Abstract
Placental transmogrification of the lung is an extremely rare lung disease frequently associated with hamartomas or unilateral bullous emphysema. We report a case of placental transmogrification of the lung in a 44-year-old male who presented with bronchial infections, hyperlucent left lung and progressive cystic and micronodular unilateral interstitial lung disease. Because of interstitial lung disease progression over 13 years, a left pneumonectomy was performed. After a two-year follow-up, the patient was asymptomatic and did not exhibit any lung infections. No recurrence was observed on the right lung. (Sarcoidosis Vasc Diffuse Lung Dis 2017; 34: 188-190)
Keywords: transmogrification, interstitial lung disease, emphysema, orphan disease
A 44-year-old male, former smoking estimated at 12 pack-years, presented with acute bronchitis. Chest computed tomography demonstrated hyperlucency and micronodular opacities of the left lung (Figure 1). Between 2001 and 2010 he presented several bronchial infections. In 2010 the physical examination was normal. Pulmonary function tests demonstrated moderate airway obstruction (FVC: 69% predicted, FEV1: 55% predicted) with lung distension (TLV: 127%). Chest computed tomography showed hyperlucency and vascular rarefaction of the left lung, confluent micro- and macronodules in the left lower lobe and parenchymal infiltration associated with consolidation in the lingula and cysts in the left basal segment (Figure 1). These abnormalities were increased compared to 2001. There was no contralateral abnormality. Bronchoscopy showed almost complete filling of the left B10 bronchus by a whitish lesion (Figure 2). Bronchial biopsies of the whitish lesion were not contributory. A positron emission tomography was normal. Surgical lung biopsy was performed due to deterioration of the parenchymal lesion and revealed destruction of the pulmonary parenchyma, including emphysematous lesions and alveolar distension related to bronchiolitis, replaced by placental transmogrification lesions (Figure 3). Quantitative ventilation-perfusion scan demonstrated markedly diminished perfusion (16%) and ventilation (10%) of the left lung. In the context of repeated bronchial infections and limited function of the left lung, left pneumonectomy was performed in 2014. In February 2016 the patient was asymptomatic and did not exhibit lung infections.
Fig. 1.
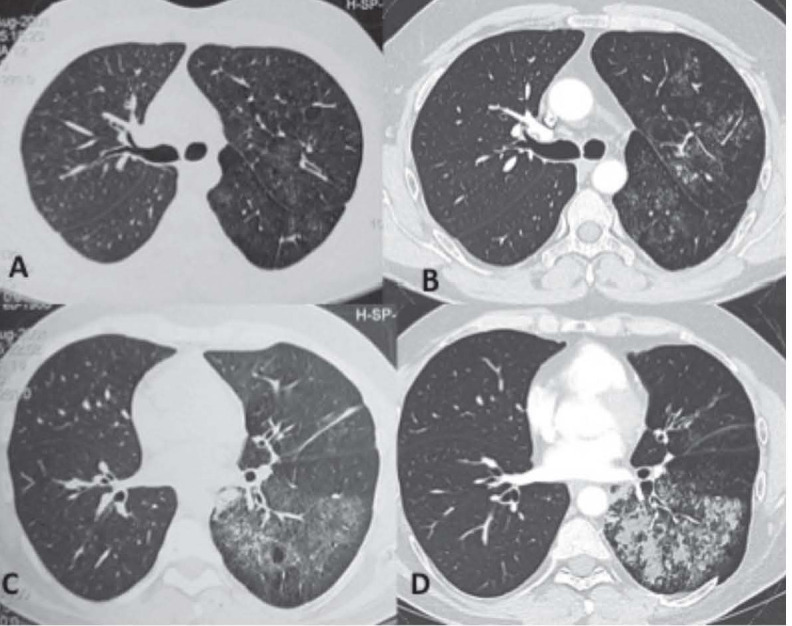
Chest computed tomography (two sections: carina and right inferior pulmonary vein) in 2001 (A and C) and 2014 (B and D): multiple cystic lesions of the left basal segment with a stable appearance, associated with active micronodular infiltration of the left upper and lower lobes, with more extensive involvement of the left lower lobe comprising consolidation and confluent lesions. A pseudo nodular zone of the apical segment of the left lower lobe is visible within this infiltration. Note the presence of an intercostal lung hernia through the thoracotomy scar; hyperlucency of the left lung with no loss of lung volume and no bronchial abnormalities
Fig. 2.
