1. Introduction
Unintentional injury remains a leading cause of mortality in children.1–3 Despite advances in trauma systems and critical care, early mortality after injury has persisted.4–7 This early mortality suggests that interventions targeting the early care of injured patients may have the most potential to improve outcomes. While the mortality associated with severe injury is high, the frequency to which severely injured pediatric trauma patients present to emergency departments is low.8, 9 The low frequency of major pediatric trauma resuscitation in emergency rooms results in limited provider experience in these settings.10, 11 This limited experience can lead to errors in management, which are known to be relatively common in trauma care. The results of errors during trauma resuscitation can be catastrophic when the stakes are high.12, 13
Simulation-based training (SBT) is a method that has been associated with improvements in trauma team performance, individual provider confidence, and team communication in simulated and actual trauma resuscitations.14–17 High-fidelity simulation for trauma resuscitation training is costly, however, and to date has no proven benefit on patientlevel clinical outcomes. Single-center studies reporting SBT use for trauma evaluation show the use of a diversity of training methods.17–19 The current nationwide trend in SBT use is not known. Local factors may be associated with usage of SBT as well as barriers to implementation, but these factors have not been described.
The primary objective of this study was to determine the frequency of usage of SBT within pediatric trauma centers in the United States. The secondary objectives of this study were to describe center characteristics associated with the use of SBT, type of SBT used, and barriers to implementation of SBT.
2. Methods
2.1. Study Design, Participants, and Data Collection Procedures
This study was a cross-sectional survey of United States pediatric trauma centers that participated in the American College of Surgeons Trauma Quality Improvement Program (ACS TQIP Pediatric) in calendar year 2016 (N=125). This study was approved by the Institutional Review Board at Children’s Hospital of Los Angeles. Responses from individual trauma centers were obtained from either trauma program managers or trauma medical directors by staff members at ACS TQIP. Trauma center identity was known to ACS TQIP staff but was coded before data release to the study team to preserve center anonymity. Surveys were first administered using Qualtrics online survey software (Provo, UT and Seattle, WA). Telephone surveys were then administered to centers not responding to the online survey.
2.2. Survey Development and Piloting
A 17-item survey was developed by a team of experts in pediatric trauma care and SBT. Domains in this survey included: usage of SBT for trauma resuscitation; annual number of adult and pediatric simulations for each of the past three years; duration of center usage of SBT; characteristics of SBT including the duration of simulation sessions, scheduling, location, and team composition; characteristics of debriefing including frequency and duration; whether sessions were video-recorded; type of SBT scenarios used; and barriers to implementation of SBT including perceived lack of funding, lack of technical expertise, lack of data supporting SBT use, lack of support of SBT by trauma providers and lack of leadership. After iterative revision for content by the developing team of experts, the survey was piloted for content, readability, and understandability by a panel of former trauma program managers.
2.3. Trauma Center Clinical Characteristics and Clinical Volume
Trauma center annual pediatric admissions and self-reported center characteristics were abstracted from the ACS TQIP registry and linked to survey responses. Center characteristics included: hospital teaching status (university, community teaching hospital, or nonteaching hospital), hospital type (for-profit or not-for-profit), ACS pediatric trauma verification level (1, 2, or unverified), state trauma designation level (1, 2, or not designated), association with a pediatric-specific hospital, presence of a pediatric ward or pediatric intensive care unit, and presence of all pediatric acute care services or shared resources with an adult center. Clinical volumes abstracted included: annual number of TQIP-pediatric trauma center admissions; annual number of acute trauma resuscitations with Injury Severity Score (ISS) > 16; annual number of pediatric trauma admissions with age ≤ 18 years; annual number of pediatric trauma admissions with age ≤ 14 years; annual number of pediatric trauma admissions with ISS > 16 and age ≤ 14 years; and annual number of acute pediatric trauma resuscitations with ISS > 16 and age ≤ 14 years. Transfers were excluded from acute resuscitation data.
