Abstract
Introduction
We aimed to quantify health outcomes and programmatic implications of scaling up cervical cancer (CC) screening and treatment options for women living with HIV in care aged 18–65 in Kenya.
Methods
Mathematical model comparing from 2020 to 2040: (1) visual inspection with acetic acid (VIA) and cryotherapy (Cryo); (2) VIA and Cryo or loop excision electrical procedure (LEEP), as indicated; (3) human papillomavirus (HPV)-DNA testing and Cryo or LEEP; and (4) enhanced screening technologies (either same-day HPV-DNA testing or digitally enhanced VIA) and Cryo or LEEP. Outcomes measured were annual number of CC cases, deaths, screening and treatment interventions, and engaged in care (numbers screened, treated and cured) and five yearly age-standardised incidence.
Results
All options will reduce CC cases and deaths compared with no scale-up. Options 1–3 will perform similarly, averting approximately 28 000 (33%) CC cases and 7700 (27%) deaths. That is, VIA screening would yield minimal losses to follow-up (LTFU). Conversely, LTFU associated with HPV-DNA testing will yield a lower care engagement, despite better diagnostic performance. In contrast, option 4 would maximise health outcomes, averting 43 200 (50%) CC cases and 11 800 (40%) deaths, given greater care engagement. Yearly rescreening with either option will impose a substantial burden on the health system, which could be reduced by spacing out frequency to three yearly without undermining health gains.
Conclusions
Beyond the specific choice of technologies to scale up, efficiently using available options will drive programmatic success. Addressing practical constraints around diagnostics’ performance and LTFU will be key to effectively avert CC cases and deaths.
Keywords: HIV, screening, health systems, public health
Key questions.
What is already known?
Cervical cancer (CC) screening and treatment strategies have been shown to be cost-effective and life-saving.
Modelling studies to date have focused on the cost-effectiveness of CC screening and treatment options in hypothetical cohorts.
What are the new findings?
This is the first study to evaluate the potential population-level impact of CC screening and treatment interventions among women living with HIV (WHIV) in care by recreating the entire population of interest, including their demographic structure, their age and HIV-specific risk of human papillomavirus (HPV) disease progression and antiretroviral therapy initiation currently and over time.
Also for the first time, this study assesses the scale-up of a country’s CC screening and treatment guidelines and identifies how intervention factors (eg, diagnostic performance, losses to follow-up) will affect programmatic success.
What do the new findings imply?
Maximising health outcomes among WHIV in care in Kenya will rely more on the efficient use of available resources than on specific CC screening and treatment technologies.
A successful scale-up of HPV-DNA tests will require concerted efforts to minimise losses to follow-up (eg, single-visit, test-and-treat approach), while scaling up visual inspection methods will demand continuous provider training and technological improvements (eg, digitally enhanced imaging) to maximise its diagnostic performance.
Introduction
Cervical cancer (CC) remains a major cause of cancer-related morbidity and mortality among women globally, despite being largely preventable.1 Sub-Saharan Africa (SSA) has the highest CC incidence for a region in the world, likely due to both low coverage of preventative services and high prevalence of HIV.1 2 HIV is thought to increase the risk of acquiring cervical infection with human papillomavirus (HPV) and developing cancerous lesions.3 4
The WHO recently issued a call to eliminate CC.5 They advise countries to aim for at least 70% coverage with CC screening and treatment services, in order to achieve population-level health gains, with women living with HIV (WHIV) signalled as a key target population.5 6 Kenyan guidelines recommend screening WHIV for CC at HIV diagnosis and yearly thereafter.6 For WHIV, HPV-DNA tests are the screening method of choice, with pragmatic approaches like visual inspection with acetic acid (VIA) as an alternative.7 Recommended treatments for precancerous lesions include cryotherapy (Cryo) and loop excision electrical procedure (LEEP).6 However, a recent national survey indicated that only 16.4% of eligible women, regardless of HIV status, had ever been screened for CC.8 Practical challenges to achieving screening targets include overall low acceptability of CC screening, high loss to follow-up (LTFU) rates, and infrastructure and commodity constraints.9 10
We aim to quantify potential population-level health benefits of scaling up CC screening and treatment services among WHIV in care (ie, those on antiretroviral therapy (ART)) in the coming two decades and compare diagnostic and treatment options recommended by Kenyan guidelines to identify factors that could affect programmatic success. This analysis aims to support ongoing policy and implementation discussions in Kenya and the wider SSA region.
