Abstract
Face masks have traditionally been used in general infection control, but their efficacy at the population level in preventing transmission of influenza viruses has not been studied in detail. Data from published clinical studies indicate that the infectivity of influenza A virus is probably very high, so that transmission of infection may involve low doses of virus. At low doses, the relation between dose and the probability of infection is approximately linear, so that the reduction in infection risk is proportional to the reduction in exposure due to particle retention of the mask. A population transmission model was set up to explore the impact of population‐wide mask use, allowing estimation of the effects of mask efficacy and coverage (fraction of the population wearing masks) on the basic reproduction number and the infection attack rate. We conclude that population‐wide use of face masks could make an important contribution in delaying an influenza pandemic. Mask use also reduces the reproduction number, possibly even to levels sufficient for containing an influenza outbreak.
Keywords: Influenza, mask use, pandemic, preparedness
1. INTRODUCTION
Pandemic preparedness involves implementation of both pharmaceutical (vaccination and antiviral drugs) and nonpharmaceutical countermeasures. As adequate pharmaceutical supplies will not be available immediately and may be insufficient for the total population, the WHO working group for public health interventions recommends nonpharmaceutical interventions as an important additional control measure.( 1 ) Such measures fall into four groups, aiming to (1) limit international spread of the virus; (2) reduce spread within populations; (3) reduce the individual risk of infection (through personal protection and hygiene measures); and (4) raise public awareness of the risks.( 2 )
Masks have traditionally been used for centuries, for example, during the 17th‐century plagues,( 3 ) the 1918 influenza pandemic( 4 ) and, more recently, the SARS epidemic in 2003. Retrospective case‐control studies showed that mask use by the general public may have offered significant protection against SARS.( 5 , 6 ) Nevertheless, no studies have assessed the efficacy of such mask use in preventing transmission of influenza viruses.( 4 )
This article addresses the following questions:
-
•
What is the efficacy of mask use by healthy uninfected persons in protecting themselves against infection with influenza?
-
•
What might be the effect of population‐wide mask use on the total impact of an influenza pandemic? Does it contain infection, delay spread, and/or reduce the total numbers of people infected?
Applying a mathematical model, we show that mask use at population level can play an important role in delaying and containing an influenza pandemic.
2. METHODS
2.1. Literature Search
A literature search using various search strategies was performed to answer the following questions:
-
•
What are the characteristics of the main transmission routes of the influenza virus?
-
•
What is the efficacy of mask use by a healthy person in preventing infection with influenza virus?
We applied two approaches to quantify infections, considering the risk of infection after exposure at the individual level and modeling the effect of population‐wide mask use on transmission of infection (transmission modeling).
2.2. Virus Infectivity
For exploring the risk of individual infection after exposure, the single hit model of microbial infection( 7 ) provides a general framework for studying the relation between exposure to a certain dose of virus and the probability of becoming infected (= P inf.).
Experimental studies show that influenza A virus is more infectious in humans exposed by aerosol than in humans exposed by nasopharyngeal instillation of droplets.( 2 , 8 , 9 , 10 )
Aerosol inoculation of a few virus particles has been shown to potentially lead to infection while intranasal droplet inoculation requires several hundreds of viruses for infection. Nicas and Jones( 11 ) infer that aerosol inoculation may be 3,200 times more efficient than intranasal inoculation, but because of the high uncertainty in their dose‐response estimates they cannot exclude that these two inoculation routes are equally efficient.
If the virus is released in an entirely susceptible population (as during an influenza pandemic), the average number of secondary cases caused by any infectious subject during the complete infectious period (the basic reproduction number, R 0) is estimated to range from 1.5 to 3.0.( 12 , 13 , 14 , 15 , 16 , 17 )
2.3. Virus Transmission
To estimate the impact of face mask use by the public during an influenza pandemic, a deterministic SIR model was employed. Assuming pandemic spread of the virus, initial immunity was assumed to be absent.
The basic equation we used to predict the basic reproduction number R 0 of an influenza pandemic is:
where b is the risk of transmission per contact, κ is the number of such contacts that an average person in the population would normally have per time unit (in the absence of any disease), and D is the duration of infectivity of an infected person, measured in the same time units as used for κ.( 18 )
Based on this equation, we estimated the effects of mask use (and the inherent reduction of P inf.) on the R 0 of the pandemic.