2.4. Statistical Analyses
Center characteristics were compared between centers that reported using simulation and those that did not using the Mann-Whitney U test for ordinal or interval variables, the Chi-square test for categorical variables, or the Fisher’s exact test for comparisons with less than five events per category. Center characteristics were available for all centers from the TQIP database and were compared between survey respondents and non-respondents to assess response bias. Frequency of SBT use over time was compared for both total trauma SBT use and pediatric-specific SBT use between 2014 and 2016 using the Wilcoxon Signed-Rank test for related samples. Barriers to implementation were scored using an ordinal scale of: 0 – not a barrier, 1 – minor barrier, 2 – major barrier, or 3 – barrier that makes SBT impossible. Scores were treated as ordinal data and compared between centers using and not using SBT with the Mann-Whitney U test. Scores were correlated with annual SBT use within center using Spearman’s Rho (r). Analyses were performed using SPSS v 17.0 (Chicago, IL). All analyses were two-tailed with alpha=0.05.
3. Results
3.1. Response Rate and Characteristics of Respondents
The survey response rate was 75% (94/125), with 78% of respondents (73/94) reporting using SBT to train providers for trauma resuscitation. All respondents provided a response to the primary survey question of whether or not they use SBT for trauma resuscitation, but only 69% (65/94) of surveys included complete responses for all secondary items. Eighty-eight percent (83/94) of respondents provided perceptions related to barriers. Seventy-eight percent (57/73) of SBT users provided quantity of annual sessions and 63% (46/73) quantified the duration of use. Characteristics related to training methodology were provided by 76% (56/73) of SBT users.
Respondents that reported SBT use were more likely to be non-profit, university-based hospitals compared to centers reporting no SBT use (Table 1). No differences between mean annual pediatric trauma volume, the volume of severely injured (ISS > 16) children, or annual number of acute pediatric trauma resuscitations was observed for SBT users and non-users. Non-respondents were less likely to have obtained state or ACS pediatric trauma center verification and less likely to have a pediatric intensive care unit. Mean annual pediatric trauma volume was similar between respondents and non-respondents.
Table 1:
Clinical volume and characteristics of trauma centers participating in the ACS Trauma Quality Improvement Program (TQIP) for centers using vs not using simulation, or not responding to the survey.
| Simulation Use | Survey | ||||
|---|---|---|---|---|---|
| Yes | No | p-value1 | Non-responder | p-value2 | |
| N=73 | N=21 | N=31 | |||
| Annual Trauma Admissions | 1585 (1704) | 1410 (920) | 0.24 | 1671 (1817) | 0.73 |
| Annual Trauma Admissions, Age < 18 | 421 (480) | 309 (518) | 0.27 | 505 (574) | 0.90 |
| Annual Trauma Admissions with ISS >16, Excluding Transfers | 295 (520) | 238 (334) | 0.11 | 289 (381) | 0.72 |
| Annual Trauma Admissions, Age < 14 | 298 (439) | 179 (489) | 0.41 | 389 (461) | 0.84 |
| Annual Trauma Admissions, Age < 14 with ISS >16 | 46 (77) | 35 (42) | 0.30 | 56 (59) | 0.57 |
| Annual Trauma Admissions, Age < 14 with ISS > 16, Excluding Transfers | 17 (28) | 17 (16) | 0.60 | 21 (25) | 0.71 |
| TQIP-Pediatric Trauma Center Type | 0.71 | 0.48 | |||
| Mixed Adult-Pediatric Hospital | 45 (62%) | 12 (57%) | 21 (68%) | ||
| Freestanding Children’s Hospital | 28 (38%) | 9 (43%) | 10 (32%) | ||
| Hospital Teaching Status | 0.01 | 1.00 | |||
| University Hospital | 54 (74%) | 10 (48%) | 19 (61%) | ||
| Community Teaching Hospital | 18 (25%) | 8 (38%) | 11 (35%) | ||
| Nonteaching Hospital | 1 (1%) | 3 (1%) | 1 (3%) | ||
| Hospital Type | 0.03 | 0.36 | |||
| For Profit | 1 (1%) | 3 (14%) | 3 (10%) | ||
| Not for Profit | 72 (99%) | 18 (86%) | 28 (90%) | ||
| ACS Pediatric Verification | 49 (67%) | 12 (57%) | 0.40 | 14 (45%) | 0.05 |
| Level 1 Pediatric Verification | 30 (41%) | 9 (43%) | 8 (26%) | ||
| Level 2 Pediatric Verification | 19 (26%) | 3 (14%) | 6 (19%) | ||
| Not Verified for Pediatric Trauma | 24 (33%) | 9 (43%) | 17 (55%) | ||
| State Pediatric Designation | 53 (73%) | 17 (81%) | 0.44 | 17 (55%) | 0.04 |
| Level 1 State Designation | 38 (52%) | 8 (38%) | 12 (39%) | ||
| Level 2 State Designation | 15 (21%) | 9 (43%) | 5 (16%) | ||
| No State Designation | 20 (27%) | 4 (19%) | 14 (45%) | ||
| Patient Care Characteristics | |||||
| Associated with a Pediatric Hospital | 59 (81%) | 18 (86%) | 0.61 | 25 (81%) | 0.87 |
| Have a Pediatric Ward | 72 (99%) | 21 (100%) | 1.00 | 31 (100%) | 1.00 |
| Have a Pediatric Intensive Care Unit | 73 (100%) | 21 (100%) | 1.00 | 29 (94%) | 0.06 |
| Transfer severely injured children to other centers | 3 (4%) | 2 (10%) | 0.31 | 4 (13%) | 0.22 |
Values expressed as Mean (SD) or N (%). Comparisons performed using Chi-square for categorical variables, Fisher’s Exact for comparisons with less than five events in one category, and Mann-Whitney U for continuous variables.
