Abstract
Background
Although TKA is a common and proven reliable procedure for treating end-stage knee osteoarthritis, a minority of patients still do not achieve satisfactory levels of pain relief and functional improvement. Even though several studies have attempted to identify patients at risk of having poor clinical outcomes, few have approached this issue by considering the outcome of the patient-acceptable symptom state (PASS), defined as the value on a patient-reported outcome measure scale above which the patient deems their current symptom state acceptable.
Questions/purposes
(1) What is the proportion of patients who do not attain the PASS in pain and function at 1 year after TKA? (2) Which preoperative patient factors are associated with not achieving the PASS in pain at 1 year after TKA? (3) Which preoperative patient factors are associated with not achieving the PASS in function at 1 year after TKA?
Methods
This retrospective study is a secondary analysis of the 1-year follow-up data from a prospective, international, multicenter study of a single TKA system. Inclusion criteria for that study were patients diagnosed with primary osteoarthritis or post-traumatic arthritis and who were able to return for follow-up for 10 years; exclusion criteria were infection, osteomyelitis, and failure of a previous joint replacement. Between 2011 and 2014, 449 patients underwent TKA at 10 centers in five countries. At 1 year, 13% (58 of 449) were lost to follow-up, 2% could not be analyzed (eight of 449; missing 1-year KOOS), leaving 85% (383 of 449) for analysis here. The primary outcomes were not surpassing evidence-derived PASS thresholds in the Knee Injury and Osteoarthritis Outcome Score (KOOS) Pain and Activities in Daily Living (ADL) sub-scores. Multivariate binary logistic regressions considering preoperative demographic, radiographic, and patient-reported outcome measure data were constructed using a forward stepwise elimination algorithm to reach the simplest best-fit regression models.
Results
At 1 year after TKA, 32% of the patients (145 of 449) did not reach the PASS in KOOS Pain, 31% (139 of 449) did not reach the PASS in KOOS ADL, and 25% (110 of 449) did not achieve the PASS in either KOOS Pain or ADL. After controlling for potentially confounding variables such as gender, age, BMI, and comorbidity scores, we found that men (odds ratio 2.09; p = 0.01), and patients with less-than-advanced radiographic osteoarthritis (OR 2.09; p = 0.01) were strongly associated with not achieving the PASS in pain. After controlling for the same potentially confounding variables, we found that patients with less-than-advanced radiographic osteoarthritis (OR 2.09; p = 0.01) were also strongly associated with not achieving the PASS in function.
Conclusions
We found that patients with less severe osteoarthritis were much less likely to attain the PASS in pain and function at 1 year after TKA, and that men were much less likely to achieve the PASS in pain at 1 year after TKA. Based on these findings, surgeons should strongly consider delaying surgery in patients who present with less-than-severe osteoarthritis, with increased caution in men. Surgeons should counsel their patients on their expectations and their chances of achieving meaningful levels of pain and functional improvement. Future regional and national registry studies should assess the true proportion of patients attaining PASS in pain and function after TKA and confirm if the preoperative factors identified in this study remain significant in larger, more diverse patient populations.
Level of Evidence
Level III, therapeutic study.
Introduction
TKA is a common and proven reliable procedure for treating end-stage osteoarthritis in patients with pain and physical disability [34]. Despite low revision and complication rates, studies report that up to 20% of patients do not achieve a level of pain relief and functional increase that they deem to be satisfactory [4, 11]. The number of procedures performed per year continues to grow worldwide, and recent work has urged researchers to identify modifiable patient factors to help decrease the proportion of patients who do not achieve satisfactory outcomes [34].
In recent years, patient-reported outcome measures (PROMs) have been increasingly used to quantify the patient’s subjective experience throughout their treatment and recovery. Although PROMs offer insight into the patient-perceived outcome of an operation, they also require special considerations that are not necessary for more traditional outcome measures such as survival, reoperation, and infection. One important consideration, especially when working with a large number of PROMs, is the possibility of finding a statistically significant, yet clinically irrelevant, difference in PROM scores between study groups [23, 25]. In response to this issue, concepts such as the patient-acceptable symptom state (PASS) and minimal important change have been introduced to improve our ability to assign qualitative meaning to quantitative PROM scores.
The PASS represents the value on a PROM scale above which the patient deems his or her current symptom state satisfactory, while the minimal important change represents the smallest change in a PROM that is perceived as important to the average patient [21, 47]. The two concepts are roughly equivalent to determining if the patient is feeling better (minimal important change) or if the patient is feeling good (PASS) after the intervention. Although both concepts can readily be applied to procedures such as TKA, the PASS offers an additional advantage in that it may be used to evaluate post-intervention scores in isolation [21]. Additionally, the PASS threshold allows the estimation of the probability of a satisfactory outcome, which in health outcomes research provides an advantage over relying on the patient’s subjective satisfaction scores alone, which can be affected by a variety of factors such as gender, poor mental health, preoperative opioid use, and socioeconomic status [2, 27]. The PASS concept is an evidence-based outcome that could be used to estimate success in clinical trials and quality assessments conducted in local and national joint registries [40].