The presumed effect of mask use was a decrease in the risk of acquiring infection during contact, depending on the filter efficiency (= M eff) of the mask. In case of a low transferred dose it is likely that any decrease in exposure due to mask use causes an approximately proportional decrease in infection risk( 19 ) and hence also in transmission of the virus. Given the high infectivity of the influenzavirus and its relatively low reproduction number, it seems likely that transmission may involve small doses of influenza virus.
Therefore, the probability of transmission per contact b will be reduced by this same fraction M eff and thus R 0 will be reduced with this same fraction as well, on the condition that masks are properly used during all contacts. We will refer to this new R 0 that changes due to interventions as R int.
Therefore,
As masks will probably not be properly used during all contacts with the risk of transmission, we use the “mask coverage” within a population to indicate the proportion of mask use within this population. This mask coverage (= M cov.) is defined as the proportion of contacts that are taking place with the proper use of a certain mask (compared to the total of all contacts within the population).
Only those who wear the mask properly are protected with its mask efficiency (M eff). The remaining proportion (1 – M cov) will not be protected by a mask. This changes the equation for the reproduction number to:
In estimating the possible effects of mask use on the infection attack rate we used the following equation:
Here, the infection attack rate a is the proportion of the population that is infected after the first pandemic wave has passed through a completely susceptible population. During this first wave, the number of infectious contacts per infection is Rint, and the total number of infectious contacts during the wave per person is a Rint. Assuming random mixing, the probability that an individual is not contacted by any infectious person is  . Hence, the probability that an individual is contacted by at least one infectious person is
. Hence, the probability that an individual is contacted by at least one infectious person is  . And because all individuals are susceptible at the start, this same term
. And because all individuals are susceptible at the start, this same term  also gives the probability that an individual is infected. This probability that an individual is infected is, by definition, equal to the infection attack rate a.
also gives the probability that an individual is infected. This probability that an individual is infected is, by definition, equal to the infection attack rate a.
3. RESULTS
3.1. Transmission of Influenza
Influenza is spread mainly by direct or indirect contact transmission, droplet transmission, and aerosol transmission.
3.1.1. Contact Transmission
Contact transmission can occur as influenza viruses can survive on hard, nonporous surfaces (such as stainless steel and plastic) for 24–48 hours; on cloth, paper, and tissues for up to 8–12 hours; and (after transfer from these environmental surfaces) on hands for up to 5 minutes. However, the importance of contact transmission probably varies with the amount of virus present and the type of surface.( 20 )
The effect of mask use on contact transmission is unknown, but it seems reasonable that a face mask reduces contact transmission by preventing wearers from touching their mouths or noses with their hands or other objects potentially contaminated with virus. As face masks are not a standard intervention for the prevention of contact transmission, we focus in this study on the possible effect of mask use on the spread of influenza, transmitted by droplet or aerosol.
3.1.2. Droplet and Aerosol Transmission
Droplet and aerosol transmission occur when contagious droplets or aerosols are produced by an infected host during talking, coughing, or sneezing. Droplets are particles large enough to settle quickly, while aerosols are small enough to remain suspended in air for an indefinite period.( 10 ) Fabian et al. showed that regular exhalation mainly results in aerosol production (>99% of exhaled particles <5 μm), with most people exhaling more than 500 particles per liter of air and influenza virus RNA being detected in the exhaled breath of 33% of influenza patients.( 21 )
Droplets smaller in diameter than a few micrometers are believed to evaporate to about half their initial size. These small liquid particles are usually referred to as “droplet nuclei.”( 22 )
Many guidelines and review articles state that droplet transmission may be the main mode of influenza transmission. However, compelling scientific evidence supports the occurrence and significance of aerosol transmission( 21 , 23 ) and suggests that it plays an important role in the spread of influenza( 24 ) or may even be the dominant way of transmission.( 25 )
Certainly, the different features of droplets and aerosols may affect these types of transmission, thus influencing also the expected mask efficiency in either case. In Table I we summarize the main features for these two types of transmission.
Table I.
