We describe barriers to clinical care and research participation unique to transgender and gender nonbinary people and offer concrete suggestions for creating more inclusive environments.
Abstract
We aim to make evident that solely referencing cisgender women in the context of sexual and reproductive health—particularly pregnancy planning and care—excludes a diverse group of transgender and gender nonbinary people who have sexual and reproductive health needs and experiences that can be similar to but also unique from those of cisgender women. We call on clinicians and researchers to ensure that all points of sexual and reproductive health access, research, sources of information, and care delivery comprehensively include and are accessible to people of all genders. We describe barriers to sexual and reproductive health care and research participation unique to people of marginalized gender identities, provide examples of harm resulting from these barriers, and offer concrete suggestions for creating inclusive, accurate, and respectful care and research environments—which will lead to higher quality health care and science for people of all genders.
Pregnancy—as well as contraception, abortion, prenatal care, birth, postpartum care, chestfeeding or breastfeeding, and childrearing—are often presented as experiences of cisgender women. Cisgender is a term that describes a person whose current gender identity is consistent with the gender identity generally assumed for the sex they were designated or assigned at birth, which is typically based on external genitalia. For example, a cisgender woman is a person who identifies as a woman and was assigned female sex at birth (ie, the sex listed on their birth certificate). Yet, people of many genders—women, men, genderqueer, nonbinary, and more—can and do carry pregnancies.1,2 We, the authors of this commentary, are sexual and reproductive health advocates, counselors, health-care providers, and researchers with a range of identities, including those who are transgender and gender nonbinary. Transgender is an umbrella term for people whose gender identity differs from the gender identity generally assumed for the sex they were assigned at birth. People with nonbinary genders have gender identities that do not fit exclusively into the binary categories of woman or man. For example, some nonbinary people have a gender that blends elements of being a man or a woman, and some nonbinary people do not identify with any gender. Some people's gender changes over time (genderfluid). People whose gender is not that of a woman or man may use many different terms to describe themselves, with nonbinary being one of the most common. Other terms include agender, bigender, genderqueer, and more. None of these terms are identical or synonymous—but all speak to an experience of gender that is not just that of a man or woman exclusively.3
We aim to make evident that solely referencing cisgender women (or cisgender men) in the context of sexual and reproductive health—particularly pregnancy planning and care—excludes a diverse group of people who have sexual and reproductive health needs and experiences that are both similar to and unique from those of cisgender people.4 This exclusion prevents the advancement of science and clinical care for people of all genders, including cisgender women. We call on clinicians and researchers to ensure that all points of sexual and reproductive health access, sources of information, and care delivery comprehensively include and are accessible to people of all genders.
We describe harms imposed by a narrow focus on cisgender women in clinical and research settings. We also provide specific and concrete suggestions for how to be inclusive, accurate, and effective in our work to achieve gender justice and improve health care for all.
BARRIERS TO SEXUAL AND REPRODUCTIVE HEALTH FOR TRANSGENDER AND NONBINARY PEOPLE
An estimated 1–1.4 million adults (0.4–0.6% of the adult population) in the United States are transgender,5,6 although this number is almost certainly an underestimate.6,7 Population proportions may be substantially higher among the next generation; for instance, a study from the GLAAD Institute found that 12% of people aged 18–34 years in the United States identify as a gender other than cisgender.8 Yet, owing to inadequacies of existing research, there is much that we do not know about the sexual and reproductive health needs and experiences of transgender and gender nonbinary people. Gaps regarding transgender and gender nonbinary people's health and health care needs include contraceptive method preferences, the influence of gender-affirming hormone use9 on fertility, transgender and gender nonbinary people's desires for and experiences with pregnancy and experiences of abortion, and a range of other core sexual and reproductive health outcomes.10–13 The existing literature emphasizes that many transgender and gender nonbinary people do not seek needed health care as a result of experiences with discrimination and lower quality care related directly to gender identity.14 Transgender and gender nonbinary people are more likely than the general U.S. population to be uninsured, to experience discrimination and mistreatment in health care settings, and to be adversely affected by limited clinician knowledge or refusal to provide care.10,14–17 For sexual and reproductive health care, although much less is known than for general health care services, these barriers are compounded by the highly gendered environments in which people obtain health care related to contraception, abortion, pregnancy, and birth, among others—care that is widely conceptualized as “women's” health services.11,18 Similarly, equating gestational-related services with “women's” health marginalizes both transgender women who cannot (currently19) carry a pregnancy as well as cisgender women who by choice, congenital anomaly, infertility, or other process cannot or do not want to carry a pregnancy, and thereby reinforces the misguided notion that womanhood is inherently linked to the anatomic and functional capacity for pregnancy.