Studies reporting on the preoperative predictors of achieving the PASS in pain and function are limited [8, 24]. However, several previous studies sought to identify preoperative factors that predict achieving other outcomes such as the minimal important change or minimal clinically important improvement, a concept similar to minimal important change, in pain or function after TKA. These studies have found that factors correlated with postoperative outcomes include BMI [35], comorbidity burden [36], mental health [2, 9], functional status [36], and osteoarthritis severity [13, 49]. There is, however, no clear consensus on which factors are associated with achieving acceptable levels of pain and functional improvement after TKA, and very few of these studies used a validated PROM evaluation such as a PASS threshold as an outcome.
Therefore, we asked, (1) what is the proportion of patients who do not attain the PASS in pain and function at 1 year after TKA? (2) Which preoperative patient factors are associated with not achieving the PASS in pain at 1 year after TKA? (3) Which preoperative patient factors are associated with not achieving the PASS in function at 1 year after TKA?
Patients and Methods
Study Design and Setting
This retrospective study is a secondary analysis of the 1-year follow-up data from a prospective, international, multicenter study of a single TKA system. The aim of the original prospective study was to evaluate the safety and efficacy of vitamin-E infused polyethylene at long-term follow-up after TKA (clinicaltrials.gov NCT01374230). The data collected in the original prospective, multicenter study was well-suited for the present study because it followed a cohort of patients who received a modern, widely-used implant system; gathered data from a wide array of countries, surgeons, and practice settings; and used a robust battery of disease-specific and general-health PROMs at the preoperative and 1-year timepoints. The current study considers only 1-year data from this study because improvements in PROM scores typically reach a maximum at 1 year, and do not change significantly in subsequent years [30, 37].
Participants
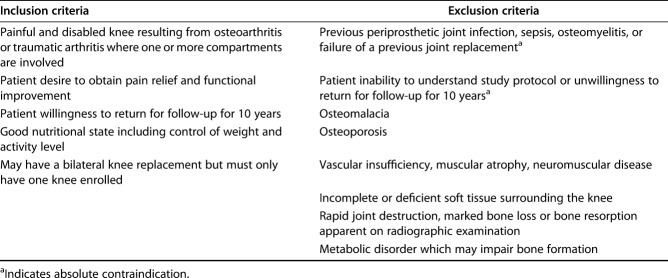
Inclusion criteria for the original study were patients with a diagnosis of primary osteoarthritis or post-traumatic arthritis who were able to return for follow-up for 10 years; absolute exclusion criteria were infection, osteomyelitis, failure of a previous joint replacement, and inability to understand the study protocol (Table 1). Between 2011 and 2014, 449 patients underwent TKA at 10 centers in five countries. Patients were enrolled in the United States (four centers; 138 patients), Denmark (two centers; 127 patients), Sweden (one center; 41 patients), Korea (two centers; 100 patients), and Australia (one center; 43 patients). At 1 year, 13% (58 of 449) were lost to follow-up, 2% could not be analyzed (eight; missing 1-year KOOS), leaving 85% (383 of 449) for analysis here. Additional criteria for inclusion in the multivariable models included complete preoperative demographic data, PROMs, and standing AP radiographs, leaving 70% (315 of 449) for inclusion in multivariate analyses. When comparing patients with incomplete versus complete preoperative data for inclusion in the multivariable models, there were no differences in age (p = 0.80) or BMI (p = 0.35), although there was a higher proportion of men in the incomplete cohort (49%, 34 of 69) than in the complete cohort (34%, 107 of 314; p = 0.01). After collection, all data were anonymized and transferred to an academic contract research organization (ACRO) at the Massachusetts General Hospital, Boston, USA, via a secure, web-based portal by all participating study sites. Informed consent was obtained from all patients, and the original study protocol was approved by the institutional review board at each respective study site and the ACRO. Additional consent was not required for the present analysis.
Table 1.
Inclusion and exclusion criteria for the prospective, multicenter study on which the current retrospective analysis is based
Description of Experiment, Treatment, or Surgery
All patients underwent unilateral TKA using vitamin E-diffused highly cross-linked polyethylene (E1) in the Vanguard® Knee System (Zimmer-Biomet, Warsaw, IN, USA). For each patient, the tibial bearing’s level of constraint was decided by the operating surgeon. Of those with complete 1-year data, 49% of the knees (186 of 383) received cruciate-retaining (CR) implants and 47% (179 of 383) received posterior-stabilized implants. The proportion of patients receiving CR differed by country (p < 0.01). Patellar resurfacings were performed at the discretion of the surgeon, resulting in 76% (292 of 383) patients with patellar resurfacing. The proportion of patients receiving patellar resurfacing differed by country (p < 0.01). All TKAs in this study were cemented. The medial parapatellar approach was used in 99% (378 of 383) of TKAs, while the lateral parapatellar and mid-vastus approaches were used in 1% (two of 383) and 1% (three of 383) of TKAs, respectively. Postoperative care and rehabilitation programs were based on the standard of care defined by each participating surgeon.
