Abstract
The saving of many lives in history has been duly credited to blood transfusions. What is frequently overlooked is the fact that, in light of a wealth of evidence as well as other management options, a therapy deemed suitable yesterday may no longer be the first choice today. Use of blood has not been based upon scientific evaluation of benefits, but mostly on anecdotal experience and a variety of factors are challenging current practice. Blood is a precious resource with an ever limiting supply due to the aging population. Costs have also continually increased due to advances (and complexities) in collection, testing, processing and administration of transfusion, which could make up 5% of the total health service budget. Risks of transfusions remain a major concern, with advances in blood screening and processing shifting the profile from infectious to non‐infectious risks. Most worrying though, is the accumulating literature demonstrating a strong (often dose‐dependent) association between transfusion and adverse outcomes. These include increased length of stay, postoperative infection, morbidity and mortality. To this end, a recent international consensus conference on transfusion outcomes (ICCTO) concluded that there was little evidence to corroborate that blood would improve patients’ outcomes in the vast majority of clinical scenarios in which transfusions are currently routinely considered; more appropriate clinical management options should be adopted and transfusion avoided wherever possible. On the other hand, there are patients for whom the perceived benefits of transfusion are likely to outweigh the potential risks. Consensus guidelines for blood component therapy have been developed to assist clinicians in identifying these patients and most of these guidelines have long advocated more conservative ‘triggers’ for transfusion. However, significant variation in practice and inappropriate transfusions are still prevalent. The ‘blood must always be good philosophy’ continues to permeate clinical practice. An alternative approach, however, is being adopted in an increasing number of centres. Experience in managing Jehovah’s Witness patients has shown that complex care without transfusion is possible and results are comparable with, if not better than those of transfused patients. These experiences and rising awareness of downsides of transfusion helped create what has become known as ‘patient blood management’. Principles of this approach include optimizing erythropoiesis, reducing surgical blood loss and harnessing the patient’s physiological tolerance of anaemia. Treatment is tailored to the individual patient, using a multidisciplinary team approach and employing a combination of modalities. Results have demonstrated reduction of transfusion, improved patient outcomes and patient satisfaction. Significant healthcare cost savings have also followed. Despite the success of patient blood management programmes and calls for practice change, the potential and actual harm to patients caused through inappropriate transfusion is still not sufficiently tangible for the public and many clinicians. This has to change. The medical, ethical, legal and economic evidence cannot be ignored. Patient blood management needs to be implemented as the standard of care for all patients.
Introduction
‘I will prescribe regimens for the good of my patients according to my ability and my judgment and will do no harm or injustice to them’ [1].
There is no doubt that the way many clinicians think about and use blood transfusion is progressively changing. Blood management, or as it is increasingly known, patient blood management may be seen to be a trendy term; however, many of the strategies commonly applied in blood management such as anaemia therapy, surgical blood loss reduction and tolerance of anaemia are far from new.
The mounting wealth of medical, physiological, ethical, legal and financial evidence necessitates a change in practice to ensure best quality of care and outcome for patients. Nonetheless, patient blood management challenges the way many clinicians have been taught and is therefore still difficult for some to embrace. This article will examine the reasons that are driving this shift and describe the patient‐centred, multidisciplinary, multimodal, planned approach to patient care, which is embodied in blood management.
Historical perspective
For centuries, the blood has been seen as the life force and the carrier of mystical qualities. Primitive attempts at transferring blood between humans and animals were made and recorded through history with often horrifying outcomes. It was not until during the wars of last century that the modern practice of transfusion began to develop. Advances such as the understanding of human blood groups, development of anticoagulation to allow blood storage, techniques to separate and process blood into components and testing to detect contaminating infectious agents have all contributed to modern day availability of blood and blood products.
Modern transfusion medicine was born out of the necessity to revitalize severely bleeding patients in the context of relatively limited resuscitation options available then, and it undoubtedly saved many lives. Given its initial success, transfusion support was considered to be an indispensable tool in the development of many modern therapies such as high dose chemotherapy, transplantation and complex surgeries. Focus was on ensuring the safety and quality of the products used, with much less attention directed to addressing the clinical use of the product. Much of the use of blood associated with such treatments has not been based upon science, but on tradition and anecdotal experience. A variety of factors are, however, now changing our previous paradigm, as we begin to question the clinical benefits of blood transfusion.
Drivers of change
Supply issues
Blood is a precious and scarce resource. Yearly increases in demand have been noted since the 1980s due to an increase in complex surgery and more aggressive treatment of haematological and other malignancies. Although Blood Services have extensive programmes to actively recruit new donors, often the difference between numbers of donors recruited and donors leaving due to deferment or illness balances out.
Population modelling for most high human development index (HDI) countries for the next decades shows an increasing percentage of the population aged over 65 years. Historic and projected data in Western Australia, for example, show that this age segment will increase by 146% from 1997 to 2026. At the same time, the population aged 64 years or less, which includes the age range eligible to donate blood, will only increase by 38% [2]. This is an important observation because studies show that significantly more blood is used for patients in the older age groups [3]. Therefore, we have a fast growing ‘blood using but non‐donating’ segment compared with a slow growing donor base. Supply pressures are therefore only likely to increase.
In addition to large‐scale imbalances between supply and demand, blood supply is often an issue at a local level. Given the strict requirements for blood procurement, storage and transportation and its limited shelf life, supplying enough blood under extraordinary circumstances can pose additional challenges. Blood shortage in US hospitals during winter storms is not unheard of, and natural disasters, catastrophic events and conflicts can easily overload and break the delicate supply chain. Therefore, even creating a wide margin between supply and demand at a national level cannot ensure that local and temporal shortages would not happen.
True cost of blood transfusion
Blood is also a costly resource. Improvements in the collection, testing and processing of blood have come at a progressively increasing cost. The nominal cost of a unit of red cells varies between countries. For instance, in the United States, it is somewhere between US$230 and $265 [4], £140 in the UK [5] and around A$330 in Australia. Platelets are more expensive and fractionated products often more so.
However, in addition to the acquisition costs are the costs involved administering transfusions to patients. Crémieux et al. showed that product and product preparation costs accounted for approximately 50% of the total cost of a RBC transfusion while overheads comprised 19·1%, purchased materials 18·0%, and direct labour 11·9% [6]. An earlier study by Cantor et al. came to similar conclusions [7]. Process cost analysis shows how many steps are involved in ‘delivering’ a blood transfusion to a patient and each of these is a cost to the health system [8]. A recent study, shortly to be published, mapped the encounters involved in providing and administering red cell transfusions to patients in two teaching hospitals in Australia. Costs of potential adverse outcomes were not included. From this analysis, the cost of transfusion of a single unit of red cells, including acquisition costs, was AUS$700 [A Hofmann; E Wood; unpublished data]. Another multi‐centre study analyzed process cost in the surgical setting and showed even higher cost per RBC unit transfused [9]. All transfusion related costs, including short term adverse effects and suspected mid‐ and long‐term adverse effects, might equal up to 5% of the total public healthcare budget of some HDI countries. In our increasingly strained health economies, minimizing unnecessary transfusion will result in significant health savings.
Risk profile of transfusion
Infectious risks
It is often quoted that ‘blood is safer than it has ever been’. Certainly from the perspective of transfusion‐transmitted infections, this appears to be correct.
From the late 1980s onwards, a series of measures have been implemented that have largely eliminated the risks of transmitting hepatitis and HIV/AIDS through transfusion. Recent risk estimates per unit in the Australian donor population have been calculated to be approximately one in 5·4 million for HIV, one in 2·7 million for HCV and one in 739 000 for HBV [10] with similar rates quoted for many other developed countries. Risk of bacterial contamination has also been reduced with the implementation of improved sterility measures at time of blood collection and screening for bacterial contamination which is now undertaken in many countries. Transfusion‐associated sepsis is, however, still one of the most common causes of death from transfusion‐transmitted infections: current risk of bacterial sepsis is about one in 75 000 for platelets and one in 500 000 for red cell transfusion [10].
