TSANZ Respiratory Nurses SIG Symposium
TO‐001: Development of a Breathlessness Clinic for Patients with Chronic Obstructive Pulmonary Disease (COPD)
MM Roberts1,2, T Smith1, & JR Wheatley1,2,3
1Department of Respiratory and Sleep Medicine, Westmead Hospital, NSW, Australia, 2Ludwig Engel Centre for Respiratory Research, Westmead Institute for Medical Research, NSW, Australia, 3University of Sydney at Westmead Hospital, NSW, Australia
Introduction
Patients with chronic obstructive pulmonary disease (COPD) are often breathless despite optimal medical care and pulmonary rehabilitation. Breathlessness frequently becomes more disabling as COPD advances and may precipitate hospitalisation. Proactively managing breathlessness may improve patient outcomes.
Aim
To describe the development of a multidisciplinary (MD) non‐pharmacological Breathlessness Clinic for patients with COPD.
Methods
A literature review of evidence‐based non‐pharmacological treatments for breathlessness was undertaken. Two randomised controlled trials (RCT) reported on MD clinics in England focusing on the non‐pharmacological interventions for breathlessness. A travel grant enabled visits to the clinics, to meet with clinicians, identify assessment parameters, treatment options and outcome measures. On return to Australia, a framework for the clinic was refined and a range of resources developed including a Breathlessness DVD and a relaxation CD, and the acquisition of affordable and effective handheld fans and pedometers. In order to evaluate the service, an RCT was designed with an eight‐week wait‐list control to ensure evaluation was planned, standardised and rigorous.
Results
The clinic began accepting referrals in May 2016 with a team consisting of a respiratory physician, specialist respiratory nurses, physiotherapists, occupational therapist, dietitian and clinical psychologist. The target population are patients with documented COPD who remain breathless despite standard care. The primary outcome for the RCT is the Chronic Respiratory Questionnaire mastery of breathlessness subscale. Secondary outcomes include breathlessness intensity and unpleasantness and confidence managing breathlessness measured by a numerical rating scale.
Conclusion
The development of a non‐pharmacological Breathlessness Clinic for patients with COPD has resulted in an exciting option for patients experiencing refractory breathlessness. The RCT will objectively assess the benefit of this intervention for the patients. Patients remaining breathless may be offered additional psychological and/or pharmacological treatment.
Grant Support
Judith Meppem Travel Scholarship 2015
Declaration of interest
Nil
TO‐002: Nurse Led Obstructive Sleep Apnea (OSA) Assessments: Impact of a change to referral criteria
Deborah Box
Clinical Nurse Specialist ‐ Community Respiratory, South Canterbury District Health Board, Timaru, New Zealand
Introduction/Aim
In November 2013 SCDHB introduced nurse lead OSA assessments, however in June 2015 due to high unsustainable demand on the service referral criteria was changed to accept only referrals for patients with high risk for OSA who were likely to reach the thresholdn
The aim is to critically review the referral, demographic and outcome data for patients referred via the sleep pathway in 2015 and compare the data before and after the high risk referral criteria.
Methods
Referral, demographic and outcome data for the calendar year 2015 was analysed and reviewed. The data for referrals from January to June 2015 was compared to the data from July 2015. Comparisons were made of the data.
Results
123 referrals were received in 2015 for OSA nurse assessment with 87 (70%) of the referrals received prior to the new criteria being introduced. Most referrals came from general practitioners (GPs) with referral source not changing. 59% of patients referred prior to the new criteria were discharged to the GP with only 36% with the new criteria.
Conclusion
There was a significant change to the number and quality of referrals resulting in reduced workload in managing patients not likely to meet treatment criteria. With the new criteria the majority of patient outcomes were referral for treatment or a higher level sleep study. This suggests that the new referral criteria results in a more efficient system.
Grant Support
Nil
TO‐003: Presentation re development of newly established Integrated Respiratory Nursing Service in Canterbury
Jenny MCWHA
1Cardio Respiratory Integrated Specialist Service, Respiratory Services, Christchurch Hospital, Canterbury District Health Board, Canterbury, New Zealand
Introduction/Aim
The Canterbury District Health Board aims to provide services which are “better, sooner, and more convenient” for the people of Canterbury.
Historically Canterbury has had three speciality nursing services offering assessment and education to respiratory patients in the community. This has led to confusion as to the role of each nursing service and to which service primary health and hospital staff should refer too. In some cases, this has led to duplication of referrals and service, with at times a referral sent to all three nursing services.
The aim of the project was to integrate three community nursing services, Cardio‐Respiratory Integrated Specialist Service (Christchurch Hospital), the Community Respiratory Service (formally known as Canterbury Initiative) and CanBreathe (local Asthma Society).
To offer a coordinated approach to patient education on COPD and Asthma and streamline access across services.
To stop duplication of referrals across services.
To support primary health to manage complex respiratory patients within their community.
Methods
A small working group of five was set up, with representation from the three respiratory nursing services. They have developed an algorithm outlining the referral pathway to the appropriate nursing service via a single point of entry. The patient intervention takes place in the community, which may include development of management plans and referrals to other health providers. There is increased collaboration with General Practice through education and joint community visits. The group has identified the need for a shared electronic platform to increase visibility of patient outcomes. Healthpathways provides information regarding the Integrated Respiratory Nursing Service, and can be accessed from Primary and Secondary Care.
Results
The project has:
Simplified the referral process with a single point of entry.
Stopped duplication of referrals and service provision.
Increased collaboration between the community nursing providers and general practice.
Conclusion
Development of an Integrated Respiratory Nursing Service now provides a “better, sooner, and more convenient” intervention for the people of Canterbury.
Grant Support
Nil
Nominated for review by Respiratory Nurses SIG
TO‐004: Transforming respiratory care in Hawke's Bay (NZ): Engaging patients as informed partners in their own health care
Sue Ward1, Kate Te Pou 2, Trish Freer3, Julie Shaw4
1Sue Ward, Respiratory Clinical Nurse Specialist, (RCNS)Hawkes Bay District Health Board, Hawke's Bay, New Zealand, 2 Kate Te Pou, Respiratory Clinical Nurse Specialist, (RCNS) Hawkes Bay District Health Board, Hawke's Bay, New Zealand, 3 Trish Freer, Health Programmes Manager, Health Hawke's Bay, Hawke's Bay, New Zealand, 4 Julie Shaw, Nurse Manager, Breathe Hawke's Bay (BHB), Hawke's Bay, New Zealand
Introduction/Aim
Management of respiratory conditions has historically been by secondary care responding to the 20% of acute hospital presentations.
Chronic Obstructive Pulmonary Disease is the 4th leading cause of death in New Zealand.
New Zealand has the 2nd highest prevalence of asthma and associated high death rates; 6 times higher for Pacific, 5 times higher for Maori.
We aimed to form an evidence based pathway of integrated care for patients diagnosed with or suspected to have respiratory disease.
Methods
Early intervention in primary care:
Developing competent workforce
Sector boundaries removed
Service – Practice Nurse Led – performing spirometry across 18 practices.
Spirometry training with annual accreditation – Respiratory Scientist
Mentors for practice nurses – RCNS and BHB
Information technology:‐ Diagnostic support and care planning tool leading to joint care planning.
Priorities
Patient directed education enabling good understanding of their condition
Empowering patients to be active partners in their health and well‐being
Ongoing long term monitoring and support
Results
Obvious growth in patient knowledge and improved quality of life
Improved service quality in primary care leading to greater equity of care
Decrease in secondary service referrals from 658(2012) to 28(2015) for diagnostics
Decrease in bed days by 740 days (2014–2015)
Decrease in length of stay, decrease in emergency presentations/admissions
Significant engagement from high deprivation areas and indigenous people
Improved health literacy
Conclusion
Additional funding for primary care has removed the barrier of cost of accessing early intervention and provided protected time for patient education.
Diagnostic software has assisted health practitioners to standardise best practice intervention ensuring accurate diagnosis, and progression to evidence based care planning, optimising medication, and improving quality of life.
Change management drove itself once staff recognised the benefits to all concerned but particularly for patients.
Patient quote: ‘This has changed my life and given me back my independence…..I didn't think I would ever feel this good ever again’.
TO‐005: Nurses Confidence and Competence in Providing Inhaled Medication Education to Patients
V Swami1 and MM Roberts1,2
1Department of Respiratory and Sleep Medicine, Westmead Hospital, 2Ludwig Engel Centre for Respiratory Research, Westmead Millennium Institute, NSW, Australia
Introduction
Chronic obstructive pulmonary disease (COPD) is a common respiratory disorder. Inhaled medications are widely used to control symptoms and improve the quality of life of patients. Studies have shown that up to 93% of patients with COPD are unable to use their inhaler devices correctly, resulting in inadequate drug deposition. This figure could be higher since the influx of new devices over the past 18 months.
Aim
To assess the confidence and competence of nurses working on a respiratory ward in delivering inhaler device education to patients.
Methods
Subjects were given a questionnaire evaluating confidence in providing inhaler device education to patients. Subjects were asked if supervision of patients taking inhaled medication is required and how often it should be done. Subjects then undertook a competency assessment reviewing the correct steps in using each of the 8 different inhaler devices.
Results
25 subjects (85% female, 8yrs (±7.9) experience in nursing) were enrolled in the study. 96% of subjects reported that patients should be supervised when taking inhaled medications and rated their confidence in inhaler device knowledge as ‘not confident’ (16%), ‘moderate’ (76%) or ‘extremely high’ (8%). No subject could correctly perform all the steps of use for all inhalers. When the steps for all devices were tallied, the average total score of correct steps was 47% (SD ± 17%). There was no correlation between total correct steps and years in nursing, or confidence levels.
Conclusion
Despite confidence, competence and knowledge of the correct steps of inhaler use required to teach inhaler technique to patients is poor amongst a group of respiratory ward nurses. There is a need to provide an ongoing educational intervention to improve the inhaler device competence of nurses working in respiratory medicine so that patients receive education regarding correct inhaler use to optimise disease management.
TO‐006: Respiratory nurses' knowledge and practice behaviours in copd‐related advance care planning: Preliminary findings from a crosssectional survey study
DR Rebecca Disler,1,2 MS Yuxiu Cui,1 DR Tim Luckett,2 DR Doranne Donesky,3 Assoc Prof Louis Irving,4 Prof David Currow,5 Lynn Horsfall,6 DR Natasha Smallwood4
1Sydney Nursing School, The University of Sydney, Sydney, NSW, Australia, 2Centre for Cardiovascular and Chronic Care, Faculty of Health, University of Technology Sydney (UTS), Sydney, NSW, Australia, 3Department of Physiological Nursing, University of California San Francisco, 4Department of Respiratory & Sleep Medicine, Royal Melbourne Hospital, Melbourne Health, Australia, 5Department of Palliative and Supportive Services, Flinders University, Adelaide, South Australia, Australia, 6Emu Creek Health Professionals, VIC, Australia
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive illness that leads to significant morbidity and mortality. Despite high symptom burden, COPD patients have limited access to palliative care, and many are unaware of their prognosis. Advance care planning (ACP) is crucial for patients to make their wishes known if they are unable to speak for themselves in the future. However, ACP is not routine in practice, and many health professionals are reluctant to initiate end‐oflife conversations.
Aims
To explore respiratory nurses' knowledge and practices regarding ACP for patients with COPD.
Methods
ANZ respiratory nurses were invited to participate in an online survey via email listservs and snowballing. Questions covered validated ACP‐related knowledge and practice indicators1. Data were analysed using descriptive statistics, with thematic analysis of free response questions.
Results
Eighty‐nine respiratory nurses participated. Between 64–86 (72–97%) correctly answered 8/10 key knowledge indicators, but 57 (64%) were unsure regarding inter‐state transferability of advance directives (AD) and 38 (42%) incorrectly thought that a formal AD template was necessary to be legally binding. While 54–85 (61–95%) agreed/strongly agreed with 21/23 ACP practice indicators, 22 (25%) were ambivalent regarding personal confidence in communicating ‘bad news’ and only 45 (50%) routinely initiated ACP. Seventy‐four (83%) agreed/strongly agreed that ACP was part of their professional role, but 22 (25%) were ambivalent as to whether ACP was the physician's responsibility and or indeed their own (26, 29%). Thematic analysis identified a need for time, clear guidance and training to be consistent concerns.
Conclusions
While respiratory nurses are well placed to commence ACP with COPD patients, many were uncertain of ACP legislation and unsure which members of the clinical team should engage in ACP discussions. Variation in confidence to undertake ACP suggests the need for further training to help nurses support patients in articulating their wishes.
Status of research at time of abstract submission
Data collection still ongoing.
Grant Support
Nil
Zhou, D. N. P., et al. “Knowledge, attitudes, and practice behaviors of oncology advanced practice nurses regarding advanced care planning for patients with cancer.” (2010): 400.
Declarations
The authors have no conflicts of interest to declare.
With thanks to
TSANZ (State and special interest groups), RCN, PCNA, NZNO, LFA, PCV, SVHA, ADHB, SAFGP, and all those clinicians, that facilitated circulation of this survey, and to Dr Tracy Smith for involvement in study design.
TO‐007: Improving patient flow and reducing bed block during Influenza season in a tertiary hospital
Dunford, M1 , Boston B 1,Cook C 1,Day C1 , Zhou L1 , S O'Brien S 1Keighley C2 Weatherall C1 Lindstrom1
1St George Hospital Kogarah NSW , 2SEALS Microbiology Kogarah NSW
Introduction/Aim
Seasonal influenza places increased demand on the emergency department and hospital resources. Limited single room capacity means that patients often remain in the emergency department >24hours or there is suboptimal ward placement increasing the risk of transmission between both patients and staff.
Methods
This year, patient and clinical decision making was improved due to development of an Influenza flowchart based on current best practice guidelines.1,2 A local clinical business rule was developed and resources disseminated widely. Once single room capacity was exhausted, patients meeting case definition were cohorted in the respiratory ward, a viral swab taken and oseltamivir commenced.3 Cohort rooms on other wards were co‐opted depending on demand.
Results
Improved placement of influenza patients
During June to September 2016 a total of 298 patients were identified as testing positive for influenza A or B. Overall 85% of patients who tested positive, n=252 required admission. Despite high number of influenza admissions 84.5% of patients were isolated correctly (n=213). 25% of total admissions were placed on the respiratory ward with at least 43% of these patients cohorted in a four bedded room (n=28/64).
Decreased length of stay
A four‐fold reduction in the number of patients who stayed in ED for more than 24 hours was apparent over the peak winter month of August despite a higher number of presentations to ED overall.
Improved awareness of influenza symptoms and clinical decisions in line with matrix
Despite a 75% increase in presentations in the peak month of August the increased familiarity with the risk matrix was reflected in improved management of patients. A total of 59.8% of patients (n=178) were given oseltamivir, thus greatly reducing the length of stay in single rooms from 7 to 3 days providing the patient was afebrile. Local hospital data also demonstrated an absence of influenza outbreaks in areas where the matrix was used correctly.
Conclusion
The cohort flowchart directed care and provided guidance to clinicians to ensure the safe and appropriate placement of patients thus reducing the risk of influenza outbreaks. Cohorting reduced demand on respiratory single rooms and emergency department length of stay remained lower than yearly predictions despite higher presentations in 2016.
Grant Support
Nil
REFERENCES
NSW Health. Influenza Control Guideline for Public Health Units. Updated May 1, 2016 http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/influenza.aspx.
NSW Health Influenza Policy. Influenza ‐ Minimising Transmission of Influenza in Healthcare Facilities: 2010 Influenza Season. Updated 22 June 2011 http://www0.health.nsw.gov.au/policies/gl/2010/pdf/GL2010_006.pdf
Australian Drug Information Resource (AusDI). Tamiflu‐ Oseltamivir product summary. http://ausdi.hcn.com.au/productSummary.hcn?id=4418.SimplePS. Updated: 29 September 2016.
Asthma and Allergy 1
TO‐008: Asthma control, airway inflammation and gut microbiome are improved by soluble fibre supplementation
LG Wood1, BS Berthon1, R Zapirain1, LEX Leong2, KJ Baines1, PG Gibson1,3, D Arnold3, GB Rogers2
1Centre for Healthy Lungs, University of Newcastle, Newcastle, NSW, Australia, 2South Australia Health and Medical Research Institute, Flinders University, Adelaide, SA, Australia, and 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, NSW, Australia.
Introduction/Aim
Westernised diets are typically low in fibre, which may be contributing to asthma development and progression. Observational data has shown that a low fibre intake is associated with worse airway inflammation and lung function. To date, there have been no fibre intervention studies in humans with asthma. However in animal models of airway disease, dietary fibre has been shown to modulate the gut microbiome and reduce airway inflammation. This study aimed to investigate the effects of soluble fibre supplementation in asthmatic adults.
Methods
A randomised, placebo controlled 3‐way crossover study in 17 stable asthmatics, using 7 days supplementation with inulin (12g/day), inulin+probiotic (multi‐strain >25 billion CFU) and placebo. Clinical assessment, induced sputum and faecal collection occurred before and after each treatment. Selected sputum was dispersed and total and differential leucocyte counts performed. Faecal bacteria were determined by fluorescent in situ hybridisation and faecal SCFA by HPLC‐MS. Changes in asthma control (ACQ), lung function (FEV1), gut microbiota, SCFAs and induced sputum cell counts were analysed using Wilcoxon signed–rank and Spearman's correlations.
Results
ACQ improved (∆‐0.35(−0.50,‐0.13) (median(IQR)); p=0.006) and sputum eosinophil% decreased (∆‐1.0(−2.5,0.0), p=0.006) following the inulin intervention only. Significant changes in bacterial taxon relative abundance were seen; Bifidobacterium increased following inulin+probiotic supplementation with a trend following inulin supplementation. Anaerostipes increased following both the inulin and inulin+probiotic supplements. An unidentified Erysipelotrichaceae taxon and Roseburia decreased following inulin supplementation only. Total faecal SCFA and acetate showed a trend to increase following inulin supplementation and changes in SCFA were correlated with changes in FEV1 (Rs=0.53, p<0.001; Rs=0.51, p<0.001), sputum eosinophils (Rs=−0.39, p=0.019; Rs=−0.34, p=0.048) and Erysipelotrichaceae (Rs=−0.40, p=0.013; Rs=−0.35, p=0.030).
Conclusion
Short term inulin supplementation beneficially alters gut microbiome, improves asthma control and airway inflammation in asthma. Soluble fibre supplementation warrants further investigation as a potential non‐pharmacological addition to asthma management strategies.
Grant Support
John Hunter Hospital Charitable Trust
TO‐009: New measures of adherence to inhaled therapy in patients with asthma
Chinh D. Nguyen1,2, Juliet M. Foster1, Helen K. Reddel1 and Cindy Thamrin1
1 Woolcock Institute of Medical Research, University of Sydney, Glebe, NSW, Australia, 2Neuroscience Research Australia (NeuRA), Randwick, NSW, Australia
Introduction
Poor adherence is an important contributor to inadequate asthma control. Electronic monitors provide an objective measure of inhaler adherence. Adherence is often expressed as the mean proportion of prescribed puffs taken during the study period, but this may not adequately reflect variations in use over time. This work aims to develop new metrics to examine patterns in both dose and time to better quantify adherence.
Methods
This is a retrospective analysis of previously published data (Foster et al, JACI 2014) comparing subjects with uncontrolled asthma who received inhaler reminders and usage feedback (IRF), designed to improve preventer adherence versus no reminder or feedback (non‐IRF). The adherence of all participants was measured by electronic monitoring. Daily dose records were divided into AM and PM (half‐days). We constructed curves based on the proportion of prescribed puffs taken (dose‐based measure) and whether or not any puff was taken (time‐based measure) over time, and calculated the difference in the area under the actual and expected cumulative curves (AUC). Mann–Whitney test was used to assess differences in these measures between groups.
Results
We examined data from 105 asthma patients with Asthma Control Test (mean±SD) of 14.6±3.4 and age of 41±15 years. IRF patients took more doses on average than non‐IRF patients in the first two months (104.9±89.4 vs 64±40.4% of prescribed dose, p<0.0001). They also had shorter average gaps between doses (2.5±3.4 vs 4.4±6.9 half‐day, p<0.01). Dose‐based and time‐based AUC were higher in IRF‐ compared to non‐IRF‐patients (1.7±62.2 vs −33.2±37.8%, and −21.9±23.9 vs −44.8±28.2% of expected AUC, p<0.0001, respectively).
Conclusion
We have partitioned adherence into dose‐based and time‐based measures. Patients differed both in amount of medication taken as well as gaps between doses. Further study will determine the relationship between these patterns and aspects of symptom control and future risk.
Grant Support
Nil
TO‐010: “I'm a person with asthma…not the asthma first.”: Personal experiences of severe asthma: A review
Daniela Eassey1, Helen Reddel 2, Lorraine Smith1
1Faculty of Pharmacy, University of Sydney, NSW, Australia, 2Woolcock Institute of Medical Research, University of Sydney, NSW, Australia
Introduction/Aim
5‐10% of the asthma population have severe asthma, which is diagnosed when good asthma control is not achieved with high doses of inhaled treatment, or, good control can be achieved only with high dose inhaled treatment. Previous studies have largely focused on the clinical aspects of severe asthma, and there is very little exploring the personal experience of living with the condition. Our aim was to review the qualitative literature examining the personal experiences of adults living with severe asthma.
Methods
We conducted a systematic review to identify qualitative English‐language publications about the personal experience of adults living with severe asthma, excluding studies in which patients were pre‐selected by their participation in other research. A meta‐ethnographic method and comparative thematic analysis approach were adopted.
Results
From 574 articles, five studies met the inclusion criteria. The topics of the included papers were notably medically focussed. There was a paucity of literature on the physical burden of asthma symptoms. Our analysis revealed that the side effects of medications, particularly oral corticosteroids, communication with health care providers, physical and mental burden, and effects on relationships, work and leisure played a dominant role in these experiences. Feeling excluded from decision‐making and being left uninformed about the condition were common experiences.
Conclusion
To our knowledge, this is the first systematic review of the qualitative literature regarding people's experiences of living with severe asthma. Together, these findings suggest the experience of severe asthma poses challenges to personal autonomy and that people with severe asthma make efforts to re‐claim control over their lives. These findings provide important signposts for a deeper exploration of this experience. Our findings suggest there is a paucity of studies exploring the personal experience of living with severe asthma and there is clearly much more to be understood.
Support
CRE for Severe Asthma
TO‐011: Medication adherence in a difficult asthma population
Joy Lee1, Tunn Ren Tay1, Naghmeh Radhakrishna1, Fiona Hore‐Lacy1, Ryan Hoy1, Eli Dabscheck1, Robyn O'Hehir1, Mark Hew1,2
1 Allergy, Immunology & Respiratory Medicine, Alfred Hospital, Melbourne, Australia, 2Public health & Preventive Medicine, Monash University, Melbourne, Australia
Introduction
Medication non‐adherence in asthma may lead to poor asthma control and inappropriate escalation of prescribed treatment. This issue may be particularly significant in patients with difficult‐to‐treat asthma. Since 2014, the Alfred has undertaken systematic evaluation of specialist‐referred patients with difficult asthma. In this population, we examined the feasibility of using an electronic monitoring device (EMD) to measure preventer inhaler adherence, and compared the results with clinician assessment.
Methods
59 consecutive patients with difficult asthma referred by respiratory specialists underwent systematic evaluation at the Alfred between June 2015 and June 2016. Preventer inhaler adherence was assessed by both an electronic monitoring device (Adherium Ltd) and specialist physician and asthma nurse assessment.
Results
The majority of patients were on high‐dose inhaled ICS/LABA combination therapy, with significant impairment of lung function and a high burden of disease. Of 59 patients, 13 patients (22%) had an inhaler incompatible with an EMD, 3 (5%) had an EMD malfunction, 2 (3%) refused to accept an EMD and 7 (12%) did not return the EMD. Of 34 patients who returned useable EMD data, the proportion of patients adherent to preventers > 75% of the time was 68%. In these patients, physician and nursing assessments significantly under‐estimated non‐adherence. Clinician assessment was poorly sensitive (physician 9%, nurse 18%) but highly specific (physician 92%, nurse 90%) at detecting non‐adherence.
Conclusion
In this real‐life study of non‐adherence in difficult asthma, the true rate of non‐adherence is likely to lie between 29% (among patients who returned the device) and 44% (including patients who refused or did not return the device). Clinician assessment of non‐adherence in this cohort was highly unreliable. Objective assessment of inhaler non‐adherence should be an integral part of systematic evaluation in difficult asthma.
Grant Support
The authors acknowledge an unrestricted grant from GSK to fund the electronic monitoring devices. GSK did not contribute to study design, conduct or analysis.
TO‐012: Improving asthma emergency department discharge processes
Tanya Raineri1, Dr Kate Halton2, Dr Adel De Klerk‐Braasch3, Dr Krishna Bajee Sriram4, Melanie Harris4, Dr Peter Anderson1
1Asthma Foundation Queensland and New South Wales, 2Institute of Health and Biomedical Innovation, Queensland University of Technology, 3 Ipswich Hospital, 4Gold Coast Hospital and Health Service
Introduction/Aim
Repeated asthma related emergency department (ED) presentations are associated with an increased risk of life threatening asthma. This study aimed to determine if a streamlined ED discharge process would improve level of asthma control and asthma self‐management behaviours, encourage patients to follow up with their GP and reduce asthma related re‐presentations to EDs.
Methods
We used a controlled cohort study design to evaluate the Asthma ED Discharge Protocol intervention. Patients presenting to the intervention site were provided with a spacer, an education resource (Asthma Control Pack), written prompt to visit GP, comprehensive education and referral to 1800 ASTHMA for follow‐up at 1, 5 and 16 weeks post discharge. Control site patients received usual care and referral to 1800 ASTHMA for follow‐up at 5 and 16 weeks. Data on behavioural and health outcomes was collected for each cohort via telephone follow‐up.
Results
Demographic characteristics at five week contact point:
| Intervention | Control | |
|---|---|---|
| Number of participants | 24 | 16 |
| Female | 75% (18) | 88% (14) |
| Average age (mean s.d.) | 48 (15.7) | 47 (19.6) |
Rapid and significant improvements in level of asthma control and delivery device accuracy are seen when a systematic and formalised discharge process is implemented. Results at five weeks post discharge:
| Intervention | Control | p‐value | |
|---|---|---|---|
| Asthma Control Score 20+ | 79% (19/24) | 19% (3/16) | <0.001 |
| Correct delivery device technique | 96% (23/24) | 44% (7/16) | <0.001 |
| Using spacer | 100% (24/24) | 94% (15/16) | 1.00 |
| Visited GP | 75% (18/24) | 56% (9/16) | 0.22 |
| Received asthma action plan from GP | 22% (4/18) | 33% (3/9) | 0.53 |
The cost of delivering the Asthma ED Discharge Protocol was $96 per participant, representing a cost of $282 per patient with well controlled asthma at five weeks.
Conclusion
Formalising asthma related ED discharge processes shows potential in enhancing longer term asthma management. Patients who received this intervention were four times more likely to have well controlled asthma and twice as likely to use their delivery device correctly.
Grant Support
Australian Centre for Health Services Innovation (AusHSI)
TO‐013: Azithromycin reduces exacerbations in adults with persistent symptomatic eosinophilic asthma
Peter G. Gibson1,2,3, Ian A. Yang4,5, John W. Upham4,6, Paul N. Reynolds7,8, Sandra Hodge7,8, Alan L. James9,10, Christine Jenkins11,12, Matthew J. Peters12,13, Guy B. Marks3, 14, Melissa Baraket15, Heather Powell1,2, Jodie L. Simpson1, 2
1Department of Respiratory & Sleep Medicine, Hunter Medical Research Institute, NSW, Australia., 2Priority Research Centre for Healthy Lungs, University of Newcastle, NSW, Australia, 3Woolcock Institute of Medical Research, NSW, Australia, 4School of Medicine, The University of Queensland, QLD, Australia, 5Department of Thoracic Medicine, The Prince Charles Hospital, QLD, Australia, 6Department of Respiratory Medicine, Princess Alexandra Hospital, QLD, Australia, 7Department of Thoracic Medicine, Royal Adelaide Hospital, SA, Australia, 8Lung Research Laboratory, Hanson Institute, SA, Australia, 9Department of Pulmonary Physiology and Sleep Medicine, Sir Charles Gairdner Hospital, WA, Australia, 10School of Medicine and Pharmacology, University of Western Australia, WA, Aus., 11Respiratory Trials, The George Institute for Global Health, NSW, Australia, 12Faculty of Medicine and Health Sciences, Macquarie University, NSW, Australia, 13Department of Thoracic Medicine, Concord General Hospital, NSW, Australia, 14South Western Sydney Clinical School, UNSW, Australia, 15Respiratory Medicine Department and Ingham Institute, Liverpool Hospital, Australia
Introduction/Aim
Acute exacerbations of asthma cause a significant global burden of illness. Macrolide antibiotics may treat persistent asthma.
Methods
We performed a randomized double‐blind placebo controlled trial to determine whether oral azithromycin decreases the frequency of severe asthma exacerbations in adults with symptomatic asthma despite current use of inhaled corticosteroid (ICS) and long‐acting bronchodilator (LABD), and who had no hearing impairment or prolongation of the corrected QT interval.
Results
We screened 582 patients and randomized 420 to receive azithromycin 500mg (213 patients) or placebo (207 patients) 3 times per week for 48 weeks. Azithromycin reduced severe asthma exacerbations (0.61/patient‐year) compared with placebo (1.07/patient‐year; incidence rate ratio [IRR] 0.59; 95% confidence interval [CI] 0.42, 0.83; p=0.002). In eosinophilic asthma (EA), azithromycin reduced severe asthma exacerbations (IRR 0.40, CI 0.23, 0.69) and reduced the proportion of patients experiencing at least one severe exacerbation (placebo 44.7%, azithromycin 26.7%, p=0.010). Azithromycin reduced exacerbations in EA defined using blood eosinophils (IRR 0.44, CI, 0.23, 0.83), but not in the non‐eosinophilic asthma phenotype (IRR0.92, CI 0.62, 1.37). Diarrhoea was more common in azithromycin treated patients (34% vs 19%, p=0.001). Azithromycin treated patients had fewer respiratory infections (20% vs 36%, p<0.001).
Conclusion
Adults with persistent symptomatic eosinophilic asthma despite ICS/LABD experience fewer severe asthma exacerbations when treated with the addition of oral azithromycin for 48 weeks. With azithromycin, there is an increase in gastrointestinal adverse effects but fewer respiratory infections. Azithromycin can be added to ICS/LABD therapy in persistent eosinophilic asthma to reduce severe asthma exacerbations.
Grant Support
National Health and Medical Research Council of Australia
Declaration of interest
None.
ANZCTR No: 12609000197235
Evidence‐Based Medicine and Practice
TO‐015: Pulmonary Rehabilitation Guidelines for Australia and New Zealand
Jennifer Alison1,4, Zoe McKeough1 , Kylie Johnston2, Renae McNamara3 , Lissa Spencer4, Sue Jenkins5, Catherine Hill6, Vanessa McDonald7 , Peter Frith8, Paul Caferella8, Anne Holland9 on behalf of the Guideline writing group, the Lung Foundation Australia and the Thoracic Society of Australia and New Zealand.
1Discipline of Physiotherapy, Faculty of Health Sciences, University of Sydney, NSW Australia, 2 Physiotherapy Discipline, School of Health Sciences, University of South Australia, SA, Australia, 3Department of Physiotherapy, Prince of Wales Hospital, Sydney, NSW, Australia, 4Department of Physiotherapy, Royal Prince Alfred Hospital, Sydney, NSW, Australia, 5Physiotherapy Department, Sir Charles Gairdner Hospital, Perth, WA, Australia, 6Department of Physiotherapy, Austin Hospital, Melbourne, VIC, Australia, 7School of Nursing and Midwifery, University of Newcastle, Newcastle, NSW, Australia, 8Department of Respiratory Medicine, Repatriation Hospital, Daw Park, Adelaide, SA, Australia, 9 Physiotherapy, Alfred Health and La Trobe University, Melbourne, VIC, Australia,
Introduction/Aim
The aim of the Pulmonary Rehabilitation Guidelines (Guidelines) is to provide evidence‐based recommendations for the practice of pulmonary rehabilitation (PR) specific to Australian and New Zealand (NZ) healthcare contexts.
Methods
A writing group of 28 experts in PR (10 in the lead group), was selected from expressions of interest. The Guideline methodology adhered to the Appraisal of Guidelines for Research and Evaluation (AGREE) II criteria. Nine key questions were constructed in accordance with the Population, Intervention, Comparator, Outcome (PICO) format and reviewed by a COPD consumer group for appropriateness. Systematic reviews were undertaken for each question and recommendations made with the strength of each recommendation based on the Gradings of Recommendations, Assessment, Development and Evaluation (GRADE) criteria. The Guidelines were externally reviewed by a panel of experts (Australian and NZ respiratory physicians, physiotherapists).
Results
In brief, the Guideline panel recommended that people with mild to severe COPD should undergo PR to improve quality of life and exercise capacity and to reduce hospital admissions; that PR could be offered in hospital gyms, community centres or at home, and could be provided irrespective of the availability of a structured education program; that PR should be offered to people with bronchiectasis, interstitial lung disease and pulmonary hypertension, with the latter in specialised centres. Due to insufficient evidence, the Guideline panel was unable to make recommendations relating to: PR program length beyond 8 weeks; optimal model for maintenance after PR; use of supplemental oxygen during exercise training. The Guideline document discussed the need for culturally appropriate PR programs for Indigenous people with COPD in Australia and NZ to reduce the gap in health outcomes.
Conclusion
The Australian and New Zealand Pulmonary Rehabilitation Guidelines present an evaluation of the evidence for nine PICO questions, with recommendations to provide guidance for clinicians and policy makers.
Grant Support
The Lung Foundation Australia funded the face‐to‐face meetings and teleconferences and provided administrative support.
TO‐016: Understanding barriers and facilitators to Pulmonary Rehabilitation referral, uptake and participation using the Theoretical Domains Framework: A systematic review
NS Cox1, CC Oliveria2, A Lahham3, AE Holland4
1Physiotherapy, La Trobe University & Institute for Breathing and Sleep, Melbourne, Vic., 2Physiotherapy, La Trobe University, Melbourne, Vic & Federal University of Juiz de Fora, Minas Gerais, Brazil, 3Physiotherapy, La Trobe University & Institute for Breathing and Sleep, Melbourne, Vic., 4Physiotherapy, La Trobe University and Alfred Health & Institute for Breathing and Sleep, Melbourne, Vic.
Introduction/Aim
Strong evidence supports pulmonary rehabilitation (PR) for people with COPD, yet <5% of those eligible receive PR annually. The Theoretical Domains Framework (TDF) is an integrative framework to explain issues around implementation of best practice evidence in healthcare settings. The TDF was used to understand the constructs that influence referral to, attendance at, and completion of PR by people with COPD.
Methods
A systematic review of studies (qualitative or quantitative) reporting data relating to referral, uptake and/or participation in PR. Extracted data were mapped to one of the 14 domains of the TDF in order to understand the nature of barriers and facilitators.
Participants: Individuals aged >18years with a diagnosis of COPD; or health professionals working with people with COPD.
Results
A total of 6969 references were screened with 48 studies included and 323 relevant items mapped to the TDF. The most frequently represented domain was ‘Environment’ (34/48 included studies, 34% of mapped items) which included waiting time, burden of illness, travel, transport and health system resources. Other frequently represented domains were ‘Knowledge’ (18/48 studies, eg clinician knowledge of referral processes, patient understanding of rehabilitation content) and ‘Beliefs about consequences’ (16/48 studies, eg beliefs regarding role and safety of exercise, expectations of rehabilitation outcomes). Barriers to referral, uptake or participation represented 61% (n=191) of all items mapped to the TDF. All domains of the TDF were represented, however items were least frequently coded to the domains of ‘Optimism’ and ‘Memory’. Methodological quality of included studies was fair (mean quality score 9/12, SD 2).
Conclusion
The benefits of PR for people with COPD are well established. This review highlights the complex interaction between environment, knowledge, attitudes and behaviours influencing uptake and participation in PR. Overcoming challenges associated with the personal and/or healthcare system environment will be imperative to improving access and uptake of PR.
Grant Support
Nil
TO‐017: Antibiotics for persistent cough or wheeze following acute bronchiolitis in children (Review)
Erin J Plumb1, Anne B Chang1,2, Peter S Morris1, Gabrielle B McCallum 1.
1Child Health Division, Menzies School of Health Research, Darwin, Australia. Charles Darwin University, Darwin, Australia., 2Queensland Children's Medical Research Institute, Children's Health Queensland, Queensland University of Technology, Brisbane, QLD Australia
Introduction/Aim
Bronchiolitis is a significant health burden globally. It is a clinically diagnosed condition, characterised by tachypnoea; crackles and/or wheeze in children <2 years. Although typically self‐limiting, persistent symptoms may continue beyond the acute phase (<14 days), increasing the burden of disease and risk of re‐hospitalisation. This review aims to determine the efficacy of antibiotics, compared to a control, to reduce persistent respiratory symptoms following acute bronchiolitis (within six months of illness).
Methods
The previous review was updated in August 2016, using the following databases: Cochrane Airways Group Register of Trials; Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; EMBASE; http://Clinicaltrials.gov; WHO Trial Portal; and the Australian and New Zealand Clinical Trials Registry.
Two review authors independently assessed articles against predetermined selection criteria: randomised controlled trials (RCTs), comparing antibiotics with controls, in the post‐acute phase of bronchiolitis (>14 days), in children < 2 years of age diagnosed with bronchiolitis.
Results
Of 344 papers retrieved, only 2 studies1,2 involving 249 children were included. Using an intention‐to‐treat analysis at 6 months, no significant difference was observed between treatment groups for the primary outcomes: number not cured at follow up (OR 0.69; 95%CI 0.37 – 1.28.), or the number re‐hospitalised with respiratory illness (OR 1.19; 95%CI 0.67 ‐ 2.12). There was no significant difference for any of the secondary outcomes at 6 months: recurrent wheeze (OR 0.78; 95%CI 0.35 – 1.73) or bacterial resistance (OR 0.78; 95%CI 0.31 – 1.94).
Conclusion
There is currently no evidence to support the use of antibiotic treatment at the point of illness to prevent post‐acute bronchiolitis symptoms. However, there were only 2 studies and children were randomised at the point of bronchiolitis. No studies have randomised children at the point of symptom persistence confirming the need for further RCTs to inform clinical practice.
Key Words
Bronchiolitis, Indigenous, antibiotics, persistent symptoms, respiratory
Nomination for New Investigator Award
No
Grant Support
Nil
Conflict of interest
No conflicts of interest to declare
1. McCallum GB, Morris P, Grimwood K, Maclennan C, White A, Chatfield MD, et al, Frontiers in Pediatrics, 2015, 3, 1–9.
2. Tahan F, Ozcan A, Koc N. European Respiratory Journal, 2007, 29, 91–97.
Lung Cancer
TO‐018: TLG increases the specificity of PET‐CT analysis of the mediastinum in NSCLC
Dr Koliarne Tong1, Dr Socrates Angelides2, Professor John Wheatley1,3, Dr Peter Wu1
1Department of Respiratory & Sleep, Westmead Hospital, Sydney, 2Department of Radiology, Westmead Hospital, Sydney, 3The Westmead Institute for Medical Research, Sydney
Introduction/Aim
Endobronchial ultrasound‐guided transbronchial needle aspirate (EBUS‐TBNA) and positron emission tomography‐computed tomography (PET‐CT) are crucial in mediastinal staging of non‐small cell lung cancer (NSCLC). However, the specificity of PET‐CT in assessing the malignancy status of a mediastinal or hilar lymph node is only 40‐79%. Total lesion glycolysis (TLG), defined as lesion volume multiplied by lesion SUVmean, has prognostic value in NSCLC, but to our knowledge has not been used to predict the malignancy status of lymph nodes. Our aim was to determine if the TLG can improve the specificity of PET‐CT analysis in predicting the malignancy status of mediastinal and hilar lymph nodes in NSCLC.
Methods
A retrospective study of patients with NSCLC who underwent EBUS‐TBNA and PET‐CT between January 2012 and December 2014 at Westmead Hospital was performed. A blinded, experienced nuclear medicine physician measured the PET‐CT TLG of lymph nodes sampled via EBUS‐TBNA. The malignancy status of each lymph node was determined by the EBUS‐TBNA histopathology, or the results of surgical sampling when this was performed.
Results
We identified 40 patients who met study criteria. A total of 39 mediastinal and hilar lymph nodes were analysed. Using a cut‐off TLG of 5000, the sensitivity of PET‐CT was 87% and the specificity was 92%. A receiver operating characteristic curve generated showed good accuracy of TLG, with an area under the curve of 0.92.
Conclusion/discussion:
The TLG may be a helpful tool in determining the malignancy potential of mediastinal and hilar lymph nodes in NSCLC, in particular by increasing the specificity of PET‐CT analysis. This in turn would aid the avoidance of unnecessary EBUS‐TBNA procedures, and the associated costs and delays to surgery. Prospective studies are required to further evaluate this novel tool.
Grant Support
Nil
TO‐019: Preoperative exercise training for patients with non‐small cell lung cancer: a Cochrane systematic review.
Vinicius Cavalheri1,2,3, Catherine Granger4,5
1School of Physiotherapy and Exercise Science, Faculty of Health Science, Curtin University, WA, Australia, 2Cancer Council Western Australia, WA, Australia, 3Institute for Respiratory Health, WA, Australia, 4Department of Physiotherapy, The University of Melbourne, Victoria, Australia, 5Department of Physiotherapy, Royal Melbourne Hospital, Victoria, Australia
Aim
To determine the effect of preoperative exercise training on postoperative outcomes including risk of developing a postoperative pulmonary complication, postoperative duration of intercostal catheter and length of hospital stay in adults scheduled to undergo lung resection for non‐small cell lung cancer (NSCLC).
Methods
We searched the Cochrane Central Register of Controlled Trials, PubMed, EMBASE, PEDro and SciELO (The Scientific Electronic Library Online) up to March 2016. Randomised controlled trials (RCTs) were included in which study participants who were scheduled to undergo lung resection for NSCLC were allocated to receive either preoperative exercise training or no exercise training. The two review authors independently screened and assessed studies for inclusion. Risk of bias was assessed using the Cochrane seven evidence‐based domain table Meta‐analyses were conducted were possible.
Results
Five RCTs involving 167 participants were identified. Overall, the risk of bias in the included studies was high. Pooled data from three studies demonstrated that preoperative exercise training reduced the risk of developing a postoperative pulmonary complication by 70% (RR 0.30; 95% CI 0.14 to 0.66). Compared to the control group, the number of days patients in the intervention group needed intercostal catheters was lower (MD −3.33 days; 95% CI −5.35 to −1.30 days) (pooled data from two studies), and postoperative length of hospital stay was also lower in the intervention group (MD −4.34 days; 95% CI −5.65 to −3.03 days) (pooled data from three studies).
Conclusion
Preoperative exercise training appears to reduce the risk of developing a postoperative pulmonary complication, the duration of intercostal catheter and postoperative length of hospital stay in people undergoing lung resection for NSCLC. The findings of this review should be interpreted with caution due to disparities between the studies, methodological limitations, risk of bias and small sample sizes. This systematic review emphasises the need for larger RCTs.
Grant Support
Catherine Granger is supported by a NHMRC Translating Research Into Practice Fellowship co‐funded by Cancer Australia, Australia. Vinicius Cavalheri is supported by a Cancer Council WA Postdoctoral Fellowship
Declaration of interest
Nil.
Nomination for awards: Physiotherapy.
TO‐020: Is it lung cancer?: Evaluating the performance of a “lung lesion for investigation” service at a new secondary hospital
Claire S Waddington1,2,3, Francesco Piccolo1, Simon Jones1, David Manners1
1Department of Medicine, St John of God Midland, WA, Perth, 2Sir Charles Gairdner Hospital, Nedlands, WA, Perth, 3Wesfarmers Centre for Vaccines and Infectious Diseases, Telethon Kids Institute, WA, Perth
Introduction/Aim
Access to, and quality of cancer services are important determinants of patient outcomes from respiratory malignancy. Existing Australian data is limited to retrospective analyses of patients with proven malignancy; these data do not fully describe the journey of all patients with suspected respiratory malignancy. A prospective registry was developed to inform service requirements and benchmark quality.
Methods
Patients referred to St John of God Midland Hospital, a general secondary hospital, for assessment of possible respiratory malignancy were prospectively included. Analyses of clinical data were descriptive.
Results
Between November 2015 and September 2016, 107 patients were referred. 69 were referred by general practitioners and 79 were seen in outpatient clinics. Referral triggers were symptoms with radiological abnormality (76/109), incidental findings (24/107) or abnormality on CT scans performed for lung cancer screening (7/107). The commonest abnormalities were mass (25/107), and pulmonary nodules (single, 23/107; multiple, 16/107). Invasive diagnostic investigations (undertaken in 64/107) established a tissue diagnosis of malignancy in 54, of which 39 were lung cancer. CT surveillance was recommended for 39; four patients were not investigated further. Median time from outpatient referral to first review was eight days (range 0–190; 58/79 of outpatient were seen within 14 days. Patients who required endobronchial ultrasound at a tertiary centre waited a median of 34 days (n=6, range 25–98) from first review to referral for treatment compared to a median of 15 days (n=46, range 0–115) for those who did not.
Conclusion
This pilot registry describes the wide variation in diagnostic pathways taken when investigating possible lung cancer. In addition to providing prompt outpatient assessment, lung cancer services are needed for inpatients presenting acutely unwell. The waiting times for outpatient assessment and diagnostic testing was short for the majority of patients, but there were delays for some patients highlighting the need for ongoing service improvement.
Grant Support
Nil
TO‐021: PLEURX Catheter Drainage Systems are a safe, effective and economical strategy for the management of malignant pleural effusion and ascites. A single Center Experience.
Wilson Petrushnko MBBS1 , Robyn Daniel1, Lucy Morgan BMed Phd FRACP1 , Peter Flynn FRACS 1
1NBMLHD Nepean Lung Cancer Group
Introduction/Aim
Malignant pleural effusion (MPE) and malignant ascites (MA) contribute to significant breathlessness for patients with advanced cancer. Managing this fluid has required frequent admission for repeated needle thoracocentesis or pleurodesis. Since 2008, we have added indwelling tunnelled catheters to the management options available to clinicians within our LHD.
Methods
This project is a retrospective review of our experience with PleurX catheters inserted for management of MPE and MA between 2008–2016.
Results
All patients reported immediate improvement in breathlessness.
Two hundred and ninety‐three PleurX catheters were inserted. The indication was MPE in 176 and MA in 111. Bilateral pleural PleurX were inserted in 17 patients. Pleural and peritoneal catheters were inserted simultaneously in 3 patients.
A technical success rate of 100% was achieved. Drains remained in situ for a mean of 64.0 days (range 2–392 days). Almost all (87%) of patients died with the PleurX catheter insitu. Pleurodesis was achieved in 6.1% (n=18) of patients and PleurX was removed without fluid accumulation. The remaining patients 6.9% remain alive with the PleurX insitu.
PleurX were inserted in patients MPE and MA due to NSCLC 20.5% (n=60), breast 19.8% (n=58), gastric/esophageal 7.8%(n=23), pancreatic 7.5% (n=22), ovarian 7.5% (n=22), colorectal 6.1% (n=18), adenocarcinoma of unknown origin 4.1% (n=12), mesothelioma 3.8% (n=11), hepatocellular carcinoma 2.7% (n=8), SCLC 1.7% (n=5), melanoma 1.7% (n=5), bladder 1.7% (n=5), cholangiocarcinoma 1.4% (n=4), renal cell carcinoma 1% (n=3), angiosarcoma 0.7% (n=2), endometrial 0.7% (n=2), and alcoholic cirrhosis 1.4% (n=4), others/unknown 9.9% (n=29).
Complications from drain insertion included; wound infection 2.4% (n=7), blocked catheter 1.7% (n=5), fell out/cuff exposed 1.7% (n=5), leakage from drain site 0.7% (n=2), bowel injury 0.3 % (n= 1)
The cost per patient on average for the entire duration of pleural and peritoneal PleurX was $1759 and $984 respectively (ongoing hardware cost and insertion cost). The average number of pleural drainage bottles and peritoneal drainage bags per patient was twenty‐nine and twenty‐two respectively.
Conclusion
This study demonstrates the safe use of tunnelled PleurX catheters in patients who present with MPE or MA. Once inserted, subsequent drainage of re‐accumulated effusion or ascites can be managed in the comfort of the patients home. We believe the use of a PleurX catheter should be considered as a first line approach in the management of refractory MPE and MA.
Grant Support
Nil
No conflict of interest to disclose
TO‐022: A new lung cancer pathway in Auckland region reduces time to diagnosis and treatment
Paul Dawkins1, Janet MCWILLIAMS2 , Richard Sullivan3
1Respiratory Medicine, Middlemore Hospital, Auckland, New Zealand, 2Northern Regional Alliance, Auckland, New Zealand, 3Oncology Services, Auckland City Hospital, Auckland, New Zealand
Introduction
A new pathway for the 4 district health boards in the greater Auckland region was developed incorporating rapid access clinics (RACs) and upfront PET‐CT scans for those considered potentially curable at initial assessment, in order to enable quicker lung cancer diagnosis.
Methods
In this 12‐week pilot, patients graded as high suspicion of lung cancer were seen in RACs with spirometry, performance status assessment and available radiology (chest x‐ray or CT scan). Those considered potentially curable by surgery or radiotherapy (FEV1 >=1 litre, ECOG score <2, no advanced disease evident on imaging, no comorbidities precluding radical treatment) received an upfront PET‐CT scan; those who were not received a standard CT scan if not already done. Time through the pathway was measured and compared with historical data from the regional lung cancer database in a 6‐month period the year before the pilot.
Results
165 patients completed the pathway, of which 105 were found to have lung cancer. 41 patients had upfront PET‐CT scans; 30 were confirmed as lung cancer, 7 of which subsequently had palliative treatment. 11 had non‐lung cancer diagnoses (9 not cancer or nodule follow up; 1 metastasis; 1 other cancer). 17 patients had PET‐CT scans later in the pathway, 4 of which subsequently had curative treatment. Median time from referral to first treatment was reduced by 16.7 days (patients with curative treatment intent 17.2 days and palliative treatment intent 12.7 days), significantly reducing the time from referral to multidisciplinary meeting (MDM) and MDM to first treatment. Achievement of 62‐day referral to treatment targets was 85.7% compared with 56.6% in the historical data.
Conclusion
A regional lung cancer pathway incorporating RACs and upfront PET‐CT scans for potentially curative patients resulted in improvements in diagnostic delays and 62‐day treatment targets. These findings subsequently led to implementation of this pathway regionally.
Grant Support
The study was funded by a New Zealand Ministry of Health project grant
TO‐023: MDT v non‐MDT care in lung cancer: does co‐morbidity status have an impact?