Main Features of Aerosol Transmission Versus Droplet Transmission
| Features | Aerosol Transmission | Droplet Transmission |
|---|---|---|
| Definition | Infection via inhalation of pathogen‐carrying aerosol( 22 ) | Infection via exposure to droplets sprayed by coughing or sneezing onto conjunctiva or mucous membranes( 22 ) |
| Transmission vehicle | Aerosol | Droplet |
| Mean particle size (diameter) of | < 5 μm in diameter( 10 , 22 ) | > 10 μm( 10 , 22 ) |
| transmission vehicle | However, there is no consensus on the exact size criterion of an aerosol( 22 ) | However, there is no consensus on the exact size criterion of a droplet( 22 ) |
| Particle suspension time in the air | Sufficiently small to remain suspended in air for several minutes or more( 10 , 22 ) | Do not stay suspended in the air but rapidly settle out( 10 , 22 ) |
| Distance at which the virus can be spread | Can be disseminated by air currents throughout a room or facility( 10 ) | Short distance( 10 ) |
| Inoculation site | Lower respiratory tract is thought to be the main inoculation site( 8 , 9 , 10 ) | Conjunctiva or mucous membranes( 10 , 22 ) |
| Dose of virus required to induce infection | Low doses of virus may be sufficient( 8 ) | Compared to aerosol inoculation, a higher dose of virus seems to be needed( 8 , 9 , 11 ) |
| % of particles of this size emitted during exhalation | 70% between 0.3 and < 0.5 μm, 17% between 0.5 and < 1 μm, and 13% between 1 μm and < 5 μm( 21 ) | < 0.1% of particles larger than 5 μm( 21 ) |
| % of particles of this size emitted during cough or sneeze | Approximately equal numbers of particles in aerosol and droplet classes( 22 ) | Most emitted pathogens are carried in droplets because of their greater volume( 22 ) |
Influenza virus administered via aerosol appears to be more infectious than via intranasal application of droplets, but this difference is difficult to quantify.( 11 )
In establishing the importance of droplet versus aerosol transmission for influenza, two more factors need to be considered. First, sedimenting droplets are bigger than nonsedimenting aerosols, thus containing more virus than an aerosol produced from the same virus suspension. For example, the volume of a particle with diameter 5 μm is 1,000 times smaller than the volume of a droplet of 50 μm, and thus likely contains a proportionally smaller number of virus particles. Second, virus in nonsedimenting aerosol resides in a closed (indoors) environment for hours while virus in sedimenting droplets remains suspended in air only for seconds after expulsion. Aerosolized virus can be inhaled as long as a subject is in a room, whereas droplets have a much smaller time window during which they are accessible for deposition on mucosal surfaces. These three factors—higher infectivity of aerosolized virus, higher virus content of larger droplets, and longer residence times of smaller aerosols—tend to balance each other. Thus the dominance of droplet transmission versus aerosol transmission cannot be easily established.
3.2. Mask Efficiency in Virus Transmission
An overview of published studies on face mask protection against influenza viruses and or other respiratory viruses is shown in Table II.
Table II.
Overview of Published Studies on Face Mask Protection Against Influenza or Other Respiratory Viruses
| Type of Study | Studied Viruses | Studied Population | Type of Mask Used | Results | Reference |
|---|---|---|---|---|---|
| Prospective case‐control study | Influenza A and B | Hong Kong influenza patients and their household contacts | Surgical masks | • Influenza patients comply better with mask use than their contacts • Between 28 and 45% of influenza patients wearing mask “often or always” • 21% or less of contacts wearing mask “often or always” | 26 |
| Cluster randomized controlled trial | Influenza A and B | Hong Kong influenza patients and their household contacts | Surgical masks | • No significant difference was found between hand hygiene or hand hygiene plus face mask in household contacts of influenza patients | 27 |
| • Hand hygiene and face masks can reduce influenza virus transmission if implemented early after symptom onset in an index patient | |||||
| • Only half of the influenza patients reported regular use of a surgical mask during follow‐up; face mask adherence among household contacts was lower | |||||
| Prospective case‐control study | Influenza A, B, and other acute viral respiratory infections | Adult household contacts of a child with respiratory illness | Surgical masks, P2 masks | • Adherent mask use gives relative reduction of 60–80% in risk of acquiring a respiratory infection | 28 |
| • < 50% of participants wearing the mask “most or all” of the time | |||||
| • No difference in adherence between P2 and surgical mask use | |||||