Despite all the improvements, infectious agents are expected to keep their edge, as evident by the newly emerging threats, not known and previously not tested for. Recent experience with West Nile Virus, Severe Acute Respiratory Syndrome (SARS) virus, Chagas disease and variant Creutzfeldt Jakob disease shows the ever changing profile of potential infectious risk from transfusion. This will be an ongoing challenge, with exacerbating costs and complexities.
Non‐infectious risks
Infectious risks of blood tend to be scary and gather much media attention, but thanks to continuous screening and testing efforts, their risk can be considered negligible. Unfortunately, transfusions are associated with a host of much more common non‐infectious risks, many of which are poorly defined and hard to remove. Some of these risks include transfusion‐related acute lung injury (TRALI), immunomodulation, allergic and febrile reactions.
As a result, despite dramatic improvements in reducing risk of infections, non‐infectious risks have remained little changed. In the combined FY2005, FY2006 and FY2007 reports to the Food and Drug Administration (FDA) of fatalities following transfusion, TRALI and haemolytic transfusion reaction were the leading causes of death. Similar data are also found in other haemovigilance schemes. Data from the UK Serious Hazards of Transfusion (SHOT) reporting scheme for the years 1996 to 2007 have indicated that ‘incorrect blood component transfused’ continues to be the most significant transfusion risk [11]. While some of the non‐infectious risks stem from human and systems error and should be amenable to corrective and preventive measures, some are related to the very nature of blood products and the only way to avoid them may ultimately lie in avoiding blood transfusions altogether.
In addition to these recognized non‐infectious risks of transfusion, a growing wealth of evidence links transfusion with numerous general adverse outcomes (see Table 1). Reports of increased incidence of postoperative infection [12, 13, 14, 15, 16], increased ICU and hospital length of stay [14, 17, 18, 19], increased rates of acute respiratory distress syndrome and multi‐organ failure in ICU and trauma patients [13, 20, 21] and increased morbidity and mortality [18, 22, 23, 24, 25, 26, 27, 28, 29, 30] are now common in the medical literature. Possibility of red cell transfusion affecting tumour growth and cancer progression or recurrence has also been suggested [31, 32].
Table 1.
Reported adverse outcomes associated with transfusion and populations affected.
| Adverse outcomes reported to be associated with RBC transfusion | |
| Infection | Cardiac arrest |
| Septicaemia | Renal failure |
| Transfusion‐related acute lung injury (TRALI) | Stroke |
| Multisystem organ failure (MOF) | Thromboembolism |
| Systemic inflammatory response syndrome (SIRS) | Diminished postoperative functional recovery |
| Acute respiratory distress syndrome (ARDS) | Bleeding requiring re‐operation |
| Prolonged mechanical ventilation | Increased admission to ICU |
| Vasospasm | Increased ICU length of stay |
| Low‐output heart failure | Increased hospital length of stay |
| Atrial fibrillation | Increased hospital readmission |
| Myocardial infarction | Increased mortality |
| Patient populations in whom adverse outcomes associated with RBC transfusion have been reported | |
| ICU patients | Transplantation surgery |
| Paediatric patients | Colorectal surgery |
| Trauma patients | Gastric surgery |
| Burn patients | Biliary surgery |
| Combat casualties | Splenectomy |
| Acute coronary syndrome patients | General surgery |
| Oncology patients | Vascular surgery |
| Population based studies | Orthopaedic surgery |
| Obstetrics | Thoracic aneurysm surgery |
| Cardiac surgery | Lung surgery |
| Neurosurgery | Head and neck surgery |
| Hepatic surgery | Mastectomy and reconstruction |
| Pancreatic surgery | Oesophageal surgery |
The increased mortality is not only short term but has been reported up to 10 years after transfusion in cardiac surgery patients [18, 33, 34, 35]. In addition, data have suggested a dose–response relationship with risk increasing proportionally to the number of units transfused [14, 15, 18, 25, 36, 37, 38, 39, 40]. Storage age of the transfused blood is another factor playing a role here, with studies indicating higher mortality rates in patients receiving older blood, particularly when volume of transfused blood is larger [41, 42].
Despite uncontrolled methodology of most of these studies, observation of similar results across several independent studies (with various degrees of matching between transfused and not‐transfused cohorts) supports that these risks are real and clinically significant. Adverse events and unfavourable outcomes occurring in association with transfusion add a significant further health and financial burden [8, 14, 18, 30, 43].
Transfusion efficacy: when should we transfuse?
Historically, the trigger for red cell transfusion has been a haemoglobin of 100 g/l (10 g/l) or haematocrit of 30% [44]. However, this number was more of a convention and it was not based upon any human or animal oxygen supply‐demand research. Studies have shown that the haemoglobin level at which compensatory mechanisms are exhausted and metabolism switches from aerobic to anaerobic is much lower at approximately 30–45 g/l [45]. This also correlates with the level at which patients experience an increased mortality [46, 47]. Moreover, factors other than haemoglobin levels are also likely to affect this critical threshold, and relying on a single blood parameter may not be accurate enough to distinguish individual patients’ oxygenation status [48]. Nonetheless, most transfusions are given preventatively so that such critical levels are not reached.
Unfortunately, very few studies are available to give direction on when to transfuse. The single largest prospective randomized trial, the TRICC study, involved more than 800 intensive care patients in 25 centres across Canada [49]. Patients were randomly assigned to receive transfusion at either the standard < 100 g/l (liberal group) or < 70 g/l (restrictive group) haemoglobin level. The haemoglobin level was maintained between 100 and 120 g/l in the liberal group and 70–90 g/l in the restrictive group.
The overall 30‐day mortality was not significantly different between the restrictive and the liberal groups (18·7% vs. 23·3% respectively; P = 0·11). However, the mortality rate in patients who were younger (< 55 years) or less sick (APACHE II scores ≤ 20) was significantly lower in the restrictive group compared with liberal transfusion group (5·7% vs. 13·0%; P = 0·02 and 8·7% vs. 16·1%; P = 0·03 respectively). This difference was not seen though in patients with acute myocardial infarction and unstable angina (20·5 vs. 22·9; P = 0·69). There were lower rates of pulmonary oedema (5·3% vs. 10·7%, P < 0·01), acute respiratory distress syndrome (7·7% vs. 11·4%, P = 0·06), myocardial infarction (0·7% vs. 2·9%, P = 0·02) and in‐hospital mortality (22·2% vs. 28·1%, P = 0·05) in the restrictive vs. liberal transfusion groups respectively. Subgroup analysis of patients with cardiovascular disease, critically ill trauma patients and patients with head injury has been subsequently published and no benefit from a liberal transfusion strategy in any of these subgroups has been reported [50, 51, 52].
In a similar study conducted in critically ill children (TRIPICU) [53], 637 stable critically ill paediatric patients were randomized to a liberal (haemoglobin threshold of 95 g/l) or restrictive (70 g/l) transfusion strategy. The incidence of new or progressive multiple‐organ dysfunction syndrome, mortality rates, other outcomes and adverse events were similar in the liberal and restrictive transfusion groups, indicating that in this population, a haemoglobin threshold of 70 g/l for transfusion is safe and does not increase adverse outcomes.
Two randomized controlled trials (RCT) comparing liberal vs. restrictive transfusion thresholds have been conducted in premature neonates. A study in a single centre of 100 premature infants [54] found that a restrictive transfusion policy was generally well tolerated with no difference in most clinical outcomes although there did appear to be a relationship between a lower transfusion threshold and increased brain injury. However, in a larger multi‐centre study [55] of 451 premature infants, this was not confirmed. This study found no difference in outcomes between a liberal and a restrictive transfusion threshold.