Emily Stone1, Nicole Rankin2, Tess Bewes3, Stephen Kerr4, Jane Phillips5, Kwun Fong6, David Currow7, Tim Shaw8
1St Vincent's Hospital and The Kinghorn Cancer Centre, Darlinghurst NSW, 2Sydney Catalyst Camperdown NSW, University of Sydney NSW, 3Faculty of Medicine, UNSW, 4Kirby Institute, UNSW, 5University of Technology, NSW, 6The Prince Charles Hospital, Brisbane QLD, 7Flinders University SOUTH AUSTRALIA, 8Sydney Catalyst Camperdown NSW, University of Sydney NSW
Introduction/Aim
Multidisciplinary team (MDT) care affects lung cancer outcomes including treatment receipt1,2 and survival1,3. This project analyses lung cancer outcomes according to MDT care in an Australian dataset from 2006–2012 aiming to adjust outcomes for co‐morbidity status (Charlson co‐morbidity index and Colinet simplified co‐morbidity score).
Methods
A consecutive cohort of cases diagnosed between 1 January 2006 and 31 December 2012 were identified through the local Clinical Cancer Registry (ClinCR). Histopathology, TNM stage, ECOG status and survival were analysed according to MDT care. The Charlson co‐morbidity index has been calculated via ICD coding. Colinet simplified co‐morbidity scoring will be completed via validated items in institutional medical records.
Results
1022 cases of primary lung carcinoma were identified; 296 (29%) were presented at MDT (“MDT”), 726 (71%) were not (“non‐MDT”). SCLC comprised 33/296 (11%) of MDT and 121/726 (17%) of non‐MDT cases. TNM data showed higher rates of staged (vs unstaged) cases for the MDT group compared with non‐MDT group (97% vs 84.4%, p<0.001). Stage IV patients were half as likely to be presented at MDT than other stages (22% stage IV vs 45% stage 1‐III combined). ECOG status was better recorded for MDT than non‐MDT (72% v 49.6%, p<0.001). Survival analysis, adjusted for age, disease stage and ECOG status, showed an overall 52% increase in the relative probability of death for non‐MDT vs MDT patients (HR 1.52 (95%CI 1.25 – 1.85); P<0.0001. An initial data extract comprising ICD coding for a subset of 264 patients included 168 (63%) MDT cases and 96 (36%) non‐MDT cases, most of whom had a co‐morbidity score of 2 or less.
Discussion/Conclusion
In an analysis adjusted for age, TNM stage and ECOG status, MDT care is associated with improved survival. This project seeks to update this analysis with adjustment for co‐morbidity status according to two previously validated measures.
1Mitchell et al. MJA, 2013, 199, 674–679. 2Boxer et al, Cancer, 2011, 117, 5112–5120. 3Pan et al. PLoS One, 2015, 10.
Grant Support
Nil
OLIV 1
TO‐024: A Sit‐to‐Stand Test is useful to assess exercise oxygenation in patients with Interstitial Lung Disease
Visser S1 ,2, Piggott A3 , Spencer L3 , Alison J3 , Webster S1 , Troy L1 ,2, Hayen A4 , Torzillo P1 ,2, Corte P1 , Corte T1 ,2
1Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, 2University of Sydney, Faculty of Medicine, 3Department of Physiotherapy, Royal Prince Alfred Hospital, Sydney, 4University of Technology, Sydney
Introduction/Aim
Exercise desaturation on six‐minute walk test (6MWT) is associated with poorer outcomes in patients with interstitial lung disease (ILD). The 60s sit‐to‐stand test (STST) is faster and requires less space than 6MWT, however its utility in ILD patients has not been assessed. The aim was to compare oxygen desaturation between the 6MWT and STST in ILD patients.
Methods
Consecutive subjects were recruited from RPAH ILD clinic. Patients performed 6MWT & STST in randomised order with 30mins recovery. 6MWT was performed according to ATS/ERS standards. STST was performed by a single operator, requiring the patient to sit and stand out of a chair as many times as possible in 60s whilst oxygen saturations (SpO2) and heart rate (HR) were monitored. Nadir SpO2 was defined as the lowest SpO2 recorded during the exercise or recovery period. Significant desaturation on 6MWT was defined as nadir SpO2≤88%.
Results
50 subjects were studied (mean age 63.4±11.7 years; 30 males). The underlying cause of ILD was idiopathic pulmonary fibrosis (48%), connective tissue disease (38%), and other (14%). Mean FVC was 72.58±16.3%, DLCO 57.46±16.2%, and resting SpO2 98.64±1.4%.
Median 6MWD was 500m (range 300‐817m) and nSTS was 26 (range 18–66). Patients desaturated more on 6MWT than STST (mean nadir SpO2 90.34±6.7% vs 93.28±5.4%, p<0.0001). There was a strong correlation between nadir SpO2 on 6MWT and STST (Spearman's rho = 0.88, p<0.0001). The area under the receiver operating curve for significant desaturation on 6MWT using the nadir SpO2 on STST was 0.96 (95%CI 0.91‐1.0). Nadir SpO2 of <94% on STST gave a sensitivity of 100% and specificity of 87.1% for significant desaturation on 6MWT.
Conclusion
In an ILD cohort, nadir SpO2 on STST and 6MWT correlated strongly. The STST is suitable in an office setting, and nadir SpO2 on STST of ≥94% appears to rule out significant destauration on 6MWT.
Grant Support
Nil
TO‐025: Vascular remodelling is reversed following BMPR2‐expressing endothelial progenitor cell therapy in a MCT‐induced PAH rat model
R L Harper1, Claudine S Bonder2, Paul N Reynolds1
1Royal Adelaide Hospital & University of Adelaide, Adelaide, SA, 5001, 2University of South Australia, Adelaide, SA, 5001
Introduction/Aim
Pulmonary arterial hypertension (PAH) is caused by pulmonary vascular remodelling. Reduced expression of the bone morphogenetic protein receptor type‐2 (BMPR2) is causally linked to PAH. Previously, we have augmented endothelial progenitor cells (EPCs) to over‐express BMPR2 and transplanted them in a monocrotaline (MCT)‐induced PAH rat model resulting in an amelioration of the disease. We now assess the effects of our BMPR2‐EPC and EPC only therapy on vascular remodelling in this MCT‐induced PAH rat model.
Methods
Rats (n=8) were injected with MCT, and then at day 10, rats were intravenously injected with EPCs only, AdBMPR2 transfected EPCs, AdTrackLuc transfected EPCs or uninjected. After a further 8–10 days, PAH was assessed and lungs were extracted and processed into paraffin blocs. Immunohistochemical analysis on vessels 50μm or less was performed with α‐smooth muscle actin (α‐SMA) Ki67 and proliferating cell nuclear antigen (PCNA).
Results
After 10 days PAH was attenuated as shown by a significant reduction in RVSP, mPAP and Fulton Index in the BMPR2‐transduced EPC group compared to disease only, EPCs only and irrelevant virus‐transduced EPC groups. BMPR2‐EPC treated animals a significant reduction in vessel muscularisation (31.88%) vessel thickness (24.87%) and a significant reduction in cellular proliferation as shown by PCNA (35.77%) and Ki67 (66.86%) staining compare to disease only.
Conclusion
Amelioration of PAH can be achieved using BMPR2 modified EPCs. There's a significant reduction in distal vessel muscularisation and cellular proliferation following EPCs and BMPR2‐EPCs treatment, with a greater effect seen in the BMPR2‐EPCs group.
Grant Support
NHMRC & RAH.
TO‐026: Reduced GCR, HDAC2 and Hsp90 in pro‐inflammatory lymphocytes in the small airways during BOS
Greg Hodge1,2, Sandra Hodge1,2, Aeneas Yeo1,2, Phan Nguyen1,2, Emily Hopkins1,2, Chien‐Li Holmes‐Liew1,2,3, Paul N. Reynolds1,2, Mark Holmes1,2,3
1Lung Research, Hanson Institute and Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, South Australia; 2Department of Medicine, University of Adelaide, Adelaide, South Australia; 3South Australian Lung Transplant Service, Adelaide, South Australia
Introduction
Immunosuppression therapy following lung transplantation fails to prevent bronchiolitis obliterans syndrome (BOS), primarily a disease of the small airways, which we have shown is associated with lack of suppression of pro‐inflammatory lymphocytes. We have also recently shown reduced glucocorticoid receptor (GCR), histone deacetylase 2 (HDAC2) and heat shock protein 90 (Hsp90) in these pro‐inflammatory lymphocytes following transplant. We hypothesize that these lymphocytes target the small airways during BOS.
Methods
Blood, bronchoalveolar lavage, proximal and distal airway bronchial brushings were collected from patients with BOS (n=5), stable lung transplant patients (n=18) and healthy aged‐matched controls (n=10). Intracellular pro‐inflammatory cytokines and expression of GCR, HDAC2 and Hsp90 were measured in lymphocytes subsets following culture using flow cytometry.
Results
BOS was associated with an increase in CD8 T, NKT‐like and NK cells in the distal airways compared with stable patients and controls. There was an increase in IFNγ, TNFα and reduced GCR, HDAC2 and Hsp90 expression in these lymphocyte subsets in patients with BOS compared with stable patients and controls. There was a correlation between the percentage of CD8+T cells expressing HDAC2, GCR and Hsp90 from distal brushings with FEV1 (HDAC2:R=.676 , p=.031; GCR: R=.632 , p=.039).
Conclusions
BOS is associated with increased pro‐inflammatory CD8+ T, NKT‐like and NK cells in the distal airways. Treatments that increase GCR, HDAC2 and Hsp90 in these lymphocyte subsets may reduce graft rejection.
Grant Support
RAH Respiratory Clinical Trials
Declaration of interest
No declaration of interest
TO‐027: Matrix metalloproteinase‐7 (MMP7) may be a biomarker of early chronic lung rejection
Jaffar J1 ,2, Phan T1 ,2, Stewart M2 , Levey B2 , Paraskeva M2 , Snell G2 , Westall G1 ,2
1Department of Immunology and Pathology, Monash University; Australia 2Department of Allergy Immunology and Respiratory Medicine, The Alfred, Australia
AIM
Lung transplantation is the best option for patients with end‐stage lung diseases. Chronic rejection is a major complication post‐operation. More than half of all lung transplant recipients experience chronic rejection but early in the course of disease few symptoms are clinically apparent. The aim of this study was to investigate the use of MMP7 as a biomarker of early chronic lung rejection.
METHODS
Forty adult lung transplantation patients at The Alfred had blood collected and lung function measured at 4 time points; pre‐transplantation, 3‐, 12‐ and 24 months post‐transplant. Measurements of plasma MMP7 were performed using sandwich immunoassay. Clinical variables including age, BMI, smoking history and history of acute graft rejection were also recorded. Univariate and multivariate analyses assessed the clinical variables associated with plasma MMP7 levels. The utility of MMP7 as a biomarker of disease progression was assessed by receiver‐operating characteristic curve analysis. Disease progression was defined as a greater than 5% fall in percent predicted Forced Vital Capacity in 1 second (FEV1%) between the 12 and 24 month time points.
RESULTS
Seventeen of 40 patients experienced a decline in lung function between 12 and 24 months post‐operation. Patients who experienced disease progression had higher levels of plasma MMP7 at 12 months post‐transplant than those who remained stable (mean stable 0.6 pg/mL vs mean progressed 1.1 pg/mL; p<0.001). Increased levels of MMP7 predicted disease progression (area under the curve = 0.8, p=0.003).
CONCLUSION
There are no biomarkers able to detect disease progression of chronic rejection before patients experience lung function decline. MMP7 is a biomarker of disease progression in idiopathic pulmonary fibrosis, a fibrotic lung disease with shared mechanisms of pathogenesis to chronic rejection. Elevated MMP7 levels may be detectable prior to clinical manifestation of lung function decline. MMP7 levels may be a biomarker of disease progression in chronic rejection.
Grant Support
Nil
TO‐028: Dead space ventilation is linked to exercise capacity and survival in distal chronic thromboembolic pulmonary hypertension
Laurent Godinas1, Edmund Lau2, David Montani3, Xavier Jais3, Olivier Sitbon3, Gérald Simonneau3, Marc Humbert3, Pierantonio Laveneziana3, Gilles Garcia3
1Departement of Pneumologie, Centre Hospitalier Universitaire, Université Catholique de Louvain Mont‐Godinne, Yvoir, Belgium, 2Department of Respiratory Medicine, Royal Prince Alfred Hospital, Camperdown 2050, Australia, 3Assistance Publique‐Hôpitauxde Paris, Centre deRéférencedel’ Hypertension Pulmonaire Sévère, Département Hospitalo‐Universitaire Thorax Innovation, Service de Pneumologie, Hôpital de Bicêtre, LeKremlin Bicêtre, France
Introduction
Cardiopulmonary exercise testing (CPET) is frequently used for the evaluation of patients with pulmonary hypertension (PH). Patients with non‐operable distal CTEPH represent a unique subgroup of PH where microvascular disease resembling pulmonary arterial hypertension (PAH) may predominate and efficacious medical therapy is now available. However, little is known regarding the detailed CPET profile of distal CTEPH, and whether ventilation and gas exchange responses are different to PAH.
Methods
Forty‐nine consecutive patients with non‐operable distal CTEPH according to multidisciplinary team assessment and 45 matched PAH patients underwent CPET and right heart catheterization. Patients were followed up for median of 3.2 years.
Results
Pulmonary haemodynamics were similar in distal CTEPH and PAH groups but patients with distal CTEPH achieved lower percentage predicted peak oxygen consumption (59±13 vs 66±14%, p<0.05), At peak exercise, higher physiological deadspace fraction (VD/VT) (0.45±0.07 vs 0.35±0.07, p<0.0001) and larger arterial‐to‐end tidal carbon dioxide gradient (9±3 vs 5±3mmHg, p<0.0001) were observed in distal CTEPH compared with PAH. Ventilatory efficiency expressed as VE/VCO2 slope was also more impaired in distal CTEPH (52.2±10.1 vs. 43.8±8.4 L/min/L/min, p<0.0001). In only the distal CTEPH group, higher VD/VT correlated with lower peak oxygen consumption (r = −0.46, p = 0.003) and was associated with worse survival.
Conclusions
Compared with PAH, a distinct pattern of pathophysiology is observed in distal CTEPH which is characterized by increased deadspace ventilation resulting in worse ventilatory efficiency and greater impairment of exercise capacity. In distal CTEPH, deadspace ventilation correlates with exercise capacity and may have potential prognostic relevance.
Conflict of Interest:
Nil
TO‐029: Oxygen attenuates oxidative stress in ILD patients with nocturnal and exercise‐induced hypoxaemia
L.K. Troy1,2, I.H. Young1,2, N.A. Taylor1,2, S.E. Webster1, B. Brown3, C. Hawkins3, T.J. Corte1,2.
1Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Camperdown, NSW, Australia, 2Sydney Medical School, University of Sydney, Sydney, NSW, Australia, 3Heart Research Institute, Newtown, NSW, Australia
Aim
Patients with interstitial lung disease (ILD) frequently experience intermittent hypoxaemia (IH) during exercise and sleep. Chronic IH is associated with increased oxidative stress and maladaptive cardiovascular consequences, including pulmonary hypertension (PH). We aimed to compare plasma markers of oxidative stress [protein carbonyl (PC) and thiol concentrations] in two ILD cohorts who were exposed to the intervention of oxygen versus medical air.
Methods
Two previously described ILD patient cohorts with either significant sleep‐related hypoxia (>10% of sleep time with SpO2<90%), or exercise‐induced desaturation (SpO2<88% during 6‐minute walk test, 6MWT) participated in randomised, double‐blinded, sham‐controlled, cross‐over studies. Paired plasma samples were taken following both supplemental oxygen and medical air usage during either sleep or incremental cardiopulmonary exercise testing. A sensitive enzyme‐linked immunosorbent assay (ELISA) was used for pro‐oxidant PC detection, and anti‐oxidant thiols were quantified using the DTNB assay with the 96‐well plate method.
Results
Eleven Sleep‐ILD patients and 14 Exercise‐ILD patients were studied (combined population: 11 females; mean age 66.9±9.1 yrs; BMI 30.9±5.8; FVC 71.4±16.8%; DLCO 49.1±11.4%, nadir 6MWT SpO2 84.5±4.8%, RVSP 40.3±13.7mmHg, %sleep time<90% 30.8±17.9 (n=11)). Baseline plasma PC concentrations (on air) were elevated, ranging between 0.12‐0.90 nmol/mg, (normal 0.1 nmol/mg), and baseline thiol concentrations were depleted (range 68.0‐256.3 μmol/L; normal: 400–600 μmol/L). Lower thiol concentrations were associated with lower nadir sleep SpO2 (R=0.82, p=0.002), and increased RVSP (R=0.62, p=0.03). With the application of oxygen during sleep and exercise, plasma PC levels were not significantly reduced, compared with air. Anti‐oxidant thiol levels however, were significantly improved with oxygen in both sleep and exercise cohorts [Sleep: 131.0±28.0 μmol/L (air), 173.8±50.7 μmol/L (oxygen), p=0.03. Exercise: 171.4±52.4μmol/L (air), 213.9±70.5 μmol/L (oxygen), p=0.002].
Conclusion
ILD patients with IH during sleep or exercise have an increased burden of oxidative stress. Lower anti‐oxidant thiol levels are associated with more severe sleep hypoxia and PH. Supplemental oxygen improves anti‐oxidant capacity in ILD cohorts.
Grant Support
Primary Care
Primary Care
TO‐030: High rates of respiratory symptoms and airways disease in mental health inpatients in a tertiary centre
Andrew Burke1,2, Karen Hay3, Alex Chadwick1, Judith Sheridan4
1The Prince Charles Hospital, Brisbane, Queensland, Australia, 2The University of Queensland, Brisbane, Queensland, Australia, 3QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia, 4Queensland University of Technology, Brisbane, Queensland, Australia
Introduction
People with severe mental illness (SMI) have a lower life expectancy than the general population. A significant proportion of this excess mortality is due to a higher prevalence of cardiac and metabolic disease. Less is known of the prevalence of respiratory disease in this group. This cross sectional, observational study aimed to assess the prevalence of respiratory disease and symptoms in patients admitted to an inpatient mental health unit.
Methods
82 inpatients had a structured interview and questionnaire completed. The questionnaire included self‐reported diagnoses of common diseases and screening questions designed to detect respiratory disease and sleep disordered breathing. Spirometry was performed on the basis of symptoms and smoking status. Access to primary care was assessed including surrogate markers for comprehensive care such as vaccination status.
Results
Patients reported high rates of respiratory symptoms including wheeze, dyspnoea and cough. Productive cough was significantly associated with tobacco use (p<0.005). 52% of patients reported daily tobacco use and 13% used cannabis at least monthly. Ten patients (17%) had spirometry consistent with COPD of whom 6 did not have a formal diagnosis of COPD previously. Symptoms suggestive of sleep disordered breathing were common with 9 patients (11%) reporting witnessed apnoeic episodes while sleeping. Vaccination rates were low for both pneumococcal and influenza vaccine.
Conclusions
People with SMI have high rates of respiratory symptoms with a high prevalence of COPD on spirometry. Half of the COPD cases were not previously diagnosed suggesting a hidden burden of respiratory disease in patients with SMI.
Key words
mental illness, COPD, smoking.
Support
Prince Charles Foundation Novice Researchers Grant
TO‐031: A qualitative study using innovative technology via a smartphone application to provide demonstrative inhaler technique education for asthma patients
Charmaine M King1,2,3, Kristin V Carson1,2,3, Joep Van Agteren2,3, Zoe A Kopsaftis1,2,3, Brian J Smith1,2,3
1School of Medicine, The University of Adelaide, SA 5000, 2Clinical Practice Unit, Basil Hetzel Research Institute, SA 5011, 3Respiratoy Medicine, The Queen Elizabeth Hospital, SA 5011
Introduction/Aim
Evidence suggests more than 75% of asthma patients fail to use their inhalers correctly resulting in frequent exacerbations. Sub‐optimal education for health professionals and subsequently their patients, may be a contributing factor. Innovative technology (‘augmented reality’), accessed via smartphone applications, can function as an educational tool to address these issues. Therefore the aim of this study is to obtain health professional, asthma patient and key community stakeholder perspectives on the feasibility of augmented reality technology to improve asthma inhaler technique education.
Methods
A patient information poster displaying images of the 22 asthma inhaler devices was produced based on existing evidence based recommendations and resources. Augmented reality technology was then utilised to provide a video demonstration of correct inhaler technique for each device, made accessible via a free smartphone application. Twenty‐one semi‐structured, one‐on‐one interviews with health professionals, asthma patients and key community stakeholders were conducted between August and September 2016. Data was analysed thematically using the Triandis model of interpersonal behaviour.
Results
Interviews with asthma patients highlighted perceived competence with inhaler technique. However, health professionals and key community stakeholders identified that this perception was misguided and that poor inhaler technique is a facilitating condition for incorrect inhaler use and sub‐optimal disease management.
Delivering inhaler technique education using augmented reality was favoured by all participants, particularly around ease of use with the ability to visually display various inhaler techniques for each device. However, all participants identified some barriers, particulalry for use among the elderly.
Conclusion
Augmented reality may be a novel means to address poor inhaler technique among certain cohorts of asthma patients and serve as a prompt for health professionals to initiate review of inhaler devices. A randomised controlled trial design is needed to evaluate efficacy of this technology for use in the clinical care setting.
Grant Support
The Hospital Research Foundation; COI: None
TO‐032: The debilitating burdens of living with severe asthma
Juliet M Foster1, Vanessa M McDonald2, Michael Guo3, Helen K Reddel1
1Woolcock Institute of Medical Research, University of Sydney, NSW, Australia, 2Centre for Healthy Lungs, Centre of Excellence in Severe Asthma, The University of Newcastle, Newcastle, Australia, 3AustralAsian Severe Asthma Network, Woolcock Institute of Medical Research, University of Sydney, Sydney, Australia
Introduction/Aim
People with severe refractory asthma (SRA) likely face a sizeable burden, beyond that of people with milder disease. We aimed to explore the little‐known experiences of people living with SRA.
Methods
Participants identified as SRA via the Australasian Severe Asthma Network and/or specialist asthma clinics across seven Australian states were invited for telephone interview. Semi‐structured interviews were conducted consecutively until no new themes emerged. Interviews were recorded, transcribed and thematically analysed.
Results
Most of the 25 participants (aged 23–81 yrs; 68% female) experienced daily symptoms. Key themes were: ‘The body as a hindrance’: SRA placed wide‐ranging limits on life from daily chores to career, relationships and family life; ‘Alone with asthma’: Interviewees felt alone in understanding the experience of asthma; they suffered emotional distress including frustration, hopelessness and/or depression, but formal emotional support services were lacking; ‘Striving to adapt’: Participants expressed varying degrees of adjustment to their diagnosis, from denial to full acceptance; ‘Concerns and experience with treatments’: Most interviewees accepted the need for medicines but were concerned about oral corticosteroid side‐effects and disliked reliance on treatment, which they felt took over their life; ‘Day‐to‐day medical care’: Participants reported need for more accessible, knowledgeable GPs, and better communication with GPs/specialists; ‘Acute care’: Exacerbations were frightening for participants/family yet they avoided emergency department presentation to avoid the disruption that hospitalisations placed on daily lives; ‘Support needs’: practical and emotional support varied from none at all to provision by willing/fatigued family. Participants felt compelled to 'push through' due to parenting/financial responsibility.
Conclusion
SRA imposes long‐term, debilitating burdens and should be considered differently to milder asthma. There is an urgent need to improve support services and primary care for SRA patients, and assistance for their families.
Grant Support
Funded by Asthma Australia with independent research grants from Boehringer Ingelheim, GlaxoSmithKline and Novartis
TO‐033: Quitting experiences and smoking cessation preferences of smokers in Australian general practices
Liang J1 , Abramson MJ2 , Zwar N3 , Russell G4 , Holland AE5 , Bonevski B6 , Mahal A2 ,10, van Hecke B7 , Phillips K8 , Eustace P9 , Petrie K1 , Wilson S1 , George J1 .
1Centre for Medicine Use and Safety, Monash University, VIC, Australia, 2Epidemiology & Preventive Medicine, Monash University, VIC, Australia, 3Public Health and Community Medicine, University of New South Wales, NSW, Australia, 4Dept of General Practice, School of Primary Health Care, Monash University, VIC, Australia, 5Physiotherapy, La Trobe University and Alfred Health, VIC, Australia, 6Medicine & Public Health, University of Newcastle, NSW, Australia, 7Boehringer Ingelheim Pty Ltd, NSW, Australia, 8Lung Foundation of Australia, QLD, Australia, 9Eastern Melbourne PHN, VIC, Australia, 10The Nossal Institute for Global Health, University of Melbourne, VIC, Australia
Introduction/Aim
Approximately one in five patients attending general practice is a daily smoker. Information on previous quitting experiences and smoking cessation preferences of smokers attending general practice is necessary to inform effective interventions.
Methods
Current/ex‐smokers (aged≥40 years, ≥10 pack years) were recruited from general practices across Melbourne for the RADICALS© study – a cluster randomised controlled trial of an interdisciplinary model of care to reduce the burden of smoking and lung disease in Australian primary care. Patients completed an exhaled carbon monoxide (CO) test to confirm smoking status and a structured questionnaire during a face‐to‐face interview.
Results
Of the 653 participants identified across 38 general practice clinics in Melbourne, 456 (70%) were current smokers; 425 (93%) of whom were daily smokers. The median exhaled CO reading was 22ppm (IQR 14–29). On a scale of 1 (low) to 10 (high), the self‐reported motivation (median 6; IQR 4–8), and confidence to quit (median 5; IQR 3–7) were modest among current smokers. Of the current smokers, 237 (52%) had attempted quitting in the previous 12 months; 156 (66%) of whom reported two or more attempts in the past year. The most common pharmacological treatments used were nicotine replacement therapy (128, 54%) and varenicline (72, 30%). The most popular non‐pharmacological treatment was hypnotherapy (40, 17%). Approximately 40% of smokers would use medications to aid future quit attempts. E‐cigarettes have been used by 21 (9%) current smokers with at least one quit attempt in the previous year, and would be considered to help future quit attempts by 132 (29%) current smokers.
Conclusion
Many smokers in primary care consider and have used non‐evidence‐based smoking cessation aids. Healthcare professionals should use motivational counselling and emphasise evidence‐based treatments when providing support to smokers.
Grant Support
NHMRC, Cyril Tonkin Scholarship, Boehringer Ingelheim, Lung Foundation of Australia, Eastern Melbourne PHN
TO‐034: Diagnosis of COPD in Australian general practices: experience from the RADICALS © trial
Liang J1 , Petrie K1 , Abramson MJ2 , Zwar N3 , Russell G4 , Holland AE5 , Bonevski B6 , Mahal A2 ,10, van Hecke B7 , Phillips K8 , Eustace P9 , Wilson S1 , George J1
1Centre for Medicine Use and Safety, Monash University, VIC, Australia, 2Epidemiology & Preventive Medicine, Monash University, VIC, Australia, 3Public Health and Community Medicine, University of New South Wales, NSW, Australia, 4 Dept of General Practice, School of Primary Health Care, Monash University, VIC , Australia, 5Physiotherapy, La Trobe University and Alfred Health, VIC, Australia, 6Medicine & Public Health, University of Newcastle, NSW, Australia, 7Boehringer Ingelheim Pty Ltd, NSW, Australia, 8Lung Foundation of Australia, QLD, Australia, 9Eastern Melbourne PHN, VIC, Australia, 10The Nossal Institute of Global Health, University of Melbourne, VIC, Australia
Introduction/Aim
Diagnosis and management of COPD are underpinned by strong scientific evidence and local guidelines are available to guide decision making. However, previous studies have suggested underdiagnosis and misdiagnosis of COPD in primary care. We describe our experience in case‐finding from the RADICALS© (Review of Airway Dysfunction and Interdisciplinary Community‐based care in Adult Long‐term Smokers) trial in Australian general practices.
Methods
Current/ex‐smokers (aged≥40 years, ≥10 pack years, including those with an existing diagnosis of COPD) have been recruited from 38 general practices across Melbourne. Following case‐finding using the COPD‐6® (Vitalograph Inc., Kansas, USA), those with FEV1/FEV6≤0.75 underwent spirometry. COPD diagnosis was made based on spirometry (FEV1/FVC<0.7), COPD assessment test (CAT) score and modified Medical Research Council (mMRC) dyspnoea scale grade.
Results
Of 990 participants, 201 (20%) individuals had an existing diagnosis of COPD. Spirometry referrals have been made for 396 individuals (40%). Spirometry has been performed in 335, of whom 238 (71%) have been confirmed as having COPD. Only 105 (52%) of those currently managed as having COPD had spirometric confirmation. COPD‐6® (FEV1/FEV6≤0.75) testing had a positive predictive value of 70% for COPD.
Conclusion
Case‐finding of at risk patients using handheld devices measuring FEV1/FEV6, and subsequent spirometry testing revealed continuing under‐diagnosis of COPD. Diagnostic spirometry is essential in avoiding misdiagnosis of COPD in Australian primary care.
Grant Support
NHMRC, Cyril Tonkin Scholarship, Boehringer Ingelheim, Lung Foundation of Australia, Eastern Melbourne PHN
TO‐035: Feasibility of a peer‐led asthma and smoking prevention program (ASPP) in Australian schools with high Indigenous youth
Smita Shah1, Gabrielle B McCallum 2, Cate Wilson1, Jan Saunders3, Anne B Chang2,4
1Primary Health Care Education and Research Unit, Western Sydney Local Health District, NSW, 2Child Health Division, Menzies School of Health Research, Charles Darwin University, Darwin, Northern Territory, 3Asthma Foundation Northern Territory, 4Queensland Children's Medical Research Institute, Children's Health Queensland, Queensland University of Technology, Brisbane, Queensland,
Introduction/Aim
The high global burden of asthma and tobacco smoking among Indigenous people may potentially be reduced by appropriate interventions that target prevention of tobacco smoke uptake and improved asthma management. We undertook a pilot study in two Darwin schools with a high proportion of Indigenous youth to determine the feasibility of an innovative, peer‐led, school‐based education program called the Asthma and Smoking Prevention Project (ASPP). A subset of children with reported persistent respiratory symptoms were also clinically evaluated to determine the lower airway inflammatory profile and optimise asthma management.
Methods
The ASPP is founded on an evidence‐based program to improve asthma management and prevent the uptake of tobacco smoking. The program uses a student‐centred approach in which senior students (Peer Leaders) deliver the ASPP to Grade 7 students using activities, videos and games. Students completed questionnaires related to asthma and smoking at baseline and 3‐months after program delivery. Students with respiratory symptoms at 3‐months were invited for a comprehensive clinical evaluation and tests including sputum induction.
Results
The ASPP was well received. Of the 203 students involved, 56 (28%) were Indigenous and 70% completed baseline and follow‐up questionnaires. Self‐reported asthma was high (19%), 10% of students reported smoking and 63% reported exposure to tobacco at home. Of the 22 students who were clinically evaluated, 41% were Indigenous. Clinically important airway inflammation was high; 23% had Fractional Exhaled Nitric Oxide levels ≥35ppb, 88% had airway neutrophilia (>15%) and 29% had airway eosinophilia (>2.5%). Optimisation of medication and management was required in 59% of students.
Conclusion
Our study demonstrates the feasibility of implementing a school‐based prevention and intervention program for at‐risk groups. The high prevalence of clinically important airway inflammation and suboptimal asthma management highlights the need for a community‐based study on persistent respiratory symptoms in adolescents to reduce the burden of chronic lung disease particularly for Indigenous Australians.
Grant Support
Asthma and Allergy 2
TO‐036: Response of airway epithelial cells to rhinovirus in an allergic cytokine environment
Cristan Herbert1, Kimchi Do1, Vincent Chiu1, Linda Garthwaite1, Daniela Traini2, Paul Young2, Rakesh K. Kumar1
1Mechanisms of Disease and Translational Research, School of Medical Sciences, UNSW Australia, Sydney, NSW, Australia, 2Discipline of Pharmacology, Woolcock Institute of Medical Research, University of Sydney, Sydney, NSW, Australia
Introduction/Aim
Rhinovirus is the most common trigger of acute exacerbations of allergic asthma. The airway epithelium is the target of rhinovirus infection, and is an important source of pro‐inflammatory and anti‐viral mediators. Airway epithelial cells (AECs) from patients with allergic asthma exhibit a pro‐inflammatory phenotype. We aimed to characterise how the Th2 cytokine environment in allergic asthma alters the response of AECs to rhinovirus and to investigate the signalling pathways involved.
Methods
Cells of the well‐differentiated human airway epithelial line, Calu‐3, were cultured with or without the Th2 cytokines IL‐4 and IL‐13 for 48 hours, then stimulated with Poly I:C (TLR3 agonist) or imiquimod (TLR7 agonist), or infected with rhinovirus16. Quantitative real‐time PCR and nCounter assays were used to characterise changes in expression of mRNA for pro‐inflammatory and anti‐viral mediators as well as viral pattern‐recognition molecules.
Results
In the allergic cytokine environment, enhanced expression of mRNA for the pro‐inflammatory cytokines IL6 and IL8 was induced by Poly I:C and imiquimod, while expression of anti‐viral response genes IFIT1, STAT1, IRF7 and IFIH1 was induced only by Poly I:C. Following rhinovirus infection, Calu‐3 cells pre‐treated with Th2 cytokines exhibited significantly higher expression of IL6, IL8, CXCL10, CCL5, IL32 and CFB. Expression of IFNB1 and IFNL2/3 was either unchanged or modestly increased in cells pre‐treated with Th2 cytokines. These alterations were accompanied by increased expression of the pattern recognition receptor genes TLR3, IFIH1, DDX58, and also of ICAM1, the cell surface receptor for rhinovirus.
Conclusion
Th2 cytokines appear to promote increased production of pro‐inflammatory mediators following rhinovirus infection. Furthermore, any impairment of anti‐viral host defence observed in allergic asthmatics is unlikely to be due to the effects of Th2 cytokines. Increased viral entry, together with enhanced signalling via TLR‐3, MDA‐5, and RIG‐I, may explain the exaggerated inflammatory response to rhinovirus infection observed in patients with allergic asthma.
Conflict of Interest
No
Grant Support
Nil
TO‐037: Sex dependent effects on airway responsiveness of maternal hypoxia‐induced intrauterine growth restricted juvenile mice
Wang KC1 , Larcombe AN1 , Morton JS2 , Davidge ST2 , James AL3 & Noble PB4
1Telethon Kids Institute, WA 6008, Australia, 2Department of Physiology, University of Alberta, Edmonton, Alberta, Canada; Department of Obstetrics and Gynecology, University of Alberta, Edmonton, Alberta, Canada, 3Department of Pulmonary Physiology and Sleep Medicine, West Australian Sleep Disorders Research Institute, Sir Charles Gairdner Hospital and School of Medicine and Pharmacology, University of Western Australia, WA 6009, Australia, 4School of Anatomy, Physiology and Human Biology, University of Western Australia, WA 6009, Australia
Aim
Previous studies have shown that intrauterine growth restriction (IUGR) is associated with asthma in children, however the reason is unknown. In early childhood, the prevalence of asthma is greater in males than females. The aim of this study was to investigate the impact of maternal hypoxia‐induced IUGR on airway hyperresponsiveness in male and female juvenile mice.
Methods
Pregnant female BALB/c mice were housed under hypoxic conditions (10.5% O2) from gestational days E11‐E17.5 (IUGR group; gestation period = 21 days). Following hypoxic exposure, mice were returned to a normoxic environment (21% O2). A second group of pregnant mice were housed under normoxic conditions throughout pregnancy (Control group). Weights of offspring were recorded until 2 weeks of age at which point responsiveness to methacholine and thoracic gas volume (TGV) were assessed.
Results
The IUGR offspring were lighter at birth compared with Control offspring, but not at 2 weeks of age. There were no differences in snout‐vent length or abdominal circumference between groups at 2 weeks of age. At 2 weeks, airway resistance after methacholine challenge was greater in male IUGR offspring compared with Controls, but not in female IUGR offspring compared with Controls. In contrast, while there was no difference in peripheral lung mechanics between male IUGR offspring and Controls, IUGR female offspring had increased tissue damping and elastance after methacholine challenge, compared with Controls. There was no difference in TGV between groups.
Conclusion
Maternal hypoxia induced IUGR offspring were smaller at birth but exhibited ‘catch up’ growth by 2 weeks of age. The physiological consequences of IUGR in the juvenile period were sex dependent: airway hyperresponsiveness in male offspring, and impaired peripheral mechanics in female offspring. Sexual dimorphism in the response to IUGR may contribute to differences in the prevalence of asthma between males and females in early childhood.
Grant Support
NHMRC, Asthma Foundation WA.
Declaration of Interest Statement
None.
TO‐038: Determinants of rhinovirus and nucleic acid induced cytokine production in a large cohort
Liisa Murray1, Yang Xi1, Joana A. Revez2, Manuel A. Ferreira2, John W. Upham1,3
1Translational Research Institute, The University of Queensland, Brisbane, 2QIMR Berghofer Medical Research Institute, Brisbane, 3Respiratory and Sleep Medicine, Princess Alexandra Hospital, Brisbane
Introduction
Individual susceptibility to otherwise innocuous RNA viruses such as rhinoviruses (RV) is not well understood, but may be linked to variations in cytokine production and virus sensing toll‐like receptors (TLRs).
Aim
Determine the key demographic, immunologic and genetic factors associated with cytokine production.
Methods
Cold frequency was documented by questionnaire. DNA and RNA were extracted from whole blood; plasmacytoid dendritic cell (pDC) numbers were assessed using CD303 expression. Mononuclear cells were stimulated for 24h with RV or synthetic TLR ligands. Relationships between variables were evaluated by multivariable regression.
Results
301 subjects (mean age 33 years; 62% women) were recruited. The table indicates variables independently associated with RV and TLR8 ligand stimulated interferon (IFN)‐α, TNF and IL‐12. * p<0.05; ** p<0.01; ns = not significant
| Sex | Age | BMI | Cold frequency | pDC numbers | |
|---|---|---|---|---|---|
| RV stim IFNα | Female > male** | Inverse* | Inverse** | ns | Positive** |
|
TLR8 stim TNF |
Male > female** | ns | ns | Positive* | Inverse** |
|
TLR8 stim IL‐12 |
Male > female** | ns | ns | ns | Positive* |
Conclusions
Cytokine production was independently associated with several variables particularly sex and pDC numbers. TNF production (but not IFNα) was linked to self‐reported cold frequency. Future experiments will examine TLR7 and TLR8 genetic variants, as we predict these two X chromosome genes modify cytokine production and virus susceptibility.
Grant Support
NHMRC, Asthma Foundation of Qld, Astra Zeneca
TO‐039: Measuring bronchial hyperresponsiveness using a more sophisticated biostatistical method: the linear mixed effects model
Byrne S1 ,Milanzi E1 ,Burgess J1 ,Hodge A1 ,2,Matheson MC1 , Erbas B1 , Perret J1 ,3, Thompson BR4 , Abramson MJ5 , Walters EH1 , Dharmage S1 , Jenkins M1
1Centre for Epidemiology and Biostatistics, The University of Melbourne, VIC, Australia, 2Cancer Council Victoria, VIC, Australia, 3The Institute of Breathing and Sleep, VIC, Australia, 4Allergy, Immunology and Respiratory Medicine, The Alfred Hospital, VIC, Australia, 5School of Public Health & Preventive Medicine, Monash University, VIC, Australia
Introduction/Aim
Bronchial hyperresponsiveness (BHR) is typically measured using a dichotomous variable or the log transformed dose response slope (logDRS), both of which lead to loss of information. Furthermore, regression of the logDRS does not consider the initial FEV1 and the resulting estimates are difficult to interpret. In contrast, linear mixed models (LMM), a standard biostatistical tool that appears to have never been used for BHR, overcome these limitations, using all the data collected and producing more intuitive estimates. We aimed to test the utility of modelling BHR using a LMM on associations with known risk factors. Regression of the logDRS was used as a comparison.
Methods
In 2010–2012, a subsample (n=687) of the 1961‐born Tasmanian Longitudinal Health Study (TAHS) cohort were assessed by questionnaire, spirometry and methacholine challenge. Repeated FEV1 measurements were modelled using a LMM. Linear regression was used to model logDRS. Predictors evaluated in both models were sex, age, height, smoking and asthma status. The LMM included random intercepts and slopes, and interactions between dose and all other predictors.
Results
In both models current smoking, asthma status, and age were associated with BHR, sex, height and former smoking were not.
| Predictor | Mixed effects – difference in rate of change in FEV1 (ml/μmol methacholine) | Linear regression (logDRS) | ||
|---|---|---|---|---|
| β‐coefficient (95%CI) | p‐value | β‐coefficient (95%CI) | p‐value | |
| Sex (Female=1) | −2.54 (−10.4,5.36) | 0.53 | 0.14 (−0.11,0.39) | 0.28 |
| Smoking | ||||
| ‐Former | 0.68 (−5.15,6.51) | 0.82 | 0.01 (−0.17,0.19) | 0.92 |
| ‐Current | −14.1 (−22.0,‐6.31) | <0.001 | 0.26 (0.016,0.50) | 0.037 |
| Asthma | ||||
| ‐Remitted | −13.3 (−19.8,‐6.83) | <0.001 | 0.43 (0.23,0.64) | 0.001 |
| ‐Current | −36.9 (−44.1,‐29.6) | <0.001 | 1.16 (0.95,1.37) | <0.001 |
| Height | −0.17 (−0.63,0.29) | 0.46 | −0.01 (−0.02,0.01) | 0.21 |
| Age | −10.0 (−14.5,‐5.52) | <0.001 | 0.26 (0.12,0.40) | <0.001 |
Conclusion
A LMM can be used to assess risk factors for BHR. By incorporating all data, it is likely to be more sensitive and provide more statistical power to identify risk factors.
Grant Support
NHMRC, Clifford Craig Medical Research Trust
TO‐040: Mechanical forces attenuate anti‐viral immunity in primary human airway epithelial cells from asthmatic donors
Punnam Veerati1, Nathan Bartlett1, Kristy Parsons1, Fatemeh Moheimani1, Peter Wark1,2, Darryl Knight1, Chris Grainge1,2.
1Centre for Healthy Lungs, Hunter Medical Research Institute, The University of Newcastle, Newcastle, New South Wales, Australia, 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, New South Wales, Australia.
Introduction/Aim
Bronchoconstriction (BC) is a major physiological event in asthma, leading to clinical symptoms and the generation of mechanical force within the airway. Asthma is characterised by periods of good health, interrupted by exacerbations. Most asthma exacerbations are caused by respiratory viruses, including rhinovirus(RV). During a viral exacerbation of asthma, BC and viral infection occurs simultaneously; these factors may interact in the airway. This study aims to investigate the role of mechanical forces on innate anti‐viral immunity during RV infection in primary human airway epithelial cells.
Methods
Primary airway epithelial cells from asthmatic donors (n=5) were collected at bronchoscopy and air liquid interface(ALI) cultures established. After 21 days, cell were infected with RV1B at a multiplicity of infection of 0.001 for 6 hours. Infected and control cells were then exposed to apical compression (30cm H2O pressure) using 5%CO2 in air for 10 minutes every hour for 96 hours. Cells were harvested at 24‐hour intervals. Samples were analysed for viral and interferon(IFN) RNA, and IFN, transforming growth factor‐β 2(TGF‐β 2) and mucus proteins.
Results
Compression induced the release of TGFβ 2 protein across all time points (At 96 hours post infection, control(Mean±SEM):302±120pg/ml, compressed:1726±909pg/ml). Compressed cells produced less type‐I and type‐III IFNs following RV1B infection (At 96 hours. IFNb virus alone(Mean±SEM):173±89pg/ml, compression+virus 58±17pg/ml and INFl virus alone: 603±280 (SEM) pg/ml, compression+virus 125±35pg/ml. Compression also induced an increase in viral replication.
Conclusion
We demonstrate that mechanical forces similar to those induced during bronchoconstriction in vivo induce production of TGFβ 2 and impair innate anti‐viral immunity in primary human airway epithelial cells. This is the first time that mechanical forces have been shown to impact on innate immunity and the data have direct relevance to human disease.
Grant Support
University of Newcastle post graduate scholarship, The Singleton Foundation.
Conflict of Interest
Nil
TO‐041: Potential protective role of microRNA‐22 against airway remodelling
Fatemeh Moheimani1,2, Teresa Williams1,2, Andrew T. Reid1,2, Peter A. Wark 1,2, Darryl A. Knight1,2,3
1School of Biomedical Sciences and Pharmacy, University of Newcastle (UoN), Callaghan, NSW, Australia, 2Priority Research Centre for Healthy Lung, Hunter Medical Research Institute (HMRI), The University of Newcastle, NSW, Australia, 3Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver, Canada
Introduction/Aim
The epithelium of asthmatics is differentially dysregulated, which may allow repair but not proper regeneration after noxious stimuli (e.g. viruses and allergens) leading to further remodelling. The influenza virus H1N1 is one of the major causes of asthma exacerbations. Differentiation specific microRNAs; e.g. miR‐22, may be key epigenetic factors involved in aberrant epithelial cell differentiation of asthmatics upon exposure to H1N1. We hypothesise that the impaired miR‐22 expression in epithelium of asthmatics after H1N1 infection may be the link between abnormal differentiation and innate immune dysregulation in these cells. Our aims are to determine the role of miR‐22 in primary bronchial epithelial cells of severe asthmatics by determining its target.
Methods
Primary bronchial epithelial cells (pBEC) from severe asthmatic and non‐asthmatic subjects were cultured under air‐liquid‐interface (ALI) condition. Cells were incubated with H1N1 (MOI 5). miRNAs and mRNA were isolated using RNAeasy mini kit with some modifications and subjected to Taqman miR‐22 and mRNA assays.
Results
pBEC from non‐asthmatics and asthmatics infected with H1N1 showed the same viral titers. In cells from non‐asthmatics, miR‐22 expression decreased 6h after infection but then incresased and recovered to basal levels by 24h post infection. In cells from asthmatics, miR‐22 expression remained unchanged during infection. Expression of the miR‐22 targets, CD147 (MMP inducer) and HDAC4 (epigenetic regulator) mRNA were decreased during infection in cells from non‐asthmatics. However in cells from asthmatics, CD147 expression increased during infection and HDAC4 remained unchanged.
Conclusion
Despite similar level of infection, miR‐22 expression differs in epithelial cells from asthmatics and non‐asthmatics during H1N1 infection. The reduction of CD147 and HDAC4 during H1N1 infection in cells from non‐asthmatics may represent a self‐defence mechanism against further cellular remodelling.
Grant Support
McDonald Jones Homes Group grant‐HMRI to FM and DK, NHMRC project grant # 1064405 to DK.
Grant Support
Cell Biology/Immunology 1
TO‐042: Acute inhibition of NOTCH signalling ablates MUC5AC production in human airway epithelial cells from Asthmatic, Non‐Asthmatic and COPD donors.
Andrew Reid1,2, Fatemeh Moheimani1,2, Kristy Nichol2,3, Nathan Bartlett1,2, Peter Wark2,3,4, Chris Grainge2,4, Darryl Knight 1,2,5
1School of Biomedical Sciences and Pharmacy, University of Newcastle, Callaghan, NSW, 2Priority Research Centre for Healthy Lung, Hunter Medical Research Institute (HMRI), The University of Newcastle, NSW, Australia, 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, NSW, 4School of Medicine and Public Health, University of Newcastle, Callaghan, NSW, 5Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver, Canada
Introduction
Mucus overproduction in patients with asthma and COPD is linked to increased hospitalisations and morbidity. The Notch family of receptor proteins regulate airway mucus production via differentiation mechanisms that direct cells towards secretory or ciliated morphology. However little is known about Notch's role during mucus production, following differentiation.
Aim/Hypothesis
To examine the impact of inhibiting Notch signalling on mucus production in fully differentiated primary bronchial epithelial cells (pBECs) from control subjects as well as patients with asthma or COPD. We hypothesize that Notch inhibition will downregulate mucus production.
Methods
pBECs from 4–5 donors of each cohort were grown at air‐liquid interface (ALI) culture for 25 days to promote multicellular differentiation. At this time, cells were treated with dibenzazepine (DBZ), a potent inhibitor of Notch signalling for a further 96h during which, apical lining fluid was collected every 24h for assessment of Muc5AC release. At the completion of the experiment, samples were also collected for protein, mRNA and histological analysis.
Results
DBZ treatment significantly reduced MUC5AC expression and release in all phenotypes as assessed by qPCR, ELISA and immunofluorescence. Western blotting/qPCR revealed significant reduction of NOTCH3 intracellular domain (NICD3) and Notch3 mRNA in pBEC from all donor phenotypes. Reduced expression of NICD1 was also observed, but was restricted to cells from non‐asthmatic following treatment. Finally, the goblet cell marker protein CLCA1 was unchanged across all treatments.
Conclusion
Notch inhibition reduced MUC5AC expression and secretion from differentiated pBECs, independent of goblet cell number. This reduction is NOTCH3 dependent and occurs in pBECs from control, asthmatics and patients with COPD, suggesting that Notch regulates MUC5AC production independent of secretory cell differentiation. The decrease of NICD1 in pBEC from control donors suggests additional regulation of MUC5AC production that may be compromised in cells from COPD or asthma patients.
Grant Support
NHMRC project grant #1064405.
TO‐043: Cigarette smoke‐induced inflammation in macrophages is initiated by NLRP3/AIM2 inflammasomes: involvement of the sphingosine‐1‐phosphate (S1P) signalling
Hai B Tran1, Rhys Hamon1, Tung T Truong1,2, Miranda Ween1, Eugene Riscioli1, Hubertus Jerssman1,3, Greg Hodge1,3, Paul Reynolds1,3, Sandra Hodge1,3
1Lung Research Unit, Hanson Institute and Dept. Thoracic Medicine, Royal Adelaide Hospital, Adelaide, 2Dept. of TB & Lung Diseases, Hospital 175, HCMC, Vietnam, 3Dept. of Medicine, University of Adelaide, Adelaide, Australia
Introduction/Aim
There have been conflicting reports on the possible role of NLRP3 inflammasome activation in IL‐1‐driven inflammation in COPD. We hypothesized that in COPD and/or in response to cigarette smoke, there is increased activation of the NLRP3 and/or alternative AIM2 inflammasomes, regulated via sphingosine‐1‐phosphate (S1P) signalling.
Methods
Human primary alveolar macrophages and THP‐1‐derived macrophages were analysed for release of IL‐1β (ELISA) and its cleavage‐activation in response to cigarette smoke extract (10%, 24h). Expression and localization of IL‐1β, NLRP3, AIM2, ASC (pro‐caspase‐1 recruiter), and cleaved caspase‐1 were assessed by immunofluorescence/confocal microscopy and/or Western blot. The effects of the caspase‐1 inhibitor ZYVAD‐fmk or NLRP3 antagonist glyburide, and treatment with S1P or the S1P receptor regulator FTY720, with or without exposure to cigarette smoke extract were investigated.
Results
In alveolar macrophages, cigarette smoke induced increased intracellular expression of IL‐1β (~15%, p<0.05 on pooled data from 3 donors), with particulate staining for cleaved IL‐1β increased both inside and outside the cell (5 fold, p<0.001 on pooled data). These particles were partially co‐localized with particulate NLRP3 or AIM2 which were also increased. In THP‐1 macrophages, cigarette smoke induced similar NLRP3/cleaved IL‐1β complexes, which were inhibited by 20uM ZYVAD‐fmk or 20uM glyburide (p<0.05). At 10nM, S1P or FTY720 significantly protected THP‐1 macrophages from cigarette smoke‐induced activation of IL‐1β.
Conclusion
IL‐1‐driven inflammation in cigarette smoke‐exposed macrophages is initiated by both NLRP3 and AIM2 inflammasomes, the former regulated by S1P signalling system, which suggests novel therapeutic targets in COPD.
