Abstract
Introduction
Person-centred care (PCC) has become a global movement in healthcare. Despite this, the level of PCC is not routinely assessed in clinical practice. This protocol describes the adaptation and validation of the Person-Centred Practice Inventory-Staff (PCPI-S) tool that will be used to assess person-centred practices of primary healthcare providers in Malaysia.
Methods and analysis
To ensure conceptual and item equivalence, the original version of the PCPI-S will be reviewed and adapted for cultural context by an expert committee. The instrument will subsequently be translated into Malay language using the forward-backward translation method by two independent bilingual speaking individuals. This will be pretested in four primary care clinics and refined accordingly. The instrument will be assessed for its psychometric properties, such as test-retest reliability, construct and internal validity, using exploratory and confirmatory factor analysis.
Ethics and dissemination
Study findings will be disseminated to healthcare professionals and academicians in the field through publication in peer-reviewed journals and conference presentations, as well as at managerial clinic sites for practice improvement. The study was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (KKM/NIHSEC/ P18-766 (14) and Monash University Human Research Ethics Committee (2018-14363-19627).
Keywords: person-centred, primary care, healthcare provider, cultural adaptation, Malaysia, PCPI-S, study protocol
Strengths and limitations of the study.
This study is anchored on culture of person-centredness, a practice which has not been extensively explored in a middle-income country primary care setting.
The adapted questionnaire is designed to include statements relevant to all health professions and is practical for use in different care settings at individual, unit, organisational and regional levels.
Findings can be used as a guide for learning and development to support person-centred practice in workplace.
Administrative staff were excluded because some items focused on seeking practices related to clinical decision making.
The process of translating the questionnaire into a different language will be challenging, especially in maintaining the original meaning while adapting it culturally and conceptually.
Introduction
‘Person-centredness’ is a term that is becoming increasingly familiar within health and social care at a global level. This concept has been a longstanding priority in health policy and systems reform in many countries such as England, Germany, Italy, Netherlands and Spain, which advocate for healthcare institutions to place greater emphasis on the individual.1 Early works of Rogers in 1986 on person-centred theory initiated much research on improving relationship and client gain,2 with many of the practices found within the field of gerontology, such as dementia care, due to the influence of Kitwood’s scholarship.3 Over the years, there have been major advances in conceptual and theoretical developments in person-centred care (PCC), as well as a growing body of evidence evaluating processes and outcomes. The theoretical framework of PCC by McCormack and McCance focused on the therapeutic relationship between healthcare providers and service users. The therapeutic relationship is promoted by values of respect for the person, individual’s right to self-determination, mutual respect and understanding.4 This would involve working with the individual alongside health professionals to develop appropriate solutions, and for the individual to take responsibility of their own health and guide clinical decisions.
As the world’s population begin to live longer and age, the concept of PCC is even more important given the growing complexity of patient health needs. There will be a dramatic increase in healthcare consumption. PCC, with the interaction between healthcare providers and the person of the patient, can facilitate, compensate and develop more effective healthcare services for the future.5 Primary care, as the backbone of any healthcare system, is the ideal setting for provision of continuous comprehensive PCC to ensure effective delivery of healthcare.6 Indeed, services within primary care need change to be flexible to meet people’s needs in a manner that best suits them.
To achieve the goal of providing PCC, this requires good transition of care and close interdisciplinary cooperation among engaged healthcare providers.7 Studies show that PCC is achieved when healthcare providers trust each other and have high job satisfaction.8 9 This concept aptly explains that person-centredness can happen only if cultures in a healthcare setting enable staff to experience person-centredness and work in a person-centred manner.4 In Malaysia, a ‘person focus’ principle is part of the national health service goal, consistent with the ideals and principles of PCC.10 These include a focus on preventive health, patient empowerment, tailored health services, as well as an integrated services throughout care delivery.10 Importantly, with a nominal fee, primary healthcare services are accessible to all.
While there are broad policy commitments, there is limited understanding of PCC practices especially in primary care from a middle-income country. This study aims to describe the process of translation, cultural adaptation and validation of an instrument capable of exploring provider practices within a primary healthcare setting. The resulting instrument will enable healthcare teams to understand their existing work culture and take evidence informed action to move closer to a person-centred culture in Malaysia.
