Abstract
Objective
To examine the psychometric properties of the Activities-specific Balance Confidence (ABC) scale using Rasch analysis for individuals poststroke.
Design
Retrospective cohort.
Setting
Data was extracted from the Locomotor Experience Applied Post-Stroke phase 3, multisite, randomized controlled clinical trial.
Participants
Community-dwelling, ambulatory, older adults (N=406) (mean age ± SD, 61.97±12.76y; 45.07% female) approximately 2 months poststroke.
Intervention
None.
Main Outcome Measures
We examined unidimensionality, local dependence, rating-scale structure, item and person fit, person-item match, and separation index of the ABC scale.
Results
Confirmatory and exploratory factor analysis showed the ABC scale was adequately unidimensional and 3-item pairs had local dependence. A collapsed 5-category rating scale was superior to the 101-category scale. The hardest item was “walking outside on an icy sidewalk,” the easiest item was “getting into or out of a car,” and no items misfit. The ABC scale had high person reliability (0.93), despite 10.5% of individuals misfitting the expected response pattern. Mean ability level of the sample was slightly lower (−0.56 logits) than the mean item difficulty indicating that the ABC scale adequately matched our sample’s balance confidence. The ABC scale did not have a floor or ceiling effect and separated individuals into 5 statistically distinct strata (separation index=3.71).
Conclusions
The Rasch model supports the use of the ABC scale to measure balance confidence in individuals poststroke. The consistency of our results with previous Rasch analyses on the ABC scale demonstrates the instrument responds similarly across multiple populations; community-dwelling older-adults, outpatient orthopedic physical therapy, stroke, Parkinson disease, and lower-limb amputation. Recommendations include collapsing the rating scale and developing a computerized-adaptive test version of the scale to enhance clinical utility.
Keywords: Postural balance, Psychometrics, Rehabilitation, Stroke
List of abbreviations: ABC scale, Activities-specific Balance Confidence scale; ANPT, Academy of Neurologic Physical Therapy; CFA, confirmatory factor analysis; EFA, exploratory factor analysis; LEAPS, Locomotor Experience Applied Post-Stroke
Highlights
-
•
The ABC scale fits the Rasch model for measuring balance confidence poststroke.
-
•
Items on the ABC scale follow a theoretical hierarchal order of difficulty.
-
•
The ABC scale can separate individuals poststroke into 5 distinct strata.
-
•
The ABC scale category rating scale can be collapsed from 101 to 5 categories.
Individuals poststroke are at high risk for devastating consequences from falls including increased health care use and fracture rate1,2 with approximately 3 of 4 individuals falling during the first 6 months back at home and up to one quarter experiencing recurrent falls.3,4 Because falls are associated with fear of falling and balance confidence,5 measurement of an individual’s confidence in their balance is an important component of clinical practice for physical therapists in stroke rehabilitation. The Activities-specific Balance Confidence (ABC) scale was designed to measure balance confidence and takes approximately 20 minutes to complete.6 Individuals rate their confidence that they “will not lose their balance or become unsteady” when performing each daily task (item) on the scale from 0% (low confidence) to 100% (high confidence). A total score is calculated by averaging scores from all 16 items.
The ABC scale is widely used in stroke rehabilitation7 and has psychometric evidence to support its use for quantifying balance confidence in stroke survivors.8, 9, 10, 11, 12, 13 Total scores on the ABC scale have concurrent validity with measures used to assess activity and participation domains of the International Classification of Functioning, Disability and Health including the Berg Balance Scale,9, 10, 11 walking speed,9,10,12,13 Timed Up and Go,10,12,13 6-minute walk test,10,12 Barthel Index,10 Lower Extremity Fugl-Meyer Assessment,11 5-time sit-to-stand test,11 modified Rivermead Mobility Index,13 and physical function scale of the Medical Outcomes Study 36-Item Short-Form Health Survey.10,12 The ABC scale also has strong internal consistency,13 strong test-retest reliability for the scale’s total score (intraclass correlation coefficient=0.85,9 0.8212), and moderate to strong test-retest reliability at the item level (intraclass correlation coefficient=0.53-0.93).9 Most of the individuals poststroke score between 20% and 80% suggesting there is not a floor or ceiling effect and standard error of measurement has been reported between 6.819 and 5.05.10 Cutoff values for distinguishing between individuals with a history of multiple falls and no falls after suffering a stroke has been reported as 81.18 and 63.75,14 where lower confidence is associated with more falls.
