ABSTRACT
Objectives: To evaluate the association of resting blood pressure with pain response and evaluate the cardiovascular effects of anterior-to-posterior [AP] versus lateral [LAT] techniques of cervical spine non-thrust manipulation [NTM].
Methods: Forty-three (23 females) participants with non-chronic neck pain (mean age 29.00 ± SD 9.09 years) randomly received AP or LAT NTM to the cervical spine. Blood pressure and heart rate were measured before, during, and after the intervention. Disability and pain were measured pre- and post-intervention.
Results: Resting systolic blood pressure (SBP) was significantly associated with average pain reduction two days later on univariate and multivariate analyses (coefficients −0.029 ± SD 0.013, p = 0.036; −0.026 ± 0.012, p = 0.032).
No significant differences existed between AP and LAT NTM groups in disability, pain reduction, and cardiovascular variables. The decrease in ‘worst neck pain’ rating 2-days post-intervention was clinically significant within the AP (mean −2.43 ± SD 2.66) group. Mixed-effect model ANOVA revealed a significant change in SBP over time (estimate −1.94 ± SD 0.70, p = 0.007).
Discussion: This spinal NTM study was the first to relate resting SBP with short-term pain reduction, demonstrating SBP-related hypoalgesia. In normotensive individuals with unilateral non-chronic neck pain, each 10 mmHg higher resting SBP was associated with a 0.29-unit decrease in average pain at follow-up when holding baseline pain constant.
AP and LAT NTM equally reduced short-term pain and decreased SBP during-intervention, suggesting SBP-sympathoinhibition. These techniques have previously been shown to be sympatho-excitatory when delivered under different dosage parameters. SBP’s mediating and moderating role should be investigated.
“Level of Evidence: 1b.”
KEYWORDS: Mechanical neck pain, blood pressure, sympatho-inhibition, hypoalgesia, dosage
Introduction
Neck pain is reported in 10 to 20 percent of the population [1–3], and the incidence appears to be increasing [4]. A gender difference is also seen with neck pain, increasing with age, and being more common in women around the fifth decade [3,5]. For patients with non-traumatic, non-chronic neck pain, weak evidence supports clinicians providing cervical spine non-thrust manipulation [NTM] [6,7], with anterior-to-posterior [AP] seemingly more effective than a transverse/lateral [LAT] technique for pain reduction [8]. Various mechanisms describe the complex, multifaceted effects of NTM [8,9]. Although systematic reviews documenting a sympatho-excitatory response to NTM have been published [10–12], only two cited studies investigated the association of mechanisms with pain reduction. Of these two, Goodsell [13] found no association between stiffness (biomechanical mechanism) response and hypoalgesia, whereas Vicenzino et al. [14] were able to associate sympatho-excitatory (a neurophysiologic mechanism) skin blood flow response to pain reduction (hypoalgesia) in patients with lateral epicondylalgia. However, a systematic review of using skin blood flow as an indicator of the sympathetic nervous system response is now disputing this practice and its previous interpretation [15]. The current understanding is that sympathetic, and various non-sympathetic mechanisms regulate skin blood flow [15].
Moreover, instead of the anticipated skin blood flow vasoconstriction from a sympatho-excitatory mechanism, a randomized cross-over study [16] found vasodilation (typically related to sympatho-inhibition) during and post spinal NTM. Bialosky et al. [9] presented a comprehensive theoretical model on how manual therapy works and recommended increased research into mechanisms associated with hypoalgesia following manual therapy; however, it did not include blood pressure-related hypoalgesia as a mechanism. Resting or baseline blood pressure [BP] is known to be associated with pain reduction, a mechanism called BP-related hypoalgesia [17,18], but this mechanism is not well known in manual therapy due to a lack of literature. An autonomic/cardiovascular mechanistic study demonstrated sympatho-excitatory (heart rate increase) effects using AP NTM [19] when dosed at 3 × 2 minutes, but it did not study BP effects. Vicenzino et al. [14] associated sympatho-excitation with immediate hypoalgesia using LAT NTM when dosed at 3 × 30 seconds; however, their study did not investigate any cardiovascular variables. In a separate investigation, Vicenzino et al. [20] utilized LAT NTM to the neck and demonstrated a sympatho-excitatory cardiovascular response in pain-free adults but did not associate these responses with pain since the subjects did not have pain. In our experience, patients who are typically normotensive may at times exhibit a new onset of systolic blood pressure (SBP) increase (≥30 mmHg) following acute pain, and a further NTM-related BP increase may be worrisome.
Conversely, AP NTM displayed an SBP and heart rate decrease in pain-free adults when dosed at 5 × 10 seconds [21], but the cardiovascular effects of this dose application remain unknown in those with spinal pain. Therefore, it seems beneficial to investigate if either LAT or AP NTM (when dosed at 5 × 10 seconds) results in sympatho-excitation or sympatho-inhibition, whether one technique is better than the other in reducing neck pain and if this pain reduction correlates with resting BP. It would be useful to understand if this association extends beyond the immediate pain outcome and if there is any co-variance of improvement between associated cardiovascular response and clinical pain outcome [9]. Therefore, this study aimed to: (1) evaluate the association of resting BP with short-term neck pain reduction, and (2) compare the cardiovascular response and pain reduction effects of AP versus LAT NTM.
Methods
Study design
This study was a randomized clinical trial. Data were collected in the clinical research laboratories of Sacred Heart University and Azusa Pacific University. Research invitation emails were sent across both universities and respondents who met the inclusion/exclusion criteria for the study participated and attended one data collection session. The Ethics Committee of two institutions approved the study. Before study enrollment, all participants provided their written informed consent after they were informed of their rights and the purpose and procedure of the study.