TO‐044: Evaluating anti‐CD20 therapy for STAT3‐mediated lung fibrosis
Cecilia M Prêle1,2, David Pearce3, Andrew D Lucas2, Chuan Bian Lim1,2, Svetlana Baltic1, Robert O'Donoghue4, Matthias Ernst4, Geoffrey J Laurent1,2, Darryl A Knight5, Gerard Hoyne6, Robin MCANULTY3 and Steven E Mutsaers1,2
1Institute for Respiratory Health and Centre for Respiratory Health, School of Medicine and Pharmacology, The University of Western Australia, 2Centre for Cell Therapy and Regenerative Medicine, School of Medicine and Pharmacology, The University of Western Australia and Harry Perkins Institute of Medical Research, Nedlands WA, 3Centre for inflammation and Tissue Repair, Division of Medicine, University College London, London UK, 4Olivia Newton John Cancer Research Institute, Heidelberg, VIC, 5The University of Newcastle, Callaghan, NSW, 6The University of Notre Dame, Perth WA.
Introduction
The STAT3 signalling pathway has recently been implicated in the pathogenesis of Idiopathic Pulmonary Fibrosis (IPF).
Hypothesis
We hypothesise that the pro‐fibrotic effects of STAT3 involve B cell‐mediated immune regulation.
Methods
We have analysed immune cell composition in human lung biopsy tissue and examined the effect of B cell depletion on bleomycin‐induced lung fibrosis in vivo.
Results
A trend towards increased B‐cell activating factor, APRIL and CXCL13 are observed in IPF patient serum versus age match controls. In addition we observed an increase in the number of mature B cells in the lungs of IPF patients. Genetic depletion of B cells in gp130757F;μT −/− attenuated bleomycin‐induced fibrosis. The therapeutic potential of depleting follicular B cells using anti‐CD20 treatment was assessed. Mice were given two 100 μg doses of anti‐CD20 antibody (provided by Genentech Inc USA), or IgG2a isotype control i.p. 7 days prior to and 7 days after bleomycin, and the extent of fibrosis measured 21 days after the last dose. FACS analysis of blood taken on days 0, 7 and 28 days post‐bleomycin‐treatment revealed an almost complete depletion of CD19+ and B220+ B cells. However, the extent of fibrosis, assessed using micro‐CT imaging and HPLC analysis of hydroxyproline levels, was not significantly different between treatment groups.
Conclusion
Although antibody depletion of follicular B cells had no effect on bleomycin‐induced fibrosis, residual B cells remained in the lung of these mice. Current studies are analysing B cell subsets in fibrotic lung tissue from mice and IPF patients.
Grant Support
This work is funded by NHMRC Project Grant GNT1067511 and a British Lung Foundation Priming Grant.
TO‐045: Interaction of dietary fatty acids with obesity‐induced cytokines in primary pulmonary fibroblasts
Sandra Rutting1,2, Lisa Wood4, Phil Hansbro2, Brian Oliver1,3
1 Cellular and Molecular Biology, Woolcock Institute of Medical Research, Sydney, Australia, 2 Priority Research Centre for Asthma and Respiratory Disease, The University of Newcastle, Newcastle, Australia, 3 School of Medical and Molecular Biosciences, University of Technology Sydney, Sydney, Australia, 4 School of Biomedical Science and Pharmacy, University of Newcastle, Newcastle, New South Wales, Australia
Introduction
Obesity is an important risk factor for developing severe asthma. Dietary fatty acids, increased in the serum of obese people, activate systemic innate immune responses. Furthermore, we have shown that a single high fat meal increases airway inflammation and impairs bronchodilator recovery in asthma.
Aim
The aim of this study was to investigate whether dietary fatty acids directly cause inflammation and/or synergise with obesity‐induced cytokines in human pulmonary fibroblasts and to elucidate underlying mechanisms.
Methods
Primary human pulmonary fibroblasts were incubated with BSA‐conjugated fatty acids for 24hr, before stimulation with TNFα for another 24hr. IL‐6 and CXCL8 release was measured using ELISA. IL‐6 acts as a general marker for inflammation and CXCL8 is a potent neutrophilic chemoattractant. The following fatty acids were used: arachidonic acid (AA, ω‐6), eicosapentaenoic acid (EPA, ω‐3), and palmitic acid (PA, saturated fatty acid) at increasing concentrations of 1, 10 and 100μM.
Results
AA induced substantial IL‐6 (n=11, P<0.05) and CXCL8 (n=9, P<0.0001) release by pulmonary fibroblasts. EPA and PA did not induce CXCL8 or IL‐6 release. Stimulation with the combination of AA and TNFα resulted in greater IL6 (n=9, P < 0.0001) and CXCL8 (n=8, P <0.0001) release than AA alone. The effect of the combination AA/TNFα on IL‐6 release was greater than the sum of the individual effect of AA and TNFα, indicating synergy.
Conclusion
These findings suggest that dietary fatty acids are important modulators of inflammatory responses and that there is an interaction between arachidonic acid and TNFα, resulting in a synergetic inflammatory response in pulmonary fibroblasts. This could indicate that obese asthmatics compared to lean individuals, are more prone to airway inflammation after a high fat meal.
Grant Support
Nil
TO‐046: Novel role of inflammasomes in the molecular pathogenesis of emphysema
Saleela M. Ruwanpura1, Louise McLeod1, Lovisa F. Dousha2, Paul T. King1,3, Philip G. Bardin1,3, Gary P. Anderson2 and Brendan J. Jenkins1
1Centre for Innate Immunity and Infectious Diseases, Hudson Institute, Monash University, Victoria, 3168, Australia, 2Department of Pharmacology and Therapeutics, The University of Melbourne, Parkville, Victoria, 3050, Australia, 3Monash Lung and Sleep, Monash Medical Centre, Victoria, 3168, Australia.
Introduction/Aim
Innate immune responses within the lung mucosa, for instance against cigarette smoke (CS), depend on the activation of pattern recognition receptors via multiprotein complexes called inflammasomes, which facilitate the maturation and release of the pro‐inflammatory cytokines interleukin (IL)‐1β and IL‐18. In recent years a plethora of data from clinical studies and mouse disease models have demonstrated that excessive inflammasome activation promotes several diseases. In that regard, emphysema a major debilitating components of COPD, has shown a link between IL‐1β and IL‐18 and disease. Despite these observations, a causal role for specific inflammasomes in emphysema is unknown. Therefore we aim to reveal a novel functional link between inflammasome activation and the pathogenesis of emphysema.
Methods
To identify whether inflammasomes promote emphysema, we have utilised a genetic model (gp130 F/F) for spontaneous emphysema and an acute (4 days) CS‐induced model, both characterised by elevated alveolar type II cell (ATIIC) apoptosis that is driven by the cytokine IL‐6.
Results
Here, we demonstrate that lung tissues from emphysema patients, as well as from spontaneous (gp130 F/F mice) and CS‐induced emphysema mouse models, are characterized by excessive productions of the gene encoding AIM2 which forms a cytoplasmic DNA‐sensing inflammasome and IL‐1β (but not IL‐18) protein. Furthermore, genetic blockade of Aim2 in gp130 F/F mice prevents the development of emphysema by suppressing augmented ATIIC apoptosis. A positive correlation also exists between elevated IL6 and AIM2 mRNA levels, and AIM2 mRNA and IL‐1β protein expression levels, in emphysema patients.
Conclusion
Collectively, we define for the first time that hyper‐activation of the endogenous IL‐6/AIM2/ IL‐1β axis in the lung augments ATIIC apoptosis, which in turn causes emphysema. Finally, we believe our study also has the potential to aid future therapeutic strategies to target inflammasomes (AIM2) alone or in combination with IL‐6 in human emphysema.
Grant Support
Nil
TO‐047: Steroid resistant CD8+CD28nullNKT‐like pro‐inflammatory cytotoxic cells in COPD
Greg Hodge1,2, Hubertus Jersmann1,2, Mark Holmes1,2, Paul N. Reynolds1,2, Sandra Hodge1,2
1Lung Research, Hanson Institute and Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, South Australia, 2Department of Medicine, University of Adelaide, Adelaide, South Australia
Introduction
NKT‐like cells represent a bridge between innate and adaptive immunity. We have reported increased numbers of steroid resistant cytotoxic/pro‐inflammatory senescent CD28nullNKT‐like cells in BAL in COPD associated with increased cytotoxicity to bronchial epithelial cells. These cells express drug efflux pump Pgp‐1 and loss of glucocorticoid receptor (GCR). Recently, loss of histone deacetylase 2 (HDAC2) and heat shock protein 90 (Hsp90) have been reported from CD8+ T cells from COPD patients and we hypothesized these molecules may be decreased in CD28nullNKT‐like cells (particularly the CD8+ subset).
Method
Blood was collected from a group of COPD patients and aged matched controls and expression of CD28, Pgp‐1, GCR, HDAC2, Hsp90 and pro‐inflammatory cytokines determined in CD8+ and CD8‐ NKT‐like cells in the presence of ± 1μM prednisolone ± 2.5ng/mL cyclosporine A (binds to GCR‐Hsp90 complex) ± 5 μg/mL theophylline following culture using flow cytometry, western blot and immunofluorescence.
Results
Loss of GCR, HDAC2 and Hsp90 (but not Pgp‐1) expression was identified from CD28nullCD8+NKT‐like cells compared with CD28+ counterparts. Loss of GCR, HDAC2 and Hsp90 was associated with increased production of IFNγ and TNFα and increased steroid resistance. Upregulation of GCR, HDAC2 and Hsp90 was noted in the presence of prednisolone + low dose cyclosporine A and increased HDAC2 was noted in the presence of prednisolone + theophylline.
Conclusion
Steroid resistance in pro‐inflammatory CD28nullCD8+NKT‐like cells is associated with multiple mechanisms. Combination prednisolone, low‐dose cyclosporine A and theophylline treatment therapy inhibits pro‐inflammatory cytokine production from these cells and may reduce systemic inflammation in COPD.
Grant Support
NHMRC
Declaration of Interest
No declaration of interest
Chronic Obstructive Pulmonary Disease 3
TO‐048: Effect of tiotropium and olodaterol, alone and with exercise training, on exercise endurance in COPD
Peter Frith1on behalf of Thierry Troosters2, Jean Bourbeau3, François Maltais4, Nancy Leidy5, Damijan Erzen6, Dorothy De Sousa7, Lawrence Korducki8, Kim L Lavoie9,10, Wim Janssens11, and Alan Hamilton7
1Respiratory Medicine, Repatriation General Hospital and Flinders University, SA, Australia, 2KU Leuven, Department of Rehabilitation Sciences and University Hospital Leuven, Pulmonary Rehabilitation and Respiratory Division, Leuven, Belgium, 3Respiratory Epidemiology and Clinical Research Unit, McGill University Health Centre, Montreal, Quebec, Canada, 4Centre de Recherche, Institut Universitaire de Cardiologie et de Pneumologie de Quebec, Université Laval, Quebec, Canada, 5Scientific Affairs, Evidera, Bethesda, Maryland, United States of America, 6Department of Clinical Operations, Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach an der Riss, Germany, 7Medical Department, Boehringer Ingelheim (Canada) Ltd, Burlington, Ontario, Canada, 8Department of Biostatistics & Data Sciences, Boehringer Ingelheim Pharmaceuticals Inc., Ridgefield, Connecticut, United States of America, 9Montreal Behavioural Medicine Centre, Research Centre, Hopital du Sacré‐Coeur de Montreal, Montreal, Quebec, Canada, 10Department of Psychology, University of Quebec at Montreal (UQAM), Montreal, Quebec, Canada, 11Respiratory Division, University Hospital Gasthuisberg, Leuven, Belgium
Introduction/Aim
Physical deconditioning is common in patients with COPD, limiting exercise tolerance. PHYSACTO® (NCT02085161) tested the effects of bronchodilators alone or with exercise training (ExT), combined with a standardised physical activity selfmanagement behaviour‐modification (BM) programme, on exercise endurance time (EET) in patients with COPD.
Methods
A 12‐week randomised, partially double‐blind, placebo (P)‐controlled, parallel‐group trial at 34 sites in Australia, New Zealand, USA, Canada and Europe. Interventions (all with 12‐week BM): P; tiotropium (T) 5 μg; T + olodaterol (T+O) 5/5 μg; T+O 5/5 μg with 8 weeks' ExT (T+O 5/5 μg + ExT). EET (log transformed) during an endurance shuttle‐walk test (ESWT) to symptom limitation was assessed after 8 weeks (primary end point) and 12 weeks.
Results
303 patients (200 men) were randomised and treated (full analysis set n=274). Mean post‐bronchodilator FEV1 was 1.59 L (56.7% predicted). EET significantly increased with T+O 5/5 μg and T+O 5/5 μg + ExT versus P at 8 weeks (Figure); 13 patients reached test termination criteria (20 minutes) without symptom limitation (P, n=0; T, n=3; T+O, n=2; T+O + ExT, n=8) at 8 weeks. No safety concerns were identified.
Conclusion
T+O 5/5 μg, alone and combined with ExT, improved EET during ESWT compared to P in moderate to severe COPD.

Grant Support
The study was funded by Boehringer Ingelheim
Declaration of interest statement
PF has received in the past 5 years honoraria for educational and advisory board involvement and/or received conference attendance support for the following: Global Initiative for COPD (GOLD), Improvement Foundation, Lung Foundation Australia, and Remedy Healthcare; AstraZeneca, Boehringer Ingelheim, CSL‐Behring, GlaxoSmithKline, Menarini, MundiPharma, and Novartis. TT is the Principal Investigator of PROactive project and received speakers/consultancy fees from Boehringer Ingelheim, Novartis, and Bayer. JB received research funding via the Research Institute of the McGill University Health Centre from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Merck, Novartis, Nycomed, Pfizer and Theratechnologies; and has served on speakers, consultation panels and/or advisory boards for these pharmaceutical companies. FM is a consultant for Boehringer Ingelheim and served on advisory boards for Boehringer Ingelheim, GlaxoSmithKline, and Pfizerand has received payment for lectures including service on speaker bureaus from Boehringer Ingelheim, GlaxoSmithKline, Nycomed and Pfizer. NL is an employee of Evidera and works with a variety of companies and organizations and expressly prohibited from receiving any payment or honoraria directly from these organizations for services rendered. DE, DDS, LK and AH are employees of Boehringer Ingelheim. WJ served on advisory boards and/or speaker bureaus for Astra Zeneca, Boerhinger Ingelheim, Novartis and GSK. KLL received grants/research support from GSK, consulting fees from Schering‐Plough and Merck Frosst and served on speaker bureaus/honoraria for GSK, Astra‐Zeneca, Pfizer, Merck Frosst, Air Liquide and Health International.
Declaration of interest statement: Peter Frith has received in the past 5 years honoraria for educational and advisory board involvement and/or received conference attendance support for the following: Global Initiative for COPD (GOLD), Improvement Foundation, Lung Foundation Australia, and Remedy Healthcare; AstraZeneca, Boehringer Ingelheim, CSL‐Behring, GlaxoSmithKline, Menarini, MundiPharma, and Novartis.
TO‐049: Responsiveness of two‐minute walk distance after pulmonary rehabilitation in chronic obstructive pulmonary disease
Kylie Johnston1, Adrian Potter2, Anna Phillips3
1International Centre for Allied Health Evidence, Sansom Institute for Health Research, University of South Australia, 2School of Health Sciences, University of South Australia, 3School of Health Sciences, University of South Australia
Aim
Field exercise tests (e.g. six minute walk distance [6MWD]) are important measures of functional exercise capacity in people with COPD. Shorter tests such as the two‐minute walk distance may offer advantages in some populations, but lack information about responsiveness to change. This study examined reliability, validity and responsiveness of the two‐minute walk test in people with COPD attending pulmonary rehabilitation (PR).
Methods
At pre‐PR assessment, study participants completed a two‐minute walk test twice in addition to usual measures (6MWD, Chronic Respiratory Questionnaire). At post‐PR assessment following a standard PR program, measures were repeated and global rating of change scores obtained (patient and therapist). Pre‐post program change scores were examined for correlations with change in two‐minute walk distance and used (where r>0.3) to estimate the minimal importance difference through anchor‐based methods. Distribution‐based estimates based on standard error of measurement were examined. Test‐retest reliability (ICC, Bland Altman agreement) and validity (Pearson correlation with 6MWD) were reported.
Results
Pre‐program assessment was conducted in 59 participants (68±10 years, FEV1%pred=48 ± 20%). Test‐retest reliability of two‐minute walk distance was high (ICC=0.985) with mean difference between trials of 2.4m (95%CI 0.7 to 4.0, p=0.006). Two and six‐minute walk distance was highly correlated (r=0.87, p<0.01). Post‐program assessment was completed in 36 patients (69 ± 8 years, FEV1%pred=52 ± 21%). Anchored against clinically meaningful change in 6MWD, the minimal important difference in two‐minute walk distance was 3.5m (area under curve=0.82, 95%CI 0.67 to 0.97) and agreed with the distribution‐based estimate of 3.4m. Two‐minute walk distance and 6MWD did not significantly improve post‐program in this sample, in contrast to QOL measures.
Conclusion
Improvement in two‐minute walk distance of at least 3.5m following a PR program corresponded to a clinically meaningful change. Due to a learning effect between first and second trials a practice two‐minute walk test is recommended.
Grant Support
Nil
TO‐050
No additional benefit for 6MWT or HADs in combining cognitive behavioural therapy and pulmonary rehabilitation
Marie T Williams1 , David John 2, Paul Cafarella3 , Peter Frith2,3
1Health and Alliance for Research in Exercise, Nutrition and Activity (ARENA), Sansom Institute for Health Research, School of Health Sciences, University of South Australia, South Australia, Australia, 2School of Health Sciences, University of South Australia, South Australia, Australia, 3Department of Respiratory Medicine, Southern Adelaide Local Health Network & School of Medicine, Flinders University of South Australia, South Australia, Australia
Introduction/Aim
Controlled trials of psychological interventions in people with chronic obstructive pulmonary disease (COPD) generally target generalised anxiety and depression. This randomised controlled trial aimed to determine whether adding a cognitive behavioural therapy program for the sensation of breathlessness (CBT‐BREVE) to a comprehensive pulmonary rehabilitation program (CPRP) significantly improved health outcomes beyond those achieved with a CPRP alone.
Method
Eight week CPRP cycles at the Repatriation General Hospital were block randomised to include CBT (BREVE) or social group (CPR) interventions. People with COPD and at least moderate airflow obstruction (FEV1 < 80 % pred, FEV1/FVC <70%, GOLD Grade ≥ 2) were eligible for inclusion. Primary (six minute walk test ‐ 6MWT, Hospital Anxiety and Depression scale ‐HADs) and secondary outcomes (Multidimensional Dyspnoea Profile ‐MDP, Chronic Respiratory Questionnaire‐ CRQ, sedentary and physical activity (accelerometry ‐Actigraph GT3X+) and symptom scores) were assessed one month before and one, six and 12 months post intervention. Participant feedback was sought after completion of the 12 month assessment. Differences between groups (intention to treat) were assessed across all four assessment points with random effects mixed models
Results
101 participants met all inclusion criteria with no significant (p<0.001) differences between subjects eligible for participation but declining (n=66 GOLD grade ≥ 2)) and those participating in the trial (n=101 mean age 70.1 ± SD 8.5, 54 males, FEV1 % pred 47.7 ± 16.3). Preliminary analysis indicates no statistical or clinically significant differences between groups at any assessment point for 6MWT or HADs. Analysis of secondary outcomes is ongoing. Participant feedback was uniformly positive for both forms of intervention
Conclusion
Despite overwhelmingly positive feedback for the CBT program, combining CPR with a CBT program specific for sensation of breathlessness did not result in greater improvements in functional exercise capacity, anxiety or depression, beyond those achieved with standard CPR.
Key Words
Pulmonary rehabilitation, chronic obstructive pulmonary disease, cognitive behavioural therapy
Grant Support
National Health and Medical Research Council Project Grant (# 1010309) Clinical Trial registration: ANZCTR12611000292976
TO‐051: Enhancement of training response following pulmonary rehabilitation with downhill walking: a randomised controlled trial.
Christian Osadnik1,2,3,4*, Carlos A. Camillo2*, Matthias Loeckx2,5, Fernanda M Rodrigues2, Miek Hornikx5, Heleen Demeyer2, Chris Burtin6, Wim Janssens2, Thierry Troosters2,5
1Department of Physiotherapy, Monash University, Melbourne, VIC, Australia, 2Department of Rehabilitation Sciences, KU Leuven, Leuven, Belgium, 3Monash Lung and Sleep, Monash Health, Melbourne, VIC, Australia, 4Institute for Breathing and Sleep, Heidelberg, VIC, Australia, 5Respiratory Division and Rehabilitation, UZ Gasthuisberg, Leuven, Belgium, 6Rehabilitation Research Centre, Biomedical Research Institute, Faculty of Medicine and Life Sciences, Hasselt University, Diepenbeek, Belgium, *Both authors contributed equally
Introduction/Aim
Downhill walking (DW) enhances quadriceps contractile muscle fatigue (CMF) with less symptoms than level walking (LW) in patients with COPD. This study sought to determine the effectiveness of DW compared to LW as part of a 12‐week comprehensive pulmonary rehabilitation program in patients with COPD.
Methods
39 COPD patients (62±9yrs; FEV1 49±17%pred) were randomised to PR with DW or LW. Exercise capacity (6‐minute walk test, 6MWT [primary outcome]; cycle endurance test), muscle function and quality of life were assessed before and after program completion. Training responses and the proportion of patients exceeding the 30m minimally important difference (MID) for 6MWT were compared between groups via Chi2 test.
Results
The magnitude of improvement was similar across all outcomes in both groups (Table 1). However, a significantly greater proportion of patients in DW exceeded the 6MWT MID compared to LW (94% vs 65%, p=0.03).
Table 1. Training responses in LW and DW.
| Outcome | LW (n=17) | DW (n=22) | p value |
|---|---|---|---|
| Δ 6‐minute walk test (metres) | +67 [22–103] | +62 [45–98] | 0.52 |
| Δ Cycle endurance test (seconds) | +260 [55–665] | +740 [85–885] | 0.16 |
| Δ Muscle Force (NM) | +29 [13–48] | +17 [5–26] | 0.20 |
| Δ CRDQ (total points) | +12 [10–22] | +20 [10–27] | 0.47 |
Conclusion
These results support the use of downhill walking as a useful adjunct in pulmonary rehabilitation programs for patients with COPD.
Grant Support CAC ‐ CNPq/Brazil (202425/2011–8); CO ‐ ERS (LTRF 2014); HD ‐ ERS/SEPAR (LTRF 2015); TT‐ FWO/Belgium (G.0871.13).
TO‐052: The effect on HRQoL of ongoing feedback during a maintenance walking program : An RCT
Wootton SL 1,2, McKeough ZJ 1, Ng LWC 3,4, Jenkins SC 4,5,6, Hill K4,6, Eastwood PR 4,7,8, Hillman DR7 , Jenkins C9, Cecins N 5, Spencer LM 10, Alison JA 1,10
1Discipline of Physiotherapy, The University of Sydney, New South Wales, Australia, 2Chronic Disease Community Rehabilitation Service, Northern Sydney Local Health District, New South Wales, Australia, 3Physiotherapy Department, Singapore General Hospital, Singapore, 4School of Physiotherapy and Exercise Science, Faculty of Health Sciences, Curtin University, Western Australia, Australia, 5Physiotherapy Department, Sir Charles Gairdner Hospital, Western Australia, Australia, 6Institute for Respiratory Health, Western Australia, Australia, 7Department of Pulmonary Physiology & Sleep Medicine, Sir Charles Gairdner Hospital, Western Australia, Australia, 8Centre for Sleep Science, School of Anatomy, Physiology & Human Biology, University of Western Australia, Australia, 9Department of Thoracic Medicine, Concord Hospital, New South Wales, Australia, 10Physiotherapy Department, Royal Prince Alfred Hospital, New South Wales, Australia
Introduction/Aim
This study evaluated the effect on health‐related quality of life (HRQoL), endurance exercise capacity and daily physical activity of the addition of ongoing feedback (Intervention Group [IG]) versus no feedback (Control Group [CG]), to a 12‐month unsupervised maintenance walking program which followed a supervised walking training program in people with COPD.
Methods
Participants were randomised at baseline to the IG or CG. Both groups completed the same 2‐month supervised, walking training program followed by a 12‐month unsupervised maintenance walking program during which the IG received ongoing feedback (telephone calls, biofeedback and progressive goal setting) and the CG received no feedback.
Results
Seventy‐five of 95 (79%) participants who entered the maintenance program [mean (SD): age 69 (8) yrs.; FEV1 43% predicted (15)] completed the study. There were no between‐group differences in HRQoL, endurance exercise capacity or daily physical activity levels on completion of the 12‐month maintenance program when compared to baseline measures (St George's Respiratory Questionnaire [SGRQ] total score mean difference (MD): 2 point, 95% CI −4 to 8; Endurance Shuttle Walk Test [ESWT] time: MD −96 seconds, 95% CI −253 to 61; Daily steps: MD 757 steps, 95% CI −103 to 1617) or compared to the 2‐month assessment (following supervised training) (SGRQ total score MD: 4 points, 95% CI −2 to 10; ESWT time: MD −54 seconds, 95% CI −254 to 137; Daily steps: MD 617 steps 95% CI −435 to 1669).
Conclusion
This study demonstrated that following a 2‐month supervised walking training program, ongoing feedback was no more effective than no feedback in maintaining HRQoL, endurance exercise capacity or daily physical activity levels in people with COPD during a 12‐month unsupervised maintenance walking program.
Grant Support
Australian National Health and Medical Research Council project grant: 570814
Declaration of interest
Nil.
Nomination for awards
Physiotherapy
TO‐053: Participants who do not achieve the MID in the 6MWT may still have a training‐response
N.R. Morris1,2,3, L.Adams1, J.Paratz1, Z MCKEOUGH4 and J.R Walsh1,3
1Menzies Health Institute of Queensland and School of Allied Health Sciences, Griffith University, Southport, QLD. Australia, 2Allied Health Research Collaborative. The Prince Charles Hospital. Brisbane. QLD., 3Heart Lung Institute. The Prince Charles Hospital Brisbane. QLD. Australia, 4Discipline of Physiotherapy. The University of Sydney. Sydney, NSW. Australia
Introduction/Aim
The six minute walk test (6MWT) is a clinical tool widely used for evaluating functional exercise capacity. The primary outcome of the 6MWT is the six minute walk distance (6MWD). Current practice recognises the use of the minimally important difference (MID) as a key index of a response to pulmonary rehabilitation (PR). However, the 6MWT also provides information on dyspnoea, heart rate (HR) and degree of desaturation (nadir SpO2) achieved during the test. This information is typically not considered when evaluating patient outcome to PR. Whilst an individual may not achieve the MID, it is possible other indices from the 6MWT may reflect improvement. The aim of this study was to compare changes in peak dyspnoea, HR and nadir SpO2 following PR in participants that did not have a clinically significant change (non‐MID) in their 6MWD (−30m≤MID≤30m) with a group that did achieve the MID (>30m).
Methods
Data was retrospectively analysed from subjects that completed a 6MWT both pre and post PR over a 2 year period. The 6MWT was measured prior to and immediately following an 8 wk, twice weekly PR program. Dyspnoea (0–10 Borg scale) and HR were recorded immediately at the end of the 6MWT while nadir SpO2 was measured during the test.
Results
81 subjects did not achieve the MID (∆6MWD: 3 ± 17m) whereas 91 subjects achieved the MID (∆6MWD: 74 ± 42m). For the non‐MID group, following PR subjects reported a lower dyspnoea (∆=0.7 ± 1.7, p<0.01) and lower nadir SpO2 (∆=1.3 ± 4.4%, p<0.01) whereas HR remained unchanged (∆=2.6 ± 13.5 beats.min −1, p=0.12). For the MID group, nadir SpO2 (∆=1.6 ± 4.7%, p<0.01) was lower following PR and there was a tendency for dyspnoea (∆=0.4 ± 1.9, p=.053) to be lower. End exercise HR for the MID group remained unchanged (∆=0.2 ± 12.3 beats.min −1, p=0.9).
Conclusion
These data demonstrate the benefit of using all the data obtained from the 6MWT to evaluate the overall response to PR. Individuals who may not show a clinical improvement in 6MWD may be less breathless during the 6MWT suggesting an improved response to exercise. Whilst the 6MWD remains the primary outcome from the 6MWT, other exercise related indices from this test should be considered when evaluating overall response to an intervention.
Grant Support
Nil
Paediatric
TO‐054: Patients with X‐linked retinitis pigmentosa have altered airway cilial function and structure
Gabby McCray1 , John Ruddle2,3, Paul Griffin1, Paul Martinello1, Philip Robinson1
1Respiratory Medicine, Royal Children's Hospital, Melbourne, Australia, 2Opthalmology Dept, Royal Children's Hospital, Melbourne, 3Royal Eye and Ear Hospital, Melbourne
Introduction/Aim
Cilia are tentacle‐like extensions from cell bodies, which are motile or immotile depending on their function. The airways contain motile cilia to move mucus, whereas cilia in the eyes act as immotile sensory antennas. Ciliopathies are diseases caused by developmental defects in motile or immotile cilia. Relationships between motile ciliary diseases and immotile ciliary diseases have not been studied. Case reports have emerged that infer patients exist with a phenotype consistent with both diseases. We hypothesised that patients with a pre‐diagnosed immotile ciliopathy – Retinitis Pigmentosa – will also have altered motile cilia
Methods
The inferior nasal turbinate was brushed for samples of airway epithelium from 12 patients (range 8–73 years) with Retinitis Pigmentosa. Epithelial strips of each patient were examined under high‐speed videomicroscopy to capture ciliary waveform and beat frequency. Epithelium was also processed for electron microscopy and cilia were photographed. Ciliary structure and orientation was quantified from these photographs. A Mann–Whitney U test was used to analyse the difference in ciliary orientation between patients with and without Retinitis Pigmentosa.
Results
Ciliary beat frequency of patients with Retinitis Pigmentosa was normal (mean 8Hz). Ciliary waveform was uncoordinated in video playback. Mean Ciliary Deviation of normal patients was 17°, which was in keeping with previously published normal values. Mean Ciliary Deviation of Retinitis Pigmentosa patients was 32°, which is considered almost random orientation of cilia on a cell surface.
Conclusion
Our data demonstrates a shared developmental link between motile and immotile cilia and may help explain the previously reported predisposition to respiratory problems in some patients with Retinitis Pigmentosa. Airway cilia movement was uncoordinated and the cilia may have been malfunctioning due to almost random ciliary orientation. Further clinical evaluation is required to characterise the respiratory history of patients with Retinitis Pigmentosa.
Grant Support
Nil
TO‐055: Detection and definition of abnormal paediatric breath sounds using digital stethoscopes compared to standard auscultation
Ajay C Kevat1,2, Anaath Kalirajah1,3, Robert Roseby1,3
1Monash Health, Clayton VIC 3168, 2Royal Children's Hospital, Parkville VIC 3052, 3Monash University, Clayton VIC 3168
Introduction/Aim
The audio characteristics of abnormal paediatric breath sounds are not well‐defined and digital techniques to capture them have not been widely investigated. Our study aimed to define the audiological features of abnormal paediatric breath sounds objectively and compare the ability of digital stethoscopes to detect them against auscultation using standard bell‐and‐diaphragm stethoscopes.
Methods
Twenty children with normal breath sounds, generalized wheeze or crackles, and some with a diagnosis of cystic fibrosis were auscultated by a paediatric consultant and digitally recorded using both the Littman™ 3200 Digital Electronic Stethoscope and a Clinicloud™ Digital Stethoscope. We used spectrographic analysis and recording playback to detect abnormal breath sounds and define their audio waveform characteristics.
Results
Digital stethoscopes were more sensitive than standard auscultation in detecting wheeze in our study. Patients with clinically‐described wheeze had periodic waveform segments of increased intensity and frequency compared to background breath sounds, mostly spanning expiration for a period of 0.03–1.2 seconds at frequencies of 100–1050Hz, and occasionally spanning shorter inspiratory segments. Recordings of patients with crackles revealed brief (6–20 millisecond) discontinuous sounds with a distinguishing waveform identifiable within them.
Conclusion
Digital breath sound analysis may be more sensitive than manual auscultation in detecting breath sound abnormalities in children, with potential applications for improved diagnosis, data sharing and disease monitoring. Further research and development is needed.
Grant Support
Nil
TO‐056: The effect of particle size delivered by pressurized meter dose inhalers (pMDIs) in asthmatic adolescents
Natalie Johnson1, William Ditcham1, Charlotte Allen2, Stephanie Trend1,3, Sunalene Devadason1
1School of Pediatrics and Child Health, University of Western Australia, Australia, 2Department of General Pediatrics, Princess Margaret Hospital for Children, Western Australia, Australia, 3Telethon Kids Institute, Centre for Child Health Research, University of Western Australia, Australia
Introduction/Aim
Spacer device use is currently recommended with aerosolised corticosteroids to reduce mouth and throat deposition produced by larger particle generating inhalers. Anecdotally, spacers are seldom used as prescribed, which has particularly been observed in the adolescent age group at Princess Margaret Hospital for Children in Perth. The recommendation to use a spacer may not be necessary with new asthma medications producing smaller particle sized aerosols. We aimed to assess the effect of particle size in pMDIs with and without a spacer.
Methods
Fourteen adolescents aged 13–17 years with mild stable asthma were randomised to use a pMDI with or without a spacer in a randomised cross‐over study. Radiolabelled (Tc99m) corticosteroids of different mass median aerodynamic diameters (fluticasone propionate 3.5 μm (Flixotide®), and becolmethasone diproprionate 1.1μm (QVAR™)) were inhaled using correct technique, as assessed by a Clinical Nurse Specialist, and dose of drug quantified immediately after with a 2D gamma camera scan. Radiation detected was quantified per region of interest accounting for attenuation by body tissues. Drug deposition in the lungs and orogastric regions was compared in adolescents inhaling the same drug with and without a spacer using a Wilcoxon matched pairs signed‐rank test.
Results
Fourteen adolescents completed two visits each, with and without a spacer. We did not observe a significant difference in the QVAR group lung deposition with or without spacer (median 32.9 vs 23.0, p=0.47) or the Flixotide group lung deposition with and without spacer (median 38.3 vs 34.1, p=0.08). However, we may not have had the power to detect differences given the small sample size in the dataset.
Conclusion
Preliminary data suggests QVAR (p=0.47) may be used without a spacer in adolescents, provided inhalation technique is assessed by an appropriately trained clinical professional. We would still recommend that Flixotide be used with a spacer.
Grant Support
Princess Margaret Hospital Foundation
TO‐057: Effects of in utero smoke exposure on lung function from infancy to adulthood and the contribution of Glutathione S‐transferase polymorphisms
Louisa Owens1,2, Ingrid Laing1,3, Guicheng Zhang1,4,Jasminka Murdzoska3, Steven Turner5, David Mullane6,Des Cox 7, Peter Le Souef1
1University of Western Australia, School of Paediatrics and Child Health, 2 Sydney Children's Hospital Network, Randwick, New South Wales, 3 Telethon Kid's Institute, Perth, Western Australia, 4 Curtin University, Perth, Western Australia, 5 University of Aberdeen, Scotland, 6 Cork University Hospital, Ireland, 7 Our Lady's Children's Hospital, Ireland
Introduction/Aim
In utero smoke exposure is associated with abnormal lung function, wheeze and asthma from infancy and throughout childhood. The negative influence of in utero smoke exposure is modified by genetic polymorphisms in genes important in detoxifying tobacco by‐products, including the Glutathione S‐transferase (GST) gene, a respiratory anti‐oxidant. The longterm effects of in utero exposure on respiratory health into adulthood are unclear.
Methods
The Perth Infant Asthma follow up study is a longitudinal birth cohort of 253 subjects recruited antenatally from a general population with lung function carried out 1, 6,12 months, 6,11,18 and 24 years of age. Antenatal smoking history was collected from both parents at recruitment. DNA was collected at 6 and 11 years on a subgroup of 180 subjects.
Results
Either parent smoking during the pregnancy was associated with wheeze (OR=2.5, 95% CI 1.01‐ 6, p=0.048) and asthma (OR 2.7, 95% CI 1.2‐5.9, p=0.012; n=123) in the offspring at 6 years of age, but not thereafter. Maternal smoking during the pregnancy was associated with reduced lung function in the offspring at 1 month (mean V'maxFRC of 90ml/sec (SD) versus 104ml/sec ; p=0.034; n=242) and 6 years of age (mean FEV1% predicted 99% 15 (SD) versus 105% 15, p=0.039; n=110) but not at later assessments.
Amongst those children exposed to in utero tobacco smoke (n=32), the GSTM1 homozygote null genotype was associated with significantly lower lung function at 6 years of age compared to those with GSTM1 non‐null genotype (mean FEV1% predicted 93.5 15 (SD) versus 104.6; p=0.03).
Conclusion
In utero tobacco smoke exposure negatively impacts lung function and respiratory symptoms up to 6 years of age, but this effect does not persist into adulthood. Polymorphisms in anti‐oxidant genes may contribute to worse lung function in children who were exposed to in utero tobacco smoke.
Grant Support
NHMRC grant 2011
Asthma Foundation of Western Australia PhD top up Scholarship 2013
PMH Foundation Seeding grant 2013
TO‐058: Spectrum of Lung Damage in Primary Ciliary Dyskinesia as seen on Computed Tomography
Katelyn Tadd1, Lucy Morgan2, Andre Schultz3, Tim Rosenow3, Connor Murray4, Phil Robinson1
1Respiratory Medicine, Royal Children's Hospital, Melbourne., 2Respiratory Medicine, Concord Hospital, Sydney, 3Respiratory Medicine, Princess Margaret Hospital, Perth., 4Medical imaging, Princess Margaret Hospital, Perth.
Introduction/Aim
Primary Ciliary Dyskinesia (PCD) and Cystic Fibrosis (CF) are both inherited, progressive, incurable, respiratory conditions causing significant morbidity and mortality. In the lungs, damage is reflected as a spectrum of structural changes that can be detected on computed tomography (CT). To monitor disease progression and guide therapy, scoring systems for CT scans have been developed in CF, which quantify the extent and severity of changes seen. Most research examining structural lung changes on CT scans use scoring systems derived from a CF cohort. All studies to date describing lung damage in PCD use these CF‐derived tools. This assumes lung damage in the two conditions is identical, which potentially results in a failure to identify PCD‐specific changes. Our study addresses this assumption
Methods
We retrospectively analysed of 58 CT scans from 40 adult and paediatric patients with PCD. The following abnormalities found in CF were scored according to presence and extent: bronchiectasis, bronchial wall thickening, atelectasis, mucous plugging, and air trapping. In addition, an experienced respiratory radiologist reviewed all scans to look for the presence of any abnormalities that differ from the above.
Results
Bronchial wall thickening was the most common abnormality, and air trapping the least common. All abnormalities were present significantly more often in the middle and lower lobes compared to the upper lobes, with all p values <0.001. When present, all abnormalities were significantly more extensive in the middle and lower lobes compared to the upper lobes. Bronchiectasis, mucus plugging, atelectasis (p<0.001) and air trapping (p=0.005) were all present significantly more often in the PCD cohort than the respective CF cohorts. The PCD‐unique changes identified were dextrocardia, extensive tree‐in‐bud patterns, whole lobe atelectasis, and interlobar and interlobular septal thickening.
Conclusion
Significant structural changes were seen on CT scans in patients with PCD, which were not consistent with those previously described in patients with CF. Our findings illustrate the need for development of a PCD‐specific scoring system, which can function as a tool for the objective assessment of disease status, progression and efficacy of therapy.
Grant Support
Nil
TO‐059: The ventilatory response to hypoxia remains blunted in preterm infants with bronchopulmonary dysplasia
Zoe A. Faulkner1,2, Benjamin Stöcklin2,3, Graham L. Hall1,4, Andrew C. Wilson4,5,6, J. Jane Pillow2,3, Shannon J. Simpson1
1Children's Lung Health, Telethon Kids Institute, WA, 2School of Anatomy, Physiology and Human Biology, University of Western Australia, 3King Edward Memorial Hospital for Women and Infants, WA, 4School of Physiotherapy and Exercise Science, Curtin University, WA, 5Princess Margaret Hospital for Children, 6School of Paediatrics and Child Health, University of Western Australia
Introduction/Aim
The early postnatal environment in which very preterm infants develop is relatively hyperoxic compared to in utero. Additionally, very preterm infants often require breathing support, including supplemental oxygen (O2); neonatal exposure to > 28 d O2 is an NICHD diagnostic criterion for bronchopulmonary dysplasia (BPD). Neonatal supplemental O2 may alter chemoreceptor “resetting”. Therefore, we aimed to quantify the hypoxic ventilatory response (HVR) in very preterm infants (<32 w gestation) during the neonatal period and determine if neonatal supplemental O2 has lasting effects on the HVR at 12–15 m corrected postnatal age (PNA).
Methods
The HVR was evaluated in very preterm infants at 36 w postmenstrual age (PMA) and 12–15 m corrected PNA. Breathing variables, including tidal volume (V T), respiratory rate (f), minute ventilation (V E) and inspiratory flow (VT/ t I) were measured under normoxic (21% O2) and hypoxic (14% O2) conditions. Hypoxia induced change in breathing variables was assessed using Wilcoxon Matched‐Pair Signed‐Rank test.
Results
Preterm infants (n=28; 17 with BPD) had no HVR at 36 w PMA (p>0.05). In contrast, the HVR was present at 12–15 m PNA (n=13; 3 with BPD), manifest during hypoxia as 1) increased V T (mean difference 2.0 mL/kg; 95% CI 1.2, 2.9 mL/kg; p<0.001); 2) increased V E (28.3; 12.7, 44.0 mL/min/kg; p=0.002) and 3) increased V T/t I (52.8; 41.2, 64.3 mL/s; p<0.001). Low birth weight z‐score (Spearman Rho= 0.622; p=0.031) and increased duration of supplemental O2 (−0.613; p=0.034) were associated with smaller increases in V T during hypoxia. Preterm infants with BPD had less change in V T (p=0.048) and V E (p=0.024) during hypoxia at 12–15 m PNA compared to preterm infants without BPD.
Conclusion
Infants born very preterm have absent ventilatory response to hypoxia in the neonatal period. Persistence of a blunted HVR beyond the first year of life in infants with BPD warrants further investigation.
Grant/Fellowship Support
NHMRC (APP 1047689, 1057614, 1077691, 1025550, 1073301), Swiss National Science Foundation.
TSANZ Ann Woolcock Young Investigator Awards
TO‐060: PRAGMA‐CF: a quantitative measure of structural lung disease in young children with cystic fibrosis.
Tim Rosenow1,2, Clara Mok1,2, Lidija Turkovic1, Conor Murray3, Harm Tiddens4, Graham Hall1, Sarath Ranganathan5,6, Peter Sly7, Stephen Stick1,8 on behalf of AREST CF.
1Telethon Kids Institute, The University of Western Australia, WA, 2School of Paediatrics and Child Health, The University of Western Australia, WA, 3Department of Diagnostic Imaging, Princess Margaret Hospital for Children, WA, 4Department of Pulmonology, Sophia Children's Hospital, Rotterdam, Netherlands, 5Infection and Immunity Theme, Murdoch Children's Research Institute, VIC, 6Department of Respiratory Medicine, Royal Children's Hospital Melbourne, VIC, 7Child Health Research Centre, The University of Queensland, QLD, 8Department of Respiratory and Sleep Medicine, Princess Margaret Hospital for Children, WA
Introduction/Aim
Chest computed tomography (CT) is the gold standard for detecting structural lung disease in cystic fibrosis (CF), however there has been a lack of outcome measures appropriate for young children. The aim of this study was to develop and validate a quantitative CT‐based measure of structural lung disease in children aged below 6 years. We hypothesised that this outcome is biologically relevant and suitable for use as a clinical trial outcome.
Methods
All patients undergoing annual surveillance CT and bronchoalveolar lavage (BAL) were included. To assess structural lung disease extent, the PRAGMA‐CF method was developed: a grid was overlaid on CT slices and annotated hierarchically for the presence of bronchiectasis, bronchial wall thickening, and mucous plugging (inspiratory scan) or trapped air (expiratory scan). Overall disease (%Dis) and trapped air (%TA) were expressed as the proportions of cells with disease and trapped air (respectively) compared to healthy.
Thirty scans were randomly selected for rescoring to assess repeatability (intraclass correlation coefficient, ICC). Linear mixed model analysis was used to compare CT outcomes to the presence of neutrophil elastase (NE) and infection from BAL.
Results
683 scans from 256 patients were included in the final analysis. ICCs to assess repeatability were above 0.8 (grade of excellent). CT outcomes were associated with both the presence and history of NE and infection. Sample size calculations showed that multicentre clinical trials of intervention can be performed with around 100 patients.
Discussion
PRAGMA‐CF is a sensitive tool to monitor structural lung disease in CF. It is highly repeatable, biologically plausible (associated with clinical markers of lung disease), and is suitable for use as an outcome measure in multicentre clinical trials. This study provides both a rationale and a means to test interventions aimed at preventing structural lung disease in young children with CF.
TO‐061: Identification of a plasma microRNA profile in pulmonary tuberculosis patients that is modulated by anti‐microbial therapy
Barry, Simone E1 ; Ellis, Magda1; Yang, YuRong2 ,3; Guan, Guangyu4; Wang, Xiaolin5; Britton, Warwick J1 ,6; and Saunders, Bernadette M1 ,7.
1Centenary Institute, The University of Sydney, Locked Bag No 6, Newtown, NSW 2042, Australia; 2Ningxia Medical University, Yinchuan, Ningxia, P.R. China; 3QIMR Berghofer Medical Research Institute, QLD, Australia, 4Ningxia Centre for Disease Control and Prevention, Yinchuan, Ningxia, P.R. of China, 5Infectious Disease Hospital of Ningxia, Yinchuan, P.R. of China, 7500004, 6Discipline of Medicine, Sydney Medical School, The University of Sydney, Sydney, NSW 2006 Australia; 7University of Technology Sydney, NSW, 2007 Australia.
Introduction/Aim
microRNA expression profiles are of interest as a biomarker of tuberculosis (TB). The effect of anti‐TB therapy on miRNA profiles in pulmonary TB patients is unknown and was examined in this study.
Methods
Plasma miRNA levels for 175 miRNAs were compared in 20 TB patients and matched healthy controls from China. 87 miRNAs were differentially regulated between the two groups. Ten of these were analysed in a test cohort of 100 pulmonary TB patients sampled prior to the commencement of antibiotic therapy and at one, two and six months during treatment.
Results
Six miRNA were differentially expressed in the test group of TB patients. miRs ‐29a and ‐99b were up‐regulated, whilst miRs −21, 26a, −146a and −652 were down‐regulated. A combination of 4 miRNA distinguished pulmonary TB from healthy controls with a sensitivity of 90% and a specificity of 84%, with an AUC of 0.941. Within one month of treatment, significant modulation of miRs ‐29a, −99b,‐26a and 146a was seen in successfully treated patients, although not all miRNAs had returned to baseline at completion of treatment.
Conclusion
Six miRNA were differentially expressed in the test group of TB patients. miRs ‐29a and ‐99b were up‐regulated, whilst miRs −21, 26a, −146a and −652 were down‐regulated. A combination of 4 miRNA distinguished pulmonary TB from healthy controls with a sensitivity of 90% and a specificity of 84%, with an AUC of 0.941. Within one month of treatment, significant modulation of miRs ‐29a, −99b,‐26a and 146a was seen in successfully treated patients, although not all miRNAs had returned to baseline at completion of treatment.
Funding
NHMRC CRE‐TB (APP1043225), RL Cooper Medical Research Foundation, Australian Respiratory Council, Perpetual Trust.
TO‐062: Zinc dyshomeostasis and autophagy as critical determinants for airway epithelial dysfunction in COPD
Eugene Roscioli1,2, Hai Bac‐Tran1, Hubertus Jersmann1,2, Greg Hodge1,2, Emily Hopkins1, Rhys Hamon1, Phan T Nguyen1, Paul N Reynolds1,2, Peter Zalewski1, Sandra Hodge1,2
1Lung Research Laboratory, Hanson Institute and Department of Thoracic Medicine, Royal Adelaide Hospital, South Australia, Australia, 2Department of Medicine, University of Adelaide, South Australia, Australia
Introduction/Aim
Airway inflammation and cigarette smoke in COPD induces autophagy in bronchial airway epithelial cells (bAEC). Zinc (Zn) deficiency is also a stimulus for autophagic dysfunction. We hypothesised Zn deficiency potentiates COPD, and with cigarette smoke exposure, causes autophagic insufficiency and epithelial fragility.
Our aims were to determine whether cigarette smoke‐exposure produces Zn dyshomeostasis and autophagic dysfunction, and if this impairs the epithelia barrier, and induces the production of a COPD‐related pro‐inflammatory phenotype.
Methods
Emphysematous mouse lung tissues were assessed via immunofluorescence for free‐Zn. Air‐liquid interface (ALI) cultures of human bAECs were exposed to Zn depletion, TNFα/IFNγ, and cigarette smoke extract (CSE10%). End points included western analysis for Zn transporters ZIP1 and ZIP2, autophagy/apoptosis regulators e.g. Light chain‐3‐II, Sequestosome, Bcl2 and X‐linked inhibitor of apoptosis (XIAP), and tight junction proteins Claudin‐1 and ZO‐1, transmission electron microscopy to visualise autophagy, barrier function assessment including permeability of fluorescein tracers, and ELISA for RANTES and Thymic stromal lymphopoietin (TSLP).
Results
Lung tissues from cigarette smoke‐exposed mice showed significantly reduced free‐Zn in the epithelium. Further, human bAECs stimulated with TNFα/IFNγ, in ZnDep/CSE10% showed an increase in ZIP1 (p=0.001) and decrease in ZIP2 (p=0.007), and increased autophagy with reduced capacity to degrade cellular debris. Autophagic dysfunction associated with the induction of apoptosis via the reduction of Bcl2 and XIAP proteins (both p<0.05). Reduced epithelial barrier function was evidence by decreases in Claudin‐1 and ZO‐1 protein, reduced electrical impedance (3.5‐fold, p<0.05), and increased permeability. A significant increase in RANTES and TSLP was observed for ZnDep, with/without CSE10%.
Conclusion
We demonstrate cigarette smoke depletes free‐Zn from the airway epithelium, and Zn deficiency is a significant potentiator of autophagic and apoptotic dysregulation, the production of potent AEC‐derived inflammatory mediators, and epithelial fragility. In combination with cigarette smoke exposure, Zn dyshomeostasis may be a major determinant for the pathogenesis of the COPD phenotype.
Grant Support
The Thoracic Society of Australia and New Zealand / AstraZeneca – Early Career Research Fellowship.
The National Health and Medical Research Council: Application 1099040.
The Royal Adelaide Hospital Research Fund.