| Case‐control study | Influenza A, B, and RS‐viruses | Dentists | Not specified | No marked reduction in infection | 29 |
| Observational study | Influenza and other acute viral respiratory infections | Lab respiratory specimens from Hong Kong population | *** | • Possible association between population‐based hygienic measures and reduced incidence • The relative contribution of each of these measures could not be estimated | 30 |
| Retrospective case‐control study | SARS | Hong Kong citizens (probable SARS patients and matched controls) | Not specified | Using a mask frequently in public places was significant protective factor against SARS (OR = 0.27, p< 0.001 in multivariate analysis) | 5 |
| Retrospective case‐control study | SARS | Beijing citizens (probable SARS patients and matched controls) | Not specified | • Wearing masks outside the home was significantly protective against SARS (OR = 0.3 for consistent mask use and OR = 0.4 for sometimes mask use, in multivariate analysis) | 6 |
| • Many persons wearing masks in the community did not use N95 or similar highly efficient masks | |||||
| Retrospective case‐control study | SARS | Health care workers in 5 Hong Kong hospitals | Surgical masks, N95 masks, and paper masks | • The use of masks was significantly associated with noninfection (OR = 0.077, p = 0.0001) | 31 |
| • Surgical and N95 masks were both effective, while paper masks did not significantly reduce the risk of infection | |||||
| Retrospective cohort study | SARS | Nurses in 2 critical care units in Toronto | N95 masks and surgical masks | • Consistently wearing a mask while caring for a SARS patient was significantly protective against SARS (RR = 0.23, p = 0.02) | 32 |
| • The data suggest that N95 masks offer better protection than surgical masks | |||||
| Cohort study | RS‐virus | New York hospital | Not specified | The use of masks does not seem warranted if other infection control procedures such as handwashing are used | 33 |
| Review | SARS | Health care workers | N95 masks and surgical masks | • In most studies, mask use was associated with a reduced risk of infection | 34 |
| • It is still unclear whether N95 masks offered significantly better protection than surgical masks in all clinical situations | |||||
Most of these studies focus on the efficiency of face masks in virus transmission when used during contact with patients, while only a few studies look into the possible reduction of infection risk when using a face mask in the general population.
For protection against nonbiological particles, standards specify the minimum requirements for different classes of masks.( 35 ) Classifications depend mainly on the efficiency of the filter material and the maximum total inward leakage, that is, face‐seal leakage, exhalation valve leakage, and filter penetration.( 35 ) The testing procedures and criteria are standardized for a given laboratory setting and can differ from country to country. In order of increasing efficacy, these classes are the FFP1, FFP2, and FFP3 masks in Europe( 35 ) and N95, N99, and N100 masks in the United States.( 36 )
Apart from these certified masks, there are many types of masks not certified as respiratory protective devices. Their exact protective effect against particles is unknown, as is their efficiency.
Van der Sande et al. showed that uncertified masks such as surgical masks and home‐made masks can still give a considerable reduction in aerosol exposure.( 37 )
As Balazy et al. found that nonbiological particle simulants can be used to assess mask protection against biological particles of similar shape and size,( 38 ) the minimum filtering efficiency of masks for nonbiological particles may be applied for virus‐containing particles as well.
Mask efficiency for sedimenting droplets is likely to be better than for aerosol particles: proper mask use completely blocks droplet transmission to the mucous membranes of the upper respiratory tract, although it cannot prevent infection through the conjunctivae. We therefore presume mask protection factors for aerosols to represent a worst‐case assumption for protection against droplets.
3.3. Effect of Mask Use at Population Level
Assuming an R 0 of 2.0 during an influenza pandemic, we show in Fig. 1 the effect of mask coverage M cov and mask efficiency M eff on the value of the reproduction number R int (Fig. 1A) and the infection attack rate (Fig. 1B).
Figure 1.
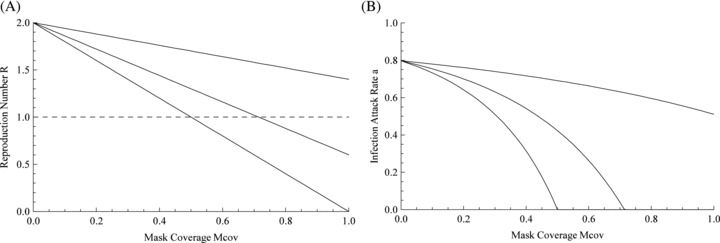
(A) Effect of mask efficiency and mask coverage on the reproduction number R int; upper line: M eff= 0.3; middle line: M eff= 0.7; lower line: M eff= 1.0. (B) The effect of mask use on the infection attack rate; upper line: M eff= 0.3; middle line: M eff= 0.7; lower line: M eff= 1.0.