CONSEQUENCES OF EXCLUSIVE LANGUAGE AND ENVIRONMENTS IN SEXUAL AND REPRODUCTIVE HEALTH CLINICAL CARE
Although scarce formal documentation exists, powerful community testimony highlights the harms of gender-exclusive language (eg, “women's” health) and representation.20–23 This can be particularly pronounced in clinical care settings, such as obstetrician–gynecologist (ob-gyn) offices, family planning centers, and other sexual and reproductive health clinics. For example, entering a clinic where the sign advertises “Women's Health,” where the walls and chairs are pink, where images of only cisgender women hang in the waiting room and visit rooms, where instructional brochures use language relevant for cisgender women only, and where the patient restroom is labeled a “women's” restroom can be stigmatizing and isolating for a person who is not a woman.24 Similarly, experiences of mis-gendering by clinic staff, such as a clinic receptionist referring to a man as “Miss” or “she,” or the experience of being seen by a health care provider who is not knowledgeable about the provision of affirming sexual and reproductive health care for transgender and gender nonbinary patients25—or who outright refuses to provide care to transgender and gender nonbinary patients11—can traumatize patients and deter them from seeking future health care. Electronic medical records (EMRs) can complicate the issue by preventing even well-informed clinicians from completing a patient's chart accurately simply because specific codes are inconsistent with someone's sex or gender as registered in the EMR.12,26 For instance, a clinician may find that the EMR does not display the appropriate checkboxes to document a prostate examination on a transgender woman who is registered as a woman, or that they are unable to complete charges for a man of transgender experience who is undergoing intrauterine device placement because this is inconsistent with the sex of his registration in the EMR (Fig. 1). Another challenge with some EMR systems is the electronic communication of laboratory values to patients as soon as they are available using laboratory “normal” ranges based on cisgender patients, meaning that a patient may see their result flagged as “abnormal” even when it is actually normal based on the medications or hormones the patient is taking or the surgeries they have had. Similar challenges arise with some health insurance plans that refuse to cover preventive sexual and reproductive health care (eg, Pap tests, contraceptive care, sexually transmitted infection screening) or pregnancy care for someone who has registered as a man on their insurance, even though the Affordable Care Act defines this as illegal under Section 1557.27
Fig. 1. Screenshot of electronic medical record system preventing intrauterine device removal and cervical examination for a patient because their registered sex is male. Epic Systems Corporation. Used with permission.
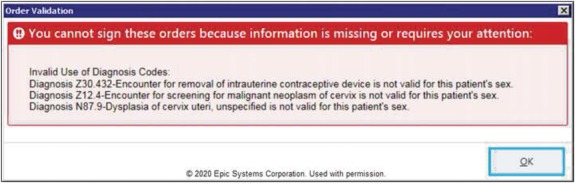
Moseson. Transgender and Gender Nonbinary Inclusion. Obstet Gynecol 2020.