Methods
Mathematical model
We adapted an existing individual-based model coded in C++ to represent the entire Kenyan population from 1950 to 2035. The model design and mechanism has been described previously.11 12 The model runs in continuous time and simulates births, deaths, HIV infection, disease progression and treatment. Demographic events (eg, age composition in 1950, births and deaths) were assigned probabilistically, based on age-specific fertility and age and sex-specific mortality rates for Kenya from the United Nations World Population Prospects (UNWPP), accounting for changes over time (online supplementary figure S2).13 HIV-related events (eg, age and sex-specific HIV incidence, including paediatric infections), and access to ART, accounting for historic changes in CD4 eligibility, were simulated based on data from the Joint United Nations Programme (UNAIDS) for Kenya.14 CD4 count at seroconversion, disease progression and mortality were based on modelling estimates for SSA (online supplementary figure S3).15 Although individual-level ART adherence and failure were not explicitly modelled, the model recreated trends of ART coverage by age, sex and CD4 count at ART initiation over time.14
bmjgh-2019-001886supp001.pdf (639.9KB, pdf)
A validated natural history model of HPV infection and progression through mutually exclusive stages of related cervical disease was used.16 For the case of females aged 15–65, events of cervical infection with HPV were assigned probabilistically, accounting for age and HIV-specific risk (figure 1). On infection with HPV, individuals progress through the mutually exclusive stages of cervical intraepithelial neoplasia (CIN) grade 1, CIN grade 2/3, carcinoma in situ and CC, or experience spontaneous recovery from HPV infection, CIN 1 or CIN 2/3.16 Transition through disease stages or spontaneous recovery was modelled probabilistically, also accounting for individuals’ age and HIV-related risk (online supplementary table S1).16 Individuals who recover from cervical disease were at risk of new infection events, assuming no gained immunity.16
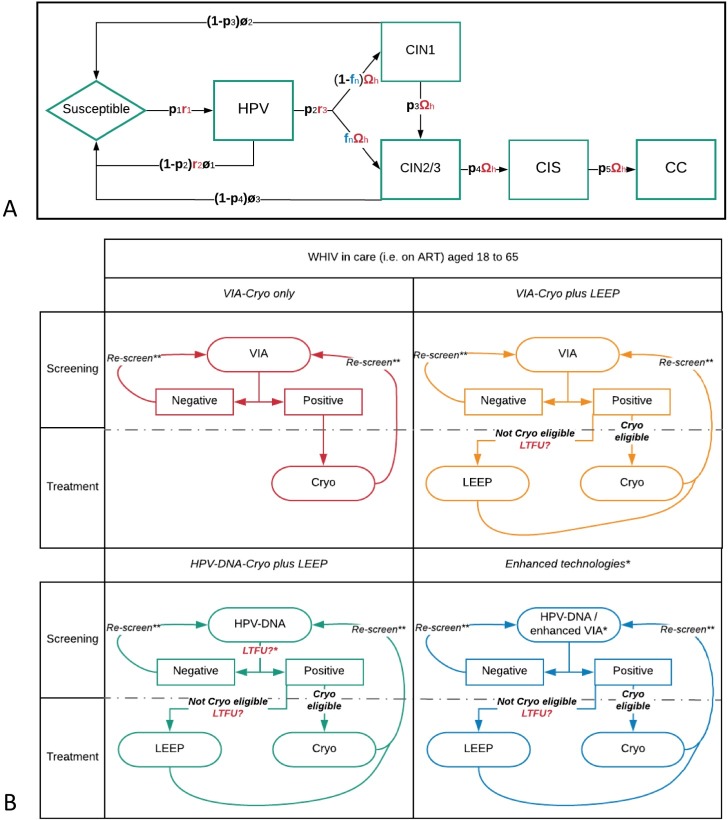
Figure 1.
(A) HPV natural history model and (B) outline of the options of care evaluated for scale-up. (A) Transition probabilities and rates vary by age and HIV status, as shown in blue and red annotations, respectively. Spontaneous recovery is possible from HPV and CIN stages. (B) Losses to follow-up (LTFU) are shown in red and occur when another visit to a health facility is necessary (ie, during HPV-DNA testing and from screening to LEEP). For definition and values of model parameters, see table 1. *Represents screening with either digitally enhanced VIA or same-day HPV-DNA. **Rescreening carried out yearly from 2023 onwards (phase II), with pool of age-eligible WHIV in care being sampled each year at random for 70% coverage. ART, antiretroviral therapy; CC, cervical cancer; CIN, cervical intraepithelial neoplasia; CIS, carcinoma in situ; Cryo, cryotherapy; HPV, human papillomavirus; LEEP, loop excision electrical procedure; LTFU, loss to follow-up; VIA, visual inspection with acetic acid; WHIV, women living with HIV.
The model makes four key assumptions about cervical disease progression among WHIV compared with HIV-negative women (figure 1A—red annotations, and online supplementary table S1):
Higher risk of HPV infection.4
Lower probability of recovering from HPV infection.4
Higher risk of progression from HPV to CIN stages.3
WHIV on ART for 2 years or more were assumed to have the same natural history as HIV-negative women.
HPV disease progression was modelled independent of CD4 count. Instead, duration on ART (≥2 years) was assumed to be a proxy of immunological reconstitution and, therefore, reduce the risk of cervical disease states, in line with recent robust evidence comparing time on ART for longer than 2 years to no or shorter term use.17
Model parameters (online supplementary table S1 and figure S1) were drawn from the literature, where available, or calibrated by exploring plausible ranges and fitting simultaneously to available Kenyan epidemiological data (online supplementary table S2).16 Epidemiological data were collated through an original systematic review and meta-analysis of age and HIV-specific prevalence of composite HPV (ie, any genotype) and of CIN 2/3, age-specific CC incidence and standardised incidence rate of CC among WHIV compared with HIV-negative women, as described in a recent publication from our group.16 Briefly, we adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses and Meta-analyses of Observational Studies in Epidemiology recommendations for systematic reviews and meta-analyses,18 19 and searched Embase, Medline and the Cochrane Library, from inception to 30 May 2018, as well as grey literature. Data on the cervical disease outcomes of interest were pooled in a meta-analysis with random effects model.16 Outcomes from the meta-analysis were used as calibration targets for the model parameters (online supplementary material - figure S4).
Scale-up of CC screening and treatment care options
From 2020 to 2040, the model compared the scale-up of the following four options to 70% coverage of WHIV in care (ie, WHIV on ART) aged between 18 and 65 (figure 1B and table 1):
Table 1.
Parameters for CC screening and treatment options
| Parameter | Description | Value (%) | Reference |
| Diagnostic performance | |||
| VIA | Values specific for detection of CIN 2+ lesions among WHIV in Kenya, irrespective of age or stage of cervical abnormality. | 28 | |
| Sensitivity | 62.70 | ||
| Specificity | 65.90 | ||
| HPV-DNA | |||
| Sensitivity | 83.60 | ||
| Specificity | 55.70 | ||
| Treatment efficacy | |||
| Cryo (eligible lesions)* | Values specific to WHIV in Kenya, irrespective of age or stage of cervical abnormality. | 70 | 20 |
| Cryo (ineligible lesions)* | Efficacy was defined as the probability of remaining cervical disease free at 24 months after treatment. | 35 | Assumed |
| LEEP (Cryo ineligible)* | For Cryo-ineligible lesions, the model assumed efficacy of Cryo to be half, in absence of empirical data. | 80.20 | 21 |
| Proportion of Cryo-ineligible* lesions | |||
| CIN 1 | CIN 1 and CIS values were assumed. CIN 2/3 value from an implementation study from the Zambia, specifically using VIA without digital enhancement or other means for increased sensitivity. | 0 | 43 |
| CIN 2/3 | 16.70 | ||
| CIS | 100 | ||
| Individuals refusing CC services | Averaged value from two Kenyan surveys, one of which specifically included diagnosed WHIV in its sample. | 13 | 22 23 |
| LTFU | |||
| From testing with HPV-DNA to obtaining of results | Testing with HPV-DNA assumed to require two clinic visits (one for testing and one to obtaining results). | 25 | 9 10 |
| From obtaining results (either with VIA or HPV-DNA) to treatment with LEEP | Treatment with LEEP assumed to require referral to a specialised clinic. | 49 | |
*The model assumed that 16.7% of individuals with CIN 2/3 status and that all with CIS and CC status had signs of Cryo ineligibility. Per clinical practice guidelines, Cryo-eligible lesions are those that do not have signs of invasive cancer (eg, bleeding), that are visible in their entirety, that do not extend more than 2–3 mm into the endocervical canal (which should be normal in appearance) and that can be fully covered by the Cryo probe.