Simulation Use ‘Yes’ compared to ‘No’ and
Survey non-responders compared to all survey responders.
3.2. Characteristics of Simulation Use and Program Administration
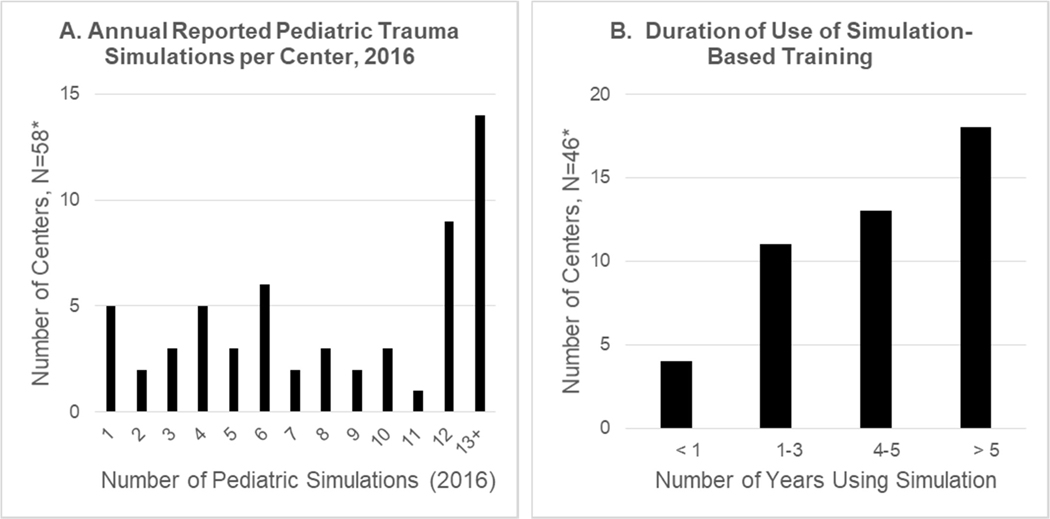
Among centers that reported SBT use, the annual total median SBT use increased from 6.0 (IQR 3,12) SBT sessions in 2014 to 8.5 (IQR 4, 12) SBT sessions in 2016 (p<0.01). Pediatric-specific trauma SBT use also increased from 5.5 (IQR 0,12) pediatric SBT sessions in 2014 to 6.5 (IQR 3, 12) pediatric SBT sessions in 2016 (p<0.01). The frequency of annual SBT sessions ranged from 1 (N=5 centers) to 13+ (N=14 centers). In 67% of centers SBT had been implemented longer than four years (Figure 1a–b). Trauma SBT was most frequently administered as a shared responsibility between the trauma program and a simulation center (41% of respondents), instead of being administered by the trauma program (28%) or simulation center alone (20%).
Figure 1:
A) Annual reported number of simulated pediatric trauma resuscitations by trauma center for calendar year 2016, and B) Reported duration of use of simulation-based training for trauma resuscitation within TQIP Pediatric centers. *15 and 27 centers did not respond to this question, respectively.
3.3. Training Program Characteristics
Among centers that reported using SBT, the most frequently reported time allocated to a training session was 41–60 minutes, with 11–20 minutes set aside for debriefing (Table 2). Debriefing occurred after all or most scenarios in 85% of centers. Implementation of training was variable, with 43% of programs using a simulation lab and 52% of programs using in situ simulation in the emergency department or trauma bay. Only 22% of all programs reported using unannounced in situ simulation. The use of mostly multidisciplinary training was reported in 80% of centers. The most commonly used scenarios represented a child with blunt trauma with pneumothorax, traumatic brain injury, and facial trauma requiring a surgical airway (Table 3).