However, no studies have examined measurement characteristics of the ABC scale for stoke survivors using item response theory psychometric methods, like Rasch analysis. Rasch analysis takes advantage of probabilistic mathematical modeling to examine a measurement tool’s ability to quantify abstract constructs in a meaningful way. This is accomplished by assuming the probability of successfully passing an item is dependent on the relation between a person’s ability and item difficulty. Results from a Rasch model order a measure, so scores can be interpreted linearly with set interval distances.15 Often, Rasch analysis identifies items that overlap in measurement properties and can be used to develop short forms or computerized-adaptive tests to reduce the time required to administer an instrument.16
Previous studies examined the ABC scale with Rasch analysis in different populations: Arnadottir et al (community-dwelling older adults),17 Sakakibara et al (lower-limb amputees),18 Franchignoni et al (Parkinson disease),19 and Wang et al (outpatient physical therapy).20 These studies found similar psychometrics for the ABC scale indicating that Rasch methods may support the comparison and use of the scale across patient populations, which is recommended for physical therapists in neurologic physical therapy practice by the Academy of Neurologic Physical Therapy (ANPT).21
Therefore, the purpose of this study is to examine the ABC scale using Rasch analysis for individuals poststroke. We hypothesize the ABC scale will fit the Rasch model for these individuals similarly to other populations. Results from this analysis will provide support for comparison and use of the ABC scale across populations as recommended by the ANPT.
Methods
Data source
This study is a secondary analysis of data from 406 individuals poststroke who participated in the Locomotor Experience Applied Post-Stroke (LEAPS) phase 3, multisite, randomized controlled clinical trial.22 The Institutional Review Board approval of this secondary analysis was not required because data were free of identifiers. Included individuals had a stroke and (1) were older than 18 years; (2) were able to ambulate a minimum of 10 ft with maximum 1-person assist; (3) had a self-selected walking speed <0.8 m/s; and (4) were living in the community.23 Individuals were excluded who had (1) additional neurologic pathology and comorbidities; (2) severe pain, amputation, or orthopedic conditions limiting ambulation; or (3) severe cardiovascular comorbidities that would prevent participation in high-intensity exercise.23 Demographic data for the trial were collected during an enrollment window (within 30d of diagnosis).23 We analyzed ABC scale data collected at approximately 2 months poststroke (baseline assessment). Summary demographic data were analyzed with SAS version 9.4a and presented in table 1.
Table 1.
Participant demographics
| N=406 | |
|---|---|
| Demographic Characteristics | Totals |
| ABC Score (2mo poststroke) | 45.06 (23.88) |
| Age | 61.97 (12.76) |
| Sex | |
| Male | 54.93 |
| Female | 45.07 |
| Race | |
| American Indian | 1.23 |
| Asian | 13.3 |
| Black or African American | 22.17 |
| White | 57.64 |
| Native Hawaiian | 4.68 |
| >1 race | 0.74 |
| Unknown | 0.25 |
| Hispanic or Latino | 15.52 |
| Stroke type | |
| Ischemic | 80.05 |
| Hemorrhagic | 18.72 |
| Uncertain | 1.23 |
| Stroke location | |
| Right hemisphere | 48.03 |
| Left hemisphere | 35.22 |
| Brainstem | 62 |
| Bilateral hemispheres | 6 |
NOTE. Continuous variables are presented in mean ± SD; categorical variables are presented as a percentage.
Rasch analysis
Rasch analysis of the ABC scale was done with Winsteps version 3.93.1.b Tests of unidimensionality and local dependence were performed in Mplus version 7.4.c
Rating-scale structure
Appropriateness of the rating scale structure was determined based on Linacre’s 3 rating-scale criteria24: (1) each rating-scale category has a minimum of 10 observations; (2) average measures within each category advance monotonically (ie, demonstrate increasing observed item difficulty with increasing category value); and (3) outfit mean-squares are <2. Category probability curves were examined to see if categories of the rating scale had distinct peaks (indicating each category of the rating scale is the most probable response for a given portion of the measure).15 The rating scale was collapsed for further analysis if it did not meet designated criteria.
Unidimensionality
An assumption of the Rasch model is that the measure is unidimensional. A confirmatory factor analysis (CFA) with 1 factor was performed on a random sample from our data (n=203) to assess unidimensionality. Model fit from the CFA was evaluated against recommendations from Reeve et al25: (1) comparative fit index>0.95; (2) root mean square error approximation<0.06; (3) Tucker-Lewis Index>0.95; and (4) standardized root mean residuals <0.08. If model fit was poor, an exploratory factor analysis (EFA) was done on another random sample (n=203) to determine additional factors. Additional factors from EFA were evaluated on model fit (Reeve’s recommendations25), eigenvalue ratio (>4 indicates sufficient unidimensionality), visualization of the scree plot, and clinical interpretation.