Description of the Follow-up Routine
All patients provided consent to be followed with plain standing AP and supine lateral radiographs and a set of PROMs preoperatively (median preoperative period: 1.3 weeks, interquartile range 0.1-3.5 weeks) and at 1 year postoperatively (mean follow-up period: 1.1 ± 0.3 years). Radiographs and PROMs were administered at the same clinic visits. At enrollment, basic demographic data were collected, and comorbidity classes of A, B, and C were assigned using an adaptation of the Charnley Comorbidity Classes [5].
Variables, Outcome Measures, Data Sources, and Bias
The Knee injury and Osteoarthritis Outcome Score (KOOS) is a knee-specific questionnaire including five subscales: pain, symptoms, activities of daily living (ADL), sports and recreation (Sports/Rec), and knee-related quality of life (QOL) [41]. All subscales are scored separately from 0 to 100 points, with 0 points indicating extreme knee problems, 25 points indicating severe problems, 50 points indicating moderate problems, 75 points indicating mild problems, and 100 points indicating no knee problems.
The EuroQol (EQ)-5D is a generic, health-related quality of life instrument that evaluates patients in five dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. All dimensions are combined to yield a global health index with a weighted total value ranging from -0.594 to a maximum of 1.0 [10]. The EQ-5D also includes a VAS (EQ-VAS), used to represent the general health state, that ranges from 0 (worst imaginable) to 100 (best imaginable).
The final PROM evaluated was the University of California Los Angeles Activity Score, which classifies patients’ physical activity on a 0 to 10 scale, with 10 corresponding to a high level of physical activity [28].
Through the inclusion of validated knee-specific and generic, health-related QOL PROMs, we gained a multidimensional understanding of treatment outcome from the patient’s perspective. All PROMs were administered on paper in the local languages of the study sites and transferred to the ACRO via a secure, internet-based portal.
Radiographic Analysis
Preoperative standing AP knee radiographs taken within 6 months before the index surgery were also collected and used to calculate the degree of osteoarthritis severity using the Kellgren-Lawrence osteoarthritis grading system [16]. Based on this grading system, preoperative radiographs were used to grade osteoarthritis as Grade 0 (none; no radiographic features of osteoarthritis), Grade 1 (mild: doubtful joint space narrowing and possible osteophytic lipping), Grade 2 (moderate: definite osteophytes and possible joint space narrowing on AP views), Grade 3 (severe: multiple osteophytes, definite joint space narrowing, sclerosis, and possible bony deformity), or Grade 4 (advanced: large osteophytes, marked joint space narrowing, severe sclerosis, and definite bony deformity). All radiographic readings were performed by a single board-certified orthopaedic surgeon (CSN) who was blinded to patient demographics and clinical outcomes. The reader’s intra-reader reliability score was high (kappa value > 0.9). Only three patients had Kellgren-Lawrence Grade 1 osteoarthritis in our cohort. For multivariate analyses, Kellgren-Lawrence Grades 1, 2, and 3 osteoarthritis were grouped together and compared with Kellgren-Lawrence Grade 4 for the multivariate analysis.
Statistical Analysis, Study Size
The two primary outcomes considered in this study were the PASS values for the KOOS Pain and ADL sub-scores at 1 year after TKA. The PASS values were derived from a previous international multicenter study using valid, anchor-based methodology: 84.5 for the KOOS Pain subscale and 83.0 for the KOOS ADL subscale [6]. We chose to use the PASS thresholds determined by Connelly et al. [6] because they (1) were the only evidence-derived and validated thresholds in previous studies for the KOOS at 1 year after TKA, (2) calculated PASS thresholds using an anchor-based approach, and (3) used data from a large, multicenter, international cohort.
A post-hoc power analysis was conducted to determine the number of patients needed in each group to detect a 5% or 10% difference in the proportion of patients who did not achieve the PASS in either KOOS Pain or ADL with 80% power and a Type I error rate of 0.05. To detect a 5% or 10% difference in the proportion of patients who did not achieve the PASS, a minimum of 901 or 196 patients in each group would be needed, respectively.
First, we calculated the percentages of patients who achieved the PASS in KOOS Pain, KOOS ADL, and both KOOS Pain and ADL using all patients who had a complete KOOS questionnaire at 1 year. Then, we performed Spearman’s rank correlation test for not achieving the PASS in KOOS Pain and not achieving the PASS in KOOS ADL to determine the relationship between the two outcome variables.
Next, we entered all preoperative variables into a multivariable binary logistic regression analysis which predicted not achieving the PASS in either KOOS Pain or ADL, using a forwards stepwise inclusion algorithm. Variables included in the models were demographic information, general health state, comorbidity score, generic and knee-specific PROMs, and preoperative Kellgren-Lawrence osteoarthritis grade. Only patients with complete data for all covariates were included in the multivariate analysis. KOOS Pain and KOOS ADL scores were included in the multivariate models testing not reaching the PASS in Pain and ADL because studies have shown that achievement of the PASS is not confounded by the patient’s preoperative PROM levels [39, 47].
Significance was set at p < 0.05 for all comparisons. SPSS Statistics Version 26.0 (IBM, Armonk, NY, USA) was used for all analyses.