Table 2:
Simulation program training characteristics.
| Amount of Time Planned for a Simulation with Debriefing | N (%) |
|---|---|
| < 20 minutes | 1 (2%) |
| 21–40 minutes | 9 (20%) |
| 41–60 minutes | 21 (46%) |
| 61–90 minutes | 7 (15%) |
| > 90 minutes | 8 (17%) |
| Location Where Simulation-Based Training Usually Occurs | |
| Always in the Simulation Center | 8 (17%) |
| Usually in the Simulation Center | 12 (26%) |
| Equally in the Simulation Center and in the ED/Trauma Bay | 2 (4%) |
| Usually in the ED/Trauma Bay | 10 (22%) |
| Always in the ED/Trauma Bay | 14 (30%) |
| Scheduling of Providers to Participate in Simulation-Based Training | |
| Always Pre-Announced | 26 (56%) |
| Usually Pre-Announced | 10 (22%) |
| Equally Pre-Announce and Unannounced | 0 (0%) |
| Usually Unannounced | 5 (11%) |
| Always Unannounced | 5 (11%) |
| Providers Participating in Simulation-Based Training | |
| Always Discipline-Specific | 1 (2%) |
| Usually Discipline-Specific | 5 (11%) |
| Equally Discipline-Specific and Multidisciplinary | 3 (7%) |
| Usually Multidisciplinary | 11 (24%) |
| Always Multidisciplinary | 26 (56%) |
| Do you use Structured Debriefing? | |
| Never | 1 (2%) |
| Rarely | 1 (2%) |
| Sometimes | 5 (11%) |
| After Most Scenarios | 6 (13%) |
| Always | 33 (72%) |
| How Much Time do you Spend Debriefing? | |
| < 10 minutes | 10 (22%) |
| 11–20 minutes | 28 (61%) |
| 21–40 minutes | 7 (15%) |
| 41–60 minutes | 1 (2%) |
Table 3:
Reported frequency of case scenario use within simulation centers.
| Simulated Scenario | N (%) |
| •Blunt Trauma with Pneumothorax | 39 (85%) |
| •Traumatic Brain Injury | 35 (76%) |
| •Facial Trauma Requiring Surgical Airway | 26 (57%) |
| •Blunt Abdominal Trauma with Shock | 10 (22%) |
| Penetrating Trauma with Shock | 4 (9%) |
| Pelvic Fracture with Massive Transfusion | 4 (9%) |
| Cardiac Tamponade or Cardiac Injury | 3 (7%) |
| Cases “Identified by PI Process“ | 3 (7%) |
| Pregnancy | 2 (4%) |
| Disaster or Multiple Casualty Scenario | 2 (4%) |
| Burn | 2 (4%) |
| Spine Trauma | 1 (2%) |
*Scenarios are not mutually exclusive, †Specifically queried on survey.
3.4. Perception of Optimal Use and Implementation Barriers
The frequency of SBT use was perceived to be appropriate by 43% of respondents, while 54% perceived that more SBT is needed. Centers perceiving appropriate frequency of use reported more annual simulated resuscitations than centers that perceived inadequate use (median 9 vs. 4 annual trauma simulations, p<0.05). Among centers not using SBT, 89% of respondents indicated that SBT would be beneficial for their centers, and 67% are planning on implementing SBT in the coming year.
Common implementation barriers were seen in centers using and not using SBT. Funding for faculty or staff time to participate in the sessions and funding to run the sessions were commonly rated barriers in both groups. Funding to purchase simulators ranked as the greatest barrier among centers not using SBT (Table 4). The lack of technical expertise to run simulation was reported as a greater barrier in centers not using SBT (4th vs 8th, p=0.01). The perceived lack of data to support SBT use was also a stronger barrier in centers not using SBT but was not rated as a strong barrier in either group (7th rank versus 10th rank). Seven of the ten rated barriers were negatively associated with number of annual simulations in 2016. (Table 4).