Local dependence
Local independence assumes no significant associations among items responses when controlling for the dominant factor of the measure.25 A residual correlation matrix from the CFA was used to identify dependent item pairs. Residual item correlations >0.2 or <−0.2 were considered locally dependent.25
Item and person fit
Items or individuals were classified as misfitting if fit statistics had mean-square standardized residuals ≥1.4 and standardized z scores ≥2.24,26
Item difficulty hierarchy
Item difficulty was used to evaluate theoretical construct validity of the ABC scale. The Rasch model assigns item difficulty and person ability measures to a logit scale. Items that are easier or persons with lower ability are assigned lower values, and items with higher difficulty or persons with high ability are assigned higher values. Item measure estimates were used to determine if items overlapped. Items were considered overlapping if the item’s measure estimate was within 2 standard errors of another item.
Person-item match
Observation of the person-item map was used to evaluate for floor (within error of worst possible outcome [raw score 0/100]) and ceiling effects (within error of best possible outcome [raw score 100/100]). We considered the ABC scale to have a floor or ceiling effect if >15% of individuals scored the worst or best possible outcomes.27
Separation index
The person separation index was used to evaluate the ABC scale’s ability to differentiate people into statistically distinct strata. The number of strata was determined from the following formula28:
Results
Rating-scale structure
We initially analyzed the data using a 101-category (0%-100%) rating scale. Only a few rating-scale categories had >10 observations. No outfit mean-squares values exceeded 2.0; however, there were disordered rating-scale estimates. Collectively, this demonstrates that rating-scale categories were underused, and the ABC scale was not adequately fitting the Rasch model. Therefore, we tested a collapsed 5-category rating scale based on previous publications (0%-9%, 10%-30%, 31%-60%, 61%-90%, 91%-100%).18,20 The new rating scale had >10 observations per category, demonstrated appropriate rating-scale estimates of increasing ability level (rating-scale categories advanced monotonically), and no category exceeded the outfit mean square threshold of 2. The rating-scale structure results are presented in table 2.
Table 2.
Rating-scale structure
| Score | Observed Average | Infit Mean-Square |
Outfit Mean-Square |
Frequency Counts (%) |
|---|---|---|---|---|
| 0 (no confidence) | −2.72 | 1.06 | 1.07 | 1521 (23) |
| 1 (low confidence) | −1.32 | 0.90 | 0.84 | 1352 (21) |
| 2 (moderate confidence) | −0.20 | 0.85 | 0.78 | 1594 (25) |
| 3 (high confidence) | 0.95 | 0.91 | 0.92 | 1400 (22) |
| 4 (complete confidence) | 2.25 | 1.40 | 1.33 | 629 (10) |
Unidimensionality
CFA using the collapsed rating scale returned the following fit statistics: (1) comparative fit index 0.95 (>0.95 indicates good fit); (2) root mean square error approximation 0.15 (<0.06 indicates good fit); (3) Tucker-Lewis Index 0.95 (>0.95 indicates good fit); and (4) standardized root mean residuals 0.09 (<0.08 indicates good fit).
EFA returned 2 factors with eigenvalues >1.0 and the following fit statistics for a 2 factor model: (1) comparative fit index 0.96 (>0.95 indicates good fit); (2) root mean square error approximation 0.14 (<0.06 indicates good fit); (3) Tucker-Lewis Index 0.95 (>0.95 indicates good fit); and (4) standardized root mean residuals 0.05 (<0.08 indicates good fit). Eigenvalues for the first 2 factors were 10.17 and 1.41, respectfully. The second factor included the following items: “stand on your tiptoes and reach for something above your head,” “stand on a chair and reach for something,” “sweep the floor,” “walk in a crowded mall where people rapidly walk past you,” “are bumped into by people as you walk through the mall,” “step onto or off an escalator while you are holding onto a railing,” “step onto or off an escalator while holding onto parcels such that you cannot hold onto the railing,” “walk outside on icy sidewalks.” The ratio of eigenvalues for the first and second factors is 7:21, and visual interpretation of the scree plot favors accepting only 1 factor. Although all criteria were not met, the results of the factor analysis support that the ABC scale adequately meets the assumption of unidimensionality.