Carson performed a meta‐analysis of 10 RCTs comparing liberal to restrictive transfusion [56]. No benefit from liberal transfusion was found. To the contrary, restrictive transfusion was found to be associated with less blood usage, a marginally significant reduction in cardiac events (24% lower; RR 0·76; 95% CI 0·57–1·0; P = 0·048) and a non‐significant reduction in mortality (20% lower; RR 0·80; 95% CI 0·63–1·02; P = 0·07). However, it was noted that most studies involved only small sample size and the results were dominated by the large numbers of patients from the TRICC study.
The only RCTs to compare transfusion with no transfusion were conducted in Africa with a total of 230 clinically stable children with severe malarial anaemia (haemoglobin levels between 40 g/l–57 g/l) [57, 58]. A meta‐analysis [59] of the two trials found there was a non‐significant trend towards fewer deaths in the transfused group compared with the non‐transfused patients (1/118 vs. 3/112; RR 0·41; 95% CI 0·06–2·70; P = 0·4); however, there were significantly more severe adverse events in transfused group compared with the non‐transfused (RR 8·60; 95% CI 1·11–66·43; P = 0·04).
Transfusion guidelines
The ‘evidence‐based’ recommendations for adoption of a conservative haemoglobin threshold have been incorporated into many of the currently available consensus transfusion guidelines. In fact, 10 years prior to publication of the TRICC study, the US National Heart, Lung and Blood Institute, National Institutes of Health and FDA Consensus Conference on Peri‐operative Red Cell Transfusion [60] concluded that there was a remarkable lack of evidence to guide decisions about transfusion, but available evidence suggested a haemoglobin level of 70 g/l may be acceptable in some patients. It nevertheless cautioned that decisions should not be based on a single haemoglobin value.
Published guidelines recommend a transfusion trigger around a haemoglobin level of 60 to 70 g/l [61, 62, 63, 64, 65] for most stable patients. Haemoglobin values > 70 g/l may be appropriate if there is evidence of ischaemia, ongoing blood loss and/or other risk factors [65, 66]. Current guidelines unanimously maintain that transfusion in patients with haemoglobin levels > 100 g/l is almost never indicated. Another common theme in guidelines is the emphasis on inadequacy of making transfusion decisions based on an arbitrary haemoglobin value. Decisions should be guided by patient factors including signs and symptoms of hypoxia, ongoing blood loss and risks of anaemia vs. risks of transfusion for individual patients. In addition, the importance of transfusing a single unit at a time followed by assessment of response and further need is outlined [65, 67].
Practice variations
Despite consensus guidelines, there remains a wide variation in transfusion practice, with transfusion rates for similar procedures varying from hospital to hospital and from clinician to clinician. An Austrian benchmark study found that for similar orthopaedic surgery patients in 18 hospitals, rates of transfusion ranged from 12 to 87% [68]. A study of cardiac surgery patients in 12 Australasian teaching hospitals found red cell transfusion rates ranging from 17 to 79% [69]. These are similar to the findings of others [70, 71, 72, 73, 74].
It appears that practice guidelines are not being applied and that transfusion is dictated by either institutional‐based protocols or clinician preferences. Opportunity exists to reduce transfusion exposure by simply adopting current best practice guidelines.
Other factors to consider when making transfusion decisions
Patients’ outcomes
It is clear that there is a paucity of evidenced based data to guide when to transfuse. At the same time, there are an increasingly large number of data‐based analyses related to transfusion outcomes. A logical approach to make transfusion decisions is to weigh risks vs. benefits of transfusion in improving a patient’s outcome and decide accordingly. The majority of the studies on outcomes of transfusion are not randomized controlled trials and their individual results need to be interpreted with caution. However, the value of large observational studies has recently been acknowledged as an important tool in establishing evidence and identifying safety issues [76, 77].
Based on recent work by epidemiologists, Spiess [44] has pointed out that when multivariate analysis shows a twofold or greater increase in an adverse outcome it is most likely a causal relationship rather than simply an association. Confounders generally have less effect than a twofold or greater response.
How then can clinicians analyze the current and expanding transfusion literature and make appropriate conclusions to guide their practice? The International Consensus Conference on Transfusion Outcomes (ICCTO) held in April 2009 [78] was convened to assist with this issue. The conference brought together a broad range of experts and was overseen by the FDA, the American and Australian Red Cross, the Joint Commission on Healthcare and other stakeholders.
Using the validated Rand/UCLA appropriateness methodology [78], the conference aimed to identify the characteristics of patients with selected medical, surgical and traumatic conditions for whom allogeneic red blood cell transfusions would have a positive impact on health outcomes and survival. The Rand/UCLA appropriateness methodology has its origins in the reality that, although randomized clinical trials are regarded as the gold standard for evidence‐based medicine, they may not be available or don’t provide adequate evidence for the management of specific clinical scenarios or patients. The methodology does not ‘force’ consensus, but allows for degrees of uncertainty. The results of this conference should be available in the near future. However, the major outcome of the meeting was broad consensus that there is uncertainty about allogeneic red cell transfusions’ improving clinical outcomes in the majority of stable anaemic peri‐operative patients. The real concern is that most peri‐operative transfusions in haemodynamically stable patients are not appropriate and may be exposing patients to risk without evidence for benefit in terms of improving clinical outcomes. It is hoped that the conclusions from this conference will open the way for larger multi‐centre clinical trials in which transfusion can be compared with non‐transfusion management.
Patients’ viewpoints and ethical issues
An often forgotten consideration in the decision to transfuse is the patient’s viewpoint. Every patient has the right to know the nature of the treatment being recommended, its risks and benefits in their particular situation and what possible alternatives are available. This is the principle of informed consent. Patients, however, still appear to be poorly informed regarding transfusion choices and many clinicians and institutions are not routinely and systematically attempting to improve this situation [79].
A study in Western Australia in 1998 found that 96% of patients would avoid a transfusion if possible though only 4% were aware that alternatives to transfusion were available [80]. Similar results have been shown in US, Europe and Canada [81, 82, 83].
The medical community also expresses a preference to avoid allogeneic transfusion. All professionals surveyed in the UK [83] would prefer their own blood to donated blood and anaesthetists would prefer a blood substitute to receiving a transfusion.
Why then are clinicians continuing to prescribe blood while they would prefer to avoid transfusion themselves? It is essential that patients are adequately informed and participate in the decision regarding their management. The legal ramifications of a patient suffering an adverse outcome where a transfusion was not warranted, or could have been avoided, is all too obvious [84].
It is also frequently forgotten that there is an ethical responsibility to blood donors who voluntarily give their blood and time in trust. Blood Services and clinicians need to provide stewardship of this expensive and valuable resource by ensuring that it is used appropriately and for those in greatest need.
A new way of practicing: patient blood management
Background
No one who objectively examines the evidence can disagree that we owe it to our patients to reduce transfusion exposure as far as possible. How can this be achieved? Much has been learnt to help us through the experience of caring for Jehovah’s Witness patients who, although refusing blood for religious reasons, actively seek non‐blood medical management.
In 1979, Jehovah’s Witnesses formed Hospital Liaison Committees in an attempt to establish a more co‐operative approach between Witness patients and medical institutions and to help inform hospital staff of valid alternatives to transfusion [85]. Although many clinicians had difficulty with the concept of ‘bloodless’ or ‘transfusion‐free’ medicine, there were some clinicians who took up the challenge to manage these patients.
One of the pioneers was cardiac surgeon Denton Cooley [86, 87, 88]. Others followed and treatment of complex procedures including cardiac, orthopaedic and cancer surgery was progressively able to be performed as experience increased. Publication of results not only showed that patients were surviving complex procedures without the use of transfusion, but that their outcomes were as good as, if not better than, similar patients who received blood transfusion [89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99].
With news of treatment success, other Witness patients as well as other patients who preferred to avoid allogeneic blood for any reasons, were attracted to the care of these clinicians and the foundations for the early ‘bloodless programmes’ was laid [80, 100, 101]. The clinical outcomes in these patients should have been a stimulus to the medical community to question the general use of blood transfusion in most surgical procedures. However, it was not until the recognition in the 1980s that HIV/AIDS could be transmitted by transfusion that general concern regarding the benefits and use of transfusion began to really be expressed.