CC, cervical cancer; CIN, cervical intraepithelial neoplasia; CIS, carcinoma in situ; Cryo, cryotherapy; HPV, human papillomavirus; LEEP, loop excision electrical procedure; LTFU, loss to follow-up; VIA, visual inspection with acetic acid; WHIV, women living with HIV.
VIA-Cryo only: screening with VIA and, for those with a positive test, treatment with Cryo on the same visit in a pragmatic way (ie, regardless of Cryo eligible or not, assuming they were the only technologies available).
VIA-Cryo plus LEEP: where, added to the above, LEEP was available for individuals with Cryo-ineligible lesions (assuming the need for referral to a specialised clinic).
HPV-DNA-Cryo plus LEEP: screening with HPV-DNA testing, which was assumed to require two visits (ie, one for testing and another to collect results) and treatment with either Cryo or LEEP. For HPV-DNA-positive women, Cryo was performed at collection of results or, if ineligible, LEEP on referral to a specialised clinic.
Enhanced technologies: where testing was assumed to be done with either same-day HPV-DNA testing or digitally enhanced VIA (ie, use of digital imaging devices to visualise VIA-stained cervix and increase its sensitivity to that of HPV-DNA testing). Treatment was performed with either Cryo during the same visit or LEEP on referral, given Cryo eligibility.
Options were modelled individually as a uniform (national-level) two-phase process scale-up strategy, to allow for comparisons. Phase I, from 2020 to 2022, consisted of a first delivery of the option to 70% of age-eligible WHIV in care. During phase II, from 2023 to 2040, delivery was scaled up to target 70% of age-eligible WHIV in care annually, including WHIV who newly started ART. The sensitivity and specificity of screening tests and the efficacy of treatment options replicated reported parameters from recent Kenyan studies among WHIV in care (table 1). Also, rates of individuals refusing CC screening services and LTFU reflect those observed in programmatic evaluations within HIV care facilities in Kenya.9 10 20–23 Individuals for whom treatment was effective and who recovered were assumed to remain cervical disease free for 24 months and, as above, go back to susceptible thereafter and be at risk of new HPV infections accounting for their age and ART status. The model assumed individuals’ LTFU during a specific year remained eligible for screening and treatment on subsequent years, as long as they remained within age eligibility. For simplicity, no modes of differentiated care (eg, offering LEEP for those recurring with cervical disease regardless of their cervical status) were simulated. Also, the present modelling analyses do not consider any scale-up in screening and treatment activities among HIV-negative women.
For each option, we quantified the following outcomes:
Number of incident CC cases and CC deaths.
Age-standardised incidence of CC by 5-year periods (eg, 2020–2024, and so on), using the WHO population and standardisation method.24
Care engagement, including numbers screened, treated and cured.
Number of screening tests performed, treatment administered and LTFU.
Outcomes were compared with a scenario with no scale-up in CC screening and treatment, henceforth referred to as status quo. Forward projections assumed a UNWPP medium variant in fertility and mortality, that HIV incidence remained stable at 2017 levels, that ART coverage reached UNAIDS 90:90:90 targets by 2020 and remained stable thereafter. All results were based on an average of 100 model runs. Sensitivity analyses were performed to account for uncertainty around target coverage, LTFU probabilities and frequency of rescreening, HIV incidence and ART coverage (online supplementary material).
To ensure transparency and reproducibility of our modelling analyses, we adhered to standardised guidelines for reporting of agent-based simulation studies, as further discussed in the online supplementary material - table S7.25 All modelling estimates refer solely to the simulated population of WHIV in care.
Patient and public involvement
No patients or members of the public were involved in the design or carry-out of the present study.
Results
Burden of HPV-related cervical disease under status quo
The model estimates that the population of WHIV in care in Kenya will increase from 0.91 million in 2020 to 1.73 million in 2040, with their mean age rising from 37.5 in 2020 to 44.1 in 2040. This will be driven by the effect of ART on extending their life expectancy. In the same period, the prevalence of HPV and CIN 2/3 is predicted to decrease from 55.8% and 7.6%, respectively, in 2020 to 47.7% and 4.0%, respectively, in 2040. This decrease by 8.1% in HPV prevalence and by 3.6% in CIN 2/3 prevalence will mainly be driven by the protective effect of ART against HPV infection and progression to CIN 2/3. In the hypothetical absence of ART only a 3.6% and 0.8% reduction in HPV and CIN 2/3 prevalence, respectively, would be observed over the 20-year period, driven by a younger population of WHIV with a higher mortality, similar to the pre-ART era.