Local dependence
Three item pairs were found to have local dependence: (1) “walk outside on icy sidewalks”–“walk outside the house to a car parked in the driveway” (r= −0.23); (2) “walk outside the house to a car parked in the driveway”–“step onto or off an escalator while holding onto parcels such that you cannot hold onto the railing” (r=−0.25); and (3) “walk outside on icy sidewalks”–“reach for a small can off a shelf at eye level” (r=−0.21).
Item and person fit
No items misfit the Rasch model. The findings related to item fit are reported in table 3. Forty-three individuals (10.6%) responses did not fit with the Rasch model (mean-square standardized residuals ≥1.4 and standardized z scores ≥2 of fit statistics.24,26). We found nearly identical results from the Rasch analysis when misfitting persons were removed. Therefore, we are reporting findings for the whole sample because (1) individuals included in the sample are largely representative of community-dwelling stroke survivors and (2) the ABC scale is designed and advocated to be broadly applicable for this patient population. The ABC had high person reliability (0.93) and Cronbach alpha (0.95).
Table 3.
Item measure order
| Item | Item Number | Measure | Model Standard Error | Infit Mean-Square |
Infit z Score | Outfit Mean-Square |
Outfit z Score | Point Measure Correlation |
|---|---|---|---|---|---|---|---|---|
| “Walk outside on icy sidewalks” | 16 | 1.98 | 0.08 | 0.96 | −0.4 | 0.94 | −0.4 | 0.67 |
| “Stand on chair and reach for something” | 6 | 1.79 | 0.08 | 1.29 | 3.4 | 1.10 | 0.8 | 0.65 |
| “Step onto or off an escalator while holding onto parcels such that you cannot hold onto the railing” | 15 | 1.45 | 0.07 | 1.00 | 0.0 | 0.93 | −0.6 | 0.71 |
| “Are bumped into by people as you walk through the mall” | 13 | 0.49 | 0.07 | 0.73 | −4.2 | 0.69 | −4.1 | 0.80 |
| “Stand on your tip toes and reach for something above your head” | 5 | 0.43 | 0.07 | 1.04 | 0.6 | 1.02 | 0.3 | 0.74 |
| “Sweep the floor” | 7 | 0.36 | 0.07 | 1.35 | 4.5 | 1.31 | 3.4 | 0.71 |
| “Step onto or off an escalator while you are holding onto a railing” | 14 | 0.11 | 0.07 | 1.05 | 0.7 | 0.98 | −0.2 | 0.76 |
| “Walk in a crowded mall where people rapidly walk past you” | 12 | −0.04 | 0.07 | 0.65 | −5.7 | 0.62 | −5.6 | 0.82 |