Participants
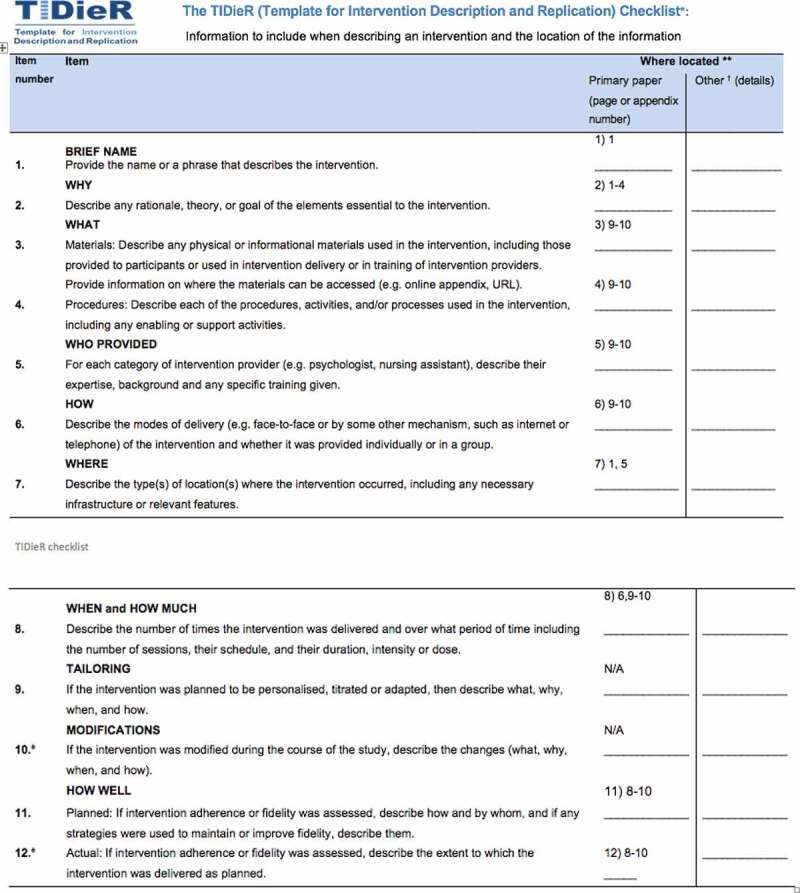
Forty-three participants were enrolled by research assistants at both universities and were treated by the primary author between 9/23/2015–6/19/2017. Figure 1 indicates the flow chart of enrollment, allocation, follow-up, and analysis (Appendix 1). The results section reports the participant demographics.
Figure 1.
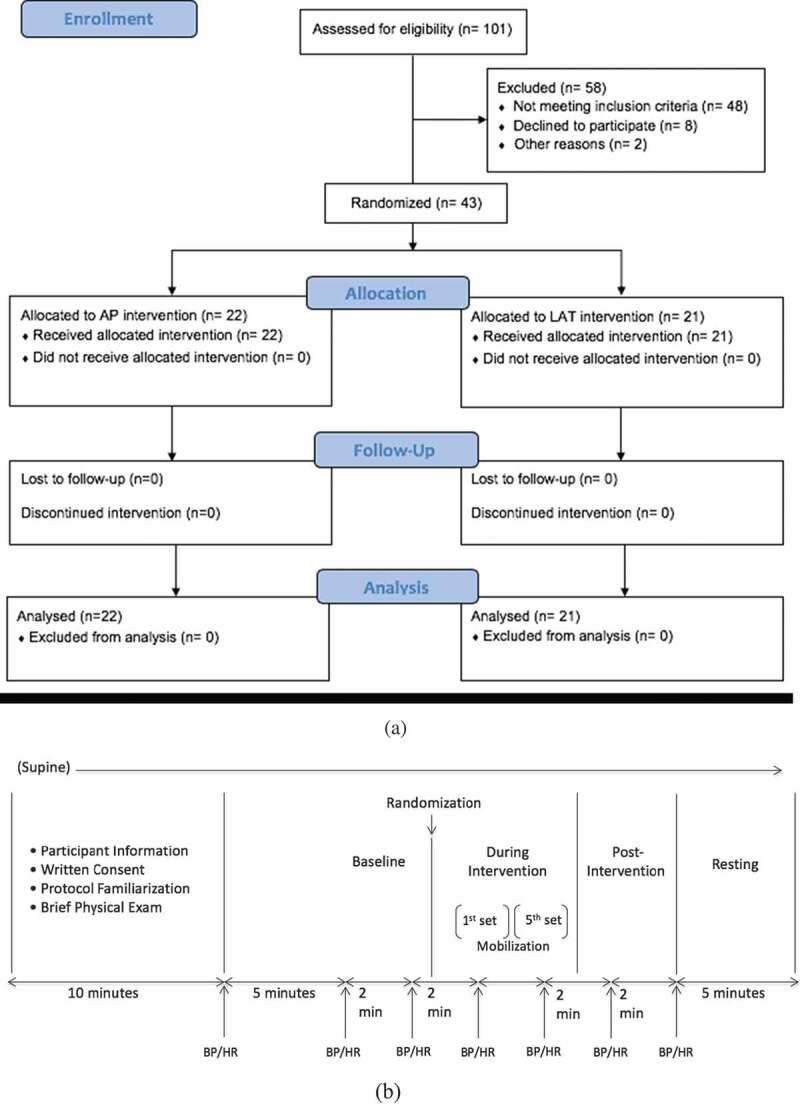
(1a) Flow chart (above). Abbreviations AP anterior to posterior NTM, LAT lateral glide NTM. (1b) Experimental procedure (below). BP blood pressure, HR heart rate.
Participants included were: between 21–50 years of age, having unilateral non-traumatic non-chronic neck pain, whose most painful neck movement with its corresponding numeric pain rating scale [NPRS] was determined. The ‘most painful neck movement’ was then retested with the addition of passive scapular elevation, and the NPRS was reassessed with the scapula elevated. Passive scapular elevation was added to ‘the most painful neck movement’ to minimize the contribution of muscle tension/guarding to the patient’s ‘most painful neck movement’ [22]. In doing so, it may indicate whether the underlying pain is related to an impairment in joint mobility, which is what the NTM is hypothesized to be addressing [22]. Furthermore, subjects were required to have resting SBP between 90 and 138 mmHg and resting diastolic blood pressure (DBP) between 60 and 88 mmHg [18], resting heart rate (HR) between 60 and 90 beats per minute and subjects had no prior exposure to AP or LAT NTM. Excluded participants were current smokers and those who had a history of fainting spells or loss of consciousness. Also excluded were those presently on blood thinners or oral contraceptives, or those taking medications for or who had a history of diabetes mellitus. Others excluded had neurologic [23] or cardiovascular disease, had a history of spinal surgery or had neck pain classified or associated with headache, radiating pain [23], or movement coordination impairments [7], or lacked written English proficiency.
Randomization/blinding
Baseline cardiovascular variables (primary outcome measures: SBP, DBP, HR) were measured (during time points #1 and #2- please refer to the next section) before randomization and before the procedure. After which subjects were randomized in blocks either to AP or LAT (n = 5 per block) NTM to equalize the number of participants in each group. One assistant investigator at each university generated a random-allocation sequence from an online randomizer (www.randomizer.org) and another assistant assigned each participant a sequential number and a random allocation number (1, AP NTM; 2, LAT NTM), that was concealed in an opaque envelope from the physiotherapist and the participants. Accordingly, the participants and the physiotherapist did not know the random allocation number until 30 seconds before the procedure (time point #3). The assistant made sure that the patient received the correct treatment allocation based on the card indicating either AP or LAT NTM, and the therapist provided 5 sets of 10-seconds of NTM delivered per the previously determined protocol. Besides being blinded to the cardiovascular variables measured, the physiotherapist was further blinded to all other outcomes [secondary outcome measures: Neck Disability Index (NDI), Numeric Pain Rating Scale (NPRS), Global Rating of Change (GROC)- please see below].