A recent study shows that uncertified masks such as surgical masks and home‐made masks used by untrained subjects may have a median protection factor of 2.4 to 6.5,( 36 ) or a mask efficiency M eff of 58–85%. In Fig. 1 we can see these masks can still give a considerable reduction of the reproduction number R int and the infection attack rate.
Fig. 1A shows that, depending on mask efficiency and mask coverage, R int might decrease below the threshold level of 1.0, effectively containing the pandemic.
These results are based on the reduction of aerosol exposure: the effect of mask use with droplet transmission is expected to be stronger.
4. DISCUSSION
This study attempts to predict the possible effects of population‐wide mask use on the development of an influenza pandemic. Comparing aerosols (nonsedimenting particles) and droplets (sedimenting particles), we argue that in case of droplet transmission mask use may be at least as effective as for aerosol transmission.
Our results suggest that the use of face masks at the population level can delay an influenza pandemic, decrease the infection attack rate, and may reduce transmission sufficiently to contain the pandemic. The effect on final size of the epidemic depends on features of virus transmission, mask efficiency, and coverage of mask use in the population.
Our findings are based on data from published literature and mathematical models. As such models imply highly simplified situations in which only few variables can be studied, we focused on the effect of population‐wide mask use in reducing the risk of infection in healthy individuals.
Additional effects, not included in the model, might render the effect of population‐wide mask use even stronger than estimated in this study, as illustrated by the following three examples.
First, mask use not only protects healthy individuals but also reduces the infectiousness of symptomatic and asymptomatic carriers, thus reducing the number and effectiveness of transmission sources within the population. Since masks are not normally tested on their properties in preventing “outgoing infections,” we did a separate study to estimate this secondary effect, and found considerably lower, but still measurable, retention factors,( 37 ) indicating that masks worn by infectious subjects may increase the protective effect of population‐wide use of face masks.
Second, mask use is expected to influence behavior. Wearing a mask can raise awareness of the infection risk and the importance of additional preventive behaviors such as more frequent hand‐washing or avoiding physical contact and avoiding crowded public places. A face mask may also reduce contact transmission by preventing wearers from touching their mouths or noses with their hands or other objects potentially contaminated with virus.
However, on the other hand, face mask use might engender a false sense of security and lead to reduced use of other measures such as personal hygiene.
Finally, mask use is virtually the only way to prevent aerosol transmission, which may cause the most severe cases of influenza. Experimental aerosol inoculation displayed the spectrum of symptoms seen in natural infections, whereas experimental infection with intranasal drops produced milder disease, usually without involvement of the lower respiratory tract.( 8 , 9 , 10 , 24 ) General sanitary interventions and social distancing can largely prevent transmission by contact and droplets, but is much less effective against transmission by aerosols.
The magnitude of such additional effects is unknown. More research on influenza transmission is needed to improve insight into the impact of mask use.
This study is based on the features (infectivity, route of transmission) most commonly expected in influenza. Changes in these features can change the effect of mask use within the population. If, for example, the pandemic virus spreads mainly by contact transmission, the preventive contribution of mask use might be small compared to routine hygienic measures.
We have not distinguished between different subpopulations (children vs. adults) or environments (open air vs. small rooms). If transmission depends more on some groups or environments than others, high mask coverage and mask efficiency within those groups or situations may have a disproportional effect on the course of the pandemic. The specification of such conditions depends on virus properties, such as transmission route and survival rate, and on host properties, such as risky behavior.
For example, we expect infectivity, mask efficiency, mask coverage, and virus transmission to be different for children than for adults. The impact of heterogeneity can only be estimated when more is known about the transmission features of the particular influenza virus and the specific risk groups for this virus. If small children (with a lower mask coverage and mask efficiency) play a more important role in transmission than adults, population‐wide use of masks might be less effective than found in this study.
Mask efficiency might also be lower if the devices are used improperly or by people with aberrant face shapes or features such as facial hair. Respiratory protective devices are usually tested on healthy adult males who are clean‐shaven. On the other hand, the mask efficiency indicated for a specific type of mask indicates the minimum needed for certification, and actual mask efficiency often exceeds the minimum.
Mask protection factors are characterized for nonbiological particles. Because even few pathogenic organisms passing through the filter may cause serious problems,( 39 ) more information on infectivity and exposure is needed to refine our estimates of protection against respiratory infection.