Theoretical framework of person-centred care
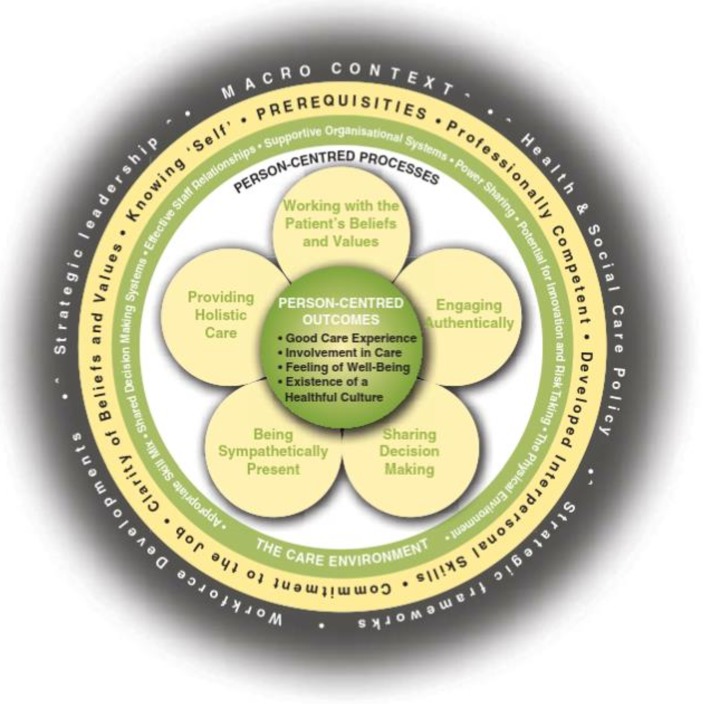
The Person-Centred Practice Framework (figure 1) by McCormack and McCance4 consolidated four domains: (1) prerequisites that focus on healthcare provider’s attributes; (2) the care environment that focuses on care delivery context; (3) care processes that focus on care delivery activities; and (4) person-centred outcomes that focus effective person-centred practice results.11 The authors suggest that staff attributes must first be considered as a prerequisite to a well-managed and supportive care environment, in order to deliver PCC.11
Figure 1.
Person-centred Practice Framework (adapted with permission from McCormack and McCance4).
To ensure the effective delivery of PCC, the authors developed the Person-entred Practice Inventory—Staff (PCPI-S) Questionnaire, a 59-item Likert scale questionnaire to examine how an individual perceive self-practice.12 The instrument contains 17 constructs in three domains—prerequisites, care environment and care processes. The tool was evaluated for its reliability and validity among nursing staff drawn from four organisations representing eight acute hospital settings.12
Methods and analysis
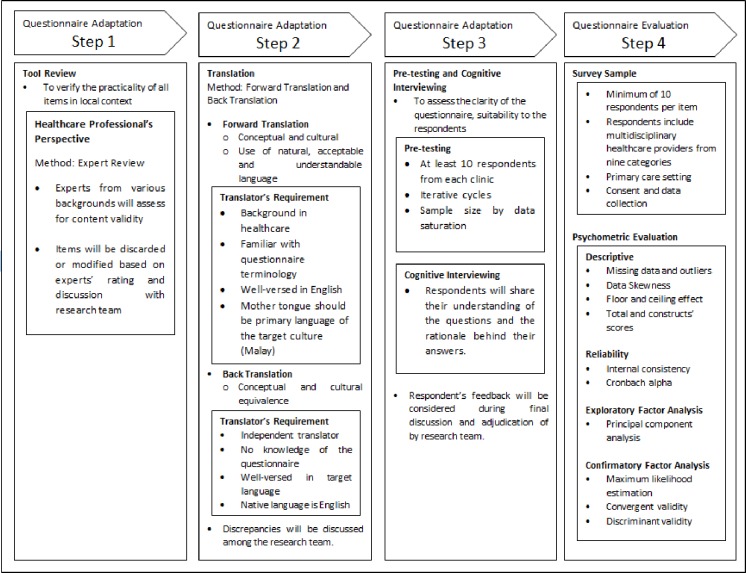
The cultural adaptation and validation of the PCPI-S questionnaire will involve a four-step process, detailed in figure 2. Details of each step are explained below.
