabilitation from specifically trained physiotherapists. The primary endpoint is change in Health Related Quality of Life (HRQoL), as measured by the St George's Respiratory Questionnaire (SGRQ), at 6 months from baseline. Other outcomes include changes in lung function, dyspnoea, COPD assessment test (CAT) score and EuroQol‐5D at 6 and 12 months.
Results
A total of 275 patients with COPD were included – 161 in ICG and 114 in UCG. Their mean (±SD) age was 64.4 (±11.0) years; 171 (62%) were male and 168 (61%) were current smokers. Mean/median baseline SGRQ, CAT and mMRC scores were 32.3 (±18.2), 13.1 (±7.8) and 1 [IQR 0‐2]. A total of 85 ICG participants received the HMR, 71 completed home‐based pulmonary rehabilitation, and 62 received both components. Six month follow‐ups are complete (n=208); 12 month follow‐ups are in progress and will be completed by February 2018.
Conclusion
An interdisciplinary model of care for COPD has been developed, implemented and evaluated in general practice. HMR and home‐based pulmonary rehabilitation had moderate acceptance as interventions by GPs and patients.
Grant/in‐kind support: NHMRC, Lung Foundation Australia, Boehringer Ingelheim, Eastern Melbourne PHN, Cyril Tonkin Scholarship
Conflict of Interest: Funding was received from Boehringer Ingelheim. Boehringer Ingelheim was involved in project discussions, planning and progress review, but had no involvement in the design of the intervention program and will not be contributing to decisions regarding data analysis and dissemination of findings.
TO 043
LUNG FOUNDATION AUSTRALIA (LFA) CONSUMER SURVEY RESULTS 2017
Allan H1, Phillips K, Aami D, McDonald C2
1Lung Foundation of Australia, Brisbane, Queensland, Australia, and 2Faculty of Medicine, University of Melbourne, Melbourne, Victoria, Australia
Introduction
LFA undertook a survey to gain insight into the key issues facing consumers and carers, and to understand how LFA meets ‐ or can better meet – their needs.
Methods
9,000 surveys were distributed (via email and post) to consumers with any lung disease that subscribe to the LFA network.
Results
1700 surveys were completed, representing a response rate of approximately 19%. Of these, 65% were female, 57% were aged between 65‐79 years, 87% had a lung disease and 13% were carers. Respondents indicated that 39% see family and friends less often, 29% feel isolated from society and 59% do the things they love less often because of their lung disease. When asked specifically about how they felt at time of diagnosis, 30% felt less deserving of help than people with other medical conditions, 23% felt shame, guilt or fear of being discriminated against, 41% felt stigmatised by the view that lung diseases are self‐inflicted and smoking‐related and 58% felt they had all the support they needed to deal with the diagnosis. Suggestions were received about additional LFA supports; responses highlighted the need for psychosocial support through more telephone, online and face‐to‐face connection with LFA and other consumers, as well as the need for additional education seminars and webinars, and more information on specific disease treatments and research.
Conclusion
People impacted by lung disease face many challenges. This survey has detailed the effect on community and social interactions, with feelings of isolation and less contact with loved ones highlighted. Also it demonstrates the shame, stigma and guilt some people may experience when diagnosed with a lung disease.
Grant support: LFA receives financial support from donors, philanthropic trusts and foundations, fundraising and corporate partners
Cell, Immunology & Molecular Biology of the Lung 1
TO 044
HDAC6 PROMOTES DDX1‐MEDIATED ANTIVIRAL IMMUNITY AND IS IMPAIRED IN COPD
Hsu A1, Hansbro P1, Wark P1,2
1University of Newcastle, Newcastle, Australia, and 2John Hunter Hospital, Newcastle, Australia
Introduction/Aim
COPD primary bronchial epithelial cells (pBECs) are characterised with deficient innate antiviral response to influenza virus infection, leading to heightened viral replication. The molecular mechanisms underpinning this deficiency is unclear. HDAC6 is a unique cytoplasmic deacetylase, its roles in innate immunity is less well characterised. In this study we aim to determine the function of HDAC6 in antiviral immunity, and how HDAC6 expression/function is altered in COPD pBECs.
Methods
CRISPR‐Cas9 HDAC6 Knockout plasmid and HDAC6‐plasmid was transfected into a human minimally immortalised bronchial epithelial cell line BCi‐NS1.1, and infected with H1N1. Protein interactions/expression levels were measured by immunoprecipitation, immunoblotting, and cytometric bead array. Viral replication was measured by plaque assay. pBECs from those with COPD (GOLD III‐IV) and healthy controls were infected with H1N1. Similar measurements were performed.
Results
HDAC6 deficiency showed an overall reduction in antiviral response. Immunoprecipitation (IP) of HDAC6, mass spectroscopy, and co‐IP identified that DDX1 is a direct binding target. DDX1 is an important viral RNA sensor. We found that HDAC6 deacetylated DDX1 and promoted DDX1‐mediated type I and III interferon (IFN) induction. HDAC6 expression, DDX1 deacetylation, and antiviral responses were reduced in COPD pBECs. This reduction in HDAC6 expression in COPD pBECs was due to increased expression of miRNAs miR‐141/‐200a. Inhibition of miR‐141/‐200a increased HDAC6‐DDX1‐mediated antiviral response and decreased viral replication in both COPD and healthy control pBECs.
Conclusion
HDAC6 is essential in DDX1‐mediated antiviral signaling to influenza viral infection, reduced HDAC6 expression and DDX1 deacetylation in COPD led to deficient antiviral signalings and increased viral replication, which could be restored by specific inhibition of miR‐141/‐200a.
Grant Support: Alan Hsu is supported by The Thoracic Society of Australia and New Zealand (TSANZ) / AstraZeneca Respiratory Research Fellowship. This study is funded by University of Newcastle Early Career Research Grant and NH&MRC.
TO 045
NONTYPEABLE HAEMOPHILUS INFLUENZAE (NTHi) EXPLOITS DEFECTS IN AIRWAY EPITHELIAL CELL XENOPHAGY AS A MEANS OF PERSISTENCE DURING COPD
Roscioli E1,2, Bac‐Tran H1, Kicic A3, Poh M3, Jersmann H1,2, Hodge S1,2
1Royal Adelaide Hospital, Adelaide, Australia, 2University of Adelaide, Adelaide, Australia, and 3Telethon Kids Institute, Subiaco, Australia
Introduction/Aim
NTHi infection causes approximately 50% of COPD exacerbations, inflammation, and FEV1 decline. Normally intracellular microbes are degraded by microbe‐specific autophagy (xenophagy). We hypothesise NTHi exploits defects in xenophagy in COPD, potentiated by cigarette smoke, enabling infection and propagation between airway epithelial cells (AEC).
Methods
Cultures of bronchial AEC (bAEC) lines, and from control and COPD donors differentiated at an air‐liquid interface (ALI) were exposed to 10% cigarette smoke‐extract (CSE) and NTHi. Markers of xenophagic flux and intracellular NTHi were assessed using western analysis, immunofluorescence and transmission electron microscopy (TEM).
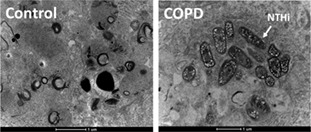
Figure 1 TEM of bAEC from control donors revealed no detectable NTHi, and considerable autophagic activity (evidenced by dark electron dense regions) within vesicular structures. Conversely, NTHi was readily evident in AEC derived from COPD donors and in close proximity to similar vesicular structures.
Results
AEC exposed to 10% CSE exhibit a block in autophagic flux and down‐regulation of the xenophagy‐microbial adapter protein NDP52. Immunofluorescence analysis resolved intracellular NTHi within AEC exposed to 10% CSE in proximity to the autophagic apparatus marker LC3. Importantly, control ALI cultures exposed to NTHi for 24h contained no detectable infection and evidence of normal autophagic activity, whereas COPD‐derived bAEC contained multiple infective particles (Fig.1), some which remained intact within autophagosome‐like vesicles. Further, TEM analysis demonstrated the expulsion of autophagosome‐like vesicles.
Conclusion
NTHi is able to avoid xenophagic degradation in AEC exposed to 10% CSE or in cultures of COPD‐derived AEC, and may usurp the defective autophagic apparatus as a mode of persistence and extracellular propagation. Hence, modes of therapeutic intervention which restore normal xenophagic activity in AECs will significant utility to improve the clearance of intracellular NTHi infection, and thereby decrease the influence of this damaging pathogen in the airways afflicted by COPD.
Grant Support: Thoracic Society of Australia and New Zealand/AstraZeneca
TO 046
INTRANASAL DELIVERY OF THE TLR7 AGONIST, IMIQUIMOD, PROTECTS AGAINST INFLUENZA A VIRUS‐INDUCED MORBIDITY IN MICE
To E1,2, Erlich J1, Luong R1,2, Liong F1, Hendricks K2, Bozinovski S1, O'Leary J3, Brooks D4, Vlahos R1, Selemidis S1,2
1School of Health and Biomedical Sciences, RMIT University Bundoora, Victoria, Australia, 2Department of Pharmacology, Monash University, Clayton, Victoria, Australia, 3School of Medicine, Trinity Translational Medicine Institute, Trinity College Dublin, Ireland, and 4School of Pharmacy and Medical Sciences, Sansom Institute for Health Research, University of South Australia, Adelaide, 5001, Australia
Introduction/Aim
Influenza is a significant global burden with 5 million cases per year, 10% of which are fatal and thus, there is an urgent need for new therapeutics. Toll like receptor 7 (TLR7) is a pattern recognition receptor, which drives a powerful anti‐viral signalling pathway that helps clear virus infections. The aim of the present study was to determine the effect of the TLR7 agonist imiquimod on morbidity, lung inflammation, oxidative stress and antibody production caused by influenza A virus (IAV) infection in mice.
Methods
Saline or imiquimod (50μg/mouse) was delivered intranasally to anaesthetised male C57BL/6J mice one day (d‐1) prior to infection with a low (103PFU/mouse) or high dose (105PFU/mouse) of the mouse adapted Hong Kong X31 virus strain and everyday thereafter until mice were culled day 3 (d3) or 7 (d7) post‐infection for analysis. Bronchoalveolar lavage (BAL) was performed to assess airways inflammation, and inflammatory cell oxidative burst (by L‐012 enhanced chemiluminescence). In addition, BAL fluid and serum was used to determine antibody titres. The lungs were then harvested and used to assess inflammation (H&E staining) and pro‐inflammatory cytokine gene expression by qPCR. Bodyweights were recorded daily during the experimental process.
Results
Imiquimod significantly suppressed body weight loss caused by IAV infection with a maximum reduction of ~60% starting from day 4 (d4) (103 PFU/mouse, n=7‐13, p<0.001). At d3 post infection, imiquimod treatment caused a significant reduction (~50‐60%) in airway and peri‐bronchial inflammation and BALF neutrophil populations (105 PFU/mouse, n=8‐15, p<0.01) but had no effect on macrophage and lymphocyte populations, and the oxidative burst. TNF‐α and IL‐6 mRNA expression was supressed by ~60% (p<0.01 and p<0.05, respectively), whilst IFN‐β and IL‐1β mRNA expression were unaffected. Day 7 data showed a modest but significant increase in IgE, IgM, IgG1, and IgG2a (p<0.05) in BALF following imiquimod treatment compared to control. There were no changes in antibody titres within the serum.
Conclusion
Our findings highlight a potential of imiquimod as a therapeutic option for the treatment of influenza disease.
Grant Support: NHMRC Australia (Project Grant ID 1122506, 1128276). ARC (FT120100876)
TO 047
AIRWAY EPITHELIAL INNATE IMMUNE RESPONSES TO CORONAVIRUSES
Loo S1, Nichol K1, Hsu A1, Londrigan S2, Reading P2,3, Bartlett N1, Wark P1,4
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and The University of Newcastle, Newcastle, Australia, 2Department of Microbiology and Immunology, The University of Melbourne, Parkville, Australia, 3WHO Collaborating Centre for Reference and Research on Influenza, Victorian Infectious Diseases Reference Laboratory, North Melbourne, Australia, and 4Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, Australia
Introduction/Aim
Despite the recurring emergence of novel pathogenic coronaviruses (CoVs) SARS‐CoV (2002) and MERS‐CoV (2012), there is a lack of understanding of host immunity during respiratory infection with CoVs. In this study, we characterised the innate immune responses of differentiated primary bronchial epithelial cells (pBECs) to infection with related less‐virulent OC43‐CoV and 229E‐CoV.
Methods
Human pBECs were grown at the air liquid interface (ALI) until differentiation was observed (25‐30 days), and infected at a multiplicity of infection (MOI) 0.1 with OC43‐CoV or 229E‐CoV for 0, 24, 96 hours and 7 days. Supernatants and RNA were collected to measure pro‐inflammatory‐ and anti‐viral‐cytokines and viral replication. Using microarray, the gene expression profile of OC43‐CoV and 229E‐CoV infection was analysed (n=1). A549 cells transduced to overexpress Interferon‐induced transmembrane proteins (IFITM) 1, 2 and 3 were infected with OC43‐CoV or 229E‐CoV. Viral replication was measured at 0, 8, 24 and 48 hours post‐infection.
Results
OC43‐CoV and 229E‐CoV demonstrated different viral replication kinetics. 229E‐CoV replicated earlier and more efficiently, peaking at 24 hours. This was associated with a delayed but robust activation of the innate host response, with induction of type I and III interferons (IFN‐β, IFN‐λ1/3), IFN stimulated genes and IP‐10. In contrast, replication of OC43‐CoV peaked between 96 and 168 hours, with attenuated levels of IFN‐β, IFN‐λ1/3 and IP‐10. Microarray data also identified IFITM protein upregulation during 229E‐CoV infection. In A549 cells over‐expressing IFITM 1, 2 or 3, 229E‐CoV replication was suppressed by IFITM 1 and 3, while the IFITM2 clone displayed similar replication kinetics to the control. OC43‐CoV replication was unhindered by over‐expression of all IFITM proteins.
Conclusion
This study demonstrated that both OC43 and 229E‐CoVs replicated in differentiated pBECs, but they induce a divergent innate immune response potentially linked to their different replication kinetics. Understanding the host‐virus interaction for these less virulent coronaviruses will give insight into pathogenic mechanisms underpinning SARS‐CoV and MERS‐CoV‐induced respiratory disease.
Grant Support: University of Newcastle Research Scholarship UNRSC
TO 048
VIRAL INFECTION IS EXACERBATED IN A CHRONIC MODEL OF INFLAMMATORY LUNG DISEASE
Thomas B1,2,3, Kan‐o K4, Li H1, Simpson I2, Elias J5, Bardin P1,2,3
1Hudson Institute Of Medical Research, Clayton, Victoria, Australia, 2Monash Medical Centre, Clayton, Victoria, Australia, 3Monash University, Clayton, Victoria, Australia, 4Kyushu University, Fukuoka, Japan, and 5Brown University, RI, USA
Introduction/Aim
Infective exacerbations of chronic inflammatory lung diseases, such as asthma and chronic obstructive pulmonary disease (COPD), are associated with incremental scarring and fibrosis and gradual decrements in lung function. Central to this pathology is the pleiotropic cytokine transforming growth factor‐beta (TGFB) that regulates cell proliferation, tissue remodelling and lung fibrosis. Our previous studies have demonstrated that TGFB suppresses the immune response, resulting in enhanced viral infection.
Methods
We have utilised a transgenic mouse model of lung‐specific TGFB over‐expression and established an acute and chronic model of inflammatory lung disease. We infected the mice with influenza A virus (IAV; strain HKx31) and examined disease severity, inflammatory and immune responses, and viral loads.
Results
In the acute model, TGFB was over‐expressed for 2 days prior to IAV infection. These mice experienced more severe bronchitis and pneumonia, increased inflammatory cell infiltrates and enhanced cytokine and chemokine production in bronchoalveolar lavage (BAL) fluid compared to mice with normal TGFB levels. These mice also demonstrated a suppressed innate immune response that was associated with enhanced viral titres.
In the chronic model, TGFB was over‐expressed for 8 weeks, which resulted in thickening of the respiratory bronchiole epithelium and surrounding smooth muscle, and an emphysematous appearance within the airspaces, resembling phenotypic changes characteristic of asthma and COPD. Preliminary results in this model demonstrate that IAV infection is more severe compared to mice with normal TGFB levels.
Conclusion
Our transgenic mouse model provides us with a unique tool to evaluate the direct effects of TGFB on viral infection, or in the context of chronic inflammatory lung disease, and to investigate potential therapeutic strategies to combat viral‐induced disease exacerbation.
Grant Support: NHMRC
Declaration of Interest: none.
TO 049
DIFFERENTIATION BETWEEN APOPTOTIC AND NECROTIC CELL DEATH IN AIRWAY EPITHELIAL CELLS IN RESPONSE TO VIRAL INFECTION AND ANAEROBIC CONDITIONS USING FLOW CYTOMETRY
Montgomery S1, Stick S1,2,3,4, Kicic A1,2,3,4,5
1School of Paediatrics and Child Health, University of Western Australia, Crawley, Australia, 2Telethon Kids Insitute, Subiaco, Australia, 3Department of Respiratory Medicine, Princess Margaret Hospital for Children, Subiaco, Australia, 4Centre for Cell Therapy and Regenerative Medicine, School of Medicine and Pharmacology, The University of Western Australia, Crawley, Australia, and 5School of Public Health, Curtin University, Bentley, Australia
Introduction/Aim
Necrosis of airway epithelial cells (AEC) resulting in airway inflammation is a characteristic finding in cystic fibrosis (CF), driven by mucus obstruction of the airway and previously suggested as a potential response to respiratory viral infection. Current methodologies to measure apoptotic and necrotic cell death using flow cytometry in AEC are not adequate to completely differentiate between the two. The aim here was to determine whether a novel flow cytometry methodology described in other cell types could be optimized and adapted to AEC to sufficiently differentiate apoptotic and necrotic AEC.
Methods
Non‐CF and CF AECs were permeabilised, infected with human rhinovirus for 24 hours (MOI 1 & 3), or incubated in a limited O2 environment (0% O2 for 15 hours). Cells were then collected and stained with Annexin‐V (A5) and TO‐PRO‐3 (TP3) before analysis via flow cytometry. Data was analysed using a seven‐step gating process to differentiate six different populations from AEC.
Results
Flow cytometry using A5 and TP3 was able to differentiate viable, apoptotic, and necrotic cells, plus apoptotic bodies and cellular debris in stimulated and unstimulated epithelial samples.
| Viable | A5+ Apoptotic | A5‐ Apoptotic | Necrotic | Apoptotic Bodies | Debris | ||
|---|---|---|---|---|---|---|---|
| non‐CF | Control | 82.43% | 1.88% | 0.50% | 9.82% | 3.92% | 1.44% |
| Permeabilised | 3.01% | 75.21% | 0.23% | 18.64% | 3.16% | 0.26% | |
| Virus | 76.91% | 1.97% | 0.49% | 11.01% | 5.23% | 3.51% | |
| CF | Control | 59.46% | 8.83% | 1.28% | 17.92% | 6.81% | 2.56% |
| Permeabilised | 0.98% | 60.43% | 2.09% | 26.94% | 7.51% | 0.89% | |
| Virus | 58.10% | 9.63% | 1.88% | 15.51% | 8.31% | 2.75% |
Conclusion
Flow cytometry utilising A5 and TP3 in conjunction with a seven‐step gating process is sufficient to differentiate six populations from both stimulated and unstimulated AEC of healthy and diseased individuals. Further studies utilising this technique will allow quantification of AEC necrosis in patients with and without CF, with the aim to investigate differences in mechanisms driving cell death and airway inflammation.
Grant Support: Australian Cystic Fibrosis Research Trust Postgraduate Studentship
Chronic Obstructive Pulmonary Disease (COPD) 1
TO 050
SMALL AIRWAY FIBROSIS ASSOCIATED WITH DECREASED LUNG FUNCTION IN COPD
Eapen M1, Walters H2, Hackett T3, Sohal S1
1School of Health Sciences, Launceston, Launceston, Australia, 2NHMRC Centre for Research Excellence for Chronic Respiratory Disease, School of Medicine, University of Tasmania, Hobart, Australia, and 3Department of Anesthesiology, Pharmacology & Therapeutics, University of British Columbia, Vancouver, British Columbia, Canada; and UBC Centre for Heart Lung Innovation, St. Paul's Hospital, Vancouver, Canada
Aim
The primary source of airflow limitation in COPD is small airway (SA) fibrosis and obliteration. We previously showed that epithelial mesenchymal transition (EMT) is an active process in small airways contributing to fibrotic pathogenesis. Myofibroblast is highly active fibrotic cells that excessively secrete extracellular matrix (ECM). Here we explore the consequence of SA myofibroblast proliferation and relate them to physiological outcomes and airway remodeling in smokers and COPD patients.
Methods
SA lung resections, from non‐smoker controls (NC), normal lung function smokers (NLFS), COPD current (CS) and ex‐smokers (ES) were stained with anti‐human αSMA, collagen‐1, and fibronectin. αSMA+ cells were enumerated in Reticular basement membrane (Rbm), Lamina Propria (LP), and adventitia and represented as per mm of Rbm and mm2 of the respective area surveyed. Collagen‐1 and fibronectin are represented as a percentage change. All measurements including the sub‐epithelial LP and adventitia thickness were measured using Image‐proplus 7.0.
Results
We observed a general increase in sub‐epithelial LP and adventitia thickness in all pathological groups compared to NC. Similar increases in αSMA+ myofibroblasts was observed in sub‐epithelial Rbm, LP, and adventitia in the pathological groups compared to NCs, though the changes were prominently higher in the LP. Further, the increase in myofibroblast population in the LP was strongly associated with a decrease in lung function, and an increase in ECM proteins collagen‐1 and fibronectin deposition in the LP. Finally, we observed EMT markers expressed in epithelial basal cells and Rbm, correlated to the increased SA myofibroblasts and airway thickness.
Conclusion
This is the first report that systematically characterizes the myofibroblasts in COPD based on their localization and statistically correlates them to lung function. The increase in myofibroblast population also directly related to pathological changes in ECM proteins. Driving these changes is likely to be EMT activity in the basal epithelial cells.
Grant Support: Clifford Craig Foundation, Launceston
Conflict of Interest: Nil.
TO 051
SKELETAL MUSCLE REGENERATION AND FUNCTION IS IMPAIRED IN EXPERIMENTAL COPD
Cerni C1, Passey S1, Seow H1, Bernardo I1, van der Poel C2, Dobric A1, Brassington K1, Selemidis S1, Bozinovski S1, Vlahos R1
1RMIT University, Melbourne, Australia, and 2La Trobe University, Bundoora, Australia
Introduction/Aim
Skeletal muscle wasting is a major comorbidity of COPD and a powerful predictor of mortality. Current therapeutic strategies aim to increase muscle mass by augmenting protein synthesis and reducing protein degradation. Muscle mass can also be increased through the activation of satellite cells, which play a pivotal role in skeletal muscle regeneration. However, the role of satellite cells in COPD is not fully understood. Thus, we explored whether muscle regeneration in response to injuring the Tibialis Anterior (TA) muscle is impaired in mice exposed to cigarette smoke (CS).
Methods
Male BALB/c mice were exposed to room air (sham) or CS generated from 9 cigarettes/day, 5 days/week for 8 weeks. After 8 weeks of CS exposure, the right TA muscle was injured by injection of 40μl barium chloride (BaCl2). The mice were then exposed to CS for another 7, 14 and 21 days at which time the contractile properties of the right TA muscle were measured. Mice were then culled and both the uninjured left TA and injured right TA muscles dissected out, weighed and used to examine the expression of genes associated with muscle regeneration (e.g. Pax 7) and for histological assessment of muscle injury.
Results
BaCl2‐induced injury significantly decreased the weight of the TA muscle at 7 days post injury and this was further exacerbated in CS‐exposed mice (n=10, p<0.05). BaCl2 also caused significant muscle injury as demonstrated by centrally located nuclei and altered tissue architecture when assessed 7 days post injury. However, muscle injury was even greater in CS‐exposed mice when compared to injured sham mice (n=8, p<0.05). Injured TA muscle from CS‐exposed mice had at least a two‐fold increase in Pax 7 mRNA expression compared to injured TA muscle from sham‐exposed mice at 7 days post injury (n=8, p<0.001). Moreover, TA muscle contractile function was significantly impaired in the injured CS‐exposed mice compared to the injured sham‐exposed mice (n=7, p<0.05).
Conclusion
Skeletal muscle regeneration and function is impaired in experimental COPD.
Grant Support: NHMRC Australia (Project Grant ID 1084627)
TO 052
TRANSFORMING GROWTH FACTOR ALPHA PRODUCES AIRWAY REMODELLING AND REDUCES AIRWAY DISTENSIBILITY
Wang K1,2, Le Cras T3, Larcombe A2,4, Zosky G2,5, Berry L2, Elliot J6, James A6, Noble P1,2
1School of Human Sciences, University of Western Australia, Crawley, Western Australia, Australia, 2Clinical Sciences, Telethon Kids Institute, Subiaco, Western Australia, Australia, 3Division of Pulmonary Biology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA 4School of Public Health, Curtin University, Perth, Western Australia, Australia, 5School of Medicine, University of Tasmania, Hobart, Tasmania, Australia, and 6Department of Pulmonary Physiology and Sleep Medicine, West Australian Sleep Disorders Research Institute, Sir Charles Gairdner Hospital and School of Medicine and Pharmacology, University of Western Australia, Nedlands, Western Australia, Australia
Introduction/Aim
Airway distensibility is reduced in patients with COPD. Transforming growth factor alpha (TGF‐α) is increased in the serum of COPD patients and produces airway remodelling in mouse models. We hypothesised that TGF‐α overexpression reduces airway distensibility. Our aim was to determine the effect of TGF‐α and its regulatory gene, early growth response one (Egr‐1), on airway thickness and distensibility.
Methods
Conditional expression of TGF‐α in the airways of transgenic mice (Clara cell secretory protein‐rtTA(+/‐)/[tetO]7‐TGF‐α(+/‐)) was induced by doxycycline (Dox). Mice were Egr‐1 homozygous (+/+) or heterozygous (+/‐). At 4 weeks of age, mice were fed Dox in chow or a control diet for 3 weeks and then anaesthetised, mechanically ventilated and had lung function measured using low frequency force oscillation. Airway conductance (G) was measured at trans‐respiratory pressures of 0 (G0) and 5cmH2O (G5). Distensibility was calculated from the change in conductance (G5‐G0). Lungs were fixed for morphometry and stereology.
Results
Dox‐fed mice had increased thickness of the airway epithelium, inner and outer wall and airway smooth muscle layer. While the increase in thickness of the epithelium and inner wall was greater in Egr‐1+/‐ mice, other changes were not affected by genotype. Dox‐fed mice had reduced airway distensibility independent of genotype.
Conclusion
Increased TGF‐α expression within the airway wall is associated with increased wall thickness and reduced airway distensibility. The effects of TGF‐α were largely unaffected by partial modification of the Egr‐1 gene. Findings suggest that TGF‐α signalling may contribute to airflow limitation in COPD by reducing airway distensibility.
Grant Support: NHMRC (1090888, 1027218, 1045824)
Declaration of Interest Statement: None.
TO 053
LIPOSOMAL FORMULATION OF QUERCETIN AND RESOLVIND1 FOR TREATMENT OF STEROID RESISTANT AIRWAY INFLAMMATION
Komalla V1,2, McAlinden K1,2, Ramaccini D1,3, Scalia S3, Sharma P2,4, Oliver B2,4, Haghi M1
1Graduate School of Health, University of technology Sydney, Sydney, New South Wales, Australia, 2Woolcock Institute of Medical Research, Glebe point Road, Australia, 3University of Ferrara, Italy, and 4School of Life Sciences, University of Technology Sydney, Ultimo, Australia
Introduction/Aim
Steroids are the mainstay treatment targeting airway inflammation. However, in some patients increased oxidative stress could result in resistance to steroid treatment. Therefore, combining anti‐inflammatory, resolvin D1 (RvD1), and antioxidant quercetin (Q) could be a promising therapeutic strategy. Here, we aim to prepare liposomal formulation of Q and RvD1 and investigate its effectiveness in human airway epithelial cells (BEAS‐2B).
Methods
Blank, Q and QRvD1 liposomes were prepared and characterised. Cell uptake studies were performed using confocal microscope and antioxidant activity of the liposomes was determined.
Results
The results demonstrated a monomodal size distribution of 163.26 ± 1.69 nm, 158.16 ± 1.89 nm, 167.3 ± 0.8 nm for blank, Q and QRvD1 liposomes respectively.The concentration of Q encapsulated was found to be 4.99 ± 2.6 μg/ml and 2.5 ± 1.97 μg/ml in Q and QRvD1 liposomes respectively and concentration of RvD1 in QRvD1 liposomes was found to be 9.57 ± 0.01 pg/ml. There was a time‐dependent uptake of liposomes (Q and QRvD1) observed over 6 hours following treatment with liposomes. The antioxidant activity of Q was found to be significantly higher (P<0.05) when formulated as liposomes (48.177 ± 6.99% for Q and 48.33 ± 5.626% for QRvD1) compared to free Q (30.79 ± 2.51%).
Figure 1. Uptake of Q liposomes into the Beas‐2B cells 6 hours following treatment
Conclusion
In conclusion, liposomal formulations demonstrate acceptable characteristics for inhalation with significantly increased antioxidant properties when compared with the free Q. These liposomal formulations could potentially improve the therapeutic outcomes in steroid resistant patients. Further studies will investigate the anti‐inflammatory activity of these liposomes in in vitro and in vivo.
TO 054
CHARACTERISTICS OF PATIENTS WITH AND WITHOUT PERIPHERAL EOSINOPHILIA IN PATIENTS PRESENTING WITH AN ACUTE COPD EXACERBATION; GOLD COAST UNIVERSITY HOSPITAL EXPERIENCE
Semasinghe Bandaralage S1,2, Teng R2, Sriram K1,2, Sivakumaran P1,2
1Gold Coast Hospital and Health Services, Southport, Queensland, Australia, and 2School of Medicine, Griffith University, Southport, Queensland, Australia
Introduction/Aim
COPD patients with peripheral eosinophilia may have increased frequency of COPD exacerbations, respond better to oral corticosteroids and reduced mortality. Peripheral eosinophilia in COPD patients (eosinophil count of ≥ 2% of white blood cell count) has a prevalence in the range of 37‐45%. To our knowledge, there is little epidemiological data of Australian COPD patients concerning peripheral eosinophilia, its prevalence and its association with rehospitalisation rates, steroid responsive disease and mortality rates. With this literature gap in mind, records of patients presenting with COPD exacerbations were audited retrospectively to determine the prevalence of peripheral eosinophilia in an Australian population.
Methods
Consecutive patients with spirometry confirmed COPD admitted to our institution with a COPD exacerbation during the period of July 2016 – December 2016 were considered for the study. These patients' records were subsequently followed up until June 2017. The variables recorded were white blood cell count, absolute and relative eosinophil count, readmission rate, decompensated type 2 respiratory failure rate, non‐invasive ventilation initiation rate, intensive care admission rate and mortality rate.
Results
240 patients were included for analysis and of these 37% had peripheral eosinophilia. Using Pearson's coefficient, there appeared to be a statistically significant correlation between increasing peripheral eosinophil count and increased number of readmissions (R=0.175, p=0.007) but not with decompensated type 2 respiratory failure, non‐invasive ventilation initiation rate, intensive care admission rate or mortality rate. Two‐sample t‐Test for equal means when comparing those with peripheral eosinophilia ≥ 2% and those without was also in keeping with a statistically significant difference in readmission rates (t=‐2.367, p=0.019).
Conclusion
Prevalence of peripheral eosinophilia in Gold Coast patients was similar to overseas cohorts. In congruence with findings in previous overseas studies, Gold Coast patients with eosinophilia were prone to readmission but not increased type 2 respiratory failure, non‐invasive ventilation, intensive care admission or mortality. As such peripheral eosinophilia can be used in Australian COPD patient cohorts to predict rehospitalisation rate. Future studies should look to prospectively evaluate the effect inhaled corticosteroids have on readmission rates in patients with peripheral eosinophilia.
Grant Support: None
TO 055
TARGETING APOPTOSIS SIGNAL‐REGULATING KINASE 1 IN CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Sharma P1,2, Deshpande D3, Oliver B1,2
1Medical Sciences Discipline, University of Technology Sydney, Sydney, Australia, 2Emphysema Centre, Woolcock Institute of Medical Research, Glebe, Australia, and 3Thomas Jefferson University, Philadelphia, PA, USA
Introduction
Increased airway smooth muscle (ASM) mass is part of overall structural changes observed in COPD, and is correlated with severity of the disease and has been found to negatively impact lung function. Thus, there is clear unmet clinical need for finding new therapies for COPD which can target airway remodeling and disease progression. Apoptosis signal‐regulating kinase 1 (ASK1) is a ubiquitously expressed MAP3K activated by various stress stimuli, including ROS, TNF‐α, and LPS. However, the role of ASK1 in airway remodeling is not established. In this study, we aimed to determine the effects of ASK1 inhibition on ASM growth and pro‐mitogenic signaling using ASM cells from well‐established COPD patients.
Methods and Results
It is known that ASM cells from COPD patients have greater proliferative capacity to variety of mitogens in vitro. We used human lung tissue samples and primary human ASM cells obtained from COPD patients and healthy controls. IHC revealed increased expression of ASK1 in COPD lung when compared with non‐COPD lung. Pre‐treatment of human ASM cells with highly selective (IC50:14 nM) and orally available ASK1 inhibitor; TCASK10 resulted in a dose‐dependent reduction in mitogen (FBS, 10%; PDGF and EGF; 10 ng/ml, 72 hours)‐induced ASM growth as measured by CyQuant assay. Furthermore, ASK1 siRNA prevented mitogen‐induced human ASM cell growth, while immunoblotting revealed that the anti‐mitogenic effect of ASK1 inhibition or silencing is mediated by JNK and p38MAP kinase‐signalling pathways evident by reduced phosphorylation of downstream effectors JNK1/2 and p38MAP kinase respectively with no effect on ERK1/2 signalling.
Conclusions
Collectively, these findings establish the anti‐mitogenic effect of ASK1 inhibition and identify a novel pathway that can be targeted to reduce or prevent excessive ASM mass in COPD.
Key Words
COPD, airway remodelling, mitogen
Grant Support: UTS Chancellors Fellowship and NHMRC
OLIV 1
TO 056
NOVEL ANTI‐FXII ANTIBODY INHIBITS FXII‐INDUCED PRO‐FIBROTIC FUNCTIONS IN LUNG FIBROBLASTS
Wong M1, Jaffar J2, McMillan L1, Westall G2, Wilson N1, Panousis C1
1Translational Research, CSL Ltd, Bio21 Institute, Melbourne, Victoria, Australia, and 2Alfred Hospital, Melbourne, Victoria, Australia
Introduction/Aim
Excessive pro‐coagulant activity drives recurrent inflammation and fibrosis in patients with Idiopathic Pulmonary Fibrosis (IPF). Coagulation factors promote healing during damage, but can also exert pro‐fibrotic cellular effects. Coagulation factor XII (FXII) has been identified as a potential mediator of lung fibrosis. The aim of this study is to further define a role for FXII in fibrogenesis.
Methods
Blood from 35 IPF patients was collected repeatedly (0‐15 months) and compared to age and gender‐matched healthy controls. Plasma FXII and IL‐6 were measured. Immunohistochemical analysis for FXII was performed on paraffin‐embedded lung tissue from IPF patients and non‐diseased controls (NDC). In vitro effects of FXII on primary IPF and NDC fibroblasts were evaluated for cytokine production, proliferation and migration. The effect of a novel, fully human monoclonal antibody against FXII (CSL312) was evaluated.
Results
Baseline and longitudinal levels of FXII in IPF patients with progressive disease was elevated compared to those with stable disease (27.7 vs 17.6μg/ml, p=0.04 baseline; 26.3 vs 20.6μg/ml, p=0.014 longitudinal) but were not increased in IPF compared to healthy controls. Baseline plasma IL‐6 was elevated in IPF patients when compared to healthy controls (3.9vs 1.5 pg/ml, p=0.001). IHC analysis revealed significant FXII staining in IPF lung tissue with minimal staining observed in non‐fibrotic lung tissue. Activated FXII induced IL‐6 production and enhanced proliferation/migration in primary lung fibroblasts. Migration and IL6 production were effectively inhibited by CSL312.
Conclusion
FXII is elevated in the lungs of progressing IPF patients and can drive pro‐fibrotic and pro‐inflammatory functions of fibroblasts. An anti‐FXII antibody (CSL312) can inhibit these activities. The ability of FXII to drive IL‐6 production in lung fibroblasts may contribute to elevated IL‐6 levels seen in IPF patients' blood. Blocking FXII activity may be novel avenue to treat IPF and other inflammation‐driven interstitial lung diseases.
Grant Support: Nil
Conflict of Interest: Employee of CSL Ltd.
TO 057
A SINGLE CENTRE, PROSPECTIVE, LONGITUDINAL STUDY OF THE HUMAN RESPIRATORY VIROME AFTER LUNG TRANSPLANTATION
Mitchell A2, Mourad B2, Morgan L4, Oliver B3, Glanville A1
1Lung Transplant Unit, St Vincent's Hospital, Sydney, Australia, 2University of Technology Sydney, Sydney, Australia, 3The Woolcock Institute of Medical Research, Glebe, Australia, and 4Concord Clinical School, University of Sydney, Concord, Australia
Introduction/Aim
Lung transplantation (LTX) provides a unique opportunity to investigate the dynamics of viruses present within the human pulmonary virome which is transplanted into the recipient within the donor lungs. The aim of our study was to elucidate interactions between viral species within the respiratory virome of the LTX recipient and describe their impact on allograft function.
Methods
A prospective, longitudinal study of viral dynamics after LTX. Multiple sample types were collected. Samples were processed and assayed using multiple uniplex PCRs for human rhinovirus (HRV), respiratory syncytial virus (RSV), influenza A and B, (Flu A, B), parainfluenza (PIV) 1,2,3 and human metapneumovirus. Clinical outcomes were analysed and compared with microbial detection.
Results
52 consecutive LTX were recruited. Swabs of explanted lungs were positive for viruses in 18/52 despite recipient vaccination and negative recipient NPS. Day 1 BAL showed Flu A (n=28), HRV (n=9) and PIV (n=1). Donor swabs showed influenza (A=1, B=1), and HRV (n=3). Donor transmission of Flu A was observed. 47/52 recipients had BAL positive samples for viruses (38/47 on multiple BAL) and viruses persisted for up to 14 weeks.
