ABSTRACT
Objectives: Tinnitus is the perception of sound without any external auditory stimulus. Cervicogenic somatic tinnitus (CST) is a subset in which symptoms are modulated by maneuvers of the neck. The evidence for effective diagnosis and treatment of CST is limited. Mechanical Diagnosis and Therapy (MDT) is a biopsychosocial assessment and management system that uses the response to mechanical forces to classify clinical presentations accurately. The purpose of this case report is to describe the MDT assessment and management of a patient with chronic subjective tinnitus.
Methods: A 67-year-old female with a 5-year history of left-sided subjective tinnitus, neck pain, and headache was referred for physiotherapy. Outcome measures included the Visual Analogue Scale (VAS), Tinnitus Handicap Inventory (THI), and Neck Disability Index (NDI). She was evaluated and treated according to MDT principles with management consisting of individualized directional preference exercises and postural correction.
Results: Significant improvements in symptoms, cervical range of motion, function, and psychosocial status were observed over the long-term. At 6 months, THI scores dropped from 62/100 to 18/100 and NDI scores dropped from 18/50 to 3/50.
Discussion: A comprehensive MDT assessment led to a classification of Derangement, with treatment focusing on tailored self-management. Contrary to other interventions described for CST, the patient was able to make significant and lasting changes to her symptoms without the need for any externally applied interventions. The emphasis on self-management dovetails well with the biopsychosocial model of care. This case provides preliminary evidence for the utility of screening for Derangement in conservative tinnitus assessments.
Level of Evidence: 4
KEYWORDS: Tinnitus, mechanical diagnosis and therapy, MDT, derangement, directional preference
Background
Tinnitus is described as the conscious perception of sound in the absence of an external auditory stimulus. Its prevalence ranges between 10 to 15% in adult populations [1]. Symptoms may vary widely with regards to pitch, intensity, type and number of sounds, spatial localization, and temporal pattern [2]. It is often associated with other aural symptoms, such as hearing loss, hyperacusis, and phonophobia [3]. Subjective tinnitus, which is experienced by the individual alone, is more common than the objective type, which is perceptible by another observer [1]. It can be accompanied by significant comorbidities such as insomnia, depression, and anxiety [4,5], and can have severe consequences for quality of life [6].
Tinnitus is considered to have multiple etiologies. It can be caused or worsened by hearing loss, acoustic trauma, ototoxic drug use, infections, and psychological stress [7]. A subset of tinnitus exists in which the somatosensory system of the upper extremities, jaw, or neck is related to symptoms [8]. A frequently reported characteristic of this group is the ability to modulate symptoms in terms of pitch or loudness with active movements or muscular contractions of the head, neck, and jaw [7,9–16]. It is referred to as Cervicogenic Somatic Tinnitus (CST) when symptoms are specifically modulated by maneuvers of the cervical spine [17].
There have been conflicting diagnostic criteria reported in the literature for CST [2,16,18]. Michiels et al. [19] diagnosed patients with CST if they reported temporal coincidence of neck pain and tinnitus symptoms [16], and then evaluated the prevalence of cervical spine dysfunction in these patients. Although it was significantly more prevalent in CST (47-81% across 4 tests) than non-CST patients, it was still common in the latter (10-50%) [19]. This is perhaps unsurprising, as basing CST diagnosis on one historical criterion is problematic; a recent Delphi study on the diagnostic criteria of somatosensory tinnitus [20] identified more than 15 historical or physical factors that imply a somatosensory influence on symptoms. Furthermore, tinnitus symptoms were equally modifiable by cervical maneuvers in both the CST and non-CST group, and only 68% of CST population had limited cervical range of motion [19]. Taken together, these findings suggest that the utility of clinical diagnostic tools is insufficient.
Evidence to support treatment options for CST is limited. Interventions have been described in case reports, cohort studies, and randomized controlled trials with various rationales, including targeting cervical misalignment and range of motion with manipulation and/or exercise [20–24], normalizing cervical muscle function through stretching or repeated contraction [14,25], and deactivation of trigger points by stretching or pressure release [26]. CST appears to be a syndrome with complex and varying presentations; therefore, the narrow approach of these treatment strategies may be limited in their applicability to individual patients. A systematic and individualized approach to the evaluation and management of CST is necessary.