Results
What Is the Proportion of Patients Who Do Not Attain the PASS in Pain and Function at 1 Year After TKA?
Based on the evidence-derived values, 38% of the patients (145 of 383) did not reach the PASS in KOOS Pain, 36% (139 of 383) did not reach the PASS in KOOS ADL, and 29% (110 of 383) did not achieve the PASS in either KOOS Pain or ADL. There was a strong correlation between not attaining acceptable pain relief and not attaining acceptable improvement in functional status (rs = 0.64; p < 0.01).
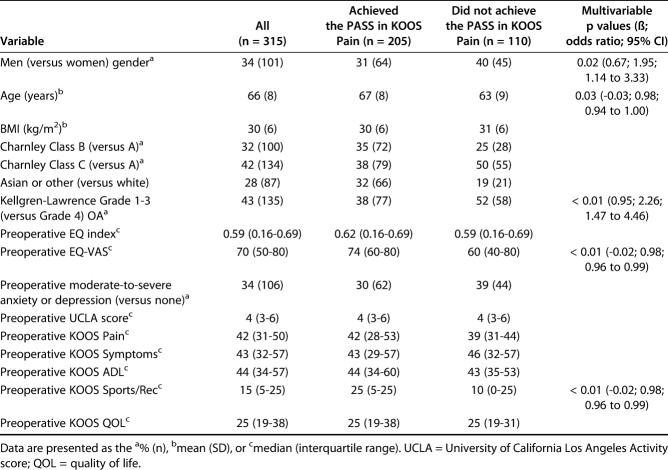
Which Preoperative Factors Are Associated with not Achieving the PASS in Pain at 1 Year After TKA?
After controlling for potentially confounding variables such as gender, age, BMI, and comorbidity scores, we found that men and patients with less-than-advanced radiographic osteoarthritis findings were strongly associated with not achieving the PASS in pain. Additionally, we found several other factors that were weakly associated with not achieving the PASS in pain, but the effect sizes of these additional factors were small. Specifically, our model demonstrated that gender (men) (odds ratio 1.95; 95% CI 1.14 to 3.33; p = 0.02), Kellgren-Lawrence Grades 1-3 (versus Grade 4) (OR 2.26; 95% CI 1.47 to 4.46; p < 0.01), younger age (OR 0.97; 95% CI 0.94 to 1.00; p = 0.03), lower preoperative EQ-VAS scores (OR 0.98; 95% CI 0.96 to 0.99; p < 0.01), and lower preoperative KOOS Sports/Rec scores (OR 0.98; 95% CI 0.96 to 0.99; p < 0.01) were independently associated with not achieving the PASS in KOOS Pain (Table 2). It is important to note that the effect sizes of younger age, lower EQ-VAS, and lower KOOS Sports/Rec scores were small, indicating that these scores likely have clinically relevant impact only when patients fall at the upper and lower extremes of the scales.
Table 2.
Demographics, preoperative PROM values, and multivariable model results for patients who did and did not achieve the PASS in KOOS Pain
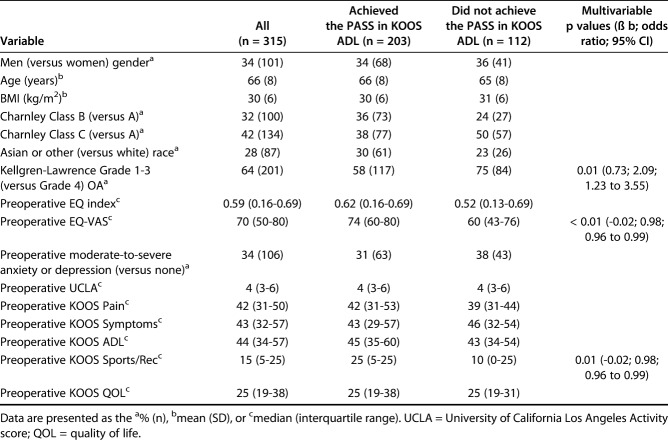
Which Preoperative Factors Are Associated with Not Achieving the PASS in Function at 1 Year After TKA?
After controlling for potentially confounding variables such as gender, age, BMI, and comorbidity scores, we found a strong association between less severe radiographic osteoarthritis findings and failure to attain acceptable functional outcomes, as well as two other factors weakly associated with not achieving the PASS in function. Specifically, we found that Kellgren-Lawrence osteoarthritis Grades 1-3 (versus Grade 4) (OR 2.09; 95% CI 1.23 to 3.55; p = 0.01), lower EQ-VAS scores (OR 0.98; 95% CI 0.96 to 0.99; p < 0.01), and lower preoperative KOOS Sports/Rec scores (OR 0.98; 95% CI 0.96 to 0.99; p = 0.01) were independently associated with not achieving the PASS in KOOS ADL (Table 3). It is important to note that the effect sizes of lower EQ-VAS and lower KOOS Sports/Rec scores were small, indicating that these scores likely have clinically relevant impact only when patients score at the upper and lower extremes of the scales.
Table 3.
