Abstract
Background: Sarcoidosis is a multi-system granulomatous disease in which T-helper type 1 cytokines play a key role. We evaluated the clinical value of serum soluble interleukin-2 receptor (sIL-2R) as a marker of disease activity and prognosis in sarcoidosis. Methods: This study included 67 patients who were newly diagnosed with sarcoidosis from 2006 to 2012 at our department. The clinical and follow-up data were retrospectively collected from their medical records. Results: The mean (±SD) age of the patients was 53.9±15.4 years; 41 patients were women and were significantly older than men. Serum angiotensin-converting enzyme had a mean value of 15.3±6.1 U/L and a positive rate of 10.4%. Serum sIL-2R had mean level of 818.8±453.1 U/mL and a positive rate of 45.9%. Moreover, the sIL-2R level of patients who had lung parenchymal lesions was significantly higher than that of patients who had no lung parenchymal lesions. Fifty-two patients who had no medications were followed up at our hospital for a median period of 37 months (range, 0–107 months). Patients who demonstrated chest imaging evidence of exacerbation (n = 8) tended to have higher sIL-2R levels than those who remained stable. Conclusion: Serum sIL-2R may have a role as a diagnostic and prognostic marker in pulmonary sarcoidosis. (Sarcoidosis Vasc Diffuse Lung Dis 2017; 34: 41-47)
Keywords: sarcoidosis, serum IL-2 receptor, lung, ACE
1. Introduction
Sarcoidosis is a granulomatous disease of unknown etiology that most commonly affects the lungs. The findings that indicate a systemic reaction from sarcoidosis include bilateral hilar lymphadenopathy (BHL), hypercalcemia, increased serum angiotensin-converting enzyme (ACE) (>20 U/mL), negative purified protein derivative test, abnormally high uptake of gallium-67 citrate on scintigraphy, elevated lymphocyte count, and/or elevated CD4/CD8 ratio in bronchoalveolar lavage fluid (BALF).
Soluble interleukin-2 receptor (sIL-2R), which was reported to reflect a Th1-type reaction, and other serum markers, such as KL-6 and anti-vascular endothelial cell antibody-related (ACEA), have been studied as new markers for sarcoidosis (1–5). However, to the best of our knowledge, no serum marker has been reported to be clinically useful in evaluating sarcoidosis activity. Although serum ACE level has been widely measured in practical medicine, it may not be associated with disease activity, partly because of varying influence of gene polymorphisms (6). On the other hand, sIL-2R is secreted from activated T cells and is known to reflect a Th1-type reaction. In some patients with sarcoidosis, a prolonged Th1 reaction suggests disease progression. In this study, we investigated the relationship between sIL-2R level and clinical characteristics of sarcoidosis in Japanese patients.
2. Patients and Methods
2.1 Study design and patients
Among all patients who were admitted at Kyushu University Hospital between January 1, 2006 and December 31, 2012, we studied 67 patients who were newly diagnosed with sarcoidosis, based on the statement of the American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) in 1999 (5). 52 patients of these, we also studied about clinical course up to 3 years, with an average of 1 month. We divided the 52 patients into the exacerbation group and the stable group and compared the clinical parameters. The clinical data of the study population were investigated retrospectively.
Instead of informed consent, we showed about this study on our web page. This study was reviewed and approved (No. 25–36, May 14, 2013) by the institutional review board of Kyushu University.
2.2 Measurements
The electronic medical records of patients were reviewed for demographic data, such as age, gender, smoking history; disease-related symptoms; blood tests; BALF findings; and chest computed tomography (CT) scan findings. We defined an abnormally high BALF analysis as the presence of ≥ 10% lymphocytes and a CD4/CD8 lymphocytes ratio of ≥ 3.5. The blood levels of white blood cell (WBC), C-reactive protein (CRP), lactate dehydrogenase (LDH), KL-6, ACE, corrected calcium (Ca), IgG, and sIL-2R were examined. At our hospital, the normal values were WBC 3500–9000 U/L, CRP <0.1 mg/dL, LDH 119–229 U/L, KL-6 <430 U/L, ACE 6–22 U/L, Ca 8.7–10.3 mg/dL, IgG 872–1815 mg/dL, and sIL-2R <206 U/mL. In this study, positive was defined as values that exceeded these normal values.
