Abstract
As many as 50% of hospitalised patients are estimated to be malnourished or at risk of malnutrition on hospital admission, but this condition often goes unrecognised, undiagnosed and untreated. Malnutrition is associated with an elevated need for continued medical interventions, higher costs of care and increased patient safety risks. Tampa General Hospital (TGH), a large teaching hospital in the southeastern USA, initiated a project to improve the quality of patient care at its institution. They did this first by focusing on improving the care quality for their malnourished patients (or patients who were at risk of malnourishment) and by using elements of the national Malnutrition Quality Improvement Initiative (MQii) Toolkit as a mechanism to measure and improve quality. The aim of this study was to evaluate the impact of quality improvement interventions on patient length of stay (LOS), infection rates and readmissions, particularly for malnourished patients. The structure of the MQii and the use of the MQii Toolkit helped staff members identify problems and systematically engage in quality improvement processes. Using the MQii Toolkit, TGH implemented a multipronged approach to improving the treatment of malnourished patients that involved creating interdisciplinary teams of staff and identifying gaps in care that could be improved through a series of changes to hospital-wide clinical workflows. They enhanced interdisciplinary coordination through increased dietitian engagement, the use of electronic health record alerts and new surgical protocols. These interventions lasted 8 months in 2016 and data reported here were collected from 985 patients before the interventions (2015) and 1046 patients after the interventions (2017). The study examines how these process changes affected LOS, infection rates and readmissions at TGH. Following implementation of these quality improvement processes, patients who were malnourished or at risk of malnutrition had a 25% reduction in LOS (from 8 to 6 days, p<0.01) and a 35.7% reduction in infection rates (from 14% to 9%, p<0.01). No statistically significant changes in readmission rates were observed. This study adds to a growing body of literature on quality improvement processes hospitals can undertake to better identify and treat malnourished patients. Hospitals and health systems can benefit from adopting similar institution-wide, quality improvement projects, while policy-makers’ support for such programmes can spur more rapid uptake of nutrition-focused initiatives across care delivery settings.
Keywords: quality improvement, teams, hospital medicine, quality measurement
Problem
Tampa General Hospital (TGH) is a private, not-for-profit, 1010-bed teaching hospital in Tampa, Florida. Located in a metropolitan area in the southeastern USA, it serves a dozen counties with a combined population of over four million people. The top three ethnic groups represented among patients admitted at the time of the study are Caucasian (52%), African-American (21%) and Hispanic (8%). Approximately 44% of its patients are 65 and older and 40% are Medicare or Medicare Advantage beneficiaries. TGH has over 7300 employees on staff and has been designated with Magnet status in nursing care for the past 4 years. It is a designated Centre of Excellence for cardiac services, cancer care and integrative medicine.
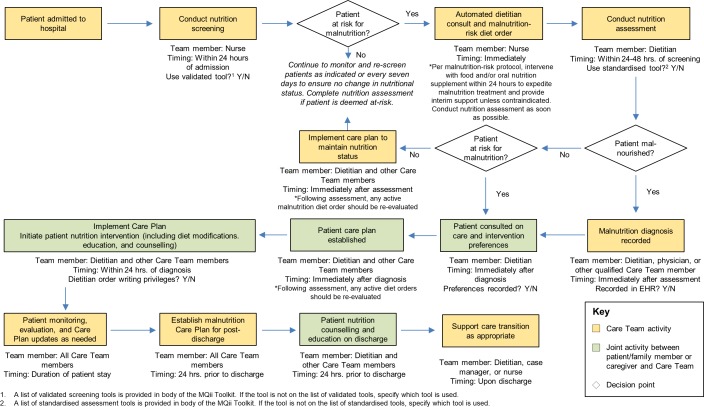
In 2015, TGH had hospital-wide goals of reducing patient length of stay (LOS), infection rates and readmission rates. As TGH began that project, they recognised that malnutrition is an underdiagnosed condition associated with adverse patient outcomes. Optimal nutrition care, as outlined in the clinical workflow in figure 1, aims to fully diagnose and manage malnutrition.1 In 2015, a dietitian-led clinical team at TGH evaluated its own clinical workflows to uncover gaps in care for malnourished patients. Barriers that they identified included:
Figure 1.