Mechanical Diagnosis and Therapy (MDT) is a biopsychosocial classification system that is widely used in assessing and managing neck pain and cervicogenic headache [27,28]. Clinicians use MDT to evaluate a patient’s symptomatic and mechanical response to loading strategies in order to accurately classify their presentation. The fact that tinnitus symptoms can be modulated by certain head or neck movements [10–16] indicates a possible role for MDT in assessing and treating this population.
The purpose of this case report is to describe the evaluation, treatment, and outcomes of a patient with chronic subjective tinnitus using MDT assessment and management principles.
Case description
History
A 67-year-old French-speaking female was evaluated and treated in an outpatient physiotherapy clinic by a Certified MDT physiotherapist (DW). She gave her written consent for this case report. She was referred by her family physician after finding information online regarding the link between the cervical spine and tinnitus, and the possible role of physiotherapy in ameliorating symptoms. She presented with a five-year history of subjective tinnitus in her left ear. It had an insidious onset and a progressive course, initially presenting as an intermittent whistling sound. The intensity increased and became constant after two ear infections in the previous two years. Other sounds began to appear, including high-pitched buzzing, hissing, and mechanical knocking. At its worst, she was able to discern up to five different noises simultaneously, and sometimes it would also be present in the right ear. She had three episodes of symptoms attributed to Meniere’s disease within the previous year, lasting about six hours each, during which she had severe vertigo, vomiting, and difficulty standing up. The tinnitus symptoms were more prominent during and after these attacks.
She described her current tinnitus as a continuous whistling with a pulsatile ‘chou-chou’ sound. It worsened with fatigue, stress, and through exposure to strong ambient noise. It improved with relaxation and neck massage. She noticed it disappeared temporarily when she turned her head to the left and lifted her arms overhead. Other associated symptoms included left-sided hearing loss and a sensation of blockage. She also complained of frequent headaches as well as pressure and tension in her neck, which were quite severe in the previous two months. She had a dental prosthesis but denied any pain in her jaws.
The tinnitus caused her significant functional impairment and psychosocial stress. Hearing the television and speech was problematic, with resulting comprehension difficulty during conversations. She struggled to concentrate, read, and had stopped knitting. Falling asleep was troublesome and she reported waking up about three times per night, and so was easily fatigable. Certain sounds, such as police sirens, were intolerable, and she had to stop attending the cinema and concerts, which she had previously enjoyed. She sometimes felt frustrated and desperate, as she felt she had no control over the tinnitus and could not escape from it. Moreover, she reported at times feeling anxious, depressed, insecure, and irritable; the problem had placed stress on her personal relationships.
Her past medical history included atrial fibrillation and hypothyroidism, for which she was taking prophylactic aspirin and Synthroid, respectively. She had no history of head injury or any surgery involving the head or ear and had never taken any ototoxic medications. She had never worked anywhere with significant ambient noise and denied having any noisy hobbies or activities. She had seen an optometrist to exclude any vision changes that might be related to her headaches. She attended eight sessions of acupuncture and two sessions of massage therapy with only temporary relief of symptoms.
An MRI showed no pathology of her internal auditory canal, mastoid, and cranial nerves VII and VIII. Audiogram tests revealed neurosensory hearing loss in her left ear, with 20% discrimination of monosyllables. A cervical X-ray displayed a discrete anterolisthesis of C4/C5 and C5/C6, likely related to facet arthrosis, and mild C6-7 disc narrowing with osteophytic proliferation and uncarthrosis, which moderately reduced left foraminal space.
Outcome measures
The intensity of the tinnitus fluctuated from 3-8/10 on the Visual Analogue Scale (VAS), which is a valid and reliable instrument for measuring tinnitus loudness [29]. The Tinnitus Handicap Inventory (THI) and the Neck Disability Index (NDI) were used as functional outcome measures. Both have demonstrated good reliability and have been validated in French [30,31]. The THI is a 25-item questionnaire that assesses the deficits in function, emotion, and the catastrophic responses of tinnitus [32]. Its score ranges from 0 to 100 with a minimal detectable change of 20 points [32]. Her initial score was 62/100, indicating ‘Severe’ disability. The NDI is a 10-item questionnaire that assesses both physical and mental health related to cervical pain [33,34]. Its score ranges from 0 to 50 [34] with a minimal detectable change of 10.5 points [35]. Her initial score was 18/50, indicating ‘Moderate’ disability.