Demographics, preoperative PROM values, and multivariable model results for patients who did and did not achieve the PASS in KOOS ADL
Discussion
Recent research has projected that the demand for TKA will increase by 401% by 2040 [45]. Despite generally high success rates, roughly 20% of patients still do not achieve a level of pain relief and functional increase that they deem to be satisfactory [4, 14]. As the number of people undergoing TKA continues to grow, it will be critical to identify modifiable risk factors to help improve patient satisfaction, pain relief, and functional improvement. As we attempt to address this issue, it is vital that studies consider objective, validated outcomes that are fundamentally tied to the patient’s experience, such as the PASS. Based on our international, multicenter cohort of patients treated with a modern, widely-used implant system, we found that patients with less severe osteoarthritis were less likely to reach the PASS in both pain and function. We also found that men were less likely than women to reach the PASS in pain but not function.
Limitations
Our study was not without limitations. First, only standing AP radiographs were used to assess osteoarthritis severity. A recent study has suggested the weight-bearing posterior-anterior flexed view (Rosenberg view) may be superior to the standing AP view for grading the severity of knee osteoarthritis [42]. However, this study demonstrated improved diagnostic improvement only in valgus osteoarthritis, and showed no statistically significant improvement in detection of varus or patellofemoral osteoarthritis. Additionally, other peer reviewed publications examining the effects of osteoarthritis severity on TKA outcomes have relied upon standing AP radiographs [26, 49]. Second, two studies have shown that the Kellgren-Lawrence osteoarthritis grading system may have a poor correlation with the actual severity of osteoarthritis or underestimate the actual osteoarthritis severity [1, 19]. Therefore, our study may have underestimated or misclassified the actual severity of osteoarthritis in our patient population, although the Kellgren-Lawrence osteoarthritis grading system using standing AP radiographs is still widely used, accepted, and provides high diagnostic accuracy [20].
Third, the use of the PASS concept to analyze postoperative outcomes might be limited by the instrument’s dichotomization of a continuous outcome, which can lead to a loss of information. Furthermore, the PASS may vary based on the statistical method used to calculate it [38, 46]. Slightly different PASS thresholds for the same PROM could theoretically yield differing results as to factors associated with not achieving the PASS. Despite this potential limitation, it is imperative that orthopaedic outcomes research use patient-centered outcome measures such as the PASS, which correlate PROM scores to the patient’s subjective experience without having to rely on VAS satisfaction scores, which can be affected by a variety of factors outside of the surgeon’s control [2, 27]. At the time of this study, only one evidence-based, internally validated set of PASS thresholds was available in the literature for the KOOS subscales at 1-year after TKA [6]. Despite the potential statistical limitations of PASS, it is a state-of-the-art metric tied to the patient’s experience through self-reported satisfaction, which increases confidence in the clinical relevance of our findings.
Fourth, study inclusion criteria required patient willingness to return for follow-up until 10 years after surgery, which may have introduced selection bias in our study cohort. Patients who are willing and able to return for such stringent follow-up may also be more inclined to strictly follow postoperative rehabilitation regiments. Therefore, our cohort may not be representative of the TKA population as a whole, and readers must take this into consideration when deciding if our results apply to their patients. Fifth, the prospective study on which this retrospective analysis is based was not specifically designed to answer our specific study question, and thus we are missing some important preoperative factors shown to affect pain and functional outcomes after TKA, such as smoking and opioid use [12, 50]. These known risk factors for poor clinical outcomes should be considered in addition to the risk factors identified in the current study. Finally, we considered only patients with a single TKA system, which may limit the generalizability of the findings. However, the use of a single TKA system may also be viewed as an advantage, as the implant type was eliminated as a confounding variable in the analysis. Additionally, the Vanguard knee system is a widely used and modern TKA system.
What Is the Proportion of Patients Who Do Not Attain the PASS in Pain and Function at 1 Year After TKA?
A sizable proportion of patients did not reach the PASS for pain relief, function, or both at 1 year. The current study is the first to report factors associated with not achieving the PASS in KOOS Pain and ADL at 1 year after TKA. One prospective, multicenter study from the Netherlands using the Oxford Knee Score to assess pain and function found that 26% of patients did not achieve the PASS at a mean of 3.2 years after surgery [18]. Another multicenter study from the United States assessed function via the WOMAC Physical Function subscale and found that 29% of patients did not reach the PASS at a minimum of 6 months after TKA [24]. Our study found a higher proportion of patients did not attain the PASS in pain and function than these two previous studies, although it is important to note that direct comparison between the KOOS, OKS, and WOMAC is imperfect. In addition, the current study used a more geographically and culturally diverse cohort of TKA patients than the two previous studies examining PASS after TKA, which may partially explain the differences in the rates of achieving the PASS. Specifically, our study cohort included many Scandinavians, who have been shown in one previous study to score lower on postoperative PROMs than patients in the United States and Korea [43]. The relatively high rate of patients who failed to attain the PASS in pain and function at 1 year after TKA highlights that there remains room for improvement in how surgeons identify which patients are likely or unlikely to benefit from TKA.
Which Preoperative Factors Are Associated with not Achieving the PASS in Pain at 1 Year After TKA?