TO‐063: Identifying a novel therapeutic strategy for asthma: targeting airway epithelial cell restitution
Iosifidis T 1 ,2, EE Gill3, AH Lee3, Buckley AG4 ,5, Sutanto EN4 ,6, Ling KM4 , Garratt LW1 ,4, Looi K1 ,4, Kicic‐Starcevich E4 ,6, Martinovich KM4 , Shaw NC4 , Montgomery ST1 , Lannigan FJ1 ,7, Rigby PJ5 , Hancock RE3 , Knight DA8 ,9,10, Stick SM1 ,2,4,6 and Kicic A1 ,2,4,6
1School of Paediatrics & Child Health, The University of Western Australia, Western Australia, Australia, 2Centre for Cell Therapy & Regenerative Medicine, Western Australia, Australia, 3Centre for Microbial Diseases and Immunity Research, University of British Columbia, Vancouver, Canada, 4Telethon Kids Institute, Western Australia, Australia, 5Centre for Microscopy, Characterisation & Analysis, Western Australia, Australia, 6Department of Respiratory Medicine, Princess Margaret Hospital for Children, Western Australia, Australia, 7School of Medicine, Notre Dame University, Western Australia, Australia, 8School of Biomedical Sciences & Pharmacy, University of Newcastle, New South Wales, Australia, 9Priority Research Centre for Asthma & Respiratory Disease, Hunter Medical Research Institute, New South Wales, Australia, 10Department of Anesthesiology, Pharmacology & Therapeutics, University of British Columbia, British Columbia, Canada
Introduction/Aims
Recent advances have implicated the airway epithelium as a key driver in asthma pathogenesis, partly due to its dysregulated response to damage. Novel therapies focusing on protecting and repairing vulnerable airways, particularly in early life, could transform asthma treatment by preventing disease development/progression. (1)To analyse primary airway epithelial cells (pAEC) migration patterns post‐wounding in‐vitro. (2)To identify mechanisms and potential therapeutic targets enhancing wound repair processes.
Methods
pAEC were obtained from non‐asthmatic and asthmatic paediatric airways. Scratch wounds were performed on pAEC monolayers to assess repair and imaged every 30 minutes (IncuCyte ZOOM®,Essen Bioscience). Migration trajectories of leading‐edge pAEC were analysed using ImageJ. Integrin gene and protein expression were investigated by qPCR and In‐Cell™ Western,respectively. Total RNA was sequenced(Illumina Hi‐Seq2500) and differential gene‐expression analysis was performed(DESeq2 and Ingenuity Systems(QIAGEN)).
Results
Response to wounding in asthmatic children was deficient and lacked specificity with significantly lower mean migration distance(non‐asthma and asthma; 256.9±7.1 and 152.3±8.6μm(mean±SEM)), velocity(0.42±0.02 and 0.22±0.01μm/min), directionality (91.3±0.1 and 61.1±0.1%) and forward migration index(95.3±0.1 and 64.6±0.1%). A major regulator of cell migration, i.e. integrin α5β1, was investigated in pAEC. Lower gene(α5, 5.9‐fold, p<0.0001; β1,1.5‐fold, p<0.05). and protein(α5, 2.8‐fold, p<0.05; β1, 3.1‐fold, p<0.05) levels in pAEC from asthmatic children(n≥11) compared to control(n≥23). RNA‐seq analysis identified 1,153 differentially expressed genes in asthmatic children(n=6) relative to control(n=4) with overrepresented gene ontologies related to integrins and extracellular matrix. Drug database screening identified several clinically safe drugs that are now being examined for drug repurposing potential to restore integrin expression and aid wound repair.
Conclusion
These novel experiments demonstrate abnormal migration behaviour of asthmatic airway epithelium post‐wounding. Some mechanisms controlling this disease phenomenon were identified like decreased integrin α5β1, and multiple transcriptional mechanisms were dysregulated in asthmatics, some of which are targetable by existing drugs. Supporting airway epithelial repair and barrier integrity may be a novel therapeutic avenue for asthma.
Grant Support
NHMRC (#1048910), APA (UWA), Centre for Cell Therapy & Regenerative Medicine PhD Top‐Up Scholarship, Asthma Foundation WA Fiona Staniforth PhD Top‐Up Scholarship
Prize Eligibility
Ann Woolcock New Investigator Award, Janet Elder International Travel Award, oral prize
Conflict of interest
None
TO‐064: Persistent IL‐33 in a preclinical chronic asthma model underpins rhinovirus‐induced exacerbation by dampening antiviral immunity
Rhiannon B. Werder1, Vivian Zhang1, Jason P. Lynch1, Kirsten Spann2,3, and Simon Phipps1,2
1School of Biomedical Sciences, University of Queensland, Queensland 4072, Australia, 2Australian Infectious Diseases Research Centre, The University of Queensland, Queensland, Australia, 3School of Biomedical Sciences, Queensland University of Technology, Queensland, Australia
Introduction/Aim
Rhinovirus infection triggers acute exacerbations of asthma. Expression of IL‐33, an instructive cytokine of type 2 inflammation, is upregulated during experimental rhinovirus infection of asthmatic subjects and correlates with the production of type‐2 cytokines and eosinophilic inflammation. Using a novel model of virus and allergen exposure, we sought to determine whether anti‐IL‐33 therapy attenuates a rhinovirus‐induced asthma exacerbation in mice.
Methods
To simulate the synergistic effects of virus infection and allergen exposure on asthma susceptibility, mice were exposed to low dose pneumonia virus of mouse (PVM; 1pfu) and low dose (1μg) cockroach antigen (CRE) in early life and again in later life. Four weeks after the final CRE exposure, mice were inoculated with rhinovirus (RV‐1B, TCID50 5x106). Anti‐IL‐33 or dexamethasone was administered intraperitoneally twice/week between the CRE and RV challenge, then daily until euthanasia.
Results
Both early‐life and later‐life exposures to PVM and CRE were necessary for disease onset and progression. IL‐33 levels were elevated immediately following the final CRE exposure and persisted in the airways until the time of RV‐1B challenge. Mice co‐exposed to PVM/CRE, but not CRE or PVM alone, presented with eosinophilic inflammation, increased numbers of type 2 innate lymphoid cells, mucous hypersecretion and elevated IL‐13 levels following RV infection. Treatment with anti‐IL‐33 or dexamethasone attenuated the RV‐1B‐induced type 2 inflammation but had no effect on mucous production. Critically, anti‐IL‐33, but not dexamethasone, promoted the expression of antiviral cytokines, accelerating RV‐1B viral clearance.
Conclusion
Both anti‐IL‐33 and dexamethasone suppress the magnitude of type 2 inflammation during an rhinovirus‐induced acute exacerbation, however anti‐IL‐33 has the added benefit of boosting antiviral immunity and lowering viral burden.
Grant Support
Pfizer Inc, and The Australian Infectious Disease Research Excellence Award, The University of Queensland.
TO‐065: Self‐perceived burden as a barrier to communication at the end of life in COPD
Phillipa Southwell1, Judith Crockett 2, Deborah Burton 1, Judith Gullifer 3
1School of Biomedical Sciences, Charles Sturt University, Orange NSW, 2School of Community Health, Charles Sturt University, Orange NSW, 3Faculty of Arts, Charles Sturt University, Bathurst NSW
Introduction/Aim
The end of life (EOL) trajectory in Chronic Obstructive Pulmonary Disease (COPD) is known to complicate prognostication, potentially preventing timely transition to palliative care, thus the primary responsibility for care provision remains with the family of the person with COPD. We aimed to explore the experiences of older people living with Stage IV COPD in a rural community, and how COPD influenced their relationships and identity.
Methods
Eleven older people with Stage IV COPD living in regional NSW undertook narrative interviews, discussing their ‘COPD journey’. The interviews were transcribed, then analysed and interpreted in accordance with a hermeneutic phenomenological methodology.
Results
Spousal care was generally well accepted and expected by married participants as an extension of the marital role. However, when adult children were involved in care or decision making, participants expressed guilt and frustration about perceived and actual burden placed on them. This self‐perceived burden, grounded in their own experiences caring for loved ones, had flow on effects to their uptake of coping and treatment strategies, and Advance Care Planning (ACP) as well as creating communication barriers between each of the parties. Parents aimed to protect their adult children from distress or impacting on their lives, by prioritising the children's wishes above their own, whilst simultaneously under‐communicating need and disease specific information. Paradoxically, many participants went on to design their ACP to refuse treatment rather than extend any impact on their children's lives, contrary to their children's ACP requests of them.
Conclusion
With the protection of adult children being a primary determinant of end of life decision making, it is critical to establish more formal and effective communication pathways between family and health professionals to facilitate a ‘good death’ within the family group.
Grant Support
Charles Sturt University Faculty of Science Fee Waiver for Higher Degree Research Students
Asthma and Allergy 3
TO‐066: Asthma and physical activity in childhood: Are they longitudinally related?
Cassim R1,2, Milanzi E1, Koplin J J1,2, Dharmage S C1,2, Russell M A1,2
1Allergy and Lung Health Unit, Centre for Epidemiology and Biostatistics, School of Population and Global Heath, University of Melbourne, Parkville, Victoria 3052, Australia, 2Gastro and Food Allergy Group, Murdoch Childrens Research Institute, Parkville, Victoria 3052, Australia
Aim
There is increasing interest in the role of physical activity (PA) in the development of asthma but the potential for asthma to influence PA has hindered the progress in understanding this given the lack of relevant longitudinal data in children. The primary aim of this study was to explore whether having asthma leads to lower PA levels, and/ or whether lower PA levels leads to more asthma in children and adolescents between the ages of 8 and 14 years.
Methods
This analysis was conducted in 4983 children who participated in the Longitudinal Study of Australian Children (LSAC) between the ages of 6 and 14. Data on asthma and PA were collected via questionnaires and Time Use Diaries biennially since the children were 4 years old. Bi‐directionality of this relationship was investigated using a cross‐lagged model for PA and asthma implemented using structural equations modelling. Incident‐current asthma was defined as doctor's diagnosis since previous wave and either use of asthma medications or current wheeze in the past 12 months. PA was time in minutes spent doing medium to vigorous physical activities in a day. Included confounders were gender, older siblings, socioeconomic z‐score and body mass index (BMI).
Results
Effect estimates for each regression suggested that there was no association between PA and asthma at any age and in either direction; the adjusted regression coefficients for the effect of asthma on subsequent PA were: 0.98 (0.90, 1.07), 0.93 (0.85, 1.01), 1.07 (0.97, 1.17) and 0.99 (0.88, 1.11). Similarly, the adjusted log of OR for the effect of PA on asthma was 0.99 (0.99, 1.00) at each age.
Conclusions
These results suggest that PA at any of the observed ages does not prospectively predict incident‐current asthma in this longitudinal analysis. Similarly, incident‐current asthma does not predict future PA in the observed ages.
Grant Support
N/A
Declaration of conflict of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Keywords
asthma, adolescents, children, physical activity
TO‐067: Blood eosinophils and serum IgE predict response to omalizumab in patients with severe allergic asthma: INNOVATE trial post‐hoc analysis
Volkan Manga, MD1 , Marc Humbert, MD, PhD2 , Ratko Djukanovic3, Steve Greenberg, MD4 , Theodore A. Omachi, MD, MBA5 , Benjamin Trzaskoma, MS5 , Roland Buhl6
1Novartis Pharma AG, Basel, Switzerland, 2Hospital Antoine Beclere, Unversite Paris‐Sud, Clamart, France, 3University of Southampton, Southampton, United Kingdom, 4Novartis Pharmaceutical Corporation, East Hanover, NJ, 5Genentech, Inc., South San Francisco, CA, United States, 6University Hospital Mainz, Mainz, Germany.
Introduction
Response to biologic therapy differs among severe allergic asthma (SAA) patients. Biomarker‐guided therapy may help to identify subgroups who demonstrate greater clinical benefits from omalizumab than the overall SAA population.
Methods
A post‐hoc analysis of INNOVATE trial data (Humbert et al. Allergy 2005) was performed to determine the impact of treatment on exacerbation rates and health‐related quality‐of‐life (AQLQ) of SAA patients stratified by peripheral blood eosinophils per mcl (EOS) and serum IgE (IU/ml). Negative binomial regressions were utilized within biomarker strata to estimate response to omalizumab vs placebo, controlling for potential confounders.
Results
An exacerbation reduction was observed among omalizumab‐treated patients vs placebo in EOS‐high strata: EOS≥300 (n=245) 38.98%, p=0.0399; EOS≥150 (n=316) 39.01%, p=0.0178. Exacerbation reduction increased further upon enriching these strata according to increased IgE (>75 IU/ml): EOS≥300/IgE>75 (n=184) 53.88%, p=0.0018; EOS≥150/IgE>75 (n=235) 53.75%, p=0.0005. Mean placebo‐subtracted benefits on AQLQ exceeded the minimal clinically‐important difference (≥0.5) and demonstrated statistically significant improvements in both EOS‐high strata: EOS≥300 (n=24) 0.55, p=0.0001; EOS≥150 (n=310) 0.53, p<0.0001. The benefit on AQLQ was most apparent in the EOS≥150/IgE>75 stratum (n=231): 0.59, p<0.0001.
Conclusion
This analysis is among the first to examine a combination of biomarkers to assess response to omalizumab in SAA patients. They suggest that subgroups with a combination of increased IgE and EOS may experience a greater clinical benefit. However, caution must be used in interpreting these results given their post‐hoc nature.
Grant Support
This analysis was supported by Novartis Pharma AG and Genentech.
TO‐068: Increased expression of IL‐27 in neutrophilic asthma
Kavita Pabreja1, Peter G. Gibson1,2, Katherine J. Baines1, Fiona Eyers1, Ming Yang1, Parameswaran Nair3, Paul S. Foster1, Jodie L Simpson1
1Priority Research Centre for Healthy Lungs, The University of Newcastle, NSW, Australia, 2 Department of Respiratory and Sleep Medicine, Hunter New England Area Health Service, Newcastle NSW Australia, 3 St Joseph's Healthcare & McMaster University, Ontario, Canada
Introduction/Aim
Asthma is a heterogeneous inflammatory disorder consisting of multiple endotypes, those with neutrophilic asthma (NA) have innate immune activation and tend to be resistant to corticosteroid therapy. We have shown that steroid‐resistant asthma can involve IL‐27, a monocyte/macrophage‐derived innate cytokine speculated to be involved in TH1 responses. The aim of this study was to examine the expression of IL‐27 in asthma inflammatory phenotypes and determine relationship between IL‐27 and other immune factors involved in asthma pathogenesis. We hypothesised that sputum gene expression of IL‐27 would be increased in participants with NA compared with other asthma phenotypes.
Methods
Induced sputum samples from 80 non‐smoking adults with stable asthma were assessed for total and differential cell counts along with gene expression for IL‐27R, IL‐27p28, IL‐27EBI3, IFN‐γ and TNF‐α. Inflammatory phenotype was determined using a single sputum samples we eosinophilic asthma (EA) when eosinophils≥2% and neutrophils <61%, neutrophilic asthma (NA) when neutrophils ≥61% eosinophils <2% and paucigranulocytic asthma (PA) when eosinophils <2% and neutrophils <61%.
Results
The participants had a mean age of 55 years, 37 (42%) were males and 63 (79%) were prescribed inhaled corticosteroids. FEV1 %predicted was lowest in NA (mean 63%) and significantly lower than those with PA (80%; p=0.009). Sputum gene expression of both IL‐27 subunits (p28 and EBI3), IFN‐γ and TNF‐α were significantly increased in NA compared with EA. Furthermore, the expression of IL‐27EBI3 in NA was significantly (p<0.05) higher than PA participants. IL‐27R mRNA level was significantly negatively correlated with degree of airflow obstruction (FEV1/FVC%) (r=0.244, p<0.05), while gene expression of the subunit, IL‐27EBI3 mRNA, was positively associated with sputum total cell count (r=0.315, p<0.05), neutrophil% (r=0.486, p<0.05) and age (r=0.223,p<0.05).
Conclusion
Elevated gene expression of IL‐27 suggests this may be an important cytokine in the pathogenesis of NA.
Grant Support
NHMRC, Canada Research Chair Program
TO‐069: Risk factors for vocal cord dysfunction in a difficult asthma population
Joy Lee1, Tunn Ren Tay1, Naghmeh Radhakrishna1, Fiona Hore‐Lacy1, Catherine Smith2, Eli Dabscheck1, Robyn O'Hehir1, Ryan Hoy1,2, Mark Hew1,2
1Allergy, Immunology & Respiratory Medicine (AIRMED), Alfred Hospital, Melbourne, VIC, Australia, 2Public Health & Preventive Medicine, Monash University, Melbourne, VIC, Australia
Introduction/Aim
Vocal cord dysfunction (VCD) is characterized by inappropriate adduction of the vocal cords giving rise to symptoms of dyspnea, voice change, wheezing and throat tightness. VCD can be misdiagnosed as asthma, resulting in delayed or inappropriate treatment. A high proportion of patients with difficult‐to‐treat asthma are reported to also have co‐existing VCD.
Methods
One hundred and seventeen consecutive difficult asthma patients referred by respiratory specialists underwent the Alfred assessment protocol. Vocal cord dysfunction was diagnosed either by; an ENT specialist; or clinically, based on characteristic symptoms, and supported by a positive Pittsburgh VCD index or VCD‐Questionnaire. Univariate analyses were performed to identify clinical factors associated with vocal cord dysfunction. Predictors were comared using unpaired t‐test or chi‐square test where appropriate. Predictors with a p‐value ≤ 0.25 were then included in a multivariate logistic regression model. Each predictor was assessed for confounding and significance. Continuous variables were expressed in mean (SD).
Results
Forty (34.2%) of 117 difficult asthma patients had VCD. The majority (n=33) of these also had asthma demonstrable by variable airflow obstruction. Patients with VCD were more likely to; be female (OR 2.45, 95%CI 1.03‐5.84, p=0.04); have poorer asthma control and quality of life (ACT 13±5 vs. 15±5, p=0.023; AQLQ 3.59±1.41 vs 4.61±1.38, p<0.001); have more frequent exacerbations [3(2–5) versus 2 (0–2) over six months, p=0.003], and; be less severely obstructed (FEV1/FVC ratio 68%±13 vs. 61%±16, p=0.028). On multivariate logistic regression, independent predictors for VCD were FEV1/FVC and AQLQ.
Conclusion
VCD was present in a third of our patients with difficult asthma. VCD was associated with female sex and poorer asthma outcomes despite better lung function. Improved lung function and poorer quality of life were both independent predictors of VCD. Our findings highlight the importance of identifying and addressing VCD in this challenging patient group.
Grant Support
Nil
TO‐070: Asthma gene signatures expression in bronchial biopsy
Stephany Sanchez1,Peter Wark1,2, Katherine Baines1, Jodie Simpson1
1Priority Research Centre for Healthy Lungs, Faculty of Health and Medicine, University of Newcastle, NSW 2308, 2 Respiratory and Sleep Medicine, John Hunter Hospital NSW 2305
Introduction/Aim
The expression of TH‐2 high (CLCA1, POSTN, and SERPINB2) genotype has been shown to predict response to inhaled steroids in mild asthma and a 6 genes signature (6GS) in sputum cells (CLC, CPA3, DNASEI1L3, IL1B, ALPL, and CXCR2) distinguishes between asthma inflammatory phenotypes. The aim was to determine gene expression of both signatures in endobronchial biopsies from adults with asthma and related to asthma severity and airway inflammatory phenotypes.
Methods
Non‐smoking adults with asthma had current respiratory symptoms, and evidence of variable airflow obstruction. Asthma severity was defined according to GINA. Inflammatory phenotypes using BAL cell count. The 9 genes were analyzed by qPCR using extracted RNA.
Results
Biopsies were evaluated from; severe asthma (n=40), mild/moderate asthma (n=32), with no differences in age, sex, atopy or smoking history between the groups.
Gene expression of SERPINB2 was significantly increased in severe compared with mild/moderate asthma (p=0.022) and inversely associated with FEV1% predicted in participants with asthma (r=−0.337,p=0.005).
Gene expression CLC and SERPINB2 were significantly increased in eosinophilic asthma (n=20) compared with paucigranulocytic asthma (n=21, p=0.003 and P=0.0009 respectively), while ALPL was increased in eosinophilic compared with mixed‐granulocytic asthma (n=13, p=0.0056). Only gene expression for CLC was associated with asthma BAL eosinophils % r=0.325 p=0.006. Gene expression for
IL‐1β was increased in neutrophilic (n=18) compared with paucigranulocytic asthma (p=0.006) and was significantly associated with BAL neutrophils % r=0.234, p=0.0496.
Conclusion
SERPINB2 expression in bronchial biopsy is associated with severe asthma, while CLC and IL‐1β gene expression are associated with BAL eosinophilia and neutrophilia respectively.
Grant Support
John Hunter Hospital Charitable Trust 2016.
TO‐071: Macrophages regulate the development of RSV induced asthma exacerbations
Thi Hiep Nguyen1, Steven Maltby2, Jodie L. Simpson3, Fiona Eyers4, Katherine J. Baines5, Peter G. Gibson6, Paul S. Foster7 & Ming Yang8
1Priority Research Centre for Asthma and Respiratory Diseases, Faculty of Health and Hunter Medical Research Institute, University of Newcastle, Callaghan, NSW 2300, Australia, 2Priority Research Centre for Asthma and Respiratory Diseases, Faculty of Health and Hunter Medical Research Institute, University of Newcastle, Callaghan, NSW 2300, Australia, 3Department of Respiratory and Sleep Medicine, Hunter New England Area Health Service, Newcastle, New South Wales, Australia., 4Priority Research Centre for Asthma and Respiratory Diseases, Faculty of Health and Hunter Medical Research Institute, University of Newcastle, Callaghan, NSW 2300, Australia, 5Department of Respiratory and Sleep Medicine, Hunter New England Area Health Service, Newcastle, New South Wales, Australia., 6Department of Respiratory and Sleep Medicine, Hunter New England Area Health Service, Newcastle, New South Wales, Australia., 7Priority Research Centre for Asthma and Respiratory Diseases, Faculty of Health and Hunter Medical Research Institute, University of Newcastle, Callaghan, NSW 2300, Australia, 8Priority Research Centre for Asthma and Respiratory Diseases, Faculty of Health and Hunter Medical Research Institute, University of Newcastle, Callaghan, NSW 2300, Australia
Introduction/Aim
Viral respiratory infections trigger severe exacerbations of asthma, worsen disease symptoms and impair lung function. To investigate the mechanisms underlying viral exacerbation, we established a mouse model of respiratory syncytial virus (RSV)‐induced exacerbation after allergen sensitisation and challenge.
Method
We investigated the effects of RSV infection on the induction of asthma exacerbation in a mouse model. Airway hyper‐responsiveness (AHR) was assessed by flexivent. In some experiments, pulmonary macrophages were depleted by 2‐Chloroadenosine; TNFα and MCP‐1 were neutralized by monoclonal antibodies.
Results
RSV infection of OVA‐sensitised/challenged BALB/c mice resulted in significantly increased AHR and macrophage and neutrophil lung infiltration. Exacerbation was accompanied by increased levels of inflammatory cytokines (including TNFα, MCP‐1, and KC) compared to uninfected OVA‐treated mice or OVA‐treated mice exposed to UV‐inactivated RSV. Dexamethasone treatment completely inhibited all features of allergic disease including AHR and eosinophil infiltration in uninfected OVA‐sensitised/challenged mice. Conversely, dexamethasone treatment following RSV‐induced exacerbation only partially suppressed AHR, and failed to dampen macrophage and neutrophil infiltration or inflammatory cytokine production (TNFα, MCP‐1, and KC). This mimics clinical observations in patients with exacerbations, which is associated with increased neutrophils and often poorly responds to corticosteroid therapy. Interestingly, we also observed increased TNFα levels in sputum samples from neutrophilic asthmatic patients. While RSV‐induced exacerbation was resistant to steroid treatment, inhibition of TNFα and MCP‐1 function or depletion of macrophages suppressed features of disease including AHR, macrophage and neutrophil infiltration.
Conclusion
Our findings highlight critical roles for macrophages and inflammatory cytokines (including TNFα and MCP‐1) in viral‐induced exacerbation of asthma and suggest examination of these pathways as novel therapeutic approaches for disease management.
Key Words
RSV, macrophage, steroid resistance, airway hyperresponsiveness, asthma exacerbation, mouse model
Nomination for New Investigator Award, N/A
Grant Support NHMRC project grants
Cystic Fibrosis
TO‐072: Investigating the non‐ion channel effects of CFTR modulators on innate immune viral responses
*Luke W Garratt1, *Kevin Looi1, Kelly M Martinovich1,2, Thomas Iosifidis1,2, Kak‐Ming Ling1,2, Nicole Shaw1,2, Samuel T Montgomery1,2, Elizabeth Kicic‐Starcevich1, Erika N Sutanto1, Anthony Kicic1,3, Stephen M Stick1,3, on behalf of AREST CF
1Telethon Kids Institute, University of Western Australia, 2 School of Paediatric and Child Health, University of Western Australia, 3 Princess Margaret Hospital for Children
*Joint first authors
Introduction & Aims
Airway epithelial cells (AEC) from CF lungs respond to viral infection with poor innate immune responses. The contribution of defective CF transmembrane conductance regulator (CFTR) channel function is not known. We investigated whether CFTR correcting drugs could improve responses by CF AEC to human rhinovirus (HRV).
Methods
Primary AEC obtained from 11 children with CF (five Class II, six Class III mutations) and six healthy controls by bronchial brushing, were expanded in vitro. Monolayers were stimulated with purified HRV1b at multiplicity of infection 12.5 for 24 hours, with or without 72 hours treatment by CFTR therapies lumacaftor and/or ivacaftor. RNA was collected and sequenced on the Illumina HiSeq 2500 platform. Supernatant was assessed by ELISA for interferons (IFN) and inflammatory cytokines.
Results
Data were interpreted as ratio of treatment response to unstimulated AEC. In healthy AEC, HRV1b stimulation resulted in increased IL‐8 and RANTES, but not IL‐6, IFNβ, IFNλ1 or IFNλ2. Responses to HRV1b by healthy AEC did not significantly change in the presence of CFTR modulators. In contrast, AEC of both CF genotypes generated an IL‐8 and an IL‐6 response to HRV1b (p<0.05) Interestingly, IL‐6 response by CF AEC was no longer significant following CFTR modulator treatment. Combined CFTR therapy for Class II CF was also found to reduce RANTES production (p<0.05). The IFN response to HRV1b was mixed, with minimal levels detected following stimulation except for IFNλ1, which was elevated in CF AEC supernatant (p<0.05). This was no longer significant after CFTR modulator therapy for both Class II and II (p<0.05).
Conclusion
CFTR therapies had a counter‐intuitive effect on responses by CF AEC to HRV1b. We are currently analysing RNAseq data to compare innate immune gene networks between treatments and phenotypes.
Grant Support
Glenn Brown Memorial Grant (2015), US Cystic Fibrosis Foundation.
TO‐073: Molecular and proteomic approach to investigate abnormal iron homeostasis in the cystic fibrosis airway
Pramila Maniam1, Xiahui Tan1, Ama‐Tawiah Essilfie1, Greg Anderson1, David Frazer1, Justin Mulvenna1, Jeremy Potriquet1, David W Reid 1,2,3
1QIMR‐Berghofer Institute of Medical Research, Herston, Brisbane, Queensland, 2 The Prince Charles Hospital, Chermside, Brisbane, Queensland, 3 University of Queensland, Brisbane, Queensland
Introduction/Aim
Iron homeostasis appears to be abnormal in the lungs of individuals with the genetic disease cystic fibrosis (CF). Disruption of iron homeostasis in the lung may promote bacterial infection and generate oxidative stress. We therefore tested the hypothesis that iron homeostasis in airway epithelial cells (AEC) from CF patients is abnormal and that this results in oxidative stress.
Methods
Cultured AEC from a CF patient with the F508del/W1282X mutations (immortalized IB3‐1 cell line) were exposed to ferric ammonium citrate (FAC; 50 & 200 μg/mL) and the response of iron regulatory pathways assessed by reverse transcription polymerase chain reaction (RT‐PCR) and proteomics. Interleukin (IL)‐6 levels were also assessed by enzyme‐linked immune‐assay in the AEC culture supernatant to determine whether iron exposure resulted in a pro‐inflammatory response. Control AEC (immortalized C38 cell line) underwent identical challenges and procedures for comparison.
Results
IB3‐1 CF AEC demonstrated a significant increase in the expression of transferrin receptor (TFR)‐1 (iron uptake) at baseline (pre‐iron challenge) compared to C38 AEC. The IB3‐1 AEC also demonstrated a significant increase in the expression of the iron exporter ferroportin (FPN) by at baseline compared to C38 AEC. Following FAC challenge, the expression of TFR‐1 by RT‐PCR was significantly reduced in both the IB3‐1 and C38 AEC, but expression of FPN remained essentially unchanged. Interleukin‐6 levels were significantly increased in the IB‐3 CFTR mutant compared to C38 AEC supernatants at baseline and both AEC lines demonstrated a significant increase in IL‐6 production following FAC challenge. Preliminary pathway analyses from the proteomic data reveal significant differential expression of proteins involved in oxidative stress and mitochondrial stress responses in the IB3‐1 compared to C38 AEC.
Discussion
The airway epithelium in CF demonstrates abnormalities of iron regulation, exhibits a pro‐inflammatory phenotype and activation of cell pathways involve in oxidative stress.
Key Words
Iron, cystic fibrosis, airway epithelial cells
Nomination for
New Investigator Award
Grant Support
NHMRC and TPCH Foundation.
TO‐074: Structural determinants of long term functional outcomes in children with cystic fibrosis
Lidija Turkovic1, Daan Caudri1, Tim Rosenow1, Sarath Ranganathan2,3, Graham L Hall1 and Stephen Stick1,4 on behalf of AREST CF
1Telethon Kids Institute, University of Western Australia, Roberts Road, Subiaco WA, 2 Murdoch Children's Research Institute, Australia, 3 Royal Children's Hospital Melbourne, Australia, 4 Department of Respiratory Medicine, Princess Margaret Hospital for Children, Roberts Road, Subiaco WA
Introduction/Aim
Chest computed tomography (CT) is a potential surrogate endpoint for children with cystic fibrosis (CF). The relationship between structural abnormalities at an early age and long term functional outcomes has not been previously described. We aimed to determine whether CT scores in children under 6 years are predictive of later lung function.
Methods
Volumetric and limited slice CT scans were obtained annually from children enrolled in AREST CF program aged 0 to 6 years. Follow up spirometry measurements were available for some of the AREST CF cohort from ages 5 to 15. Cox regression and mixed effects models were used to determine at what age and to what extent are CF‐CT scores predictive of future lung function decline. Results are presented adjusted for intrinsic disease severity (Homozygous D508 mutation, meconium ileus presence and gender), time elapsed between CT scan and spirometry and test centre.
Results
681 spirometry measurements were available (mean age 9.3±2.1) years). Total CF‐CT score at 5–6 years (n=171) that was greater than the median was significantly associated with shortened time before FEV1 falls below −1.645 Z scores (hazard ratio 3.16 (1.25, 7.99) p=0.015). The extent of mucus plugging and trapped air at ages 5–6 years were strongly associated with lower FEV1 Z scores between ages of 5–15 (−0.17 (−0.26, −0.07) p<0.001 and −0.09 (−0.14, −0.04) p=0.001 respectively). Predictive power of CT scores in young children is consistently stronger the more time elapses between initial CT scan and spirometry (mucus plugging score at 5–6 explains only 3% of variation in FEV1 Z score at the same age but 37% of variation 5 years later).
Conclusion
Non‐bronchiectatic lung abnormalities in young children with CF are important markers of future disease progression. Structural abnormalities are predictive of future FEV1 trajectories and represent promising endpoints in early intervention trials.
Grant Support
NHMRC and USA CF Foundation
TO‐075: Face masks and cough etiquette reduce cough generated bioaerosols containing pseudomonas aeruginosa in patients with cystic fibrosis
1,2,3, Stockwell, RE1,2, Johnson, G4, Ramsay K2, Sherrard LJ1, Jabbour N4, Knibbs LD2, Kidd TJ2,5, Wainwright CE2,6, Morawska L4, Bell SC1,2,3
1QIMR Berghofer Medical Research Institute, Queensland, Australia, 2The University of Queensland, Queensland, Australia, 3The Prince Charles Hospital, Queensland, Australia, 4Queensland University of Queensland, Queensland, Australia, 5Queen's University Belfast, United Kingdom, 6Lady Cilento Children's Hospital, Queensland, Australia
Introduction/Aim
The CF Foundation (USA) recently updated their infection control guidelines to include the recommendation that patients with cystic fibrosis (CF) wear surgical face masks in communal areas of health facilities to reduce transmission of aerosolised pathogens. The aim of this study was to investigate the effectiveness of face masks and cough etiquette techniques for reducing viable bioaerosols in patients with CF and chronic
P. aeruginosa infection.
Methods
Subjects were enrolled from the Adult CF Centre, The Prince Charles Hospital, Brisbane and positioned in a validated, aerosol‐sampling device and performed activities for 5 minutes each: 1.talking; 2.talking with surgical mask; 3.unmasked coughing; 4.coughing with surgical mask; 5.coughing with N95 mask; 6.coughing with hand covering mouth. A 6‐stage Andersen Cascade Impactor, positioned at 2 metres, collected and sized viable aerosols. Quantitative sputum and aerosol cultures was performed. Subjects rated their comfort levels with the masks
Results
25 (15 male) adults, mean (SD) age of 31.2 (7.7) years and FEV1 of 50.7 (17.4) % predicted were enrolled. 76% subjects produced viable P. aeruginosa during unmasked coughing. Cough etiquette, surgical mask and the N95 reduced infectious cough aerosols of 53.4, 93.8, 94.5% respectively, with the surgical mask rated more comfortable.
Conclusion
Face masks are effective in reducing cough generated infectious droplet nuclei in people with CF, with the surgical mask providing enhanced patient comfort. Cough etiquette provides less protection than masks.
Grant Support
CFF Therapeutics (USA), The Prince Charles Hospital Foundation (Australia)
TO‐076: Differences in the lower airway microbiota of infants with and without cystic fibrosis
KB Frayman1, DS Armstrong2, R Carzino3, TW Ferkol4, K Grimwood5 GA Storch6, SM Teo7, KM Wylie8, SC Ranganathan9
1Department of Respiratory Medicine, Royal Children's Hospital, Victoria, Australia; Respiratory Diseases Group, Murdoch Children's Research Institute, Victoria, Australia; Department of Paediatrics, University of Melbourne, Victoria, Australia., 2 Department of Respiratory Medicine, Monash Children's Hospital, Victoria, Australia; Department of Paediatrics, Monash University, Victoria, Australia., 3 Department of Respiratory Medicine, Royal Children's Hospital, Victoria, Australia; Respiratory Diseases Group, Murdoch Children's Research Institute, Victoria, Australia., 4 Department of Pediatrics, Washington University, St Louis, MO, United States; Department of Cell Biology and Physiology, Washington University, St Louis, MO, United States., 5 Menzies Health Institute Queensland, Griffith University, Queensland, Australia; Gold Coast Health, Queensland, Australia., 6 Department of Pediatrics, Washington University, St Louis, MO, United States., 7 Centre for Systems Genomics, University of Melbourne, Victoria, Australia., 8 Department of Pediatrics, Washington University, St Louis, MO, United States; McDonnell Genome Institute, Washington University, St Louis, MO, United States., 9 Department of Respiratory Medicine, Royal Children's Hospital, Victoria, Australia; Respiratory Diseases Group, Murdoch Children's Research Institute, Victoria, Australia; Department of Paediatrics, University of Melbourne, Victoria, Australia.
Introduction/Aim
Infection plays a critical role in the pathogenesis of early cystic fibrosis (CF) lung disease. Differences in the nasopharyngeal microbiota of subjects with CF and healthy controls are apparent from early infancy. This study aimed to compare the composition and structure of the lower airway microbiota of infants below 12 months of age with and without CF.
Methods
Bronchoscopies and bronchoalveolar lavage (BAL) procedures were performed in infants newly diagnosed with CF following newborn screening. Infants undergoing clinically‐indicated bronchoscopy were recruited as controls. Quantitative microbiological culture and inflammatory marker (interleukin‐8 and neutrophil elastase) measurements were undertaken contemporaneously. 16S ribosomal RNA gene sequencing was conducted on stored samples.
Results
Seventeen infants with CF (median age 2.6 months (interquartile range (IQR) 1.6‐4.9 months); male 59%; P.Phe508del homozygous 71%) and nine control infants (median age 5.0 months (IQR 2.9‐8.2 months); male 78%) contributed BAL samples. Diversity was reduced in CF compared with control BAL samples (median shannon diversity index 1.3 (IQR 0.9‐2.0) and 2.0 (IQR 1.4‐2.3) respectively). Firmicutes was the most prevalent phylum in both groups, accouting for 76.9% and 49% of total reads respectively, however Staphylococcus was predominant in CF samples only (39.8% total reads). The next most prevalent genera in the CF samples were Streptococcus (15.0%), Haemophilus (9.9%), Granulicatella (9.2%) and Gemella (6.7%). In contrast, the five most abundant genera in the control samples were Streptococcus (30.0%), Fusobacterium (12.8%), Neisseria (12.4%), Gemella (6.3%) and Veillonella (6.1%). Staphylococcus and Haemophilus each accounted for 0.4% of total reads.
Conclusion
There are substantial perturbations in the structure and composition of the lower airway microbiota of infants with CF in the first months of life, most notably increased prevalence of Staphylococcus and reduced diversity. Larger longitudinal studies are required to determine the clinical significance of these findings.
Grant Support
KBF is supported by the TSANZ/Vertex CF Paediatric Clinical Fellowship, the Australian Cystic Fibrosis Research Trust Postgraduate Studentship and the Royal Children's Hospital Cystic Fibrosis Research Trust. 16S rRNA gene sequencing was funded by grants from the Murdoch Children's Research Institute “65km for CF” and the RCH CF Research Trust. TWF, SCR, GAS and KMW were supported by the National Institutes of Health (NIH) grant, HL116211 and National Health and Medical Research Council award, NHMRC1043768. These bodies had no role in the study design, data analysis, interpretation or reporting of results.
Declaration of interests
There are no conflicts of interest.
TO‐077: The relationship between exercise capacity and hospitalisation in adult cystic fibrosis
Barry, R.1,2, Chambers, R.1,2, Smith, D.1,3, Walsh, J.2,4, Roll, M.2, Hall, K.1,2, Cobb, R.1,2, & Morris, N.4,5
1Adult Cystic Fibrosis Centre, The Prince Charles Hospital, Queensland, Australia, 2 Physiotherapy Department, The Prince Charles Hospital, Queensland, Australia, 3 School of Medicine, University of Queensland, Queensland, Australia, 4 The Menzies Health Institute, Griffith University, Queensland, Australia, 5 The Allied Health Research Collaborative, The Prince Charles Hospital, Queensland, Australia
Introduction/Aim
The six minute walk test (6MWT) is an objective tool used to assess functional exercise capacity in cystic fibrosis (CF). However, the relationship between 6MWT outcomes and need for hospitalisation for treatment of pulmonary exacerbation (PE) has not been studied. Therefore, the primary aim was to determine the relationship between six minute walk distance (6MWD), subjective breathlessness (Modified Borg score) and oxygen saturation (SpO2) during the 6MWT, and frequency and duration of hospitalisation in adults with CF.
Methods
Retrospective cohort study of all adult CF patients treated at The Prince Charles Hospital, Brisbane, who completed a 6MWT in 2014 or 2015. 6MWD, maximum Modified Borg score and nadir SpO2 during the 6MWT were correlated with the number of hospital admissions and total hospital days of treatment for PE's during the same calendar year.
Results
A 6MWT was performed in 94 subjects [mean age 29.8±9.3yrs, FEV1 56±22% predicted, 6MWD 590±114m, median (IQR) hospital admissions 2 (1–4), median (IQR) hospital days 18.5days (8.3‐57.5days)]. Reduced 6MWD significantly correlated with number of yearly hospital admissions and total yearly hospital days for treatment of PE's. However, strongest correlations were seen between maximum Modified Borg score, nadir SpO2 and total hospital days (Table 1).
| 6MWD | Maximum Modified Borg score | Nadir SpO2 | ||||
|---|---|---|---|---|---|---|
| Correlation | P‐value | Correlation | P‐value | Correlation | P‐value | |
| Yearly hospital admissions | −0.254 | <0.02 | 0.546 | <0.001 | −0.388 | <0.001 |
| Total yearly hospital days | −0.253 | <0.02 | 0.591 | <0.001 | −0.470 | <0.001 |
Conclusion
Maximum perceived breathlessness and oxygen desaturation more strongly correlated with hospital utilisation than distance walked, suggesting that subjective exertional dyspnoea and exercise‐induced hypoxaemia may be important predictors of exacerbation frequency.
Grant Support
Nil
Occupational & Environmental Lung Disease / Population Health 1
TO‐078: Occupational lung diseases remain underreported and undercompensated in Australia
Theodora Ahilas1
1Maurice Blackburn Lawyers,201 Elizabeth St, Sydney, NSW 2000, Australia
Introduction/Aim
Whilst much of the focus on the legal claims in this arena has been on asbestos, the re‐emergence of coal workers pneumoconiosis in Queensland over the past 18 months has justifiably showcased lung diseases caused by toxic exposures at work.
The Senate Select Committee on Health stated in The Fifth Interim Report (April 2016) “…a litany of regulator failure and regulatory capture, industry indifference and incompetence, inconsistent risk mitigation and patchy and sometimes compromised health monitoring in Australia” was responsible for the return of a disease that was considered eradicated over 30 years ago.
Theodora Ahilas will present on the rights to compensation for workers with occupational lung diseases.
Theodora will discuss legal entitlements that flow from the diagnosis of an occupational lung disease. The different legal and statutory entitlements that follow in the different States together with the complexity of assessing these claims particularly in the presence of co‐morbidities.
TO‐079: Lifetime occupational exposures in a population‐based sample of older Australian adults.
Rawson SL1 , Benke G1 , Corte TJ2 , Dharmage S3 , Hopkins P4 , Hoy R1 , Walters EH5 , Wolfe R1 , Abramson MJ1
1School of Public Health & Preventive Medicine, Monash University, Melbourne, 2 Royal Prince Alfred Hospital, Sydney, 3 Melbourne School of Population and Global Health, University of Melbourne, Melbourne, 4 School of Medicine, University of Queensland, Brisbane, 5 Menzies Research Institute, University of Tasmania, Hobart
Introduction/Aim
Little is known about how many Australians have been exposed to potentially hazardous agents in workplaces during their lifetime. Assessment of exposure status using only current job data can miss earlier exposures with potential long‐term effects, and does not account for changes to occupational exposures over time.
This analysis determines proportions of a national population‐based sample of Australian adults ever‐exposed to potentially hazardous agents during their working life.
Methods
Individuals were recruited by telephone to participate in a study as controls to a national sample of Idiopathic Pulmonary Fibrosis (IPF) cases in Australia; individually matched 2:1 for age, sex and State. Consenting participants completed a telephone interview collecting data including demographics, self‐reported environmental exposures and detailed occupational history. Each reported job was coded to the Finnish Job Exposure Matrix (FinJEM) to assign associated exposures during the relevant time period. Participants were considered exposed to an agent in a job if the probability of exposure was >25%. Data from each job in participants’ occupational history were collated to assess lifetime exposure status. Descriptive statistics were conducted to assess the proportions ever‐exposed.
Results
902 participants completed the interview (625 males and 277 females, mean±SD age 70.8±8.4), reporting a total of 2670 jobs. The FinJEM analysis of ever‐exposure produced the following Results
Respirable dust 36.5%; Animal dust 13.6%; Iron 13.0%; Plant dust 13.0%; Asbestos 12.5%; Environmental tobacco smoke 11.0%; Moulds 10.3%; Quartz dust (Silica) 9.9%. Analysis of self‐reported occupational exposure data yielded higher proportions: Dusty environment 50.6%; Gases/fumes/chemicals 47.0%; Asbestos 33.7%; Silica 19.5%. As expected, significantly more males were exposed than females for all agents (p<0.05).
Conclusion
A considerable number of older Australians have been exposed to potentially harmful agents within their working life. Data about these lifetime occupational exposures are required to examine potential occupational risk factors for diseases such as IPF.
Grant Support
National Health and Medical Research Council (Project Grant #1106601)
Declaration of interest statement
MJA holds investigator initiated grants for unrelated research from Pfizer and Boehringer‐Ingelheim. The other authors declare that they have no competing interests.
TO‐080: Dust exposure impacts non‐typeable Haemophilus influenzae infection of human airway epithelial cells
HD Clifford1, TH Teo1,2, L Kirkham1,2, R Thornton1,2, GR Zosky1,3, J Pickering1,2
1Telethon Kids Institute, University of Western Australia, Western Australia, 2 School of Paediatrics and Child Health, University of Western Australia, Western Australia, 3 School of Medicine, University of Tasmania, Hobart, Tasmania
Introduction
The development and progression of chronic lung diseases such as bronchiectasis involve recurrent episodes of severe bacterial respiratory infections. Inhaled environmental dust exposure can exacerbate immune responses to respiratory infections in mice. Whether dust exposure leads to more common and severe bacterial infections in the human airway is not yet known.
Aim
We aimed to determine the impact of community‐sampled geogenic dust PM10 (particulate matter <10μm diameter) on immortalized human airway epithelial cells (NuLi‐1). In particular, we aimed to determine its effects on non‐typeable Haemophilus influenzae (NTHi) infection.
Methods
Geogenic dust was collected from remote towns in Western Australia and PM10 was extracted. NuLi‐1 cells were exposed to PM10 (10μg/mL in PBS) in vitro for 24h before the addition of live NTHi‐86 (MOI 10:1) for 3h. Trypan blue staining was used to determine cell viability, and bacterial infection (attachment and invasion) was determined using a gentamicin survival assay. Epithelial release of IL‐6 and IL‐8 was assessed using a bead based immunoassay.
Results
Pre‐treatment of NuLi‐1 cells with dust PM10 significantly increased the ability of NTHi to attach to and invade cells (p<0.001 and p=0.013, respectively). After dust exposure, the IL‐6 response was increased (p=0.043) and the IL‐8 response was suppressed (p=0.041).
Conclusion
Geogenic dust preparations increased NTHi infection of human airway cells and may contribute to more common and severe respiratory infections. This has important implications for lung health in individuals living in arid environments, such as those in remote Australia, who are exposed to high loads of geogenic dust.
Grant Support
BrightSpark Foundation, Raine Medical Research Foundation
Conflict of Interest
None
TO‐081: Self‐reported geogenic dust exposure is associated with increased severity of infectious diseases in Aboriginal children
Graeme Zosky1, Francis Mitrou2, Shannon Melody3, Ellen Bennett1, Fay Johnston3Zachary Alach4, Matthew Lester4, Peter Franklin4, David Reid5, Carrington Shepherd2
1School of Medicine, University of Tasmania, Hobart, Tasmania, 2 Telethon Kids Institute, Subiaco, Western Australia, 3 Menzies Institute for Medical Research, University of Tasmania, Hobart, Tasmania, 4 Department of Health, Western Australia, 5 QIMR Berghofer Medical Research Institute, Herston, Queensland
Introduction/Aim
Australian Aboriginal children have a much higher incidence of infectious diseases than their non‐Aboriginal counterparts. Many Aboriginal communities are exposed to high levels of ambient dust from a geogenic (earth‐derived) origin. We have previously reported an association between self‐reported dust exposure and poor health in remote Aboriginal communities. The aim of this study was to examine the association between self‐reported dust exposure and infectious diseases in Aboriginal children.
Methods
We collected data on self‐reported dust levels and dust suppression programs from communities surveyed during the 2004 Environmental Health Needs Survey (EHNS) of remote Aboriginal communities in Western Australia. Health data on infectious diseases from hospitalisation records (2000–2002) and the Western Australia Aboriginal Child Health Survey (WAACHS) were linked to the EHNS. Odds ratios for the association between the health outcomes and exposure were calculated using multivariate logistic regression models within a multi‐level framework to take into account the hierarchical structure of the data.
Results
Dust exposure levels were not associated with the prevalence of infectious diseases in the children (p > 0.09 for all comparisons). Lack of a dust suppression program was associated with an increased risk of having chronic ear infections (OR 1.70 95%CI [1.03‐2.83], p = 0.04). Higher levels of dust exposure were associated with an increased risk of being hospitalised for upper (OR 1.79 95%CI [1.06‐.02]) and lower (OR 2.52 95%CI [1.08‐5.89]) respiratory tract infections. Lack of a dust suppression program was associated with an increased risk of being hospitalised for skin infections (OR 1.85 95%CI [1.24‐2.76]) and gastrointestinal disease (OR 1.74 95%CI [1.02‐2.96]).
Conclusion
While acknowledging that dust exposure in this instance was self‐reported, our data suggest that exposure to high levels of geogenic dust may be contributing to the increased prevalence and severity of infectious disease in Aboriginal children.
Grant Support
Nil
TO‐082: Resurgence of Coal Worker's Pneumoconiosis in QLD: Preliminary results from a Clinical, Occupational and Radiological Review
Dr Newbigin K1 , Dr Edwards B, Dr Dickinson S, Dr Bradley B, Dr Murrlink O.
1 Wesley Medical Imaging, Brisbane, QLD, Australia
Aim
To identify the radiological pattern and severity of Queensland cases of coal worker's pneumoconiosis and to correlate with clinical symptoms and occupational history.
Method
Retrospective review of CT and plain radiograph findings in twenty coal miner's with radiological and clinical diagnosis of coal worker's pneumoconiosis. Radiological grade of disease based on the ILO classification has been correlated with clinical symptoms, length of occupational exposure and job roles. Statistical analysis performed with Fisher exact test for categorical data and Wilcoxon test for continuous data.
Results
Preliminary results highlight the difficulties in diagnosis of coal worker's pneumoconiosis. Although data collection is ongoing, the radiological grade in the majority of cases to date has been low grade (ILO 1). In addition, this case series highlights that in the early stages coal workers presents with soft or ground glass nodules that are low density and therefore extremely difficult to detect on plain radiograph. There has been no case of progressive massive fibrosis from coal exposure alone. Clinical and occupational history is predictive of diagnosis with most patients having a symptomatic cough and a strong occupational history of dust exposure.
Conclusion
The resurgence of coal worker's pneumoconiosis in Queensland has been in workers with occupational histories of heavy dust exposure who are usually symptomatic. Radiographic changes are often subtle, particularly on plain radiograph.
Grant Support
Nil
TO‐083: Effect of in utero exposure to ceiling particles on post‐natal lung function
Ling Chen1, Ellen Bennett1, Amanda Wheeler2, Fay Johnston2, Graeme Zosky1
1School of Medicine, Faculty of Health, University of Tasmania, Hobart, Tasmania, Australia, 2 Menzies Institute of Medical Research, University of Tasmania, Hobart, Tasmania, Australia
Introduction/Aims
Assessing the community health impacts of short‐term particle exposure events (e.g. fires) can be difficult. One approach involves collecting particle samples from the roof‐space of exposed dwellings as a proxy for particles that were generated during the exposure event. In follow up studies from a 2014 fire, we collected particles from ceilings of houses at different distances from the particle source. Using a mouse model, we aimed to determine whether in utero exposure to these particles alters post‐natal lung function.
Methods
C57BL/6 mouse dams were intranasally exposed to ceiling particles (100μg in 50μL saline), carbon black particles (control) or saline alone at gestation day (E)13.5, E15.5 and E17.5. At two weeks of age, lung volume (TGV) and lung mechanics (airway resistance; Raw; tissue damping, G; tissue elastance, H) were measured in anaesthetised and tracheostomised mice using plethysmography and the forced oscillation technique (FOT) respectively.