Time frame for measurements
A research assistant collected the NDI, NPRS, and measured the SBP, DBP and, HR with an OMRON HEM-790IT automatic blood pressure monitor [24] (Omron Healthcare, Inc., Bannockburn, IL) that was placed on the left humerus over the brachial artery for each subject. The blood pressure cuff remained intact throughout the entire recording time points. The start button on the automatic blood pressure monitor was pressed at the following time points: (1) 5 minutes, and (2) 7 minutes after lying supine; (3) the start of the 1st set of 10- second glides, (4) the start of the 5th set of 10- second glides, (5) 2 minutes after time point #4, and (6) 4 minutes after time point #4 (Figure 1(b)). Subsequently, the GROC was obtained post-intervention for the most painful neck movement. Two days following the intervention, each of the 43 subjects filled out the NDI and NPRS based on how the patient felt on the second-day post-intervention, and these results were either emailed or texted back to the research assistant (without any identifier). Within these two days, participants were instructed to continue their regular daily routine. Finally, to assess for any subsequent adverse reactions or side effects [8], follow-up phone calls and emails (at two weeks and again at one month) were performed by one of the co-investigators not responsible for implementing the AP or LAT NTM.
Participant flow
The day before the study, phone/email screened participants who met the inclusion criteria were given directions via emails not to do any of the following: ingest caffeinated drinks within four hours of the study, drink alcoholic beverage during the day of the study, or engage in exercise during the day of the study [25].
On the day of the study, participants filled out questionnaires (NDI, NPRS, past medical and current medication history), followed by a brief physical examination (BP, HR, and manual determination of the most symptomatic cervical spine segment for treatment) to confirm meeting the remainder of the inclusion criteria. Participants who met the criteria were then enrolled, and their data were de-identified by assigning a unique number so that their number, not their name, was linked to the test data collected.
Treatment groups
The subject either received (unilateral) AP or LAT (arm in neutral) NTM performed by a licensed physical therapist who was trained and had used these techniques for more than 15 years. This physical therapist is an orthopaedic clinical specialist certified by the American Board of Physical Therapy Specialties and a fellow of the American Academy of Orthopaedic Manual Physical Therapists. Concurrently, another co-investigator monitored the subject with a finger pulse oximeter placed on the right index finger during the treatment to ensure there was no pulselessness occurring greater than 3 seconds. For safety, an a priori decision was made to discontinue or stop the procedure if the blood pressure reading showed a drop of 50 mm Hg or if there were 3 seconds or greater of pulselessness.
For AP NTM, the thumbs were placed over the costal process, anterior to the most symptomatic facet and gentle oscillatory pressure was applied so that there was movement sensed posteriorly by the assessor’s second/third fingers or until the participant reported no greater than 2/10 pain on the NPRS [21,26]. For LAT NTM, the primary investigator placed the anterolateral aspect of the 2nd metacarpophalangeal joint over the most symptomatic segment and moved the postero-lateral aspect of the segment laterally toward the subject’s asymptomatic side [20,26] with oscillatory pressure. Importantly, the therapist performed each technique with a novel dose consisting of five sets of 10 seconds of mobilization, with 10-seconds rest between sets. The therapist applied AP or LAT NTM at a rate of 15 oscillations per 10 seconds (approximately 1.5 Hz) for a total number of 75 oscillations. Following the completion of cardiovascular recording (time point #6), each subject was asked to relax in supine for five more minutes before standing up. Afterward, the subject sat up and rested in the sitting position for at least 5 minutes to determine if there were any immediate adverse reactions or side effects (i.e., nausea, dizziness, lightheadedness, or increased neck pain). A research assistant at each university assessed intervention adherence per the protocol and indicated 100% intervention adherence (Appendix 2- TIDieR checklist).
Sample size calculation
Published sympatho-excitatory responses using LAT [20] NTM versus sympatho-inhibitory responses using AP [21] NTM, assuming common baseline values of the latter study provided cardiovascular data for sample size calculation. Thus, the estimated pre-/post-intervention changes of between-group differences in mean HR was −5.46 ± 11.65 beats per minute, mean SBP was −13.0 ± 14 mmHg, and mean DBP was −7.94 ± 5.4 mmHg. Using an unpaired t-test, if powered at 80% for a Type I error = 0.05 [27], the number of pairs of subjects needed in a paired design study were 18, 10, and 5 per group, respectively. Consequently, 18 participants were chosen per group with an additional three subjects to account for possible loss to follow-up, thereby resulting in 42 as the total number of participants.
Statistical analysis
The demographic and clinical characteristics of subjects were first summarized using descriptive statistics and reported as the mean ± standard deviation for continuous variables or percentage (counts) for categorical variables. All continuous outcome variables were checked for normality and homogeneity of variance before the statistical analyses. We evaluated the changes of clinical characteristics between baseline and post-treatment on all subjects using a paired T-test or Wilcoxon nonparametric test, and the changes of HR, SBP, and DBP across baseline, during, and post-treatment using an analysis of variance test. A linear regression model was used to evaluate the association between independent variables and pain score reduction in a univariate manner. Subsequently, multivariate regression models were also fitted to the data to identify independent predictors of outcomes while controlling for confounders. All variables with p < 0.1 on the univariate analysis were considered for initial inclusion in the multivariate model, but the final model retained only those which remained significant at p < 0.05.
All baseline demographic and clinical characteristics were also compared between AP and LAT NTM groups using unpaired T-tests for continuous data and chi-squared tests for categorical data. Mean differences between AP and LAT NTM groups on HR, SBP and DBP were compared using multilevel mixed-effect modeling for repeated measures across three-time points, adjusting for baseline characteristics by entering treatment, time, and baseline values [age, gender, and body mass index as covariates]. Separate analyses were performed with HR, SBP, and DBP as the dependent variables. All statistical analysis was conducted in the R-statistical package (www.r-project.org). The fits of the mixed model were done using function lme of the nlme package for the R environment of version 3.0.3. Statistical significance of p < 0.05 was considered to be relevant. Bonferroni correction was applied to account for multiple comparisons.
Results
A total of 43 participants started and completed the study providing a baseline to post-treatment differences in BP and HR, changes in neck pain, and NDI scores. The mean age (SD) of all participants was 29.00 (9.09) years, and 53.5% (n = 23) were female. Changes of HR, SBP, and DBP values across the baseline to follow-up times for all subjects were first assessed (Table 1). Cardiovascular parameters and ‘neck pain at best’ were not statistically significant, whereas all other changes in outcome measures from baseline to post-treatment were statistically significant but not clinically meaningful [9]. Also, the overall comparison of ‘neck pain at worst’ over time for all patients demonstrated statistical significance (p < 0.001), almost reaching a clinically significant reduction of 2/10 on the NPRS (Table 1). The ANOVA test did not reveal significant differences across follow-up times in HR and BP (Table 1).