Nutrition care clinical workflow. EHR, electronic health record.
Nurses did not consistently use the validated Malnutrition Screening Tool (MST)2 that was built into the electronic health record (EHR) to identify at-risk patients at admission, thereby missing opportunities to trigger nutrition consults for patients.
Hospital clinicians were not actively using a high-quality nutrition assessment technique (such as the Nutrition-Focused Physical Examination) to confirm malnutrition in those identified as at risk.
Hospital dietitians had order writing privileges, but their orders were not thoroughly incorporated into patient treatment plans.
Malnutrition treatment recommendations were not fully integrated into the discharge planning process.
The project team identified that at baseline in 2015, 985 patients were malnourished or at risk of malnutrition, according to the Academy of Nutrition and Dietetics (“the Academy”)/American Society for Parenteral and Enteral Nutrition Malnutrition Clinical Characteristics. Out of a total of 48 636 patients admitted in 2015, 43% of patients over 65 years were malnourished or at risk of malnutrition. Using Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) data on the average cost of an inpatient stay per malnourished patient (up to US$25 200), compared with a well-nourished counterpart (US$12 500), TGH extrapolated this number and estimated its annual cost of malnutrition to be over US$12 million.3 While that number may be overstated since TGH’s patient population includes those at risk, at-risk patients often become malnourished and incur comparable costs. As a result of these analyses, TGH pursued an interdisciplinary quality improvement (QI) project focused on an institution-wide series of QI changes to rapidly improve care for patients who were malnourished or at risk. The aim of the QI project was to reduce LOS, infection rates and 30-day readmissions and associated costs within 12 months of the intervention.
Background
As many as 50% of hospitalised patients are estimated to be malnourished or at risk of malnutrition.4–6 Malnutrition is defined as the inadequate intake of nutrients, particularly protein, over time, and can occur in individuals of any weight, including those who are overweight or obese.7 Malnutrition is prevalent in highly vulnerable populations, such as individuals with chronic disease, illness, injury and poor social determinants of health.5 8 While malnutrition is rarely the primary reason for patient hospitalisations, it can compound the severity of illness and slow recovery. Studies estimate that only 8% of hospitalised patients are diagnosed with malnutrition,3 even though evidence-based nutrition interventions exist that can improve accuracy of screening and assessment and minimise the development of malnutrition-related complications.7 9
Many studies demonstrate correlations between malnutrition and elevated needs for continued medical interventions, higher costs of care and increased patient safety risks. For example, malnourished hospitalised patients experience slower wound healing, higher risks of infection and longer LOS.4 Malnourished patients are also 56% more likely to be readmitted to the hospital within 30 days and have a higher likelihood of being discharged to other healthcare facilities for ongoing health services.10 It is therefore unsurprising that hospital costs for malnourished patients are 31%–34% higher,6 with cost per readmission 26%–34% higher, than for well-nourished patients.3 11
Emerging evidence suggests malnutrition-focused QI can have a beneficial impact on these patient outcomes.7 8 12–15 A number of recent studies demonstrating successful results of QI programmes focused on malnutrition were published in a supplement to the Journal of the Academy of Nutrition and Dietetics that can be accessed at https://jandonline.org/issue/S2212-2672(19)X0003-9. While many studies evaluate the ability of specific screening tools to correctly identify malnutrition risk, few assess treatment and follow-up care activities.16–21 Studies looking at the impact of specific nutrition interventions have shown positive effects of an interdisciplinary care team developing and implementing a comprehensive nutrition care and discharge plan.8 14
Measurement
The main processes tracked as part of this initiative included nutrition screening using the EHR-embedded MST (TGH uses EPIC Hyperspace, 2019 as their EHR), adjusting the nutrition assessment policy from completion within 24–48 hours to completion within 24 hours, and making simultaneous consults for both pharmacy and dietitians for all new patients requiring total parenteral nutrition.