Examination and clinical impression
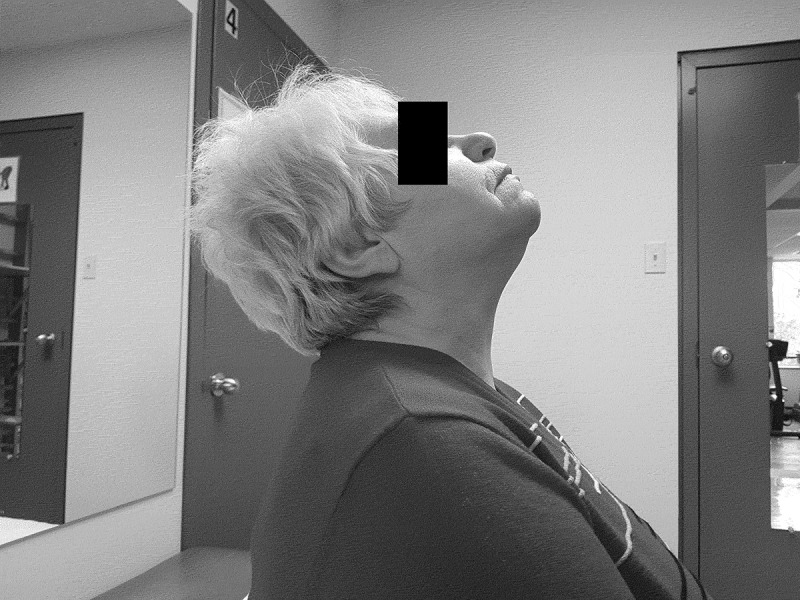
Upon examination, the patient reported her tinnitus severity was 8/10 and her headache symptoms were 5/10 at rest in sitting. Correction of her resting position from a forward head posture to upright sitting immediately decreased her tinnitus intensity. Range of motion (ROM) assessment of her cervical spine showed a painful, moderate loss of left rotation and left lateral flexion, and minimal losses in all other directions. Protrusion increased her headache, while retraction decreased both the headache and tinnitus. Supine lying further decreased her tinnitus, and after performing 15 repetitions of retraction in this position (Figure 1), her tinnitus and headache severity decreased to 6/10 and 3/10, respectively. Additionally, left lateral flexion and rotation increased in range. A provisional classification of cervical Derangement with a Directional Preference of retraction was made. She was instructed to perform 10–15 repetitions of retraction in lying every one to two hours, and to maintain a more upright sitting posture with a lumbar roll.
Figure 1.

Retraction in lying.
Treatment and follow-up
One week later, reporting full adherence with the management plan, she described a 40% improvement overall. Her tinnitus had decreased to 5/10 in severity and the pulsatile ‘chou-chou’ noise was less annoying. She had been headache-free for a week and sleep quality had improved. She had significantly less neck stiffness; ROM assessment exhibited minimal loss of left rotation and extension, with full flexion and right rotation. She was instructed to continue with her existing program due to ongoing symptomatic and mechanical improvement.
At follow-up a week later, she reported that for the preceding 4 days she experienced nasal congestion, cough, and difficulty breathing secondary to bronchitis. Because of this she had difficulty lying down and so had to stop her exercises for 2 days. Her tinnitus severity was 10/10, accompanied by pulsatile ‘chou-chou’, knocking, and buzzing sounds. There was a moderate loss of cervical extension and left rotation, with a minimal loss of right rotation. Retraction in sitting was introduced in lieu of lying (Figure 2). After performing 10 repetitions, her tinnitus severity had decreased. She was instructed to perform these exercises, instead of in lying, every 1–2 hours.
Figure 2.

Retraction in sitting.
Two weeks later, her bronchitis was abating, and she was approximately 90% adherent with her new exercises. Her sleep quality had improved. She reported her daytime tinnitus averaged 7/10 in severity, but at night it was still 10/10, and she described this as a pulsatile knocking. Physical examination revealed a moderate loss of extension and minimal loss of left rotation. A progression of her existing exercise was tested into further range. Cervical retraction followed by extension (Figure 3) significantly decreased the pulsatile knocking noise, from 7/10 to 1/10. Ten repetitions of this abolished the pulsatile tinnitus; this was prescribed as her new home exercise program every 1–2 hours.