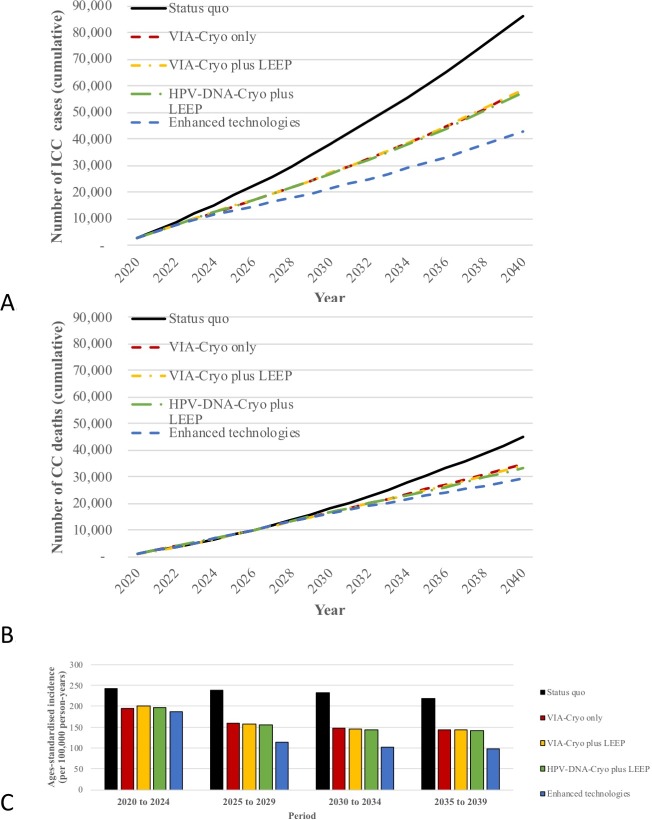
The above reduction in cervical HPV infection and precancerous lesions will result on an overall decrease in the age-standardised incidence of CC among WHIV from 241 per 100 000 women-years in 2020–2024 to 218 per 100 000 women-years in 2035–2039 (figure 2C). However, the predicted growth in population numbers will drive a rise in the yearly number of incident CC cases and deaths among WHIV in care (). These will reach a cumulative total of 86 115 CC cases and 44 742 CC-related deaths between 2020 and 2040 (figure 2A, B and supplementary material table S3).
Figure 2.
Predicted health outcomes of scaling up different options of cervical cancer (CC) screening and treatment. (A) Cumulative incident CC cases, (B) cumulative CC-related deaths, and (C) age-standardised incidence of CC per 100 000 person-years. Cryo, cryotherapy; HPV, human papillomavirus; ICC, invasive cervical cancer; LEEP, loop excision electrical procedure; LTFU, loss to follow-up; VIA, visual inspection with acetic acid.
Impact of CC screening and treatment options
The model predicts that scaling up any of the CC screening and treatment options would achieve substantial improvements in health outcomes (figure 2). VIA-Cryo only, VIA-Cryo plus LEEP and HPV-DNA-Cryo plus LEEP are expected to perform similarly, averting approximately 32.6% (28 000) of CC cases and 23.9% (10 702) of CC deaths by 2040, compared with status quo (figure 2A, B - and supplementary table S3). As a result, these three options would achieve a reduction in the age-standardised incidence of CC to 143 per 100 000 women-years by 2035–2039 (figure 2C - and supplementary table S3).
In contrast to the above, scaling up an option with enhanced technologies (ie, same-day HPV-DNA test or digitally enhanced VIA) could reduce CC cases and deaths by 50.2% (43 200) and 34.9% (15 612), respectively (figure 2A, B - and supplementary table S3). The age-standardised incidence of CC would in turn reduce to 99 per 100 000 women-years by 2035–2039 (figure 2C - and supplementary table S3).
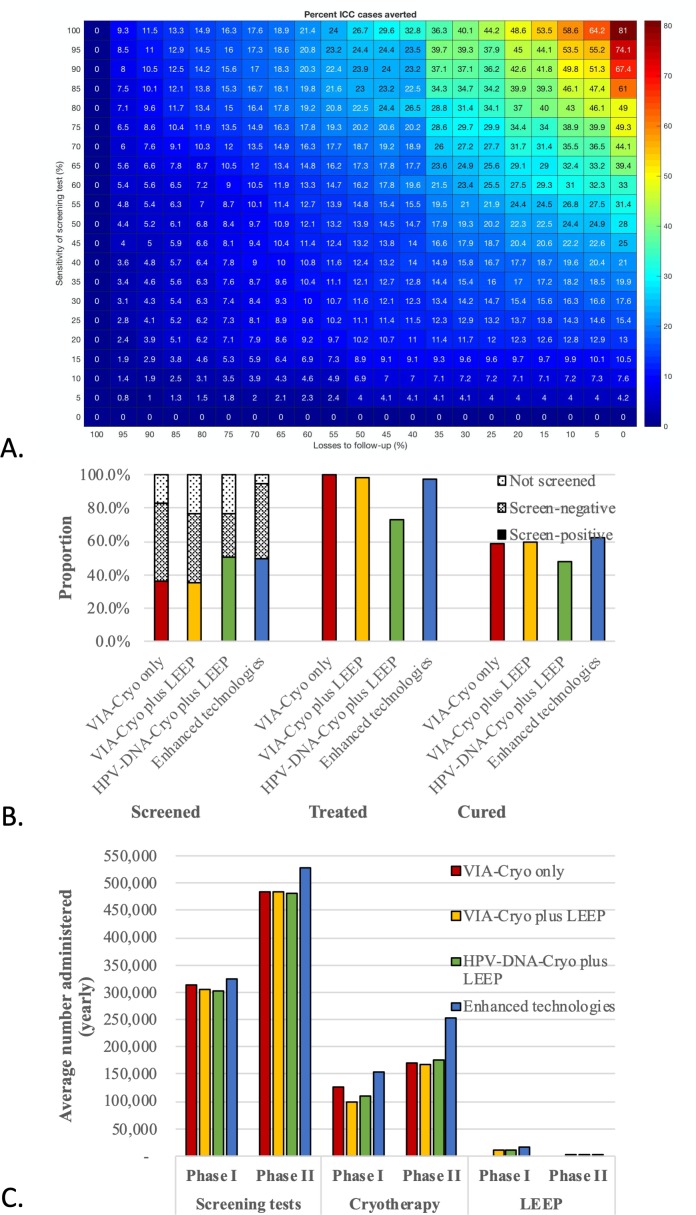
A number of factors explain the similar performance of the three options without enhanced technologies. On the one hand, LEEP availability will likely have its highest impact during phase I, when a higher proportion of individuals will present with Cryo-ineligible lesions. Yearly rescreening during later years (phase II) will allow for earlier detection of lesions at Cryo-eligible stages, thus reducing the need for LEEP (9.4% Cryo-ineligible lesions in phase I vs 1.0% in phase II). On the other hand, there will be a trade-off between the higher sensitivity of HPV-DNA testing and lower proportion of LTFU associated with same-day VIA-based options (figure 3A). Of all individual screening events over the 20-year period, an average of 35.8% (3.45 million) will be positive with VIA, compared with 50.2% (4.81 million) with an HPV-DNA test (figure 3B - and supplementary table S4). Despite the higher sensitivity of the latter, only 73.5% (3.54 million) of all of those with screen-positive results will receive treatment in the HPV-DNA-Cryo plus LEEP option (due to LTFU), compared with >97.9% (3.41 million) in both VIA-based options (figure 3A - and supplementary table S4). Moreover, the absolute cure rate (proportion cured among those treated with an actual precancerous lesion) will show a similar trend at 47.9% (0.22 million) compared with 59.1% (0.21 million), respectively (figure 3B - and supplementary table S4).