Table 4:
Perceived barriers to implementation within centers using and not using simulation-based training for trauma resuscitation.
| Centers that do NOT Use Simulation (N=20) | Centers that Use Simulation (N=63) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not a Barrier | Minor Barrier | Major Barrier | Makes Simulation Impossible | Weighted Ordinal Rank | Not a Barrier | Minor Barrier | Major Barrier | Makes Simulation Impossible | Weighted Ordinal Rank | 1p-value | 2Association with Sim Use, r | |
| Funding to Buy Simulators | 12 (60%) | 2 (10%) | 3 (15%) | 3 (15%) | 1 | 48 (76%) | 5 (8%) | 9 (14%) | 1 (2%) | 4 | 0.11 | −0.36 |
| Funding for Faculty/Staff Time to Participate | 13 (65%) | 0 (0%) | 5 (25%) | 2 (10%) | 2 | 43 (68%) | 5 (8%) | 13 (21%) | 2 (3%) | 1 | 0.55 | −0.34 |
| Funding to Run Sessions | 11 (55%) | 3 (15%) | 5 (25%) | 1 (5%) | 2 | 39 (62%) | 15 (24%) | 8 (13%) | 1 (2%) | 2 | 0.35 | −0.36 |
| Technical Expertise to Run Simulations | 11 (55%) | 4 (20%) | 5 (25%) | 0 (0%) | 4 | 55 (87%) | 6 (10%) | 2 (3%) | 0 (0%) | 8 | 0.01 | −0.27 |
| Physician Buy-In | 12 (60%) | 5 (25%) | 3 (15%) | 0 (0%) | 5 | 43 (68%) | 7 (11%) | 13 (21%) | 0 (0%) | 3 | 0.70 | NS |
| Leadership | 14 (70%) | 3 (15%) | 3 (15%) | 0 (0%) | 6 | 45 (62%) | 12 (19%) | 6 (10%) | 0 (0%) | 5 | 0.81 | −0.27 |
| Data to Support Simulation Use | 14 (70%) | 4 (20%) | 2 (10%) | 0 (0%) | 7 | 56 (89%) | 7 (11%) | 0 (0%) | 0 (0%) | 10 | 0.03 | −0.24 |
| Nursing Buy-In | 15 (75%) | 3 (15%) | 2 (10%) | 0 (0%) | 8 | 50 (79%) | 11 (18%) | 2 (3%) | 0 (0%) | 7 | 0.60 | −0.24 |
| Lack of Scenarios to Run | 16 (80 %) | 2 (10%) | 2 (10%) | 0 (0%) | 9 | 55 (87%) | 7 (11%) | 1 (1%) | 0 (0%) | 9 | 0.36 | NS |
| Ancillary Staff Buy-In | 16 (80%) | 3 (15%) | 1 (5 %) | 0 (0%) | 10 | 47 (75%) | 12 (19%) | 3 (5%) | 1 (2%) | 6 | 0.62 | NS |
Mann-Whitney U comparing median ordinal barrier scores for each barrier category between centers using and not using simulation-based training for trauma resuscitation.
Spearman’s Rho comparing barrier score for each scale within each center to number of pediatric simulations implemented in 2016 (all significant correlations have p<0.05).
4. Discussion
This cross-sectional survey of 125 ACS TQIP Pediatric trauma centers found that 78% of respondents use SBT and that these centers were more likely to be university-based and not-for-profit. Mean annual pediatric trauma volume was not associated with SBT use or with survey response. Simulation non-users were more likely to cite lack of technical expertise and lack of data supporting SBT use as barriers to SBT implementation. Funding for SBT-related costs were the most commonly cited barriers to SBT implementation in users and non-users. Seven of the ten queried barriers had significant negative associations with number of annual pediatric simulations in 2016. While SBT usage has increased overall, perceived barriers related to lack of funding, technical expertise, and data to support SBT use may be limitations to more widespread implementation and usage.
Our findings suggest that the use of SBT for pediatric trauma is increasing, but widespread use is limited primarily by funding concerns. Centers that reported SBT usage were more likely to be university-based and not-for-profit. Perceived barriers (the top three of which were related to funding) were inversely proportional to the number of annual pediatric simulations. Most centers not using SBT indicated that it would be beneficial. These findings suggest that funding is the main concern for centers related to the use or expansion of SBT.
University-based programs or non-profit institutions may have easier access to SBT-related funding or may have greater acceptance of unfunded academic activities. To achieve greater use of SBT, centers may need to devise strategies that include sharing resources and/or finding lower cost approaches for implementing and conducting SBT.