Figure 3.
Retraction-extension in sitting.
Outcomes
At six weeks post-evaluation, the patient was continuing to perform retraction-extension exercises at a 90% adherence rate and reported an 85-90% improvement overall. There was no pulsatile tinnitus, although there was a 7/10 whistling noise that persisted when she woke up. After performing the exercises, the intensity decreased to 4/10. During the day, she barely noticed the sound, and only heard it when there was total silence. She reported significant improvements in her mood and ability to sleep. She had not had neck pain for a week, and demonstrated full cervical flexion, lateral flexion, and rotation, with a minimal loss of extension. Her THI score had decreased to 22/100, and her NDI score to 5/50. One week later she had an audiogram done, which showed a slight improvement in the discrimination of monosyllables (20% to 40%) in her left ear compared to pre-physiotherapy treatment. She was asked to continue with the same home exercise program and would be followed up by phone.
At 6-month follow-up, she reported her tinnitus was well controlled. She described it as a continuous whistling sound that did not exceed 3/10 in severity and there was no pulsatile ‘chou-chou’ or knocking sounds. Her THI score had further decreased to 18/100, and her NDI score had decreased to 3/50. Overall, she reported significant symptomatic, functional, and psychosocial improvements compared to intake (Table 1). A recent audiogram displayed a slight decrease in the discrimination of monosyllables (24%) in her left ear. She saw a new specialist who diagnosed her with vestibular migraine, as opposed to Meniere’s disease, to explain her episodes of vertigo, vomiting, and difficulty standing up.
Table 1.
Summary of symptomatic, functional, and psychosocial issues reported at intake with 6-month outcomes.
| Reported Issues at Intake | 6 Month Outcome |
|---|---|
| Symptomatic | |
| Up to 5 noises simultaneously | 1 whistling sound only |
| 3-8/10 continuous tinnitus | Maximum 3/10, difficult to detect at times |
| Pulsatile quality | No pulsatile quality |
| Neck pressure and tension | No neck symptoms |
| Headaches | Improved headache symptoms |
| Dizziness episodes lasted 6 hours | Dizziness episodes lasted 20–120 minutes |
| Functional | |
| Difficulty hearing/comprehending speech | No difficulty hearing speech |
| Difficulty falling asleep, awakes 3 times/night | Able to sleep continuously without waking up |
| Easily fatigable | No longer fatigued |
| Difficulty concentrating/reading | Occasional difficulty concentrating/reading |
| Could not go to cinema/concerts | Did not go – fearful of getting worse |
| Psychosocial | |
| Frustrated and desperate | Occasional frustration, no longer desperate |
| No control over symptoms | Had control with regular exercise |
| Anxious, depressed, insecure, irritable | No longer anxious, depressed, or insecure |
| Stress on personal relationships | Symptoms did not put stress on relationships |
Discussion
This case outlines the evaluation and successful management of a patient presenting with chronic subjective tinnitus. Through the provision of a comprehensive MDT assessment and treatment, significant reductions in tinnitus, headache, and neck symptoms were noted, accompanied by mechanical, functional, and psychosocial improvements. At 6-month follow-up, her THI score had decreased 44 points and her NDI by 15 points compared to intake, far surpassing minimal detectable change thresholds for each instrument [32,35]. The pulsatile aspect of her tinnitus was abolished, and the severity decreased from a range of 3-8/10 to a maximum of 3/10. Notably, her audiogram demonstrated improvement in left-sided monosyllable discrimination at 6 weeks, although this had returned close to baseline at 6-month follow-up, possibly as a result of ongoing vestibular migraines. Because these results were observed in response to extension-based loading strategies of the cervical spine, she satisfied the criteria for a Directional Preference of extension and was thus classified as having a cervical Derangement [36].
These findings deviate somewhat with the responses reported for other tinnitus patients. The phenomenon of tinnitus modulation is well-documented, wherein somatic maneuvers of the head, neck, jaw, and upper extremity can affect tinnitus symptoms. However, these modulations have been found to either improve or worsen symptoms and are commonly transient in nature [2,7,8,16], as opposed to the long-term improvements observed in this case. It could be speculated that some patients who exhibit tinnitus modulation may in fact have an unrecognized Derangement, which requires end-range motion or positioning in a specific direction to bring about clinical improvement [36]. Indeed, our patient had transient relief with shoulder elevation and neck rotation, which in retrospect could be considered a historical clue that Derangement was likely.