Figure 3.
Predicted impact on the health system of scaling up cervical cancer (CC) screening and treatment options. (A) Percentage of CC cases averted (vs status quo) according to sensitivity and losses to follow-up of screening tests. (B) Care engagement. Treated refers to women who receive either Cryo or loop excision electrical procedure (LEEP) among those who are screen positive (ie, includes true and false positives); Cured refers to the number of women who were cured from a cervical intraepithelial neoplasia (CIN) lesion among those who were treated and had screened true positive. (C) Average number of screening tests, and Cryo and LEEP treatments administered per year in phase I (2020–2022) and phase II (2023–2040). Cryo, cryotherapy; HPV, human papillomavirus; ICC, invasive cervical cancer; VIA, visual inspection with acetic acid.
The trade-off between LTFU and test’s sensitivity will be seen across the whole spectrum of possible scenarios. For example, if sensitivity of VIA drops to 40% (ie, lowest reported values, given its operator-dependent nature) while maintaining LTFU at 0%, only 21.0% (18 084) of CC cases will be averted. Conversely, if the sensitivity of HPV-DNA testing decreases to 75% (ie, lower bound of reported CIs in the literature) at the same time its LTFU decreases from 25% to 10%, the proportion of CC cases averted will still be higher than baseline at 38.9% (33 499).
The better health outcomes under the adoption of enhanced technologies will be the result of a substantial strengthening in care engagement. That is, treatment and true cure rates would be of 97.8% (5.13 million) and 62.7% (0.32 million), respectively (figure 3B). Neither health gains nor care engagement would be substantially improved by increasing target programmatic coverage beyond 70%. Moreover, health outcomes would not be undermined by spacing out the frequency of rescreening from yearly to three yearly (online supplementary material - table S5 and S6).
The scale-up of any of the options will have an important impact on the health system in terms of diagnostic and treatment resources needed. Approximately 9.6 million tests (either VIA or DNA) and 3.5 million treatments (either Cryo or LEEP) would be needed during the 20-year period with either of the three options that do not use enhanced technologies. To target 70% of WHIV at least once during phase I of either of these three options the health system will have to provide an average of 307 000 screening tests, 112 000 Cryo treatments and, for the case of VIA-Cryo plus LEEP and HPV-DNA-Cryo plus LEEP, 11 700 LEEP treatments per year. These annual requirements would need to be scaled up in phase II in order to maintain rescreening and coverage targets. The proportional increase would be of approximately 155% (average of 483 000) and 154% (average of 171 000 per year) for the case of screening tests and Cryo treatments (figure 3C). However, LEEP requirements would decrease by 86% (approximately 1600 per year—figure 3C), as individuals with precancerous lesions are increasingly diagnosed at earlier, Cryo-eligible stages during phase II.
The average number of yearly tests administered with the use of enhanced technologies would need to increase by approximately 163% (from 320 000 per year in phase I to 530 000 in phase II), given the aforementioned optimised care engagement (figure 3B). Similarly, the number of Cryo treatments would increase by 165% (from 154 000 to 253 000 per year), and the number of LEEP treatments would decrease by 89% (from 16 000 to 3000) (figure 3C). This intensive need for resources could be decreased by spacing out the frequency of rescreening in phase II from yearly to three yearly (online supplementary material).
Discussion
Our results show that any of the CC screening and treatment options recommended in Kenya for WHIV would translate to substantial population-level health gains. Despite the better diagnostic performance of HPV-DNA testing, its use will not result in superior health gains compared with the efficient use of VIA, unless LTFU is substantially minimised and, thus, engagement in care ensured. The adoption of enhanced CC screening technologies, such as same-day HPV-DNA testing or digitally enhanced VIA, could further improve health outcomes and care engagement. Our model also highlights that comprehensive treatment capabilities, including immediate access to Cryo and a widespread availability of facilities with LEEP capabilities, will be important to ensure maximal health benefits from the initial phases of service scale-up. As Kenya and other countries in the SSA region scale up CC screening and treatment services, there will be a need to be sensitive to health system constraints and not dismiss pragmatic options at the cost of preventable CC-related morbidity and mortality.
Our results are in line with previous evidence suggesting that integrated CC screening and treatment services into HIV care can be life-saving and that the added benefits of HPV-DNA tests, compared with VIA, depend on ensuring LTFU is minimised.26 27 These and our results highlight key implications for health systems of SSA that, like Kenya, are looking to scale up CC screening coverage and respond to the WHO’s call to eliminate CC.
First, a significant and immediate decrease in the number of CC cases and deaths is possible with the scale-up of any option of services, especially while waiting for HPV vaccination to confer population-level protection. The availability of and capacity to provide CC screening and treatment services in SSA will differ by region and over time. Even in settings where resource constraints hinder the use HPV-DNA testing, the efficient use of VIA and Cryo only could yield significant reductions in the incidence and mortality of CC at the population level. The latter, however, must be contextualised as a mean to scale up service delivery to be subsequently leveraged on to provide same-day HPV-DNA testing and/or digitally enhanced VIA.