Over the last two decades, we have seen transition of practice away from the ‘blood is always good’ philosophy to focus on managing the patient’s problem and not defaulting to transfusion as the only treatment avenue. This new treatment focus requires a combination of approaches and involves all disciplines of the patient’s care: medical, surgical, anaesthetic, nursing, pharmacy and health support.
The approach is now more commonly known as ‘blood management’ or ‘patient blood management’ (PBM) rather than ‘bloodless’ or ‘transfusion‐free’ medicine as it is recognized that a transfusion may still be a necessary part of patient care.
Evidence of success
Across the world PBM has been adopted by an increasing number of individual departments, hospitals and whole health networks such as recently adopted in Western Australia [84]. Reports of the success of these programmes are now also populating the medical literature and they are likely to propagate the interest in these programmes.
In Canada, in 2000, the Ontario government supported a three year provincial PBM focusing on elective knee surgery, aortic aneurysm repair and elective coronary artery bypass surgery [102, 103]. Results have shown reduction in blood use (14 to 24%) together with reduction in length of stay and postoperative infection. Significant financial savings were also identified.
In USA, there are now reportedly more than 200 individual programmes with numbers progressively increasing. Published results mirror those seen in Canada. At Englewood Hospital and Medical Center in New Jersey, there was a 42% reduction in blood use over the first 4 years of their programme [104, 105]. Their RBC transfusion rate in coronary artery bypass graft (CABG) surgery is 8% with a 30‐mortality rate of 0% [106]. A comparison of their transfusion utilization data with other US transfusion statistics is shown in 1, 2. Other centres report similar trends, with lower costs both in terms of actual blood costs, plus savings due in particular to reduction in length of stay and incidence of complications [107, 108, 109, 110, 111].
Figure 1.
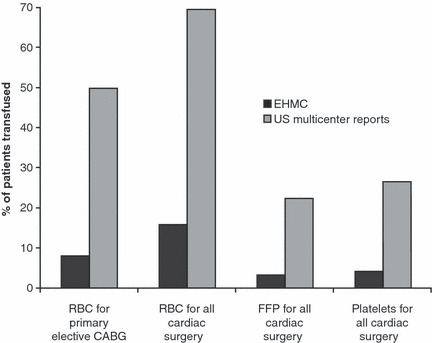
Unstratified cardiac surgery transfusion statistics for EHMC compared with published transfusion statistics in US multi‐centre studies. CABG = coronary artery bypass surgery; all cardiac surgery = CABG, valve and combined procedures. Data compiled from New Jersey Department of Health, Stover 1998 and Syder‐Ramos 2008.
Figure 2.
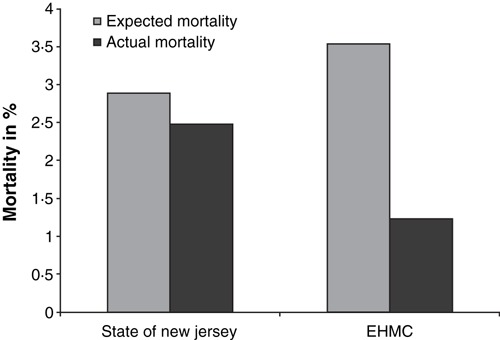
State of New Jersey Department of Health reported expected compared with actual mortality rates for cardiac surgery for the State of New Jersey and Englewood Hospital and Medical Center (EHMC). (*Englewood is reported to have the oldest average age in the US and thus the higher expected mortality rate).
Results from programmes in Austria, France, Spain and the Netherlands have all been published [68, 112, 113, 114]. In addition, blood management programmes to address the needs of more complex patients such as liver transplant recipients and stem cell transplantation of haematological malignancy have been adopted with successful results [115, 116]. Most recently, the government of Western Australia has recognized the significant benefits of patient blood management and has supported its implementation between 2008 and 2012 throughout the whole WA Health service [84].
What is involved?
A PBM programme aims to identify patients at risk of transfusion and provide a management plan aimed at reducing or eliminating the need for transfusion [117, 118, 119].
In surgical patients, the main factors which are recognized to increase the risk of transfusion are [68]:
-
1
preoperative anaemia or low red cell mass
-
2
volume of surgical blood loss
-
3
failure to adopt a more conservative haemoglobin threshold for transfusion.
Strategies to address these are referred to as the three pillars of blood conservation/management [68, 120].
(1) Preoperative anaemia
Peri‐operative anaemia and anaemia in hospitalized patients in general is common. The reported prevalence of anaemia in patients presenting for elective surgery varies between 5 and 75% depending on the patient population being screened, underlying pathology and definition of anaemia [121]. In addition, iron and other haematinic deficiencies without anaemia are frequent, particularly among the elderly population, and may compromise patients’ ability to recover haemoglobin following surgery [122, 123].
Anaemia is associated with increased morbidity, hospital length of stay, and mortality [124] and a significant predictor of transfusion usage [68, 125]. Transfusion to treat anaemia, however, has been demonstrated to be an independent and additive risk factor for adverse outcomes [37, 126, 127]. Experts have identified anaemia detection, evaluation and appropriate management as a specific intervention opportunity to reduce transfusion and improve patient outcomes [128]. Anaemia should be viewed as a significant clinical condition, not simply an abnormal laboratory value, and unexplained anaemia warrants immediate attention and proper management prior to surgery in elective cases [128, 129].
Anaemia management with iron (enteral or parenteral), haematinics and with or without erythropoiesis‐stimulating agents (ESAs) has been achieved in a wide range of clinical settings. Anaemia management is an important part of PBM and has been shown to result in the reduction or avoidance of transfusion [105, 107, 110, 130].
2. Surgical blood loss
Peri‐operative blood loss can be reduced by employing a variety of strategies dependent upon the nature of the procedure and patient factors including [100, 131, 132]:
-
•
meticulous surgical technique and use of technical aids such as harmonic scalpel or argon beam coagulation
-
•
cell salvage and re‐transfusion of surgical blood loss
-
•
anaesthetic considerations such as type of anaesthetic agent and technique, maintenance of normothermia and judicious use of fluid replacement
-
•
use of pharmacologic agents such as antifibrinolytics.
3. Tolerance of anaemia
Adoption of a lower haemoglobin‐based trigger for transfusion as recommended in consensus guidelines is the third important strategy to reduce unnecessary transfusion exposure. As previously noted, several lines of evidence indicate that restrictive transfusion strategies are safe for the vast majority of patients.
Similar principles can be applied to medical patients. Tools and guidelines to assist clinicians in implementing blood management strategies are now available in the medical literature, websites and texts [133, 134, 135, 136, 137, 138, 139], for example, the 2007 Clinical Practice Guidelines for Peri‐operative Blood Transfusion and Blood Conservation developed by the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists [64]. In Australia and New Zealand, revision of the Guidelines for Clinical Use of Blood Components [65] is underway. The new guidelines will provide a PBM approach to care across the whole spectrum of medical, surgical, obstetric and paediatric/neonatal settings, with the first two guidelines, peri‐operative patient blood management and patient blood management in critical bleeding and massive blood loss, anticipated to be released in the first half of 2010.
The most successful adoption of blood management practices has occurred where there is a team approach with strong commitment by all management and staff to reduce transfusion exposure. It involves a co‐ordinated, multidisciplinary and multimodality approach, with management tailored to the individual patient’s needs. Data collection and monitoring to evaluate progress, ongoing education and communication to patients and staff and readiness to adopt new evidence‐based methods or techniques are also essential [100, 117].