The management plan for this patient was also a departure in comparison to CST treatment strategies reported in the literature. They include exercises and a range of passive interventions, such as manual mobilization, manipulation, auricular acupuncture, soft tissue massage, myofascial trigger point inactivation, injections, and electrical stimulation [8,16,21–24,37]. Cherian et al. [23] reported on a patient with tinnitus who improved with repeated movements of the neck and thoracic spine that were similar in part to those used here, but treatment also included soft tissue massage and trigger point release in addition to jaw exercises. Michiels et al. [19] recommended that CST be treated multimodally with mobilization/manipulation, mobility and stability exercises, and muscle relaxation. In contrast, the reduction in tinnitus symptoms observed here was uniquely elicited via the patient’s movements only, without the application of any external manual therapies or modalities. A strength of this approach is it allowed for clarification of the relationship between symptoms and intervention, due to the utilization of solely cervical extension-based treatments. These outcomes suggest that clinically important results could be similarly achieved in other CST patients if a Derangement is identified, and the multimodal treatment approach as outlined above [19] may be superfluous.
Thus, assessing for Derangement could be considered an important component of a thorough tinnitus assessment. Previous work has shown that Derangements can be reliably detected by appropriately trained MDT clinicians in both the spine and extremity [38–41]. McKenzie and May [36] have advocated for a thorough MDT assessment and management of the cervical and thoracic spines for patients with cervicogenic headache and dizziness, with the assertion that for some patients, symptoms will be responsive to spinal movements and/or positions. This idea can now be extended to patients with tinnitus, as to the authors’ knowledge, this is the first reported cervical Derangement with tinnitus as a responsive symptom. Given the ongoing dilemma of identifying CST [20] and the prominence of cervical dysfunction in those deemed not to have CST [19], assessing for Derangement could be a significant piece of the diagnostic puzzle. However, because the results of one case report are not necessarily generalizable to the clinical population of tinnitus as a whole, more expansive research studies should be conducted to investigate this idea in greater detail.
As exhibited in this case, the successful management for Derangement can commonly be achieved solely through self-management strategies [36], which aligns well with the biopsychosocial model of care [42,43]. By demonstrating to the patient that she was able to reduce her symptoms without any clinician-dependent intervention, she was given agency over her own problem. This was particularly poignant for someone who at intake reported distress due to no perceived control over her symptoms. Promotion of self-management can lead to improved self-efficacy and perceived controllability of symptoms, which have positive effects on pain and disability [42]. It is an essential part of management for persistent musculoskeletal disorders [43]; previously it has been shown that an episode of care with an MDT clinician leads to improved self-efficacy and self-management skills [44]. Additionally, by virtue of the focus on patient-generated movements, any potential side effects of external interventions were avoided.
At intake, the patient thoroughly described how her symptoms affected her psychosocial status. Interestingly, despite a lack of explicit psychosocial interventions, her status improved significantly as symptoms improved, as evidenced by her subjective report, THI, and NDI score improvements, the latter two of which capture some of the psychosocial domains affected by tinnitus and neck pain. This is consistent with previous work demonstrating that if psychosocial factors are present when the clinical diagnosis of Derangement is made, they often improve concomitantly with Derangement-specific management; overt psychosocial intervention is often unnecessary [45–48].
Conclusion
This case report details the successful reduction of tinnitus symptoms with concomitant improvement in function and psychosocial status through self-management exercises and posture correction according to an identified Directional Preference. The outcomes highlight the potential utility of screening for Derangement as part of a comprehensive tinnitus assessment. In addition, because the treatment of this condition is rooted in self-management, tinnitus patients who have a Derangement may not require passive, multimodal interventions to improve, maximizing self-efficacy and perceived control over symptoms. To the authors’ knowledge, this is the first report of Derangement in tinnitus, so its prevalence in this population is currently unknown. However, given that the tinnitus modulation phenomenon appears to be common, there is the possibility that it could be a frequent finding. Because of this, and the inherently limited evidence that can be garnered from a case report, further research on this topic with more robust study design is required for clarification.