Second, while adopting HPV-DNA tests as the primary screening method is desirable to maximise individual and population-level health outcomes, phasing in this technology will require strengthening service delivery platforms to ensure treatment with minimal LTFU. This is still not universally possible, either because of recommendations of two-step approaches (triage of HPV-DNA-positive women with VIA or cytology, which significantly decreases its diagnostic sensitivity) or resource constraints.6 28 Nevertheless, transitioning to point-of-care, screen-and-treat HPV-DNA testing or digitally enhanced VIA has been shown to be possible in SSA after establishing basic infrastructure and human resources (eg, to provide VIA and Cryo).29–33 This can be particularly feasible in HIV care facilities, as WHIV represent a population regularly accessing healthcare. Notably, digitally enhanced VIA warrants further evaluation before it can be recommended as a screening technology with similar performance to HPV-DNA testing. While mobile phone-based technologies are in development, which could facilitate its widespread adoption in resource-constrained settings, their evaluation outside trial conditions is still needed.33
Third, the availability of LEEP would be particularly important during the early stages of CC screening and treatment service scale-up. Its delivery requires specialised infrastructure to address potential complications, such as severe haemorrhages, which forestalls its availability in primary care facilities. Scale-up programmes in SSA have successfully expanded LEEP services by leveraging on provincial facilities.32 Moreover, the successful expansion of infrastructure to safely provide LEEP within low-resource HIV care facilities has been demonstrated.9 Achieving this at a national scale in Kenya, while limiting LTFU, could improve health gains during the early stages of service scale-up, when more women will present with advanced cervical lesions. Expanding LEEP availability will be an important factor to consider for screening programmes targeting WHIV, as they remain a population at high risk of both residual and recurrent CIN 2+ cervical disease,34 and thus may need repeated screening and treatment with LEEP to minimise this risk.
Lastly, given expected population growth in SSA in the upcoming decades, resource needs of any CC screening programme will substantially increase over time. Health systems will need to plan for a large upfront investment in human resources and availability of commodities to reach a target coverage of 70% and rescreening frequency. Our model suggests this could be lessened by spacing out the frequency of rescreening recommendations to three yearly, in line with global recommendations,35 without repercussions on population-level health gains. Top-level discussions around the optimal frequency of rescreening towards achieving this goal must be informed by prospective programmatic evidence, with disaggregation by age and HIV status. Thus, any scale-up must be accompanied by a robust monitoring and evaluation framework that can effectively track programme performance.
To our knowledge, this is the first time a modelling study evaluates potential population-level impact of CC screening and treatment interventions by recreating the entire population of interest, including their demographic structure, their age and HIV-specific risk of HPV disease progression and ART initiation currently and over time. Moreover, this is the first study to assess the scale-up of a country’s CC screening and treatment guidelines and identify how intervention factors (eg, availability of specific technologies, diagnostic performance, LTFU) can affect programmatic success. Our analyses highlight that a phased scale-up of CC screening and treatment services for WHIV in Kenya will be crucial to achieve the 2030 benchmarks set by the WHO towards CC elimination.5 We believe these results are applicable to other high-HIV burden countries and the directionality of the results to be applicable to HIV-negative populations. Previous models of CC among WHIV in SSA have focused on cohort approaches to produce key contributions to the cost-effectiveness literature of CC screening strategies.26 27 36 However, population-level health outcomes have not been at the core of these studies, and simulated strategies have been outside of those recommended by national guidelines (eg, once in a lifetime) and/or targeted idealised cohorts (where infection with HIV and treatment with ART happens statically at an early age).
Several limitations to our modelling analyses must be acknowledged. First, the model made a simplified assumption that WHIV on ART for ≥2 years had the same natural history of HPV-related disease as HIV-negative women, and ART adherence and failure were not explicitly modelled. Our assumptions may result in an overestimation of the protective effect of ART against HPV-related cervical disease and therefore underestimate the impact of the simulated CC screening and treatment strategies. However, the comparative impact of the different options modelled would not differ. These assumptions were based on most recent evidence in the field,3 4 17 and the model performed well when compared with HIV-specific epidemiological data from Kenya on various stages of cervical disease (online supplementary material). Second, the model assumed that HPV epidemiological data mainly collected from urban populations in Kenya were applicable to the whole country. While this may result in a different crude national-level burden of HPV-related cervical disease among WHIV (depending on urban/rural risk distribution), the proportion and directionality of our results are unlikely to change. Prospectively collected data, disaggregated by region and HIV status, will be key for better parameterising future modelling analyses. Third, no data are available from Kenya regarding population-level CC mortality rates and we thus fitted the model against available estimates for the country from The Global Burden of Disease and Globocan.37 38 This approach inherently introduces external assumptions embedded in the modelling estimates from these two sources. Any estimation of CC deaths will, as a result, be an overestimation or underestimation of the true population-level mortality. However, in our mortality fit we ensured no assumptions on changes to future trends of CC mortality were made, aiming to represent what would be seen under status quo. Data from nationally representative cancer registries are necessary to better inform future analyses. Finally, the model did not account for any vaccination-related immunity against HPV in the population. While a national campaign to vaccinate school-aged girls has been announced in Kenya, there are no estimates of coverage rates in the country.39 If a national-level HPV vaccination campaign, with a catch-up component for girls older than 15 years, was to be rolled out in the near future, the role of CC screening and treatment in preventing morbidity and mortality would be lessened over time. However, if such vaccination catch-up component is not implemented, population-level protection would be delayed for decades.40 Moreover, until nationwide vaccination programmes are fully implemented, screening and treatment of precancerous cervical lesion remains the best option to avert CC. Importantly, while immunogenicity studies suggest WHIV achieve protection levels against HPV strains similar to those of HIV-negative women,41 long-term prospective studies to assess clinical outcomes among vaccinated adolescent WHIV are missing.