114 paired transbronchial biopsies and viral PCR on BAL were performed. 21 patients showed evidence of acute cellular rejection on biopsy (Grade A2B0=3, Grade A1B1=6, Grade A1B0=12). Of these, 11/21 had viruses detected in the BAL collected concurrently. Conversely, in patients who showed no evidence of cellular rejection on biopsy, 51 were virus positive, while 42 were virus negative. Analysis using Fisher's exact test (2 tailed) indicated no significant correlation (p=1.00) between viral detection and the presence of acute cellular rejection.
Conclusion
The finding of frequent donor transmission and early acquisition of viruses (particularly influenza A) support the importance of respiratory virome surveillance after LTX to direct acute therapies. In this cohort, viral presence after LTX was not correlated with acute rejection events.
Grant Support: N/A
TO 058
EXOSOMES AND PAH: THE ROLE OF CELLULAR COMMUNICATION IN BOTH DISEASE PROGRESSION AND THERAPEUTIC SUCCESS
Harper R1, Maiolo S1, Lim R2, Greening D3, Cockshell M4, Bonder C4, Reynolds P1
1Royal Adelaide Hospital & University of Adelaide, Adelaide, South Australia, Australia, 2Hudson Institute, Monash University, Clayton, Victoria, Australia, 3La Tribe University, Melbourne, Victoria, Australia, and 4Centre for Cancer Biology, University of South Australia, Adelaide, South Australia, Australia
Introduction/Aim
Previously we reported the therapeutic effect of BMPR2 augmented endothelial progenitor cell therapy in a rat PH model. We know there is little direct cell integration into the pulmonary endothelium following intravenous injection, thus we attribute the positive physiological effects of our cell therapy to cell‐to‐cell communication via secreted factors such as exosomes (exos). In this study we look at comparing PAH‐EPC and control‐EPC protein profiles via mass spectrometry, and we assess their capacity to interact with and transport BMPR2 into endothelial cells (EC).
Methods
EPCs are isolated and cultured from 15mL of PAH or control peripheral blood. Cells were either transduced with AdBMPR2 or AdTrackLuc, or untransduced for subsequent exo isolations. Exosomes are isolated via differential centrifugation, and characterised with a NanoSight, TEM and SEM. Exosome protein profile was via mass spectrometry. Exo‐Quick™ treated exos and GFP‐exos labelled were used to view exo localisation within the target ECs both live and fixed via confocal microscopy. BMPR2‐Exos were incubated on ECs for 48hrs before being washed off, and the cells lysed for western blot analysis.
Results
Exosomes were positively identified as 40‐200nm via NanoSight, TEM and SEM. Protein profiling of exos showed differential protein expression in the PAH vs control for 326 proteins, including a relative down‐regulation of BMPR2 in PAH exos. Exosome interaction with ECs demonstrated localisation around the nucleus of the cell, both in live and fixed EC samples. Additionally, BMPR2 expression was significantly increased in cells treated with BMPR2‐Exos.
Conclusion
Differential protein expression between exos derived from PAH compared to control EPCs was shown. Additionally, we have characterised exos interaction with ECs and shown that they are involved in BMPR2 transfer from BMPR2 transduced EPCs to naïve ECs. These results indicate the potential role of exos in our BMPR2‐cell therapy.
Grant Support: RAH Research Fund
TO 059
DORNASE ALFA DURING LOWER RESPIRATORY TRACT INFECTION POST LUNG TRANSPLANTATION
Tarrant B1,2, Snell G3,4, Ivulich S4,5, Button B1,4,6, Thompson B4,7, Holland A1,2
1Physiotherapy, Alfred Health, Melbourne, Australia, 2La Trobe University, Bundoora, Australia, 3Lung Transplant, Alfred Health, Melbourne, Australia, 4Monash University, Clayton, Australia, 5Pharmacy. Alfred Health, Melbourne, Australia, 6Cystic Fibrosis Service, Alfred Health, Melbourne, Australia, and 7Lung Function Laboratory, Alfred Health, Melbourne, Australia
Introduction/Aim
Lung transplant (LTx) recipients are at a high risk of lower respiratory tract infection (LRTI) secondary to immunosuppression, while altered respiratory physiology can make it difficult to clear secretions. Inhaled mucoactive agents alter mucus properties and/or facilitate mucocilliary clearance in suppurative lung disease. However there are no randomised controlled trials (RCTs) studying these effects post LTx. We aimed to evaluate the safety and efficacy of nebulised dornase alfa compared to isotonic saline during LRTI > 2 months post LTx.
Methods
Inpatient adults with LRTI and sputum production following bilateral sequential LTx were eligible for this assessor blinded RCT. Randomisation was stratified by LTx indication (±cystic fibrosis (CF)). Participants received either 5ml isotonic saline, or 2.5ml dornase alfa, nebulised once daily for 1 month followed by 2 months symptom diary only. The primary outcome was change in lung clearance index (LCI) measured by multi‐breath washout. Secondary outcomes included adverse events; spirometry; quality of life; readmission; length of stay and self‐reported exacerbations at baseline, 1 month and 3 months.
Results
32 participated, 16 each group (18M,14F), mean(SD) age 50±14, FEV1% 58±22, median(IQR) length of stay 7±5, days since LTx 1275±2482. LTx indications included CF (n=11) and chronic obstructive pulmonary disease (n=11). There were no significant between‐group differences in LCI at any time point (one month mean difference ‐0.34, 95% confidence interval (CI) ‐1.57 to 0.89; three months mean difference ‐0.76, 95% CI ‐2.29 to 0.78, both favouring dornase alfa). Secondary outcomes were not different between groups.
Conclusion
These results do not support the routine use of dornase alfa during LRTI in LTx recipients.
Grants: Alfred Research Trusts Small Project Grant; Professor Carey and Laura Denholm
Conflict of Interest: No conflict of interests to declare.
TO 060
VARIATION IN SENSITIVITY TO PIRFENIDONE AMONG FIBROBLASTS DERIVED FROM PATIENTS WITH AND WITHOUT IDIOPATHIC PULMONARY FIBROSIS
Jaffar J1,2, Organ L1,2, Symons K2, Glaspole I2, Westall G1,2
1Department of Immunology and Pathology, Monash University; Australia, Melbourne, Australia, and 2Department of Lung Transplant Service, The Alfred, Australia, Australia
Introduction/Aim
Lung fibrosis is the end‐stage consequence of interstitial lung diseases (ILDs) which involve excessive numbers of activated lung fibroblasts with elevated alpha‐smooth muscle actin (αSMA) expression. Pirfenidone is approved for use in patients with idiopathic pulmonary fibrosis (IPF), the most common and fatal of the idiopathic ILDs. Poor tolerability and large variation in efficacy of pirfenidone is a significant barrier to best patient outcomes. This study aims to investigate whether an in‐vitro fibroblast test can identify patients most likely to benefit from pirfenidone therapy.
Methods
Primary lung fibroblasts were derived from the apex and base of the lungs from patients with IPF (N=10), patients with other end‐stage non‐IPF ILDs (N=10) and normal donors whose lungs were deemed unsuitable for transplantation (NDC)(N=10). Determined by in‐cell western, αSMA and GAPDH levels in fibroblasts were measured before and after treatment with pirfenidone (0‐1mM) and in the presence/absence of transforming growth factor‐β (TGFβ) (0‐10ng/mL). Sensitivity to pirfenidone was defined by a decrease in αSMA/GAPDH level from baseline by ≥10%.
Results
Treatment with pirfenidone decreased αSMA levels in N=9 fibroblast lines at 72 hours (Figure 1). Fibroblast αSMA levels correlated with the extent of αSMA decline in response to pirfenidone (Spearmans' R = ‐0.76, p=0.037). In patients with IPF, basal αSMA level of the fibroblast line correlated with forced vital capacity (FVC, % predicted) of the patient from whom the line was derived (Spearmans' R = 1, p=0.016).
Conclusion
The response of lung fibroblasts to pirfenidone may identify patients with IPF who would benefit from said treatment. Our data suggest that patients who have high numbers of αSMA+ fibroblasts would in particular benefit from pirfenidone therapy, although further screening is required. Variation in αSMA level of fibroblasts may be reflective of the overall lung fibrotic burden as it correlated with FVC.
Grant Support: None
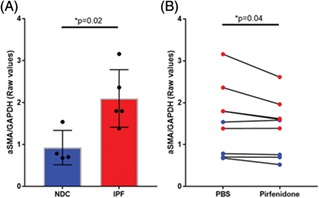
Figure 1 Quantification of aSMA levels in primary lung fibroblasts pre and post Pirfenidone therapy by in‐cell‐western. Primary fibroblasts were derived from N=5 patients with idiopathic pulmonary fibrosis (IPF, red dots) and N=4 donors without lung disease (NDC, blue dots). (A) Fibroblasts derived from patients with IPF express greater levels of aSMA compared to fibroblasts from NDC donors. (B) Treatment with 1mM Pirfenidone (in PBS) decreased aSMA expression in lung fibroblasts. Each dot is an experimental triplicate.
TO 061
CHARACTERISATION OF PULMONARY ARTERIAL HYPERTENSION ENDOTHELIAL PROGENITOR CELLS UNDER HYPOXIA
Maiolo S1,2, Cockshell M3, Bonder C3, Harper R1,2, Reynolds P1,2
1Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, South Australia, Australia, 2University of Adelaide, Adelaide, South Australia, Australia, and 3Centre for Cancer Biology, Adelaide, South Australia, Australia
Introduction/Aim
Pulmonary arterial hypertension (PAH) is a devastating lung condition characterised by pulmonary vascular remodelling and over proliferation of vascular cells. Mutations in BMPR2 are causally linked to PAH. Endothelial progenitor cells (EPCs) are cells that can differentiate into endothelial cells, play a role in vascular repair and are dysfunctional in PAH patients. Hypoxia is thought to play a significant role in disease pathogenesis and is used to induce PAH in animal models of disease. This study aimed to characterise the differences in PAH and control EPCs in hypoxic conditions.
Methods
EPCs were isolated from PAH and control patient's peripheral blood (15mL). Following characterisation and expansion, cells were exposed to either normoxia (5%CO2/ atmosO2) or hypoxia (1%O2/5% CO2/94% N2). Proliferation and apoptosis were assessed using MTT assays and flow cytometry. Protein analysis was conducted via western blots.
Results
EPCs originating from PAH patients proliferated at a similar rate to control EPCs in normoxia (increases of 198%±60% and 206%±17% over 72hrs respectively). However, under hypoxic conditions proliferation of control cells was 88% less than PAH cells (7%±36% and 95%±11% increase over 72hrs respectively). Preliminary data suggests this continued proliferation could be due to apoptosis resistance in PAH lines as assays revealed lower apoptosis levels after hypoxia exposure for 72hrs in PAH lines (2.8%) than in control lines (8.5%). Activated SMAD 1/5/8 was decreased by 68% in hypoxic PAH cells compared to controls.
Conclusion
EPCs isolated from peripheral blood of PAH patients are functionally different under hypoxic conditions to those isolated from control subjects. Most notably, the PAH EPCs appear to possess a higher resistance to apoptosis and hypoxia. These findings suggest EPCs could play a role in the pathogenesis of PAH as they can contribute to the aberrant proliferation, apoptosis and vascular remodelling seen in PAH.
Grant Support: NHMRC, RAH Research Fund.
Ann Woolcock Young Investigators Award
TO 062
RCT OF NHF THERAPY COMPARED WITH NIV IN HYPERCAPNIC COPD
McKinstry S1,2,3, Baarsma J1,4, Singer J1, Weatherall M3,5, Beasley R1,2,3, Fingleton J1,2,3
1Medical Research Institute of NZ, Wellington, New Zealand, 2Victoria University, Wellington, New Zealand, 3Capital and Coast DHB, Wellington, New Zealand, 4University of Groningen, Groningen, The Netherlands, and 5University of Otago School of Medicine, Wellington, New Zealand
Introduction/Aim
Acute hypercapnic respiratory failure secondary to an exacerbation of COPD is associated with poor clinical outcomes and increased mortality. Non‐invasive ventilation (NIV) is part of the standard of care but can be poorly tolerated.
We have shown Nasal High Flow therapy (NHF) produces a small reduction in transcutaneous CO2 tension (PtCO2) in stable COPD.
Our aim was to compare NHF and NIV in hypercapnic COPD.
Methods
Design: Single‐blind randomised controlled two‐way cross‐over trial.
Setting: Single centre institute in New Zealand recruiting participants from hospital databases.
Participants: 24 participants with a doctor's diagnosis of COPD, FEV1:FVC ratio <0.7, ≥40 years, smoking history of ≥10 pack years, PcapCO2 >45.0mmHg, BMI <35kg/m2 , no recent exacerbations and no diagnosis of obstructive sleep apnea or obesity hypoventilation syndrome.
Interventions: NHF at 45Lmin and BiPAP at 15/4cmH2O, each for 60mins with a 15min washout in between.
Primary outcome measure: PtCO2 at 60mins, adjusted for baseline.
Secondary outcomes included tolerability and the proportion of participants with a decrease in PtCO2 ≥4mmHg and ≥8mmHg at 60 minutes.
Results
PtCO2 was 2.5mmHg (95% CI ‐4.5 to ‐0.5) lower with NIV compared to NHF, p=0.016.
The proportion of participants with a reduction of PtCO2 ≥4mmHg with NIV versus NHF was 45.8% versus 25.0%. For a reduction in PtCO2 ≥8mmHg it was 25% versus 8.3%. These differences were not statistically significant. Participants rated NHF significantly better for ease of application, comfort, fit and willingness to use in the future.
Conclusion
In stable COPD patients with chronic hypercapnia, NIV resulted in a small reduction in PtCO2 compared with NHF, which is of uncertain clinical significance. NHF was better tolerated. NHF may be a therapeutic option for some people with hypercapnic respiratory failure and studies in acute exacerbations of COPD are required.
Grant Support: Health Research Council (NZ)
Trial Registration: ACTRN12616001701415
TO 063
MULTIDIMENSIONAL AETIOLOGICAL ASSESSMENT IDENTIFIES CLINICAL PHENOTYPES AMONGST HOSPITALIZED ACUTE EXACERBATIONS OF COPD
MacDonald M1, Osadnik C1, King P1, Bardin P1
1Monash Health, Melbourne, Australia
Introduction/Aim
Hospitalized AECOPD are heterogenous events of diverse aetiology. We hypothesized that comprehensive AECOPD evaluation would reveal clinical phenotypes amongst AECOPD.
Methods
Nasopharyngeal viral PCR, sputum culture, C‐reactive protein, chest X‐ray, troponin I (hs‐TnI), N‐terminal pro brain natriuretic peptide (NT‐proBNP) and Hospital Anxiety and Depression Scale (HADS) were used to construct a cumulative aetiological phenotype for each AECOPD using a simple acronym: A=airway viral infection, B=bacterial infection, C=coinfection, D=depression/anxiety, E=embolism (pulmonary), F=failure (cardiac), G=general environment, X=unknown.
Results
Aetiologies identified among 155 unique AECOPD admissions were diverse (viral=35, bacterial=61, coinfection=8, no infection=44) and often multifactorial, with 1 aetiology in 31%, 2 in 48.4%, 3 in 5.2% and no identifiable aetiology in 5.8%.
Baseline lung function and symptoms were similar across exacerbation subtypes. Infective exacerbations were associated with lower eosinophils (p<0.001) and non‐infective exacerbations with lower pH (p=0.004). NIV requirement was higher in non‐bacterial v bacterial (p=0.03). AECOPD patients with no identifiable aetiology (X) were generally “frequent exacerbators” with severe acute presentations but prompt stabilization. Admissions ≤4 days were most common in non‐infective groups (viral 22.9% v bacterial 39.3% v co‐infection 12.5% v non‐infective 47.7%, p=0.06). Subclinical cardiac dysfunction was highly prevalent in both infective and non‐infective AECOPD with elevated hs‐TnI in 27.3% and elevated NT‐proBNP in 61.7% overall. Anxiety/depression was prevalent in all aetiological subgroups (overall population HADS mean/SD =16.7/8.7). Survival at 12 months post discharge was lower in non‐viral versus viral AECOPD (p=0.03).
Conclusion
Hospitalized AECOPD are multidimensional and multifactorial. Subtyping by infection type identified significant differences in comorbidities, health care utilization, laboratory parameters, inpatient management and post exacerbation survival. Anxiety/depression and cardiac dysfunction appear prevalent but underdiagnosed. Our clinically oriented methodology provides a feasible framework for clinicians and researchers to address AECOPD complexity and target therapeutic interventions.
Grant Support: This project was supported by an unrestricted educational grant from GlaxoSmithKline.
TO 064
RELAXIN POTENTIATES SALBUTAMOL‐MEDIATED AIRWAY RELAXATION IN MULTIPLE SPECIES
Lam M1, Bourke J1, Royce S1, Samuel C1, Donovan C1, Jelinic M2, Parry L2
1Monash University, Melbourne, Australia, and 2University of Melbourne, Melbourne, Australia
Introduction
Treatment with β‐adrenoceptor agonists may not overcome symptoms of severe asthma. Relaxin (rhRLX), an RXFP1 receptor agonist, exerts cardioprotective effects in acute heart failure and elicits vascular relaxation via RXFP1 and nitric oxide signalling. Although we have previously established its bronchodilator efficacy in rat airways (Lam et al., 2016), its effects in other species and its potential to enhance β‐adrenoceptor‐mediated relaxation have yet to be explored.
Aim
To compare the bronchodilator effects of relaxin alone and in combination with the β2‐adrenoceptor agonists, isoprenaline (ISO) or salbutamol (SAL) in multiple species.
Methods
Tracheal rings or bronchi were dissected and/or precision cut lung slices (PCLS) containing intrapulmonary airways were prepared from mice, rats, guinea pigs and marmosets and human lungs (unused donor). rhRLX alone and in combination with ISO or SAL were added to airways pre‐contracted to MCh.
Results
rhRLX (100 nM) elicited partial relaxation in rat airways that was more rapid in PCLS than trachea but was ineffective as a direct bronchodilator in guinea pig trachea or mouse PCLS. rhRLX markedly increased the potency of ISO by 10‐fold in rat PCLS without increasing maximum relaxation, and of SAL by 27‐fold in guinea pig trachea. SAL only elicited partial relaxation in mouse PCLS but synergism was evident between rhRLX and SAL (maximum relaxation: rhRLX no response; SAL 41±5%; rhRLX/SAL 90±6%; n= 4‐7; P<0.001). Preliminary data showed rhRLX elicited relaxation and potentiated SAL‐mediated relaxation in marmoset and human small airways.
Conclusion
rhRLX elicits airway relaxation in some species and enhances responsiveness of both small and large airways to salbutamol across all species tested. Since rhRLX increases the potency of salbutamol, further investigations are warranted to define its therapeutic potential as an add‐on asthma therapy in human lungs, particularly when responsiveness to current dilator therapy is limited.
Grant Support: NHMRC Project Grant (1041575)
TO 065
ENDOSOMAL NOX2 OXIDASE INHIBITOR PROTECTS AGAINST HIGHLY PATHOGENIC INFLUENZA VIRUS MORBIDITY
To E1,2, Luong R1, Liong F1, Diao J3, Bozinovski S1, Porter C3, Quach T3, O'Leary J4, Brooks D5, Vlahos R1, Selemidis S1,2
1RMIT University, Bundoora, Australia, 2Monash University, Clayton, Australia, 3Monash Institute of Pharmaceutical Sciences, Parkville, Australia, 4Trinity Translational Medicine Institute, Ireland, and 5University of South Australia, Australia
Introduction/Aim
Influenza A viruses cause respiratory tract infections that can lead to fatal outcomes when the virus spreads to the alveolar space, more predominantly observed with high pathogenic influenza virus strains. We have shown that influenza A viruses, irrespective of strain, cause a burst of reactive oxygen species (ROS) production via NOX2 oxidase that occurs in endosomes. Evidently, an endosome targeted NOX2 oxidase inhibitor called cholestenol conjugated gp91ds‐TAT (Cgp91) abrogated disease caused by a seasonal strain of influenza A virus (IAV) in mice (1). The aim was to determine the effect of Cgp91 treatment on the lung pathology induced by a highly pathogenic strain of IAV.
Methods
Male C57Bl/6J mice were treated daily via intranasal administration with Cgp91 (0.2mg/kg) or DMSO (2%; control) over a 4‐day period. Mice were infected with the PR8 (H1N1; 500 PFUs) strain of IAV or PBS control, one‐day post initial drug treatment and analysed at day 3 post‐infection. Bronchoalveolar lavage (BAL) fluid collected from mice was used to assess airway inflammation. Histopathological analysis of lung was assessed using H&E stain and scored for alveolitis, inflammatory cell infiltrate and peribronchiolar inflammation. Superoxide generation in the BAL was measured using L‐012 enhanced chemiluminescence and changes in cytokine and viral mRNA expression in the lung were quantified using real‐time QPCR.
Results
Cgp91 treatment significantly (P<0.05) reduced airway inflammation, neutrophil influx, and pulmonary inflammation as measured by the degree of alveolitis, inflammatory cell infiltrate and peribronchiolar inflammation. Additionally, Cgp91 attenuated ROS generation and influenza viral mRNA expression in PR8‐infected mice.
Conclusion
The spatial inhibition of NOX2 in endosomal compartments with Cgp91 could be used as a potential treatment strategy for highly pathogenic influenza A virus infections.
Grant Support: NHMRC Australia (Project Grant ID 1122506, 1128276), ARC (FT120100876)
(1) To et al. Nature Communications, 2017, 8, Article number: 69.
TO 066
AMOXYCILLIN‐CLAVULANATE VS AZITHROMYCIN FOR RESPIRATORY EXACERBATIONS OF BRONCHIECTASIS IN CHILDREN: A MULTI‐CENTRE DOUBLE BLIND NON‐INFERIORITY RCT
Goyal V1,2,3, Grimwood K4, Masters I1,2, Brynes C5, Marchant J1,2,3, Morris P6,7, Ware R4, Van Aspern P8, O'Grady K2,3, Torzillo P9, McCallum G6, Champion A10, Buntain H1, Mackay I11, Sloots T11, Ungerer J12, Binks M6, Chang A1,2,3,6
1Lady Cilento Children's Hospital, Brisbane, Australia, 2University of Queensland, Brisbane, Australia, 3Centre for Children's Health Research, Queensland University of Technology, Brisbane, Australia, 4Menzies Health Institute Queensland, Griffith University and Gold Coast Health, Southport, Gold Coast, Australia, 5Department of Paediatrics, Unit of Auckland & Starship Children's Hospital, Auckland, New Zealand, 6Menzies School of Health Research, Charles Darwin University, Darwin,, Darwin, Australia, 7Department of Paediatrics, Royal Darwin Hospital, Darwin, Australia, 8Department of Respiratory Medicine, The Children's Hospital at Westmead, , Sydney, Australia, 9Royal Prince Alfred Hospital, Sydney, Australia, 10Department of Pharmacy, Lady Cilento Children's Hospital, Brisbane, Australia, 11Forensic and Scientific Services, Department of Health, Coopers Plains, Australia, and 12Department Chemical Pathology, Queensland Pathology, Royal Brisbane Hospital, Brisbane, Brisbane, Australia
Introduction
Based on limited available data, amoxycillin‐clavulanate is the current recommended first‐line empirical oral‐antibiotic treatment for non‐severe bronchiectasis exacerbations in children. Azithromycin is an attractive alternative because of its long half‐life, reduced dosing schedule, and good safety profile in children. We tested our primary hypothesis that oral azithromycin is non‐inferior (within 20% margin) to amoxycillin‐clavulanate at achieving resolution of exacerbation by day‐21 of treatment in children with bronchiectasis.
Methods
We conducted a multicentre, parallel group, double‐dummy, double‐blind placebo‐controlled RCT trial in 4 centres. At the start of an exacerbation, 179 children were randomised to receive either amoxycillin‐clavulanate (22.5 mg/kg bd)/placebo or azithromycin (5mg/kg/day)/placebo for 21‐days. Our primary outcome was resolution of exacerbation (defined as ‘return to baseline') by 21‐days. Study was powered for 90% (α=0.05, 1‐sided) with 20% non‐inferiority margin to detect 80% resolution rate by day‐21. Secondary outcomes were cough‐specific quality of life (PC‐QoL) and duration of exacerbation. Generalised linear model was used to calculate relative differences between groups.
Results
Baseline characteristics of the 2 groups (amoxycillin‐clavulanate n=97 and azithromycin n=82) were similar. By day‐21, resolution was comparable between groups, relative risk 0.99 95%CI 0.84‐1.17, falling within the a‐priori calculated 20% non‐inferiority margin. Between group differences for duration of exacerbation (2 days 95%CI ‐1.7, 5.3) and PC‐QoL at day‐21 compared to beginning of exacerbation was also within our non‐inferiority margin (0.42, 95%CI ‐0.06, 0.89).
Conclusion
Azithromycin is non‐inferior to amoxicillin‐clavulanate for treating non‐severe exacerbations of bronchiectasis in children. Azithromycin may be preferred to amoxicillin‐clavulanate in selected settings e.g. adherence. However, its use needs to be balanced with risk of treatment failure (within 20% compared to amoxicillin‐clavulanate) and inducing macrolide resistance.
Grant Support: NHMRC project grant (number 1019834). VG was supported by NHMRC PG scholarship. ABC is supported by a NHMRC practitioner fellowship
TO 067
LUNG ELASTIC RECOIL, INFLAMMATION AND PERSISTENT AIRFLOW LIMITATION IN ASTHMA
Tonga K1,2,3,4, Farah C1,2,3, Thamrin C1,2, Tang F1, Santos J5,6, Sharma P1,7, Oliver B1,7, King G1,2,4
1Woolcock Institute Of Medical Research, Glebe, Australia, 2Sydney Medical School, University of Sydney, Sydney, Australia, 3Concord Hospital, Concord, Australia, 4Royal North Shore Hospital, St Leonards, Australia, 5School of Life Sciences, University of Technology, Broadway, Australia, 6CIRIMAT, University of Toulouse, Toulouse, France, and 7Faculty of Sciences, University of Technology Sydney, Broadway, Australia
Introduction/Aim
Persistent airflow limitation (PAL) may develop in older non‐smokers with asthma however the mechanism is unknown. Reduced lung elastic recoil may contribute as this occurs with age and may occur in asthma. Neutrophilic airway inflammation is also more common in older people with asthma. We aimed to determine the relationship between lung elastic recoil, airway inflammation and airflow limitation. We hypothesise that reduced lung elastic recoil and neutrophilic airway inflammation are associated with PAL in older non‐smoking asthmatics.
Methods
Non‐smoking adults with asthma, treated with standardised high dose inhaled corticosteroid/long acting beta agonist for two months, underwent standard lung function, lung elastic recoil measurement using an oesophageal balloon to derive indices of loss of lung elastic recoil (increased K and reduced B/A), and bronchoscopy to obtain bronchoalveolar lavage fluid (BAL) for differential leukocyte count and TH17 cytokine measurement. Spearman correlations were assessed and multiple linear regressions were used to adjust for age, BMI and disease duration.
Results
Nineteen subjects (11 male; mean±SD age 63±9 years, asthma duration 38±22 years) demonstrated moderate PAL ((mean±SD z‐score) post‐bronchodilator FEV1 ‐2.05±0.75, FVC ‐0.61±0.95, FEV1/FVC ‐2.46±0.90). Reduced lung elastic recoil was demonstrated in 8/18 subjects (median (IQR) z‐score K 1.57(‐1.08–3.43), B/A ‐1.18(‐1.65–‐0.02)). FEV1/FVC correlated negatively with K (r=‐0.53, p=0.023) independent of age, BMI and disease duration. Neutrophilic airway inflammation was not demonstrated (mean±SD: neutrophils 9.1±18.1%, n=10). Lung elastic recoil did not correlate with BAL neutrophil count or TH17 cytokines.
Conclusion
Loss of lung elastic recoil contributes to PAL in older non‐smokers with asthma. This may be due to lung tissue changes in addition to airway remodeling. Despite the lack of relationship with airway inflammation in this exploratory study, the underlying cellular mechanisms require further investigation. An alternate paradigm of ‘lung remodeling' would have potential implications on preventing PAL in this population.
Grant Support: University of Sydney Bridging Grant
TOL 001
LUNG CELLS FROM PEOPLE WITH COPD ARE HYPER RESPONSIVE TO E‐CIGARETTE VAPOUR
Bozier J1,2, Xenaki D1,2, Adcock I3, Oliver B1,2
1University of Technology Sydney, Sydney, Australia, 2Woolcock Institute of Medical Research, University of Sydney, Sydney, Australia, 3NHLI, Imperial College London, London, UK
Introduction/Aim
E‐cigarettes are proposed as an alternative to smoking and as nicotine replacement therapy. There is confusion around the safety and efficacy of E‐cigarettes as smoking cessation aids stemming from contradictory findings across multiple studies. The aim of this study was to determine the inflammatory response of both Chronic Obstructive Pulmonary Disease (COPD) and non‐COPD cells to E‐vapour under realistic physiological conditions.
Methods
Primary human airway smooth muscle cells were stimulated with increasing concentrations of 18mg/ml nicotine and 0mg/ml nicotine (tobacco and menthol flavoured, Vaper empire) E‐vapour extract for 24 hours. An MTT assay was performed to determine cytotoxicity and ELISA was used to assess IL‐6 and CXCL8 production. Cells were isolated from explanted and resected lung tissue from COPD patients and smokers without COPD.
Results
All 4 E‐vapour extracts were cytotoxic to cells (n=9‐14, p≤0.0001), cytotoxicity of E‐vapour was increased in aerosols created at higher temperatures. All 4 E‐vapour extracts stimulated CXCL8 production compared to unstimulated controls (n=14, p<0.05). Cells from people with COPD were hyperresponsive to E‐vapours, with 18mg/ml nicotine tobacco flavoured E‐vapour stimulating significantly greater CXCL8 production from COPD cells compared to non‐COPD cells (n=7, p<0.05). IL‐6 production was not stimulated.
Conclusion
E‐cigarettes have the potential to contribute to the pathology of COPD. Cytotoxicity can cause cell death and ineffective repair, as seen in both the airways and parenchyma in COPD. Increased CXCL8 would contribute to the proinflammatory environment in the lung. Our data suggests that COPD patients should not use them as a smoking cessation aid or cigarette replacement.
Grant Support
None
TOL 002
DOES ASTHMA CONTROL IN PRESCHOOLERS PREDICT THE LIKELIHOOD OF DISEASE REMISSION?
Ducharme F1, Blais L1, Brownell M2, Quail J3, Sadatsafavi M4, Forget A5, Nie Y2, Li W3, Qutuyba H4, Fan Y6, Platt R6
1University of Montreal, Montreal, Canada, 2University of Manitoba, Winnipeg, Canada, 3Health Quality Council, Saskatoon, Canada, 4University of British Columbia, Vancouver, Canada, 5Research Centre, Hôpital du Sacré‐Cœur de Montréal, Montreal, Canada, 6McGill University, Montreal, Canada
Introduction/Aim
Many preschoolers with asthma experience disease remission. As the first 5 years of life may offer a window of opportunity to modify long‐term outcomes, we explored the relationship between the likelihood of remission and asthma control in the two years following the diagnostic of asthma in preschoolers.
Methods
We assembled a retrospective birth cohort of children born between 1990‐2013 in four Canadian provinces (Quebec, Manitoba, Saskatchewan, British Columbia). Preschool asthma was defined by one hospitalisation or 2 medical visits within a 2‐year period for asthma in children aged less than 5 years. Remission was assumed after two years without any asthma‐related drug claims, medical visit or hospitalization. The main exposure was asthma control in the 2 years following diagnosis, measured on the validated 4‐level Pediatric Pharmacoepidemiology Asthma Control Index (PPACI) and ascertained over 4 consecutive 6‐month periods. Cohort exit occurred at death, loss of medical or drug coverage, or date of last available data. Within each province, a Cox regression model served to estimate the strength of association between the PPACI stability over 2 years post diagnosis and remission, after adjusting for potential confounders and covariates, namely demographics (e.g., sex, social assistance), disease characteristics (e.g., age, atopy), therapy (e.g., first controller therapy). A random‐effects meta‐analysis aggregated the province‐specific results.
Results
Of 1.3 million live births in the 4 provinces, 118,785 children less than 5 years met the definition of asthma; 63% were male, 69% were aged less than 3 years at diagnosis. The pooled rate of remission was 7.74 (95% CI: 7.67, 7.81)/100 person‐years. Poorer asthma control over the 2 years following diagnosis was associated with incrementally lower likelihood of asthma remission (Table).
| PPACI 2 years post‐dx | Adjusted HR *(95% CI) |
| Controlled throughout | reference |
| Improving control | 0.80 (0.68, 0.95) |
| Varying control | 0.59 (0.52, 0.68) |
| Worsening control | 0.50 (0.42, 0.59) |
| Out of control throughout | 0.31 (0.27, 0.36) |
*Adjusted for demographic and disease characteristics (3 provinces)
Conclusion
Poorer asthma control in the two years following diagnosis is associated with an incrementally lower rate of remission. Better asthma control appears as a promising target to modify long‐term outcomes of asthmatic preschoolers.
Grant Support
This study was funded by the Canadian Respiratory Research Network. The Canadian Respiratory Research Network (CRRN) is supported by grants from the Canadian Institutes of Health Research (CIHR)—Institute of Circulatory and Respiratory Health; Canadian Lung Association (CLA)/Canadian Thoracic Society (CTS); British Columbia Lung Association; and Industry Partners Boehringer‐Ingelheim Canada Ltd, AstraZeneca Canada Inc., and Novartis Canada Ltd. The funders had no role in the study design, data collection and analysis, or preparation of the manuscript.
TOL 003
AN ASSESSMENT OF EARLY LIFE EXPOSURE TO COAL MINE FIRE SMOKE AND CHILDREN'S LUNG HEALTH
Shao J1, Zosky G2, Hall G3, Wheeler A1, Dalton M1, Dharmage S4, Foong R3, Williamson G5, O'Sullivan T1, Johnston F1
1Menzies Institute for Medical Research, University of Tasmania, Hobart, Australia, 2School of Medicine, Faculty of Health, University of Tasmania, Hobart, Australia, 3Children's Lung Health Telethon Kids Institute, School of Physiotherapy and Exercise Science Curtin University, Centre for Child Health Research, University of Western Australia, West Perth, Australia, 4Allergy and Lung Health Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia, 5School of Biological Sciences, University of Tasmania, Hobart, Australia
Introduction/Aim
In 2014, emissions from a fire in an open cut coal mine caused markedly increased concentrations of fine particulate matter (PM2.5) in the Latrobe Valley of Victoria, Australia, for approximately six weeks. We aimed to evaluate the impacts of infant (<2 years of age) exposure to mine fire emissions on lung function measured three years after the fire.
Methods
Hourly PM2.5 from the fire at 1x1 km2 was derived from an atmospheric transport model. Daily average and maximum PM2.5 were assigned to participants' residential address during the fire. Lung function was evaluated using the forced oscillation technique (FOT), which generated z scores for resistance (Rrs) and two measures of reactance as follows: (1) Reactance at a frequency of 5Hz, (Xrs) and (2) area under the reactance curve (AX). We used generalised linear models, adjusted for maternal smoking in pregnancy and maternal stress during the fire to assess associations between PM2.5 exposure and lung function.
Results
71 children, with a mean age of 4.3±0.6 (SD) years were included. Median [IQR] daily PM2.5 exposures were 6.8 [1.9‐12.7] μg/m3 (average) and 107.4 [60.4‐167.0] μg/m3 (maximum). The baseline mean (SD) z scores were Rrs 0.6 (0.8), Xrs 0.8(0.9) and AX 0.7(1.0). A 10μg/m3 and 100μg/m3 increase in average and maximum PM2.5 respectively was independently associated with z scores for AX coefficient (95%CI): Average PM2.5: 0.23 (0.02 to 0.44); Maximum PM2.5: 0.13 (0.00 to 0.25), but not with the other measures of lung function. Maternal smoking was strongly associated with Xrs5: 1.15 (0.60 to 1.69) and AX: 0.89 (0.30 to 1.48), while maternal stress during the fire was protective for Xrs5: ‐0.62 (‐1.19 to ‐0.06).
Conclusion
Exposure to coal mine fire emissions during infancy may be associated with reduced lung reactance. Further research is required to validate these findings.
Grant Support
Department of Health & Human Services, Victoria
Declaration of Interest Statement
The authors declared no competing interests.
TOL 004
LUNG DIFFUSING CAPACITY IN YOUNGER SMOKERS WITH NORMAL SPIROMETRY
Yong T1, Cheung T1, Papanikoloau V1,2, Finlay P1,2, Bardin P1,2, King P1,2
1Monash Health, Clayton, Australia, 2Monash University, Clayton, Australia
Introduction/Aim
The prevalence of Chronic Obstructive Pulmonary Disease (COPD) has been extensively studied, however limited evidence exists for the role of lung diffusing capacity for carbon monoxide (DLCO) in the management of COPD. Various predicted equations have been used in the interpretation of DLCO. Recently the Global Lung Initiative (GLI) has been established with new reference equations for calculating DLCO. We aimed to assess the prevalence of low DLCO in younger smokers with normal spirometry using the GLI predicted equations.
Methods
We performed a cross‐sectional analysis of subjects who have had both spirometry and TLCO measured at the Respiratory Laboratory at Monash Lung and Sleep, Monash Health. Subjects included males and females, aged 40 to 60 years with normal spirometry and significant smoking history. As sub‐study, CT scanning was used to assess the prevalence of parenchymal lung diseases in this group. Initially, the ROCA (Roca J, 1990) predicted equations were used in the calculation of lower limit of normal (LLN). Subsequently the results were reanalysed with the GLI equations and both sets of data were compared.
Results
We screened 15,226 lung function tests and identified 470 subjects aged between 40 and 60 with normal spirometry and a significant smoking histories. Of this cohort, 290 subject (60% of the group) had a TLCO below their lower limit of normal when using the ROCA equations. Subjects with the low DLCO had higher prevalence of emphysema and bronchiectasis on CT scanning. When GLI equations were applied, there was a markedly lower prevalence of low DLCO, with 24.3% of subjects in this cohort having a DLCO below LLN.
Conclusion
A low transfer factor for carbon monoxide (DLCO) is prevalent amongst younger smokers with normal spirometry. This low TLCO may be an important early indicator of potential lung damage in COPD.
