Dear Editor,
Since last month, the coronavirus disease (COVID-19) epidemic, which is caused by severe acute respiratory disease coronavirus 2 (SARS-COV-2) infection, has rapidly spread around the world. SARS-COV-2 has stronger infectivity than SARS, and can easily cause cross infection in hospitals [1]. In the early stage of the epidemic in Wuhan, China, most of the infected workers were not in respiratory department but in neurosurgery or ophthalmology departments, so practical experience of protection was needed for operations. However, in the Department of Ophthalmology (DO) of Tongji Hospital in Wuhan City, no medical staff were infected despite treatment of a large number of COVID-19 patients and patients undergoing emergency eye surgery during the 3-month outbreak.
During the outbreak, some DO staff were assigned to participate in the treatment of infected patients, while the others carried out emergency ophthalmic work. Special workflows had to be developed to cope with this situation, to screen infected patients whenever possible and to adopt different prevention strategies during the perioperative period. The emergency operation staff were trained in protective knowledge and the procedure of emergency operations (Fig. 1). To discover the source of infection in time and avoid large-scale cross infection among colleagues, temperatures of DO staff were checked twice everyday, and further checks were made for those who had symptoms of infection.
Fig. 1.
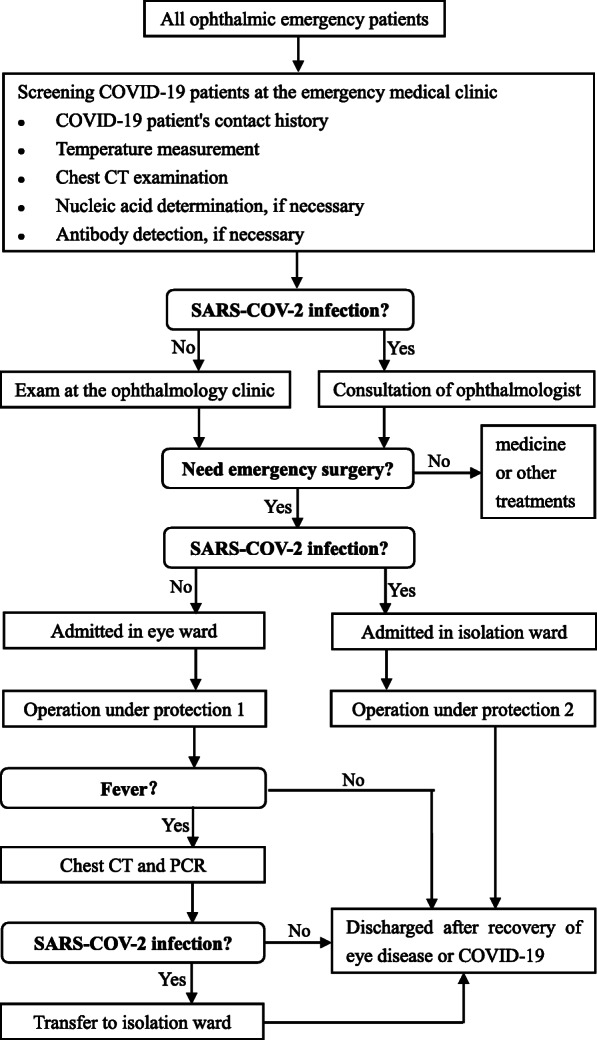
Procedures for emergency patients during the epidemic. Some exams are required in the outpatient clinic to screen COVID-19 patients. Patients infected with SARS-COV-2 are admitted to isolation wards before or after ophthalmic emergency surgery. Protections 1 and 2 are detailed in Table 1
The scope of emergency surgery was defined based on the specific epidemic prevention and control measures in Tongji Hospital and Wuhan City, focusing on glaucoma surgery, emergency vitrectomy, debridement suture surgery and treatment of retinopathy of preterm infants. Glaucoma surgery was the most common emergency surgery during the epidemic, and eye trauma surgery was rare, possibly because people were less active outside. To reduce the risk of cross infection, operation methods had to be considered that minimised follow-up frequency and time spent in hospital. For example, the first emergency operation we performed during the epidemic was for a 60-year-old female patient suffering from recurrent attacks of acute angle-closure glaucoma. Normally, we might choose cataract extraction and trabeculectomy surgeries for her, but this time, as a result of the discussion between eye doctors and epidemic prevention experts, we only performed a trabeculectomy and performed a peripheral iridectomy on the other eye to prevent the acute onset of glaucoma. Anaesthesia during the outbreak was also different from usual, using local anaesthesia as often as possible for adults and using either an oxygen mask plus intravenous anaesthesia or laryngeal mask anaesthesia for children [2]. While these measures seemed to be successful at Tongji Hospital, emergency operation plans should be made based on the specific situation of a region.
SARS-COV-2 is mainly transmitted by droplets, aerosols and contact. The aim of protective measures is to cut off these transmission routes [1]. But resources should also be considered as much as possible to save protective materials for the treatment of COVID-19 patients. The following are the recommendations for protection (see also Table 1).
Table 1.