Table 1.
Descriptive summary over time on all subjects (n = 43).
| Variable | Baseline | Post-treatment | P value1 | |
|---|---|---|---|---|
| Neck pain at best (0–10) | 1.09 ± 1.25 | 0.79 ± 1.28 | 0.090 | |
| Neck pain at worst (0–10) | 5.69 ± 1.92 | 3.74 ± 2.39 | <0.001 | |
| Neck pain at present (0–10) | 2.12 ± 1.58 | 1.21 ± 1.19 | 0.0002 | |
| Neck pain average (at best, at worst, & at present) | 2.92 ± 1.25 | 1.90 ± 1.26 | <0.001 | |
| Neck Disability Index |
7.74 ± 3.41 |
4.95 ± 4.04 |
<0.001 |
|
| |
Baseline |
During |
Post |
P value2 |
| `Heart rate | 61.34 ± 8.70 | 61.24 ± 8.88 | 61.62 ± 9.39 | 0.98 |
| SBP | 114.16 ± 13.84 | 112.22 ± 12.80 | 113.79 ± 13.99 | 0.78 |
| DBP | 71.23 ± 6.95 | 70.41 ± 7.75 | 70.90 ± 7.84 | 0.88 |
Abbreviation: SBP = Systolic blood pressure. DBP = Diastolic blood pressure.
Values are expressed as mean ± standard deviation.
P value1 using a paired T-test or Wilcoxon nonparametric test.
P value2 using ANOVA.
Pain levels at rest.
SBP and average pain scores at baseline were significantly associated with the averaged pain reduction under the univariate (p = 0.036 and 0.002) and multivariate (p = 0.032 and 0.002) models, respectively (Table 2).
Table 2.
Potential predictive variables for averaged pain reduction using linear regression.
| Variable | Univariate |
Multivariate |
|---|---|---|
| Coefficient (SD)/p-value | ||
| Technique LAT NTM |
−0.063 (0.385)/0.870 | NA |
| BMI | −0.042 (0.034)/ 0.226 | NA |
| Gender Male |
0.168 (0.385)/ 0.665 | NA |
| Age | −0.024 (0.021)/ 0.249 | NA |
| SBP at baseline* | −0.29 (0.13)/ 0.036 | −0.26 (0.12)/ 0.032 |
| Average Pain at baseline | 0.453 (0.136)/ 0.002 | 0.435 (0.130) /0.002 |
Pain reduction = baseline-post-intervention (higher + indicates a greater reduction, whereas – indicates increase).
SD: Standard deviation. LAT: Lateral glide non-thrust manipulation (NTM). BMI: Body mass index. NA: not applicable, not selected from the univariate analysis.
*Each 10 mmHg higher baseline SBP was associated with a 0.29 unit decrease in average pain at follow-up, holding baseline pain constant.
Table 3 indicates that the p-values for all comparisons between AP and LAT NTM groups were not significant, except ‘(neck pain at) worst’ experienced ‘2-days post-intervention’ using AP NTM (mean 2.95 ± SD 1.86) which was significantly lower (p = 0.027) than post LAT NTM (mean 4.60 ± SD 2.64). However, the change in ‘worst’ pain (‘Δ = Baseline – Post’ accounting for the change in pain from the baseline) was not significantly different between the AP and LAT NTM groups (p = 0.191). Therefore, there was no difference between AP and LAT NTM in their ability to reduce pain in this study.
Table 3.
Comparison between AP and LAT NTM for baseline to post-intervention outcomes in GROC, NPRS, and NDI.
| Variable | AP (n = 22) | LAT (n = 21) | P Value* | |
|---|---|---|---|---|
| Gender (n female) | 12 (54.5%) | 11 (52.4%) | 1* | |
| Age, years | 29.00 ± 9.09 | 30.38 ± 9.59 | 0.631 | |
| BMI | 24.56 ± 3.34 | 26.86 ± 6.98 | 0.181 | |
| Heart rate | Baseline | 61.23 ± 8.78 | 61.45 ± 8.84 | 0.933 |
| During | 60.45 ± 9.13 | 62.07 ± 8.76 | 0.556 | |
| Post | 61.32 ± 9.20 | 61.93 ± 9.81 | 0.834 | |
| SBP | Baseline | 113.89 ± 13.15 | 114.45 ± 14.84 | 0.895 |
| During | 112.25 ± 12.42 | 112.19 ± 13.50 | 0.988 | |
| Post | 114.36 ± 13.07 | 113.19 ± 15.20 | 0.787 | |
| DBP | Baseline | 71.50 ± 6.62 | 70.95 ± 7.44 | 0.800 |
| During | 70.25 ± 7.49 | 70.57 ± 8.21 | 0.894 | |
| Post | 71.09 ± 8.03 | 70.69 ± 7.83 | 0.869 | |
| GROC | ||||
| Post-intervention | 1.73 ± 1.88 | 1.71 ± 1.76 | 0.892 | |
| PAIN | ||||
| Best | ||||
| Baseline | 1.05 ± 1.29 | 1.14 ± 1.24 | 0.801 | |
| 2 Days post-intervention | 0.91 ± 1.60 | 0.67 ± 0.86 | 0.537 | |
| ∆ = Baseline – Post | −0.14 ± 1.25 | −0.48 ± 1.03 | 0.334 | |
| Worst | ||||
| Baseline | 5.33 ± 1.96 | 6.05 ± 1.86 | 0.232 | |
| 2 Days post-intervention | 2.95 ± 1.86 | 4.60 ± 2.64 | 0.027 | |
| ∆ = Baseline – Post | −2.43 ± 2.66 | −1.50 ± 1.73 | 0.191 | |
| Present | ||||
| Baseline | 2.18 ± 1.71 | 2.05 ± 1.47 | 0.783 | |
| 2 Days post-intervention | 1.32 ± 1.32 | 1.10 ± 1.04 | 0.542 | |
| ∆ = Baseline – Post | −0.86 ± 1.58 | −0.95 ± 1.02 | 0.827 | |
| Average | ||||
| Baseline | 2.76 ± 1.39 | 3.08 ± 1.11 | 0.417 | |
| 2 Days post-intervention | 1.73 ± 1.31 | 2.1 ± 1.22 | 0.345 | |
| ∆ = Baseline – Post | 1.06 ± 1.44 | 1 ± 0.97 | 0.869 | |
| NDI | ||||
| Baseline | 7.73 ± 3.48 | 7.76 ± 3.42 | 0.973 | |
| 2 days post-intervention | 5.14 ± 4.54 | 4.76 ± 3.55 | 0.764 | |
| ∆ = Baseline – Post | −2.59 ± 2.24 | −3.00 ± 2.53 | 0.578 | |
Abbreviation: AP = anterior to posterior non-thrust manipulation (NTM). LAT = lateral glide NTM. BMI = Body mass index. GROC = Global rating of change. NDI = Neck Disability Index. NPRS = Numeric pain rating scale. SD = standard deviation.