Any outcome of a study like this mainly depends on the proportion of the population that is actually going to use a mask during an influenza pandemic. Past experience indicates considerable willingness to use face masks in case of such a threat. The proportion of people using masks in Hong Kong during the SARS epidemic ranged from 61.2%( 40 ) to more than 90%.( 5 ) Compliance with mask use in other times and other places to prevent other diseases is unknown but is expected to depend on the perceived threat of the pandemic.
In conclusion, the population‐wide use of face masks can be a valuable strategy to delay or contain an influenza pandemic, or at least decrease the infection attack rate. We therefore strongly recommend including the use of face masks within pandemic control guidelines.
ACKNOWLEDGMENTS
We thank M. van der Sande and M. van der Lubben from RIVM, L. Steenweg and I. Tuinman from TNO, and T. Daha from the WIP for their useful discussions and advice.
We thank W. ten Have for assistance with the literature search, R. Stumpel and GGD Gooi & Vechtstreek for support in writing this article, and L. Phillips in editing.
REFERENCES
- 1. WHO consultation on priority public health interventions before and during an influenza pandemic. Geneva , Switzerland , 2004. Available at: http://www.who.int/csr/disease/avian_influenza/final.pdf, Accessed on May 2006. [PubMed] [Google Scholar]
- 2. World Health Organization writing group . Nonpharmaceutical interventions for pandemic influenza, international measures. Emerging Infectious Diseases, 2006; 12:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zanderink R. Werken maskers nu wel of niet? Een speurtocht van enige eeuwen geleden tot heden? Nederlands Tijdschrift voor Anesthesiologie, 2003; 16:83–93. [Google Scholar]
- 4. World Health Organization writing group . Nonpharmaceutical interventions for pandemic influenza, national and community measures. Emerging Infectious Diseases, 2006; 12(1):88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lau JTF, Tsui H, Lau M, Yang X. SARS transmission, risk factors and prevention in Hong Kong. Emerging Infectious Diseases, 2004; 10:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu J, Xu F, Zhou W, Feikin DR, Lin CY, He X, Zhu Z, Liang W, Chin DP, Schuchat A. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerging Infectious Diseases, 2004; 10:210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Teunis P, Havelaar A. The beta poisson dose‐response model is not a single‐hit model. Risk Analysis, 2000; 20:513–520. [DOI] [PubMed] [Google Scholar]
- 8. Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proceedings of the Society for Experimental Biology and Medicine, 1966; 122:800–804. [DOI] [PubMed] [Google Scholar]
- 9. Henle W, Henle G, Stokes J, Maris EP. Experimental exposure of human subjects to viruses of influenza. Journal of Immunology, 1945; 52:145–165. [PubMed] [Google Scholar]
- 10. Bridges C, Kuehnert M, Hall C. Transmission of influenza: Implications for control in health care settings. Clinical Infectious Diseases, 2003; 37:1094–1101. [DOI] [PubMed] [Google Scholar]
- 11. Nicas M, Jones MJ. Relative contributions of four exposure pathways to influenza infection risk. Risk Analysis, 2009; 29:1292–1303. [DOI] [PubMed] [Google Scholar]
- 12. Longini IM Jr, Halloran ME, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. American Journal of Epidemiology, 2004; 159:623–633. [DOI] [PubMed] [Google Scholar]
- 13. Mills CE, Robins JM, Lipsitch M. Transmissibility of 1918 pandemic influenza. Nature, 2004; 432:904–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature, 2005; 437:209–214. [DOI] [PubMed] [Google Scholar]
- 15. Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature, 2006; 442:448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wallinga J, Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proceedings. Biological Sciences/The Royal Society, 2006; 274:599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chowell G, Nishiura H, Bettencourt LM. Comparative estimation of the reproduction number for pandemic influenza from daily case notification data. Journal of the Royal Society, Interface/the Royal Society, 2007; 4:155–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Giesecke J. Mathematical models for epidemics Pp. 119–132 in Giesecke J. (ed). Modern Infectious Disease Epidemiology, 2nd ed London : Arnold Publishers, 2002. [Google Scholar]
- 19. Teunis PFM, Nagelkerke NJD, Haas CN. Dose response models for infectious gastro‐enteritis. Risk Analysis, 1999; 19:1251–1260. [DOI] [PubMed] [Google Scholar]