Figure 2.
Summary of adaptation and validation process for comprehensibility, feasibility and contextualise to Malaysian setting.
Step 1: tool review
We will conduct a review to assess and determine the relevance and acceptance of items in the PCPI-S instrument for Malaysia.13 To ensure content validity, a range of experts will be recruited for the review, including:
Stakeholders to assess relevance of items in local context.
Primary healthcare providers to assess the layout standards.
Public health specialists to critique the items, drawing from their previous experience, theory and policy.
Items will be considered to be culturally, semantically and regionally appropriate, and modified accordingly based on the experts’ rating and research team discussion.
Step 2: translation
The resultant instrument will subsequently be translated into the Malay language by a health professional familiar with the instrument terminology. The translator is knowledgeable in the English-speaking culture and the primary language of the target culture, that is, Bahasa Malaysia. While translating, emphasis will be on ensuring conceptual and cultural adaptation, rather than literal translations, as well as the need to use natural and acceptable language for the broadest respondents.
To achieve cross-cultural adaptation, the guidelines for the translator include to:
Aim at conceptual equivalence of a word or phrase, rather than word-for-word translation. Original terms and definitions will be considered and translated in the most relevant way.
Strive to be simple, clear and concise in formulating a question.
Consider and avoid terms that might be considered sensitive or offensive.
Using the same approach as outlined above, the instrument will be back-translated to English by an independent translator, whose first language is English and who has no knowledge of the questionnaire contents. As for initial translation, emphasis in the back-translation will be on conceptual and cultural equivalence and not linguistic accuracy. Discrepancies will be discussed with all team members to achieve consensus.
Step 3: pretesting and cognitive interviewing
The instrument will be pretested among the nine healthcare provider categories who spend most of their work hours with service users in primary healthcare delivery. These healthcare providers are: family medicine specialists, medical doctors, pharmacists, medical assistants, nurses, occupational therapists, physiotherapists, dieticians and nutritionists. Respondents will be purposefully selected from four primary care clinics based on their willingness to participate. A total of ten respondents from each clinic (n=40) will be recruited for participation in the self-administered questionnaire and cognitive interviewing. Respondents from each clinic will be divided into groups of five and interviewed for their understanding, acceptability as well as emotional impact of each item in order to detect confusing or misleading items/terms. The pretest will be repeated until the research team believes the final version is comprehensible and can be understood by respondents, and inclusion of new respondents is unlikely to provide new insight.14
All interviews will be transcribed verbatim and coded into one of the themes identified using a standardised coding form as in table 1.15 Coding will be done by two researchers (NZB-A and PSS) using a constant comparative approach. It is anticipated that each focus group discussion will take approximately 1 hour to complete. The feedback will then be used to finalise a set of recommendations for final discussion and adjudication with team members.
Table 1.
Coding to be used to group responses into themes
| Code | Behaviour |
| 1 | Request for clarification |
| 2 | Answer with uncertainty, misunderstanding |
| 3 | Disagree with terms/sentences used |
| 4 | Don’t know/wrong interpretation |
| 5 | Not applicable/non-response |
| 6 | Translated version carries different meaning |
Step 4: psychometric evaluation
Sample size and recruitment process
To evaluate the psychometric properties of the questionnaire, the instrument will be administered in primary care clinics within 2 states of Malaysia. A minimum of 300 respondents will be recruited into the study as literature suggested a minimum of 5:1 ratio per item as adequate for factor analyses.16
To increase the response rate, a few strategies will be implemented. Research team will liaise and engage with each identified clinic on receiving state and district office approvals. During the engagement, representatives from each clinic will be briefed about the intention and aim of the study, and the sequence of data collection processes. This includes roles of representatives in questionnaire distribution and collection, as well as liaisons who will engage with research team members throughout the process. All respondents will receive an information sheet explaining about the study and will be asked to sign the consent form, which is separated from the questionnaire. Although the estimated time to complete each questionnaire is around 15–30 min, all clinics will be given 2 weeks to complete and return the questionnaires. This allows respondents to complete the questionnaire during their preferred time, thus avoid burdening the healthcare providers involved. To ensure confidentiality, respondents will receive the questionnaires in envelopes and on completion, they are to insert the completed questionnaires into the envelope and seal it. The research team will collect all completed questionnaires from the clinics.