This article has focused on the patient population at risk of receiving 1–3 units of red cells, the largest group at risk. Those patients with haemorrhagic disorders or critical anaemia were not addressed. In these patients, despite the fact that transfusions can improve short‐term survival, it remains a potential risk factor for adverse outcomes. The principles of PBM still apply but the issues are different. Transfusion may be indicated while all efforts to contain bleeding are made. The quality and quantity of the transfusion is more important than emphasizing avoidance of transfusion. Having kept the patient alive in order for the underlying cause to be treated, PBM has a role in tolerating anaemia, restoring haemoglobin as quickly as possible and minimizing further blood loss. In these patients, it is unlikely that level I evidence from RCTs will ever be available and the focus will remain on the clinical approach to care and the quality and quantity of blood products they receive.
The future
There is a growing interest in PBM: more programmes are being established, it is on the agenda of major medical meetings, numerous publications are present in the medical literature and professional societies dedicated to furthering PBM have been founded throughout the world. These all foster an exchange of ideas and information and further promote the adoption and expansion of blood management.
However, the ‘silent transfusion epidemic’ [140, 141, 142], as it has been called, still continues. Apart from the HIV and HBV ‘blood scandals’, the potential and actual harm to patients caused through inappropriate transfusions is not sufficiently tangible for the public and clinicians [127, 143].
This has to change. Transfusion is a transplant and should never be a trivial decision. PBM is possible today and needs to be implemented in our hospitals. The medical, physiological, ethical, legal and economic evidence cannot be ignored. PBM is plainly good medical practice and more importantly, good medical common sense.
PL5
References
- 1. Hippocratic Oath, original translated into English. Available at: http://en.wikipedia.org/wiki/Hippocratic_Oath#cite_note-2 (accessed July 2009)
- 2. Compiled from Western Australia tomorrow: population projections for planning regions 2004 to 2031 and local government areas 2004 to 2021 Population report (Western Australian Planning Commission); no. 6, 2005, Perth, WA [Google Scholar]
- 3. Wells AW, Mounter PJ, Chapman CE, Stainsby D, Wallis JP: Where does blood go? Prospective observational study of red cell transfusion in north England. BMJ 2002; 325:803–804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Blood Collection and Utilisation Survey Report 2007 ; Department of Health and Human Services, US. Available at http://www.hhs.gov/ophs/bloodsafety/2007nbcus_survey.pdf
- 5. UK Department of Health . Available at: http://hospital.blood.co.uk/library/pdf/NCG_Letter_to_Hospitals_final_dec07%20(2).pdf (accessed July 2009)
- 6. Cremieux PY, Barrett B, Anderson K, Slavin MB: Cost of outpatient blood transfusion in cancer patients. J Clin Oncol 2000; 18:2755–2761 [DOI] [PubMed] [Google Scholar]
- 7. Cantor SB, Hudson DV Jr, Lichtiger B, Rubenstein EB: Costs of blood transfusion: a process‐flow analysis. J Clin Oncol 1998; 16:2364–2370 [DOI] [PubMed] [Google Scholar]
- 8. Shander A, Hofmann A, Gombotz H, Theusinger OM, Spahn DR: Estimating the cost of blood: past, present, and future directions. Best Pract Res Clin Anaesthesiol 2007; 21:271–289 [DOI] [PubMed] [Google Scholar]
- 9. Shander A, Hofmann A, Ozawa S, Theusinger O, Eombotz H, Spabn D on behalf of the COBCON participants : Transfusion 2009; in press [Google Scholar]
- 10. ARCBS . Available at: http://www.transfusion.com.au/Consent-and-Risk.aspx (accessed July 2009)
- 11. SHOT UK . Available at: http://www.shotuk.org (accessed July 2009)
- 12. Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP: Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta‐analysis. J Trauma 2003; 54:908–914 [DOI] [PubMed] [Google Scholar]
- 13. Marik PE, Corwin HL: Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med 2008; 36:2667–2674 [DOI] [PubMed] [Google Scholar]
- 14. Manganaro L, Cytron M, Lesko MF, Arnzen K, Cappadoro C, Fu M, Plisco MS, Sadaka FG, Veremakis C: Red blood cell transfusions and nosocomial infections in critically ill patients. Crit Care Med 2006; 34:2302–2308 [DOI] [PubMed] [Google Scholar]
- 15. Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB: Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30‐day mortality, surgical‐site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg 2009;208: 931–937, 7 e1–2; discussion 8–9 [DOI] [PubMed] [Google Scholar]
- 16. Shander A, Spence RK, Adams D, Shore‐Lesserson L, Walawander CA: Timing and incidence of postoperative infections associated with blood transfusion: analysis of 1,489 orthopedic and cardiac surgery patients. Surg Infect (Larchmt) 2009; 10:277–283 [DOI] [PubMed] [Google Scholar]
- 17. Corwin HL, Gettinger A, Pearl RG et al. : The CRIT Study: anemia and blood transfusion in the critically ill – current clinical practice in the United States. Crit Care Med 2004; 32:39–52 [DOI] [PubMed] [Google Scholar]
- 18. Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD: Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007; 116:2544–2552 [DOI] [PubMed] [Google Scholar]
- 19. Malone DL, Dunne J, Tracy JK, Putnam AT, Scalea TM, Napolitano LM: Blood transfusion, independent of shock severity, is associated with worse outcome in trauma J Trauma 2003; 54:898–905; discussion ‐7 [DOI] [PubMed] [Google Scholar]
- 20. Chaiwat O, Lang JD, Vavilala MS et al. : Early packed red blood cell transfusion and acute respiratory distress syndrome after trauma. Anesthesiology 2009; 110:351–360 [DOI] [PubMed] [Google Scholar]
- 21. Croce MA, Tolley EA, Claridge JA, Fabian TC: Transfusions result in pulmonary morbidity and death after a moderate degree of injury. J Trauma 2005; 59:19–23; discussion ‐4 [DOI] [PubMed] [Google Scholar]
- 22. Koch CG, Li L, Duncan AI et al. : Morbidity and mortality risk associated with red blood cell and blood‐component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006; 34:1608–1616 [DOI] [PubMed] [Google Scholar]
- 23. Rao SV, Jollis JG, Harrington RA et al. : Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004; 292:1555–1562 [DOI] [PubMed] [Google Scholar]
- 24. Doyle BJ, Rihal CS, Gastineau DA, Holmes DR Jr: Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J Am Coll Cardiol 2009; 53:2019–2027 [DOI] [PubMed] [Google Scholar]
- 25. Salim A, Hadjizacharia P, DuBose J et al. : Role of anemia in traumatic brain injury. J Am Coll Surg 2008; 207:398–406 [DOI] [PubMed] [Google Scholar]
- 26. Khorana AA, Francis CW, Blumberg N, Culakova E, Refaai MA, Lyman GH: Blood transfusions, thrombosis, and mortality in hospitalized patients with cancer. Arch Intern Med 2008; 168:2377–2381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bateman ST, Lacroix J, Boven K et al. : Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med 2008; 178:26–33 [DOI] [PubMed] [Google Scholar]