Values expressed as mean ± SD or count (%), except where otherwise indicated. *p-value by T-tests for normal data/Wilcoxon test non-normal data.
Within the AP NTM group, the change in the worst pain (∆ = Baseline – Post = −2.43 ± 2.66) exceeded 2/10 on the NPRS, making it clinically significant.
Finally, linear mixed-effects models were fitted to examine the longitudinal relationship between techniques and heart rate, systolic and diastolic blood pressure, while adjusting for patient baseline characteristics such as age, gender, and BMI. As shown in Table 4, there was no evidence of a significant between-treatment difference in HR, SBP, and DBP. Conversely, the SBP was significantly reduced from baseline to during (p = 0.007 Figure 2). Male patients had a significantly lower HR (estimate −5.62, SD 2.62, p = 0.03) and higher SBP (estimate 14.54, SD 3.39, p < 0.001) than female patients (Table 4).
Table 4.
Estimated effects of technique, time and demographics on heart rate, systolic blood pressure and diastolic blood pressure .
| Heart rate |
SBP |
DBP |
||||
|---|---|---|---|---|---|---|
| Variable | Estimate (SD) | p-value* | Estimate (SD) | p-value* | Estimate (SD) | p-value* |
| Treatment | ||||||
| AP NTM | Ref | Ref | Ref | |||
| LAT NTM | 0.03 (2.49) | 0.74 | -1.84 (3.22) | 0.94 | -1.08 (2.21) | 0.92 |
| Time | ||||||
| Baseline | Ref | Ref | Ref | |||
| During | -0.09 (0.69) | 0.89 | -1.94 (0.70) | 0.007 | -0.82 (0.51) | 0.11 |
| Post | 0.27 (0.69) | 0.68 | -0.37 (0.70) | 0.59 | -0.33 (0.51) | 0.51 |
| Gender | ||||||
| Female | Ref | Ref | Ref | |||
| Male | -5.62 (2.62) | 0.03 | 14.54 (3.39) | <0.001 | 1.08 (2.32) | 0.51 |
| Age | 0.07 (0.14) | 0.33 | −0.06 (0.18 | 0.78 | 0.04 (0.12) | 0.42 |
| BMI | 0.35 (0.24) | 0.16 | 0.60 (0.31) | 0.06 | 0.35 (0.21) | 0.11 |
(Abbreviation: AP = anterior to posterior non-thrust manipulation (NTM). LAT = lateral glide NTM. Ref = Reference category. SBP = Systolic blood pressure. DBP = Diastolic blood pressure. SD = standard deviation. BMI = Body mass index.)
*p-value by mixed-effect model for repeated measures analysis adjusted for age, gender and BMI.
Figure 2.
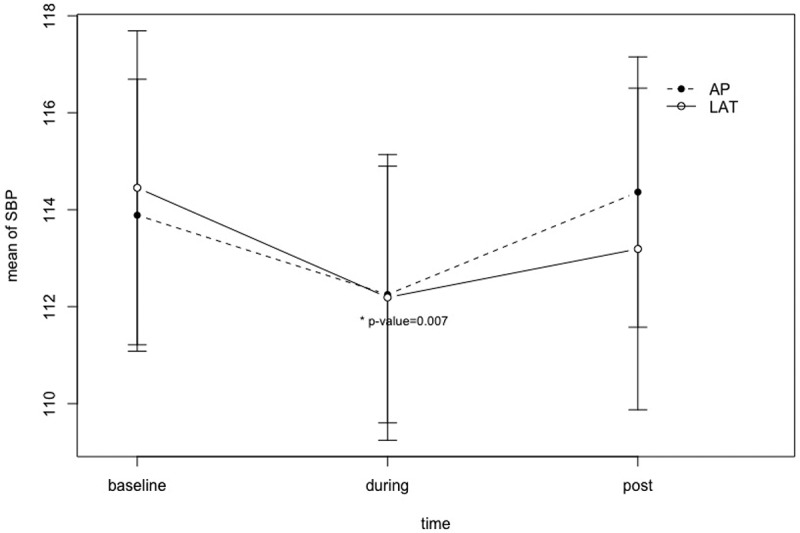
Mean changes in systolic blood pressure (SBP) across the follow-up time. Values expressed as means and standard errors. Error bars represent the standard error of measurement (SEM). The significant reduction is seen from baseline to during intervention (p = 0.007). (Abbreviation: AP = anterior to posterior non-thrust manipulation (NTM). LAT = lateral glide) NTM.
As a post-hoc analysis, we further evaluated the SBP reduction in each gender group separately. Although the SBP was significantly reduced between baseline and during the intervention among male patients (p-value estimate −2.87, SD 1.23, p = 0.026, Figure 3), it did not achieve statistical significance after Bonferroni correction for multiple comparisons (p < 0.025).
Figure 3.
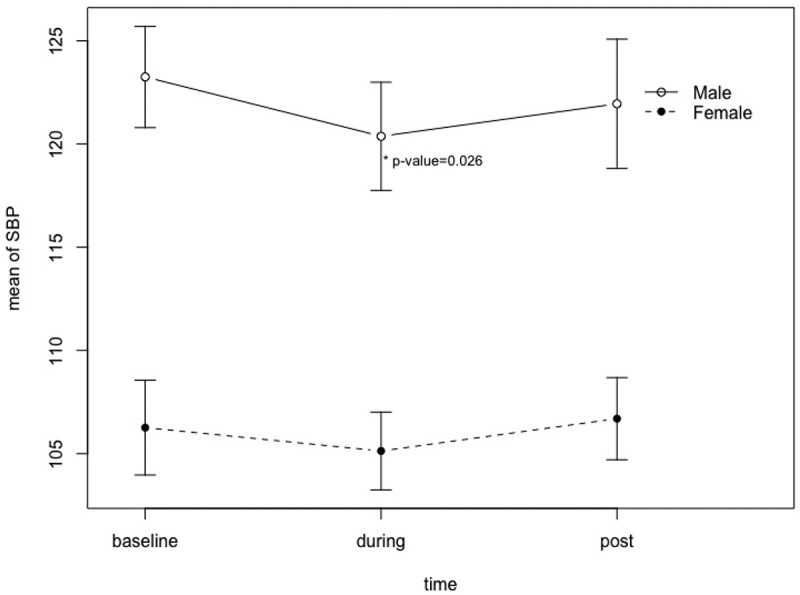
Mean changes in systolic blood pressure (SBP) by gender and the follow-up time. Values expressed as means and standard errors. The significant reduction is seen from baseline to during intervention among males (p = 0.026). Male patients also had significantly higher SBP than female patients.