Psychometric properties
The results will be used for both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). EFA is known as a data-driven method aiming to uncover the underlying structure of a relatively large set of variables, while CFA is a theory-driven method used for testing a priori hypothesis and application of both analyses to the same dataset should be strictly considered.17 Many researchers stressed the need to employ EFA as dimensionality of items may change when a study differs in terms of setting, culture, socioeconomic and lapse in time.18–23 Our study seeks to conduct further analysis and testing on appropriateness for use of the framework among Malaysian healthcare providers in a primary care context, and thereby explore the influential factors for a different set of target population and setting. The results will be compared against the original PCPI-S Questionnaire that was analysed using CFA.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination of our research because the subject of the instrument are healthcare providers.
Data analysis and statistics
Descriptive
A descriptive analysis of respondents’ characteristics and items score will be presented. We will determine the floor and ceiling effects of items and accept a maximum level of 15% as moderate standards pertaining to score distribution.24 Prior to analysis, missing data and outliers will be examined and treated accordingly depending on the impact towards the results. Missing data will be included in the analysis if the pattern is random and the impact is negligible.
Reliability
We will determine intraclass correlation coefficient for test-retest reliability evaluation. A value of 0.6 and above will be deemed adequate.25 The internal consistency of the instrument will be determined using Cronbach’s alpha for both total and individual constructs. Values greater than 0.70 will be accepted as evidence of adequate internal reliability.26
Exploratory factor analysis
EFA with principal component analysis will be conducted to analyse questionnaire and construct validity. Prior to EFA, we will check for multicollinearity using Bartlett’s test of sphericity and calculate sampling adequacy using Kaiser-Meyer-Olkin criterion (≥0.50).27 The number of factors will be determined using Eigenvalue>=1 (Kaiser criterion) and scree plot.27
We will use varimax rotation if multiple factors are to be found. The items’ factor loadings will be examined and the minimum individual loading required is 0.4.28 Cross loadings will be examined as well.
Confirmatory factor analysis
We will test the predefined structure with maximum likelihood estimation method. Literature recommend the use of at least one criterion from each components of absolute fit, incremental fit and parsimonious fit. In this study, the model fit will be tested using Tucker-Lewis Index (acceptable fit ≥0.9), Comparative Fit Index (acceptable fit ≥0.9), root mean square error of approximation (acceptable fit ≤0.08) and χ2/df (acceptable fit ≤5.0)29
After evaluating model fit, we will calculate the factor loadings, composite reliability (CR) for convergent reliability and average variance extracted (AVE) for discriminant validity.29 In general, factor loadings and CR should be equal to or greater than 0.7. Discriminant validity is achieved when the square root of AVE is higher than the value of correlation between constructs.30 31 Additionally, the values of correlation between constructs should not exceed 0.85.26 All analyses will be performed in AMOS (SPSS) or SPSS V.21 (IBM Corp).
Discussion
The strength of using the Person-Centred Practice Framework is that it allows practice developers to adopt a reflective approach.4 This assessment provides a snapshot of the practice setting that enables a comparison of the ‘reality of practice’ with existing practice, triggering the need for transformation.4 We are aware that several innovations have been introduced in primary care clinics in Malaysia to improve quality of care and person-centredness. Efforts have also been made to shape workplace culture towards greater professionalism, caring and teamwork.10 However, it is not clear whether these initiatives are changing healthcare providers and organisational practices. The PCPI-S questionnaire is timely to address areas of concern, as it: (1) explores in-depth person-centred values and work culture; (2) is based on an established framework; and (3) targets healthcare providers. The context and cultural influence will be taken into consideration when adapting the PCPI-S questionnaire for local use. By enhancing its applicability, clinics will be inclined to use the questionnaire findings for their practice.