Grant Support
NA
Cystic Fibrosis 2
TO 068
EFFECT OF LUMACAFTOR/IVACAFTOR ON CT SCORES: EXPLORATORY IMAGING SUBSTUDY
Wainwright C1, Brody A2, Nagle S3, Hug C4, Marigowda G4, Waltz D4, Goldin J5, Ratjen F6, Wang L4
1Lady Cilento Children's Hospital, South Brisbane, Australia, 2Department of Radiology, Cincinnati Children's Hospital Medical Center, OH, USA 3Departments of Radiology, Medical Physics, and Pediatrics, University of Wisconsin‐Madison, WI, USA 4Vertex Pharmaceuticals Incorporated, MA, USA 5Department of Radiologic Sciences, David Geffen School of Medicine, CA, USA and 6Hospital for Sick Children, University of Toronto, Canada
Introduction/Aim
To evaluate lumacaftor (LUM) and ivacaftor (IVA) combination therapy on lung morphology with CT scanning in patients aged 6‐11 years with cystic fibrosis (CF) homozygous for the F508del‐CFTR mutation.
Methods
Baseline CT scans were obtained in 19 patients (12 LUM/IVA, 7 placebo) from the phase 3 trial (NCT02514473), and 24‐week CT scans were completed in 7 active treatment and 3 placebo patients. CT scans were obtained at total lung capacity and at residual volume (RV). CT scans were scored by 2 independent readers blinded to all patient and time point information using the Brody score, which evaluates extent and severity of multiple aspects of CF lung disease, including bronchiectasis and air trapping. Scores are presented as mean ± SD; no statistical testing was performed for this preliminary study.
Results
Mean total CT score (sum of the subcomponent scores) decreased from 20.6 to 12.5 (mean change ± SD, 8.1±13.6) in the LUM/IVA group and increased from 32.8 to 41.4 (8.6±14.6) in the placebo group. Mean bronchiectasis score decreased from 3.2 to 2.5 (0.7±1.3) in the LUM/IVA group and increased from 6.4 to 8.1 (1.7±2.1) in the placebo group. Additionally, there was a suggestion that several ectatic bronchi decreased in size in patients on active treatment. Mean air trapping score decreased from 7.8 to 5.9 (1.9±6.8) in the active group and increased from 9.8 to 14.5 (4.7±11.7) in the placebo group.
Conclusion
This is the first report to describe CT lung findings after CFTR corrector/potentiator therapy in patients 6‐11 years of age homozygous for F508del. In this 24‐week exploratory analysis, bronchiectasis and air trapping scores improved in patients treated with LUM/IVA and worsened in the placebo group. These data suggest that LUM/IVA may reduce CF disease‐related changes in lung morphology and support the need for further study.
Grant Support: Sponsored by Vertex Pharmaceuticals Incorporated.
Conflict of Interest: CEW received grant income on a per patient basis for conducting studies, personal fees, and travel support from Vertex Pharmaceuticals Incorporated during the conduct of the study. She also received personal fees and travel support from Novartis Pharmaceuticals, a research grant from Novo Nordisk, and grant income on a per patient basis for conducting studies from Vertex Pharmaceuticals Incorporated, Boehringer‐Ingelheim, and Ablynx NV outside of the submitted work.
TO 069
LONGITUDINAL ASSESSMENT OF CT REGIONS OF LOW ATTENUATION REVERSIBILITY IN YOUNG CHILDREN WITH CYSTIC FIBROSIS
Mok L1,2, Andrinopoulou E3, de Bruijne M4,5, Tiddens H6,7, Stick S1,2,8, Rosenow T1
1Telethon Kids Institute, The University of Western Australia, Perth, Australia, 2School of Paediatrics and Child Health, The University of Western Australia, Perth, Australia, 3Department of Biostatistics, Erasmus Medical Center, Rotterdam, Netherlands, 4Biomedical Imaging Group Rotterdam, Departments of Medical Informatics and Radiology, Erasmus Medical Center, Rotterdam, Netherlands, 5Department of Computer Science, University of Copenhagen, Copenhagen, Denmark, 6Departments of Pediatric Pulmonology and Allergology, Erasmus Medical Center, Sophia Children's Hospital, Rotterdam, Netherlands, 7Department of Radiology, Erasmus Medical Center, Rotterdam, Netherlands, and 8Department of Respiratory Medicine, Princess Margaret Hospital for Children, Perth, Australia
Introduction
Low attenuation regions (LAR) on chest CT are an important component of end‐stage lung disease and reflect small airways disease in cystic fibrosis (CF). However, the extent of LAR reversibility in young children is unknown. We aimed to assess localised changes in LAR distribution over time in relation to CF‐lung disease outcomes. We hypothesised that a proportion of LAR is irreversible in young children with CF and indicative of clinical severity.
Methods
Children in the AREST CF cohort contributed CT scans and clinical data from annual consecutive visits. Localised changes in LAR distribution were assessed using specialised image analysis software by matching CT lung images from two time points and measuring the lung volume proportion of new (%LARnew), reversed (%LARreversed) and stable (%LARstable) LAR. Linear mixed effects models adjusted for age and multiple visits, assessed differences between LAR outcomes and their association with clinical predictors. These include: age, pancreatic sufficiency, bronchiectasis extent determined from the PRAGMA‐CF method and pulmonary inflammation and infection measured by bronchoalveolar lavage.
Results
The entire cohort comprised 139 CT scans from 45 CF patients with mean age (range) of 4.5(2.0‐6.8) years. Approximately one‐third of total LAR was stable over time. Age‐corrected log%LARnew (0.49[0.31, 0.66]; p<0.001) and log%LARreversed (0.59[0.41, 0.76]; p<0.001) were significantly higher than log%LARstable. Log%LARnew was inversely correlated with pancreatic sufficiency (‐0.702[‐1.197, ‐0.208]; p=0.006) and log%LARreversed was associated with the presence of neutrophils in the previous year (0.016 [0.008, 0.024]; p<0.001). Log%LARstable was associated with pancreatic sufficiency (‐0.769[‐1.386, ‐0.151]; p=0.016) and the previous detection of neutrophilic inflammation (0.011[0.003, 0.0184]; p=0.009).
Conclusion
CT‐detected LAR is present in early life and around one‐third of LAR is irreversible over time. Progressive LAR is associated with pancreatic insufficiency and neutrophilic inflammation in children with CF, which suggest a role for LAR as a secondary imaging endpoint.
Grant Support: European Respiratory Society Short‐Term Research Fellowship
TO 070
SCHOOL‐AGED OUTCOMES OF INFANT LUNG FUNCTION IN CYSTIC FIBROSIS
Foong R1,2, Ramsey K1,3, Zajakovski N4,5, Skoric B4,5, King L4,5, Turkovic L1, Harper A1, Stick S1,6, Hall G1,3, Ranganathan S4,5
1Telethon Kids Institute, Perth, Australia, 2Curtin University, Perth, Australia, 3Bern University Hospital, Bern, Switzerland, 4Murdoch Children's Research Institute, Melbourne, Australia, 5Royal Children's Hospital, Melbourne, Australia, and 6Princess Margaret Hospital, Perth, Australia
Introduction/Aim
Studies show that a significant proportion of infants with cystic fibrosis (CF) have diminished lung function within the first 2 years of life. However, it is unknown whether lung function tests in infancy have the potential to predict worse prognosis and determine which infants are most likely to benefit from treatment early in life. This study aims to investigate whether diminished lung function detected in infants diagnosed following newborn screening is associated with worse lung function when re‐measured at school‐age.
Methods
Lung function was assessed in 58 individuals with CF diagnosed after newborn screening (0‐2 years) and again at school age (7–10 years). The raised volume rapid thoraco‐abdominal compression (RVRTC) technique and multiple breath washout (MBW) test was performed at infancy, and spirometry and MBW performed again at school‐age. Mixed‐effects models were used to determine if outcomes from RVRTC such as forced expiratory volume in 0.5 second (FEV0.5) and FVC, as well as lung clearance index (LCI) from the MBW test were associated with FEV1, FVC and FEV1/FVC measured by spirometry, and LCI at school‐age.
Results
Age and height‐adjusted FEV0.5 and FVC and height‐adjusted LCI at infancy were not associated with zFEV1, zFVC and zFEV1/FVC and LCI at school‐age. The coefficients, 95% confidence intervals and p‐values of the mixed‐effects models are shown below.
| Infant LCI | Infant FEV0.5 | Infant FVC | |
|---|---|---|---|
| zFEV1 | 0.13 (‐0.66, 0.91) p=0.742 |
‐0.27 (‐1.66, 1.12) p=0.696 |
0.25 (‐1.40, 1.91) p=0.760 |
| zFEV1/FVC | 0.45 (‐0.22, 1.12) p=0.186 |
‐0.02 (‐1.18, 1.13) p=0.967 |
‐0.26 (‐1.63, 1.11) p=0.703 |
| LCI |
0.60 (‐0.55, 1.74) p=0.300 |
‐1.89 (‐4.85, 1.08) p=0.206 |
‐3.29 (‐6.80, 0.21) p=0.065 |
Conclusion
Lung function measured in infancy is not associated with lung function outcomes at school‐age. Other factors such as respiratory infections and clinical status should be investigated and may be better predictors of worse lung function at school‐age.
Grant Support: NHMRC APP1020555
Conflict of Interest: All authors have no conflict of interest to declare.
TO 071
PREVALENCE OF NONTUBERCULOUS MYCOBACTERIA (NTM) IN POTABLE WATER
Stockwell R1,2, Leong L3, Wood M1,2,4, Sherrard L1,5, Thomson R6, Rogers G3, Bell S1,2,4
1Lung Bacteria Group, QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia, 2Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia, 3Microbiome Research, South Australia Health and Medical Research Institute, Adelaide, South Australia, Australia, 4Adult Cystic Fibrosis Centre, The Prince Charles Hospital, Brisbane, Queensland, Australia, 5School of Pharmacy, Queen's University Belfast, Belfast, UK, and 6Respiratory Research Unit, Greenslopes Medical Research Institute, Brisbane, Queensland, Australia
Introduction/Aim
NTM is an emerging respiratory infection in people with cystic fibrosis (CF) with one species, Mycobacterium abscessus complex (MABSC), causing concern. The mode of acquisition is unknown but their prevalence in potable water may be a risk factor in people with CF. This study is investigating if NTM can be recovered from the potable water systems of The Prince Charles Hospital (TPCH) and Queensland homes.
Methods
Water was collected from showers and sink taps of two respiratory wards at TPCH across five time points (2014 to 2017). Water was collected from homes in Queensland from four groups: 1) People with CF who had active MABSC respiratory infection (<2 years since positive sputum culture); 2) People with CF and past MABSC respiratory infection (>2 years since positive sputum culture); 3) People with CF never infected with NTM; 4) People with no lung disease. The hospital and home water samples were filtered, inoculated into growth media and incubated for 8 weeks. DNA was extracted from presumptive NTM isolates and sent for whole genome sequencing.
Results
The water sampling recovered 257 presumptive NTM isolates (hospital, n=69; home, n=188). To date, 94 presumptive NTM isolates have been sequenced. Two isolates were contaminants. Thirty‐nine isolates from the hospital water were identified as Mycobacterium kansasii (n=25), MABSC (n=7), unidentified Mycobacterium (n=5) and Mycobacterium avium (n=2). Fifty‐five isolates from the home water were identified as MABSC (n=29), M. kansasii (n=10), unidentified Mycobacterium (n=10) and M. avium (n=4). These water isolates are being compared to CF MABSC respiratory isolates as well as other environmental isolates.
Conclusion
NTM species can be found in potable water systems of homes and a hospital. The most dominant NTM species were M. kansasii in the hospital water and MABSC in the home water.
Grant Support: Cystic Fibrosis Foundation Therapeutics (USA), The Prince Charles Hospital Foundation (Australia), Advance Queensland.
TO 072
HIGH FREQUENCY HEARING LOSS IN CYSTIC FIBROSIS ADULTS
Song Y1,2, Lennon J1,2, Burns T1,2, Middleton P1,2,3
1Department of Respiratory and Sleep Medicine, Westmead Hospital, Westmead, Australia, 2Ludwig Engel Centre for Respiratory Research, Westmead Institute for Medical Research, Westmead, Australia, and 3Sydney Medical School, University of Sydney at Westmead Hospital, Westmead, Australia
Introduction/Aim
Cystic Fibrosis (CF) is characterised by chronic lung infections often with Pseudomonas aeruginosa, requiring repeated aminoglycoside therapy. Aminoglycosides are recognised to cause both acute and chronic damage to the inner ear with sensorineural hearing loss (SNHL), especially of the higher frequencies. This study examined hearing in CF adults at Westmead Hospital, comparing pure tone audiometry (PTA) with high frequency audiometry (HFA).
Methods
Asymptomatic CF adults were recruited from the outpatient CF clinic. In a quiet room, PTA examined frequencies of 500Hz to 6000Hz, whilst HFA tested frequencies of 8000Hz to 16000Hz. Hearing loss severity was categorised as follows: 26‐40dB (slight), 41‐60dB (moderate), 61‐80dB (severe), and 81+dB (profound), recording the worst 2 consecutive frequencies in standard and high ranges.
Results
A total of 134 CF adults, mean (SD) age 26.7 (8.7) years were recruited. Standard PTA detected hearing loss in both ears with 5 showing slight, 3 moderate and 2 severe impairment. HFA detected more hearing loss with 20 having slight, 16 moderate, 9 severe and 4 profound impairment. All those with hearing loss at standard frequencies exhibited similar or worse abnormalities at high frequencies. Older patients showed more hearing abnormalities both at standard and high frequencies.
Conclusion
These preliminary results suggest that HFA is more sensitive than standard PTA for measurement of potential hearing loss in the CF population. Comparison of these results with the cumulative doses of aminoglycosides is being undertaken in this cross‐sectional study.
Grant Support: This study was supported by a Novartis Grant‐in‐Aid.
TO 073
A REVIEW OF PERIPHERALLY INSERTED CENTRAL CATHETER‐ASSOCIATED DEEP VENOUS THROMBOSIS IN ADULT CYSTIC FIBROSIS PATIENTS IN WESTERN AUSTRALIA
Moore I1, Tai A1,2,3, Morey S1,2, Mulrennan S1,2,3
1Sir Charles Gairdner Hospital, Perth, Australia, 2Institute of Respiratory Health, Perth, Australia, and 3School of Medicine, University of Western Australia, Perth, Australia
Introduction
Peripherally inserted central catheters (PICC) have an integral role in managing pulmonary exacerbations in Cystic Fibrosis (CF). They allow effective delivery of intravenous antibiotics both in inpatient and outpatient settings. With repeated use of PICC lines, however, the incidence of complications rises. One such complication is deep venous thrombosis (DVT) and treatment with anti‐coagulation can prove challenging in the setting of haemoptysis or CF related liver disease.
Aim
A retrospective audit was undertaken at Sir Charles Gairdner Hospital of all PICC line insertions in patients with CF between January 2016 and February 2017. The objectives were (i) to assess current practice of PICC insertion and (ii) to determine the frequency of PICC‐associated DVT.
Methods
Information was obtained through computer records and included basic patient demographics, prior history of haemoptysis or venous thrombosis, complications and outcomes.
Results
A total of 121 4Fr PICC insertions in 63 patients (33 males and 30 females) took place during the study period. Twenty‐eight percent of patients had a history of haemoptysis and one fifth (13/63; 20.6%) had a prior history of DVT or pulmonary embolus. The majority of patients had PICC lines inserted by a Radiologist (55.4%) and the rest were performed by Nurse Practitioners (44.6%). Symptomatic DVT (or pulmonary embolism) occurred in 6/121 (4.96%).
Conclusion
Our audit shows that the rate of PICC‐associated DVT in adults attending the WA adult CF centre is equivocal to that reported in the literature of between 3.5 – 16.4%. It is well recognised that factors including PICC size, the thrombotic state of patients with CF and history of DVT can impact the likelihood of PICC‐associated DVT. Following this audit we plan to assess the role of enoxaparin prophylaxis, particularly in the outpatient setting, aiming to further minimise the risk of PICC associated DVT.
Grant: Dr Anna Tai is the recipient of the following grants:
Glenn Brown Memorial Grant, Institute of Respiratory Health, WA;
Conquer CF Program Grant, Institute of Respiratory Health, WA
TSANZ Vertex Adult Cystic Fibrosis Fellowship
Conflict of Interest: Nil.
Grant Support:
Interventional Pulmonology / Bronchology 1
TO 074
PLeural Effusion And Symptom Evaluation (PLEASE) STUDY ON THE PATHOPHYSIOLOGY OF BREATHLESSNESS IN PATIENTS WITH SYMPTOMATIC PLEURAL EFFUSIONS
Muruganandan S1,2,3, Azzopardi M4, Thomas R1,2, Fitzgerald D1,2, Kuok Y5, Read C2, Murray K6,7, Budgeon C6,7, Jenkin S11,12, Singh B8,9,10, Eastwood P8,9,10, Lee Y1,2,3
1Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Australia, 2Pleural Medicine Unit, Institute for Respiratory Health, Perth, Australia, 3Centre for Respiratory Health, School of Medicine & Pharmacology, University of Western Australia, Perth, Australia, 4Department of Respiratory Medicine, Sunshine Coast University Hospital, Sunshine Coast, Australia, 5Department of Radiology, Sir Charles Gairdner Hospital, Perth, Australia, 6Centre for Applied Statistics, University of Western Australia, Perth, Australia, 7School of Population and Global Health, University of Western Australia, Perth, Australia, 8West Australian Sleep Disorders Research Institute, Perth, Australia, 9Centre for Sleep Science, School of Human Sciences, University of Western Australia, Perth, Australia, 10Pulmonary Physiology & Sleep Medicine, Sir Charles Gairdner Hospital, Perth, Australia, 11Physiotherapy Unit, Institute for Respiratory Health, Perth, Australia, and 12Physiotherapy Department, Sir Charles Gairdner Hospital, Perth, Australia
Introduction/Aim
Breathlessness is common in patients with pleural effusion, but its pathophysiology is unclear. PLEASE is a comprehensive study assessing physiological and symptom responses to pleural effusion drainage and aims to i) identify etiologic factors that correlate with breathlessness and ii) determine incidence and factors influencing symptomatic benefit from fluid drainage.
Methods
Consecutive patients with symptomatic pleural effusion undergoing therapeutic drainage were recruited. Pre‐ and Post‐measurements included 1) Patient and effusion‐related characteristics; 2) Degree of breathlessness using three separate grading systems; 3) 6‐minute Walk Distance (6MWD) capacity; 4) Spirometry; and 5) Diaphragm morphology and motion with ultrasonography.
Results
The 145 patients (median age 69; 55% male) most commonly (63%) had malignant effusions and heart failure effusions (15%). Most (93%) effusions were moderate‐ or large‐sized (≥25% hemithorax on CXR) and had 1680 [median, IQR 1100–2600] mL drained.
All breathlessness measurements improved significantly after effusion drainage: Visual Analog Score by 30.0mm (minimal clinical important difference=14mm); Dyspnoea‐12 score by ‐10; Borg score by 0.62 (all p<0.05). Respiratory and heart rates, 6MWD (increase by 26m), FEV1 and FVC (by 8% and 6.6%) all improved (p<0.05). Abnormal diaphragmatic morphology (flattened or inversion, 50%) and motion (paralysed or paradoxical, 48%) were common pre‐drainage, and normalized in 94% and 73% of patients, respectively, post‐drainage. Most (73%) reported significant relief of breathlessness (by VAS).
Conclusion
The pathophysiology of breathlessness in patients with pleural effusion is complex and multifactorial. Drainage of pleural effusion improves symptoms, functional capacity, and spirometry and normalises diaphragm morphology and motion.
Grant Support: NHMRC Fellowships (RT, YCGL, SJ, PE), WA Cancer Council (RT, YCGL), WACPCN Fellowship (MA, SM).
Conflict of Interest: All authors declare no conflict of interests.
TO 075
RELATIONSHIPS OF PLEURAL FLUID PH AND GLUCOSE LEVELS: A MULTI‐CENTRE STUDY OF 2971 CASES
Fitzgerald D1,2, Leong S1,2, Budgeon C3, Murray K4, Rosenstengel A5, Smith N6, Bielsa S7, Clive A8, Maskell N8, Porcel J7, Lee Y1,2,9
1Department of Respiratory Medicine, Sir Charles Gairdner Hsopital, Nedlands, Australia, 2Pleural Medical Unit, Institute for Respiratory Health, Nedlands, Australia, 3Centre for Applied Statistics, University of Western Australia, Nedlands, Australia, 4School of Population and Global Health, University of Western Australia, Nedlands, Australia, 5Holy Spirit Northside Hospital, Brisbane, Australia, 6Wellington Regional Hospital, Wellington, NZ, 7Pleural Diseases Unit, Arnau de Vilanova University Hospital, Lleida, Australia, 8North Bristol Lung Centre, Bristol, UK, and 9School of Medicine and Pharmacology, University of Western Australia, Nedlands, Australia
Introduction/Aim
Pleural fluid pH and glucose levels are both recommended in current guidelines as investigations in the workup of pleural effusions. Both parameters are reduced in inflammatory and/or metabolically active conditions. Whether pleural fluid pH and glucose levels provide duplicated information or independent knowledge is unclear. We aimed to investigate the relationships between pleural fluid pH and glucose levels in unselected pleural effusions, and the incidences of discordance in their levels.
Methods
Setting: Pleural services of three centres in Spain, UK and Australia.
Data: Clinical information and pleural fluid pH and glucose levels were collected.
Analyses: i) To assess the relationship between pH and glucose using smooth curves from restricted cubic spline models; ii) Concordance between pH and glucose for varying cut‐off levels was assessed.
Results
Pleural fluid samples (n=2971) were separated into four categories: malignant (n=1045), bacterial infection (n=1133), TB pleuritis (n=544) and other benign effusions (n=249). The mean pH was 7.38 (SD 0.22) and median glucose was 5.99 (range 0‐29.4) mmol/L. Linear regression modelling of the relationship between glucose (log‐transformed) and pH with a restricted cubic spline showed linear (p<0.01) and nonlinear effects (p<0.01). Most (91.6%; n=2720) of the samples were concordant in pH and glucose levels (i.e. at cutoffs of 7.20 and 3.3mmol/L respectively). Concordance was the lowest in the TB group (80.7%) and highest in the other benign pleuritis group (98.2%). Patients with a low pH but high glucose (n=99) were more likely to be diabetic (31% were diabetic vs 8% of those with low glucose and high pH), p<0.001, and have bacterial infection.
Conclusion
Pleural fluid pH and glucose correlate and are concordant in the majority of cases. Either test below its cut‐off level can be used to aid diagnosing infection. Pleural fluid glucose should be interpreted with care in diabetic/hyperglycaemic patients.
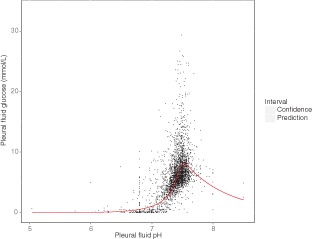
TO 076
COMPARISON OF THE 19‐GAUGE AND THE 21/22‐GAUGE ASPIRATION NEEDLE IN ENDOBRONCHIAL ULTRASOUND‐GUIDED TRANSBRONCHIAL NEEDLE ASPIRATION (EBUS‐TBNA) IN DIAGNOSING MEDIASTINAL LESIONS
Hsu K1, Tan E2, Karunarathne S2
1Royal Adelaide Hospital, Adelaide, Australia, and 2Lyell McEwin Hospital, Adelaide, Australia
Introduction/Aim
This study aims to examine whether there is a difference between the 19 and 21/22‐G EBUS‐TBNA needles in obtaining adequate tissue for diagnosis and ancillary testing, as well comparing their safety.
Methods
This was a retrospective review of EBUS‐TBNA cases done at the Lyell McEwin Hospital between June 2016 to September 2017. We included 25 cases done with the 19‐G needle. For comparison, we randomly selected the same number of cases using the 21 or 22‐G needle. Data collection included the patients' demographic data, diagnosis based on fine needle aspiration (FNA) samples, average size of lymph nodes biopsied, number of needle passes, sample adequacy for immunohistochemistry (IHC) and molecular mutation testing in cases of primary lung adenocarcinoma (EGFR and ALK), sample quality and procedure complication data. Results were analysed and compared statistically using the Fisher's test.
Results
With the 19‐G needles, the diagnostic yield was 96% and 80% with the 21/22‐G needles (p= 0.19). Sample adequacy was obtained with IHC in 90% in the 19‐G compared to 50% in the 21/22‐G group (p= 0.04). In both groups, molecular mutation testing was achieved in 100% of patients with primary lung adenocarcinoma. Average size of lymph nodes was significantly larger in the 19‐G group compared with the 21/22‐G group (30mm ± 10.5mm cf. 18mm ± 9.8mm, p= 0.0006) However, there was slight increase in bleeding in the 19‐G group (20% cf. 4%, p= 0.19).
Conclusion
There was no significant difference between the 2 needle sizes used in EBUS‐TBNA with regards to diagnostic yield and sample adequacy for molecular mutation testing. However, in this study, there was a significant difference between sample adequacy for IHC testing. This comes at a slight increased risk of bleeding.
Grant Support: Nil
Declaration of Interest: Nil
References: Nil
TO 077
INTRAPLEURAL TPA WITH DNASE FOR IPC RELATED PLEURAL INFECTION
Fitzgerald D1,4, Popowicz N1,2,3, Muruganandan S1,2,4, Thomas R1,4, Lee Y1,2,4
1Pleural Medicine Unit, Institute for Respiratory, Perth, Western Australia, Australia, 2School of Medicine & Pharmacology, University of Western Australia, Perth, Western Australia, Australia, 3Department of Pharmacy, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia, and 4Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia
Introduction/Aim
Indwelling pleural catheter (IPC) is an effective treatment for recurrent, especially malignant, pleural effusions. Pleural infection, though uncommon, remains physicians' major concern in the use of IPCs. Intrapleural tPA/DNase therapy has revolutionized care of pleural infection, but its use in IPC‐related pleural infection has not been the subject of prior reports.
Methods
Single centre, retrospective review of patients with IPC‐related pleural infection treated with tPA/DNase in our tertiary pleural unit. Demographics, interventions and outcomes of treatment were described. Treatment success is defined as survival to hospital discharge and avoidance of surgery. Data are presented as percentages or median [IQR] as appropriate.
Results
Nineteen patients (63% male, age 68 [59‐73] years) received intrapleural tPA/DNase. Most had malignant effusions from mesothelioma (68.4%) or non‐small cell lung carcinoma (15.8%). Median time from IPC insertion to diagnosis of pleural infection was 162 [57‐363] days. Median follow‐up was 262 [124‐453] days. One patient died before 30‐day follow‐up from cancer progression. Fever (73.7%), dyspnoea (42.1%) and decreased fluid drainage (36.8%) were the commonest presenting complaints. Staphylococcus aureus and gram‐negative bacilli were the most common organisms found in pleural fluid culture. tPA/DNase therapy successfully cured 90% (17/19) of cases. The remaining two patients underwent surgery because of inadequate clinical improvement. Three patients required additional chest drain or thoracentesis. CRP improved from 170 [135‐250)IU/L pre‐tPA/DNase to 17 [10.1–66.0]IU/L at outpatient follow‐up and WCC from 11.8 [8.5–14.3] x109/L to 8.8 [6.5‐10.2]x109/L, p=0.001 and 0.036 respectively. Pleural opacity on CXR improved in most (84.2%) patients. Post‐infective pleurodesis developed in 11 patients allowing IPC removal. Length of hospital stay was 7 [6‐9] days. No significant complications (including bleeding) associated with tPA/DNase therapy were observed.
Conclusion
Intrapleural tPA/DNase therapy can be safely administered via IPC for pleural infection and provides a high cure rate.
Grant Support: NHMRC Fellowships (RT, YCGL), WA Cancer Council (RT, YCGL), WACPCN Fellowship (SM).
Declaration: Rocket Med Ltd has provided free IPC drainage kits and a unrestricted educational grant for previous trials led by YCGL. YCGL has served on advisory boards of Carefusion/BD, Lung Therapeutics Inc. and Sequana Med Ltd.
TO 078
PREVIOUS PLEURAL INJURY INCREASES PNEUMOTHORAX RISK POST‐ENDOBRONCHIAL VALVE INSERTION FOR BRONCHOSCOPIC LUNG VOLUME REDUCTION
Oh A1, Grosser D1, Nguyen P2, Hnin K3, Smith B1
1The Queen Elizabeth Hospital, Woodville South, South Australia, Australia, 2Royal Adelaide Hospital, Adelaide, South Australia, Australia, and 3Ashford Hospital, Ashford, South Australia, Australia
Introduction/Aim
Bronchoscopic lung volume reduction (BLVR) via endobronchial valve (EBV) insertion is an accepted treatment for patients with severe emphysema. The most common complication of EBV insertion is pneumothorax, with a reported incidence of up to 25%. The aim of this study was to determine if previous pleural injury, or paraseptal/panlobular emphysema morphological subtype, would contribute to pneumothorax risk post‐EBV insertion.
Methods
EBV insertion for BLVR that occurred in Adelaide, South Australia over the period 2014 to September 2017 were examined in 3 centres: the Royal Adelaide Hospital, The Queen Elizabeth Hospital, and ChestCare Clinic.
Emphysema subtype was determined by evaluating pre‐EBV CT chest scans. The presence of pleural injury was determined by assessing patients for previous pneumothorax, pleural instrumentation, and pleural plaques/nodules in their pre‐EBV CT chest scans.
Results
86 procedures were completed within the study timeframe. 13 (15.1%) procedures resulted in pneumothorax. Mean age at EBV insertion was 67.31 years. 54.6% (47/86) of EBV insertions occurred in male patients. Statistical analysis was undertaken via logistic regression.
Previous pleural injury significantly increased the risk of pneumothorax post‐EBVI (OR 22.55, 95% confidence interval 2.51‐202.51, p = 0.005,). Gender, age at EBV insertion, and paraseptal/panlobular emphysema subtypes did not significantly increase pneumothorax risk.
Conclusion
This is the first Australian study to examine risk factors for pneumothorax incidence in EBV insertion. Previous pleural injury significantly increases the pneumothorax risk after EBV insertion. This data will contribute to our ability to predict pneumothorax in patients evaluated for EBV insertion, thus allowing improved risk assessment, and facilitating discharge planning post‐EBV insertion. We plan further studies evaluating other possible risk factors, including quantitative CT scoring of pleural adhesions.
Grant Support: None
TO 079
EPITOME (EARLY PLEURODESIS VIA INDWELLING PLEURAL CATHETER WITH TALC FOR MALIGNANT EFFUSIONS): A PILOT STUDY OF THE STATE‐OF‐THE‐ART MANAGEMENT ALGORITHM
Fitzgerald D1,2,3, Muruganandan S1,2,3, Stanley C2,3, Read C2,3, Thomas R2,3, Lee Y1,2,3
1School of Medicine and Pharmacology, University of Western Australia, Australia, Nedlands, Australia, 2Respiratory Department, Sir Charles Gairdner Hospital, Nedlands, Australia, and 3Pleural Medicine Unit, Institute for Respiratory Health, Nedlands, Australia
Introduction
Talc pleurodesis (TP) and indwelling pleural catheter (IPC) are recognized treatments for malignant pleural effusions (MPEs); each with its own advantages. Combining them can potentially provide best fluid control, facilitate early IPC removal, minimize re‐intervention, hospitalization, long term IPC costs and complications.
Methods
A single‐centre pilot study of a new treatment algorithm, EPIToME. All patients with symptomatic MPEs requiring definitive treatment were offered inpatient IPC (unless contraindications) insertion. Upon complete drainage (usually overnight), CXR was performed. If the lung full re‐expanded, talc slurry (4g) was instilled via the IPC and patient discharged the following day with daily IPC drainage using suction‐bottle for 10‐14 days (longer if continual reduction of drainage volumes). IPCs were removed if pleurodesis was successful (defined as fluid drainage <50ml for 3 consecutive drainages without significant residual effusion on imaging). Patients with trapped lung, or contraindication to talc, were discharged with IPC and drainage when symptomatic. Data were presented as median [IQR].
Results
Patients with MPE (n=40: 60% male, median age 70) from metastatic cancers (47.5%) or mesothelioma were included. A median volume of 2.5 [1.9‐3.5] litres were drained within 24 hours of IPC insertion. Sixteen patients fulfilled the criteria and received talc instillation via the IPC, usually one day post‐IPC insertion. The median total hospitalization was 3 [2‐3] days. Nine patients (56%) achieved pleurodesis after median of 14 days [11‐27] and underwent catheter removal with no evidence of recurrence; median follow‐up 116 [81‐55] days. Talc was not administered in 24 patients due to trapped lung (50%), prior failed talc pleurodesis (21%), etc. Complications of talc included reversible tube blockage (n=2), self‐limiting fever (n=2) and subsequent development of symptomatic loculations (n=3 successfully managed tube drainage ± intrapleural tPA).
Conclusion
The EPIToME protocol combining IPC and talc pleurodesis is feasible, safe and has potential advantages over individual therapies.
Grant Support: NHMRC Fellowships (RT, YCGL), WA Cancer Council (RT, YCGL), WACPCN Fellowship (SM)
Declaration: Rocket Med Ltd has provided free IPC drainage kits and a unrestricted educational grant for previous trials led by YCGL. YCGL has served on advisory boards of Carefusion/BD and Sequana Med Ltd.
Pulmonary Physiology & Sleep 1
TO 080
OBSTRUCTIVE SLEEP APNOEA EPIDEMIOLOGY IN THE BUSSELTON HEALTHY AGEING STUDY (BHAS)
Cunningham J1, James A1, Knuiman M2, Singh B1, Murray K2, Hunter M2,3
1Sir Charles Gairdner Hospital, Perth, Western Australia, Australia, 2University of Western Australia, Perth, Western Australia, Australia, and 3Busselton Population Medical Research Institute, Perth, Western Australia, Australia
Introduction/Aim
Obstructive sleep apnoea (OSA) is common and associated with significant morbidity and mortality. There are few objective prevalence data in Australia, particularly for women. In Busselton, Western Australia, the prevalence of OSA (respiratory disturbance index >15) was estimated in 1990 at 4.7% in men, and in 2007 (N=793) at 12.4% in men and 5.7% in women (apnea‐hypopnea index (AHI)>15 in participants without known OSA). We assessed OSA prevalence in the Busselton Healthy Ageing Study, a comprehensive health study of both sexes aged 46‐64 years.
Methods
Between 2010 and 2015, all residents on the Busselton Shire electoral roll born 1946 to 1964 were invited to participate, with 75% participance (N=5,082). Dual channel ApneaLink devices for home sleep study were issued to 3,745 participants (73.7%) and 2,707 (53.3%) collections were suitable for analysis. The prevalence of OSA was defined by the AHI obtained from the ApneaLink automated event scoring algorithm, and its relation to demographic data and co‐morbidities was assessed. Moderate and severe OSA were defined as AHI>15 and >30 respectively.
Results
The prevalence of OSA (AHI>15) 20.4% in men and 10.1% in women (see table). Increasing OSA severity was associated with increased BMI and alcohol use in both sexes, and with sleepiness in men only.
| Men | p | Women | P | |||||
|---|---|---|---|---|---|---|---|---|
| AHI | <15 | 15‐29.9 | ≥30 | <15 | 15‐29.9 | ≥30 | ||
| n (%) | 958 (79.6) | 183 (15.2) |
63 (5.2) |
1352 (90) | 121 (8.1) |
30 (2) |
||
| BMI, kg/m2 |
27.9 ±3.7(SD) |
29.7 ±4.4 | 31.3 ±5.3 | <0.001 | 27.7 ±5.2 | 31.1 ±6.5 | 32.3 ±8.5 | <0.001 |
| Alcohol, glasses/wk | 15.1 ±14.5 |
17.4 ±16.2 |
21.8 ±19.3 | <0.001 |
6.9 ±8.2 |
5.2 ±8.8 |
5.0 ±6.7 |
<0.001 |
| ESS | 6.0 ±3.7 | 6.6 ±4.1 | 7.2 ±4.0 | 0.01 | 5.6 ±3.7 | 6.2 ±3.8 | 5.9 ±3.5 | 0.165 |
Compared with AHI<15, an AHI>15 was associated with: hypertension in both sexes (p<0.001); with current depression in men only (20.3% vs 13.3%, p=0.005); and with diabetes (11.3% vs 5%, p=0.002) and cancer (22.5% vs 14.9%, p=0.014) in women only.
Conclusion
The prevalence of OSA in Busselton has increased, and the prevalence in women is higher than previously reported. Sex‐based differences in comorbidities are observed.
Grant Support: National Health and Medical Research Council (NHMRC); The Office of Science and Department of Health of the Government of Western Australia; in‐kind equipment and consumable support from ResMed Science Centre.
TO 081
CORTICAL CONTRIBUTION TO QUIET BREATHING IN COPD IS ASSOCIATED WITH AGEING
Hudson A1,2, Nguyen D1,2, Boswell‐Ruys C1,2,3, McBain R1,2,3, Eckert D1,2, Gandevia S1,2, Butler J1,2
1Neuroscience Research Australia, Randwick, Australia, 2University of New South Wales, Sydney, Australia, and 3Spinal Injuries Unit, Prince of Wales Hospital, Randwick, Australia
Introduction/Aim
Current evidence indicates that inspiratory loads engage cortical mechanisms to defend ventilation. A cortical contribution to breathing is determined via the presence of a Bereitschafts (readiness) potential – a low amplitude negativity which begins ~1s before inspiration. In chronic obstructive pulmonary disease (COPD), changes in the lung, chest wall and respiratory muscles induce an inspiratory load. We hypothesised that there is a cortical contribution to quiet breathing in COPD and that a cortical contribution to inspiratory threshold loading is related to dyspnoea – a major symptom of COPD.
Methods
Electroencephalographic activity (EEG) was recorded in 15 COPD patients (10 males; age: 57‐87) and 30 healthy controls (15 age‐matched and 15 young) during quiet breathing and inspiratory threshold loading (10% maximal inspiratory pressure). Two blinded observers evaluated the presence of Bereitschaftspotentials prior to inspiration from ensemble averages of 80 or more epochs of EEG at Cz and FCz. Dyspnoea was rated using a modified Borg scale.
Results
The incidence of a cortical contribution to quiet breathing was significantly greater in the COPD patients (7/15) than the young (0/15) (P < 0.01), but not the age‐matched (5/15) (P = 0.46), controls. A cortical contribution to inspiratory threshold loading was associated with higher Borg scores in the young (P < 0.05), but not the age‐matched controls (P = 0.25) or the COPD patients (P = 0.43).
Conclusion
This study provides evidence that age, rather than COPD, is associated with a cortical contribution to quiet breathing. A cortical contribution to inspiratory threshold loading may be associated with more severe dyspnoea, at least in healthy young people.
Grant Support: A.L. Hudson is supported by a Lung Foundation Australia/Boehringer Ingelheim COPD Research Fellowship.