- 28. Engoren M, Mitchell E, Perring P, Sferra J: The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma 2008; 65:1411–1415 [DOI] [PubMed] [Google Scholar]
- 29. Surgenor SD, DeFoe GR, Fillinger MP et al. : Intraoperative red blood cell transfusion during coronary artery bypass graft surgery increases the risk of postoperative low‐output heart failure. Circulation 2006; 114:I43–I48 [DOI] [PubMed] [Google Scholar]
- 30. Reeves BC, Murphy GJ: Increased mortality, morbidity, and cost associated with red blood cell transfusion after cardiac surgery. Curr Opin Cardiol 2008; 23:607–612 [DOI] [PubMed] [Google Scholar]
- 31. Blumberg N: Deleterious clinical effects of transfusion immunomodulation: proven beyond a reasonable doubt. Transfusion 2005; 45:33S–39S; discussion 9S–40S [DOI] [PubMed] [Google Scholar]
- 32. Atzil S, Arad M, Glasner A et al. : Blood transfusion promotes cancer progression: a critical role for aged erythrocytes. Anesthesiology 2008; 109:989–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ: Effect of blood transfusion on long‐term survival after cardiac operation. Ann Thorac Surg 2002; 74:1180–1186 [DOI] [PubMed] [Google Scholar]
- 34. Koch CG, Li L, Duncan AI et al. : Transfusion in coronary artery bypass grafting is associated with reduced long‐term survival. Ann Thorac Surg 2006; 81:1650–1657 [DOI] [PubMed] [Google Scholar]
- 35. Surgenor SD, Kramer RS, Olmstead EM et al. : The association of perioperative red blood cell transfusions and decreased long‐term survival after cardiac surgery. Anesth Analg 2009; 108:1741–1746 [DOI] [PubMed] [Google Scholar]
- 36. Bochicchio GV, Napolitano L, Joshi M, Bochicchio K, Meyer W, Scalea TM: Outcome analysis of blood product transfusion in trauma patients: a prospective, risk‐adjusted study. World J Surg 2008; 32:2185–2189 [DOI] [PubMed] [Google Scholar]
- 37. Beattie WS, Karkouti K, Wijeysundera DN, Tait G: Risk associated with preoperative anemia in noncardiac surgery: a single‐center cohort study. Anesthesiology 2009; 110:574–581 [DOI] [PubMed] [Google Scholar]
- 38. Karkouti K, Wijeysundera DN, Yau TM et al. : Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 2009; 119:495–502 [DOI] [PubMed] [Google Scholar]
- 39. Rogers MA, Blumberg N, Saint SK, Kim C, Nallamothu BK, Langa KM: Allogeneic blood transfusions explain increased mortality in women after coronary artery bypass graft surgery. Am Heart J 2006; 152:1028–1034 [DOI] [PubMed] [Google Scholar]
- 40. Palmieri TL, Caruso DM, Foster KN et al. : Effect of blood transfusion on outcome after major burn injury: a multicenter study. Crit Care Med 2006; 34:1602–1607 [DOI] [PubMed] [Google Scholar]
- 41. Koch CG, Li L, Sessler DI et al. : Duration of red‐cell storage and complications after cardiac surgery. N Engl J Med 2008; 358:1229–1239 [DOI] [PubMed] [Google Scholar]
- 42. Weinberg JA, McGwin G Jr, Marques MB et al. : Transfusions in the less severely injured: does age of transfused blood affect outcomes? J Trauma 2008; 65:794–798 [DOI] [PubMed] [Google Scholar]
- 43. Blumberg N: Allogeneic transfusion and infection: economic and clinical implications. Semin Hematol 1997; 34:34–40 [PubMed] [Google Scholar]
- 44. Spiess BD: Red cell transfusions and guidelines: a work in progress. Hematol Oncol Clin North Am 2007; 21:185–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lieberman JA, Weiskopf RB, Kelley SD et al. : Critical oxygen delivery in conscious humans is less than 7.3 ml O2 x kg(‐1) x min(‐1). Anesthesiology 2000; 92:407–413 [DOI] [PubMed] [Google Scholar]
- 46. Viele MK, Weiskopf RB: What can we learn about the need for transfusion from patients who refuse blood? The experience with Jehovah’s Witnesses. Transfusion 1994; 34:396–401 [DOI] [PubMed] [Google Scholar]
- 47. Tobian AA, Ness PM, Noveck H, Carson JL: Time course and etiology of death in patients with severe anemia. Transfusion 2009; 49:1395–1399 [DOI] [PubMed] [Google Scholar]
- 48. Weiskopf RB, Viele MK, Feiner J et al. : Human cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA 1998; 279:217–221 [DOI] [PubMed] [Google Scholar]
- 49. Hebert PC, Wells G, Blajchman MA et al. : A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999; 340:409–417 [DOI] [PubMed] [Google Scholar]
- 50. Hebert PC, Yetisir E, Martin C et al. : Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases? Crit Care Med 2001; 29:227–234 [DOI] [PubMed] [Google Scholar]
- 51. McIntyre L, Hebert PC, Wells G et al. : Is a restrictive transfusion strategy safe for resuscitated and critically ill trauma patients? J Trauma 2004; 57:563–568; discussion 8 [DOI] [PubMed] [Google Scholar]
- 52. McIntyre LA, Fergusson DA, Hutchison JS et al. : Effect of a liberal versus restrictive transfusion strategy on mortality in patients with moderate to severe head injury. Neurocrit Care 2006; 5:4–9 [DOI] [PubMed] [Google Scholar]
- 53. Lacroix J, Hebert PC, Hutchison JS et al. : Transfusion strategies for patients in pediatric intensive care units. N Engl J Med 2007; 356:1609–1619 [DOI] [PubMed] [Google Scholar]
- 54. Bell EF, Strauss RG, Widness JA et al. : Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics 2005; 115:1685–1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kirpalani H, Whyte RK, Andersen C et al. : The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 2006; 149:301–307 [DOI] [PubMed] [Google Scholar]
- 56. Carson JL, Hill S, Carless P, Hebert P, Henry D: Transfusion triggers: a systematic review of the literature. Transfus Med Rev 2002; 16:187–199 [DOI] [PubMed] [Google Scholar]
- 57. Holzer BR, Egger M, Teuscher T, Koch S, Mboya DM, Smith GD: Childhood anemia in Africa: to transfuse or not transfuse? Acta Trop 1993; 55:47–51 [DOI] [PubMed] [Google Scholar]
- 58. Bojang KA, Palmer A, Boele van Hensbroek M, Banya WA, Greenwood BM: Management of severe malarial anaemia in Gambian children. Trans R Soc Trop Med Hyg 1997; 91:557–561 [DOI] [PubMed] [Google Scholar]
- 59. Meremikwu M, Smith HJ: Blood transfusion for treating malarial anaemia. Cochrane Database Syst Rev 2007; 1:CD001475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Consensus Conference : Perioperative red blood cell transfusion. JAMA 1988; 260:2700–2703 [PubMed] [Google Scholar]
- 61. Simon TL, Alverson DC, AuBuchon J et al. : Practice parameter for the use of red blood cell transfusions: developed by the Red Blood Cell Administration Practice Guideline Development Task Force of the College of American Pathologists. Arch Pathol Lab Med 1998; 122:130–138 [PubMed] [Google Scholar]
- 62. American College of Physicians : Practice strategies for elective red blood cell transfusion. American College of Physicians. Ann Intern Med 1992; 116:403–406 [DOI] [PubMed] [Google Scholar]
- 63. An Updated Report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies: Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology 2006; 105:198–208 [DOI] [PubMed] [Google Scholar]
- 64. Ferraris VA, Ferraris SP, Saha SP et al. : Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guideline. Ann Thorac Surg 2007; 83:S27–S86 [DOI] [PubMed] [Google Scholar]