We understand that PCC is not a ‘one-off’ event. Instead, it requires sustained commitment to ongoing practice development, paying attention to rigorous processes, continuous evaluation of person-centred effectiveness and celebration of successes. Only then can these ‘person-centred moments’ be transformed into ‘person-centred cultures’ of practice where satisfaction, involvement and feelings of well-being are routinely experienced.32
This study has several strengths. First, the study is anchored on concepts in a theoretical framework based on established theories. The findings from this study will be translatable to practice in the local context and can be used as a guide for learning and development to support PCC. We anticipate that administering the questionnaire itself will help promote awareness and understanding of the concept among respondents, thus fostering the conventions of ‘knowing, being and doing’.4 In ‘knowing’, respondents will be able to recognise the values of the patient and move towards clarity of one’s own values and beliefs through reflection on their practice. Fundamental to the framework, this can support subsequent work in guiding implementation of PCC towards ‘being and doing’. Nevertheless, this needs to be taken in the context of the instrument’s limitation. First, the instrument does not address administrative staff work practices but focused on practices related to clinical decision making. While the original PCPI-S tool was tested only on a sample of nursing staff,12 the translated version is designed to include statements relevant to all health professions and practical for usage in different care settings at individual, unit, organisational and regional levels.
The risk of deviating from the original questionnaire is possible. The process of translating the questionnaire to a different language will be challenging, especially in maintaining the original meaning while adapting it culturally and conceptually. Similar challenge was encountered in another study adapting PCPI-S into Norwegian.13 The same is applicable to our study and risk of conceptual misinterpretation may be present. We are aware that the whole process of adaptation and validation is time-consuming and costly. However, this study is crucial to allow data collection efforts to be comparable across different countries.
Ethics and dissemination
Informed written consent will be obtained from all respondents in the study. Respondents willing to take part in the study will be asked to sign a consent form and provided with a copy of the information sheet with detailing study background.
We aim to disseminate the findings to healthcare professionals and academicians in the field through publication in peer-reviewed journals and conference/stakeholder presentations. The datasets used and analysed during the current study are available on reasonable request with permission from Ministry of Health Malaysia.
Supplementary Material
Acknowledgments
The authors would like to declare our gratitude to the Director General of Health Malaysia for his permission to publish this paper.
Footnotes
NZB-A and PSS contributed equally.
Contributors: SS, SWHL and WHF devised the project, the main conceptual ideas and proof outline. NZB-A and PSS conceived the study and were in charge of overall direction and planning. ASJ planned and verified almost all the analytical methods. PSS, NZB-A, ASJ and TWY wrote the manuscript in consultation with SS, SWHL, WHF, NMS, TPZTB and CAM. All authors provided critical feedback and helped shape the research, analysis and manuscript. All authors of this paper have read and approved the final version submitted.
Funding: Funding for this study is from the Ministry of Health Malaysia research grant.
Disclaimer: The funder had no role in study design, data collection, analysis, decision to publish, preparation or review of the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study is part of a larger study and was registered under the National Medical Research Register, Ministry of Health Malaysia (NMRR-18-309-40447). The study was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (KKM/NIHSEC/ P18-766 (14)) and Monash University Human Research Ethics Committee (2018-14363-19627). The authors obtained permission to publish this paper from the Director General of Health Malaysia.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Paparella G. Person-Centred care in Europe: a cross-country comparison of health system performance, strategies and structures. Policy Briefing 2016. [Google Scholar]
- 2.Rogers CR. Carl Rogers on the development of the person-centered approach. Person-Centered Review 1986. [Google Scholar]
- 3.Kitwood TM. Dementia reconsidered: the person comes first. open university press, 1997. [Google Scholar]
- 4.McCormack B, McCance T. Person-Centred practice in nursing and health care: theory and practice. John Wiley & Sons, 2016. [Google Scholar]