TO 082
USE OF CLOUD BASED TECHNOLOGY TO OPTIMISE CPAP INITIATION IN OSA
Georgiou H1, Kee K1, Goldin J1
1Royal Melbourne Hospital, Melbourne, Australia
Introduction/Aim
Despite advances in technology of Continuous Positive Airway Pressure (CPAP) in the treatment of Obstructive Sleep Apnea (OSA) and well validated benefits in quality of life and health outcomes, long term adherence remains a major challenge. Remote access cloud based technology has become a standard feature of new CPAP devices. Currently, this feature may not be optimally utilised to improve compliance and patients' experience with CPAP.
We sought to determine whether, remote based assessment of CPAP usage at regular intervals with follow up telephone assessment could improve CPAP usage and Epworth sleepiness score (ESS) in patients commencing CPAP therapy for OSA through a well‐supported sleep service.
Methods
We sought to prospectively assess 50 consecutive patients commencing CPAP therapy for OSA. Each patient had CPAP usage remotely assessed at weeks 1, 3, 6 and 9 post commencement. Telephone assessment with a standardised questionnaire was carried out at each interval if CPAP usage was <4/hrs per night. CPAP usage and final ESS were compared to 50 consecutive retrospective controls. Current preliminary data includes 37 of target 50 patients in the intervention group.
Results
The mean age was 56.1±14.5 years (SD) vs 52.5±14.4, Body mass index (BMI) 37.0±9.1 vs 37.7±7.4 kg/m2, Apnea Hypopnea Index (AHI) 46.5±29.0 vs 46.2±29.0 events/hour and baseline ESS 8.8±5.3 vs 10.6±5.3 in control and intervention groups, respectively.
There was no significant difference in CPAP usage between control group and intervention group at 1week: 5.0±2.6 vs 4.4±2.7 hours (SD) (p=0.55); 3weeks: 4.8±2.6 vs 4.2±2.6 hours (p=0.49); 6weeks: 4.6±2.5 vs 4.4±2.8 hours (p=0.90); or 9weeks: 4.3±2.5 vs 5.2±2.8 hours (p=0.23), respectively. Additionally, there was no significant difference in change in ESS score ‐0.6±5.6 vs ‐2.7±4.3 (p=0.24), respectively.
Conclusion
Regular interval remote based assessment of CPAP usage in OSA, in addition to usual care, does not improve 2‐month CPAP usage or ESS.
Grant Support: Nil
TO 083
RETROSPECTIVE CASE‐CONTROLLED STUDY OF OBSTRUCTIVE SLEEP APNOEA IN DOWN SYNDROME
Sulaiman N1, Catcheside P1,2, McEvoy D1,2, Chai‐Coetzer C1,2
1Sleep Health Services, Southern Adelaide Local Health Network, Adelaide, Australia, and 2Flinders University, Bedford Park, Australia
Introduction/Aim
Down syndrome (DS) is associated with multiple health issues including obstructive sleep apnoea (OSA). Dysmorphic craniofacial features inherent to DS predispose to OSA. The aims of this study were to ascertain the prevalence and severity of OSA in DS adults and identify possible barriers/enablers to treatment by comparing demographic and polysomnography (PSG) indices, continuous positive airway pressure (CPAP) prescription rates and adherence in DS adults matched to a group of non‐DS adults referred for a sleep study at Repatriation General Hospital.
Methods
Data were collected from electronic and paper‐based records. DS patients with OSA were identified by case review and compared to a randomly selected matched gender, age (±3), body mass index (BMI) (±3kg/m2) and study date (±90 days) (ratio1:3). Between group comparisons were conducted using independent samples t‐tests and Mann‐Whitney U tests for continuous data and Fisher's or Chi2 tests for categorical variables.
Results
30 DS were matched with 58 non‐DS patients for gender, age (mean±SD 38.8±12.5 versus 41.4±12.4 years) and BMI (34.9±9.1 versus non‐DS 32.8±6.8 kg/m2). 28 (93%) DS had OSA compared to 32 (55%, p<0.001) non‐DS patients. 25 DS (92.8%) and 15 non‐DS (46.9%) patients with OSA were commenced on CPAP (p<0.001). DS had more severe OSA (total apnoea hypopnoea index 56.4[28‐73.8] (median [IQR]) versus controls 15.5[4.4‐17.6]). CPAP adherence at 6 months: average hours use DS 4.6±0.7 (mean±SEM) versus controls 6.4±0.6 in controls (p=0.044). There was similar intensity of follow up visits in the first year after CPAP initiation: DS 5.0±0.5 (mean±SEM) versus controls 4.1±0.6 (p=0.288). DS patients with higher intensity of supervision overnight had better CPAP compliance.
Conclusion
DS patients had significantly more severe OSA but reduced CPAP adherence. Further research is required to elucidate barriers to treatment and potential solutions to improve CPAP compliance amongst DS patient with OSA.
Grant Support: Nil.
Declaration of Interest: Nil
TO 084
ARTIFICIAL INTELLIGENCE HELPS DETECTING LUNG DISEASE WITH PULMONARY FUNCTION TESTS
Topalovic M1, Das N1, Troosters T1, Decramer M1, Janssens W1
1KU Leuven, Leuven, Belgium
Introduction/Aim
Pulmonary function testing (PFT) is a main tool to evaluate the function of the respiratory system. However, used alone, it hardly leads to disease diagnosis. Based on artificial intelligence (AI) we aimed to develop a smart software which improves the clinical reading of a lung function and suggests a respiratory disease diagnosis if possible.
Methods
Data of 1430 subjects with respiratory symptoms were taken from 33 Belgian hospitals to develop the algorithm. The final diagnosis (healthy, asthma, COPD, ILD, neuromuscular disease, chest wall or pleural disease, pulmonary vascular disease, other obstructive disease) was obtained from clinical history, lung function and all additional tests, and confirmed by an expert panel. A cloud‐based solution was incorporated into clinical setting to validate the accuracy of the algorithm on a random sample of 136 new subjects. Finally, the software diagnoses were compared with the diagnostic opinions of 85 pulmonologists (from 11 different European hospitals) provided with PFT and clinical data of 50 new subjects.
Results
At development, software presented a high accuracy of 74% after 10‐fold cross‐validation when detecting lung diseases (8 possible disease categories). During validation, the high accuracy was maintained in a real clinical setting (76%). At the external multicentric validation, the software‐based automated diagnoses (82% accuracy) were superior over the suggested diagnoses of 85 pulmonologists (44.6 ± 3.7 % mean accuracy). Great disagreement between readers is observed with a low kappa score of 0.34.
Conclusion
AI can be used to identify different lung diseases. Due to its superiority and work consistency, such software can provide a powerful decision support system in daily clinical routine.
Grant Support: VLAIO Flanders
TO 085
THE ASSOCIATION BETWEEN REGIONAL LUNG DISTENSION AND GENE EXPRESSION DURING MECHANICAL VENTILATION
Yen S1, Preissner M2, Bennett E1, Fouras A2, Dargaville P1,3,4, Zosky G1
1School of Medicine, University of Tasmania, Hobart, Australia, 24Dx Limited, Melbourne, Australia, 3Neonatal and Paediatric Intensive Care Unit, Royal Hobart Hospital, Hobart, Australia, and 4Menzies Institute for Medical Research, University of Tasmania, Hobart, Australia
Introduction/Aim
Mechanical ventilation, a lifesaving therapy for patients with respiratory failure, contributes to mortality by inducing inflammation, which can lead to multisystem organ failure. Different regions of the lung have been shown to heterogeneously respond to mechanical ventilation, however, the association between this variation in regional lung distension and regional lung inflammation is unknown. The aim of this study was to assess this association in the healthy lung.
Methods
We ventilated two groups of adult BALB/c mice (n = 8 per group) for 2 h using a protective [low tidal volume with moderate positive end expiratory pressure (PEEP)] or injurious [high tidal volume with zero PEEP] ventilation strategy. RNA levels of 19 genes were quantified regionally by qPCR array. Gene expression was correlated with regional FRC, tidal volume and distension (FRC + tidal volume). FRC and tidal volume were obtained from analysis (cross‐correlation‐based velocimetry) of dynamic high‐resolution (phase contrast) 4DCT lung images at baseline and after two hours of ventilation.
Results
Two genes had differential regional expression that varied between ventilation strategies (IL‐6, P=0.02 and Ccl‐2, P<0.01). The expression of these genes was positively correlated with regional tidal volume and distension (P<0.05 for all correlations). The expression of Cxcl2, Tnf‐α, Wnt1, c‐fos and Nfe2l2 also varied between ventilation strategies (P<0.01), but they did not appear to be associated with FRC, tidal volume or distension.
Conclusion
We have demonstrated associations between regional gene expression and tidal volume. Our results provide critical insight into the regional lung response to mechanical ventilation. In particular, these results highlight the importance of the balance between under‐ventilation and over‐stretch (tidal volume) and how each of these can contribute to lung inflammation and, potentially, patient outcomes.
Grant Support: This study is funded by NHMRC grant # 1077905
Asthma & Allergy 3
TO 086
ORAL CORTICOSTEROID USE IN ASTHMA PATIENTS: AN EASY WAY OUT
Bradbury T1,2, Azzi E1,2, Srour P1,2, Armour C1,2,3, Kritikos V1,2,3, Bosnic‐Anticevich S1,2,3
1Woolcock Institute of Medical Research, Glebe, Australia, 2The University of Sydney, Sydney, Australia, and 3Sydney Local Health District, Sydney, Australia
Introduction/Aim
Although significant progress has been made in asthma management, 5‐10% of patients have severe asthma (SA) that is associated with increased morbidity, mortality and an economic burden. Within this group, 30‐40% of patients are prescribed continuous or near‐continuous oral corticosteroids (OCS) to achieve or maintain asthma control. However, in primary care, a subset of these patients may exist with poor asthma management practices and thus less severe disease, relying on OCS to achieve asthma control instead of regular inhaled preventer medication. The aim of this study is to identify patterns of medication taking behaviour and describe the respiratory status of people with asthma in primary care. This will allow for the development of a framework that identifies patients based on asthma severity through medication records.
Methods
Patient data (n=493) was utilised from a quality‐controlled community pharmacy database. Correlational analysis and regression modelling were employed to determine potential predictors of asthmatic oral corticosteroid users (n=72) based on asthma severity, lung function, symptom control, comorbidities, adherence, inhaler technique and medication management.
Results
Fifteen percent of asthmatics recruited were prescribed OCS in the last 12 months. Ninety‐three percent of OCS users were classified as having poor asthma control, 96% identified potential barriers to non‐adherence (determined by the Brief Medication Questionnaire (Svarstad BL et al. 1999)), and 86% had incorrect inhaler technique. Significant relationships were found between OCS users and ownership of an asthma action plan (p<0.00), the existence of depression (p=0.002) and eczema (p=0.02), potential for non‐adherence (p=0.018), poor asthma control (p<0.00), poor lung function test (p=0.04) and a higher prescribed rate of inhaled combination therapy (p<0.000), including a higher rate of visits to the doctor regarding asthma (p=0.044).
Conclusion
This research has uncovered a heterogeneous group of people with asthma in primary care, with less severe disease who put themselves at risk of exacerbations due to their medication taking behaviour. By better understanding the behaviour of individuals in the context of their day‐to‐day management, we will be able to tailor interventions for these patients reflecting current guidelines.
REFERENCE
Svarstad, B. L. et al. The brief medication questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ. Couns. 37, 113–124 (1999).
TO 087
WORKING WHILE UNWELL: WORKPLACE IMPAIRMENT IN PEOPLE WITH SEVERE ASTHMA
Hiles S1, Harvey E2,3, McDonald V1,2,3, SAWD Investigators3, Gibson P1,2,3
1Centre of Excellence in Severe Asthma, Faculty of Health, University of Newcastle, New Lambton Heights, Australia, 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, Hunter Medical Research Institute, University of Newcastle, New Lambton Heights, Australia, and 3Australasian Severe Asthma Network, New Lambton Heights/Glebe, Australia
Introduction/Aim
Severe asthma substantially impairs quality of life and may impair workplace productivity, although this has rarely been quantified. The aim of this study was to compare workplace impairment in severe and non‐severe asthma over time, and identify characteristics associated with presenteeism in severe asthma.
Methods
Patients were enrolled in the Severe Asthma Web‐based Database (SAWD), an ongoing observational registry of 434 patients with severe refractory asthma and 102 with non‐severe controlled asthma from 26 sites across Australia, New Zealand and Singapore (18 to 88 years; 59% female). Participants provided baseline clinical and questionnaire data and were followed‐up every 6 months until 24 months. Workplace absenteeism (% time absent from work), presenteeism (% self‐reported impairment at work) and activity impairment (% self‐reported impairment in daily activities outside work) in the past week were derived from a validated questionnaire.1
Results
Half of participants were employed at baseline. A quarter of workers reported absenteeism and two‐thirds reported presenteeism. People with severe compared with non‐severe asthma were 3.15 times more likely to report presenteeism (95%CI 1.75‐5.69) and 2.26 times more likely to report daily activity impairment (95%CI 1.44‐5.54). Having poorer asthma control or more exacerbations in the previous year was associated with greater absenteeism, presenteeism and activity impairment (all p<0.05). Worsening asthma control scores were associated with increasing presenteeism over time (time interaction p=0.011). In participants with severe asthma, worse asthma control (p<0.001), asthma‐related quality of life (p<0.001), depression symptoms (p=0.001) and anxiety symptoms (p=0.002) were associated with greater odds of presenteeism.
Conclusion
Impaired work and non‐work functioning are important components of the disease burden of severe asthma. Optimising workplace productivity requires improvement in asthma control and attention to mental health. Absenteeism and presenteeism may be key metrics for assessing intervention efficacy among people with severe asthma of working age.
Grant Support: SAWD is supported by GSK, Roche, AZ, Novartis and Boehringer Ingelheim.
REFERENCES
1 Reilly et al, 1993, PharmacoEconomics, 4:353‐365.
TO 088
CASEIN KINASE 1DELTA/EPSILON: A NOVEL PATHWAY SENSITIZING GLUCOCORTICOID ACTIVITY
Li M1, Keenan C1, Xia Y1, Langenbach S1, Harris T1, Stewart A1
1Department of Pharmacology and Therapeutics; University of Melbourne, Melbourne, Australia
Introduction/Aim
Glucocorticoids (GCs) remain central to treatment of asthma, but therapeutic responses are impaired in severe asthma and during asthma exacerbation. Our laboratory found TGF‐β1 per se impairs GC activity, and is a key mediator of viral infection‐induced GC insensitivity in airway epithelium. The key CLOCK component CK1δ/ε, implicated in TGF‐β1 signalling, also regulates GCs activity. In the current study, we demonstrate that targeting CK1δ/ε prevents TGF‐β1‐indcued GC insensitivity, and attenuates virus mimic Poly (I:C)‐induced inflammatory responses.
Methods
Differential expression of CK1δ/ε was assessed by IHC in human asthmatic cohort. GC responsiveness of bronchial epithelial cells (BEAS‐2B, air‐liquid interface (ALI)‐differentiated primary human bronchial epithelial cells (HBEC)) in the presence of TGF‐β1 was assessed by RT‐qPCR and GRE‐SEAP. Poly (I:C)/TNF‐α‐induced inflammatory responses in BEAS‐2B cells was assessed by ELISA. The potential involvement of CK1δ/ε in the above experimental settings was determined using pharmacological (PF670462) and genetic (siRNA) approaches.
Results
CK1δ expression was significantly higher in the airway wall of severe asthmatics compared to well‐controlled asthma and healthy subjects. In BEAS‐2B cells and ALI‐HBECs, TGF‐β1 suppression of GC‐induced GRE activity and endogenous gene expression was prevented by CK1δ/ε (3μM PF670462). Poly (I:C)/TNF‐α‐induced pro‐inflammatory cytokines (IL‐6, IL‐8 and GM‐CSF) were attenuated by inhibition of CK1δ/ε using 3μM PF670462 and CK1δ/ε‐targeting siRNAs.
Conclusion
We have identified CK1δ/ε as a novel target with therapeutic potential to restore anti‐inflammatory efficacy of GCs in severe asthma and asthma exacerbation.
Grant Support: NHMRC, Asthma Australia
TO 089
A SPUTUM SIX GENE SIGNATURE PREDICTS INFLAMMATORY AND EXACERBATION PHENOTYPES IN UNCONTROLLED MODERATE‐TO‐SEVERE ASTHMA: AN AMAZES SUB‐ANALYSIS
Fricker M1, Powell H1, Gibson P1, Baines K1
1University of Newcastle, Newcastle, Australia
Introduction/Aim
Improved diagnostic tools for predicting airway inflammatory phenotype and future exacerbation frequency in asthma are required. We previously demonstrated a sputum gene expression signature of 6 biomarkers (6GS) could predict inflammatory phenotype and corticosteroid responsiveness in stable asthma. We recently demonstrated that azithromycin add‐on treatment in uncontrolled moderate‐to‐severe asthma significantly reduced asthma exacerbations (AMAZES clinical trial). We aimed to test whether the 6GS predicts airway inflammatory and future exacerbation phenotypes in a subpopulation of the AMAZES clinical trial. We also tested whether 48 weeks of azithromycin treatment altered 6GS expression compared to placebo.
Methods
142 patients (73 placebo‐treated, 69 azithromycin‐treated) produced adequate sputum for differential cell count and PCR of 6GS markers at baseline and after 48 weeks of treatment. Logistic regression and ROC analysis was performed on baseline results to compare the predictive value of 6GS and conventional biomarkers for airway inflammatory phenotype and future exacerbation frequency.
Results
The 6GS significantly predicted airway inflammatory subtype at baseline, outperforming systemic biomarkers peripheral blood eosinophils (PBE) and fractional exhaled nitric oxide (FENO). 6GS significantly predicted future exacerbation phenotype, was numerically superior to all biomarkers examined (sputum eosinophils, sputum neutrophils, PBE and FENO), and identified patients who would go on to experience frequent (≥ 2/year) severe exacerbations. Azithromycin treatment did not significantly alter 6GS expression compared to placebo, nor did it affect the prediction of exacerbation phenotype using the 6GS.
Conclusion
The sputum 6GS is useful as a diagnostic tool for inflammatory phenotyping and predicting future frequent severe exacerbations. The 6GS retains this predictive capacity in azithromycin‐treated asthma, suggesting a novel therapeutic mechanism independent of known exacerbation‐associated inflammatory factors.
Grant Support: Work supported by the NHMRC. MF holds an NHMRC post‐doctoral research fellowship within the CRE in Severe Asthma. PGG holds an NHMRC practitioner fellowship. KJB holds a Lung Foundation Australia Boehringer Ingelheim COPD research fellowship.
TO 090
THE EFFECT OF TREATMENT WITH OMALIZUMAB ON ANTIVIRAL RESPONSES IN ADULTS WITH SEVERE ALLERGIC ASTHMA
Wark P1,2, Nichol K1, Dorahy D1, Collison A3, Mattes J3
1Centre for Healthy Lungs, HMRI, University of Newcastle, New Lambton, Australia, 2Department of Respiratory and Sleep Medicine John Hunter Hospital, New Lambton, Australia, and 3Centre for Growing Up Well, HMRI, University of Newcastle, New Lambton, Australia
Introduction/Aim
Severe asthma is characterised by frequent exacerbations, that lead to poor asthma control and worsened quality of life. Tthe majority of these exacerbations are triggered by viral respiratory tract infections. Poorly controlled asthma is associated with impaired antiviral immune responses. Treatment of severe allergic asthma with Omalizumab, a monoclonal antibody against IgE, has been shown to improve asthma control and reduce exacerbation risk. We sought to determine if treatment with Omalizumab resulted in improvement in antiviral innate immune responses to influenza A (IAV) and rhinovirus (RV).
Methods
We recruited 10 adults, with poorly controlled allergic asthma; atopic to one or more aeroallergens, on maximal dose inhaled corticosteroid/ long acting bronchodilators, with persisting poor asthma symptom control, exacerbations requiring oral corticosteroids and a serum total IgE >30IU/ml. They were compared to healthy aged matched controls with no asthma or atopy. Participants were assessed prior to commencing treatment with Omalizumab and then 6 months later at the time effectiveness of treatment was assessed. Blood was drawn and peripheral blood monocytes (PBMCs) were isolated. PBMCs were then exposed for 48 hours to IAV, and RV.. Response was assessed by ELISA/bead arraywith release of interferon (IFN)‐α, IFN‐λ, IFN‐γ, IL‐6, IL‐10, IL‐5 and IL‐13.
Results
At baseline visit subjects with severe allergic asthma compared to healthy controls demonstrated impaired IFN‐α, and IFN‐λ release in response to IAV (p<0.001) and RV (p=0.003). Following 6 months treatment, 9/10 demonstrated an improvement in asthma symptom control to continue treatment. In the clinical responders there was a significant increase seen in IFN‐α, and IFN‐λ to IAV and a trend towards improvement to RV.
Conclusion
Adults with severe allergic asthma demonstrate impaired systemic innate immune responses to IAV and RV. Treatment with Omalizumab, that results in improved asthma control is associated with improvement in innate antiviral responses.
Grant Support:
TO 091
SEVERE ASTHMA TREATABLE TRAITS: PREVALENCE AND EXACERBATION PREDICTION
McDonald V1,2,3, Godbout K2,4, Hiles S1, Harvey E1,3, SAWD Investigators S3, Gibson P1,2,3
1Centre of Excellence in Severe Asthma, Faculty of Health, University of Newcastle, Newcastle, Australia, 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, New Lambton Heights, Australia, 3Australasian Severe Asthma Network, New Lambton Heights/Glebe, Australia, and 4Institut universitaire de cardiologie et de pneumologie de Québec, Université Laval, Québec, Canada
Introduction/Aim
Treatable traits (TT) have been proposed as a new approach for airway disease management, however supporting data are currently limited. We aimed to determine if identification of TT is possible using a severe asthma registry, to assess their prevalence in severe compared to non‐severe asthma, and to assess the relationship between TT and future exacerbation risk.
Methods
The Severe Asthma Web‐based Database is an observational registry of 434 severe asthma patients and a comparison group of 102 patients with non‐severe asthma from 26 sites in Australasia (18‐88 years, 59% female). Participants were characterised at enrolment and followed for 24 months. Published traits1,2 were mapped to registry data fields and prevalence determined. Bayesian model averaging was applied to identify traits that best predicted future exacerbation risk.
Results
Seven pulmonary, 13 extrapulmonary and 4 behavioural risk‐factor traits were identified. More pulmonary and extrapulmonary traits were expressed in severe than non‐severe asthma (p<0.001). Traits significantly more common in severe asthma were incompletely reversible airflow limitation (58% vs. 39%, p=0.002), frequent exacerbations (51% vs 6%, p<0.001), neutrophilic airway inflammation (23% vs 4%, p=0.023), obesity (49% vs 27%, p<0.001), systemic inflammation (41% vs 13%, p<0.001), reflux (49% vs. 36%, p=0.021), inhaler‐device polypharmacy (29% vs. 18%, p=0.018) and Aspergillus sensitisation (39% vs 19%, p<0.001). During follow‐up, patients with severe asthma reported more exacerbations (median [IQR]: 2 [0‐4]) than non‐severe (0 [0‐2]; IRR 2.33, p<0.001). Each additional trait was associated with a 13% increase in exacerbation risk (p<0.001). Previous exacerbations, inhaler‐device polypharmacy, sleep apnea and depression best predicted exacerbation risk.
Conclusion
A registry‐based systematic characterisation of asthma may be used to assess TT. We report traits that predict exacerbation risk and confirm greater burden associated with severe asthma. Trials evaluating the efficacy and cost‐effectiveness of the TT approach are needed.
1. Gibson etal, Lancet, 2010, 376:803‐813
2. Agusti etal, ERJ, 2016, 47:410‐419.
Grant Support: SAWD is supported by GSK, Roche, AZ, Novartis and Boehringer Ingelheim.
Cell, Immunology & Molecular Biology of the Lung 2
TO 092
THE UNFOLDED PROTEIN RESPONSE VARIES BETWEEN INFLAMMATORY PHENOTYPES OF ASTHMA
Pathinayake P1, Nichol K1, Baines K1, Wood L1, Hsu A1, Wark P1,2
1Priority Research Centre for Healthy Lungs, University of Newcastle and Hunter Medical Research Institute, Australia, and 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, Australia
Introduction/Aim
Asthma is a chronic inflammatory airway disease which is characterized by recurrent attacks of breathlessness and wheezing. The pathogenesis of asthma is complex and still unclear. The unfolded protein response (UPR) of the endoplasmic reticulum (ER) has recently been identified as playing a decisive role in inflammatory diseases. Worsening of asthmatic condition can be brought on by stimuli such as oxidative stress, pathogenic infection, and allergen exposure. All of which can induce ER stress and activate UPR. Activated arms of UPR induce different inflammatory pathways and dysregulate the innate immune response. However, how UPR is associated with asthma is unclear. Here we investigate the UPR signature in different inflammatory phenotypes of asthma using human clinical samples.
Methods
Broncho alveolar lavage fluid (BALF), endobronchial biopsies and induced sputum samples were collected from eosinophilic, neutrophilic, paucigranulocytic asthma patients, and from healthy individuals. The expression of UPR associated genes in BALF cells, and biopsy samples were analysed by qPCR. UPR related protein expressions was analysed by immunoblot. UPR gene expression in sputum cells were analysed by microarray.
Results
UPR genes (GRP78, CHOP, XBP1s, and PDIA4) in lung immune cells were significantly induced (p<0.05) in eosinophilic asthma while neutrophilic asthma demonstrated an increased trend. GRP78 and CHOP protein expression were significantly higher in both eosinophilic and neutrophilic groups. Microarray data from sputum cells demonstrated an upregulation of various UPR genes mostly in the eosinophilic asthma group, but not in paucigranulocytic or mixed granulocytic groups. UPR gene expression in lung biopsies did not show significant differences between groups. However, bronchial epithelial cells (BECs) treated with asthma allergens demonstrated an increased trend of UPR.
Conclusion
UPR is heightened in eosinophilic and neutrophilic asthma. Airway immune cells have a major role in regulating UPR in airways of asthma.
TO 093
PLASMA CELL AND REGULATORY B CELL‐INFILTRATION IN THE LUNGS OF BLEOMYCIN‐TREATED MICE
Prele C1,2, Pearce D3, Miles T1,2, O'Donoghue R4, Lucas A2, Fear M5, Ernst M4, Laurent G1,2, Knight D6, Hoyne G7, McAnulty R3, Mutsaers S1,2
1Institute for Respiratory Health, The University of Western Australia, Perth, Australia, 2Centre for Cell Therapy and Regenerative Medicine, School of Biomedical Sciences, The University of Western Australia , Perth, Australia, 3Centre for inflammation and Tissue Repair, Division of Medicine, University College London, London, UK, 4Olivia Newton John Cancer Research Institute and La Trobe University School of Cancer Medicine, Heidleberg, Australia, 5Burn Injury Research Unit, School of Biomedical Sciences, The University of Western Australia, Perth, Australia, 6The University of Newcastle, Callaghan, Australia, and 7The University of Notre Dame, Perth, Australia
Introduction
STAT3 and B cells are implicated in the development of lung fibrosis. We have previously demonstrated that hyper‐activated STAT3, B cell‐deficient gp130757F;μMT‐/‐ mice are protected from bleomycin (BLM)‐induced lung fibrosis suggesting that B cells are important in the regulation of STAT3‐mediated fibrosis.
Hypothesis
We hypothesise that the pro‐fibrotic effects of STAT3 involve B cell‐mediated immune regulation.
Methods
The effect of anti‐CD20 therapy in bleomycin‐treated wildtype and gp130757F mice on lung fibrosis and immune cell composition was examined. Mice were given two 100μg doses of anti‐CD20 antibody (Genentech Inc USA) or IgG2a isotype control i.p. either 7 days prior to and 7 days after bleomycin or on day 10 and day 19 post‐bleomycin treatment (following the initiation of fibrosis), and the extent of fibrosis measured at 28 days.
Results
FACS analysis of blood taken on days 0, 7 and 28 days post‐bleomycin‐treatment revealed an almost complete depletion of CD19+ B cells in the circulation of wildtype mice but not gp130757F. However, the extent of fibrosis, assessed using micro‐CT imaging and HPLC analysis of hydroxyproline levels was not significantly different between treatment groups. Histological analysis revealed an abundance of CD5+ B cells and CD138+ (plasma cells) in the lungs of the anti‐CD20‐treated mice. FACS analysis identified an expansion of CD138+ (days 7 and 28) and CD5+ cells in the lungs of bleomycin treated mice at day 28.
Conclusion
Although antibody depletion of follicular B cells had no effect on bleomycin‐induced fibrosis, residual CD138+ plasma cells and CD5+ B are abundant in the lungs of bleomycin‐treated mice. The activity of these B cell subsets may contribute to the fibrotic phenotype.
Grant Support: This work is funded by NHMRC Project Grant GNT1067511 and British Lung Foundation Grant PPRG15‐10.
TO 094
THE EFFECT OF THE DIETARY ω‐6 POLYUNSATURATED FATTY ACID, ARACHIDONIC ACID, ON AIRWAY INFLAMMATION AND REMODELING IN COPD
Rutting S1, Papanicolaou M1, Xenaki D1, Wood L3, Horvat J2, Hansbro P2, Oliver B1,4,5
1Woolcock Institute of Medical Research, Sydney, Australia, 2Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and University of Newcastle, Newcastle, Australia, 3School of Biomedical Science and Pharmacy, The University of Newcastle, Newcastle, Australia, 4School of Medical and Molecular Biosciences, University of Technology, Sydney, Australia, and 5Emphysema Centre, Woolcock Institute , Sydney, Australia
Introduction/Aim
Obesity appears to have protective effects on lung pathology and inflammatory responses in COPD, however, the underlying relationships between obesity, diet and disease outcomes in COPD are not fully understood. This study explored the relationship between the dietary ω‐6 polyunsaturated fatty acid (PUFA) arachidonic acid (AA) and airway inflammation and remodeling, in primary human pulmonary fibroblasts in vitro from people with and without COPD. Also, the effect of body mass index (BMI) on the inflammatory response was assessed.
Methods
Primary human lung fibroblasts derived from COPD patients and non‐COPD patients were challenged with BSA‐conjugated AA for 48hr. Release of the pro‐inflammatory cytokines, IL‐6 and CXCL8, was measured using ELISA. Messenger RNA (mRNA) expression of the extracellular matrix (ECM) proteins, fibronectin (FN), collagen I (COL I) and tenascin (TNC) was measured using quantitative PCR.
Results
We found that challenge with AA results in increased IL‐6 and CXCL8 release from fibroblasts, however IL‐6 (p<0.001) and CXCL8 (p<0.05) release in COPD (n=12) was lower compared to non‐COPD (n=24). Regression analysis revealed no relationship between BMI and cytokine release in COPD. AA reduced basal FN (P<0.01) and COL I (P<0.05) mRNA expression in fibroblasts from COPD patients (n=5).
Conclusion
This study demonstrates that AA, commonly found in obese diets, affects inflammatory processes and ECM deposition in COPD. COPD cells compared to non‐COPD cells are hyporesponsive to AA, suggesting that in COPD meals rich in ω‐6 PUFAs are not as potent in the induction of inflammatory responses compared to other lung diseases. However, the reduced capacity to produce ECM proteins could negatively affect healing processes which is likely to manifest as perturbed and excessive tissue remodeling in COPD.
TO 095
LYMPHOCYTE SENESCENCE IN COPD IS ASSOCIATED WITH DECREASED SIRT1 EXPRESSION IN STEROID RESISTANT PRO‐INFLAMMATORY LYMPHOCYTES
Hodge G1,2, Jersmann H1,2, Holmes M1,2, Reynolds P1,2, Hodge S1,2
1Royal Adelaide Hospital, Adelaide, South Australia, Australia, 2Department of Medicione, University of Adelaide, Adelaide, South Australia, Australia
Introduction
Class III NAD‐dependent histone deacetylase (HDAC) sirtuin 1 (SIRT1) is an important regulator of senescence, aging and inflammation through de‐acetylation of chromatin histones thereby silencing inflammatory gene transcription. We have reported increased steroid resistant senescent pro‐inflammatory CD28nullCD8+ T cells in patients with COPD. We hypothesized that expression of SIRT1 would be reduced in these cells in COPD and that treatment with SIRT1 activators (resveratrol) and agents that prevent NAD depletion (theophylline) would upregulate SIRT1 expression and reduce pro‐inflammatory cytokine expression in these steroid resistant cells.
Methods
Blood was collected from COPD patients and aged matched controls and expression of CD28, SIRT1 and pro‐inflammatory cytokines determined in CD8+ and CD8‐ T and NKT‐like cells cultured in the presence of ± 1μM resveratrol ± 5.0mg/mL theophylline ± 1 μM prednisolone using flow cytometry.
Results
Decreased SIRT1 expression was identified in CD28nullCD8+T and NKT‐like cells compared with CD28+ counterparts from both patients and controls (eg., CD28null 7±3% vs. CD28+ 55±5%). Loss of SIRT1 was associated with increased production of IFNγ and TNFα and steroid resistance. SIRT1 expression was upregulated in the presence of 1μM resveratrol and 5.0mg/mL theophylline and was associated with a decrease in steroid resistance and IFNγ and TNFα production by CD28nullCD8+T and NKT‐like cells.
Conclusion
Steroid resistance in pro‐inflammatory CD28nullCD8+ T and NKT‐like cells is associated with decreased SIRT1 expression. Combination resveratrol and/or theophylline treatment increases SIRT1 expression, restores steroid sensitivity and inhibits pro‐inflammatory cytokine production from these cells and may reduce systemic inflammation in COPD.
Grant Support:
TO 096
ESTROGEN AFFECT THE IMMUNE SYSTEM AND LEADS TO MORE SEVERE ASTHMA IN FEMALES
Leffler J1, Lauzon‐Joset J1, Abad A1, Short B1, Holt P1, Stumbles P1,2,3, Strickland D1
1Telethon Kids Institute, Subiaco, Western Australia, Australia, 2School of Veterinary and Life Sciences, Murdoch University, Murdoch, Western Australia, Australia, and 3School of Paediatrics and Child Health, The University of Western Australia, Perth, Western Australia, Australia
Introduction/Aim
Women have a higher incidence of asthma compared to men and exacerbations in women are often more severe and correlate with high estrogen levels. Using an experimental animal model for asthma, we have observed that female rats with experimental asthma also develop more severe exacerbations compared to male rats. The aim of the study was to investigate if the female sex hormone estrogen can impact the asthma response and identify the immunological mechanism for this effect.
Methods
By implanting estrogen‐releasing pellets into male rats prior to ovalbumin‐sensitisation and re‐challenge we investigated how estrogen‐exposed males responded compared to untreated males and females. We used multi parameter flow cytometry to investigate proportion and activation of antigen presenting dendritic cells, responding T effector and regulatory T cells in airways before and after allergen re‐challenge.
Results
We discovered that estrogen was sufficient to induce a female‐like disease phenotype during exacerbations in male rats. Interestingly, male and female rats also displayed significant differences in CD4+/CD8+ T cell ratios in airway draining lymph nodes and this was directly impacted by estrogen exposure. In addition, female and estrogen treated male rats, but not male rats, displayed signs of recruitment of CD4+ cells into the airways following allergen re‐challenge which most likely contributed to the exacerbated response.
Conclusion
Our data suggest that estrogen is sufficient to induce female like asthma symptoms in male rats and appears to alter the T cell balance promoting allergic responses.
Grant Support: The study was funded by the Asthma Foundation of Western Australia, the Telethon Kids Institute and the Swedish Society for Medical Research.
TO 097
PERSONALIZED CELL CULTURE MODEL FOR HIGH‐THROUGHPUT SCREENING FOLLOWING CFTR CORRECTION
Looi K1, Garratt L1, Sutanto E1,2, Kicic A1,2,3,4, Stick S1,2,3,4, AREST C F1,2,5,6
1Telethon Kids Institute, Subiaco, Perth, Australia, 2Department of Respiratory Medicine, Princess Margaret Hospital for Children, Subiaco, Perth, Australia, 3School of Paediatrics and Child Health, The University of Western Australia, Nedlands, Perth, Australia, 4Centre for Cell Therapy and Regenerative Medicine, School of Medicine and Pharmacology, The University of Western Australia, Nedlands, Perth, Australia, 5Department of Respiratory Medicine, Royal Children's Hospital, Melbourne, Australia, and 6Murdoch Children's Research Institute, Melbourne, Australia
Introduction and Aims
Small molecules can correct CFTR production or function and greatly improve CF outcomes. Rarer mutations are hindered by the lack of appropriate primary culture models. Modifying primary airway epithelial cells (AECs) from children with CF modified to express a fluorescence marker that allows functional CFTR assessment would provide a culture‐based high‐throughput screening platform. We compared methodologies to achieve stable fluorescence in primary AEC.
Methods
Primary AECs were obtained from children (CF and non‐CF) by bronchial brushing and cultured using a conditional reprogramming methodology. Cells were transfected with a pcDNA3.1 plasmid via Lipofectamine® or Nucleofector™ device. Alternatively, AEC were transduced by a replication‐deficient retroviral vector with fluorescent tag. After 48 hours, cells expressing fluorescence were selected by fluorescence activated cell sorting (FACS) flow cytometry and then expanded further in culture to assess stability of gene expression.
Results
Primary AECs were amenable to all three methodologies. Transfection by Lipofectamine® was 24.1% efficient and the best electroporation protocol achieved a slightly higher efficiency (30.0%). Replication deficient retrovirus was most effective with 78.9% positive cells. There was no difference in transfection efficiency observed between non‐CF and CF AECs. Cells could be successfully cultured after FACS selection, but only AEC transduced by retroviral vector maintained their fluorescence through two passages of cultures.
Conclusion
Retroviral vector could stably induce fluorescence into primary AECs. We are constructing a retroviral vector containing the YFP gene and validating the CFTR functional assay across a range of CFTR mutations.
Grant Support: BHP Billiton Telethon Kids Institute Blue Sky Research Grant
Chronic Obstructive Pulmonary Disease (COPD) 2
TO 098
MANAGEMENT OF ACUTE COPD EXACERBATIONS: DO WE FOLLOW THE GUIDELINES?
Cousins J1, Wood‐Baker R2, Wark P3, Yang I4, Hutchinson A5, Sajkov D6, Gibson P3, McDonald V1,3
1School of Nursing and Midwifery, The University of Newcastle; Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute, New Lambton, Australia, 2School of Medicine, University of Tasmania, Hobart, Australia, 3School of Medicine and Public Health, The University of Newcastle; Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute; Department of Respiratory and Sleep Medicine, Hunter Medical Research Institute, John Hunter Hospital , New Lambton, Australia, 4The Prince Charles Hospital and University of Queensland, Brisbane, Australia, 5School of Nursing and Midwifery, Deakin University, Geelong, Australia, and 6Australian Respiratory and Sleep Medicine Institute, Flinders University and Flinders Medical Centre, Bedford Park, Australia
Introduction/Aim
Chronic Obstructive Pulmonary Disease (COPD) is the second leading cause of avoidable hospital admission in Australia, but to date no national data exists that compares the recommendations of clinical practice guidelines for inpatient management of acute exacerbations against actual practice. We aimed to compare contemporary management against the recommendations of the COPD‐X guidelines.