Further research is needed to clarify the economic implications of scaling up national preventative programmes towards achieving the goal of CC elimination among both WHIV and HIV-negative women. No study has looked into the cost benefit and cost equity of such CC preventative interventions, nor the potential impact of increasing heard immunity against HPV (ie, as a result of vaccination) on the efficiency of screening programmes. Accurate data collection on cost elements and the above analyses would be key to inform relevant policy and funding discussions in the coming years, as countries gear up to scale up CC preventative efforts. There is also an evidence gap of large-scale trials comparing cervical disease outcomes between Cryo ablation for women with an HPV-DNA-positive test without versus already with cervical lesions. Current evidence shows the former approach can lead to higher cervical disease-free (CIN 2+) rates.35 42
Kenyan recommendations for HPV-DNA testing as the primary screening method for WHIV and the WHO call to eliminate CC are ambitious. As health systems in Kenya and the wider SSA region work to scale up CC preventative services, different options of screening and treatment technologies are at their disposal. The emphasis, however, needs to remain on providing downstream treatment for those positively diagnosed in order to avert CC cases and deaths. Our analyses show that either of these options will have a positive impact on the health of WHIV in care, but potential challenges to their implementation must be critically assessed by policymakers and programme managers. Beyond opting for better performing technologies, it will be the quality of implementation of CC screening and treatment scale-up that will drive programmatic success. Health systems choosing to scale up HPV-DNA testing will need to do so hand in hand with concerted efforts to minimise LTFU. Conversely, those choosing to scale up VIA will need to emphasise continuous provider training and technological improvements to maximise its diagnostic performance. Additionally, comprehensive treatment capabilities, including immediate access to Cryo and a widespread availability of referral facilities to perform LEEP, will be key to maximise health outcomes from the initial phases of service scale-up. Foremost, health systems in SSA must aim for an early and sustainable engagement of patients in CC screening and treatment services by efficiently employing currently available technologies, thereby effectively reducing CC morbidity and mortality.
Acknowledgments
The authors thank the funders for supporting this work as well as all national stakeholders who have supported the work by giving guidance on scope, data and interpretation. The authors acknowledge the joint centre funding from the UK Medical Research Council and the Department for International Development.
Footnotes
Handling editor: Sanni Yaya
Contributors: PNPG, MS and TBH conceived the study. MS and PNPG adapted the demographic and HIV parameters of the main individual-based model to Kenya. PNPG developed the HPV natural history model, adapted it to Kenya and carried out all modelling and statistical analyses. MS and TBH supervised all analyses and secured funding for the work. MHC provided epidemiological data for the prevalence of CIN 2/3 among WHIV. MHC, HDV, SD, KKM, BK and KM contributed to the conceptual development of the options and the contextualisation of the discussion in the Kenyan and SSA setting. PNPG did the first draft of this manuscript. All authors extensively reviewed and contributed equally to the drafting of the final version of this manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding: This study was funded by CDRF Global, MRC Centre for Global Infectious Diseases Analysis, and Foundation for the National Institutes of Health.
Disclaimer: The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request. Access to the mathematical model code and all outputs used to calculate outcomes of the present study can be granted upon request.
References
- 1.Serrano B, Brotons M, Bosch FX, et al. . Epidemiology and burden of HPV-related disease. Best Pract Res Clin Obstet Gynaecol 2018;47:14–26. 10.1016/j.bpobgyn.2017.08.006 [DOI] [PubMed] [Google Scholar]
- 2.Campos NG, Tsu V, Jeronimo J, et al. . When and how often to screen for cervical cancer in three low- and middle-income countries: a cost-effectiveness analysis. Papillomavirus Res 2015;1:38–58. 10.1016/j.pvr.2015.05.003 [DOI] [Google Scholar]
- 3.Liu G, Sharma M, Tan N, et al. . HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS 2018;32:795–808. 10.1097/QAD.0000000000001765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Looker KJ, Rönn MM, Brock PM, et al. . Evidence of synergistic relationships between HIV and human papillomavirus (HPV): systematic reviews and meta-analyses of longitudinal studies of HPV acquisition and clearance by HIV status, and of HIV acquisition by HPV status. J Int AIDS Soc 2018;21:e25110 10.1002/jia2.25110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Cervical cancer elimination strategy, 2019. Available: https://www.who.int/cancer/cervical-cancer/cervical-cancer-elimination-strategy [Accessed 5 Aug 2019].
- 6.Ministry of Health, Kenya. Kenya National cancer screening guidelines. Nairobi, 2018. [Google Scholar]
- 7.Ministry of Health, Kenya Guidelines on use of antiretroviral drugs for treating and preventing HIV in Kenya, 2018. Available: http://cquin.icap.columbia.edu/wp-content/uploads/2017/04/ICAP_CQUIN_Kenya-ARV-Guidelines-2018-Final_20thAug2018.pdf [Accessed 29 Aug 2019].
- 8.Ng'ang'a A, Nyangasi M, Nkonge NG, et al. . Predictors of cervical cancer screening among Kenyan women: results of a nested case-control study in a nationally representative survey. BMC Public Health 2018;18:1221 10.1186/s12889-018-6054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khozaim K, Orang'o E, Christoffersen-Deb A, et al. . Successes and challenges of establishing a cervical cancer screening and treatment program in Western Kenya. Int J Gynaecol Obstet 2014;124:12–18. 10.1016/j.ijgo.2013.06.035 [DOI] [PubMed] [Google Scholar]
- 10.Orang'o EO, Wachira J, Asirwa FC, et al. . Factors associated with uptake of visual inspection with acetic acid (via) for cervical cancer screening in Western Kenya. PLoS One 2016;11:e0157217 10.1371/journal.pone.0157217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smit M, Olney J, Ford NP, et al. . The growing burden of noncommunicable disease among persons living with HIV in Zimbabwe. AIDS 2018;32:773–82. 10.1097/QAD.0000000000001754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smit M, Perez-Guzman PN, Mutai KK, et al. . Mapping the current and future noncommunicable disease burden in Kenya by human immunodeficiency virus status: a modeling study. Clin Infect Dis 2019;11 10.1093/cid/ciz1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Nations World population prospects, 2019. Available: https://population.un.org/wpp/Graphs/Probabilistic/404 [Accessed 5 Aug 2019].
- 14.AIDSinfo, UNAIDS Available: http://aidsinfo.unaids.org/ [Accessed 5 Aug 2019].