Men and patients with less severe arthritis (Kellgren-Lawrence grades < 4) were strongly associated with not achieving the PASS in pain at 1 year after TKA. Younger age, lower preoperative general health scores, and lower preoperative KOOS Sports/Rec were also weakly associated with not achieving the PASS in pain, although the effect sizes of these variables were small. Our finding regarding gender disagrees with several previous studies that have shown men typically have better outcomes than women regarding pain and functional outcomes after TKA [14, 29]. Our finding may be due to the fact that men were slightly underrepresented in our study cohort, at just 37%. Nevertheless, our study’s contrary findings highlight the need for large-scale registry studies to clarify the relationship between gender and pain and functional outcome. Although we do not believe that gender should play a role in the surgeon’s decision to perform TKA, it is imperative that surgeons use the available data to manage patient expectations. With regard to preoperative osteoarthritis grade, our findings are consistent with previous single-center [48] and multicenter studies [15, 49] that have reported worse pain outcomes in patients with less severe osteoarthritis grade before TKA. However, other studies have shown no associations between preoperative osteoarthritis severity and pain outcomes [26, 33]. The diverging findings between these studies may be due to differences in the outcome measures used, radiologic criteria for osteoarthritis, and differing follow-up times after TKA. Our multinational study provides further evidence for the association between less severe osteoarthritis and worse pain outcomes after TKA using the PASS, a known, clinically relevant outcome. Given the fact that osteoarthritis severity is a potentially modifiable risk factor, we recommend that surgeons carefully consider osteoarthritis severity while counselling their patients and consider delaying TKA in patients with less severe osteoarthritis, especially in patients with Kellgren-Lawrence Grades 1 or 2. Our findings that younger age, lower preoperative EQ-VAS scores, and lower preoperative KOOS Sports/Rec likely have little clinical utility based on their small effect sizes in our cohort. The small effect of younger age on attaining PASS in pain could be related to higher expectations for postoperative outcomes, as has been demonstrated by several previous studies [32, 44]. As TKA becomes more common in the younger population [22], it will be crucial to gain a better understanding of the role young age plays in pain and functional outcomes after TKA. Previous large multicenter studies have shown that lower self-reported general health predicted poor outcomes in pain after TKA [3, 29]. Our findings weakly support this notion, but further research is needed to elucidate this relationship. The clinical utility of the KOOS Sports/Rec score in determining likelihood of attaining the PASS in pain is doubtful given that the score may have limited applicability to patients undergoing TKA [31].
Which Preoperative Factors Are Associated with Not Achieving the PASS in Function at 1 Year After TKA?
We found that several factors were weakly associated with poorer functional outcomes, but the strongest association was with less severe radiographic findings. Our findings are consistent with previous single-center [7] and multicenter [15, 17] studies, which have demonstrated that those with more severe osteoarthritis experienced greater improvements in function. However, other studies have shown no associations between preoperative osteoarthritis severity and pain and functional outcomes [26, 33]. These studies varied based on the outcome measures used, radiologic criteria for osteoarthritis, and differing follow-up times after TKA, which may partially explain the inconsistency in findings. Our study is the first to examine the impact of osteoarthritis severity on the PASS in function specifically, and therefore adds important evidence that the association between less severe osteoarthritis grade and worse functional outcomes has a clinically relevant impact. Given the fact that OA severity is a potentially modifiable risk factor, we recommend that surgeons carefully consider osteoarthritis severity while counselling their patients and consider delaying TKA in patients with less severe osteoarthritis, especially in patients with Kellgren-Lawrence Grades 1 or 2. Our findings that lower preoperative general health scores and lower preoperative KOOS Sports/Rec likely have little clinical utility based on their small effect sizes in our cohort. With regard to general health, several studies have shown that lower self-reported general health are associated with worse functional outcomes after TKA [3, 29]. Our findings weakly support this relationship, and further research on the topic is warranted. Based on the preoperative KOOS Sports/Rec score’s minimal effect size and the metric’s limited applicability to TKA patients [31], its clinical utility is likely minimal.
Conclusions
In conclusion, we found that patients with less severe osteoarthritis were much less likely to attain the PASS in pain and function at 1 year after TKA than patients with more severe disease, and that men were much less likely than women to achieve the PASS in pain at 1 year after TKA. Based on these findings, surgeons should strongly consider delaying surgery in patients who present with less-than-severe osteoarthritis, with increased caution in men. Based on our findings, we recommend surgeons use our results to guide patient expectations by counseling their patients on their chances of achieving meaningful levels of pain and functional improvement. Future regional and national registry studies should assess the true proportion of patients attaining PASS in pain and function after TKA and confirm if the preoperative factors identified in this study remain significant in larger, more diverse patient populations.
Acknowledgments
None.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
One of the authors certifies that he (AT), or a member of his immediate family, has received personal fees in an amount of USD (USD 10,000 to USD 100,000) from Zimmer Biomet (Warsaw, IN, USA), advisory board membership, and personal fees for lectures including service on speakers’ bureaus. The institution of one or more of the authors (JWC, VPG, PR, CRB, HM) has received, during the study period, research support funding, in an amount of USD 100,001 to USD 1,000,000 from Zimmer Biomet.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Harris Orthopedics Laboratory, Massachusetts General Hospital, Boston, MA, USA.