Results
There was no effect of in utero exposure to ceiling dust or carbon particles on TGV in 2‐week‐old mice (female, P = 0.59; male, P = 0.73). Similarly, there was no effect of exposure to particles on Raw (female, P = 0.18; male, P = 0.88) or G (female, P = 0.46; male, P = 0.10). However, while there was no effect in females (P = 0.35), male mice exposed to ceiling dust (P = 0.04), but not carbon (P = 0.22) had higher H. The magnitude of the response was not associated with distance from the particle source.
Conclusion
In utero exposure to particles of ceiling dust increased lung stiffness, but only in male mice. These data suggest that exposure to ceiling dust may impact on lung growth in a sex specific manner. These responses appeared to be unrelated to the relative contamination of the ceiling dust with particles from a combustion source.
Grant Support
UTas Research Enhancement Grant Scheme; CAR CRE
Competing interests
The authors declare that they have no competing interests.
Respiratory Infectious Diseases 1
TO‐084: The Australasian Bronchiectasis Registry – early steps in mapping the impact of bronchiectasis in Australia and New Zealand
Simone Visser1, Heather Allan2, Lucy Burr3, Anne Chang4, Chien‐Li Holmes‐Liew5, Cameron Hunter6, Dan Jackson7, Paul King8, Graeme Maguire9, Peter Middleton10, Daniel Smith11, Rachel Thomson12, Grant Waterer13, Conroy Wong14, Lucy Morgan15
1Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, Sydney, NSW; Australia. Faculty of Medicine, The University of Sydney, Sydney, NSW; Australia, 2 Lung Foundation Australia, Brisbane, QLD; Australia, 3 Department of Respiratory and Sleep Medicine, Mater Health Services, Brisbane, QLD; Australia. Faculty of Medicine, The University of Queensland, Brisbane, QLD; Australia, 4 Department of Respiratory and Sleep Medicine, Lady Cilento Children's Hospital, Brisbane, QLD; Australia. Menzies School of Health Research, Darwin, NT; Australia, 5 Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, SA; Australia. School of Medicine, The University of Adelaide, Adelaide, SA; Australia, 6 Department of Respiratory Medicine, Wyong Hospital, Wyong, NSW; Australia, 7 Lung Foundation Australia, Sydney, NSW; Australia, 8 Department of Respiratory and Sleep Medicine, Monash Health, Melbourne, VIC; Australia. Faculty of Medicine, Nursing and Health Sciences, Monash University, Melbourne, VIC; Australia, 9 Baker IDI Heart and Diabetes Institute, Melbourne, VIC; Australia. Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, VIC; Australia, 10 Department of Respiratory and Sleep Medicine, Westmead Hospital, Sydney, NSW; Australia. Ludwig Engel Centre for Respiratory Research, Westmead Millennium Institute, Sydney, NSW; Australia. Sydney Medical School, The University of Sydney, Sydney, NSW; Australia, 11 Department of Thoracic Medicine, The Prince Charles Hospital, Brisbane, QLD; Australia. Faculty of Medicine, The University of Queensland, Brisbane, QLD; Australia, 12 Pulmedica, Greenslopes Private Hospital, Brisbane, QLD; Australia. Department of Thoracic Medicine, The Prince Charles Hospital, Brisbane, QLD; Australia. Metro South Clinical TB service, Princess Alexandra Hospital, Brisbane, QLD; Australia. Faculty of Medicine, The University of Queensland, Brisbane, QLD; Australia, 13 Department of Respiratory Medicine, Royal Perth Hospital, Perth, WA; Australia. Faculty of Medicine, Dentistry and Health Sciences, University of Western Australia, Perth, WA; Australia. Feinberg School of Medicine ‐ Northwestern University, Chicago; USA, 14Department of Respiratory and Sleep Medicine, Middlemore Hospital, Auckland; New Zealand. Faculty of Medical and Health Sciences, The University of Auckland, Auckland; New Zealand, 15 Department of Respiratory Medicine, Concord Repatriation General Hospital, Sydney, NSW; Australia. Respiratory Medicine, Nepean Hospital, Penrith City, NSW; Australia. Faculty of Medicine, The University of Sydney, Sydney, NSW; Australia.
Introduction/Aim
Despite a growing worldwide recognition of bronchiectasis as a cause of substantial morbidity and healthcare utilisation, little is known about the prevalence or burden of disease for Australians and New Zealanders. The Australasian Bronchiectasis Registry (ABR) was established to fill this gap and to promote international collaborative research.
Methods
A comprehensive Registry has been developed by the Australasian Bronchiectasis Consortium with the support of Lung Foundation Australia (LFA), the European (EMBARC) and US Bronchiectasis Registries, with common data fields to ensure interoperability and future collaboration, and some unique data‐fields to capture information specific to Australia and New Zealand.
Investigators identify participants during episodes of care or from pre‐existing local databases. Patients are eligible if non‐CF bronchiectasis is reported on high‐resolution computed tomography chest scan. Patient demographics and clinical information are obtained at baseline, annual review and during clinical exacerbations. Linkage to Medicare and Pharmaceutical Benefits Scheme (PBS) information provides the opportunity to study health care resource utilisation.
Results
As the first step towards a regional standardised registry, the project has been initiated at 15 hospitals, including adult, paediatric, metropolitan and regional sites. Enrolment commenced at the pilot site (Concord Hospital) in March 2016 and as of October 2016 is being undertaken at 10 sites, with the remainder awaiting research governance approvals. To date, 261 patients have been enrolled; females 166 (64%), mean age 64.7 ± 19.4 years.
Conclusion
The ABR is a secure, web‐based platform to capture the first comprehensive longitudinal data set of patients with bronchiectasis in Australia and New Zealand. Unique features include the use of opt‐out consent, collection of paediatric data and linkage to PBS/Medicare data which will allow for the first time, a topographic map of bronchiectasis in Australia and New Zealand
Grant Support
The ABR is an initiative LFA and supported by COPD Foundation, EMBARC, Bayer, Insmed, Aradigm, and Pfizer.
TO‐085: The role of Bronchoalveolar lavage (BAL) in the diagnosis of opportunistic infection in immunocompromised haematology patients
Caroline Kronborg1, Hayley Barnes1, Robert Stirling1, Michael Abramson1, 2
1 Department of Allergy, Immunology & Respiratory, Alfred Hospital, Victoria, Australia., 2Deputy head of Department of epidemiology and preventative medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, Victoria, Australia.
Introduction
Immunocompromised haematology patients are at an increased risk of developing invasive pulmonary infections with significant morbidity and mortality. Where pulmonary sepsis is suspected, our usual practice is to perform chest imaging and refer for fibreoptic bronchoscopy (FOB). We evaluated the diagnostic yield of BAL, the impact of timing and complication rate in a single centre cohort.
Methods
We performed a retrospective study of patients with haematological conditions undergoing FOB between 31/8/2013 to 31/8/2016 by searching The Alfred Bronchoscopy Database and reviewing electronic medical records.
Results
Eighty‐one patients underwent bronchoscopy. The average age was 53 years (range 19–78 years). Bronchoscopy was performed within 24 hours of HRCT in 22% and within 72 hours in 54%. Sixty percent of patients returned positive BAL cultures. Fungi were most common (69%), followed by bacterial, viral and malignant causes. Where a radiological diagnosis was suggested, this correlated with BAL findings in 50% of cases. BAL findings were concordant with pre‐FOB sputum isolates in 1/20 and 3/10 viral swabs. No major complications were recorded; 16% experienced minor bleeding (<30ml). BAL yield may have been limited by late referral, treatment commenced prior to BAL, or non‐infectious causes. Complications were poorly recorded. The impact on management was difficult to determine. The finding of a new organism was likely to lead to commencement of new therapy, but negative findings were unlikely to lead to rationalisation of treatment.
Conclusion
BAL has an important role in the diagnosis of invasive pulmonary infections in haematology patients. Our centre demonstrates a high diagnostic yield, prompt performance of the procedure and likely low complication rate.
Declaration of Interests
None to declare.
Grant support
Nil.
TO‐086: Community acquired respiratory virus detection: Comparing the diagnostic laboratory with the research laboratory
Alicia B. Mitchell1,2,3, Bassel Mourad2,3, Monique A. Malouf1, Mark Benzimra1, Damian Stark4, Lucy C. Morgan5, Brian G. Oliver2,3, Allan R. Glanville1
1Lung Transplant Unit, St Vincent's Hospital, Sydney, Australia, 2 University of Technology, Sydney, Australia, 3 Woolcock Institute, Sydney, Australia, 4 Department of Microbiology, St Vincent's Hospital, Sydney, Australia, 5 Concord Clinical School, University of Sydney, Australia.
Introduction
Pathogen detection by hospital diagnostic microbiology laboratories (HDML) is the standard operating procedure for diagnosis. However, a causative pathogen is often not identified in symptomatic respiratory tract infections. Our study compared pathogen detection in a research laboratory with an HDML to determine differences in testing sensitivity for community acquired respiratory viruses (CARV).
Methods
Samples were derived from a prospective, longitudinal study of lung transplant (LTX) recipients. Swabs of donor and explanted lungs were collected as well as bronchoalveolar lavage (BAL) fluid on post‐operative days 1, 7, 21, 42, 63 and 84. BAL sample replicates were sent to the HDML and to a research laboratory where multiple uniplex real‐time PCRs were run for human rhinovirus (HRV), respiratory syncytial virus, influenza A (Flu A), influenza B (Flu B), parainfluenza virus (PIV) 1, 2, 3, and human metapneumovirus.
Results
19 consecutive LTX subjects were recruited (bilateral: heart lung = 18:1) (age 48 ±14 years, mean ±SD) (M=9). Follow up was 59±37 days, range 7–120 days. Using a multiplex PCR, the HDML detected Flu A (n=1) and Flu B (n=1) on donor swabs plus HRV in 7/44 BAL samples. The research laboratory detected Flu A (n=4) in swabs of explanted lungs plus in BAL, HRV (n=7), Flu A (n= 23), Flu B (n = 2) and PIV (n=2). Overall concordance was 19/44, with an unweighted kappa co‐efficient of 0.113 (SE 0.054).
Conclusion
The real‐time PCR used in the research laboratory appeared to have a greater sensitivity for CARV detection compared with the HDML multiplex PCR, perhaps reflecting the greater cycle threshold value allowing detection of lower viral loads in the research laboratory. CARV (particular Flu A) are common early after LTX. The importance of low levels of persistent CARV following LTX is yet to be elucidated.
Grant Support
Nil
TO‐087: Pleural procalcitonin is not useful in differentiating parapneumonic from other effusions
AKY Teoh1, K Kairaitis1,2,3
1Department of Respiratory and Sleep Medicine, 2Ludwig Engel Centre for Respiratory Research, The Westmead Institute for Medical Research, 3University of Sydney at Westmead Hospital
Introduction/Aim
Pleural effusions are a common complication of pneumonia and chronic diseases. Pleural procalcitonin has been postulated to be useful in differentiating parapneumonic effusions (PPE) from other aetiologies. We aimed to assess the utility of additional pleural procalcitonin measurement to differentiate PPE from non‐PPE.
Methods
Consecutive patients with pleural effusion requiring thoracentesis were recruited, and clinical and anthropometric data recorded. Pleural fluid and serum were collected for standard analysis and additional procalcitonin level measurement. PPE were identified as: exudative effusions [Light's criteria (pleural/serum ratio for protein>0.5 or lactate dehydrogenase (LDH) >0.6)] with radiological evidence of a lower respiratory tract infection. Malignant pleural effusions were excluded. Data were compared using a Mann Whitney test or unpaired t‐test, correlational analysis via a Spearmans, p <0.05 considered significant.
Results
38 patients [(63.5±15.8)years; 19 male (mean±SD)] were recruited,11 (28.8%) with PPE, while 27 (71%) were non‐PPE. Pleural:serum ratios were not significantly different (p>0.05) for protein; 0.61(0.57‐0.65) (PPE; median, IQ range) and 0.51(0.36‐0.63) (non‐PPE), or LDH; 1.36(0.86‐2.17) (PPE) and 0.90(0.38‐1.35) (non‐PPE). Serum procalcitonin was equivalent in PPE and non‐PPE [0.2(0.1‐0.33)ug/L vs 0.1(0.1‐0.21)ug/L respectively, p=0.07]. Pleural procalcitonin was significantly greater in PPE compared with non‐PPE [0.21(0.17‐0.41)ug/l and 0.1(0.1‐0.15)ug/l respectively, p<0.01]. There were no significant differences between PPE or non‐PPE for:‐ serum CRP (40 (26–96)mg/L vs 27.5 (15.5‐73.25)mg/L, pleural LDH (258 (112–365)U/L vs 147 (87–300)U/L, or serum WCC (8.3 (5–13)x109/L vs (7.6 (4.8‐9.0)x109/L, all p>0.05. Serum and pleural procalcitonin correlated significantly in both PPE (r =0.99, p<0.0001) and non‐PPE (r=0.613, p=0.0007).
Conclusion
Compared with non‐PPE, pleural procalcitonin is significantly greater in subjects with PPE, and correlates with serum procalcitonin. However, the difference is small, and unlikely to assist in clinical management of PPE effusions.
Grant Support
Nil
TO‐088: Impact of a single educational intervention on antibiotic prescribing in pneumonia and COPD is not sustained beyond 6 months
Yoon Ji Jina Rhou1,2, Aruvi Thiruvarudchelvan1, Claire Thomson1, Noelia Nunez1, Keith Wong1,2,3, Paul Torzillo1,2, Lauren Troy1,2.
1Department Respiratory and Sleep Medicine, Royal Prince Alfred Hospital Camperdown, NSW, Australia, 2 Sydney Medical School, University of Sydney, Sydney, NSW, Australia, 3 Woolcock Institute of Medical Research, Glebe, NSW, Australia
Aim
The emergence of multi‐resistant organisms has been linked to injudicious antibiotic prescribing. We previously showed that a single education session increased adherence to antibiotic guidelines for Chronic Obstructive Pulmonary Disease (COPD) and Community Acquired Pneumonia (CAP). We aimed to measure the longer‐term effect of educational intervention.
Methods
Data was collected from all Respiratory admissions to an Australian tertiary hospital for CAP and COPD exacerbations over three consecutive 6 month periods (Period 1: Oct 2013‐Mar 2014; Period 2: Apr‐Sep 2014; and Period 3: Oct 2014‐Mar 2015). Following Period 1, Emergency and Respiratory Department staff attended a one‐hour education session. Adherence to guidelines in Period 3 was compared to earlier periods using chi‐squared tests for independent proportions.
Results
Period 1 comprised 194 patients (106 COPD, 88 CAP, 69.2±13.5 years, length of hospital stay (LOHS) 8.3±2.9 days, 2 deaths); Period 2: 285 patients (145 COPD, 139 CAP, 68.4±10.5 years, LOHS 8.0±6.5 days, 4 deaths); and Period 3: 196 patients (70 COPD, 126 CAP, 68.0±15.3 years, LOHS 5.8±5.1 days, 3 deaths). In Period 2, appropriate initial antibiotic prescribing for COPD improved from 46% to 71% (p<0.0001), but decreased to 42% in the subsequent 6 months, a significant reduction from Period 2 (p<0.0001) and comparable to pre‐intervention rates (p=0.5). Guideline adherence for CAP improved from 31% to 46% immediately post‐intervention (p=0.04), but declined towards pre‐intervention rates in Period 3 (38.2%, p=0.3). There was a sustained improvement in appropriate change to antibiotics for CAP (13% in Period 1 to 34% in Period 3, p=0.004). Mortality was not significantly different between periods but LOHS was significantly lower in Period 3 for both COPD and CAP.
Conclusion
An educational intervention led to a significant increase in adherence to antibiotic guidelines for COPD and CAP, but this impact waned over time.
TO‐089: Elevated neutrophil–lymphocyte count ratio is associated with increased adverse outcome in influenza
C Siew1, S Sharma2, F Hashem2, P Sivakumaran3
1Department of Medicine, GCHHS, QLD, Australia; School of Medicine, Griffith University, QLD, Australia, 2 Department of Medicine, GCHHS QLD, Australia; School of Medicine, Griffith University, QLD, Australia; School of Medicine, Bond University, QLD, Australia., 3 Department of Respiratory Medicine, GCHHS QLD, Australia; School of Medicine, Griffith University, QLD, Australia; School of Medicine, Bond University, QLD, Australia.
Introduction/Aim
The neutrophil‐lymphocyte count ratio (NLCR) has been demonstrated to be a useful predictive marker for disease severity. In this retrospective study, we investigated the prognostic impact of this biomarker in patients with influenza infection.
Methods
We retrospectively analysed patients with confirmed influenza A and/or B infection on nasopharyngeal swabs between 1st July 2015 and 31st September 2015. The clinical characteristics, laboratory markers including NLCR and radiological findings were assessed. Influenza complications including pneumonia, respiratory failure, intensive care unit (ICU) admission, length of stay, and 30‐days mortality were evaluated. We used NLCR > 5 as a cut off value and the strength of association was reported as odds ratio (OR) and 95% confidence interval (CI).
Results
Total of 320 patients were included in this study. Mean age was 53.82 years. 4.69% (n=15) of the study cohort required ICU admission and inpatient mortality was 3.43% (n=11). The overall mean NLCR was 7.17±7.32 and was significantly higher in patients who developed complications. Patients with NLCR greater than 5 were significantly associated with increased risk of developing pneumonia (OR 3.19, 95% CI = 1.76 to 5.8; p<0.0001), respiratory failure (OR 2.56, 95% CI = 1.33 to 4.91; p<0.005), and had longer length of stay (116.3 hours vs 77.11 hours, p<0.0002). There was no significant association between rate of ICU admission and 30‐days mortality with elevated NLCR.
Conclusion
A high NLCR is associated with increased unfavourable outcome in patients with influenza. The utility of NLCR as a predictive marker for pneumonia and respiratory failure in influenza to guide clinical decision making warrants further evaluation.
Grant Support
Nil
Asthma and Allergy 4
TO‐090: Saturated fatty acids, but not n‐6 polyunsaturated fatty acids or carbohydrates, increase airway inflammation in non‐obese asthmatics
LG Wood1, Q Li1, BS Berthon1, PG Gibson1,2 KJ Baines1
1Centre for Healthy Lungs, University of Newcastle, Newcastle, NSW, Australia, 2 Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, NSW, Australia
Introduction/Aim
We have previously shown that consumption of a high energy, fast food meal, rich in saturated fatty acids (SFA), n‐6 polyunsaturated fatty acids (n‐ 6PUFA) and simple carbohydrates (CHO), causes increased airway neutrophilia in asthma. This study aimed to compare the individual effects of each of these macronutrients on airway inflammation in asthma.
Methods
A randomised, crossover study in 23 adults with asthma (n=12 non‐obese, n=11 obese) was conducted. Subjects consumed 3 different isocaloric meals (~1800kJ) on 3 separate occasions, with a minimum washout period of 7 days. The meals were: SFA (delivered as double cream and butter, 70% SFA), n‐ 6PUFA (delivered as safflower oil, 72% n‐6PUFA) or simple CHO (delivered as glucose confectionary, 100% CHO). Blood and induced sputum were collected at 0 and 4 hours after consumption of the meal for measurement of inflammatory cells. Postprandial changes in sputum cell gene expression were measured by microarray analysis.
Results
Total white blood cell and blood neutrophil counts increased in both the obese and non‐obese subjects, following both of the high fat meals, while there was no increase following the high CHO meal. In sputum, neutrophils increased in the non‐obese subjects following the high SFA meal (25.8(16.5‐48.0)% median(IQR) versus 60.3 (6.0‐94.5)%, p=0.018), but there were no changes following the n‐6PUFA or CHO meals. There were no postprandial changes in airway cells in the obese subjects. The genes most significantly upregulated in the non‐obese subjects following the high SFA meal were NLRP3 and TLR4.
Conclusion
SFA, but not n‐6PUFA or CHO, cause an acute increase in airway neutrophilia in non‐obese asthmatics, associated with an activation of the NLRP3 inflammasome. The airways of obese subjects appear to be resistant to the inflammatory effects of SFA, possibly due to desensitisation resulting from chronic exposure to high circulating SFA levels.
Grant Support
NHMRC project grant
TO‐091: High fat diet‐induced obesity promotes steroid‐resistant asthma through an NLRP3 inflammasome‐dependent mechanism
James Pinkerton1, Richard Kim1, Jemma Mayall1, Md. Khadem Ali1, Malcolm Starkey1, Avril Robertson2, Luke O'Neill3, Matthew Cooper2, Philip Hansbro1, Jay Horvat1
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and The University of Newcastle, NSW, Australia, 2 Institute for Molecular Bioscience, The University of Queensland, QLD, Australia, 3 School of Biochemistry and Immunology, Trinity College, Dublin, Ireland
Introduction/Aim
Steroid‐resistant asthma is the major unmet need in asthma management. Effective treatments are urgently required, however, their development is hampered by a lack of understanding of the pathogenic mechanisms involved. An increasing body of evidence shows that a high fat diet (HFD) and/or obesity are associated with steroid‐resistant asthma, however, the precise mechanisms involved remain unclear. Studies show that HFD‐induced obesity causes increased airway hyper‐responsiveness (AHR) in mice and that these responses are driven by NLRP3 inflammasome‐mediated IL‐1β responses. However, whether HFD/obesity affects steroid responsiveness and whether therapeutically inhibiting the NLRP3 inflammasome is effective for the treatment of HFD/obesity‐induced experimental asthma is unknown.
Methods
We have developed a novel mouse model of HFD/obesity and combined it with an established model of ovalbumin‐induced steroid sensitive, allergic airway disease (AAD). The effects of steroid treatment and the roles and potential for targeting of NLRP3‐inflammasome responses in the lung in HFD/obesity‐induced AAD were examined using therapeutic treatment with dexamethasone and a potent, highly selective NLRP3 inhibitor, MCC950.
Results
We show HFD results in significant increases in adiposity and weight gain. Significantly, HFD/obesity induces increased eosinophil numbers in the lung and steroid‐resistant AHR in both the absence and presence of AAD. We also show that HFD results in an increase in NLRP3 staining in the airway epithelium as well as significant increases in active caspase‐1 in whole lung tissue. Significantly, treatment with MCC950 suppressed HFD/obesity‐induced steroid‐resistant AHR in both the absence and presence of AAD.
Conclusion
We have developed a novel murine model of HFD‐induced obesity that induces steroid‐resistant AAD. We have also identified a previously unrecognised role for HFD/obesity‐induced, NLRP3 inflammasome‐mediated responses in the lung the development of steroid‐resistant AAD. Thus, HFD/obesity induces increased NLRP3 inflammasome responses in the lung that may be therapeutically targeted in for the treatment of steroid‐resistant asthma.
Grant Support
NHMRC & HMRI
Conflict of interest:
None
TO‐092: Impaired induction of Slc26a4 promotes respiratory acidosis and severe, steroid‐insensitive asthma
Jay Horvat1, James Pinkerton1, Brittany Rae1, Jemma Mayall1, Alexandra Brown1, Md Khadem Ali1, Bridie Goggins1, Ama‐tawiah Essilfie1, Malcolm Starkey1, Anthony Bosco2, Richard Kim1, Philip Hansbro1
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and The University of Newcastle, NSW, Australia, 2 Telethon Institute for Child Health Research and the Centre for Child Health Research, the University of Western Australia, Perth, WA, Australia
Introduction/Aim
Respiratory acidosis (RA) is associated with airways hyper‐responsiveness (AHR) in severe, steroid‐insensitive (SSI) asthma and treatment with sodium bicarbonate (NaHCO3) has been used to correct RA and improve lung function in severe asthma. Thus, dysfunction of the mechanisms that govern homeostatic acid–base balance in the airways may induce RA and the cardinal features of SSI asthma. CO2 produced by cellular respiration is hydrated by carbonic anhydrases into carbonic acid (H2CO3) that dissociates into H+ and HCO3 −. These are transported in the plasma to the lungs where HCO3 − is converted back into H2CO3 and CO2 that are expelled through breathing. Reduced lung function, which occurs in SSR asthma, impairs removal of volatile H2CO3 and CO2, resulting in acid accumulation and increased arterial PaCO2. Patients with severe asthma often develop complications from increased PaCO2, which skews the PaCO2/HCO3 − ratio resulting in increased H+ concentration and reduced pH.
Methods
We developed mouse models of respiratory infection and ovalbumin‐induced SSI allergic airways disease (SSIAAD) that are highly representative of human disease. Microarray analyses of the lungs of mice with SSIAAD showed that all three infections decrease the expression of the chloride (Cl−)/HCO3 − pump, Slc26a4, which is crucial for secretion of HCO3 − into the airway lumen. Thus, we assessed the roles and potential for targeting of Slc26a4 and RA in SSIAAD.
Results
We show that respiratory infections suppress the induction of Slc26a4 in the airway epithelium in AAD. This is associated with increased levels of free H+ ions in bronchoalveolar lavage. Treatment with NaHCO3 during infection‐induced SSIAAD suppressed steroid‐resistant AHR. In a complementary gain‐of‐function study, administration of acetazolamide (a carbonic anhydrase inhibitor) in steroid‐sensitive AAD, to mimic the effect of decreased Slc26a4 responses, induced steroid resistance of AHR.
Conclusion
We have identified a previously unrecognised role for Slc26a4 in promoting RA and SSRAAD.
Grant Support
NHMRC, HMRI
TO‐093: Limited exacerbation of asthma symptoms by electronic‐cigarette aerosol exposure in a mouse model of asthma
Alexander Larcombe1, Maxine Janka1,Luke Berry1, Benjamin Mullins2,3
1Telethon Kids Institute, University of Western Australia, Subiaco, Australia, 2 Fluid Dynamics Research Group, Curtin University, Perth, Australia, 3 Health, Safety and Environment, School of Public Health, Curtin University, Perth, Australia,
Introduction/Aim
Electronic cigarettes (“e‐cigarettes”) heat and aerosolise a liquid producing an inhalable aerosol often containing nicotine and flavourings. Very little is known about their potential to impact health – however some research indicates they increase airway resistance in healthy and asthmatic individuals and may facilitate asthma attacks. We aimed to assess the effects of e‐cigarette use on lung function (early and late phase asthmatic responses; EPR and LPR respectively) in mice with and without existing ovalbumin‐induced allergic airways disease.
Methods
We assessed volume and lung function using plethysmography and the forced‐oscillation technique in naïve and asthmatic adult female BALB/c mice each minute for 30 minutes after an acute e‐cigarette aerosol exposure. We also measured airway hyper‐responsiveness (AHR) in a second group of mice 6 hours after 30 minutes of aerosol exposure. Four types of e‐cigarette were tested.
Results
For EPR studies, acute e‐cigarette exposure had little effect on lung function, except for mice exposed to vegetable‐glycerin vapours, which exhibited immediate, temporary impairments in lung function. There was little difference between asthmatic and non‐asthmatic mice. For LPR studies, previous e‐cigarette exposure did not exacerbate functional asthmatic responses, and there was a protective effect of nicotine free e‐cigarette vapour on inflammation. For both studies, sensitisation and challenge with ovalbumin increased AHR and cellular inflammation, and there was exacerbation of eosinophilia and neutrophilia e‐cigarette exposed asthmatic mice.
Conclusion
This study showed that acute e‐cigarette aerosol exposure has limited effects on respiratory health in a mouse model of allergic airways disease. E‐cigarette aerosol exposure had both negative and protective effects on respiratory health, apparently dependent on the type of e‐cigarette excipient. Until more information is available, caution should be exercised when advocating e‐cigarettes as a safe alternative to tobacco smoking, especially in asthmatics.
Declaration of interest
None.
Grant Support
Supported by an Asthma Foundation of Western Australia Project Grant.
TO‐094: Multidimensional assessment and targeted therapy of severe persistent asthma: A randomised controlled trial
VM McDonald1 ,2,3,4 VL Clark1,2,4, PAB Wark1,3,4, KJ Baines4 & PG Gibson1,3,4
1Centre for Research Excellence in Severe Asthma, 2 School of Nursing and Midwifery, University of Newcastle, NSW Australia, 3 Department of Respiratory and Sleep Medicine, John Hunter Hospital, HMRI, NSW, Australia, 4 Priority Research Centre for Healthy Lungs, University of Newcastle, NSW, Australia
Introduction/Aim
Severe asthma is a heterogeneous disease that causes significant disease burden, is often refractory to treatment and is associated with comorbidities and risk‐factors that confound management. Multidimensional assessment (MDA) followed by management that is targeted to ‘treatable traits’ has been proposed as a superior treatment approach. We aimed to test the hypothesis that MDA and targeted‐therapy for severe asthma would lead to improved control measured by the asthma control questionnaire (ACQ5).
Methods
A randomised controlled trial of MDA and targeted‐therapy (Intervention group, IG) versus usual severe asthma care (UC) was conducted. Participants with severe asthma (n=55) underwent a baseline MDA and 16 week follow‐up. The intervention involved individualised therapies tailored to treatable traits of the airway, comorbidities, risk‐factors and self‐management, delivered via case‐management. The UC arm received evidence‐based treatment within a severe asthma clinic.
Results
Twenty‐eight participants were randomised to IG and 27 to UC; 65.5% were female, with a mean (SD) age of 52.2 (13.9) years and post‐bronchodilator FEV1 was 73.0% (21.2).
The intervention resulted in significant improvements in asthma control compared to UC; mean difference (SE) in ACQ5 post IG −0.61 (0.18) compared to 0.07 (0.19) for UC, p=0.01.
IG also resulted in significant improvements in health‐status, mean difference (SE) in Asthma Quality of Life Questionnaire was 1.01 (0.18) compared to −0.01 (0.18) for UC, p=0.001. Sputum eosinophils (%) increased in the UC 8.20 (3.49) compared to −2.52 (3.73) for IG, p=0.04. There was also a significant reduction in IG CRP; −4.90 (1.42) compared to UC 0.61 (1.36), p=0.01.
Conclusion
Management of severe asthma that is based on multidimensional assessment followed by therapy targeted to treatable traits results in significant improvements. This study supports a precision‐based medicine approach in severe asthma.
Grant Support
Hunter Medical Research Institute, University of Newcastle, John Hunter Hospital
TO‐095: Physical inactivity and sedentary time in severe asthma
L Cordova‐Rivera1,2, PG Gibson1,2,3, PA Gardiner5 & VM McDonald1 ,2,3,4
1Centre for Research Excellence in Severe Asthma, 2 Priority Research Centre for Healthy Lungs, University of Newcastle, NSW, Australia 3Department of Respiratory and Sleep Medicine, John Hunter Hospital, HMRI, NSW, Australia 4School of Nursing and Midwifery, University of Newcastle, NSW Australia, 5 The University of Queensland, School of Medicine, Brisbane, Qld., Australia
Introduction/Aim
Physical inactivity and sedentariness are behaviours that are likely to be particularly extreme in severe asthma (SA) populations, secondary to a high symptom and comorbidity burden. The degree of inactivity in SA however has not been quantified. We aimed to objectively measure physical activity (PA) and sedentary time (ST) in patients with SA compared to controls, and describe the correlations of these behaviours with clinical outcomes.
Method
A cross‐sectional study of adults with physician diagnosed SA (n=65) and healthy controls (HC) (n=33) was conducted. Participants underwent a multidimensional assessment involving measurement of lung function, exercise capacity, airway and systemic inflammation, asthma control and quality of life. PA and ST were measured for 14 consecutive days using a triaxial accelerometer (ActiGraph wGT3X‐BT).
Results
The SA group included 33 (50.7%) females, aged (mean±SD) 53.4±15.7 years. The HC group included 26 (76%) females, [median, IQR] age 39 [29–62] yrs. Compared to controls, people with SA spent significantly less minutes/day in moderate and vigorous intensity PA: 22.7 [12.9‐39.7] versus 39.3 [29.2–47.0] (p <0.01); and took less steps per day: 5685 [4109–7832] versus 7594 [6136–8837] (p <0.01). However, SA participants performed more minutes/day of light PA than controls: 195.18 (58.22) versus 166.53 (50.76) (p <0.05). No statistically significant differences in ST were found between the two populations. There were moderate correlations between PA and ST and systemic inflammation, exercise capacity, asthma control and quality of life.
Conclusion
Compared to controls, people with SA perform less moderate intensity activity, despite engaging in more light physical activity. The amount of activity is associated with important disease outcomes. These data show the potential benefits of targeting inactivity as a non‐pharmacological strategy in the management of severe asthma.
Key Words
severe asthma, physical activity, sedentary behaviour, correlation.
Nomination for New Investigator Award
Grant Support
John Hunter Hospital Charitable Trust.
Cell Biology/Immunology 2
TO‐096: Lung fibroblasts of IPF patients display senescence‐like features in vitro
Michael Schuliga1, Dmitri V. Pechkovsky2, David Waters1, Emily Fogarty1, Cory M. Hogaboam3, Eric Yao2,4, Nasreen Khalil5, Victor J. Thannickal6, Moisés Selman7, Janette K Burgess8, Jade Jaffar9, Glen Westall9, Chris Grainge1 and Darryl A. Knight1,2,4
1School of Biomedical Sciences and Pharmacy, University of Newcastle, Australia, 2 James Hogg iCAPTURE Centre, University of British Columbia (UBC), Canada., 3 Department of Pathology, University of Michigan, USA, 4 Dept of Anesthesiology, Pharmacology and Therapeutics, UBC, Canada., 5 Dept of Respiratory Medicine, UBC, Canada, 6 Division of Pulmonary, Allergy and Critical Care Medicine, Department of Medicine, University of Alabama at Birmingham, USA, 7 Instituto Nacional de Enfermedades Respiratorias, Mexico, 8 Department of Pathology and Medical Biology, UMCG, Netherlands, 9 Allergy, Immunology and Respiratory Medicine, Alfred Hospital, Australia
Introduction/Aim
Idiopathic pulmonary fibrosis (IPF), a fatal lung disease of unknown etiology, occurs predominantly in the elderly. The mechanisms that link aging with the persistent accumulation of lung fibroblasts (LFs) in IPF, remain incompletely understood. Fibroblast senescence, characterized by growth arrest, apoptosis resistance and a senescence‐associated secretory phenotype (SASP), occurs in aging and may contribute to IPF. The aim of this study was to characterize senescence in human LFs in vitro, and to ascertain the role of mitochondrial dysfunction in the acquisition and/or reinforcement of the senescent phenotype.
Methods
IPF‐LF lines established from lung tissue of IPF patients were compared with LFs of age‐matched controls (Ctrl‐LFs). Cell proliferation, telomere length, SASP cytokine production, senescent‐associated β‐galactosidase (SA‐β‐Gal) activity and levels of p16 and p21 were assessed by cell counting, PCR, ELISA, cytochemistry and immunoblotting respectively. Increased levels of mitochondrial DNA and superoxide, features of mitochondrial dysfunction, were evaluated by PCR and the MitoSox fluorogenic dye respectively. Rotenone was used to disrupt mitochondrial activity.
Results
IPF‐LFs displayed slower growth accompanied by decreased levels of cellular protein and telomere length when compared with Ctrl‐LFs (p<0.05). Conversely, IPF‐LFs were more resistant to H2O2‐induced cytoxicity than Ctrl‐LFs (p<0.05). IPF‐LFs also exhibited increased SA‐β‐Gal activity, SASP cytokine production and levels of p16 and p21 (p<0.05). Furthermore, IPF‐LFs had lower levels of the mitochondria‐driven proteins Bcl‐2 and Bax, but higher levels of mitochondrial DNA and superoxide production than Ctrl‐LFs. Rotenone (0.6 μM) increased mitochondrial superoxide in Ctrl‐LFs, preceding increases in markers of senescence.
Conclusion
Our study suggests that IPF‐LFs exhibit senescent like features, including replicative arrest, resistance to oxidative stress‐induced cytoxicity and induction of a SASP. Mitochondrial dysfunction is tightly linked with senescence and is likely to contribute to the healing/repairing malfunction of LFs in IPF.
Grant Support
NHMRC #1099569 and the LFA David Wilson Scholarship
TO‐097: Non‐antibiotic macrolides restore airway macrophage phagocytic function with potential anti‐inflammatory effects in chronic lung diseases
Rhys Hamon1, Hai Tran1, Eugene Roscioli1, Hubertus Jersmann1,2, Paul N Reynolds1,2, Sibylle Wilbert3, Sandra Hodge1,2
1Lung Research Unit, Hanson Institute and Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, Australia;, 2 Department of Medicine, University of Adelaide, Adelaide, Australia;, 3 Gilead Sciences, Seattle, Washington, USA.
Introduction/Aim
We reported defective efferocytosis associated with cigarette smoking and/or airways inflammation in chronic lung diseases including chronic obstructive pulmonary disease and severe asthma. We also showed defects in phagocytosis of non‐typeable H. influenzae (NTHi), a common colonizer of the lower airway in COPD. These defects could be substantially overcome with low‐dose Azithromycin; however, chronic usage may induce bacterial resistance. We investigated two novel macrolides, GS‐459755 (2'‐desoxy‐9‐(S)‐erythromycylamine) and GS‐560660 (Azithromycin‐based 2'‐desoxy molecule) with significantly diminished antibiotic activity against S. aureus, S. pneumonia, M. catarrhalis, and H. influenzae.
Methods
Macrolide effects on efferocytosis, phagocytosis of NTHi, cell viability, receptors involved in recognition of apoptotic cells and/or NTHi (flow cytometry), secreted and cleaved intracellular IL‐1β (CBA, immunofluorescence/ confocal microscopy) and NLRP3, were tested on primary alveolar macrophages and THP‐1 macrophages ± 10% cigarette smoke extract.
Results
Dose response experiments showed optimal pro‐phagocytic effects of GS‐459755 and GS‐560660 at low concentrations of 0.5‐1μg/mL, comparable to our findings with Azithromycin. Both macrolides significantly improved phagocytosis of apoptotic cells and NTHi (eg, increases in efferocytosis and phagocytosis of NTHi: GS‐459755 23% and 22.5% p=.043; GS‐560660 23.5% and 22% p=.043, respectively). Macrophage viability remained >85% following 24h exposure to either macrolide at concentrations up to 20μg/mL. Secreted and intracellular cleaved IL‐1β were decreased with both macrolides with no significant changes in recognition molecules MerTk, SRA1, TLR2/4 or CD36. Particulate cytoplasmic immunofluorescence of NLRP3 inflammasome was also significantly reduced.
Conclusion
We conclude that GS‐459755 and GS‐560660 may be useful for reducing airway inflammation in chronic lung diseases without inducing bacterial resistance.
Grant Support
Supported by a National Health and Medical Research Council Project Grant 1106377 and Career Development Award 104551
TO‐098: Antenatal Vitamin C administration in sheep is protective against fetal hypoxemia‐induced oxidative stress and airway remodelling in early adulthood
Sandra Orgeig1, Erin V. McGillick1 ,2, Beth J. Allison3, Kirsty L. Brain3, Youguo Niu3, Nozomi Itani3, Katie L. Skeffington3, Christian Beck3, Kimberley J Botting3, Dino A Giussani3 Janna L. Morrison2
1Molecular & Evolutionary Physiology of the Lung Laboratory and 2Early Origins of Adult Health Research Group, School of Pharmacy & Medical Sciences, Sansom Institute for Health Research, University of South Australia, 3 Department of Physiology, Development & Neuroscience, University of Cambridge
Introduction/Aim
Chronic fetal hypoxemia is a common pregnancy complication associated with intrauterine growth restriction (IUGR) and respiratory disease at birth and in later life. The molecular mechanisms that are responsible are not understood. Hypoxia and oxidative stress are linked to poorer cardiovascular outcomes at birth and in later life and antenatal antioxidant administration ameliorates these effects. Here, we investigate the effect of chronic fetal hypoxemia and antenatal administration of the antioxidant, Vitamin C, on molecular regulation of lung structure and function in lambs.
Methods
Chronically catheterised pregnant sheep carrying female singletons were exposed to normoxia (N; n=20) or hypoxia (H; n=18; 10% O2) with either saline (NS=11; HS=8) or Vitamin C (NVC=9; HVC=10; maternal 200mg/kg i.v. daily) from 105‐138d (term, ~145d). Lung tissue was collected from lambs 9 months after birth. Lung expression of genes as markers of oxidative stress (NADPH oxidase 4, NOX‐4), airway remodelling (elastin, ELN) & surfactant maturation (surfactant proteins (SP) ‐ A, −B, −C, −D) were quantified by qRT‐PCR. Numerical density of SP‐B positive cells in lung tissue was determined by point counting. Data were analysed by two‐way ANOVA (P<0.05) for treatment (N vs. H) and drug (S vs. VC).
Results
H induced fetal growth restriction but there was no effect of H or VC on body weight or relative lung weight in lambs at 9 months. H increased gene expression of NOX‐4 (NS: 0.0029±0.00017 vs HS: 0.0039±0.00056 mean normalised expression (MNE)) and ELN (NS: 0.159±0.02 vs HS: 0.280±0.04 (MNE)) in postnatal lung tissue but this was ameliorated by antenatal VC administration (HVC; NOX‐4: 0.0028±0.0003 & ELN: 0.164±0.02 MNE). There was no effect of H or VC on expression of surfactant proteins or number of surfactant producing cells present in lung tissue.
Conclusion
Here we show effects of chronic fetal hypoxemia on molecular programming of oxidative stress and airway remodelling in the lung in early adulthood and that maternal antenatal antioxidant treatment is protective, offering insight into mechanism and possible treatment to improve offspring respiratory outcomes.
Grant Support
British Heart Foundation & NHMRC of Australia
TO‐099: Role of increased iron levels in the pathogenesis of lung disease
Md Khadem Ali1, Richard Kim1, Daniel Johnstone3, Ama‐Tawiah Essilfie1, Jemma Mayall1, Rafia Karim1, James Pinkerton1, Moones Heidari2, Chantal Donovan1, Gang Liu1, Kristy Martin2, Liz Milward2, Philip Hansbro1 and Jay Horvat1
1Priority Research Centre for Asthma and Respiratory Diseases, Hunter Medical Research Institute and School of Biomedical Sciences and Pharmacy, University of Newcastle, NSW 2308 Australia, 2 School of Biomedical Sciences and Pharmacy, The University of Newcastle, Newcastle, New South Wales, Australia., 3 Bosch Institute and Discipline of Physiology, University of Sydney, NSW 2006, Australia
Introduction
Iron is essential for many biological processes. Too much or too little iron can result a wide variety of pathologies. Altered iron levels and/or dysregulated iron homeostasis have been associated with a number of lung diseases, including chronic obstructive pulmonary disease, lung cancer and cystic fibrosis, however, the mechanisms that underpin these associations and whether iron plays a role in the pathogenesis of lung disease are yet to be fully elucidated.
Aim
To determine the effects of systemic iron overloading on iron levels in the lung and to assess the effects of increased iron on lung structure and function.
Methods
Levels of systemic and pulmonary iron and lung structure and function were assessed in transferrin receptor (TFR)2 mutant mice and wild‐type (WT) BALB/c mice fed a 2% carbonyl iron diet compared to WT and normal diet controls, respectively. The effects of increased iron loading on murine models of bleomycin‐induced fibrosis and house dust mite (HDM)‐induced allergic airway disease (AAD) were also assessed.
Results
Excess iron accumulation was observed in the lungs in both the genetic and diet‐induced models of iron overloading. Increased iron levels in the lung were associated with emphysema‐like alveolar enlargement, small airways collagen deposition, alterations in baseline lung function and increased airways hyper‐responsiveness (AHR). Whilst iron overloading in the absence of bleomycin administration results in the generation of fibrosis in the small airways and AHR to similar levels observed with bleomycin‐induced fibrosis, iron overloading had minimal additional effects when combined with bleomycin. Iron overloading also resulted in increased eosinophilic inflammation and severe AHR in HDM‐induced AAD.
Conclusion
These data show that increased iron levels in the lung results in emphysema and airways fibrosis that corresponds with reduced lung function. These models will be used to better understand the role of iron in the pathogenesis of lung disease.
Grant Support
NHMRC & HMRI
Conflict of interest
None
TO‐100: Dysregulated STAT3 signaling induces and reinforces fibroblast senescence in lung fibroblasts of IPF patients
David W. Waters1, Michael Schuliga1, Emily Fogarty1, Janette Burgess2, Chris Grainge3 Glen Westall4, Geoffrey Laurent 5 , Cecilia M Prêle 6,7 , Steve E. Mutsaers 6,7 , and Darryl A. Knight1
1School of Biomedical Sciences and Pharmacy, University of Newcastle, Australia, 2 GRIAC, University of Groningen, Groningen, Netherlands, 3School of Medicine and Public Health, University of Newcastle, Australia, 4Allergy, Immunology and Respiratory Medicine, Alfred Hospital, Victoria, Australia 5Centre for Cell Therapy and Regenerative Medicine, University of Western Australia, Crawley WA 6009, Australia. 6Lung Institute of Western Australia and Centre for Asthma, Allergy and Respiratory Research, School of Medicine and Pharmacology, University of Western Australia, Harry Perkins Institute of Medical Research, Nedlands, WA, Australia, 7Centre for Cell Therapy and Regenerative Medicine, School of Medicine and Pharmacology, University of Western Australia and Harry Perkins Institute of Medical Research, Nedlands, WA, Australia
Introduction/Aim
Idiopathic pulmonary fibrosis (IPF) is a chronic fibrosing interstitial pneumonia of unknown cause and has a median survival of only 3 years. We have previously shown that dysregulated activation of the transcription factor STAT3 characterizes functionally different subsets of fibroblasts, the presence of which correlates with IPF progression. The question of what drives these phenotypically divergent cells and prolongs their lifespan remains unanswered. Our hypothesis is that activated STAT3, a transcription factor that is increased in fibrotic lung tissue of IPF patients, contributes to senescence via its roles in cytokine expression and mitochondrial dysfunction. The aim of this work is to evaluate whether STAT3 has a role in senescence of lung fibroblasts (LFs) in IPF.
Method
Primary cultures of LFs were established from lung tissue of IPF patients (IPF‐LF) and control donors (Ct‐LF). Senescence was induced by exposing cells to hydrogen peroxide (H202, 150 μM) for 2 hr. STAT3 activation was assessed at different passages or following H202 by immunoblotting. Senescence was evaluated by measuring senescent‐associated‐β‐galactosidase (SA‐β‐Gal) activity, IL‐6 production and expression of cell‐cycle arrest protein p21. Mitochondrial superoxide production was assessed using the mitosox flourogenic assay. STAT3 was inhibited with pharmacological inhibitors or by transfection with siRNA.
Results
A higher percentage of IPF‐LFs were positive for SA‐β‐Gal at earlier or equivalent passages than the Ct‐LFs, as were levels of p21 and mitochondrial superoxide (p<0.05). At both early (6) and late (15) passages, IPF‐LFs (n=4) produced more IL‐6 than Ct‐LFs (n=3) (p<0.05). Baseline levels of pSTAT3 were higher in IPF‐LFs and increased in Ct‐LFs following treatment with H202. Targeting STAT3 attenuated IL‐6 production, levels of p21 and mitochondrial superoxide production.
Conclusion
Our data suggests that IPF‐LFs display accelerated senescence in association with increased STAT3 activation and superoxide production. STAT3 contributes to senescence in IPF through regulating mitochondrial activity.
Grant Support
This research was funded by NHMRC grant 1099569 and by the Lung Foundation Australia David Wilson Scholarship awarded to David Waters.
Key Words
Nomination for New Investigator Award
Grant Support
TO‐101: Fiublin‐1c plays critical roles in lung remodelling in idiopathic pulmonary fibrosis
Gang Liu1, Marion A Cooley2, Andrew G Jarnicki1, Alan C‐Y Hsu1, Prema Mono Nair1, Tatt Jhong Haw1, Gavin Tjin3, Bernadette Jones1, Celeste L Harrison1, Michael Fricker1, Mark D Inman4, Marjorie M. Walker1, Jay C Horvat1, Brian G Oliver3,5, William S Argraves2, Darryl A Knight1, Janette K Burgess4,6, Philip M Hansbro1
1Priority Research for Asthma and Respiratory Diseases, Hunter Medical Research Institute and The University of Newcastle, Newcastle, New South Wales, Australia, 2Department of Regenerative Medicine and Cell Biology, Medical University of South Carolina, Charleston, USA, 3Woolcock Institute of Medical Research, Discipline of Pharmacology, The University of Sydney, Sydney, New South Wales, Australia, 4Division of Respirology, Department of Medicine, McMaster University, Hamilton, Ontario, Canada, 5School of Life Sciences, The University of Technology, Sydeny, New South wales, Australia, 6Department Pathology and Medical Biology, University of Groningen, University Medical Center, Groningen, The Netherlands
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, and lethal interstitial fibrotic lung disease with poor survival rate after diagnosis. Airway and/or lung remodeling are major features of IPF and associated with accumulation of extracellular matrix (ECM) proteins. Fibulin‐1 (Fbln1), an important ECM protein has four variations (Fbln1a/b/c/d) and stabilizes other ECM proteins. Fbln1c, one of Fbln1 variants, predominates in both humans and mice, and involves in lung fibrosis.
Aims
To determine Fbln1c levels in IPF patients and elucidate the role Fbln1c in pathogenesis of pulmonary fibrosis.
Methods
Fbln1c was measured in IPF patients and bleomycin‐induced lung fibrosis model. Fbln1c deficiency (−/−) mice were used to investigate the mechanism of Fbln1c regulated remodelling in lung fibrosis.
Results
Fbln1 was increased in lung tissue of IPF patients and Fbln1c protein was increased bleomycin‐induced experimental lung fibrosis in mice. Fbln1c −/− mice had reduced airway remodelling and lung fibrosis, and were protected against lung function impairment after 28 days bleomycin challenge. In experimental lung fibrosis, Fbln1c interacted with fibronectin, periostin and tenascin‐c to stabilise collagen deposition around the small airway and in whole lungs. Fbln1c regulated transforming growth factor‐beta (TGF‐β) activation by binding with latent TGF‐β binding protein (LTBP1), and mediated phosphorylated Smad3 level, a downstream molecular of TGF‐β pathway. This process also regulated myofibroblasts number and collagen deposition. Interestingly, Fbln1c −/− mice also had less inflammatory cells, and interleukin (IL)‐33 in lungs of experimental lung fibrosis than WT mice.
Conclusions
Our data demonstrates a novel role of Fbln1c in lung remodelling in IPF. Inibhition of Fbln1c may be a therapeutic target in IPF.
Grant Support
NHMRC grant, LFA/Lizotte Family Research Award
Chronic Obstructive Pulmonary Disease 2
TO‐102: Home‐based rehabilitation for COPD using minimal resources: an economic evaluation
AT Burge1,2,3, AE Holland1,2,3, CF McDonald3 ,4, CJ Hill3,5, AL Lee1,2,3, NS Cox1,3, R Moore5,C Nicolson2, A Lahham1, R Gillies5, MJ Abramson6, A Mahal7
1Physiotherapy, La Trobe University, 2Physiotherapy, The Alfred, 3Institute for Breathing and Sleep, Austin Health, 4Respiratory and Sleep Medicine, Austin Health, 5Physiotherapy, Austin Health, 6Public Health and Preventive Medicine, Monash University, 7Nossal Institute for Global Health, The University of Melbourne
Introduction/Aim
Pulmonary rehabilitation (PR) is a cornerstone of care for COPD. A new model using a home‐based programme has shown equivalent short‐term clinical outcomes to a centre‐based programme for comparable direct intervention costs. This economic evaluation sought to determine and compare the costs and benefits of both intervention models during the 12‐month follow‐up period.