The clinical staging of sarcoidosis using the chest X-ray is defined as stage 0, with extrapulmonary lesion alone; stage I, with BHL alone; stage II, with BHL plus lung parenchymal lesion; stage III, with lung parenchymal lesion alone; and stage IV, with pulmonary fibrosis.
2.3 Statistical analysis
Data were expressed as mean±SD (standard deviation). Student’s t-test was used to evaluate the differences in each parameter. Linear regression analysis was used to evaluate the correlation in each parameter. A P value of less than 0.05 was considered to be statistically significant. Statistical analysis was conducted using JMP Pro 11 software (SAS institute Japan Ltd, Tokyo, Japan).
3. Results
3.1 Characteristics of the study population (Table 1)
Table 1.
Patient’s background
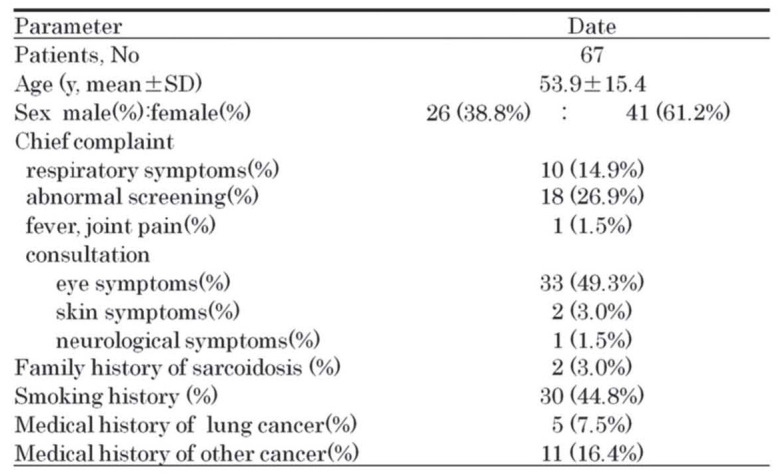
The study population consisted of 26 men and 41 women, with the mean (±SD) age of the patients was 53.9±15.4 years. The most frequent symptom was visual disturbance (49.3%); 18 patients (26.9%) had abnormal imaging studies without any symptoms. The demographic data of our present population were similar to those that were previously reported in Japan (6,7).
3.2 Results of laboratory tests (Table 2)
Table 2.
Laboratory test on hospitalization
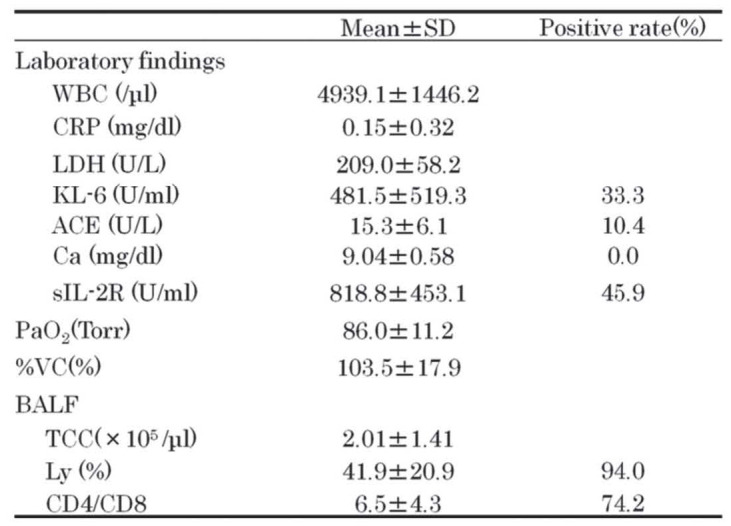
In serum chemistry, 10.4% were positive for ACE and 45.9% were positive for sIL-2R. In BALF analysis, 56 patients (94%) showed lymphocytic predominance and 44 patients (74.2%) showed increased CD4/CD8 ratio. By linear regression analysis, there was a weak correlation between ACE and sIL-2R (R2 = 0.36, p < 0.0001).
3.3 Clinical features and results of imaging studies (Table 3)
Table 3.