References
- 1.Abdelaziz H, Balde OM, Citak M, Gehrke T, Magan A, Haasper C. Kellgren-Lawrence scoring system underestimates cartilage damage when indicating TKA: preoperative radiograph versus intraoperative photograph. Arch Orthop Trauma Surg. 2019;139:1287-1292. [DOI] [PubMed] [Google Scholar]
- 2.Ali A, Lindstrand A, Sundberg M, Flivik G. Preoperative anxiety and depression correlate with dissatisfaction after total knee arthroplasty: a prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J Arthroplasty. 2017;32:767–770. [DOI] [PubMed] [Google Scholar]
- 3.Baker PN, Deehan DJ, Lees D, Jameson S, Avery PJ, Gregg PJ, Reed MR. The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement. J Bone Joint Surg Br. 2012;94:1058–1066. [DOI] [PubMed] [Google Scholar]
- 4.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 6.Connelly JW, Galea VP, Rojanasopondist P, Matuszak SJ, Ingelsrud LH, Nielsen CS, Bragdon CR, Huddleston JI, Malchau H, Troelsen A. Patient Acceptable symptom state at 1 and 3 years after total knee arthroplasty: thresholds for the Knee Injury and Osteoarthritis Outcome Score (KOOS). J Bone Joint Surg Am. 2019;101:995–1003. [DOI] [PubMed] [Google Scholar]
- 7.Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009;68:642–647. [DOI] [PubMed] [Google Scholar]
- 8.Escobar A, García Pérez L, Herrera-Espiñeira C, Aizpuru F, Sarasqueta C, Gonzalez Sáenz de Tejada M, Quintana JM, Bilbao A. Total knee replacement: Are there any baseline factors that have influence in patient reported outcomes? J Eval Clin Pract. 2017;23:1232–1239. [DOI] [PubMed] [Google Scholar]
- 9.Escobar A, Quintana JM, Bilbao A, Azkárate J, Güenaga JI, Arenaza JC, Gutierrez LF. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford) . 2007;46:112–119. [DOI] [PubMed] [Google Scholar]
- 10.EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. [DOI] [PubMed] [Google Scholar]
- 11.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32:3854–3860. [DOI] [PubMed] [Google Scholar]
- 12.Halawi MJ, Allen DA, Baron S, Savoy L, Williams VJ, Cote MP. Tobacco smoking independently predicts lower patient-reported outcomes: new insights on a forgotten epidemic. J Arthroplasty. 2019; 34:S144-S147. [DOI] [PubMed] [Google Scholar]
- 13.Hoorntje A, Witjes S, Koenraadt KLM, Aarts R, Weert T De, van Geenen RCI. More severe preoperative Kellgren-Lawrence grades of knee osteoarthritis were partially associated with better postoperative patient-reported outcomes in TKA patients. J Knee Surg. 2019;32:211–217. [DOI] [PubMed] [Google Scholar]
- 14.Judge A, Arden NK, Cooper C, Kassim Javaid M, Carr AJ, Field RE, Dieppe PA. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford) . 2012;51:1804–1813. [DOI] [PubMed] [Google Scholar]
- 15.Kahn TL, Soheili A, Schwarzkopf R. Outcomes of total knee arthroplasty in relation to preoperative patient-reported and radiographic measures: data from the Osteoarthritis Initiative. Geriatr Orthop Surg Rehabil. 2013;4:117-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keurentjes JC, Fiocco M, So-Osman C, Onstenk R, Koopman-Van Gemert AWMM, Pöll RG, Kroon HM, Vliet Vlieland TPM, Nelissen RG. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PLoS One. 2013;8:e59500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keurentjes JC, Van Tol FR, Fiocco M, So-Osman C, Onstenk R, Koopman-Van Gemert AWMM, Pöll RG, Nelissen RGHH. Patient acceptable symptom states after total hip or knee replacement at mid-term follow-up: Thresholds of the Oxford hip and knee scores. Bone Joint Res . 2014;3:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kijowski R, Blankenbaker D, Stanton P, Fine J, De Smet A. Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol. 2006;187:794–799. [DOI] [PubMed] [Google Scholar]
- 20.Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kvien TK, Heiberg T, Hagen KB. Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): what do these concepts mean? Ann Rheum Dis. 2007;66:iii40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Losina E, Katz JN. Total knee arthroplasty on the rise in younger patients: Are we sure that past performance will guarantee future success? Arthritis Rheum. 2012;64:339-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maltenfort M, Díaz-Ledezma C. Statistics in brief: minimum clinically important difference-availability of reliable estimates. Clin Orthop Relat Res. 2017;475:933–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maxwell JL, Felson DT, Niu J, Wise B, Nevitt MC, Singh JA, Frey-Law L, Neogi T. Does clinically important change in function after knee replacement guarantee good absolute function? The multicenter osteoarthritis study. J Rheumatol. 2014;41:60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. 2014;312:1342–1343. [DOI] [PubMed] [Google Scholar]