Biographies
Di Wu obtained his medical degree at China Medical University in 2004. He completed an orthopaedic surgery residency at Beijing Tiantan Hospital and worked as an orthopaedic surgeon at Fuxin Central Hospital from 2007 to 2010. After emigrating to Canada, he attended McGill University and received his Master of Science in Physical Therapy in 2013. He is now a clinical physiotherapist at Physio Cabrini, Montreal and treats a variety of musculoskeletal conditions and pelvic disorders. He has an interest in musculoskeletal conditions’ impact on other medical conditions. As a Certified Mechanical Diagnosis and Therapy (MDT) therapist, Di has innovatively used MDT as a screening tool to rule out spinal sources of pelvic pain and dysfunction and has described this approach in a published case series.
David Ham graduated with a Master of Science in Physical Therapy from the University of Toronto in 2011. He is a clinical physiotherapist working in outpatient orthopaedics. He received the 2017 Phil Burchell MDT Diploma Scholarship in 2017 and obtained his Diploma in Mechanical Diagnosis and Therapy (Dip. MDT) in 2018. He is a Diploma Educator for the Theoretical Component of the McKenzie Institute International’s Diploma Program, co-teaching a module on Differential Diagnosis using MDT, and regularly assists on MDT courses presented to local clinicians.
Richard Rosedale graduated from Guy’s Hospital School of Physiotherapy (London, UK) in 1992. After emigrating to Canada, he completed his Diploma in Mechanical Diagnosis and Therapy (Dip. MDT) in 1997. He worked in orthopaedics and provided musculoskeletal care at London Health Sciences Centre, Ontario between 1993 and 2018. He has been active in research since 2007 and has authored or coauthored over a dozen papers, primarily exploring the clinical utility of MDT. He has been the Institute’s Reference Coordinator since 2015. Since 2003 Richard has been one of the McKenzie Institute’s teaching faculty, instructing clinicians internationally in the principles, application of MDT. He has served on and chaired the scientific committees of many McKenzie Institute Conferences and is a Diploma examiner. In 2005 Richard was appointed onto the Institute’s International Education Council. He has since been involved in numerous educational projects including the development of online learning courses and other core educational materials. Richard was the recipient of the McKenzie Institute's 2014 Bronze Lady Award for his outstanding contributions over many years to both MDT research and MDT education. In 2018 Richard was appointed as the McKenzie Institute’s International Director of Education and Diploma Coordinator.
Funding Statement
The authors have no funding details to disclose.
Disclosure statement
David Ham is contracted as a Diploma Educator with the McKenzie Institute International. Richard Rosedale is employed as the International Director of Education and an International Instructor for the McKenzie Institute International.
References
- [1].Baguley D, McFerran D, Hall D.. Tinnitus. Lancet. 2013;382:1600–1607. [DOI] [PubMed] [Google Scholar]
- [2].Levine RA, Oron Y. Tinnitus. Handb Clin Neurol. 2015;129:409–431. [DOI] [PubMed] [Google Scholar]
- [3].Langguth B, Kreuzer PM, Kleinjung T, et al. Tinnitus: causes and clinical management. Lancet Neurol. 2013;12:920–930. [DOI] [PubMed] [Google Scholar]
- [4].Zoger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2006;47(4):282–288. [DOI] [PubMed] [Google Scholar]
- [5].McKenna L, Hallam RS, Hinchcliffe R. The prevalence of psychological disturbance in neurotology outpatients. Clin Otolaryngol Allied Sci. 1991;16(5):452–456. [DOI] [PubMed] [Google Scholar]
- [6].Zeman F, Koller M, Langguth B, et al. Which tinnitus-related aspects are relevant for quality of life and depression: results from a large international multicentre sample. Health Qual Life Outcomes. 2014;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ralli M, Greco A, Turchetta R, et al. Somatosensory tinnitus: current evidence and future perspectives. J Int Med Res. 2017;45(3):933–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Haider HF, Hoare DJ, Costa RF, et al. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: a scoping review. Front Neurosci. 2017;11:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pinchoff RJ, Burkard RF, Salvi RJ, et al. Modulation of tinnitus by voluntary jaw movements. Otol Neurotol. 1998;19(6):785–789. [PubMed] [Google Scholar]