Clinical features of sarcoidosis
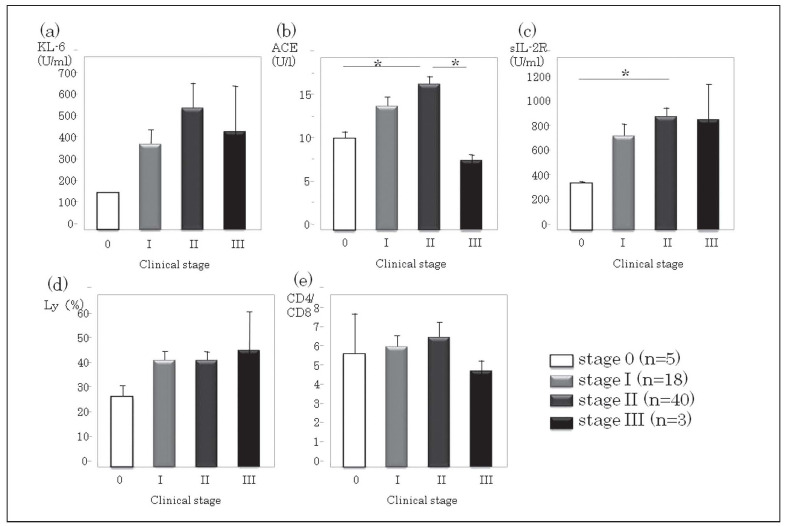
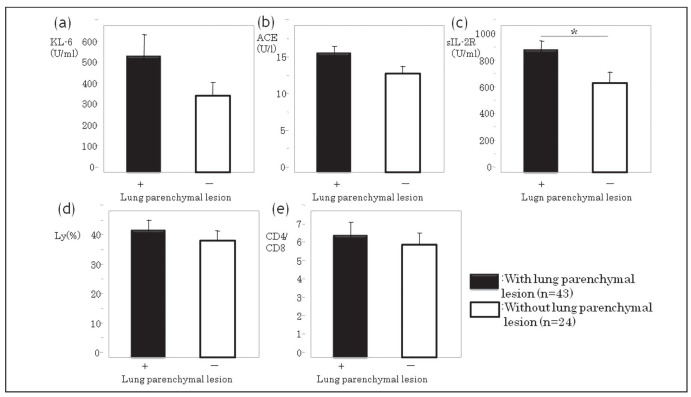
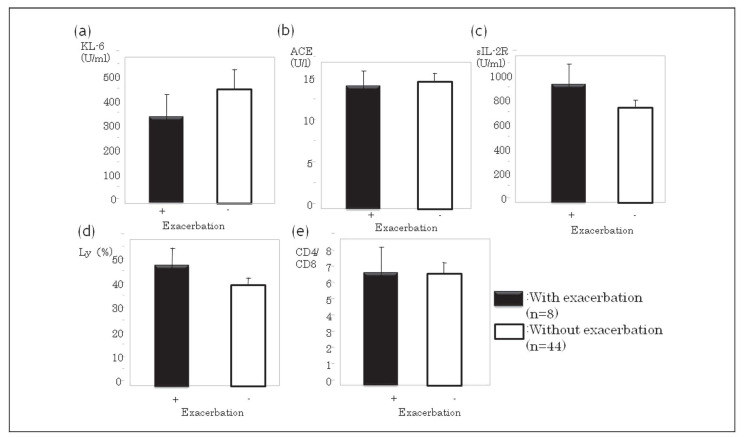
Sarcoidosis patients were categorized into five clinical stages, based on the findings on chest X-ray: stage 0, with extrapulmonary lesion alone (n = 5); stage I, with BHL alone (n = 18); stage II, with BHL plus lung parenchymal lesion (n = 40); stage III, with lung parenchymal lesion alone (n = 3); and stage IV, with pulmonary fibrosis (n = 0). The comparison of various parameters according to stage is shown in Fig. 1. The serum sIL-2R level in patients with lung parenchymal lesions (stage II+III) was significantly higher than those without lung parenchymal lesions (stage 0+I) (stage II+III vs. stage 0+I, respectivery; p = 0.044) (Fig. 2.). However, there were no significant differences between stage 0+I and stage II+III in terms of the other parameters.
Fig. 1.