Beyond deterring patients from seeking care, these factors can also negatively affect the quality of care received. For instance, in a health record in which a transgender man is registered as male, the EMR will not typically prompt the clinician to ensure that the patient is up to date on his Pap tests or present options to record an obstetric history; a transgender man or nonbinary patient may skip an intake form section marked “For women only,” omitting key information about reproductive history; or simply, a health care provider may skip questions on patient sexual history because they do not know what language to use and are afraid of being offensive.26 Research suggests that efforts toward incorporating transgender health into undergraduate and graduate medical educations are nascent. Such programs are sparse, with only 16% of Liaison Committee on Medical Education-accredited academic practices reporting a comprehensive LGBTQ competency training program; more than half (52%) report no LGBTQ training.28,29 Even when training is provided, it may not be of high quality.30 More specifically, a survey of ob-gyns in the United States found that only a third (or less) were comfortable providing care for transgender patients. Each of these realities (and others) additively acts to deter many transgender and gender nonbinary people from seeking sexual and reproductive health services. Further, they reduce the quality of care if obtained and lead to reluctance to seek future care, thereby reducing access to care for related sexual and reproductive health services, such as desired pregnancies, assisted reproductive techniques, and fertility preservation, and could increase the chance of sexually transmitted infections and unintended pregnancy, missed cancer screenings, and more.
CONSEQUENCES OF EXCLUSIVE LANGUAGE AND IMAGES IN SEXUAL AND REPRODUCTIVE HEALTH RESEARCH
The focus on cisgender women in sexual and reproductive health research has led to data that are either irrelevant to or inaccurate for those of us who are transgender and gender nonbinary. The limited data on the specific sexual and reproductive health needs and experiences of transgender and gender nonbinary people are fraught with misclassification bias owing to lack of specificity in defining terms, vague inclusion criteria, negation of the importance of gender self-identification, heteronormative assumptions about sex and reproduction, clinical and investigational selection bias, and legal or practical requirements for sterilization for gender affirmation. Conflation of language is common, with lack of distinction between “sex” (ie, the classification of people as male, female, intersex, or another sex based on a combination of genital anatomy, hormones, and chromosomes) compared with “gender” (ie, one's internal sense of being a man, woman, neither of these, both, or another gender[s]), despite different meanings and implications. Incomplete or vague eligibility criteria lead to study samples that systematically exclude portions of the target population; for instance, studies on pregnancy experiences recruiting women only, thereby excluding pregnant transgender and gender nonbinary people from the study. Relatedly, many examples exist of researchers misclassifying people in ways that do not reflect their gender identity (eg, erroneously including transgender women in research about men who have sex with men5), which undermines the identity of research participants and also the inferences that can be derived from study findings. Heteronormative assumptions about sexual activity and pregnancy desires underpin many of these research blind spots, such as the assumption that only cisgender women who are straight or bisexual can get pregnant or would want to be pregnant, when, in fact, that does not capture the diversity of experiences that occur. Further, the historical and current intersection between research and gatekeeping (eg, research being conducted by health care providers who also control patients' access to gender-affirming treatment), as well as requirements that transgender people be surgically sterilized to be legally recognized in their gender,31,32further contribute to inaccuracies and bias in sexual and reproductive health research by inducing selection bias in both who can and who does present for care.
Whether the invisibility of transgender and gender nonbinary experiences in sexual and reproductive health research is the result of study design and analysis practices that lack consideration of transgender and gender nonbinary experiences or of transgender and gender nonbinary people choosing not to participate in research because of a long history of discrimination and mistreatment, the result is the same—selection bias and invisibility about the needs of transgender and gender nonbinary people. As a result, most existing sexual and reproductive health research cannot be used to inform clinical or public health practice improvements for transgender and gender nonbinary people because the data simply have not been collected. One example of this is in the Behavioral Risk Factor Surveillance System, a national system of health-related telephone surveys conducted in the United States. The Behavioral Risk Factor Surveillance System asks for “sex” as well as “gender identity” but does not provide a definition of “sex” and asks questions about preconception health and family planning only to respondents who report their sex as female. Yet, in 2017 for instance, potentially owing to the lack of clarity in definitions of “sex” and “gender,” our analyses of Behavioral Risk Factor Surveillance System data indicated that 77 transgender men reported their sex as male and 139 transgender women reported their sex as female.33 This means that, in this one dataset, at least 139 people who could never have gotten pregnant were asked questions about contraception and 77 people who may or may not have the capability to become pregnant were not asked these questions. Similarly, another analysis found that up to 29.6% of BRFSS respondents are misclassified by sex assigned at birth in the 2014–2016 datasets.34 This misclassification bias leads to issues with data quality and accuracy and inferential errors that researchers and others draw from study data. Further, the lack of inclusion of transgender and gender nonbinary people in much sexual and reproductive health research limits the advancement of reproductive medicine. For instance, in the small but growing body of research in which transgender and gender nonbinary patients have been included, we are learning about the effect of testosterone on ovarian function, puberty, bone health, and sex drive, as well as other biological and pathologic processes.35–39 Broader inclusion in research could open up new understandings of medicine for people of all genders.