To assess the impact of this QI process, data were collected on several hospital-prioritised outcomes: LOS, infection rates (postoperative surgical site infections per 100 procedures) and readmissions among malnourished patients and those at risk of being malnourished. Data were collected from the EHR for a 1-year period preimplementation (January 2015–December 2015) and again for a year postimplementation (September 2016–August 2017). The earlier period provides a control group for estimating the effect of the QI interventions. This approach uses temporal variation within the hospital, controlling for constant features specific to the hospital’s setting that could affect patient outcomes. This strategy was adopted because many of the most important confounders, such as hospital characteristics and local patient populations, are relatively stable within a hospital over time.
In total, the analysis compared 985 patients who were malnourished or at risk of malnutrition during the preintervention period with 1046 patients identified as malnourished or at risk during the postintervention period. Only deidentified data from the EHR that reflected characteristics of the entire patient population were collected, thereby negating the need for randomisation or selection or individual patient consent.
Changes in the proportion of patients identified with malnutrition or malnutrition risk were assessed using a difference in proportions test to evaluate statistical significance at the 95% confidence level. To assess changes in LOS, a Mann-Whitney test was used to compare medians since these data are prone to outliers.
Design
In 2016, TGH staff began their quality improvement initiative by using the Malnutrition Quality Improvement Initiative (MQii) Toolkit, a set of resources that can be tailored to individual hospital needs.22 They did so because they recognised that their existing strategies to care for malnourished patients were insufficient. The structure of the MQii enabled them to uncover and address the nutrition needs of these patients. The toolkit helps interdisciplinary clinical teams determine gaps in identification and management of malnourished patients, undertake changes to address these gaps and coordinate care across disciplines. It also offers guidance on engaging patients and caregivers in nutrition care, including opportunities for patient education and shared decision-making. Finally, the toolkit includes a set of quality indicators that may be employed to measure project impact and success. TGH did not receive any funding to use these materials or implement a malnutrition QI project.
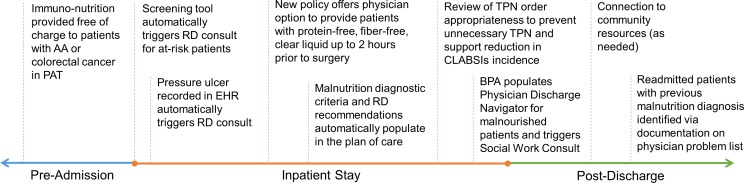
Using evidence-based best practice recommendations from the MQii Toolkit, an interdisciplinary team was established that included dietitians, nurses, physicians, pharmacists, coders, information technology (IT) staff, social workers and other health professionals. TGH’s dietitian-led team of clinicians identified a series of QI changes to implement based on the barriers to optimal malnutrition care outlined above. This project team worked to identify a range of important care gaps, raise awareness of these gaps, educate staff on best practices and adopt the changes outlined in figure 2. Patient informed consent was collected when dietitians provided education, but otherwise was not necessary to obtain from participants. The project received Institutional Review Board approval in January 2016 and was implemented from January 2016 to August 2016. Overall, TGH put in place a comprehensive series of interventions during the implementation period with the goals of closing multiple care gaps, improving clinician engagement and care processes for patients with malnutrition and malnutrition risk, and decreasing associated costs.
Figure 2.
Malnutrition quality improvement activities adopted by the hospital across the preadmission, inpatient and postdischarge care continuum. AA, aortic aneurysm; BPA, Best Practice Alert; CLABSIs, central line-associated bloodstream infections; EHR, electronic health record; NPO, ‘Nil per os’ (nothing by mouth); PAT, preadmission testing; RD, registered dietitian; TPN, total parenteral nutrition.
To raise awareness about the screening, diagnosis and treatment of malnutrition, a critical care gap identified by the TGH staff, the project team performed trainings and educational sessions over the course of 8 months with clinical staff, social workers, nurse educators and registered dietitians at their scheduled department meetings. Information was also posted to physician electronic information boards. Trainings with clinicians aimed to share data on malnutrition prevalence and best practices for nutrition care.