Severely injured pediatric trauma patients are relatively rare in most emergency departments. As a result, experience with the acute resuscitation of these patients is often limited,9, 20 making SBT a potentially useful tool in the development and maintenance of highstakes skills for this population. Multidisciplinary SBT has been associated with improved trauma team performance in adult and pediatric settings.14, 15, 17, 19, 21, 22 Simulation has also been associated with improvements in non-technical skills such as communication, fund of knowledge, and provider confidence.21, 23, 24 In one pediatric emergency department, SBT was associated with improved patient safety.25 Despite growing evidence supporting the efficacy of SBT, 30% of non-users reported lack of evidence to support SBT as a barrier to implementation. This may be related to the lack of investigation of the impact of SBT on patient-level clinical outcomes for trauma patients. All of the previously mentioned studies measured improvements in provider and team performance but have not assessed an impact on patients. Higher quality studies supporting the association between SBT and improved clinical outcomes may increase its national uptake and help overcome funding barriers.
This study has several limitations. The primary limitation is potential survey response bias. Despite attempts to recruit non-respondents, we only achieved a 75% response rate. We would expect non-respondents to be more likely to not use SBT, leading to an overestimation of SBT use nationally. We compared center characteristics between non-respondents and respondents, finding that non-respondents were less likely to have ACS or state pediatric trauma verification and less likely to have a pediatric ICU – both markers of local institutional resources. Response bias may have also led to type II error in analyzing barriers to implementation. The second limitation of this study is potential social desirability bias – a type of response bias in which survey respondents are more likely to give favorable answers. If this bias were present, it may have contributed to overestimation of SBT use, but may have been evaluated by the inclusion of barriers to implementation questions in the survey instrument. Furthermore, social desirability bias may have possibly suppressed the endorsement of “lack of evidence”, particularly for systems in which evidence is more important than profit. The final limitation is the lack of uniformity of SBT methodology and the human resource and time cost of differing training methods. While some centers may have considered annual disaster exercises or ATLS training to be SBT, other centers use in situ, unannounced multidisciplinary training. Program managers at an institution that use low-cost, in situ SBT may have different views on barriers to implementation when compared to those using a high-fidelity simulation center with dedicated simulation personnel. This lack of SBT uniformity may have been an additional source of type II error in comparing implementation barriers.
In conclusion, this study provides a view of the current state of SBT for pediatric trauma resuscitation at ACS TQIP Pediatric centers. Simulation use increased from 2014 to 2016, but barriers to widespread adoption still exist. Funding for SBT is a top concern for all centers, particularly those not using SBT. Innovations targeted at reducing cost and sharing resources may help increase SBT use. Translational studies to assess return-on-investment for SBT on clinical outcomes may justify the cost.
Acknowledgments
This work was supported by grant #KFVS6290 from the National Institute for Child Health and Development (NICHD) and grant #KL2TR001854 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Poster presentations at the Annual Meeting of the Pediatric Trauma Society, Charleston, SC (November 2017) and the Trauma Quality Improvement Program Annual Scientific Meeting, Chicago, IL (November 2017) Children’s Hospital Los Angeles Institutional Review Board Exemption # CHLA-16-00341.
References
- 1.Borse N, Sleet DA. CDC Childhood Injury Report: Patterns of Unintentional Injuries Among 0- to 19-Year Olds in the United States, 2000–2006. Fam Community Health. 2009;32:189. [DOI] [PubMed] [Google Scholar]
- 2.Borse NN, Gilchrist J, Dellinger AM, et al. Unintentional childhood injuries in the United States: key findings from the CDC childhood injury report. J Saf Res. 2009;40:71–74. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention and Control, CDC using WISQARS. https://www.cdc.gov/injury/wisqars/LeadingCauses.html; 2017. Accessed 17 May 2017.