| “Walk up or down stairs” | 2 | −0.11 | 0.07 | 1.03 | 0.5 | 1.02 | 0.2 | 0.75 |
| “Bend over and pick up a slipper from the front of a closet floor” | 3 | −0.27 | 0.07 | 1.01 | 0.1 | 0.97 | −0.4 | 0.76 |
| “Walk up or down a ramp” | 11 | −0.44 | 0.07 | 0.81 | −2.9 | 0.76 | −3.4 | 0.80 |
| “Walk across a parking lot to the mall” | 10 | −0.51 | 0.07 | 0.88 | −1.8 | 0.82 | −2.4 | 0.80 |
| “Walk outside the house to a car parked in the driveway” | 8 | −1.11 | 0.07 | 0.88 | −1.7 | 0.84 | −2.1 | 0.80 |
| “Walk around the house” | 1 | −1.22 | 0.07 | 1.03 | 0.4 | 1.02 | 0.3 | 0.73 |
| “Reach for a small can off a shelf at eye level” | 4 | −1.35 | 0.07 | 1.23 | 3.0 | 1.26 | 3.0 | 0.73 |
| “Get into or out of a car” | 9 | −1.56 | 0.07 | 1.21 | 2.8 | 1.14 | 1.7 | 0.71 |
Item difficulty and person-item match
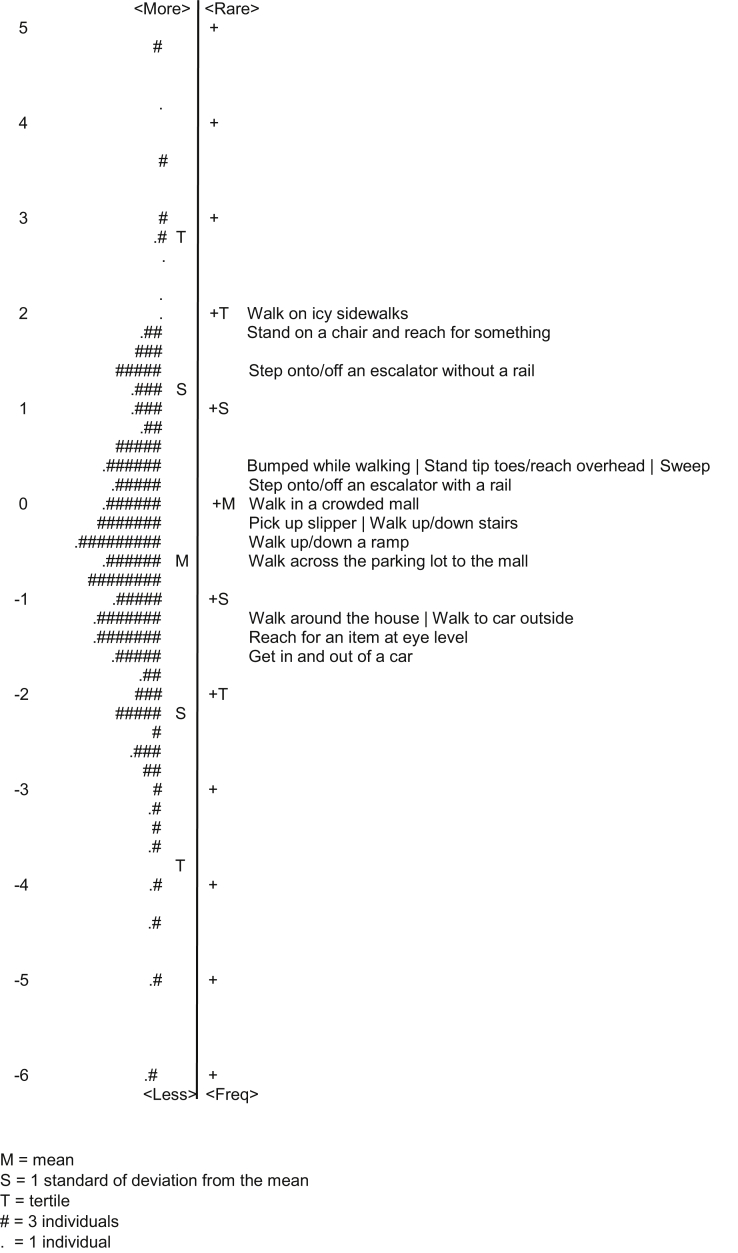
The results of the item difficulty analysis are presented in table 3 and visually displayed using a person-item map in fig 1. The hardest item was “walking outside on icy sidewalks,” while the easiest item was “getting into or out of a car.”
Fig 1.
Person-item map. Abbreviations: Bumped while walking, Are bumped into as you walk in a mall; Pick up a slipper, Pick up a slipper from the floor; Stand tip toes/reach overhead, Stand on tip toes and reach overhead; Walk to car outside, Walk outside to a car in the driveway.
The person-item map in fig 1 shows the distribution of (1) people based on ability (left: low ability, bottom; high ability, top) and (2) item difficulty (right: easy, bottom; hard, top). The range of the distribution was 11 logits with the mean ability of our sample (−0.58 SE 0.38) below the mean difficulty of the items (anchored at 0) indicating the model adequately matched our participants’ confidence. We did not have a ceiling effect (no individuals had a maximum score) and observed negligible floor effects (4 individuals had a minimum score [0.9%]). In addition to the overlapping items in fig 1, we found occurrences where item measures were within 2 standard errors of another item indicating several items have overlapping difficulty. Item measures and standard errors are presented in table 3.
Separation index
The ABC scale differentiated individuals in our sample into 5.28 statistically distinct strata (separation index=3.71).