SUGGESTIONS FOR INCLUSIVITY IN SEXUAL AND REPRODUCTIVE HEALTH CARE AND RESEARCH
Regardless of context, there are almost always simple, direct ways of shifting our language and environments of care and research to be inclusive—subtle changes that may carry much significance for people's experiences with sexual and reproductive health care. Based on a nascent and growing literature on the needs and preferences of transgender and gender nonbinary populations with regard to sexual and reproductive health care,10,11,19 and personal experiences as researchers, clinicians, and members of the transgender and gender nonbinary community, we offer this set of context-specific suggestions to facilitate a shift in our field toward inclusion. In particular, we focus on two settings: clinical care and research.
CLINICAL CARE
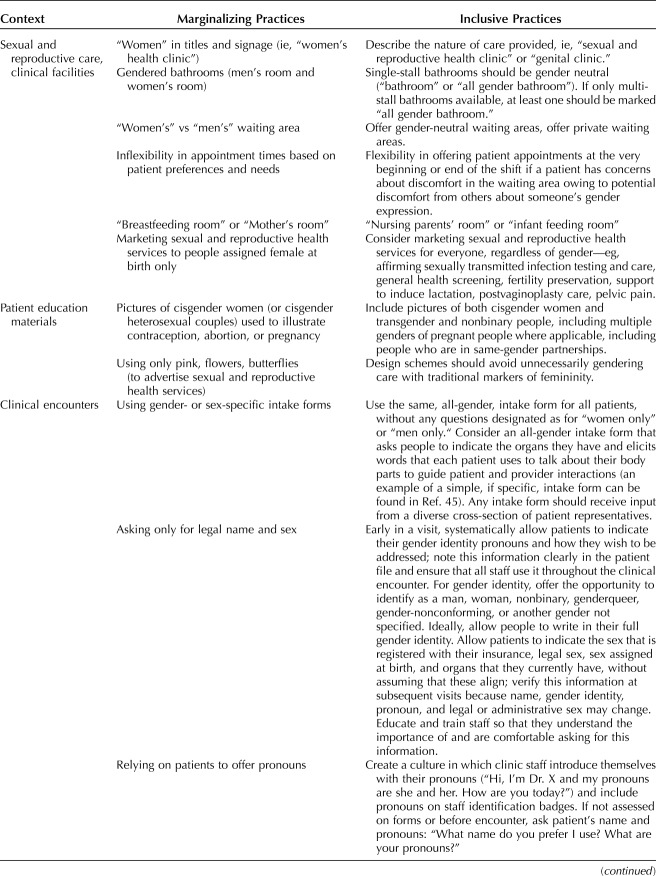
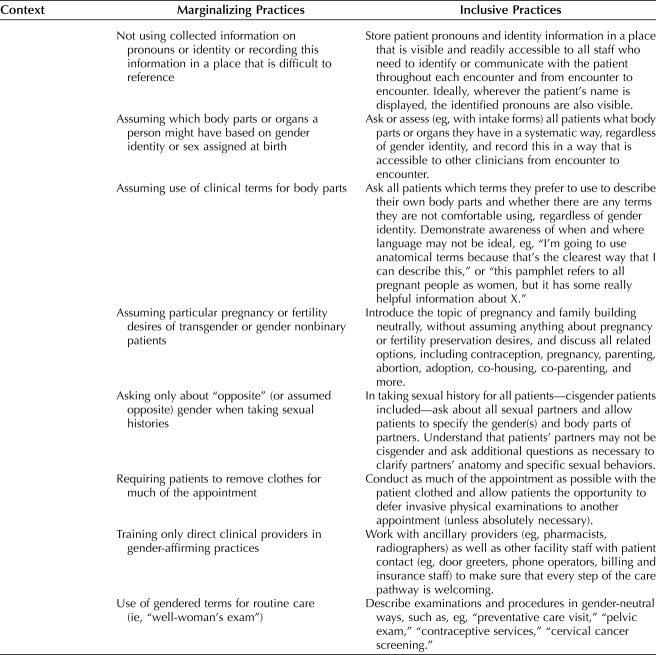
It is essential that health care providers and staff communicate information clearly while also prioritizing and being flexible to the unique needs of each individual patient. To achieve this balance, we have identified best practices to make gender-affirming care the norm for patients of all genders (Table 1). We group these recommendations according to physical aspects of care facilities (signage, services provided), patient informational materials and intake forms, and interactions between staff and patients. Our recommendations build off of guidance provided by clinicians who specialize in the care of transgender and gender nonbinary patients,11–13,18 and we broaden our recommendations for clinical encounters with patients of all genders.