Perioperative protective measures of emergency ophthalmic surgery for medical staff, patients, environment and instruments
| Medical personal protection | Patient protection | Environmental protection | Instrument disinfection | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Masks | Caps | Gloves | Homemade goggles | Protective clothing | Hand hygiene | Masks | Caps | Gloves | Isolation clothing | UV | Air disinfectant | Ventilation | Spraying | Slit lamp | Tonometer | Laser machine | |
| Eye/isolation ward | √ | √⁕ | √ | √⁕ | √⁕ | √ | √ | √ | √ | √ | |||||||
| Transfer between wards and operation room | √ | √⁕ | √ | √⁕ | √ | √ | √⁕ | √⁕ | √⁕ | √ | √ | √ | √⁕ | ||||
| During operation | √ | √ | √ | √ | √⁕ | √ | √ | √⁕ | √⁕ | √⁕ | √ | ||||||
| Medical ward round | √ | √⁕ | √ | √⁕ | √⁕ | √ | √ | √ | √ | ||||||||
| Before or after examination | √ | √⁕ | √ | √⁕ | √ | √ | √ | √ | √ | √⁕ | √ | √ | √ | ||||
| During examination | √ | √ | √ | √⁕ | √⁕ | √ | √ | √⁕ | √⁕ | √ | √ | ||||||
⁕Protective measures for the patients with SARS-COV-2 infection
Wear an N95 mask during surgery or contact with COVID-19 patients. Gloves should be worn in direct contact with patients and even doubled during surgery. But gloves cannot replace hand sanitising, and hand hygiene is the most basic and important thing at all times. Protective clothing is only needed in close contact with COVID-19 patients, such as during surgery or in the isolation ward, and for the most part an isolation suit will suffice. Protective screens are only needed for anaesthetic intubation or throat swab sampling, generally not required by ophthalmologists. Ordinary goggles seriously impede microsurgery. We replaced it with homemade goggles by sealing the own glasses or flat lenses around the eyes with plastic wrap and remove the plastic wrap from the centre of the lens to get protection and clear vision during the ophthalmic microsurgery. Protective shields can be added to the slit lamp microscope to reduce the risk of close face-to-face contact between doctors and patients. Adjust the examination light from weak to strong, increasing gradually to avoid tears or a reflex sneeze [3], which easily produce droplets and aerosol.
Ultraviolet irradiation and air disinfection can effectively inactivate the SARS coronavirus and should be done for SARS-COV-2 [4]. Proper ventilation and instrument disinfection are very necessary, especially in the non-contact tonometer measurement which will produce local aerosol in the process [5].
All patients are recommended to wear masks during hospitalisation and during surgery, and the DO of Tongji Hospital provides them, as well as hand sanitiser, free of charge. COVID-19 patients should wear isolation clothing in the operating room. Psychological counselling is more important than ever for these patients; they will face the dual concerns of eye surgery and cross infection in hospital. Relieving these stresses may help them recover from eye disease and develop resistance to infection [6].
In conclusion, these measures protect both the medical staff and patients in ophthalmic surgery by blocking the transmission of SARS-COV-2 and avoid excessive waste of protective materials. However, it is difficult to determine which measure was most important in the DO of Tongji Hospital, given there were zero infections. Hopefully, our experience will help ophthalmologists get through this outbreak.
Acknowledgements
We would like to express our gratitude to all those who have helped us during the outbreak. We gratefully acknowledge the helps of Professor Yang Hong, Dr. Chen BO and Dr. Zhang Xian in the operations.
Funding information
This work was supported by grants from the Natural Science Foundation of Hubei province, China (Grant No. 2017CFB785).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hao Du and Meng Zhang contributed equally to this work.
Contributor Information
Hao Du, Email: tongjiduhao@163.com.
Meng Zhang, Email: jiandaoshou0126@163.com.
Xufang Sun, Email: sunxufang2016@163.com.
References
- 1.World Health Organization (WHO) (2020) China Joint Mission on coronavirus disease 2019 ( COVID-19 ). 2019:16–24
- 2.Ong GYK, Chan ILY, Ng ASB, et al. Singapore paediatric resuscitation guidelines 2016. Singap Med J. 2017;58:373–390. doi: 10.11622/smedj.2017065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hydén D, Arlinger S. On light-induced sneezing. Eye. 2009;23:2112–2114. doi: 10.1038/eye.2009.165. [DOI] [PubMed] [Google Scholar]
- 4.Duan SM, Zhao XS, Wen RF, et al. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci. 2003;16:246–255. [PubMed] [Google Scholar]
- 5.Britt JM, Clifton BC, Barnebey HS, Mills RP. Microaerosol formation in noncontact ‘air-puff’ tonometry. Arch Ophthalmol. 1991;109:225–228. doi: 10.1001/archopht.1991.01080020071046. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S, Janicki-Deverts D, Turner RB, Doyle WJ. Does hugging provide stress-buffering social support? A study of susceptibility to upper respiratory infection and illness. Psychol Sci. 2015;26:135–147. doi: 10.1177/0956797614559284. [DOI] [PMC free article] [PubMed] [Google Scholar]