Additionally, the project team worked with nursing staff to ensure accurate and consistent use of the MST during the intake process to improve identification of malnutrition risk (one of the significant care gaps). The project team provided specific education sessions to the Chief Nursing Officer and various hospital councils and committees on the association between malnutrition and pressure ulcers and increased LOS. A Nurse Nutrition Council was established to review patient cases and intake documentation, confirm appropriate identification of patients at risk of malnutrition and discuss opportunities for continuous QI and collaboration. The council also supported documentation changes to foster dietitian consults for newly identified pressure ulcers. The results of the MST were also added to the patient’s summary to improve visibility within the EHR.
The project team worked with IT on additional opportunities to solve care gaps by integrating patient nutritional status and care information into the EHR. A tool was added to the EHR that automatically requested dietitian consults for patients identified as at risk based on the nurse intake screening. This allowed dietitians to see patients more rapidly for a comprehensive nutrition assessment to determine their nutritional status, form nutrition care recommendations and communicate nutritional needs to other providers. To ensure awareness among all care team members, the hospital incorporated malnutrition diagnostic criteria and intervention recommendations into the EHR-based plan of care. Support from hospital leadership was gained through partnerships and presentations to various hospital committees and TGH’s Interdisciplinary Documentation Team, which reviewed and approved all updates to EHR documentation.
The project team also established hospital-wide partnerships to address specific concerns about the malnutrition care gap. Physicians on the Medical Nutrition Committee worked with the project team to create a new ‘nothing by mouth’ (NPO) policy for surgeries. This occurred after a review of the literature demonstrated that nutrition support prior to surgery—rather than the standard order of NPO past midnight—resulted in more timely recovery, improved postsurgical outcomes and prevention of in-hospital nutritional decline.23 This protocol, which allows patients to receive a fibre-free, protein-free, clear liquid carbohydrate beverage up to 2 hours before surgery, was established in partnership with the Chief of Anesthesiology and in support of Enhanced Recovery After Surgery protocols. To implement this change, a policy document, order set and tip sheets were disseminated to nurses and physicians through trainings.
In addition to surgical patients, and as a means of further addressing the care gap related to malnutrition care, the project team sought to provide better preadmission nutrition support to a subset of at-risk patients to optimise their nutritional status and prevent infection preadmission and postadmission. TGH began providing free, early immunonutrition supplements and nutrition education to high-risk patients with colorectal cancer or abdominal aortic aneurysms in its preadmission testing process.
To improve nutrition care related to discharge planning, the project team created an automated Best Practice Alert (BPA) system to flag malnourished patients for the discharge planning team. This enabled physicians to incorporate a review of the patients’ nutritional status and postdischarge nutrition recommendations into discharge discussions. The BPA also triggered a consult for the hospital’s social workers to perform a psychosocial assessment, determine what factors may inhibit patients from eating normally (eg, access to food, inability to feed themselves) and connect them to appropriate community resources. Finally, capturing patients’ malnutrition diagnoses as part of the discharge process allowed malnutrition to be placed on patients’ problem lists for easy identification and intervention in case of readmission.
Notably, TGH used existing clinical and administrative staff to implement this series of interventions and did not need to hire new personnel. Additionally, because the tools were available from the MQii at no cost to the institution, the only implementation cost was staff time required to educate clinicians on malnutrition best practices and work with hospital leadership and IT staff to support the collection of data. The permanence of many of these changes—including the automated BPA, revised NPO procedures and tool integration into the EHR—helped to eliminate the slate of gaps in malnutrition care and ensure the sustainability of the process improvements.
Strategy
The aim of this project was to make a series of institution-wide care improvements for patients who are malnourished or at risk of malnutrition to reduce LOS, infection rates, and 30-day hospital readmissions. The project team implemented one QI cycle, focused on raising staff awareness, educating patients and improving documentation—activities that were identified as ways to improve the three primary outcome measures.
Including the Chief Operating Officer on the Medical Nutrition Committee was particularly critical for successful implementation. She helped to form partnerships between physicians and the Director of Clinical Nutrition, obtain support from the Chief of Anesthesiology and members of his team to change the NPO policy and engage Hospital Business Intelligence to assist with integrating the tool in the EHR. Her involvement will be necessary to assure success in future QI cycles of this initiative.