Table 1.
Recommendations for Building Gender-Inclusive Clinical Settings
RESEARCH SETTING
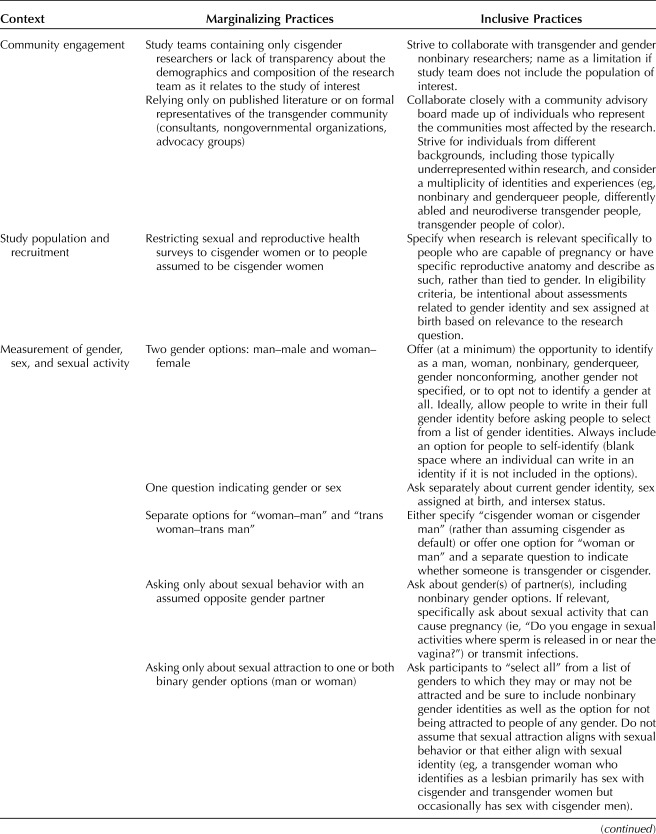
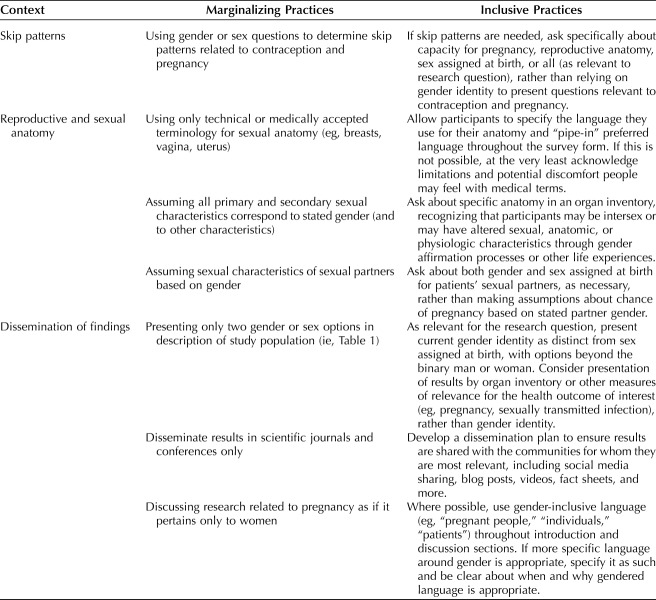
Specificity and precision in language are essential to conducting high-quality research and to communicating results clearly. Although some have argued that expanding the focus beyond cisgender women in sexual and reproductive health research may confuse people,41 or generalize the research to an extent that it is difficult to understand, we disagree. Failing to clearly articulate the relevant study population for a given research question in terms of gender identity, sex assigned at birth, hormonal milieu, or current organs can restrict (or broaden) the sample population unnecessarily, leading to the systematic exclusion of certain populations from research and complicating our ability to understand whether and to whom research results apply. Further, most widely used or validated measures of sexual and reproductive health experiences are laden with heteronormative, cisnormative assumptions about the types of sex people are having42,43; the gender, sex assigned at birth, and current organs of people's partners; and their capacity for pregnancy. These assumptions bias the questions and, consequently, the data that they collect. We make recommendations for how researchers can more appropriately consider and define the relevant study population for a given research question (in terms of gender identity and sex assigned at birth); develop and field more inclusive, relevant, and precise research measures; report and disseminate findings with more thought and nuance in relation to gender and sex; and involve transgender and gender nonbinary individuals at each step of the process, including on the research team itself (Table 2).
Table 2.
Recommendations for Conducting Gender-Inclusive Research
CONCLUSION
Clinical care and research are closely linked; questions that arise in clinical care motivate much research, and research subsequently informs changes and innovations in clinical care. If people are left out of either space, they are left out of both. In this commentary, we have endeavored to highlight key barriers to inclusion of transgender and gender nonbinary people in sexual and reproductive health care and research and to provide suggestions for addressing these barriers. We have by no means covered all barriers and, indeed, know that more is needed to understand barriers faced by more vulnerable and differently resourced communities within the larger transgender and gender nonbinary umbrella, including barriers specific to youth and adolescents, such as parental involvement and consent, coming out or disclosure to parents, and more, as well as barriers unique to transgender and gender nonbinary people of color, people with disabilities, and people who do not speak English.