Adverse effects
All participants denied any adverse and side effects during the intervention and the post-treatment follow-up period of 2 days, two weeks, and four weeks.
Discussion
To our knowledge, this is the first spinal NTM study that used blood pressure as a primary outcome measure in a clinical population [10–12]. Cardiovascular response to AP and LAT NTM in the cervical spine was investigated as a possible mechanism for pain relief. The results from the current study indicated there was no difference in the change in cardiovascular parameters between the AP and LAT NTM groups. This study identified a significant reduction in SBP from baseline to during-intervention for both AP and LAT NTM, suggesting sympatho-inhibitory SBP. In healthy individuals, the literature presents conflicting findings regarding the SBP response during cervical NTM with both sympatho-excitatory [20,25] and sympatho-inhibitory [21,28] SBP effects reported.
The novel dosage used in this study has demonstrated sympatho-inhibitory cardiovascular effects previously in pain-free subjects [21,28] and has now shown sympatho-inhibitory effects in subjects with neck pain. Research has not fully explored the impact of various dosage parameters for NTM, and our results suggest that this dosage may provide an alternative for clinicians seeking to use cervical NTM to reduce pain without causing an increase in BP.
Historically, sympatho-excitatory cardiovascular effects were believed to result from cervical NTM. La Touche and colleagues [19] reported sympatho-excitatory heart rate effects resulting from an AP NTM in subjects with cervico-craniofacial pain delivered for three bouts of 2 minutes each with 30-seconds rest in between bouts. Vicenzino and colleagues [20] also found sympatho-excitatory cardiovascular effects following LAT NTM in healthy individuals, provided for three sets of 30 seconds each with a 60-second rest period between sets. McGuiness and colleagues [25] demonstrated sympatho-excitatory cardiovascular effects in healthy volunteers following central posterior-to-anterior NTM, dispensed for three bouts of 60 seconds, with a 60-second rest between each bout. The contradicting response reported from the current study may be explained, in part, by the dosage of the NTM technique. This study is the first to demonstrate that short-term neck pain reduction with a decrease in SBP (during-intervention signifying sympatho-inhibition) is possible using a novel dosage of two cervical NTM techniques which have previously been shown to be sympatho-excitatory when delivered under traditional dosage parameters.
This spinal NTM study is the first to evaluate the association of resting SBP with short-term pain reduction [10–12]. Biomechanical, neurophysiological, and placebo effects are proposed mechanisms for improvements in pain and function following NTM [8]. Neurophysiological effects were examined in the current study through a cardiovascular response to explore that as a mechanism linked to pain relief. The results indicated that resting SBP was significantly associated with average pain reduction two days later, consistent with a mechanism referred to as BP-related hypoalgesia [17,18,29–31].
Table 2 shows that each 10 mmHg higher resting SBP was associated with a 0.29-unit decrease in average pain at follow-up, holding baseline pain constant. When considering a clinical scenario where a difference of 40 mmHg exists in resting SBP between two patients with an average baseline pain of 3/10 (as was seen in our cohort), the patient with the higher resting SBP may experience a reduction in pain by 1.16 (−0.029*40), resulting in a clinically insignificant pain rating of 1.84/10. The current study adds new knowledge and clinical value by offering an alternative for some patients who have a resting borderline BP (e.g., 138/90 mmHg).
On the one hand, their resting borderline hypertensive BP may be associated with better hypoalgesia (than those with lower BP, based on the above calculation derived from our study). Performing either AP or LAT NTM with the novel dose used in this study would likely not increase the BP toward the hypertensive range, which may add an important safety value to the clinical reasoning process. This study did not use a placebo as previous work has demonstrated a difference between placebo and cervical NTM [20,21,23,28].
The results also provide additional evidence supporting the pain-relieving effects of cervical spine NTM. The application of either AP or LAT NTM in subjects with non-chronic unilateral neck pain resulted in a significant decrease in the self-reported level of average pain. On average, the GROC and NDI did not reveal any meaningful improvements in the ‘most painful neck movement’ and self-reported function in this study, respectively. However, 36.4% [or 8/22] of the AP NTM group versus 28.6% [or 6/21] of the LAT NTM group achieved a clinically meaningful GROC of 3 or greater perceived improvement [32], with no significant difference between both proportions. These findings agree with previous literature that has failed to identify a significant benefit from cervical NTM in individuals with neck pain for improving function and quality of life in the immediate and intermediate timeframe [8].
The present study has limitations. First, the sample consisted of a younger population of individuals with lower levels of self-reported pain and dysfunction and may not be representative of those individuals who commonly present to physical therapy for the treatment of neck pain. Lower levels of pain and dysfunction at baseline may have also limited the ability to achieve significant reductions in pain and dysfunction with treatment. Additionally, this sample consisted specifically of individuals with unilateral non-chronic neck pain and thus limited the generalizability of the findings. Having a single, highly trained, and experienced physiotherapist delivers the intervention further limits the generalizability of these findings.
Additional research should be conducted to determine the differences in pain modulation between females and males as well as continue to explore dosage parameters of cervical NTM. Further investigation could assist in revealing the complex and multifactorial mechanisms underlying NTM techniques and aid in determining the appropriate dosage or procedure based on the possible mechanism that is mediating, moderating [9] and causing relief in a patient’s pain.
Conclusion
Both AP and LAT NTM reduced pain and SBP in subjects with non-chronic unilateral neck pain. SBP reduction was noted from baseline to during-intervention, suggesting sympathoinhibition. SBP at baseline was associated with the averaged pain reduction two days later, indicating SBP-associated hypoalgesia. Using a distinct dose of either AP or LAT NTM, physiotherapists could reduce neck pain 2-days later and produce a possible sympatho-inhibitory decrease in BP during-intervention. This effect may be ideal for cases where a sympatho-excitatory BP increase during treatment is worrisome.
Biographies
Emmanuel Yung, DPT, OCS, FAAOMPT is a Clinical Assistant Professor of Physical Therapy at Sacred Heart University in Fairfield, Connecticut. Manny is a Board-Certified Orthopaedic Clinical Specialist since 1998 and is a Fellow in the American Academy of Orthopaedic Manual Physical Therapists having completed his Manual Therapy Fellowship training at Southern California Kaiser Permanente program since 2003. He graduated from the University of Southern California with a Doctor of Physical Therapy and is a PhD student at New York University.