Discussion
This is the first study to examine ABC scale psychometrics using Rasch analysis for individuals poststroke. We found the Rasch model strongly supports the use of the ABC scale to measure balance confidence in these individuals. Like previous studies,18,20 we found the scale fits the Rasch model better using a collapsed 5-category rating scale. Collapsing the rating scale corrected its disorder and prevented item misfit. Additionally, we found the ABC scale was adequately unidimensional to meet the necessary assumption for Rasch analysis. Although EFA suggested a second factor, we do not feel that it is warranted provided (1) the improvement in model fit is minimal, (2) the eigenvalue ratio for the first and second factors greatly exceeds the recommended value of 4, and (3) visualization of the scree plot confirms 1 dominant factor. Also, there is no clinical rationale to support items grouped in the second factor except for the fact they are the more difficult items on the scale. Therefore, there is not enough evidence that unidimensionality is violated, which is consistent with previous publications.17, 18, 19, 20 Our analysis of local dependence identified 3 item pairs with residual correlations >0.2 magnitude. One recommendation is to remove items with high dependence when performing Rasch analysis because item dependence can be a threat to unidimensionality.25 However, there is a discrepancy as to what magnitude of association constitutes removing items.19,25 Therefore, we reported results with all items under the caveat that effects of local dependence should be closely evaluated when translating the ABC scale into a computerized-adaptive test because item pairs with local dependence may need to be identified as “enemies.”25
We found other similarities and only minor differences in the ABC scale’s psychometrics for individuals poststroke compared to other populations. We report a separation index (3.71) for the ABC scale indicating that the scale separated our sample into 5.28 statistically distinct strata based on balance confidence, similar to previous publications (5.2,20 417). Other congruent psychometrics include high Cronbach alphas (0.94,18 0.95,19 0.93,20 0.95 in our study) and no floor or ceiling effects.17,18,20 The range of the scale in our model was 11 logits (−6 to 5), which was comparable to other publications.17, 18, 19, 20 The three items “walk outside on an icy sidewalk,” “standing on a chair and reaching for something,” and “step onto or off an escalator while holding onto parcels such that you cannot hold onto the railing” are consistently (with the exception of order) the 3 most difficult items.17, 18, 19, 20 However, there is more variability in item difficulty for easy items. We found the item “getting into or out of a car” to be the easiest item, which is comparable with 2 publications where this item was the second easiest.18,20 Yet, in other publications, this item was considered moderately difficult and fell close to the center of the scale.17,19
A component of validating measurement scales derived from Rasch analysis is to determine whether the item hierarchy is consistent with clinical and theoretical expectations.19 The item hierarchy in table 3 and fig 1 shows item difficulty progress from discrete stable tasks (ie, reaching and transferring) to stable walking to walking tasks in conditions of increasing instability. Thus, item hierarchy is consistent with clinical and theoretical expectations for individuals poststroke and more broadly, individuals with balance impairments.
Therefore, we can conclude that the ABC scale responds similarly for individuals poststroke and other populations including community-dwelling older adults, outpatient orthopedic physical therapy participants, individuals with lower limb amputation, and individuals with Parkinson disease. As a result, clinicians or researchers interested in measuring balance confidence for these clinical populations do not need to develop diagnosis specific versions of the instrument and can compare scores between patient groups. The ABC scale’s ability to respond similarly across a variety of patient populations supports recent recommendations by the ANPT for the scale to be included in a core set of outcome measures in the rehabilitation of adults with neurologic diagnoses21 and allows one to hypothesize that the instrument may be “diagnosis free.”
Implications for future research and practice
We present 2 recommendations for future research and practice to facilitate the clinical adoption of the ABC scale. First, we recommend implementing a 5-category rating scale (“no confidence” [0], “low confidence” [1], “moderate confidence” [2], “high confidence” [3], “complete confidence” [4]).18 Second, we recommend reducing the number of items by creating short forms and computerized-adaptive tests of the ABC scale based on the Rasch model. Although 3 short forms exist for the ABC scale,29, 30, 31 they were not developed from a Rasch model and should be approached with caution because they may have diminished measurement characteristics relative to the full scale.19,32
In general, these recommendations should facilitate clinical adoption of the ABC scale by reducing test administration time, a commonly cited barrier to outcome measurement use by practitioners.33,34
Study limitations
There are some limitations with this research. One limitation is that the authors were not in control of the data collection procedure, which is typical of archival data secondary analyses. Selection bias associated with selection of acute care facilities for urgent stroke care may exist potentially limiting our findings’ generalizability. Generalizability of our findings may also be limited by the inclusion criteria required for individuals to participate in the LEAPS trial. Specifically, participants in the trial were community dwelling and able to ambulate indicating that our findings may not extend to more functionally limited individuals.
Conclusions
Consistent with calls to use the ABC scale across neurologic diseases in adult populations,21 Rasch analysis supports the use of the ABC scale for measuring balance confidence in individuals poststroke. The ABC scale’s psychometrics are largely enhanced with a 5-category rating scale. We recommend using the ABC scale to quantify balance confidence in these individuals based on absent floor and ceiling effects and the scale’s ability to distinguish 5 strata of individuals. Collapsing the ABC’s rating scale and developing a computerized-adaptive test will enhance measurement capability and efficiency for clinicians and researchers working in stroke rehabilitation.
Suppliers
-
a.
SAS version 9.4; SAS Institute Inc.
-
b.
Winsteps version 3.93.1; John Lincare.
-
c.