Comparison of sarcoidosis patients by clinical stage. The values of a) KL-6, b) ACE, c) sIL-2R, d) lymphocyte ratio in BALF, and e) CD4/CD8 ratio in BALF are compared. ACE, angiotensin-converting enzyme; sIL-2R, soluble interleukin-2 receptor; BALF, bronchoalveolar lavage fluid. *p < 0.05 [Student’s t-test]
Fig. 2.
Comparison of sarcoidosis patients with and without lung parenchymal lesions. The values of a) KL-6, b) ACE, c) sIL-2R, d) lymphocyte ratio in BALF, and e) CD4/CD8 ratio in BALF are compared. ACE, angiotensin-converting enzyme; sIL-2R, soluble interleukin-2 receptor; BALF, bronchoalveolar lavage fluid. *p < 0.05 [Student’s t-test]
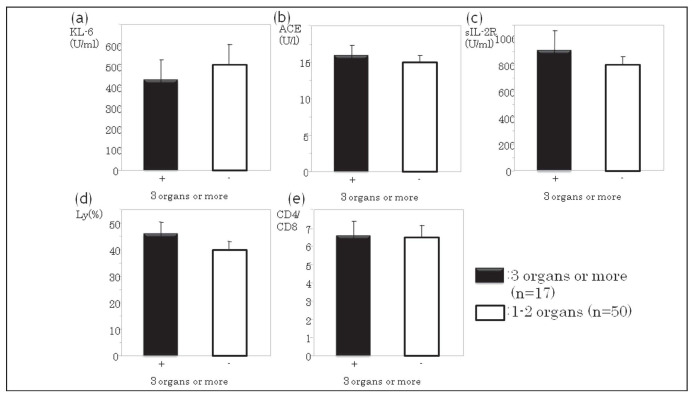
There was no significant difference between patients with involvement of ≥ 3 organs/lesions and patients with involvement of 1–2 organs/lesions (Fig. 3). The serum levels of sIL-2R tended to be positive in the group of patients with extrapulmonary lesions (p = 0.1565) and in the group that had ≥ 3 organs/lesions involved (p = 0.4348), but these were not significant.
Fig. 3.
Comparison of sarcoidosis patients according to the number of organs involved. The values of a) KL-6, b) ACE, c) sIL-2R, d) lymphocyte ratio in BALF, and e) CD4/CD8 ratio in BALF are compared. ACE, angiotensin-converting enzyme; sIL-2R, soluble interleukin-2 receptor; BALF, bronchoalveolar lavage fluid. *p < 0.05 [Student’s t-test]
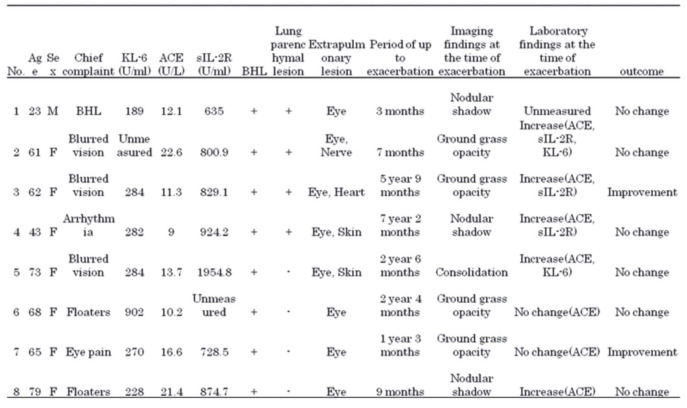
3.4 Clinical course of lung parenchymal lesion
Of the 67 patients, 52 were observed by chest radiograph without any treatment. Follow-up period was up to 3 years, with an average of 1 month. Of the 52 patients, 8 (15.4%) showed exacerbation of lung parencymal lesion on chest radiograph (Table 4). The average period until exacerbation was 1 year and 9 months (range, 3–86 months). Chest X-ray and Chest CT scan showed ground glass opacity in 4 patients, granular shadow in 4 patients, and consolidation in one patient.
Table 4.