- [10].Levine RA. Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis. Am J Otolaryngol. 1999;20(6):351–362. [DOI] [PubMed] [Google Scholar]
- [11].Sanchez TG, Guerra GC, Lorenzi MC, et al. The influence of voluntary muscle contractions upon the onset and modulation of tinnitus. Audiol Neurootol. 2002;7(6):370–375. [DOI] [PubMed] [Google Scholar]
- [12].Levine RA, Abel M, Cheng H. CNS somatosensory-auditory interactions elicit or modulate tinnitus. Exp Brain Res. 2003;153(4):643–648. [DOI] [PubMed] [Google Scholar]
- [13].Abel MD, Levine RA. Muscle contractions and auditory perception in tinnitus patients and nonclinical subjects. Cranio. 2004;22(3):181–191. [DOI] [PubMed] [Google Scholar]
- [14].Sanchez TG, da Silva Lima A, Brandao AL, et al. Somatic modulation of tinnitus: test reliability and results after repetitive muscle contraction training. Ann Otol Rhinol Laryngol. 2007;116(1):30–35. [DOI] [PubMed] [Google Scholar]
- [15].Levine RA, Nam EC, Oron Y, et al. Evidence for a tinnitus subgroup responsive to somatosensory based treatment modalities. Prog Brain Res. 2007;166:195–207. [DOI] [PubMed] [Google Scholar]
- [16].Sanchez TG, Rocha CB. Diagnosis and management of somatosensory tinnitus: review article. Clinics (Sao Paulo). 2011;66(6):1089–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Michiels S, Van de Heyning P, Truijen S, et al. Diagnostic value of clinical cervical spine tests in patients with cervicogenic somatic tinnitus. Phys Ther. 2015;95(11):1529–1535. [DOI] [PubMed] [Google Scholar]
- [18].Oostendorp RA, Bakker I, Elvers H, et al. Cervicogenic somatosensory tinnitus: an indication for manual therapy? Part 1: theoretical concept. Man Ther. 2016;23:120–123. [DOI] [PubMed] [Google Scholar]
- [19].Michiels S, De Hertogh W, Truijen S, et al. Cervical spine dysfunctions in patients with chronic subjective tinnitus. Otol Neurotol. 2015;36(4):741–745. [DOI] [PubMed] [Google Scholar]
- [20].Michiels S, Sanchez TG, Oron Y, et al. Diagnostic criteria for somatosensory tinnitus: a Delphi process and face-to-face meeting to establish consensus. Trends Hear. 2018;22:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Alcantara J, Plaugher G, Klemp DD, et al. Chiropractic care of a patient with temporomandibular disorder and atlas subluxation. J Manipulative Physiol Ther. 2002;25(1):63–70. [DOI] [PubMed] [Google Scholar]
- [22].Kessinger RC, Boneva DV. Vertigo, tinnitus, and hearing loss in the geriatric patient. J Manipulative Physiol Ther. 2000;23(5):352–362. [PubMed] [Google Scholar]
- [23].Cherian K, Cherian N, Cook C, et al. Improving tinnitus with mechanical treatment of the cervical spine and jaw. J Am Acad Audiol. 2013;24(7):544–555. [DOI] [PubMed] [Google Scholar]
- [24].Michiels S, Van de Heyning P, Truijen S, et al. Does multi-modal cervical physical therapy improve tinnitus in patients with cervicogenic somatic tinnitus?. Man Ther. 2016;26:125–131. [DOI] [PubMed] [Google Scholar]
- [25].Bjorne A. Assessment of temporomandibular and cervical spine disorders in tinnitus patients. Prog Brain Res. 2007;166:215–219. [DOI] [PubMed] [Google Scholar]
- [26].Rocha CA, Sanchez TG. Myofascial trigger points: another way of modulating tinnitus. Prog Brain Res. 2007;166:209–214. [DOI] [PubMed] [Google Scholar]
- [27].Manca A, Dumville JC, Torgerson DJ, et al. Randomized trial of two physiotherapy interventions for primary care back and neck pain patients: cost effectiveness analysis. Rheumatology. 2007;46(9):1495–1501. [DOI] [PubMed] [Google Scholar]
- [28].Rose T, Butler J, Salinas N, et al. Measurement of outcomes for patients with centralising versus non-centralising neck pain. J Man Manip Ther. 2016;24(5):264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Adamchic I, Langguth B, Hauptmann C, et al. Psychometric evaluation of visual analog scale for the assessment of chronic tinnitus. Am J Audiol. 2012;21(2):215–225. [DOI] [PubMed] [Google Scholar]