- 65. NHMRC/ASBT : Clinical Practice Guidelines on the Use of Blood and Blood Components. Commonwealth of Australia, NHMRC/ASBT, 2001. [Google Scholar]
- 66. Madjdpour C, Spahn DR, Weiskopf RB: Anemia and perioperative red blood cell transfusion: a matter of tolerance. Crit Care Med 2006; 34:S102–S108 [DOI] [PubMed] [Google Scholar]
- 67. Spence RK: Surgical red blood cell transfusion practice policies. Blood Management Practice Guidelines Conference. Am J Surg 1995; 170:3S–15S [DOI] [PubMed] [Google Scholar]
- 68. Gombotz H, Rehak PH, Shander A, Hofmann A: Blood use in elective surgery: the Austrian benchmark study. Transfusion 2007; 47:1468–1480 [DOI] [PubMed] [Google Scholar]
- 69. Daly DJ, Myles PS, Smith JA et al. : Anticoagulation, bleeding and blood transfusion practices in Australasian cardiac surgical practice. Anaesth Intensive Care 2007; 35:760–768 [DOI] [PubMed] [Google Scholar]
- 70. Stover EP, Siegel LC, Parks R et al. : Variability in transfusion practice for coronary artery bypass surgery persists despite national consensus guidelines: a 24‐institution study. Institutions of the Multicenter Study of Perioperative Ischemia Research Group. Anesthesiology 1998; 88:327–333 [DOI] [PubMed] [Google Scholar]
- 71. Shehata N, Wilson K, Mazer CD et al. : The proportion of variation in perioperative transfusion decisions in Canada attributable to the hospital: [La proportion de variation dans les pratiques transfusionnelles perioperatoires au Canada imputable aux hopitaux]. Can J Anaesth 2007; 54:902–907 [DOI] [PubMed] [Google Scholar]
- 72. Hutton B, Fergusson D, Tinmouth A, McIntyre L, Kmetic A, Hebert PC: Transfusion rates vary significantly amongst Canadian medical centres. Can J Anaesth 2005; 52:581–590 [DOI] [PubMed] [Google Scholar]
- 73. Rao SV, Chiswell K, Sun JL et al. : International variation in the use of blood transfusion in patients with non‐ST‐segment elevation acute coronary syndromes. Am J Cardiol 2008; 101:25–29 [DOI] [PubMed] [Google Scholar]
- 74. Snyder‐Ramos SA, Mohnle P, Weng YS et al. : The ongoing variability in blood transfusion practices in cardiac surgery. Transfusion 2008; 48:1284–1299 [DOI] [PubMed] [Google Scholar]
- 75. Howick J, Glasziou P, Aronson JK: The evolution of evidence hierarchies: what can Bradford Hill’s ‘guidelines for causation’ contribute? J R Soc Med 2009; 102:186–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vlahakes GJ: The value of phase 4 clinical testing. N Engl J Med 2006; 354:413–415 [DOI] [PubMed] [Google Scholar]
- 77. Reuters : Available at: http://www.reuters.com/article/idUS122936+22-Apr-2009+PRN20090402 (accessed April 2009)
- 78. Fitch K, Bernstein SJ, Aguilar MS, Burnand B, LaCalle JR, Lazaro P, Van Het Loo M, McDonnell J, Vader J, Kahan JP: The RAND/UCLA Appropriateness Method User’s Manual. Available at: http://www.rand.org/pubs/monograph_reports/MR1269/ (accessed July 2009) [Google Scholar]
- 79. Sazama K: The ethics of blood management. Vox Sang 2007; 92:95–102 [DOI] [PubMed] [Google Scholar]
- 80. Farmer S: Your Body, Your Choice. Singapore, Media Masters, 2000. [Google Scholar]
- 81. Eurobarometer : Europeans and Blood. Prepared for the European Commission on Employment, Industrial Relations and Social Affairs. Paris, Institut National de la recherche Agronomique, 1995. [Google Scholar]
- 82. Lowe KC, Ferguson E: Benefit and risk perceptions in transfusion medicine: blood and blood substitutes. J Intern Med 2003; 253:498–507 [DOI] [PubMed] [Google Scholar]
- 83. Farmer S, Webb D: Your body, your choice. Media Masters, Singapore, 2000. [Google Scholar]
- 84. Spahn DR, Moch H, Hofmann A, Isbister JP: Patient blood management: the pragmatic solution for the problems with blood transfusions. Anesthesiology 2008; 109:951–953 [DOI] [PubMed] [Google Scholar]
- 85. Bodnaruk ZM, Wong CJ, Thomas MJ: Meeting the clinical challenge of care for Jehovah’s Witnesses. Transfus Med Rev 2004; 18:105–116 [DOI] [PubMed] [Google Scholar]
- 86. Ott DA, Cooley DA: Cardiovascular surgery in Jehovah’s Witnesses. Report of 542 operations without blood transfusion. JAMA 1977; 238:1256–1258 [PubMed] [Google Scholar]
- 87. Cooley DA, Crawford ES, Howell JF, Beall AC Jr: Open heart surgery in Jehovah’s Witnesses. Am J Cardiol 1964; 13:779–781 [DOI] [PubMed] [Google Scholar]
- 88. Carmichael MJ, Cooley DA, Kuykendall RC, Walker WE: Cardiac surgery in children of Jehovah’s Witnesses. Tex Heart Inst J 1985; 12:57–63 [PMC free article] [PubMed] [Google Scholar]
- 89. Reyes G, Nuche JM, Sarraj A et al. : Bloodless cardiac surgery in Jehovah’s witnesses: outcomes compared with a control group. Rev Esp Cardiol 2007; 60:727–731 [PubMed] [Google Scholar]
- 90. Jabbour N, Gagandeep S, Mateo R et al. : Live donor liver transplantation without blood products: strategies developed for Jehovah’s Witnesses offer broad application. Ann Surg 2004; 240:350–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kitchens CS: Are transfusions overrated? Surgical outcome of Jehovah’s Witnesses. Am J Med 1993; 94:117–119 [DOI] [PubMed] [Google Scholar]
- 92. Joseph SA Jr, Berekashvili K, Mariller MM et al. : Blood conservation techniques in spinal deformity surgery: a retrospective review of patients refusing blood transfusion. Spine 2008; 33:2310–2315 [DOI] [PubMed] [Google Scholar]
- 93. Nelson CL, Bowen WS: Total hip arthroplasty in Jehovah’s Witnesses without blood transfusion. J Bone Joint Surg Am 1986; 68:350–353 [PubMed] [Google Scholar]
- 94. Varela JE, Gomez‐Marin O, Fleming LE, Cohn SM: The risk of death for Jehovah’s Witnesses after major trauma. J Trauma 2003; 54:967–972 [DOI] [PubMed] [Google Scholar]
- 95. Chigbu B, Onwere S, Kamanu C et al. : Lessons learned from the outcome of bloodless emergency laparotomies on Jehovah’s Witness women presenting in the extremis with ruptured uterus. Arch Gynecol Obstet 2009; 279:469–472 [DOI] [PubMed] [Google Scholar]
- 96. Bonakdar MI, Eckhous AW, Bacher BJ, Tabbilos RH, Peisner DB: Major gynecologic and obstetric surgery in Jehovah’s Witnesses. Obstet Gynecol 1982; 60:587–590 [PubMed] [Google Scholar]
- 97. DeCastro RM: Bloodless surgery: establishment of a program for the special medical needs of the Jehovah’s witness community – the gynecologic surgery experience at a community hospital. Am J Obstet Gynecol 1999; 180:1491–1498 [DOI] [PubMed] [Google Scholar]
- 98. Rosengart TK, Helm RE, DeBois WJ, Garcia N, Krieger KH, Isom OW: Open heart operations without transfusion using a multimodality blood conservation strategy in 50 Jehovah’s Witness patients: implications for a “bloodless” surgical technique. J Am Coll Surg 1997; 184:618–629 [PubMed] [Google Scholar]
- 99. Estioko MR, Litwak RS, Rand JH: Reoperation, emergency and urgent open cardiac surgery in Jehovah’s Witnesses. Chest 1992; 102:50–53 [DOI] [PubMed] [Google Scholar]
- 100. Martyn V, Farmer SL, Wren MN et al. : The theory and practice of bloodless surgery. Transfus Apher Sci 2002; 27:29–43 [DOI] [PubMed] [Google Scholar]
- 101. Morgan TO: Cost, quality, and risk: measuring and stopping the hidden costs of coronary artery bypass graft surgery. Am J Health Syst Pharm 2005; 62:S2–S5 [DOI] [PubMed] [Google Scholar]