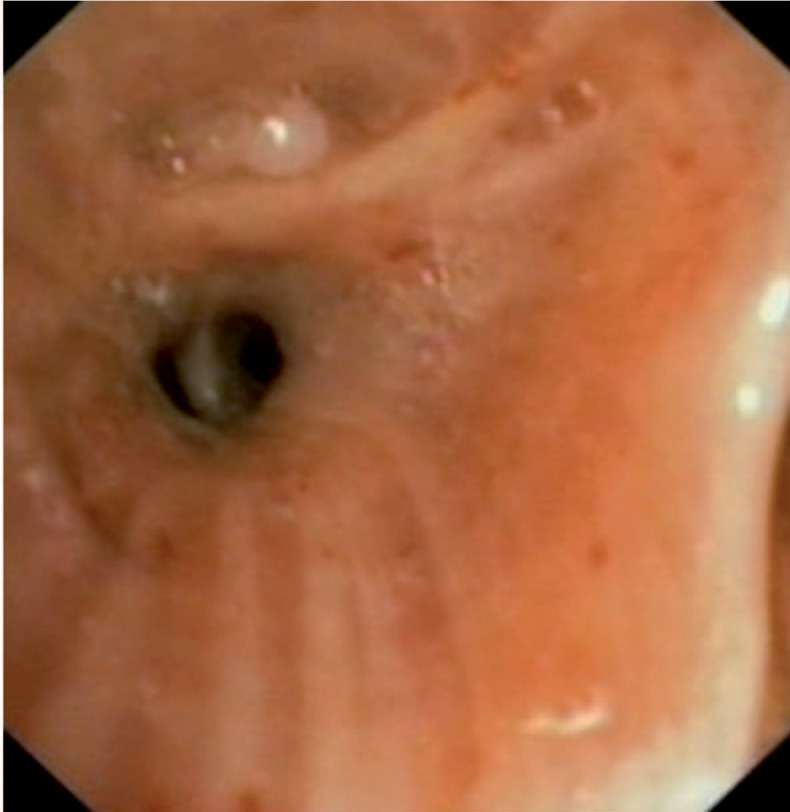
Bronchoscopy: presence of a whitish material in the left B10 bronchus with contact bleeding of the mucosa.
Fig. 3.
Left lower lobe lesion: Macroscopic examination of the fresh specimen (A): bullous parenchymal lesion with a spongiform, villous appearance. Microscopy (B): Multiple papillary structures resembling chorionic villi; presence of optically empty vacuoles, corresponding to adipose involution of alveolar walls.
Placental transmogrification of the lung is an extremely rare lung disease. The diagnosis is based on histological examination demonstrating replacement of pulmonary parenchyma by lesions resembling the microscopic features of the chorionic villi of the placenta (1). To our knowledge, this is the first case of placental transmogrification presenting as a progressive unilateral interstitial lung disease in a patient with a long follow-up. The first description of placental transmogrification of the lung was reported by McChesney in 1979 (1) and 39 cases are described in the literature to date. These cases essentially concerned men between the ages of 30 and 50 years with respiratory features in 2/3 of cases: dyspnoea, cough, chest pain, pneumothorax, and more rarely acute respiratory distress or haemoptysis. Six cases were described in a retrospective histological series of pulmonary hamartomas (2). Chest CT scan usually shows features of emphysema or cysts or sometimes nodules or masses (3), and more rarely consolidation associated with bullae (4). The lesions were unilateral in all of the published cases. When described, treatment is always surgery and consists of atypical resection, lobectomy or pneumonectomy. The natural history of placental transmogrification with or without surgery remains unknown, as only two cases, apart from the case reported here, have sufficient follow-up: one case with a follow-up of five years treated by bullectomy (5), and one case with a follow-up of two years treated by pneumonectomy (6). Surgical treatment was curative in both cases and no recurrence was observed during follow-up. In one case, an adenocarcinoma was discovered incidentally on histological examination (7), derived from the epithelial component of the cyst leading to the discovery of placental transmogrification.
In conclusion, we reported herein the first des-cription of placental transmogrification of the lung, a rare disease with unknown pathophysiology, presenting as unilateral interstitial lung disease associated with emphysematous lesions.
References
- 1.McChesney T. Placental transmogrification of the lung: a unique case with remarkable histopathologic features. Lab Invest. 1919;40:245–6. [Google Scholar]
- 2.Xu R, Murray M, Jagirdar J, et al. Placental transmogrification of the lung is a histologic pattern frequently associated with pulmonary fibrochondromatous hamartoma. Arch Pathol Lab Med. 2002;126:562–6. doi: 10.5858/2002-126-0562-PTOTLI. [DOI] [PubMed] [Google Scholar]
- 3.Hochhegger B, Camargo S, Camargo J, et al. Placental Transmogrification of the Lung. Lung. 2015;193:855–7. doi: 10.1007/s00408-015-9772-0. [DOI] [PubMed] [Google Scholar]
- 4.Mohning MP, Schwarz MI, McKinley SJ. Placental transmogrification of the lung: a rare cause of unilateral bullous disease. Am J Respir Crit Care Med. 2014;190:e1. doi: 10.1164/rccm.201307-1361IM. [DOI] [PubMed] [Google Scholar]
- 5.Cavazza A, Lantuejoul S, Sartori G, et al. Placental transmogrification of the lung: clinicopathologic, immunohistochemical and molecular study of two cases, with particular emphasis on the interstitial clear cells. Hum Pathol. 2004;35:517–21. doi: 10.1016/j.humpath.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro M, Vidal C, Lipskar AM, et al. Placental transmogrification of the lung presenting as emphysema and a lung mass. Ann Thorac Surg. 2009;87:615–6. doi: 10.1016/j.athoracsur.2008.05.076. [DOI] [PubMed] [Google Scholar]
- 7.Kronz JD, Palmer C, Askin FB. Images in pathology. Placental transmogrification of the lung. Arch Pathol Lab Med. 1999;123:856. doi: 10.5858/1999-123-0856-PTOTL. [DOI] [PubMed] [Google Scholar]