- 4.McLaughlin C, Zagory JA, Fenlon M, et al. Timing of Mortality in Pediatric Trauma Patients: A National Trauma Databank Analysis. J Pediatr Surg. In press 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gunst M, Ghaemmaghami V, Gruszecki A, et al. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc. 2010;23:349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demetriades D, Kimbrell B, Salim A, et al. Trauma Deaths in a Mature Urban Trauma System: Is “Trimodal” Distribution a Valid Concept? J Am Coll Surg. 2005;201:343–348. [DOI] [PubMed] [Google Scholar]
- 7.Valdez C, Sarani B, Young H, et al. Timing of death after traumatic injury—a contemporary assessment of the temporal distribution of death. J Surg Res. 2016;200:604–609. [DOI] [PubMed] [Google Scholar]
- 8.Green SM, Ruben J. Emergency Department Children Are Not as Sick as Adults: Implications for Critical Care Skills Retention in an Exclusively Pediatric Emergency Medicine Practice. J Emerg Med. 2009;37:359–368. [DOI] [PubMed] [Google Scholar]
- 9.Mittiga MR, Geis GL, Kerrey BT, Rinderknecht AS. The spectrum and frequency of critical procedures performed in a pediatric emergency department: implications of a provider-level view. Ann Emerg Med. 2013;61:263–270. [DOI] [PubMed] [Google Scholar]
- 10.Falcone RA, Haas L, King E, et al. A multicenter prospective analysis of pediatric trauma activation criteria routinely used in addition to the six criteria of the American College of Surgeons. J Trauma Acute Care Surg. 2012;73:377–384; discussion 384. [DOI] [PubMed] [Google Scholar]
- 11.Williams D, Foglia R, Megison S, et al. Trauma activation: are we making the right call? A 3-year experience at a Level I pediatric trauma center. J Pediatr Surg. 2011;46:1985–1991. [DOI] [PubMed] [Google Scholar]
- 12.Ivatury RR, Guilford K, Malhotra AK, et al. Patient safety in trauma: maximal impact management errors at a level I trauma center. J Trauma. 2008;64:265–270; discussion 270–272. [DOI] [PubMed] [Google Scholar]
- 13.Pucher PH, Aggarwal R, Twaij A, et al. Identifying and addressing preventable process errors in trauma care. World J Surg. 2013;37:752–758. [DOI] [PubMed] [Google Scholar]
- 14.Capella J, Smith S, Philp A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ. 2010;67:439–443. [DOI] [PubMed] [Google Scholar]
- 15.Steinemann S, Berg B, Skinner A, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. 2011;68:472–477. [DOI] [PubMed] [Google Scholar]
- 16.Knudson MM, Khaw L, Bullard MK, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma. 2008;64:255–263. [DOI] [PubMed] [Google Scholar]
- 17.Holcomb JB, Dumire RD, Crommett JW, et al. Evaluation of trauma team performance using an advanced human patient simulator for resuscitation training. J Trauma. 2002;52:1078–1085. [DOI] [PubMed] [Google Scholar]
- 18.Couto TB, Kerrey BT, Taylor RG, et al. Teamwork skills in actual, in situ, and in-center pediatric emergencies: performance levels across settings and perceptions of comparative educational impact. Simul Healthc. 2015;10:76–84. [DOI] [PubMed] [Google Scholar]
- 19.Falcone RA Jr, Daugherty M, Schweer L, et al. Multidisciplinary pediatric trauma team training using high-fidelity trauma simulation. J Pediatr Surg. 2008;43:1065–1071. [DOI] [PubMed] [Google Scholar]
- 20.Chen EH, Cho CS, Shofer FS, et al. Resident exposure to critical patients in a pediatric emergency department. Pediatr Emerg Care. 2007;23:774–778. [DOI] [PubMed] [Google Scholar]
- 21.Steinemann S, Berg B, DiTullio A, et al. Assessing teamwork in the trauma bay: introduction of a modified “NOTECHS” scale for trauma. Am J Surg. 2012;203:69–75. [DOI] [PubMed] [Google Scholar]
- 22.Auerbach M, Roney L, Aysseh A, et al. In situ pediatric trauma simulation: assessing the impact and feasibility of an interdisciplinary pediatric in situ trauma care quality improvement simulation program. Pediatr Emerg Care. 2014;30:884–891. [DOI] [PubMed] [Google Scholar]
- 23.Popp J, Yochum L, Spinella PC, et al. Simulation training for surgical residents in pediatric trauma scenarios. Conn Med. 2012;76:159–162. [PubMed] [Google Scholar]
- 24.Miller D, Crandall C, Washington C, McLaughlin S. Improving teamwork and communication in trauma care through in situ simulations. Acad Emerg Med. 2012;19:608–612. [DOI] [PubMed] [Google Scholar]
- 25.Patterson MD, Geis GL, LeMaster T, Wears RL. Impact of multidisciplinary simulation-based training on patient safety in a paediatric emergency department. BMJ Qual Saf. 2013;22:383–393. [DOI] [PubMed] [Google Scholar]