- [30].Ghulyan-Bedikian V, Paolino M, Giorgetti-D’Esclercs F, et al. Psychometric properties of a French adaptation of the tinnitus handicap inventory. Encephale. 2010;36(5):390–396. [DOI] [PubMed] [Google Scholar]
- [31].Wlodyka-Demaille S, Poiraudeau S, Catanzariti JF, et al. French translation and validation of 3 functional disability scales for neck pain. Arch Phys Med Rehabil. 2002;83(3):376–382. [DOI] [PubMed] [Google Scholar]
- [32].Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the tinnitus handicap inventory (THI) for evaluating treatment outcome. J Am Acad Audiol. 1998;9(2):153–160. [PubMed] [Google Scholar]
- [33].Ackelman BH, Lindgren U. Validity and reliability of a modified version of the neck disability index. J Rehabil Med. 2002;34(6):284–287. [DOI] [PubMed] [Google Scholar]
- [34].Cleland JA, Fritz JM, Whitman JM, et al. The reliability and construct validity of the neck disability index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31(5):598–602. [DOI] [PubMed] [Google Scholar]
- [35].Pool JJ, Ostelo RW, Hoving JL, et al. Minimal clinically important change of the neck disability index and the Numerical pain rating scale for patients with neck pain. Spine (Phila Pa 1976). 2007;32(26):3047–3051. [DOI] [PubMed] [Google Scholar]
- [36].McKenzie R, May S. The cervical & thoracic spine: mechanical diagnosis & therapy. 2nd ed. Raumati Beach (NZ): Spinal Publications New Zealand Ltd; 2006. [Google Scholar]
- [37].Latifpour DH, Grenner J, Sjodahl C. The effect of a new treatment based on somatosensory stimulation in a group of patients with somatically related tinnitus. Int Tinnitus J. 2009;15(1):94–99. [PubMed] [Google Scholar]
- [38].Razmjou H, Kramer JF, Yamada R. Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. J Orthop Sports Phys Ther. 2000;30(7):368–383. [DOI] [PubMed] [Google Scholar]
- [39].Kilpikoski S, Airaksinen O, Kankaanpaa M, et al. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine (Phila Pa 1976). 2002;27(8):E207–E214. [DOI] [PubMed] [Google Scholar]
- [40].Clare HA, Adams R, Maher CG. Reliability of McKenzie classification of patients with cervical or lumbar pain. J Manipulative Physiol Ther. 2005;28(2):122–127. [DOI] [PubMed] [Google Scholar]
- [41].Takasaki H, Okuyama K, Rosedale R. Inter-examiner classification reliability of mechanical diagnosis and therapy for extremity problems – systematic review. Musculoskelet Sci Pract. 2017;27:78–84. [DOI] [PubMed] [Google Scholar]
- [42].Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. [DOI] [PubMed] [Google Scholar]
- [43].Hutting N, Johnston V, Staal JB, et al. Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. J Orthop Sports Phys Ther. 2019;49(4):212–215. [DOI] [PubMed] [Google Scholar]
- [44].Takasaki H. Mechanical diagnosis and therapy enhances attitude toward self-management in people with musculoskeletal disorders: A preliminary evidence with a before-after design. SAGE Open Med. 2017;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Werneke MW, Hart DL, George SZ, et al. Clinical outcomes for patients classified by fear-avoidance beliefs and centralization phenomenon. Arch Phys Med Rehabil. 2009;90(5):768–777. [DOI] [PubMed] [Google Scholar]
- [46].Edmond SL, Werneke MW, Hart DL. Association between centralization, depression, somatization, and disability among patients with nonspecific low back pain. J Orthop Sports Phys Ther. 2010;40(12):801–810. [DOI] [PubMed] [Google Scholar]
- [47].Werneke MW, Edmond S, Young M, et al. Directional preference and functional outcomes among subjects classified at high psychosocial risk using STarT. Physiother Res Int. 2018;23:e1711. [DOI] [PubMed] [Google Scholar]
- [48].Edmond SL, Werneke MW, Young M, et al. Directional preference, cognitive behavioural interventions, and outcomes among patients with chronic low back pain. Physiother Res Int. 2019. [cited 2019 June16];9. DOI: 10.1002/pri.1773. [DOI] [PubMed] [Google Scholar]