Results
Following the multipronged series of interventions described above, the hospital documented a 25% (2-day) overall reduction in LOS for malnourished/at-risk patients (from 8 days to 6 days, p<0.01) and a 22.2% (2-day) reduction in LOS for malnourished/at-risk patients with infections (from 9 days to 7 days, p=0.10). Infection rates among malnourished patients declined 35.7% (from 14% to 9%, p<0.01). Changes in readmission rates over time were not statistically significant. Results are reflected in table 1. Additionally, process improvement was noted for the rate at which nursing staff completed malnutrition risk screening (88% to 95% pre-to-postimplementation). There were no missing data or known contextual factors that notably led to these results.
Table 1.
Changes in malnutrition-related outcomes between preintervention (1 January 2015 to 31 December 2015) and postintervention (1 September 2016 to 31 August 2017) groups*
| Outcome | Preintervention | Postintervention | Change (p value) |
Percentage of change |
| No of patients (ages 18+ years) malnourished or at risk of malnutrition | 985 | 1046 | ||
| Infection rates among patients malnourished or at risk of malnutrition | 14% | 9% | −5 (p<0.01) |
−35.7 |
| Median LOS for patients malnourished or at risk of malnutrition | 8 days | 6 days | −2 days (p<0.01) |
−25.0 |
| Median LOS for patients malnourished or at risk of malnutrition with an infection | 9 days | 7 days | −2 days (p=0.10) |
−22.2 |
| 30–60 days of readmission rates among patients malnourished or at risk of malnutrition | 27% | 28% | +1 (p=0.58) |
3.7 |
*The data reflect the preintervention time period of 2015, and another 12 months of data in late 2016–mid 2017 (following the intervention period) to demonstrate the impacts of this QI project.
LOS, length of stay; QI, quality improvement.
Project results have garnered leadership support to implement future changes that better address patients’ clinical nutrition issues predischarge and postdischarge. These include successfully obtaining a grant and partnering with Meals on Wheels to conduct a pilot programme on dietitian-approved home-delivered meals to 200 malnourished patients postdischarge. TGH has also employed a dedicated dietitian to assist with physician documentation of malnutrition and has received approval to add supplements to the Medication Administration Record, which will better enable communication of malnutrition diagnoses and interventions provided in the hospital to the next-in-line provider. Further, TGH recently received approval to launch a food pantry at the TGH clinic where physicians and dietitians can write prescriptions for patients to pick up healthy food items.
Lessons and limitations
Given that this was only the first cycle of what could become a multicycle QI programme, we learned that much can be accomplished from implementing this initial multipronged QI initiative.
Our results support the claim that routine screening, diagnosing and treatment of patients who are malnourished or at risk of malnourishment can result in significant reductions in patients’ LOS and infection rates. The process of systematically training staff, using the EHR as a communication tool for malnutrition discharge planning and creating interdisciplinary care teams that included nutrition experts can also be important in improving patient care and decreasing costs associated with longer hospital stays.
The use of evidence-based and validated malnutrition screening and assessment tools adds to the internal validity of this study and the large sample size adds to the external validity (or generalisability). Additionally, TGH’s team of infection prevention specialists assessed the patients’ infections, so variance among the assessments by these trained professionals is unlikely to have influenced the results.
The major limitation of this study was that the staff at TGH only completed the first of what ideally would be a series of Plan–Do–Study–Act cycles. While the trends observed here are promising, the next step would be to implement another cycle of QI to ensure both that the observed gains were maintained and that we could continually improve the care of malnourished patients. Additional measurements of LOS, infection rates and medically unnecessary 30-day readmissions could be taken to see if the gains sustained were indeed held and that the experiences were not just temporal in nature. The creation of influential committees, new opportunities for clinician nutrition training and other procedural changes can continue to offer opportunities for staff to work on interdisciplinary teams and incorporate nutrition into patient care planning.