Methods
Participants with stable COPD were randomly assigned to complete either home or centre‐based PR. Complete case analysis was undertaken for participants who completed the Short‐form 36 (SF‐36v2) questionnaire at the end of PR and 12 months following programme completion, to enable preference‐based classification of health status using the SF‐6D and calculation of quality‐adjusted life years (QALYs). Direct provider costs for healthcare utilisation were collected from hospitals and the Department of Health & Human Services during the 12‐month follow‐up period.
Results
Complete SF‐36 data were available for 59 participants (36 female, mean [SD] age 71 [8] years, FEV1 53 [19] %predicted) who completed home‐based PR (74%) and 60 people (33 female, mean age 68 [9] years, FEV1 50 [20] %predicted) who undertook a centre‐based programme (70%). Participants in the home‐based programme had lower costs for COPD‐related outpatient appointments (mean difference $415, 95%CI ‐$808 to ‐$22) and tended to have lower costs for hospital admissions ($4600, 95%CI ‐$10,331 to $1130). Overall healthcare provider costs tended to be lower in the home‐based group (−$6449, 95%CI ‐$15,347 to $2450). The difference in QALYs was not significantly different between groups (0.021, 95% CI −0.022 to 0.064).
Conclusion
In the 12 months following PR, healthcare provider costs were equivalent or lower for home‐based participants compared to people undertaking a centre‐based programme. This group also demonstrated equivalent QALYs. These results support the clinical implementation of this new model of PR.
Grant Support
Lung Foundation Australia, National Health and Medical Research Council
Declaration of interest
None Declared
TO‐103: Electrocardiograms and chest radiographs in patients with abnormal cardiac biomarkers during exacerbations of COPD
Eskandarain Shafuddin1 2,Manisha Cooray 1,Catherina L Chang1, Kim McAnulty3 , Noel Karalus1, Marcus Lee4, Robert J Hancox1 2
1Department of Respiratory Medicine, Waikato Hospital, Hamilton, New Zealand, 2 Department of Preventive and Social Medicine, University of Otago, Dunedin, New Zealand, 3 Department of Radiology, Waikato Hospital, New Zealand, 4 Department of Cardiology, Waikato Hospital, Hamilton, New Zealand
Introduction/Aim
Biochemical evidence of cardiac dysfunction is common in exacerbations of chronic obstructive pulmonary disease (COPD), even in patients without clinically suspected cardiac disorders. We investigated associations between abnormal N‐terminal pro‐B‐type natriuretic peptide (NT‐proBNP) and troponin T and abnormalities on electrocardiograms and chest radiographs in patients hospitalised for exacerbations of COPD.
Methods
Electrocardiograms were assessed for tachycardia, atrial fibrillation, right and left ventricular hypertrophy, and ischaemic changes in 389 patients. Chest radiographs were assessed for signs of heart failure in 350 patients. All assessments were done by two independent examiners blinded to cardiac biomarker status. Associations between abnormalities with at least moderate inter‐rater agreement and high cardiac biomarkers (NT‐proBNP >220pmol/L and troponin T >0.03ug/L or high‐sensitivity >50ng/L) were analysed.
Results
High NT‐proBNP values were associated with atrial fibrillation (22% vs. 6%), right ventricular hypertrophy (24% vs. 15%), left ventricular hypertrophy (15% vs. 4%), ischaemia (59% vs. 33%) on electrocardiogram and cardiomegaly (42% vs. 20%) on chest radiographs. High troponin T values were associated with tachycardia (65% vs. 41%), right ventricular hypertrophy (26% vs. 15%) and ischaemic changes (60% vs. 36%) on electrocardiogram. None of these tests were very sensitive or specific for biochemical indicators of cardiac dysfunction: the best‐performing indicator for NT‐proBNP was ischaemic change (sensitivity 59% and specificity 67%). For troponin T the best indicators were tachycardia and ischaemic change (sensitivity 65% and 60%, specificity 59% and 64% respectively).
Conclusion
Abnormal electrocardiograms and chest radiographs are associated with abnormal cardiac biomarkers and may indicate cardiac disease in patients with exacerbations of COPD. However, electrocardiograms and chest radiographs have poor sensitivity and specificity for diagnosing acute cardiac dysfunction in this setting. Cardiac biomarkers provide additional information about acute cardiac dysfunction in patients with exacerbations of COPD.
Grant Support
Partially supported by the Waikato Medical Research Fund and the Heart Foundation New Zealand
TO‐104: MicroRNA‐21 drives experimental chronic obstructive pulmonary disease through a SATB1/S100A9/NF‐κB axis
Richard Kim1, Krishna Sunkara1, Andrew Jarnicki2, Ken Bracke3, Tatt Jhong Haw1, Peter Wark1, Griet Conickx3, Guy Brusselle3, Jay Horvat1, Paul Foster1, Philip Hansbro1
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and The University of Newcastle, NSW, Australia, 2 Department of Pharmacology and Therapeutics, University of Melbourne, VIC, Australia, 3 Department of Respiratory Medicine, Ghent University Hospital, Ghent, Belgium
Introduction/Aim
Chronic obstructive pulmonary disease (COPD) is the 3rd leading cause of chronic morbidity and death worldwide. Cigarette smoking is the major cause of COPD in developed countries. Current therapies have limited efficacy, fail to halt disease progression, and can cause adverse side effects. Effective treatments are urgently required, however, their development is hampered by a lack of understanding of the mechanisms that promote the pathogenesis of disease. The functions of microRNAs (miRs) in health and disease are firmly established and their aberrant expression has been associated with several lung diseases, including COPD. This study aimed to identify miRs that promote the development of COPD and assess the therapeutic potential of targeting the miRs that we identify.
Methods
We performed miR microarray analyses of the lungs of mice exposed to our highly representative, cigarette smoke (CS)‐induced model of experimental COPD. We identified miR‐21 as one of the highest upregulated miRs. The roles and potential for targeting of CS‐induced miR‐21 in the lung were examined using treatment with a specific miR‐21 inhibitor (antagomir, Ant‐21).
Results
Lung miR‐21 expression was increased throughout CS exposure in experimental COPD. Reduced lung function in human COPD patients correlated with lung miR‐21 expression. Treatment with Ant‐21 inhibited CS‐induced lung miR‐21 expression and suppressed airway inflammation and small airway fibrosis, and improved lung function, in experimental COPD. In silico analyses identified a potential miR‐21/SATB1/S100A9/NF‐κB axis. SATB1 is a putative miR‐21 target that negatively regulates S100A9, a known inducer of NF‐κB activity. Significantly, CS exposure decreased lung SATB1 in our model, and Ant‐21 treatment restored SATB1 levels and decreased S100A9 expression and NF‐κB activity.
Conclusion
We have identified a previously unrecognised pathogenic role for a miR‐21/SATB1/S100A9/NF‐κB axis in experimental COPD. Our data highlights miR‐21 as a novel therapeutic target for the treatment of COPD.
Grant Support
NHMRC
Conflict of interest
None
TO‐105: Relationship between TLCO, Emphysema Index, FEV1 and Pulmonary Artery Distensibility ‐ a sub‐analysis of the 4C cohort
Lin Mo1, Martin MacDonald1 , Christian Osadnik12, Paul King1, John Troupis3, Philip Bardin1
1Monash Lung and Sleep, Monash Health, Monash Medical Centre, Clayton VIC 3168, 2 Monash University Department of Physiotherapy, Frankston VIC 3199, 3 Monash Imaging, Monash Medical Centre, Clayton VIC 3168
Introduction/Aim
Pulmonary hypertension is an important complication of Chronic Obstructive Pulmonary Disease (COPD), however it can be difficult to identify. Reduction in Carbon Monoxide Transfer Factor (TLCO) is a feature of both emphysema and pulmonary hypertension. CT can quantify emphysema via the emphysema index (EI). In addition, pulmonary artery distensibility (PAD) is known to correlate with mean pulmonary artery pressure measured at right heart catheterisation and can be measured simultaneously using ECG‐gated CT. The impact of pulmonary artery distensibility on the relationship of FEV1 and Emphysema Index (EI) with TLCO has never been examined. The aim of this study is to determine the effect of PAD, FEV1(%) and EI on TLCO, with the hypothesis that the addition of PAD data would help account for variability in TLCO unexplained by the other two parameters.
Methods
Patients were analysed from the 4C cohort, a prospective group of patients who were recruited over a 1 year period during acute exacerbations of COPD and had subsequent ECG gated CT and pulmonary function tests performed during stable periods. After excluding patients with missing data, significant motion artefact on CT and those unable to perform TLCO, 34 patients were entered into a multiple linear regression model.
Results
TLCO corrected for haemoglobin was entered as the dependent variable and in order FEV1(%), EI and PAD were entered into the regression model as independent variables. Overall, the model was able to explain 62.5% of the variation in TLCO (Corrected R2 0.625). Both FEV1(%) and EI were significantly correlated with TLCO after controlling for the other variables (FEV1(%) r = 0.512 and P<0.001, EI r = −0.431 and p = 0.003) However, after controlling for FEV1pp and EI, PAD was not significantly correlated with TLCO (r = −0.055, p = 0.637).
Conclusion
FEV1(%) was significantly positively correlated and Emphysema Index was significantly negatively correlated with TLCO after controlling for the other variable. The addition of PAD data did not appear to add to the analysis.
Grant Support
Nil
TO‐106: The prevalence of reduced transfer factor for carbon monoxide (TLCO) in smokers with normal spirometry
Tim Cheung1, Vicki Papanikolaou 1,2,Paul Finlay1,2,Theresa Yong1, Martin MacDonald1 ,2, Philip Bardin1,2,Paul King1,2
1Monash Lung & Sleep, Monash Health, Clayton Victoria 3168, 2Monash University, Clayton Victoria 3168
Introduction/Aim
The prevalence of Chronic Obstructive Pulmonary Disease (COPD) using spirometry cirteria has been extensively studied, however little evidence exists for the usefulness of Transfer Factor for carbon monoxide (TLCO) in the diagnosis and classification of COPD. The guidelines for the Global Initiative for Chronic Obstructive Lung Disease (GOLD) currently utilise spirometry predominately to aid a physician‐diagnosis of COPD. Since only a relatively small proportion of smokers develop COPD, we aim to assess how TLCO can serve as a useful early biomarker for the detection of lung disease in younger smokers with normal spirometry.
Methods
We performed a cross‐sectional analysis of subjects who have had both spirometry and TLCO measured at the Respiratory Laboratory at Monash Lung & Sleep, Monash Health. Subjects included male and females aged 40 to 60 years with normal spirometry and at least 10 pack‐years smoking history.
Results
One hundred and six subjects aged between 40 and 60 with normal spirometry and significant smoking histories were identified. Of this cohort, 77 subjects (73% of the group) had a TLCO below their lower limit of normal (using ATS criteria). The cohort was equally divided into 53 males (of whom 33 had a low TLCO) and 53 females (of whom 43 had a low TLCO)
Conclusion
A low transfer factor for carbon monoxide (TLCO) is prevalent amongst younger smokers with normal spirometry. This low TLCO may be an important early indicator of potential lung damage in COPD.
Grant Support
TO‐107: Self‐management interventions including COPD exacerbation action plans improve hospitalisation rate and health‐related quality of life – a Cochrane review
Anke Lenferink 1–3 , Marjolein Brusse‐Keizer1, Paul van der Valk1, Peter Frith3,4, Marlies Zwerink1, Evelyn Monninkhof5, Job van der Palen1,2, Tanja Effing3,4
1Department of Pulmonary Medicine, Medisch Spectrum Twente, Enschede, the Netherlands, 2 Department of Research Methodology, Measurement, and Data‐Analysis, Behavioural Sciences, University of Twente, Enschede, the Netherlands, 3 School of Medicine, Flinders University, Adelaide, Australia, 4 Department of Respiratory Medicine, Repatriation General Hospital, Adelaide, Australia, 5 Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, the Netherlands
Introduction/Aim
Exacerbation action plans are considered as a key component of a COPD self‐management intervention. Studies of these interventions show contradictory results. In this systematic Cochrane review, we have assessed the effectiveness of COPD self‐management interventions that include exacerbation action plans compared to usual care.
Methods
After a literature search, full‐text articles were independently assessed by two authors. Study inclusion criteria were: randomised controlled trials published from 1995–May 2015; self‐management interventions that included a written action plan for COPD exacerbations; and an iterative process between patient and healthcare provider.
Results
Of 1,633 identified records, 22 studies were included with follow‐up times between two and 24 months. Statistically significant beneficial effects of self‐management were detected on health‐related quality of life (St George's Respiratory Questionnaire total score, mean difference −2.69 (95% CI −4.49 to −0.90), 10 studies, 1,799 participants, I2: 46%) and respiratory‐related hospitalisations (OR 0.69 (95% CI 0.51 to 0.94), 14 studies, 3,157 participants, I2: 57%). Furthermore, a borderline significant trend towards fewer all‐cause hospitalisations (OR 0.74 (95% CI 0.54 to 1.03), 10 studies, 2,467 participants, I2: 62%) was observed. No effects on all‐cause mortality were found (risk difference 0.00 (95% CI −0.02 to 0.03), 16 studies, 3,296 participants, I2: 48%).
Conclusion
Self‐management interventions that include a COPD exacerbation action plan are associated with better health‐related quality of life and lower probability of respiratory‐related hospitalisations. No excess all‐cause mortality risk was observed.
Grant Support
Lung Foundation Australia / Cochrane Airways Australia Scholarship 2016, Lung Foundation Netherlands (grant number 3.4.11.061).
Interventional Pulmonary / Bronchology 1
TO‐108: EBUS TBNA pre‐surgical staging highlights the importance of confirming cytological negativity in cases of technically N3 NSCLC on PET
Eric Douglas1, Geoffrey Fanning2, Farzad Bashirzadeh3, Alexander Ritchie4, Justin Hundloe5, David Fielding6
1‐ 6Department of Respiratory Medicine, Royal Brisbane and Women's Hospital, Queensland, Australia
Introduction/Aim
Following radical treatment of non‐small cell lung cancer (NSCLC), surveillance is recomended. Endobronchial ultrasound and transbronchial needle aspirate (EBUS‐TBNA) has emerged as a bronchoscopic modality for sampling pulmonary lymph nodes detected on surveillance imaging. Previous treatments that patients have received may make reinterpretation of their imaging, and perhaps bronchoscopic lymph node sampling difficult.
Method
We performed an single‐centre audit of all patients who underwent EBUS‐TBNA to investigate abnormal CT lymph node appearance following radical treatment for NSCLC from 2005 to 2015. A combination of bronchoscopy reports, pathology reports, imaging reports and chart reviews were used to identify patient information.
Results
Overall, 47 cases were identified. The median duration between treatment and re‐biopsy was 30.5 months. PET scans were performed in 57.4% of patients and of those the pulmonary lymph nodes were the sole sites of metastases in 74.1% of cases. The nodes sampled were N1 (34.0%), N2 (72.3%) and N3 (2.1%). The frequency of TBNA samples positive for malignancy was 78.7%. The frequency of biopsies positive for malignancy post surgery was 89.2%, post chemoradiation 50% and post radiation alone 33.3%. Patients with samples positive for malignancy went on to have a change in their treatment in 51.4% of cases. Of those, 72.2% received chemotherapy, 38.9% received radiation and 11.1% received surgery.
Conclusion
EBUS‐TBNA has a very high yield in detecting regional lymph node recurrence of disease in the post radical treatment setting. Additionally, the regional lymph nodes were frequently the only readily available biopsy target. The yield of positive biopsies was higher in this case series in surgical patients compared to chemoradiotherapy and radiation. EBUS‐TBNA allowed for a change in management in a significant number of patients.
Key Words
EBUS‐TBNA, endobronchial ultrasound
Nomination for New Investigator Award: N/A
Grant Support
Nil
Declaration of Interest
There were no competing interests in this study.
TO‐109: A novel management of distal active haemoptysis by an intrabronchial valve and TISSEEL
Pan C.J1 , Arnold D.J5 , Ing A.J,1,3,4 and Saghaie T1 ,2,3,4
1Department of Thoracic Medicine, Concord Repatriation General Hospital, Concord, NSW, 2 Bankstown Hospital, Bankstown, NSW, 3 Faculty of Medicine and Health Sciences, Macquarie University Hospital, NSW, 4 Sydney Medical School, University of Sydney, 5 John Hunter Hospital, New Lambton Heights NSW
Introduction
TISSEEL (combination of synthetic aprotinin, factor VIII and fibrinogen combined with Thrombin) is a fibrin sealant indicated for use as an adjunct to haemostasis in patients undergoing surgery when control of bleeding by conventional surgical techniques is ineffective or impractical. It is widely used in general surgical procedures but remains a non‐standard approach in the management of haemoptysis.
There have been recent case reports describing its effective usage in massive haemoptysis where other techniques such as bronchial embolisation, bronchoscopic suctioning or surgical resection have failed or may be ineffective. However, when TISSEEL is used independently endoscopially, migration, dislodgment or even expectoration of the fibrin clot is a common complication that leads to recurrence of haemoptysis.
We present the first ever reported case of successful endobronchial use of TISSEEL in controlling active distal bronchial bleeding. A 67 year old lady suffering from ongoing haemoptysis secondary to recurrent non small cell lung cancer involving lateral segment of left lower lobe (LB9) underwent therapeutic bronchoscopy utilising a therapeutic video scope (Olympus T180) introduced via a rigid bronchoscope which provided secure airway access. After identifying the source of bleeding, 1ml of TISSEEL was injected into distal LB9. A size 6 Spiration IBV was then inserted to add stability and prevent expectoration of the fibrin clot. A further 1 mL of TISSEEL was then injected proximally on top of the valve. There was excellent seal after the procedure with resolution of bleeding.
Conclusion
The combination of TISSEEL and an endobronchial valve provides a safe and effective therapeutic option for the medium term control of distal bronchial bleeding secondary to malignancy.
Grant Support
Nil
TO‐110: Endobronchial valve insertion outcomes for emphysema: a retrospective analysis in a local public health network.
Sarkar P1 , Tee V1 , Jersmann H1 ,2, Grosser D3 , Lorraine B1 , Chew G 1, Nguyen P1
1Department of Thoracic Medicine, Royal Adelaide Hospital, SA, Australia, 2 The University of Adelaide, SA, Australia, 3 Department of Respiratory Medicine, The Queen Elizabeth Hospital, SA, Australia
Introduction/Aim
Lung volume reduction (LVR) with endobronchial valves (EBV) for severe emphysema has established evidence demonstrating subjective and objective clinical response. In Australia, the majority of these procedures are funded and performed in the private sector. In this audit, we assessed a cohort of patients treated in a public hospital setting after the implementation of a publically funded LVR‐EBV program.
Methods
Patients were selected from established criteria by a multidisciplinary team.10 patients underwent EBV insertion in the first 18 months of this program. One patient who did not have complete post procedure lung function was excluded. The change in residual volume (RV), total lung capacity (TLC) and relative change in FEV1 was calculated for each patient from testing done prior to EBV insertion compared to three month post procedure follow up. Minimally clinically important differences (MCID) were used to assess for objective response. Patients also underwent clinical review to ascertain for any subjective change in wellbeing.
Results
There was a relative increase in mean FEV1 by 16.2% (p<0.05), a decrease in mean residual volume by 600mls (p<0.05) and a decrease in mean TLC by 540 mls (p<0.05) following EBV insertion. With regards to minimally clinically important differences, 55.6% of the patient cohort had a greater than 430mls volume reduction in their RV whereas 66.7% of the patient cohort had a relative increase in their FEV1 by more than 10%. One patient had a pneumothorax following valve insertion and one of nine patients had valve migration that required repositioning. All of the patients had a subjective response in their first clinical review post valve insertion with one patient no longer requiring home oxygen.
Conclusion
Our audit demonstrated both a subjective and objective benefit of EBV insertion for carefully selected patients with symptomatic emphysema on best current management. Such a program can be successful in a public hospital setting with local support.
Grant Support
Nil
TO‐111: EBUS TBNA sampling of regional lymph nodes as a substitute for biopsy for concomitant pulmonary nodules; strong supportive evidence of primary lung cancer from EBUS TBNA sample immunohistochemistry and PET
Geoffrey Fanning1, Eric Douglas1, Farsad Bashirzadeh1, Justin Hundloe1, Alex Ritchie1, David Fielding1
1Department of Thoracic Medicine, Royal Brisbane and Women's Hospital, Queensland, Australia
Introduction/Aim
A peripheral lung nodule with hilar or mediastinal nodes is an opportunity for single biopsy (EBUS TBNA alone) to give diagnosis and staging. This avoids subsequent procedures to confirm nodal metastasis.
Methods
A single‐centre audit of medical records of all patients who underwent EBUS‐TBNA of hilar or mediastinal lymph nodes as a diagnostic procedure for a peripheral lung lesion from 2007 to 2015 at the Royal Brisbane and Women's Hospital, Brisbane, Australia. Patients with a distant metastasis were excluded.
Results
There were 194 cases of EBUS TBNA, 157 (81%) were diagnostic of malignancy. 30 patients had malignancy diagnosed at a subsequent procedure. No side effects of EBUS TBNA were observed.
Table 1. Method of diagnosis of malignancy
| Procedure | Cases (N=187) |
|---|---|
| EBUS TBNA | 157 (84%) |
| Surgery | 10 (5%) |
| Endobronchial ultrasound guide sheath | 7 (4%) |
| CT guided fine needle aspiration | 5 (3%) |
| Repeat EBUS TBNA | 5 (3%) |
| Other | 3 (1%) |
Table 2. Malignancy types diagnosed at EBUS TBNA
| Subtype | Cases |
|---|---|
| Primary lung adenocarcinoma (Supportive immunohistochemistry in 85% and morphological appearance in 15%) | 61 (39%) |
| Squamous cell carcinoma | 29 (18%) |
| Mesothelioma | 2 (1%) |
| Small cell lung cancer and neuroendocrine carcinoma | 32 (20%) |
| Immunohistochemically confirmed metastasis from other sites | 6 (4%) |
| Non small cell lung carcinoma, not otherwise specified (NSCLC NOS) | 27 (18%) |
Of the 27 cases of NSCLC NOS, 23 patients underwent a PET scan, all of which were reported to be consistent with a primary lung lesion with nodal metastasis. All malignancy cases were discussed at a multidisciplinary case conference.
Conclusion
In patients who have a peripheral lung nodule and hilar or mediastinal lymph node enlargement, EBUS TBNA is an effective method of providing both diagnosis and staging, avoiding additional procedures. The use of combination pathology and PET gives convincing evidence between the nodal disease and peripheral lung lesion.
Grant Support
Nil
TO‐112: Texture analysis using unconstrained regions of interests from radial EBUS images can help predict malignant aetiology
Badiei A, Nguyen P, Jersmann HPA, and Wong MX
Department of Thoracic Medicine, Royal Adelaide Hospital, Adelaide, South Australia
Introduction/Aim
Analysis of grey‐scale texture features from lesions identified on radial endobronchial ultrasound (EBUS) images can characterise benign versus malignant aetiologies1. Previously reported analyses with expert defined region‐of‐interest (ROI) correctly classified 76.8% of lesions with a positive predictive value (PPV) of 75%1. However, the main limitation of that study was the restricted ROI to a maximum 32x32 pixels. The aim of this study was to assess whether unconstrained ROI selection, resulting in a larger portion of the lesion being analysed, would improve results.
Methods
Radial EBUS images (n=84) from the prediction set of Nguyen et al's study were utilised. Using custom written image analysis software, an expert physician identified an unconstrained, polygonal ROI. From this the following grey‐scale features were calculated: mean, maximum, minimum, maximum ‐ minimum, standard deviation, entropy, contrast, correlation, energy, and homogeneity. Mann–Whitney U tests were used to compare features. Receiver‐operating characteristic (ROC) curves were generated and optimal cut‐off points determined for malignant versus benign differentiation. The sensitivity, specificity, accuracy, and PPV were calculated.
Results
There were 46 malignant and 38 benign cases. Five grey‐scale texture features (maximum, maximum ‐ minimum, mean, standard deviation, entropy) were significantly different between malignant and benign groups. Maximum, maximum ‐ minimum, and standard deviation had area‐under ROC curves of 0.85, 0.8, and 0.74, respectively. At optimal cut‐off values: maximum pixel value had 78% sensitivity, 87% specificity and 88% PPV for malignancy; maximum ‐ minimum pixel value had 67% sensitivity, 84% specificity and 84% PPV and standard deviation had 84% sensitivity, 74% specificity and 76% PPV. Maximum grey‐scale pixel value had the highest diagnostic accuracy (82%).
Conclusion
Grey‐scale texture analysis of radial EBUS images using unconstrained ROI, which is less expert dependent, can characterise lesions as benign or malignant with relatively good sensitivity, specificity and PPV. Formal validation series are pending.
Grant Support
Nil
Reference
Nguyen, P. et al, Respirology, 2015, 20, 960 – 966
TO‐113: Pre operative EBUS TBNA pre‐surgical staging highlights the importance of confirming cytological negativity in cases of technically n3 disease on pet scans
Eric Douglas1, Geoffrey Fanning2, Farzad Bashirzadeh3, Alexander Ritchie4, Justin Hundloe5, David Fielding6
1‐ 6Department of Respiratory Medicine, Royal Brisbane and Women's Hospital, Queensland, Australia
Introduction/Aim
Endobronchial ultrasound and transbronchial needle aspirate (EBUS‐TBNA) and Positron Emission Tomography (PET) have emerged as common modalities of staging pulmonary lymph nodes in non‐small cell lung cancer (NSCLC). The findings of PET scans are often limted by factors such as infection, inflammation, or dust inhalation. As such, bilateral pulmonary lymphadenopathy in patients with known small cell lung cancer is frequently not representative of their true lymph node stage.
Method
We performed an single‐centre audit of all patients with known NSCLC who had a PET scan and also underwent EBUS‐TBNA for the explicitly stated purpose of pulmonary lymph node staging from 2005–2015. A combination of bronchoscopy reports, pathology reports, imaging reports and chart reviews were used to identify patient information.
Results
Overall, 40 cases were identified; 4 were excluded due to incomplete collection of date. Of these, PET demonstrated 12 cases of low to intermediate grade bilateral lymph node uptake, 22 cases of unilateral lymph node uptake and two cases of no PET uptake. Of cases with bilateral uptake, there were no cases in which EBUS‐TBNA sampling was positive for malignancy. Two cases (9%) were subsequently upstaged to positive nodal involvement when they underwent surgery. Of cases with unilateral nodal involvement on PET scan, the frequency of biobsies positive for malignancy on both EBUS‐TBNA, and on those who subsequently underwent surgery was 50%. Dust inhalation was seen on biopsy specimens of 41.7% of patients with bilateral PET uptake and 13.6% of patients with unilateral PET uptake.
Conclusion
This case series also adds to the growing body of evidence of dust inhalation associated with PET positivity. Although symmetrical uptake on PET scanning technically represents N3 disease, both EBUS‐TBNA and surgery demonstrate a low rate of positive lymph node metastases. This highlights the role of EBUS‐TBNA to rule patients in for surge, rather than be excluded by PET findings alone.
Key Words
EBUS‐TBNA, endobronchial ultrasound
Grant Support
Nil
Declaration of Interest
There were no competing interests in this study.
OLIV 2
TO‐114: Predicting life expectancy for pirfenidone and best supportive care in IPF (Encore)
Mark Fisher,1 Toby M Maher,2 Steven D Nathan,3 Christian Hill,4 Jade Marshall,4 Fred Dejonckheere,5 Per‐Olof Thuresson,5 Nitya Mathew6
1FIECON, St Albans, UK, 2 Interstitial Lung Disease Unit, Royal Brompton Hospital/Imperial College London, London, UK, 3 Advanced Lung Disease & Transplant Program, Inova Fairfax Hospital, Falls Church, VA, USA, 4 MAP BioPharma, Cambridge, UK, 5 Roche, Basel, Switzerland, 6 Genentech, San Francisco, CA, USA
Introduction/Aim
Clinical trials in IPF are not designed to estimate long‐term survival. This analysis used a survival model to predict life expectancy for patients with idiopathic pulmonary fibrosis (IPF) receiving pirfenidone or best supportive care (BSC).
Methods
Life expectancy was estimated by the area under the curve of parametric survival distributions fit to Kaplan‐Meier survival data from clinical studies and IPF registries. Kaplan‐Meier survival data for pirfenidone were derived from clinical studies (CAPACITY, ASCEND, RECAP). Kaplan‐Meier survival data for BSC were obtained from two independent registries of patients with IPF: the Inova Fairfax Hospital database (n=815) and the National Jewish Health Interstitial Lung Disease (NJH‐ILD) database (n=321). The best‐fitting distributions were chosen by statistical consideration, visual inspection of the fitted curve and by clinical interpretation. To account for differences between patients enrolled in the clinical trials and the registries, covariate adjustment using propensity scores was used.
Results
Mean life expectancy (95% confidence intervals) was calculated as: 8.7 years (7.7, 10.2) with pirfenidone; 5.9 years (5.1, 6.9) with BSC (Inova); and 6.1 years (5.7, 6.5) with BSC (NJH‐ILD). Therefore, pirfenidone improved life expectancy relative to BSC by 2.8 years and 2.6 years as measured by the Inova and NJH‐ILD registries, respectively.
Conclusion
The survival model suggests that pirfenidone significantly improves life expectancy compared with BSC by almost 3 years in patients with IPF. Although these findings are based on cross‐trial comparisons, they provide support for pirfenidone as an effective treatment option for IPF.
Grant Support
Funded by InterMune International AG, which became a wholly owned subsidiary of F. Hoffmann‐La Roche Ltd. in 2014.
TO‐115: Long‐term treatment with nintedanib in patients with idiopathic pulmonary fibrosis: an update from INPULSIS®‐ON
Lauren Troy1on behalf of Bruno Crestani2, Manuel Quaresma3,4, Mitchell Kaye5, Wibke Stansen4, Susanne Stowasser4, Michael Kreuter3
1Royal Prince Alfred Hospital, Sydney, Department of Respiratory Medicine, Missenden Rd Camperdown, NSW, Australia, 2 Hôpital Bichat, Pneumologie, Paris, France, 3 Department of Pneumology, Thoraxklinik, University of Heidelberg, and Translational Lung Research Center Heidelberg, German Center for Lung Research Germany, 4 Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany, 5 Minnesota Lung Center, Ltd., Minneapolis, Minnesota, USA
Introduction/Aim
The INPULSIS® trials assessed the efficacy and safety of nintedanib in patients with idiopathic pulmonary fibrosis (IPF). Patients who completed the 52‐week treatment period and follow‐up visit 4 weeks later in INPULSIS® could receive open‐label nintedanib in INPULSIS®‐ON. Our aim was to assess the long‐term efficacy and safety of nintedanib in INPULSIS®‐ON based on a data snapshot in October 2015.
Methods
Patients treated with placebo in INPULSIS® initiated nintedanib in INPULSIS®‐ON; patients treated with nintedanib continued nintedanib.
Results
734 patients were treated in INPULSIS®‐ON (430 continuing nintedanib; 304 initiating nintedanib). Baseline characteristics were similar between groups. Mean (SD) exposure in INPULSIS®‐ON was 22.9 (10.9) months. Mean (SD; minimum–maximum) total exposure for patients treated with nintedanib in INPULSIS® and continuing nintedanib in INPULSIS®‐ON was 35.7 (10.5; 11.9–51.1) months. In INPULSIS®, mean (SD) change in FVC from baseline to week 52 was −89 (264) mL in the nintedanib group and −203 (293) mL in the placebo group. For patients treated with nintedanib in both INPULSIS® and INPULSIS®‐ON, mean (SD) change in FVC was −96 (237) mL from baseline to week 48 of INPULSIS®‐ON and −124 (248) mL from week 48 to week 96 of INPULSIS®‐ON. The adverse event profile of nintedanib in INPULSIS®‐ON was similar to that in INPULSIS®.
Conclusion
A recent data snapshot from INPULSIS®‐ON indicated that the effect of nintedanib on reducing disease progression observed in INPULSIS® was maintained over long‐term treatment. Nintedanib treatment (up to 51 months) had an acceptable safety and tolerability profile with no new safety signals identified.
Grant Support
The study was funded by Boehringer Ingelheim.
Declaration of Interest Statement
LT has been involved with clinical trials conducted by Boehringer‐Ingelheim, Intermune, Roche, Medamune, Merck and Bayer and has also received a speaker's fee from Boehringer‐Ingelheim for presenting at the Airways Conference in 2016. BC received of grants, personal fees and non‐financial support from Roche/InterMune and Boehringer Ingelheim; personal fees and non‐financial support from Sanofi; grants from Cardif, LVL and MedImmune, and personal fees from AstraZeneca. MQ, WS and SS are employees of BI. MKaye has no financial disclosures. MKreuter received fees for speaking and/or organising education from ERS, Almirall, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, GlaxoSmithKline, InterMune, Novartis, NYCOMED, Pfizer, and Roche and consulting fees from Boehringer Ingelheim, InterMune, GlaxoSmithKline, and Roche.
TO‐116: Twenty‐four week decline in FVC predicts mortality at week 52 in the INPULSIS ® trials
Tamera Corte1 on behalf of Luca Richeldi2, Arata Azuma3, Moisés Selman4, Wenbo Tang5, Jorge Capapey6, Susanne Stowasser 6, Vincent Cottin7
1Respiratory Medicine, Royal Prince Alfred Hospital, Missenden rd, Camperdown 2050, NSW, Australia, 2 National Institute for Health Research Southampton Respiratory Biomedical Research Unit and Clinical and Experimental Sciences, University of Southampton, Southampton, UK, 3 Department of Pulmonary Medicine and Oncology, Graduate School of Medicine, Nippon Medical School, Tokyo, Japan, 4 Instituto Nacional de Enfermedades Respiratorias, Mexico City, Mexico, 5 Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, Connecticut, USA, 6 Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany, 7 Louis Pradel Hospital, Claude Bernard University Lyon 1, Lyon, France
Introduction/Aim
In Phase III INPULSIS® trials, a significantly lower proportion of patients with idiopathic pulmonary fibrosis treated with nintedanib vs placebo had disease progression with absolute FVC decline of ≥5% or ≥10% predicted at week 52. We explored the impact of FVC change over 24 weeks on subsequent FVC decline and mortality.
Methods
Post‐hoc descriptive analysis of proportions of patients with absolute FVC declines of <5%, ≥5%,or ≥10% predicted from baseline to week 24 and changes in FVC% predicted and mortality between weeks 24 and 52 in these groups conducted using pooled data from both INPULSIS® trials.
Results
1061 patients (nintedanib 638, placebo 423) were included. FVC decline of ≥5% or ≥10% predicted from baseline to week 24 did not predict FVC decline of ≥5% or ≥10% predicted, respectively, from week 24 to 52. The proportion of patients who died between weeks 24 and 52 increased with increasing FVC decline from baseline to week 24. Among patients with FVC declines of ≥5% or ≥10% predicted from baseline to week 24, more patients treated with nintedanib vs placebo had no further decline or an increase in FVC between weeks 24 and 52.
Conclusion
FVC declines of ≥5% or ≥10% predicted in the first 24 weeks did not predict FVC decline but were associated with higher mortality in the following 24 weeks.
| Absolute FVC decline % predicted from baseline to week 24 | Outcome between weeks 24 and 52 | Nintedanib n(%) | Placebo n(%) |
|---|---|---|---|
| <5% | n | 444 | 259 |
| Increase/no decline in FVC% predicted | 155(34.9) | 55(21.2) | |
| FVC decline ≥5% predicted | 133(30.0) | 110(42.5) | |
| Death | 8(1.8) | 6(2.3) | |
| ≥5% | n | 143 | 136 |
| Increase/no decline in FVC% predicted | 56(39.2) | 47(34.6) | |
| FVC decline ≥5% predicted | 48(33.6) | 41(30.1) | |
| Death | 11(7.7) | 14(10.3) | |
| ≥10% | n | 46 | 53 |
| Increase/no decline in FVC% predicted | 24(52.2) | 21(39.6) | |
| FVC decline ≥10% predicted | 9(19.6) | 10(18.9) | |
| Death | 5(10.9) | 7(13.2) |
Grant Support
The study was funded by Boehringer Ingelheim.
Declaration of Interest Statement
TC received unrestricted educational grants, travel assistance and served on an advisory board for Boehringer Ingelheim and Roche Products Ltd, received unrestricted educational grants from Intermune Pharmaceuticals, and served on an advisory board for Astra Zeneca. LR served on the scientific advisory boards of InterMune, Boehringer Ingelheim, FibroGen, GlaxoSmithKline, Sanofi‐Aventis, Anthera, Genentech, MedImmune, Takeda, UCB, and Promedior and as a trial Principal Investigator for Boehringer Ingelheim, InterMune, Gilead, Roche, Takeda, and UCB; received research grants from InterMune, Biogen, Italian Ministry of Health, Italian National Drug Agency, and Wellcome Trust and speaker's fees from InterMune, Boehringer Ingelheim, and Cipla. AA is a member of Advisory Boards for Boehringer Ingelheim and Shionogi & Co., Ltd, and is on the nintedanib in IPF Steering Committee for Boehringer Ingelheim. MS is a member of a steering committee and consultant for Boehringer Ingelheim. WT, JC and SS are employees of Boehringer Ingelheim. VC received honoraria for consulting or participating in advisory board meetings or steering committee meetings from Actelion, Bayer, Boehringer Ingelheim, Gilead, GlaxoSmithKline, InterMune/Roche Promedior, and Sanofi.
TO‐117: Biomarkers can predict disease progression in Idiopathic Pulmonary Fibrosis: Analysis from the Australian IPF Registry.
Helen E Jo1,2*, Tamera J Corte1,2, Ian Glaspole3,4, Christopher Grainge5, Nicole Goh3,6, Peter MA Hopkins7, Paul N Reynolds8, Sally Chapman8, E Haydn Walters9, Christopher Zappala10, Heather Allan11, Gregory J Keir12, Andrew Hayen13, Wendy A Cooper14, Annabelle M Mahar14, Samantha Ellis15, Sacha Macansh11, Yuben Moodly16
1Department of Respiratory Medicine, Royal Prince Alfred Hospital, Sydney, NSW; Australia, 2 Faculty of Medicine, University of Sydney, Sydney, NSW; Australia, 3 Department of Allergy and Respiratory Medicine, The Alfred Hospital, Melbourne, VIC; Australia, 4 Faculty of Medicine, Monash University, Melbourne, VIC; Australia, 5 Department of Respiratory Medicine, John Hunter Hospital, Newcastle, NSW; Australia, 6 Department of Respiratory Medicine, Austin Hospital, VIC; Australia, 7 School of Medicine, University of Queensland, Brisbane, QLD; Australia, 8 Department of Respiratory Medicine, Royal Adelaide Hospital, Adelaide, SA; Australia, 9 University of Tasmania, Hobart, TAS; Australia, 10 Department of Thoracic Medicine, Royal Brisbane & Women's Hospital, Brisbane, QLD; Australia, 11 Lung Foundation Australia, Brisbane, QLD; Australia, 12 Department of Respiratory Medicine, Princess Alexandra Hospital, Brisbane, QLD; Australia, 13 University of Technology, Sydney, Australia, 14Tissue pathology and diagnostic oncology, Royal Prince Alfred Hospital, Sydney, NSW; Australia, 15Department of Radiology, The Alfred Hospital, VIC; Australia, 16Department of Respiratory Medicine, Fiona Stanley Hospital, Perth, WA; Australia
Introduction/Aim
The natural history of patients with idiopathic pulmonary fibrosis (IPF) is highly variable and difficult to predict. With the advent of new treatments that slow disease progression, there is growing interest in the potential of biomarkers as a method of differeniating rapidly progressive from more stable IPFdisease.
Methods
The Australian IPF Registry is linked to a biobank where the blood of a sub‐population of patients are stored for analysis. Using this blood we analysed a panel of 11 plasma proteins thought to be important in IPF pathogenesis: ICAM1, OPNp, MMP7, CXCL13, FBLN1, SPA, MUC1, VCAM1, ENRAGE, IL8, CRP. The plasma protein concentrations were measured using the ELISA technique. Multivariate Cox analysis adjusted for baseline demographic features (age, gender, smoking, BMI) and disease severity (FVC%predicted) was used to determine the effect of these biomarkers in predicting mortality and progression free survival (PFS). PFS was defined as death, or fall in FVC≥10% or DLco≥15% from baseline.
Results
170 participants (Age 68.4±8.2, 74% male, FVC 81.7±19.3) had blood available for analysis. The median concentrations were (ng/mL): ICAM1 298.9, OPNp 384.75, MMP7 2.8, CXCL13 0.045, FBLN1 60772.5, SPA 223.5, MUC1 0.27, VCAM1 1531, ENRAGE 78.9, IL8 0.063, CRP 7261.4. There were too few particpants with measurable IL8 and MUC1 for further analysis. Higher conentrations of ENRAGE (HR 1.01, 95%CI 1.00‐1.01, p=0.013), SPA (HR1.01, 95%CI 1.00‐1.02, p=0.007) and OPNp (HR 1.02, 95%CI 1.00‐1.04, p=0.01) were associated with increased mortality whereas higher OPNp (HR 1.01, 95%CI 1.00‐1.02, p=0.029) and ICAM1 (HR 1.00, 95%CI 1.00‐1.004, p=0.05) levels were associated with shorter progression free survival.
Conclusion
Biomarkers have a potential role in predicting mortality and disease progression in IPF.
Grant Support
TO‐118: Effect of continued pirfenidone treatment following ≥15% decline in 6MWD in IPF patients‐pooled analysis (encore)
Steven Nathan,1 Carlo Albera,2 Ulrich Costabel,3 Ian Glaspole,4 Marilyn Glassberg,5 Lisa Lancaster,6 David Lederer,7 Carlos Pereira,8 Jeffrey Swigris,9 Andrey Pavlov,10 John Stauffer,11 Bann‐Mo Day,11 Willis Chou,11Athol Wells12
1Inova Fairfax Hospital, Falls Church, VA, USA, 2 University of Turin, Turin, Italy, 3 Ruhrlandklinik, University of Duisburg‐Essen, Essen, Germany, 4 Alfred Hospital, Melbourne, Australia, 5 University of Miami Miller School of Medicine, Miami, FL, USA, 6 Vanderbilt University Medical Center, Nashville, TN, USA, 7 Columbia University Medical Center, New York, NY, USA, 8 Paulista School of Medicine, Federal University of São Paulo, São Paulo, Brazil, 9 National Jewish Health, Denver, CO, USA, 10 Everest Clinical Research, Markham, Canada;, 11 Genentech, Inc., South San Francisco, CA, USA, 12 Royal Brompton Hospital, London, UK
Introduction/Aim
Previous analyses of patients with idiopathic pulmonary fibrosis (IPF) receiving pirfenidone showed that continued treatment following a ≥ 10% absolute or relative decline in percent predicted forced vital capacity (FVC) or hospitalization during the first 6 months of treatment provided a benefit during the subsequent 6 months. The aim is to further explore the potential benefit of continued pirfenidone treatment in patients with IPF who had a worsening of 6‐minute walk distance (6MWD) within the first 6 months of treatment.
Methods
A pooled analysis included all patients randomized to pirfenidone 2403 mg/d or placebo in the ASCEND and CAPACITY studies (N = 1247). All patients who had a 6MWD decline ≥ 15% within the first 6 months of study treatment were selected. FVC, 6MWD, mortality and hospitalization outcomes were assessed during the subsequent 6‐month period.
Results
A total of 116/623 (18.6%) and 141/624 (22.6%) patients in the pooled pirfenidone and placebo groups, respectively, demonstrated a 6MWD decline ≥ 15% within the first 6 months of treatment. Outcomes during the subsequent 6 months of continued treatment in these patients are shown in the Table.
Conclusion
These results suggest that continued treatment with pirfenidone may confer a significant benefit to patients with IPF who experienced a 6MWD decline ≥ 15% within the first 6 months of treatment.
Grant Support
Supported by F. Hoffmann‐La Roche Ltd.

TO‐119: Annual rate of FVC decline in patients with IPF treated with pirfenidone: pooled analysis (encore)
Paul W. Noble,1 Carlo Albera,2 Willis Chou,3 Ulrich Costabel,4 Bann‐mo Day,3 Ian Glaspole,5 Marilyn K. Glassberg,6 Lisa Lancaster,7 David J. Lederer,8 Steven D. Nathan,9Carlos A. Pereira,10John Stauffer,3Jeffrey J. Swigris11
1Cedars‐Sinai Medical Center, Los Angeles, CA, USA, 2 University of Turin, Turin, Italy, 3 Genentech, Inc., South San Francisco, CA, USA, 4 Ruhrlandklinik, University of Duisburg‐Essen, Essen, Germany, 5 Alfred Hospital and Monash University, Melbourne, Australia, 6 University of Miami School of Medicine, Miami, FL, USA, 7 Vanderbilt University Medical Center, Nashville, TN, USA, 8 Columbia University Medical Center, New York, NY, USA, 9 Inova Fairfax Hospital, Falls Church, VA, USA, 10 Paulista School of Medicine, Federal University of São Paulo, São Paulo, Brazil, 11 National Jewish Health, Denver, CO, USA
Introduction/Aim
Pirfenidone has been shown to decrease the annual rate of decline in forced vital capacity (FVC) volume in patients with idiopathic pulmonary fibrosis (IPF). This analysis explored this effect in various patient subgroups.
Methods
Patients randomized to pirfenidone 2403 mg/d or placebo in the CAPACITY or ASCEND studies were included. The annualized rate of decline in FVC volume from baseline through 12 months was estimated using a mixed‐effects model, with study, time‐by‐treatment, age‐by‐sex and height‐by‐sex as fixed effects and patients and time‐by‐patient (slope) as random effects. The annual rate of FVC decline was estimated from the slope within the subgroups, defined by demographics and baseline disease activity measures.
Results
A total of 623 patients in the pirfenidone group and 624 in the placebo group were included in the pooled analysis. Overall, the adjusted annual rate (SE) of FVC decline from baseline to 12 months was −132.0 (12.4) mL for pirfenidone vs −223.5 (12.4) mL for placebo, a difference of 91.5 (16.4) mL. The annual rate of FVC decline favoured pirfenidone over placebo across various baseline demographic and lung function subgroups.
Conclusion
Patients with IPF treated with pirfenidone, regardless of baseline demographic or lung function, had a significantly lower annual rate of decline in FVC volume vs those treated with placebo after 12 months.
Grant Support
Funded by F. Hoffmann‐La Roche Ltd.
Physiology and Sleep 1
TO‐120: Determining regional (over)distension in the mechanically ventilated lung in vivo using a laboratory X‐ray source
Melissa H. Preissner1, Stephen Dubsky1, Richard Carnibella3, Chaminda R. Samarage3, Ellen Bennett2, Seiha Yen2, Graeme R. Zosky2, Andreas Fouras1
1Department of Mechanical and Aerospace Engineering, Monash University, Victoria, 2 School of Medicine, Faculty of Health, University of Tasmania, Tasmania, 3 4Dx Limited, Melbourne, Victoria
Introduction/Aim
Paradoxically, mechanical ventilation, which is a life‐saving strategy for acute respiratory distress syndrome (ARDS), can lead to ventilator‐induced lung injury (VILI) which can increase morbidity and mortality. Despite decades of research, progress in designing ventilation strategies to prevent VILI has been limited. This is in part due to our inability to assess regional responses to mechanical ventilation. The aim of this study was to use a novel non‐invasive X‐ray imaging approach to quantify regional responses to mechanical ventilation and explore the impact of tidal volume on regional heterogeneity in VILI.
Methods
BALB/c female mice were anaesthetised, surgically intubated and ventilated with either an injurious strategy (high tidal volume: 22.5 mL/kg, PIP: 20 cmH2O, PEEP: 0 cmH2O) or a protective strategy (low tidal volume: 10 mL/kg, PIP: 12 cmH2O, PEEP: 2 cmH2O) for 2 hours. The mice were imaged using a laboratory X‐ray source and acquisition was synchronised with the ventilator to obtain 4DCT images. The images were post‐processed using 3D X‐ray velocimetry combined with quantitative CT to obtain regional volume data (tidal volume and FRC) in situ.
Results
Qualitatively, the tissue expansion contours in the imaging data show substantial regional variation in tidal stretch in both groups in response to mechanical ventilation. Globally, after 2 hours of ventilation, for mice on the protective strategy, there was no significant change in tidal volume (−3 ±13% (SD); n = 8, p = 0.589) or FRC (−5 ±7% (SD); n = 8, p = 0.071). In contrast, mice on the injurious strategy had a decrease in tidal volume (−14 ±7% (SD); n = 6, p = 0.003), and a decrease in FRC (−25 ±5% (SD); n = 6, p < 0.001).
Conclusion
Preliminary results are promising and show a clear regional variation in distension for both ventilation groups. Quantitative data is possible on a regional (lobar or sub‐lobar) basis with this imaging technology and is the focus of ongoing work. The results of this investigation will lead to a better understanding of VILI, resulting in improved outcomes for critically ill patients requiring mechanical ventilation.
Grant Support
NHMRC grant number 1077905, Multimodal Australian ScienceS Imaging and Visualisation Environment (MASSIVE Project No. NCIy40).
TO‐121: The effect of high‐dose, high fine‐particle fraction combination therapy on ventilation heterogeneity in uncontrolled asthma
Francesca S.M Tang1, Catherine E. Farrow1, Joanna C. Watts1, Jessica R. Dame Carroll1, Amy Bertolin1, Cindy Thamrin1, Gregory G. King1
1Woolcock Institute of Medical Research, University of Sydney, NSW, Australia
Introduction/Aim
Both the large and small airways are important in severe asthma. However, their response to treatment with high‐dose, high‐fine particle fraction inhaled corticosteroid/long acting beta agonist (ICS/LABA) combination has yet to be established. We aimed to measure the effect of fluticasone/eformoterol on ventilation heterogeneity measured by multiple breath nitrogen washout and on clinical outcomes. In addition we aimed to determine predictors of improvements in conductive (Scond) and acinar (Sacin) ventilation heterogeneity. We hypothesised that changing to high‐dose fluticasone/eformoterol would improve Scond and Sacin, along with clinical improvement in asthma control.
Methods
21 patients (7 males) with a doctor diagnosis of asthma, were uncontrolled (5 component asthma control questionnaire score (ACQ5)>1.5) and were currently on ICS or ICS/LABA (maximum of 500μg/day fluticasone equivalent) were enrolled. Baseline Scond, Sacin, ACQ5, exhaled nitric oxide (FeNO), airway hyperresponsiveness (AHR) to methacholine (log10 dose response slope (log10DRS)), and spirometry were measured. Patients took 250/10μg ii bd of fluticasone/eformoterol via a spacer for 8 weeks before repeat testing. The relationship between changes in Scond and Sacin, and baseline ACQ5, AHR, spirometry and FeNO were examined.
Results
Treatment improved Scond (0.041±0.025 to 0.030±0.017L−1, p=0.002) and Sacin (0.127±0.079 to 0.104±0.067L−1, p=0.002). There were improvements in ACQ5 (2.11±0.85 to 1.11±0.85, p=0.0003), log10DRS (1.48±0.64 to 0.92±0.45%μmol−1, p<0.0001), FeNO (19.71±13.68 to 11.40±4.94ppb, p=0.001), FEV1 (83.61±14.92 to 89.78±14.7%predicted, p=0.007) and FVC (96.95±12.28 to 101.2±12.99%predicted, p=0.04). The improvements in Sacin and Scond were predicted only by baseline Sacin and Scond, respectively (r=0.54, p=0.01 and r=0.73, p=0.0002, respectively).