Methods
A prospective audit of COPD hospital admissions from five tertiary care hospitals in five states in Australia was conducted. A standardised audit tool was used to collect data. Telephone follow‐up at 28 days after discharge assessed readmission and health‐status. Data were assessed against the COPD‐X guidelines.
Results
Prospective data were obtained for 207 admissions in 171 patients between October 2012–April 2013. The mean±SD age was 70.2±9.9 years, 50.3% were male, and 95.3% caucasian. The mean number of comorbidities per patient was 3.6±1.9, with hypertension (48.5%), gastrointestinal disease (37.5%), ischaemic heart disease (28.5%), psychiatric/anxiety/depression disorders (28.1%) the most prevalent. Over half were ex‐smokers (58.6%) and lived at home with another (56.2%). Of the 171 patients, 21.1% were readmitted within 28 days, there were 2 inpatients deaths (1.2%), and a further 9 deaths (5.3%) within 28 days of discharge.
Concordance to the COPD‐X recommendations varied. Prescription of oral corticosteroids (95.1% [inter‐hospital range 90‐100%]), antibiotic therapy (89.2% [42.9‐94.9%]), and performance of chest x‐ray (99.5% [87.5‐100%]) was high. However, performance of spirometry 22.3% (range 0‐52.4%), written inpatient prescription of acute oxygen therapy 27% (range 3.2‐76.9%), and referral to pulmonary rehabilitation 29.1% (range 10.3‐50.8%) were poor.
Conclusion
Important gaps in management were seen nationally when compared against clinical practice guidelines.
Grant Support: Nil
Declaration of Interest: We declare that we have no conflicts of interest related to the above project.
TO 099
ASSOCIATIONS OF TYPE‐SPECIFIC PHYSICAL ACTIVITY WITH MORTALITY RISK IN COPD
Cheng S1, McKeough Z1, Alison J1, Dennis S1, Hamer M2, Stamatakis E1
1The University of Sydney, Sydney, Australia, and 2University of Loughborough, Loughborough, UK
Introduction/Aim
To examine the dose‐response associations between specific types of physical activity (PA) and mortality risk in people with chronic obstructive pulmonary disease (COPD).
Methods
A prospective cohort study was used. People with COPD aged ≥40 years were identified from the 1997 Health Survey for England and the 1998 and 2003 Scottish Health Survey cohorts. Self‐reported walking, domestic PA, and sport/exercise were assessed at baseline, and were classified into three groups: 1) No participation in that type of PA (the referent group); 2) below the median level of activity of the cohort (‘Low'); or 3) equal to or above the median level of activity of the cohort (‘High'). The medians were 5.25 metabolic equivalent (MET)‐hours/week for walking, 5.70 MET‐hours/week for domestic PA, and 8.00 MET‐hours/week for sport/exercise. Cox proportional hazards models were used to examine the association between PA and mortality risk.
Results
2398 participants with COPD were included in the analysis (mean age (SD) 62.6 (11.5), mean FEV1% predicted 73.4% (25.4), 52% men). Over 8.5 (3.9) years follow‐up, there were 571 deaths. Dose‐response associations with mortality risk were demonstrated for walking and sport/exercise, but not for domestic PA. Compared to the referent group, participants in the ‘High' walking group had a reduced mortality risk (hazard ratio (HR) 0.70, 95% confidence interval (CI) 0.56 to 0.88), as did participants in the ‘High' sport/exercise group (HR 0.69, 95% CI 0.51‐0.93). No significant mortality risk reductions were observed in the ‘Low' groups for walking or sport/exercise.
Conclusion
Walking and structured exercise should be encouraged in people with COPD to gain mortality benefit, but the effects of domestic PA on mortality remain unclear.
Grant support: ES is funded by the National Institute for Health Research (UK) (award code: CDF2010‐03‐30) and the National Health and Medical Research Council (award code: APP1110526) for dataset acquisition, processing and harmonisation.
TO 100
OXYGEN SUPPLEMENTATION DURING EXERCISE TRAINING IN COPD: A RCT
Alison J1,2, McKeough Z1, Jenkins S3,4, Holland A5,6, Hill K4, Morris N7,8, Leung R9, Spencer L2, Hill C10, Lee A5, Seale H8, Cecins N3, McDonald C11,12
1Discipline of Physiotherapy, Faculty of Health Sciences, University of Sydney, Sydney, Australia, 2Depatment of Physiotherapy, Royal Prince Alfred Hospital, Sydney, Australia, 3Department of Physiotherapy, Sir Charles Gairdner Hospital, Perth, Australia, 4School of Physiotherapy and Exercise Science, Curtin University, Perth, Australia, 5Discipline of Physiotherapy, School of Allied Health, La Trobe University, Melbourne, Australia, 6Department of Physiotherapy, Alfred Health, Melbourne, Australia, 7School of Allied Health Sciences, Griffith University, Brisbane, Australia, 8Lung Heart Program, The Prince Charles Hospital, Brisbane, Australia, 9Department of Respiratory and Sleep Medicine, Concord Hospital, Sydney, Australia, 10Department of Physiotherapy, Austin Health, Melbourne, Australia, 11Department of Respiratory and Sleep Medicine, Austin Health, Melbourne, Australia, and 12Department of Medicine, University of Melbourne, Melbourne, Australia
Introduction/Aim
Approximately 47 % of people with chronic obstructive pulmonary disease (COPD), referred to pulmonary rehabilitation, desaturate during exercise.
The aim was to determine whether supplementary oxygen during exercise training was more effective than medical air in improving exercise capacity and health‐related quality of life in people with COPD who desaturate to < 90% during the six‐minute walk test.
Methods
Multi‐centre randomised controlled trial with randomisation (independent, concealed allocation), blinding (participants, exercise trainers and assessors) and intention‐to‐treat analysis. Participants were randomised to either an Oxygen Group (OG) or Air Group (AG). Both groups received the respective gas from a concentrator via nasal prongs at 5 litres/minute during exercise training of treadmill and cycle exercise, three times/week for eight weeks. Primary outcome measures were the endurance shuttle walk test (ESWT) and the Chronic Respiratory Questionnaire (CRQ). The study had ethics approval and trial registration.
Results
111 participants (60 males), mean (SD) age 69 (7) years, FEV1/FVC 0.43 (0.13), FEV1 46 (17) % predicted were recruited and 97 completed (OG n=52; AG n=45). Within‐group changes at 8 weeks were significant for ESWT, CRQ Total (T), CRQ Dyspnoea (D) (ESWT: OG mean difference [95%CI]: 163 s [76, 249]; AG 149 s [56, 242]; CRQ T: OG 0.4 points(pts) [0.2, 0.7]; AG 0.5 pts [0.2, 0.7]; CRQ D: OG 0.6 pts [0.3, 0.9]; AG 0.7 pts [0.3, 1.0] (all p<0.01). There were no between group differences with p> 0.05 for all outcomes.
Conclusion
Exercise capacity and health‐related quality of life improved significantly in both groups, with no greater benefit from training with supplemental oxygen than with medical air. This is the largest rigorous RCT to report such findings.
Grant Support: NHMRC Project grant (App1019989)
TO 101
REDUCTION IN THE RATE AND RISK OF MODERATE OR SEVERE EXACERBATIONS WITH ONCE‐DAILY INDACATEROL/GLYCOPYRRONIUM COMPARED WITH TWICE‐DAILY SALMETEROL/FLUTICASONE IN A SUBSET OF GOLD GROUP D COPD PATIENTS WITH A HISTORY OF ≥2 EXACERBATIONS OR 1 HOSPITALIZATION: THE FLAME STUDY
Banerji D1, Vogelmeier C2, Wedzicha J3, Donohue J4, Fucile S1, Yadao A1, Ayers T1, Thach C1, Olsson P5, FowlerTaylor A1, Fogel R1, Patalano F6
1Novartis Pharmaceuticals Corporation, East Hanover, 2University Medical Center Giessen and Marburg , Marburg, Germany, 3National Heart and Lung Institute, Imperial College London, London, UK, 4Department of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, 5Novartis Sverige AB, Taby, Sweden, and 6Novartis Pharma AG, Basel, Switzerland
Introduction
The FLAME study demonstrated the superiority of indacaterol/glycopyrronium (110/50 μg, once daily), in reducing exacerbations, improving lung function, and health status versus salmeterol/fluticasone in moderate‐to‐very severe COPD patients with a history of exacerbations.1 We assessed the effect of indacaterol/glycopyrronium versus salmeterol/fluticasone on the rate and risk of moderate or severe exacerbations in a subset of GOLD Group D patients who had a history of ≥2 exacerbations or 1 hospitalization for exacerbation from the FLAME study.
Methods
FLAME was a 52‐week, randomized, double‐blind, double‐dummy, parallel‐group study. Patients with moderate‐to‐very severe COPD, post‐bronchodilator FEV1 ≥25% to <60% predicted normal, and a history of ≥1 exacerbation in the previous year were randomized (1:1) to receive either indacaterol/glycopyrronium (110/50 μg) once‐daily or salmeterol/fluticasone (50/500 μg) twice‐daily. The rate and time to moderate or severe exacerbations were analyzed in the subset of GOLD Group D patients.
Results
Of the 3362 patients randomized, 2514 were categorized as GOLD Group D. The mean post‐bronchodilator FEV1 was 44.1% of the predicted normal value and 56.3% patients were on ICS at screening. Indacaterol/glycopyrronium demonstrated superior efficacy over salmeterol/fluticasone in reducing the rate of moderate or severe exacerbations (rate ratio, 0.86;Table). Indacaterol/glycopyrronium delayed the time‐to‐first moderate or severe exacerbation compared with salmeterol/fluticasone (median days: 291 versus 215;Table). The patients treated with indacaterol/glycopyrronium had a 19% lower risk of a moderate or severe exacerbation compared with salmeterol/fluticasone.
Table 1 Effect of indacaterol/glycopyrronium versus salmeterol/fluticasone on moderate or severe exacerbations in the subset of GOLD Group D patients with a history of ≥2 exacerbations or 1 hospitalization for exacerbation
| Annualized rate | ||
|---|---|---|
| Indacaterol/glycopyrronium (n=531) | Salmeterol/fluticasone (n=503) | |
| Rate (95% CI) | 1.26 (1.06 to 1.51) | 1.47 (1.24 to 1.75) |
| Rate ratio* (95% CI) | 0.86 (0.74 to 1.00) | |
| P value | 0.05 | |
| Time‐to‐first exacerbation | ||
| Indacaterol/glycopyrronium (n=536) | Salmeterol/fluticasone (n=511) | |
| Patients with event, n (%) | 281 (52.4) | 299 (58.5) |
| Patients without event, n (%) | 255 (47.6) | 212 (41.5) |
| Time at risk (days), median (range) | 247.5 (1 to 419) | 181 (2 to 386) |
| Time‐to‐event (days), median (95% CI) | 291 (254 to 352) | 215 (175 to 261) |
| Hazard ratio*(95%CI) | 0.81 (0.69 to 0.96) | |
| P value | 0.013 | |
| * indacaterol/glycopyrronium versus salmeterol/fluticasone | ||
Conclusion
Indacaterol/glycopyrronium was superior to salmeterol/fluticasone in reducing the rate and risk of moderate or severe exacerbations in subset of GOLD Group D patients with a history of ≥2 exacerbations or 1 hospitalization for exacerbation, confirming its use as a preferred treatment option for COPD patients at high risk of exacerbations.
Grant Support: Novartis Pharma AG, Basel
REFERENCE
1. Wedzicha JA et al, N Engl J Med, 2016,374, 2222–2234
TO 102
PARENTAL RESPIRATORY DISEASE IS ASSOCIATED WITH REDUCED OFFSPRING LUNG HEALTH AT AGE 45 VIA PATHWAY OF MATERNAL AND PERSONAL SMOKING
Li L1, Williams M1, Johnston K1, Frith P1, Hypponen E1, Paquet C1
1University of South Australia, Adelaide, South Australia, Australia
Introduction
Familial aggregation of chronic lung conditions may result from a combination of genetic susceptibility and exposure to risk factors throughout life. We used a life‐course approach to investigate factors contributing to the relationship between parental respiratory disease history and Reduced Lung Health (RLH) in adulthood using data from the 1958 British Birth Cohort Study.
Methods
Cohort participants (n=6304) were characterised in terms of RLH (presence of respiratory symptoms at 42yrs and airway obstruction [FEV1/FVC<0.7 at 45yrs]) and parental history of respiratory disease (at offspring age 0,11,16yrs).
Life‐course factors evaluated were maternal smoking (0yrs), living with smoker (16,23,33,42yrs), social class (0,7,16,23,33,42yrs), respiratory illness (7,11,16,23,33,42yrs), smoking status (23,33,42yrs), and occupational exposure to dust or fumes (33,42yrs), operationalised for life periods (birth, childhood [7,11,16yrs], adulthood [23,33,42yrs]). Path analysis was used to investigate the mediating role of life‐course factors in the relationship between parental respiratory disease history and RLH, adjusting for gender, asthma and recent chest infection.
Results
Within this cohort, 3.7% had a parental respiratory history and 6.3% of offspring had RLH. Parental respiratory history was positively associated with RLH (p=0.023). Maternal smoking during pregnancy, personal smoking in adulthood, social class (0, 23 and 42yrs) and occupational exposure to dust or fumes were the only factors related to both parental history and RLH. Mediating pathway testing indicated that the sequence through maternal and adulthood smoking contributed most to model fit (indirect effect p=0.015), explaining 30% of the parental history‐RLH relationship.
Conclusion
An association between parental history of respiratory disease and offspring RLH at 45yrs was partly mediated by a sequence of exposure to maternal smoking and being a smoker during their adulthood. A large proportion of the relationship between parental history‐RLH remains unexplained by smoking, suggesting that assessing parental history of respiratory disease may provide insights into earlier diagnosis and intervention.
Grant Support: Australian Government Research Training Program Scholarship (LSK Li)
TO 103
ASSOCIATIONS OF ACTIVITY PHENOTYPES WITH HEALTH OUTCOMES IN COPD
McKeough Z1, Cheng S1, Alison J1,2, Jenkins C3, Stamatakis E4
1Discipline of Physiotherapy, The University of Sydney, Sydney, New South Wales, Australia, 2Allied Health Professorial Unit, Sydney Local Health District, Sydney, New South Wales, Australia, 3Respiratory Discipline, The University of Sydney, Sydney, New South Wales, Australia, and 4School of Public Health, The University of Sydney, Sydney, New South Wales, Australia
Introduction/Aim
To examine the association of four activity phenotypes with mortality and cardiometabolic risk factors in people with Chronic Obstructive Pulmonary Disease (COPD).
Methods
A prospective cohort was analysed. People with COPD aged >40 years who were current or ex‐smokers were identified from the 2003 Scottish Health Survey and grouped into one of the following activity phenotypes based on their self‐reported activity levels: 1) ‘Couch Potatoes': insufficiently active with high leisure‐based sitting time and/or no domestic physical activity (PA); 2) ‘Light Movers': insufficiently active with some domestic PA; 3) ‘Sedentary Exercisers': sufficiently active with high leisure‐based sitting time; or 4) ‘Busy Bees': sufficiently active with low leisure‐based sitting time. ‘Sufficiently active' involved adhering to PA recommendations of ≥ 7.5 metabolic equivalent (MET) hours per week. ‘Low leisure‐based sitting time' was defined as ≤ 200 minutes of recreational screen time per day. Associations between the phenotypes with mortality and cardiometabolic outcomes was made using Cox proportional hazards models or binary logistic regression models respectively.
Results
The sample comprised 584 participants (mean age (SD) 63.8 (11.5) years, 52% male). Over 5.5 (1.3) years follow‐up, there were 81 all‐cause deaths from 433 COPD participants with available data. Compared to the ‘couch potatoes', there was a reduced risk of all‐cause mortality in the ‘busy bees' (hazard ratio 0.26, 95% confidence interval (CI) 0.11‐0.65) with a trend towards a reduction in mortality risk in the other phenotypes (p‐trend = 0.02). There was a reduced risk of diabetes in the ‘busy bees' compared to the ‘couch potatoes' (odds ratio 0.14, 95% CI (0.03 to 0.67).
Conclusion
This analysis demonstrated a mortality benefit and reduced risk of diabetes in people with COPD when leisure‐based sitting time was low and PA guidelines were adhered to, indicating the health benefits of PA and the importance of measuring these activity outcomes in the COPD population.
Grant Support: Nil
Declaration of Interest: Nil.
Nomination for Awards: Physiotherapy.
Conflicts of Interest: Nil
Pulmonary Physiology & Sleep 2
TO 104
CLINICAL OUTCOMES IN COPD PATIENTS ATTENDING PULMONARY REHABILITATION ARE PREDICTED BY FORCED OSCILLOMETRY
Zimmermann S1,2,3, Fraser A4, Scott L4, Bertolin A1, Watts J1, Thamrin C1, Chan A1,2,3,4, King G1,2,3
1The Woolcock Emphysema Centre, Woolcock Institute of Medical Research, Sydney, Australia, 2The Northern Clinical School, The University of Sydney, Sydney, Australia, 3Department of Respiratory Medicine, Royal North Shore Hospital, St Leonards, Australia, and 4Department of Pulmonary Rehabilitation, Royal North Shore Hospital, St Leonards, Australia
Introduction/Aim
In COPD, lung hyperinflation reduces inspiratory reserve, thereby limiting exercise. Respiratory system reactance (Xrs) measured by forced oscillation technique (FOT) reflects heterogeneous airway narrowing and closure in COPD, and may relate to clinically important outcomes. We hypothesized that Xrs relates to quality of life, hyperinflation and exercise capacity in COPD.
Methods
15 COPD subjects from the Royal North Shore Hospital Pulmonary Rehabilitation department underwent spirometry, plethysmographic lung volumes, St. George's Respiratory Questionnaire (SGRQ) and 6‐minute walk distance (6MWD). Xrs was measured at 5Hz by FOT during 60s of tidal breathing followed by 3 deep inspirations, from which mean Xrs over the recording (Xmean), Xrs during inspiration only (Xinsp), the expiratory decrease in Xrs as an index of expiratory flow limitation (EFLI), and inspiratory capacity were derived. FOT, SGRQ and 6MWD were repeated at rehabilitation completion and 3 months later.
Results
Participants were (mean±SD) 75.2±6.1years old with FEV1 51.8±17.4%predicted. Xinsp correlated with SGRQ (r=‐0.60, p=0.04) and IC (r=0.80, p<0.001) but was unrelated to 6MWD at baseline. EFLI was unrelated to either IC or 6MWD. Xinsp and 6MWD improved significantly post‐rehabilitation (‐2.35±0.98 cmH2O*s*L‐1 to ‐2.04±0.82cmH2O*s*L‐1, p=0.008 and 399±99m to 451±123m, p=0.005, respectively). IC did not change. Both, baseline Xinsp and baseline EFLI predicted improvement in 6MWD, 3 months after completion of rehabilitation (r=0.59, p=0.04 and r=‐0.62, p=0.03, respectively).
Conclusion
Reactance during inspiration (Xinsp) and EFLI reflect different aspects of mechanical impairment of the respiratory system in COPD and have different clinical correlates. The correlations between Xinsp and quality of life and hyperinflation suggest it may be a useful clinical parameter in managing COPD, and this deserves further evaluation in larger prospective studies. EFLI does not add any further information above that of Xinsp, within the context of the present study. Therefore, separating Xrs into its inspiratory and expiratory components may be more clinically useful than using the mean value, in COPD.
Grant Support: NHMRC Postgraduate Scholarship.
TO 105
THE PHYSIOLOGICAL PROPERTIES OF THE KANGAROO AIRWAY
Wong J1, Wang K1,2, Henry P3, Maloney S1, Noble P1,4
1School of Human Science, The University of Western Australia, Perth, Australia, 2Clinical Sciences, Telethon Kids Institute, Subiaco, Australia, 3School of Medicine and Pharmacology, The University of Western Australia, Crawley, Australia, and 4Centre for Neonatal Research and Education, School of Pediatrics Child Health, The University of Western Australia, Crawley, Australia
Introduction/Aim
Comparative physiology is a powerful approach to help understand the relationship between structure and function. The kangaroo exhibits a unique breathing mechanism when hopping: respiration depends more on motional forces and less on active contraction of the diaphragm. We asked how structural and mechanical properties of the kangaroo airway might accommodate the respiratory pressures generated during hopping. This study compared mechanical and structural properties of airways from kangaroos and sheep, the latter of which is not subject to the same motion‐driven movement of air.
Methods
Bronchial segments from kangaroos (n=8) and sheep (n=12) were mounted in an organ bath chamber. Pressure‐volume curves were obtained between ‐10 and 20 cmH2O before and after theophylline. Airway stiffness was calculated from the change in pressure over normalized volume (∆ volume/initial volume). Closing pressure (pressure required for airway collapse) and airway wall morphology were also assessed. Data is mean±SEM.
Results
The stiffness of kangaroo airways was less than in sheep (kangaroo, 6±2 cmH2O; sheep, 16±4 cmH2O; p<0.05). Theophylline caused a reduction in sheep airway stiffness (p<0.05) but had no effect on kangaroo airway stiffness, suggesting a role for smooth muscle tone in the former. Kangaroo airways also required a less negative pressure for collapse compared with sheep airways (kangaroo, ‐15±3 cmH2O; sheep, ‐30±3 cmH2O; p<0.05). The kangaroo airway had a thicker inner (p<0.05) and thinner outer wall (p<0.05) compared with the sheep airway. While the total thickness of cartilage was comparable between groups, there were a greater number (p<0.05) of smaller (p<0.05) cartilage plates in the kangaroo airway.
Conclusion
Kangaroo airways have low stiffness and are more collapsible compared with sheep airways. Fragmented cartilage plates and absence of smooth muscle tone contributes to the lower stiffness. Low airway stiffness may maintain functional residual capacity during hopping in response to large variations in respiratory pressures.
Grant Support: N/A
Declaration of Interest Statement: None.
TO 106
FORCED OSCILLATION TECHNIQUE REFLECTS COMMUNICATING LUNG VOLUME (VA/TLC RATIO), BUT NOT TOTAL LUNG CAPACITY, IN CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Milne S1,3,4,5,6, Chapman D1,2, Farah C1,4,6, Thamrin C1, King G1,3,5
1Woolcock Emphysema Centre, Woolcock Institute of Medical Research, University of Sydney, Glebe, Australia, 2Department of Respiratory and Sleep Medicine, Royal North Shore Hospital, Northern Sydney Local Health District, St Leonards, Australia, 3Department of Respiratory Medicine, Concord Repatriation General Hospital, Sydney Local Health District, Concord, Australia, 4Northern Clinical School, Sydney Medical School, University of Sydney, Camperdown, Australia, 5Central Clinical School, Sydney Medical School, University of Sydney, Camperdown, Australia, and 6School of Life Sciences, University of Technology Sydney, Ultimo, Australia
Introduction/Aim
The lung in COPD demonstrates expiratory flow limitation, airway closure and ventilation heterogeneity. Reactance at 5 Hz (X5) measured by the forced oscillation technique (FOT) is influenced by each of these pathophysiological phenomena, but is also dependent on lung volume. In the presence of airway closure, where oscillating pressure waves are not able to penetrate all lung segments, X5 may not relate to the total thoracic gas volume. Single‐breath alveolar volume (VA), measured during the diffusing capacity test, estimates the communicating gas volume by dilution during a breath hold. The ratio of VA to plethysmographic total lung capacity (TLC), or VA/TLC, is therefore reduced in obstructive airways disease due to incomplete gas mixing and gas trapping. We hypothesised that X5 would relate to VA/TLC but not TLC in COPD.
Methods
15 subjects with mild‐moderate COPD (11 male, mean (range) age 68 (58‐79), mean ± SD %pred FEV1 64 ± 17) were tested using FOT (Thorasys tremoFlo c100) during 60 s normal tidal breathing. Spirometry, body plethysmography and the single‐breath diffusing capacity test were then performed according to standard quality criteria. Spearman rank correlation coefficients were determined before and after adjustment for known covariates from published reference equations.
Results
X5 was moderately correlated with VA/TLC (r = 0.66, p = 0.008) and VA (r = 0.58, p = 0.03) but not with TLC. After adjustment for known covariates, X5 Z‐score remained moderately correlated with VA/TLC (r = 0.60, p = 0.02) but not VA or TLC Z‐scores. VA/TLC correlated with the severity of airflow obstruction measured by FEV1/FVC ratio Z‐score (r = 0.77, p = 0.001).
Conclusion
In COPD, X5 measured by FOT during normal tidal breathing reflects the communicating lung volume rather than the total lung volume. FOT therefore may compliment traditional lung function measurements.
TO 107
PHYSIOLOGICAL RESPONSES TO THE SIX MINUTE WALK TEST AND MAXIMAL EXERCISE TESTING IN PULMONARY HYPERTENSION
Morris N1,2,3,4, Lin A1,3,4, Harris J1,4, Sabaratnam M1, Feenstra J4, Seale H4
1School of Allied Health Sciences, Griffith University, Gold Coast, Australia, 2Allied Health Research Collaborative, The Prince Charles Hospital, Brisbane, Australia, 3Menzies Health Institute, Griffith University, Gold Coast, Australia, 4Heart Lung Institute, The Prince Charles Hospital, Brisbane, Australia
Introduction/Aim
The six minute walk test (6MWT) remains the most commonly used clinical measure of exercise capacity in pulmonary hypertension (PH). Whilst maximal exercise testing using a cardiopulmonary exercise test (CPET), remains the gold standard estimate of exercise capacity, this test is much less common in clinical practice. The purpose of this study was to compare the physiological responses to the 6MWT and CPET in a group of PH subjects.
Methods
Eighteen individuals with Group I/IV PH patients (Functional Class I‐III) completed a CPET on a cycle ergometer and a 6MWT on separate days. During both tests, gas exchange was measured using a calibrated portable metabolic system (Cortex, Metamax). Oxygen uptake (VO2), carbon dioxide production (VCO2), ventilation (VE), heart rate (HR), oxygen (O2) pulse, VE/VCO2, end tidal carbon dioxide (PETCO2), oxygen saturation (SPO2) and breathlessness (Borg, 0‐10) were averaged over the final 30s and compared between the 6MWT and CPET. In a subgroup of 8 participants, end exercise lactate (HLa) was also measured using a portable lactate analyser (Lactate Scout).
Results
The mean peak power achieved by participants was 74 ± 20 W, whilst the mean 6MWT distance was 574 ± 89m. There was no significant difference between CPET and the 6MWT for peak VO2 (CPET: 16.3±6.6 vs 6MWT: 15.5±3.8 ml.kg‐1.min‐1), VE (54.7±13.8 vs 49.7±15.8 L.min‐1), HR (136±22 vs 143±27 beats.min‐1), O2 pulse (6.8±1.3 vs 7.0±1.7 ml.beat ‐1), VE/VCO2 (35±6 vs 36±5), PETCO2 (30±5 vs 29±4 mmHg) or SpO2 (88±11 vs 87 ± 14%). Peak VCO2 (1.43±0.46 vs 1.20±0.31 L.min‐1), breathlessness (5.5±2.2 vs 3.6±1.9) and lactate (8.5±1.5 vs 5.0±1.9) were all significantly higher(p<0.05) with CPET.
Conclusion
We found that the physiological responses to CPET and 6MWT in our group of PH participants were similar. This would suggest that the 6MWT is similar to a peak exercise challenge the PH population.
Grant Support: Office for Health and Medical Research, Queensland
TO 108
EFFECTIVENESS OF A SUBMAXIMAL CYCLE TEST TO PRESCRIBE TRAINING INTENSITY
Dowman L1,2,3, Ringin C1, Gergely K1, Hill C1,3
1Physiotherapy, Austin Health, Heidelberg, Victoria, Australia, 2Department of Respiratory & Sleep Medicine, Austin Health, Heidelberg, Victoria, Australia, and 3Institute for Breathing and Sleep, Heidelberg, Victoria, Australia
Introduction/Aim
In pulmonary rehabilitation (PR), cycle training is recommended at 60% peak oxygen uptake measured during cardiopulmonary exercise testing (CPET). However, access to CPET is limited and estimation of an equivalent intensity from the 6‐minute walk distance (6MWD) using published equations is associated with substantial variation. This study aimed to investigate whether a submaximal cycle exercise test (SMCT) can prescribe appropriate cycle training intensity and whether initial training intensity estimated from 6MWD and SMCT is similar.
Methods
Retrospective data was collected from patients who attended PR over the previous 12 months. Each patient routinely performed a 6‐minute walk test at baseline and completed a SMCT during the second exercise session. In the subsequent exercise session, cycle training was prescribed at 50% of peak work (Watts) achieved on SMCT. Initial intensity was considered appropriate if the patient could complete 15 minutes as prescribed with a reported dyspnoea and/or RPE score of 3‐4 on the Borg 0‐10 score.
Results
Forty‐three patients (23 male) with chronic lung disease (23 COPD, 10 ILD, 10 other) were included, with mean (SD) age of 70(11), 6MWD 437(86) metres and SMCT peak work of 60(22) watts. Eight one percent of patients achieved the target intensity, 16% found the initial workload too easy and 2% were unable to maintain the target intensity. There was a moderate correlation between work rate predicted from 6MWD 35(8) Watts and SMCT 30(11) Watts (r= 0.71, p<0.001). Estimating cycle training intensity from 6MWD over‐predicted (>5 Watts) appropriate training in 44% patients and under‐predicted in 7%.
Conclusions
In chronic lung disease, prescribing cycle exercise intensity at 50% of SMCT peak work achieves an appropriate training intensity that was tolerated by > 80% of patients. Prescribing work rate from SMCT and 6MWD results in similar training loads, although SMCT may provide more accurate cycle training intensity.
Grant support: nil
TO 109
FATTY ACIDS DO NOT ALTER BOVINE TRACHEALIS MUSCLE CONTRACTILITY
Chapman D1,2,3, Baroffio M4, Chiappori A4, Irvin C2, Brusasco V4
1University Of Technology Sydney, Ultimo, Australia, 2University of Vermont, Burlington, USA 3Woolcock Institute of Medical Research, Glebe, Australia, and 4University of Genoa, Genoa, Italy
Introduction/Aim
Increased dietary fat is associated with an increased risk of asthma and airway hyperresponsiveness. A single high fat meal reduces the efficacy of salbutamol, suggesting that dietary fatty acids may alter airway smooth muscle (ASM) contractility. Therefore our aim was to determine the effect of fatty acids on in vitro bovine trachealis smooth muscle responsiveness to relaxant and contractile stimuli.
Methods
Oleic acid, linoleic acid, alpha‐linolenic acid, palmitic acid, stearic acid and elaidic acid were compared at 10‐4.5M. Bovine trachealis muscle strips (n = 7/group/experiment) were mounted in tissue baths with warmed, aerated Krebs solution. All experiments were done in the presence of tetradotoxin (10‐6M). To test sensitivity to relaxant stimuli, muscle strips were contracted with acetylcholine (half maximal effective concentration, EC50) before addition of vehicle or fatty acid and cumulative dose‐response curves to isoproterenol (10‐9M to 10‐4M) performed. To test sensitivity to contractile stimuli, separate muscle strips were incubated with vehicle or fatty acid for 20min before cumulative dose‐response curves to acetylcholine (10‐9M to 10‐2M) were performed.
Results
In the relaxation experiment, ASM force following acetylchoine was not affected by addition of any of the fatty acids. Similarly, there was no effect of fatty acid on the EC50 concentration to isoproterenol (RANOVA p = 0.52). In the contraction experiment, baseline force was unaltered by addition of any of the fatty acids. Similarly, there was no effect of fatty acid on the EC50 to acetylcholine (RANOVA p = 0.86).
Conclusion
Dietary fatty acids do not alter bovine trachealis ASM function.
Grant Support: DGC was supported by a European Respiratory Society Short‐term Research Fellowship (STRTF 2015 – 8388)
Respiratory Infectious Diseases
TO 110
QUANTIFICATION OF PIPERACILLIN AND TAZOBACTAM IN PLASMA AND PLEURAL FLUID MEASURED BY A NOVEL LC‐MSMS ASSAY
Popowicz N1,2,3, O'Halloran S2,4, Fitzgerald D5, Lee Y1,2,5, Joyce D2,4
1Pleural Medicine Unit, Institute for Respiratory Health, Perth, Western Australia, Australia, 2School of Medicine, University of Western Australia, Perth, Western Australia, Australia, 3Department of Pharmacy, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia, 4PathWest, Clinical Pharmacology and Toxicology, Perth, Western Australia, Australia, and 5Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia
Introduction
Piperacillin (PIP) with tazobactam (TAZ) is commonly used for treatment of pleural infection, the pleural pharmacokinetics however, have not been reported. We developed and validated a rapid and sensitive ultra‐performance liquid‐chromatography with tandem mass‐ spectrometry assay for quantification of PIP/TAZ.
Methods
Both drugs were extracted from human plasma and pleural fluid by protein precipitation in methanol containing internal standards (IS) piperacillin‐d5 and sulbactam. 5uL of sample was mixed with 125uL of methanol containing IS, vortexed and centrifuged. Supernatant was diluted into mobile phase containing 10mM of ammonium bicarbonate and water. The chromatographic separation was achieved using an Acquity BEH C‐18 column.
This method was applied to two patients with pleural infection. Six pleural fluid and blood samples were obtained at steady‐state before and over 6‐hours post‐infusion of 4500mg‐PIP/TAZ.
Results
Electrospray ionisation in positive mode and multiple reaction monitoring (MRM) were used for PIP and piperacillin‐d5 at the transitions m/z 518.2→143.2 and m/z 523.2→148.2 respectively and in negative mode for TAZ and SUL at the transitions m/z 299.1→138.1 and m/z 232.4→140.1. Linearity was observed over the concentrations of 0.25‐352mg/L and 0.25‐50.5mg/L for PIP and TAZ respectively. Complete method validation was performed according to US FDA guidelines for selectivity, specificity, precision, accuracy, matrix effects and stability; results were within acceptable limits.
In both patients, the time to maximum concentration (Cmax) for PIP and TAZ in pleural fluid were delayed compared to plasma. The Cmax for PIP in pleural fluid reached 63mg/L and 59mg/L at 90 and 150‐minutes in each patient. This was 77% and 52% of the Cmax achieved in plasma for each patient respectively.
Conclusion
The two cases had notably different concentration‐time profiles for both drugs in pleural fluid but did not differ in systemic elimination of PIP/TAZ. The assay is feasible to use for future pharmacokinetic studies.
Grant Support: NHMRC; Cancer Council WA; Cancer Australia; NSW Dust Diseases Board (YCGL); Sir Charles Gairdner Research Advisory Group (NP, YCGL, SO, DAJ); WA Cancer & Palliative Care Network (DF).
TO 111
HIGH LEVELS OF HOSPITAL HEALTH CARE UTILIZATION ASSOCIATED WITH BRONCHIECTASIS
Maguire G1, King P2, Wong C3, Morgan L4, Middleton P5
1Baker Heart and Diabetes Institute, Melbourne, Australia, 2Monash Medical Centre, Clayton, Australia, 3Middlemore Hospital, Auckland, New Zealand, 4Concord Hospital, Sydney, Australia, and 5Westmead Hospital, Sydney, Australia
Introduction/Aim
Bronchiectasis not related to cystic fibrosis (non‐CF BEx) is an increasingly recognised cause of chronic lung disease that can occur in isolation or with other lung diseases including asthma and COPD. In other settings bronchiectasis is associated with significant health care utilisation but its impact in both Australia and New Zealand is poorly understood, including for Indigenous populations. We aimed to described the impact of non‐CF BEx on inpatinet hospital care in this setting
Methods
A multicentre Australian and New Zealand retrospective audit of hospital admission data relating to patients with non‐CF BEx admitted once or more to five hospitals in Melbourne, Sydney and Alice Springs (Australia) and Auckland (New Zealand) was undertaken. The number and length of stay (LOS) of respiratory admissions was determined. For Melbourne, Alice Springs and Auckland additional information was obtained regarding the requirement for ventilatory support.
Results
Data regarding hospitalisation are presented below.
| (95% CI) | AUSTRALIA | NEW ZEALAND | |||
|---|---|---|---|---|---|
| Alice Springs Indigenous | Melbourne | Sydney | Auckland Indigenous | Auckland non‐Indigenous | |
| Number of participants | 85 | 79 | 37 | 157 | 85 |
|
Admission (no/pers.yr) |
2.9 (2.7‐3.1) |
0.7 (0.6‐0.8) |
0.4 (0.3‐0.4) |
0.7 (0.6‐0.8) |
0.7 (0.6‐0.8) |
| LOS (day/pers.yr) |
16.9 (16.4‐17.3) |
6.4 (6.1‐6.7) |
3.1 (2.9‐3.3) |
4.1 (4.0‐4.3) |
4.0 (3.8‐4.2) |
|
LOS (med, IQR) |
4 (3‐7) |
6 (4‐11) |
7 (5‐11) |
4.5 (3‐7) |
4 (3‐7) |
| Ventilate % |
50.6 (39.5‐61.6) |
19.0 (11.0‐29.4) |
‐ |
7.6 (4.0‐13.0) |
2.4 (0.3‐8.2) |
| non‐invasive |
37.6 (27.4‐48.8) |
17.7 (10.1‐27.9) |
‐ |
5.7 (2.7‐10.6) |
1.2 (0.0‐6.4) |
| invasive |
8.2 (3.4‐16.2) |
5.1 (1.4‐12.5) |
‐ |
0.0 (0.0‐2.3) |
0.0 (0.0‐4.2) |
Conclusion
Health care utilisation for non‐CF BEx is substantial. The number of admissions varies substantially by site as does the cummulative LOS. Average LOS also varies and Australian patients have longer LOS compared to NZ patients. Indigenous Australian patients have a shorter LOS compared with non‐Indigenous counterparts despite more frequent admission and overall greater hospitalisation days. LOS is comparable to COPD (ranging from 4.1‐7.3 days in Australia) and the frequency of admission for non‐CF BEx is likely to be the major factor driving hospital‐based health care utilisation. The utilisation of ventilatory support varies by country and is particularly high in Indigenous Australians. The impact and optimal level of admission frequency, LOS and ventilatory support on susequent representation to hospital, quality of life and survival should be a focus of further investigation.