In addition, this study only included readmissions at TGH, resulting in potential under-reporting of total readmission rates. It is possible that some patients who were discharged from TGH were readmitted at local hospitals; however, since TGH is not part of a larger system, researchers could not access other hospitals’ records to follow these patients.
The lack of statistical significance in readmission rates may be due, in part, to the limited support patients receive following discharge to ensure that their nutrition needs continue to be met. TGH has found that many of its patients struggle to maintain their nutritional status postdischarge due to factors, such as food insecurity, loneliness and other social determinants of health.
Another potential limitation of this study is the lack of distinction between pre-existing and iatrogenic malnutrition. It is possible that the estimated prevalence of malnutrition and malnutrition risk includes those who became malnourished due to complications in their care. Given that screening occurs within 8–12 hours and assessment within 24 hours of admission (see figure 1), it is unlikely that these metrics include many patients who became malnourished during their hospital stays.
Conclusion
While malnutrition QI efforts have been implemented elsewhere, TGH’s QI efforts to eliminate the malnutrition care gaps using the MQii Toolkit improved on existing approaches in two ways. First, the hospital adopted a project focused on building interdisciplinary teams—including physicians, nurses, pharmacists and social workers—to improve the quality of malnutrition care, rather than only implementing dietitian-specific interventions. Despite calls for an interdisciplinary approach,24 few articles reflect the adoption and evaluation of such coordinated QI models within hospitals.
Second, TGH implemented and evaluated a suite of hospital-wide QI interventions targeted to the needs of the organisation. Previous literature has demonstrated the promise of targeted interventions,16–21 25–28 but few articles have evaluated an institution-wide, multipronged model for detecting deficiencies in malnutrition care and implementing changes to address them. This study offers a unique assessment of the implementation of such a strategy.
The benefit of close professional collaboration on behalf of patients and the opportunity to measure progress by using the MQii tools could potentially be applied to other patient conditions, such as patients who are about to have major surgeries or who need clinical support for wound healing. Documenting the importance of including physicians and nurses in establishing and meeting nutrition goals for patients was an important contribution of this project that cannot be understated.
Given the adverse impact of malnutrition on patient outcomes and the costs associated with hospital-acquired infections and increased LOS, hospitals and other care delivery organisations can use the example of TGH to adopt an interdisciplinary, nutrition-focused QI initiative. Broader uptake of such initiatives can improve outcomes and potentially decrease costs associated with undiagnosed and/or untreated malnutrition. The TGH project did not directly measure the cost reductions gained from this QI process, so cost measurement would be an important element to include in the next process cycle. Calculating the savings from a 25% reduction in LOS and a 35.7% reduction in infection rates on a targeted population would be an important addition to this study and a compelling argument for other hospitals to adopt both the MQii as an intervention and to implement process improvement.
The experience of TGH in implementing a novel approach to malnutrition QI offers a model for other hospitals to adopt. Undertaking a multipronged, hospital-wide series of interventions fuelled by an engaged interdisciplinary team is a critical success factor. Improved malnutrition care in the hospital setting has the potential to promote better health and improved outcomes for patients, address care gaps and enhance patient safety for a variety of care delivery organisations and lower the overall burden of malnutrition on the healthcare system.
Most importantly, the success of this QI programme has led to greater and more systematic changes at TGH in the quality arena. A new Chief Quality Officer has been hired and a department of quality has been established. As a result of the first malnutrition QI described here, the Chief Quality Officer has chosen malnutrition as one of the conditions that will be measured on a hospital-wide basis. Having an institutionalised department, funded and staffed by the hospital and led by a physician member of the executive team, will ensure the sustainability of QI cycles across a spectrum of conditions over time.
The staff and researchers believe that the QI infrastructure provided by this focus on malnutrition care not only showcased the improvement in malnutrition care gaps but also resulted in creating an environment that will ensure the uptake and adoption of future QI programmes. They now are in the process of successfully establishing a community of QI that can be expanded across all the hospital’s sites.
bmjoq-2019-000735supp001.pdf (22.1KB, pdf)
bmjoq-2019-000735supp002.pdf (348.6KB, pdf)
Acknowledgments
The authors thank Sara Correa, Haydy Rojas, Amit Patel and the Registered Dietitian Staff at TGH for their efforts to implement the malnutrition QI project; Meredith Ponder Whitmire, Policy Director for Defeat Malnutrition Today, for her input on the policy implications of malnutrition; and Wendy Everett and Sheila Fifer, senior advisors for Avalere Health, for their reviews of the article.