- 15.Mangal TD, UNAIDS Working Group on CD4 Progression and Mortality Amongst HIV Seroconverters including the CASCADE Collaboration in EuroCoord . Joint estimation of CD4+ cell progression and survival in untreated individuals with HIV-1 infection. AIDS 2017;31:1073–82. 10.1097/QAD.0000000000001437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smit M, Perez-Guzman PN, Mutai KK, et al. . Mapping the current and future non-communicable disease burden in Kenya by HIV status: a modelling study. Clin Infect Dis 2019. 10.1093/cid/ciz1103. [Epub ahead of print: 17 Nov 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kelly H, Weiss HA, Benavente Y, et al. . Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. Lancet HIV 2018;5:e45–58. 10.1016/S2352-3018(17)30149-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, et al. . Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (moose) group. JAMA 2000;283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 20.Greene SA, De Vuyst H, John-Stewart GC, et al. . Effect of cryotherapy vs loop Electrosurgical excision procedure on cervical disease recurrence among women with HIV and high-grade cervical lesions in Kenya: a randomized clinical trial. JAMA 2019;322:1570–9. 10.1001/jama.2019.14969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greene SA, Topazian H, De Vuyst H. LEEP treatment of extensive cervical intraepithelial neoplasia in HIV-infected women. Boston; 2018: A658. [Google Scholar]
- 22.Sudenga SL, Rositch AF, Otieno WA, et al. . Knowledge, attitudes, practices, and perceived risk of cervical cancer among Kenyan women: brief report. Int J Gynecol Cancer 2013;23:895–9. 10.1097/IGC.0b013e31828e425c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosser JI, Njoroge B, Huchko MJ. Knowledge about cervical cancer screening and perception of risk among women attending outpatient clinics in rural Kenya. Int J Gynaecol Obstet 2015;128:211–5. 10.1016/j.ijgo.2014.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmad OB, Boschi-Pinto C, Lopez AD, et al. . Age standardization of rates: a new who standard;14. [Google Scholar]
- 25.Monks T, Currie CSM, Onggo BS, et al. . Strengthening the reporting of empirical simulation studies: introducing the stress guidelines. J Simul 2019;13:55–67. 10.1080/17477778.2018.1442155 [DOI] [Google Scholar]
- 26.Zimmermann MR, Vodicka E, Babigumira JB, et al. . Cost-effectiveness of cervical cancer screening and preventative cryotherapy at an HIV treatment clinic in Kenya. Cost Eff Resour Alloc 2017;15:13 10.1186/s12962-017-0075-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campos NG, Lince-Deroche N, Chibwesha CJ, et al. . Cost-effectiveness of cervical cancer screening in women living with HIV in South Africa: a mathematical modeling study. J Acquir Immune Defic Syndr 2018;79:195–205. 10.1097/QAI.0000000000001778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chung MH, McKenzie KP, De Vuyst H, et al. . Comparing Papanicolau smear, visual inspection with acetic acid and human papillomavirus cervical cancer screening methods among HIV-positive women by immune status and antiretroviral therapy. AIDS 2013;27:2909–19. 10.1097/01.aids.0000432472.92120.1b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murenzi G, Dusingize J-C, Rurangwa T, et al. . Protocol for the study of cervical cancer screening technologies in HIV-infected women living in Rwanda. BMJ Open 2018;8:e020432 10.1136/bmjopen-2017-020432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viviano M, DeBeaudrap P, Tebeu P-M, et al. . A review of screening strategies for cervical cancer in human immunodeficiency virus-positive women in sub-Saharan Africa. Int J Womens Health 2017;9:69–79. 10.2147/IJWH.S103868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Umulisa MC, Franceschi S, Baussano I, et al. . Evaluation of human-papillomavirus testing and visual inspection for cervical cancer screening in Rwanda. BMC Womens Health 2018;18:59 10.1186/s12905-018-0549-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parham GP, Mwanahamuntu MH, Kapambwe S, et al. . Population-level scale-up of cervical cancer prevention services in a low-resource setting: development, implementation, and evaluation of the cervical cancer prevention program in Zambia. PLoS One 2015;10:e0122169 10.1371/journal.pone.0122169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Urner E, Delavy M, Catarino R, et al. . A smartphone-based approach for triage of human papillomavirus-positive sub-Saharan African women: a prospective study. JMIR Mhealth Uhealth 2017;5:e72 10.2196/mhealth.6697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Debeaudrap P, Sobngwi J, Tebeu P-M, et al. . Residual or recurrent precancerous lesions after treatment of cervical lesions in human immunodeficiency virus-infected women: a systematic review and meta-analysis of treatment failure. Clin Infect Dis 2019;69:1555–65. 10.1093/cid/ciy1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santesso N, Mustafa RA, Schünemann HJ, et al. . World Health organization guidelines for treatment of cervical intraepithelial neoplasia 2-3 and screen-and-treat strategies to prevent cervical cancer. Int J Gynaecol Obstet 2016;132:252–8. 10.1016/j.ijgo.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 36.Atashili J, Smith JS, Adimora AA, et al. . Potential impact of antiretroviral therapy and screening on cervical cancer mortality in HIV-positive women in sub-Saharan Africa: a simulation. PLoS One 2011;6:e18527 10.1371/journal.pone.0018527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Institute for Health Metrics and Evaluations GBD compare. Institute for Health Metrics and Evaluation, 2014. http://www.healthdata.org/data-visualization/gbd-compare [Google Scholar]
- 38.Globocan Cancer tomorrow. Available: http://gco.iarc.fr/tomorrow/home [Accessed 13 Nov 2019].
- 39.Bruni L, Albero G, Serrano B, et al. . Human papillomavirus and related diseases report in Kenya, 2019. Available: https://hpvcentre.net/statistics/reports/KEN.pdf [Accessed 2 Aug 2019].
- 40.Jit M, Brisson M, Portnoy A, et al. . Cost-effectiveness of female human papillomavirus vaccination in 179 countries: a PRIME modelling study. Lancet Glob Health 2014;2:e406–14. 10.1016/S2214-109X(14)70237-2 [DOI] [PubMed] [Google Scholar]
- 41.Lacey CJ. HPV vaccination in HIV infection. Papillomavirus Res 2019;8:100174 10.1016/j.pvr.2019.100174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Franceschi S. Past and future of prophylactic ablation of the cervical squamocolumnar junction. Ecancermedicalscience 2015;9:527 10.3332/ecancer.2015.527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pfaendler KS, Mwanahamuntu MH, Sahasrabuddhe VV, et al. . Management of cryotherapy-ineligible women in a "screen-and-treat" cervical cancer prevention program targeting HIV-infected women in Zambia: lessons from the field. Gynecol Oncol 2008;110:402–7. 10.1016/j.ygyno.2008.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001886supp001.pdf (639.9KB, pdf)