Mplus version 7.4; Muthén & Muthén.
Acknowledgments
We thank the LEAPS investigator team (principal investigator: Pamela Duncan, PT, PhD, FAPTA, FAHA) for data collection and archival. We also thank the National Institute of Neurological Disorders and Stroke for funding the LEAPS trial (grant no. R01 NS050506).
Footnotes
Supported by the VA Office of Research and Development (ORD), with additional support from the VA/ORD Rehabilitation R&D Service (grant no. 1I01RX001935), support from the National Institutes of Health (NIH, grant no. P20 GM109040), and the Promotion of Doctoral Studies Level 1 Scholarship from the Foundation for Physical Therapy Research. Data for the study was provided by the NIH National Institute of Neurological Disorders and Stroke from the Locomotor Experience Applied Poststroke (LEAPS) trial (grant no. R01 NS050506). Any opinions expressed in this publication are those of the authors and do not necessarily reflect the view of the United States Department of Veterans Affairs or the NIH. Data from the LEAPS trial can be obtained by contacting the National Institute of Neurological Disorders and Stroke at www.ninds@nih.org.
Disclosures: none.
Clinical Trial Registration No.: NCT00243919.
References
- 1.Pouwels S., Lalmohamed A., Leufkens B. Risk of hip/femur fracture after stroke: a population-based case-control study. Stroke. 2009;40:3281–3285. doi: 10.1161/STROKEAHA.109.554055. [DOI] [PubMed] [Google Scholar]
- 2.Tilson J.K., Wu S.S., Cen S.Y. Characterizing and identifying risk for falls in the LEAPS study: a randomized clinical trial of interventions to improve walking poststroke. Stroke. 2012;43:446–452. doi: 10.1161/STROKEAHA.111.636258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forster A., Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995;311:83–86. doi: 10.1136/bmj.311.6997.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh M.E., Sorensen J., Galvin R. First year post-stroke healthcare costs and fall-status among those discharged to the community. Eur Stroke J. 2018;3:254–262. doi: 10.1177/2396987318764954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman S.M., Munoz B., West S.K., Rubin G.S., Fried L.P. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 6.Powell L.E., Myers A.M. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50a:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan J.E., Crowner B.E., Kluding P.M. Outcome measures for individuals with stroke: process and recommendations from the American Physical Therapy Association Neurology Section Task Force. Phys Ther. 2013;93:1383–1396. doi: 10.2522/ptj.20120492. [DOI] [PubMed] [Google Scholar]
- 8.Beninato M., Portney L.G., Sullivan P.E. Using the International Classification of Functioning, Disability and Health as a framework to examine the association between falls and clinical assessment tools in people with stroke. Phys Ther. 2009;89:816–825. doi: 10.2522/ptj.20080160. [DOI] [PubMed] [Google Scholar]
- 9.Botner E.M., Miller W.C., Eng J.J. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil Rehabil. 2005;27:156–163. doi: 10.1080/09638280400008982. [DOI] [PubMed] [Google Scholar]
- 10.Salbach N.M., Mayo N.E., Robichaud-Ekstrand S., Hanley J.A., Richards C.L., Wood-Dauphinee S. Balance self-efficacy and its relevance to physical function and perceived health status after stroke. Arch Phys Med Rehabil. 2006;87:364–370. doi: 10.1016/j.apmr.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 11.An S., Lee Y., Lee D., Cho K.H., Lee G., Park D.S. Discriminative and predictive validity of the short-form activities-specific balance confidence scale for predicting fall of stroke survivors. J Phys Ther Sci. 2017;29:716–721. doi: 10.1589/jpts.29.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forsberg A., Nilsagård Y. Validity and reliability of the Swedish version of the Activities-specific Balance Confidence Scale in People with Chronic Stroke. Physiother Can. 2013;65:141–147. doi: 10.3138/ptc.2011-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ylva N., Anette F. Psychometric properties of the Activities-Specific Balance Confidence Scale in persons 0-14 days and 3 months post stroke. Disabil Rehabil. 2012;34:1186–1191. doi: 10.3109/09638288.2011.637604. [DOI] [PubMed] [Google Scholar]
- 14.Park E.Y., Lee Y.J., Choi Y.I. The sensitivity and specificity of the Falls Efficacy Scale and the Activities-specific Balance Confidence Scale for hemiplegic stroke patients. J Phys Ther Sci. 2018;30:741–743. doi: 10.1589/jpts.28.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bond T.G., Fox C.M. 3rd ed. Routledge; New York: 2015. Applying the Rasch model: fundamental measurement in the human sciences. [Google Scholar]