Footnotes
Contributors: KJP provided guidance and resources to support TGH’s implementation of the QI project and served as the lead author for this manuscript. KM similarly helped develop MQii materials and inform their use at TGH. BH was the lead for the project at TGH and provided expert dietetics guidance for its implementation, in addition to supporting the data collection and contributing to the authorship of the article. JB and RB helped guide and inform the MQii tools and helped identify author implications from this research. All authors have approved the final article.
Competing interests: The Toolkit used by TGH was developed as part of the MQii, a project of the Academy, Avalere Health and other stakeholders who provided guidance and expertise through a collaborative partnership. The Academy is a leading professional organisation for food and nutrition service professionals. Avalere is an advisory services organisation with expertise in evidence-based QI and quality indicator/measure development. TGH did not receive any compensation for this project or their use of MQii materials. We do not have any other conflicts of interest regarding this publication.
Patient and public involvement: Patients and/or the public were involved in the design, conduct, reporting or dissemination plans of this research. Refer to the Design section for further details.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request.
References
- 1.McCauley SM. Malnutrition care: preparing for the next level of quality. J Acad Nutr Diet 2016;116:852–5. 10.1016/j.jand.2016.03.010 [DOI] [PubMed] [Google Scholar]
- 2.Ferguson M, Capra S, Bauer J, et al. . Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999;15:458–64. 10.1016/S0899-9007(99)00084-2 [DOI] [PubMed] [Google Scholar]
- 3.Barrett ML, Bailey MK, Owens PL. Non-maternal and non-neonatal inpatient stays in the United States involving malnutrition, 2016. Rockville, MD: Agency for Healthcare Research and Quality, 2018. [Google Scholar]
- 4.Barker L, Gout B, Crowe T, et al. . Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health 2011;8:514–27. 10.3390/ijerph8020514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agarwal E, Ferguson M, Banks M, et al. . Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: results from the nutrition care day survey 2010. Clin Nutr 2013;32:737–45. 10.1016/j.clnu.2012.11.021 [DOI] [PubMed] [Google Scholar]
- 6.Curtis LJ, Bernier P, Jeejeebhoy K, et al. . Costs of hospital malnutrition. Clin Nutr 2017;36:1391–6. 10.1016/j.clnu.2016.09.009 [DOI] [PubMed] [Google Scholar]
- 7.Meehan A, Loose C, Bell J, et al. . Health system quality improvement: impact of prompt nutrition care on patient outcomes and health care costs. J Nurs Care Qual 2016;31:217–23. 10.1097/NCQ.0000000000000177 [DOI] [PubMed] [Google Scholar]
- 8.Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol 2012;24:623–7. 10.1097/BOR.0b013e328358d59b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sriram K, Sulo S, VanDerBosch G, et al. . A comprehensive Nutrition-Focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. JPEN J Parenter Enteral Nutr 2017;41:384–91. 10.1177/0148607116681468 [DOI] [PubMed] [Google Scholar]
- 10.Weiss A, Fingar KR, Barrett ML, et al. . Characteristics of hospital stays involving malnutrition, 2013. Rockville, MD: Agency for Healthcare Research and Quality, 2016. [PubMed] [Google Scholar]
- 11.Fingar K, Weiss AJ, Barrett ML, et al. . All-Cause readmissions following Hospital stays for patients with malnutrition, 2013. Rockville, MD: Agency for Healthcare Research and Quality, 2016. [PubMed] [Google Scholar]
- 12.Elia M, Normand C, Norman K, et al. . A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr 2016;35:370–80. 10.1016/j.clnu.2015.05.010 [DOI] [PubMed] [Google Scholar]