Cheongeun Oh, PhD did her postdoc training in Biostatistics at Yale University, after receiving her PhD from the State University of New York at Stony Brook. She holds a tenure track assistant professorship from Biostatistics Division at Department of Population Health, New York University School of Medicine. Dr. Oh has over 70 peer-reviewed publications and teaches numerous statistical courses in NYU School of Medicine. Over the past five years, she has collaborated and has supported the Department of Orthopaedic Surgery. She has served as a senior advisory member of collaborative research groups in funded collaborations.
Michael Wong, DPT, OCS, FAAOMPT holds a full-time appointment as an Associate Professor at Azusa Pacific University, teaching in the specialty areas of Orthopedic Physical Therapy. He is a residency and fellowship trained orthopaedic clinical specialist. Dr. Wong currently lectures for the Southern California Kaiser Permanente Orthopaedic Fellowship and Sports Rehabilitation Program and the University of Southern California Spine Fellowship. He also currently serves as Chair of the Institutional Review Board at Azusa Pacific University.
Jason K. Grimes PT, DPT, PhD is a Clinical Associate Professor in the Doctor of Physical Therapy Program at Sacred Heart University where he also serves the Sacred Heart University Orthopaedic Physical Therapy Residency Program Director. He graduated with his Master’s degree in Physical Therapy from Quinnipiac University and DPT and PhD from Nova Southeastern University. He has been Board-Certified as an Orthopaedic Clinical Specialist since 2007 and has over 15 years of clinical experience working with orthopaedic and sports populations.
Erica Mae Barton, DPT, OCS graduated with a Doctorate of Physical Therapy from Azusa Pacific University, Azusa, California. Dr. Barton is a Board-Certified Orthopaedic Clinical Specialist who is currently the Physical Therapist at Kaiser Permanente Regional Spine Center in Panorama City, California. She completed both her Orthopaedic Residency and Spine Rehabilitation Fellowship at Southern California Kaiser Permanente in Los Angeles, California.
Muhammad I. Ali, DPT is a physical therapist with the United States Air Force currently stationed in the United Kingdom. He graduated from Sacred Heart University with a Doctor of Physical Therapy and completed his orthopaedic residency program with Evidence In Motion Prior to serving in the Air Force, Dr. Ali also served in the United States Army Reserve for eight years as a Medical Laboratory Noncommissioned Officer and has been a Platoon Sergeant for three years, overseeing 40 officers.
Allison Breakey, DPT graduated from Sacred Heart University Doctor of Physical Therapy Program. She is a physical therapist for Hartford Healthcare at Backus Outpatient Care Center in Norwich, Connecticut. Previously, she was a member of the APTA Student Assembly Board of Directors and represented the student assembly as a student physical therapist delegate. Allison is also engaged in patient advocacy and was awarded the Victor Vaughan Legislative Service award by Sacred Heart University for her dedication to advocacy efforts.
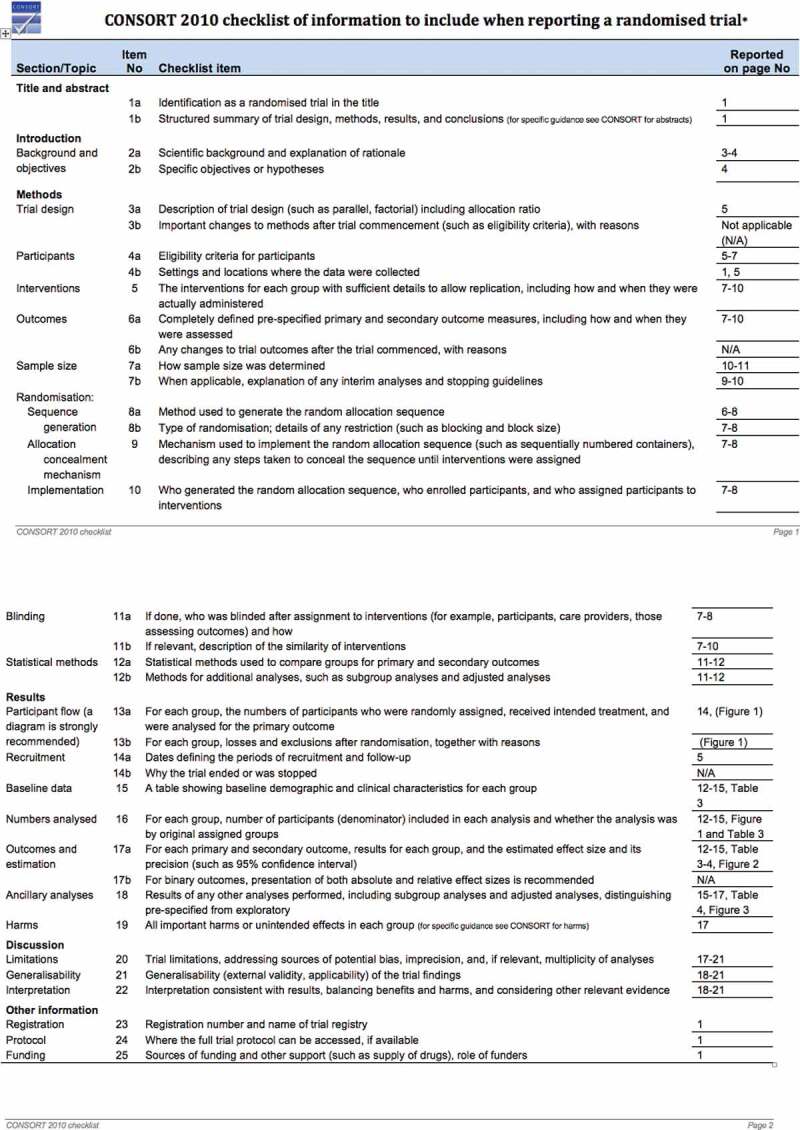
Appendix 1. CONSORT statement.
Appendix 2: TIDieR checklist.
Funding Statement
The American Academy of Orthopaedic and Manual Physical Therapists OPTP Grant provided funding for this study.The Ethics Committees of Sacred Heart University and Azusa Pacific University approved the protocol of this study. All participants provided their written informed consent after they were informed of their rights and the purpose and procedure of the study.