Examination of each case of lung parenchimal exacerbation group
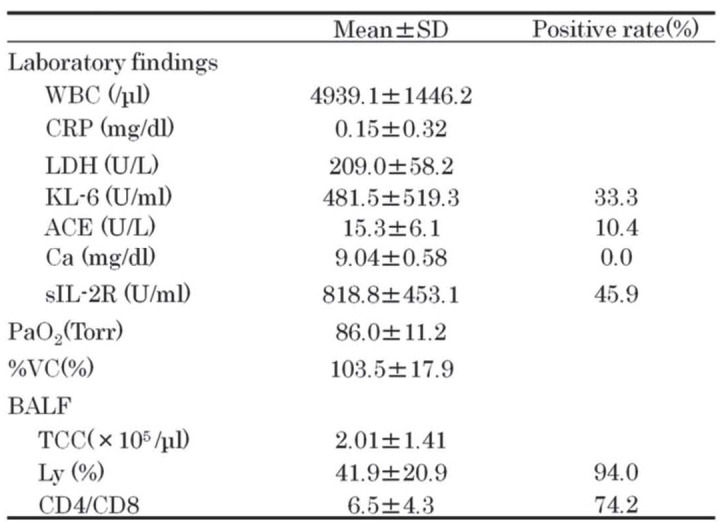
We divided the 52 patients into the exacerbation group of lung parenchymal lesion (n = 8) and the stable group (n = 44) and compared the clinical parameters. Compared with the stable group, the exacerbation group of lung parenchymal lesion had a non-significant tendency to have positive sIL-2R level (p = 0.2495) and CD4/CD8 ratio (p = 0.2733) (Fig. 4). Cutoff levels of sIL-2R, ACE, KL-6, LDH and %VC between two groups were 728.5 U/ml, 13.7 U/L, 284.0 U/ml, 220.0 U/L and 87.0%.
Fig. 4.
Comparison of sarcoidosis patients with and without exacerbation. The values of a) KL-6, b) ACE, c) sIL-2R, d) lymphocyte ratio in BALF, and e) CD4/CD8 ratio in BALF are compared. ACE, angiotensin-converting enzyme; sIL-2R, soluble interleukin-2 receptor; BALF, bronchoalveolar lavage fluid. *p < 0.05 [Student’s t-test]
4. Discussion
Although serum ACE and Ca levels are widely used to diagnose sarcoidosis, these tests have relatively low sensitivity. Serum ACE level has been reported to be affected by genetic polymorphisms; group D/D had high levels, whereas group I/I had low levels (2,10). The rate for positive serum Ca was also previously reported to be low (9). Therefore, there is a need for a new serum marker to diagnose and evaluate the disease activity of sarcoidosis. The candidates for this purpose have included sIL-2R, KL-6, and vascular endothelial cell antibodies (11). Among these, we focused on sIL-2R and evaluated its clinical usefulness in a retrospective analysis.
The pathogenesis of sarcoidosis is suggested to be a Th1 cell-mediated immunological response to an unknown antigen that results to IL-2 and IFNγ secretion. Therefore, sIL-2R may be a reasonable marker to evaluate such an immunological reaction (12). In fact, our results showed that the positive rate of sIL-2R in sarcoidosis patients was as high as 45.9%. However, sIL-2R was also reported to be high in lung cancer, adult T-cell leukemia, and malignant lymphoma (13,15). Since hilar or mediastinal lymph nodes are frequently involved, we need to rule out these malignant diseases in order to diagnose sarcoidosis correctly. A combination of sIL-2R and other tumor markers may improve the accuracy of diagnosis.
In this study, sIL-2R was significantly increased in the group with lung parenchymal lesions on chest X-ray staging; therefore, it may be useful for the diagnosis of clinical stage II or III sarcoidosis. It is important to note that sIL-2R may not reflect the total extent of granuloma in sarcoidosis because serum levels were the same regardless of the number of involved organs or sites.
Second, we examined sIL-2R as a prognostic factor for sarcoidosis, as reported previously (15,16). In this study, sIL-2R level tended to be higher in the exacerbation group of lung parenchymal lesion than the stable group; however, this was not statistically significant, probably due to the small number of patients. The cutoff levels with two groups were slightly lower than those of reported by Miyoshi S, et al (2).
The limitation is that there was a difference in date extraction point and the check contents and the follow up point was not unified because of retrospective study. So, we need to prospective study that investigates the role of sIL-2R on sarcoidosis.
5. Conclusion
In this study, we examined the role of sIL-2R as a parameter for disease activity in sarcoidosis and found that it may be a promising marker for diagnosis, as well as for prediction of lung parenchymal involvement and exacerbations.