- 13.Siegel S, Fan L, Goldman A, et al. . Impact of a nutrition-focused quality improvement intervention on hospital length of stay. J Nurs Care Qual 2019;34:203–9. 10.1097/NCQ.0000000000000382 [DOI] [PubMed] [Google Scholar]
- 14.Sulo S, Feldstein J, Partridge J, et al. . Budget impact of a comprehensive nutrition-focused quality improvement program for malnourished hospitalized patients. Am Health Drug Benefits 2017;10:262–70. [PMC free article] [PubMed] [Google Scholar]
- 15.Silver HJ, Pratt KJ, Bruno M, et al. . Effectiveness of the malnutrition quality improvement initiative on practitioner malnutrition knowledge and screening, diagnosis, and timeliness of Malnutrition-Related care provided to older adults admitted to a tertiary care facility: a pilot study. J Acad Nutr Diet 2018;118:101–9. 10.1016/j.jand.2017.08.111 [DOI] [PubMed] [Google Scholar]
- 16.Cascio BL, Logomarsino JV. Evaluating the effectiveness of five screening tools used to identify malnutrition risk in hospitalized elderly: a systematic review. Geriatr Nurs 2018;39:95–102. 10.1016/j.gerinurse.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 17.Isenring EA, Banks M, Ferguson M, et al. . Beyond malnutrition screening: appropriate methods to guide nutrition care for aged care residents. J Acad Nutr Diet 2012;112:376–81. 10.1016/j.jada.2011.09.038 [DOI] [PubMed] [Google Scholar]
- 18.Hartz LLK, Stroup BM, Bibelnieks TA, et al. . ThedaCare nutrition risk screen improves the identification of Non-Intensive care unit patients at risk for malnutrition compared with the nutrition risk screen 2002. JPEN J Parenter Enteral Nutr 2019;43:70–80. 10.1002/jpen.1315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roller RE, Eglseer D, Eisenberger A, et al. . The Graz malnutrition screening (GMS): a new Hospital screening tool for malnutrition. Br J Nutr 2016;115:650–7. 10.1017/S0007114515004924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leiva Badosa E, Badia Tahull M, Virgili Casas N, et al. . Hospital malnutrition screening at admission: malnutrition increases mortality and length of stay. Nutr Hosp 2017;34:4 10.20960/nh.657 [DOI] [PubMed] [Google Scholar]
- 21.Donini LM, Poggiogalle E, Molfino A, et al. . Mini-Nutritional assessment, malnutrition universal screening tool, and nutrition risk screening tool for the nutritional evaluation of older nursing home residents. J Am Med Dir Assoc 2016;17:959.e11–959.e18. 10.1016/j.jamda.2016.06.028 [DOI] [PubMed] [Google Scholar]
- 22.Malnutrition Quality Improvement Initiative MQii toolkit, 2018. Available: http://malnutritionquality.org/mqii-toolkit.html [DOI] [PubMed]
- 23.American Society of Anesthesiologists Committee Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on standards and practice parameters.. Anesthesiology 2011;114:495–511. 10.1097/ALN.0b013e3181fcbfd9 [DOI] [PubMed] [Google Scholar]
- 24.Tappenden KA, Quatrara B, Parkhurst ML, et al. . Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult Hospital malnutrition. J Acad Nutr Diet 2013;113:1219–37. 10.1016/j.jand.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 25.Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev 2012;11:278–96. 10.1016/j.arr.2011.12.008 [DOI] [PubMed] [Google Scholar]
- 26.Philipson TJ, Snider JT, Lakdawalla DN, et al. . Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care 2013;19:S6–7. 10.1016/S0261-5614(13)60017-5 [DOI] [PubMed] [Google Scholar]
- 27.Avenell A, Smith TO, Curtain JP, et al. . Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev 2016;11:CD001880 10.1002/14651858.CD001880.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neelemaat F, Bosmans JE, Thijs A, et al. . Oral nutritional support in malnourished elderly decreases functional limitations with no extra costs. Clin Nutr 2012;31:183–90. 10.1016/j.clnu.2011.10.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2019-000735supp001.pdf (22.1KB, pdf)
bmjoq-2019-000735supp002.pdf (348.6KB, pdf)