Grant Support: Australia Bronchiectasis Consortium – Lung Foundation of Australia
TO 112
RIFAMPICIN MONO‐RESISTANT TUBERCULOSIS IN QUEENSLAND, AUSTRALIA
Gibson J1,2, Eather G1,2
1Respiratory and Sleep Medicine Department, Princess Alexandra Hospital, Brisbane, Australia, and 2Metro South Clinical Tuberculosis Service, Princess Alexandra Hospital, Brisbane, Australia
Introduction/Aim
Drug resistant tuberculosis (TB) is an emerging problem. Rifampicin resistance is rare and is usually seen in multi‐drug resistant (MDR) TB. Rifampicin mono‐resistant (RMR) TB is less common.
The World Health Organization recommends RMR‐TB should be treated as per MDR TB guidelines. This requires prolonged treatment with second line agents including intravenous aminoglycosides, and is associated with increased risk of toxicity and cost. The evidence to support this recommendation in RMR‐TB is lacking.
We predicted MDR TB regimens are not commonly used in Queensland for RMR‐TB and to confirm this we carried out a study to examine the clinical features, treatment regimens and outcomes of RMR‐TB in Queensland, Australia.
Methods
This retrospective case series identified all cases of RMR‐TB in Queensland from 2000 to 2016. Data was gathered through the Notifiable Conditions System database with cross‐reference using medical records.
Results
Twelve cases of RMR‐TB were identified. The mean age was 29.1 years. All patients were overseas born. Nine cases (75%) had pulmonary disease.
Drug susceptibility testing confirmed isolates were resistant to Rifampicin and sensitive to other first line agents (Isoniazid, Pyrazinamide and Ethambutol).
Complete data on treatment and outcomes were available for 8 cases. No patients were treated with a MDR TB regimen. All patients who completed treatment in Queensland were cured. The mean duration of treatment was 14.6 months. The majority of patients were treated with the first line agents plus Moxifloxacin was added to the regimen in 5 cases. Only 1 patient received intravenous Amikacin.
Conclusion
This study confirms RMR‐TB is rare in Queensland but is not being managed with MDR TB regimens. Generally an extended regimen with first line agents +/‐ a Fluroquinolone was used. These regimens achieved good outcomes with 100% cure rates. Management of RMR‐TB requires further studies to determine the optimal treatment regimen, however based on this data extended courses with MDR type regimens are not necessary.
Grant Support: Nil
TO 113
5‐YEAR OUTCOME AND RAPID SCORE: AN AUSTRALIAN PLEURAL INFECTION COHORT
Goddard J1, Law B1, Azzopardi M1
1Respiratory Department, Sunshine Coast University Hospital, Birtinya, Queensland, Australia
Introduction/Aim
Mortality from pleural infection (PI) remains high. Many patients die after successful treatment of their PI. Few studies report on longer term outcomes and cause of death; one US study reported 76% 5‐year mortality. The RAPID score is a recently introduced risk stratification tool for PI, encompassing 5 parameters ‐ age, renal function, pleural fluid purulence, infection source and serum albumin. We aimed to validate the RAPID score in our single centre cohort, and examine longer term outcomes and cause of mortality.
Methods
All cases of PI treated at Nambour General Hospital 1st July 2007 – 1st July 2012 were reviewed. PI was defined by positive pleural fluid gram stain or culture or complicated parapneumonic effusion. Data until date of censor (1st July 2017) was extracted from hospital records and electronic pathology database. In‐hospital and 5‐year mortality and cause of death were recorded. GP practices were contacted to confirm death data.
Results
41 cases where included. Mean age was 58 (18). 68% were male. 61% were hospital‐acquired PI. 76% were culture positive. In‐hospital mortalty was 17.1% and 5‐yr mortality 46.3%. Most cases were stratified as medium‐risk by RAPID score (low n=12, medium n=21, high n=8). In‐hospital mortality for low‐, medium‐ and high‐risk groups was 0%, 28.6%, 12.5%. 5‐yr mortality for low‐, medium‐ and high‐risk groups was 0%, 66.7%, 62.5%. Cause of death for cases that were discharged but deceased at 5 years (n=12) included chronic liver disease, malignancy, myocardial infarction, bowel obstruction, cellulitis and aspiration pneumonia. These patients had a median of 4 comorbidities at the time of their PI.
Conclusion
In our cohort, the RAPID score accurately stratified the low risk group.
Poor longer term outcomes post PI likely relates to significant patient co‐morbidities.
Addressing co‐morbidity management at the time of PI is important.
TO 114
HIGH IMPACT OF INFLUENZA ON HOSPITALISATION RATES IN CHILDREN WITH CHRONIC LUNG DISEASES: A POPULATION‐BASED STUDY
Homaira N1,2, Briggs N3, Oei J4, Hilder L5, Bajuk B6, Snelling T7,8,9, Jaffe A1,2
1Discipline of Paediatrics, School of Women's and Children's Health, UNSW, Sydney, New South Wales, Australia, 2Respiratory Department, Sydney Children's Hospital, Randwick, Australia, 3Stats Central, Mark Wainwright Analytical Centre, UNSW, Sydney, New South Wales, Australia, 4Department of Newborn Care, Royal Hospital for Women, Randwick, Australia, 5Centre for Big Data Research in Health UNSW Sydney, New South Wales, Australia, Randwick, Australia, 6NSW Pregnancy and Newborn Services Network, Sydney Children's Hospitals Network, Randwick, Australia, 7Princess Margaret Hospital, Perth, Australia, 8Wesfarmers Centre of Vaccines & Infectious Diseases, Telethon Kids Institute, University of Western Australia, Perth, Australia, and 9Menzies School of Health Research, Charles Darwin University, Darwin, Australia
Introduction/Aim
Severe influenza infection in children with chronic lung diseases results in, unscheduled hospital presentations and substantial burden to the health system. National influenza burden data in children with chronic lung diseases are limited. Such data are crucial to monitor burden of disease and evaluate effectiveness of influenza vaccination program. We conducted a retrospective population‐based cohort study to measure the impact of influenza on hospitalisation rates in children with chronic lung diseases.
Methods
We performed a retrospective cohort study using population‐based linked administrative data for all children born in New South Wales between 2001‐2010 with complete follow‐up until December 31st 2011. The cohort was divided in to two groups: i) children with chronic lung diseases including all children with asthma, bronchopulmonary dysplasia, cystic fibrosis, and congenital lung disorders; and ii) all other standard‐risk children.
The primary outcome was any episode of influenza associated hospitalisation (ICD codes J.09‐J11). Incidence rates for influenza hospitalisation were calculated for 2001‐2011. We used Poisson estimation to calculate 95% confidence interval around incidences.
Results
Our cohort comprised of 9,708 children with chronic lung diseases and 877,240 standard‐risk children. The adjusted rate/1000 child‐years of influenza hospitalisation in children with chronic lung diseases was 5.21 (95% CI 2.57‐7.84) and for all other standard‐risk children was 0.92 (95% CI 0.46‐1.38). During 2001‐2011, the rate in children with chronic lung diseases ranged between 0.20‐12.57/1000 child‐years. The rate/1000 child‐years was similar in male and female children with chronic lung diseases and was 5.45 (95% CI 2.63‐8.26) for boys and 5.15 (95% CI 2.41‐7.89) for girls.
Conclusion
Our study has demonstrated that children with chronic diseases are at least five times more at risk of being hospitalised with influenza than standard‐risk children. Future studies investigating the effectiveness of universal vaccination program for these and all other children may help reduce the burden.
Grant Support: This work was funded by Rotary club of Sydney Cove and Cerebral Palsy Alliance
Conflict of Interest: The authors have no conflict of interest.
TO 115
THE SPREAD OF PSEUDOMONAS AERUGINOSA INFECTION IN BRONCHIECTASIS AND COPD
Stockwell R1,2, Chin M3, Wood M1,2,3, Johnson G4, Sherrard L1,5, Jabbour N4, Knibbs L6, Morawska L4, Bell S1,2,3
1Lung Bacteria Group, QIMR Berghofer Medical Research Institute, Brisbane, Australia, 2Faculty of Medicine, The University of Queensland, Brisbane, Australia, 3Adult Cystic Fibrosis Centre, The Prince Charles Hospital, Brisbane, Australia, 4International Laboratory for Air Quality and Health, Queensland University of Queensland, Brisbane, Australia, 5School of Pharmacy, Queen's University Belfast, Belfast, UK, and 6School of Public Health, The University of Queensland, Brisbane, Australia
Introduction/Aim
Pseudomonas aeruginosa (Pa) is the dominant respiratory pathogen in people with cystic fibrosis (CF) and can be released as viable aerosols during coughing. These aerosols can travel for at least 4 metres and remain airborne for at least 45 minutes. There is no research to determine if people with other chronic lung conditions can release Pa in cough aerosols. This project aimed to determine if people with non‐CF bronchiectasis (nCFB) and chronic obstructive pulmonary disease (COPD) release Pa aerosols during cough.
Methods
Twenty participants with nCFB (n=16) and COPD (n=4) and Pa lung infection were recruited. Participants underwent testing in two validated aerosol‐sampling devices to measure Pa viability at 2 and 4 m (distance) and at 5, 15 and 45 min (duration) during voluntary cough. Aerosols from each test were sampled using a 6‐stage Andersen Cascade Impactor. Quantitative sputum counts and aerosol cultures were performed with the total number of colony forming units (CFUs) determined.
Results
Twenty participants with mean (SD) age of 62.5 (11.0) years, FEV1 56.7 (20.7)% predicted and BMI 25.3 (4.3) kg/m2 were recruited. On the day of testing, 1 participant did not culture Pa in their sputum. Nine participants completed all five cough tests. Viable Pa was detected in cough aerosols from 6/19 (31.6%) participants at 2m, 6/19 (31.6%) participants at 4m, 2/15 (13.3%) participants at 5 minutes and 2/15 (13.3%) participants at 15 minutes. No participants produced Pa cough aerosols at 45 minutes. The concentration of Pa in the sputum did not correlate with the Pa CFU in the aerosol cultures.
Conclusion
Pa can be released as viable cough aerosols in people with nCFB and COPD, although at lower CFU compared to people with CF. These results highlight the importance of respiratory hygiene and infection control strategies in hospitals.
Grant Support: The Prince Charles Hospital Foundation, Advance Queensland
Asthma & Allergy 4
TO 116
DISCORDANT PERCEPTIONS OF ASTHMA CONTROL AND RELIEVER DEPENDENCE AMONG USERS OF SHORT‐ACTING BETA‐AGONISTS
Vyas‐Price B1, Ampon R1, Peters M2, Sawyer S3, Reddel H1
1Woolcock Institute of Medical Research, Sydney, Australia, 2Concord Repatriation General Hospital, Concord, Australia, and 3Centre for Adolescent Health, Royal Children's Hospital, Department of Paediatrics, Melbourne, Australia
Introduction/Aim
Overuse of short‐acting beta‐agonists (SABA) can compromise asthma control and increase burden of disease, especially among those with poorly‐controlled symptoms. This study assessed perception of control and dependence on reliever medication among patients who were taking SABA alone.
Methods
Cross‐sectional population‐based internet survey of participants with current asthma aged >16 years. Using Likert‐type questions (ranging from strongly disagree to strongly agree), the survey captured attitudes about asthma and asthma treatment. Asthma control was assessed using the Asthma Control Test (ACT: Poorly‐controlled <20; Well‐controlled 20‐25).
Results
SABA‐only respondents who had poor symptom control (n=374) compared with SABA‐only users with well‐controlled symptoms (n=632) were almost 3 times more likely to agree/strongly agree that they felt anxious without a reliever when out (30.6 vs. 11.6%, respectively; p<0.0001), and almost twice as likely to feel anxious when without a reliever around triggers (36.9 vs. 19.2%, respectively; p<0.0001). Additionally, those with poorly‐controlled vs. well‐controlled symptoms were more likely to agree/strongly agree that they relied on their reliever for their asthma (50.9% vs. 39.9%, respectively; p<0.0001), and that their reliever was “a life‐saver” (43.6% vs. 24.4%, respectively; p<0.0001). Half of respondents in both groups agreed/strongly agreed that their reliever gave them control over their asthma (49.7% vs 52.2%, respectively; p=0.74).
Conclusion
Patients with poor symptom control appeared overly reliant on SABA compared to patients with well‐controlled asthma. While optimal asthma control in this population requires preventative treatment, half of SABA‐only respondents viewed their reliever as their means of achieving control over their asthma. Given this, public messages such as “you can control your asthma” that are aimed at encouraging preventer use may inadvertently give the opposite message to many people. These data call into some question the preventer‐reliever‐control paradigm as currently used. Terminology that interacts better with patients' thoughts and beliefs may be more effective.
Grant Support: AstraZeneca
Conflict of Interest: This study was funded by a research grant from AstraZeneca. In the last 3 years, BV‐P has provided medical writing support through medical communication agencies to Boehringer Ingelheim and Novartis unrelated to the topic of her present research.
TO 117
FETAL GROWTH RESTRICTION CAUSES FUNCTIONAL AND STRUCTURAL ABNORMALITIES OF THE AIRWAY WALL IN ADULT MOUSE OFFSPRING
Noble P1, Kowlessur D1,2, Wang K1,2
1University of Western Australia, Crawley, Australia, and 2Telethon Kids Institute, Subiaco, Australia
Introduction/Aim
Intrauterine growth restriction (IUGR) is associated with increased risk of asthma in later life. Developmental changes to airway structure and function may impact susceptibility to subsequent disease. This study used a maternal hypoxia‐induced mouse model of IUGR to assess changes in airway smooth muscle (ASM) contractility and thickness in male and female adult offspring.
Methods
Pregnant BALB/c mice were housed under hypoxic conditions (10.5% O2) from gestational day (GD) 11‐GD17.5 (IUGR group; term=GD21). Following hypoxic exposure, mice were returned to a normoxic environment (21% O2). A second group of pregnant mice were housed under normoxic conditions throughout pregnancy (Control). Weights of offspring were recorded until 8 weeks of age at which point they were euthanized and a tracheasectomy was performed. Trachea segments were studied in an organ bath chamber to measure isometric force production to carbachol and subsequently fixed for morphometry. Maximal active tension and stress were calculated from force normalised to segment length and ASM cross‐sectional area respectively.
Results
The IUGR offspring were lighter at birth (Control, n=60; IUGR, n=58; p<0.05) and remained lighter at 8 weeks of age compared with Controls (Control, n=21; IUGR, n=21; p<0.05). Active tension (p<0.05) and stress (p<0.05) were reduced in male IUGR offspring compared with Controls with no difference in ASM thickness. There were no statistical differences in active tension or stress in IUGR female offspring despite a reduction in ASM thickness (p<0.05). Sensitivity of ASM to contractile agonist was not altered by IUGR.
Conclusion
There are persisting effects of IUGR on the mature airway wall which favour reduced contraction of the ASM layer, including lower ASM contractility in male offspring and a thinner ASM layer in female offspring. Findings suggest that altered development of the fetal airway can impact susceptibility to future airway disease through changes in ASM structure and function.
Grant Support: NHMRC (1090888, 1120128)
Declaration of Interest Statement: None.
TO 118
INTRINSIC AIRWAY SMOOTH MUSCLE TONE IN PERIPHERAL AIRWAYS IS DETERMINED BY THE VOLUME FRACTION OF MUSCLE AND EXTRACELLULAR MATRIX
Cairncross A1, Sanai F2,3, McParland B2, King G2, McFawn P1, Elliot J4, James A4,5, Noble P1,6
1School of Human Sciences, University Of Western Australia, Crawley, Australia, 2Woolcock Institute of Medical Research, University of Sydney, Glebe, Australia, 3School of Medical Sciences and Bosch Institute, University of Sydney, Sydney, Australia, 4Department of Pulmonary Physiology and Sleep Medicine, Sir Charles Gairdner Hospital, Nedlands, Australia, 5School of Medicine and Pharmacology, University of Western Australia, Crawley, Australia, and 6Centre for Neonatal Research and Education, School of Paediatrics and Child Health, University of Western Australia, Crawley, Australia
Introduction/Aim
Abnormalities in small airways are implicated as a primary cause of functional impairment in obstructive airway disease. Contraction of the airway smooth muscle (ASM) layer in the absence of an exogenous stimulus is termed ‘intrinsic tone' and may contribute to airflow limitation. The aim of this study was to assess the underlying structural determinants of ASM intrinsic tone in peripheral human airways.
Methods
Subjects (12M:6F, 37‐85 years) undergoing lung resection surgery were recruited and baseline lung function assessed prior to surgery. Peripheral airways were dissected from resected tissue and further cut into bronchial rings (1‐4 rings/subject) for measurement of force in organ bath chambers. Length‐tension curves were constructed to KCl (60 mM) to establish optimum length (LO) for contraction and subsequently adapted to repeated KCl stimulation. All experiments were performed at LO. Tension (mN/mm) in the ring was determined before and after complete relaxation to theophylline (10‐2M) and then fixed for stereology. Sections (0.5 μm) were stained using Masson's trichome technique and relative fractions of ASM (VVASM) and ECM (VVECM) within the ASM layer measured by point counting. Muscle tension was converted to stress (mN/mm2) after normalising to muscle thickness.
Results
Subjects had a pre‐bronchodilator FEV1(%Pred) of 89.4±4.5 and FEV1/FVC of 0.72±0.03. Bronchial rings exhibited a mean intrinsic stress of 20.1±3.4mN/mm2. Intrinsic stress (n=18) was negatively correlated with VVECM (r=‐0.47, p<0.05) and positively correlated with VVASM (r=0.51, p<0.05). There was also a non‐significant trend for a decrease in FEV1 (%Pred) with increasing intrinsic stress (r=‐0.56, p=0.07). There was no association between lung function and VVECM or VVASM.
Conclusion
The presence of intrinsic stress in the peripheral ASM layer is determined by the underlying layer composition, increasing with greater muscle fraction and decreasing with ECM fraction respectively. We propose that muscle composition affects lung function through regulation of intrinsic tone.
Grant Support: NHMRC (1063068, 1045824)
TO 119
ASSOCIATIONS BETWEEN THE DIETARY INFLAMMATORY INDEX AND LUNG FUNCTION IN MIDDLE‐AGE DIFFER BY ASTHMA STATUS
Byrne S1, Milanzi E1, Burgess J1, Jenkins M1, Abramson M2, Walters E1,3, Shivappa N4,5,6, Hebert J4,5,6, Hodge A1,7
1Centre for Epidemiology and Biostatistics, The University of Melbourne, Melbourne, Australia, 2School of Public Health & Preventive Medicine, Monash University, Melbourne, Australia, 3School of Medicine, University of Tasmania, Hobart, Australia, 4Cancer Prevention and Control Program, University of South Carolina, Columbia, USA, 5Department of Epidemiology and Biostatistics, University of South Carolina, Columbia, USA, 6Connecting Health Innovations LLC, Columbia, USA, and 7Cancer Council Victoria, Melbourne, Australia
Introduction/Aim
A pro‐inflammatory diet may contribute to poor lung function and, in turn, the development and/or progression of chronic inflammatory lung diseases. Few studies have assessed the relationship between the dietary inflammatory index (DII®), a literature‐derived measure of the inflammatory potential of the diet, and lung function. We aimed to investigate this relationship in a population‐based sample of middle‐aged adults.
Methods
A random sample of middle‐aged adults (45‐72 years) from inner south‐east Melbourne were assessed by spirometry and questionnaires (n=1183). An energy‐adjusted DII was calculated for each participant from a semi‐quantitative food frequency questionnaire. Regression methods were used to model relationships between DII quintiles and lung function outcomes, adjusting for age, gender, height, energy intake, BMI, asthma, atopy and smoking. Asthma status was also examined as an effect modifier.
Results
Associations between DII and FEV1 and between DII and FVC differed by asthma status (p=0.001 and <0.001, respectively). Current asthmatics with a diet in the highest DII quintile had a mean FEV1 516ml lower than those in the lowest DII quintile (95%CI 212, 819ml; Ptrend=0.003) and a mean FVC 588ml lower (95%CI 249, 926ml; Ptrend=0.006). Remitted asthmatics with a diet in the highest DII quintile had a mean FEV1 364ml lower than those in the lowest DII quintile (95%CI 81, 646ml; Ptrend=0.02) and a mean FVC 391ml lower (95%CI 76, 706ml; Ptrend=0.01). For those who had never had asthma, there were no associations between DII and any of the lung function measures. There were also no associations between DII and FEV1/FVC in any asthma category.
Conclusion
A pro‐inflammatory diet was associated with poorer lung function in current and remitted asthmatics. If this association is causal, it argues for a low inflammatory diet for people with a history of asthma.
Grant Support: NHMRC, NIDDK (USA)
TO 120
A MULTIDISCIPLINARY TEAM (MDT) CLINIC FOR VOCAL CORD DYSFUNCTION (VCD)
Bardin P1, Baxter M2, Ruane L1, Leahy E1, Phyland D2
1Monash University & Hospital, Melbourne, Australia, and 2Monash ENT and Speech Therapy, Melbourne, Australia
Introduction/Aim
Vocal cord dysfunction (VCD) is often mistaken for severe asthma and accurate diagnosis is crucial – but difficult. Treatment is complex and dedicated follow‐up is essential. To examine optimal overall management of VCD a Multidisciplinary Team (MDT) clinic was initiated and operationalized. This type of clinic has not yet been described.
Methods
Patients with suspected VCD (n=80) were referred by Respiratory physicians (n=76) and ENT surgeons (n=4). The clinic was staffed by a Respiratory physician, ENT surgeon (laryngologist), Speech therapist and Respiratory Nurse specialist. Patients completed questionnaires, had spirometry and dynamic CT larynx prior to review. At review by the team a history was obtained, physical examination conducted and laryngoscopy performed. Diagnosis of VCD was based on detection (CT larynx or laryngoscopy) of inspiratory paradoxical vocal cord movement (PVCM) on at least one occasion. The team finally reviewed all data, a likely diagnosis was formulated and treatment was selected in consultation with the patient.
Results
A total of 80 patients are reported of whom 61 (76%) had established asthma. A diagnosis of VCD was established in 53/80 cases (67%) and 44 elected to access speech therapy services. Based on symptoms speech therapy was gauged unsuccessful in 29/44 patients (65%) and 22/29 individuals elected to have botulinum toxin injection. In a second group of 17/80 cases (21%) a diagnosis of VCD was considered unlikely. In this group 13/17 patients had poorly controlled asthma and 4/17 patients had other diagnoses. In a third group of 10/80 patients (12%) VCD was strongly suspected but not confirmed. All patients were offered speech therapy and success was achieved in 7/10 cases.
Conclusion
A VCD MDT clinic was established providing an integrated multidisciplinary approach to diagnosis and management of VCD. Our experience indicates that this strategy is feasible and can be employed to optimise management of this problematic condition.
Grant Support: Monash Lung & Sleep Institute, Monash Health
TO 121
MULTIDIMENSIONAL ASSESSMENT OF TREATABLE TRAITS IN SEVERE ASTHMA AND COPD
Clark V1,2,4, Gibson P1,3,4, Cordova‐Rivera L1,4, Wark P1,3,4, McDonald V1,2,3,4
1Centre of Research Excellence in Severe Asthma, Newcastle, Australia, 2School of Nursing and Midwifery, University of Newcastle, Callaghan, Australia, 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, HMRI, New Lambton Heights, Australia, and 4Priority Research Centre for Healthy Lungs, University of Newcastle, Newcastle, Australia
Introduction/Aim
Treatable traits have been proposed as a new paradigm for airway disease management. Our aim was to determine the prevalence of traits in severe asthma and COPD compared to healthy controls and to compare trait prevalence by diagnostic label.
Methods
Participants with severe asthma, COPD and age‐matched healthy controls were recruited to this cross sectional study and underwent a clinic‐based multidimensional assessment to characterise their treatable traits.
Results
Recruited were 140 severe asthma, 45 COPD and 67 healthy control participants. Overall the mean±SD age was 56.6±16.2 years, and 57.5% were female. COPD participants were older compared to those with severe asthma and healthy controls, p<0.001. Post‐bronchodilator FEV1 % predicted was lower in COPD (53.0±19.8) compared to severe asthma (74.7±21.1) and healthy controls (99.0±13.8); p<0.001. Of the 23 possible traits, significantly more were identified in COPD (10.6±2.4) and severe asthma (9.0±2.8) compared to healthy controls (2.4±1.4); p<0.001, with a significant difference between COPD and severe asthma; p< 0.001. However, the number of comorbidities was not different between disease groups (COPD 6.8±3.1 versus severe asthma 5.9±2.7). Traits that were more prevalent in COPD compared to severe asthma were dyspnoea; p<0.01, exertional O2 desaturation; p<0.001, mucous‐hypersecretion; p<0.05 and airflow limitation; p<0.001. Those with severe asthma had significantly more daytime‐sleepiness; p<0.01, musculoskeletal problems; p<0.01, obesity; p<0.05, upper‐airway diseases; p<0.001 and dermatitis; p<0.001. Airway‐eosinophilia was more common in severe asthma and airway‐neutrophilia and systemic inflammation in COPD, p<0.05, p <0.001, respectively. The prevalence of frequent chest infections, pathogen colonisation, smoking, non‐adherence, inhaler‐polypharmacy, dysfunctional breathing, reflux, anxiety or depression did not differ between COPD and severe asthma.
Conclusion
This study confirms the heterogeneity of COPD and severe asthma. Multidimensional assessment in chronic airway disease allows for the detection of traits that can be targeted using a precision medicine approach. Trials testing these approaches are needed to advance management.
Grant Support: NHMRC, Hunter Medical Research Institute, University of Newcastle, John Hunter Hospital Charitable Trust
Declaration of Interest: No interest to declare.
Cell, Immunology & Molecular Biology of the Lung 3
TO 122
MicroRNA SIGNATURES IN MALIGNANT PLEURAL MESOTHELIOMA EFFUSIONS
Birnie K1, Prele C1, Musk A3,4, de Klerk N4,5, Lee Y1,4, Allcock R6, Bass P7, Thompson P1, Badrian B1, Mutsaers S1,2
1Institute For Respiratory Health, Perth, Australia, 2Occupational Respiratory Epidemiology, School of Population and Global Health, University of Western Australia, Perth, Australia, 3Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Australia, 4Telethon Kids Institute, WA, Australia and Centre for Child Health Research, Perth, Australia, 5School of Pathology and Laboratory medicine, University of Western Australia, Perth, Australia, 6Department of Thoracic Oncology, The Netherlands Cancer Institute, Amsterdam, The Netherlands, and 7Centre for Cell Therapy and Regenerative Medicine, Perth, Australia
Introduction/Aim
Malignant pleural mesothelioma (MPM) is an incurable cancer of the pleura that can be difficult to diagnose. Biomarkers for an earlier and/or easier diagnosis are urgently needed. The powerful gene regulators microRNA, have become popular diagnostic targets due to their stable expression within the body. Studies have examined microRNA in MPM and control samples, however it is still unclear which microRNA are potential biomarkers for MPM. Approximately 90% of patients develop pleural effusions which are an ideal source of diagnostic targets as sample collection is minimally invasive. The biomarker potential of microRNA in MPM frozen/fresh effusions is yet to be determined. We hypothesise that microRNA expressed in effusions are potential biomarkers for MPM.
Methods
Taqman OpenArray profiling and real‐time quantitative PCR were used to analyse microRNA in a cohort (Cohort 1) of 48 effusion cell and supernatant samples from MPM, lung adenocarcinoma and benign pleural disease patients. The potential microRNA biomarkers were then analysed in a second cohort (Cohort 2) of 60 MPM and lung adenocarcinoma samples.
Statistics
MicroRNA expression was determined to be significantly different between diseases on a volcano plot with a 2 or more‐fold change and a p< 0.05. MicroRNA combinations were analysed using logistic regression and diagnostic efficiency was assessed using receiver operating characteristic curves.
Results
An effusion cell signature based on the combination of miR‐143, miR‐210 and miR‐200c for the diagnosis of MPM was identified in Cohort 1 (AUC – 0.92) and validated in Cohort 2 (AUC – 0.71).
Conclusion
MicroRNA expressed in effusion cells are potential biomarkers for differentiating MPM from lung adenocarcinoma.
Grant Support: This work was supported by grants from Dust Diseases Board N.S.W, Maurice Blackburn and Sir Charles Gairdner Hospital Research Committee. S Mutsaers was supported on a Cancer Council WA Research Fellowship.
Declaration of Interest: No conflicts of interest.
TO 123
TRANSCRIPTIONAL PROFILING OF EPITHELIUM REVEALS SIMILAR COMPOSITION, BUT PARTIALLY DIFFERING ORGANIZATION BETWEEN THE UPPER AND LOWER AIRWAY
De Jong E1, Ling K3, Nichol K6,7, Anderson D1, Wark P6,7, Knight D6,7,8, Bosco A1, Stick S1,2,3,4, Kicic A1,2,3,4,5
1Telethon Kids Institute, Perth, Australia, 2School of Paediatrics and Child Health, The University of Western Australia, Perth, Australia, 3Department of Respiratory Medicine, Princess Margaret Hospital for Children, Perth, Australia, 4Centre for Cell Therapy and Regenerative Medicine, School of Medicine and Pharmacology, The University of Western Australia and Harry Perkins Institute of Medical Research, Perth, Australia, 5Occupation and Environment, School of Public Health, Curtin University, Perth, Australia, 6School of Medicine and Public Health, University of Newcastle, Australia, 7Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute, Newcastle, Australia, and 8Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver, Canada
Introduction/Aim
Emerging evidence suggests that the upper and lower airway are unified and that under disease settings, a pathological process in one region of the airway would affect the function of the entire airway. However, direct evidence supporting this is extremely limited and only inferred by the fact that the respiratory tract is continuous lined with epithelial cells and clinical observations of improved outcomes for lower airway disease following management of upper airway disease.
Methods
Here, we directly tested this hypothesis by performing RNA‐sequencing on predominantly matched nasal and bronchial epithelial brushings from 63 children with or without atopy or asthma. We then used a combination of differential gene expression, and gene co‐expression analyses to determine similarity of the transcriptional landscape between the upper and lower airway.
Results
Overall, we report ~50% homology and ~50% divergence between the two sites, independent of disease phenotype and atopy. We identified sixteen modules of co‐expressed genes (enriched for specific biological functions) to be conserved across nasal and bronchial epithelium. However, almost half of these were differentially expressed between the two regions.
Conclusion
Our findings suggest that in part the upper and lower airway do share a similar transcriptional composition, but also exhibit significant differences that is reflective of their region‐specific functions. With significant interest in biomarker development, our data suggests that in certain settings nasal epithelial cells, may inform on lower airway disease and thus has considerable clinical implications.
Grant Support: Asthma Australia
Conflict of Interest: No conflict of interest.
TO 124
MITOCHONDRIAL DYSFUNCTION REINFORCES THE SENESCENT PHENOTYPE IN IPF LUNG FIBROBLASTS
Schuliga M1, Waters D1, Blokland K1,2, Jaffar J3, Westall G3, Burgess J2, Prêle C4, Mutsaers S4, Grainge C1, Knight D1,5
1University of Newcastle, Callaghan, Australia, 2University of Groningen, Groningen, Netherlands, 3Alfred Hospital, Prahran, Australia, 4University of Western Australia, Nedlands, Australia, and 5University of British Columbia, Vancouver, Canada
Introduction/Aim
Increasing evidence highlights that cellular senescence contributes to idiopathic pulmonary fibrosis (IPF). The DNA damage response (DDR) in senescence also leads to escalated mitochondrial superoxide production to reinforce senescence. This study characterises senescence in lung fibroblasts from IPF patients (IPF‐LFs) and age‐matched controls (Ctrl‐LFs), delineating the role of mitochondria in senescence stabilization.
Methods
Fibroblast senescence was assessed using a composite set of markers, including p21 expression and senescence‐associated‐β‐galactosidase activity, which were measured by PCR and cytochemical staining, respectively. The DDR was detected by formation of phosphorylated‐p53 nuclear foci using immunofluorescence. A senescent‐associated secretory phenotype (SASP) was characterised by measuring increases in cytokine production and inflammatory gene expression with ELISA and Nanostring technology, respectively. Mitochondrial dysfunction was monitored by increases in mitochondrial stress, mass and superoxide using the fluorogenic dyes, n‐nonyl‐acridine orange, Mitotracker Green and MitoSOX, respectively.
Results
Even at early passage, IPF‐LFs were more senescent‐like than Ctrl‐LFs, exhibiting an intensified DDR, a SASP and mitochondrial dysfunction. The DNA damaging agent etoposide augmented senescence in Ctrl‐LFs accompanied by heightened mitochondrial stress, mass and superoxide production. However, it had no effect on IPF‐LFs. Mitochondrial perturbation by rotenone also evoked a DDR and senescence in Ctrl‐LFs. Inhibition of mTORC1, a regulator of mitochondrial function or incubation with the antioxidant, N‐acetyl cysteine attenuated pharmacological‐induced senescence.
Conclusion
IPF‐LFs exhibit senescent‐like features and mitochondrial dysfunction reinforces the senescent phenotype. Understanding the mechanisms by which mitochondria contribute to fibroblast senescence in IPF has potentially important therapeutic implications.
Grant support: NHMRC research grant #1099569
TO 125
NOTCH3 INHIBITION SIGNIFICANTLY REDUCES MUC5AC IN HUMAN AIRWAY EPITHELIAL CELLS
Reid A1,2, Nichol K2,3, Wei L1,2, Moheimani F1,2, Bartlett N1,2, Hansbro P1,2, Wark P2,3,4, Grainge C2,4, Knight D1,2,5
1School of Biomedical Sciences and Pharmacy, University Of Newcastle, Callaghan, Australia, 2Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute (HMRI), The University of Newcastle, Newcastle, Australia, 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, Australia, 4School of Medicine and Public Health, University of Newcastle, Callaghan, Callaghan, Australia, and 5Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver, Canada
Introduction
Mucus overproduction in patients with asthma is linked to increased hospitalisations and morbidity. The Notch family of receptor proteins regulate airway mucus production via differentiation mechanisms that direct cells towards secretory or ciliated morphology. However little is known regarding Notch's role during mucus production, following differentiation.
Aim/Hypothesis
To examine the impact of inhibiting Notch signalling on mucus production in fully differentiated primary bronchial epithelial cells (pBECs) from control subjects as well as patients with asthma. We hypothesize that Notch inhibition will downregulate mucus production.
Methods
pBECs from 5‐6 donors of each cohort were grown at air‐liquid interface (ALI) culture for 25 days to promote multicellular differentiation. At this time, cells were treated with dibenzazepine (DBZ), a potent inhibitor of Notch signalling for a further 96h during which, apical lining fluid was collected every 24h for assessment of MUC5AC release. At the completion of the experiment, samples were also collected for protein, mRNA and histological analysis. To assess the direct role of Notch3 on MUC5AC, siRNA knockdown of Notch3 was also performed in monolayer cultures of human epithelial cells.
Results
DBZ treatment significantly reduced MUC5AC expression and release in all phenotypes as assessed by qPCR, ELISA and IHC. Western blotting/qPCR revealed significant reduction of NOTCH3 intracellular domain (NICD3) and Notch3 mRNA in pBECs from all donor phenotypes. Notch3 siRNA knockdown significantly reduced MUC5AC protein. Finally, the goblet cell marker protein CLCA1 was unchanged across all treatments.
Conclusion
Notch3 inhibition reduced MUC5AC expression and secretion from differentiated pBECs, independent of goblet cell number. This reduction is NOTCH3 dependent and occurs in pBECs from asthmatics and non‐asthmatics. This suggests that Notch3 regulates MUC5AC production outside of Notch's well characterised role during secretory cell differentiation.
Grant Support: NHMRC project grant #1064405.
TO 126
INVESTIGATING THE ROLE OF HISTONE ACETYLATION IN TGF‐βINDUCED FIBROSIS IN COPD
Zakarya R1,2, Chen H1, Brandsma C3, Adcock I4, Oliver B1,2
1School of Life Sciences, University of Technology Sydney, Australia, Sydney, Australia, 2The Molecular Pathogenesis Group, Respiratory Cell and Molecular Biology, Woolcock Institute of Medical Research, Sydney, Australia, 3Department of Pathology and Medical Biology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands, and 4Airways Disease, Imperial College London, UK
Introduction/Aim
Fibrosis and thickening of the airway smooth muscle (ASM) layer are components of airway remodeling and have been attributed to an increase in the ECM fraction in the ASM layer2. It has been shown that epigenetic changes occur in COPD (immune cells and peripheral lung tissue)3 but it is not known if airway mesenchymal cells are reprogrammed. This project aims to identify differentially expressed ECM proteins and investigate the effect of epigenetic inhibition on protein expression.
Methods
Primary human ASM cells were isolated from lung tissue of COPD and non‐COPD smoking patients. ASM cells were grown in culture and stimulated with TGF‐β (10ng/ml) +/‐ histone deacetylase inhibitor Trichostatin A (TSA), bromo‐ and extra terminal domain (BET) protein inhibitor (+)JQ1, or histone acetyltransferase inhibitor Curcumin. Cell lysates were collected after 48 hours of treatment. Microarray analyses were carried out to identify basal differences in expression of ECM and epigenetic gene targets between COPD and non‐COPD smokers. qPCR carried out to confirm microarray analyses and determine effect of epigenetic inhibitors.
Results/Conclusion
ASM cells from COPD patients show augmented col5a1, col15a1 and TNC expression in response to stimulation with TGF‐β (10ng/mL) when compared to cells of smokers without COPD. Inhibition with TSA had no effect on col5a1, or TNC expression in cells from both patient groups, whilst inhibiting col15a1 expression in COPD. (+)JQ1 treatment significantly abrogated expression of col15a1 COPD and non‐COPD groups, whilst col5a1 expression was abrogated in COPD and TNC in non‐COPD. Col5a1 expression was significantly repressed with Curcumin treatment in non‐COPD group only. The different responses between non‐COPD susceptible smokers and COPD group highlights the epigenetic differences in disease, and that targeting histone acetylation may be a therapeutic option of small airway fibrosis in COPD.