- 20. Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH. Survival of influenza viruses on environmental surfaces. Journal of Infectious Diseases, 1982; 146:47–51. [DOI] [PubMed] [Google Scholar]
- 21. Fabian P, McDevitt JJ, DeHaan WH, Fung RO, Cowling BJ, Chan KH, Leung GM, Milton DK. Influenza virus in human exhaled breath: An observational study. PloS One, 2008; 3:e2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nicas M, Nazaroff W, Hubbard A. Toward understanding the risk of secondary airborne infection: Emission of respirable pathogens. Journal of Occupational and Environmental Hygiene, 2005; 2:143–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Morawska L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air, 2006; 16:335–347. [DOI] [PubMed] [Google Scholar]
- 24. Tellier R. Review of aerosol transmission of influenza A virus. Emerging Infectious Diseases, 2006; 12:1657–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Weber T, Stilianakis NI. Inactivation of influenza A viruses in the environment and modes of transmission: A critical review. Journal of Infection, 2008;57:361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cowling BJ, Fung RO, Cheng CK, Fang VJ, Chan KH, Seto WH, Yung R, Chiu B, Lee P, Uyeki TM, Houck PM, Peiris JS, Leung GM. Preliminary findings of a randomized trial of non‐pharmaceutical interventions to prevent influenza transmission in households. PloS One, 2008; 3:e2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, Sin J, Seto WH, Yung R, Chu DW, Chiu BC, Lee PW, Chiu MC, Lee HC, Uyeki TM, Houck PM, Peiris JS, Leung GM. Facemasks and hand hygiene to prevent influenza transmission in households. Annals of Internal Medicine, 2009; 151:437–446. [DOI] [PubMed] [Google Scholar]
- 28. MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, Fasher M, Wood J, Gao Z, Booy R, Ferguson N. Face mask use and control of respiratory virus transmission in households. Emerging Infectious Diseases, 2009; 15:233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Davies KJ, Herbert A‐M, Westmoreland D. Seroepidemiological study of respiratory virus infections among dental surgeons. British Dental Journal, 1994; 176:262–265. [DOI] [PubMed] [Google Scholar]
- 30. Lo JY, Tsang TH, Leung YH, Yeung EY, Wu T, Lim WW. Respiratory infections during SARS outbreak, Hong Kong, 2003. Emerging Infectious Diseases, 2005; 15:1738–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, Ho LM, Peiris JS; Advisors of Expert SARS group of Hospital Authority . Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet, 2003; 362:1519–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hlywka T, Levie J, McQueen J, Smith S, Moss L, Smith A, Green K, Walter SD. SARS among critical care nurses, Toronto. Emerging Infectious Diseases, 2004; 10:251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hall C, Douglas G. Nosocomial respiratory syncytial viral infections. Should gowns and masks be used? American Journal of Diseases of Children, 1981; 135:512–515. [DOI] [PubMed] [Google Scholar]
- 34. Gamage B, Moore D, Copes R, Yassi A, Bryce E; BC Interdisciplinary Respiratory Protection Study Group . Protecting health care workers from SARS and other respiratory pathogens: A review of the infection control literature. American Journal of Infection Control, 2005; 33:114–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. NEN: Nederlands Normalisatie‐instituut . Nederlandse norm NEN‐EN 149 (en): Ademhalingsbeschermingsmiddelen – Filtrerende halfmaskers ter bescherming tegen deeltjes – Eisen, beproeving, merken. 2001.
- 36. National Institute for Occupational Safety and Health . NIOSH‐Approved Disposable Particulate Respirators (Filtering Facepieces). Available at: http://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/, Accessed on May 2006.
- 37. Van Der Sande M, Teunis P, Sabel R. Professional and home‐made face masks reduce exposure to respiratory infections among the general population. PloS One, 2008; 3:e2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Balazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, Grinshpun SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? American Journal of Infection Control, 2006; 34:51–57. [DOI] [PubMed] [Google Scholar]
- 39. Rengasamy A, Zhuang Z, Berry Ann R. Respiratory protection against bioaerosols: Literature review and research needs. American Journal of Infection Control, 2004; 32:345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tang CS, Wong CY. Factors influencing the wearing of facemasks to prevent the severe acute respiratory syndrome among adult Chinese in Hong Kong. Preventive Medicine, 2004; 39:1187–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]