Language reflects and reinforces our attitudes. When we evaluate our language, we examine more deeply the assumptions that frame our work. Changing the language we use and the environments in which we work is necessary for greater inclusion and quality, but it is not an all-encompassing solution. Rather, it is the first of many crucial steps needed to move us toward greater inclusivity, kindness, and, ultimately, higher quality clinical care and research for people of all genders. We hope this commentary contributes to shifting the paradigm of sexual and reproductive health clinical care and research toward this vision of comprehensive inclusion and high-quality health care for all.
Footnotes
Time spent on this commentary was funded by a grant from the Society for Family Planning (no.: SFPRF11-II1, PI: HM). Juno Obedin-Maliver was partially supported by grant K12DK111028 from the National Institute of Diabetes, Digestive, and Kidney Disorders, and by Stanford University School of Medicine.
Financial Disclosure Heidi Moseson, Mary Durden, and Laura Fix report financial support from a Society of Family Planning grant. Eli Goldberg reports receiving funds from Ibis Reproductive Health. They are a Board member, Planned Parenthood of Northern New England. Jen Hastings reports being paid a stipend from Ibis Reproductive Health from the Society for Family Planning funding that supported this study. Lyndon Cudlitz, Bori Lesser-Lee, Laz Letcher, and Aneidys Reyes report receiving funding from Ibis Reproductive Health. Juno Obedin-Maliver reports receiving funds from Sage Therapeutics, Ibis Reproductive Health, and Hims Inc. The other authors did not report any potential conflicts of interest.
This work was not conducted under the auspices of the Guttmacher Institute. The views expressed herein are those of the authors and do not necessarily reflect the views of the Guttmacher Institute.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B813.
REFERENCES
- 1.Light A, Obedin-Maliver J, Sevelius J, Kerns J. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstetrics Gynecol 2014;124:1120–7. [DOI] [PubMed] [Google Scholar]
- 2.Beatie T. Labor of love: is society ready for a pregnant male? Advocate, March 14, 2008.