TO 127
DYSREGULATED NOTCH SIGNALING DURING ASTHMATIC AIRWAY EPITHELIAL REPAIR
Iosifidis T1,2,3, Sutanto E3,4, Ling K3, Looi K3, Garratt L3, Martinovich K3, Kicic‐Starcevich E3,4, Shaw N3, Montgomery S1,3, Lannigan F1,5, Rigby P6, Knight D7,8,9, Stick S1,2,3,4, Kicic A1,2,3,4,10, on behalf of WAERP3,4,11,12
1School of Paediatrics & Child Health, The University of Western Australia, Perth, Australia, 2Centre for Cell Therapy & Regenerative Medicine, Perth, Australia, 3Telethon Kids Institute, Perth, Australia, 4Department of Respiratory Medicine, Princess Margaret Hospital for Children, Perth, Australia, 5School of Medicine, Notre Dame University, Fremantle, Australia, 6Centre for Microscopy, Characterisation and Analysis, Perth, Australia, 7School of Biomedical Sciences & Pharmacy, University of Newcastle, Newcastle, Australia, 8Priority Research Centre for Asthma & Respiratory Disease, Hunter Medical Research Institute, Newcastle, Australia, 9Department of Anesthesiology, Pharmacology & Therapeutics, University of British Columbia, Vancouver, Canada, 10Occupation and Environment, School of Public Health, Curtin University, Bentley, Australia, 11School of Medicine, University of Western Australia, Perth, Australia, and 12St John of God Hospital, Subiaco, Australia
Introduction/Aim
The airway epithelium is a key driver in asthma pathogenesis, partly due to its dysregulated response to injury. Notch signalling and potential crosstalk with integrins, modulate epithelial cell migration and repair. Therefore, it was hypothesised that aberrant Notch signalling in asthmatic epithelium would result in defective repair by airway epithelial cells(AEC) via regulation of integrins.
Methods
Tracheobronchial airway brushings of non‐asthmatic (n=18; age range: 1.2‐15.6yr; 8 males) and asthmatic (n=14; 3.3‐16.9yr; 12 males) children were utilised for AEC isolation and culture. Notch receptor and ligand gene expression was investigated by qPCR (mean±SEM; arbitrary units, AU). Notch signalling in cultures was inhibited with gamma secretase inhibitor, DAPT(N‐[N‐(3,5‐Difluoro‐phenacetyl)‐L‐alanyl]‐S‐phenylglycine‐t‐butyl ester) over a dose‐range (1nM‐10μM). Linear wounds were performed on AEC to assess repair (IncuCyte ZOOM®, Essen Bioscience). Integrin α5β1 protein expression was investigated by In‐Cell™ Western.
Results
Notch receptors (NOTCH1‐4) and ligands (JAG1‐2, DLL1, 3, 4) were found to be expressed in ex vivo AEC from non‐asthmatic and asthmatic children, however only NOTCH2 and JAG1 gene expression were differentially expressed in AEC from asthmatic children (NOTCH2, 10‐fold downregulation[p<0.01]; JAG1, 3.5‐fold upregulation[p<0.01]; n=6). Following in vitro wounding, NOTCH2 (2.92±0.11AU) and JAG1 (3.35±0.14AU) mRNA levels were induced within 48hr in AEC of non‐asthmatic children. However, an earlier induction of both NOTCH2 (2.58±0.10 AU) and JAG1 (4.19±0.09 AU) at 24hr post wounding was observed in AEC from asthmatic children. Global inhibition of Notch signalling resulted in a 40% reduction in wound repair and an inability to close the wound, observed at the maximal dose, 10μM. Furthermore, Notch signalling inhibition resulted in a reduction of α5 integrin protein expression of 30% at 500 nM DAPT, but not β1 integrin protein expression.
Conclusion
Findings suggest dysregulated expression of Notch signalling molecules, in conjunction with its role in regulating integrin expression, contribute to the defective wound repair of the asthmatic airway epithelium.
Grant Support: NHMRC(#1048910), APA(UWA), Centre for Cell Therapy & Regenerative Medicine PhD Top‐Up Scholarship, Fiona Staniforth Asthma Foundation WA PhD Top‐Up Scholarship.
Chronic Obstructive Pulmonary Disease (COPD) 3
TO 128
PULMONARY REHABILITATION DOES NOT IMPROVE OBJECTIVE MEASURES OF SLEEP QUALITY IN PEOPLE WITH CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Cox N1,2, Pepin V3, Burge A1,4, Mahal A5, Hill C2,6, Lee A1,2,4, Moore R6, Nicholson C1,4, O'Halloran P1, Lahham A1,2, Gillies R2,6, McDonald C2,5,6, Holland A1,2,4
1La Trobe University, Melbourne, Australia, 2Institute for Breathing and Sleep, Melbourne, Australia, 3Concordia University & Hôpital du Sacré‐Coeur de Montreal, Montreal, Canada, 4Alfred Health, Melbourne, Australia, 5University of Melbourne, Melbourne, Australia, and 6Austin Health, Melbourne, Australia
Introduction/Aim
More than 50% of people with chronic obstructive pulmonary disease (COPD) report poor sleep quality which has been associated with increased morbidity and mortality. There are varying reports of the effect of pulmonary rehabilitation (PR) on self‐reported sleep quality. We aimed to assess the effect of PR on objectively measured sleep quality in people with COPD.
Methods
This is a secondary analysis of data collected as part of an RCT comparing home‐based to centre‐based PR for COPD. Sleep quality was assessed objectively using the SenseWear Armband (SWA, Bodymedia USA), worn for 7 days before and after an 8‐week PR programme. Sleep characteristics were derived from accelerometer positional data and registration of sleep state by the SWA, determined from energy expenditure.
Results
33 participants (17 male; mean±SD age 68±11 years, FEV1 56±21 %predicted) had paired pre and post PR sleep data. Twenty participants received centre‐based PR and n=13 were allocated to home‐based PR.
Pre‐PR median [interquartile range] sleep onset latency (SOL) was 25 [9, 41] minutes, total sleep time (TST) 390 [339, 421] minutes and wake after sleep onset (WASO) 74 [43, 106] minutes. Sleep efficiency (SE) was low (75% [64, 84]).
No significant differences were seen in any sleep parameter (SOL, TST, WASO, SE) after PR (all p>0.10), between intervention groups (all p>0.20), or within PR groups (all p=0.13). There was no association between sleep parameters and measures of quality of life or function before or after PR. Attendance at a greater proportion of PR sessions was moderately associated with more TST at end rehabilitation (rs=0.5, p=0.009).
Conclusion
Sleep quality, measured objectively using actigraphy, did not improve after an 8‐week PR programme in individuals with COPD. Whether ongoing participation in regular exercise training beyond the duration of PR may influence sleep quality is yet to be determined.
Grant Support: NHMRC (Project Grant: 1046353; Early Career Fellowship: 1119970); Lung Foundation Australia; La Trobe University Research Collaboration Grant 2015
TO 129
IMPACT OF THE 2017 GOLD STRATEGY ON TIOTROPIUM+OLODATEROL RESPONSE
Langton D1, Ferguson G2, Voss F3, Maltais F4, Grönke L3, Buhl R5, Watz H6
1Thoracic Medicine, Frankston Hospital and Monash University Faculty of Medicine, Nursing and Health Sciences, Australia, 2Pulmonary Research Institute of Southeast Michigan, USA 3Boehringer Ingelheim Corporation, Ingelheim, Germany, 4Institut Universitaire de Cardiologie et de Pneumologie de Québec, Canada, 5Johannes Gutenberg University Mainz, Mainz, Germany, 6Pulmonary Research Institute at LungClinic Grosshansdorf Pulmonary Research, Grosshansdorf, Germany
Introduction/Aim
In the 2017 GOLD COPD strategy, treatment choices are guided by patient classification based on assessment of symptoms and exacerbation history. The previous strategy also included lung function. Here, we investigated the effect of the 2017 classification on an analysis of the efficacy of tiotropium+olodaterol (T+O) in GOLD stage A/B patients with COPD.
Methods
Patients from the Phase III, replicate 52‐week TONADO studies (NCT01431274, NCT01431287), who received T+O or the mono‐components, were classed as GOLD A/B or C/D by the 2017 (exacerbation history) or 2014 (lung function and exacerbation history) criteria. Distinction between A and B was not possible as mMRC Dyspnoea Scale and COPD Assessment Test had not been used. St. George's Respiratory Questionnaire (SGRQ) and transition dyspnoea index (TDI) were analysed.
Results
More patients are classified as GOLD A/B with 2017 criteria than with 2014 guidelines. T+O was superior to monotherapy for SGRQ and TDI in 2017 A/B population (Table).
Conclusion
Using exacerbation history alone (GOLD 2017), rather than combined with lung function, results in more patients classified as GOLD A/B, leading to more statistical power to investigate differences between T+O and monotherapies. Using the 2017 strategy, T+O had a greater impact on SGRQ and TDI than monotherapies in GOLD A/B patients.
Table
| 2017 GOLD A/B | 2014 GOLD A/B | |||||
|---|---|---|---|---|---|---|
| n | Adjusted mean ±SEM | Responders n(%)a/b | n | Adjusted mean ±SEM | Responders n(%)a/b | |
| SGRQ total score change from baseline | ||||||
| T+O 5/5μg | 739 | −6.9±0.4 | 428(58) | 390 | −6.4±0.6 | 219(56) |
| Tiotropium 5μg | 719 | −5.0±0.4 | 343(48) | 393 | −5.2±0.6 | 195(50) |
| Olodaterol 5μg | 744 | −5.1±0.4 | 332(45) | 412 | −6.2±0.6 | 198(48) |
| Mahler TDI focal score | ||||||
| T+O 5/5μg | 751 | 1.95±0.11 | 400(53) | 396 | 2.12±0.15 | 219(55) |
| Tiotropium 5μg | 737 | 1.50±0.11 | 351(48) | 395 | 1.93±0.15 | 204(52) |
| Olodaterol 5μg | 768 | 1.51±0.11 | 358(47) | 425 | 1.88±0.14 | 213(50) |
aSGRQ is ≥4.0 units better than baseline; bMahler TDI is ≥1.0 unit better than baseline
Grant Support: The study was funded by Boehringer Ingelheim.
Declaration of interest statement:
DL has no conflict of interest to declare in relation to this presentation. GTF has served as a consultant for AstraZeneca, Boehringer Ingelheim, Meda, Mylan, Novartis, Pearl Therapeutics, Sunovion, Theravance and Verona. He has also received honoraria from Boehringer Ingelheim, GlaxoSmithKline, Sunovion and Meda. FV and LG are employees of Boehringer Ingelheim. FM has nothing to disclose. RB has received reimbursement for attending scientific conferences, and/or fees for speaking and/or consulting from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Nycomed and Pfizer. HW has received grants/research support from Almirall, AstraZeneca, AB2BIO, Cilag Janssen, Chiesi, Boehringer Ingelheim, Bayer, GlaxoSmithKline, Novartis, Roche, Takeda, Sterna Pharmceuticals, as well as honoraria or consultation fees from Almirall, AstraZeneca, Boehringer Ingelheim, BerlinChemie, Chiesi, GlaxoSmithKline and Novartis.
TO 130
THE IMPACT OF PULMONARY REHABILITATION ON PEOPLE WITH MILD CHRONIC OBSTRUCTIVE PULMONARY DISEASE: A RANDOMISED CONTROLLED TRIAL
Lahham A1,2, McDonald C2,3,4, Cox N1,2, Rawlings S5, Nichols A5, Moore R6, Liacos A1,7, Holland A1,2,7
1Department of Physiotherapy, La Trobe University, Melbourne, Australia, 2Institute for Breathing and Sleep, Melbourne, Australia, 3Respiratory & Sleep Medicine, Austin Health, Melbourne, Australia, 4Department of Medicine, The University of Melbourne, Melbourne, Australia, 5Department of Physiotherapy, Monash Health, Melbourne, Australia, 6Department of Physiotherapy, Austin Health, Melbourne, Australia, 7Department of Physiotherapy, Alfred Health, Melbourne, Australia
Introduction/Aim
People with mild chronic obstructive pulmonary disease (COPD) experience exercise intolerance, dyspnoea and poor health‐related quality of life. However, the role of pulmonary rehabilitation in this group is unclear. This randomised controlled trial aimed to explore effects of home‐based pulmonary rehabilitation (PR) in people with mild COPD.
Methods
People with mild COPD (FEV1/FVC<70%; FEV1>80%predicted) with a smoking history of ≥ 10 packet years were randomised to either 8‐weeks of home‐based PR (one home visit and seven once‐weekly telephone calls) or attention control (weekly social telephone calls). Six‐minute walk distance (6MWD), modified Medical Research Council (mMRC) dyspnoea score and Chronic Respiratory Questionnaire (CRQ) scores were compared between groups post intervention and at 6‐months.
Results
A total of 58 participants (34 females, mean age 68 (SD 9) years, FEV1 90 (7) %predicted, 6MWD 496 (105) metres) were included with 29 participants randomised to home‐based PR. Participants attended an average of 6.8 of the eight scheduled sessions, ranging from three to eight sessions. Both groups showed improvements in exercise capacity, symptoms and health‐related quality of life over time, however there was no between‐group differences in the primary outcome of 6MWD at end‐intervention (mean difference 1.4 metres, 95% confidence interval (CI) ‐28.7 to 31.4 metres) or six months (9.8 metres, 95% CI ‐30.5 to 50.2 metres). At 6‐months follow‐up home‐based PR participants were more likely to have clinically important improvements in CRQ emotional function (50% of home PR vs 0% control, p<0.001) and CRQ total score (45% vs 17%, p=0.05), however there were no other differences in symptoms or other aspects of health‐related quality of life.
Conclusion
For people with mild COPD, home‐based pulmonary rehabilitation did not improve exercise capacity or health‐related quality of life more than weekly social telephone calls.
Grant Support: The Eirene Lucas Foundation and Institute for Breathing and Sleep.
TO 131
NO ADDITIONAL BENEFITS FOR PULMONARY REHABILITATION INCLUDING COGNITIVE BEHAVIOURAL THERAPY
Williams M1, Paquet C1, John D1, Cafarella P2, Frith P1,3
1University of South Australia, Adelaide, Australia, 2Flinders University of South Australia and Southern Adelaide Local Health Network, Adelaide, Australia, and 3Respiratory Laboratories Southern Adelaide Local Health Network, South Australia, Adelaide, Australia
Aim
This pragmatic randomised controlled trial aimed to determine whether comprehensive pulmonary rehabilitation (CPR) including cognitive behaviour therapy (CBT) for the sensation of breathlessness significantly improved health outcomes beyond those achieved with CPR alone.
Methods
People with COPD (FEV1 < 80 % pred, FEV1/FVC <70%, GOLD Grade ≥ 2) were block randomised to eight weeks of CPR with or without CBT (BREVE). Primary (six minute walk test (6MWT), Hospital Anxiety and Depression scale (HADs)) and secondary outcomes (breathlessness in daily life (Dyspnoea‐12 (D‐12), Multidimensional Dyspnoea Profile (MDP), quality of life (Chronic Respiratory Questionnaire (CRQ) and habitual daily activity (accelerometry)) were assessed before and one, six and 12 months post intervention. Differences between groups were assessed with latent growth models (non‐linear change) with and without covariates (age, sex, BMI, GOLD grade, comorbidity, smoking status and CPRP attendance) using both intention to treat (ITT) and per protocol (PP: commenced intervention and valid 6MWT) approaches with p≤0.05 significant.
Results
101 participants (mean age 70 ± SD 8.5, 54 males, FEV1 % pred 47.7 ± 16.3) enrolled in the trial (n=88 for PP analysis). With the exception of CRQ and MDP subdomain scores, groups did not differ significantly in either trajectory or assessment points for primary or secondary outcomes (ITT, PP with and without covariates). For ITT, improvements in CRQ‐Dyspnoea favoured CPRP + BREVE (unadjusted model p = 0.03) whereas reductions in MDP‐Emotional Response favoured CPRP alone (adjusted model p = 0.03). For PP with and without adjustment for covariates, differences between groups for CRQ and MDP favoured CPRP alone (CRQ‐Mastery p = 0.04; MDP‐Immediate Perception p = 0.03; MDP‐ Emotional Response p = 0.04).
Conclusion
In this cohort of people participating in CPRP, there was no clear additional short or longer term benefit of combining CPRP with CBT for breathlessness.
Grant Support:
This study was supported by a National Health and Medical Research Council Project Grant (# 1010309).
Clinical Trial registration: Australian New Zealand Clinical Trials Registry (ANZCTR12611000292976)
TO 132
AN AUDIT OF ACTIVITY AND OUTCOMES OF THE AUSTIN RESPIRATORY HIGH DEPENDENCY UNIT
Chamula K1, McDonald C1,2,3, Jones D3,4,5, Berlowitz D1,2,3, Hannan L1,2, Rautela L2, Sheers N2, Xerri R, Lewis J, Howard M1,2,3,4
1Department of Respiratory and Sleep Medicine, Austin Health, Heidelberg, Australia, 2Institute for Breathing and Sleep, Heidelberg, Australia, 3University of Melbourne, Parkville, Australia, 4Monash University, Clayton, Australia, and 5Intensive Care Unit, Austin Health, Heidelberg, Australia
Introduction/Aim
There is a paucity of literature documenting Respiratory High Dependency Unit (HDU) outcomes. We present demographic and outcome data for patients undergoing care in the Austin Hospital Respiratory HDU, which provides single organ support for patients with acute respiratory failure.
Methods
This retrospective audit describes all admissions to the Respiratory HDU during January to December 2016. Logistic regression was used to identify factors related to in‐hospital mortality.
Results
82 patients, mean age 67.3 years (SD 16.83,) underwent 83 HDU admissions. 53% (44 patients) were male. Mean HDU length of stay (LOS) was 2.17 days (SD 2.15, 95% CI 1.71‐2.63.) The main precipitating causes for respiratory failure were exacerbation of chronic obstructive pulmonary disease (n=25, 30.12%) and infection (n=23, 27.7%.) 25 admissions (30.12%) were for management of hypoxic respiratory failure, 9 of which were treated with non‐invasive ventilation (NIV). N=18 (21.69%) admissions occurred following a ward MET call and had an average HDU LOS of 1.5 days (SD 0.99, 95% CI 1.11‐2.03.) 7 patients (8.4% of admissions) did not survive to hospital discharge. A higher age‐adjusted Charlson comorbidity score was associated with higher in‐hospital mortality (OR 1.41, p=0.021, 95% CI 1.05‐1.89.)
Conclusion
The HDU has a high turnover of patients, including post‐MET call care. Outcomes are generally good, however increased comorbidity as reflected by a higher age‐adjusted Charlson score was associated with in‐hospital mortality. A proportion of hypoxaemic patients received NIV, raising an opportunity for review of current practice.
Grant Support: None.
TO 133
ALPHA‐1 ANTITRYPSIN TREATMENT SLOWS EMPHYSEMA PROGRESSION INDEPENDENT OF BASELINE FEV1
Thompson P1, Ficker J2,3, Burdon J4, Chapman K5, Turner A6, Sandhaus R7, Wencker M8, Vit O9, Fries M10, McElvaney N11
1Molecular Genetics and Inflammation Unit, Institute of Respiratory Health and School of Medicine, University of Western Australia, Perth, Australia, 2Department of Respiratory Medicine, Allergology and Sleep Medicine, General Hospital Nuremberg, Nuremberg, Germany, 3Paracelsus Medical University, Nuremberg, Germany, 4St Vincent's Hospital, Department of Respiratory Medicine, Fitzroy, Australia, 5Department of Medicine, University of Toronto, Toronto, Canada, 6Institute of Inflammation and Ageing, Centre for Translational Inflammation Research, Queen Elizabeth Hospital Birmingham, Birmingham, UK, 7National Jewish Health, Denver, USA, 8Medical Affairs, CSL Behring, Marburg, Germany, 9Clinical Research and Development, CSL Behring, Bern, Switzerland, 10Clinical Strategy and Development, CSL Behring, King of Prussia, USA, 11Department of Respiratory Medicine, Beaumont Hospital, Royal College of Surgeons in Ireland, Dublin, Ireland
Introduction/Aim
Patients with alpha‐1 antitrypsin deficiency (AATD) develop pulmonary emphysema prematurely. RAPID, a randomized placebo‐controlled trial, showed that treatment with A1‐PI (Zemaira/Respreeza) slows emphysema progression. Based on observational data, which showed a reduced loss in FEV1 in a subgroup of patients, current guidelines recommend treatment with A1‐PI when FEV1 is between 30 and 65% predicted. However, the relationship between the effect of treatment on lung structure preservation and FEV1 is unclear. The aim was to assess the effect of treatment in relation to baseline FEV1 % predicted as measured by change in computed tomography (CT) lung density in 180 patients randomized in RAPID with baseline FEV1 between 27% and 79% predicted.
Methods
Changes in annual CT lung density decline rates for both active and placebo treated patients were calculated at 2 years. A random slope intercept model with baseline FEV1 and treatment group as covariates was used to analyse the influence on treatment effect.
Results
Baseline lung function impairment did not affect long‐term changes in lung density (p=ns), the regression line was flat. Active treatment was associated with lung density preservation (P<0.0001) and the regression line was parallel to that of placebo treated patients. The regression line for rate of annual lung density decline vs baseline FEV1% was flat with no interaction between treatment group and baseline FEV1.
Conclusion
These data demonstrate that patients with AATD who are treated with A1‐PI therapy derive an equal benefit in terms of lung tissue preservation over 2‐years that is independent of their pre‐treatment FEV1%.
Grant Support: The RAPID trial programme and preparation of this abstract was supported by CSL Behring.
Interventional Pulmonology / Bronchology 2
TO 134
DIAGNOSTIC ACCURACY OF BRONCHOSCOPY WITH CONSCIOUS SEDATION VERSUS GENERAL ANAESTHETIC IN A RANDOMISED PROSPECTIVE COHORT
Skinner T1, Churton J1, Edwards T1, Bashirzadeh F1, Zappala C1, Hundloe J1, Tan H2, Pattison A1, Fielding D1
1Department of Thoracic Medicine, Royal Brisbane And Women's Hospital, Brisbane, Australia, and 2Department of Anaesthetic Services, Royal Brisbane And Women's Hospital, Brisbane, Australia
Introduction/Aim
To assess for non‐inferiority of diagnostic accuracy for conscious sedation (CS) compared with general anaesthetic (GA) for bronchoscopic procedures.
Methods
We report on a further analysis of a prospective randomised patient group. Patients undergoing therapeutic and diagnostic procedures within the RBWH were considered for trial entry and randomization. Procedures included standard bronchoscopy, endobronchial ultrasound (EBUS) with transbronchial node aspiration (TBNA) or EBUS Guide Sheath. Patients were randomized to either CS or GA, stratified for Charlson Comorbidity Index. GA was defined as the use of a Laryngeal mask airway and/or propofol usage. Diagnosis obtained at bronchoscopy was compared to the final clinical diagnosis.
Results
93 patients were randomised. 49 of these received CS of which 32 were diagnostic procedures, with 14 being EBUS TBNAs. In the GA group these numbers were 44, 32 and 14 respectively. A final diagnosis of malignancy was made in 12 cases in the CS group (38%) and 18 cases in the GA group (56%). For all diagnostic procedures there was no significant difference in diagnostic accuracy between CS and GA, 93.3 vs 87.5% (p=0.67). Regarding EBUS TBNA diagnostic accuracy was 100 vs 92.9% (P=1.00). 24 lymph nodes were sampled in the CS group, 46% paratracheal, 17% subcarinal and 38% hilar. 21 nodes were sampled in the GA group, 24% paratracheal, 29% subcarinal and 48% hilar. Average passes per node were 3.28 ±0.79 and 3.00 ±1.00 respectively (p=0.29). For the CS cases only 2 drugs were used: Midazolam (mean dose 4.4mg ±1.0) and Fentanyl. A variety of anaesthetic agents were used in the GA group. There was no significant difference regarding mean fentanyl dosage of 90.6mcg ±16 for CS vs 86.2mcg ±52.9 for GA (p=0.60).
Conclusion
CS is not inferior to GA in terms of diagnostic accuracy, including EBUS TBNA from a wide range of nodal stations.
Grant Support: Nil
TO 135
SAFETY AND DIAGNOSTIC PERFORMANCE OF CRYOBIOPSY IN MELBOURNE, AUSTRALIA
Donovan C1, Sleep L1, See K1, Irving L1,2, Leong P1, Steinfort D1,2
1Royal Melbourne Hospital, Parkville, Australia, and 2University of Melbourne, Australia
Introduction/Aim
Cryobiopsy is an emerging technique with mounting utilisation in the settings of diffuse parenchymal lung disease (DPLD) and neoplasia. The safety and usage pattern of cryobiopsy is not well established in the Australian setting. At our tertiary institution, we routinely perform cryobiopsy with general anaesthesia, endotracheal intubation and fluoroscopy guided 1.9mm cryoprobe via ERBECRYO 2 with routine bronchial blocker balloon deployment. We thus set out to establish the safety and usage patterns of our cryobiopsy service.
Methods
Following institutional ethics approval, we conducted a retrospective audit of our institution's cryobiopsy register (November 2015‐September 2017). Records missing from our electronic records were supplemented by a hand search, and by contacting referrers. Results were cross‐checked by two authors (CD, LS), verified by a third (PL) and are presented are mean±SD.
Results
49 patients underwent cryobiopsy in the audit period, with 2.6±1.1 biopsies performed per patient, and targets as follows: right lower lobe 23, right upper lobe 15, left lower lobe 12, left upper lobe 11 and endobronchial 4. The predominant indication for cryobiopsy was suspected DPLD (43/49) with possible malignancy accounting for the remaining cases. The mean FVC was 88±17% predicted (lowest 57%) and DLCO 59±17% predicted (lowest 35%). Same day discharge was achieved in 42/49, with 2 further uncomplicated cases staying overnight for social reasons. There were no cases of severe bleeding. Bleeding was moderate (controllable with endobronchial interventions) in 5 cases; 4 cases had pneumothoraces of whom 2 required intercostal catheter insertion. Physicians agreed or strongly agreed that cryobiopsy was helpful in 45/49 patients. Cryobiopsy was suggestive or diagnostic of DPLD in 39, infection in 1 and malignancy in 6. No abnormality was present in 2, 1 of whom was referred for surgical lung biopsy.
Conclusion
Cryobiopsy appears to have an acceptable safety profile with a good diagnostic yield.
Key Words: cryobiopsy, bronchoscopy, interstitial lung disease
Grant Support: Nil
TO 136
UTILITY OF RADIAL EBUS CRYOBIOPSY IN DIAGNOSIS OF SOLITARY PULMONARY NODULES
Tan S1, Ing A1,2,3, Saghaie T1,2,3
1Concord General Repatriation Hospital, Sydney, Australia, 2The Faculty of Medicine, University of Sydney, Australia, and 3Faculty of Medicine and Health Science, Macquarie University, Australia
Introduction/Aim
Forceps biopsy through a guide sheet after locating the lesion using radial probe EBUS is an established technique in diagnosis of solitary pulmonary modules (SPN). The yield, however, drops significantly if the lesion is not concentric. Furthermore, the 1.7mm forceps often provide small samples which occasionally fall short of providing all the information required in malignancies. Using a cryoprobe in combination with radial EBUS could potentially provide larger samples and increase the yield in non‐concentric lesions.
Methods
All patients who underwent radial EBUS cryobiopsy for diagnosis of SPN at Concord and Macquarie University hospitals in Sydney were included in this study. A retrospective audit was undertaken to obtain demographic, baseline physiological and procedural data. Complications and length of stay were recorded. Yield was determined by histopathology and clinical data.
Results
A total of 9 patients (3 female, mean age 73.4 years) have so far been included in the study. All procedures were performed under general anesthesia, with rigid intubation used in 8 cases. The lesion was located in all cases using an EBUS radial probe with only one eccenteric lesion. Most targets were located in the upper lobes (66.6%). An average of 3.1 biopsies were obtained. No cases of pneumothorax or severe bleeding were observed. Only two patients stayed overnight after the procedure. Average diameter of specimens was 5mm. Definite malignant pathology was diagnosed in 5 cases with an overall yield of 7/9 (77.7%)
Conclusion
Radial EBUS cryobiopsy is a feasable alternative in diagnosis of SPN. The yield is comparable to previously reported techniques, however the larger specimens obtained by cryobiopsy could potentially provide invaluable data in malignant conditions.
Grant Support:
TO 137
TRANSBRONCHIAL CRYOBIOPSY IN INTERSTITIAL LUNG DISEASE—A RETROSPECTIVE AUDIT
She S1, Williamson J2,3, Ing A1,3,4, Ing M1, Irandoost P5, Saghaie T1,3,4
1Faculty of Medicine, University of Sydney, Australia, 2Department of Thoracic Medicine, Liverpool Hospital, Australia, 3Faculty of Medicine and Health Science, Macquarie University, Australia, 4Concord General Repatriation Hospital, Concord, Australia, 5Laverty Pathology, North Ryde, Australia
Introduction/Aim
Histolopathology is often required to achieve a multidisciplinary diagnosis in diffuse parenchymal lung disease. Surgical lung biopsy (SLB) remains the gold standard but is associated with significant morbidity and mortality. Recent emergence of transbronchial cryobiopsy (TBCB) as a potential alternative to SLB, promising less complications and a comparable yield, has divided the world of interventional pulmonology. There have been numerous publications reporting different and occasionally contradicting outcomes. Despite relative popularity of TBCB in our region, so far there have not been any published series from Australia.
Methods
All patients who underwent TBCB at Concord, Macquarie University and Liverpool Hospitals in Sydney for diagnosis of diffuse parenchymal lung disease between August 2013 and June 2017 were included. A retrospective audit was undertaken to obtain demographic, baseline physiological and Procedural data. Complications and length of stay were recorded. Diagnostic value of TBCB was assessed by its histopathological and clinical impact. All biopsy specimens were reviewed by a single investigator to record size, presence of artefact, percentage of alveolar area and presence of pleura or proximal airway structures.
Results
A total of 46 patients (25 male, average age 62.2) were enrolled in this study. All cases were performed under general anaesthesia with rigid bronchoscope access. An average of 6.1 biopsies were obtained from 1‐3 lobes. Most patients were discharged home the same day (65.7%) with average length of stay of 1.05 nights. Pneumothorax was observed in 10.5% of the patients with severe endobronchial bleeding in 5.2%. There were no deaths reported within 30 days of the procedure. Histopathological data as well as yield are currently being analysed.
Conclusion
Our preliminary data suggests that TBCB is a relatively safe procedure with an acceptable yield which could be considered as an alternative to SLB.
Grant Support:
TO 138
STUDY OF ENDOBRONCHIAL VALVES INSERTION FOR ADVANCED EMPHYSEMA AT THE ROYAL BRISBANE AND WOMEN'S HOSPITAL IN QUEENSLAND AUSTRALIA
Bilal A1, Rathnayake A1, Bashirzadeh F1
1Royal Brisbane and Women's Hospital, Brisbane/Herston, Australia
Introduction/Aim
Emphysema is a leading cause of disability and death. Its current medical treatment shows certain limitations in the advanced stage of the disease. Also, there is limited evidence in the Australian setting regarding therapeutic interventions for reducing hyperinflation, including endobronchial valves insertion (EBV). This study examined the outcomes of EBV insertion in patients with severe emphysema at the Royal Brisbane and Women's Hospital.
Methods
This is a retrospective review of patients with severe emphysema who underwent EBV insertion from 2011‐2017. The primary outcomes were change in exercise tolerance as measured by the six‐minute walk test (6MWT) and quality of life (QoL) as measured by the St. George's Respiratory Questionnaire (SGRQ) and direct questioning. Variables of interest were measured pre‐ and post‐EBV placement.
Results
Of the 31 patients included in the study, 15 were females. Age ranged from 50 to 80 years (median age=67 years). Sixteen patients had no complications, and 9 patients had multiple complications. Three patients were readmitted within 30 days and 2 died mainly due to old‐age co‐morbidities. Ninety‐day mortality rate was 0%. Pre and post values for 6MWT were obtained for 18 patients, SGRQ for 10 patients, and QoL data for 24 patients. Patients with complete data (25) showed improved mean values of SGRQ, 6MWT, and lung function. Mean SGRQ was reduced by 24 units (p=0.001), and 6MWT was increased by 78 metres (p=0.001). Mean FEV1 was increased by 4% (p=0.006), and residual volume and TLC were reduced by 25% and 11% (p=0.009 and 0.01), respectively. Significant improvement in QoL was reported in 13 patients while 11 reported improvement/slight improvement.
Conclusion
EBV is an effective and safe therapy that improves lung function, exercise capacity, and QoL in selected patients with emphysema. Further studies on a larger population need to confirm our findings.
Grant Support: Nil
Conflict of Interest: None.
Keywords
Severe emphysema, endobronchial valve, quality of life
TO 139
BRONCHIAL THERMOPLASTY REDUCES GAS TRAPPING IN SEVERE ASTHMA
Langton D1,3, Ing A2,4, Bennetts K1, Thien F3,5, Peters M2,4, Wang W3, Farah C2,4
1Frankston Hospital, Melbourne, Australia, 2Macquarie University, Sydney, Australia, 3Monash University, Clayton, Australia, 4Macquarie University Hospital, Sydney, Australia, and 5Eastern Health, Box Hill, Australia
Introduction/Aim
In randomized controlled trials, bronchial thermoplasty (BT) has been proven to reduce symptoms in severe asthma. The mechanisms by which this is achieved are still uncertain as no improvement in spirometry is observed in most studies. We postulated that BT might improve lung mechanics by altering airway resistance in the small airways of the lung in ways not measured by FEV1. This study aimed to evaluate changes in measures of gas trapping particularly the Residual Volume (RV).
Methods
A prospective cohort of 32 consecutive patients with severe asthma who were listed for BT at two tertiary institutions (Frankston Hospital and Macquarie University Hospital) were evaluated at three time points, namely baseline, and then 6 weeks and 6 months post completion of all procedures. At each evaluation, medication usage, symptom scores (Asthma Control Questionnaire, ACQ‐5) and exacerbation history were obtained, and lung function was evaluated by (i) spirometry (ii) gas diffusion (DLCO) and (iii) static lung volumes by body plethysmography.
Results
ACQ‐5 improved from 3.0±0.8 at baseline to 1.5±0.9 at 6 months (mean±SD, p<0.001). Daily reliever salbutamol usage improved from 8.3±5.6 to 3.5±4.3 puffs per day (p<0.001). Exacerbation frequency and maintenance oral corticosteroid usage also significantly declined (p<0.001), but no changes in any spirometric parameter were demonstrated. DLCO was also unaltered by BT treatment. However, a significant reduction in gas trapping was observed with RV falling from 146±37% predicted to 136±29%predicted (p,0.002, paired t test). Significant improvements in TLC and FRC were also observed. These changes were evident at the 6 week time period and maintained at 6 months. The change in RV was negatively correlated with the baseline FEV1, r=‐0.474, p=0.006, indicating that the greatest improvement was evident in the most obstructed patients.
Conclusion
Bronchial thermoplasty appears to improve gas trapping and this effect is greatest in the most severely obstructed patients. The improvement may relate to changes in the mechanical properties of small airways that are not measured with spirometry.
Grant Support: Nil
Lung Cancer
TO 140
EPITHELIAL MESENCHYMAL TRANSITION (EMT) AND NON‐SMALL CELL LUNG CANCER (NSCLC): A MUTUAL ASSOCIATION WITH AIRWAY DISEASE
Mahmood M1, Ward C2, Muller H3, Sohal S4, Walters E5
1NHMRC Centre for Research Excellence in Chronic Respiratory Disease and Lung Ageing, School of Medicine University of Tasmania Hobart, Australia, 2Institute of Cellular Medicine Newcastle University Newcastle upon Tyne, Tyne and Wear, UK, and 3Faculty of Health, School of Health Sciences University of Tasmania Launceston, Australia
Introduction/Aim
COPD and smoking play a vital role in development of NSCLC. Local progression and metastasis of NSCLC has been associated with epithelial mesenchymal transition (EMT), which is implicated in COPD pathogenesis.
Methods
We have investigated EMT biomarkers (S100A4, Vimentin, and N‐cadherin), an epithelial activation marker (EGFR) and a vascularity marker (Type‐IV collagen) in surgically resected tissue from patients with NSCLC (adeno‐ and squamous cell carcinoma), and compared them with corresponding non‐tumorous airways.
Results
EGFR, S100A4, vimentin, N‐cadherin expression was higher in tumour cells, at the peripheral leading edge of NSCLC when compared with centrally located tumour cells of same subjects (P<0.01). Same was with Type‐IV collagen expressing blood vessels. EGFR and S100A4 expression was related to differentiation status (P<0.05) and TNM stage (P<0.05) of NSCLC. Moreover, EMT markers in the leading edge were significantly related to airway EMT activity, while peripheral edge vascularity of squamous cell‐carcinoma only was significantly related to large airway Rbm vascularity (P<0.05).
Conclusion
EGFR and EMT‐related protein expression was remarkably high at peripheral leading edge of NSCLCs and related to tumour characteristics associated with poor prognosis. The relationships between EMT‐related tumour bio‐marker expression and those in the airway epithelium and Rbm, provides a background for utility of airway changes in clinical settings.
Grant Support: This study was funded by National Health and Medical Research Council (NHMRC) grant 1001062
Conflict of Interest: Authors declare no conflict of interest.
TO 141
Health‐related quality of life ‐ Queensland Lung Cancer Screening Study
Marshall H1, Passmore L1, Elizabeth M1, Yang I1, Bowman R1, Fong K1
1The University of Queensland Thoracic Research Centre, Department of Thoracic Medicine, The Prince Charles Hospital, Brisbane, Australia
Introduction/Aim
Lung cancer screening has a high false positive rate, carrying the potential for negative psychological impact. We report health‐related quality of life (HRQoL) from the first year of screening in the Queensland Lung Cancer Screening Study (QLCSS).
Methods
QLCSS screened 256 healthy volunteers aged 60‐74 with extensive current or former smoking history (pack years ≥30, quit <15 years prior). Scan results were defined based on 12 months follow‐up: false‐positive scans (FP) were lung cancer–free at 1 year; true‐positives (TP) were not. There were no false negatives. Global health status (physical and mental function) was assessed using a 4‐week recall period at baseline (pre‐screening), 1 month, 6 months and 12 months after baseline screening scan using the Short Form 12 version 2.0 (SF‐12). SF‐12 contains twelve questions. Aggregate summary measures (Mental Component Summary (MCS) and Physical Component Summary (PCS)) were calculated using factor weights derived from a 1998 US general population sample. MCS and PCS range between 0 and 100; higher values indicate better health. The Minimally Important Difference determined clinically meaningful differences (MID = half of a standard deviation (SD) of the mean).
Results
Response to each questionnaire was ≥88% (table 1). Baseline mean (SD) for MCS and PCS were 54.82 (6.83) and 49.90 (7.72) respectively. MCS was above or at the general population norm in 91%; PCS was above or at the norm in 76%. Small changes, below MID, were seen in FP and Negative groups at most time‐points (Figure 1). Larger changes were seen in TP group, however, the number of responses was very small.
Conclusion
Screening was associated with small measurable changes in global HRQoL. There was no clinically meaningful difference between participants with negative or FP scans.
Grant Support: NHMRC, Queensland Government Smart State grant, The Prince Charles Hospital Foundation.