Conclusion
Fluticasone/eformoterol with high‐dose, high‐fine particle fraction improved ventilation heterogeneity, symptoms, AHR, airway inflammation and spirometry in people with uncontrolled asthma. Baseline Sacin and Scond were the only predictors for improvements in ventilation heterogeneity.
Grant Support
NHMRC project grant 103701, MundiPharma.
TO‐122: Heterogeneous bronchoconstriction in asthma on ventilation single photon emission computed tomography/computed tomography(VSPECT/CT) decreases after treatment
Catherine E FARROW 1, Francesca SM TANG1 ,Joanna C WATTS1 , Amir MEYBODY2 , Marco TRIFUNOVIC2 , Amy BERTOLIN 1, Jessica R DAME CARROLL 1, Gregory G KING 1,3
1Woolcock Institute of Medical Research and The University of Sydney, Australia., 2 Macquarie Medical Imaging, Macquarie University Hospital, Australia., 3 Department of Respiratory Medicine, Royal North Shore Hospital, Sydney, Australia.
Introduction/Aim
Areas of heterogeneous bronchoconstriction can be seen as low ventilation on functional lung imaging in asthma. A fundamental characteristic of asthma is airway hyperresponsiveness (AHR), which is associated with ventilation heterogeneity. AHR is slow to resolve with anti‐inflammatory treatment and the mechanism is poorly understood. The aim of this study was to determine if anti‐inflammatory treatment reduces heterogenous bronchoconstriction by measuring low ventilation areas on VSPECT/CT and investigating the role of peripheral airway heterogeneity in this mechanism.
Methods
Twenty‐one asthmatic subjects (13 female Mean ± SD Age: 31 ± 13 yrs, FEV1: 83 ± 16% Pred) had baseline and methacholine challenge VSPECT/CT scans, before and after 8 weeks of combined ICS/LABA treatment. Low ventilation was measured by changes in ventilated volume at two thresholds on VSPECT(80/50 ratio). Dose response slope (DRS) was calculated to measure AHR and is reported as logDRS. Multiple breath nitrogen washout was performed at baseline and after treatment to determine peripheral ventilation heterogeneity (Sacin). Results were analysed using paired t‐test and linear regression.
Results
Mean (Range) logDRS pre treatment(preT): 1.44 (0.57‐2.4) %.umol−1, logDRS post treatment (postT): 0.96 (0.48 – 1.9) %.umol−1p=0.001; 80/50 ratio preT: 0.05 (−0.01‐0.18), 80/50 ratio postT: 0.03 (−0.04‐0.18) p=0.02; Sacin preT: 0.128 (0.024‐0.375) L−1, Sacin postT: 0.104 (0.019‐0.334) L−1p=0.005. Improvement in 80/50 ratio with treatment correlated with preT logDRS (p=0.036, r=0.46) but not Sacin.
Conclusion
Anti‐inflammatory treatment reduces heterogeneous bronchoconstriction measured on functional lung imaging. The reduction in the development of low ventilation areas (after challenge) with treatment is predicted by pre‐treatment airway hyperresponsiveness. Peripheral heterogeneity improved with treatment but did not relate to imaging. Bronchoconstriction patterns on imaging are difficult to quantify but potentially could give valuable mechanistic insight for future treatment improvements.
Grant Support
NH&MRC Project Grant 103701 and MundiPharma
TO‐123: Evidence of persistent hyperventilation following high altitude exposure
Morris, N.R.1,2,3, Stewart, G.4, Carlson, A.4, Seale, H.3, Coffman, K.4, Wheatley, C.4, and B.D. Johnson.4
1Menzies Health Institute of Queensland and School of Allied Health Sciences, Griffith University, Southport, QLD. Australia, 2 Allied Health Research Collaborative. The Prince Charles Hospital. Brisbane. QLD., 3 Heart Lung Institute. The Prince Charles Hospital Brisbane. QLD. Australia, 4 Division of Cardiovascular Diseases, Mayo Clinic, Rochester MN. USA
Introduction/Aim
High altitude exposure results in acute hypoxia and an increase in the ventilatory drive. This hyperventilatory response is characterised by a worsening breathing efficiency (increased VE/VCO2) and a lower end tidal CO2 (PETCO2) both at rest and during exercise. Whilst the time‐course changes in the hyperventilatory response are well‐characteristed in acclimated climbers, to date there has been little or no examination of the response during ascent and on return from altitude in a large group of non‐acclimated climbers. The aim of the current study was to examine the changes in gas exchange measures in a group of non‐acclimated climbers during the ascent of Mt Kilimanjaro and immediately on return from altitude.
Methods
27 (age: 44±15, range 22‐66yrs) individuals ascended Mt Kilimanjaro during an 11‐day climb. Exercise testing (4‐minute step test with gas‐exchange) was completed on four occasions at the following altitudes: (1) basecamp, 1850m (PB=690 mmHg); (2) 3500m (PB=505 mmHg); (3) 4840m (PB=428 mmHg) and on return to base camp (4) 2850m (PB=690 mmHg).
Results
During the ascent subjects became increasingly hypoxic and there was a decrease in the nadir SpO2 during exercise (nadir SpO2(%): 1850m: 96±2; 3500m: 82±3; 4840m: 73±4). During exercise breathing efficiency worsened (VE/VCO2: 1850m: 28.5±2.9; 3500m: 35.8±4.6; 4840m: 50.7±5.8) and PETCO2 fell (PETCO2 mmHg: 1850m: 37.1±3.6; 3500m: 28.5±2.6; 4840m: 20.8±1.9) as subjects ascended. On return from altitude (2850m) SpO2 normalised (SPO2(%)=97±3 ), however there was persistent evidence of hyperventilation with both breathing efficiency and PETCO2 remaining abnormal during exercise (VE/VCO2: 32.8 +3.2, PETCO2,mmHg: 31.2+3.0; p<0.01 vs 1850m) and at rest.
Conclusion
With high altitude exposure there is an increased ventilatory drive. Following high altitude exposure and once SpO2 normalises, gas exchange remains altered. We hypothesise that this altered gas exchange may be due to a sustained alkalosis with the central chemoreceptors remaining reset to defend a lower PCO2 established during high altitude exposure.
TO‐124: Proximal & Peripheral Airway Response to Direct & Indirect Bronchial Provocation in Untreated Asthma
Mahesh Dharmakumara1, Chris Stuart‐Andrews1, Celia Zubrinich1, Bruce Thompson1
1Lung Function Laboratory, The Alfred Hospital, Melbourne, VIC 3181, Australia
Introduction/Aim
Spirometry is used to assess the degree of bronchoconstriction during bronchial provocation tests. However, little is known about how specific features of the proximal and peripheral airways respond to different provocation agents. This study aims to determine how the proximal and peripheral airway resistance, ventilation heterogeneity and nitric oxide levels change in the same airways in response to standard direct and indirect provocation agents relative to placebo.
Method
Newly diagnosed (untreated) patients with atopic Asthma were recruited for the study (n=9). All subjects demonstrated a clinically positive test using Spirometry to both direct (Methacholine) and indirect (Mannitol) provocation tests on separate visits, ~7days apart. On another visit, a placebo provocation was also performed. Before and immediately after all provocation tests, the following measures were made; airway resistance using the Forced Oscillation Technique, ventilation heterogeneity using Multiple Breath Nitrogen Washout technique and nitric oxide flux and alveolar concentrations using the Multiple Exhalation Flow technique.
Results
All data expressed as mean ± SEM. *p<0.05 with respect to placebo change.
| Measure | Units | Change Post Provocation | |||
|---|---|---|---|---|---|
| Placebo | Direct | Indirect | |||
| FEV1 | L | −0.151±0.036 | −0.826±0.081* | −0.651±0.075* | |
|
Proximal Airways |
R16 | hPa/(L/sec) | +0.094±0.156 | +0.990±0.266* | +0.713±0.160* |
| Scond | 1/L | −0.003±0.003 | +0.024±0.006* | +0.025±0.004* | |
| NO‐Flux | nL/sec | −0.394±0.097 | −0.654±0.193 | −2.075±0.521* | |
|
Peripheral Airways |
R4‐R16 | hPa/(L/sec) | +0.261±0.166 | +2.703±0.506* | +2.260±0.611* |
| Sacin | 1/L | +0.013±0.013 | +0.041±0.008 | +0.054±0.010 | |
| CANO | ppb | +1.225±0.842 | −0.942±0.342 | −3.083±1.781* | |
Conclusion
In the proximal airways, both resistance and heterogeneity increased in response to direct and indirect provocation relative to placebo. However, nitric oxide flux decreased only in response to the indirect agent. In the peripheral airways, heterogeneity remained unchanged. Peripheral resistance increased in response to both direct and indirect provocation. However, alveolar nitric oxide levels decreased only in response to the indirect agent.
Support
Australia and New Zealand Society of Respiratory Science. Pharmaxis.
Chronic Obstructive Pulmonary Disease 3
TO‐125: Complex medication regimens in chronic obstructive pulmonary disease (COPD) are associated with disease severity and comorbidities
Netsanet A. Negewo1, Peter G. Gibson1,2, Peter A.B. Wark1,2, Jodie L. Simpson1, Vanessa M. McDonald1 ,2,3
1Priority Research Centre for Healthy Lungs and Hunter Medical Research Institute (HMRI), The University of Newcastle (UoN), New South Wales, Australia., 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, New South Wales, Australia., 3School of Nursing and Midwifery, UoN, New South Wales, Australia.
Introduction/Aim
COPD patients are often prescribed multiple medications to manage their respiratory disease and comorbidities. This may result in complex medication regimens, which can increase the risks of poor adherence, medication errors and drug‐drug interactions. This study aims to explore the medication burden in COPD and its relationship to clinical outcomes.
Methods
A cross‐sectional study whereby COPD patients (n=222) were assessed for demographic information, comorbidities, medication use, clinical outcomes and multidimensional indices was performed. Complexity of medication regimens was quantified using the validated Medication Regimen Complexity Index (MRCI).
Results
Participants (58.6% males) had a mean (SD) age of 69.1±8.3 years, post‐bronchodilator %predicted FEV1 of 56.5±20.4%. They suffered from a median of 5 comorbidities. Nearly half (47.8%) of the participants were taking ≥9 medications. The mean (SD) total MRCI score was high (25.1±8.9). COPD‐specific medication regimens were more complex than those of non‐COPD medications (MRCI: 14.7 versus 9, respectively; p<0.0001). Complex dosage formulations contributed the most (57%) to higher MRCI scores of COPD‐specific medications while dosing frequency primarily drove the complexity associated with non‐COPD medications (67%). Participants in GOLD quadrant D had the highest median MRCI score for COPD medications (15.5), compared to those in quadrants A (13.5; p=0.0001) and B (12.5; p<0.0001). COPD‐specific MRCI score correlated with 6‐minute walk distance (r=−0.288; p=0.0003), Saint George Respiratory Questionnaire (r=0.294; p<0.0001) and prior year exacerbation history (r=0.246; p=0.0002). Multiple regression analysis revealed that comorbid cardiovascular, gastrointestinal or metabolic diseases contributed to higher MRCI scores and/or medication counts. Charlson Comorbidity Index and COPD‐specific comorbidity test showed the highest degree of correlations with total MRCI score (r=0.289; p<0.0001 and r=0.326; p<0.0001, respectively).
Conclusion
COPD patients have complex medication regimens that are associated with disease severity and certain comorbidities. Our data support the need to reduce medication complexity in COPD.
Grant Support
NHMRC, Ramaciotti Foundation, Lung Foundation of Australia, UoN, HMRI.
TO‐126: Long‐term efficacy of A1‐PI therapy in RAPID and RAPID extension trials
N. Gerard McElvaney1 , Kenneth R. Chapman2, Jonathan Burdon3, Eeva Piitulainen4, Niels Seersholm5, James Stocks6, Robert Sandhaus7, Oliver Vit8, Michael Fries9, Jonathan M. Edelman9
1Department of Medicine, Beaumont Hospital, Royal College of Surgeons in Ireland, Dublin, Ireland, 2Department of Medicine, University of Toronto, Toronto, Ontario, Canada, M5T 2S8, 3Respiratory Medicine, St. Vincent's Hospital, Melbourne, Victoria, Australia, VIC 3056; 4Faculty of Medicine, Lunds Universitet, Malmo, Sweden, SE‐205 02, 5Department of Respiratory Medicine, Gentofte Hospital, Hellerup, Denmark, 6Pulmonary and Critical Care, University of Texas Health Science Center at Tyler, Tyler, Texas, United States, 75708, 7Division of Pulmonary, Critical Care and Sleep Medicine, National Jewish Health, Denver, Colorado, United States, 8Clinical Research and Development, CSL Behring, Bern, Switzerland, 9Clinical Strategy and Development, CSL Behring, King of Prussia, Pennsylvania, United States;
Introduction
RAPID (NCT00261833), the largest (N=180) randomized placebo‐controlled trial assessing emphysema progression in alpha‐1 antitrypsin deficiency (AATD) completed to date, was followed by the open‐label RAPID Extension trial (NCT00670007).
Methods
Subjects in RAPID received alpha‐1 proteinase inhibitor (A1‐PI, Zemaira; CSL Behring) or placebo for 2 yrs. Eligible subjects (N=140) continued in Extension to receive A1‐PI for another 2 yrs. The Early‐Start (N=75) and Delayed‐Start (n=64) cohorts were defined by their treatment with A1‐PI and placebo in RAPID, respectively. Computed tomography (CT) lung density decline rate was measured annually and forced expiratory volume in 1 sec (FEV1) was measured quarterly.
Results
Annual CT lung density decline rate in the first 2 yrs was less by 0.75 g/L/yr in the Early‐Start cohort (−1.51 g/L/yr vs −2.26 g/L/yr, p=0.021 one sided). In the Delayed‐Start cohort, lung density decline was reduced to −1.26 g/L/yr after switching to A1‐PI. Changes in FEV1 over 4 yrs correlated significantly with changes in CT lung density.
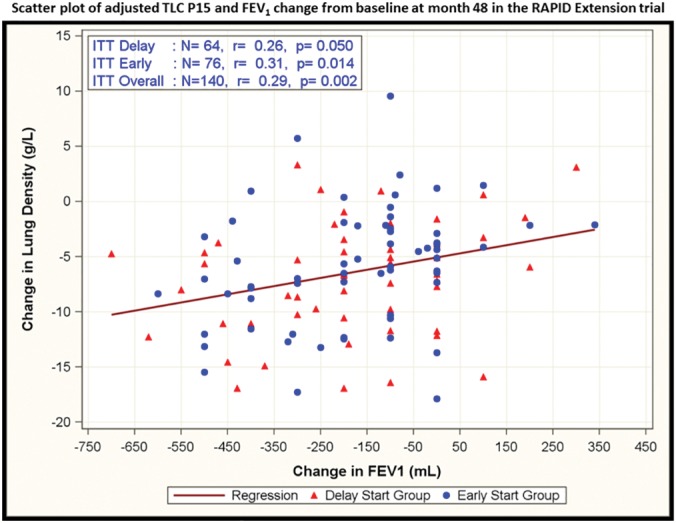
Conclusions
In RAPID, A1‐PI therapy reduced the rate of lung density decline compared to placebo. Over 48 months, the Delayed‐Start cohort showed a greater loss of lung density. These data demonstrate a disease‐modifying effect of A1‐PI therapy, suggesting that early treatment may reduce emphysema progression in AATD patients.
Funding
Trials were funded by CSL Behring.
Abstract Category
Airway Pharmacology and Treatment
Keywords
Treatments; COPD Management
TO‐127: Omalizumab treatment response in a severe allergic asthma population with overlapping COPD
Steven Maltby1,2,3, Peter G. Gibson1,2,3,4, Heather Powell2,3,4, Vanessa M. MCDONALD1 ,2,3,4
1National Health and Medical Research Council Centre of Excellence in Severe Asthma, 2Priority Research Centre for Healthy Lungs, the University of Newcastle, 3Hunter Medical Research Institute, 4Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, Australia
Introduction/Aim
Asthma and chronic obstructive pulmonary disease (COPD) are common airway diseases. Individuals with overlapping asthma and COPD experience increased health impairment and severe disease exacerbations. Efficacious treatment options are required for this population. Omalizumab (anti‐IgE) therapy is effective in patients with severe, persistent asthma, but limited data are available on efficacy in populations with overlapping asthma and COPD. In the current study, we sought to assess the effects of omalizumab treatment on this population.
Methods
Data from the Australian Xolair Registry (AXR) was used to compare treatment responses in individuals with asthma‐COPD overlap to severe asthma alone. Participants were assessed at baseline and after 6 months of omalizumab treatment. We utilised several different definitions of asthma‐COPD overlap. First, we compared participants with a previous doctor diagnosis of COPD to participants with no COPD diagnosis. We then made comparisons based on baseline lung function, comparing participants with post‐bronchodilator FEV1 <80% predicted to >80%. In the FEV1<80% population, analysis was further stratified based on smoking history.
Results
Omalizumab treatment markedly improved asthma control and health related quality of life in all populations assessed, based on ACQ‐5 and AQLQ questionnaire scores. Omalizumab treatment did not improve lung function in populations that were enriched for asthma‐COPD overlap (diagnosis of COPD or FEV1<80%/ever smokers).
Conclusion
Our study suggests that omalizumab improves asthma control and health related quality of life in individuals with severe allergic asthma and overlapping COPD. These findings provide real‐world efficacy data for this patient population and suggest omalizumab is useful in the management of severe asthma with COPD overlap.
Grant Support
The Australian Xolair Registry was supported by Novartis Pharmaceuticals Australia Pty Ltd, as an Investigator‐sponsored study. This analysis was supported by funding from the National Health and Medical Research Council Centre of Excellence in Severe Asthma (http://www.severeasthma.org.au).
TO‐128: Indacaterol/glycopyrronium (IND/GLY) reduces the risk of exacerbations versus salmeterol/fluticasone (SFC) in moderate‐to‐very severe COPD patients irrespective of prior ICS/LABA/LAMA therapy: the FLAME study
Jadwiga A. Wedzicha1, Karen Mezzi2, Tim Ayers3, Chau Thach3, Robert Fogel3, Francesco Patalano2, Donald Banerji3
1Airways Disease Section, National Heart and Lung Institute, Imperial College London, London, United Kingdom; 2Novartis Pharma AG, Basel, Switzerland; 3Novartis Pharmaceuticals Corporation, East Hanover, NJ, United States
Introduction
FLAME was the first study to show superiority of IND/GLY (LABA/LAMA) in reducing risk of exacerbations vs SFC (LABA/ICS) in COPD patients with history of exacerbations. We report results regarding effect of IND/GLY vs SFC on COPD exacerbations in patients with or without prior ICS/LABA/LAMA triple therapy.
Methods
FLAME, a 52‐week, randomised, double‐blind study, compared once‐daily IND/GLY 110/50 μg vs twice‐daily SFC 50/500 μg in patients with moderate‐to‐very severe COPD with ≥1 exacerbation in previous year. In this post hoc analysis, time to first COPD exacerbation (mild, moderate or severe) and moderate/severe COPD exacerbation with IND/GLY vs SFC were analysed. Additionally, treatment effects on rates of exacerbations were assessed in these patients.
Results
Of 3354 patients included in this analysis, 1148 (34.2%) were on prior triple therapy. IND/GLY significantly reduced the risk of any exacerbation and moderate/severe exacerbation vs SFC in patients, irrespective of prior triple therapy (Table). IND/GLY numerically reduced the rate of any and moderate/severe COPD exacerbations vs SFC in patients with/without prior triple therapy (table).
Conclusion
IND/GLY significantly reduces risk of exacerbations vs SFC, irrespective of prior triple therapy in exacerbating patients with moderate‐to‐very severe COPD.
Grant Support
The study was funded by Novartis Pharma AG, Basel, Switzerland

TO‐129: Bronchodilator therapy and exercise added to self‐management behaviour‐modification: Effects on physical activity in COPD
Peter Frith1 on behalf of Thierry Troosters2, Kim L Lavoie3,4,Nancy Leidy5, Francois Maltais6, Maria Sedeno7, Wim Janssens8, Alan Hamilton9, Damijan Erzen10, Dorothy De Sousa9, Lawrence Korducki11, Jean Bourbeau7
1Respiratory Medicine, Repatriation General Hospital and Flinders University, SA, Australia, 2Department of Rehabilitation Sciences and University Hospital Leuven, Pulmonary Rehabilitation and Respiratory Division, KU Leuven, Leuven, Belgium, 3Montreal Behavioural Medicine Centre, Research Centre, Hopital du Sacre‐Coeur de Montreal, Montreal, Quebec, Canada, 4Department of Psychology, University of Quebec at Montreal (UQAM), Montreal, Quebec, Canada, 5Scientific affairs, Evidera, Bethesda, Maryland, United States, 6Centre de Recherche, Institut Universitaire de Cardiologie et de Pneumologie de Quebec, Université Lavel, Quebec, Quebec, Canada, 7Respiratory Medicine, McGill University Health Centre, Montreal, Quebec, Canada, 8Respiratory Division, University Hospital Gasthuisberg, Leuven, Belgium, 9Respiratory Medicine, Boehringer Ingelheim (Canada) Ltd, Burlington, Ontario, Canada, 10Respiratory Medicine, Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach an der Riss, Germany, 11Respiratory Medicine, Boehringer Ingelheim Pharmaceuticals Inc., Ridgefield, Connecticut, United States
Introduction/Aim
PHYSACTO® has shown improved exercise capacity in patients with chronic obstructive pulmonary disease (COPD) receiving bronchodilators (BDs) ± exercise training (ExT) added to a self‐management behaviour‐modification programme (SMBM). We explored the influence of BDs±ExT following SMBM on physical activity (PA) and perceived PA‐related difficulty and symptoms in PHYSACTO® (NCT02085161).
Methods
A 12 week, randomised, partially double‐blind, placebo (P)‐controlled, parallel‐group trial. Interventions (all with 12 week SMBM): P; tiotropium (T) 5 μg; T + olodaterol (O) 5/5 μg; T + O 5/5 μg + 8 week ExT. A triaxial accelerometer assessed PA (steps/day), the Functional Performance Inventory assessed patient‐reported difficulty engaging in PA and the Chronic Respiratory Questionnaire assessed PArelated dyspnoea.
Results
303 patients (post BD‐FEV1: 57 [13] % predicted) were randomised and treated (full analysis set n=274). Change in steps/day at week 12 is shown in the Table; no significant gain in PA was seen by adding T+O or T+O+ExT to SMBM, versus SMBM+P. However, PA‐related difficulty and dyspnoea significantly decreased at week 12 for SMBM+T+O versus SMBM+P.
Conclusion
In moderate to severe COPD, SMBM increased PA and the addition of T+O to SMBM was associated with reduced difficulty and symptoms with PA when compared to SMBM+P.
| Intervention | Steps/daya at week 12 | |||
|---|---|---|---|---|
| Adjusted mean (SE) | Adjusted mean change from baseline (SE) | 95% CI | P value | |
| SMBM+P (n=55) | 6517.71 (325.08) | 1098.07 (325.08) | 457.47, 1738.67 | 0.0009 |
| SMBM+T (n=57) | 5572.83 (317.98) | 153.19 (317.98) | ‐473.43, 779.81 | 0.6304 |
|
SMBM+T+O (n=60) |
6813.88 (310.22) | 1394.24 (310.22) | 782.92, 2005.56 | <0.0001 |
| SMBM+T+O+ExT (n=57) | 5976.43 (317.97) | 556.79 (317.97) | ‐69.81, 1183.39 | 0.0813 |
Full analysis set. Analysis of covariance model with “treatment” and “baseline” as covariates. Common baseline mean steps/day (SE): 5419. 64 (186.15)
aMeasured via triaxial accelerometer.
Grant Support
The study was funded by Boehringer Ingelheim.
Declaration of Interest Statement
PF has received in the past 5 years honoraria for educational and advisory board involvement and/or received conference attendance support for the following: Global Initiative for COPD (GOLD), Improvement Foundation, Lung Foundation Australia, and Remedy Healthcare; AstraZeneca, Boehringer Ingelheim, CSL‐Behring, GlaxoSmithKline, Menarini, MundiPharma, and Novartis. TT is the Principal Investigator of PROactive project and received speakers/consultancy fees from Boehringer Ingelheim, Novartis, and Bayer. KLL received grants/research support from GSK, consulting fees from Schering‐Plough and Merck Frosst and served on speaker bureaus/honoraria for GSK, Astra‐Zeneca, Pfizer, Merck Frosst, Air Liquide and Health International. NL is an employee of Evidera and works with a variety of companies and organizations and expressly prohibited from receiving any payment or honoraria directly from these organizations for services rendered. FM is a consultant for Boehringer Ingelheim and served on advisory boards for Boehringer Ingelheim, GlaxoSmithKline, and Pfizerand has received payment for lectures including service on speaker bureaus from Boehringer Ingelheim, GlaxoSmithKline, Nycomed and Pfizer. MS is employed by Respiplus, a non‐profit organisation that was contracted by the study sponsor to develop the educational component of thetraining programme. AH, DE, DDS, and LK are employees of Boehringer Ingelheim. JB received research funding via the Research Institute of the McGill University Health Centre from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Merck, Novartis, Nycomed, Pfizer and Theratechnologies; and has served on speakers, consultation panels and/or advisory boards for these pharmaceutical companies.
TO‐130: Effect of indacaterol/glycopyrronium (IND/GLY) vs salmeterol/fluticasone (SFC) on moderate or severe COPD exacerbations and lung function based on baseline blood eosinophil counts: Results from the FLAME study
Kenneth R. Chapman1, Claus F. Vogelmeier2, Angel FowlerTaylor3 , Tim Ayers3, Chau Thach3, Anupama Shrinivasan4, Robert Fogel3, Francesco Patalano5, Donald Banerji3
1Department of Medicine, University of Toronto and Asthma and Airway Centre, University Health Network, Toronto, ON, Canada, 2Pulmonary and Critical Care Medicine, Philipps–Universität Marburg, Marburg, Germany, 3Novartis Pharmaceuticals Corporation, East Hanover, NJ, United States;, 4Novartis Healthcare Pvt. Ltd., Hyderabad, India, 5Novartis Pharma AG, Basel, Switzerland
Introduction
The FLAME study compared the effect of IND/GLY vs SFC on exacerbations in COPD patients with a risk of exacerbation. Here we present the rate of reduction of moderate or severe exacerbations and lung function changes based on blood eosinophils in moderate‐to‐very severe COPD patients.
Methods
This was a 52‐week, multicentre study. Patients with moderate‐to‐very severe COPD, post‐bronchodilator FEV1 ≥25 and <60% and a history of ≥1 exacerbation in the previous year were randomised (1:1) to IND/GLY (110/50 μg) once daily or SFC (50/500 μg) twice daily. The data were assessed by blood eosinophil cut offs (<150, 150–<300 and ≥300) and percentages (<2% and ≥2%).
Results
3362 patients were randomised to IND/GLY (n=1680) or SFC (n=1682). The annualised rate of moderate or severe exacerbations was significantly lower in IND/GLY‐treated vs SFC‐treated patients’ at all eosinophil counts, although not significant for small number of patients with ≥300 cells/μL. The lung function was significantly improved at all the visits with IND/GLY vs SFC irrespective of eosinophil count (Table 1).
Conclusion
In patients with high risk of exacerbations, IND/GLY was superior in reducing moderate or severe exacerbations and showed significant improvement in lung function vs SFC independent of blood eosinophil counts.
Grant Support
The study was funded by Novartis Pharma AG, Basel, Switzerland

Interventional Pulmonary / Bronchology 2
TO‐131: Changes in lung function and forced oscillatory technique (FOT) parameters following bronchial thermoplasty (BT) in patients with refractory asthma
Ing AJ1 ,4, Langton D2 , Pierucci P1 ,2,4, Farah CS1 ,3,4
1Faculty of Medicine and Health Sciences, Macquarie University, 2Monash University, 3Woolcock Institute of Medical Research, 4Sydney Medical School, The University of Sydney
Introduction/Aim
Bronchial Thermoplasty (BT) improves symptom control and reduces exacerbations in patients with refractory asthma. The precise mechanism remains unclear, but consistent improvement in spirometry has not been recorded. We postulate that assessment of lung function during tidal breathing with oscillometry to measure respiratory impedance may better reflect the clinical improvements reported.
Methods
Patients with refractory asthma (GINA Step 5) had the Asthma Control Questionnaire (ACQ5), spirometry, resistance at 5 Hz (R5) and reactance at 5 Hz (X5) recorded before and 6 weeks after completing BT. One centre measured impedance with the forced oscillation technique (FOT) [TremoFlo C‐100, Thorasys Medical Systems, Canada] and the other with impulse oscillometry(IOS) [Sensormedics].
Results
The average age was 60.8 (1.4) years in the FOT group and 61.2 (11.4) years in the IOS group. ACQ5 scores improved in both groups. In the FOT group, there were significant improvements in spirometry and X5; and the change in X5 correlated strongly with changes in vital capacity and weakly with ACQ5.
| FOT (n=12) Pre BT | Post BT | p value | IOS (n=8) Pre BT | Post BT | p value | |
|---|---|---|---|---|---|---|
| ACQ5 | 2.80 (0.75) | 1.90 (1.10) | <0.05 | 2.80 (0.91) | 1.70 (1.30) | 0.05 |
| FEV1 (%pred) | 51.7 (15.9) | 61.7 (20.9) | <0.05 | 49.7 (7.2) | 54.5 (14.3) | NS |
| FVC (%pred) | 78.5 (18.6) | 89.8 (18.6) | <0.05 | 80.5 (13.1) | 89.3 (14.9) | NS |
| R5 (cmH2O.s/L) | 5.93 (1.77) | 5.61 (1.73) | NS | 6.49 (2.29) | 6.00 (2.33) | NS |
| X5 (cmH2O.s/L) | ‐4.53 (4.23) | ‐3.68 (3.07) | <0.05 | ‐3.60 (1.88) | ‐3.58 (1.87) | NS |
Conclusion
The improvement in symptom control following BT may, in part, relate to deflation and consequent improvement in lung mechanics during tidal breathing. Differences in measuring impedance with FOT and IOS techniques will be discussed.
Grant Support
University of Sydney Post Graduate Scholarship
TO‐132: 5 year single centre experience of airway stenting
M. Cheng1, J. Williamson1, 2
1Liverpool Hospital, NSW, 2Respiratory, Sleep and Environmental Health Research Group, Ingham Institute for Applied Medical Research, Sydney, Australia
Introduction
Airway stenting is a therapeutic intervention for the management of complex malignant and benign central airway obstruction. Our institution commenced an airway stenting program 5 years ago. We present an audit of the patient case‐mix and outcomes from this service since inception.
Methods
Chart review of stent insertion cases performed at Liverpool Hospital between Dec 2010 to July 2016. Indications, stent selection, peri‐procedure and stent‐related complications, survival and impact of stent on symptoms were reviewed.
Results
37 stents (14 silicon; 20 self‐expanding metallic, 3 Dynamic Y) were inserted in 32 patients. Stent numbers increased over the first 4 years then stabilised. The case‐mix consisted of emergent malignant airway obstruction and outpatients with both benign and malignant pathology. 20 patients were from the Local Health District and 12 were referred from other Health Districts. 11 patients had stents inserted for non‐malignant indications. In these patients, post‐operative complications included mucous retention, stent migration, obstructing granulation tissue and mucosal flap tissue. Repeat bronchoscopies to address these complications averaged 4 procedures per patient (range 1–12). 21 patients had stents inserted for malignant indications primarily for palliative indications. 17 patients were able to be either transferred back to their referral centre to complete further therapy or were discharged from their acute hospital admission. There were 2 peri‐procedural stent related deaths, 1 due to post insertion hospital acquired pneumonia and another due to central airway laceration resulting in massive surgical and mediastinal emphysema.
Conclusion
Stenting offers symptomatic palliation from central airway obstruction but stent related complications are common, particularly in benign conditions. For malignant airway obstruction, the short term palliative benefits allow the majority of patients to be discharged from acute hospital admission offering scope for further treatments. Further study is required to look at physiologic and QOL improvements.
Deaths – TBM massive emphysema lady, GOershal (pneumonia),
Include massive mediastinal lymphoma patient
Grant Support
Nil
TO‐133: Identifying risk factors that predict poor tolerance in pneumothoraces following transthoracic needle biopsy (TTNB) of lung lesions.
Sharan Randhawa1, Ranjan Shrestha1
1Respiratory Department, Fiona Stanley Hospital, WA
Introduction
The average risk of developing pneumothorax following TTNB of a lung lesion is about 20%. This can be disabling especially in elderly patients with preexisting respiratory disorders and multiple comorbidities, resullting in hospital admissions either for observation or insertion of chest drain. To date there have been no studies directly correlating any risk factors in predicting poor tolerance to iatrogenic pneumothorax.
Aim
To identify all patients with pneumothorax post TTNB and record the outcomes of their hospital admissions.
To identify if age, smoking history, preexisting respiratory disease and reduced FEV1 and or DLCO are risk factors for poor tolerance of pneumothorax and increased length of stay in hospital.
Methods
Demographic data of all patients who underwent TTNB (age, gender), primary lung disease, medical histories, smoking status, lung function tests (FEV1, FVC, DLCO, KCO, TLC) and length of hospital stay if complications occurred were retrospectively collected from two centers (Fiona Stanley Hospital and Fremantle Hospital WA) from August 2014 to February 2016.
Patients who had a pneumothorax following TTNB who were either admitted for observation vs requiring a chest drain were recorded, including duration of hospital admission. Patients requiring a chest drain were defined as having “poor tolerance” to pneumothorax.
Chi square and t tests were used to determine associations between age, preexisting COPD, smoking history, comorbidities, reduced lung function (FEV1 <50% or DLCO <50%) and “poor tolerance” to pneumothorax.
Results
A total of 154 TTNB procedures were carried out. 65 of the procedures (42.2%) were complicated with a pneumothorax and 13 patients (8.4%) required aspiration or chest drain. Mean length of stay (LOS) in days were 4.17 +/−8.73 for all procedures.
Of those who had poor tolerance to pneumothorax, the average FEV1 % predicted was 66.5 +/− SD 30.6 and average DLCO % predicted was 63.5 +/− SD 19.8. Ie both were moderately reduced.
7 patients (58.3%) out of the 13 patients who requred a chest drain had COPD. Chi Square testing did not show any statistically significant association between COPD and poor tolerance to pneumothorax (p=0.599).
There was no statistically significant association between older patients >70 years and poor tolerance of pneumothorax (p=0.934) or between reduced lung function and poor tolerance to pneumothorax (p=0.091).
Conclusion
Correlation analysis shows no association between presence of COPD/having reduced lung function/older age and “poor tolerance” to pneumothorax.
This is a negative study however it was limited by its small numbers. Larger studies looking at these risk factors will be crucial to prevent unneccessary lengthy hospital stays and chest drain insertions caused by a routine TTNB procedure.
Nil declaration of interest
TO‐134: Safety and diagnostic yield of transbronchial lung cryobiopsy for diagnosis of interstitial lung disease
Michelle Tan1, Khin Hnin2, Dion Grosser1, Brian J Smith1
1Department of Respiratory and Sleep Medicine, Queen Elizabeth Hospital, Woodville South, South Australia, 2Flinders University, Bedford Park, South Australia
Introduction
Interstitial lung disease (ILD) is a heterogeneous group of respiratory conditions requiring clinical, radiological and pathological correlation. Transbronchial lung cryobiopsy (TBLC), forceps transbronchial biopsy (FTBB), CT guided core biopsy and open lung biopsy are all potential methods for obtaining lung tissue for analysis. The newest of these options is cryobiopsy and the place for this method for diagnosing ILD is yet to be fully determined. Our study aims to analyse and compare diagnostic yield and complications for the two bronchoscopically derived lung biopsy types being TBLC versus FTBB in patients with suspected ILD in the context of our hospital ‐ an academic tertiary care centre.
Methods
A retrospective observational study of patients with radiological features suspicious of ILD who have undergone TBLC and FTBB between 1 Jan 2014 and 30 Sept 2016.
Results
patients who underwent bronchoscopy, 57 eligible patients (35 females, 61% and 22 males, 39%) with a mean age of 60.1 were identified to have either TBLC (37) or FTBB (20). Grade 1 bleeding occurred in 63% of TBLC and 71% of FTBB while grade 4 bleeding occurred in 2 TBLC cases. Similar proportion of patients in both groups had a pneumothorax (10% vs 10.8%). A better diagnostic yield was achieved with TBLC (51% vs 25%). However, it was not statistically significant with odds ratio 2.1 (95% CI 0.63 to 6.9, p value 0.228). With a mean maximal diameter of 5.4 ± 2.3mm, cryobiopsies were larger than samples obtained from FTBB (2.3 ± 1.7mm, p value <0.001).
Conclusion
TBLC appears to be as safe as FTBB with the advantage of larger biopsy size although diagnostic yield of TBLC was not statistically different to FTBB in this single cohort. Larger, prospective studies are needed to establish the role of TBLC in the diagnostic algorithm of ILD.
Grant Support
Nil
TO‐135: Benefit of standard transbronchial biopsies after endobronchial ultrasound guided biopsies for peripheral lung lesions
Ghulam Sarwar1,2, Scott Twaddell1,2, Christopher Grainge1,2, David Arnold1,2
1John Hunter Hospital, New Lambton Heights, NSW 2305, 2Centre for Healthy Lungs, Hunter Medical Research Institute, NSW 2305
Introduction/Aim
Endobronchial Ultrasound Guide Sheath (EBUS‐GS) is used to locate and biopsy peripheral lung lesions with sensitivity and specificity of 73% and 100% respectively. (1) There is minimal data regarding a combined conventional transbronchial lung biopsy (cTBLB) plus EBUS‐GS biopsy approach in the same patient. We aimed to assess the utility of this approach, and assess complication rates.
Methods
A retrospective analysis of patients who underwent EBUS‐GS and cTBLB from August 2012 to October 2016 at the John Hunter Hospital, Newcastle, NSW.
Results
73 patients were eligible with mean(SD) age 71(7) years. 43 were male. Mean(SD) lesion size was 26(3.5)mm. Of the 73 patients, lesions were successfully localised using EBUS‐GS in 59(80%). Of these 59 lesions, 44 were concentric, 12 were eccentric and data was missing for the remaining 3. EBUS‐GS biopsies were positive in 29 patients (49%) and definitive atypical pattern was seen in 6 patients (10%) giving a cumulative sensitivity of 60%. Brushings via guide sheath were positive in 20 patients (33%).
cTBLB were definitively positive in 28 patients (38%) and an atypical cytology pattern was seen in 3 patients giving a cumulative sensitivity of 42% using non GS guided procedures. Standard brushing were positive in 15 patients (21%).
Four patients (7%) were diagnosed based on cTBLB alone, where EBUS‐GS guided investigations were negative. Combining cTBLB and EBUS‐GS at the same procedure increased sensitivity from 60% to 68%. There was one small pneumothorax managed conservatively and one episode of bleeding requiring local adrenaline therapy.
Conclusion
EBUS GS provides a higher success rate for diagnosis of peripheral lung lesions than cTBLB, however when EBUS‐GS is combined with cTBLB, it may further increase the diagnostic yield.
Grant Support
Nil
Declaration of interest:
Nil to declare
REFERENCE
1. Wang Memoli JS, Nietert PJ, Silvestri GA. Meta‐analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest 2012; 142: 385–93.
TO‐136: Reducing hospitalisation and procedures in malignant pleural effusion ‐ results of the AMPLE randomised trial
Fysh ETH1 , Thomas R1 , Smith N2, Lee P3, Kwan BCH4 , Yap E5 , Horwood F5 , Piccolo F1 , Garske L6 , Lam D7 , Lee YCG1
1Sir Charles Gairdner Hospita, Western Australia, 2Wellington Hospital, New Zealand, 3National University Hospital, Singapore, 4St George and the Sutherland Hospitals, New South Wales, 5Middlemore Hospital, New Zealand, 6Princess Alexandra Hospital, Queensland, 7Hong Kong University Hospital
Introduction/Aim
Malignant pleural effusions (MPEs) affect over one million people each year and herald limited prognoses. Talc pleurodesis and indwelling pleural catheter (IPC) are approved treatments with similar quality‐of‐life benefits in randomised studies to date, resulting in equipoise. Freedom from hospitalization and further interventions are important goals of management. The Australasian Malignant Pleural Effusion randomised trial aimed to determine whether IPCs are more effective than talc pleurodesis in reducing total hospitalization days in the remaining lifespan of MPE patients.
Methods
Open‐labelled, randomized controlled trial recruited 146 participants with symptomatic MPE from nine centers in Australia, New Zealand, Singapore and Hong Kong and followed them for 12 months/until death. Participants were randomized (1:1) to IPC or talc pleurodesis, minimized by region (Australasia vs Asia), malignancy (mesothelioma vs others), and trapped lung (vs not). Primary endpoint was total number of days spent in hospital from trial intervention to death, or 12 months. Secondary outcomes included further pleural interventions, patient‐reported breathlessness scores, quality‐of‐life measures, and adverse events.
Results
The IPC group spent significantly fewer days in hospital than the Pleurodesis group: median (IQR) 10.0 (14) vs 12.0 (14) days, p=0.026, which represented 6.2 (13.8)% vs 11.1 (33.7)% of their remaining lifespan, respectively, p=0.01. Mean reduction in hospitalization days was 3.6 days per patient: 12.7 (IPC) vs 16.3 (Pleurodesis) days. Fewer IPC‐treated patients required further invasive pleural drainages (4.1% vs 22.5%, 95% CI 7.7‐29.2%). Improvement in breathlessness and quality‐of‐life, and adverse event rates were comparable.
Conclusion
IPC management reduces the time MPE patients spend in hospital before death and minimizes the need for further invasive pleural interventions, while providing equivalent symptomatic improvement, when compared with conventional talc pleurodesis.
Grant Support
The Sir Charles Gairdner Research Advisory Committee, Cancer Council of Western Australia and the Dust Disease Board of New South Wales, Australia.
Declaration of Interests
The authors have no conflict of interest.
Physiology and Sleep 2
TO‐137: The impact of mechanical ventilation on regional gene expression
Seiha Yen1, Melissa Preissner2, Andreas Fouras2, Peter Dargaville3,4, Graeme Zosky1
1School of Medicine, University of Tasmania, Tasmania, Australia, 2Department of Mechanical and Aerospace Engineering, Monash University, Victoria, Australia, 3Neonatal and Paediatric Intensive Care Unit, Royal Hobart Hospital, Tasmania, Australia, 4Menzies Institute for Medical Research, University of Tasmania, Tasmania, Australia
Introduction/Aim
Mechanical ventilation, a lifesaving therapy for patients with respiratory failure, has been shown to contribute to mortality by inducing inflammation, which leads to multisystem organ failure through systemic effects. Different regions of the lung have been shown to heterogeneously respond to mechanical ventilation, which suggests that ventilator‐induced lung injury may vary regionally. However, the impact of mechanical ventilation on regional lung inflammation is unknown. The aim of this study was to assess regional gene expression in response to mechanical ventilation in the healthy lung.
Methods
We ventilated two groups of BALB/c mice (n = 8 per group) for 2 h using protective [low tidal volume with moderate positive end expiration (PEEP)] or injurious [high tidal volume with zero PEEP] ventilation strategy. mRNA levels of 19 genes of interest in ten different regions of each mouse lung were quantified using qPCR array and compared between the two groups and a free‐breathing control group (n=8).
Results
The mRNA levels of ten genes were not differentially expressed between groups (P>0.05). Five genes had significantly different mRNA levels depending on the ventilation strategy (TFN‐α, Cxcl‐2, fos, IL‐6, and Nfe2I2; P≤0.01 for all comparisons). Five genes were differentially expressed between lung regions (TFN‐α, Cxcl‐2, IL‐1β, Vim, and Ccl‐2; P<0.05 for all comparisons), while two genes had differential regional expression that depended on the ventilation strategy (IL‐6, P=0.02 and Ccl‐2, P<0.01).
Conclusion
To our knowledge, this is the first demonstration of regional variation in gene expression in response to mechanical ventilation. Our results provide critical insight into the relationship between regional lung response to mechanical ventilation and regional injury. Future studies should be aimed at understanding the link between local tissue stretch and the expression of these injury related genes.
Grant Support
This study is funded by NHMRC grant # 1077905
TO‐138: Diurnal variability of lung function and its association with sleep among patients with COPD
Kanika Jetmalani1,2,3,Louise Harkness1, Cindy Thamrin1,2,3,Craig L. Phillips1,3,Ron R. Grunstein 1,Paul M. Young1,2,Greg G. King 1,2,3,4
1Woolcock Institute of Medical Research, 2Woolcock Emphysema Centre, 3University of Sydney, NSW, 4Department of Respiratory Medicine, Royal North Shore Hospital, NSW
Introduction/Aim
Nocturnal respiratory symptoms are reported in upto half of chronic obstructive pulmonary disease (COPD) patients, and result in increased night time awakenings. Circadian variations in lung function may worsen COPD symptoms at night leading to poor sleep efficiency. In this pilot study we determined the prevalence of sleep disturbances and their association with diurnal changes in lung function in COPD.
Methods
11 COPD subjects had lung function measures of forced oscillation technique (resistance and reactance at 5 Hz) and spirometry in the evening to assess diurnal changes in lung function. Overnight, subjects undertook an in‐lab diagnostic sleep study to measure their sleep architecture. Lung function measurements were repeated in the morning, as well as standard sleep questionnaires. The overnight changes in lung function were assessed using paired T‐tests. Coefficient of repeatability (COR), defined as twice the standard deviation of the difference of the evening and morning measurements was also determined.
Results
Subject characteristics, lung function and sleep parameters are shown in table below. 6 subjects were identified with mild, 2 with moderate and 2 with severe obstructive sleep apnoea. There was a significant decline from evening to morning FEV1/FVC (mean change±SD) (2.3±2.5 %, p=0.01) and R5 (−0.78±0.82 cmH20.L/s, p=0.01) but not FEV1 (69±166 ml, p=0.19) or X5 (0.61±1.1 cmH20.L/s, p=0.09). The COR for R5 (1.64 cmH20.L/s) was twice that reported by Oostveen et al1 (0.9 cmH2O.L/s) in healthy subjects. The changes in morning to evening lung function parameters were not related to any sleep parameters.
| N (Males) | 11 (7) |
|---|---|
| Age, years | 67 ±7 |
| FEV1 % Pred | 53.64 ±16.3 |
| FEV1/FVC % | 45.88 ±9.9 |
| DLCO % Pred | 62.8 ±9.6 |
| R5 cmH20.L/s | 5.32 ±2.4 |
| R5 Z score | 1.93 ±1.0 |
| X5 cmH20.L/s | ‐3.98 ±2.7 |
| X5 Z score | ‐4.89 ±3.5 |
| Apnoea Hypopnea Index (range) | 14.2 (4‐35) |
| Epworth Sleepiness Scale (range) | 7.2 (2‐20) |
| Sleep efficiency (range) | 80.9 (65‐91) |
Conclusion
These preliminary results show that sleep abnormalities are commonly present in subjects with COPD. While diurnal variability was seen both in spirometry and FOT parameters, they were not associated with sleep outcomes. Ongoing work will help us understand the relationship between circadian changes in lung function and sleep quality and symptoms in COPD.
1. Oostveen E et al, Respiratory impedance in healthy subjects: baseline values and bronchodilator response. ERJ. 2013 Dec;42(6):1513–23
Grants
Menarini Australia
Grant Support
TO‐139: Lung ultrasound surface wave elastography – preliminary measurements in patients with interstitial lung diseases
Sanjay Kalra, M.D.1, Thomas Osborn, M.D.2, Brian Bartholmai M.D.3, Boran Zhou PhD4 , Xiaoming Zhang PhD5
1Division of Pulmonary & Critical Care Medicine, Mayo Clinic, Rochester, MN, USA, 2Division of Rheumatology, Mayo Clinic, Rochester, MN, USA, 3Department of Radiology, Mayo Clinic, Rochester, MN, USA, 4,5Department of Physiology and Biomedical Engineering, Mayo Clinic, Rochester, MN, USA
Introduction/Aim
Lung ultrasound surface wave elastography (LUSWE) is a novel technique to assess surface lung tissue elastic properties by measuring surface wave propagation speed using an ultrasound detector system. The surface wave propagation on lung is noninvasively generated by a local and small mechanical actuation on the skin of the chest wall.Since many interstitial diseases predominantly affect the lung periphery, these may be especially suitable for this type of assessment, non‐invasively and without radiation exposure.
Methods
7 healthy controls and 7 patients who had CT chest identified peripherally distributed pulmonary fibrosis were studied. LUSWE was performed by generating small 0.1 second harmonic vibrations at 100 Hz by indenting a 3 mm area in an intercostal space with a handheld shaker and measuring the surface wave propagation on the lung with a ultrasound probe placed 5 mm away in the same intercostal space. Three measurements, at full inspiration, were made in each of 3 locations over each lung.
Results
All measurements below were made at 100 Hz and and are in m/sec±SD.
| Controls | Patients | p (control v patient) | |
|---|---|---|---|
| Rt upper anterior | 2.00±0.26 | 3.46±0.67 | <0.01 |
| Rt lateral | 1.89±0.31 | 2.89±0.69 | <0.01 |
| Rt lower posterior | 2.01±0.35 | 3.25±0.73 | <0.01 |
| Lt upper anterior | 1.93±0.29 | 3.41±0.76 | <0.01 |
| Lt lateral | 2.01±0.27 | 2.99±0.69 | <0.01 |
| Lt lower posterior | 2.08±0.28 | 3.22±0.53 | <0.01 |
Conclusion
These results suggest that LUSWE can identify a difference in wave speed between control and abnormal, peripherally fibrotic, lungs. Its reproducibility, specificity and sensitivity, and ability to detect longitudinal change are yet to be defined but it has the promising advantage of being both non‐invasive and radiation‐free.
Grant Support
NIH R01HL125234 from the National Heart, Lung, and Blood Institute.
TO‐140: The ventilatory control contribution to obstructive sleep apnoea in Caucasian and Chinese patients.
Denise M O'Driscoll1,2, Shane Landry3, Chris Andara3, Jonathan Pham1, Alan Young1,2, Bradley A Edwards3
1Department of Respiratory and Sleep Medicine, Eastern Health, 2Eastern Health Clinical School, Monash University, 3Department of Physiology and School of Psychology, Monash University
Introduction/Aim
Chinese populations have a comparable prevalence of obstructive sleep apnoea (OSA) compared to their Caucasian counterparts, but are notably less obese. Craniofacial dimensions of the upper airway favouring obstruction have been described in the Chinese population suggesting that this group has an OSA phenotype less dependent on obesity. While OSA is now also recognized to be caused by a hypersensitive ventilatory control system (high loop gain [LG]) and a low arousal threshold (ArTh), no study has examined how ethnicity may influence these traits. We aimed to examine whether LG and ArTh differ between Chinese and Caucasian individuals with OSA.
Methods
Chinese (n=45) and Caucasian (n=45) subjects with moderate‐to‐severe OSA matched by age, gender and apnoea‐hypopnoea index (AHI) were studied. We measured LG (including the chemoreflex delay, Delay, and cycling period, Tn) and the ArTh by fitting a validated control system model to the pattern of ventilation during spontaneous OSA from clinical polysomnography. Data presented are Median (IQR) unless indicated otherwise.