References
- 1.Ziegenhagen MW, Rothe ME, Schlaak M, et al. Bronchoalveolar and serological parameters reflecting the severity of sarcoidosis. Eur Respir J. 2003;21(3):407–13. doi: 10.1183/09031936.03.00010403. [DOI] [PubMed] [Google Scholar]
- 2.Miyoshi S, Hamada H, Kadowaki T, et al. Comparative evaluation of serum markers in pulmonary sarcoidosis. Chest. 2010;137:1391–7. doi: 10.1378/chest.09-1975. [DOI] [PubMed] [Google Scholar]
- 3.Inui N, Matsui T, Suda T, et al. Anti-endothelial cell antibodies in patients with sarcoidosis. Chest. 2008;133:955–60. doi: 10.1378/chest.07-0850. [DOI] [PubMed] [Google Scholar]
- 4.Ina Y, Takada K, Sato T, Yamamoto M, Noda M, Morishita M. Soluble interleukin 2 receptors in patients with sarcoidosis. Possible origin. Chest. 1992;102(4):1128–33. doi: 10.1378/chest.102.4.1128. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence EC, Brousseau KP, Berger MB, Kurman CC, Marcon L, Nelson DL. Elevated concentrations of soluble interleukin-2 receptors in serum samples and bronchoalveolar lavage fluids in active sarcoidosis. Am Rev Respir Dis. 1988;137(4):759–64. doi: 10.1164/ajrccm/137.4.759. [DOI] [PubMed] [Google Scholar]
- 6.Tahir M, Sharma SK, Ashraf S, et al. Angiotensin converting enzyme genotype affects development and course of sarcoidosis in Asian Indians. Sarcoidosis Vasc Diffuse Lung Dis. 2007;24:106–12. [PubMed] [Google Scholar]
- 7.Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999;160:736–55. doi: 10.1164/ajrccm.160.2.ats4-99. [DOI] [PubMed] [Google Scholar]
- 8.Sawahata M, Suguyama Y, Nakamura Y, et al. Age-related and historical change in the clinical characteristics of sarcoidosis in Japan Respiratory Medicine. 2015;109:272–8. doi: 10.1016/j.rmed.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Morimoto T, Azuma A, Abe S, et al. Epidemiology of sarcoidosis in Japan. Eur Respir J. 2008;31:372–9. doi: 10.1183/09031936.00075307. [DOI] [PubMed] [Google Scholar]
- 10.Biller H, Zissel G, Ruprecht B, et al. Genotype-corrected reference values for serum angiotensin-converting enzyme. Eur Respir J. 2006;28:1085–90. doi: 10.1183/09031936.00050106. [DOI] [PubMed] [Google Scholar]
- 11.Handa T, Nagai S. Blood markers for the assessment of disease activity and diagnosis in patients with sarcoidosis. Jpn J Sarcoidosis and Granulomatous Disorders [in Japanese] 2010;30:99–101. [Google Scholar]
- 12.Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA. 2011;305:391–9. doi: 10.1001/jama.2011.10. [DOI] [PubMed] [Google Scholar]
- 13.A Tada, S Kawahara, T Sato, et al. Serum Soluble Interleukin-2 Receptor in patients with Lung Cancer. JJLC. 2000;40:23–7. [Google Scholar]
- 14.T Kita, S Watanabe, F Yano, et al. Clinical significance of the serum IL-2R level and Ga-67 scan findings in making a differential diagnosis between sarcoidosis and non-Hodgkin’s lymphoma. Ann Nucl Med. 2007;21:499–503. doi: 10.1007/s12149-007-0060-9. [DOI] [PubMed] [Google Scholar]
- 15.Ziegenhagen MW, Benner UK, Zissel G, et al. Sarcoidosis: TNF-alpha release from alveolar macrophages and serum level of sIL-2R are prognostic markers. Am J Respir Crit Care Med. 1997;156:1586–92. doi: 10.1164/ajrccm.156.5.97-02050. [DOI] [PubMed] [Google Scholar]
- 16.Vorselaars AD, van Moorsel CH, Zanen P, et al. ACE and sIL-2R correlate with lung function improvement in sarcoidosis during methotrexate therapy. Respir Med. 2015;109:279–85. doi: 10.1016/j.rmed.2014.11.009. [DOI] [PubMed] [Google Scholar]