- 3.National Center for Transgender Equality. Understanding non-binary people: how to be respectful and supportive. Available at: https://transequality.org/issues/resources/understanding-non-binary-people-how-to-be-respectful-and-supportive. Retrieved November 1, 2019.
- 4.Light A, Obedin-Maliver J. Opening the ob/gyn door for sexual and gender minority patients. Contemporary OB/GYN, January 15, 2019.
- 5.Sevelius JM, Keatley J, Calma N, Arnold E. “I am not a man”: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health 2016;11:1060–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health 2017;107:e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacCarthy S, Reisner S, Nunn A, Perez-Brumer A, Operario D. The time is now: attention increases to transgender health in the United States but scientific knowledge gaps remain. LGBT Health 2015;2:287–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GLAAD. Accelerating acceptance 2017: a Harris poll survey of Americans' acceptance of LGBTQ people. Los Angeles (CA): GLAAD; 2017. [Google Scholar]
- 9.Deutsch M. Overview of gender-affirming treatments and procedures. Available at: https://transcare.ucsf.edu/guidelines/overview. Retrieved November 18, 2019.
- 10.Hoffkling A, Obedin-Maliver J, Sevelius J. From erasure to opportunity: a qualitative study of the experiences of transgender men around pregnancy and recommendations for providers. BMC Pregnancy Childbirth 2017;17:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Obedin-Maliver J. Time for OBGYNs to care for people of all genders. J Women's Health 2015;24:109–11. [DOI] [PubMed] [Google Scholar]
- 12.Hahn M, Sheran N, Weber S, Cohan D, Obedin-Maliver J. Providing patient-centered perinatal care for transgender men and gender-diverse individuals: a collaborative multidisciplinary team Approach. Obstet Gynecol 2019;134:959–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krempasky C, Harris M, Abern L, Grimstad F. Contraception across the transmasculine spectrum. Am J Obstet Gynecol 2019;222:134–43. [DOI] [PubMed] [Google Scholar]
- 14.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The report of the 2015 U.S. transgender survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 15.Kates J, Ranji U, Beamesderfer A, Salganicoff A, Dawson L. Health and access to care and coverage for lesbian, gay, bisexual, and transgender individuals in the U.S. Available at: http://files.kff.org/attachment/Issue-Brief-Health-and-Access-to-Care-and-Coverage-for-LGBT-Individuals-in-the-US. Retrieved August 3, 2018. [Google Scholar]
- 16.Klein D, Berry-Bibee E, Keglovitz Baker K, Malcolm NM, Rollison JM, Frederiksen BN. Providing quality family planning services to LGBTQIA individuals: a systematic review. Contraception 2018;97:378–91. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez A, Agardh A, Asamoah B. Self-reported discrimination in health-care settings based on recognizability as transgender: a cross-sectional study among transgender U.S. citizens. Arch Sex Behav 2017;47:973–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stroumsa D, Wu JP. Welcoming transgender and nonbinary patients: expanding the language of “women's health.” Am J Obstet Gynecol 2018;219:585.e1–5. [DOI] [PubMed] [Google Scholar]
- 19.Jones B, Williams N, Saso S, Thum MY, Quiroga I, Yazbek J, et al. Uterine transplantation in transgender women. BJOG 2019;126:152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finlay J. Seahorse. Available at: https://seahorsefilm.com/. Retrieved January 26, 2020. [Google Scholar]
- 21.Barker J. A deal with the universe. Available at: https://www.imdb.com/title/tt8014038/. Retrieved January 26, 2020. [Google Scholar]
- 22.Huberdeau R. Transforming family. Available at: https://www.imdb.com/title/tt11171320/. Retrieved January 26, 2020. [Google Scholar]
- 23.Davis K. Southern comfort. Available at: https://www.imdb.com/title/tt0276515/. Retrieved January 26, 2020. [Google Scholar]
- 24.Reisner S, Perkovich B, Mimiaga M. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS 2010;24:501–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Unger CA. Care of the transgender patient: a survey of gynecologists' current knowledge and practice. J Women's Health 2015;24:114–8. [DOI] [PubMed] [Google Scholar]
- 26.Forsberg H. Practices, challenges and needs of healthcare providers doing contraceptive care for transmasculine and non-binary assigned female at birth patients. Pittsburgh (PA): American Public Health Association; 2019. [Google Scholar]
- 27.Department of Health and Human Services. Nondiscrimination in health programs and activities. 45 CFR Part 92; RIN 0945-AA02. Vol Section 1557 of the Affordable Care Act 2016.