- 26.Meding JB, Ritter MA, Faris PM, Keating EM, Harris W. Does the preoperative radiographic degree of osteoarthritis correlate to results in primary total knee arthroplasty? J Arthroplasty. 2001;16:13–16. [DOI] [PubMed] [Google Scholar]
- 27.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elb Surg. 2016;25:619-623. [DOI] [PubMed] [Google Scholar]
- 28.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neuburger J, Hutchings A, Black N, van der Meulen JH. Socioeconomic differences in patient-reported outcomes after a hip or knee replacement in the English National Health Service. J Public Health (Oxf) . 2013;35:115–124. [DOI] [PubMed] [Google Scholar]
- 30.Neuprez A, Neuprez AH, Kaux J-F, Kurth W, Daniel C, Thirion T, Huskin J-P, Gillet P, Bruyère O, Reginster J-Y. Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin Rheumatol. [Published online ahead of print November 13, 2019]. DOI: 10.1007/s10067-019-04811-y. [DOI] [PubMed]
- 31.Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Rel Res. 2006; 452:35-43. [DOI] [PubMed] [Google Scholar]
- 33.Perry KI, Strasser NL, Harmsen WS, Pagnano MW, Trousdale RT. Minimal preoperative degenerative arthritis may not predict poor TKA outcome. Orthopedics. 2015;38:e681-4. [DOI] [PubMed] [Google Scholar]
- 34.Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, Carr A, Beard D. Knee replacement. Lancet. 2018;392:1672–1682. [DOI] [PubMed] [Google Scholar]
- 35.Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23:795–800. [DOI] [PubMed] [Google Scholar]
- 36.Ramaesh R, Jenkins P, Macdonald D, Howie C, Lane J V., Knight S. Personality, function and satisfaction in patients undergoing total hip or knee replacement. J Orthop Sci. 2014;19:275–281. [DOI] [PubMed] [Google Scholar]
- 37.Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP. No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2018;33:2322-2329. [DOI] [PubMed] [Google Scholar]
- 38.Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61:102–109. [DOI] [PubMed] [Google Scholar]
- 39.Riddle DL, Stratford PW, Binkley JM. Sensitivity to change of the Roland-Morris Back Pain Questionnaire: part 2. Phys Ther. 1998;78:1197–207. [DOI] [PubMed] [Google Scholar]
- 40.Roos EM, Boyle E, Frobell RB, Lohmander LS, Ingelsrud LH. It is good to feel better, but better to feel good: whether a patient finds treatment “successful” or not depends on the questions researchers ask. Br J Sports Med . 2019;53:1474-1478. [DOI] [PubMed] [Google Scholar]
- 41.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sport Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 42.Rueckl K, Boettner F, Maza N, Runer A, Bechler U, Sculco P. The posterior-anterior flexed view is better than the anterior-posterior view for assessing osteoarthritis of the knee. Skeletal Radiol. 2018;47:511–517. [DOI] [PubMed] [Google Scholar]
- 43.Sauder N, Galea VP, Rojanasopondist P, Colon Iban YE, Florissi IS, Nielsen CS, Kappel A, Bragdon CR, Malchau H, Troelsen A. Regional differences between the US, Scandinavia, and South Korea in patient demographics and patient-reported outcomes for primary total knee arthroplasty. Arch Orthop Trauma Surg. 2020;140:93-108. [DOI] [PubMed] [Google Scholar]
- 44.Scott CEH, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94:974-981. [DOI] [PubMed] [Google Scholar]
- 45.Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: future projections to 2020-2040 using the National Inpatient Sample. J Rheumatol. 2019; 46:1134-1140. [DOI] [PubMed] [Google Scholar]
- 46.Tubach F, Giraudeau B, Ravaud P. The variability in minimal clinically important difference and patient acceptable symptomatic state values did not have an impact on treatment effect estimates. J Clin Epidemiol. 2009;62:725–728. [DOI] [PubMed] [Google Scholar]
- 47.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, Bombardier C, Felson D, Hochberg M, van der Heijde D, Dougados M. Evaluation of clinically relevant states in patient reported outcomes in knee and hip osteoarthritis: the patient acceptable symptom state. Ann Rheum Dis. 2005;64:34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valdes AM, Doherty SA, Zhang W, Muir KR, Maciewicz RA, Doherty M. Inverse relationship between preoperative radiographic severity and postoperative pain in patients with osteoarthritis who have undergone total joint arthroplasty. Semin Arthritis Rheum. 2012;41:568–575. [DOI] [PubMed] [Google Scholar]
- 49.van de Water RB, Leichtenberg CS, Nelissen RGHH, Kroon HM, Kaptijn HH, Onstenk R, Verdegaal SHM, Vliet Vlieland TPM, Gademan MGJ. Preoperative radiographic osteoarthritis severity modifies the effect of preoperative pain on pain/function after total knee arthroplasty: results at 1 and 2 years postoperatively. J Bone Joint Surg Am . 2019;101:879–887. [DOI] [PubMed] [Google Scholar]
- 50.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011; 93:1988-1993. [DOI] [PubMed] [Google Scholar]