Acknowledgments
The authors would like to acknowledge Kelly Petersen and Karen Ching for assistance with data collection and Kyle Stapleton for his contribution in reviewing the revised manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Bovim G, Schrader H, Sand T.. Neck pain in the general population. Spine (Phila Pa 1976). 1994;19:1307–1309. [DOI] [PubMed] [Google Scholar]
- [2].Holmstrom EB, Lindell J, Moritz U. Low back and neck/shoulder pain in construction workers: occupational workload and psychosocial risk factors. Part 2: relationship to neck and shoulder pain. Spine (Phila Pa 1976). 1976;1992(17):672–677. [DOI] [PubMed] [Google Scholar]
- [3].Côté P, Cassidy JD, Carroll LJ, et al. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267–273. [DOI] [PubMed] [Google Scholar]
- [4].Nygren A, Berglund A, von Koch M. Neck-and-shoulder pain, an increasing problem. Strategies for using insurance material to follow trends. Scand J Rehabil Med Suppl. 1995;32:107–112. [PubMed] [Google Scholar]
- [5].Andersson HI. The epidemiology of chronic pain in a Swedish rural area. Qual Life Res. 1994;3(suppl 1):S19–S26. [DOI] [PubMed] [Google Scholar]
- [6].Wong JJ, Shearer HM, Mior S, et al. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? An update of the bone and joint decade task force on neck pain and its associated disorders by the OPTIMa collaboration. Spine J. 2016;16(12):1598–1630. [DOI] [PubMed] [Google Scholar]
- [7].Blanpied PR, Gross AR, Elliot JM, et al. Neck Pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1–A83. [DOI] [PubMed] [Google Scholar]
- [8].Gross A, Langevin P, Burnie SJ, et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database Syst Rev. 2015;(9):CD004249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bialosky JE, Beneciuk HM, Bishop MD, et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48:10–31. [DOI] [PubMed] [Google Scholar]
- [10].Lascurain-aguirrebeña I, Newham D, Critchley DJ. Mechanism of action of spinal mobilizations: a systematic review. Spine (Phila Pa 1976). 2016;41(2):159–172. [DOI] [PubMed] [Google Scholar]
- [11].Chu J, Allen DD, Pawlowsky S, et al. Peripheral response to cervical or thoracic spinal manual therapy: an evidence-based review with meta analysis. J Man Manip Ther. 2014;22(4):220–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kingston L, Claydon L, Tumilty S. The effects of spinal mobilizations on the sympathetic nervous system: a systematic review. Man Ther. 2014;19(4):281–287. [DOI] [PubMed] [Google Scholar]
- [13].Goodsell M, Lee M, Latimer J. Short-term effects of lumbar posteroanterior mobilization in individuals with low-back pain. J Manipulative Physiol Ther. 2000;23(5):332–342. [PubMed] [Google Scholar]
- [14].Vicenzino B, Collins D, Benson H, et al. An investigation of the interrelationship between manipulative therapy-induced hypoalgesia and sympathoexcitation. J Manipulative Physiol Ther. 1998a;21(7):448–453. [PubMed] [Google Scholar]
- [15].Zegarra-Parodi R, Park PY, Heath DM, et al. Assessment of skin blood flow following spinal manual therapy: a systematic review. Man Ther. 2015;20(2):228–249. [DOI] [PubMed] [Google Scholar]
- [16].Zegarra-Parodi R, Pazdernik VK, Roustit M, et al. Effects of pressure applied during standardized spinal mobilizations on peripheral skin blood flow: a randomised cross-over study. Man Ther. 2016;21:220–226. [DOI] [PubMed] [Google Scholar]
- [17].Campbell TS, Ditto B. Exaggeration of blood pressure-related hypoalgesia and reduction of blood pressure with low frequency transcutaneous electrical nerve stimulation. Psychophysiology. 2002;39(4):473–481. [DOI] [PubMed] [Google Scholar]
- [18].Olsen RB, Bruehl S, Nielsen CS, et al. Gender differences in blood pressure-related hypoalgesia in a general population: the tromsø study. J Pain. 2013;14(7):699–708. [DOI] [PubMed] [Google Scholar]
- [19].La Touche R, París-Alemany A, Mannheimer JS, et al. Does mobilization of the upper cervical spine affect pain sensitivity and autonomic nervous system function in patients with cervico-craniofacial pain?: a randomized-controlled trial. Clin J Pain. 2013;29(3):205–215. [DOI] [PubMed] [Google Scholar]
- [20].Vicenzino B, Cartwright T, Collins D, et al. Cardiovascular and respiratory changes produced by lateral glide mobilization of the cervical spine. Man Ther. 1998b;3:67–71. [Google Scholar]
- [21].Yung E, Wong M, Williams H, et al. Blood pressure and heart rate response to posteriorly directed pressure applied to the cervical spine in young, pain-free individuals: a randomized, repeated-measures, double-blind, placebo-controlled study. J Orthop Sports Phys Ther. 2014;44(8):622–626. [DOI] [PubMed] [Google Scholar]
- [22].Van Dillen LR, Mcdonnell MK, Susco TM, et al. The immediate effect of passive scapular elevation on symptoms with active neck rotation in patients with neck pain. Clin J Pain. 2007;23(8):641–647. [DOI] [PubMed] [Google Scholar]
- [23].Sterling M, Jull G, Wright A. Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity, and motor activity. Man Ther. 2001;6:72–81. [DOI] [PubMed] [Google Scholar]
- [24].Ahmad S, Chen S, Soueidan K, et al. Electrocardiogram-assisted blood pressure estimation. IEEE Trans Biomed Eng. 2012;59(3):608–618. [DOI] [PubMed] [Google Scholar]
- [25].McGuiness J, Vicenzino B, Wright A. Influence of a cervical mobilization technique on respiratory and cardiovascular function. Man Ther. 1997;2(4):216–220. [DOI] [PubMed] [Google Scholar]
- [26].Maitland G, Hengeveld E, Banks K, et al. Maitland’s vertebral manipulation. 7th ed. Philadelphia (PA): Elsevier/Butterworth-Heinemann; 2005. [Google Scholar]
- [27].Machin D, Campbell M, Fayers PM, et al. Sample size tables for clinical studies. 2nd ed. Malden (MA): Blackwell Science; 1997. [Google Scholar]
- [28].Yung EY, Oh C, Wong MS, et al. The immediate cardiovascular response to joint mobilization of the neck - A randomized, placebo-controlled trial in pain-free adults. Musculoskelet Sci Pract. 2017;28:71–78. [DOI] [PubMed] [Google Scholar]
- [29].Ditto B, Séguin JR, Boulerice B, et al. Risk for hypertension and pain sensitivity in adolescent boys. Health Psychol. 1998;17(3):249–254. [DOI] [PubMed] [Google Scholar]
- [30].Ottaviani C, Fagioli S, Mattei E, et al. Brain-heart pathways to blood pressure-related hypoalgesia. Psychosom Med. 2018;80(9):845–852. [DOI] [PubMed] [Google Scholar]
- [31].De la Coba P, Bruehl S, Garber J, et al. Is resolution of chronic pain associated with changes in blood pressure-related hypoalgesia? Ann Behav Med. 2018;52(7):552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Cleland JA, Childs JD, Whitman JM. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89(1):69–74. [DOI] [PubMed] [Google Scholar]