Table 1 Respondents, time point by baseline scan result
| Scan result | Base‐ line | 1 month | 6 month | 12 month |
|---|---|---|---|---|
| False Positive | 123 | 112 | 112 | 115 |
| Negative | 127 | 120 | 111 | 119 |
| True Positive | 5 | 5 | 1 | 2 |
| Missing | 1 | 19 | 32 | 20 |
| Response rate % | 100 | 93 | 88 | 92 |
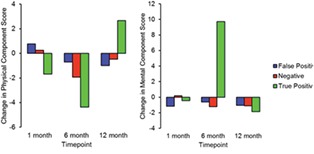
Figure 1 Mean change in Physical Component Score and Mental Component Score from baseline.
TO 142
PLEURAL FLUID CHOLESTEROL IS USEFUL IN DISTINGUISHING EXUDATES FROM TRANSUDATES
Thomas R1,2,3, Cheah H1,2, Muruganandan S1,2,3, Kendrew P4, Creaney J2,5, Lee Y1,2,3
1Pleural Medicine Unit, Institute for Respiratory Health, Perth, Western Australia, Australia, 2School of Medicine, University of Western Australia, Perth, Western Australia, Australia, 3Department of Respiratory Medicine, Sir Charles Gairdner Hospital, Perth, Western Australia, Australia, 4PathWest Laboratory Medicine, QE II Med Ctr, Perth, Western Australia, Australia, and 5National Centre for Asbestos Related Diseases, Perth, Western Australia, Australia
Introduction/Aim
Light's criteria is the gold standard for distinguishing between exudative and transudative pleural effusions (98% sensitivity, 80% specificity). The usefulness of pleural fluid cholesterol to improve diagnostic accuracy compared to Light's criteria is unclear. This study aims to determine i) the level of pleural fluid cholesterol and triglyceride and b) its use in distinguishing exudates from transudates.
Methods
Pleural fluid was prospectively collected from 110 consecutive pleural effusion cases. The fluid was analysed by an accredited laboratory (PathWest, WA) for protein, lactate dehydrogenase (LDH), cholesterol and triglycerides. Aetiology of the effusion was independently verified based on clinical, radiological and pathological assessment. The effusion was classed as an exudate (89) or transudate (21) based on final aetiology.
Results
Exudates were mainly due to malignancy (68 including 13 lung, 6 breast, and 26 mesothelioma effusions), pleural infections (6) and benign pleuritis (5). Transudates were secondary to heart failure (16), hepatic hydrothorax (4) and peritoneal dialyses (1). Exudates had higher pleural fluid protein [median 41.5 (IQR 36‐46) g/dL], LDH [314 (203‐611) mmol/L], cholesterol [2.08 (1.67‐2.61) mmol/L] and triglycerides [0.36 (0.24‐0.57) mmol/L] compared to transudates with fluid protein [21 (13‐26)], LDH [88 (72‐115)], cholesterol [0.66 (0.45‐0.97)] and triglycerides [0.2 (0.16‐0.33)]. Cholesterol and triglyceride were highest in malignant [mean 2.18 (SD 0.76) and 0.47 (0.36), respectively] and parapneumonic [1.93 (0.47) and 0.35 (0.09)] effusions. Strong Spearman correlation was found between fluid cholesterol and protein (0.798, p<0.0001) as well as fluid:serum protein ratio (0.752, p<0.0001). Exudates were identified with a high discrimination (accuracy 95.5%, sensitivity 96.7% and specificity 90.5%) when fluid protein (>35), LDH (>225) and cholesterol (>1.5) with modified cut‐offs were combined.
Conclusion
Pleural fluid cholesterol and triglyceride levels are higher in exudates, particularly malignant and parapneumonic effusions. A combined fluid protein, LDH and cholesterol criteria is useful in distinguishing exudates from transudates.
Grant Support: NHMRC; Cancer Council WA (RT, YCGL, JC); Cancer Australia; NSW Dust Diseases Board (YCGL, JC); Sir Charles Gairdner Research Advisory Group (YCGL).
Conflict of Interest: All authors declare no conflict of interests.
TO 143
SIX‐WEEK EXERCISE INTERVENTION IN PATIENTS WITH MALIGNANT PLEURAL DISEASE IMPROVES PHYSICAL FUNCTION, MUSCULAR STRENGTH AND APPENDICULAR LEAN MASS
Peddle‐McIntyre C1, Jeffery E1, Lee G2,3,4, Nowak A4,5,6, Nguyen B5, Newton R1,7
1Exercise Medicine Research Institute, Edith Cowan University, Joondalup, Australia, 2Respiratory Department, Sir Charles Gairdner Hospital, Nedlands, Australia, 3Institute for Respiratory Health, Nedlands, Australia, 4School of Medicine and Pharmacology, University of Western Australia, Nedlands, Australia, 5Medical Oncology Department, Sir Charles Gairdner Hospital, Nedlands, Australia, 6National Centre for Asbestos Related Diseases, Nedlands, Australia, and 7UQ Centre for Clinical Research, The University of Queensland, Herston, Australia
Introduction/Aim
To investigate the feasibility and efficacy of exercise to improve physical functioning, body composition, and patient‐rated outcomes in patients with malignant pleural disease (MPD).
Methods
Thirty‐three patients with MPD were recruited to complete an exercise training intervention. The exercise intervention included progressive resistance exercise training three times/week for six‐weeks. Outcomes assessed at baseline and post‐intervention included muscular strength (1‐repetition maximum leg press), functional capacity (6‐Minute Walk Test), physical functioning (Timed Up and Go), body composition (DXA scan), quality of life (Short‐Form 36 Health Survey), ratings of intervention burden and acceptability (7‐point Likert scale; 1, not at all, to 7, very much). Paired T‐test or Wilcoxon Signed Rank Test was used to assess changes over time.
Results
Mean participant age was 64 (SD =11) years. The majority had mesothelioma (93%), ECOG performance status 0‐1 (97%), and were male (70%), and sarcopenic (56%). Twenty‐six participants (79%) completed the intervention; 24 (73%) completed all post‐intervention assessments. Median adherence to supervised exercise was 100% (range 6%‐100%). Median ratings of trial evaluation were high (i.e., 7/7 for all measures) and intervention burden were low (i.e., <1.5/7 for all items). Post intervention, significant improvements were found for mean six‐minute walk distance (+59 m; 95% CI 24‐93; p<0.05), 1‐repetition maximum leg press (+17 kg; 95% CI 11‐23; p<0.001), timed up and go (‐0.51 sec; 95% CI ‐0.94 ‐ ‐0.08; p<0.05), chair rise (‐1.5 sec; 95% CI ‐2.2 ‐ ‐0.9; p<0.001), and appendicular lean mass/height squared (+0.19 kg/m2; 95% CI 0.04 – 0.34; p<0.05). For patient‐rated outcomes, only the mental health subscale of SF‐36 changed significantly (median change +2.6, IQR 0.0, 5.2; p<0.05).
Conclusion
Progressive resistance exercise training is a feasible intervention with measurable health benefits for patients with MPD.
Grant Support: Cancer Council Western Australia, Edith Cowan University
Conflict of Interest: All authors declare no conflict of interests.
TO 144
TARGETED PROFILING OF EBUS BRUSHINGS IDENTIFIES MOLECULAR DRIVERS IN NSCLC
Vannitamby A1, Makadia T1, Irving L2, Steinfort D2, Bozinovski S1
1RMIT University, Bundoora, Australia, and 2Royal Melbourne Hospital, Parkville, Australia
Introduction/Aim
Radial Endobronchial Ultrasound (EBUS) bronchoscopy in conjunction with rapid‐on‐site examination (ROSE) is a procedure that routinely achieves an adequate diagnostic yield to identify malignant cells. This study aims to improve the diagnostic value of EBUS bronchial brushings by screening these specimens for molecular changes that can identify therapeutic targets. More specifically, to assess the feasibility of using EBUS bronchial brushings to detect differentially expressed tumour markers using Taqman Low Density Array (TLDA) RT‐qPCR.
Methods
Single pass radial EBUS brushings from Non‐Small Cell Lung Cancer (NSCLC) patients (n=15) were collected following ROSE confirmation of the malignant site at the Royal Melbourne Hospital. Final diagnoses included adenocarcinoma (n=10) and squamous cell carcinoma (SCC, n=5). As a control, benign brushings were collected from clinic‐radiologic confirmed interstitial lung disease patients (n=14). Isolated DNA and RNA from individual brushings were used for TLDA gene expression analysis to determine the fold change of several tumour markers (FGFR1, PD‐L1, PTEN, RICTOR, MET and MMP‐9) and Next Generation Sequencing (NGS) using the Illumina TruSight 15 panel. Statistical significance was assessed by performing Mann Whitney t tests to compare unpaired groups.
Results
Fold change values were higher for PD‐L1 (mean±SEM: 6.24±1.73, p<0.04), FGFR1 (3.44±1.30, p<0.02), RICTOR (1.51±0.23, p<0.02) and MMP‐9 (33.79±7.38, p<0.0001) in the malignant brushings relative to the benign brushings. According to tumour type a fold increase in PD‐L1 (8.50±2.26, p<0.02), RICTOR (1.84±0.28, p<0.003) and MET (3.51±1.38, p<0.005) were observed in adenocarcinomas vs. SCCs. FGFR1 levels were higher (6.86±4.5 fold, p<0.02) and PTEN levels were lower (0.64±0.12 fold, p<0.001) in SCCs vs. adenocarcinomas. The malignant nature of the lesions were confirmed by NGS, identifying common mutations in p53 (10/15 patients), Kras (2/15), EGFR (2/15) and PI3K (3/15).
Conclusion
These findings demonstrate that targeted RT‐qPCR profiling can identify molecular abnormalities in EBUS bronchoscopy brushings collected from ROSE confirmed malignant lesions. Further investigation is warranted as to whether RT‐qPCR can be used clinically to guide individualised therapeutic options.
Grant Support: National Health and Medical Research Council (NHMRC) and Australian Research Council (ARC).
TO 145
RADIATION THERAPY AUGMENTS THE EFFICACY OF IMMUNOTHERAPY IN NON‐SMALL CELL LUNG CANCER: A CASE‐CONTROLLED STUDY
Samaranayake C1, Coucher J2, McCaffrey E3, Lehman M4, Murphy M1
1Department of Respiratory and Sleep Medicine, Princess Alexandra Hospital, Brisbane, Australia, 2Department of Radiology, Princess Alexandra Hospital, Brisbane, Australia, 3Department of Medical Oncology, Princess Alexandra Hospital, Brisbane, Australia, and 4Department of Radiation Oncology, Princess Alexandra Hospital, Brisbane, Australia
Introduction/Aim
Preclinical studies have demonstrated that radiation acts as an immune stimulus, facilitating immune mediators to enable anti‐tumour responses. Impact of previous radiation therapy to the chest on the efficacy and safety of nivolumab in patients with advanced non‐small cell lung cancer (NSCLC) is unknown.
Methods
Consecutive series of patients who received nivolumab for advanced NSCLC on an intention‐to‐treat basis over a 30 months period between January 2015 and June 2017 at a large thoracic‐oncology unit were identified. Outcomes in patients who had received radiation therapy to the chest as part of previous treatment prior to commencing nivolumab (RT group, n=20) were compared to an age, gender, tumour histology and performance status matched cohort of patients who did not receive previous radiation therapy (non‐RT group, n=20).
Results
The RT group had received a mean 53.3Gy (SD 12.3) at a median of 12.4 months prior to commencing nivolumab. The median progression free survival (PFS) was 3.4 months (95%CI 2.2‐4.5) in the RT group compared to 1.3 months (95%CI 1.0‐1.7) in the non‐RT group (p=0.01). The median overall survival was 8.4 months (95%CI 5.1‐11.6) in the RT group compared to 4.2 months (95%CI 1.0‐7.7) in the non‐RT group (p=0.08). The disease response on the initial assessment following starting nivolumab included nine (45%) patients who had stable disease or partial response in the RT group compared to five (25%) in the non‐RT group after a median of four cycles of therapy. Rate of immune related complications were 35% (n=7) and 15% (n=3) in the RT and non‐RT groups respectively (p=0.1). The RT group had a higher mean smoking pack years.
Conclusion
This study demonstrates a novel finding of previous radiation therapy to the chest resulting in significantly higher PFS in patients treated with nivolumab for advanced NSCLC. A trend towards a higher rate of immune related adverse effects seen in the RT group may due to increased activity of the immunotherapy in these patients.
Grant Support: Nil
OLIV 2
TO 146
NINTEDANIB LONG‐TERM EFFICACY IN IPF IS MAINTAINED IRRESPECTIVE OF DOSE
Goh N1, Crestani B2, Kolb M3, Wallaert B4, Quaresma M5,6, Stansen W6, Richeldi L7
1Austin Health, Australia, 2Hôpital Bichat, Pneumologie, Paris, France, 3McMaster University, Hamilton, Canada, 4University Hospital of Lille, Lille, France, 5Center for Interstitial and Rare Lung Diseases, Pneumology, Thoraxklinik, University of Heidelberg, and Translational Lung Research Center Heidelberg, German Center for Lung Research, Heidelberg, Germany, 6Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany, 7Catholic University of the Sacred Heart, Rome, Italy
Introduction/Aim
In Phase III INPULSIS® trials, nintedanib significantly reduced annual rate of FVC decline versus placebo in patients with IPF (−113.6 versus −223.5 mL/year). In an extension trial (INPULSIS‐ON), patients who completed treatment and follow‐up visit in INPULSIS® could receive open‐label nintedanib. In INPULSIS‐ON, patients receiving nintedanib or placebo 150mg twice‐daily (bd) at the end of INPULSIS® received nintedanib 150mg bd; patients receiving nintedanib or placebo 100mg bd received nintedanib 100mg bd or 150mg bd, based on discussion between the patient and the investigator. Dose reduction to 100mg bd was allowed to manage adverse events; re‐escalation to 150mg bd was permitted. We assessed the influence of nintedanib dose on FVC decline in INPULSIS‐ON.
Methods
Annual rates of FVC decline over 96 weeks in INPULSIS‐ON were assessed in patient subgroups (treated with nintedanib 150mg bd; 100mg bd; or both). Slope of FVC decline was calculated using all available FVC measurements collected between baseline and week 96 in INPULSIS‐ON. The first patient was enrolled in July 2012. Analyses were descriptive, based on a data snapshot in October 2015.
Results
Of 734 patients treated, 436 (59.4%), 53 (7.2%) and 245 (33.4%) received 150mg bd, 100mg bd and both doses, respectively. Adjusted annual rates±SEM of FVC decline over 96 weeks were −116.4±8.9, −79.0±30.1 and −126.2±11.4 mL/year in patients treated with nintedanib 150mg bd, 100mg bd and both doses, respectively. Annual rates of FVC decline in all subgroups were consistent with annual rate of FVC decline over 96 weeks in all treated patients (−117.8±6.8 mL/year).
Conclusion
Annual rate of FVC decline was similar in patients treated with nintedanib 150mg bd, 100mg bd or both. Long‐term efficacy of nintedanib in reducing disease progression was maintained in patients with IPF who required dose adjustments to manage adverse events.
Grant Support: The INPULSIS‐ON trial was funded by Boehringer Ingelheim.
Declaration of interest statement: NG has received speaker fees from Boehringer Ingelheim, AstraZeneca, Menarini and Novartis and consultation fees from Boehringer Ingelheim and Roche. BC has received grants, personal fees and non‐financial support from Roche/InterMune and Boehringer Ingelheim; personal fees and non‐financial support from Sanofi; grants from Cardif, LVL and MedImmune, and personal fees from AstraZeneca. MK has received grants and personal fees from Roche, Boehringer Ingelheim, GlaxoSmithKline, Gilead, Prometic and Alkermes; grants from Actelion, Respivert and Synairgen; and personal fees from AstraZeneca and Genoa. BW has nothing to disclose. MQ and WS are employees of Boehringer Ingelheim. LR served on the scientific advisory boards of InterMune, Boehringer Ingelheim, FibroGen, GlaxoSmithKline, Sanofi‐Aventis, Anthera, Genentech, MedImmune, Takeda, UCB, and Promedior and as a trial Principal Investigator for Boehringer Ingelheim, InterMune, Gilead, Roche, Takeda, and UCB; received research grants from InterMune, Biogen, Italian Ministry of Health, Italian National Drug Agency, and Wellcome Trust and speaker's fees from InterMune, Boehringer Ingelheim and Cipla.
TO 147
HIGH RESOLUTION CT‐BASED CHARACTERIZATION ANALYSIS OF IDIOPATHIC PULMONARY FIBROSIS
Zhang Y1, Clark A1, Kumar H1, Milne D2, Wilsher M2, Bartholmai B3, Tawhai M1
1Auckland Bioengineering Institute, University of Auckland, Auckland, New Zealand, 2Auckland City Hospital, Auckland, New Zealand, and 3Department of Radiology, Mayo Clinic, Rochester, USA
Introduction/Aim
Idiopathic pulmonary fibrosis (IPF) is the most aggressive and frequent form of idiopathic interstitial pneumonias. Progression of IPF is variable between individuals and no established quantitative tools exist to assess its development. This work aims to integrate information from volumetric imaging with pulmonary function tests using a predictive computational model under the hypothesis that abnormalities on volumetric are not sufficient to explain increased lung stiffness and decreases in DLCO.
Methods
Tissue regions in HRCT images from 8 patients with IPF were quantitatively analysed. Tissue abnormalities were classified using CALIPER (Computer‐Aided Lung Informatics for Pathology Evaluation and Ratings) software. Tissue density (TD) distribution and volume of tissue (classified as reticular, ground‐glass, normal and emphysema in each lung) were calculated. The classified data were mapped to a statistical shape model, which allows consistent comparison of regional tissue properties between patients or within one patient at different time points. Ventilation distribution and gas exchange were simulated in a computational model that was parameterised to each subject's lung tissue characterisation, to predict the relationship between V‐Q matching, DLCO and disease distribution.
Results
Fibrosis usually has a consistently higher TD (0.34/0.41 for reticular/ground‐glass) compared to normal tissue (0.28), and presents predominantly in lower lobes (72%, 58%, 65% for honeycomb, reticular, ground‐glass). In contrast, emphysema has lower density (0.08) and appears predominantly in upper lobes (73%). Model predictions of ventilation distribution and DLCO show that V‐Q mismatch occurs due to redistribution of ventilation away from diseased regions, contributing to observed DLCO decreases.
Conclusion
A quantitative analysis of the spatial distribution of IPF disease coupled with functional models provides a potential tool to improve assessment of the contributors to decline in IPF patient status over time. Decline in DLCO is a function of regional lung stiffness due to disease location combined with a redistribution of ventilation to ‘normal' lung tissue.
Grant Support:
TO 148
THE INTERSTITIAL LUNG DISEASE MULTI‐DISCIPLINARY MEETING: 3 YEAR REVIEW OF A NOVEL STATEWIDE TELEMEDICINE MODEL
Balzat L1, Chamber D1,2, Godbolt D3, Reddy T4, Keir G5, Sivakumaran S6, Bint M7, Bancroft S1, Hopkins P1,2
1Queensland Lung Transplant Service, The Prince Charles Hospital, Brisbane, Australia, 2School of Medicine, University of Queensland, Brisbane, Australia, 3Anatomical Pathology, The Prince Charles Hospital, Brisbane, Australia, 4Radiology Department, The Prince Charles Hospital, Brisbane, Australia, 5Department of Respiratory Medicine, The Princess Alexandra Hospital, Brisbane, Australia, 6Department of Respiratory Medicine, Gold Coast University Hospital, Gold Coast, Australia, and 7Department of Respiratory Medicine, Sunshine Coast University Hospital, Sunshine Coast, Australia
Introduction/Aim
A multidisciplinary meeting (MDM) model of care is recommended by TSANZ for the diagnosis and initial management of interstitial lung disease (ILD). In order to ensure equity of access to the required expertise, we established an ILD‐MDM at Prince Charles Hospital (TPCH) in Brisbane which facilitated telemedicine and active participation of sites from elsewhere in Queensland.
Methods
We reviewed all cases presented at the ILD‐MDM from July 2014 to June 2017. The ILD‐MDM included a minimum of 2 expert thoracic physicians, 1 radiologist and 1 histopathologist.
Results
313 referrals from 38 clinicians and 11 institutions were discussed. 38.3% were female, mean age 67 years, and 24.9% were from outside TPCH, including 1.9% from private practice. Mean FVC was 74.0% and carbon monoxide diffusion capacity 51.5%. Overall, 111 cases (35.5%) were classified as idiopathic pulmonary fibrosis (IPF) and 17 (5.4%) as combined pulmonary fibrosis and emphysema, with the majority eligible for antifibrotic medication. 18 (5.8%) were classified as connective tissue disease, 12 (3.8%) chronic hypersensitivity pneumonitis, whilst 18.2% remained unclassifiable. There were 105 (33.5% patients) surgical lung biopsies (SLB) reviewed with 79% performed prior to first MDM presentation. In patients with a first presentation diagnosis of IPF, 65.6% had not had a prior SLB. 71 cases (22.7%) had high‐resolution computed tomography (HRCT) reported as usual interstitial pneumonia (UIP), a further 130 (41.5%) as possible UIP and 4.5% had inadequate imaging. Of 61 SLB showing definite UIP pattern, 63.9% had possible UIP and 19.7% UIP pattern on HRCT. In 22% of initial case presentations (n=69), further investigations were recommended including surgical lung biopsy (n=30), HRCT (n=26), bronchoscopy (n=4) and extended autoimmune screen (n=9).
Conclusion
A telemedicine model is feasible and can facilitate equity of access for patients and clinicians where a low volume ILD caseload &/or absence of expertise precludes local establishment of the ILD‐MDM.
Grant Support: Roche Pharmaceuticals $20,000.
Declaration of interest: None.
TO 149
ACHIEVING THE MINIMAL IMPORTANT DIFFERENCE FOLLOWING EXERCISE IN ILD
Dowman L1,2,3, McDonald C2,3, Hill C1,3, Lee A3,4, Burge A3,4,5, Holland A3,4,5
1Physiotherapy Department, Austin Health, Heidelberg, Australia, 2Department of Respiratory and Sleep Medicine, Austin Health, Heidelberg, Australia, 3Institute for Breathing and Sleep, Heidelberg, Australia, 4Department of Rehabilitation, Nutrition and Sport La Trobe University, Bundoora, Australia, 5Physiotherapy Department, Alfred Health, Prahran, Australia
Introduction/Aim
Exercise training delivers significant short‐term improvements in functional exercise capacity, symptoms and quality of life, across the range of interstitial lung diseases (ILD)s, but to what extent do individuals experience a clinically significant benefit? This study aimed to establish the proportion of patients achieving the minimal important difference (MID) in 6‐minute walk distance (6MWD) and in the dyspnoea and fatigue domains of chronic respiratory questionnaire (CRQ).
Methods
Data from 142 participants with ILD [61 idiopathic pulmonary fibrosis (IPF), 22 asbestosis, 23 connective tissue disease‐related ILD (CTD‐ILD) and 36 with ILD of other aetiologies] randomised to either eight weeks of supervised exercise training or usual care were reviewed. We compared the percentages of patients who achieved the MID for 6MWD for ILD (29‐34m), CRQ dyspnoea (2.5 points) and CRQ fatigue (2.0 points) between exercise training and control group for the entire ILD population and each subgroup (IPF, asbestosis and CTD‐ ILD) using Pearson chi2.
Results
Following exercise training at least a third of participants achieved improvements in 6MWD that exceeded the MID, increasing to 43% and 55% in the IPF and asbestosis subgroups respectively (see Table). Compared to the control group, a greater percentage of participants achieved improvements that exceeded the MID for CRQ dyspnoea and fatigue for the entire ILD sample, IPF and asbestosis; this was significantly greater than the control group for CRQ fatigue. Improvements that exceed the MID were limited in CTD‐ILD and more likely occur in CRQ dyspnoea and fatigue than 6MWD.
Conclusion
A third to a half of participants with ILD achieve clinically meaningful improvement following exercise training, including those with IPF, the most devastating of all ILDs. Fatigue and 6MWD appear more responsive to change than dyspnoea.
Grant Support: This abstract is funded by the ATS Foundation/Pulmonary Fibrosis Foundation, National Health and Medical Research Council, Eirene Lucas Foundation and Institute of Breathing and Sleep.
Table 1 Percentage of participants who achieved the MID following the intervention
| Whole ILD | IPF | Asbestosis | CTD ILD | |||||
|---|---|---|---|---|---|---|---|---|
| 6MWD | ||||||||
| Control | 15% | p =0.01 | 11% | p=0.05 | 0% | p=0.006 | 9% | p=0.1 |
| Exercise training | 33% | 43% | 55% | 10% | ||||
| CDRQ Dyspnoea | ||||||||
| Control | 30% | p=0.1 | 35% | p=0.1 | 27% | p=0.6 | 18% | p=0.3 |
| Exercise training | 42% | 53% | 57% | 40% | ||||
| CDRQ Fatigue | ||||||||
| Control | 23% | p<0.001 | 27% | p=0.03 | 18% | p=0.07 | 36% | p=0.8 |
| Exercise training | 55% | 57% | 55% | 40% | ||||
p <0.05 compared to control group; ILD, interstitial lung disease; CTD ILD, connective tissue disease‐related ILD; IPF, idiopathic pulmonary fibrosis.
TO 150
CARDIOVASCULAR SAFETY OF NINTEDANIB IN SUBGROUPS BY BASELINE CARDIOVASCULAR RISK
Corte T1, Noth I2, Wijsenbeek M3, Kolb M4, Bonella F5, Moros L6, Wachtlin D6
1Royal Prince Alfred Hospital, Sydney, Australia, 2Pulmonary and Critical Care Medicine, University of Chicago, Chicago, USA3Erasmus MC, University Medical Centre, Rotterdam, Netherlands, 4McMaster University, Hamilton, Canada, 5Interstitial and Rare Lung Disease Unit, Ruhrlandklinik, University Hospital, University of Duisburg‐Essen, Essen, Germany, and 6Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany
Introduction/Aim
Tyrosine kinase inhibitors may be associated with an increased risk of arterial thromboembolic events. The efficacy and safety of treatment with nintedanib versus placebo in patients with idiopathic pulmonary fibrosis were assessed in the Phase II TOMORROW trial and 2 Phase III INPULSIS® trials. Exclusion criteria included: myocardial infarction in the previous 6 months, unstable angina in the previous month or stroke in the previous year. We assessed the effect of cardiovascular (CV) risk at baseline on the CV safety of nintedanib 150mg twice‐daily.
Methods
Incidence rates of major adverse CV events (MACE) in subgroups of patients with a history of atherosclerotic CV disease (CVD) and/or ≥1 CV risk factor (hypertension, dyslipidemia, body mass index >30 kg/m2, current/former smoking and diabetes) at baseline (higher CV risk) and patients with no history of atherosclerotic CVD and no CV risk factors at baseline (lower CV risk) were analysed using pooled data from the TOMORROW and INPULSIS® trials.
Results
At baseline, 1107 (89.9%) patients (656 nintedanib, 451 placebo) had higher CV risk and 124 (10.1%) patients (67 nintedanib, 57 placebo) had lower CV risk. In patients with higher CV risk, incidence rates (95% CI) of MACE were 3.88 (2.58, 5.84) and 3.49 (2.10, 5.79) per 100 patient–years in the nintedanib and placebo groups, respectively (Figure). In patients with lower CV risk, incidence rates (95% CI) of MACE were 4.78 (1.54, 14.82) and 5.37 (1.73, 16.65) per 100 patient–years in the nintedanib and placebo groups, respectively (Figure).
Conclusion
In pooled data from the TOMORROW and INPULSIS® trials, the incidence of major adverse CV events was similar between nintedanib and placebo groups both in patients with higher and lower CV risk at baseline.

Figure 1
Grant Support: The study was funded by Boehringer Ingelheim.
Declaration of interest statement: TC has received unrestricted educational grants, travel assistance and served on an advisory board for Boehringer Ingelheim and Roche Products Ltd. She has received unrestricted educational grants from Intermune pharmaceuticals and has served on an advisory board for Astra Zeneca. IN has received institutional grants from Centacor, Immuneworks, Actelion and the National Institutes of Health for conduct of clinical trials in IPF; he is supported by the National Institutes of Health, National Heart, Lung and Blood Institute. MW has received speaker and advisory board fees, paid to her institution, from InterMune, Boehringer Ingelheim and Roche, and unrestricted research grant, paid to her institution from InterMune and Roche. MK has received grants and personal fees from Roche, Boehringer Ingelheim, GSK, Gilead, Prometic and Alkermes; grants from Actelion, Respivert and Synairgen; and personal fees from AstraZeneca and Genoa. FB has received grants and honoraria from Roche/Genentech, InterMune, Boehringer Ingelheim, Serendex and Sekisui Diagnostics. LM and DW are employees at Boehringer Ingelheim.
TO 151
MULITPLE PROGRESSION EVENTS IN PATIENTS WITH IDIOPATHIC PULMONARY FIBROSIS (IPF)
Nathan S1, Costabel U2, Glaspole I3, Glassberg M4, Lancaster L5, J. Lederer D6, A. Pereira C7, Trzaskoma B8, Limb S8, U. Wells A9
1Inova Fairfax Hospital, Falls Church, USA, 2Ruhrlandklinik, University Hospital, University of Duisburg‐Essen, Germany, 3Alfred Hospital and Monash University, Melbourne, Australia, 4University of Miami Miller School of Medicine, Miami, USA, 5Vanderbilt University Medical Center, Nashville, USA, 6Columbia University Medical Center, New York, USA, 7Paulista School of Medicine, Federal University of São Paulo, São Paulo, Brazil, 8Genentech, Inc., South San Francisco, USA, and 9Royal Brompton Hospital, Interstitial Lung Disease Unit, London, UK
Introduction/Aim
Declines in forced vital capacity (FVC), declines in 6‐min walk distance (6MWD) and respiratory hospitalizations are events associated with disease progression and mortality in IPF. The incidence of multiple events in the context of a 52‐week study and in patients (pts) receiving antifibrotic treatment with pirfenidone (PFD) is unknown. To determine the incidence of multiple progression events and the proportion of pts with death subsequent to a progression event in the first 12 months of PFD treatment vs placebo (PBO).
Methods
All pts from the pooled Phase III trials (PFD n = 623; PBO n = 624) were analyzed for incidence of events, defined as relative decline in %predicted FVC ≥10%, absolute decline in 6MWD ≥50 m; respiratory hospitalization, or death from any cause.
Results
The incidence of progression events was driven by declines in FVC (total events, 202 PFD vs 304 PBO) and 6MWD (265 PFD vs 348 PBO). A lower proportion of pts had > 1 event with PFD vs PBO (17.0% vs 30.1%; P < 0.0001; Figure 1). Death following ≥ 1 progression event occurred less often with PFD vs PBO (2.1% vs 6.3%; P = 0.0002).
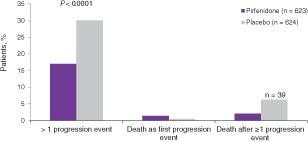
Figure 1 Multiple progression events and death as a first or subsequent progression event in the pooled CAPACITY and ASCEND phase 3 trials (N = 1247). CAPACITY‐004, NCT00287716; CAPACITY‐006, NCT00287729; ASCEND, NCT01366209.
Conclusion
PFD significantly reduced the incidence of multiple progression events and death subsequent to a progression event at 12 months vs PBO. A multiple events–driven approach may have relevance for the design of future IPF clinical trials.
Grant Support
F. Hoffmann‐La Roche Ltd./Genentech, Inc.
Evidence‐Based Medicine & Practice
TO 152
INTERVENTIONS FOR PROMOTING PHYSICAL ACTIVITY IN PEOPLE WITH COPD: A COCHRANE SYSTEMATIC REVIEW
Burge A1,2,3, Cox N1,3, Abramson M4, Holland A1,2,3
1La Trobe University, Melbourne, Australia, 2Alfred Health, Melbourne, Australia, 3Institute for Breathing and Sleep, Melbourne, Australia, and 4Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Introduction/Aim
Increasing awareness of the deleterious health impacts of physical inactivity in people with chronic obstructive pulmonary disease (COPD), coupled with technological developments permitting more accurate measurements, has led to a dramatic increase in studies that aim to improve physical activity participation. This systematic review aimed to evaluate the effectiveness of interventions to promote physical activity in people with COPD.
Methods
Randomised controlled trials of interventions designed to increase physical activity for people with COPD using objective measures for physical activity were identified from the Cochrane Airways Group's Specialised Register (to March 2017). Two review authors independently assessed studies for inclusion and risk of bias, then undertook data extraction. Results are for the primary outcome of steps/day at program completion, using published data.
Results
1950 references were screened, 189 papers assessed and 32 of 72 included studies reported steps/day. The greatest improvements were seen with physical activity counselling and a pedometer (compared to counselling alone, 1 study, mean difference 2942 [95%CI 1881 to 4002] steps/day) and telecoaching (compared to advice alone, 1 study, 1548 [1045 to 2051] steps/day). Significant improvements were also demonstrated with telephone counselling and a pedometer (compared to pedometer alone, 1 study, 1419 [698 to 2140] steps/day) and endobronchial valves (compared to usual care, 1 study, 1400 [655 to 2145] steps/day]). A deterioration in step count was seen following singing classes (compared to film workshops, 1 study, ‐1774 [‐2848 to ‐700] steps/day). Risk of selection and detection bias was generally low, with high or unclear ratings for reporting bias.
Conclusion
A range of interventions, particularly those involving physical activity counselling, can improve physical activity as measured by daily steps. These results suggest that targeted interventions may be useful to improve physical activity in people with COPD.
Grant Support: NHMRC Postgraduate Research Scholarship (ATB)
TO 153
PERIPHERAL VENOUS BLOOD GAS ANALYSIS VERSUS ARTERIAL BLOOD GAS ANALYSIS FOR THE DIAGNOSIS OF RESPIRATORY FAILURE AND METABOLIC DISTURBANCE IN ADULTS
Byrne A, Bennett M3, Pace N4, Thomas P5,6, Symons R5,6, Chatterji R6
1Heart Lung Clinic, St Vincents Hospital, Darlinghurst, Australia, 2Blacktown Hospital, Sydney, Australia, 3Department of Anaesthesia, Prince of Wales Clinical School, University of NSW, Sydney, Australia, 4Department of Anesthesiology, University of Utah, Salt Lake City, USA, 5Department of Respiratory Medicine, Prince of Wales Hospital, Sydney, Australia, and 6University of New South Wales, Sydney, Australia
Introduction/Aim
Whilst arterial blood gas (ABG) is the gold standard for the diagnosis of respiratory failure and metabolic disturbance, the peripheral venous blood gas analysis (PVBG) is increasingly being used. We sought to compare the performance (accuracy) of both tests to diagnose these target conditions.
Methods
We performed an extensive electronic and manual search of the literature for case‐control or consecutive series studies that directly compared the index test (PVBG) to the reference standard (ABG). No language restrictions were applied. Included studies provided outcome data for specified target conditions (pO2, pCO2, pH, HCO3) using generally accepted cut points. Quality assessment was conducted using the QUADAS‐2 tool. The statistical analysis utilized 2x2 tables for each outcomes' positive and negative results and Stata 12 software (Statacorp 2011). The published protocol is available at the Cochrane Database of Systematic Reviews. Article No:CD010841.
Results
We identified 7207 articles with our search strategy following the removal of duplicates. There were 16 studies meeting the inclusion criteria, however only 6 could provide sufficient data for the statistical analysis. Two authors evaluated the quality for these studies which were generally considered a low risk of bias. For (any) respiratory failure, 2 studies demonstrated poor accuracy of the PVBG compared to the ABG. The diagnostic odds ratio (DOR) was 2.73 with 95% confidence intervals 0.14‐55.2. For isolated hypercarbia (6 studies) and metabolic disturbance (3 studies), the PVBG performed well (DOR 35.5 with 95% CI 9.7‐130.2 and DOR 5.8 with 95% CI 1.5‐ 22.2). Meta‐analysis was only able to be performed for hypercapnia. The PVBG showed high sensitivity (95.4%) but low specificity (33.6%) with a high false positive rate (45.8%).
Conclusion
Limited data suggests the PVBG is useful in diagnosing metabolic disturbance but not respiratory failure. For isolated hypercarbia the PVBG has high sensitivity but poor specificity.
Grant Support: Nil
TO 154
DIAGNOSTIC YIELD AND APPROPRIATENESS OF COMPUTED TOMOGRAPHY PULMONARY ANGIOGRAM
Ong Q1, Chen C1, McAnulty K2, Gallagher H1
1Waikato Hospital Respiratory Department, Hamilton, New Zealand, 2Waikato Hospital Radiology Department, Hamilton, New Zealand
Introduction/Aim
International guidelines recommend Computed Tomography Pulmonary Angiography (CTPA) as the gold standard imaging modality for suspected Pulmonary Embolism (PE). Royal College of Radiologist suggests PE should be detected in 15% of CTPA scans. Appropriate requesting of CTPA is important to both establishing an accurate diagnosis and minimizing unnecessary testing and radiation exposure. International and Waikato Hospital guidelines recommend pre‐test probability scoring and D‐dimer assay to stratify patients prior to performing CTPA.
We aimed to determine the overall and departmental diagnostic yield of CTPA at Waikato Hospital. We also aimed to identify whether CTPA were ordered according to current guidelines.
Methods
Medical records of 200 consecutive patients who underwent CTPA for suspected PE from 01 March to 31 May 2017 were retrospectively reviewed. Patient demographics, referral source, clinical risk factors, D‐dimer levels, diagnostic yield and additional CTPA findings were recorded. We utilized an age‐adjusted D‐dimer cut‐off. CTPA images were obtained using either a Siemens 128 or 256 slice multi‐detector CT scanner. Results were compared with international guidelines as well as similar local studies.
Results
41 (20.5%) patients had PE. Orthopaedics had the highest yield (36.4%), followed by Respiratory (32.9%) and General Surgery (18.8%). According to the Wells Score, 74 (37%) patients were low risk while 134 (63%) were High Risk. D‐dimer was done in 108 (54%) patients. 34 (44.7%) patients in the low‐risk group did not have D‐dimer. Two patients who had low wells score and negative D‐dimer received CTPA, neither had PE. Of the 14 patients referred by cardiology, none had positive scans. On review, only one patient had CTPA requested inappropriately (low wells score, D‐dimer not done).
Conclusion
Diagnostic yield of CTPA in Waikato Hospital is consistent with international standard. D‐dimer has not been adequately used as a rule out test. Adherence to diagnostic protocol could potentially improve positive yield.
Grant Support: No funding or financial support was received from any organization.
TO 155
This abstract has been withdrawn