- 102. Freedman J, Luke K, Escobar M, Vernich L, Chiavetta JA: Experience of a network of transfusion coordinators for blood conservation (Ontario Transfusion Coordinators [ONTraC]). Transfusion 2008; 48:237–250 [DOI] [PubMed] [Google Scholar]
- 103. Freedman J, Luke K, Monga N et al. : A provincial program of blood conservation: the Ontario Transfusion Coordinators (ONTraC). Transfus Apher Sci 2005; 33:343–349 [DOI] [PubMed] [Google Scholar]
- 104. Personal communication
- 105. Moskowitz DM, Klein JJ, Shander A et al. : Predictors of transfusion requirements for cardiac surgical procedures at a blood conservation center. Ann Thorac Surg 2004; 77:626–634 [DOI] [PubMed] [Google Scholar]
- 106. Cardiac Surgery in New Jersey 2006. Available at: http://www.state.nj.us/health/healthcarequality/cardiacsurgery.shtml#CSR (accessed July 2009)
- 107. Brevig J, McDonald J, Zelinka ES, Gallagher T, Jin R, Grunkemeier GL: Blood transfusion reduction in cardiac surgery: multidisciplinary approach at a community hospital. Ann Thorac Surg 2009; 87:532–539 [DOI] [PubMed] [Google Scholar]
- 108. Green JA: Blood conservation in cardiac surgery: the Virginia Commonwealth University (VCU) experience. J Cardiothorac Vasc Anesth 2004; 18:18S–23S [DOI] [PubMed] [Google Scholar]
- 109. Morgan TO: Blood conservation: the CEO perspective. J Cardiothorac Vasc Anesth 2004; 18:15S–17S [DOI] [PubMed] [Google Scholar]
- 110. Ghiglione M: Blood management: a model of excellence. Clin Leadersh Manag Rev 2007; 21:E2 [PubMed] [Google Scholar]
- 111. Helm RE, Rosengart TK, Gomez M et al. : Comprehensive multimodality blood conservation: 100 consecutive CABG operations without transfusion. Ann Thorac Surg 1998; 65:125–136 [DOI] [PubMed] [Google Scholar]
- 112. Martinez V, Monsaingeon‐Lion A, Cherif K, Judet T, Chauvin M, Fletcher D: Transfusion strategy for primary knee and hip arthroplasty: impact of an algorithm to lower transfusion rates and hospital costs. Br J Anaesth 2007; 99:794–800 [DOI] [PubMed] [Google Scholar]
- 113. Lopez Soques MM, Leon A, Garcia Alvarez J, Garces P, Saez M: Benefit of a blood conservation program in elective orthopaedic surgery. Med Clin (Barc) 2002; 119:650–652 [DOI] [PubMed] [Google Scholar]
- 114. Slappendel R, Dirksen R, Weber EW, Van Der Schaaf DB: An algorithm to reduce allogenic red blood cell transfusions for major orthopedic surgery. Acta Orthop Scand 2003; 74:569–575 [DOI] [PubMed] [Google Scholar]
- 115. Jabbour N, Gagandeep S, Mateo R, Sher L, Genyk Y, Selby R: Transfusion free surgery: single institution experience of 27 consecutive liver transplants in Jehovah’s Witnesses. J Am Coll Surg 2005; 201:412–417 [DOI] [PubMed] [Google Scholar]
- 116. Ballen KK, Becker PS, Yeap BY, Matthews B, Henry DH, Ford PA: Autologous stem‐cell transplantation can be performed safely without the use of blood‐product support. J Clin Oncol 2004; 22:4087–4094 [DOI] [PubMed] [Google Scholar]
- 117. Goodnough LT, Shander A: Blood management. Arch Pathol Lab Med 2007; 131:695–701 [DOI] [PubMed] [Google Scholar]
- 118. Williams D, McCarthy R: Identifying patients for blood conservation strategies (Br J Surg 2002; 89: 1176–1182). Br J Surg 2003; 90:368 [DOI] [PubMed] [Google Scholar]
- 119. Goodnough LT, Shander A, Spence R: Bloodless medicine: clinical care without allogeneic blood transfusion. Transfusion 2003; 43:668–676 [DOI] [PubMed] [Google Scholar]
- 120. Baele P, Van der Linden P: Developing a blood conservation strategy in the surgical setting. Acta Anaesthesiol Belg 2002; 53:129–136 [PubMed] [Google Scholar]
- 121. Shander A, Knight K, Thurer R, Adamson J, Spence R: Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med 2004; 116(Suppl. 7A):58S–69S [DOI] [PubMed] [Google Scholar]
- 122. Munoz M, Garcia‐Erce JA, Cuenca J, Bisbe E: Pharmacological management of perioperative anaemia: our experience with intravenous iron in orthopaedic surgery. ISBT Sci Ser 2007; 2:257–263 [Google Scholar]
- 123. Andrews CM, Lane DW, Bradley JG: Iron pre‐load for major joint replacement. Transfus Med 1997; 7:281–286 [DOI] [PubMed] [Google Scholar]
- 124. Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ: The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 2002; 16:39–44 [DOI] [PubMed] [Google Scholar]
- 125. Khanna MP, Hebert PC, Fergusson DA: Review of the clinical practice literature on patient characteristics associated with perioperative allogeneic red blood cell transfusion. Transfus Med Rev 2003; 17:110–119 [DOI] [PubMed] [Google Scholar]
- 126. Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM: Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res 2002; 102:237–244 [DOI] [PubMed] [Google Scholar]
- 127. Rawn J: The silent risks of blood transfusion. Curr Opin Anaesthesiol 2008; 21:664–668 [DOI] [PubMed] [Google Scholar]
- 128. Goodnough LT, Shander A, Spivak JL et al. : Detection, evaluation, and management of anemia in the elective surgical patient. Anesth Analg 2005; 101:1858–1861 [DOI] [PubMed] [Google Scholar]
- 129. Shander A, Javidroozi M, Goodnough LT: Anemia screening in elective surgery: definition, significance and patients’ interests. Anesth Analg 2006; 103:778–779; author reply 9‐80 [DOI] [PubMed] [Google Scholar]
- 130. Earley AS, Gracias VH, Haut E et al. : Anemia management program reduces transfusion volumes, incidence of ventilator‐associated pneumonia, and cost in trauma patients. J Trauma 2006; 61:1–5; discussion ‐7 [DOI] [PubMed] [Google Scholar]
- 131. Spahn DR, Casutt M: Eliminating blood transfusions: new aspects and perspectives. Anesthesiology 2000; 93:242–255 [DOI] [PubMed] [Google Scholar]
- 132. Shander A: Surgery without blood. Crit Care Med 2003; 31:S708–S714 [DOI] [PubMed] [Google Scholar]
- 133. Seeber P: Basics of Blood Management. MA, USA, Blackwell Publishing, 2008. [Google Scholar]
- 134. Speiss B: Perioperative Transfusion Medicine. Philadelphia, PA, USA, Lippincott Williams & Wilkins, 2006. [Google Scholar]
- 135. Jabbour N: Transfusion‐Free Medicine and Surgery. MA, USA, Blackwell Publishing, 2005. [Google Scholar]
- 136. Waters J: Blood Management: Options for Better Patient Care. Bethesda, MD, USA, AABB Press, 2008. [Google Scholar]
- 137. Society for the Advancement of Blood Management . Available at: http://www.sabm.org (accessed July 2009)
- 138. Medical Society for Blood Managment . Available at: http://www.bloodmanagement.org (accessed July 2009)
- 139. Network for the Advancement of Transfusion Alternatives . Available at: http://www.nataonline.com (accessed July 2009)
- 140. Blumberg N, Heal JM: Blood transfusion immunomodulation: the silent epidemic. Arch Pathol Lab Med 1998; 122:117–119 [PubMed] [Google Scholar]
- 141. Spiess BD: Blood transfusion: the silent epidemic. Ann Thorac Surg 2001; 72:S1832–S1837 [DOI] [PubMed] [Google Scholar]
- 142. Rawn JD: Blood transfusion in cardiac surgery: a silent epidemic revisited. Circulation 2007; 116:2523–2524 [DOI] [PubMed] [Google Scholar]
- 143. Isbister JP: Clinicians as gatekeepers: what is the best route to optimal blood use? Dev Biol (Basel) 2007; 127:9–14 [PubMed] [Google Scholar]