- 5.Ekman I, Britten N, Bordin J, et al. . The person-centred approach to an ageing Society. Eur J Pers Cent Healthc 2013;1:132–7. 10.5750/ejpch.v1i1.644 [DOI] [Google Scholar]
- 6.Reeve J. Primary care redesign for person-centred care: delivering an international generalist revolution. Aust J Prim Health 2018;24:330–6. 10.1071/PY18019 [DOI] [PubMed] [Google Scholar]
- 7.Ducharme LJ, Knudsen HK, Roman PM. Emotional exhaustion and turnover intention in human service occupations: the protective role of coworker support. Sociological Spectrum 2007;28:81–104. 10.1080/02732170701675268 [DOI] [Google Scholar]
- 8.Surr CA, Smith SJ, Crossland J, et al. . Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: a repeated measures study. Int J Nurs Stud 2016;53:144–51. 10.1016/j.ijnurstu.2015.09.009 [DOI] [PubMed] [Google Scholar]
- 9.van den Pol-Grevelink A, Jukema JS, Smits CHM. Person-Centred care and job satisfaction of caregivers in nursing homes: a systematic review of the impact of different forms of person-centred care on various dimensions of job satisfaction. Int J Geriatr Psychiatry 2012;27:219–29. 10.1002/gps.2719 [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization People-centred care in low-and middle-income countries. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 11.McCormack B, McCance T. Person-Centred nursing: theory and practice. John Wiley & Sons, 2011. [Google Scholar]
- 12.Slater P, McCance T, McCormack B. The development and testing of the Person-centred Practice Inventory - Staff (PCPI-S). Int J Qual Health Care 2017;29:541–7. 10.1093/intqhc/mzx066 [DOI] [PubMed] [Google Scholar]
- 13.Bing-Jonsson PC, Slater P, McCormack B, et al. . Norwegian translation, cultural adaption and testing of the Person-centred Practice Inventory - Staff (PCPI-S). BMC Health Serv Res 2018;18:555 10.1186/s12913-018-3374-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patton MQ. Qualitative evaluation and research methods. SAGE publications, 1990. [Google Scholar]
- 15.Chernyak N, Ernsting C, Icks A. Pre-Test of questions on health-related resource use and expenditure, using behaviour coding and cognitive interviewing techniques. BMC Health Serv Res 2012;12:303 10.1186/1472-6963-12-303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comrey AL, Lee HB. A first course in factor analysis. Psychology press, 2013. [Google Scholar]
- 17.Hurley AE, Scandura TA, Schriesheim CA, et al. . Exploratory and confirmatory factor analysis: guidelines, issues, and alternatives. J Organ Behav 1997;18:667–83. [DOI] [Google Scholar]
- 18.Awang Z. Research methodology and data analysis. Penerbit Universiti Teknologi MARA Press, 2012. [Google Scholar]
- 19.Awang ZH. Research methodology for business & social science. Pusat Penerbitan Universiti, Universiti Teknologi MARA, 2010. [Google Scholar]
- 20.Hoque A, Awang Z, Jusoff K, et al. . Social business efficiency: instrument development and validation procedure using structural equation modeling. Int Bus Manag 2017;1:222–31. 10.3923/ibm.2017.222.231 [DOI] [Google Scholar]
- 21.Hoque A, Siddiqui BA, Awang ZB, et al. . Exploratory factor analysis of Entrepreneurial orientation in the context of Bangladeshi small and medium Enterprises (SMEs). European Journal of Management and Marketing Studies 2018. [Google Scholar]
- 22.Noor NM, Aziz AA, Mostapa MR, et al. . Validation of the Malay version of the inventory of functional status after childbirth questionnaire. Biomed Res Int 2015;2015:1–10. 10.1155/2015/972728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yahaya TAB, Idris K, Suandi T, et al. . Adapting instruments and modifying statements: the confirmation method for the inventory and model for information sharing behavior using social media. Management Science Letters 2018;8:271–82. 10.5267/j.msl.2018.4.021 [DOI] [Google Scholar]
- 24.Terwee CB, Bot SDM, de Boer MR, et al. . Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. 10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- 25.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 26.Hair JF, Black WC, Babin BJ, et al. . Multivariate data analysis. Upper saddle, NJ: Pearson Prentice Hall, 2006. [Google Scholar]
- 27.O'Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and velicer's MAP test. Behav Res Methods Instrum Comput 2000;32:396–402. 10.3758/BF03200807 [DOI] [PubMed] [Google Scholar]
- 28.Nunnally JC. Psychometric theory. New York: McGraw-Hill, 1978. [Google Scholar]
- 29.Hu Li‐tze, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 30.Chin WW. Issues and opinion on structural equation modeling. MIS Quarterly 1998;22. [Google Scholar]
- 31.Gefen D, Straub D, Boudreau M-C. Structural equation modeling and regression: guidelines for research practice. Communications of the Association for Information Systems 2000;4:7 10.17705/1CAIS.00407 [DOI] [Google Scholar]
- 32.McCormack B, Dewing J, McCance T. Developing person-centred care: addressing contextual challenges through practice development. Online J Issues Nurs 2011;16:3. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.