- 16.Porter I., Goncalves-Bradley D., Ricci-Cabello I. Framework and guidance for implementing patient-reported outcomes in clinical practice: evidence, challenges and opportunities. J Comp Eff Res. 2016;5:507–519. doi: 10.2217/cer-2015-0014. [DOI] [PubMed] [Google Scholar]
- 17.Arnadottir S.A., Lundin-Olsson L., Gunnarsdottir E.D., Fisher A.G. Application of Rasch analysis to examine psychometric aspects of the activities-specific balance confidence scale when used in a new cultural context. Arch Phys Med Rehabil. 2010;91:156–163. doi: 10.1016/j.apmr.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Sakakibara B.M., Miller W.C., Backman C.L. Rasch analyses of the Activities-specific Balance Confidence Scale with individuals 50 years and older with lower-limb amputations. Arch Phys Med Rehabil. 2011;92:1257–1263. doi: 10.1016/j.apmr.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franchignoni F., Giordano A., Ronconi G., Rabini A., Ferriero G. Rasch validation of the Activities-specific Balance Confidence Scale and its short versions in patients with Parkinson’s disease. J Rehabil Med. 2014;46:532–539. doi: 10.2340/16501977-1808. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y.C., Sindhu B., Lehman L., Li X., Yen S.C., Kapellusch J. Rasch analysis of the Activities-Specific Balance Confidence Scale in older adults seeking outpatient rehabilitation services. J Orthop Sports Phys Ther. 2018;48:574–583. doi: 10.2519/jospt.2018.8023. [DOI] [PubMed] [Google Scholar]
- 21.Moore J.L., Potter K., Blankshain K., Kaplan S.L., O'Dwyer L.C., Sullivan J.E. A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation: a clinical practice guideline. J Neurol Phys Ther. 2018;42:174–220. doi: 10.1097/NPT.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duncan P.W., Sullivan K.J., Behrman A.L. Body-weight–supported treadmill rehabilitation after stroke. N Engl J Med. 2011;364:2026–2036. doi: 10.1056/NEJMoa1010790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duncan P.W., Sullivan K.J., Behrman A.L. Protocol for the Locomotor Experience Applied Post-stroke (LEAPS) trial: a randomized controlled trial. BMC Neurol. 2007;7:39. doi: 10.1186/1471-2377-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Linacre J.M. Rasch power analysis: size vs. significance: standardized chi-square fit statistic. Rasch Measurement Transactions. 2003;17:918. [Google Scholar]
- 25.Reeve B.B., Hays R.D., Bjorner J.B. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Med Care. 2007;45(5 Suppl 1):S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 26.Wright B.D., Linacre J.M. Reasonable mean-square fit values. Rasch Measurement Transactions. 1994;8:370. [Google Scholar]
- 27.Lim C.R., Harris K., Dawson J., Beard D.J., Fitzpatrick R., Price A.J. Floor and ceiling effects in the OHS: an analysis of the NHS PROMs data set. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-007765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright B.D., Masters G.N. Number of person or item strata: (4*separation + 1)/3. Rasch Measurement Transactions. 2002;16:888. [Google Scholar]
- 29.Lohnes C.A., Earhart G.M. External validation of abbreviated versions of the activities-specific balance confidence scale in Parkinson’s disease. Mov Disord. 2010;25:485–489. doi: 10.1002/mds.22924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oude Nijhuis L.B., Arends S., Borm G.F., Visser J.E., Bloem B.R. Balance confidence in Parkinson’s disease. Mov Disord. 2007;22:2450–2451. doi: 10.1002/mds.21756. [DOI] [PubMed] [Google Scholar]
- 31.Peretz C., Herman T., Hausdorff J.M., Giladi N. Assessing fear of falling: can a short version of the Activities-specific Balance Confidence scale be useful? Mov Disord. 2006;21:2101–2105. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- 32.Wolfe E.W., Smith E.V., Jr. Instrument development tools and activities for measure validation using Rasch models: part II--validation activities. J Appl Meas. 2007;8:204–234. [PubMed] [Google Scholar]
- 33.Jette D.U., Halbert J., Iverson C., Miceli E., Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89:125–135. doi: 10.2522/ptj.20080234. [DOI] [PubMed] [Google Scholar]
- 34.Stevens J.G., Beurskens A.J. Implementation of measurement instruments in physical therapist practice: development of a tailored strategy. Phys Ther. 2010;90:953–961. doi: 10.2522/ptj.20090105. [DOI] [PubMed] [Google Scholar]