- 28.Khalili J, Leung LB, Diamant AL. Finding the perfect doctor: identifying lesbian, gay, bisexual, and transgender-competent physicians. Am J Public Health 2015;105:1114–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dubin SN, Nolan IT, Streed CG, Jr, Greene RE, Radix AE, Morrison SD. Transgender health care: improving medical students' and residents' training and awareness. Adv Med Educ Pract 2018;9:377–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 2011;306:971–7. [DOI] [PubMed] [Google Scholar]
- 31.Mendez J. Report of the Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment. New York (NY): United Nations General Assembly; 2013. [Google Scholar]
- 32.The Associated Press. Japan's Supreme Court upholds transgender sterilization requirement. Associated Press, January 25, 2019. Available at: https://www.nbcnews.com/feature/nbc-out/japan-s-supreme-court-upholds-transgender-sterilization-requirement-n962721. Retrieved March 23, 2020. [Google Scholar]
- 33.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system: 2017 BRFSS survey data and documentation.Atlanta (GA): CDC; 2017. [Google Scholar]
- 34.Tordoff D, Andrasik M, Hajat A. Misclassification of sex assigned at birth in the behavioral risk factor surveillance system and transgender reproductive health: a quantitative bias analysis. Epidemiology 2019;30:669–78. [DOI] [PubMed] [Google Scholar]
- 35.Grynberg M, Fanchin R, Dubost G, Colau JC, Brémont-Weil C, Frydman R, et al. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod Biomed Online 2010;20:553–8. [DOI] [PubMed] [Google Scholar]
- 36.De Roo C, Lierman S, Tilleman K, Peynshaert K, Braeckmans K, Caanen M, et al. Ovarian tissue cryopreservation in female-to-male transgender people: insights into ovarian histology and physiology after prolonged androgen treatment. Reprod Biomed Online 2017;34:557–66. [DOI] [PubMed] [Google Scholar]
- 37.Schagen SE, Cohen-Kettenis PT, Delemarre-van de Waal HA, Hannema SE. Efficacy and safety of gonadotropin-releasing hormone agonist treatment to suppress puberty in gender dysphoric adolescents. J Sex Med 2016;13:1125–32. [DOI] [PubMed] [Google Scholar]
- 38.Chan KJ, Liang JJ, Jolly D, Weinand JD, Safer JD. Exogenous testosterone does not induce or exacerbate the metabolic features associated with PCOS among transgender men. Endocr Pract 2018;24:565–72. [DOI] [PubMed] [Google Scholar]
- 39.Wiepjes CM, de Jongh RT, de Blok CJ, Vlot MC, Lips P, Twisk JW, et al. Bone safety during the first ten years of gender-affirming hormonal treatment in transwomen and transmen. J Bone Miner Res 2019;34:447–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dadasovich R, Auerswald C, Minnis AM, Raymond HF, McFarland W, Wilson EC. Testosterone and sexual risk among transmen: a mixed methods exploratory study. Cult Health Sex 2017;19:256–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pollitt K. Who has abortions? The Nation, March 13, 2015. [Google Scholar]
- 42.Alpert AB, CichoskiKelly EM, Fox AD. What lesbian, gay, bisexual, transgender, queer, and intersex patients say doctors should know and do: a qualitative study. J Homosex 2017;64:1368–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sevelius J. “There's no pamphlet for the kind of sex I have”: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. J Assoc Nurses AIDS Care 2009;20:398–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pederson S. A new and inclusive intake form for diagnostic imaging departments. J Med Imag Radiation Sci 2018;49:371–5. [DOI] [PubMed] [Google Scholar]