Results
Despite matched AHIs, Chinese subjects had a lower BMI compared to Caucasian subjects (27.2[4.5] vs. 34.0[9.45]kg/m2, p<0.001), and longer respiratory event durations (Mean[SEM]. Apnoeas: 25.1[1.2] vs. 19.3[1.3]s, p=0.001; Hypopnoeas 25.3[1.0] vs. 22.9[1.0]s, p=0.03). Whilst there was no difference in LG between groups, ArTh (1.3[0.3] vs. 1.2[0.3]%resting ventilation, p=0.019), Tn (45.0[15.1] vs. 39.3[14.4]s, p=0.002) and Delay (Mean[SEM]. 12.8[0.5] vs. 11.0[0.4]s, p=0.002) were all higher/longer in the Chinese group.
Conclusion
Chinese individuals with OSA have a unique sleep phenotype, compared to Caucasians, characterised by a high arousal threshold, and an increased cycling period and chemoreflex delay which is reflected in a propensity for longer respiratory events. These data suggest: (1) the mechanisms that cause OSA are influenced by ethnicity, and (2) the use of sedatives to raise the arousal threshold may be less effective in treating OSA in Chinese populations.
TO‐141: Quality of life and symptoms are related to forced oscillation mechanics during home‐monitoring in COPD
SC Zimmermann1,2,3, JC Watts1,2, CD Nguyen1, A Gobbi4, A Bertolin1, CS Farah1,5, MJ Peters5, RL Dellacà4, GG King1,2,3, C Thamrin1
1Woolcock Emphysema Centre, Woolcock Institute of Medical Research, The University of Sydney, Glebe, NSW 2037, 2Department of Respiratory Medicine, Royal North Shore Hospital, St Leonards, NSW 2065, 3Northern Clinical School, The University of Sydney, NSW 2006, 4Politecnico di Milano, Milan, Italy, 5Department of Respiratory Medicine, Concord Repatriation and General Hospital, Concord, NSW 2137
Introduction/Aim
The forced oscillation technique (FOT) is a non‐effort dependent and objective measure of airway function. Home monitoring of FOT and its day‐to‐day variability may offer value in the management of COPD where peak expiratory flow or spirometry have not. This study assessed the relationship between FOT measures obtained from home‐monitoring and quality of life and symptoms in COPD.
Methods
10 COPD patients were recruited from Royal North Shore Hospital, Concord Hospital and the Woolcock Institute of Medical Research. At study enrolment, standard lung function tests were performed. A FOT home‐monitoring device (ResTech srl, ResMon Diary device) was installed in each enrolled participant's home over a period of 8–9 months. Participants were trained to make unsupervised measurements of FOT, to obtain resistance (Rrs), its standard deviation over the past 14 days (SDRrs), and the difference between inspiratory and expiratory reactance (ΔXrs), a measure of expiratory flow limitation. Daily symptoms were assessed by e‐diary based on the COPD Assessment Test (CAT) and monthly quality of life via St. George's Respiratory Questionnaire (SGRQ). The relationship between FOT measures vs SGRQ and CAT were assessed using mixed modelling.
Results
Participants’ mean±SD age was 69.7±10.8 years, with %predFEV1 38.4±5.2 and baseline SGRQ 53.2±16.3. The median(range) adherence was 95.7%(46.6‐100%). Rrs and SDRrs were significantly related to SGRQ (fixed effect estimate 4.84±1.04 cmH2O−1s−1L, p<0.001, estimate 11.33±4.55 cmH2O−1s−1L, p=0.015, respectively). ΔXrs was significantly related to CAT (estimate −1.47±0.43 cmH2O−1s−1L, p=0.001).
Conclusion
Airway calibre and its variability in COPD were related to monthly quality of life, encompassing symptoms, activity limitation and psychosocial impact, while expiratory flow limitation related to daily symptom measures. Thus, FOT measures and variability reflect patient‐based outcomes, providing supporting evidence for the utility of home monitoring of FOT in COPD.
Conflict of interest
No.
Grant Support
NHMRC Postgraduate Scholarship, LFA/Boehringer Ingelheim Top Up Research Grant, NHMRC Project Grant #1065938.
Grant Support
NHMRC Postgraduate Scholarship, LFA/Boehringer Ingelheim Top Up Research Grant.
Grant Support
TO‐142: Randomised controlled trial of polysomnography titration of nocturnal non‐invasive ventilation
Liam M Hannan 1–4 , Linda Rautela 1–3 , David J Berlowitz 1–4 , Nicole Sheers 1–4 , Caroline Chao 1–3 , Fergal O'Donoghue 1–4 , Christine F McDonald 1 –4 , Mark E Howard 1–4
1Institute for Breathing and Sleep, 2Department of Respiratory and Sleep Medicine, Austin Health, 3Victorian Respiratory Support Service, 4Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne
Introduction/Aim
Non‐invasive ventilation (NIV) settings determined during the daytime can produce patient‐ventilator asynchrony (PVA) at night, causing sleep disruption and limiting tolerance. The aim of this study was to determine if polysomnography (PSG) titration of NIV results in less PVA and sleep disruption than daytime titration alone.
Methods
Prospective randomised controlled trial in stable, English‐speaking, treatment‐naïve individuals requiring long‐term NIV. Participants were randomly allocated to Control (daytime titration + sham PSG titration) or PSG (daytime titration + PSG titration). Primary outcome was the PVA and arousal indices on PSG at 10 weeks. Secondary outcomes included adherence (change in average daily NIV use), gas exchange (PaCO2, nocturnal oximetry), symptoms (somnolence, sleep quality, fatigue, dyspnoea) and health‐related quality of life (HRQoL)
Results
Sixty participants were randomised (n=30 each group). Most participants (88.3%) had a neuromuscular disorder. There was one death, two drop‐outs and three participants in each group did not complete the final PSG. PVA was less frequent in the PSG group (PSG 25.7 (12–68) vs. Control 41.0 (28–182), p=0.046) but there was no difference in arousals (PSG 11.4 (9–19) vs. Control 14.6 (11–19), p=0.258). Change in average daily NIV use was not different (PSG +51.8min (7 to 96) vs. Control +3.6min (−33 to 40), p=0.09) although a pre‐specified subgroup with poor early adherence (<4hrs/day) increased their use after PSG (PSG +95min (29–161) vs. Control ‐23min (−86 to 39), p=0.01). PaCO2, somnolence and subjective sleep quality improved to a similar extent, and there were no differences in HRQoL, objective sleep quality or nocturnal gas exchange.
Conclusion
PSG titration of nocturnal NIV is associated with less PVA but not less sleep disruption than daytime titration. PSG titration improved NIV adherence in those who were poor users initially. No other short‐term clinical benefits were demonstrated in this stable outpatient population. Further studies may help clarify the role of PSG titration of NIV.
Grant Support
Austin Medical Research Foundation, Institute for Breathing and Sleep, NHMRC Postgraduate Scholarship
Respiratory Infectious Diseases 2
TO‐143: Ten year retrospective clinical audit of tuberculosis in far North Queensland
Wilson MR1 , Weston J1 , Mullen AP1 , Knight TA1 , Simpson G1
1Department of Respiratory Medicine, Cairns Hospital, Queensland, Australia
Introduction/Aim
To document changes in tuberculosis epidemiology in Far North Queensland for comparison with national data and two previous audits of the region.
Methods
Retrospective clinical audit of all cases of tuberculosis notified to the Cairns Chest Clinic from January 2006 to August 2016. Each case was classified as either confirmed or presumed on the basis of available microbiology/histology and evaluated with respect to site of disease, infectivity, demographics, mycobacterial sensitivities and Human Immunodeficiency Virus (HIV) status.
Results
448 cases were identified, 370 confirmed. There were 307 cases of pulmonary tuberculosis of whom two‐thirds (190/307) were smear positive; 154 cases of extra‐pulmonary tuberculosis – mostly nodal (65) or pleural (45); and 21 cases of disseminated tuberculosis. Three‐quarters (324/448) of cases were identified in the immigrant population – eighty percent (261/324) from Papua New Guinea (PNG). Of the remaining 124 cases, there were forty Torres Strait Islanders and nineteen Aboriginal Australians. Where mycobacterial sensitivities were known, two‐thirds were fully sensitive (244/364); 41 mono‐resistant; 78 multidrug resistant; and one extensively drug resistant. Rates of HIV co‐infection were less than three percent (10/357); HIV status was not known in twenty percent of cases (91/448).
Conclusion
Tuberculosis remains a significant public health problem in Far North Queensland. Total case numbers have increased three‐fold since they were first audited in 1997. Much of the excess case burden comes from the immigrant population. Although PNG continues to account for the majority, the number of positive notifications in patients from other countries has increased five‐fold since 2010. Rates of tuberculosis amongst Aboriginal Australians have fallen in response to policy changes borne out of previous audits. Tuberculosis in Torres Strait residents, however, has increased from twelve cases in 1993–2002 to forty in 2006–2016. Additionally, rates of sputum smear positivity and drug resistance are higher in Far North Queensland than nationally.
Grant Support
Nil
Declaration of interest
none.
TO‐144: Audit of tuberculosis screening for health care workers in the Hunter New England Health Service
Xiao Ya Hu1, Samuel Stephens2, Joshua Tobin2, David Arnold1
1Department of Respiratory and Sleep Medicine, John Hunter Hospital, NSW, Australia, 2Joint Medical Program, University of Newcastle, NSW, Australia
Aim
All NSW public hospitals are required to screen new health care workers (HCWs) identified as high risk for tuberculosis (TB) with tuberculin skin testing (TST), followed by a chest x‐ray (CXR) if their TST is positive. HCWs diagnosed with TB disease or latent TB infection (LTBI) will be referred for further management.
This audit was undertaken to determine the incidence of TB and LTBI among HCWs in the Hunter New England Health Service (HNEHS), and their management following diagnosis.
Methods
An audit of the TB database Clinic Surveillance System was performed. Data from HCWs including students were collected from 2012 to 2015. This included country of birth, TST/Two‐step results, TB/LTBI diagnosis, and management options.
Results
900 high risk HCWs were audited. Most were born in Australia (36%), followed by China (9%), India (9%) and Malaysia (7%). Australian‐born HCWs had lower rates of positive TST (16%) compared to those born overseas (54%).
| Test | Result | Number of HCWs |
|---|---|---|
| TST | Positive | 340 |
| Negative | 458 | |
| Defaulted | 3 | |
| Two‐Step | Positive | 25 |
| Negative | 70 | |
| Defaulted | 4 |
Of the 365 HCWs who had a positive TST/Two‐Step, there was 1 case of TB disease, 356 cases of LTBI, 2 with TST reversion and 6 who defaulted on their CXR.
| Management of LTBI | Number of HCWs | |
|---|---|---|
| Education | 282 | |
| Serial CXR | Attended | 10 |
| Defaulted | 32 | |
| Respiratory referral | ||
| QuantiFERON‐TB Gold In‐Tube (QFT‐GIT) | Positive | 6 |
| Negative | 21* | |
| Defaulted | 4 | |
| Treatment | 7 | |
*included 2 with TST reversion
Conclusion
There was 1 (0.1%) case of TB disease and 356 (40%) cases of LTBI out of 900 high risk HCWs screened in the HNEHS. Only 7 (2%) HCWs received treatment for LTBI while the majority (79%) received education only. There was a high rate of nonattendance for serial CXR follow‐up (76%) and a high rate of negative QFT‐GIT following a positive TST (78%).
Grant Support
Nil
Declaration of interest
Nil
TO‐145: Transplanting the human respiratory virome
Alicia B. Mitchell1,2,3, Bassel Mourad2,3, Monique A. Malouf1, Mark Benzimra1, Lucy C. Morgan4, Brian G. Oliver2,3, Allan R. Glanville1
1Lung Transplant Unit, St Vincent's Hospital, Sydney, Australia, 2University of Technology, Sydney, Australia, 3Woolcock Institute, Sydney, Australia, 4Concord Clinical School, University of Sydney, Australia.
Introduction
The pulmonary component of the human respiratory virome (a subset of the human microbiome) is transplanted into the recipient at the time of lung transplantation (LTX). We explored the dynamics of virome transplantation and the role of intercurrent community acquired respiratory viruses (CARV).
Methods
A single centre, prospective, longitudinal study with measures of viral load in recipient nasopharyngeal swabs prior to LTX, swabs of explanted lungs, donor lungs prior to implantation and bronchoalveolar lavage (BAL) on post‐operative days 1, 7, 21, 42, 63, 84. Samples were processed to isolate nucleic acids, followed by RNA extraction, cDNA synthesis and qPCR for CARV (Human Rhinovirus, Respiratory Syncytial Virus, Influenza A and B, Parainfluenza Virus 1, 2, 3, and Human Metapneumovirus).
Results
18 consecutive LTX subjects (bilateral: heart lung = 17:1) (age 49 ± 13 years, mean ±SD) (M: F= 9:9) were recruited. Follow up was 51±36 days, range 2–108 days. The most frequent CARV was Influenza A, followed by influenza B. In 4 individuals, influenza A virus was detected on the swab of the explanted lung at a low viral load, and in 3 of these, Influenza A was also detected in the day 1 BAL at an increased viral load. Multiple patients had Influenza A detected in consecutive BAL from post‐operative days 1, 7 and 21, while Influenza B and Parainfluenza 1/2 were detected from day 21. Indication for transplant was not a determinate of viral detection.
Conclusion
Viral load increases in subjects at the time of LTX, likely associated with immunosuppression. CARV appear to be part of the transplant respiratory virome as analysed by BAL, showing progressive expansion of select populations following LTX. The long‐term outcomes associated with the ongoing presence of CARV may be elucidated following this longitudinal study.
Grant Support
Nil
TO‐146: Paediatric tuberculosis in Timor‐Leste: opportunities for improving recognition, diagnosis and prevention
Hersch NL1 , Hall C1 ,2, Santos R1 , Nourse C1 ,3,4, Francis JR1 ,5,6
1Bairo Pite Clinic, Dili, Timor‐Leste, 2Castle Hill Hospital, Cottingham, United Kingdom, 3Lady Cilento Children's Hospital, Brisbane, Australia, 4University of Queensland, Brisbane, Australia, 5Royal Darwin Hospital, Darwin, Australia, 6Menzies School of Health Research, Darwin, Australia
Introduction/Aim
Timor‐Leste has the highest incidence of TB in Southeast Asia but a relatively low rate of paediatric notifications. Bairo Pite Clinic (BPC) in Dili manages more than a fifth of all TB cases in the country. Improved understanding of TB epidemiology in Timor‐Leste will inform quality improvement activities focused on recognition, accurate diagnosis and prevention of TB in children. We aimed to describe the epidemiology and diagnostic features of notified paediatric TB cases at BPC and to compare this to national paediatric TB notification rates.
Methods
Prospective collection of demographic, clinical and laboratory data for all patients diagnosed with TB at BPC between January 2014 and December 2014 inclusive. Comparison is made with national notification data with respect to paediatric notification rates.
Results
In total, 4090 TB cases were notified. Of these, 426 (10%) were children aged <15y. BPC notified 886 cases, of which 110 (12%) were aged <15y. Contact with a known TB case was reported in 43/110 (39%) BPC cases; 15 (14%) were identified through screening household contacts of infectious index cases. Evidence of BCG vaccination was documented in 36/110 (33%). Malnutrition was identified in 39/110 (35%); HIV in 2/110 (2%). Pulmonary TB was diagnosed in 78/110 (71%) BPC cases and 318/426 (75%) paediatric cases nationally. Bacteriological confirmation occurred in 5/78 (6%) pulmonary cases at BPC and 36/318 (11%) cases nationally. In districts other than Dili and Baucau, 29/131 (22%) paediatric pulmonary TB cases were sputum smear positive.
Conclusion
Paediatric TB is common in high TB burden settings such as Timor‐Leste but is under‐recognised. Malnutrition is an important risk factor; HIV co‐infection is rare. Opportunities for prevention include improved BCG coverage and implementation of household contact tracing. Consideration should be given to improved specimen collection and strategic use of PCR to improve diagnostic certainty.
Grant Support
English Family Foundation
TO‐147: Airway epithelial innate immune responses to coronaviruses
Su‐Ling Loo1, Alan Hsu1, Nathan Bartlett1, Peter Wark1,2
1Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and The University of Newcastle, Newcastle, New South Wales, Australia, 2Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, New South Wales, Australia
Introduction/Aim
Despite the recurring emergence of novel pathogenic coronaviruses (CoVs) SARS‐CoV (2002) and MERS‐CoV (2012), there is a lack of understanding of host immunity and disease mechanisms during respiratory infection with CoVs. In this study, we characterised the innate immune responses of differentiated primary bronchial epithelial cells (pBECs) to infection with related less virulent OC43‐CoV and 229E‐CoV.
Methods
Human pBECs were obtained from subjects by brushing during bronchoscopy. Cells were grown at the air liquid interface (ALI) until differentiation with cilia beat and mucus production was observed (25–30 days). Cells were infected at a multiplicity of infection (MOI) 0.1or 1 with OC43‐CoV or 229E‐CoV for 6, 24, 48, 72, 96 hours and 7 days. Supernatants, total cell protein extracts and RNA were collected at each time point to measure expression of pro‐inflammatory‐ and anti‐viral‐cytokines, and virus replication.
Results
OC43‐CoV and 229E‐CoV demonstrated different viral replication kinetics. 229E‐CoV replicated earlier and more efficiently, peaking between 48 and 72 hours. This was associated with an activation of the innate host response, with induction of type I interferon (IFN‐β), and IFN stimulated genes, CXCL‐10 and viperin. In contrast, replication of OC43‐CoV peaked later between 96 hours and 7 days. This virus demonstrated attenuated levels of IFN‐β, CXCL10 and viperin. We have begun to investigate virulence factors that control epithelial responses to CoV. Sequence analysis of viral proteins (EMBO Needle) revealed only 49.2% identical matches between OC43 and 229E highlighting the potential for variation in host (epithelial)‐virus interaction.
Conclusion
This study demonstrated that both OC43 and 229E‐CoVs replicated in differentiated pBECs, but they induce a divergent innate immune response potentially linked to their different replication kinetics. Understanding the host‐virus interaction for these less virulent coronaviruses will give insight into pathogenic mechanisms underpinning SARS‐CoV and MERS‐CoV‐induced respiratory disease.
Grant Support
University of Newcastle Research Scholarship UNRSC
Declaration of Interest
The authors have no conflict of interest.
TO‐148: Influenza and bacterial co‐infections: the Gold Coast Hospital and Health Service (GCHHS) experience
Li Li Chong1, Siddharth Sharma1,2,3, Pathmanathan Sivakumaran1,2,3
1Gold Coast Hospital and Health Service, 2School of Medicine, Griffith University, 3School of Medicine, Bond University
Introduction/Aim
Seasonal influenza infections are a leading cause of mortality and morbidity. Literature suggests that bacterial co‐infections complicate 20‐33% of influenza cases and contribute to a more severe and prolonged course of illness. The challenge in clinical practice remains in the identification of patients who will benefit from empirical antibiotics.
Methods
This is a retrospective audit of patients with influenza infection diagnosed on viral nasopharyngeal swab in the GCHHS between July and September 2015. Demographics, clinical and microbiological data, complications and outcomes were collected. Data on antibiotic prescription was also collected. Patients with and without bacterial co‐infection were compared.
Results
481 patients were diagnosed with Influenza infection on viral nasopharyngeal swab. Bacterial co‐infection was present in 52 (11%) patients. The most common co‐infecting bacterial pathogen is Staphylococcus aureus (n=13, 22%), Streptococcus pneumoniae (n=11, 18%) and Pseudomonas aeruginosa (10, 17%). Chronic lung disease and COPD were associated with a significantly higher risk of bacterial co‐infection (p<0.05). Other co‐morbidities examined including active smoking, active malignancy, chronic cardiovascular disease, end‐stage renal failure, diabetes mellitus and immunosuppressed or immunocompromised states did not achieve statistical significance. 218 (51%) patients who did not have microbiological findings of bacterial co‐infection received antibiotics. Prescription of antibiotics in this group of patients resulted in no significant difference in in‐hospital mortality (p=0.22). In‐hospital mortality, length‐of‐stay and ICU admission were significantly higher in patients with bacterial co‐infection compared with those without, although 30‐day mortality was similar between the two groups.
Conclusion
The incidence of bacterial co‐infection in our cohort of patients is lower than anticipated. Our findings suggest a probable overuse of antibiotics. A group of patients who may benefit from empirical treatment with antibiotics is those with chronic lung disease and COPD. A prospective study to develop a scoring system could help identify patients who would benefit from empirical antibiotics.
Grant Support
Nil
Chronic Obstructive Pulmonary Disease 4
TO‐149: Increased proportion of slow decliners in patients with alpha‐1 protease inhibitor (A1‐PI) deficiency following treatment with A1‐PI
Prof. N. Gerard McElvaney, MD1 , Dr Niels Seersholm, MD2 , Prof. Kenneth R. Chapman, MD3 , Dr Marion Wencker, MD4 , Dr Michael Fries, PhD5 , Mr Oliver Vit, MSc6 , Dr Jonathan Burdon, MD7
1Department of Respiratory Medicine, Beaumont Hospital, Royal College of Surgeons in Ireland, Dublin, Ireland, 2Department of Respiratory Medicine, Gentofte Hospital, Hellerup, Denmark, 3Department of Medicine, University of Toronto, Toronto, Ontario, Canada, 4Global Medical Affairs, CSL Behring, Marburg, Germany, 5Clinical Strategy and Development, CSL Behring, King of Prussia, Pennsylvania, United States, 6Clinical Research and Development, CSL Behring, Bern, Switzerland, 8Department of Respiratory Medicine, St.Vincent's Hospital, Victoria, Australia
Introduction
The RAPID trial (NCT00261833) showed that intravenous A1‐PI treatment (Zemaira®; n=93) can significantly reduce the mean decline in lung density vs. placebo (n=85). Following RAPID, 140 patients completed a 2‐year open‐label Extension trial (NCT00670007) in which all received active treatment. However, it is unclear what proportion of patients had a fast or slow decline in lung tissue loss and if the proportion of fast decliners was reduced following A1‐PI treatment.
Aim
To compare the effect of A1‐PI treatment on the proportion of fast vs. slow decliners in patients completing both RAPID and RAPID Extension.
Methods
Adjusted CT scans were analysed and A loss of >2g/L/yr was used as a cut‐off to define fast decline. Relative proportions of fast (>2g/L/yr) and slow decliners (≤2g/L/yr) were compared using the Fisher's exact test.
Results
During RAPID, a significantly higher proportion of patients receiving A1‐PI were classified as slow decliners vs. placebo (72% vs 50%; p<0.009). When all subjects received A1‐PI in the RAPID Extension, the proportion of subjects classified as fast decliners was similar between the arms (67% vs 75%; p<0.352). [Table1]
| RAPID | RAPID Extension | |||
|---|---|---|---|---|
| A1‐PI | Placebo | A1‐PI–A1‐PI | Placebo–A1‐PI | |
| N=75 | N=64 | N=75 | N=64 | |
| Slow n (%) | 54 (72) | 32 (50) | 50 (67) | 48 (75) |
| Fast n (%) | 21 (28) | 32 (50) | 25 (33) | 16 (25) |
| p‐value | 0.009 | 0.352 | ||
Conclusion
Treatment with A1‐PI therapy is associated with a higher proportion of patients with a slow decline in lung tissue loss compared to placebo. After switching to active treatment there is a progressive shift from fast to slow decliners, further demonstrating the benefit of A1‐PI treatment.
TO‐150: Lysosomal‐associated membrane protein 1 (LAMP‐1) is upregulated in small airway epithelium of smokers and COPD: potential role in autophagy
Mathew Suji Eapen1; Elizabeth Tan1; Chris Ward3; Eugene H Walters1; Sukhwinder Singh Sohal1,2
1NHMRC Centre of Research Excellence for Chronic Respiratory Disease, School of Medicine, University of Tasmania, Hobart, Tasmania, Australia, 2School of Health Sciences, Faculty of Health, University of Tasmania, Launceston, TAS, Australia, 3Institute of Cellular Medicine, Newcastle University, Newcastle upon Tyne, Tyne and Wear, UK
Introduction/Aim
Cigarette smoke causes oxidative stress to the lungs inducing cellular transcriptome and proteome changes. Cells actively recycle damaged material using autophagy pathways through the fusion of autophagosomes and lysosomes forming an “autophagic flux”. However, accumulation or dysregulation of lysosomes leads to disrupted autophagy and consequently a stressed endoplasmic reticulum (ER). The current study evaluates the presence of lysosomal associated membrane protein‐1 + (LAMP1+) lysosomes in the small airway (SA) epithelium of COPD patients and assess physiological outcomes
Methods
SA lung resections from volunteers classified as nine non‐smoking controls (NC), eleven smokers with normal lung function (NLFS), nine mild‐moderate COPD current smokers (CS) and ten ex‐smokers (ES). Staining intensity of LAMP1+ cells was measured as objects per area of epithelium using an imaging software Image ProPlus Version 7.0 and further represented as percent LAMP1+ expression in SA epithelium.
Results
Both COPD‐CS and NLFS groups showed a significant increase in percent LAMP1+ lysosomes in the SA epithelium compared to NC (p<0.001) which significantly decreased in COPD‐ES (p<0.05) but still higher then NC, suggesting both COPD and smoking effect. The normal airway epithelium was devoid of any detectable LAMP1 expression. In NLFS and COPD‐ES the LAMP1+ epithelial lysosomes accumulated at the ER close to the nucleus while in the COPD‐CS the ER was disrupted and a more diffused LAMP1 expression was observed. The percent LAMP1 expression showed positive correlation to patient smoking history (pack‐years) (Spearman's rho (rs) 0.6, p = 0.002) while in COPD LAMP‐1 negatively correlated to FEV1/FVC (Spearman's rho (rs) ‐0.45, p = 0.03) and FEF 25–75 (Spearman's rho (rs) ‐0.5, p = 0.02).
Conclusions
Our data suggests that smoking actively stimulates lysosomal accumulation in the SA epithelium and is associated with decrease in lung function in COPD. The consequence of dysregulated lysosome in autophagy warrants further investigations.
Grant Support
NHMRC and Clifford Craig Foundation
TO‐151: Evaluating blood eosinophils and exacerbation history to predict inhaled corticosteroids response in COPD
Dimitar Sajkov1presenting on behalf of Peter M. A. Calverley2, Kay Tetzlaff3,4, Claus Vogelmeier5, Leonardo M Fabbri6, Helgo Magnussen7, Emiel FM Wouters8, Bernd Disse3, Helen Finnigan9, Guus M Asijee3, Henrik Watz7
1Australian Respiratory and Sleep Medicine Institute, Flinders Medical Centre, Adelaide, South Australia, 2 Institute of Ageing and Chronic Disease, Aintree University Hospital, Liverpool, United Kingdom, 3 Respiratory Medicine, Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany, 4 Department of Sports Medicine, University of Tübingen, Tübingen, Germany, 5 Department of Medicine, Pulmonary and Critical Care Medicine, University Medical Center Giessen and Marburg, Philipps‐Universität Marburg, Member of the German Center for Lung Research (DZL), Marburg, Germany, 6 Department of Metabolic Medicine, University of Modena & Reggio Emilia, Modena, NOCSAE, AUSL Modena, Baggiovara, Italy, 7Pulmonary Research Institute, Lung Clinic Grosshansdorf, Airway Research Center North, German Center for Lung Research (DZL), Grosshansdorf, Germany, 8Department of Respiratory Medicine, Maastricht University Medical Center, Maastricht, Netherlands, 9Department of Biostatistics and Data Sciences, Boehringer Ingelheim, Bracknell, United Kingdom
Introduction/Aim
Inhaled corticosteroids (ICS) are used to reduce the rate of chronic obstructive pulmonary disease (COPD) exacerbations. Debate continues over use of blood eosinophils (EOS) to predict ICS response, with some suggesting a cut‐off of ≥2%.1In the WISDOM study (NCT00975195), this response was driven by patients with higher EOS levels (≥4% or ≥300 cells/μL).2We analysed WISDOM data stratified by prior exacerbations and EOS levels to determine if the ICS responder group could be better specified.
Methods
Post hoc analysis of the rate of moderate/severe exacerbations after complete ICS withdrawal using a negative binomial regression model to estimate exacerbations rate according to number of prior exacerbations (<2 and ≥2, estimated based on the number of courses of antibiotics or steroids in the past year) and EOS subgroups.
Results
High EOS counts (≥400 cells/μL) were associated with increased exacerbations rate after complete ICS withdrawal only in patients with ≥2 prior exacerbations.
Figure: Rate ratios (ICS withdrawl/ICS) for moderate or severe exacerbations by EOS subgroup and exacerbations history

Conclusion
Withdrawal of ICS increased the rate of exacerbations only in patients with both raised EOS (≥400 cells/μL) and a history of frequent exacerbations. In patients who do not meet these criteria, ICS may not be as effective as is commonly assumed.
References
1. Pascoe S et al. Lancet Respir Med 2015, 3, 435–442. 2. Watz H et al. Lancet Respir Med 2016, 4, 390–398
Grant Support
The study was funded by Boehringer Ingelheim.
Declaration of Interest Statement
DS has no real or perceived conflict of interest that relates to this presentation. PMAC has advised various pharmaceutical companies including Boehringer Ingelheim, GlaxoSmithKline, Astra Zeneca, Novartis, Nycomed, Chiesi, Almirall and Takeda on the design and conduct of clinical trials and has spoken at meetings supported in whole or part by these companies. KT, BD, HF and GMA are employees of Boehringer Ingelheim. CV has served as an advisor or consultant for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Takeda; a speaker or a member of a speakers bureau for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Takeda; and has received grants for clinical research from GlaxoSmithKline and Grifols. LMF has consultant arrangement with, is lecturer for, is on the advisory board for, and receives research support from Boehringer Ingelheim and is lecturer and member of the advisory board for Pfizer. HM has relationships with Boehringer Ingelheim, BerlinChemie, Almirall, AstraZeneca, Chiesi, Novartis, Takeda, AB2BIO, Bayer, and Intermune. EFMW reported serving on advisory committees of Nycomed and as a speaker for AstraZeneca, GlaxoSmithKline, and Novartis; he has received research support from AstraZeneca and GlaxoSmithKline. HW has received consultancy fees and travel support from Takeda; has received consultancy fees from Almirall, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis; has received research support from AstraZeneca and GlaxoSmithKline; has received lecture fees from AstraZeneca, Almirall, Boehringer Ingelheim, BerlinChemie, GlaxoSmithKline, Merck, and Novartis; has received payment for development of educational presentations from Boehringer Ingelheim and BerlinChemie; and has received travel support from AstraZeneca, GlaxoSmithKline, and Novartis.
TO‐152: Reduced pulmonary artery distensibility on dynamic CT correlates with increased emphysema and impaired right ventricular function
Martin MacDonald1 , Christian Osadnik1,2, Paul King1, Siobhan Lockwood, Mark McCusker3 , Sinan Al‐Hedathi3, John Troupis4, Philip G Bardin1
1Monash Lung and Sleep, Monash Medical Centre, Melbourne, Australia, 2Monash University, Department of Physiotherapy, Melbourne, Australia, 3Monash Heart, Monash Medical Centre, Melbourne, Australia, 4Monash imaging, Monash Medical Centre, Melbourne, Australia
Introduction/Aim
Pulmonary hypertension (PH) in COPD is associated with increased disability and reduced survival. Detection of PH in COPD is challenging due to limitations of echocardiography and potential risks associated with right heart catheterization (RHC). The main pulmonary arteries (PA) become progressively less distensible in PH. Previous studies have shown PA distensibility to correlate well with measured mPAP at RHC. We assessed relationships between PA distensibility, cardiac function and emphysema index measured using dynamic ECG‐gated MDCT.
Methods
34 patients with stable COPD (mean[SD] age 65.8[9.7], FEV1% 43.9[22.5], 18 male) underwent dynamic retrospective ECG‐gated MDCT. Emphysema was quantified by CT densitometry based upon a density threshold of <−950 Hounsfield Units (HU). The main pulmonary artery cross‐sectional area (CSA) was measured at 10% intervals from 0‐90% of the R‐R interval. PA distensibility (%) was calculated as ((maximum CSA – minimum CSA)/minimum CSA) x 100. Cardiac function parameters were assessed using semi‐automated software with manual correction if required. The relationship of PA distensibility with both emphysema index and right ventricular ejection fraction (RVEF) was tested via Pearson's r.
Results
Mean[SD] PA distensibility was low (16.5[5.9]%). PA distensibility was significantly negatively correlated with emphysema index (r=−0.365, p = 0.031) and positively correlated with reduced RVEF (r=0.483, p=0.0025).
Conclusion
Dynamic MDCT permits simultaneous evaluation of emphysema, PA pressure and right ventricular performance. Increased severity of emphysema appears associated with reduced PA distensibility. Impaired PA distensibility appears associated with decreased RVEF. Dynamic MDCT provides a valuable tool for assessment of heart‐lung interaction in COPD.
Grant Support
Nil
TO‐153: Antimicrobial prescription in patients dying from chronic obstructive pulmonary disease
John Taverner1,2, Lauren Ross2, Claire Bartlett2, Louis Irving2, Natasha Smallwood2
1Department of Respiratory Medicine, Frankston Hospital, 2Department of Respiratory and Sleep Medicine, Royal Melbourne Hospital
Introduction
It is estimated that by 2050 antibiotic resistance will cause 10 million deaths/year, thus outstripping cancer deaths. In patients dying with advanced cancer, dementia, or residing in hospice, antimicrobials are commonly prescribed in the absence of clinical symptoms to support a bacterial infection. The extent and appropriateness of antimicrobial use in patients with chronic obstructive pulmonary disease (COPD) is unknown.
Aim
To review antibiotic prescription at the time of death in patients who died from COPD.
Methods
A retrospective medical record audit was performed for 475 patients who died over twelve years between 2004–2015. Patients were analysed within three groups: Group 1 – radiographic consolidation, Group 2 ‐ elevated inflammatory markers (WCC) or (CRP) with no radiographic consolidation and Group 3 ‐ normal inflammatory markers and no radiographic consolidation.
Results
Two hundred and twenty one patients died from COPD. Median age was 80 years and 136 (60%) were male. Median respiratory function: FEV1 0.8L (41%), FVC 2.0L (73%) and DLco 9 (41%). 109 (49%) patients used home oxygen and 156 were ex‐smokers (70.6%).
Antimicrobials were prescribed to 201 (91%) patients (Table 1). Antibiotic number and duration of use were similar in all three groups. 57 (59%) Group 2 patients received ceftriaxone and 34 (35%) received azithromycin first line, which are recommended treatments for pneumonia but not acute exacerbations of COPD (AECOPD). Similarly 24 (46%) Group 3 patients (without objective evidence of infection) received ceftriaxone and 16 (31%) received azithromycin.
Conclusion
Almost all patients who died from COPD received antimicrobials during their final hospital admission, irrespective of objective evidence suggesting infection. While antibiotics were mainly prescribed according to guidelines in patients with pneumonia, guideline or evidence based prescription of antibiotics occurred less in patients dying with AECOPD or without objective evidence of infection.
Grant Support
Nil
Table 1. First line antimicrobial use during the terminal admission
| Group 1 (n=72) | Group 2 (n=97) | Group 3 (n=52) | |
|---|---|---|---|
| Median time to death (days) | 6 (1–51) | 7 (1–66) | 6 (1–30) |
| Received antimicrobials | 68 (94%) | 91 (94%) | 42 (83%) |
| Median no. (range) | 3 (0–8) | 2 (0–8) | 2 (0–8) |
| Median duration (range) in days/agent | 4 (1–50) | 3 (1–23) | 3 (1–22) |
| 1st line antimicrobial/s | |||
| Ceftriaxone | 52 (72%) | 57 (59%) | 24 (46%) |
| Azithromycin | 49 (68%) | 34 (35%) | 16 (31%) |
| Benzylpenicillin | 7 (10%) | 16 (16%) | 4 (8%) |
| Doxycycline | 4 (6%) | 17 (18%) | 8 (15%) |
| Roxithromycin | 7 (10%) | 16 (16%) | 7 (13%) |
| Amoxicillin‐clavulanic acid | 2 (3%) | 15 (15%) | 4 (8%) |
| Other | 27 (38%) | 25 (26%) | 16 (31%) |
| Median WCC (range) | 13.2 (3.1‐48.2) | 14.2 (4–29.9) | 9.2 (3.9‐10.9) |
| Median CRP (range) | 86 (2–430) | 83 (2–394) | 13 (2–26) |
| Positive sputum culture | 26 (36%) | 29 (30%) | 6 (11%) |
| SMARTCOP score | 4 (0–8) | N/A | N/A |
| CURB‐65 score | 3 (0–5) | N/A | N/A |
TO‐154: Accuracy of transcutaneous carbon dioxide measurement for change over time
James Fingleton1,2,3, Steve MCKINSTRY1 , Janine Pilcher1, Mark Weatherall3, Richard Beasley1,2,3, George Bardsley1
1Medical Research Institute of New Zealand, Wellington, New Zealand, 2Capital and Coast District Health Board, Wellington, New Zealand, 3University of Otago Wellington, Wellington, New Zealand
Introduction/Aim
The gold standard for measuring changes in arterial CO2 in response to therapy is arterial (PaCO2) or capillary (PcapCO2) blood gas measurement. However these measurements are painful and do not allow real‐time monitoring. Transcutaneous carbon dioxide (PtCO2) monitoring is painless and allows continuous monitoring of CO2 and oxygen levels and. The limits of agreement for PtCO2 compared with PaCO2 are too wide for PtCO2 to be used to diagnose hypercapnia, but the limits of agreement for change in CO2 over time are not well described. We hypothesised that the PtCO2 trend may show more precise agreement and be sufficiently accurate to guide treatment.
Methods
Paired PtCO2 (SenTec AG, Switzerland) and PcapCO2 data were available from 80 adults with an exacerbation of COPD who took part in a study investigating the effect of oxygen driven versus air driven nebulisers. Repeat measurements were taken after 35 minutes. A limits of agreement analysis was performed, with estimation of the bias by paired t‐test for the differences in the two measurements.
Results
The limits of agreement between PtCO2 and PcapCO2 were approximately plus or minus 4mmHg for each individual measurement obtained (n=160). The mean change in PtCO2 was 1.7mmHg (SD 2.2, range −2.5 to 8.0) and the mean change in PcapCO2 was 1.7mmHg (SD 2.3, range −3.0 to 9.0), revealing an estimate of bias for change in CO2 of 0.03mmHg (95% CI −0.44 to 0.38) p=0.89.
Conclusions
Despite reasonably large limits of agreement between the two methods for individual measurements, there was no significant difference in the mean change in PCO2 over time measured by the two methods. Transcutaneous devices can be used to monitor the effect of change in PaCO2 over time without any significant bias, in this population.
Grant Support
Health Research Council, 14/835
Late Breaking Abstracts
TOL‐001: Lung function trajectories over the life span, their associated childhood factors and consequences: a population based longitudinal cohort
Bui DS1 , Burgess JA1 , Lodge C L1 , Bui MQ1 , Lowe A1 , Perret J1 , Bowatte G1 , Abramson MJ2 , Thompson BR 3, Katie J.Allen4, James AL5 , Thomas PS6 , , Hamilton GS7 ,10, Frith PA8 , Johns DP9 , Walters EH1 ,9, Matheson MC1 , Dharmage SC1
1Allergy and Lung Health Unit, The University of Melbourne, Victoria, 2School of Public Health & Preventive Medicine, Monash University, Victoria, 3Allergy, Immunology & Respiratory Medicine, The Alfred, Melbourne, Victoria, 4Murdoch Childrens Research Institute, Royal Children's Hospital and University of Melbourne, 5Department of Pulmonary Physiology and Sleep Medicine, Sir Charles Gairdner Hospital, Western Australia, 6University of New South Wales, 7Department of Respiratory and Sleep Medicine, Monash Health, Melbourne, Victoria, 8Department of Respiratory Medicine, School of Medicine, Flinders University, Adelaide, 9School of Medicine, University of Tasmania, Hobart, Tasmania, 10School of Clinical Sciences, Monash University, Clayton, Australia
Introduction/Aim
Individuals with different patterns of lung function growth and decline may have different risks for developing COPD. We investigated trajectories of lung function from childhood to middle age and their associated childhood factors.
Methods
Using 2142 subjects from the Tasmanian Longitudinal Health Study, pre‐bronchodilator FEV1, measured at 7, 13, 18, 45, 50 and 53 years, was modelled with Group Based Trajectory Modelling. Logistic regression was used to investigate the relationship between childhood factors and trajectory groups.
Result
The best fit model showed six distinct trajectories (Figure 1). Based on initial lung function at 7 years, lung function growth and decline rates, the trajectories were labelled as “early low, reduced growth, accelerated decline” (7.4%; n = 159), “early normal/high, normal growth, accelerated decline” (5%; n = 107), “early low, normal growth, normal decline” (28.7%; n = 615), “early low, accelerated growth, normal decline” (4.2%, n = 90), “persistently high” (14%; n = 300) and “normal” (40.7%; n = 871). The first three trajectories had increased risk of COPD (post‐bronchodilator FEV1/FVC < LLN) at age 53 years compared with the “normal” group. Childhood asthma, bronchitis, pneumonia/pleurisy, maternal asthma and maternal smoking were positively associated with these three trajectories while negative associations were observed for breast feeding and childhood overweight.
Figure 1.

Trajectories of FEV1 from 7 to 53 years of age. The six trajectories represent the latent growth patterns of lung function.
Conclusion
This is the first study to develop lung function trajectories from childhood to middle age in a general population. We identified three trajectories for increased risk of COPD: (1) only accelerated lung decline in adulthood, (2) low initial lung function in childhood with normal growth and normal decline, and (3) low initial lung function in childhood with reduced growth and accelerated decline. Important modifiable childhood risk factors for these three trajectories included exposure to maternal smoking in childhood and a lack of exclusive breast feeding in very early life. Strategies to maximize lung function growth from early life as well as preventing accelerated decline are important for COPD prevention.
Grant Support
National Health and Medical Research Council of Australia, Clifford Craig Medical Research Trust of Tasmania; Victorian, Queensland & Tasmanian Asthma Foundations
Declaration of Interest Statement
There is no conflict of interest.
TOL‐002: A fast track clinic improves diagnosis and treatment times for those investigated for lung cancer in rural New Zealand
Davies P1 , Williams S2 , Glaze M4 , Johnson B3 , Schick C4 , Iles S5
1,2General Medicine, 3Clinical analysis, 4Radiology, 5Respiratory Medicine, Whangarei Hospital, Northland, New Zealand
Introduction
In 2009 a Respiratory Fast Track Clinic (RFTC) was introduced successfully by the Southern District Health Board. We sought to improve on this model by incorporating further methods of biopsy in a similar rural population in New Zealand (NZ).
Methods
The RFTC introduction was bi‐phasic, initially patients had their CT scan on their first specialist assessment (FSA) (phase 2). After two months biopsy was incorporated (bronchoscopy, CT‐guided biopsy, ultrasound‐guided biopsy) into the RFTC (phase 3). Patients with suspected lung cancer were identified between December 2015 and May 2016 prior to the RFTC (phase 1) and the time for the diagnostic pathway was measured and compared to those in phases 2 (May to July 2016) and 3 (July to October 2016). Median times were used for statistical analysis as some patients underwent long waits for personal or clinical reasons thereby distorting the data.
Results
212 were investigated for suspected lung cancer. Prevalence by age was normally distributed peaking 61–70, with preference for lower socio‐economic deciles, equal gender and proportional ethnic distributions. Endobronchial ultrasound (EBUS) was the most utilised biopsy method, followed by bronchoscopy.
Time from GP referral to FSA between phase 1–3 improved significantly (p = 0.005). Similarly, time from FSA to diagnosis and treatment improved significantly, median times reducing from 15 to 0 (p = <0.001) and from 37 to 24 days (p = 0.004) respectively between phases 1–3. (Table 1)
Table 1.
The effectiveness of the rapid access clinic on pathway timing from referral to commencing treatment
| Measurement | Average difference in days phase 1 vs phase 3 | P= |
|---|---|---|
| GP referral to Appointment | −4.5 | 0.005 |
| Appointment to Diagnosis | −16.6 | <0.001 |
| Appointment to Treatment | −13.8 | 0.004 |
| GP referral to Treatment | −17 | 0.74 |
Appointment = first consultation with hospital specialist
GP referral = date of the referral to specialist from general practitioner
Diagnosis = date of diagnosis (biopsy report date or CT report date if no biopsy taken)
Treatment = day of treatment (chemotherapy, radiotherapy, surgery or best supportive care)
Discussion
The RTFC significantly shortened time to diagnosis and treatment in our population. To the best of our knowledge, this is the first study demonstrating a reduction in time to treatment for lung cancer patients in NZ in a fast track clinic. A previous study (1), using EBUS as the initial investigation resulted in faster treatment and seemed to improve survival. EBUS could easily be incorporated into the RFTC model and this may confer a survival advantage.
The Lancet Respiratory Medicine, Volume 3, Issue 4, 282–289, 2015
Grant Support
None
Conflicting Interests
None
TOL‐003: DiffQuik stained cytology smears provide improved malignant cell DNA yields from lymph nodes at endobronchial ultrasound transbronchial needle aspiration (EBUS‐TBNA)
Fielding D1, A Dalley3, Bashirzadeh F1, Singh M2, Nandakumar L2, 4, McCart Reed A3 , Black D3 , Waddell N5, Stephen Kazakoff5, Katia Nones5, John Pearson5, Lakhani S 2,3,4 Simpson P3
1Royal Brisbane and Womens Hospital Departments of Thoracic Medicine, 2Queensland Pathology, 3The University of Queensland Centre for Clinical Research, 4The University of Queensland School of Medicine, 5QIMR Berghofer Medical Research Institute
Introduction/Aim
We are currently optimising procedural aspects of Endobronchial Ultrasound Transbronchial Needle Aspiration (EBUS‐TBNA) with the aim of converging rapid on‐site evaluation (ROSE) with Targeted Amplicon Sequencing (TAS) of “hotspot” DNA mutations and RNA translocations to enhance lung cancer diagnosis. Here we explore a comparison of cellularity and DNA yields between DiffQuik stained cytology smears and formalin fixed paraffin embedded (FFPE) cell blocks.
Methods
In a prospective study of 63 consecutive patients with lung malignancy (m/f ratio 1.2, mean 66.6 ± 9.5 years), EBUS‐TBNA was performed using 2–5 (median 3) aspirates with an Olympus needle (NA‐201SX‐4021). Smear and cell block tumour cell abundance were assessed by experienced cytopathologists on a scale from 0 (absent) to 4 (abundant). Genomic DNA was isolated from both smears and blocks, quantified then sequenced using the TruSeq Amplicon Cancer Panel (Illumina, San Diego, CA) on a MiSeq platform. Diff quik slides were digitally scanned before being used for DNA exraction.
Results
Unexpectedly, the overall cellularity was higher in the cytology slides than the cell blocks: 35/63 cases had 3–4 scores for tumour cell abundance compared with 22/64 cell blocks ( p < 0.05, Chi‐squared test).39 cases provided adequate DNA for amplicon sequencing (>50 ng). The highest DNA yields from cell blocks and cytology slides were 4.80 µg and 15.96 µg respectively, with mean (standard deviation; SD) DNA yields from cell blocks (439 ng (858 ng)) and cytology slides (1745 ng (3173 ng)) differing significantly (p < 0.001, paired t‐test). Extracted DNA was of good quality exhibiting DNA fragment sizes of up to 10Kb on a 1% agarose gel.
Conclusion
DiffQuik stained cytology slides present numerous advantages over FFPE cell blocks as a source of DNA for molecular pathology including increased DNA yield, and an immediate visual confirmation of adequate malignant cell sampling.
Grant Support
Pathology Queensland Study Education and Research Grant.
Conflict of Interest
Nil
TOL‐004: Asthma control during pregnancy, 17q21 variants and childhood‐onset asthma
Matthew Morten1, Dr Adam Collison1, Dr Vanessa Murphy1, Daniel Barker3, Dr Joseph Meredith1,7, Heather Powell2,4, Dr Paul Robinson5, Prof Peter Sly6, Prof Peter Gibson2,4, Prof Joerg Mattes1,7
1Priority Research Centre GrowUpWell®, Hunter Medical Research Institute and University of Newcastle, NSW, Australia 2305, 2Department of Respiratory&Sleep Medicine, John Hunter Hospital, Newcastle, NSW, Australia 2305, 3Faculty of Health, University of Newcastle, NSW, Australia 2308, 4Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute and University of Newcastle, NSW, Australia 2305, 5Department of Paediatric Respiratory & Sleep Medicine, The Children's Hospital at Westmead, Sydney, NSW, Australia 2145, 6Centre for Children's Health Research, University of Queensland, South Brisbane, Queensland, Australia 4101, 7Department of Paediatric Respiratory & Sleep Medicine, John Hunter Children's Hospital, Newcastle, NSW, Australia 2305
Introduction/Aim
Our aim was to investigate the effect of FeNO‐guided versus symptom‐guided asthma management during pregnancy on the prevalence of childhood‐onset asthma.
Methods
The Growing Into Asthma (GIA) study is a prospective longitudinal birth cohort following up the offspring of asthmatic women involved in a double‐blind RCT comparing a treatment algorithm using FeNO in combination with asthma symptoms ascertained with the asthma control questionnaire [ACQ] (FeNO Group) against a treatment algorithm using ACQ only (clinical group) which found a 50% reduction in asthma exacerbations during pregnancy in the FeNO group. 140/179 (78%) consenting children completed the follow‐up at 4–6 years of age. Four asthma‐associated 17q21 single‐nucleotide polymorphisms (SNPs) rs7216389, rs8076131, rs9303277 and rs2290400 were genotyped.
Results
We found that FeNO‐guided asthma management during pregnancy significantly reduced the odds ratio for childhood‐onset asthma in the offspring (OR 0.45, 95% confidence interval [CI] 0.21‐0.95, p = 0.04). Furthermore frequent wheeze in the past 12 months (OR 0.26; CI 0.08‐0.81, p = 0.02), wheeze ever (OR 0.49; CI 0.25‐0.98, p = 0.04) and recurrent bronchiolitis (OR 0.20; CI 0.06‐0.62, p = 0.005), were less common in the FeNO group. Asthma was significantly associated with all four variants at 17q21 (p0.01) only in children with a past history of bronchiolitis and this interaction was significant for the majority of SNPs (p = 0.008 to 0.03). Asthma was also associated with ORMDL3 mRNA levels in PBMCs (p = 0.02) only in children with a past history of bronchiolitis and this interaction was significant (p = 0.04). Notably, no interaction between 17q21 variants and the FeNO intervention for the risk of asthma was observed.
Conclusion
FeNO‐guided asthma management during pregnancy significantly reduced asthma prevalence in childhood. 17q21 variants interact with bronchiolitis in early life to increase the asthma risk (gene‐environment interaction), but there is no evidence of an interaction with FeNO guided asthma mangement. Thus the prevention strategy may benefit children with and without variants at 17q21.
Grant Support
NHMRC, Hunter Children's Research Foundation, Hunter Medical Research Institute, John Hunter Hospital Charitable Trust, University of Newcastle Priority Research Centre GrowUpWell
(2017) TSANZ Respiratory Nurses SIG Symposium. Respirology, 22: 18–100. doi: 10.1111/resp.13009.


